Ect long term memory loss
The long-term impact of treatment with electroconvulsive therapy on discrete memory systems in patients with bipolar disorder
1. APA. Practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry 2002;159:1-50. [PubMed]
2. UK ECT Review Group et al. Efficacy and safety of electro-convulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet 2003;361:799-808. [PubMed]
3. Goodwin GM. Evidence-based guidelines for treating bipolar disorder: recommendations from the British Association for Psychopharmacology. J Psychopharmacol 2003;17:149-73. [PubMed]
4. Royal Australian and New Zealand College of Psychiatrist Clinical Practice Guidelines Team for Bipolar Disorder. Australian and New Zealand clinical practice guidelines for the treatment of bipolar disorder. Aust N Z J Psychiatry 2004;38:280-305. [PubMed]
5. Suppes T, Dennehy EB, Hirschfeld RM, et al. The Texas implementation of medication algorithms: update to the algorithms for treatment of bipolar I disorder. J Clin Psychiatry 2005;66:870-86. [PubMed]
6. Yatham LN, Kennedy SH, O'Donovan C, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines for the management of patients with bipolar disorder: consensus and controversies. Bipolar Disord 2005;7(Suppl 3):5-69. [PubMed]
7. Abraham G, Milev R, Delva N, et al. Clinical outcome and memory function with maintenance electroconvulsive therapy: a retrospective study. J ECT 2006;22:43-5. [PubMed]
8. Tharyan P, Adams CE. Electroconvulsive therapy for schizophrenia. Cochrane Database Syst Rev 2005;(2):CD000076. [PubMed]
9. Lekwauwa R, McQuoid D, Steffens DC. Hippocampal volume is associated with physician-reported acute cognitive deficits after electroconvulsive therapy. J Geriatr Psychiatry Neurol 2006;19:21-5. [PubMed]
10. Bosboom PR, Deijen JB. Age-related cognitive effects of ECT and ECT-induced mood improvement in depressive patients. Depress Anxiety 2006;23:93-101.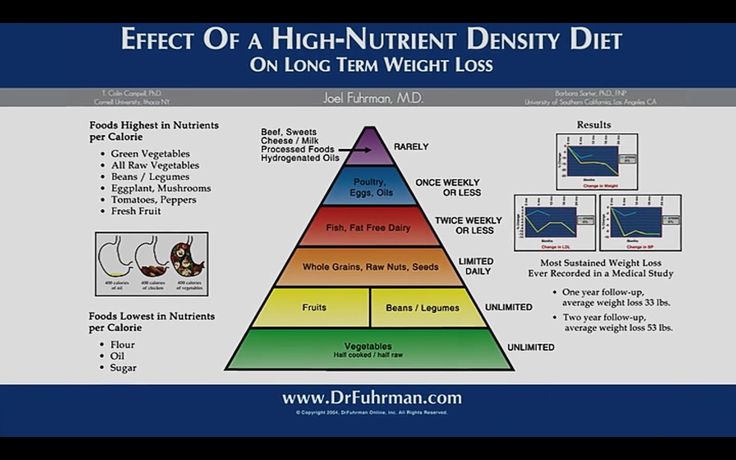 [PubMed]
[PubMed]
11. Datto CJ, Levy S, Miller DS, et al. Impact of maintenance ECT on concentration and memory. J ECT 2001;17:170-4. [PubMed]
12. Johanson A, Gustafson L, Risberg J, et al. Long-term follow-up in depressed patients treated with electroconvulsive therapy. J ECT 2005;21:214-20. [PubMed]
13. Butterfield NN, Graf P, Macleod BA, et al. Propofol reduces cognitive impairment after electroconvulsive therapy. J ECT 2004;20:3-9. [PubMed]
14. Frasca TA, Iodice A, McCall WV. The relationship between changes in learning and memory after right unilateral electroconvulsive therapy. J ECT 2003;19:148-50. [PubMed]
15. Legendre SA, Stern RA, Solomon DA, et al. The influence of cognitive reserve on memory following electroconvulsive therapy. J Neuropsychiatry Clin Neurosci 2003;15:333-9. [PubMed]
16. Rami-Gonzalez L, Salamero M, Boget T, et al. Pattern of cognitive dysfunction in depressive patients during maintenance electroconvulsive therapy.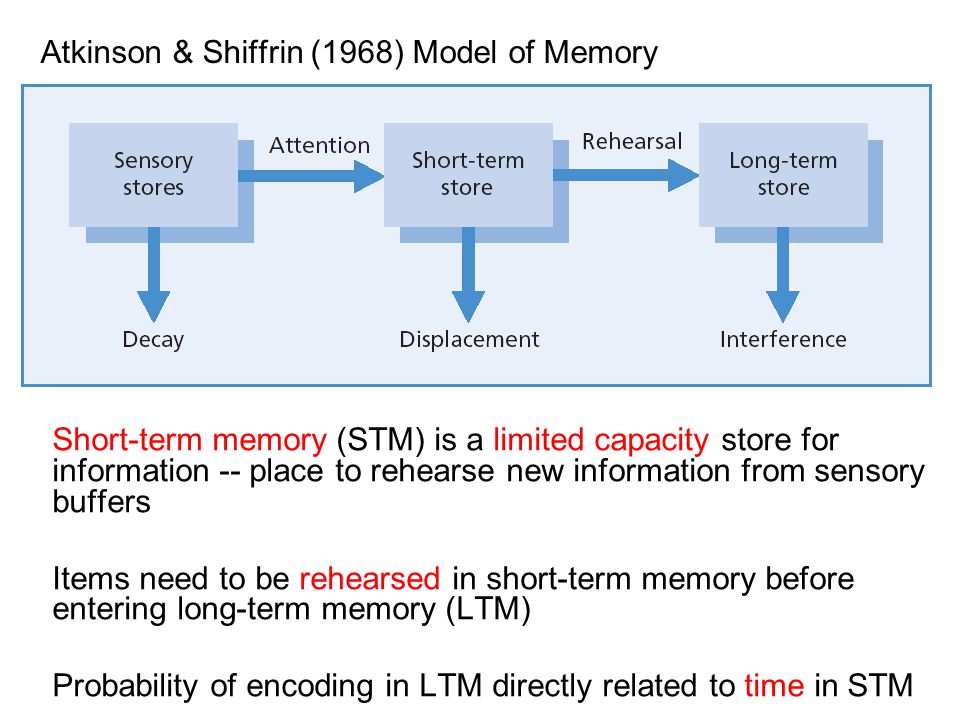 Psychol Med 2003;33:345-50. [PubMed]
Psychol Med 2003;33:345-50. [PubMed]
17. Rami L, Bernardo M, Boget T, et al. Cognitive status of psychiatric patients under maintenance electroconvulsive therapy: a one-year longitudinal study. J Neuropsychiatry Clin Neurosci 2004;16:465-71. [PubMed]
18. Abrams R. Does brief-pulse ECT cause persistent or permanent memory impairment? J ECT 2002;18:71-3. [PubMed]
19. Andre L. Memory loss: from polarization to reconciliation. J ECT 2001;17:228-9. [PubMed]
20. Donahue AB. Electroconvulsive therapy and memory loss: a personal journey. J ECT 2000;16:133-43. [PubMed]
21. Koopowitz LF, Chur-Hansen A, Reid S, et al. The subjective experience of patients who received electroconvulsive therapy. Aust N Z J Psychiatry 2003;37:49-54. [PubMed]
22. Prudic J, Peyser S, Sackeim HA. Subjective memory complaints: a review of patient self-assessment of memory after electroconvulsive therapy. J ECT 2000;16:121-32.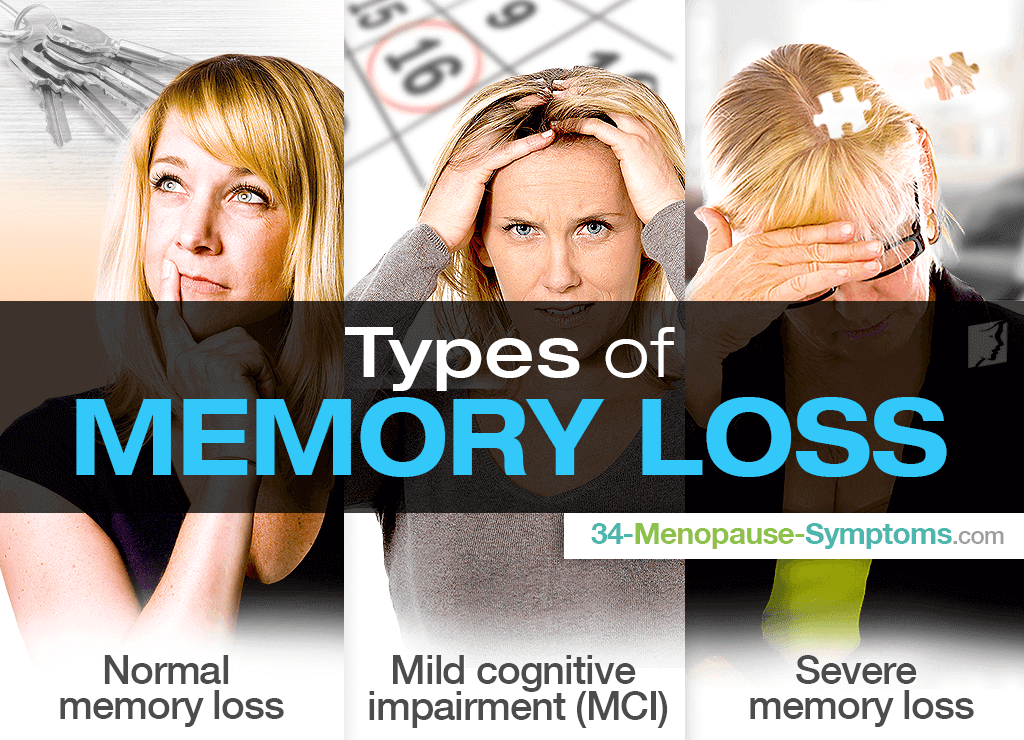 [PubMed]
[PubMed]
