Why does anxiety cause diarrhea
Link, treatment, and when to see a doctor
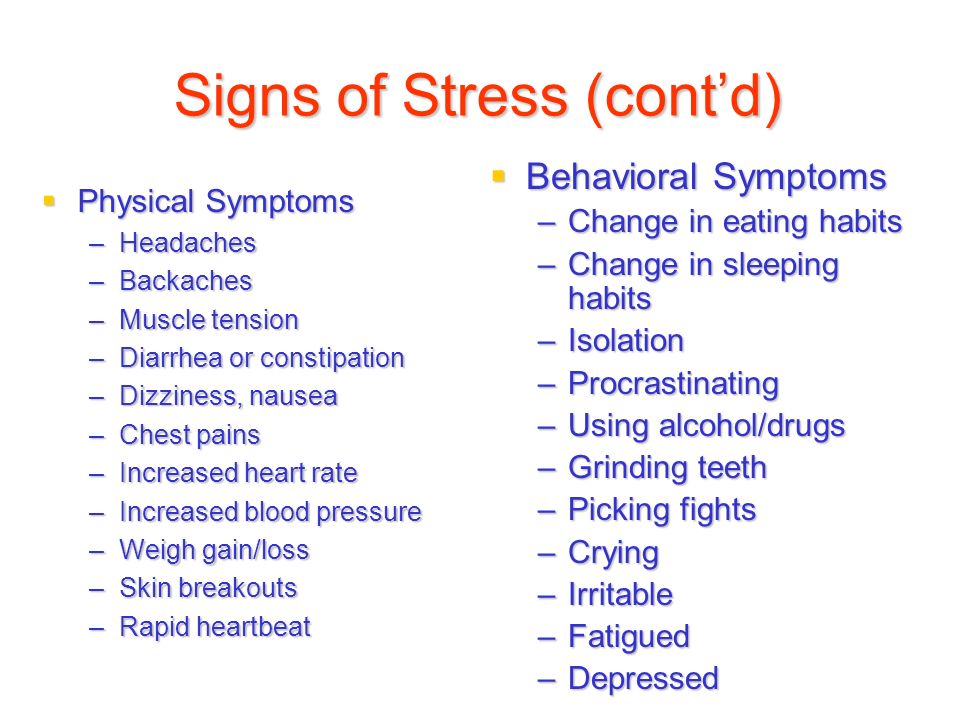
As well as affecting how a person feels mentally, anxiety can also have physical effects. A common physical manifestation of anxiety is stomach upset, including diarrhea or loose stools.
Some people believe that how a person feels can influence the way in which their stomach and intestines behave, potentially causing symptoms that include diarrhea.
Sometimes, diarrhea is a chronic condition for a person. In other cases, it is an acute response to profound anxiety, which means that it occurs once or for a limited time.
In this article, we look at why anxiety can cause diarrhea, the possible association with irritable bowel syndrome (IBS), and how a person can treat diarrhea.
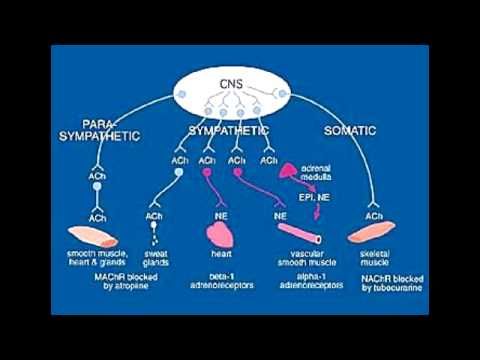
There is a connection between the gut and the brain called the “gut microbiota-brain axis.” This bidirectional network between a person’s brain and the gut microbiota allows the brain to affect gut movement.
According to the Anxiety and Depression Association of America (ADAA), when a person is anxious, the body releases hormones and chemicals. These can enter the digestive tract and disrupt the gut flora, which can result in a chemical imbalance that leads to diarrhea.
A study involving people with IBS with diarrhea (IBS-D) found that the participants who also had anxiety had higher levels of certain inflammatory compounds in the body than those who did not.
Specifically, the researchers found that those with anxiety had higher levels of a compound called interleukin-1 beta. This compound can alter the intestine’s protective barrier, which can cause pain and affect the intestine’s ability to absorb water and sodium. Diarrhea can be the result of these effects.
Another possible explanation for anxiety and its effects on diarrhea is that anxiety alters how the brain processes information from the visceral nerves (those present in the stomach and intestines). According to an article in The Lancet, anxiety may cause the brain to process messages from the stomach as indicating pain or that the intestinal movement needs to speed up.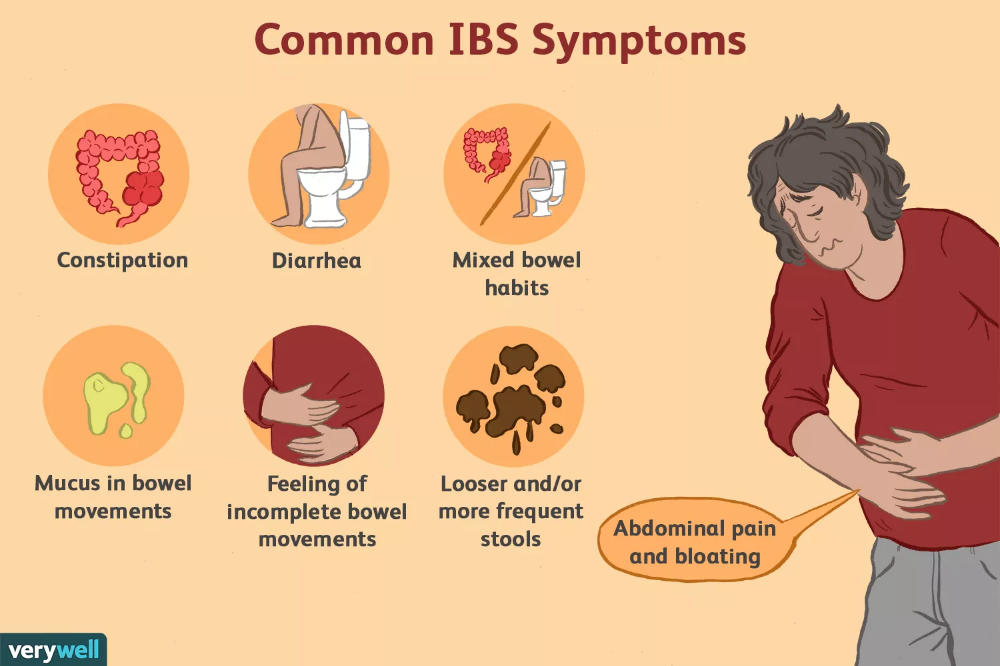
The result can be gastrointestinal dysfunction that makes the stomach and intestines feel as though they are churning. This dysfunction causes digested food to move along the intestinal tract more quickly, resulting in diarrhea.
IBS-D is a condition that can cause a person to experience the following symptoms routinely:
- abdominal pain or discomfort
- bloating
- frequent diarrhea episodes
Although many doctors do not believe that anxiety is a direct cause of IBS-D, anxiety may worsen a person’s symptoms.
An estimated 75% of people with IBS experience anxiety and depression. Chronic diarrhea not only affects the nutrients that a person’s body absorbs from their food but can also lead to dehydration and fatigue.
Having IBS-D can also worsen a person’s anxiety. They may start to fear that they will have a diarrhea episode in public. This worry can cause them to change their behavior and feel anxious.
