A specific phobia
Specific Phobia - StatPearls - NCBI Bookshelf
Chandan K. Samra; Sara Abdijadid.
Author Information
Last Update: May 8, 2022.
Continuing Education Activity
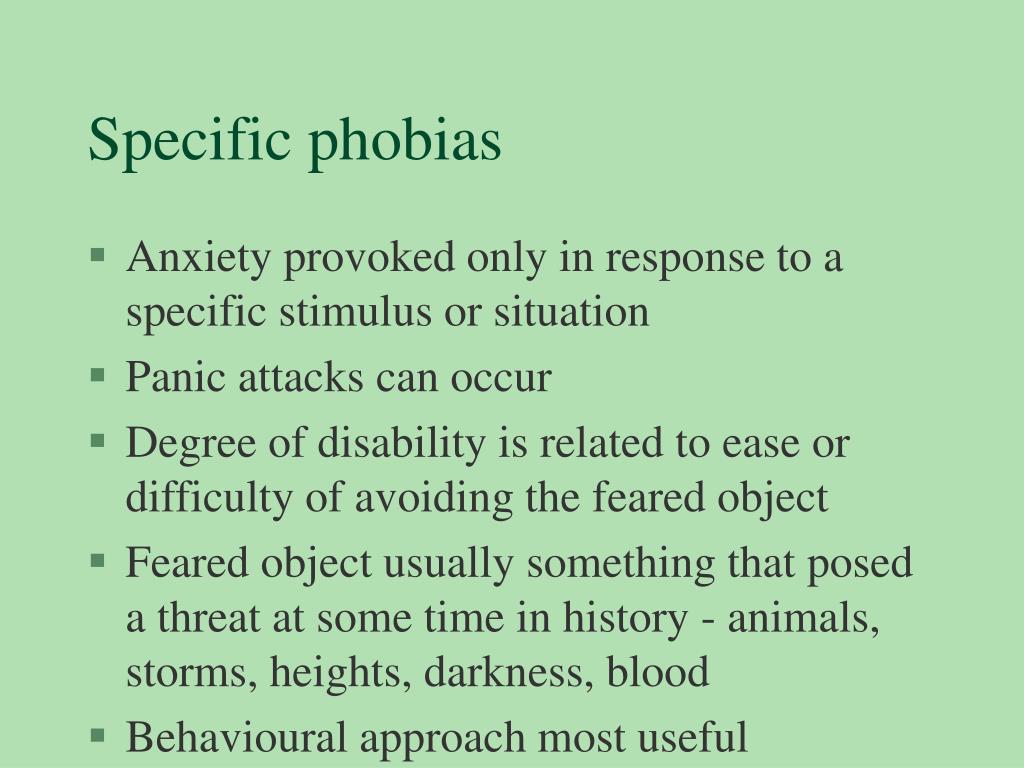
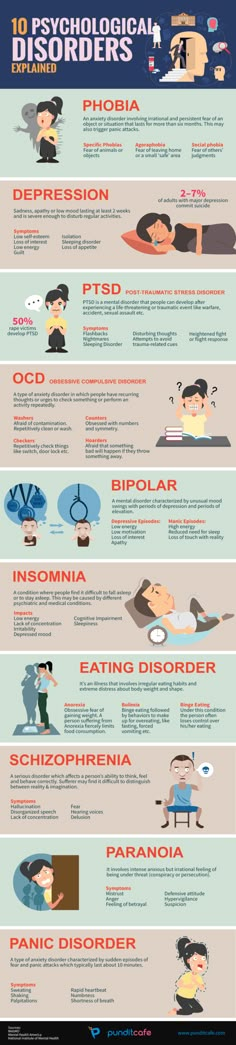
Patients with specific phobias experience anxiety and panic attacks along with unreasonable fear of exposure or anticipated exposure to a feared stimulus. According to some theories, specific phobias may develop due to an association of an object or situation with emotions such as fear and panic. This activity describes the evaluation and management of specific phobias and reviews the role of the interprofessional team in improving care for patients with this disorder.
Objectives:
Explain when a specific phobia should be considered on differential diagnosis.
Review the criteria used to diagnose specific phobias.
Describe the considerations that influence the management of specific phobias.
Review the importance of communication and cooperation among members of the interprofessional team in providing behavioral therapy as a first line treatment for patients with specific phobias.
Access free multiple choice questions on this topic.
Introduction
Patients with a specific phobia experience high levels of anxiety along with excessive and unreasonable fear due to either exposure to a phobic stimulus, the anticipation of exposure to a phobic stimulus, and even speaking about the feared stimulus. As a result, these patients will try to avoid the anxiety-provoking stimulus to any extent possible. Many patients have a strong family history of specific phobia. However, more studies need to be conducted to rule out the nongenetic transmission of specific phobias. [1][2][3]There is a high familial tendency in the blood injection injury type of phobia. Specific phobias can be categorized into the following subcategories:
Animals (spiders, insects, dogs)
Natural environment type (heights, storms, water)
Blood injection injury type (needles, invasive medical procedures)
Situational type (airplanes, elevators, enclosed spaces)
Other types of phobias that do not fit into the previous 4 categories
Etiology
The exact etiology of specific phobias is not known. However, some theories suggest that specific phobia may also develop due to an association of a specific object or situation with emotions such as fear and panic. Two theories have been proposed to show this pairing. The most common theory--classical conditioning model--postulates that a phobia precipitates when an event that provokes fear or anxiety is paired with a neutral event. An example of this would be in which a specific event such as driving is paired with an emotional experience such as an accident. As a result, the person is susceptible to a chronic emotional association between driving and anxiety. Although a person may not experience a panic attack or meet the criteria for a panic disorder, they may develop a fear that is expressed as having a specific phobia. Another mechanism of association is through modeling, in which a person observes a reaction in another person and internalizes that other person’s fears or warnings about the dangers of a specific object or situation.
However, some theories suggest that specific phobia may also develop due to an association of a specific object or situation with emotions such as fear and panic. Two theories have been proposed to show this pairing. The most common theory--classical conditioning model--postulates that a phobia precipitates when an event that provokes fear or anxiety is paired with a neutral event. An example of this would be in which a specific event such as driving is paired with an emotional experience such as an accident. As a result, the person is susceptible to a chronic emotional association between driving and anxiety. Although a person may not experience a panic attack or meet the criteria for a panic disorder, they may develop a fear that is expressed as having a specific phobia. Another mechanism of association is through modeling, in which a person observes a reaction in another person and internalizes that other person’s fears or warnings about the dangers of a specific object or situation. [4][5][6][7]
[4][5][6][7]
Epidemiology
Specific phobia affects about 5% to 10% of the US population. A bimodal distribution of onset can be seen with specific phobias. Animal phobia, natural environment phobia, and blood injection injury type of phobia tend to have a childhood peak, whereas, there is an early adulthood peak for situational phobia.
