Psychosis spectrum disorders
What are Psychotic Spectrum Disorders?
Psychotic Spectrum Disorders: A Conversation with Jane Tillman, PhD, ABPP
“Psychotic” is a term that gets tossed around a lot in the culture. How would you frame it, as a clinician?
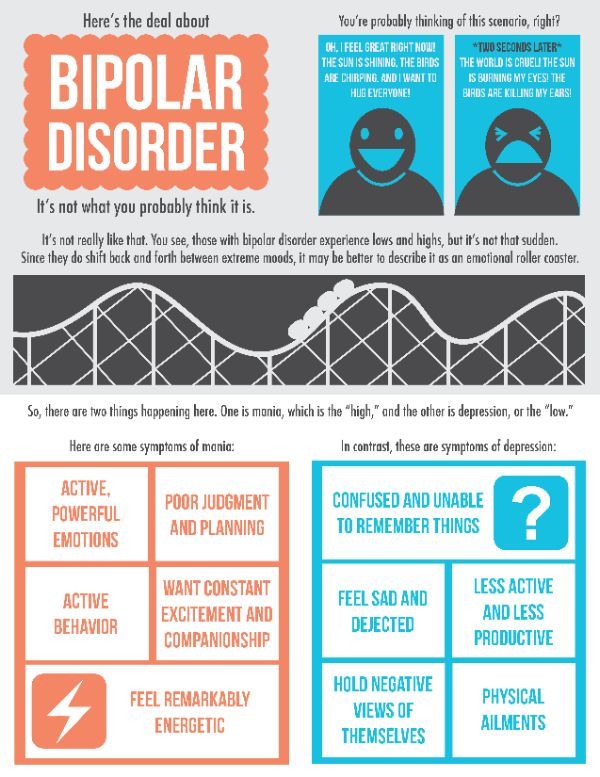
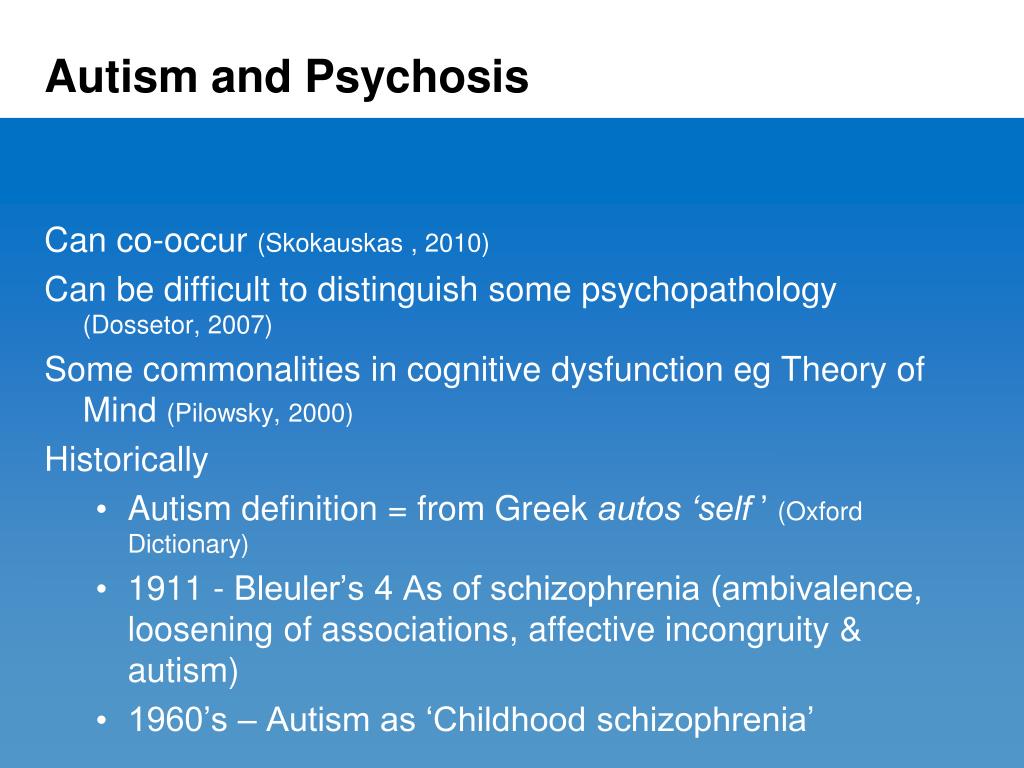
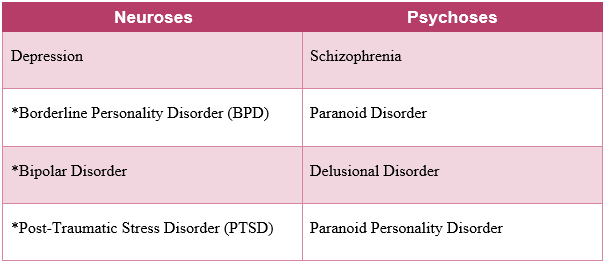
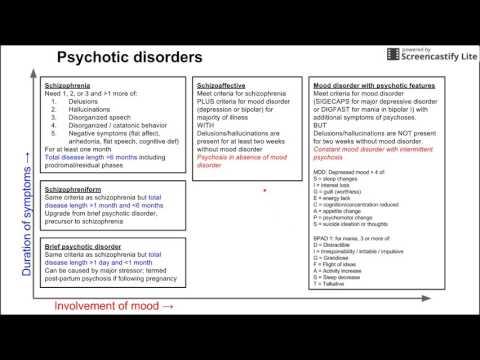
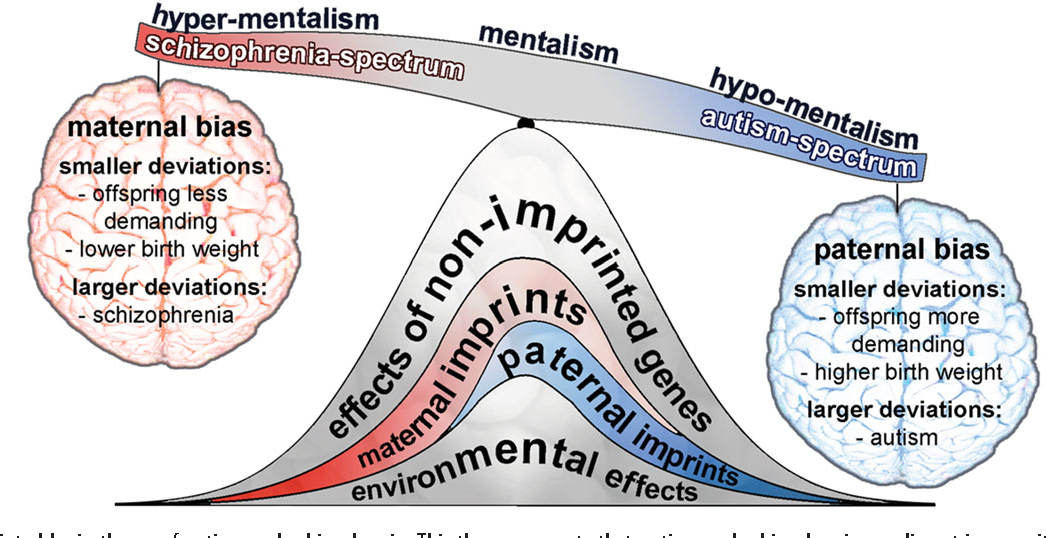
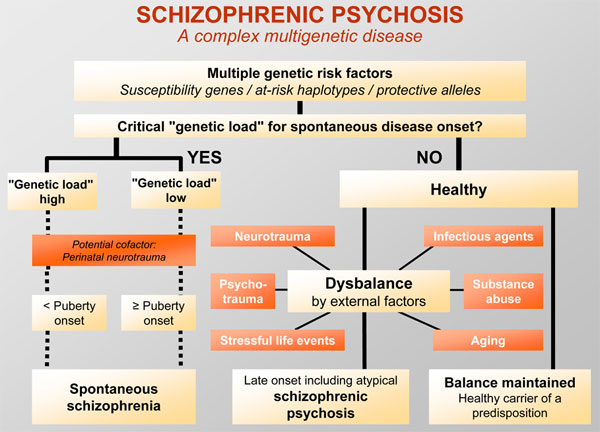
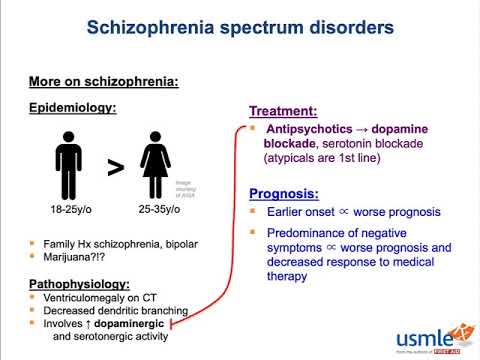
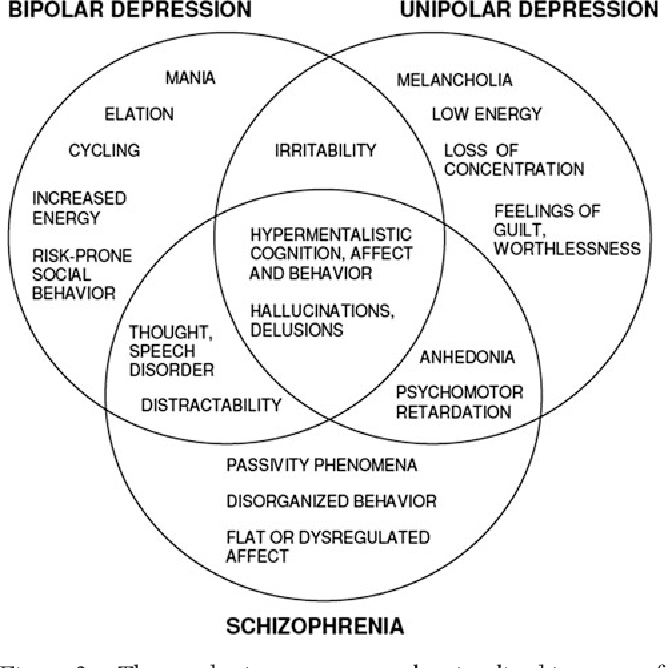
To start, psychosis represents a spectrum of disorders with many different etiologies or origins. People are most familiar with the term schizophrenia, but schizophrenia is probably going to turn out to be an umbrella diagnosis for many different conditions. People can be psychotic for all kinds of reasons, in the wake of substance abuse — with hallucinogens, for example— or because of schizophrenia. People who are bipolar can become psychotic, and so can people with various degenerative disorders. The interaction between biological and genetic vulnerabilities with family and cultural factors is known to be complex. At the Austen Riggs Center we appreciate the complexity of the etiology and treatment of psychosis, providing an integrative treatment approach using psychotherapy, family therapy, and medication along with intensive social engagement through the therapeutic community program.
