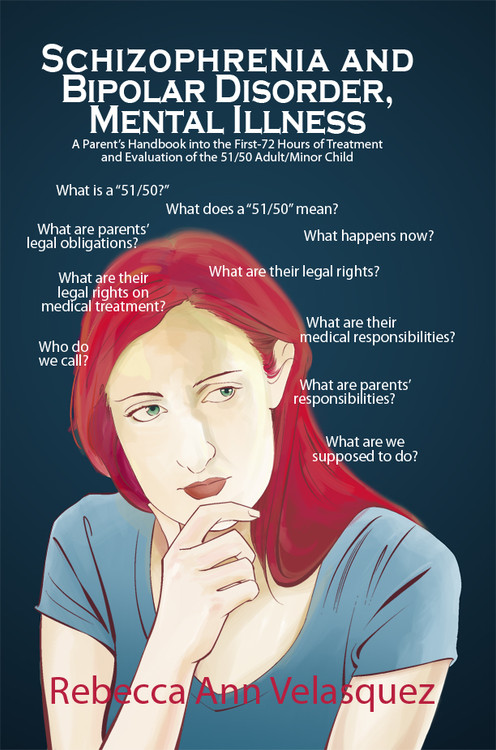
Decompensated bipolar disorder
Decompensation in Mental Health and Social Security Disability
Social Security has updated its listings that used the term “episodes of decompensation” to describe periods of mental deterioration.
Free evaluation for disability benefits. Get up to $3,345 per month.
Free evaluation for disability benefits. Get up to $3,345 per month.
Answer a few questions to check your eligibility.
How old are you?
Select an answer181920212223242526272829303132333435363738394041424344454647484950515253545556575859606162636465Select an answer181920212223242526272829303132333435363738394041424344454647484950515253545556575859606162636465
BackNext
The term "episodes of decompensation" is used by psychiatrists and psychologists to describe the deterioration of the mental health of an individual who, up till that point, was maintaining his or her mental illness. It used to be a term that Social Security used in evaluating some psychiatric and emotional claims for Social Security and SSI disability benefits.
While the term is no longer used in Social Security's mental disability listings, the concept of periods of mental or psychiatric deterioration still plays a big role in the evaluation of some types of mental illness.
If you experience times when your symptoms are exacerbated, or you just seem to fall apart, this means that your mental illness is not being maintained. And Social Security knows that you can't function and work when your mental illness is not being maintained. Increases in mental or emotional symptoms lead to a lessened ability to engage in normal daily activities and work. For that reason, you may have an easier time getting disability benefits if you suffer from these episodes of deterioration, as they are a way for some mental illnesses to qualify as disabilities.
Causes of Episodes of Decompensation or Deterioration
There are different potential causes of mental deterioration:
Your medical treatment is no longer working. This may call for an increase in medications to decrease symptoms and allow you to function on a more normal level.
A stressful situation may be affecting you. You may have taken on more mental demands, such as an attempt to work, that you are not able to handle. Or you may need changes in your environment or more structure in your support system, such as hospitalization or placement in a halfway house.
The causes of mental deterioration are not usually important to your eligibility for benefits, except those due to work attempts. What is important is that the episodes are documented and provable (see below).
Use of "Episodes of Decompensation" Term in Old Listings
The Social Security Administration (SSA) previously defined episodes of decompensation to include:
- a temporary worsening of symptoms
- a loss of the ability to adapt to normal changes and stress, and
- difficulty with normal activities of life, including concentrating, being persistent at tasks, pacing oneself, or maintaining social relationships.
In short, an episode of decompensation refers to a time when you experience an exacerbation of (increase in) symptoms and a loss of function.
Several of the old mental listings included having repeated episodes of decompensation as a way to prove that a mental illness was affecting an individual's ability to function. (Generally, you had to have had at least three episodes of decompensation per year, and each episode must have lasted for a minimum of two weeks.) Alternatively, if an individual had such a fragile mental status that a "minimal increase in mental demands or change in the environment would be predicted to cause the individual to decompensate" could help qualify someone for disability.
New Disability Listings and Mental Deterioration
Social Security updated its mental disability listings in 2017 and, in doing so, removed the term "episodes of decompensation" from all mental disability listings. However, Social Security left in similar language for some of the listings (see list below).
