Can stress cause hypoglycemia
The Hidden Dangers of Low Blood Glucose Levels and Chronic Stress
To maintain good overall health, it is important to pay greater attention to your blood sugar levels. This is because any changes in your blood sugar levels may be an indication that you are suffering from adrenal fatigue. In fact, during the advanced stages of adrenal fatigue, you may suffer from low blood glucose levels or hypoglycemia. In this case, proper management of your blood sugar levels is needed to stop hypoglycemia symptoms and prevent adrenal exhaustion from becoming far worse.
What Does Having Low Blood Glucose Levels Mean?
Hypoglycemia is a condition wherein a person is suffering from significantly low blood glucose or blood sugar levels. Typically, when you eat food, your body readily breaks down carbohydrates into different types of sugar molecules. One of these is glucose.
Glucose happens to be the body’s main energy source. However, it is not able to enter the cells of most of the body’s tissues without the help of insulin, which is secreted by the pancreas. Insulin allows glucose to properly enter the cells so that cells can be nourished and function properly. Meanwhile, any extra glucose is stored in the muscles and liver in the form of glycogen.
If you have not eaten for hours and your blood sugar drops, the glucagon hormone from the pancreas signals your liver to break down the glycogen and release glucose into your bloodstream. Cortisol can also be released from the adrenal glands to raise blood sugar levels as well. Typically, this results in an elevated blood sugar level in the body. If it doesn’t, it means that you have hypoglycemia, indicating that your blood sugar level is dangerously low.
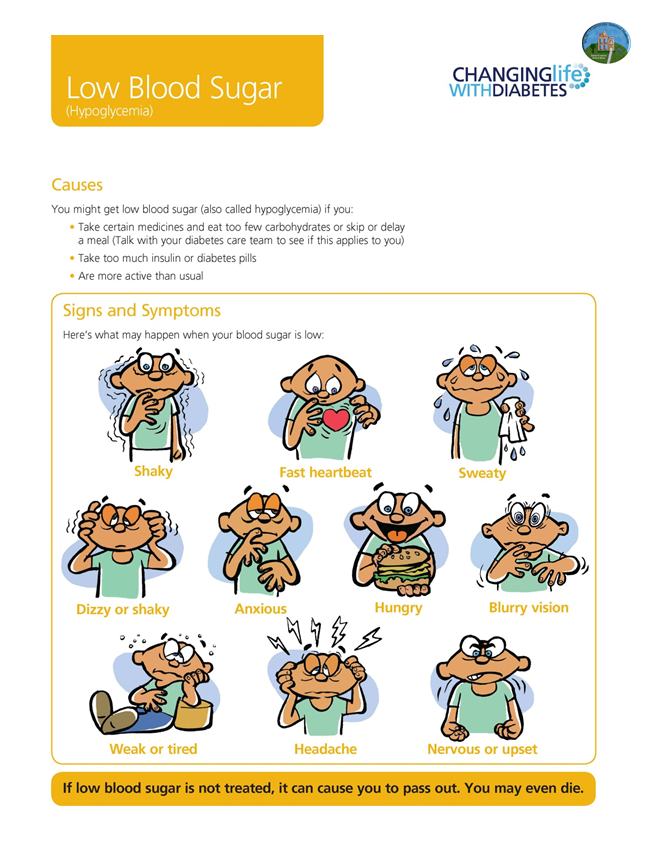
When suffering from hypoglycemia, you can experience a number of common symptoms. These include shakiness, hunger, dizziness, confusion, anxiety, weakness, irritability, and even irregular heart rhythms. As the condition becomes worse, it can even lead to confusion, visual disturbances, seizures, and even loss of consciousness.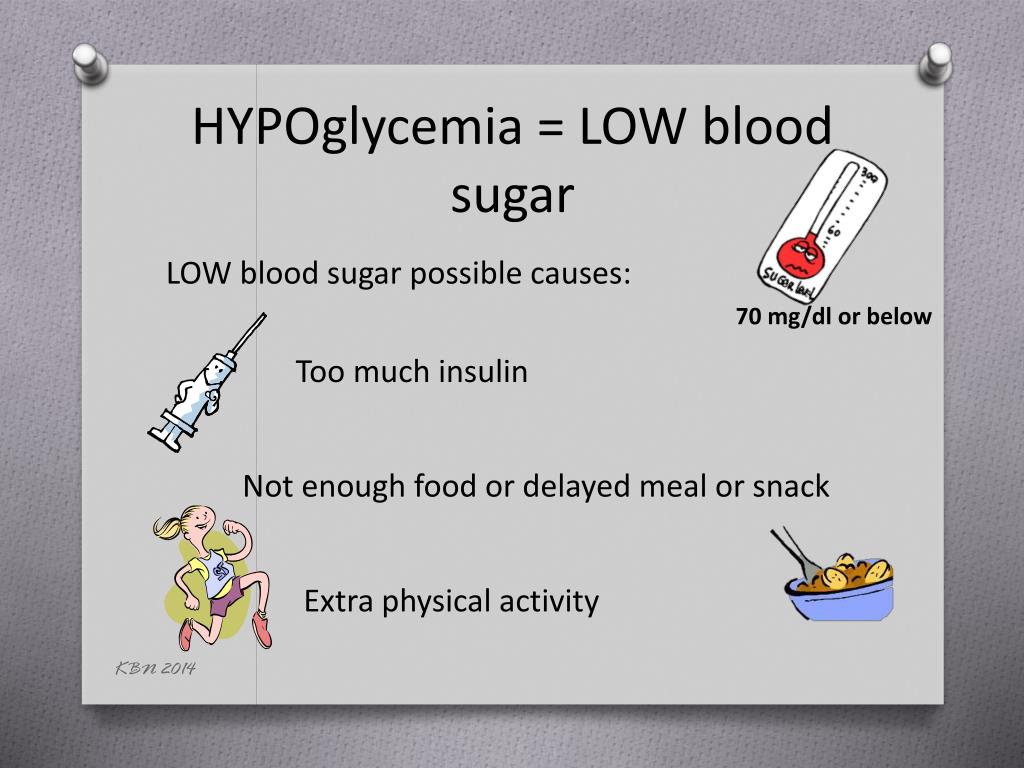
While having low blood glucose levels can be related to diabetes, a person may also experience this condition without the disease. This is because hypoglycemia can be caused by a number of factors. For example, certain types of medication can trigger this condition. This effect has been seen with the administration of quinine, which is typically used for malaria. Hypoglycemia can also be caused by an overproduction of insulin in the body and excessive consumption of alcohol. In addition, certain illnesses can also cause one’s blood glucose levels to drop. These include kidney disorders and anorexia.
Hypoglycemia and Adrenal Fatigue
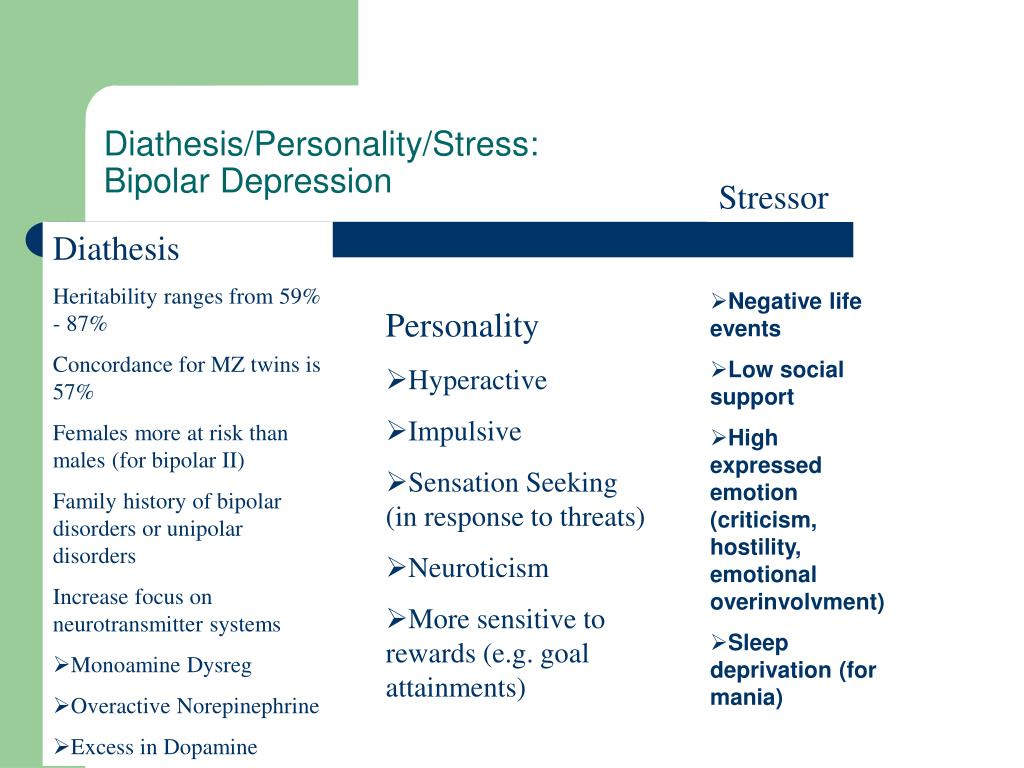
You may not realize it, but becoming severely stressed can trigger adrenal fatigue, which can lead to hypoglycemia. This is because several adrenal hormones including cortisol, epinephrine, and norepinephrine play critical roles in the regulation of your body’s blood sugar levels. In fact, epinephrine plays a role in the short-term control of your body’s blood glucose.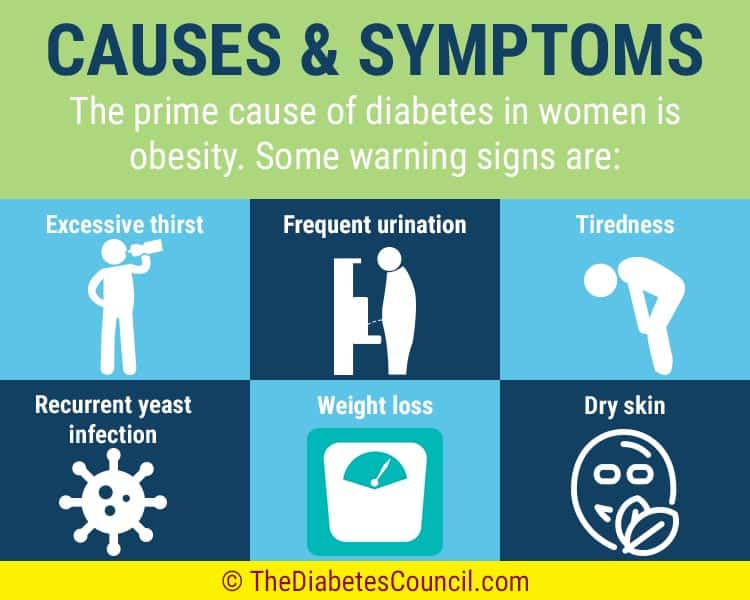 Epinephrine is involved in the increase of blood sugar when the body encounters stress. Meanwhile, cortisol is involved in the long-term maintenance of your body’s blood glucose levels.