What are the chief symptoms?
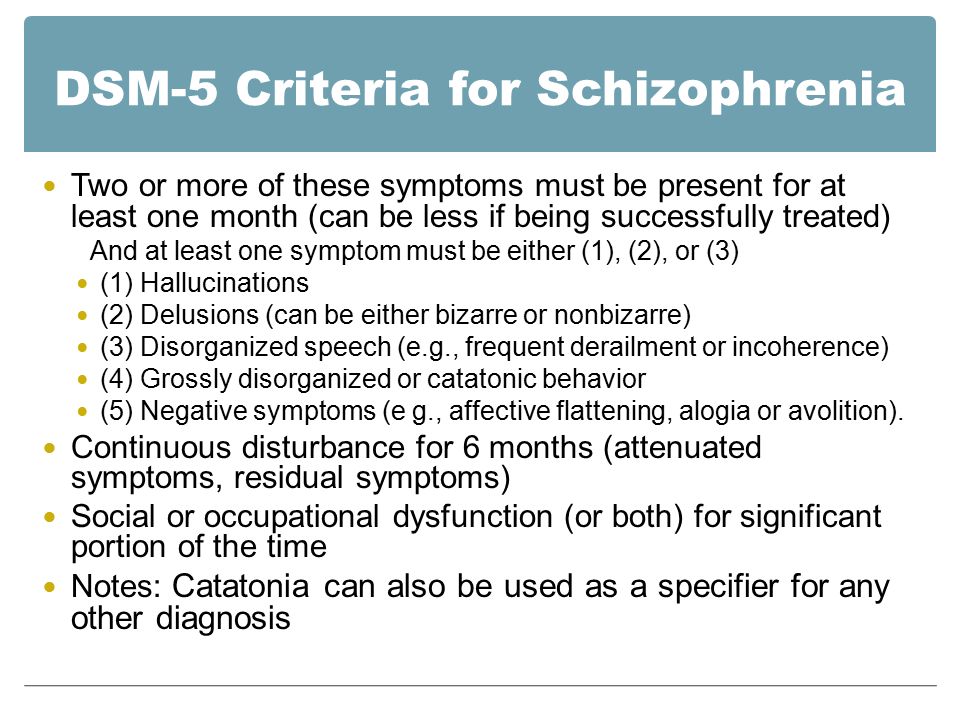
The symptoms most people are familiar with are what we call positive symptoms: hallucinations, delusions, paranoid beliefs, unusual behavioral or mood manifestations. Those are often treated acutely with medications and patients respond well to that.
Once you’ve treated the positive symptoms, people can enter what’s called the negative phase of a psychotic disorder: lack of motivation, lack of direction, flatness. There’s a quality of just being slowed down, and a withdrawal or social isolation. This can be debilitating. It is also much harder to identify and treat. Everyone is familiar with the worst-case psychotic disorder, which is the disheveled person in the street who makes everyone anxious. That’s the more obvious, positive symptom.
People in the negative phase don’t look so disorganized because they’re not having hallucinations or delusions, but they can be very isolated and shut down. They often don’t really know what they want to do.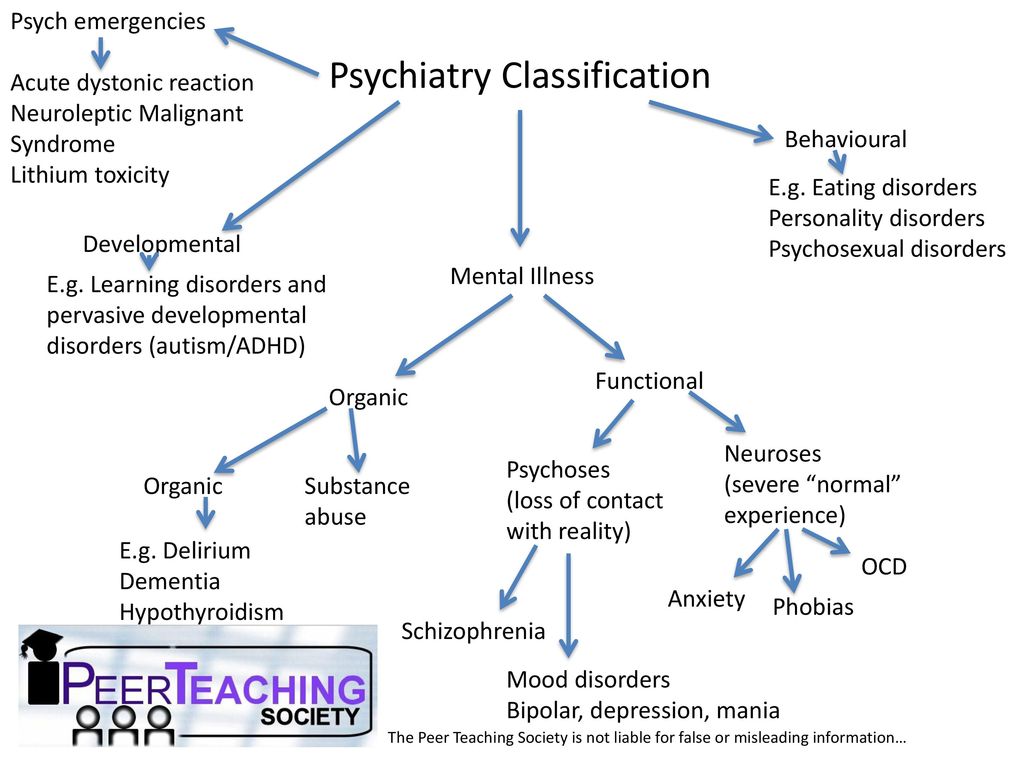 They may feel lost and ashamed. They’ve gotten help from medication, but they have a whole other road ahead of them. How are they going to pick up the pieces of their lives, go on and adapt?
They may feel lost and ashamed. They’ve gotten help from medication, but they have a whole other road ahead of them. How are they going to pick up the pieces of their lives, go on and adapt?
One feature of these disorders is tremendous denial that a person is troubled, or needs treatment. It can be very hard to treat someone who other people think is impaired when that person doesn’t think so. Typically, you see problems with family members, problems in employment. These individuals see themselves in the world quite differently, and often aren’t interested in receiving any treatment. This creates a lot of frustration in attempting to offer help.
In this five-part series exploring psychotic spectrum disorders, we will present excerpts from a longer interview with Jane G. Tillman, PhD, ABPP, Evelyn Stefansson Nef Director of the Erikson Institute for Education, Research, and Advocacy of the Austen Riggs Center, a member of the Riggs clinical staff and an authority on psychotic spectrum disorders.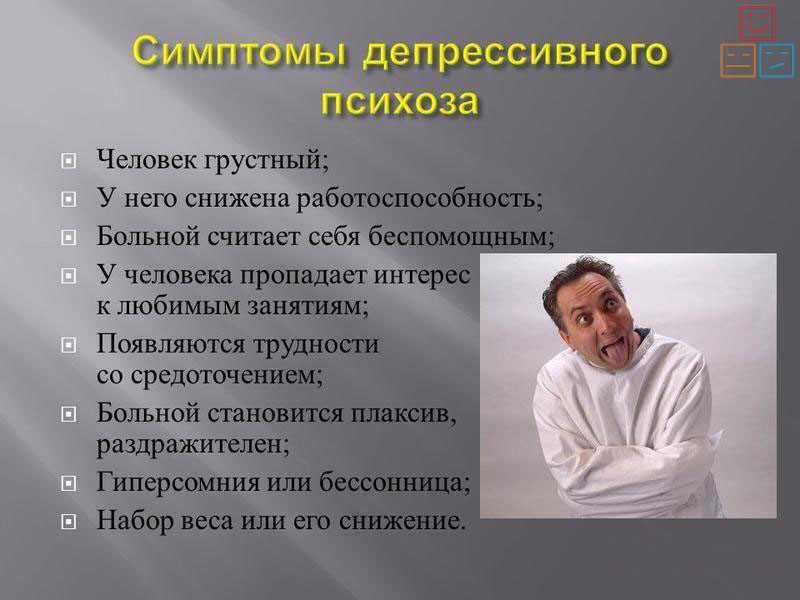
Psychosis Spectrum Disorders & Managing Stress during the COVID-19 Pandemic | Psychiatry | Michigan Medicine
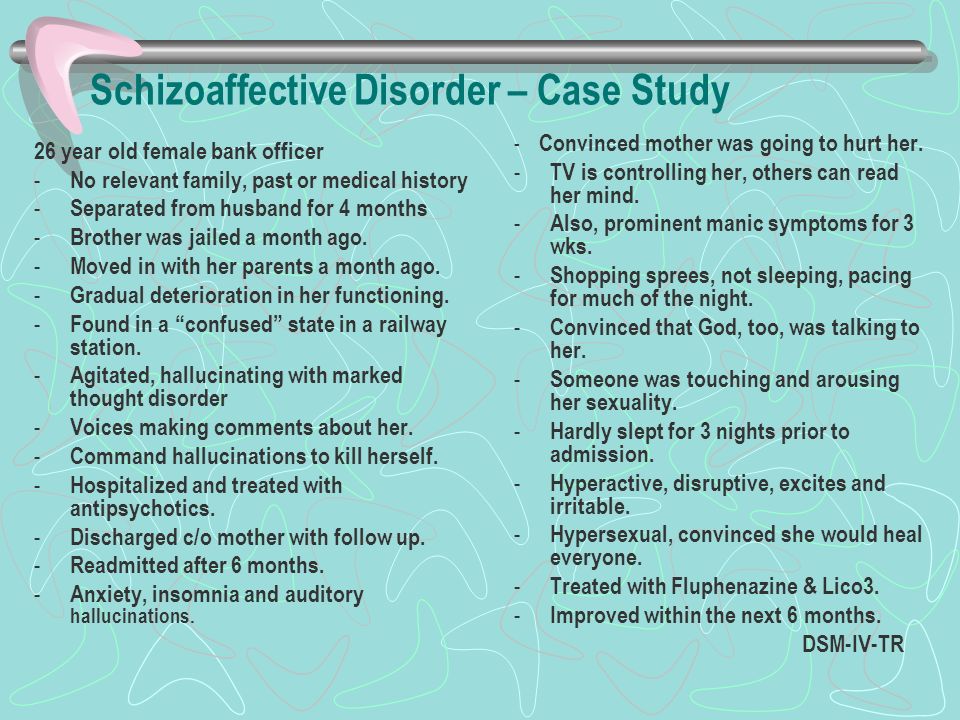
Psychosis refers to the experience of perceiving or interpreting reality in a different way than others. You may “lose touch” with reality during a psychotic experience (e.g., hallucinations, delusions). If you experience psychosis, you may be given a psychiatric diagnosis (e.g., schizophrenia, schizoaffective disorder, bipolar disorder, depression).