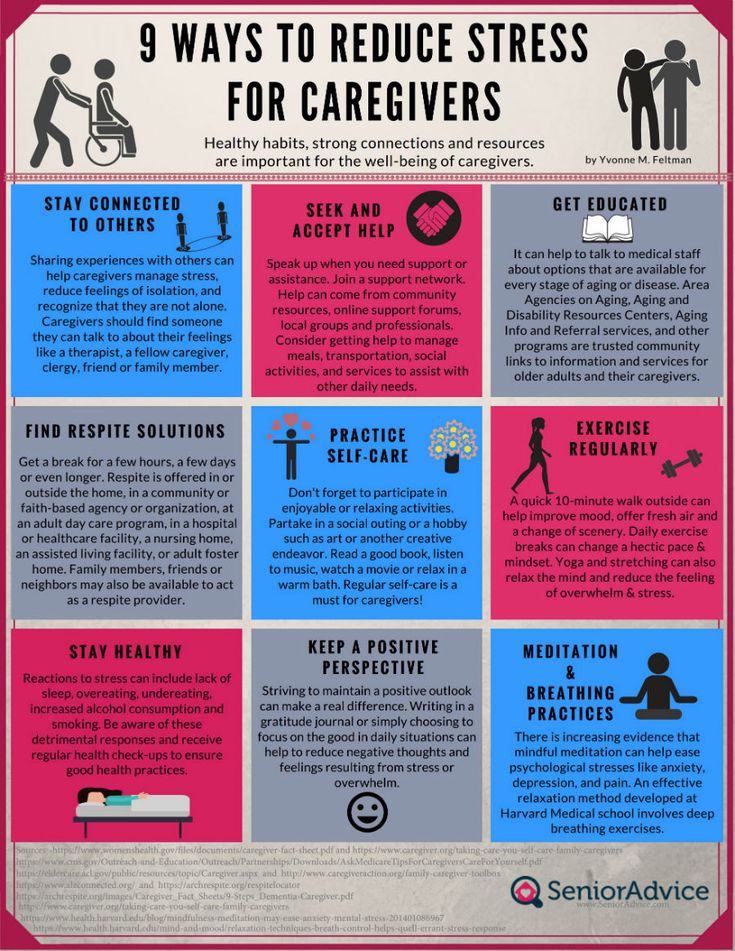
If anxiety is the underlying cause of diarrhea, minimizing anxiety may help reduce symptoms.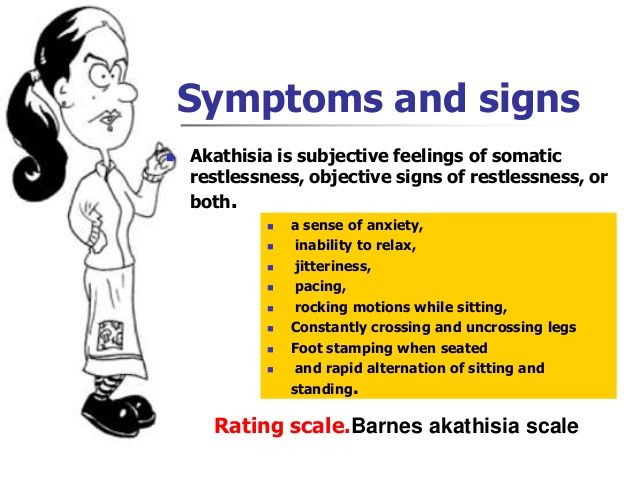
Examples of treatments and remedies that may help include:
- Avoiding foods that may contribute to stomach upset: A person should avoid consuming caffeine, spicy foods, and foods containing lactose.
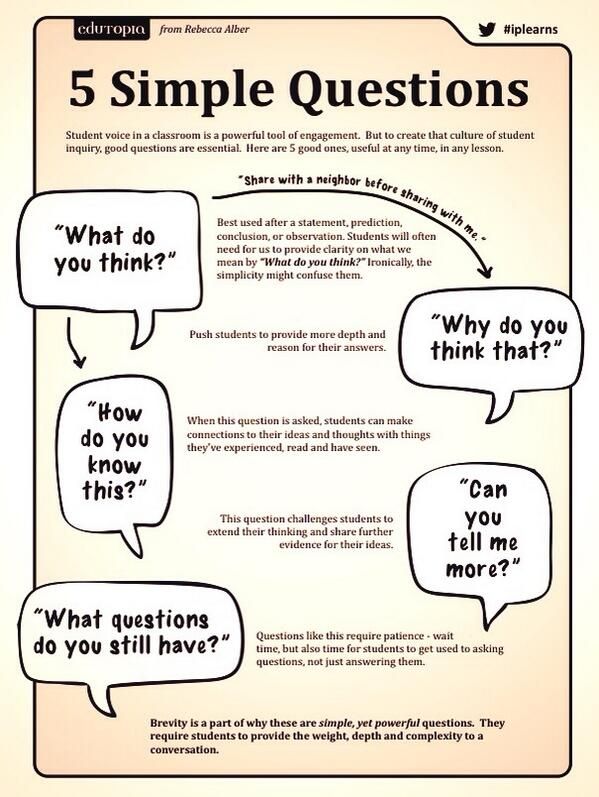
- Psychotherapy: Talk therapy can help a person identify anxiety and learn techniques to manage and reduce it. Therapists may use approaches such as mindfulness and cognitive behavioral therapy (CBT).
- Complementary health: Stress-relieving and relaxation techniques can help a person feel better. Examples include meditation, yoga, tai chi, and acupuncture. Hypnotherapy may help reduce symptoms of stomach upset, bloating, and stomach pain in those with IBS, according to an article in the journal Clinical and Translational Gastroenterology.
According to the ADAA, a person can reduce anxiety and stress by taking short breaks to breathe deeply for 1 minute at a time throughout the day. A person should breathe slowly through the nose and let the stomach inflate. As they exhale, they should let their stomach deflate.
As they exhale, they should let their stomach deflate.
Over time, a person may see a reduction in their symptoms.
Doctors may also prescribe medications to treat diarrhea. Examples of these medications include:
- Antidiarrheals: Medications such as loperamide (Imodium) may help reduce the incidence of diarrhea.
- Antispasmodics: These medications reduce the frequency of contractions in the muscles in the intestines. As a result, the stool does not move through the intestines as quickly. Doctors may prescribe medications such as hyoscyamine (Levsin) and dicyclomine (Bentyl) to help.
- Bile acid sequestrants: These medications can bind to extra bile in the intestine that may otherwise lead to diarrhea. An example is cholestyramine (Questran).
- Alosetron hydrochloride: The Food and Drug Administration (FDA) have approved a medicine called alosetron hydrochloride (Lotronex) to treat IBS in females whose primary symptom is diarrhea.
 Females are more likely to experience IBS symptoms than males, according to the ADAA.
Females are more likely to experience IBS symptoms than males, according to the ADAA.
Over-the-counter supplements, such as fiber or probiotics, may also help. A person should always speak to their doctor before they start taking these medications. The doctor can ensure that the product does not interfere with any other medicines that the person may be taking or affect any underlying health conditions.
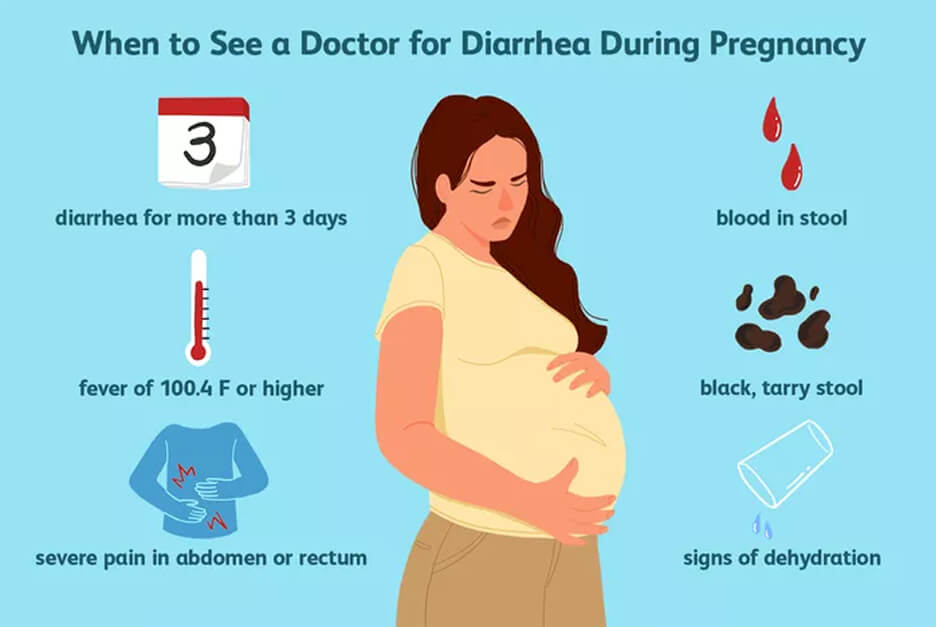
A person should see their doctor if they have diarrhea for 2–4 weeks without an underlying illness (such as a bacterial or viral infection) causing it.
Other symptoms that indicate that a person may need to see a doctor include:
- blood in the stool
- fatigue
- unexplained weight loss
A doctor can perform testing to determine the underlying cause of chronic diarrhea.
In addition to IBS-D, inflammatory bowel disease and celiac disease are possible underlying causes.