Epinephrine is involved in the increase of blood sugar when the body encounters stress. Meanwhile, cortisol is involved in the long-term maintenance of your body’s blood glucose levels.
When the body experiences stress, the adrenal glands prepare it for a fight or flight response by releasing the primary stress hormone cortisol. As cortisol levels rise in the body, both fat and muscle in the body become less sensitive to insulin. Because of this, more glucose becomes readily available in the bloodstream.
This activity is all part of the body’s entire NeuroEndoMetabolic (NEM) Stress Response system. It is made up of the response from several organs and systems in the body, including the heart, liver, hormones, immune system, and the adrenal glands. Using the hormone cortisol, the adrenal glands help ensure that the body has enough energy to deal with the stress at hand.
When stress is chronic, however, it poses a problem for both the adrenal glands and blood sugar levels. During a long period of stress, the body is forced to keep generating more energy for the body to use. At some point, however, it is no longer able to meet the higher demand for glucose. As a result, the body suffers from hypoglycemia.
During a long period of stress, the body is forced to keep generating more energy for the body to use. At some point, however, it is no longer able to meet the higher demand for glucose. As a result, the body suffers from hypoglycemia.
Hypoglycemia can occur while the body is in a state of adrenal fatigue. When it comes to the adrenal glands and the hormones they secrete, eventually adrenal fatigue results in low levels of cortisol, norepinephrine, and epinephrine in the body despite continued high levels of stress.
With increased insulin and decreased levels of cortisol, epinephrine, and norepinephrine, blood sugar levels can drop at an alarming rate. This is because these hormones help facilitate the conversion of carbohydrates, proteins, and fats into glucose. They also control the body’s energy reserve that is necessary for maintaining normal blood sugar levels even in times of stress.
This may explain why a study conducted in Tokushima, Japan found that an excessive secretion of insulin led to a sharp drop in a patient’s blood glucose level.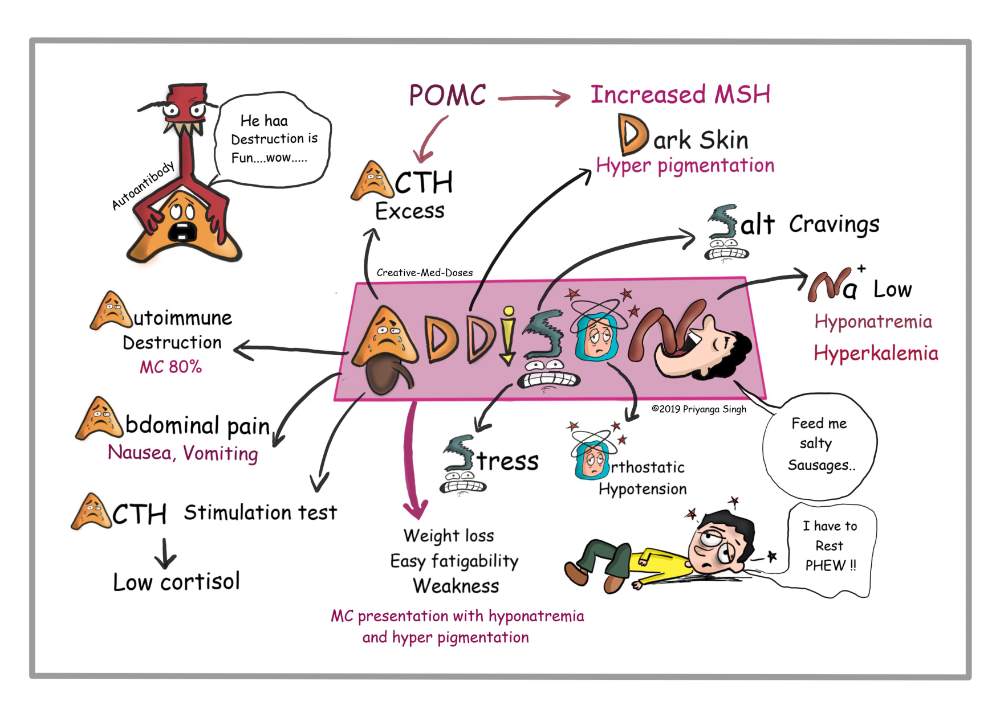 Without continued proper adrenal function to prompt the conversion of more glucose, the body fails to meet the increased demand for energy.
Without continued proper adrenal function to prompt the conversion of more glucose, the body fails to meet the increased demand for energy.
When this happens, the cells fail to receive the glucose and other nutrients that they need to stay healthy. You may find yourself craving sugar while feeling shaky, tired, and even weak.
Furthermore, stress itself can trigger unwanted blood sugar swings in the body. This can hamper the body’s ability to maintain your blood sugar balance and further worsen the symptoms of hypoglycemia that you are already feeling. In fact, it is believed that there is a positive relationship between high stress hormone levels and low blood sugar.
As you can imagine, hypoglycemia is a serious condition that you should do your best to avoid. The problem is, when you are already suffering from adrenal fatigue, it may be a challenge to determine if you are also experiencing dangerously low blood glucose levels.
Hidden Hypoglycemia
Normally, the body has a way of letting you know that you are suffering from low blood glucose levels.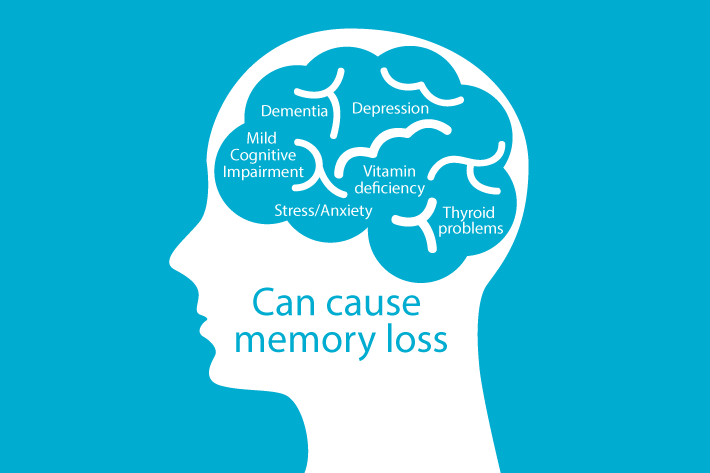 When your blood sugar level starts to drop, glucagon in the liver triggers a release of the stored glucose. Meanwhile, the adrenal hormone epinephrine also signals the liver to produce more glucose. At the same time, early warning symptoms of hypoglycemia start to show in the body. This can include trembling, tingling, numbness, rapid pulse, sweating, and butterflies in the stomach.
When your blood sugar level starts to drop, glucagon in the liver triggers a release of the stored glucose. Meanwhile, the adrenal hormone epinephrine also signals the liver to produce more glucose. At the same time, early warning symptoms of hypoglycemia start to show in the body. This can include trembling, tingling, numbness, rapid pulse, sweating, and butterflies in the stomach.
However, some people fail to experience any of these common symptoms, even when their blood glucose levels have become dangerously low. This condition is known as hypoglycemia unawareness. It is common among people suffering from type 1 diabetes.
This is because type 1 diabetes causes an impairment in the epinephrine secretion of the adrenal glands. In fact, a study conducted by the Temple University Hospital in Philadelphia found significant deficits in epinephrine secretion among two-thirds of patients experiencing diabetic autonomic neuropathy. This, in turn, is linked to significantly delayed or diminished subjective response to low blood sugar levels.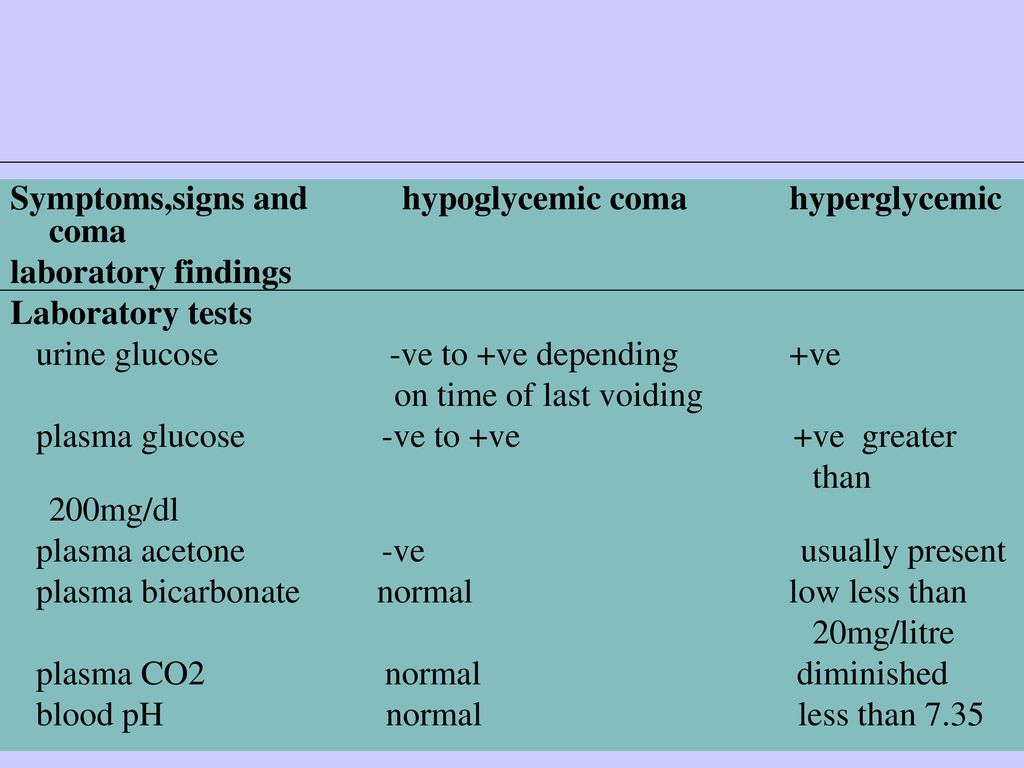
In addition, a recent study published in the American Society for Clinical Investigation also found that people with type 1 diabetes may experience a progressive blunting in their brain responses in both their frontoparietal and corticostriatal neural circuits when faced with mild to moderate hypoglycemia.