Importantly, stress can affect psychosis and people who experience psychosis can be particularly sensitive to stress. Both the uncertainty and the disruption in our daily routines associated with the COVID-19 pandemic are stressful and can make coping with symptoms difficult. We recommend three tips to help manage psychosis and stress during this time.
1) Stick to your treatment plan
When we are stressed, it’s easier to fall out of healthy habits that we worked so hard to achieve over the course of treatment.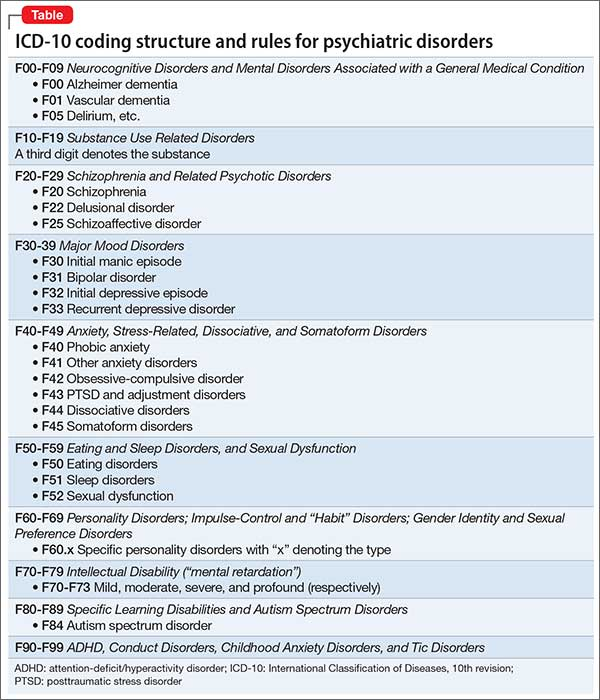 However, maintaining these healthy habits, schedules, and treatment goals as much as possible can put us in a better position to manage stress. That’s why it’s a good idea to talk with your provider to review your treatment plan and come up with strategies to help you stick with your plan. You can discuss how to keep your appointments by scheduling online or phone meetings in lieu of in-person meetings. And how to make sure you have refills of your medications. Also, ask your family and/or close friends if they can assist you with your treatment plan. If your symptoms worsen, contact your provider. If a crisis emerges, contact emergency services.
However, maintaining these healthy habits, schedules, and treatment goals as much as possible can put us in a better position to manage stress. That’s why it’s a good idea to talk with your provider to review your treatment plan and come up with strategies to help you stick with your plan. You can discuss how to keep your appointments by scheduling online or phone meetings in lieu of in-person meetings. And how to make sure you have refills of your medications. Also, ask your family and/or close friends if they can assist you with your treatment plan. If your symptoms worsen, contact your provider. If a crisis emerges, contact emergency services.
2) Practice coping skills and relaxation
Part of sticking with your treatment plan likely includes continued efforts to practice your healthy coping skills (if not, it’s a good idea to add this). We know that psychosis can come with ‘stress sensitivity,’ where even ‘minor’ stressors are disruptive.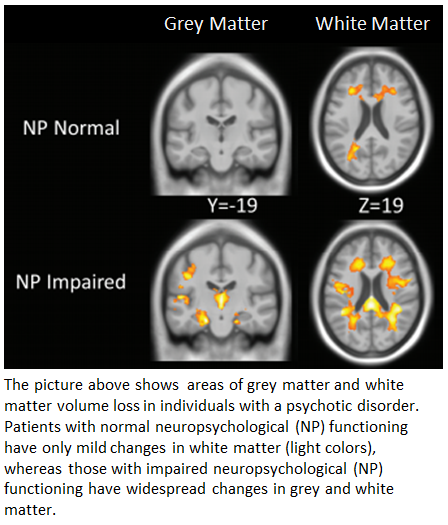 Regularly practicing a wide range of coping and relaxation skills can help manage stress. These include taking a walk (while practicing social distancing), mindful breathing, and engaging in activities that you enjoy (e.g., reading, taking a bath). Practicing these skills does not have to be a “big production.” Even just looking out the window and observing nature for a few minutes counts as a mindful moment and excellent use of your skills!
Regularly practicing a wide range of coping and relaxation skills can help manage stress. These include taking a walk (while practicing social distancing), mindful breathing, and engaging in activities that you enjoy (e.g., reading, taking a bath). Practicing these skills does not have to be a “big production.” Even just looking out the window and observing nature for a few minutes counts as a mindful moment and excellent use of your skills!
3) Stay connected
With social distancing recommendations in place, we are physically staying away from others. This can mean fewer interactions with friends and family. But we know that social connections can be important for our well-being and health. So it’s good to establish a “check-in” buddy, a person you talk to by phone or online every day. You can also schedule times to “virtually” hang-out and watch TV shows with friends and family. Online support groups are also available if you’d like to connect with others who share similar experiences.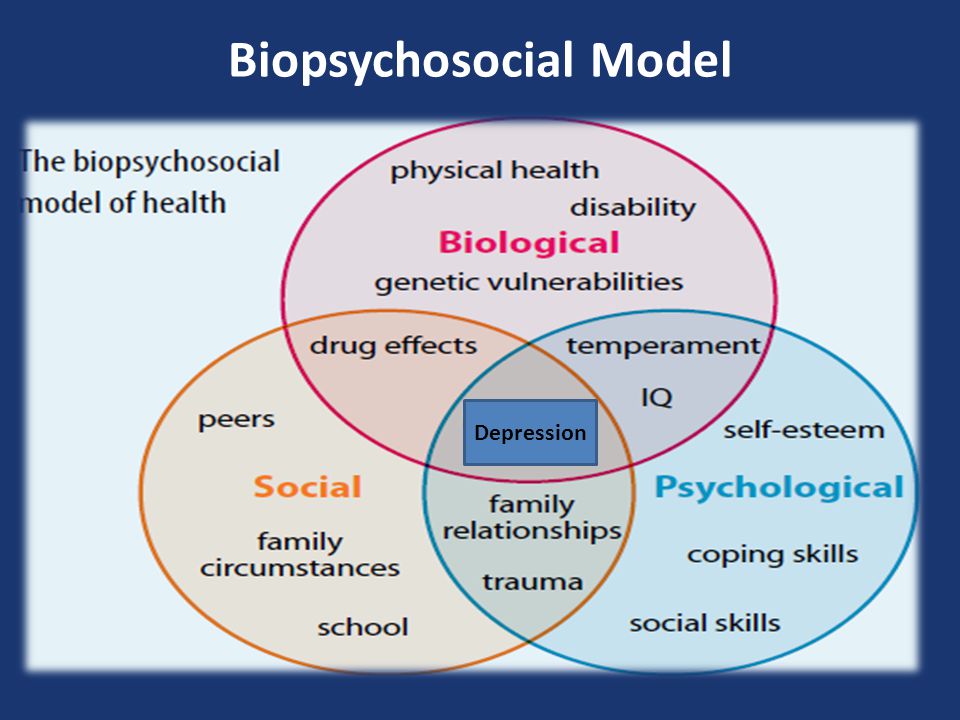 If internet access is a concern, many internet providers are currently offering discounts or free services during the pandemic. Trying to maintain connections and/or reaching out to others will help to reduce the feeling of isolation that everyone experiences while practicing social distancing. This may also be a great opportunity to reach out to friends or family members who live far away or you have not spoken to for a while!
If internet access is a concern, many internet providers are currently offering discounts or free services during the pandemic. Trying to maintain connections and/or reaching out to others will help to reduce the feeling of isolation that everyone experiences while practicing social distancing. This may also be a great opportunity to reach out to friends or family members who live far away or you have not spoken to for a while!
Above all, follow the CDC guidelines (try to avoid sensationalistic news feeds) so that you and your loved ones can stay healthy and safe!
Department of Psychotic Spectrum Disorders - Moscow Research Institute of Psychiatry
Contacts
Employees
The department was formed in the late 70s, given the name of the Department of Community Psychiatry and the Organization of Psychiatric Care.
The result of the activity of the department was a significant modification of the work of out-of-hospital units of psychiatric care, bringing care closer to the needs of patients.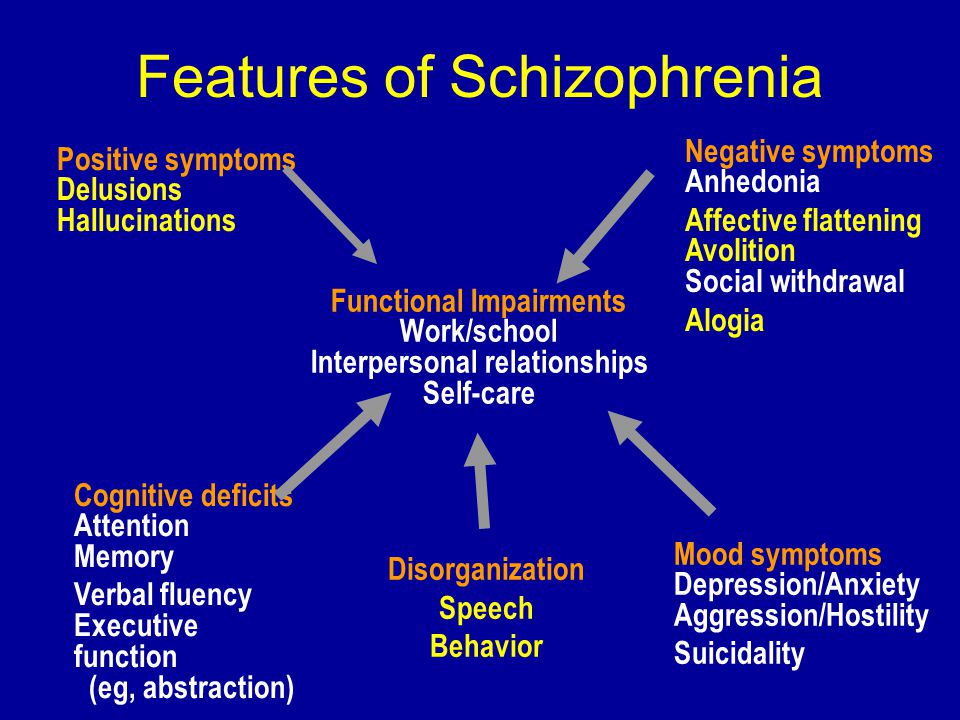 The foundations of the modern management of psychiatric patients in the dispensary were laid, criteria for dispensary observation of patients were developed and implemented, indications for removing patients from psychiatric records were substantiated. Subacute psychotic states have been extensively investigated. The work of the department formed the basis of the regulation on day hospitals, the rates of psychologists, social work specialists and social workers were introduced into the out-of-hospital link.