History and Physical
There is marked fear or anxiety regarding a specific object or situation, often including the following features:
The specific object or situation almost always provokes immediate fear or anxiety
Children may express the fear or anxiety by crying, tantrums, freezing, or by clinging
The phobic object or situation is actively and persistently avoided for 6 months or more
The fear or anxiety experienced is out of proportion to the actual danger posed by the specific object or situation
Notable, clinical distress or impairment in social, occupational, or other important areas of functioning is evident
The symptoms cannot be explained by another psychiatric disorder such as obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), separation anxiety disorder, or social anxiety disorder
Evaluation
Evaluation is usually limited to a detailed psychiatric assessment along with an elaborate psychosocial history to determine the chronicity of the symptomatology.
Treatment / Management
One of the most effective treatment modalities to mitigate specific phobias is behavioral therapy. Behavioral therapy includes implementing the principles of operant conditioning and extinction learning via systematic desensitization and flooding. In methodical desensitization, the patient is exposed to a list of stimuli ranking from the least to the most anxiety-provoking. With this method, patients are taught various techniques to deal with anxiety such as relaxation, breathing control, and alternative cognitive approaches. The cognitive-behavioral approach includes reinforcing the realization that the phobic stimulus is safe. As the patient masters these techniques, they are taught to use them in the face of anxiety-provoking stimuli and induce relaxation. As the patients become desensitized to each stimulus on the scale, they keep moving up until the most anxiety-provoking stimuli no longer elicit any fear or anxiety.[8][9][10][11] Flooding, also known as implosion, is another behavioral technique that can be used to treat specific phobias.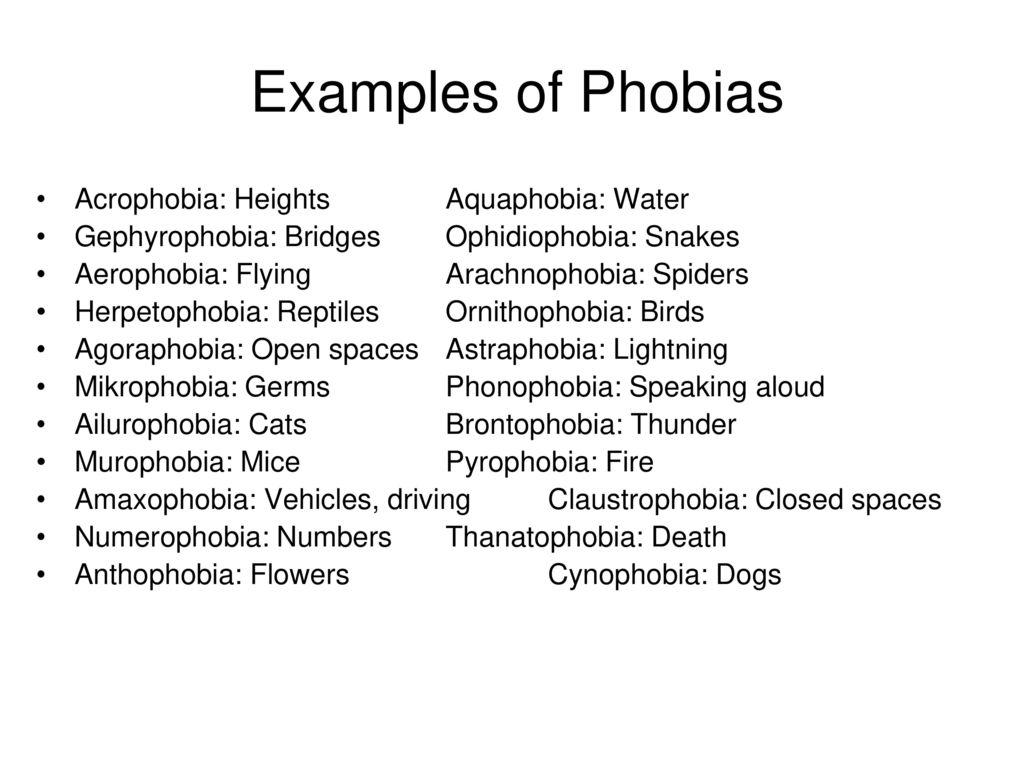 This technique involves increasing exposure to the stimulus to induce habituation and decrease anxiety. To be successful, behavioral therapy requires that patient be committed to the treatment, there are distinctly identified problems and objectives, and there are alternative strategies for dealing with the patient’s feelings.
This technique involves increasing exposure to the stimulus to induce habituation and decrease anxiety. To be successful, behavioral therapy requires that patient be committed to the treatment, there are distinctly identified problems and objectives, and there are alternative strategies for dealing with the patient’s feelings.
Patients with a blood injection injury phobia are advised to tense their bodies and remain seated during the exposure to avoid the possibility of fainting from a vasovagal reaction. Also, beta-blockers and benzodiazepines can be used in patients when the phobia is associated with panic attacks.
Other forms of treatment that may also be considered include virtual therapy in which the patient is exposed to or interacts with the phobic stimulus on a computer screen. This field of treatment is relatively novel and requires more research. Other treatment modalities include hypnosis, supportive therapy, and family therapy. The goal of all forms of therapy is to help the patient recognize that the feared stimulus is not dangerous and to provide emotional support.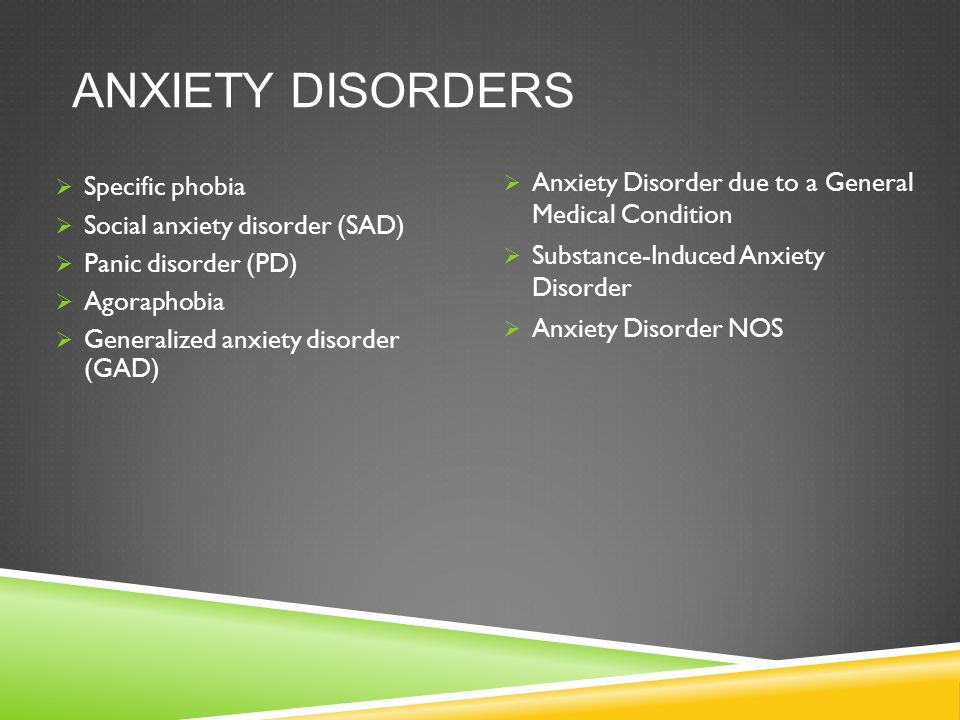
Differential Diagnosis
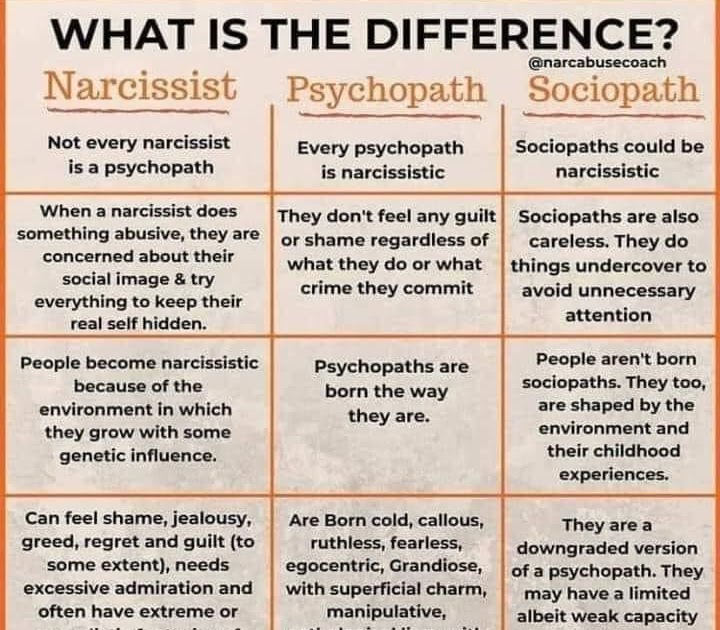
Medical conditions that can result in the development of a phobia include substance use particularly hallucinogens and sympathomimetics, central nervous system (CNS) tumors, and cerebrovascular diseases. However, in these conditions, phobic symptoms are unlikely in the absence of additional findings on physical, neurological, and mental status examinations.