An individual can still qualify under the listings if an individual has had the disorder for two years, it has been serious and persistent, and the individual is receiving intensive treatment and has "minimal capacity to adapt to changes in their environment or to demands that are not already part of their daily life. " In Social Security's words, this means the individual has achieved only "marginal adjustment."
" In Social Security's words, this means the individual has achieved only "marginal adjustment."
According to the new listings, Social Security will find that an individual has made only marginal adjustment if the medical records show that changes or increased demands have led to an "exacerbation of symptoms and signs" and to a "deterioration in functioning" (roughly the same thing as episodes of decompensation). Evidence of marginal adjustment can be documentation of "episodes of deterioration that have required you to be hospitalized or absent from work, making it difficult for you to sustain work activity over time."
The listings no longer include any guidelines for how many episodes of deterioration an individual must have had or how long they must have lasted.
Listings Including Marginal Adjustment and Deterioration Language
Social Security included the above language on minimal capacity to adapt to changes and episodes of deterioration that can prove marginal adjustment for the following mental listings:
- post-traumatic stress disorder
- anxiety
- bipolar disorder
- depression
- schizophrenia
- autism, and
- neurocognitive disorders, such as dementia or TBI (formerly called organic mental disorders).
Similar language about episodes of decompensation was removed from the listings for autistic spectrum disorders, intellectual disability (low IQ), personality disorders, and somatic symptom disorders. In other words, having had periods of deterioration, or having a doctor who is worried a patient will have periods of deterioration, is no longer allowed a way to show limitations in functioning for these mental disorders.
Documenting Episodes of Decompensation or Deterioration
It's important to have the proper documentation for any episodes of deterioration. This means that you have to seek treatment during each period of deterioration, if possible. Just as seizure patients need to have their seizures documented, and asthma patients need to have their asthma attacks documented, you need to have a record of your episodes of decompensation. And your doctor's notes concerning your deterioration must be very detailed as to the character and duration of your decompensation episodes, and how your functioning is impaired during the episodes.
Decompensation and SSDI Evaluations - Hill & Ponton, P.A.
People whose ability to work is impaired by mental illness or a psychiatric disorder may be entitled to Social Security Disability Insurance (SSDI) benefits, if the condition makes them totally disabled from working. SSDI benefits can be awarded to those suffering illnesses such as anxiety, depression, bipolar disorder (manic-depressive disorder), schizophrenia, agoraphobia (fear of public or open places), or post-traumatic stress disorder (PTSD), among others.
One common problem with proving total disability based on mental disorders is the up and down nature of some illnesses, which may not appear at first to prevent working, because a person may function relatively well for periods of time or in lower-stress situations. However, the SSA recognizes that these same individuals can experience sudden, extreme downturns known as “decompensation episodes,” which make it impossible for them to maintain employment.
“Decompensation” is a term used by mental health professionals to refer to episodes during which a person’s existing mental-health or psychiatric disorder deteriorates, for a time, to include symptoms that are unusually severe. Crippling panic attacks are a common example, but decompensation symptoms vary for different mental disorders.
Mental Illness Disability and DecompensationThe SSA defines disability as a proven medical condition that is expected to last a year or more (or result in death) and that prevents the sufferer from engaging in “substantial gainful activity” (currently, this means working enough to earn a little over $1,000/month). When the claimant has a mental illness or psychiatric disorder with symptoms that fluctuate in severity, proving the existence of decompensation episodes can be crucial to winning disability benefits.
While a sufferer might not seem fully disabled from working during better periods, the fact that decompensation episodes can produce sudden and marked changes in ability can provide additional proof necessary to show that a claimant meets the SSA’s definition of disability.
To help prove SSDI disability, the medical records of treatment for decompensation episodes must include the kind of evidence that the SSA considers important. When the SSA considers an SSDI application based on mental disorder, it first looks to see whether a claimant is diagnosed with an illness contained in SSA’s list of disabling conditions (often called the “blue book”) or equal in severity to one that is on the list, which includes 9 categories:
• Organic mental disorders
• Schizophrenic, paranoid, and other psychotic disorders
• Affective disorders
• Mental retardation
• Anxiety-related disorders
• Somatoform disorders
• Personality disorders
• Substance disorders
• Autistic and other pervasive developmental disorders
Each category is divided into parts (usually Parts A, B, and sometimes C or D) that describe what must be proven if a claimant is to be found legally disabled for SSDI purposes, including (1) the symptoms that must be present for diagnosis of the illness; and (2) the disabling results, or functional limitations, that the illness must cause, in order to be considered legally disabling for purposes of SSDI.