The foundations of the modern management of psychiatric patients in the dispensary were laid, criteria for dispensary observation of patients were developed and implemented, indications for removing patients from psychiatric records were substantiated. Subacute psychotic states have been extensively investigated. The work of the department formed the basis of the regulation on day hospitals, the rates of psychologists, social work specialists and social workers were introduced into the out-of-hospital link.
The department has long played a key role in the analysis and forecasting of the activities of the psychiatric service, as well as the formation of the modern form of community psychiatric care, including the development of new organizational forms, their methodological support, as well as the legal framework for the activities of the psychiatric service. Professor I.Ya.Gurovich was one of the main authors and developers of the Law of the Russian Federation "On psychiatric care and guarantees of the rights of citizens in its provision.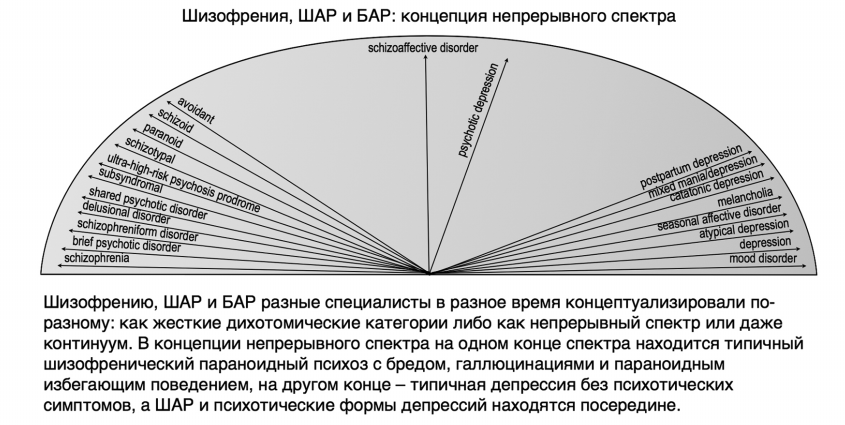 "
"
Within the framework of the biopsychosocial approach, the principles of interprofessional team management of patients, individual case management (case management) were developed, the direction of psychosocial therapy and rehabilitation was developed. Departments of the first psychotic episode were organized, both in Moscow and in many territories. The staff of the department scientifically substantiated such well-known methods as psychoeducation, compliance therapy, training of social and cognitive skills, and conducted pharmacoeconomic studies. Long-term cooperation of the department with the University of Calgary made it possible to develop joint educational programs, as a result of which a large number of specialists from the regions were trained in the methods of psychosocial therapy and rehabilitation of the mentally ill, including during internships in Canada. Such important phenomena as the stigma of mental illness and psychiatric disability have been studied. Particular attention was paid to the development and implementation of new forms of care, such as a community intensive care unit, medical rehabilitation units, a unit for the mentally ill who have lost social ties.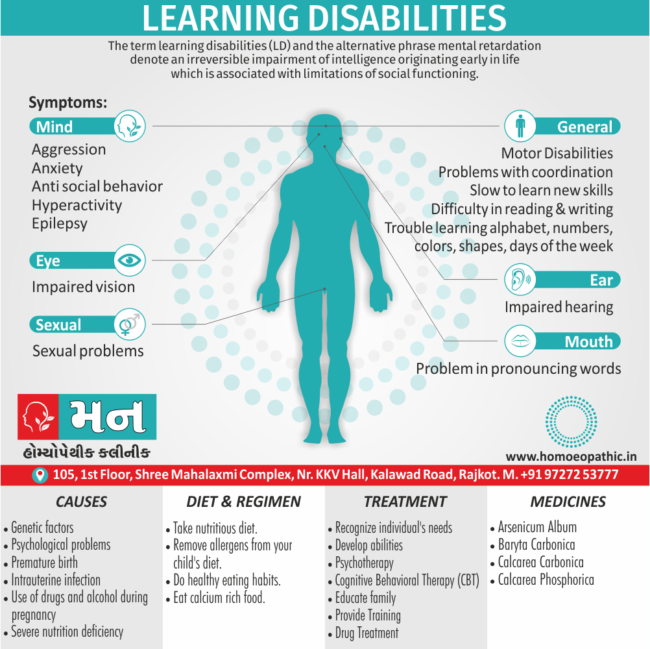 These forms formed the basis of the modern rehabilitation direction in psychiatry, used in the Procedure for the provision of psychiatric care. With the participation of the staff of the department, the first in Russia association of consumers of psychiatric care was organized, now known as the All-Russian Public Organization of Disabled Persons Due to Mental Disorders and Their Relatives "New Opportunities" with branches in more than 50 regions of the country.
These forms formed the basis of the modern rehabilitation direction in psychiatry, used in the Procedure for the provision of psychiatric care. With the participation of the staff of the department, the first in Russia association of consumers of psychiatric care was organized, now known as the All-Russian Public Organization of Disabled Persons Due to Mental Disorders and Their Relatives "New Opportunities" with branches in more than 50 regions of the country.
The work of the department is aimed at studying schizophrenia and psychotic spectrum disorders, which is reflected in numerous works of researchers. Special attention was also paid to the creation of the concept of multiprofessional care for patients with newly developed psychotic conditions. This formed the basis for the developed system of management (including long-term) of this category of patients, which is actively used in the system of providing psychiatric care. Particular emphasis is placed on the study of cognitive impairments, including social cognition impairments in psychotic disorders, which are currently considered as the third (along with productive and negative symptoms) group of symptoms in schizophrenia and schizophrenia spectrum disorders. The latest forms of cognitive remediation are tested on the basis of clinical departments. Currently, a line of work is being developed aimed at the study of biomarkers of schizophrenia and other psychotic disorders, including in cooperation with Moscow State University.
The latest forms of cognitive remediation are tested on the basis of clinical departments. Currently, a line of work is being developed aimed at the study of biomarkers of schizophrenia and other psychotic disorders, including in cooperation with Moscow State University.
Particular attention is paid to the study of the etiology and pathogenesis of acute psychotic states at the initial stages of disorders, since in some cases psychotic states can develop against the background of the action of autoimmune factors (for example, antibodies to N-methyl-D-aspartate (NMDA) receptors), which requires additional examination methods (oncoscreening, detection of the above antibodies in the blood) for differential diagnosis and other approaches to pharmacological treatment.
Another direction of modern approaches is the identification of neurophysiological markers. For this purpose, studies of social cognition disorders are being carried out using a 128-channel EEG, which allows recording the electrical activity of the brain in response to certain external stimuli (for example, faces expressing certain emotions).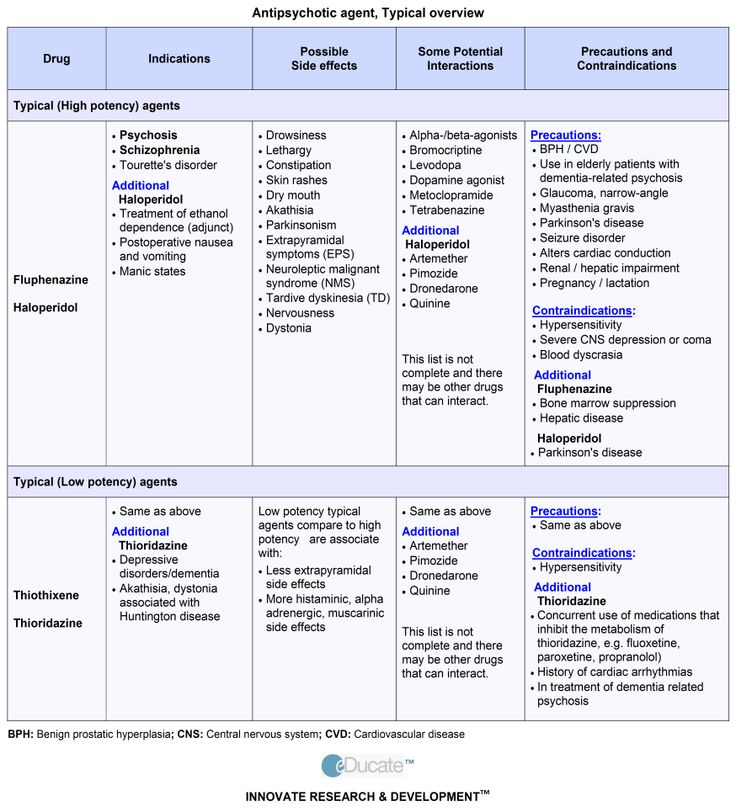 The importance of these studies is due to impairments in the recognition of all basic emotions in people with schizophrenia spectrum disorders, which can often affect the quality of life and social functioning of patients.
The importance of these studies is due to impairments in the recognition of all basic emotions in people with schizophrenia spectrum disorders, which can often affect the quality of life and social functioning of patients.
Another area of neurophysiological research carried out in the department is the study of disorders of oculomotor functions. Oculomotor indicators provide ample opportunities for assessing cognitive processes, including in mental illness. According to various parameters of eye movements, one can judge the dominance of attention subsystems, the state of working memory, executive control systems, which will determine the depth of psychopathological disorders and, in general, improve the quality of diagnostics and psychosocial therapy.
The department has trained 3 Doctors of Science, 31 Candidates of Science; published 10 monographs, 4 practical guides, more than 50 guidelines, about 1000 scientific articles.
id
Contacts
Phone: 8 (495) 963 7663
id
Employees
- Kiryanova9 Elena Mikhailovna
- Papsuev Oleg Olegovich , Leading Researcher, Candidate of Medical Sciences
- Shashkova Nina Gennadievna , Senior Researcher, Candidate of Medical Sciences
- Movina Larisa Georgievna , senior researcher, candidate of medical sciences
- Lyudmila Ivanovna Salnikova , Senior Researcher, Candidate of Medical Sciences
- Karyakina Maria Vladimirovna , researcher
- Spektor Valery Andreevich , researcher
- Murashko Alexey Andreevich , Researcher
- Novikov Alexander Vadimovich , researcher
- Churikova Marina Alexandrovna , junior researcher
- Nikolskaya Elena Nikolaevna , laboratory researcher
List of the main publications of the staff of the department:
- Psychosocial and cognitive therapy and rehabilitation of the mentally ill.
