Antipsychotics that dont cause weight gain
Antipsychotics and Weight Gain: How Antipsychotics Affects Weight
Written by Alicia Barney
In this Article
- Why Do Antipsychotics Make You Gain Weight?
- Does the Type Matter?
- What You Can Do
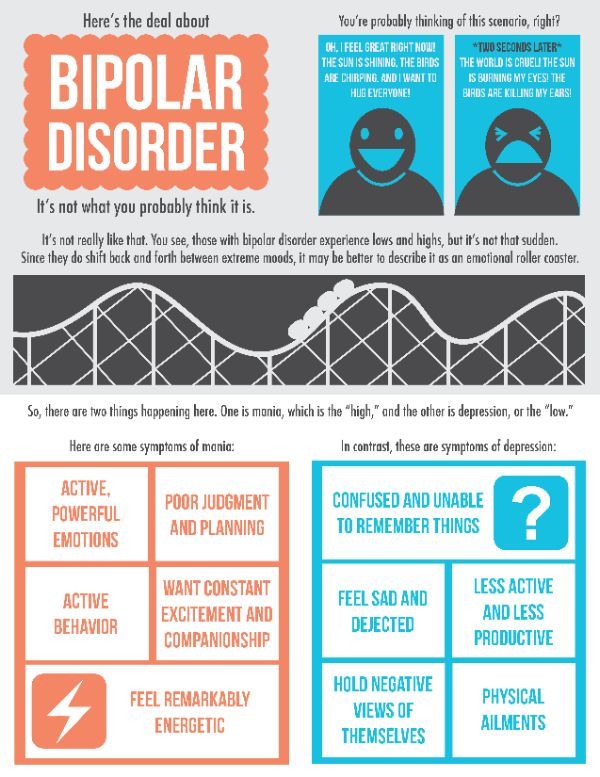
Antipsychotic drugs treat schizophrenia, bipolar disorder, and other mental health disorders. They can ease your symptoms and help you avoid a relapse (when your symptoms come back), but they can also cause weight gain.
People often quickly put on weight after they start antipsychotics and keep gaining over time. Children are more likely to gain weight. Being overweight raises your risk of diabetes, heart attack, stroke, high blood pressure, arthritis, sleep apnea, and some cancers.
Why Do Antipsychotics Make You Gain Weight?
Antipsychotic drugs can make you hungrier, so you might eat more. That’s because they change the way your brain and hormones work together to control your appetite. You might crave sweets or fatty foods. They can also raise the amount of sugar and fat in your blood.
Does the Type Matter?
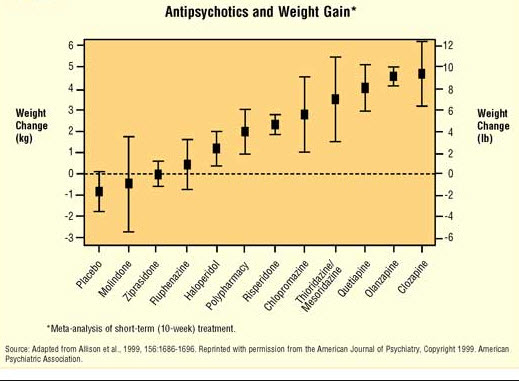
Some antipsychotic drugs are more likely than others to cause weight gain. The risk is highest with clozapine (Clozaril, FazaClo) and olanzapine (Zyprexa).
Chlorpromazine has a high to medium risk, while paliperidone, quetiapine, and risperidone have a medium risk. Drugs that cause the most weight gain tend to raise your blood’s sugar and fat levels.
Antipsychotics with a lower risk of weight gain are:
- Aripiprazole (Abilify)
- Asenapine (Saphris)
- Brexipiprazole (Rexulti)
- Cariprazine (Vraylar)
- Haloperidol (Haldol)
- Lumateperone (Caplyta)
- Lurasidone (Latuda)
- Ziprasidone (Geodon)
But everyone is different. You might gain a lot, a little, or no weight, or even lose weight when taking an antipsychotic. It all depends on what you eat, how much you exercise, and your genes.
If you put on a lot of weight in the first month on a new medication, you’ll probably gain more long term. You’ll probably gain more if you’re taking an antipsychotic for the first time.
You’ll probably gain more if you’re taking an antipsychotic for the first time.
What You Can Do
Talk to your doctor about potential weight gain before you start an antipsychotic. If you’re already taking one, don’t stop or take less without talking to your doctor. This could cause a relapse.
Your doctor should check your weight and body mass index -- a measurement of your height and weight -- often, especially during the first few months after you start antipsychotic drugs. Your doctor might also check your cholesterol and blood sugar levels.
Exercise and try to eat healthy meals (limit high-fat, high-sugar foods). A nutritionist can help you pick the right foods. Counseling can help, too.
Your doctor might also prescribe a medication like metformin to help with weight loss. You can also ask your doctor if you can switch to a drug with lower risk of weight gain.
Any weight you gain usually goes away when you stop taking antipsychotics. If stopping is right for you, your doctor will slowly lower your dose so you don’t relapse.
New Antipsychotic That Causes Less Weight Gain Gets FDA Approval
Lybalvi (olanzapine and samidorphan) may be a game changer for patients who hesitate to take their medication due to the weight gain associated with most antipsychotics.
By Christina Vogt
Everyday Health Archive
Fact-Checked
Most antipsychotic medications are tied to weight gain, with changes in weight ranging from mild to significant.
iStock (2)The U.S. Food and Drug Administration (FDA) announced the approval of a once-daily atypical antipsychotic drug, Lybalvi (olanzapine and samidorphan), to treat adults with schizophrenia and adults with bipolar I disorder.
According to its manufacturer, Alkermes, the combination of olanzapine and samidorphan causes significantly less weight gain than traditional Zyprexa (olanzapine), one of the most widely prescribed antipsychotic drugs for treating schizophrenia and bipolar I disorder.
"The weight gain on olanzapine has limited its use in patients, due to reluctance of healthcare providers to prescribe it and as a result of patients discontinuing the medication. This is unfortunate since olanzapine is one of the most effective antipsychotics on the market," says René S. Kahn, MD, PhD, who is a professor and chair of the department of psychiatry and behavioral health system at the Icahn School of Medicine at Mount Sinai in New York City. Dr. Kahn was one of the researchers who studied the effects of Lybalvi in clinical trials.
"Lybalvi combines the efficacy of olanzapine with limited weight gain, and thus provides an important alternative to olanzapine monotherapy," Kahn adds.