23. Reisner AD. The electroconvulsive therapy controversy: evidence and ethics. Neuropsychol Rev 2003;13:199-219. [PubMed]
24. Sackeim HA. Memory and ECT: from polarization to reconciliation. J ECT 2000;16:87-96. [PubMed]
25. Rose D, Fleischmann P, Wykes T, et al. Patients' perspectives on electroconvulsive therapy: systematic review. BMJ 2003;326:1363. [PMC free article] [PubMed]
26. Sienaert P, De BT, Vansteelandt K, et al. Patient satisfaction after electroconvulsive therapy. J ECT 2005;21:227-31. [PubMed]
27. Sweeney JA, Kmiec JA, Kupfer DJ. Neuropsychologic impairments in bipolar and unipolar mood disorders on the CANTAB neuro-cognitive battery. Biol Psychiatry 2000;48:674-84. [PubMed]
28. Grant MM, Thase ME, Sweeney JA. Cognitive disturbance in outpatient depressed younger adults: evidence of modest impairment. Biol Psychiatry 2001;50:35-43. [PMC free article] [PubMed]
29. Tavares JV, Drevets WC, Sahakian BJ.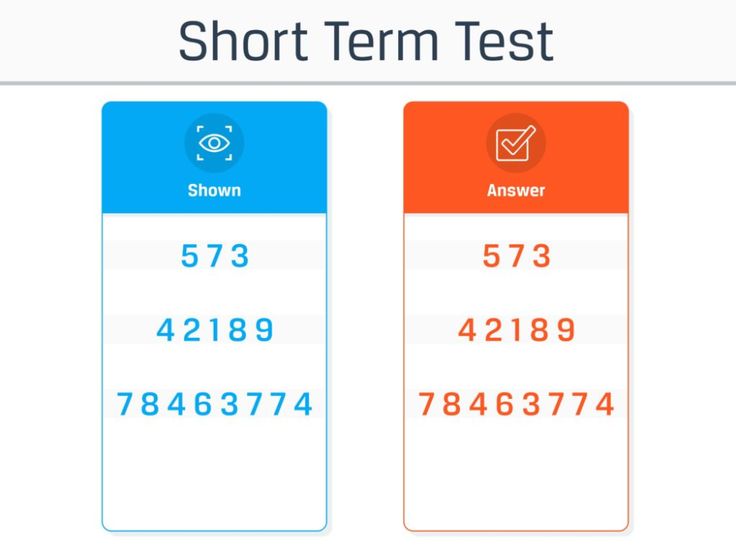 Cognition in mania and depression. Psychol Med 2003;33:959-67. [PubMed]
Cognition in mania and depression. Psychol Med 2003;33:959-67. [PubMed]
30. Borkowska A, Rybakowski JK. Neuropsychological frontal lobe tests indicate that bipolar depressed patients are more impaired than unipolar. Bipolar Disord 2001;3:88-94. [PubMed]
31. Smith DJ, Muir WJ, Blackwood DH. Neurocognitive impairment in euthymic young adults with bipolar spectrum disorder and recurrent major depressive disorder. Bipolar Disord 2006;8:40-6. [PubMed]
32. Wolfe J, Granholm E, Butters N, et al. Verbal memory deficits associated with major affective disorders: a comparison of unipolar and bipolar patients. J Affect Disord 1987;13:83-92. [PubMed]
33. Savard RJ, Rey AC, Post RM. Halstead-Reitan Category Test in bipolar and unipolar affective disorders. Relationship to age and phase of illness. J Nerv Ment Dis 1980;168:297-304. [PubMed]
34. Kessing LV. Cognitive impairment in the euthymic phase of affective disorder. Psychol Med 1998;28:1027-38. [PubMed]
[PubMed]
35. First MB, Spitzer RL, Gibbon M. Structured Clinical Interview for Axis-I-DSM-IV Disorders. New York: Biometrics Research; 1994.
36. Young RC, Biggs JT, Ziegler VE, et al. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 1978;133:429-35. [PubMed]
37. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62. [PMC free article] [PubMed]
38. Nelson H. National Adult Reading Test Manual. Windsor: NFER-Nelson; 1982.
39. Bodlund O, Kullgren G, Ekselius L, et al. Axis V–Global Assessment of Functioning Scale. Evaluation of a self-report version. Acta Psychiatr Scand 1994;90:342-7. [PubMed]
40. Broadbent DE, Cooper PF, FitzGerald P, et al. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol 1982; 21: 1-16. [PubMed]
41. MacQueen GM, Galway TM, Hay J, et al. Recollection memory deficits in patients with major depressive disorder predicted by past depressions but not current mood state or treatment status. Psychol Med 2002;32:251-8. [PubMed]
Psychol Med 2002;32:251-8. [PubMed]
42. Delis DC, Freeland J, Kramer JH, et al. Integrating clinical assessment with cognitive neuroscience: construct validation of the California Verbal Learning Test. J Consult Clin Psychol 1988;56:123-30. [PubMed]
43. Osuji IJ, Cullum CM. Cognition in bipolar disorder. Psychiatr Clin North Am 2005;28:427-41. [PubMed]
44. Otto MW, Bruder GE, Fava M, et al. Norms for depressed patients for the California verbal learning test: associations with depression severity and self-report of cognitive difficulties. Arch Clin Neuropsychol 1994;9:81-8. [PubMed]
45. Jacoby LL. Invariance in automatic influences of memory: toward a user's guide for the process-dissociation procedure. J Exp Psychol Learn Mem Cogn 1998;24:3-26. [PubMed]
46. Jacoby LL, Jennings JM, Hay JF. Dissociating automatic and consciously controlled processes: implications for diagnosis and rehabilitation of memory deficits.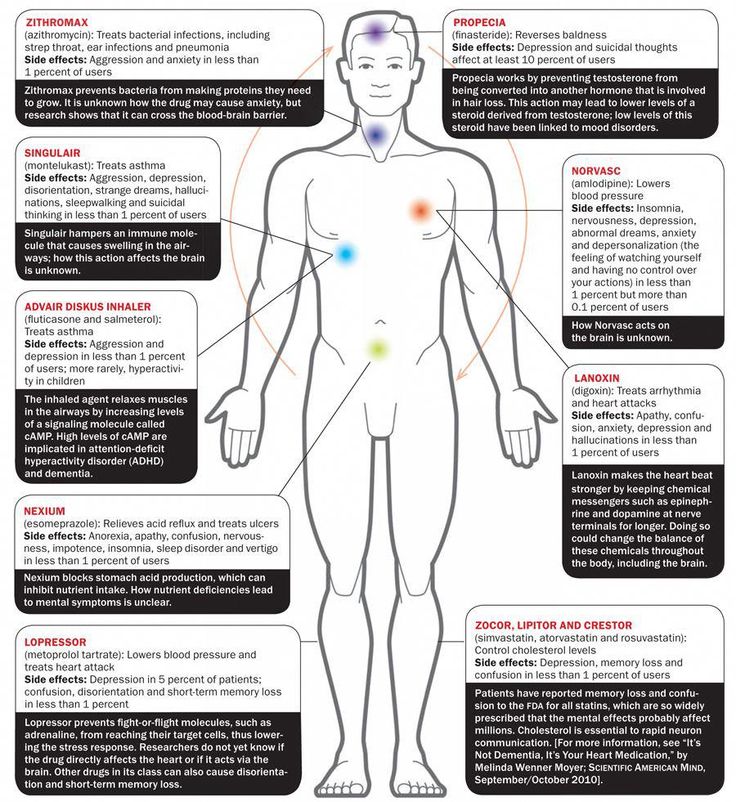 In: Herman DJ, editor. Basic and Applied Memory Research. Mahwah (NJ): Lawrence Erlbaum Associates; 1996. p. 161-93.