On the other hand, if you are already suffering from adrenal fatigue, your doctor may not as easily identify hypoglycemia, even if you exhibit symptoms. This is because adrenal fatigue tends to produce sub-clinical symptoms for hypoglycemia. In this case, blood plasma levels can continue to remain normal despite symptoms such as elevated heart rate, jittery feelings, anxiety, irritability, amnesia, dizziness, fatigue, lethargy, rage, nausea, hunger, and more.
Regardless of its cause, hypoglycemia is a problem that needs to be addressed immediately. If you should continue to have low blood glucose levels, your health can fail seemingly without warning. You can even lose consciousness as your blood sugar continues to drop.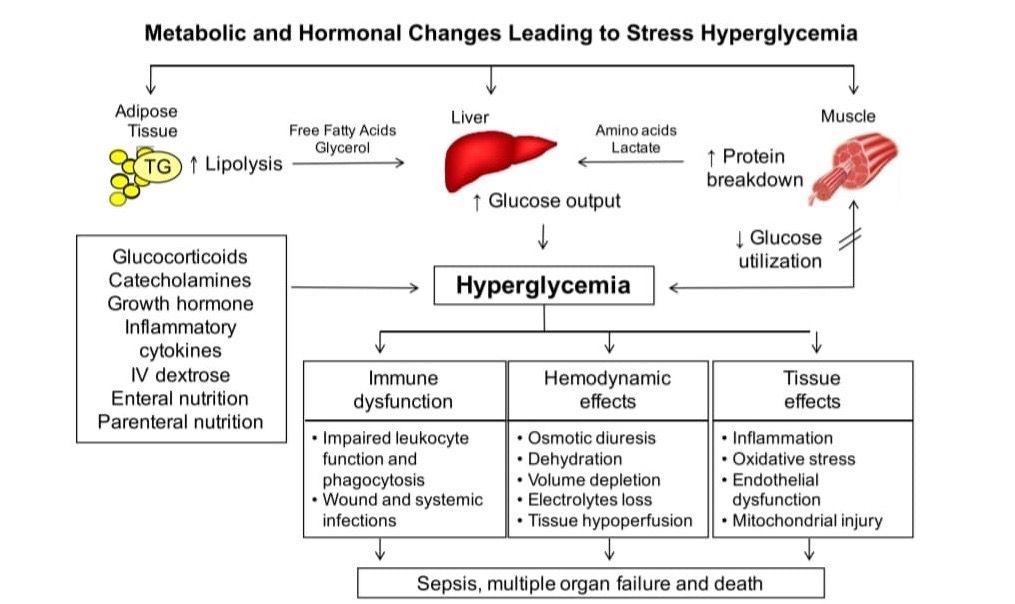
How to Avoid Low Blood Glucose Levels
Addressing low blood sugar levels as soon as possible can help prevent symptoms from getting worse. Before you try any remedy for hypoglycemia though, remember that it is always best to consult with your physician first. This way, the approach to managing your low blood sugar will be better tailored to your specific condition. This is especially helpful if you are also suffering from adrenal fatigue.
That said, here are some easy ways that you can effectively manage your blood sugar levels to keep them from becoming dangerously low.
Consider going on a hypoglycemia diet.
A good hypoglycemia diet is designed to help you normalize your body’s blood sugar levels in the healthiest way possible. This diet utilizes foods rich in fiber such as chia seeds, pumpkin seeds, avocado, beans, artichokes, apples, and flaxseeds.
At the same time, this diet also includes a variety of healthy carbohydrates, which are critical since this is what glucose is primarily made from.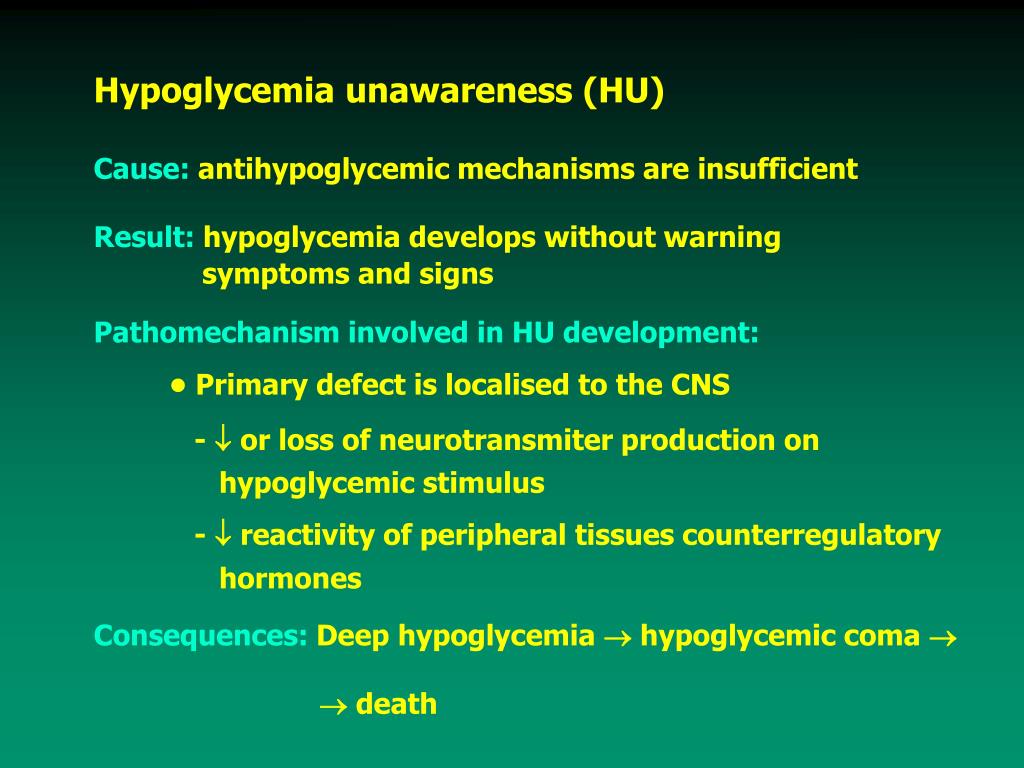 Recommended sources of carbohydrates include wild rice, brown rice, and sweet potatoes.
Recommended sources of carbohydrates include wild rice, brown rice, and sweet potatoes.
In addition, the hypoglycemia diet also includes the consumption of healthy fats. These include extra virgin olive oil and virgin coconut oil.
Take meals more frequently.
Eating more frequently will help ensure that your body has enough food that can be used to make more energy when needed. Aside from the usual breakfast, lunch, and dinner, it is important also to have both a mid-morning and mid-afternoon snack. Make sure you have another snack before you go to bed.
Consume more protein.
Consumption of proteins can slow down the release of sugar in your body. Thus, this will help extend the time that it takes to become hypoglycemic between meals. Be sure to eat healthy proteins like cottage cheese, yogurt, lean meats, nuts, and beans.
Take supplements for adrenal support.
You may also want to consider taking supplements that support your adrenal and metabolic functions.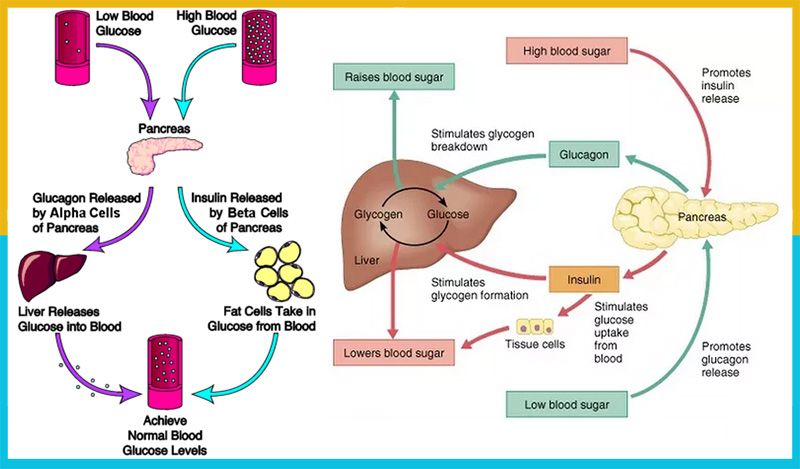 These include vitamins and minerals such as magnesium and vitamins C, B5, B12, and B6. Also, consider certain herbal supplements and probiotics. Taking these helps maintain the proper balance of both your cortisol and insulin levels.
These include vitamins and minerals such as magnesium and vitamins C, B5, B12, and B6. Also, consider certain herbal supplements and probiotics. Taking these helps maintain the proper balance of both your cortisol and insulin levels.
Conclusion
As you can see, there are steps you can take, such as changing your diet, to keep your blood sugar levels in check so that you don’t end up with hypoglycemia. This is especially critical if you feel that you are already in the early stages of adrenal fatigue. By keeping your blood sugar in check, you are also able to keep your adrenal exhaustion from getting much worse. In fact, improving your blood sugar levels can also contribute to your adrenal recovery. This, in turn, can lead to a significantly improved overall quality of life.
Dr. Lam's Key Question
How does adrenal fatigue cause low blood glucose levels?
During times of chronic stress, the adrenal glands respond by releasing cortisol.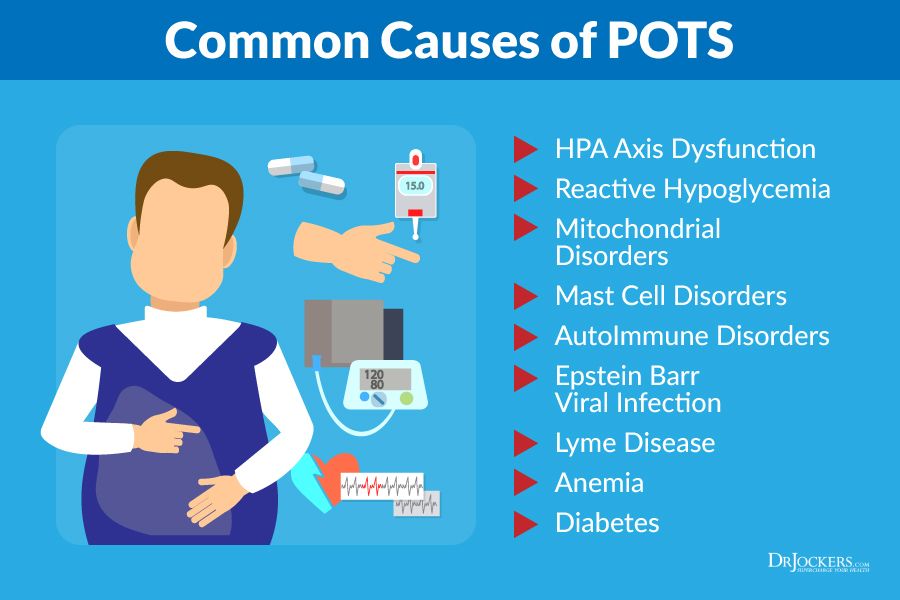 This hormone is also linked to the release of more glucose into the bloodstream. At some point, however, the adrenals become exhausted and they are no longer able to produce enough cortisol, leading to low blood glucose levels.