In many of the SSA mental disorder listings, “repeated episodes of decompensation, each of extended duration” is one factor that can be used to show evidence of disability. To qualify for SSDI on this basis, the claimant’s evidence usually must show the SSA that decompensation episodes:
• Occur at least 3 times within a year (or an average of once every 4 months) and last at least 2 weeks each time; and
• Limit functional abilities in these areas:
o Daily living activities;
o Social activities; or
o Activities that require concentration, persistence, or pace.
However, a claimant might be able to show a condition “as severe as” one on the list, with evidence of decompensation episodes that happen more often, but endure for shorter periods of time, or vice-versa. There are also other ways that decompensation episodes can be used to help prove total disability in SSDI cases.
Proving Decompensation EpisodesThe claimant must be sure to seek the right kind of medical help and provide the right details to doctors or psychiatrists. Claimants or family members should give medical providers detailed descriptions of how often the episodes occur, how long they last, and the types and degree of limitation that they place on the claimant’s ability to function.
Claimants or family members should give medical providers detailed descriptions of how often the episodes occur, how long they last, and the types and degree of limitation that they place on the claimant’s ability to function.
Seeking treatment during decompensation episodes can be crucial to an SSDI benefits claim. In SSDI cases, the key to proving the existence and impact of decompensation episodes is to compile detailed medical records. To get medical records with the right kind of detail, the claimant must get proper treatment during these downturns.
For many people seeking SSDI benefits based on a mental or emotional disability, it can be difficult to seek medical attention during periods when symptoms suddenly worsen. In fact, decompensation can often make it hard for sufferers to cope with the prospect of a trip to the doctor, causing them to cancel or reschedule appointments; but making it to the doctor can be critical to a disability case for SSDI benefits.
Proving decompensation episodes to get SSDI benefits can be a complex process. Other evidence, combined with good medical records, can also demonstrate the impact that decompensation episodes have on a person’s life. These include disability journals, which record the details of episodes as they happen, and testimony from family members, co-workers, and friends with first-hand knowledge of the limits that a mental illness places on the claimant. Every case is different, and an experienced Social Security Disability Attorney can help assess an individual case and determine the best methods of proving disability in each one.
How useful was this post?
Click on a star to rate it!
We are sorry that this post was not as useful for you!
Help us improve this post!
Tell us how we can improve this post?
Matthew Hill
Mr. Hill focuses his practice on representing the disabled veterans. He is a member of the Florida Bar and the Washington D. C. Bar. He is licensed to practice before the United States District Court in and for the Middle District of Florida, as well as the United States Court of Appeals for Veterans Claims. He represents veterans and their dependents across the nation.
C. Bar. He is licensed to practice before the United States District Court in and for the Middle District of Florida, as well as the United States Court of Appeals for Veterans Claims. He represents veterans and their dependents across the nation.
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan.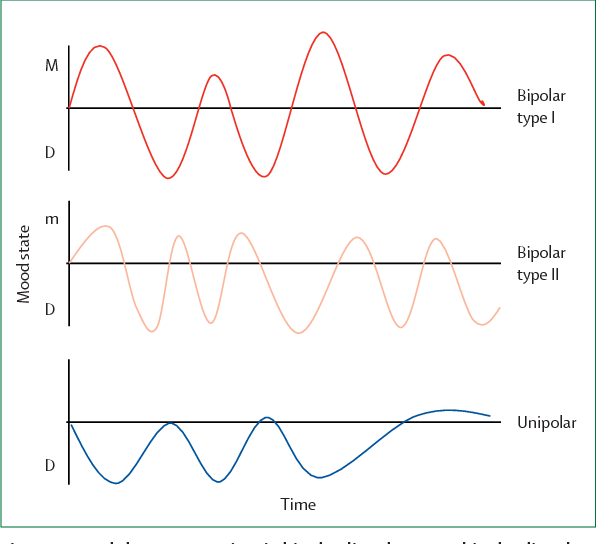 In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. They may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.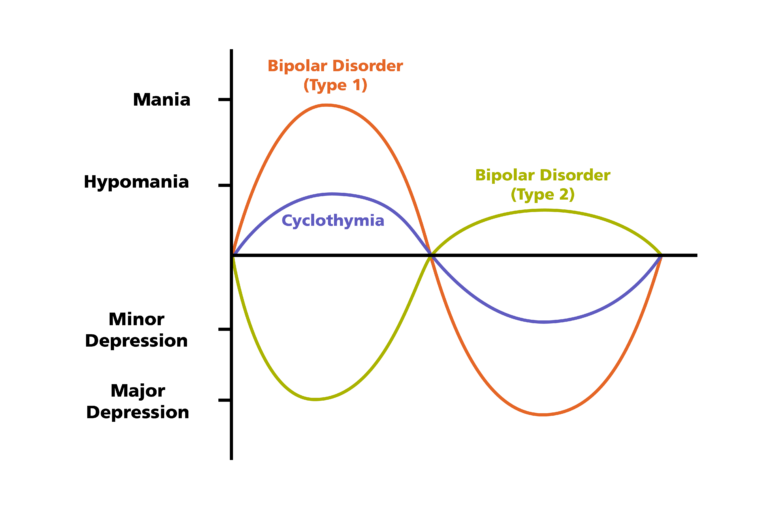 The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships.