Anxiety can lead to unnecessary worry and stress that manifests itself in a number of ways, including stomach upset that causes diarrhea.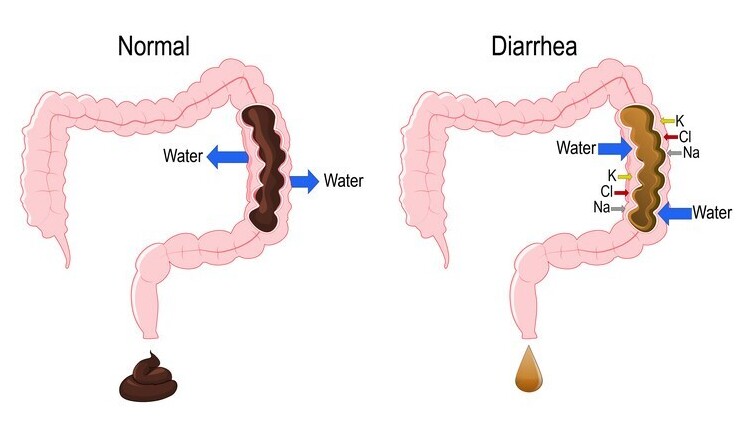
If a person’s diarrhea turns into a frequent, chronic occurrence, they should seek medical treatment.
There are medications and at-home methods to manage anxiety and reduce the physical stomach symptoms that can accompany it.
Why It Happens and How to Manage It
Anxiety is a mental health condition that has a wide range of symptoms. It can involve long-term patterns of significant worry, nervousness, or fearfulness. For many people, it can also cause physical symptoms.
If you tend to get diarrhea around stressful or anxiety-producing situations and events, you’re not alone. It’s fairly common to experience stomach troubles with anxiety. For some, worrying about having diarrhea in public or an unfamiliar location adds to existing anxiety.
But it’s possible to manage this symptom and reduce its impact on your life. Read on to learn more.
Diarrhea, along with other digestive problems that often accompany anxiety, can happen because of the connection between your gut and your brain, known as the gut-brain axis.
The axis connects your central nervous system to your enteric nervous system (ENS), which acts as your gut’s nervous system. The ENS helps regulate processes in your gastrointestinal (GI) tract. But it also has an effect on your emotions and behavior through its link to your brain.
When you’re distressed, chemical messengers carry signals from your brain to your gut. Your gut sometimes responds to these signals with physical symptoms, including diarrhea, nausea, or constipation.
This link works both ways. If you have digestive issues or other GI problems, you might experience psychological symptoms. And having irritable bowel syndrome (IBS) or related conditions is linked to an increased risk for anxiety and other mood symptoms.
If you regularly get diarrhea while in distress, it might be worth ruling out IBS. This common condition can make you more likely to experience diarrhea when you feel anxious.
Experts aren’t sure exactly what causes it. But anxiety and stress are known triggers for IBS flare-ups.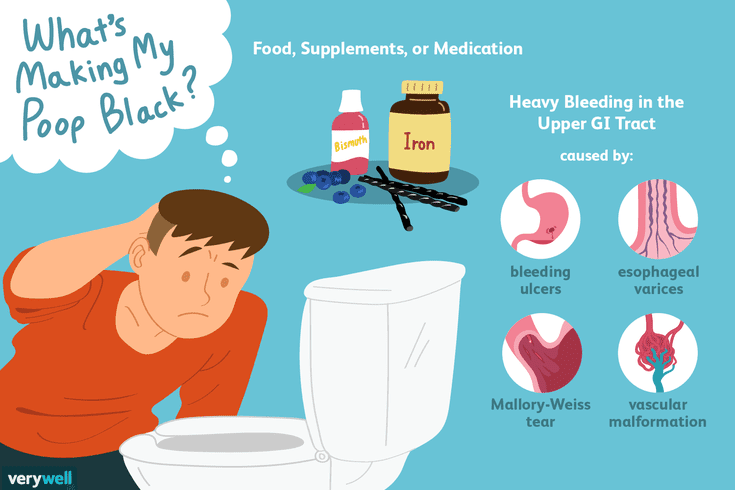
Some experts believe people who develop IBS may have an overly sensitive colon. This sensitivity can increase the chance you’ll have GI symptoms when you eat specific foods or experience anxiety or other emotional distress.
Many people have both anxiety and IBS. In fact, research consistently suggests that IBS commonly co-occurs with anxiety and depression. Living with either condition can increase your risk for the other and affect symptoms you already have.
In other words, just as you might experience increased GI distress as a result of anxiety, living with IBS can worsen mood and emotional symptoms.
know the signsCommon signs of IBS include:
- pain and discomfort in your abdomen that doesn’t go away or keeps coming back
- stomach cramps
- increased gas
- diarrhea, constipation, or alternating diarrhea and constipation
- symptoms that get worse when you smoke, have a lot of caffeine, or eat certain foods, including dairy, red wine, or wheat, among others
If you have these symptoms for three months or longer, you could have IBS.

Getting help for anxiety can make a big difference in both mental and physical symptoms. Talking to a mental health professional is a good first step.
A therapist can help you find the treatment that best fits your needs, whether it’s therapy or a combination of therapy and medication. Some people who experience GI symptoms and anxiety or depression find that antidepressants help with both sets of symptoms.
Certain lifestyle changes could also help you manage symptoms of anxiety. Some tips that may be especially helpful for diarrhea and other stomach issues include:
- avoiding alcohol and tobacco
- decreasing caffeine intake
- staying hydrated
- eating a balanced diet that includes whole grains, lean protein, and fruits and vegetables
- getting regular exercise
It’s also important to know how to cope with anxiety and stress as you experience it. If you’re working with a therapist, they can help you explore coping methods.
quick fixesWhen you start to feel your stomach knot up (or before you even experience the first twinge), the following strategies can help:
- Take a few minutes to breathe. Slow, deep breathing can help reduce anxiety and may calm your stomach.
- Take a short, brisk walk.
- If you can’t get outside, try some indoor stretches, yoga, or meditation.
- Take a moment for self-compassion. What would you tell a loved one facing the same stressful situation? Say those same words to yourself.
- Try a relaxation exercise.
- Reach out to a loved one. Hearing from someone you care about can remind you of the support in your life and help make difficult situations seem less challenging.
- Try a grounding technique. If anxiety tends to make it hard to focus on what’s happening around you, grounding techniques can help calm you and keep you present.
On a larger scale, it may also help to take inventory of your daily tasks, both at home and at work. If they feel overwhelming, set aside time to go over your responsibilities. Ask yourself if they’re essential, or if there’s anything that’s adding unnecessary stress to your life.
If they feel overwhelming, set aside time to go over your responsibilities. Ask yourself if they’re essential, or if there’s anything that’s adding unnecessary stress to your life.
Can increased self-care or division of responsibilities reduce your load? Sometimes, taking a careful look at everything you’re dealing with can help you find new ways to address challenges. If possible, involve a trusted co-worker or loved one in the process.
Talking to a medical professional may help if you experience both anxiety and digestive issues, but it’s a good idea to see your healthcare provider if lifestyle changes don’t seem to improve your symptoms.
You may also want to make an appointment if:
- symptoms get worse or don’t go away after several weeks
- you get diarrhea during the night
- you have bloody stools
- bowel movements and gas don’t relieve your pain or cramping
- it’s hard to swallow
- you experience weight loss
- you vomit for no clear reason
A medical professional can help determine what’s causing your symptoms and offer suggestions for treatment, including any dietary changes that may help relieve symptoms.
Talking to a therapist is recommended if any symptoms negatively affect your quality of life. For example, feelings of fear and worry may affect your relationships, work, and school. They might also make it hard to sleep or do the things you’d normally do.
Concerned about the cost of therapy? Our guide to affordable therapy can help.
Alarm again? We tell you what to do to reduce anxiety
T
BEAUTY•Healthy lifestyle
TEXT: Yana Karimova
Everyone experiences anxiety, anxiety and fear at certain moments. But sometimes they literally interfere with life - then we are talking about pathological anxiety or an anxiety disorder. The Blueprint tells you how to recognize them.
What are anxiety disorders?
Is any anxiety a disorder?
In psychiatry, a group of disorders associated with increased feelings of anxiety and fear - and the resulting behavioral abnormalities. According to WHO, 264 million people suffered from anxiety disorders in 2015. According to some studies, these are the most common mental disorders (at least in the US).
According to some studies, these are the most common mental disorders (at least in the US).
This category includes generalized anxiety disorder, panic disorder, specific phobias, social anxiety disorder, post-traumatic stress disorder, and others. Individuals with specific phobias usually know the cause of their anxiety—for example, in the case of agoraphobia, anxiety is exacerbated when the person is in open spaces. But generalized anxiety disorder is easy to overlook: anxiety is not directed at anything in particular, and there can be almost more physiological symptoms than psychological ones.