This hormone is also linked to the release of more glucose into the bloodstream. At some point, however, the adrenals become exhausted and they are no longer able to produce enough cortisol, leading to low blood glucose levels.
Low Blood Sugar and Anxiety: See How They're Tied
Written by Linda Rath
In this Article
- Why Low Blood Sugar Makes You Anxious
- Why Your Blood Sugar Drops
- What You Can Do
- When Lifestyle Changes Aren’t Enough
There’s plenty in life to make you anxious. When you have diabetes, you can add low blood sugar (your doctor may call it hypoglycemia) to the list. But why does it happen? More importantly, what can you do about it?
Why Low Blood Sugar Makes You Anxious
When your blood sugar drops, your body tries to bring it up. It pumps out epinephrine (adrenaline), a “fight or flight” hormone that, among other things, tells your liver to make more glucose (blood sugar).
Adrenaline also makes your heart race and your palms sweat.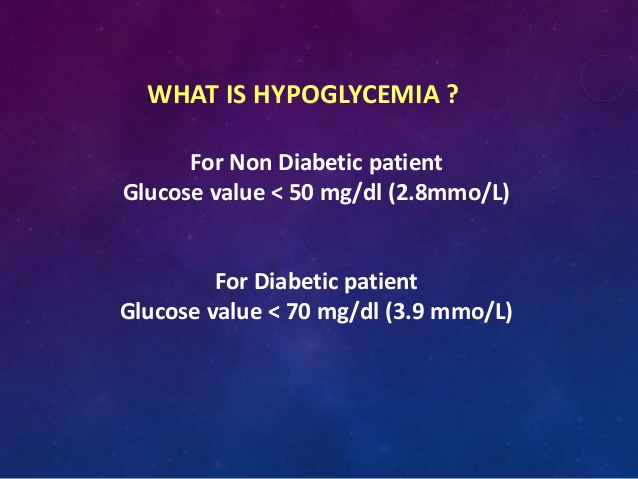 And it can make you feel cranky and anxious. These are warning signs that your blood sugar is too low. If it stays there, your body puts out more hormones, including one called cortisol, also known as "the stress hormone," partially because it helps control things like your mood and fear.
And it can make you feel cranky and anxious. These are warning signs that your blood sugar is too low. If it stays there, your body puts out more hormones, including one called cortisol, also known as "the stress hormone," partially because it helps control things like your mood and fear.
Put adrenaline and cortisol together, and you've got a recipe for anxiety.
Why Your Blood Sugar Drops
The goal of diabetes treatment is to lower your blood sugar. But sometimes, it drops too low. Most people feel symptoms if it goes below 70 milligrams per deciliter (mg/dL). It can happen when you:
- Take too much diabetes medicine
- Skip meals
- Eat less
- Exercise more than normal
People who don’t have diabetes can get low blood sugar, too. Some medicines and diseases can cause it. It can also happen if you:
- Drink too much alcohol
- Have weight loss surgery
- Eat lots of sugary, high-carb foods
What You Can Do
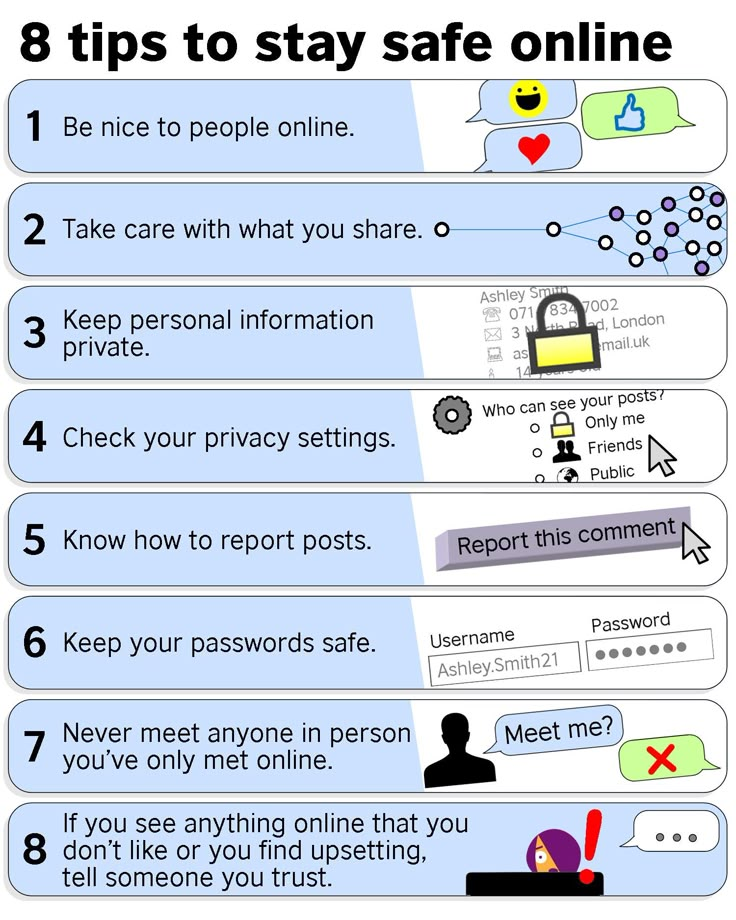
If you have diabetes, a great way to help keep anxiety away is to keep your blood sugar in a safe range.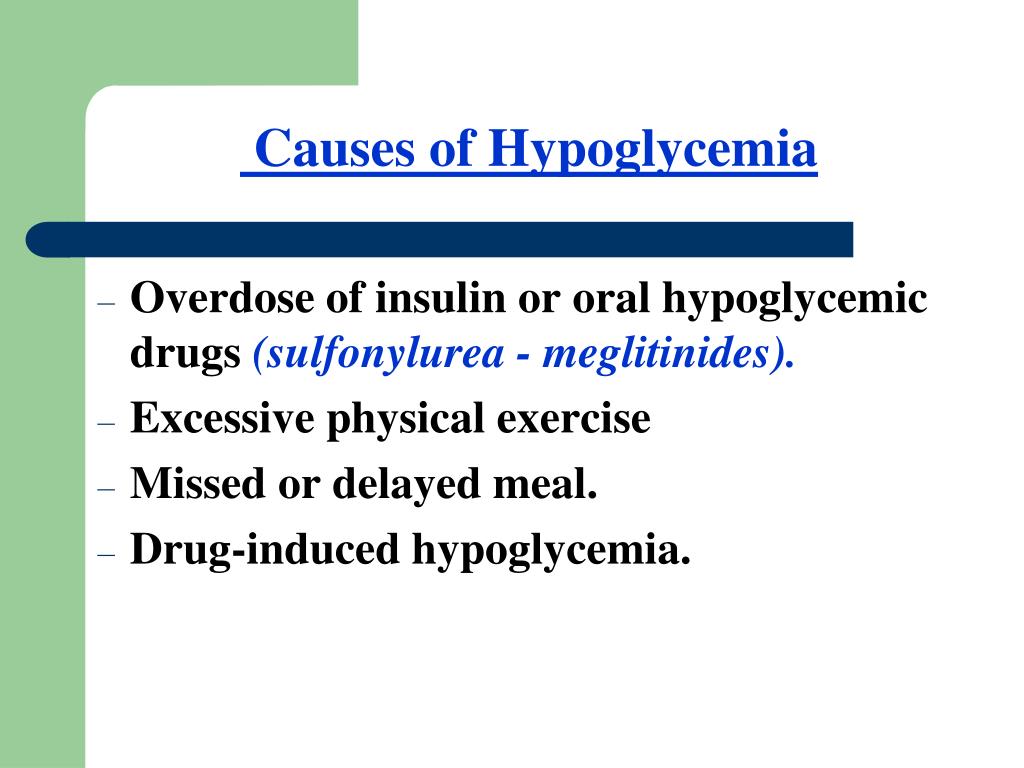 That’s not as easy as it sounds. But these tips can make it a bit easier:
That’s not as easy as it sounds. But these tips can make it a bit easier:
Be careful with insulin. Too much of it is the most common reason for low blood sugar. If you're taking insulin to treat your diabetes, be sure to use the right type and dose every time. When you inject it, make sure to do it just under your skin. A shot into the muscle absorbs too fast and doesn’t last as long.
Go low (glycemic). Some foods make your blood sugar shoot up fast and drop a few hours later. Other foods keep it on a more even keel. A food’s glycemic index is a good way to know which is which.
It's a number that gives you an idea of how fast your body turns carbs into sugar. The higher the number, the quicker it happens and the higher your blood sugar will spike. High-glycemic foods include:
- Simple sugars
- Sugary drinks
- Carbs like white bread, pasta, rice, and potatoes
Low-glycemic foods include:
- Chicken, fish, and other proteins
- Nuts
- Beans
- Non-starchy veggies like asparagus, beets, broccoli, and tomatoes
You can still eat some high-glycemic foods now and then. But enjoy smaller portions with plenty of healthy fat, protein, and carbs at the same time. What you eat matters. But how much and in what combination are just as important.
But enjoy smaller portions with plenty of healthy fat, protein, and carbs at the same time. What you eat matters. But how much and in what combination are just as important.
Exercise wisely. Exercise can lower your blood sugar. A good workout is a great way to ease anxiety. While you're getting your sweat on, your brain pumps out endorphins and other “feel-good” chemicals. Over time, exercise rewires your brain so you feel better overall.
Just be sure to adjust your carbs and insulin before you work out so that your blood sugar doesn't drop too much. How much you need to tweak it depends on things like the type of exercise you're doing and how much you weigh. Your doctor can help you figure out how you can exercise safely.