RELATED: Schizophrenia: Popular Myths, Real Facts
What Is Lybalvi? Safety, Effectiveness, and Side EffectsThe new approval is based on the results of the ENLIGHTEN-1 and ENLIGHTEN-2 studies. In ENLIGHTEN-1, which was published in the March–April issue of the Journal of Clinical Psychiatry, adults with acutely exacerbated (or worsened) schizophrenia who completed four weeks of treatment with Lybalvi experienced significant improvements compared with those who received placebo.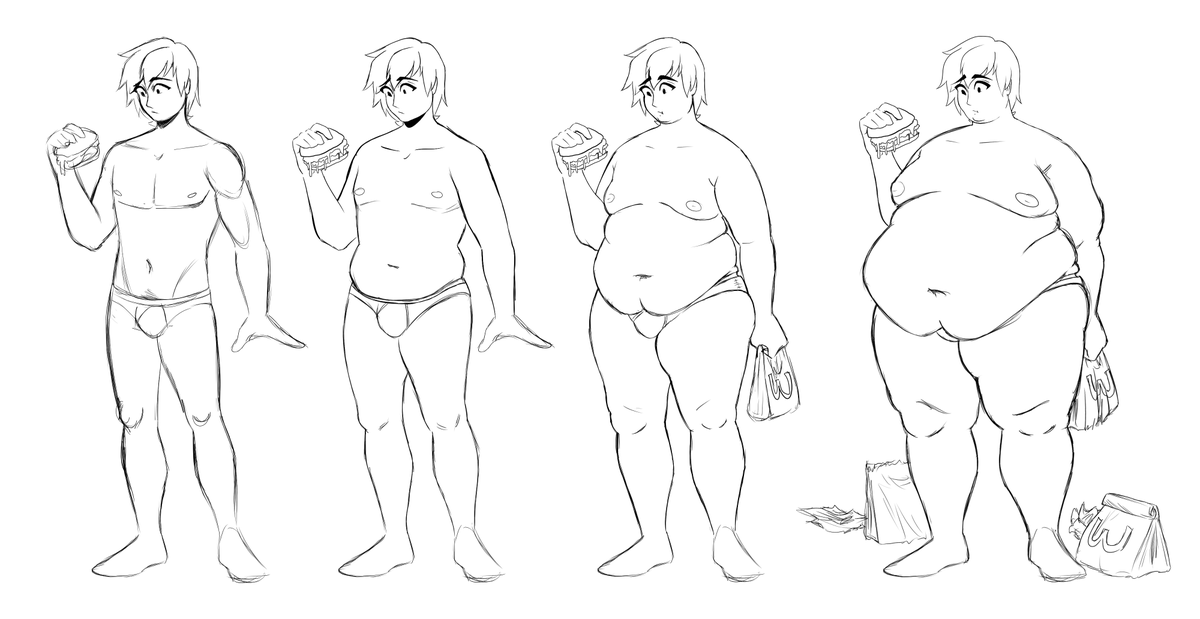
In ENLIGHTEN-2, a phase 3 study published in August 2020 in the American Journal of Psychiatry, researchers assessed the impact of Lybalvi on weight gain compared with olanzapine alone. Over the course of 24 weeks, the researchers found that Lybalvi had similar effectiveness while causing significantly less weight gain and smaller increases in waist size compared with olanzapine alone.
Lybalvi, which is taken by mouth, was found to be well tolerated in both studies. According to Lybalvi’s website, the most common side effects in adults with schizophrenia were weight gain, sleepiness, dry mouth, and headache.
In adults with bipolar I disorder, common side effects when using Lybalvi included constipation, weakness, dry mouth, dizziness, and increased appetite. In adults with bipolar I disorder who took Lybalvi along with lithium or valproate, side effects included dry mouth, back pain, memory and speaking issues, weight gain, and dizziness. Lybalvi should not be used by people who are taking opioids or going through acute opioid withdrawal.
Lybalvi is anticipated to be available for patients in late 2021, Alkermes said in a press release.
RELATED: Keeping Your Relationship Strong After a Schizophrenia Diagnosis
Weight Gain: A Common Side Effect of Antipsychotic MedsAntipsychotic drugs like Lybalvi and olanzapine play a key role in managing conditions like schizophrenia, but as Kahn mentioned, they often come with significant side effects like weight gain. A review of 307 studies that assessed weight change with antipsychotic treatment, which was published in PLOS ONE, showed that the majority of antipsychotic medications are associated with some degree of weight gain when used long term. The amount of weight gain caused by each drug ranged from mild to severe, the researchers wrote.
Weight gain associated with antipsychotic medication can play a role in a variety of problems ranging from a worse quality of life to an increased risk of cardiovascular disease and death.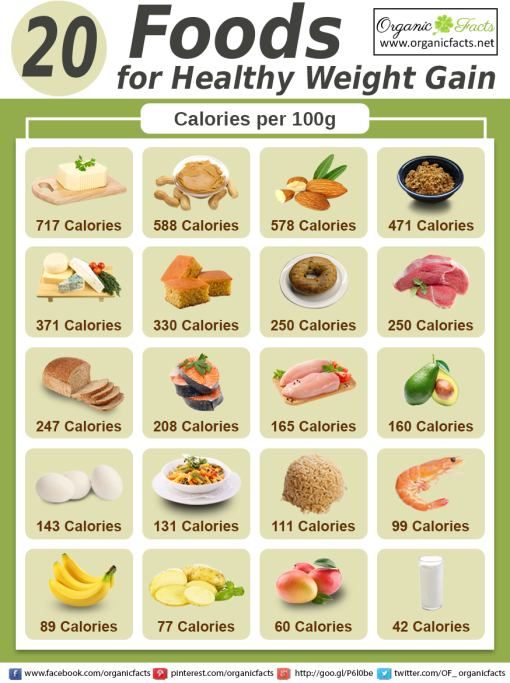 There is also a greater likelihood that patients who are prescribed these medications may fail to stick with them, according to an August 2017 article published in the journal Nonpsychiatric Disease and Treatment.
There is also a greater likelihood that patients who are prescribed these medications may fail to stick with them, according to an August 2017 article published in the journal Nonpsychiatric Disease and Treatment.
The authors of the August 2017 article wrote that the risk of weight gain “appears to be highest with olanzapine and clozapine [another antipsychotic drug that can be used to treat people with schizophrenia],” and tends to happen quickly after starting antipsychotic treatment and continue over time. Strategies to address weight gain, such as dietary counseling, exercise programs, and cognitive and behavioral interventions, appear to have “modest effects,” the authors stated, adding that although switching medication is an option, it can lead to a relapse in one’s illness.
RELATED: Schizophrenia Signs and Symptoms
By subscribing you agree to the Terms of Use and Privacy Policy.
What Are Sulfonamides? Uses, Warnings, Side Effects, and More
By Julie Lynn MarksWhat Is a Diuretic? Uses, Warnings, Side Effects, and More
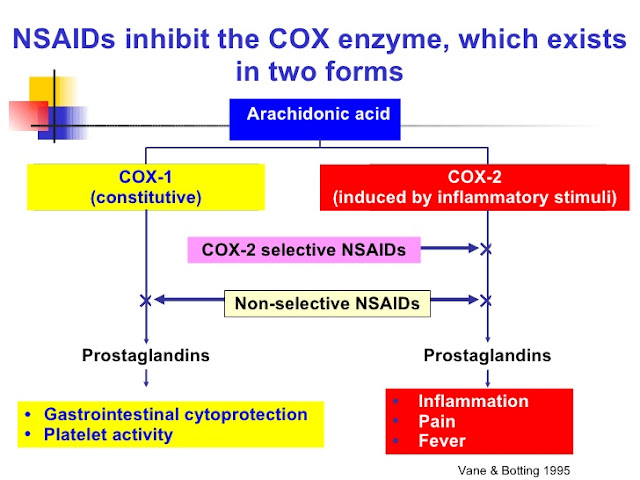
By Frieda Wiley, PharmD, CGP, RPhWhat Are COX-2 Inhibitors?