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Titov proposed to release prisoners with epilepsy and severe depression - RBC
Business Ombudsman proposed to expand the list of diseases that prevent the detention of the accused.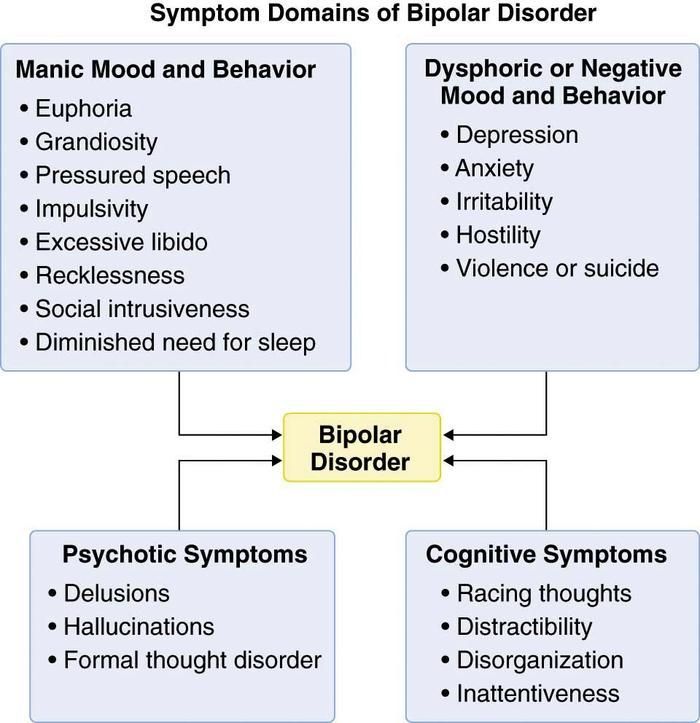 He considered it necessary to include severe forms of depression and all types of cancer requiring treatment outside SIZO
He considered it necessary to include severe forms of depression and all types of cancer requiring treatment outside SIZO
Boris Titov (Photo: Nail Fattakhov / TASS)
Commissioner for Entrepreneurs' Rights Boris Titov sent his proposals to the Supreme Court to change the list of diseases in which persons under investigation, defendants and convicts, whose sentence has not yet entered into legal force, are subject to release from custody . This was reported to RBC by the press service of the business ombudsman, a copy of his letter addressed to the deputy chairman of the Supreme Court Vladimir Davydov is at the editorial office.
In 2019, Titov headed a working group to amend Government Decree No. 3. It refers to the procedure for medical examination of suspects and defendants who are being held in a pre-trial detention center. The group has developed a position that it is necessary to expand the list of diseases for which persons under investigation should be released. At the same time, the “stages and severity of diseases” requiring release for persons whose guilt has not yet been proven by the court should be lower than for convicts held in colonies, follows from the position set out in the letter.
At the same time, the “stages and severity of diseases” requiring release for persons whose guilt has not yet been proven by the court should be lower than for convicts held in colonies, follows from the position set out in the letter.