No. Alisa Plyaskina, a psychologist at the HSE Center for Psychological Counseling, explains: “Some people are more sensitive and perceive different situations more vividly and emotionally, including with greater anxiety. This does not make them the owners of an anxiety disorder - just such a personality trait, it is within the normal range.
Does such a person need to see a specialist? Yes, if he does not cope with his experiences and emotions, does not enjoy life, cannot perform some usual daily activities or important life tasks for him - related, for example, to work or relationships.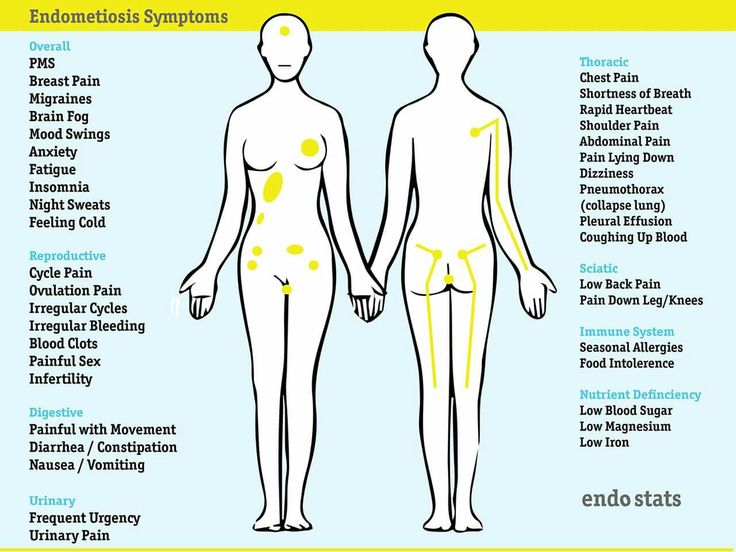
Plyaskina clarifies that increased anxiety can be situational. That is, it can manifest itself in response to an unstable social or economic environment, life changes, or very intensive long-term work. Anything that increases excitability increases anxiety.
Your body is malfunctioning
You are constantly on edge
You get tired more easily than usual
You have some pain
You have trouble sleeping
Click on the symptoms to read more
How do you know if your anxiety is most likely generalized anxiety disorder?
You can’t stop worrying
Your body is scared even when you don’t
It’s hard for you to work and relax
All this ruins your life
You can’t stop worrying fine. But anxiety disorder makes you constantly worry about the most ordinary things: household and work responsibilities, health, finances, or the prospect of being late for work.
At the same time, anxiety is clearly disproportionate to its cause.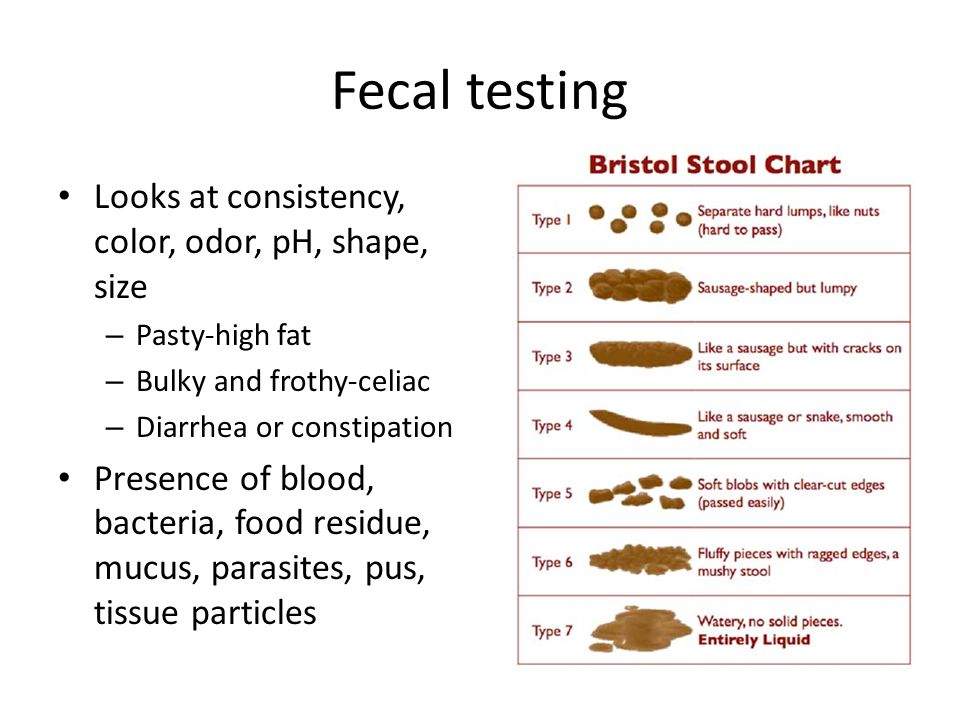 For example, not having time to get into a subway car seems to be no less frightening prospect than missing a plane. You cannot cope with this emotion: you postpone, reschedule or cancel things because of anxiety. Anxiety spreads to different areas of your life: you feel it at work, at home, and with friends. It does not pass for at least six months. Another sign is an unreasonable feeling that something terrible is bound to happen soon.
For example, not having time to get into a subway car seems to be no less frightening prospect than missing a plane. You cannot cope with this emotion: you postpone, reschedule or cancel things because of anxiety. Anxiety spreads to different areas of your life: you feel it at work, at home, and with friends. It does not pass for at least six months. Another sign is an unreasonable feeling that something terrible is bound to happen soon.
Are you constantly on edge? Looks like a few more signs of an anxiety disorder. According to studies, many patients with this diagnosis noticed increased irritability and restlessness.
You get tired more easily than usual
Sometimes fatigue has simple reasons - maybe you haven't been on vacation for a long time. But if you get tired quickly or just feel tired all the time, it could be due to elevated levels of the hormone cortisol, insomnia, or chronic pain — the three companions of anxiety.
It is difficult for you to work and rest
Anxiety disorders affect the efficiency at work: they reduce the ability to concentrate and affect short-term memory.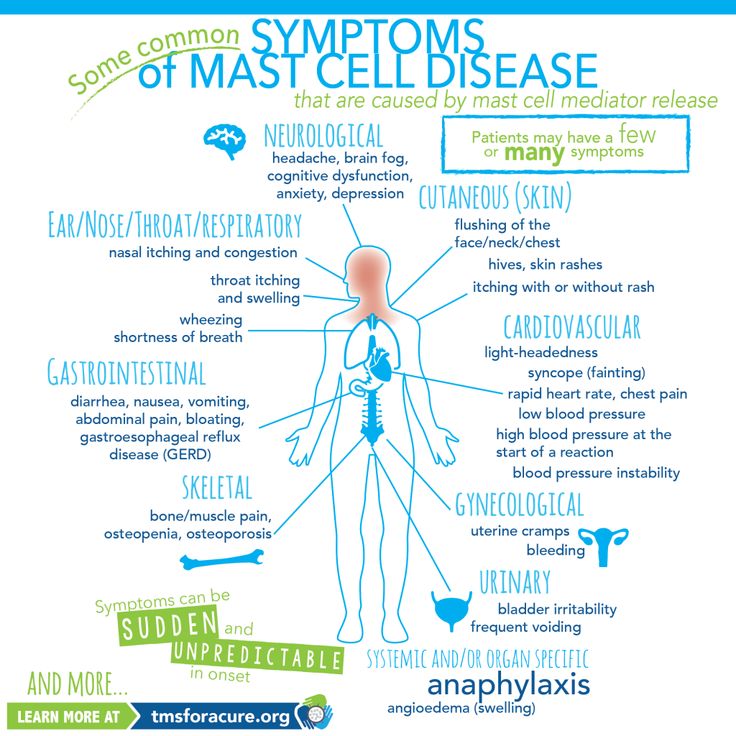 But besides this, they interfere with quality rest: due to anxiety and the feeling that there are too many thoughts in your head, you cannot really relax.
But besides this, they interfere with quality rest: due to anxiety and the feeling that there are too many thoughts in your head, you cannot really relax.
You have trouble sleeping
People with anxiety disorders often complain of insomnia: in the evening it is difficult for them to fall asleep, and at night they constantly wake up. Despite the fact that scientists have found a connection between insomnia and anxiety disorders, the nature of this connection is still unknown. According to some studies, insomniacs are at a higher risk of developing an anxiety disorder, according to others, chronic insomnia tends to begin at the same time as or after the anxiety disorder. According to the third, they mutually influence each other.
Your body is scared even when you are not.
Fear activates our sympathetic system: the body prepares to respond to danger. The pulse and breathing quicken, the mouth becomes dry, sweat appears on the forehead, palms and back. The problem is that with an anxiety disorder, this happens even without reason for fear and anxiety. If you feel dizzy, you tremble and you are thrown into heat or cold - this is right here.