By Erin Archer Kelser, RNWhat Are Aromatase Inhibitors?
By Erin Archer Kelser, RNWhat Are Sedatives?
By Erin Archer Kelser, RNWhat Are Calcium Channel Blockers?
By Diana RodriguezWhat Are Tricyclic Antidepressants?
By Frieda Wiley, PharmD, CGP, RPhWhat Are Corticosteroids?
By Julie Lynn MarksWhat Are Vasodilators?
By Julie Lynn MarksWhat Are Antipsychotics?
By Julie Lynn Marks✚ Weight gain while taking antipsychotics.
 Neuropsychiatric clinic of Professor Minutko. Article #7004
Neuropsychiatric clinic of Professor Minutko. Article #7004 Many factors contribute to weight gain in patients with psychiatric disorders, particularly psychosis. A sedentary lifestyle, unhealthy eating habits, genetic susceptibility and antipsychotics are considered to be the main contributing factors here to weight gain. Unfortunately, only one third to one half of patients adequately control the metabolic side effects of antipsychotics.
In addition to weight gain, antipsychotics also affect glucose metabolism, increase cholesterol and triglyceride levels, and cause arterial hypertension, leading to metabolic syndrome. Metabolic syndrome increases the risk of developing diabetes by five times and cardiovascular disease by two times over the next 5-10 years after the diagnosis of this syndrome. The prevalence of metabolic syndrome is high in schizophrenia. A meta-analysis of 77 publications showed an overall prevalence of this syndrome in schizophrenia of 32.5%. A similar meta-analysis performed in patients with first episode schizophrenia found lower rates of metabolic syndrome (~10%).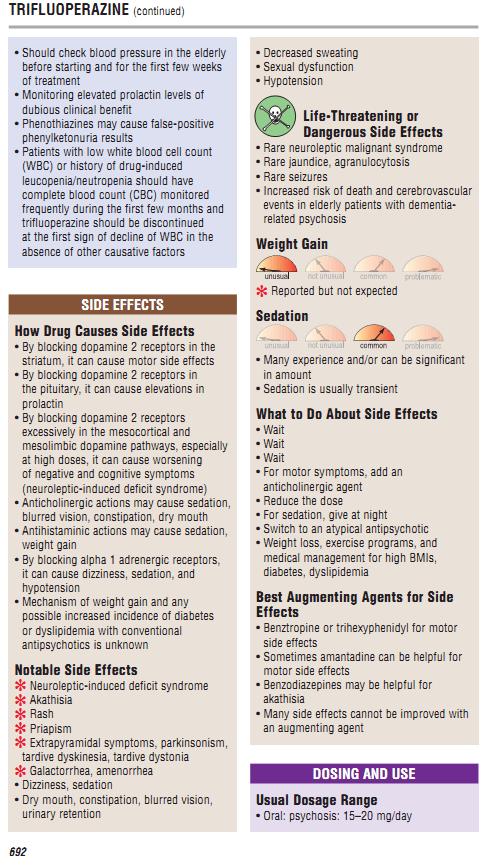 In other words, during treatment with antipsychotics, the number of overweight patients increases by almost 3 times. However, the level of obesity in the first psychotic episode remains high - 22%.
In other words, during treatment with antipsychotics, the number of overweight patients increases by almost 3 times. However, the level of obesity in the first psychotic episode remains high - 22%.
Weight gain caused by antipsychotics is one of the main problems in the treatment of patients with mental disorders. Most antipsychotics cause weight gain, with olanzapine and clozapine appearing to be at the highest risk of this side effect.
Dynamics
Weight increases rapidly during the initial period of therapy with these drugs, almost immediately after the start of antipsychotics. In the future, patients also continue to gain weight. In the first few weeks after starting antipsychotic medication, there is a rapid weight gain. The rate of weight gain then gradually decreases and levels off over several months.
Time to plateau varied for each antipsychotic, ranging from 4 to 9 months for olanzapine and 42 to 46 months for clozapine. This indicates that patients will continue to gain weight for 1–4 years. taking antipsychotics.
taking antipsychotics.
Factors associated with rapid initial weight gain were younger age, lower basal body mass index (BMI), greater response to antipsychotics, and increased appetite. Rapid weight gain of more than 5% in the first month is the best predictor of significant weight gain in the long term.
Complications
Researchers have shown that weight gain and obesity also lead to increased cardiovascular and cerebrovascular disease, reduced quality of life, and poor medication adherence.
Age-related aspects of weight gain with antipsychotics
Unlike adults, children are physically and emotionally more vulnerable to the side effects of medications.
Children are especially vulnerable to antipsychotic-induced weight gain. Atypical antipsychotics (SGA) are effective for psychiatric disorders in children, but their benefits are limited by the risks of both metabolic and neurological side effects. Weight gain is one of the most annoying side effects in children, with up to 80% of children showing significant weight gain.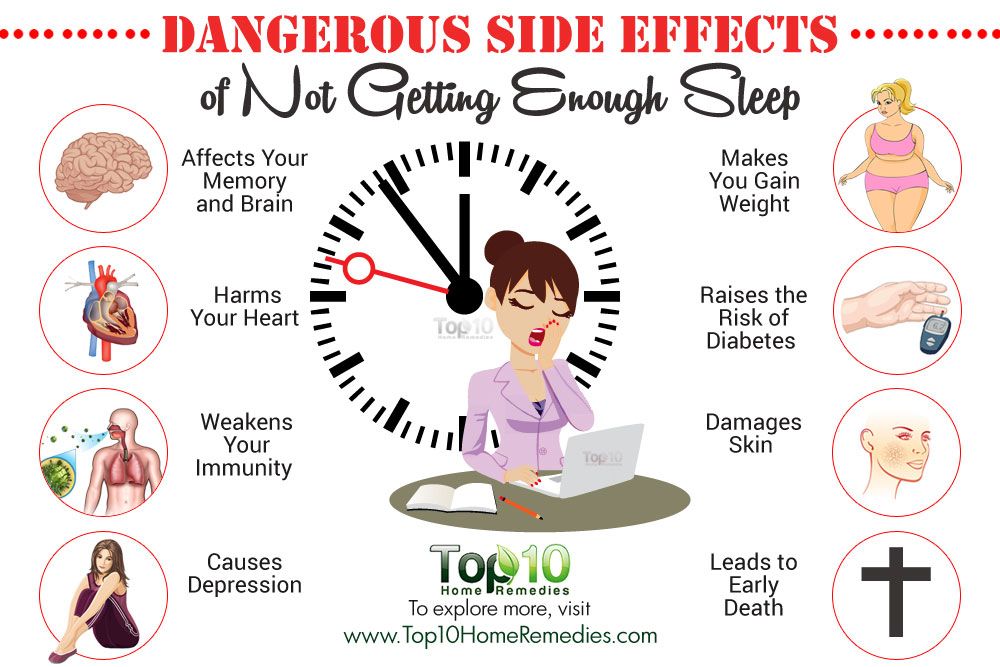 Adolescents experienced greater weight gain than older patients. Patients with autism treated with antipsychotics had greater weight gain. A higher propensity to gain weight is also observed in patients with schizophrenia.