Limit alcohol. Adult drinks can lower your blood sugar for up to 24 hours. If you drink alcohol, keep it moderate. Women should keep it to one drink a day. For men, the limit is two. A serving is 12 ounces of beer, 5 ounces of wine, or 1.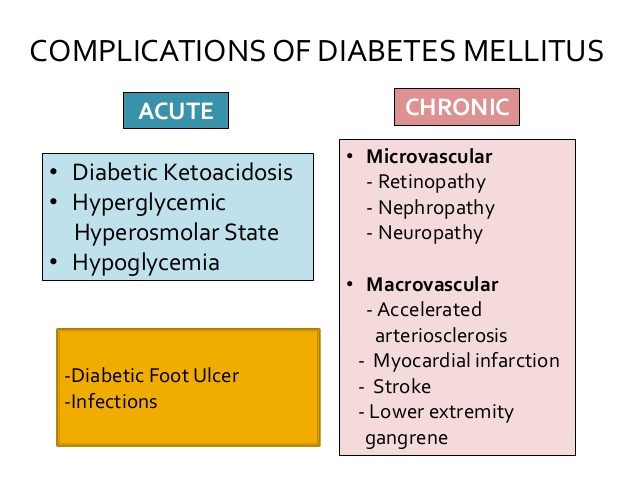 5 ounces of liquor. Never drink on an empty stomach.
5 ounces of liquor. Never drink on an empty stomach.
When Lifestyle Changes Aren’t Enough
Even if you eat healthy, stay active, and avoid lows, you might still feel anxious. If this happens, it might help to talk to a therapist or other counselor. Cognitive behavioral therapy (CBT) is one type of talk therapy proven to help with anxiety. You work with a counselor to recognize when you're having negative thoughts and think through new ways of dealing with situations that challenge you. Talk with your doctor about it.
Acute complications of diabetes mellitus
In diabetes mellitus, any type of diabetes, the most common acute complications are hypoglycemia (hypoglycemic coma) and ketoacidotic coma or condition.
Hypoglycemia (hypoglycemic coma)
Hypoglycemia (decrease in blood glucose less than 3 mmol/l) develops rapidly, sometimes almost suddenly. It is characterized by the following symptoms:
- Increased sweating
- Severe weakness, and comes on abruptly
- Trembling in the body
- Palpitations
- Hunger
It is worth noting that not all of these symptoms can be present together.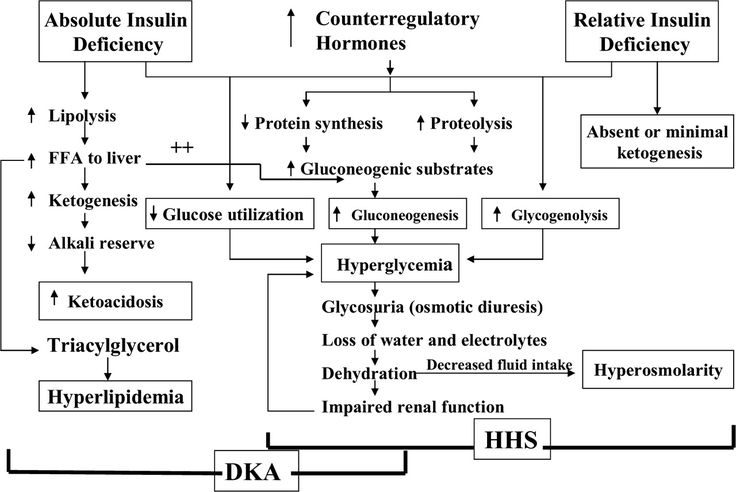 There may also be some “own” sensations that the patient notes for himself throughout the illness. For example, tingling and numbness in the nose, tongue, or upper lip. Sometimes, hypoglycemia may not immediately show any symptoms, especially in patients with long-term ongoing diabetes, and this is dangerous. If hypoglycemia is not stopped, then hypoglycemic coma may develop, when the patient cannot independently take the necessary actions to treat hypoglycemia. So, hypoglycemia needs to be removed as quickly as possible and it needs to be done correctly. To quickly increase blood sugar, you need to take fast-digesting carbohydrates: 4-5 pieces of sugar, honey, jam, sweet fruit drinks or lemonade in an amount of 200 ml. Important Rule : A person with diabetes who is being treated with glucose-lowering drugs should carry easily digestible carbohydrates with them at all times. It should be noted that in such situations, the most convenient is lump sugar or juice, lemonade.
There may also be some “own” sensations that the patient notes for himself throughout the illness. For example, tingling and numbness in the nose, tongue, or upper lip. Sometimes, hypoglycemia may not immediately show any symptoms, especially in patients with long-term ongoing diabetes, and this is dangerous. If hypoglycemia is not stopped, then hypoglycemic coma may develop, when the patient cannot independently take the necessary actions to treat hypoglycemia. So, hypoglycemia needs to be removed as quickly as possible and it needs to be done correctly. To quickly increase blood sugar, you need to take fast-digesting carbohydrates: 4-5 pieces of sugar, honey, jam, sweet fruit drinks or lemonade in an amount of 200 ml. Important Rule : A person with diabetes who is being treated with glucose-lowering drugs should carry easily digestible carbohydrates with them at all times. It should be noted that in such situations, the most convenient is lump sugar or juice, lemonade.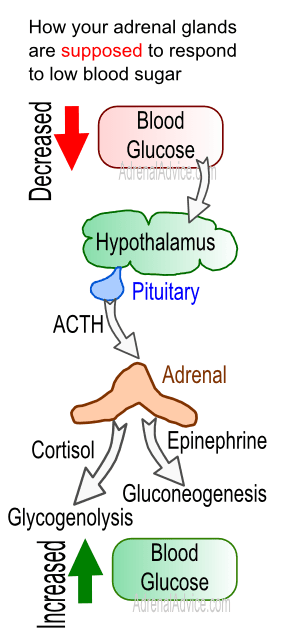 Honey - it is inconvenient to dose, it is difficult to carry with you, sweets are difficult to chew (caramel), or they may contain substances that slow down the absorption of carbohydrates (chocolate, soy candies).
Honey - it is inconvenient to dose, it is difficult to carry with you, sweets are difficult to chew (caramel), or they may contain substances that slow down the absorption of carbohydrates (chocolate, soy candies).
In case of severe hypoglycemia (numbness with the impossibility of independent adequate actions or complete loss of consciousness - hypoglycemic coma), the patient cannot help himself. If consciousness is still preserved, you need to drink or feed sweets (see above). In case of coma, call an ambulance.
Recurrent hypoglycemia requires a mandatory visit to a doctor.
Ketoacidotic coma or condition
This condition, on the contrary, occurs with elevated sugar. This is an acute complication of the disease, caused by an absolute or pronounced relative deficiency of insulin due to inadequate insulin therapy or an increase in its demand. Factors provoking the development of ketoacidotic coma:
- Insufficient dose or missed insulin injection (or tablet intake of glucose-lowering drugs)
- Unauthorized withdrawal of hypoglycemic therapy
- Violation of insulin administration technique
- Accession of other diseases (infections, injuries, operations, pregnancy, myocardial infarction, stroke, stress, etc.
 )
) - Alcohol abuse
- Taking certain medications - glucocorticosteroids, etc.
Ketoacidotic state and later coma develops gradually, from several hours to several days. Worried about dry mouth, thirst, frequent urination, indicating an increase in decompensation of diabetes. Weight loss can also be recorded, also due to the uncompensated course of the disease over a certain period of time. As ketoacidosis progresses, symptoms such as nausea and vomiting appear, which in a patient with diabetes dictate the need for a mandatory study of the content of acetone in the urine. Patients may complain of severe abdominal pain. A typical clinical symptom of a developing coma is frequent deep breathing (Kussmaul breathing), often with the smell of acetone in the exhaled air. In the analyzes, an increase in sugar, as a rule, is more than 15-17 mmol / l.
There are four main positions in the treatment of this condition:
- insulin therapy;
- recovery of lost fluid;
- correction of mineral and electrolyte metabolism;
- treatment of coma-provoking diseases and complications of ketoacidosis.

In any case, it is important for the patient to know that long-term decompensation of diabetes should not be allowed and that the attending physician should not be contacted in time.
Diabetes mellitus in questions and answers GBUZ VFD Kopeysk
Diabetes mellitus questions and answers
Diabetes mellitus is a disease caused by total or relative lack of insulin (pancreatic hormone), which results in high blood sugar levels and energy metabolism disorders, sometimes very significant.
Diabetes mellitus is a group of diseases that manifest in a similar way but have different causes. Type 1 diabetes mellitus occurs in childhood or young age, proceeds rapidly, is characterized by a strong feeling of thirst, carries the risk of a significant disruption of energy metabolism, and is treated with insulin. Type 2 diabetes is more common in the elderly, often accompanied by obesity, its symptoms are not as obvious as in type 1 diabetes, treatment can be started with a diet or taking antidiabetic drugs - in the form of tablets. Diabetes mellitus can also be caused by other diseases (so-called specific types of diabetes), such as diseases of the pancreas, and it can be caused by treatment with corticosteroids.
Diabetes mellitus can also be caused by other diseases (so-called specific types of diabetes), such as diseases of the pancreas, and it can be caused by treatment with corticosteroids.
• How does diabetes manifest itself?
It is manifested by fatigue, thirst, excretion of large amounts of urine, weight loss, inflammation of the bladder and kidneys, furunculosis can be observed. If diabetes is not treated for a long time, it can lead to a complete disruption of the basic functions of the human body, dehydration, loss of consciousness, and even death. Type 1 diabetes mellitus is characterized by a sharp manifestation and development of all the symptoms of the disease. Type 2 diabetes mellitus develops more slowly, its signs are less pronounced, they may not appear outwardly at all until late complications of diabetes appear.
• Can diabetes occur without symptoms?
Type 2 diabetes mellitus often does not manifest itself at the onset of the disease and can be detected during a preventive examination by an increase in blood glucose levels and the appearance of sugar in the urine.
• Is diabetes hereditary?
Yes, both types of diabetes, especially type 2 diabetes, can be inherited in a certain way, more precisely, predisposition to this disease is transmitted, and it depends on external influences whether a particular person will develop diabetes or not.
• Can drugs or other illnesses cause diabetes?
This type of diabetes is called secondary diabetes mellitus (or a specific type of diabetes). Certain medications, such as corticosteroids used in the treatment of rheumatic diseases, asthma, a number of non-specific intestinal diseases, skin diseases, and other autoimmune diseases, can trigger the development of this diabetes. Diabetes mellitus can appear as a symptom of pancreatic disease, with some endocrine diseases, severe infectious diseases. Some diseases, more often viral, long-term stress can trigger diabetes or worsen the course of existing diabetes.
