Who to call when your depressed
Evidence-Based Resources About Opioid Overdose
SAMHSA’s Evidence-Based Practice Resource Center (EBPRC) contains a wide variety of downloadable resources available from SAMHSA and other federal partners about opioid overdose and other substance use and mental health topics to help communities, clinicians, policy-makers and others with the information and tools to incorporate evidence-based practices into their communities or clinical settings.
Fact Sheet:
Using Naloxone to Reverse Opioid Overdose in the Workplace: Information for Employers and Workers | CDC (PDF | 785 KB) - This fact sheet helps employers understand the risk of opioid overdose and provides guidance about establishing a workplace naloxone program.
Tips for Teens: The Truth About Opioids | SAMHSA - This fact sheet for teens provides facts about opioids. It describes short- and long-term effects and lists signs of opioid use. The fact sheet helps to dispel common myths about opioids.
Access sources cited in this fact sheet.
Toolkits:
Medication-Assisted Treatment (MAT) for Opioid Use Disorder in Jails and Prisons: A Planning and Implementation Toolkit | National Council of Behavioral Health - Developed by the National Council of Behavioral Health, this guide provides correctional administrators and healthcare providers tools for implementing MAT in correctional settings.
Opioid Overdose Prevention Toolkit | SAMHSA -This toolkit offers strategies to health care providers, communities, and local governments for developing practices and policies to help prevent opioid-related overdoses and deaths. Access reports for community members, prescribers, patients and families, and those recovering from opioid overdose.
Evidence Reviews/Guidebooks:
Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States | CDC (PDF | 11.5 MB) - This CDC document reviews evidence-based strategies to reduce overdose. It explains why these strategies work, the research behind them, and examples of organizations that have put these strategies into practice.
It explains why these strategies work, the research behind them, and examples of organizations that have put these strategies into practice.
Use of Medication-Assisted Treatment in Emergency Departments | SAMHSA - This guide examines emerging and best practices for initiating medication-assisted treatment (MAT) in emergency departments.
Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings | SAMHSA -This guide focuses on using medication-assisted treatment for opioid use disorder in jails and prisons and during the reentry process when justice-involved persons return to the community.
Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders | SAMHSA - This guide reviews ways that telehealth modalities can be used to provide treatment for serious mental illness and substance use disorders including opioid overdose among adults.
Treatment Improvement Protocols/Manuals:
TIP 63: Medications for Opioid Use Disorder | SAMHSA - This Treatment Improvement Protocol (TIP) reviews the use of the three Food and Drug Administration (FDA)-approved medications used to treat OUD—methadone, naltrexone, and buprenorphine.
Advisory: Opioid Therapy in Patients With Chronic Noncancer Pain Who Are in Recovery From Substance Use Disorders | SAMHSA - This advisory addresses screening and assessment tools, nonpharmacologic and nonopioid treatment for chronic pain, and the role of opioid therapy in people with chronic noncancer pain and SUDs.
Overdose Prevention & Naloxone Manual | HRC - This Harm Reduction Coalition (HRC) manual outlines the process of developing an Overdose Prevention and Education Program that may involve a take-home naloxone component.
Websites:
SAMHSA
- Medication-Assisted Treatment (MAT)
- MAT Medications, Counseling, and Related Conditions
- Opioid Overdose
- Know the Risks of Using Drugs
Other federal websites
- HHS.gov/opioids
- Opioids | NIDA
- Drug Overdose | CDC
- Rx Awareness | CDC
Visit the EBPRC for additional information, including Treatment Improvement Protocols, toolkits, resource guides, clinical practice guidelines, and other science-based resources.
Depression Hotline Numbers: Here's Help
Depression hotlines offer free and confidential access to qualified professionals and volunteers for those in immediate need of support.
Depression is one of the most common mental health conditions. The World Health Organization estimates that 264 million people worldwide are living with depression.
Many people with depression isolate themselves from those they love and others who may want to help. Isolation can make symptoms seem worse.
A depression crisis can be scary and overwhelming, not only for the individual but also for loved ones who often don’t know what to do or what to say. In those moments, it’s hard to know where to start.
A hotline can help.
It’s estimated that in 2018, more than 2 million people called the National Lifeline for help. Many crisis centers report a 30-40% increase in calls due to the COVID-19 pandemic.
Here’s a look at hotline numbers you can call for help.
National Suicide Prevention Lifeline: 800-273-8255 (TALK)
The National Suicide Prevention Hotline offers free and confidential support to those in immediate emotional distress. The hotline provides suicide prevention resources as well as access to local crisis centers.