Adolescents experienced greater weight gain than older patients. Patients with autism treated with antipsychotics had greater weight gain. A higher propensity to gain weight is also observed in patients with schizophrenia.
Antipsychotic weight comparison
Clozapine, olanzapine, thioridazine, sertindole, chlorpromazine, and risperidone have been reported in the literature to cause significant weight gain ranging from 4.45 to 2.10 kg. Also note that all antipsychotics except haloperidol, lurasidone, and ziprasidone cause weight gain. Olanzapine and zotepine cause significantly more weight gain than most other antipsychotics. Another meta-analysis found that olanzapine and clozapine caused the greatest weight gain, while quetiapine, risperidone, and sertindole produced intermediate effects on weight. Moderate to low weight gain was observed with aripiprazole and amisulpiride. Newer antipsychotics, asenapine, iloperidone, paliperidone, and lurasidone, are reported to cause significant weight gain.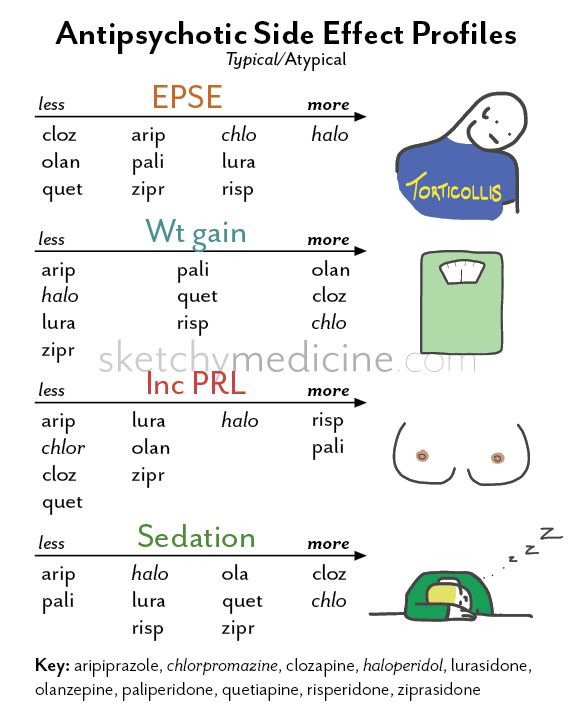 Clinically significant weight gain greater than 7% was caused by all drugs except lurasidone. It is worth reminding the reader of my Blog that clozapine, the drug with the highest risk of weight gain, is also the only antipsychotic currently licensed for the treatment of resistant schizophrenia. Similarly, olanzapine, which ranks high in terms of efficacy, carries a higher risk of weight gain than most other antipsychotics.
Clinically significant weight gain greater than 7% was caused by all drugs except lurasidone. It is worth reminding the reader of my Blog that clozapine, the drug with the highest risk of weight gain, is also the only antipsychotic currently licensed for the treatment of resistant schizophrenia. Similarly, olanzapine, which ranks high in terms of efficacy, carries a higher risk of weight gain than most other antipsychotics.
Etiology
Genetics
Genetic polymorphisms may explain individual differences in AIWG. A recent meta-analysis by Zhang et al. (2016) , Identified 13 single nucleotide polymorphisms from nine genes significantly associated with AIWG. Single nucleotide polymorphisms associated with genes ADRA2A , DRD2 , 5- HTR2C and MC4R, showed the largest effect size, indicating that candidate genes for increase which antipsychotics exert their therapeutic effects.
Pathogenesis
Receptors
The amount of weight gain depends on the type of antipsychotic and the individual patient. The high likelihood of weight gain when taking antipsychotics is associated with their actions on serotonin 5-HT2A and 5-HT2C, dopamine D2 and D3, histamine h2, and muscarinic M3 receptors. The different effects on weight are explained by the different affinities of the drugs for these receptors.
The high likelihood of weight gain when taking antipsychotics is associated with their actions on serotonin 5-HT2A and 5-HT2C, dopamine D2 and D3, histamine h2, and muscarinic M3 receptors. The different effects on weight are explained by the different affinities of the drugs for these receptors.
Hormones
Antipsychotics affect neuropeptides associated with appetite control and energy metabolism. Leptin and adiponectin are adipokines produced in white adipose tissue that are involved in the pathogenesis of antipsychotic weight gain (AIWG). Elevated leptin levels and decreased adiponectin levels have been demonstrated with short-term and long-term treatment with olanzapine. Ghrelin, which acts on the hypothalamic arcuate nucleus to enhance food intake and store adipose tissue, is also affected by antipsychotics. Changes in leptin, adiponectin, and ghrelin levels are hypothesized to be related to direct drug exposure and not secondary to weight gain.
On the other hand, the effects of antipsychotics on lipid and glucose metabolism have been linked to their effects on weight gain and obesity, leading to insulin resistance and consequently increased release of triglycerides and very-low-density lipoproteins from adipocytes.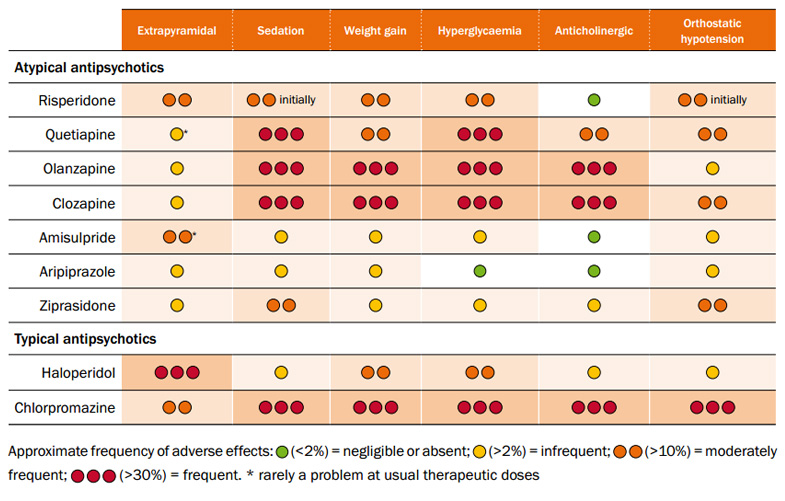
There is also evidence that antipsychotic drugs increase gene expression of the sterol regulatory element binding protein ( SREBP ) and very low density lipoprotein ( VLDL ).
Therapy
Personal selection of antipsychotic drugs according to the individual characteristics of the patient and careful monitoring of weight and other parameters (indicators) of metabolism are the best prevention of weight gain. Switching therapy to a drug with a lower propensity to cause weight gain is an option but carries the risk of a relapse of the psychiatric disorder. Non-drug therapies, such as regular nutritional consultations, specific exercise programs, cognitive training, and behavior change strategies, are equally effective in both individual and group work with patients.