 Practical guide: collective monograph / Ed. AND I. Gurovich, A.B. Shmukler. Moscow: ID "Medpraktika-M", 2015. 420 p.
Practical guide: collective monograph / Ed. AND I. Gurovich, A.B. Shmukler. Moscow: ID "Medpraktika-M", 2015. 420 p. - Gurovich I.Ya., Shmukler A.B., Golland V.B. Zaichenko N.M. Psychiatric service in Russia in 2006-2011 Dynamics of indicators and analysis of development processes: monograph. Moscow: , 2012. 600 p.
- Shmukler A.B. The problem of schizophrenia in modern research. M., 2011. 84 p.
- Gurovich I.Ya., Shmukler A.B. First psychotic episode (problems and psychiatric care): monograph. M.: MEDPRAKTIKA-M, 2010. 544 p.
- Shmukler A.B., Kiryanova E.M., Papsuev O.O., Movina L.G., Murashko A.A., Davydov K.V., Davydova A.S. The system of psychosocial therapy for the mentally ill as an integral part of psychiatric care // In the collection: Prize of the city of Moscow in the field of medicine. Collection of abstracts of scientific papers submitted for the award in 2020. Moscow, 2021, pp. 140-141.
- Murashko A.A., Pavlov K.A., Pavlova O.
 V., Gurina O.I., Shmukler A. Antibodies against NMDA receptor in psychotic disorders: a systematic review // Neuropsychobiology, 2021. Doi: 10.1159/000515930
V., Gurina O.I., Shmukler A. Antibodies against NMDA receptor in psychotic disorders: a systematic review // Neuropsychobiology, 2021. Doi: 10.1159/000515930 - Murashko A.A. Possibilities of using virtual reality in psychiatry // Social and clinical psychiatry. 2021. V. 31. No. 2 P.101-105
- Shmukler A.B., Karyakina M.V. Network analysis as a new research approach in psychiatry // Psychiatry and psychopharmacotherapy. 2020. №5. pp.4–8.
- Spector V.A., Mnatsakanyan E.V., Shmukler A.B. Changes in P100 and N170 in the perception of facial expression in patients with schizophrenia and schizoaffective disorder. Russian Psychiatric Journal. 2020. №6. pp. 82-92
- Kuznetsov S.Yu., Kozhevnikova M.Yu., Movina L.G., Papsuev O.O. Dynamics of social cognition indicators and apathy scale in patients with schizophrenia spectrum disorders who underwent metacognitive training. Russian Psychiatric Journal. 2020. №6. pp. 55-61.
- Karyakina M.V., Rychkova O.
 V. Approaches to the analysis of violations of higher mental functions // Review of Psychiatry and Medical Psychology named after V.M. Bekhterev. 2020. №2. C. 38-46
V. Approaches to the analysis of violations of higher mental functions // Review of Psychiatry and Medical Psychology named after V.M. Bekhterev. 2020. №2. C. 38-46 - Shashkova N.G., Gazha A.K. The first psychotic episode: features of the provision of psychiatric care to patients in modern conditions // Social and Clinical Psychiatry. 2020.V.30, No.2. pp.80-90
- Maloman I.S., Gazha A.K. "Housing with support" as one of the forms of psychosocial rehabilitation of the mentally ill // Social and Clinical Psychiatry. 2020.V.30, No.2. C.90-95
- A. B. Shmukler, G. P. Kostyuk, A. V. Latanov, M. Yu. Sidorova, V. N. Anisimov, M. V. Karyakina, V. A. BUT. Network analysis of cognitive, oculomotor and speech indicators in schizophrenia // Journal of Neurology and Psychiatry. S.S.Korsakov. 2020. V.120. No. 5, Issue 2. P. 54-60
- Papsuev O.O., Movina L.G., Gladyshev I.O., Shmukler A.B. Psychometric properties of the Russian version of the Brief Negative Symptom Assessment Scale (BNSS) in patients with schizophrenia and schizophrenia spectrum disorders.
 Social and Clinical Psychiatry. 2020. Vol. 30, No. 2. S.22-30
Social and Clinical Psychiatry. 2020. Vol. 30, No. 2. S.22-30 - Murashko A.A., Kiryanova E.M., Salnikova L.I., Spektor V.A. Clinical and epidemiological characteristics of psychotic spectrum disorders associated with antibodies to NMDA receptors: a study protocol // Social and Clinical Psychiatry. 2020. V. 30. No. 3. S. 37-42
- Spector V.A. Disturbances in the perception of facial emotions in patients with schizophrenia and schizoaffective disorder (clinical and neurophysiological aspects). Study design // Social and clinical psychiatry. 2020. Vol. 30, No. 2. pp.15-21
- Karyakina M.V., Shmukler A.B. Cluster analysis of neurocognitive impairments in schizophrenia and schizophrenic spectrum disorders // V.M. Bekhterev Review of Psychiatry and Medical Psychology. 2020. №1. pp.45-51
- Shmukler A.B. Clinical and psychopathological approach in the system of rehabilitation of the mentally ill // Social and Clinical Psychiatry. 2020. V.30, No.1. pp.8-12
- Kuznetsov S.
 Yu., Afyan M.V., Kozhevnikova M.Yu., Movina L.G. Meta-cognitive training: theoretical foundations, practical aspects, effectiveness // Social and clinical psychiatry. 2020.V.30, No.1, P.97-101
Yu., Afyan M.V., Kozhevnikova M.Yu., Movina L.G. Meta-cognitive training: theoretical foundations, practical aspects, effectiveness // Social and clinical psychiatry. 2020.V.30, No.1, P.97-101 - Shmukler A.B., Ivashkina A.A., Murashko A.A. A case of anti-NMDA receptor encephalitis with a clinical picture of febrile catatonia // Bulletin of Siberian Medicine. 2019. Vol. 18 No. 4
- Kibitov A.A., Shmukler A.B. Effect of CYP2D6 gene polymorphisms on the severity of extrapyramidal side effects of haloperidol therapy. Social and Clinical Psychiatry. 2019. V.29, No.3. P.56 – 63
- Moldovan R., McGhee K.A., Papsuev O., Austin J. C. Psychiatric genetic counseling: A mapping exercise. // American Journal of MedicalGeneics part B: Neuropsychiatric Genetics. 2019. Vol. 180, No. 8. P. 523-532.
- Mucci A., Vignapiano A., Bitter I., Austin S. F., Delouche C., Dollfus S., Erfurth A., Fleischhacker W. W., Giordano G. M., Gladyshev I., Glenthøj B., Gütter K., Hofer A.
 , Hubeňák J., Kaiser S., Libiger J., Melle I., Nielsen M. Ø., Papsuev O., Rybakowski J. K., … Galderisi, S. A large European, multicenter, multinational validation study of the Brief Negative Symptom Scale / / European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology.2019. Vol. 29, No. 8. P.947–959.
, Hubeňák J., Kaiser S., Libiger J., Melle I., Nielsen M. Ø., Papsuev O., Rybakowski J. K., … Galderisi, S. A large European, multicenter, multinational validation study of the Brief Negative Symptom Scale / / European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology.2019. Vol. 29, No. 8. P.947–959. - urashko A.A., Shmukler A.B. EEG correlates of face recognition in patients with schizophrenia spectrum disorders: A systematic review // Clinical neurophysiology. 2019 Vol. 130, N6. P. 986-996
- Shmukler A.B. Psychiatry as a medical discipline // Social and clinical psychiatry. 2019. V.29, No.1. pp.79-81
- Papsuev O.O., Movina L.G., Kuznetsova O.G., Levina N.B. Experience in the application of the supported employment program in the conditions of the medical rehabilitation department. Social and Clinical Psychiatry. 2019. T.29, No.1. pp.32-39
- Shashkova N.G., Semenova N.D. Patients with schizophrenia and schizophrenic spectrum disorders with refusals of observation and treatment in outpatient practice // Social and Clinical Psychiatry.
 2019. V.29, No.1. pp.24-31
2019. V.29, No.1. pp.24-31 - Sukhachevsky I.S., Anisimov V.N., Latanov A.V., Shmukler A.B. Oculomotor disorders in patients with schizophrenia // Social and Clinical Psychiatry. 2018. V. 28. No. 1. S. 83-89.
- Minyacheva M.V., Gladyshev I.O., Kiselnikova K.G., Movina L.G., Papsuev O.O. Experience in using the apathy scale in patients with schizophrenia spectrum disorders // Social and Clinical Psychiatry. 2018. V.28, No. 4. pp.17-25
- GurovichI.Ya., Shmukler A.B., Papsuev O.O. Psychosocial rehabilitation as an essential area of psychiatric care targeting the social recovery of mentally ill patients // International journal of culture and mental health. 2018 Vol. 11, No. 1. P.46-51
- Garakh Z.V., Novototskii-Vlasov V.Y., Strelets V.B., Zaitseva Y.S., Shmukler A.B. Effects of instructions on the early stages of the visual perception of verbal stimuli in health and schizophrenia // Neuroscience and Behavioral Physiology. 2018 Vol. 48, No. 4. P.463-473
- Zaytseva Y.
 , Garakh Z., Novototsky-Vlasov V., Gurovich I. Y., Shmukler A., Papaefstathiou A., Horáček J., Španiel F., Strelets V. B. EEG coherence in a mental arithmetic task performance in first episode schizophrenia and schizoaffective disorder. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2018. Vol.129, N 11. P.2315–2324.
, Garakh Z., Novototsky-Vlasov V., Gurovich I. Y., Shmukler A., Papaefstathiou A., Horáček J., Španiel F., Strelets V. B. EEG coherence in a mental arithmetic task performance in first episode schizophrenia and schizoaffective disorder. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2018. Vol.129, N 11. P.2315–2324. - Murashko A.A. Neurophysiological aspects of face perception in patients with schizophrenia spectrum disorders // Social and Clinical Psychiatry. 2018. V.28, No.3. S.87-91
- Shmukler A.B., Mazo G.E. Functional recovery vs remission of symptoms – a paradigm shift in therapeutic targets in patients with depressive disorder // Social and Clinical Psychiatry. 2018. V.28, No.3. pp.68-73
- Neznanov N.G., Shmukler A.B., Kostyuk G.P., Sofronov A.G. The first psychotic episode: epidemiological aspects of the organization of care // Social and Clinical Psychiatry. 2018. V.28, No.3. pp.5-11
- Semenova N.