The hotline provides suicide prevention resources as well as access to local crisis centers.
You don’t have to be actively thinking about suicide to use this service — anyone in emotional distress can call and use their services.
Lifeline Chat is an online chat that provides a direct connection to counselors for support.
For hearing impaired services, call 800-273-8255 or use the chat services.
SAMHSA: 800-662-4357 (HELP)
The Substance Abuse and Mental Health Services Administration (SAMHSA) highlights behavioral health impacts, like substance use and mental health conditions, in communities across the country. SAMHSA provides a confidential connection to substance use treatment facilities and behavioral health treatment service locators to make access to support easier.
You can also visit the online treatment locator to find treatment near you.
SAMHSA also offers hearing impaired services at 800-487-4889.
Samaritans: 877-870-4673 (HOPE) (call or text)
Samaritans offers immediate emotional support for those in distress. If you’re thinking about suicide or have lost someone to suicide, the volunteers at Samaritans can help.
If you’re thinking about suicide or have lost someone to suicide, the volunteers at Samaritans can help.
They also offer an online chat service through Lifeline Chat.
Crisis Text Line: Text “HOME” to 741741
The Crisis Text Line offers help for any crisis. A counselor receives your text and responds immediately from a privately secure platform.
If you live in the United Kingdom, text 85258. In Ireland, you can text 50808.
Friendship Line: 800-971-0016
As the only hotline targeted toward people 60 years old and older and adults with disabilities, the Institute on Aging’s Friendship Line offers emotional support and suicide intervention.
The Friendship Line is also there to simply listen.
Trained volunteers help older adults experiencing depression symptoms and loneliness and offer grief support.
If you live in the California area, Friendship Line can even respond to abuse reports of older people and provide well-being checks.
Veterans Crisis Line: 800-273-8255 (press 1) or Text 838255
Trained professionals from the Department of Veterans Affairs provide free and confidential support services to veterans in crisis. Support is available to all veterans, service members, and National Guard and Reserve.
Support is available to all veterans, service members, and National Guard and Reserve.
Friends and family of veterans are also able to get emotional support and resources through the hotline’s crisis responders.
A crisis chat is also available day or night.
Online hotlines
Online hotlines provide quick and easy, around-the-clock access to mental health professionals and trained volunteers ready to engage, support, and guide individuals in crisis.
Some of the most helpful include:
- IMalive.org
- Lifeline Crisis Chat
Youth hotlines
Because of their unique needs and situations, youths experiencing depression and distress often require specialized support and care to resolve crises.
Mental health counselors and volunteers provide not only crisis support but also offer abuse and self-harm resources. For a youth-specific hotline, try one of the following:
- National Youth Crisis Hotline
- Boys and Girls Town National Hotline
- Child Help USA Hotline
- Trevor Project Lifeline
Many people turn to depression hotlines because they don’t feel comfortable talking with others about their feelings. They may feel as if friends and family won’t understand or even overreact to what they say.
They may feel as if friends and family won’t understand or even overreact to what they say.
A depression crisis can be scary. Talking with someone immediately can often help. A 2019 systematic review found that crisis line services can help in the short-term and for immediate assistance.
Some reasons people call hotlines:
- Talk with someone who will listen and understand what they’re going through.
- Learn more about what they’re going through and the type of help available.
- Get confidential and anonymous help.
- Learn how to help a loved one who is experiencing depression.
- Find a counselor or therapist.
The immediate access to counselors and trained volunteers can bridge the gap between a crisis and treatment by a mental health professional.
Remember: When you call a crisis hotline, the call is confidential and private. There’s no judgment, and no one will think less of you for what you say.
You don’t have to be depressed to call a hotline, either. If you’re concerned about someone you love who may be going through a depression crisis, a hotline is a great place to learn more about how you can help.
If you’re concerned about someone you love who may be going through a depression crisis, a hotline is a great place to learn more about how you can help.
Depending on the hotline, you may be greeted by an automated message that will then reroute you to a center nearest you. You’ll likely be placed on a brief hold until someone can answer your call.
Once you’re connected, a crisis line worker will actively listen to you and not judge you for anything you say. Responders will spend as much time with you as you need.
Crisis hotlines are staffed by individuals who have been trained to handle crises. Some hotlines have volunteers with minimal training, while others may have skilled, trained counselors in your area who will answer your call.
Responders may ask questions to get more information about your situation. They may also tell you about mental health services in your area where you can receive further help.