The problem is that with an anxiety disorder, this happens even without reason for fear and anxiety. If you feel dizzy, you tremble and you are thrown into heat or cold - this is right here.
Something hurts you
Anxiety disorders are associated with seemingly different pain syndromes such as tension headache, chest pain, chronic pain (fibromyalgia, migraine, arthritis), as well as pain in the abdomen, muscles and cases of pain that cannot be explained. This is also due to the fact that stress changes our perception of pain and can cause hyperalgesia - increased sensitivity to pain.
Your body is malfunctioning
Anxiety disorders can also be indicated by symptoms that seem to be quite far from psychiatry and neurology. For example, the need to go to the toilet often. Also associated with anxiety disorders are gastrointestinal disorders - nausea, heartburn, diarrhea, constipation and irritable bowel syndrome.
All this is ruining your life
Generalized anxiety disorder differs from stress-induced anxiety in part because the symptoms greatly affect the quality of life: they interfere with normal activities, work, building and maintaining relationships.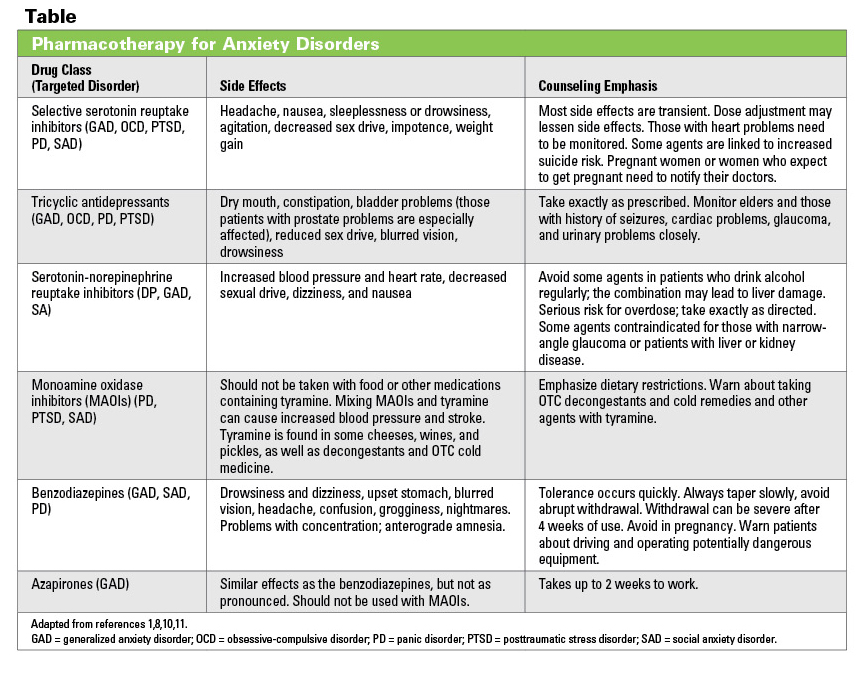
What to do next
The first thing is to contact a specialist
Even if you have found several signs from the list above, you should not get carried away with self-diagnosis. Only a psychiatrist can make a diagnosis of generalized anxiety disorder, guided by special diagnostic criteria. When he determines whether a patient has an anxiety disorder, he is faced with the task of ruling out other possible diseases with similar symptoms. Under the guise of anxiety, a variety of diagnoses can be hidden: from depression and Alzheimer's disease to diabetes and hyperthyroidism.
If anxiety affects the quality of life, it makes sense not to wait for additional symptoms or announced six months and contact a psychotherapist. Or to a psychologist - if he has a suspicion that a psychiatric consultation is needed, he will refer you to the appropriate doctor.
In modern medicine, anxiety disorders are treated with pharmacotherapy (drugs), psychotherapy, and a combination of the two.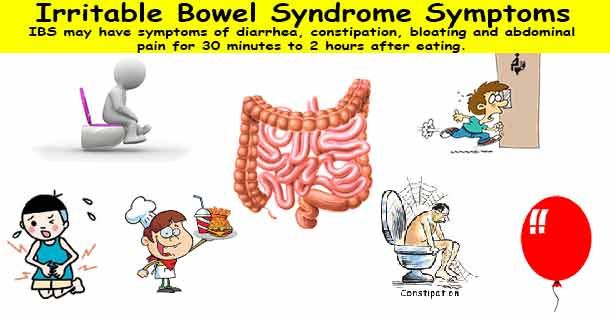 Different schools of psychotherapy have different approaches to understanding and treating generalized anxiety disorder. One of the effective types of psychotherapy is cognitive-behavioral, and its combination with medications is recommended as the main treatment strategy.
Different schools of psychotherapy have different approaches to understanding and treating generalized anxiety disorder. One of the effective types of psychotherapy is cognitive-behavioral, and its combination with medications is recommended as the main treatment strategy.
Second, change your lifestyle
"Home" methods are not a substitute for qualified anxiety care, but they can relieve symptoms of anxiety. By leading a healthier and more mindful lifestyle, we can reduce our stress levels—and thereby reduce our anxiety.
Meditate more often and breathe deeply
Do not forget about physical activity
Do not deprive yourself of sleep
Limit bad habits
Think about healthy eating
Click tips to read more
Meditate more often and breathe deeply
Several studies show that mindful breathing, mindfulness-based stress reduction, and yoga help relieve symptoms of anxiety. Perhaps this is due to the use of deep breathing practices in them, the stress-reducing effect of which has been proven by a large number of studies.
Do not forget about physical activity
The American Association for the Study of Anxiety and Depressive Disorders recommends regular exercise such as running, walking, cycling, or dancing three to five times a week for half an hour.
Do not deprive yourself of sleep
Although we have already mentioned the relationship between anxiety and insomnia, it is worth repeating that lack of sleep reduces the body's ability to resist stress and increases anxiety. Therefore, if you notice anxiety behind you, you should try to improve sleep hygiene - sleep enough time, go to bed and get up on time.
Limit bad habits
Alcohol, smoking and caffeine abuse are associated with increased anxiety. What's more, those who avoid coffee and cigarettes are less likely to develop generalized anxiety disorder.
Think Healthy Eating
Research shows that certain foods and dietary habits have a positive effect on mental health and anxiety in particular.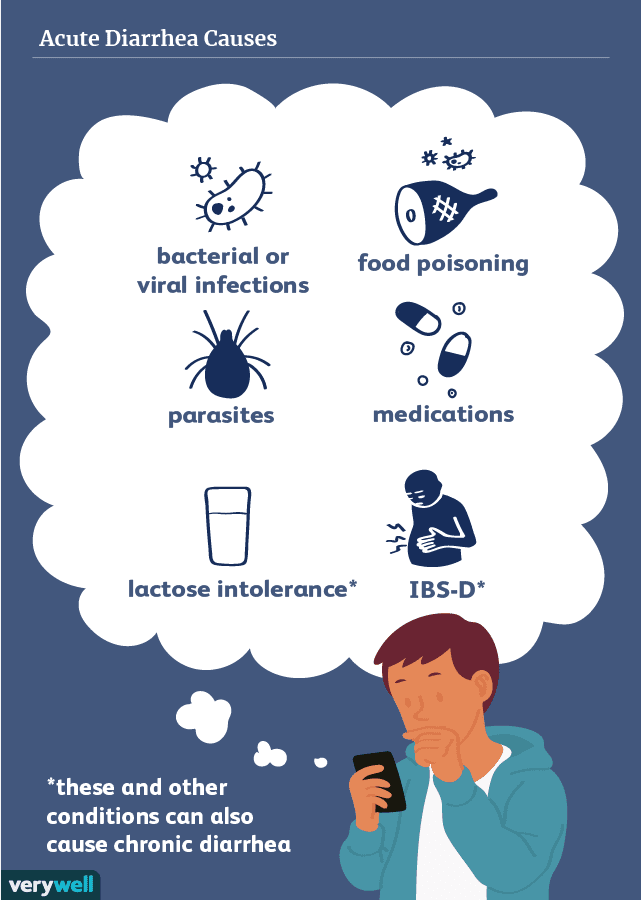 For example, probiotics and fermented foods (such as kefir and yogurt), omega-3 unsaturated fatty acids (found in sea fish and spinach), fruits and vegetables have proven themselves well. In 2010, a study was conducted with the participation of more than 1000 women. It showed that those whose diet included vegetables, fruits, meat, fish, and whole grains were less likely to be depressed and anxious than those whose diet included fried foods, high amounts of sugar, refined grains, and beer.