• What is Impaired Glucose Tolerance?
Previously, this condition was called "latent" (sleeping, asymptomatic) diabetes mellitus.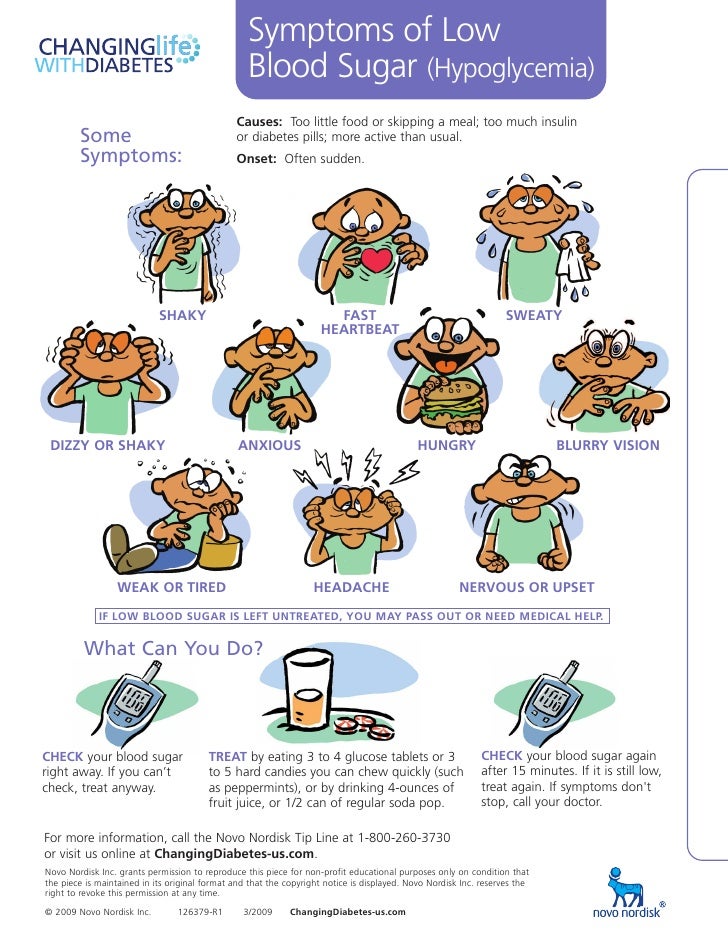 It is detected only in a laboratory analysis, with the so-called glucose tolerance test, when a patient drinks a glucose solution (75 g in 100 ml of water) and, according to the level of glucose in the blood after 2 hours, it turns out how completely his body is able to assimilate this glucose. This test measures the ability of the pancreas to produce the required amount of insulin per meal. In case of violation of glucose tolerance, medical supervision, diet, sufficient physical activity are necessary.
It is detected only in a laboratory analysis, with the so-called glucose tolerance test, when a patient drinks a glucose solution (75 g in 100 ml of water) and, according to the level of glucose in the blood after 2 hours, it turns out how completely his body is able to assimilate this glucose. This test measures the ability of the pancreas to produce the required amount of insulin per meal. In case of violation of glucose tolerance, medical supervision, diet, sufficient physical activity are necessary.
• When is diabetes diagnosed?
If the patient has symptoms typical of diabetes mellitus (thirst, heavy urination, weight loss), a blood sugar test is sufficient. If its level in capillary blood on an empty stomach is more than 6.1 mmol / l (double definition) - this is diabetes mellitus. If the patient does not have symptoms typical for diabetes, but there is only a suspicion of diabetes mellitus, a glucose tolerance test is performed, the principle of which is described above.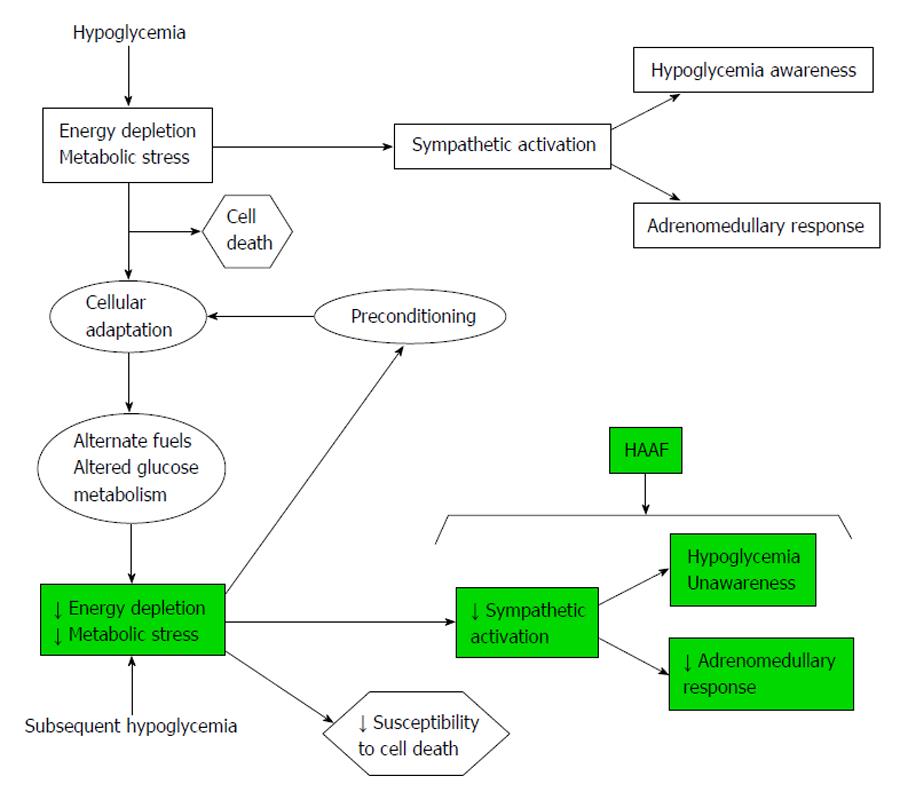 According to the body's reaction to this load (glycemia level after 2 hours more than 11.1 mmol / l) it is determined whether it is really diabetes mellitus or only a violation of glucose tolerance (glycemia level after 2 hours more than 7.8 mmol / l) .
According to the body's reaction to this load (glycemia level after 2 hours more than 11.1 mmol / l) it is determined whether it is really diabetes mellitus or only a violation of glucose tolerance (glycemia level after 2 hours more than 7.8 mmol / l) .
• Is it possible to plan a pregnancy with a diagnosis of diabetes mellitus?
Yes. However, before pregnancy (about 1 year) and throughout pregnancy, it is necessary to strictly control the compensation of the disease and adequately treat diabetes. During pregnancy, it is necessary to inject insulin, tablet preparations are not used so as not to harm the fetus and not endanger its life. To assess the compensation of the disease, it is necessary to control the level of glycated hemoglobin once every 3 months.
• Can I go in for sports and work if I have diabetes?
If you have diabetes, you can go in for sports, do physical work. Usually, physical education and increased physical activity are desirable. This increases tissue sensitivity to insulin and helps maintain optimal weight.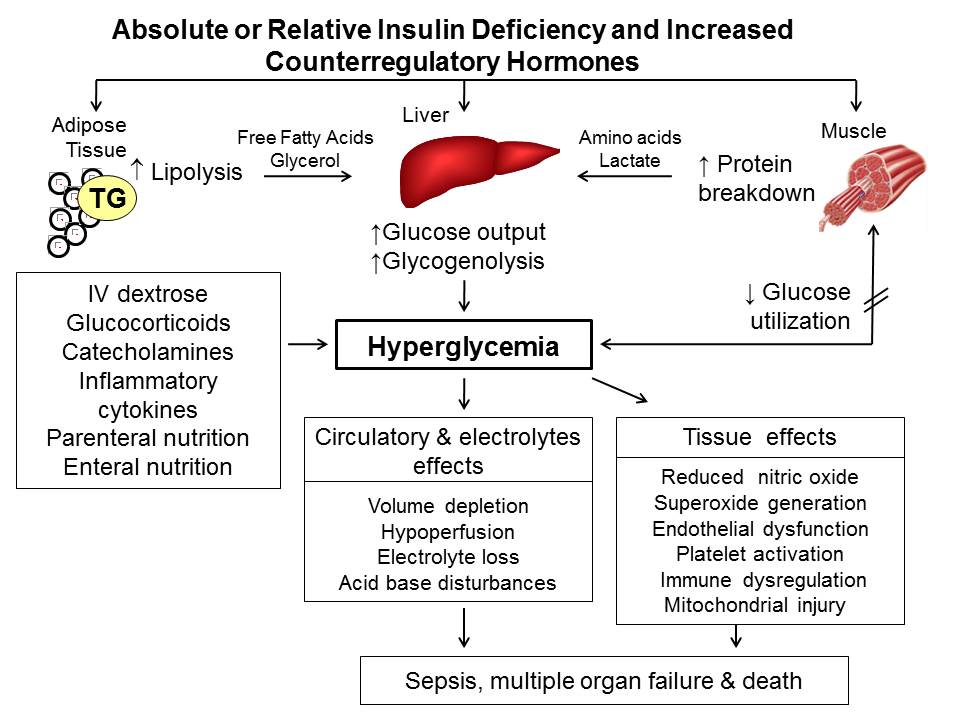 With heavy loads, it is necessary to consult a doctor, prescribe a diet and doses of insulin or hypoglycemic drugs, taking into account the load, so as not to cause hypoglycemia (a strong decrease in sugar levels). With regard to work, the patient should choose an occupation with the ability to maintain a proper diet, with uniform physical activity throughout the week. For patients with diabetes and the risk of hypoglycemia, occupations where the patient could harm himself or others are unsuitable - work at height, associated with high voltage current, driving a car, construction machines, etc.
With heavy loads, it is necessary to consult a doctor, prescribe a diet and doses of insulin or hypoglycemic drugs, taking into account the load, so as not to cause hypoglycemia (a strong decrease in sugar levels). With regard to work, the patient should choose an occupation with the ability to maintain a proper diet, with uniform physical activity throughout the week. For patients with diabetes and the risk of hypoglycemia, occupations where the patient could harm himself or others are unsuitable - work at height, associated with high voltage current, driving a car, construction machines, etc.
• How to treat diabetes?