 , Kostyuk G., Rupchev G., Chernov N. Telling us how it is: The patient’s experience of psychological assessment // European Psychiatry. 2018 Vol. 48. P.S203
, Kostyuk G., Rupchev G., Chernov N. Telling us how it is: The patient’s experience of psychological assessment // European Psychiatry. 2018 Vol. 48. P.S203 - Semenova N., Kryukova E., Karabasheva N. Psychosocial treatments: What patients say they need and what clinical psychologists can offer // European Psychiatry. 2018 Vol. 48. P.S718
- Shashkova N.G., Kiryanova E.M., Salnikova L.I., Storozhakova Ya.A. Dynamics of outpatient contingents of patients with schizophrenia and schizophrenia spectrum disorders and dispensary observation at the present stage // Social and Clinical Psychiatry. 2018. V.28, No.1. pp. 36-43
- Minyaycheva M., Gladyshev I., Papsuev O. T247. Insight into negative symptoms as an inportant target for psychosocial rehabilitation in relation to clinical characteristics // Schizophr Bull. 2018 Vol. 44 S.1.P.S213
- Faerden A., Lyngstad S. H., Simonsen C., Ringen P. A., Papsuev O., Dieset I., Andreassen O. A., Agartz I., Marder S. R.
 , Melle I. Reliability and validity of the self-report version of the apathy evaluation scale in first-episode Psychosis: Concordance with the clinical version at baseline and 12 months follow-up // Psychiatry Res. 2018 Vol. 267. P. 140-147.
, Melle I. Reliability and validity of the self-report version of the apathy evaluation scale in first-episode Psychosis: Concordance with the clinical version at baseline and 12 months follow-up // Psychiatry Res. 2018 Vol. 267. P. 140-147. - Golimbet V.E., Garakh Z.V., Zaytseva Y., Alfimova M. V., Lezheiko T. V., Kondratiev N. V., Shmukler A. B., Gurovich I. Y., Strelets V. B. The Dopamine Receptor D2 C957T Polymorphism Modulates Early Components of Event-Related Potentials in Visual Word Recognition Task // Neuropsychobiology. 2017. Vol.76, N 3. P. 143-150.
- GurovichI.Ya. Papsuev O.O. Shmukler A.B. Movina L.G., StorozhakovaYa.A., Kiryanova E.M. Cognitive bias salience in patients with schizophrenia in relation to social functioning: A four case observation study // PsyCh Journal. 2016. Vol. 5, No. 1. P. 36-47.
- Minyaycheva M.V., Kiselnikova K.G., Papsuev O.O. Battery of scales for comprehensive assessment of social cognition, neurocognition and motivation in patients with schizophrenia // European Psychiatry.
 2016. Vol. 33. P. 723.
2016. Vol. 33. P. 723. - Papsuev O.O., Minyaycheva M.V., Movina L.G. Gurovich I. Ya. Social cognition across stages and forms of schizophrenia // European Psychiatry. 2016. Vol. 33. P. 307.
- Papsuev O.O., Minyaycheva M.V., Movina L.G. Gurovich I. Ya. Trajectories of social cognition in schizophrenia and schizophrenia spectrum disorders // NPJ Schizophrenia. 2016. 2. P. 27.
- Bukovskaya O., Shmukler A.B. Neurocognition and social cognition as a distinct construct in schizophrenia: an overview // Psychopathology and Addiction Medicine.2016. Vol. 1, N 1. P. http://pam-eng.ruspsy.net/article.php?post=474.
- Garah Z., Strelets V.B., Zaytseva Y., Shmukler A.B., GurovichI.Ya., Horacek J., Fiala O. EEG correlates of a mental arithmetic task in patients with first episode schizophrenia and schizoaffective disorder // Clinical Neurophysiology. 2015. Vol. 26, No. 11. P. 2090-2098.
- Shmukler A.B., GurovichI.Ya., Agius M., Zaytseva Y. Long-term trajectories of cognitive deficits in schizophrenia: a critical overview // European Psychiatry.
 2015. Vol. 30, No. 8. P. 1002-1010.
2015. Vol. 30, No. 8. P. 1002-1010. - Uzbekov M.G., Misionzhnik E., Shmukler A.B. et al. First episode of schizophrenia is characterized by pronounced metabolic disturbances // European Archives of Psychiatry and Clinical Neuroscience. 2015. No. 265, Suppl. 1. P. 1.
- Bukovskaya O., Shmukler A.B. Neurocognition and social cognition as a distinct construct in schizophrenia: an overview // Psychopathology and Addiction Medicine. 2016. Vol. 1, N 1.
- Gurovich I.Ya., Shmukler A.B., Papsuev O.O. Psychosocial rehabilitation is the most important direction of psychiatric care for the social recovery of persons with mental disorders // Mental health of a person of the XXI century: a collection of articles / . Moscow: Gorodets Publishing House, 2016, pp. 316-317.
- Gurovich I.Ya., Papsuev O.O., Visnevskaya L.Ya. On the indicators of inpatient psychiatric care in European countries as a result of deinstitutionalization // Social and Clinical Psychiatry. 2016.
 V. 26, No. 3. C. 87-91.
V. 26, No. 3. C. 87-91. - Shmukler A.B. Cognitive impairments in the structure of depressive syndrome // Social and clinical psychiatry. 2016. V. 26, No. 1. C. 72-76.
M
Patents:
- Spatial-spectral isolation of the µ-rhythm of the human electroencephalogram: reg. Computer programs 2012618160 / Novototsky-Vlasov V.Yu., Garakh Zh.V., Zaitseva Yu.S. and etc.; applicant and copyright holder Moscow scientific research. Institute of Psychiatry; priority // Inventions. Useful models. 2012. no. S.
Acute and transient psychotic disorders
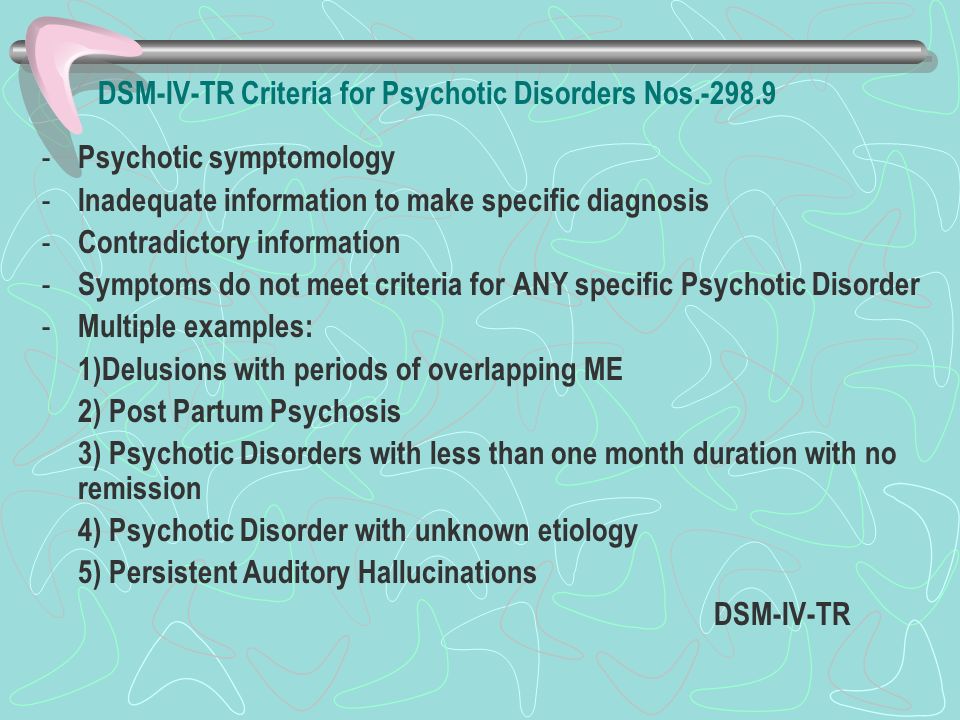
Acute and transient psychotic disorders are a group of conditions with a rapid onset of symptoms: a person's condition deteriorates sharply from a few days to two weeks. It is characterized by a variety of affective (from depression to euphoria) and psychotic (delusions, hallucinations) symptoms, which are constantly changing. A psychiatrist is in charge of diagnosing and treating the condition.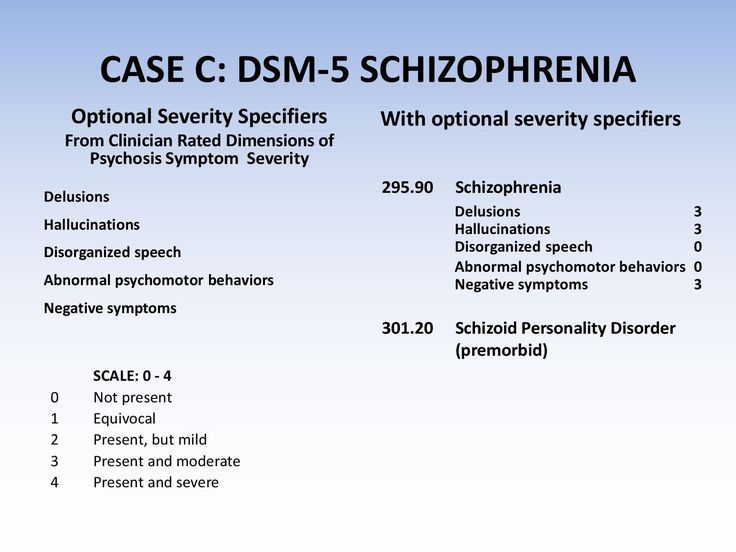
The group includes:
- acute polymorphic psychotic disorder in two variants - with and without symptoms of schizophrenia;
- acute schizophrenia-like psychotic disorder.
The exact reasons have not been established. Factors that contribute to the occurrence of disorders are strong emotional stresses: the loss of loved ones, a car accident, trauma, any kind of violence. The development of the disease can be triggered by the use of narcotic substances (even one-time and in small quantities), alcohol, or the postpartum period.
Important
Acute psychotic disorder is a sign of a serious imbalance in the nervous system. Although the acute condition is quickly relieved, treatment must be continued to prevent the transition to schizophrenia and similar diseases.
The International Classification of Diseases distinguishes three main characteristics for acute psychotic disorder (ICD-10 code: F23):
- Acute onset (up to two weeks).