Schizophrenic patients may also present with phobic symptoms. However, patients with a phobia have intact insight into their irrational fears and lack psychotic symptoms associated with schizophrenia.
It is also important to rule out panic disorder, agoraphobia, and avoidant personality disorder. It can be difficult to distinguish specific phobia from panic disorder, agoraphobia, and avoidant personality disorder. However, in specific phobias, these patients tend to experience anxiety or fear immediately upon exposure to the phobic stimulus. In addition, patients with specific phobia do not exhibit signs of fear or anxiety when they are not facing or anticipating the phobic stimulus.
It is important to rule out other conditions such as hypochondriasis, obsessive-compulsive disorder, and paranoid personality disorder. There is a subtle difference between hypochondriasis and specific phobia. For example, patients with hypochondriasis fear having the disease, and patients with specific phobia fear contracting the disease. The same holds true for the difference between obsessive-compulsive disorder and specific phobia. For example, patients with OCD may avoid knives because they have compulsive thoughts of harming their children; whereas, patients with a specific phobia may avoid knives because they fear cutting themselves. Patients with paranoid personality disorder have generalized fear, which is not found in patients with specific phobia.
Prognosis
When left untreated, phobias can be lifelong, however, studies show that phobias tend to spontaneously attenuate over time. With the appropriate behavioral techniques and medications, the prognosis is good.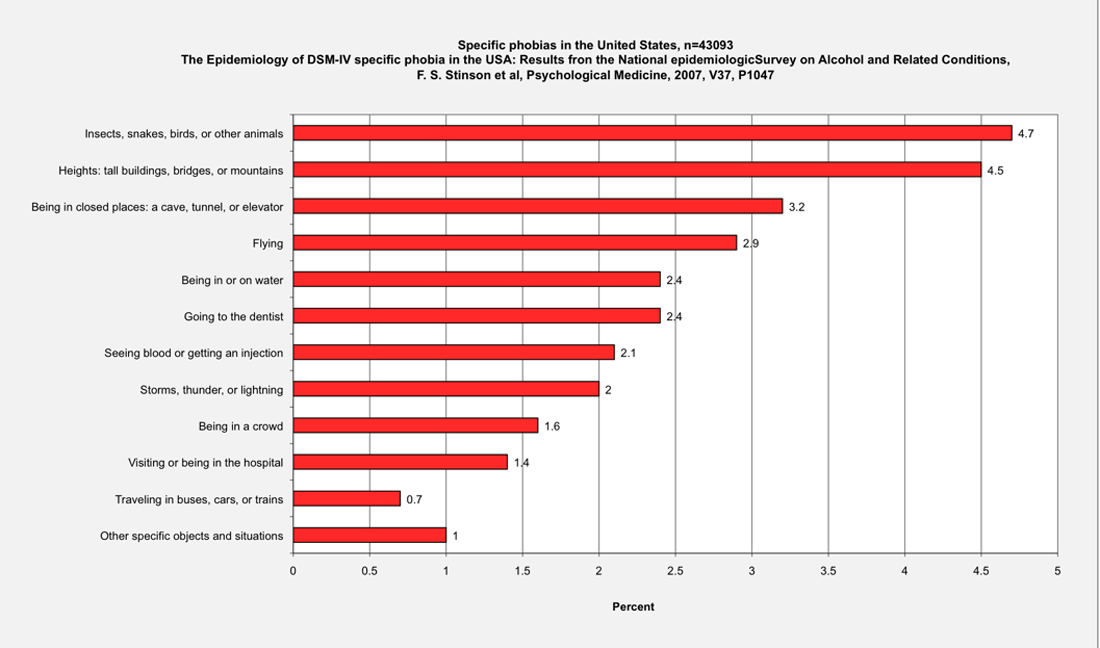
Complications
Left untreated, specific phobias can significantly impair functioning. If a patient is unable to engage in normative social dynamics due to debilitating anxiety, the patient may end up isolated away from society.
Deterrence and Patient Education
Patients are advised to see a psychiatrist when symptoms are affecting their daily activities and quality of life. With proper behavioral therapy, patients can retrain their association cortices to mitigate the conditioned fear response.
Pearls and Other Issues
The most common signs/symptoms that can be seen in specific phobia are:
Feeling nauseous, dizzy, or fainting
Difficulty breathing, chest tightness, or fast heartbeat
The fear or anxiety out of proportion to the real danger posed by the specific object or situation
Common modalities of treatment include:
Systematic desensitization
Flooding
Medications such as beta-blockers and benzodiazepines
The fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more.
The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other relevant areas of functioning.
Enhancing Healthcare Team Outcomes
The management of phobias is usually with an interprofessional team that includes a mental health nurse, psychiatrist, psychotherapist, and primary care provider. In most cases, behavior therapy is the first-line treatment and does work. However, the period of desensitization can take weeks or even months.
To be successful, behavioral therapy requires that the patient be committed to the treatment, there are distinctly identified problems and objectives, and there are alternative strategies for dealing with the patient’s feelings.
Other forms of treatment that may also be considered are virtual therapy in which the patient is exposed to or interact with the phobic object or situation on the computer screen. This field of treatment is relatively new and requires more research. Other treatment modalities include hypnosis, supportive therapy, and family therapy. The goal of all 3 forms of therapy is to help the patient recognize that the feared stimulus is not dangerous and to provide emotional support.