For example, probiotics and fermented foods (such as kefir and yogurt), omega-3 unsaturated fatty acids (found in sea fish and spinach), fruits and vegetables have proven themselves well. In 2010, a study was conducted with the participation of more than 1000 women. It showed that those whose diet included vegetables, fruits, meat, fish, and whole grains were less likely to be depressed and anxious than those whose diet included fried foods, high amounts of sugar, refined grains, and beer.
“Emotional overload, lack of sleep and adequate rest — all this increases our excitability and, consequently, anxiety. In such cases, it will not be superfluous to try to unload yourself, rest more, improve sleep and see if it becomes easier as a result. Although I, as a representative of the profession, of course, believe that in any case it can be useful for a person to go to a psychologist and try to solve their problems not alone, but with a specialist, ”concludes Plyaskina.
{"width":1200,"column_width":93,"columns_n":10,"gutter":30,"line":40}false7671300falsetrue{"mode":"page","transition_type":"slide", "transition_direction":"horizontal","transition_look":"belt","slides_form":{}}{"css":". editor {font-family: tautz; font-size: 16px; font-weight: 400; line-height: 21px;}"}true
editor {font-family: tautz; font-size: 16px; font-weight: 400; line-height: 21px;}"}true Generalized anxiety disorder in gastroenterologist practice uMEDp
The prevalence of generalized anxiety disorder in general medical practice reaches 8–10% of the total number of patients, which exceeds population figures. The so-called somatic anxiety, manifested by bodily symptoms, in this category of patients often prevails over the actual anxiety complaints. In the clinical picture of the disease, there are often (but less frequently compared to symptoms of disorders of the cardiovascular and respiratory systems) functional disorders of the gastrointestinal tract. In this regard, for the first time, the diagnosis of generalized anxiety disorder can be suggested by a gastroenterologist. The article considers the mechanism of anxiety somatization, analyzes the clinical manifestations of this disease, as well as the differential diagnosis of generalized anxiety and somatoform disorders.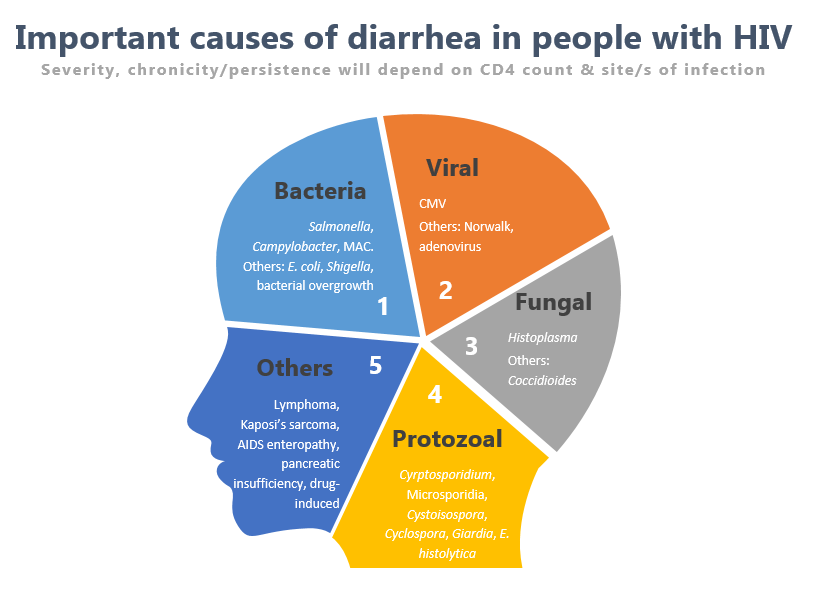
Generalized Anxiety Disorder (GAD) is a condition characterized by persistent (at least six months) unexplained anxiety. The prevalence of GAD in the general population is 6.5%, among patients of the general medical network - 8–10% [1].
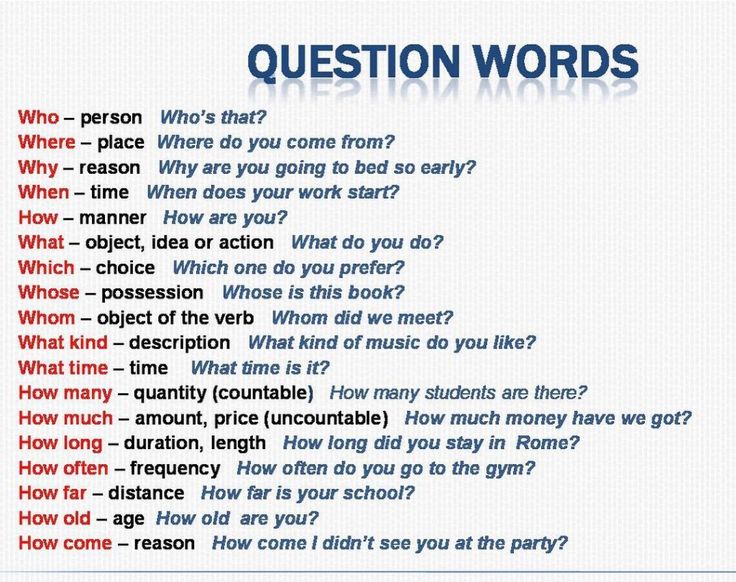
To understand the diagnosis of generalized anxiety disorder, consider the terms "anxiety", "fear", "anxiety" and define the difference between them.
Anxiety is a negatively colored emotion, or in a more pronounced version, a diffuse feeling of an indefinite threat, the nature and timing of which are unpredictable. The alarm function is a warning of danger and the inclusion of a mechanism for mobilizing the body to quickly achieve adaptation in changing environmental conditions.
Fear fundamentally differs from anxiety not only in intensity, but also in the degree of specificity of sensation: anxiety is pointless, unclear, while fear is extremely specific and is associated with a psychologically understandable danger.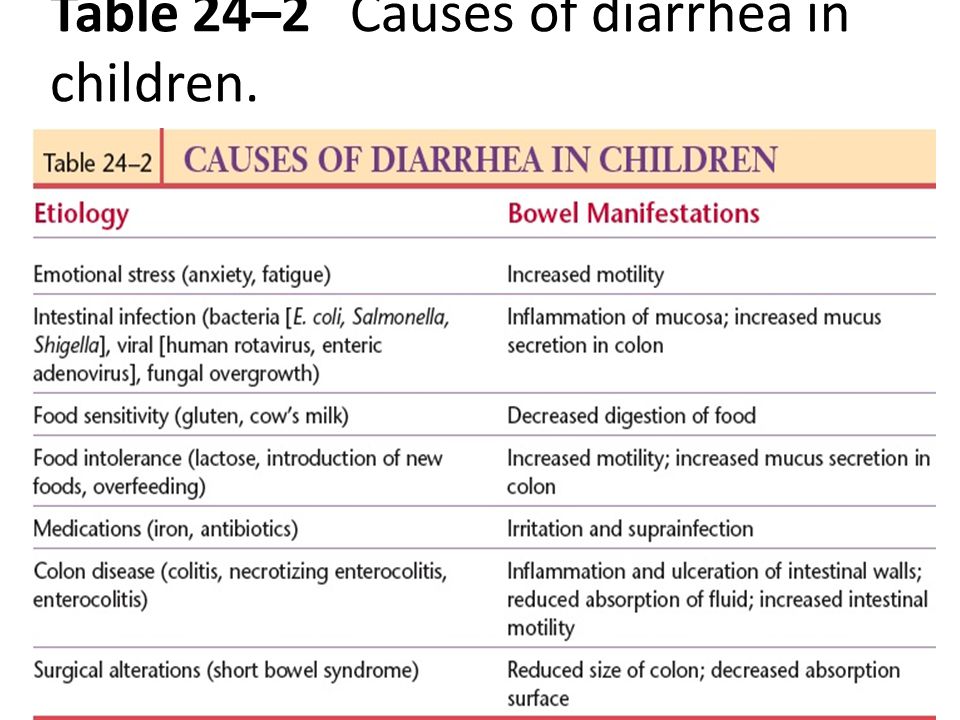
Anxiety should be distinguished from anxiety: anxiety is a state at the present moment in time, anxiety is an individual mental feature that manifests itself in a person’s tendency to often experience severe anxiety for a minor reason [2].
All human emotions have a vegetative component. In the case of anxiety, the psychological part of the emotion is just the tip of the iceberg. The vegetative correlates of anxiety do not require proof, they are well known: turn pale with fear (the result of spasm of small skin vessels), tremble with fear “like an aspen leaf” (due to motor tension), etc. Vegetative manifestations of anxiety are called somatic anxiety. Its symptoms may dominate the status of patients with GAD or completely mask the mental component of anxiety. For this reason, patients do not come to the attention of psychiatrists, but receive treatment in the general medical network, including gastroenterologists, giving priority to somatic complaints.