Each call and situation is different, so there is no script to follow, just compassionate and emphatic listeners who will help you and guide you to more resources.
Hotlines are open 24 hours, 365 days a year. They are there to answer your calls, day or night.
Living with depression can seem overwhelming at times. A crisis hotline can provide the support you need and help you to engage and diffuse a situation you’re facing right at that moment.
The trained counselors and volunteers of crisis and depression hotlines offer emotional support and help to guide you. Responders can connect you with the resources you need to help you find treatment and counseling near you.
If you’re in a crisis now, consider reaching out to a depression hotline. They’re always there, no matter the day or time.
Psychological Help Hotline, Psychological Help Helpline, free hotline 8-800
Psychological Help Hotline is a critical social service. No one is immune from a negative Psychological situation or a stressful situation, during which there is no possibility to receive outpatient Psychological assistance, at such moments the hotline is the only way to get help and support in order to overcome difficulties.
Psychological help line (helpline)
Who may need emergency Psychological Help by telephone?
Working Principles of the Helpline Hotline
Other Ways to Get Emergency Psychological Help
Competence of Operators and Response Time
Psychological Helpline (helpline)
8 (800) 333-44-34
Calls are free throughout Russia.
Hotline for Psychological Assistance EMERCOM of Russia
8 (499) 216-50-50
Toll-free 24-hour emergency Psychological assistance for Moscow residents
051
Who may need emergency Psychological assistance by phone?
- People who experience a very strong emotional experience of an intolerable nature, which requires the help of a specialist;
- People who have suffered psychological trauma;
- People who experience severe stress and want to find ways out of this state;
- People who have suffered the loss of a loved one or faced grief and who, due to circumstances, do not understand how to live on;
- Persons who cannot understand themselves;
- People who are depressed and have suicidal thoughts;
- Those people who have come to the conclusion that they need professional Psychological help, but who, for various reasons, put off visiting a specialist.

- Teenagers, in whose personal life there are difficulties in relations with a partner, and they see their solution only in a fatal act.
How the hotline works
- Anonymity. The caller and the consultant may not give their real name and provide another personal information about themselves during the conversation. This also applies to the phone number from which the call came;
- Privacy. All information received during a conversation with a hotline consultant is not transferred and is not used in the future, and the data received during the conversation is anonymized as much as possible;
- Tolerance. Whatever opinion, views and beliefs the caller holds, he is not criticized or condemned. The consultant in any situation will try to understand the subscriber.
- Call management. A caller to a hotline number can end the conversation at any time or abruptly change its subject, without explaining the reasons.
Other ways to get emergency Psychological assistance
On the website of the Ministry of Emergency Situations of Russia, you can contact the Internet service of emergency Psychological assistance with a question or problem, which is located in the appropriate section.
In it, you can create an anonymous appeal without registration and get an answer to the question as soon as possible, which will be written in the general journal.
Competence of operators and response time
The hotline answers the subscriber's call as quickly as possible, the waiting time for communication with a consultant takes about a minute.
Professional Psychologists work in the Psychological Assistance Service, who will help to cope with the problem, give advice on how to overcome life's difficulties in the right way, or simply allow the subscriber to speak out.
Best deals of the day
Compare.ru
Encyclopedia
Banks
Hotlines
Psychological help hotline
"Would rather have evening and sleep." How to recognize depression and save your life
At the beginning of this week, sad news came from the city of Karkaraly, Karaganda region: the former member of SuperStar. kz, singer Zhanar Khamitova, died. Earlier, in one of the talk shows, a 30-year-old woman spoke about depression and fear of going on stage, it was also reported that after the divorce, her children stayed with their father in Turkey. Police said they were investigating "incitement to suicide."
kz, singer Zhanar Khamitova, died. Earlier, in one of the talk shows, a 30-year-old woman spoke about depression and fear of going on stage, it was also reported that after the divorce, her children stayed with their father in Turkey. Police said they were investigating "incitement to suicide."
Tengrinews.kz correspondent Olga Pastukhova turned to psychotherapist, psychiatrist Zhibek Zholdasova with 5 questions about how to recognize and cure depression. Despite the fact that today this is a very popular diagnosis, according to world statistics, no more than 20-30 percent of patients with depression reach a specialist. Meanwhile, in 80 percent of cases, according to world statistics, suicide is committed by people suffering from severe mental disorders, including depressive ones. There are no exact data for Kazakhstan.
How to recognize depression?
When indifference to everything, unwillingness to communicate, depression last for more than two weeks, then most likely it is depression. This disease can happen to anyone - just like the flu. No one is safe from her.