Other treatment modalities include hypnosis, supportive therapy, and family therapy. The goal of all 3 forms of therapy is to help the patient recognize that the feared stimulus is not dangerous and to provide emotional support.
Overall, the prognosis for most patients is fair because relapses are common. [12][13] (level V)
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Rubo M, Huestegge L, Gamer M. Social anxiety modulates visual exploration in real life - but not in the laboratory. Br J Psychol. 2020 May;111(2):233-245. [PMC free article: PMC7187184] [PubMed: 30945279]
- 2.
Fragiotta G, Pierelli F, Coppola G, Conte C, Perrotta A, Serrao M. Effect of phobic visual stimulation on spinal nociception. Physiol Behav. 2019 Jul 01;206:22-27. [PubMed: 30902634]
- 3.
Health Quality Ontario. Internet-Delivered Cognitive Behavioural Therapy for Major Depression and Anxiety Disorders: A Health Technology Assessment.
 Ont Health Technol Assess Ser. 2019;19(6):1-199. [PMC free article: PMC6394534] [PubMed: 30873251]
Ont Health Technol Assess Ser. 2019;19(6):1-199. [PMC free article: PMC6394534] [PubMed: 30873251]- 4.
Campos D, Bretón-López J, Botella C, Mira A, Castilla D, Mor S, Baños R, Quero S. Efficacy of an internet-based exposure treatment for flying phobia (NO-FEAR Airlines) with and without therapist guidance: a randomized controlled trial. BMC Psychiatry. 2019 Mar 06;19(1):86. [PMC free article: PMC6404352] [PubMed: 30841930]
- 5.
Pary R, Sarai SK, Micchelli A, Lippmann S. Anxiety Disorders in Older Patients. Prim Care Companion CNS Disord. 2019 Jan 31;21(1) [PubMed: 30806999]
- 6.
Kawsar MDS, Yilanli M, Marwaha R. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 7, 2022. School Refusal. [PubMed: 30480934]
- 7.
Oing T, Prescott J. Implementations of Virtual Reality for Anxiety-Related Disorders: Systematic Review. JMIR Serious Games. 2018 Nov 07;6(4):e10965. [PMC free article: PMC6249506] [PubMed: 30404770]
- 8.
Spurling KJ, McGoldrick VP. Blood-Injection-Injury (B-I-I) Specific Phobia Affects the Outcome of Hypoxic Challenge Testing. Aerosp Med Hum Perform. 2017 May 01;88(5):503-506. [PubMed: 28417842]
- 9.
Kogan CS, Stein DJ, Maj M, First MB, Emmelkamp PM, Reed GM. The Classification of Anxiety and Fear-Related Disorders in the ICD-11. Depress Anxiety. 2016 Dec;33(12):1141-1154. [PubMed: 27411108]
- 10.
Zwanzger P. [Pharmacotherapy of Anxiety Disorders]. Fortschr Neurol Psychiatr. 2016 May;84(5):306-14. [PubMed: 27299791]
- 11.
Ori R, Amos T, Bergman H, Soares-Weiser K, Ipser JC, Stein DJ. Augmentation of cognitive and behavioural therapies (CBT) with d-cycloserine for anxiety and related disorders. Cochrane Database Syst Rev. 2015 May 10;(5):CD007803. [PMC free article: PMC8939046] [PubMed: 25957940]
- 12.
Tomei C, Lebel S, Maheu C, Lefebvre M, Harris C. Examining the preliminary efficacy of an intervention for fear of cancer recurrence in female cancer survivors: a randomized controlled clinical trial pilot study.
 Support Care Cancer. 2018 Aug;26(8):2751-2762. [PubMed: 29500582]
Support Care Cancer. 2018 Aug;26(8):2751-2762. [PubMed: 29500582]- 13.
van de Wal M, Langenberg S, Gielissen M, Thewes B, van Oort I, Prins J. Fear of cancer recurrence: a significant concern among partners of prostate cancer survivors. Psychooncology. 2017 Dec;26(12):2079-2085. [PubMed: 28317267]
Specific Phobias (Symptoms) | Center for the Treatment and Study of Anxiety
- Symptoms
- Diagnostic Criteria
- Types of Specific Phobia
- Etiology of Specific Phobia
Symptoms
A specific phobia is an intense, persistent, irrational fear of a specific object, situation, or activity, or person. Usually, the fear is proportionally greater than the actual danger or threat. People with specific phobias are highly distressed about having the fear, and often will go to great lengths to avoid the object or situation in question. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the year-long community prevalence estimate for specific phobias is approximately 7%-9%.
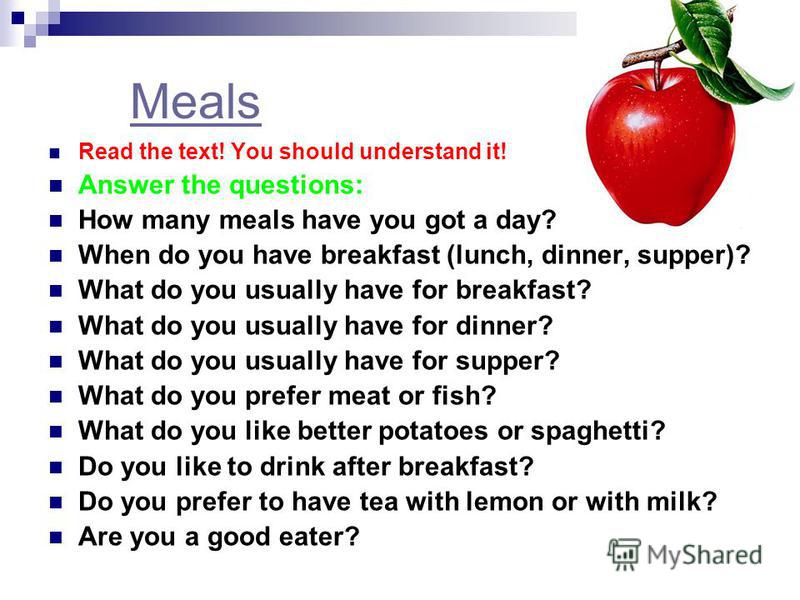
Some examples of phobias:
- A teenager with a dog phobia avoids going to the houses of friends and family who own dogs
- A businessman with a fear of flying loses out on a promotion because he is unwilling to travel
- A woman with a needle phobia avoids getting blood work her primary care physician deemed necessary for her physical health
- A young man with a fear of enclosed spaces takes the stairs each day to his office on the 11th floor to avoid taking the elevator
Note that in the people in the above situations, the presence of the phobia is causing marked distress in their everyday lives.
Back to Top
Diagnostic Criteria
Based on criteria from the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013)
- A persistent fear that is excessive or unreasonable, that occurs by the presence or anticipation of a specific object or situation (e.
 g., flying, heights, animals, receiving an injection, seeing blood).
g., flying, heights, animals, receiving an injection, seeing blood). - Exposure to the feared item or situation almost always leads to an immediate anxiety response, which may take the form of a panic attack. In children, the anxiety may be expressed by crying, tantrums, freezing, or clinging.