In: Herman DJ, editor. Basic and Applied Memory Research. Mahwah (NJ): Lawrence Erlbaum Associates; 1996. p. 161-93.
47. Ruiz-Caballero JA, Gonzalez P. Effects of level of processing on implicit and explicit memory in depressed mood. Motivation and Emotion 1997;21:195-209.
48. MacQueen GM, Campbell S, McEwen BS, et al. Course of illness, hippocampal function, and hippocampal volume in major depression. Proc Natl Acad Sci U S A 2003;100:1387-92. [PMC free article] [PubMed]
49. Schneider W. Microexperimental laboratory: an integrated system for IBM PC compatibles. Behav Res Meth Instr Comp 1988;20:206-17.
50. Larrabee GJ, Trahan DE, Curtiss G. Construct validity of the Continuous Visual Memory Test. Arch Clin Neuropsychol 1992;7:395-405. [PubMed]
51. Larrabee GJ, Curtiss G. Construct validity of various verbal and visual memory tests. J Clin Exp Neuropsychol 1995;17:536-47. [PubMed]
52. Schulze-Rauschenbach SC, Harms U, Schlaepfer TE, et al. Distinctive neurocognitive effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in major depression. Br J Psychiatry 2005;186:410-6. [PubMed]
Distinctive neurocognitive effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in major depression. Br J Psychiatry 2005;186:410-6. [PubMed]
53. Robinson LJ, Ferrier IN. Evolution of cognitive impairment in bipolar disorder: a systematic review of cross-sectional evidence. Bipolar Disord 2006;8:103-16. [PubMed]
54. Bearden CE, Glahn DC, Monkul ES, et al. Sources of declarative memory impairment in bipolar disorder: mnemonic processes and clinical features. J Psychiatr Res 2006;40:47-58. [PubMed]
55. Robinson LJ, Thompson JM, Gallagher P, et al. A meta-analysis of cognitive deficits in euthymic patients with bipolar disorder. J Affect Disord 2006;93:105-15. [PubMed]
56. Fleck DE, Shear PK, Zimmerman ME, et al. Verbal memory in mania: effects of clinical state and task requirements. Bipolar Disord 2003;5:375-80. [PubMed]
57. Savitz J, Solms M, Ramesar R. Neuropsychological dysfunction in bipolar affective disorder: a critical opinion. Bipolar Disord 2005;7:216-35. [PubMed]
Bipolar Disord 2005;7:216-35. [PubMed]
58. Deckersbach T, McMurrich S, Ogutha J, et al. Characteristics of non-verbal memory impairment in bipolar disorder: the role of encoding strategies. Psychol Med 2004;34:823-32. [PubMed]
59. Altshuler LL, Ventura J, van Gorp WG, et al. Neurocognitive function in clinically stable men with bipolar I disorder or schizophrenia and normal control subjects. Biol Psychiatry 2004;56:560-9. [PubMed]
60. Doris A, Belton E, Ebmeier KP, et al. Reduction of cingulate gray matter density in poor outcome bipolar illness. Psychiatry Res 2004;130: 153-9. [PubMed]
61. Jones BP. Duncan CC, Mirsky AF. Neuropsychological profiles in bipolar affective disorder and complex partial seizure disorder. Neuropsychology 1994;8:55-64.
62. van Gorp WG, Altshuler L, Theberge DC, et al. Cognitive impairment in euthymic bipolar patients with and without prior alcohol dependence. A preliminary study.
Arch Gen Psychiatry 1998;55:41-6. [PubMed]
[PubMed]
63. Rubinsztein JS, Michael A, Paykel ES, et al. Cognitive impairment in remission in bipolar affective disorder. Psychol Med 2000;30:1025-36. [PubMed]
64. Martinez-Aran A, Vieta E, Colom F, et al. Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord 2004;6:224-32. [PubMed]
65. Martinez-Aran A, Vieta E, Reinares M, et al. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry 2004;161:262-70. [PubMed]
66. Denicoff KD, Ali SO, Mirsky AF, et al. Relationship between prior course of illness and neuropsychological functioning in patients with bipolar disorder. J Affect Disord 1999;56:67-73. [PubMed]
67. Clark L, Iversen SD, Goodwin GM. Sustained attention deficit in bipolar disorder. Br J Psychiatry 2002;180:313-9. [PubMed]
68. Cavanagh JT, Van BM, Muir W, et al. Case-control study of neurocognitive function in euthymic patients with bipolar disorder: an association with mania.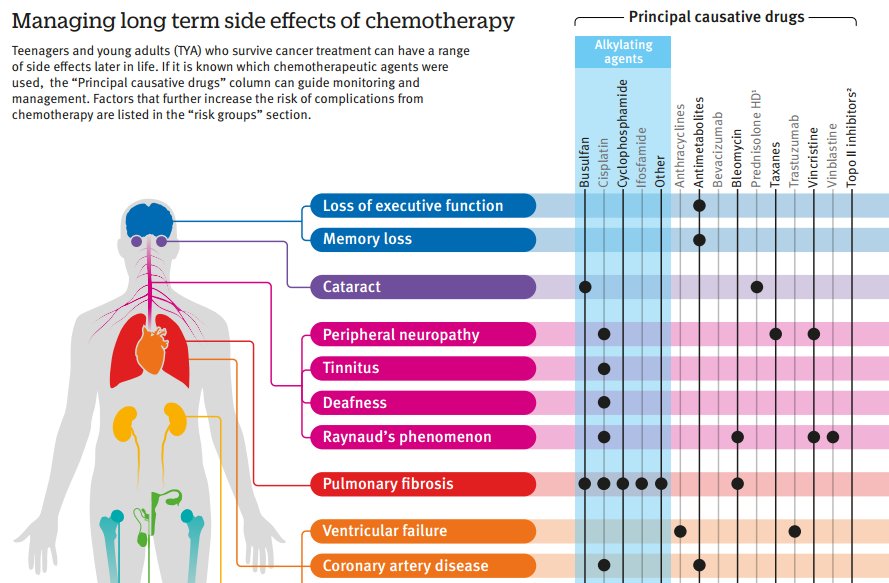 Br J Psychiatry 2002;180:320-6. [PubMed]
Br J Psychiatry 2002;180:320-6. [PubMed]
69. Prakash J, Kotwal A, Prabhu H. Therapeutic and prophylactic utility of the memory-enhancing drug donepezil hydrochloride on cognition of patients undergoing electroconvulsive therapy: a randomized controlled trial. J ECT 2006;22:163-8. [PubMed]
70. Moscrip TD, Terrace HS, Sackeim HA, et al. Randomized controlled trial of the cognitive side-effects of magnetic seizure therapy (MST) and electroconvulsive shock (ECS). Int J Neuropsychopharmacol 2006;9:1-11. [PubMed]
71. Butterfield NN, Graf P, Macleod BA, et al. Propofol reduces cognitive impairment after electroconvulsive therapy. J ECT 2004;20:3-9. [PubMed]
72. Arts B, Peters M, Ponds R, et al. S100 and impact of ECT on depression and cognition. J ECT 2006;22:206-12. [PubMed]
[Doctor, will I get my memory back? Electroconvulsive therapy and cognitive side-effects in daily practice]
. 2017;59(10):632-637.
2017;59(10):632-637.
[Article in Dutch]
E Verwijk, J Obbels, H P Spaans, P Sienaert
- PMID: 29077139
Free article
[Article in Dutch]
E Verwijk et al. Tijdschr Psychiatr. 2017.
Free article
. 2017;59(10):632-637.