- Typical psychotic and affective symptoms.
- Pre-disorder acute stress.
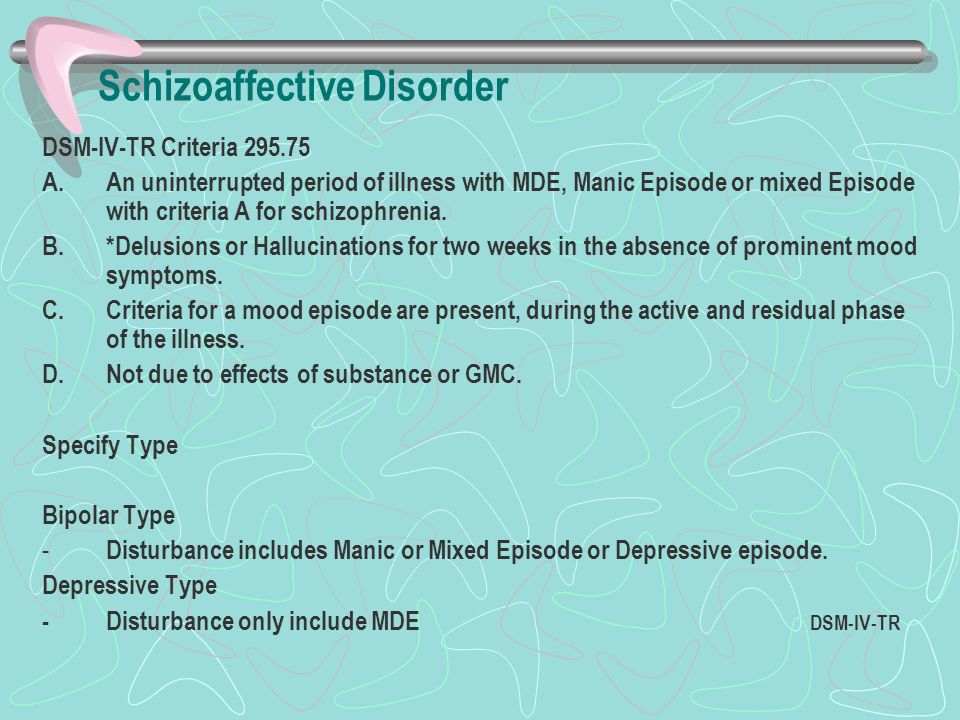
A variety of symptoms can erroneously suggest that a person has schizophrenia, a manic or depressive episode, schizoaffective psychosis, and other psychotic disorders. But due to the fact that the condition develops very quickly and is often stopped by medications within a few days or weeks, it is isolated separately.
In acute polymorphic psychotic disorder, treatment should be carried out for a long time. If you stop therapy immediately after the relief of symptoms and discharge from the hospital, an exacerbation may occur in the near future. Doses of drugs should be reduced gradually, under the supervision of an experienced psychiatrist.
Acute polymorphic psychotic disorder without symptoms of schizophrenia
This variant of the development of the disease is also called acute delusional disorder and is characterized by a rapid and multiple change in the content of hallucinations, delusions and affective disorders.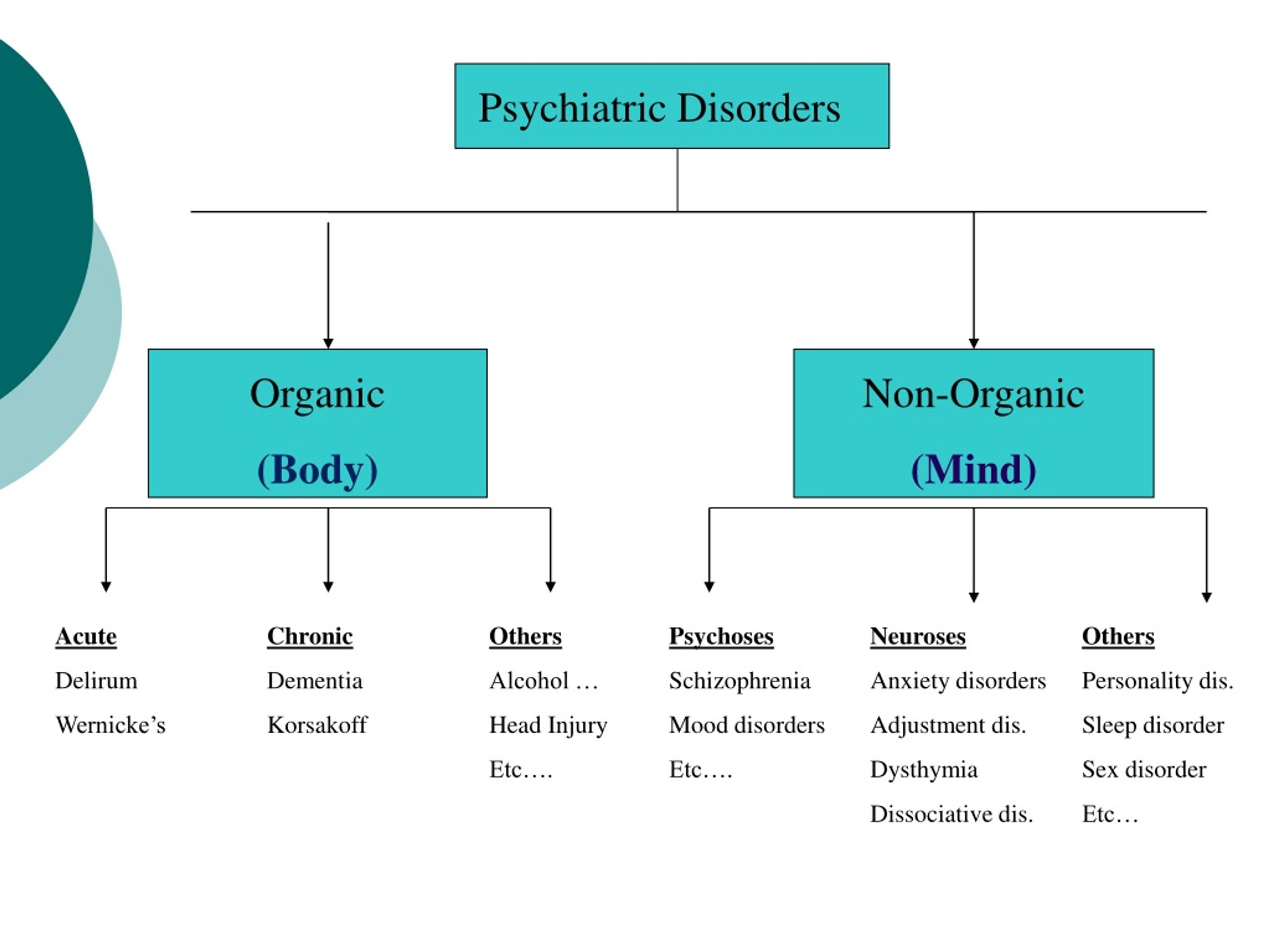
A person has suddenly successive flashes of delusions of persecution, ideas of his own greatness or confidence in his guilt and the presence of a serious illness. The content and type of accompanying hallucinations varies from day to day or more frequently. Constant changes are also observed in the emotional sphere: hypertrophied elation in a few hours is replaced by its strong decline and vice versa.
Symptoms in acute polymorphic disorder are constantly changing, sometimes every few hours.
There may be an acceleration or deceleration of thinking, physical retardation or motor excitation. The person is confused, anxious, inattentive.
Thus, the main distinguishing features of acute polymorphic psychotic disorder without symptoms of schizophrenia are:
- Constant change in the nature and intensity of psychotic (delusions and hallucinations) and affective manifestations (mood).
- Sudden onset and rapid development of symptoms.
- Not meeting diagnostic criteria for other psychotic disorders.
Acute polymorphic psychotic disorder with symptoms of schizophrenia
In this form of acute psychotic disorder, the necessary criterion is the presence of typical schizophrenic features. The most significant of them are:
- delusional states - for example, delusions of influence: a person is convinced that he is influenced by certain physical or mental forces - electromagnetic fields, electric current, hypnosis; some patients are convinced that they have superpowers;
- the patient's confidence that someone is influencing his thoughts - reading them, stealing them or bringing and putting into the brain new, alien ideas. A person may consider that his thoughts have become "visible" to everyone, that everyone can hear and read them;
- hallucinations - for example, a person hears a non-existent voice that evaluates his actions and thoughts, or several voices talking to each other.
These signs develop against the background of psychotic manifestations and emotional disorders that are characteristic of the previous form of the disease.
Important
The symptoms of schizophrenia are not yet schizophrenia. With adequate, complete treatment, the transition to a serious illness can be avoided.
The following characteristic symptoms of acute polymorphic psychotic disorder with symptoms of schizophrenia are distinguished:
- Abrupt onset of the disease and rapid development.
- Typical schizophrenic symptomatology, which is observed for no more than a month.
- Changeable nature of psychotic and affective manifestations.
Polymorphic psychotic disorder with schizophrenic symptoms is an insidious form due to its similarity to schizophrenia. Such episodes can often be the debut of schizophrenia and subsequently lead to deep personality defects, social isolation and disability.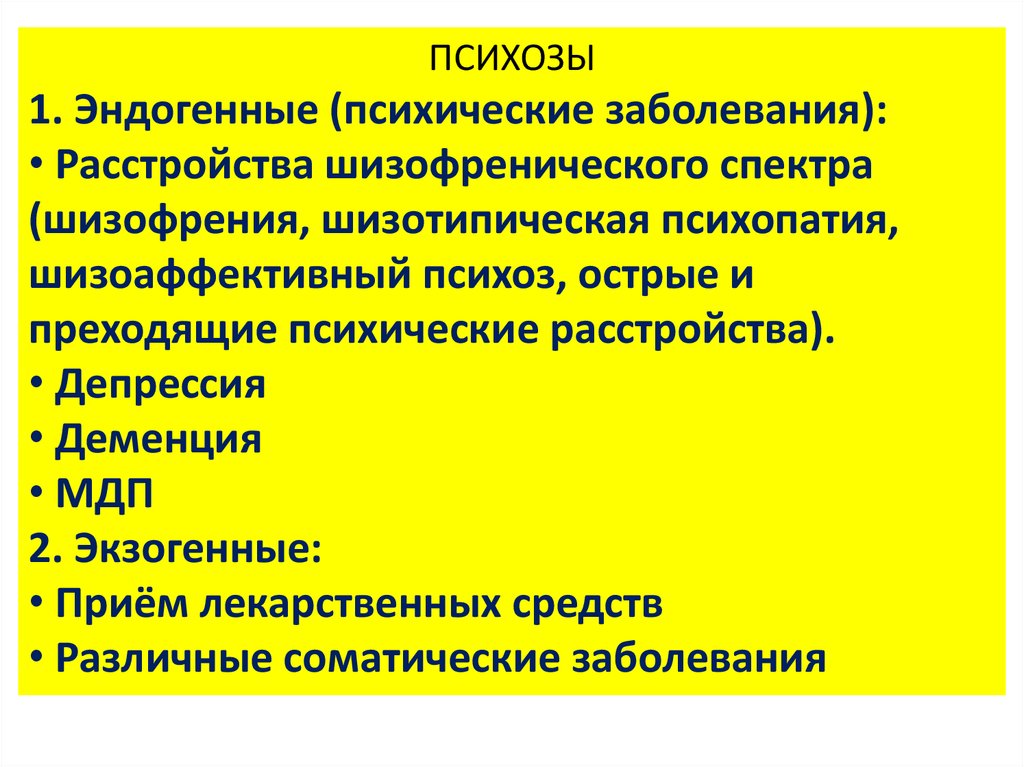 Successful control of the condition requires rapid diagnosis and correct treatment by a competent specialist with extensive experience.