- The person recognizes that the fear is excessive or out of proportion to the actual threat posed. In children, this feature may be absent.
- The phobic situation(s) is avoided or else is endured with intense anxiety or distress.
- The avoidance, anxious anticipation, or distress during the feared situation(s) interferes significantly with the person's normal routine, work (or school) functioning, or social activities or relationships, or there is marked distress about having the phobia.
- The fear is persistent, typically lasting for at least six months.
- The anxiety, panic attacks, or avoidance associated with the specific object or situation are not better accounted for by another mental disorder, such as Obsessive-Compulsive Disorder, Posttraumatic Stress Disorder, Separation Anxiety Disorder (e.
 g., avoidance of school), Social Phobia, Panic Disorder, etc.
g., avoidance of school), Social Phobia, Panic Disorder, etc.
Back to Top
Types of Specific Phobia
There are five different types of specific phobia.
- Animal Type (e.g. dogs, snakes, or spiders)
- Natural Environment Type (e.g., heights, storms, water)
- Blood-Injection-Injury Type (e.g. fear of seeing blood, receiving a blood test or shot, watching television shows that display medical procedures)
- Situational Type (e.g., airplanes, elevators, driving, enclosed places)
- Other Types (e.g., phobic avoidance of situations that may lead to choking, vomiting, or contracting an illness; in children, avoidance of loud sounds like balloons popping or costumed characters like clowns)
Specific Phobias versus Normal Childhood Fears
It is important to differentiate between specific phobias and normal childhood fears.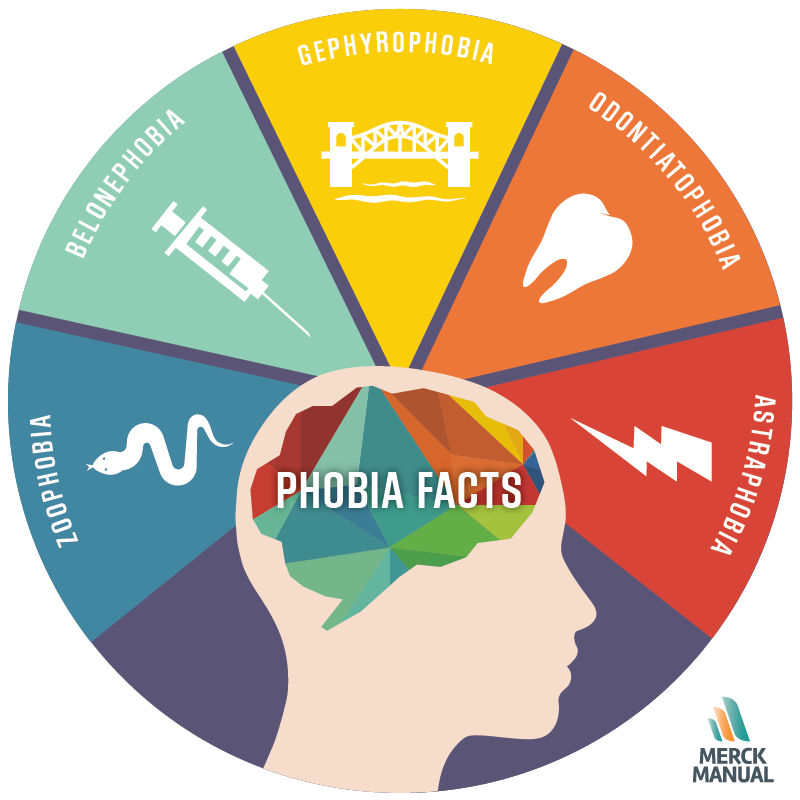 According to the Child Anxiety Network (www.childanxiety.net), some research shows that 90% of children between the ages of 2-14 have at least one specific fear. Not all fears interfere with daily functioning, and do not necessarily merit psychological treatment. Below are some examples of typical childhood and early adolescent fears.
According to the Child Anxiety Network (www.childanxiety.net), some research shows that 90% of children between the ages of 2-14 have at least one specific fear. Not all fears interfere with daily functioning, and do not necessarily merit psychological treatment. Below are some examples of typical childhood and early adolescent fears.
- Infants/Toddlers (ages 0-2 years) loud noises, strangers, separation from parents, large objects
- Preschoolers (3-6 years) imaginary figures (e.g., ghosts, monsters, supernatural beings, the dark, noises, sleeping alone, thunder, floods)
- School Aged Children/Adolescents (7-16 years) more realistic fears (e.g., physical injury, health, school performance, death, thunderstorms, earthquakes, floods)
Back to Top
Etiology of Specific Phobia
As with any psychological disorder, the etiology of specific phobias are complex, and include a number of factors such a learned history, past experiences, and biology.
Learning History
- Direct learning experiences: Specific phobias can sometimes begin following a traumatic experience in the feared situation. For example, a child who is bitten by a dog might develop a fear of dogs, or someone who has a car accident might develop a fear of driving.
- Observational learning experiences: Some people may learn to fear certain situations by watching others show signs of fear in the same situation. For example, a child growing up with a father who is afraid of heights may learn to fear heights himself.
- Informational learning: Sometimes, people develop specific phobias after hearing about reading about a situation that may be dangerous. For example, a person learns to fear flying after watching news footage of 9/11.
However, it is important to remember that learning is not the sole cause of specific phobias. Many people are bitten by dogs or get into car accidents and do not go on to develop phobias.
Biological Factors
Risk factors may include genetic susceptibilities, but not much is known about the biological factors that cause and maintain specific phobias. However, when a person encounters a feared stimulus, many biological changes occur in the body, including changes in brain activity, the release of cortisol, insulin, and growth hormone, and increases in blood pressure and heart rate.
CALDA Program Specific Phobia | The CALDA Clinic
You will get rid of your fears in just one week! This program is indicated and very effective for specific (isolated) phobias.
Specific phobia is an anxiety disorder in which there is a persistent fear of a particular object, place or situation, and the feeling of threat or danger is disproportionate to the fear-causing factor. The patient by all means tries to avoid a situation that causes fear. If this fails, an immediate and uncontrollable fear reaction occurs, which can develop into a panic attack. These irrational fears and reactions have a devastating effect on a person's social and professional life.
Weekly program cost per patient: CHF 130,000.00 fr.
Diagnosis and Therapy
Diagnosis
In psychiatric diagnosis, we determine your mental status, collect your personal and social history (medical history), as well as addiction and family history.
After this comprehensive diagnosis, we will offer you an individual treatment plan.
Therapy
Neuroscientists have confirmed the presence of abnormal hyperactivation in response to danger in patients with phobias. Cognitive Behavioral Therapy has proven effective in reducing the intensity of response to threats. You need to start with her. Another effective form of therapy is immersion in sensu (in the processes occurring only in the imagination), which is a form of desensitization. With its help, you will be able to cope with fear in a safe environment.
The combination of these methods is the most effective way to treat specific phobias.
A personal coach will live with you around the clock throughout the therapy. The therapeutic program is designed for six to eight hours a day, seven days a week and consists of the following blocks.
Psychiatry and psychotherapy
- Management of fears.
- Diagnostics.