Authors
E Verwijk, J Obbels, H P Spaans, P Sienaert
- PMID: 29077139
Abstract
Background: Patients undergoing or about to undergo electroconvulsive therapy (ECT) are often afraid they will experience negative cognitive side-effects.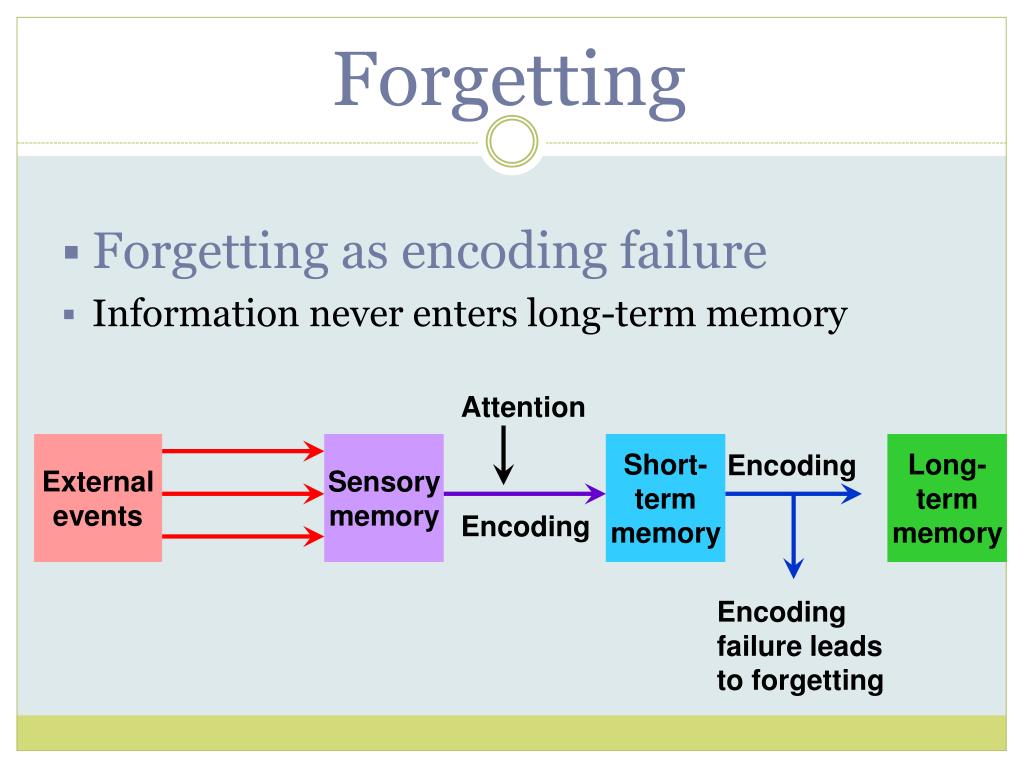
Aim: To answer questions that patients and referring clinicians often ask about cognitive problems that can result from ECT.
Method: To discuss, on the basis of clinical perception and literature, the cognitive problems resulting from ECT.
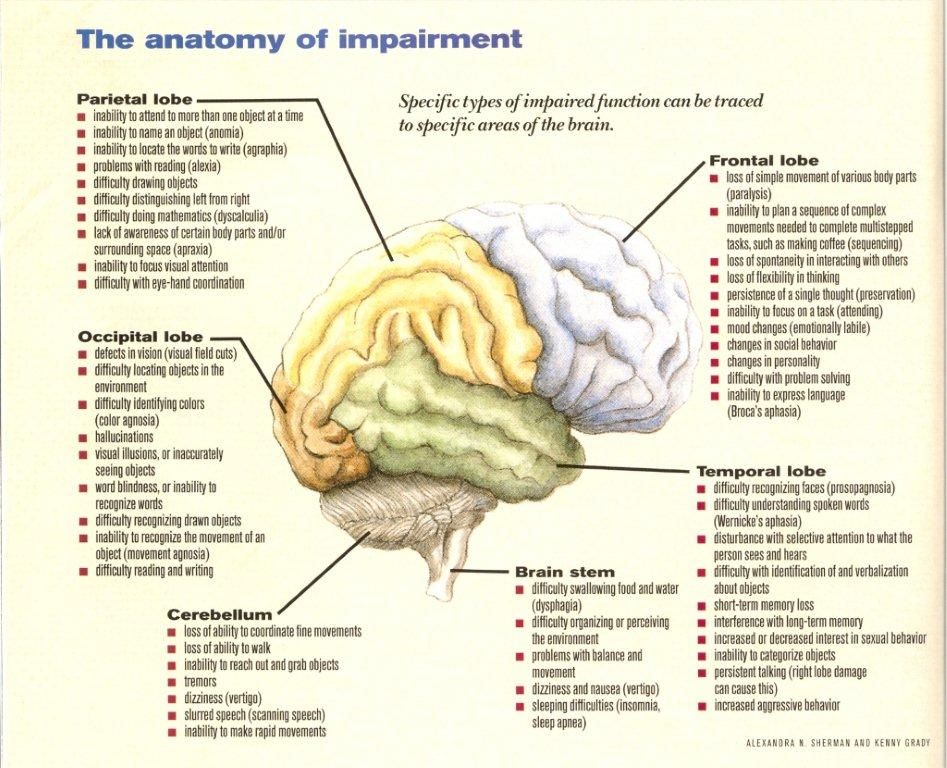
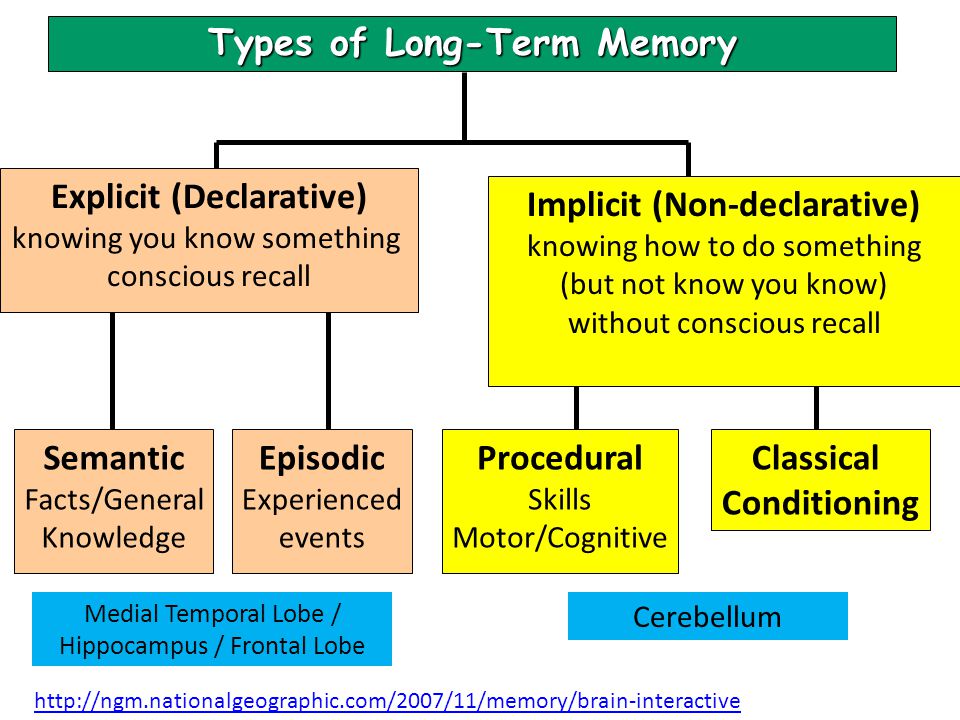
Results: The cognitive problems resulting from ect are threefold: short-term postictal confusion (immediately after the treatment), anterograde amnesia and retrograde amnesia. A patient affected by anterograde amnesia, is temporarily less able to remember what he or she has experienced over a period of three months after treatment. The brain of a patient with retrograde amnesia is unable to retrieve or remember information or procedures 'saved' before the treatment took place. More specifically the patient with retrograde amnesia has three main types of problems: semantic memory problems (relating to facts), episodic memory problems (no longer able to retrieve memories concerning non-personal events), and procedural memory problems (no longer able to operate various devices). It is difficult to predict which patients will experience cognitive problems as a result from ect and to what extent. However, the problems are not intensified by maintenance treatment. Factual and autobiographical memory problems following ect-induced retrograde amnesia seems to have a more permanent character. According to the Dutch guidelines for ECT, cognitive side-effects need to be monitored. If patients are monitored before and after ect, they can be given a more targeted psycho-education and eventually a more targeted training course.
It is difficult to predict which patients will experience cognitive problems as a result from ect and to what extent. However, the problems are not intensified by maintenance treatment. Factual and autobiographical memory problems following ect-induced retrograde amnesia seems to have a more permanent character. According to the Dutch guidelines for ECT, cognitive side-effects need to be monitored. If patients are monitored before and after ect, they can be given a more targeted psycho-education and eventually a more targeted training course.
Conclusion: We conclude that in clinical practice increasing attention is being given to ECT-related cognitive side-effects. Clearly, however, more consideration needs to be given to inter-individual variability. Cognitive monitoring is advisable because the course of the side-effects of ect must be followed and evaluated.
Similar articles
-
The effects of electroconvulsive therapy on memory of autobiographical and public events.