Metformin is one of the drugs that is used for weight loss, however, in my opinion, it should be prescribed for elevated levels of glycated hemoglobin.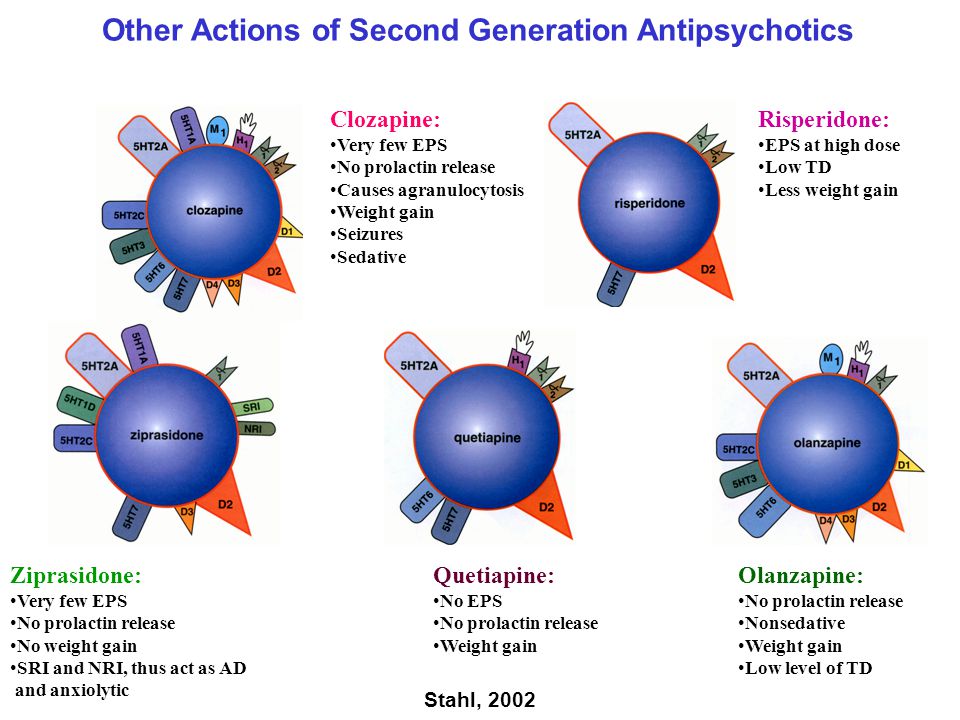 Metformin has the most evidence of efficacy, while topiramate and reboxetine may also be effective. These drugs prevent or treat weight gain through various mechanisms. For example, metformin and rosiglitazone improve insulin resistance, while aripiprazole and metformin lower lipid levels.
Metformin has the most evidence of efficacy, while topiramate and reboxetine may also be effective. These drugs prevent or treat weight gain through various mechanisms. For example, metformin and rosiglitazone improve insulin resistance, while aripiprazole and metformin lower lipid levels.
Metformin is an antihyperglycemic agent that has been used for many decades. It exerts its action by inhibiting hepatic gluconeogenesis and improving insulin sensitivity in skeletal muscle via adenosine monophosphate kinase. It also lowers low-density lipoprotein cholesterol and triglycerides. The main mechanism of weight loss here may be the reduction of insulin resistance and appetite suppression. The data show that metformin leads to clinically significant weight loss in about half of patients.
The antiepileptic drug topiramate has shown promising results in the treatment of AIWG. Topiramate exerts its weight loss action by stimulating lipoprotein lipase while inhibiting carbonic anhydrase and lipogenesis. It also suppresses appetite and increases satiety. Low baseline levels of thyrotropin hormones predicted the amount of weight gained, and topiramate was particularly effective in reducing weight gain in this subgroup. Use of topiramate 100 or 200 mg has shown a dose-response relationship for weight loss. There is evidence that topiramate may have a therapeutic effect on psychotic states, which may be explained by the antagonism of glutamate-induced excitotoxicity at α-amino-3-hydroxy-5-methyl-4-isoxazolpropionic acid (AMPA) and kainate receptors.
It also suppresses appetite and increases satiety. Low baseline levels of thyrotropin hormones predicted the amount of weight gained, and topiramate was particularly effective in reducing weight gain in this subgroup. Use of topiramate 100 or 200 mg has shown a dose-response relationship for weight loss. There is evidence that topiramate may have a therapeutic effect on psychotic states, which may be explained by the antagonism of glutamate-induced excitotoxicity at α-amino-3-hydroxy-5-methyl-4-isoxazolpropionic acid (AMPA) and kainate receptors.
Norepinephrine reuptake inhibitors (NRIs), such as reboxitin, act by inhibiting the reuptake of norepinephrine. They are prescribed in order to reduce appetite, thereby causing weight loss. The study of atomoxetine did not give positive results. The cardiovascular side effects of changes in blood pressure and heart rate caused by NRIs may interfere with the weight loss benefits of this group of drugs. The combination of reboxetine-betahistine showed clinically significant attenuation of olanzapine-induced weight gain. Betahistine is a histaminergic H1 receptor agonist and H3 antagonist that has been investigated as a co-treatment for olanzapine-induced weight gain. The weight loss potential of betahistine is due to its action on the hypothalamus and liver to induce thermogenesis and reduce food intake. An additional benefit of taking this drug is the reduction in Epworth sleepiness scores during treatment.
Betahistine is a histaminergic H1 receptor agonist and H3 antagonist that has been investigated as a co-treatment for olanzapine-induced weight gain. The weight loss potential of betahistine is due to its action on the hypothalamus and liver to induce thermogenesis and reduce food intake. An additional benefit of taking this drug is the reduction in Epworth sleepiness scores during treatment.
The exact mechanism of action of the new antiepileptic drug zonisamide is unknown. It may act by changing the threshold for rapid inactivation of sodium channels in a voltage dependent manner. It also reduces persistent high-frequency action potential re-firing and inhibits low-threshold T-type calcium channels in neurons. Researchers have demonstrated that zonisamide leads to a moderate but persistent reduction in AIWG.
GLP-1 is an intestinal hormone synthesized in the intestinal mucosa. GLP-1 stimulates glucose-induced insulin secretion in the pancreas and inhibits glucagon secretion. In addition, it reduces appetite and food intake by activating central and peripheral GLP-1 receptors. A meta-analysis showed that GLP-1 reduced weight in obese, diabetic and non-diabetic patients compared to other antidiabetic drugs, including metformin.
In addition, it reduces appetite and food intake by activating central and peripheral GLP-1 receptors. A meta-analysis showed that GLP-1 reduced weight in obese, diabetic and non-diabetic patients compared to other antidiabetic drugs, including metformin.
Diethylpropion and phentermine are dopamine agonists that stimulate dopamine secretion. They are postulated to increase energy expenditure, resulting in weight loss. Both of these drugs are indicated for the short-term treatment of obesity. However, these two drugs have not been studied for AIWG.
Amantadine increases dopamine synthesis and release with some dopamine reuptake inhibition. It is also N - methyl - d - α-aspartate receptor antagonist. One study showed that amantadine 100–300 mg was effective in attenuating or inducing weight loss in patients who experienced weight gain with olanzapine.