The main goal of treatment is to achieve normal blood sugar levels and maintain this level throughout life. This is necessary to prevent complications of diabetes. Treatment is based on changing the optimal physical activity and diet. It is necessary to achieve weight loss with its excess. If physical activity and diet are not enough to achieve normal sugar levels, it is necessary to connect antidiabetic drugs (tablets or insulin).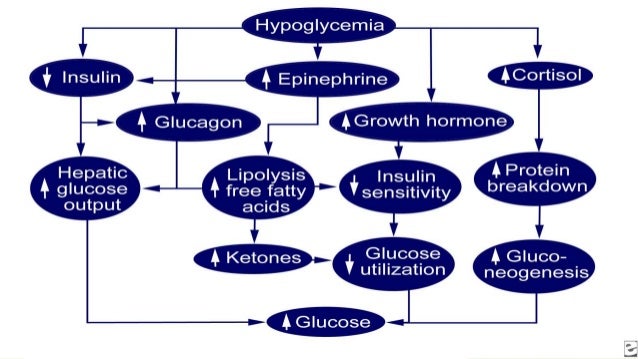 Type 1 diabetes requires insulin treatment from the start of the diagnosis, as it is associated with primary damage to the cells of the pancreas.
Type 1 diabetes requires insulin treatment from the start of the diagnosis, as it is associated with primary damage to the cells of the pancreas.
• What should be the diet for diabetes?
A diabetic diet is not just about cutting out sugar, sweets and sugary foods. Each patient should have an individually formulated diet with a certain amount of carbohydrates, fats, proteins and calories so that the blood sugar level is normal, fat metabolism is not disturbed, the patient has an ideal weight and maintains it. Simple sugars, which are rapidly absorbed, should be excluded from the diet, causing a sharp rise in blood sugar. The total amount of carbohydrates should be 55-60%, with a predominance of coarse fiber, fats - 25-30% (with a predominance of vegetable fats), proteins - 15-20%.
• Do I need to diet if I take tablets or insulin?
Yes, you must! Diet (rational nutrition) is necessary for every patient, even if he must take pills or insulin.
• What if I don't diet?
If the diet is not observed, there is a risk of poor compensation with the risk of complications. If you do not follow the diet and increase the doses of drugs or doses of insulin, the patient may gain weight, worsen the sensitivity of cells to insulin, diabetes treatment will fall into a vicious circle. The only way to avoid these complications is to adjust the diet in such a way as to normalize and maintain weight.
If you do not follow the diet and increase the doses of drugs or doses of insulin, the patient may gain weight, worsen the sensitivity of cells to insulin, diabetes treatment will fall into a vicious circle. The only way to avoid these complications is to adjust the diet in such a way as to normalize and maintain weight.
• Why can some patients take pills while others need insulin right away?
It depends on the type of diabetes. In patients with type 1 diabetes, the pancreas does not produce insulin and therefore insulin must be used from the very beginning of the disease. In patients with type 2 diabetes, the lack of insulin is only relative, often at the initial stage of the disease it is enough to follow a diet and take medications that improve the body's sensitivity to insulin or increase its secretion by pancreatic cells. If treatment with tablets ceases to help, it is necessary to start injecting insulin.
• How many times a day do you need to “shot” insulin?
When treating diabetes, we strive to keep blood sugar levels in line with those of healthy people.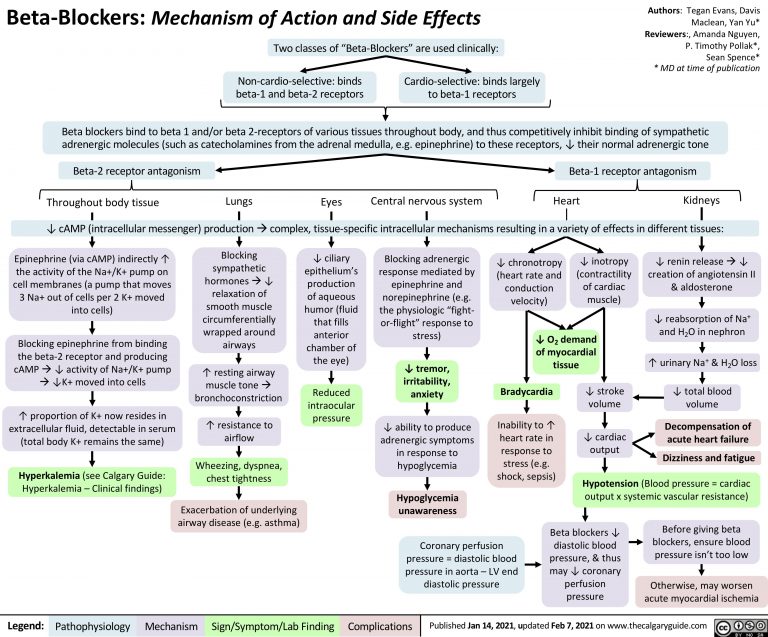 Different schemes of insulin administration are used, which depend on the type of diabetes and the course of the disease. Often in young patients and patients with complications, intensive regimens of insulin therapy are used, i.e. the patient injects insulin 3-5 times a day. In elderly patients, the number of insulin injections is reduced to avoid hypoglycemia and depends on the course of the disease.
Different schemes of insulin administration are used, which depend on the type of diabetes and the course of the disease. Often in young patients and patients with complications, intensive regimens of insulin therapy are used, i.e. the patient injects insulin 3-5 times a day. In elderly patients, the number of insulin injections is reduced to avoid hypoglycemia and depends on the course of the disease.
• How to evaluate the quality of diabetes care?
A well-compensated patient should feel like a healthy person, without experiencing intense thirst or hunger, his body weight is maintained at an ideal level, and there is no loss of consciousness due to hypoglycemia. How well diabetes is compensated can be found out with a blood and urine test for sugar. When properly treated, urine does not contain sugar. Blood sugar levels should be monitored at home throughout the day for the correct selection of the diet and dose of the drug. Once every 3 months, it is necessary to determine the level of glycated hemoglobin, which can be used to judge diabetes compensation for this period, which is currently the main criterion for compensating carbohydrate metabolism.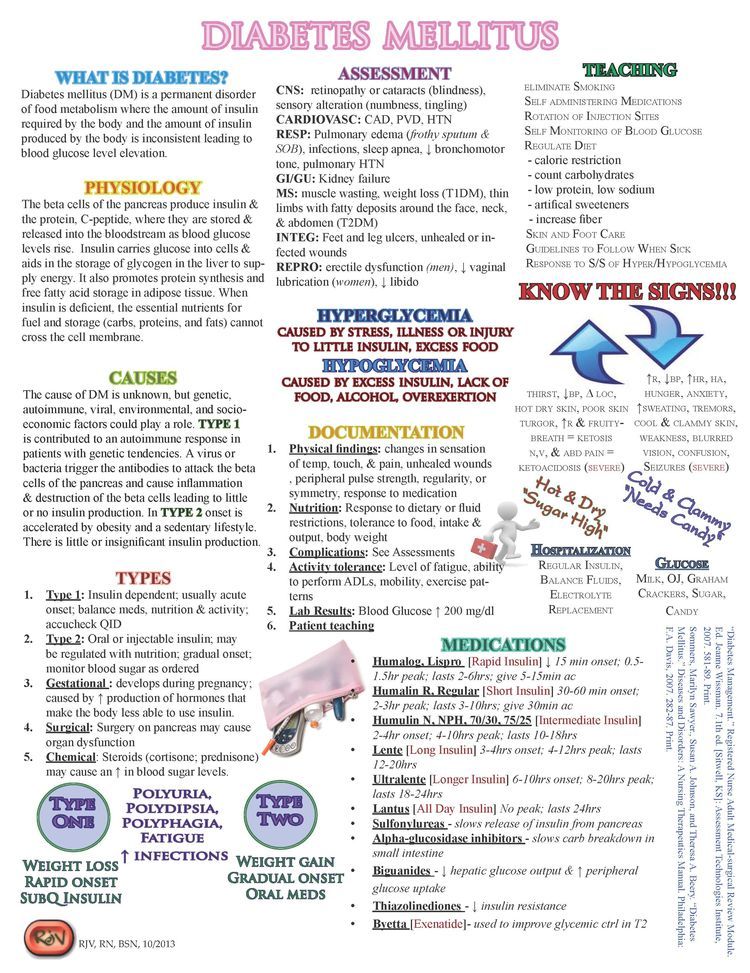
• What is hypoglycemia?
Hypoglycemia is a condition caused by low blood sugar. This occurs as a result of a discrepancy between the intake of sugar from food and the consumption of sugar associated with physical activity or the intake of an inadequate dose of hypoglycemic drugs. Hypoglycemia often occurs when the patient falls asleep and forgets to eat, when the insulin dose is not sufficiently reduced due to poor appetite, or as a result of increased physical activity. With mild hypoglycemia, the patient experiences hunger, with more severe - sweating, weakness, with severe - loss of consciousness may occur
• How can hypoglycemia be avoided and treated?
Hypoglycemia can be avoided by following a proper diet. With the expected increase in load, you need to increase the intake of carbohydrates with food, maybe even reduce the dose of insulin. Hypoglycemia should be treated already at the initial stage - give the patient sweet tea, cookies, candy. In a severe condition, it becomes necessary to inject a glucose solution into a vein or intramuscularly inject glucagon.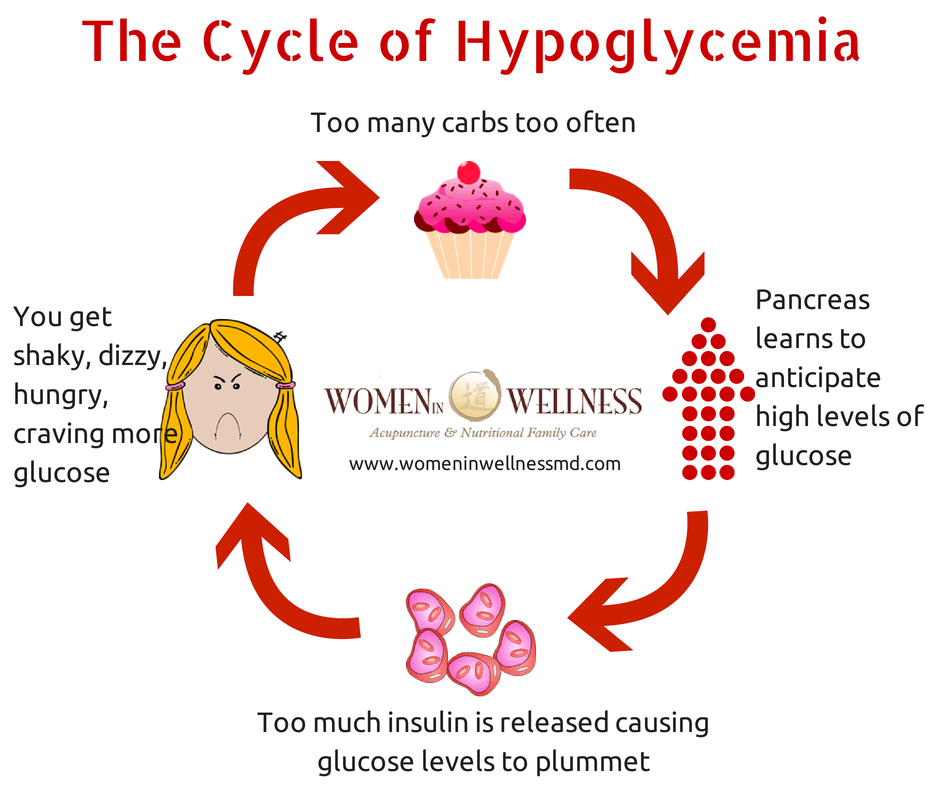 The drug glucagon is desirable to have in patients with a tendency to hypoglycemia, since it can be administered by the patient himself or by a relative.