Lisanby SH, Maddox JH, Prudic J, Devanand DP, Sackeim HA. Lisanby SH, et al. Arch Gen Psychiatry. 2000 Jun;57(6):581-90. doi: 10.1001/archpsyc.57.6.581. Arch Gen Psychiatry. 2000. PMID: 10839336 Clinical Trial.
-
Predictors of retrograde amnesia following ECT.
Sobin C, Sackeim HA, Prudic J, Devanand DP, Moody BJ, McElhiney MC. Sobin C, et al. Am J Psychiatry. 1995 Jul;152(7):995-1001. doi: 10.1176/ajp.152.7.995. Am J Psychiatry. 1995. PMID: 7793470 Clinical Trial.
-
The Role of Baseline Cognitive Function in the Neurocognitive Effects of Electroconvulsive Therapy in Depressed Elderly Patients.
Dybedal GS, Tanum L, Sundet K, Bjølseth TM. Dybedal GS, et al. Clin Neuropsychol.
 2015;29(4):487-508. doi: 10.1080/13854046.2015.1050457. Epub 2015 Jun 1. Clin Neuropsychol. 2015. PMID: 26029851
2015;29(4):487-508. doi: 10.1080/13854046.2015.1050457. Epub 2015 Jun 1. Clin Neuropsychol. 2015. PMID: 26029851 -
Measuring retrograde autobiographical amnesia following electroconvulsive therapy: historical perspective and current issues.
Semkovska M, McLoughlin DM. Semkovska M, et al. J ECT. 2013 Jun;29(2):127-33. doi: 10.1097/YCT.0b013e318279c2c9. J ECT. 2013. PMID: 23303426 Review.
-
ECT and memory loss.
Squire LR. Squire LR. Am J Psychiatry. 1977 Sep;134(9):997-1001. doi: 10.1176/ajp.134.9.997. Am J Psychiatry. 1977. PMID: 331969 Review.
See all similar articles
Cited by
-
Seizures induced in electroconvulsive therapy as a human epilepsy model: A comparative case study.

Pottkämper JCM, Verdijk JPAJ, Hofmeijer J, van Waarde JA, van Putten MJAM. Pottkämper JCM, et al. Epilepsia Open. 2021 Dec;6(4):672-684. doi: 10.1002/epi4.12532. Epub 2021 Aug 20. Epilepsia Open. 2021. PMID: 34351710 Free PMC article.
MeSH terms
Fundamental Guide to Know
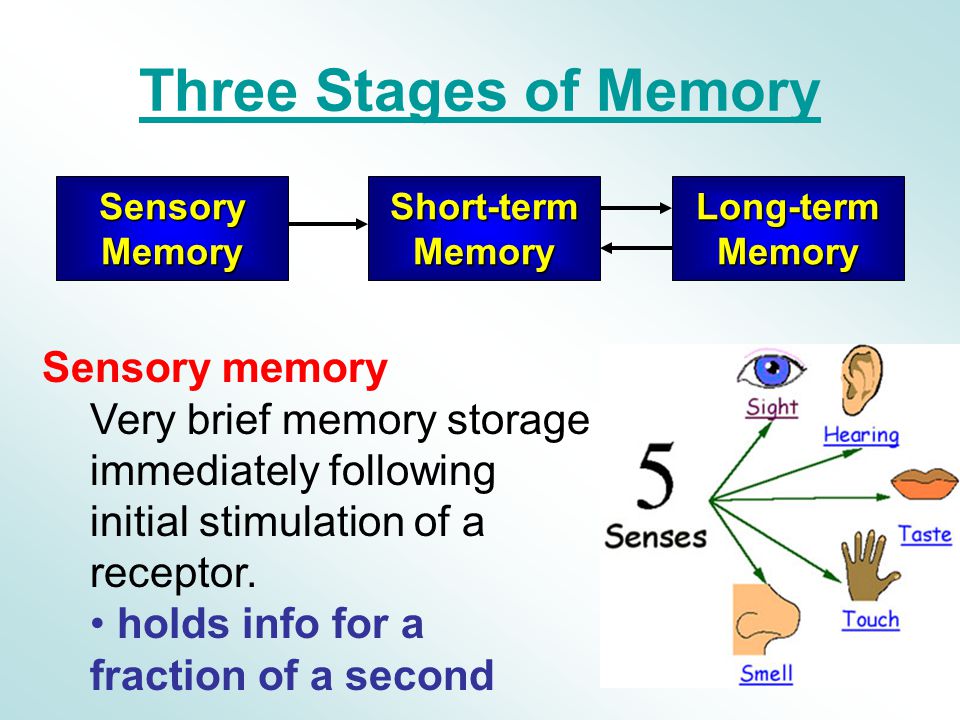
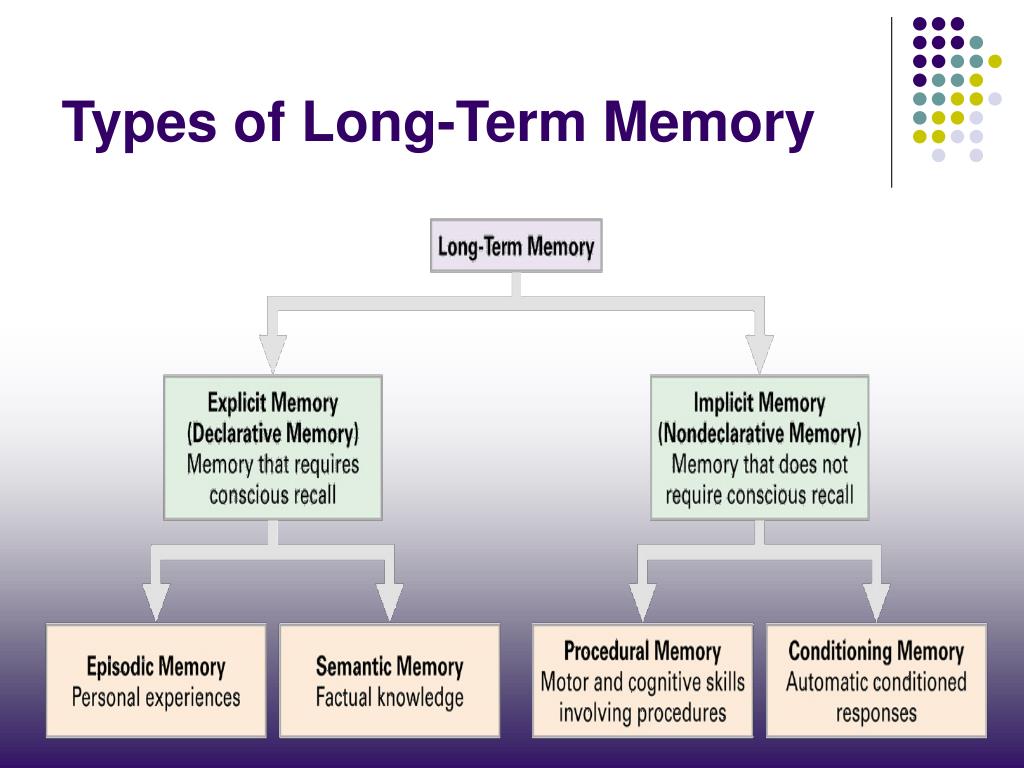
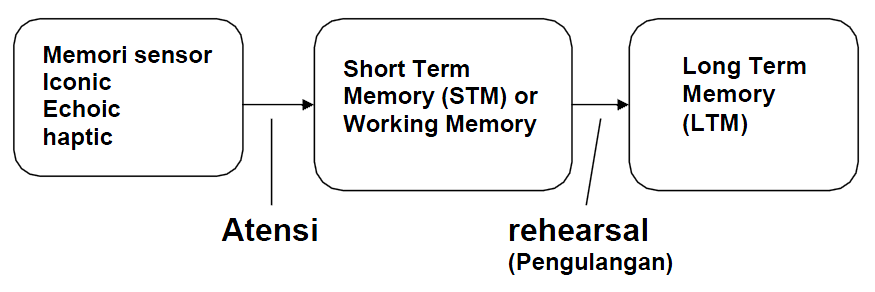
Our brains use different structures to deal with existing types of memory. There are two main types of memory: short-term memory and long-term memory. Although dysfunctions of both types of memory are possible, we will focus on Long-Term Declarative Memory.
- Short-term memory stores a limited amount of information for a short period of time.
- Long-term memory stores a large amount of complex information for a long time. This is what is usually called "memory". In turn, there are two types of Long-term memory: Non-declarative or Implicit Memory (cycling, driving) and Declarative or Explicit memory, used to remember our personal experience or knowledge about the world (what is the name of my relative, where I left clues as to who is in charge of my country, what happened five minutes or five months ago).