H2 receptor antagonists such as famotidine and nizatidine are thought to reduce weight by suppressing appetite caused by increased cholecystokinin levels.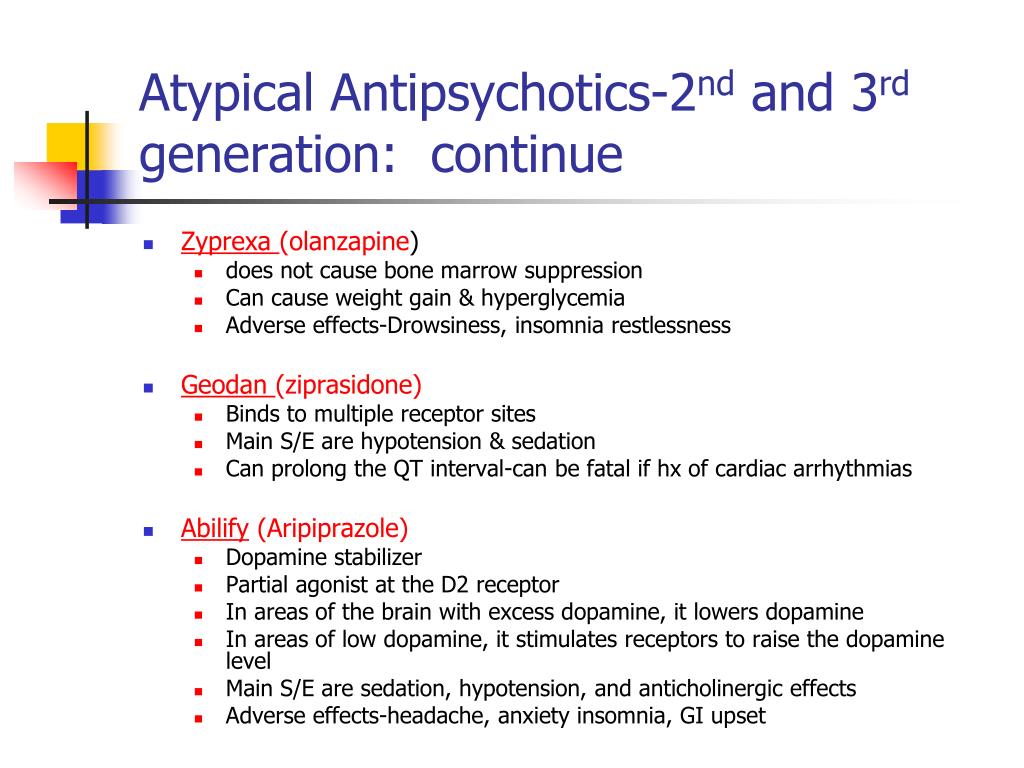 An open study showed that treatment with nizatidine resulted in significant weight loss, and this correlated with leptin levels.
An open study showed that treatment with nizatidine resulted in significant weight loss, and this correlated with leptin levels.
The glucocorticoid and progesterone antagonist mifepristone is effective in reducing weight gain in patients receiving risperidone or olanzapine. Modafinil exerts its action by stimulating monoaminergic receptors. One RCT showed that modafinil resulted in significantly less weight gain compared to placebo in patients treated with olanzapine. Although orlistat is FDA approved for weight loss, there is no evidence that it is effective against AIWG.
Non-drug strategies include cognitive and behavioral psychotherapy, diathetic counseling, and exercise. Cognitive strategies include understanding eating behavior and physical well-being. Behavior modification includes training in problem solving, proper goal setting, social support, and monitoring exercise and eating habits. Dietary counseling includes a reduction of 500–1000 kcal/day from the current diet and a reduction in dietary fat intake by up to 30% of energy intake. Exercise includes 150 minutes of moderate (55-69% of maximum heart rate) of exercise per week.
Exercise includes 150 minutes of moderate (55-69% of maximum heart rate) of exercise per week.
Treatment regimen
Just as extrapyramidal side effects lead to poor compliance (FGA), weight gain is a cause of non-adherence to SGA treatment. However, there is little direct evidence linking weight gain to poor adherence. Obese patients are 13 times more likely to stop taking medication due to weight gain than non-obese patients. This was also reported in the CATIE study, where more patients discontinued olanzapine due to weight gain compared to other drugs, despite olanzapine showing the lowest overall withdrawal rate.
On the other hand, it has also been noted that weight gain is indicative of a better response to antipsychotics, and as a result improved compliance can be expected. A recent study examining factors associated with poor adherence in patients with bipolar disorder reported no difference in adherence between different patient groups.
Quality of life
Weight gain affects patients' quality of life and self-esteem. Waist circumference and body mass index (BMI) predict poor health-related quality of life in patients receiving antipsychotics. Weight gain, cognitive side effects, and sexual dysfunction are strongly associated with poor quality of life satisfaction and distress, especially in women. A change in self-identification follows a change in appearance as a result of weight gain.
Waist circumference and body mass index (BMI) predict poor health-related quality of life in patients receiving antipsychotics. Weight gain, cognitive side effects, and sexual dysfunction are strongly associated with poor quality of life satisfaction and distress, especially in women. A change in self-identification follows a change in appearance as a result of weight gain.
There is evidence that patient weight gain is a concern for caregivers. A mail-order survey of relatives of patients with schizophrenia found that relatives rated weight as the second most problematic side effect. The biggest concern was drowsiness and sedation.
Researchers believe that adherence to treatment is determined by patients' assessment of the benefits of treatment (including side effects) and the risk of relapse, as well as the cost of treatment.
Blog Post Category:
Biological Psychiatry
You must enable JavaScript to use this form.
Your name *
Your phone number (privacy guaranteed) *
Main complaint *
Presumptive diagnosis
Taking medication
Consent to the processing of personal data *
I agree to the processing of personal data, I have read the privacy policy
Weight gain
Numerous studies suggest that psychotropic drugs, including modern atypical antipsychotics, can lead to weight gain while indirectly impairing glucose metabolism and contributing to the development of diabetes. Weight gain is also associated with hypertension, coronary heart disease, stroke, varicose veins, and some other somatic diseases.
Only a few authors believe that overweight is less common in patients with schizophrenia than in other people.
Drugs with a sedative effect that limits the patient's physical activity can slow down the metabolism of substances, which also contributes to the patient's weight gain.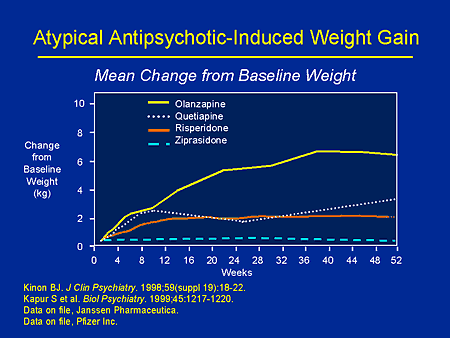
Mechanisms of weight gain with antipsychotics:
- Restriction of physical activity as a result of the sedative effect of the drug.
- The pleasure of eating as a means of combating depression.
- Changing the mechanism of saturation.
- Metabolism slowdown due to the effect of antipsychotics on various networks of neurons: serotonin (5HT1A receptor agonists cause hyperphagia, 5HT2 antagonists cause hypophagia), histamine (blockade), dopamine, norepinephrine, muscarinic, etc.
- Fluid retention in the body.
- Endocrine disorders: increase in prolactin, changes in insulin and cortisol secretion.