The issues of diagnosing GAD, differential diagnosis and treatment approaches are reflected in the Guidelines of the Russian Society of Psychiatrists [3], as well as in the Collection of instructive and methodological materials for doctors [4].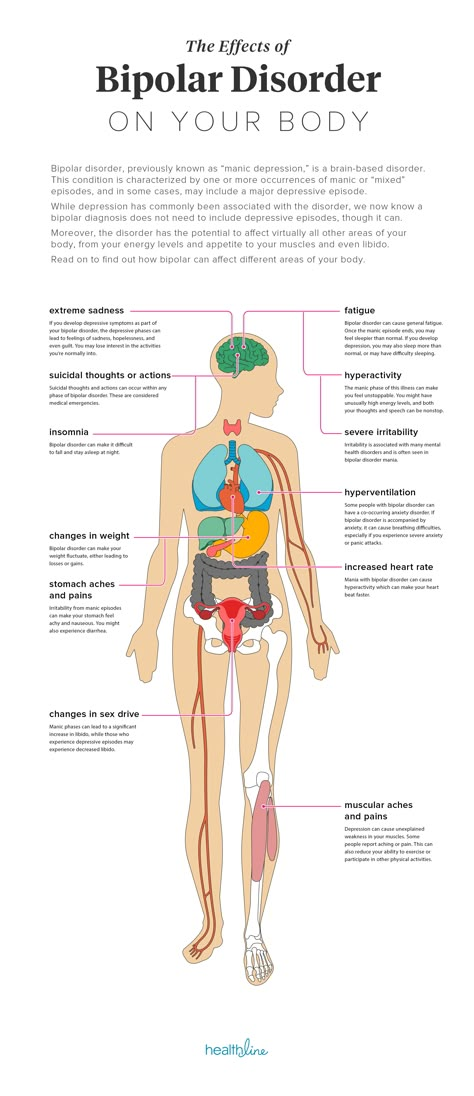 In addition, the experience of clinicians and researchers regarding this issue is presented in a number of modern monographs [5–7] .
In addition, the experience of clinicians and researchers regarding this issue is presented in a number of modern monographs [5–7] .
Anxiety is a universal psychophysiological reaction to stress. This feeling is familiar to everyone. In a healthy person, anxiety is a temporary sensation associated with a threatening external situation. Physiological anxiety (sometimes called normal) is mentally understandable, the duration of the anxiety state depends on the factor that provoked it. Experiencing anxiety, a person is afraid that he can cause harm, and, as a result, pays more attention to what worries. As a result, behavior becomes more intelligent and efficient. This type of anxiety can be called constructive, since its function is to identify undeveloped areas of the life situation and change behavior. Therefore, in some situations it is useful to worry. The purpose and result of physiological anxiety is the acquisition of life experience and the strengthening of the adaptive capabilities of the body.
With the physiological anxiety of a healthy person, the mental component is more pronounced. Factors that increase normal anxiety are a high degree of stressfulness of a traumatic situation, a lack of information and a lack of time to make a decision. Vegetative changes during physiological anxiety are minimal and do not lead to impaired adaptation.
Things are different with pathological anxiety, which is felt as pointless, groundless anxiety. More often it is due to internal causes, and the psychogenic factor in some cases becomes the reason, and not the cause of its occurrence. Even if anxiety is provoked by external circumstances, its intensity is inadequate to the situation.
Pathological anxiety is associated with a long-term danger, often accompanied by fear, which naturally prepares the body to respond to the threat and triggers numerous autonomic reactions to "rescue". The diversity and variability of long-term vegetative disorders lead to maladjustment and depletion of the body's resources.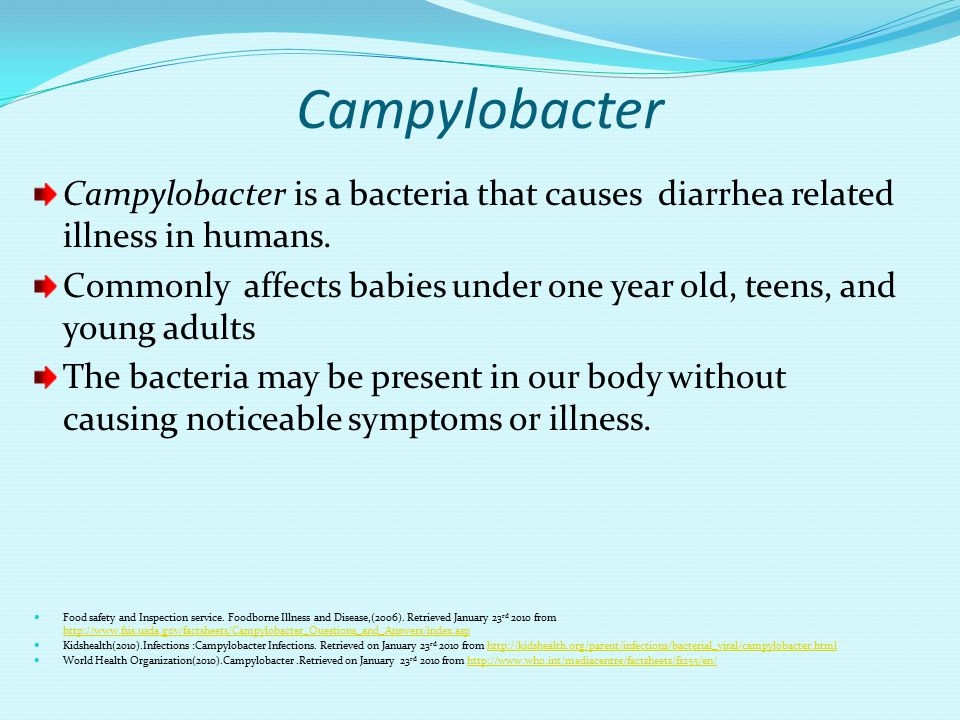
Anxiety in individuals with a high level of personal anxiety occupies a borderline position between normal and pathological anxiety. Patients themselves consider themselves emotional, sensitive, overreacting to ordinary life problems, suspicious, capable of exaggerating emerging problems. Even with prolonged anxiety, they explain it as a natural reaction to what is happening. Fluctuations in the intensity and duration of anxiety depend on external circumstances, but are not always adequate to them. In this case, the transition of anxiety into a pathological form is possible. During periods of difficult life situations (especially long ones), pronounced vegetative dysfunctions with corresponding somatic symptoms may be present.
In the International Classification of Diseases of the 10th revision [8], pathological anxiety is reflected in the framework of several diagnoses, combined in section F40-F48 "Neurotic stress-related and somatoform disorders". In the section, the diagnoses are differentiated as follows:
- F40 - phobic anxiety disorders;
- F41 - other anxiety disorders, in particular: F41.
 0 - panic disorder, F41.1 - generalized anxiety disorder, F41.2 - mixed anxiety and depressive disorder;
0 - panic disorder, F41.1 - generalized anxiety disorder, F41.2 - mixed anxiety and depressive disorder; - F42 - obsessive-compulsive disorder;
- F43 - reaction to severe stress and adaptation disorders.
When establishing a diagnosis, it should be borne in mind that different forms of anxiety disorders in the process of clinical dynamics can pass one into another.
Of the anxiety disorders mentioned, the most common in somatic practice is generalized anxiety disorder (F41.1).
To understand the essence of GAD, the process of somatization of anxiety must be considered from a neurophysiological and psychological point of view [9, 10]. Anxiety is a signal of danger, to which the body responds with a cascade of changes that bring it into a state of "combat readiness". The central place in the management of emotional reactions at the physical level is occupied by the autonomic nervous system. It is no coincidence that it is called the bridge between the psyche and the body. Turning on the active part of the autonomic nervous system (its sympathetic division) prepares the body for salvation, which can be achieved in two ways - flight and attack. In both cases, the first natural step is to increase the tone of the skeletal muscles. Working muscles need oxygen: heart rate increases, blood pressure rises, breathing deepens. With intensive work, a balanced internal temperature regime is especially important. Depending on the situation, its settlement is associated with manifestations such as fever, cold sweat or chills. Since intense physical activity is expected, all energy resources should be directed to the work of skeletal muscles. The body tries to get rid of the “ballast”: the smooth muscles of the hollow organs contract sharply, leading to urges that empty the bladder and intestines.