With what diagnoses it is proposed to release
www.adv.rbc.ru
According to the current Decree No. 3, oncological diseases of the “4th clinical group in the presence of distant metastases in the preterminal state” (that is, types and stages of cancer that are not subject to any treatment other than palliative) can be the basis for the release of a prisoner. Also, these are curable oncological diseases that require hospitalization in a specialized hospital.
www.adv.rbc.ru
Titov proposes to slightly change this norm: his proposals refer to all forms of cancer if treatment cannot be obtained in a place of deprivation of liberty. In addition, it is proposed to cancel the rule on mandatory histological confirmation of the diagnosis (which includes a biopsy and a serious laboratory test), if it is a hard-to-reach or intracranial tumor.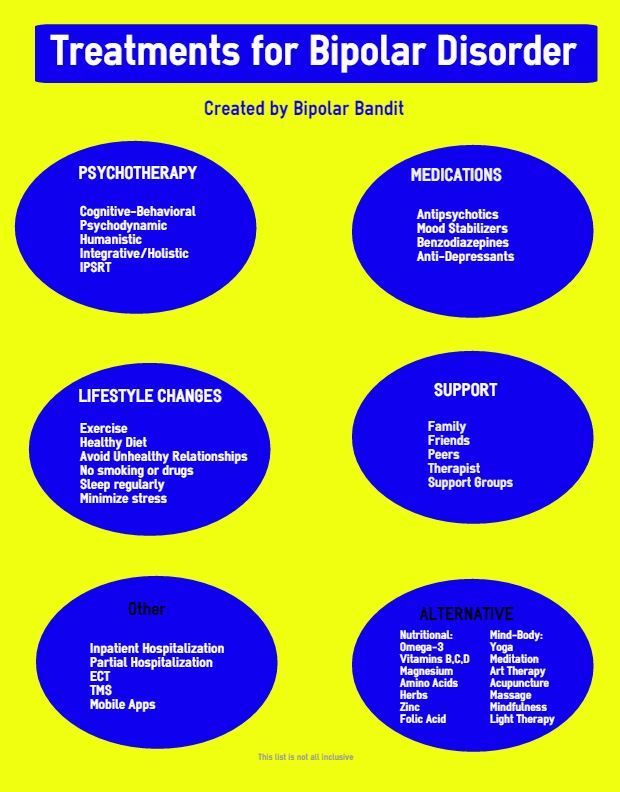 In addition to malignant neoplasms that "compress internal organs or grow into them," Titov's list includes various types of leukemia, aplastic anemia, and space-occupying tumors of the brain or spinal cord that affect a person's ability to serve himself.
In addition to malignant neoplasms that "compress internal organs or grow into them," Titov's list includes various types of leukemia, aplastic anemia, and space-occupying tumors of the brain or spinal cord that affect a person's ability to serve himself.
Another proposed change relates to prisoners with HIV in phase 4B, which involves the development of "severe, life-threatening" secondary illnesses. The current resolution assumes that in order to be released, the patient must have "persistent impairment of body functions, leading to a significant limitation of life and requiring long-term treatment in a specialized medical hospital." The business ombudsman also proposes to release prisoners with HIV in phase 4B “in the progression stage”.
It is also proposed to release persons under investigation with certain mental illnesses (the current list does not contain them at all). On his list are any “chronic and prolonged mental disorders”, the manifestations of which do not allow the sick person to realize their actions and their danger, as well as depressive episodes and severe recurrent depressions, bipolar affective disorder in the severe depressive phase, delirium and dementia (as associated with alcohol and drug use, and not), panic disorder with severe cardiac symptoms, severe agoraphobia or in combination with hypertension and asthma.![]()
The Ombudsman considers that it is necessary to include in the list milder than the current list of cardiovascular diseases (for example, hypertensive and coronary heart disease with chronic heart failure stage III instead of IV). Among the diseases of the nervous system, Titov names severe Parkinson's disease and epilepsy with a certain frequency and severity of seizures. Also on the proposed list are more detailed lists of tuberculosis and endocrine diseases (including various types of diabetes with complications, cystic fibrosis and severe pituitary dysfunction), decompensated cirrhosis of the liver, neurosyphilis, and extremely rare diseases such as fatal familial insomnia.
Titov proposes to extend this list to defendants and convicts whose sentences have not yet entered into force. Now people who have already been convicted, but continue to be held in a pre-trial detention center until an appeal, often find themselves in a “blind zone”: there is no definite position on whether to apply the norms from the 3rd resolution or from the 54th to them. In addition, the Ombudsman suggests that the decision on the medical examination of prisoners in the pre-trial detention center should not be taken by representatives of the investigating authorities or the administration of institutions; this should only be done by healthcare professionals.