- Intensive psychotherapy with in vivo and in sensu immersion (cognitive behavioral therapy, virtual reality therapy: desensitization and processing through eye movement, clinical hypnosis).
- Psychological self-help training.
- Stress management.
Orthomolecular medicine
- Amino acids, minerals and vitamins from day one.
- Personal coach for personal growth.
Alternative and alternative medicine
Along with classical academic medicine, there are a number of traditional medical and therapeutic methods. As supporters of integrative medicine, we have complemented our range of interventions with proven and successful methods of alternative and alternative medicine.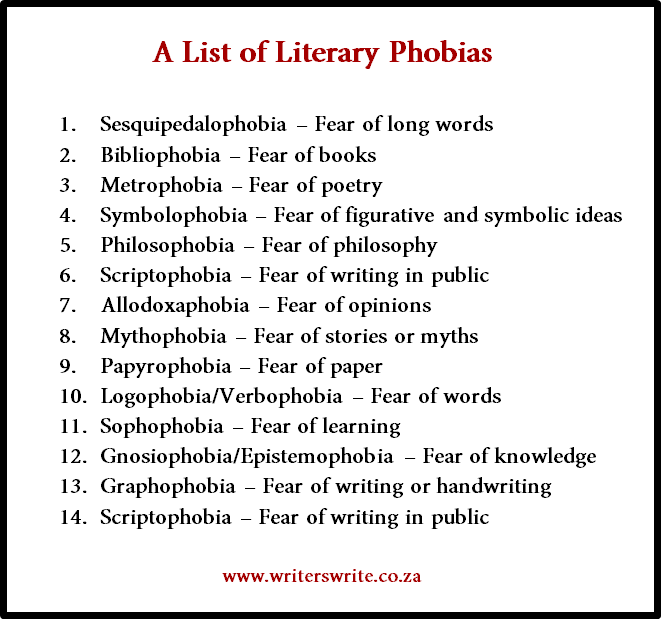 The most successfully used elements of treatment are listed below.
The most successfully used elements of treatment are listed below.
- Acupressure, acupuncture.
- Alpha stimulation.
- Manual therapy.
- Meditation and nonjudgmental conscious observation.
- Training with a personal trainer.
- Yoga.
Residences
In our luxurious private residences you can escape from everyday worries, relax and undergo a treatment in a peaceful environment. The price includes a full range of services, including butler, chef and limousine service.
You can find more information about our residences here.
Cost
The cost per week of the CALDA Specific Phobia program for one patient is CHF 130,000.00. fr. in Week.
The price does not include hotel accommodation, medical services from other institutions and post-rehabilitation programs.
Always ready to answer your questions
CALDA program Specific phobia PDF
Amyotrophic lateral sclerosis specific phobia: Alsphobia
Specific phobias account for about 12. 5% in the structure of affective disorders [1, 3, 4]. These include nosophobia, for example, cancerophobia (fear of getting cancer), etc. In this paper, the phobia of amyotrophic lateral sclerosis (ALS) is described for the first time and its name “alsphobia” (from the English amyotrophic lateral sclerosic – ALS) is proposed.
5% in the structure of affective disorders [1, 3, 4]. These include nosophobia, for example, cancerophobia (fear of getting cancer), etc. In this paper, the phobia of amyotrophic lateral sclerosis (ALS) is described for the first time and its name “alsphobia” (from the English amyotrophic lateral sclerosic – ALS) is proposed.
As is known, ALS is a progressively developing disease ending in death. This determines the development of a phobia on the basis of obtaining information about this disease.
The literature contains the work of A. Hentali et al. [2], which mentions the possibility of developing an anxiety disorder in relatives of ALS patients who were informed of the results of medical genetic counseling, but does not indicate whether they had a phobia or affective disorders. The authors also conducted a selective survey of foreign ALS specialists, but none of them indicated that they had met the phobia that interested the researchers.
In this article, alsophobia is described in a group of people living in Russia, who are mentally and somatically healthy, or who had a history of phobias.
In all patients, a phobia developed after receiving information about the symptoms of ALS with subsequent extrapolation of this information to their own interoceptive sensations, which were transformed as hypochondriacal fixation developed into pathological bodily sensations with an obsessive coloring of psychopathological affect.
Material and methods
In the period from 2006 to 2012, 21 patients with phobia were observed, 11 men and 10 women aged 28-72 years. Among them were relatives of patients with ALS - 3, neurologists - 4, persons informed about ALS from different sources - 14, with a history of aggravated mental illness was 5 (23%) people. All of them underwent a neurological examination and 17 were assessed using the Hamilton Depression Scale ( US -D).
Statistical analysis of quantitative indicators was carried out using the Mann-Whitney test (BIOSTAT statistical software package (Hungary, 1999).
Results
The clinical picture of alsphobia was represented by an obsessive sensation of generalized muscle twitches - in 21 (100%) people, general weakness - in 14 (66. 6%), fatigue during prolonged walking or talking - in 6 (28.5%), muscle pain - in 2 (9.5%), hoarseness - in 2 (9.5%).5%), subjective feeling of lack of air (more often in stuffy rooms) with a transient impairment of sensitivity (hyperventilation syndrome) - 1 (4.7%).
6%), fatigue during prolonged walking or talking - in 6 (28.5%), muscle pain - in 2 (9.5%), hoarseness - in 2 (9.5%).5%), subjective feeling of lack of air (more often in stuffy rooms) with a transient impairment of sensitivity (hyperventilation syndrome) - 1 (4.7%).
The mental status of patients with alsphobia was characterized by obsessive thoughts about the presence of ALS, an obsessive desire to conduct more and more new examinations, anxiety, sleep disturbances of varying severity.
In 5 patients with a burdened psychiatric history, there were repeated visits to psychiatrists both in the past and after the diagnosis of the syndrome, while one patient was diagnosed in the past with neuroleptic-induced oromandibular dyskinesia. 8 patients with somatic somatic alsphobia had L5 root neurinoma, distal myopathy, spinal osteochondrosis and L5-S1 root radiculopathy, diabetic polyneuropathy, Guyon's tunnel syndrome, carpal tunnel syndrome, dysfunction of the temporomandibular joint, Melkersson-Rosenthal syndrome.
At the time of the study, the duration of phobia symptoms was 3 ± 1.4 months, while 5 (28.5%) patients had already done needle electromyography 1 or 2 times, 6 (23.5%) - it was done to exclude ALS after consultation (in both cases no signs of ALS were found), 10 (47.6%) patients did not undergo this procedure, because the patients were dissuaded by the doctor in its expediency.
In 10 cases, the severity of the phobia was assessed as mild (patients succumbed to dissuasion and demonstrated the presence of criticism, a score of US -D 1-10), in 6 - as moderate (when patients succumbed to only partial dissuasion, but at the same time agreed to cooperate, score according to US -D 11-20), in 5 - as severe (patients did not succumb to dissuasion and / or refused to cooperate with the doctor, a score for US -D more than 21).
Among relatives of patients with ALS, a mild disorder occurred in 2 cases and of moderate severity in 1; among neurologists (3 of 4 had a burdened mental history), 1 mild, 1 moderate and 2 severe disorders were observed. The phobia was iatrogenic in 2 patients.