The drug glucagon is desirable to have in patients with a tendency to hypoglycemia, since it can be administered by the patient himself or by a relative.
•How often should I visit an endocrinologist?
It depends on the type of diabetes, the method of treatment and the state of compensation. Patients with type 2 diabetes with good compensation, once every 3 months is enough, patients with complications of diabetes and an intensive insulin regimen need monthly monitoring. But a trained patient can help himself in compensating for diabetes by doing his own blood tests during the day with a glucometer (a device for measuring blood sugar levels).
• What are the complications of diabetes?
Complications may be early or late, involving small vessels (microangiopathy) or large vessels (macroangiopathy). Early complications include the following: ketoacidosis (with poor compensation, ketone bodies are formed - products of fat metabolism, which, together with high blood sugar levels, can lead to disruption of the functions of the main biological systems of the body with the threat of loss of consciousness and death), hypoglycemia
Late complications occur with prolonged, poorly compensated diabetes.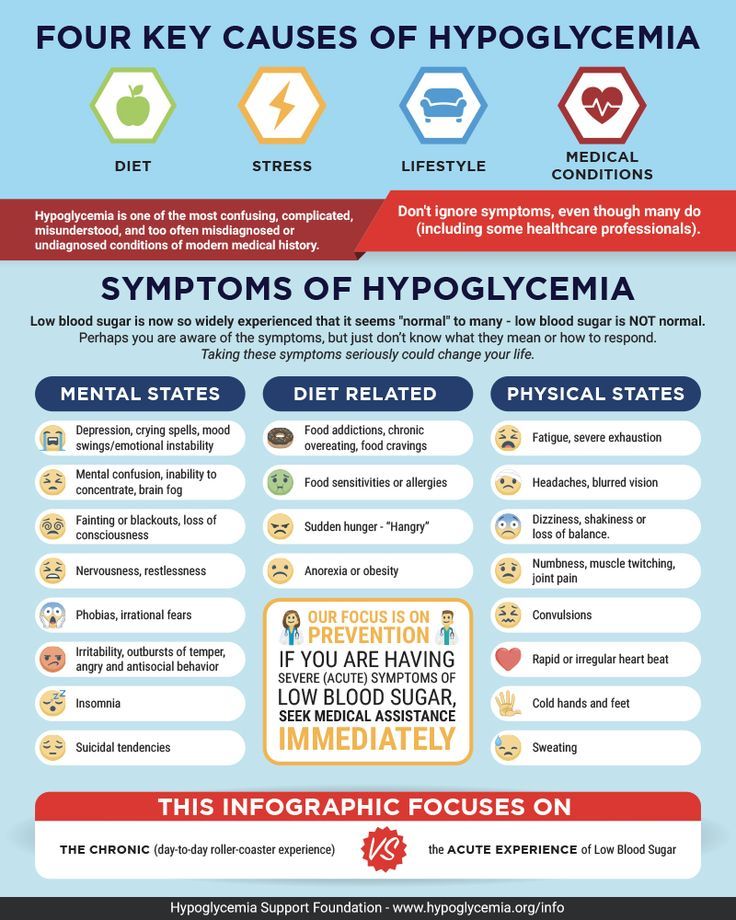 The eyes may be affected (retinal changes with a risk of blindness), kidneys (renal failure may develop with the need for hemodialysis), the vessels of the lower extremities are affected (which can lead to gangrene with the need for amputation), the gastrointestinal tract, the cardiovascular system and the nervous system are affected. system. The doctor's task is to acquaint the patient with possible complications and explain how to prevent them.
The eyes may be affected (retinal changes with a risk of blindness), kidneys (renal failure may develop with the need for hemodialysis), the vessels of the lower extremities are affected (which can lead to gangrene with the need for amputation), the gastrointestinal tract, the cardiovascular system and the nervous system are affected. system. The doctor's task is to acquaint the patient with possible complications and explain how to prevent them.
• How to avoid the complications of diabetes?
First of all, long-term compensation of diabetes (glycated hemoglobin level below 7%) is necessary, which depends on adherence to a correctly established diet, correct treatment and adequate physical activity. Regular monitoring of blood sugar levels is necessary. To prevent vascular complications, in addition, it is necessary to regularly monitor and maintain a normal level of blood pressure (below 130/80 mm Hq). the level of triglycerides (below 1.7 mmol / l), cholesterol in the blood (below 4.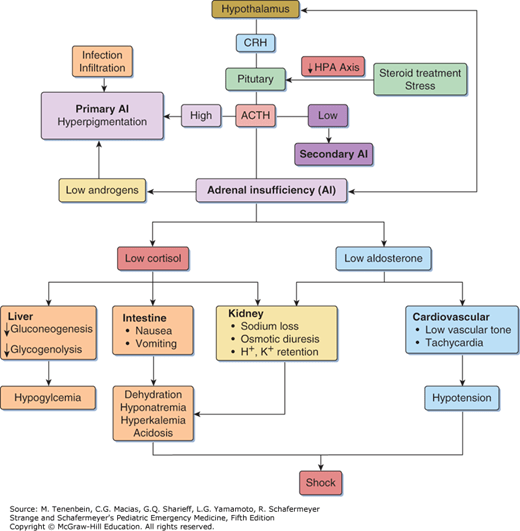 8 mmol / l). Taking into account the special sensitivity of the feet to injuries and the danger of the so-called "diabetic foot", constant care of the feet is needed, which consists in wearing comfortable shoes, treating small wounds and hygienic care of the skin of the feet.
8 mmol / l). Taking into account the special sensitivity of the feet to injuries and the danger of the so-called "diabetic foot", constant care of the feet is needed, which consists in wearing comfortable shoes, treating small wounds and hygienic care of the skin of the feet.
• What should a patient with diabetes carry with them when they are away from home and on the road?
Each patient must carry an identity card with passport details and a phone number, with clear indications of the drugs used, a supply of antidiabetic drugs or insulin. Do not forget to have a few pieces of sugar in your pocket in case of hypoglycemia, and a glucometer is often necessary.
• What diseases or medicines make the condition worse?
If the patient falls ill with another disease, two situations may arise:
1. The disease will worsen the state of diabetes compensation and there will be an increase in sugar levels, which will necessitate an increase in the dose of drugs or insulin.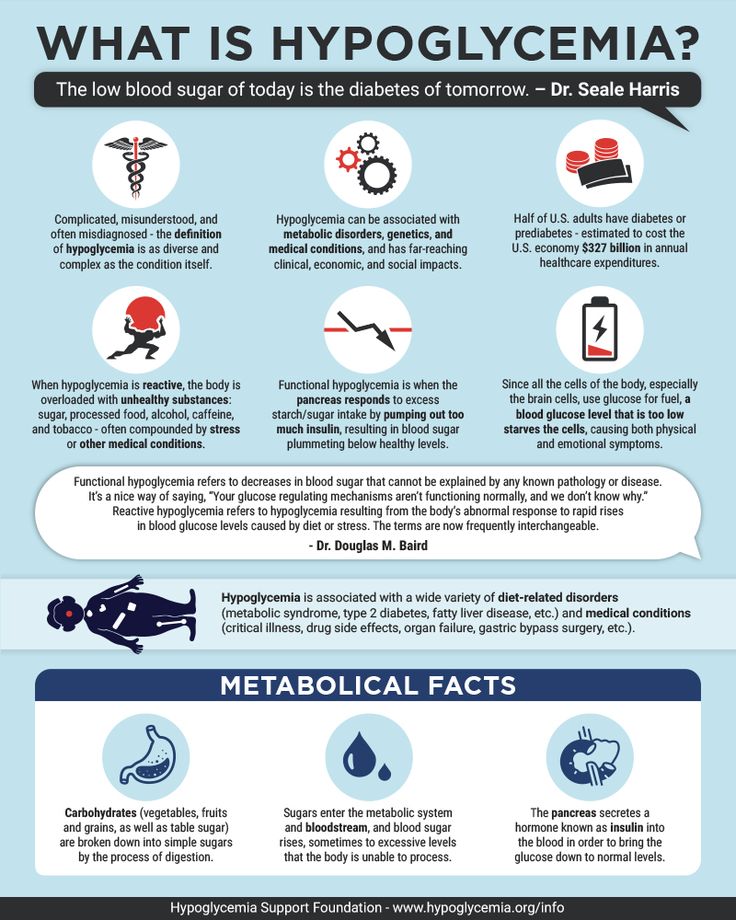
2. The patient does not eat during illness and hypoglycemia may occur, then it is necessary to recheck the blood sugar level and possibly reduce the dose of the hypoglycemic drug. In case of serious illnesses, the patient should be admitted to the hospital and the compensation for diabetes should be adjusted quickly. Therefore, in case of infectious diseases with high temperature, before planned operations, in diseases of the gastrointestinal tract with lack of appetite and vomiting, medical supervision is necessary, and if necessary, the patient should be admitted to the hospital.
• Diabetes self-management.
At present, the treatment of the patient and the achievement of normal blood sugar levels include the mandatory self-monitoring of blood sugar at home. This requires a glucometer with test strips. The use of a glucometer is taught in "diabetes schools".
• Do you need to have a blood test every time you visit a doctor, maybe a urine test is enough?
Urinalysis data is not enough, a blood test for glycemia or glycated hemoglobin will better determine the state of compensation and allow you to change the treatment regimen if necessary.