- Changes in the level of the hormone - leptin peptide in the blood plasma and changes in the sensitivity of the hypothalamus receptors to it.
Patients with schizophrenia have been observed to prefer sweet foods, drink large amounts of high-calorie drinks (cola and sprite), eat more, while getting a certain pleasure from eating.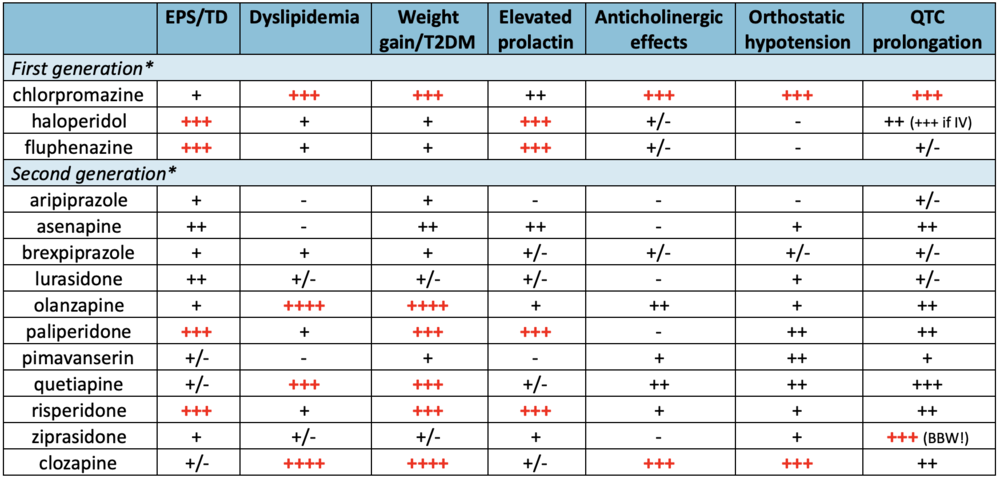
Many psychotropic drugs also have an anticholinergic effect that reduces metabolic processes. They delay the release of fluid from the body, contributing to endocrine system disorders (increase in prolactin, changes in the secretion of cortisol, insulin, etc.), which also increases the weight of patients.
In the development of obesity that occurs while taking certain atypical antipsychotics, the hormone peptide leptin is of great importance, which is produced by adipocytes in an amount that is directly proportional to the amount of fat in the cells of the body.
Leptin plays an important role in the regulation of body weight, affects appetite by blocking leptin receptors in the hypothalamic satiety center proportional to the mass of adipose tissue. It stimulates a sequence of responses that regulate appetite, metabolism, energy expenditure, and food satisfaction.
The peripheral effect of leptin is expressed in the suppression of intracellular lipid metabolism.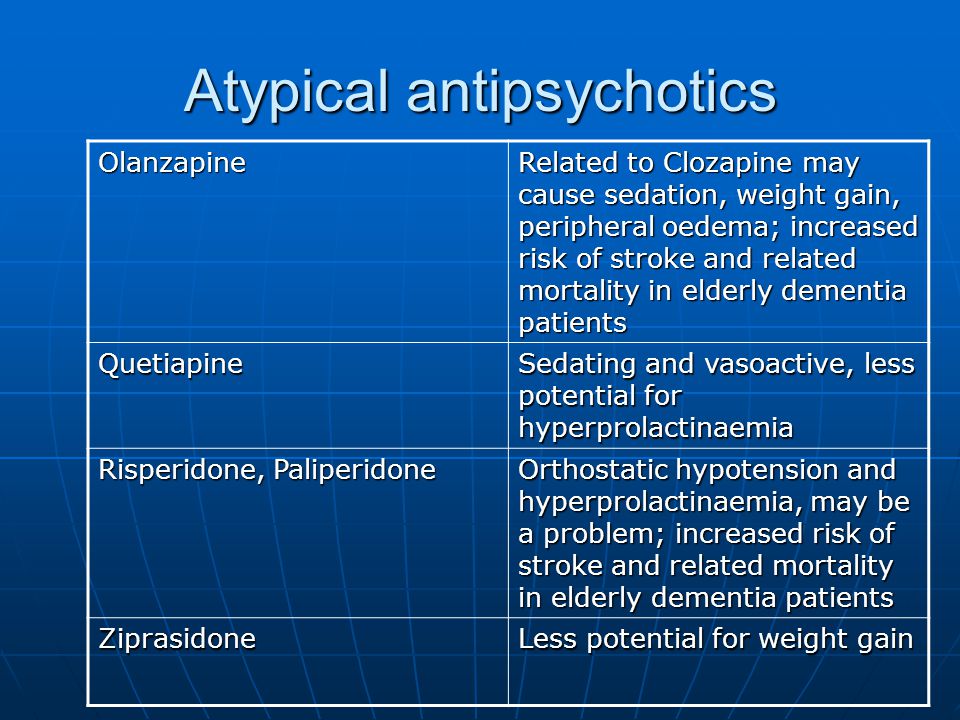 Taking leptin reduces appetite and thus leads to weight loss. However, obesity is often accompanied by an increase in the level of leptin in the blood and, probably, a decrease in the sensitivity of the hypothalamic receptors to this hormone, which in turn leads to an increase in appetite and an increase in body weight.
Taking leptin reduces appetite and thus leads to weight loss. However, obesity is often accompanied by an increase in the level of leptin in the blood and, probably, a decrease in the sensitivity of the hypothalamic receptors to this hormone, which in turn leads to an increase in appetite and an increase in body weight.
Elevated blood leptin also has an effect on tissue insulin resistance. The connection of the latter with the development of obesity is well known. Insulin stimulates the secretion of leptin by adipocytes. The effect of leptin, both stimulating and inhibitory in relation to insulin, on the function of pancreatic beta cells was noted. In other words, not all patients with schizophrenia, even receiving antipsychotics such as olanzapine and clozapine, show weight gain. Currently, many experts explain this phenomenon as a genetic variation of pharmacodynamic factors. There is ample evidence to support this view, as well as the influence of genetic factors on eating behavior.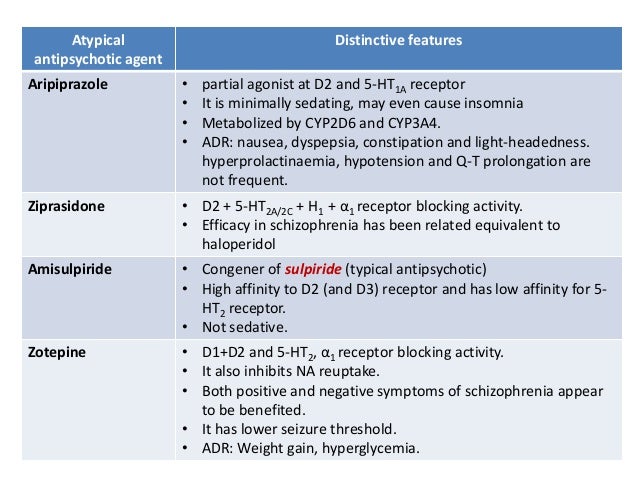 Some researchers have found a relationship between single nucleotide polymorphisms - 759C/T and weight gain at 6 and 10 weeks of hospitalization in patients with a first psychotic episode treated with antipsychotics such as clozapine and risperidone. Other authors have determined that patients without the 759T allele have a higher risk of weight gain during a 6-week course of olanzapine therapy than patients with the 759T allele. At the same time, individuals without the allele - 759T of the 5HT2C receptor gained weight to a much greater extent than individuals with the T allele. Thus, it turned out that carriers of the T allele have a lower risk of weight gain than individuals without this allele. The study of polymorphisms of promoter regions in the 5HT2C serotonin receptor and leptin genes for the presence of an association with weight gain as a result of taking antipsychotics showed that patients prone to weight gain had a 5HT2C receptor polymorphism - 759C/T and leptin polymorphism - 2548A/G.