What is memory loss and symptoms
When we forget something, we usually don't "lose" the memory itself, but our brain "can't find a way" to what we're trying to remember. This "pathological" loss of memory is called amnesia. Here are some symptoms of memory loss:
- Often lose personal items.
- It's hard to find the right words.
- Asking repeated questions in a conversation or telling the same story over and over.
- Forgetting whether or not you have done something, such as taking medicine.
- Become disoriented or lost in familiar places.
- Confuse year or day of the week.
- Forget about meetings or events.
- Having difficulty making decisions or following instructions.
Types of memory loss: Transient and Permanent
Memory loss can manifest itself in two forms: temporary (transient) and permanent (permanent) memory loss.
- Transient or temporary memory loss is a temporary forgetting of information that is restored in our memory after a while. If we cannot remember the name but then remember it an hour later, or if we wake up in the morning and cannot remember what happened the night before after drinking alcohol, this is considered a temporary memory loss.
- Permanent or permanent memory loss is information that we lose and cannot recover. If we fail to remember, even if we are reminded of it by the other person where we left the keys to the house, or if we forget about the meeting with the brother made the night before, we are dealing with permanent memory loss.
Causes of memory loss: medical, emotional and age-related problems
There are several factors that can lead to involuntary memory loss in both young and old age. Many of these factors are not due to poor memory performance, but due to the interference of other cognitive abilities (such as attention) or certain substances (such as drugs).
- Memory loss due to health problems which, in most cases, are treatable: side effects of certain medications, an unbalanced diet with a reduced content of vitamins B6, B9 and B12 can lead to temporary memory loss, alcohol abuse, thyroid, kidney or liver diseases, lack of oxygen in the brain (as stroke), the effects of traumatic brain injury (head trauma), cancer treatment (chemotherapy or radiation therapy), brain tumors or infections, emotional problems (such as depression), and anxiety (such as post-traumatic stress).
- Loss of memory due to stress, anxiety and other emotional problems : In addition, stress, anxiety and some of the consequences of strong emotions such as anger can cause forgetfulness. If we're in a car accident, stress can make us lose our memories of what happened that morning. But typically, these memory losses occur because we focus on threatening stimuli and remove less meaning from our surroundings. Thus, we can remember what caused us these strong emotions, but we cannot recall all the events that occurred during this time.
 This occurs in the case of Post Traumatic Stress Disorder and Obsessive-Compulsive Disorder. In these disorders, the person is so focused on the emotional episode or object of obsession that he ultimately does not remember anything except for this stimulus.
This occurs in the case of Post Traumatic Stress Disorder and Obsessive-Compulsive Disorder. In these disorders, the person is so focused on the emotional episode or object of obsession that he ultimately does not remember anything except for this stimulus. - Memory loss with age and normal aging : Although forgetfulness and memory disorders do not occur exclusively in older people, it is true that these people are more susceptible to such problems. With age, the ability to learn and the quality of memory can deteriorate even without the presence of any pathology. However, when these problems become more severe than usual, we may speak of mild cognitive impairment or, in more severe impairments, dementia.
- Memory loss due to emotional problems in the elderly: It is common for older people to feel lonely when they lose loved ones or not feel useful when they retire. Given these changes, it is normal that some of the older people suffer from emotional disorders such as depression.
 Depressed older adults may experience feelings of memory loss more often and confuse these symptoms with Alzheimer's disease or other memory problems. Depression can cause serious memory problems in both the elderly and young people, but in the case of older patients, it is very important to conduct an appropriate differential diagnosis in order to rule out the presence of Alzheimer's disease. Although memory problems in people with depression may not be as relevant as in other pathologies, it is necessary to pay attention to the emotional problems that they suffer from.
Depressed older adults may experience feelings of memory loss more often and confuse these symptoms with Alzheimer's disease or other memory problems. Depression can cause serious memory problems in both the elderly and young people, but in the case of older patients, it is very important to conduct an appropriate differential diagnosis in order to rule out the presence of Alzheimer's disease. Although memory problems in people with depression may not be as relevant as in other pathologies, it is necessary to pay attention to the emotional problems that they suffer from. - Mild cognitive impairment memory loss: Mild cognitive impairment is a disorder that results in memory loss but does not interfere with the person suffering from it in their daily activities. Some research indicates that mild cognitive impairment may be an early sign of Alzheimer's disease, although these impairments do not lead to Alzheimer's disease in all cases.
- Memory loss due to dementia is one of the most important health problems affecting the elderly, but it is not a normal consequence of aging.
 Dementia usually involves the onset of chronic cognitive problems such as problems with memory, speech, behavior, etc. There are various types of dementia, but the most common form is Alzheimer's disease.
Dementia usually involves the onset of chronic cognitive problems such as problems with memory, speech, behavior, etc. There are various types of dementia, but the most common form is Alzheimer's disease. - Memory loss caused by Alzheimer's disease In this disease, a protein called "beta-amyloid" accumulates in neurons, forming senile plaques, until these neurons lose their vitality. This leads to a gradual and severe deterioration in memory, problems with orientation (patients often do not know what day it is and where they are), difficulties in calculations and, in general, with the performance of daily tasks. The severity of the disease varies depending on the stage at which the patient is. In the mild stage, a person with Alzheimer's disease may show significant memory loss, become lost in a familiar place, withdraw from routine activities and conversations, forget dates, and exhibit symptoms of depression and hostility. In the moderate stage, cases of memory loss are most prominent, sufferers may forget names or things that happened a few minutes ago, have difficulty shopping or preparing food, may neglect personal hygiene, have speech problems or show aggression, tend to forget their way, and eventually, their daily life becomes impossible without outside help.
 In the advanced stage, patients may have problems with eating or understanding simple information, they do not recognize relatives and friends, and behave inappropriately in public. At this stage, the person becomes completely dependent.
In the advanced stage, patients may have problems with eating or understanding simple information, they do not recognize relatives and friends, and behave inappropriately in public. At this stage, the person becomes completely dependent.
Prevention of memory loss
How to prevent memory loss? Factors that have been shown to be most effective in preventing or slowing the progress of Alzheimer's and other memory problems are healthy sleep , proper nutrition , exercise , an active social life and cognitive activity . Our brain functions like a muscle: the more actively we use it, the better its condition will be. Conversely, if our brain is not getting enough nutrition and oxygen through exercise, and if we do not apply our social and cognitive abilities, there will be a tendency to atrophy. For this reason, an active and healthy lifestyle can be very beneficial for our memory.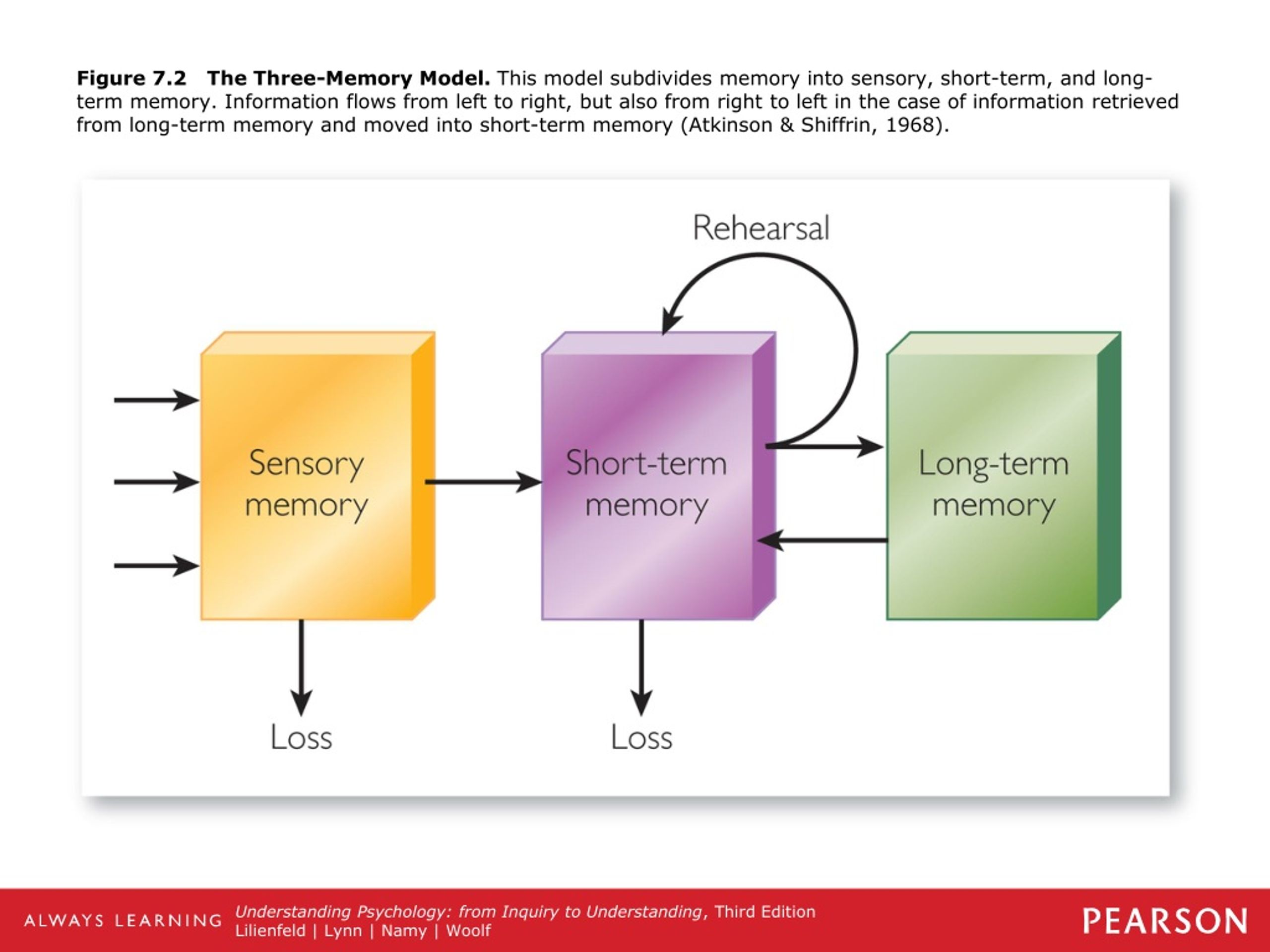 CogniFit offers a wide range of scientifically proven exercises to keep your brain active and improve your cognitive abilities. In addition, cognitive activity not only strengthens memory in adults and the elderly, but can also contribute to the development of intellectual abilities in children and young people.