The phobia was iatrogenic in 2 patients.
The duration of phobic symptoms was significantly higher in patients with severe and moderate phobia than in mild ones (1.5±0.6 and 5.0±1.1 months; p<0.05).
In the course of a psychotherapeutic conversation, 17 patients agreed to receive treatment with the use of psychotropic drugs for 3 months. For mild alopecia, a thymoleptic, an antidepressant, and an adaptogen or hypnotic were prescribed; for a moderate disorder, a thymoleptic, an adaptogen, or a hypnotic, an antidepressant, and an atypical neuroleptic; sleeping pills.
At the beginning of the observation, the indicator NAM -D in 17 people was 17±4 points. Each patient was asked to complete this scale 1 month and 3 months after treatment. Among those who refused to complete the scale after 1-3 months were all patients with severe phobia.
Later, six months later, each patient was interviewed about the mental state by phone and/or e-mail. In 7 (33.3%) patients, symptoms persisted to some extent. Dynamics of scale indicators HAM -D in patients with alsphobia on the background of treatment with psychotropic drugs was as follows: at the initial examination (n=17) - 17±4 points, after 1 month (n=13) - 8±2 points, after 3 months (n= 11) - 3 ± 1. Thus, after 1 month, the indicator HAM -D decreased by an average of 50% in 76.4%, and after 3 months it again decreased by 50% in 64% of patients. It should be noted that in 6 patients who dropped out of the study due to refusal of observation, re-filling the scale and treatment, the initial score of HAM -D was significantly higher than in patients who underwent a three-month course of treatment - they had 22±3 and 14±4 points, respectively (p<0.05). At the same time, the former more often motivated the refusal of further observation by the fact that the drugs did not help them, rather than by the fact that there was no need to fill in the scale. Thus, the proven therapeutic effect after 3 months was achieved only in 11 (52.
In 7 (33.3%) patients, symptoms persisted to some extent. Dynamics of scale indicators HAM -D in patients with alsphobia on the background of treatment with psychotropic drugs was as follows: at the initial examination (n=17) - 17±4 points, after 1 month (n=13) - 8±2 points, after 3 months (n= 11) - 3 ± 1. Thus, after 1 month, the indicator HAM -D decreased by an average of 50% in 76.4%, and after 3 months it again decreased by 50% in 64% of patients. It should be noted that in 6 patients who dropped out of the study due to refusal of observation, re-filling the scale and treatment, the initial score of HAM -D was significantly higher than in patients who underwent a three-month course of treatment - they had 22±3 and 14±4 points, respectively (p<0.05). At the same time, the former more often motivated the refusal of further observation by the fact that the drugs did not help them, rather than by the fact that there was no need to fill in the scale. Thus, the proven therapeutic effect after 3 months was achieved only in 11 (52.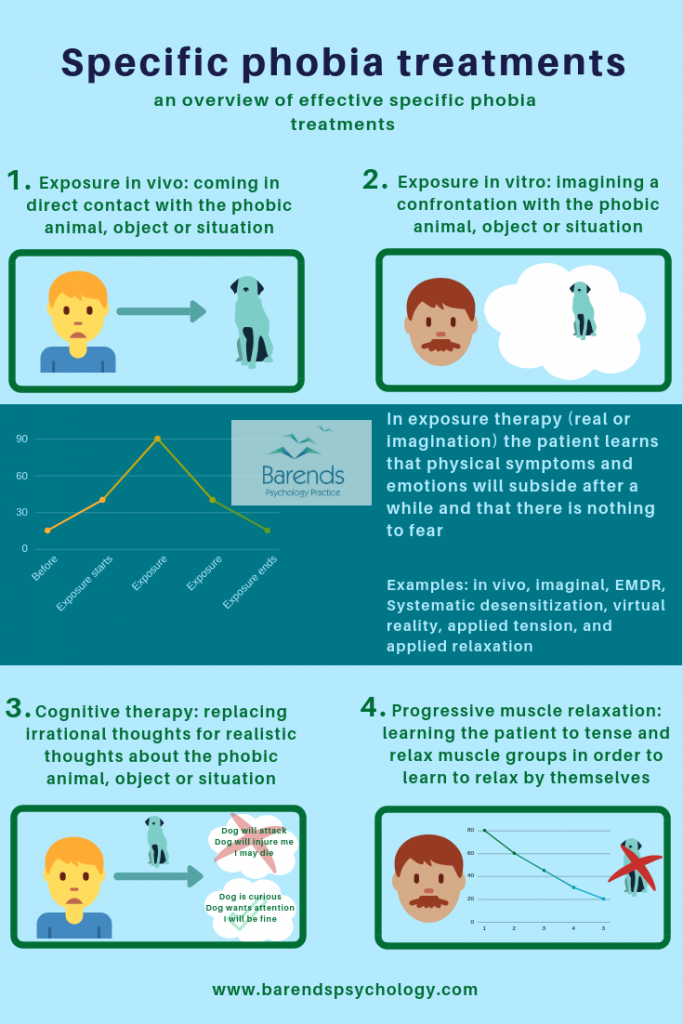 4%) patients. Deactualization of the phobic affect in about 17% of patients was observed even after the end of treatment. After a telephone survey six months later, 7 (33.3%) of 21 patients had symptoms in the form of a persistent sensation of generalized muscle twitches in different parts of the body and general weakness, while 5 of them had a burdened mental anamnesis.
4%) patients. Deactualization of the phobic affect in about 17% of patients was observed even after the end of treatment. After a telephone survey six months later, 7 (33.3%) of 21 patients had symptoms in the form of a persistent sensation of generalized muscle twitches in different parts of the body and general weakness, while 5 of them had a burdened mental anamnesis.
As examples of the described phobia, we give two of our own observations.
Observation 1
Patient K., aged 53, director of a company, complained of twitching in the calves, pain in the lower back and fatigue in the legs when walking and climbing stairs. Stimulation electroneuromyography revealed signs of mild demyelinating sensorimotor polyneuropathy of the lower extremities and radiulopathy of the left peroneal nerve. He was referred for evaluation to rule out ALS.
Neurological examination revealed decreased Achilles reflexes; fasciculations and muscle hypotrophy were not detected; slight hypoesthesia of the lateral margin of the left foot was noted. Needle electromyography showed no signs of current denervation and reinnervation. There were signs of chronic venous insufficiency of the lower extremities, which were later confirmed by Doppler ultrasound. According to US -D - 12 points.
Needle electromyography showed no signs of current denervation and reinnervation. There were signs of chronic venous insufficiency of the lower extremities, which were later confirmed by Doppler ultrasound. According to US -D - 12 points.
The patient was explained that he has osteochondrosis of the spine, radiculopathy of the left peroneal nerve, as well as chronic insufficiency of the veins of the lower extremities without signs of ALS. He agreed, but then asked several questions, from which it was clear that he doubted the correctness of the diagnosis.
The patient was recommended treatment with detralex 500 mg 2 times a day and thiogamma 600 mg 1 time a day for 2 months.