Turning on the active part of the autonomic nervous system (its sympathetic division) prepares the body for salvation, which can be achieved in two ways - flight and attack. In both cases, the first natural step is to increase the tone of the skeletal muscles. Working muscles need oxygen: heart rate increases, blood pressure rises, breathing deepens. With intensive work, a balanced internal temperature regime is especially important. Depending on the situation, its settlement is associated with manifestations such as fever, cold sweat or chills. Since intense physical activity is expected, all energy resources should be directed to the work of skeletal muscles. The body tries to get rid of the “ballast”: the smooth muscles of the hollow organs contract sharply, leading to urges that empty the bladder and intestines.
It follows from the above that nature has created an amazing system of neurophysiological reactions that ensure biological survival in case of danger. Creating this masterpiece, nature could not foresee the further course of evolution: there were incomparably fewer direct external threats. Meanwhile, the reaction to the threatening danger remained the same (as in animals and primitive man). The body, due to the activation of vegetative reactions, prepares for an escape or a retaliatory attack [9, ten].
Meanwhile, the reaction to the threatening danger remained the same (as in animals and primitive man). The body, due to the activation of vegetative reactions, prepares for an escape or a retaliatory attack [9, ten].
A person's reaction to danger has its own characteristics. Unlike animals, humans have a more developed cerebral cortex. In the formation of "human" anxiety, a complex interpretation of a dangerous situation, that is, how a person understands danger, plays an important role. This can reinforce the negative and, if misinterpreted, further increase anxiety (“twist yourself”). At the same time, the highly developed nerve centers of the cerebral cortex are able to inhibit the underlying centers, which allows the body to mitigate the manifestations of the intensity of anxiety and fear. This neurophysiological mechanism underlies effective anxiety psychotherapy.
The diagnosis of anxiety disorder is associated with a number of difficulties. One of them is the above-mentioned predominance in the clinical picture of somatovegetative disorders that set the patient up for a somatic (serious) diagnosis.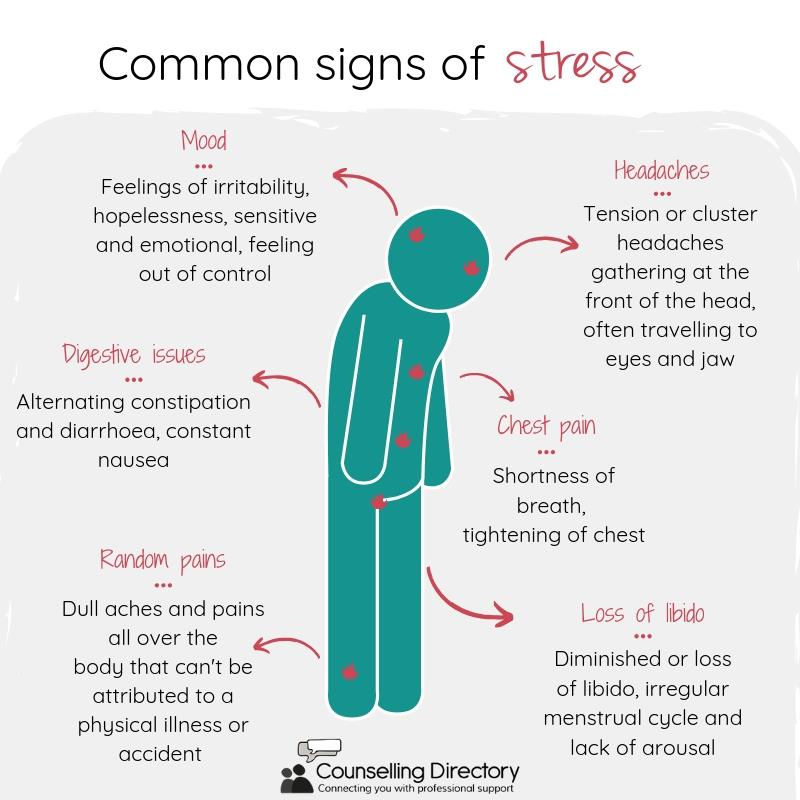 As clinical observations show, at an appointment with an internist, patients, for various reasons, try to hide their anxiety. Certain difficulties are also associated with some difference between the psychological term of anxiety and anxiety, which in ordinary life means only a fairly intensely expressed negative emotion. In this regard, patients deny the existence of anxiety and describe their condition in less anxious words, which nevertheless refer to the terminology of the anxiety series: anxiety over trifles or constant anxiety about supposed failures, bad forebodings, "anticipation" of danger, poor tolerance of uncertainty, need in exaggerated control, fearfulness, irritability, tension, alertness, a feeling of agitation, being on the verge of a breakdown, inability to relax, sleep disturbance (more often difficulty falling asleep, frequent awakenings, disturbing dreams).
As clinical observations show, at an appointment with an internist, patients, for various reasons, try to hide their anxiety. Certain difficulties are also associated with some difference between the psychological term of anxiety and anxiety, which in ordinary life means only a fairly intensely expressed negative emotion. In this regard, patients deny the existence of anxiety and describe their condition in less anxious words, which nevertheless refer to the terminology of the anxiety series: anxiety over trifles or constant anxiety about supposed failures, bad forebodings, "anticipation" of danger, poor tolerance of uncertainty, need in exaggerated control, fearfulness, irritability, tension, alertness, a feeling of agitation, being on the verge of a breakdown, inability to relax, sleep disturbance (more often difficulty falling asleep, frequent awakenings, disturbing dreams).
Manifestations of emotions may vary, but each of them has a vegetative accompaniment. This explains the general vegetative lability of patients with GAD - indefinite discomfort in the whole body or its individual parts, discomfort in the abdomen that does not reach the level of pain, dry mouth, general malaise, a feeling of "brokenness". In this state, the body is maladjusted, vegetative reactions come into conflict with each other, a person is not capable of physical labor.
In this state, the body is maladjusted, vegetative reactions come into conflict with each other, a person is not capable of physical labor.
Unlike other complaints, weakness and decreased performance are almost constant. Anxiety covers the entire body. This is due to the fact that the nerve impulse from the sympathetic system, which has a huge number of connections and nerve endings, spreads diffusely throughout the body. An obligate feature of somatic manifestations of anxiety is their polysystemic nature. As already noted, anxiety prepares the body for an active response to a threatening situation, skeletal muscles, cardiovascular and respiratory systems are involved. This explains the fact that the clinical picture of GAD is dominated by cardiovascular and respiratory disorders. Patients turn to a cardiologist (with complaints of discomfort or pain in the heart area, palpitations, a feeling of interruptions in the work of the heart, fluctuations in blood pressure), a pulmonologist (about a feeling of lack of air, disturbing uneven breathing, dissatisfaction with inspiration) or a neurologist with a wide variety of complaints (muscle pain, muscle stiffness, inability to relax, tension headache, trembling in the arms and legs, numbness, tingling, goosebumps, etc. ).
).
The gastrointestinal tract is closely connected with the autonomic nervous system, so the imbalance between its sympathetic and parasympathetic divisions cannot but affect the digestion process (although a negative effect on the cardiovascular and respiratory systems is noted more often). Any gastroenterological symptoms can be manifestations of these disorders: nausea, dry mouth, diarrhea or constipation, abdominal pain, flatulence, loss of appetite. In this regard, the high level of comorbidity of GAD and diseases of the gastrointestinal tract is beyond doubt. To a greater extent, this applies to diseases of the intestine. According to a number of authors [1], about 40% of patients with irritable bowel syndrome suffer from GAD. The frequency of anxiety and depression in patients with irritable bowel syndrome is even higher than in patients with objectively more severe inflammatory bowel diseases [11].
A full gastroenterological examination of patients with GAD is difficult due to their characteristic fear of mandatory probe studies (esophagogastroduodenoscopy, colonoscopy). The way out of this situation may be to conduct such studies using intravenous sedation.
The way out of this situation may be to conduct such studies using intravenous sedation.
Gastrointestinal disorders are often combined with disorders in the urinary system, which are usually manifested by frequent urge to urinate. If at the same time subfebrile condition is present in the clinical picture, both symptoms can be erroneously interpreted as signs of inflammation.
Thus, when establishing the diagnosis of GAD, it is necessary to take into account not only the duration of the disease (at least six months), but also the mandatory presence of at least four of these symptoms.
Differential diagnosis of GAD and somatoform disorder is very difficult due to the similarity of the clinical manifestations of these diseases. With an anxiety disorder, the emotional (mental) component is more attention-grabbing, while with a somatoform disorder, bodily manifestations. The "rudiments" of a somatoform disorder appear in childhood (difficulties in waking up from sleep, whims during sudden changes in the weather, motion sickness) and at a transitional age, characterized by increased requirements for adaptation.