CogniFit offers a wide range of scientifically proven exercises to keep your brain active and improve your cognitive abilities. In addition, cognitive activity not only strengthens memory in adults and the elderly, but can also contribute to the development of intellectual abilities in children and young people.
Cognitive Stimulation allows you to stimulate, train and strengthen various cognitive abilities such as attention, perception, memory, speech and executive functions. These are precisely the abilities that can be impaired in dementia and other diseases associated with memory loss. By doing exercises that involve various cognitive abilities, we help the brain to strengthen neural connections, preventing damage to it. However, cognitive stimulation cannot be random, it needs to be applied with reliable techniques and detailed organization, according to the needs of each patient. CogniFit focuses on personalizing your exercise program to maximize your workouts and help prevent cognitive problems.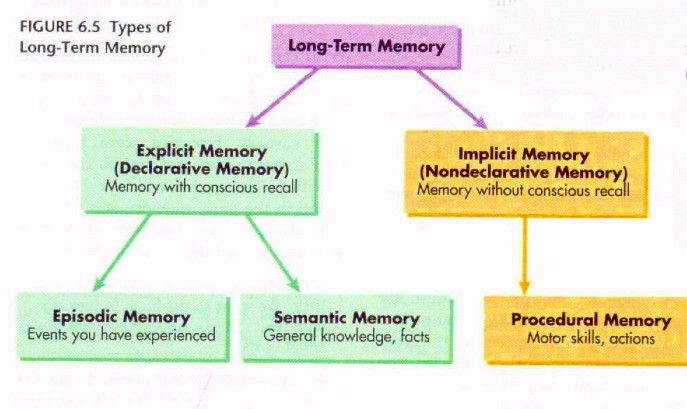
In addition, proper sleep patterns and frequent reading help keep your memory in good condition. Of course, it is necessary to give up bad habits associated with the use of alcohol, tobacco or other drugs - this will help strengthen both memory and overall health.
When should you seek help? Detect and evaluate memory problems
It is very common for people with memory problems to be unaware of their existence, so these problems are usually first discovered by their relatives.
On the other hand, people prone to anxiety and depression can dwell on their mistakes. Often they overestimate their forgetfulness, thinking that they have memory problems, but this is far from always the case. If we sometimes suddenly forget the name of an object or the name of a person with whom we usually communicate a lot, or forget why we went to the room or where we left the keys, or forget to take lunch to work - this is not a cause for concern.
However, if the person is having trouble doing daily tasks, or if they seem confused and disoriented, it is time to see a doctor.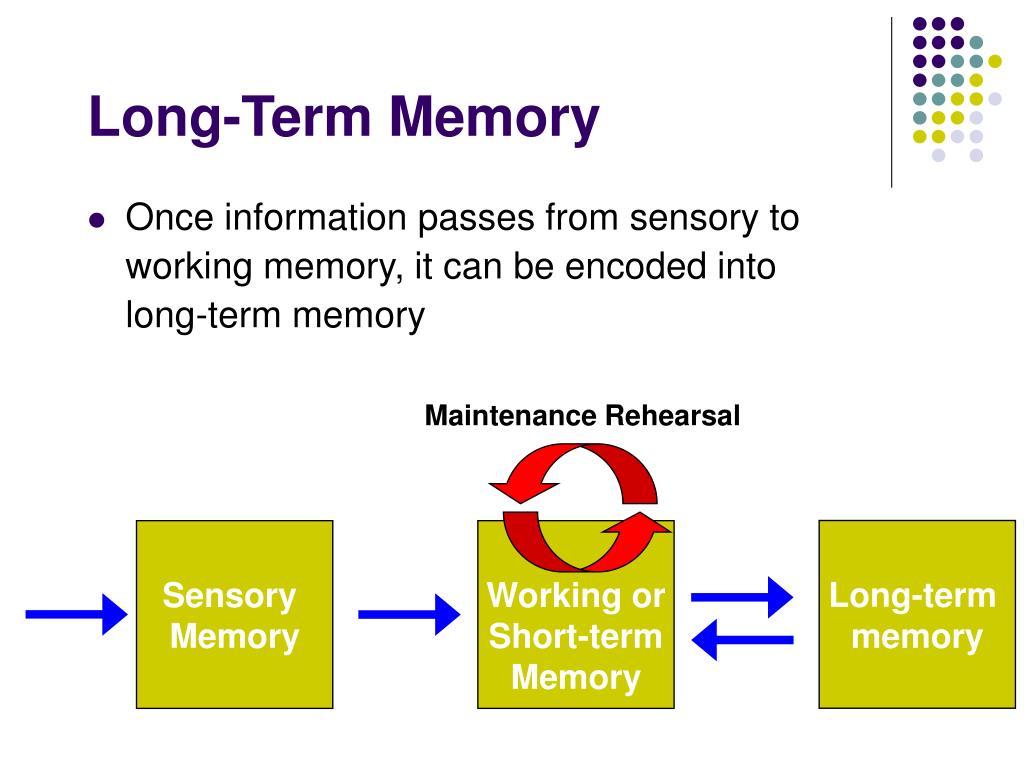 It is recommended to write down all the information about the course of the impairment: when did the memory problems start, what kind of deterioration was observed, what type of information is forgotten, how it affects daily, social and work life. The attending physician must make an accurate diagnosis and determine whether the patient has memory problems, and if so, what kind of problems they are. When in doubt, it is always best to consult a specialist.
It is recommended to write down all the information about the course of the impairment: when did the memory problems start, what kind of deterioration was observed, what type of information is forgotten, how it affects daily, social and work life. The attending physician must make an accurate diagnosis and determine whether the patient has memory problems, and if so, what kind of problems they are. When in doubt, it is always best to consult a specialist.
However, short-term episodes of memory loss do not mean that we are talking about serious memory problems, not to mention Alzheimer's disease. We all forget something from time to time, and this is normal (mild memory loss). Our brain has to forget something in order to process new information correctly.
How to treat or reduce memory loss?
Treatment of dementia should be carried out from a multidisciplinary point of view. Depending on 9 the type of disease, the phase in which the patient is, and the specific characteristics of the patient, the involvement of a neurologist, family doctor, internist, geriatrician, psychologist, neuropsychologist, speech therapist, physiotherapist, occupational therapist and nursing staff may be required .
In the case of Alzheimer's disease, the attending physician must develop an appropriate diagnosis and treatment. In addition, exercises for cognitive stimulation of the brain of patients with Alzheimer's disease at an early stage can be included in the treatment program. In more advanced stages, as a rule, other types of treatment are used, including medication. Despite the fact that Alzheimer's disease is currently considered incurable, these drugs are aimed at maintaining the patient's impaired abilities and behavioral problems associated with this disease.