A month later, the twitching in his legs continued to bother him, and insomnia developed. The patient always thought that he had ALS. He stopped coping with work duties, took a vacation and turned to a psychiatrist, whom he told that he had abused alcohol 2 years ago. The EEG showed irritation of the mesodiencephalic structures of the brain.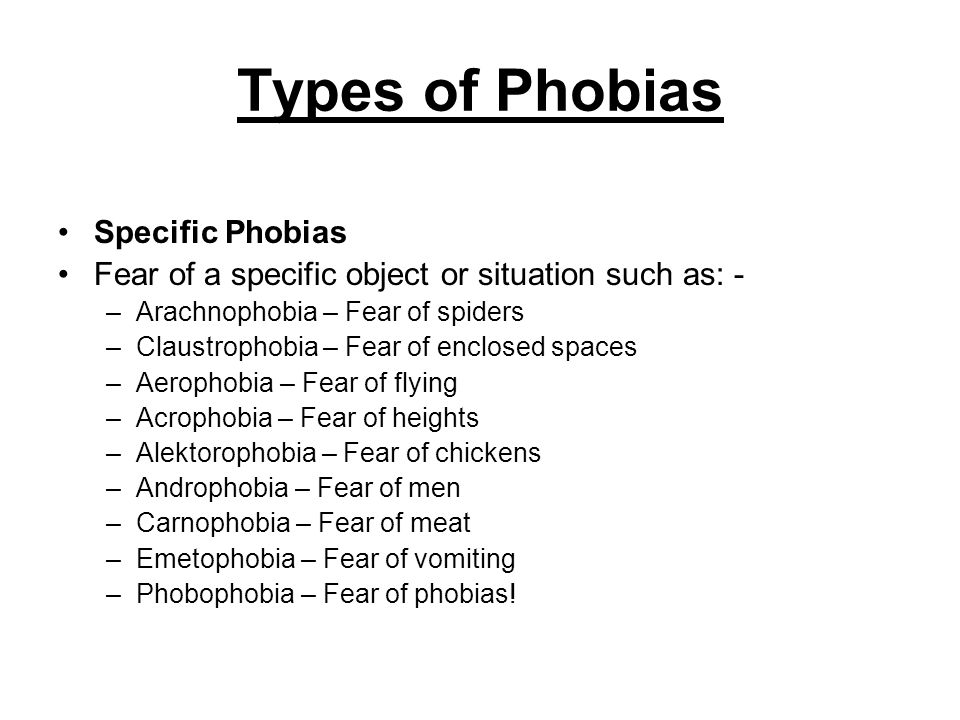 Topiramate 25 mg twice a day, tiapridal 100 mg in the morning and evening, pyrazidol 25 mg in the morning and afternoon, and imovan 7.5 mg at night were prescribed. The symptoms persisted for 3 months and the patient continued to think about the possibility of developing ALS due to twitching in the legs (score US -D during this period was 5 points). After 6 months the symptoms stopped.
Topiramate 25 mg twice a day, tiapridal 100 mg in the morning and evening, pyrazidol 25 mg in the morning and afternoon, and imovan 7.5 mg at night were prescribed. The symptoms persisted for 3 months and the patient continued to think about the possibility of developing ALS due to twitching in the legs (score US -D during this period was 5 points). After 6 months the symptoms stopped.
Observation 2
Patient P., aged 29, manager, together with her sister took part in the care of her mother, suffering from moderately progressive ALS with a cervical debut. The patient received Rilutek and non-invasive ventilation.
At the first examination complained of twitching in the tongue, insomnia and anxiety. Indicator US -D was 15 points.
Electromyography revealed no pathology, but the doctor advised to test for thyroid hormones, which turned out to be normal. The neurological examination also revealed no pathology. Mental status: the patient is emotionally labile, she expressed thoughts that she had familial ALS. It was explained to her that she had no evidence of the onset of ALS, and she was advised to take medication to improve sleep and reduce anxiety. The psychiatrist prescribed carbamazepine 100 mg twice daily, sulpiride 50 mg twice daily, fluvoxamine 100 mg, and nitrazepam 5 mg at night.
It was explained to her that she had no evidence of the onset of ALS, and she was advised to take medication to improve sleep and reduce anxiety. The psychiatrist prescribed carbamazepine 100 mg twice daily, sulpiride 50 mg twice daily, fluvoxamine 100 mg, and nitrazepam 5 mg at night.
After 3 months, she again visited a psychiatrist and said that she began to sleep peacefully 3 weeks after starting the drugs, the “bad thoughts” were gone, but sometimes she still feels twitching in her tongue, and this makes her nervous. The HAM-D index decreased to 8. However, the patient still insisted on repeating the electromyography and conducting a genetic study for familial ALS. The dose of sulpiride was increased to 250 mg per day. After 6 months, she reported that her tongue twitches had stopped, descriptions of ALS had disappeared, which corresponded to a score of 9.0108 US -D - 1.
Talk
The results of the present study make it possible to include Alsphobia in the list of anxiety disorders (nosophobias) related to specific phobias.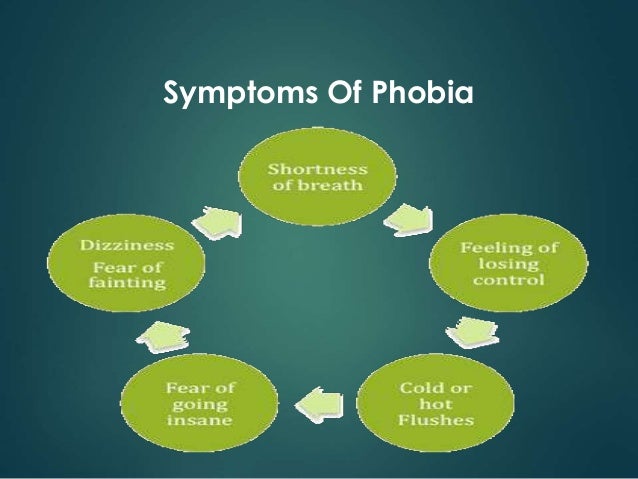 This is indicated by a specific history, primary indicators HAM -D and the fact of regression of phobic symptoms after treatment with psychotropic drugs in 52.4% of patients. Since in 77% of patients the anamnesis was not burdened with mental illness, this indicates the primary nature of the phobia. It should be noted that in the present study, patients with alsphobia were relatives of ALS patients only in 14.3% of cases.
This is indicated by a specific history, primary indicators HAM -D and the fact of regression of phobic symptoms after treatment with psychotropic drugs in 52.4% of patients. Since in 77% of patients the anamnesis was not burdened with mental illness, this indicates the primary nature of the phobia. It should be noted that in the present study, patients with alsphobia were relatives of ALS patients only in 14.3% of cases.
As mentioned above, the treatment was successful in 52.4% of cases, the remaining patients only partially made contact with doctors. The severity of the phobia correlated with the duration of the symptoms (r= -0.5; p=0.004). The tactics of dissuasion in mild and some moderate cases of alsophobia as part of a psychotherapeutic conversation probably played a positive role in the management of patients, and therefore we recommend that ALS specialists adhere to such tactics in all cases of alsophobia and recommend in moderate cases a psychiatrist's consultation and the use of a scale US -D.