Some researchers have found a relationship between single nucleotide polymorphisms - 759C/T and weight gain at 6 and 10 weeks of hospitalization in patients with a first psychotic episode treated with antipsychotics such as clozapine and risperidone. Other authors have determined that patients without the 759T allele have a higher risk of weight gain during a 6-week course of olanzapine therapy than patients with the 759T allele. At the same time, individuals without the allele - 759T of the 5HT2C receptor gained weight to a much greater extent than individuals with the T allele. Thus, it turned out that carriers of the T allele have a lower risk of weight gain than individuals without this allele. The study of polymorphisms of promoter regions in the 5HT2C serotonin receptor and leptin genes for the presence of an association with weight gain as a result of taking antipsychotics showed that patients prone to weight gain had a 5HT2C receptor polymorphism - 759C/T and leptin polymorphism - 2548A/G. Leptin polymorphism - 2548 did not correlate with short-term weight gain, but significantly correlated with this indicator after 9 months of antipsychotic therapy. At the same time, variations in the H1 and H2 receptor genes were not associated with weight gain in patients treated with clozapine for 5 weeks.
Leptin polymorphism - 2548 did not correlate with short-term weight gain, but significantly correlated with this indicator after 9 months of antipsychotic therapy. At the same time, variations in the H1 and H2 receptor genes were not associated with weight gain in patients treated with clozapine for 5 weeks.
Tricyclic and tetracyclic antidepressants (amitriptyline, nortriptyline) significantly increase weight. Selective serotonin reuptake inhibitors (SSRIs), with the exception of paroxetine, are neutral in relation to weight gain, mirtazapine, on the contrary, increases body weight. Valproate and lithium have a fairly high potential in terms of weight gain. Among the classic antipsychotics, thioridazine increases weight the most, and pimozide has been reported to reduce body weight.
Usually, weight gain is observed in the first months of therapy and subsequently its rate decreases markedly in its severity. At the same time, the stigma of schizophrenia is aggravated by the stigma of obesity, which significantly affects the social status and the level of compliance of the patient with the medical staff.
Weight gain at 3-6 weeks of therapy is a predictor of overall weight gain.
The total level of high and low density lipoproteins practically differs little when taking various antipsychotics. When taking classical neuroleptics, the average level of triglycerides corresponds to 1.8 mmol / l.
The central norepinephrine and dopamine neural networks play an important role in the regulation of food intake.
It is likely that weight gain during treatment with some atypical antipsychotics (olanzapine) depends on many factors and includes effects on histamine (H1), serotonin receptors (5HT2A, 5HT2C), and alpha-adrenergic receptors (alpha 1 and alpha 2) , muscarinic M3 receptors and changes in plasma leptin levels.
Note that sulpiride (selective blocker of D2/D3 receptors), which noticeably increases the body weight of patients with schizophrenia, does not affect histamine receptors (H1).
Among atypical antipsychotics, clozapine therapy is most often associated with an increase in triglyceride levels and does not affect cholesterol levels.
Comparative studies of the effect of atypical antipsychotics on lipid metabolism in patients with schizophrenia indicate that patients treated with olanzapine exhibit higher triglyceride levels (mean level - 2.3 mmol / l) than those patients who received risperidone (mean level - 1.7 mmol / l) and ziprasidone.
Despite the small number of publications on the effect of quetiapine and zotepine on lipid metabolism, it can be assumed that due to the structural similarity of the latter with clozapine and olanzapine, these drugs may affect lipid levels.
In patients receiving clozapine and olanzapine, there is an increase in serum leptin levels, while, as noted above, white adipocyte leptin regulates insulin secretion and energy metabolism by acting on specific receptors (OB-R) of the hypothalamus, fat cells and skeletal muscles .
With respect to amisulpiride and aripiprazole, there are no data in the literature regarding their effect on lipid metabolism.
The risk group for weight gain includes women, individuals prone to narcissism, and patients with a hereditary burden of obesity.
Weight gain during therapy with psychotropic drugs makes it difficult to cooperate with the doctor and is, especially in women, one of the main reasons for discontinuation of the drug.
Unfortunately, at present, almost 60% of patients with schizophrenia with signs of dyslipedemia do not receive the therapy they need, aimed at correcting metabolic disorders.
If weight gain due to the use of antipsychotics is detected, a psychoeducational program specially designed for a particular case should be carried out with the patient and his relatives. Typically, the duration of such a program, which includes information about the features of the action of antipsychotics and a healthy lifestyle, is several weeks.
A strict diet, including the restriction of high-calorie foods, and physical exercise reduce the severity of the development of obesity that occurs against the background of taking psychotropic drugs.
A significant increase in body weight when taking atypical antipsychotics (olanzapine, quetiapine, risperidone) is usually observed in 14-27% of cases by 6-8 weeks of therapy, in 40% of patients after 3. 5 years.
5 years.
Patients taking clozapine gain an average of 4.5 kg of weight within 10 weeks (Allison D. et al., 1999), with an annual weight gain ranging from 5.7 to 8.0 kg (Lamberti Y. et al., 1992). Up to 94% of patients taking olanzapine also gain weight (Gupta S. et al., 1999). Patients using olanzapine for 10 weeks increase their weight by
4.15 kg (Allison D. et al., 1999), an average of 12 kg per year (Beasley C., 1997).
Risperidone causes moderate to minimal weight gain (2.1 kg in 10 weeks (Allison D. et al., 1999), patients gain an average of 1.7 kg in one year) (Sachs G. 1999) .
For quetiapine, average weight gain over several months of therapy is between 1.0 and 4.0 kg (Borison R. et al., 1996). If against the background of taking respiridone, weight gain is especially noticeable in the first year and a half of using the drug, then the effect of quetiapine on this indicator lasts up to two years.
Ziprasidone causes the least weight gain (Allison D. et al., 1999). According to some researchers, almost the same weight gain is observed against the background of taking amisulpiride.
et al., 1999). According to some researchers, almost the same weight gain is observed against the background of taking amisulpiride.
Weight changes with antipsychotics are shown in Table 42.
Table 42. Weight changes with antipsychotics
| Preparations | Mean expected weight gain after one year of use |
| Clozapine | 5.7 |
| Olanzapine | 4.2 |
| Thioridazine | 2.8 |
| Quetiapine | 2.5 |
| Risperidone | 1.7 |
| Haloperidol | 0.5 |
| Ziprasidone | 0.3 |
| Aripiprazole | 0. |