In addition, taking preventive measures can help slow the progression of dementia once the diagnosis is made. Combining drug treatment with proper diet, exercise, social life and cognitive stimulation helps to minimize the effects of dementia in the patient's daily life.
What if a family member has memory loss?
In case of undiagnosed memory problems with a friend of yours, you should recommend 0006 contact specialist . It is normal to receive a rejection of offered care, as many patients are not aware of their problems. Therefore, one should approach this issue with patience and caution .
It is normal to receive a rejection of offered care, as many patients are not aware of their problems. Therefore, one should approach this issue with patience and caution .
Once the doctor has made a diagnosis, follow his instructions. If this is a mild stage of the disease, we should help this person to carry out daily tasks both at home and socially. One of the main problems of Alzheimer's disease is temporary disorientation, so it is important to place clocks and calendars in the patient's field of vision. Despite the fact that the disease interferes with the learning process, it is strongly recommended to accustom the patient to use a diary and not reduce the usual volume of tasks. Close people should help him follow the doctor's recommendations, take the pills correctly and carry out the activities associated with the treatment. It can be very difficult for a patient to accept their diagnosis. Therefore, it is very important to him emotional support for loved ones, so that the situation is not perceived so painfully.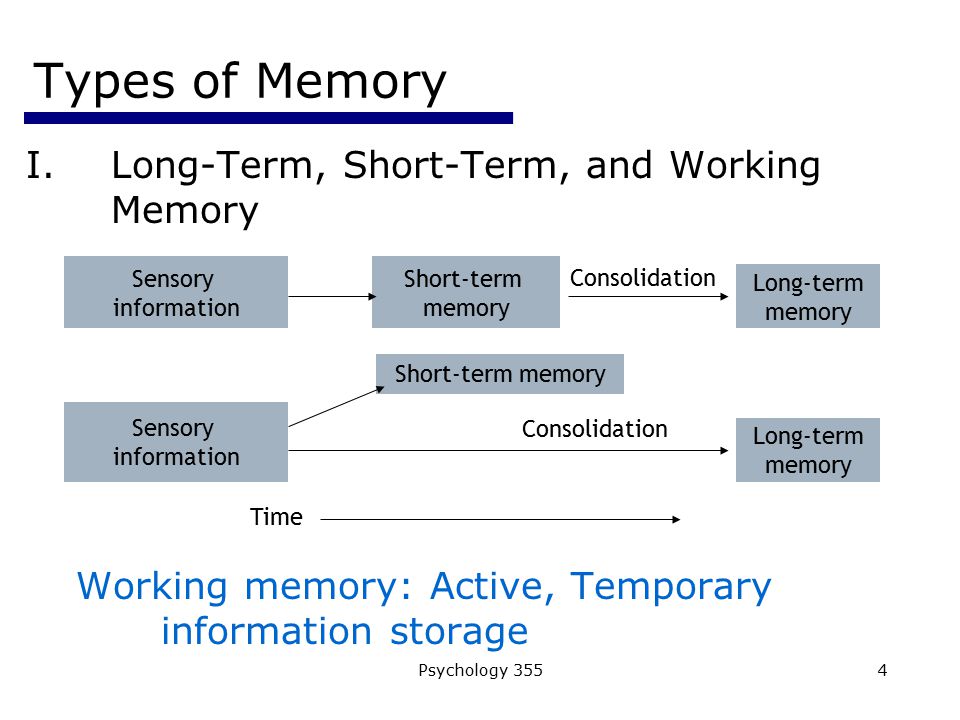 If symptoms of depression are found, a doctor or psychologist should be informed as soon as possible.
If symptoms of depression are found, a doctor or psychologist should be informed as soon as possible.
In conclusion:
- Forgetfulness does not mean the presence of memory problems.
- It is important to be able to distinguish between the signs of Mild Cognitive Impairment and dementia, such as in Alzheimer's disease, in order to detect them as soon as possible and seek professional help. However, not all memory problems are associated with these disorders, however, they also require medical attention.
- The impact of Mild Cognitive Impairment and dementia can be reduced through proper nutrition, exercise, adequate rest, socialization and cognitive stimulation.
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error.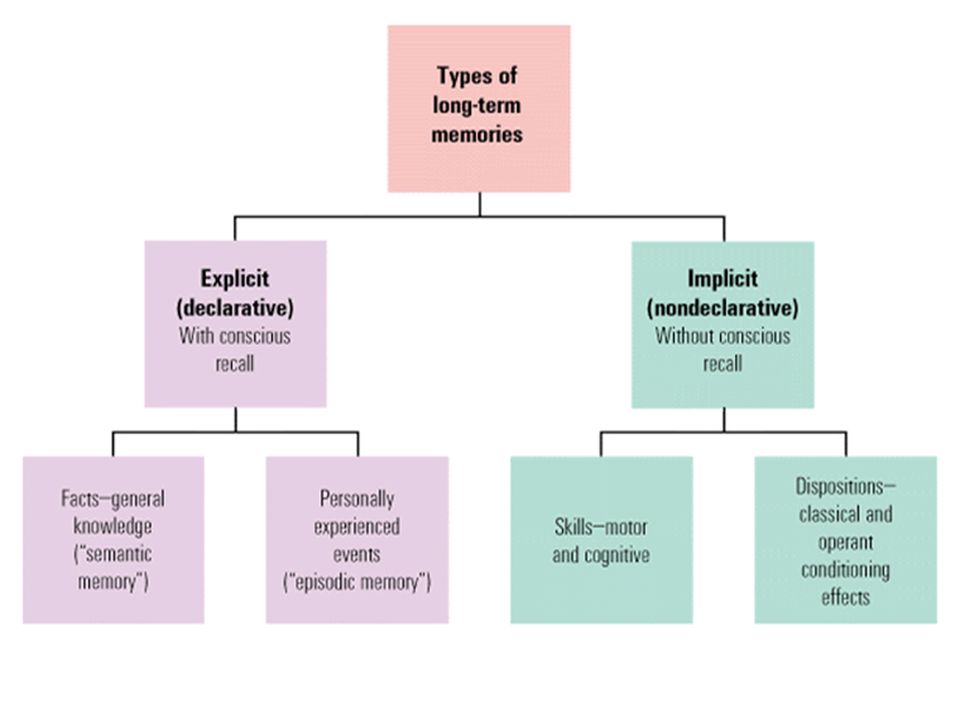 thank you.
thank you.
Please wait, download may take time
Loading...
You know which doctor you want to book
You know the service you want to book
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment.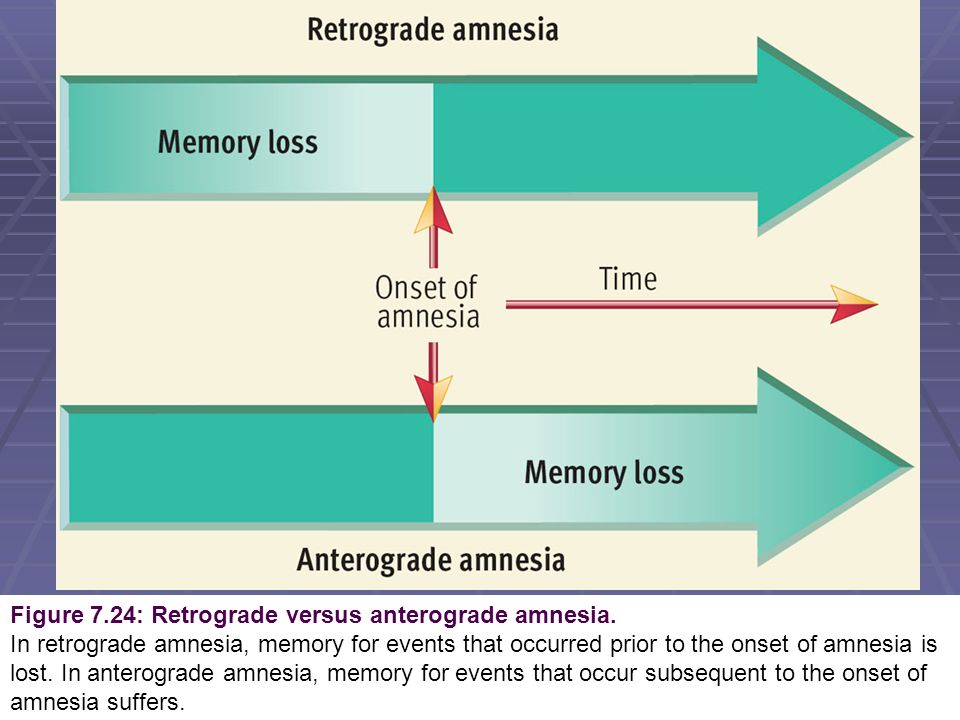 On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st. Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Comment
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022. N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia of July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.