Successful control of the condition requires rapid diagnosis and correct treatment by a competent specialist with extensive experience.
Acute schizophrenia-like psychotic disorder
This condition is characterized by typical schizophrenic symptoms, but, unlike the two variants of acute transient psychotic disorder described above, affective and psychotic manifestations become stable. Permanent changes and variability of symptoms do not occur with this variant.
In schizophrenia-like psychosis, the following symptoms are observed:
- Onset and development of symptoms within two weeks.
- Absence of variability in psychotic and affective manifestations that are observed in acute polymorphic psychotic disorder.
- Symptoms characteristic of schizophrenia.
Schizophrenia-like disorder must also be carefully differentiated from schizophrenia. If the symptoms do not stop for more than a month, it makes sense to change the diagnosis.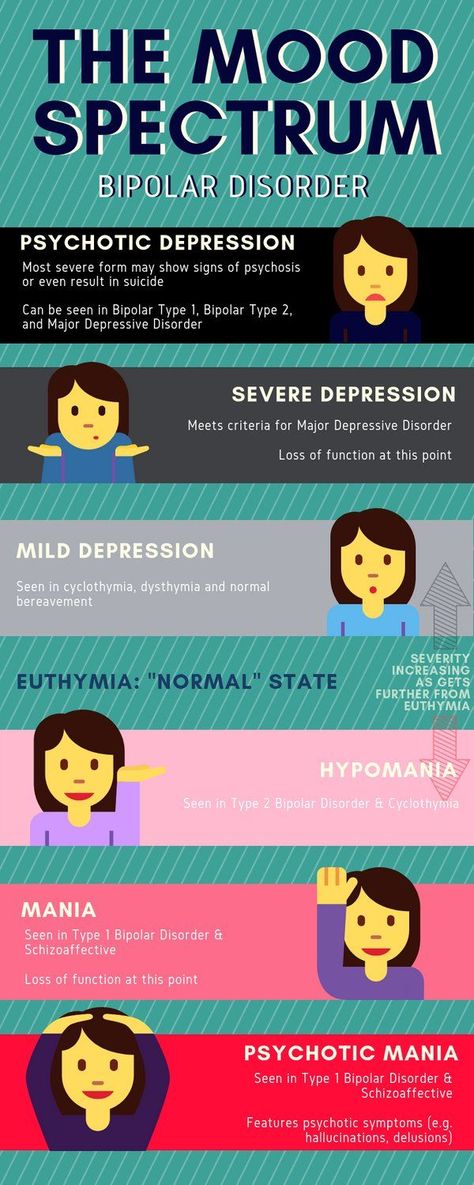
Diagnosis in acute polymorphic psychotic disorder
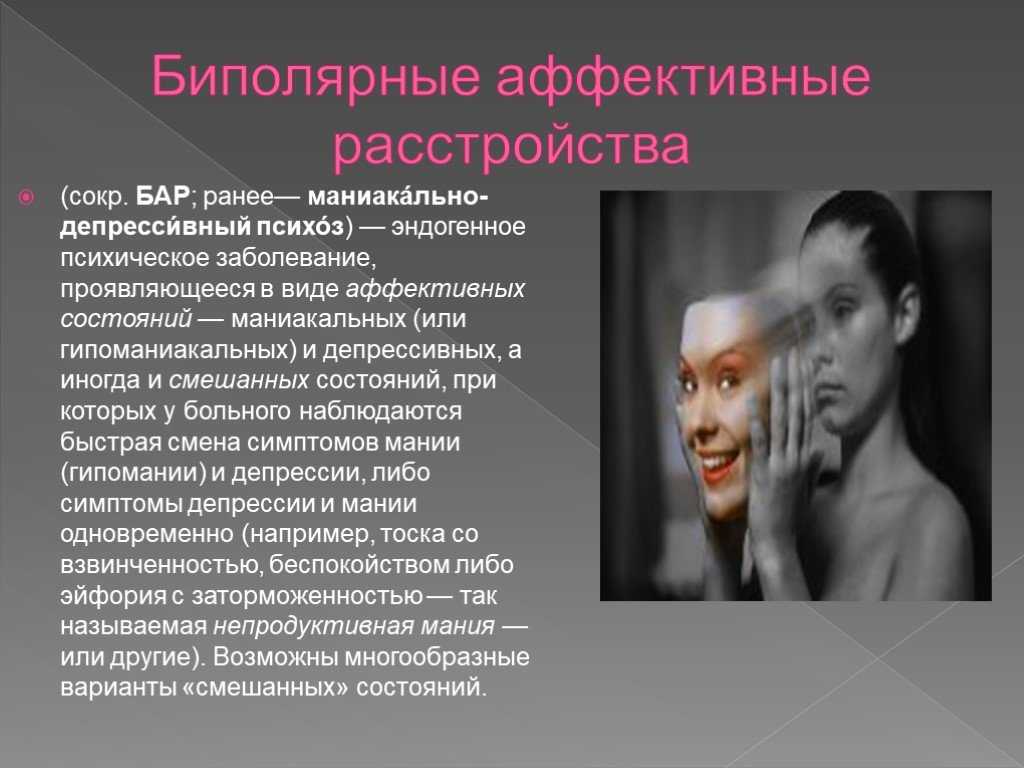
When making a diagnosis of acute psychotic disorder, it is necessary to exclude other mental illnesses: schizophrenia, schizoaffective psychosis, or bipolar disorder. It is necessary to make sure that there are no organic lesions and that various toxic substances affect the body. To do this, it is necessary to conduct a thorough examination, which only a competent specialist can handle.
For the differential diagnosis of acute psychotic disorder with schizophrenia, there are modern methods - Neurotest and Neurophysiological test system.
The following methods apply:
- functional and laboratory studies of the body - blood test, EEG; the influence of drugs, alcohol and organic lesions is excluded;
- psychiatric examination with analysis of anamnestic data and consultation with a clinical psychologist;
- Neurotest and Neurophysiological test system allow you to confirm the disease of the schizophrenic spectrum, assess the depth of the defect and the severity of the condition.
Treatment of acute psychotic disorders
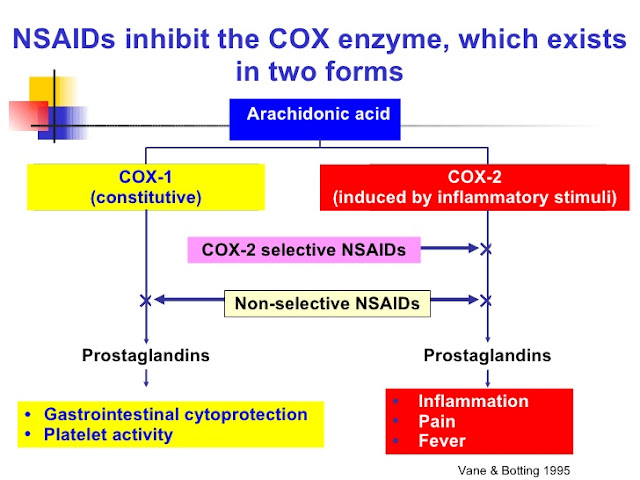
In the treatment of acute psychotic disorder, it is necessary to combine drug therapy and conversations with a psychiatrist. Medications are used that stimulate brain activity and increase the body's resistance to stress: nootropics, vitamins, hepatoprotectors. Modern neuroleptics are also used, with the help of which it is possible to achieve the best control of symptoms.
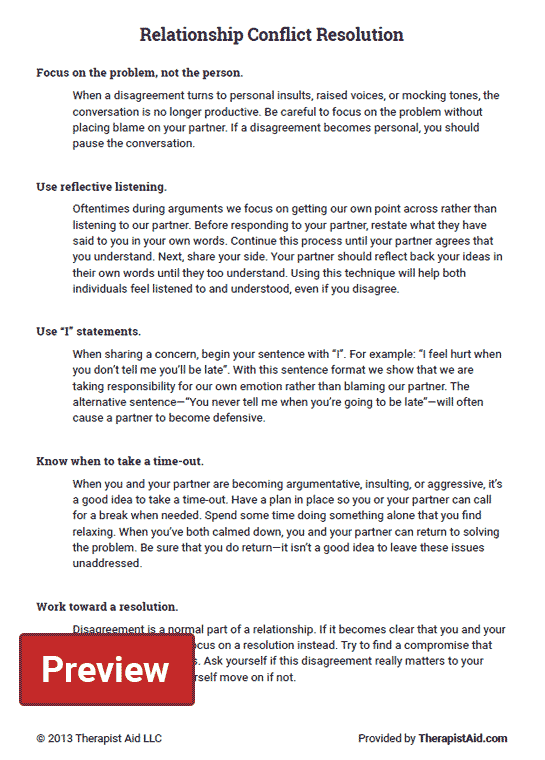
The positive effect of drugs is successfully supported by individual psychotherapy: such approaches help to deal with the stressful situation associated with the debut of the disease, teach you to control your psychological state and allow you to feel the support of loved ones.
One of the causes of acute psychotic disorder is severe stress. Psychotherapy helps not to succumb to the influence of external factors and thereby prevent new attacks.
To reduce the risk of the disorder turning into schizophrenia, schizoaffective psychosis, bipolar affective disorder, treatment by a psychiatrist should be continued for a long time, gradually reducing the dosage of drugs.