In addition, the Ombudsman suggests that the decision on the medical examination of prisoners in the pre-trial detention center should not be taken by representatives of the investigating authorities or the administration of institutions; this should only be done by healthcare professionals.
Problems with the application of the list
The proposed changes “are of a revolutionary nature, and if they are adopted in this form, it will play a significant role” in humanizing the penitentiary system and bringing it closer to international standards, Anastasia, head of the Trans-Baikal Human Rights Center, told RBC Kopteev. According to her, the most fundamental of the proposed amendments concern prisoners with HIV, tuberculosis, diabetes and cancer, while missing some important diseases of the musculoskeletal system.
There are more problems with the institution of releasing sick prisoners under investigation than with releasing sick convicts, Kopteeva said: for example, government decree No. 54, dedicated to convicts, initially contained a wider list of diagnoses and subsequently underwent significant adjustments; with Resolution No. 3, this did not happen. “According to the 54th resolution, it is somehow possible to work, the third one does not work at all,” says Kopteeva, explaining that, as a rule, prisoners are not released at the investigation stage under any circumstances. In some situations, in order to achieve the release of a prisoner, one has to wait for a guilty verdict, the lawyer says.
54, dedicated to convicts, initially contained a wider list of diagnoses and subsequently underwent significant adjustments; with Resolution No. 3, this did not happen. “According to the 54th resolution, it is somehow possible to work, the third one does not work at all,” says Kopteeva, explaining that, as a rule, prisoners are not released at the investigation stage under any circumstances. In some situations, in order to achieve the release of a prisoner, one has to wait for a guilty verdict, the lawyer says.
There are indeed problems with the impossibility of obtaining the release of seriously ill prisoners, but they are more related to law enforcement than to the regulatory framework, believes Alexei Fedyarov, head of the legal department of the Rus Sitting Foundation: for example, there is a large category of prisoners who fall under the list, but not can achieve release.
The lawyer gave an example of how the institute for the release of seriously ill prisoners works: “We had a case when, according to the third decision, we pulled a person under investigation under house arrest.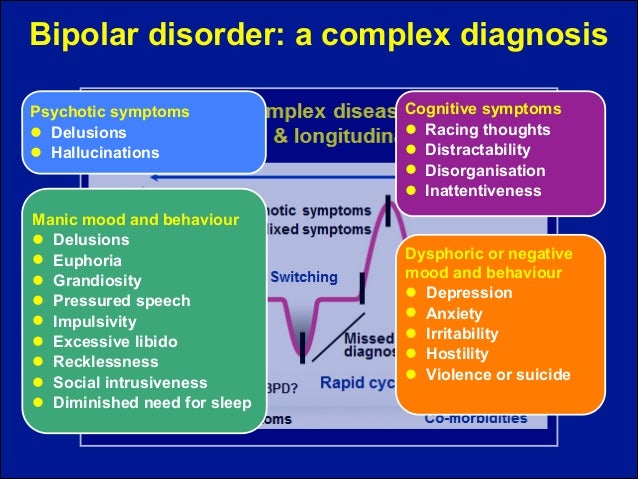 Then he was arrested by verdict, we again secured his release. After an appeal, he was again taken into custody. The doctors concluded that he also fits under the 54th ruling, the court granted the petition for his release. The prosecutor appealed against this, the second instance granted his appeal and sent a request for release for a new consideration. Without waiting for the second consideration, the person died.
Then he was arrested by verdict, we again secured his release. After an appeal, he was again taken into custody. The doctors concluded that he also fits under the 54th ruling, the court granted the petition for his release. The prosecutor appealed against this, the second instance granted his appeal and sent a request for release for a new consideration. Without waiting for the second consideration, the person died.
The expansion of the list of diseases that prevent detention is a positive thing, but it would be better if, instead of closed lists, there were criteria for the severity of the condition of a sick prisoner, on the basis of which the issue of his release would be decided, said RBC, cooperating with a human rights organization " Law Zone” lawyer Svetlana Sidorkina. “Movement in this direction is good, but this is a partial measure that does not solve the problem globally,” she explained. Among her clients were the auditor Vladimir Topekhin, convicted in a fraud case, who in 2014 sought release with complete paralysis of the lower body for several months, and Margarita Charykova, accused under the “drug” article of the Criminal Code, who was kept in a pre-trial detention center with a congenital pathology associated with the lack of rectum, which required daily medical care.