This disease can happen to anyone - just like the flu. No one is safe from her.
If a person wakes up in the morning with the thoughts “it would be better to sleep in the evening” and there is a feeling of lengthening the time, then this can be either a mild degree of depression or a manifestation of emotional burnout. Very often people think that depression will go away if you go on vacation or have a holiday. However, such a switch will only help in case of emotional burnout. If you have depression, you need to consult a specialist - a psychotherapist or a psychiatrist.
A person can be under the supervision of ordinary doctors for a long time. In some cases, depression is disguised as somatic diseases: osteochondrosis, migraines, abdominal pain, high blood pressure, addiction to alcohol and drugs, and so on. If a patient cannot be diagnosed for a long time or he is overcome by more and more new ailments, then this may be another reason to think about depression. A separate place is occupied by postpartum depression - mental changes can occur after childbirth, miscarriage, abortion or stillbirth in the first two months.
Normally, a person - both a child and an adult - has an instinct for self-preservation. If a person too often gets into unpleasant situations, emergencies, injuries, etc. happen to him, then this is another bell about self-destruction. After all, perhaps, after one of these situations, he will not be saved. We do not know what is the percentage of hidden suicides in those situations that were classified as accidents.
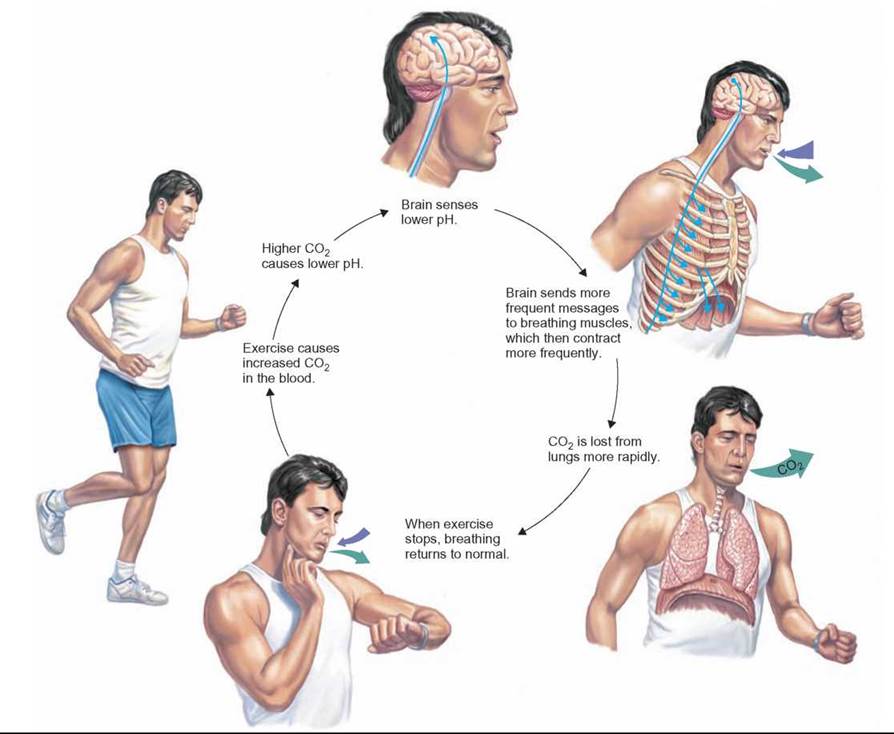
Any psychotraumatic situation affects a person either mobilizing or destructive. Normally, stress should mobilize a person. But if a person at a difficult moment was weakened by an illness, for example, the flu, or was left without friendly support - he has no one to call, then he will suffer a new blow of fate harder. And then, instead of mobilization, distress begins - a program of self-destruction of the body.
How can depression lead to suicide?
The algorithm from depressive mood to suicide is as follows.
First comes self-accusation: "Why did I do this and not do this?", "Probably should have said that?". This is followed by self-flagellation and humiliation: "I'm a loser, a loser", "I need to be like this ...". That is, a person gradually drives himself into a corner. When self-flagellation reaches the limit, thoughts about the aimlessness of life and the desire for death appear: “I am not capable of anything”, “I am not worthy to live in this world”, “I wish a brick fell on my head, I would get a serious illness, I'd get hit by a car to end it."
If at this stage you do not seek medical help, then thoughts become suicidal. The thought "I wish I was hit by a car" is transformed into "I'll go and throw myself under the car."
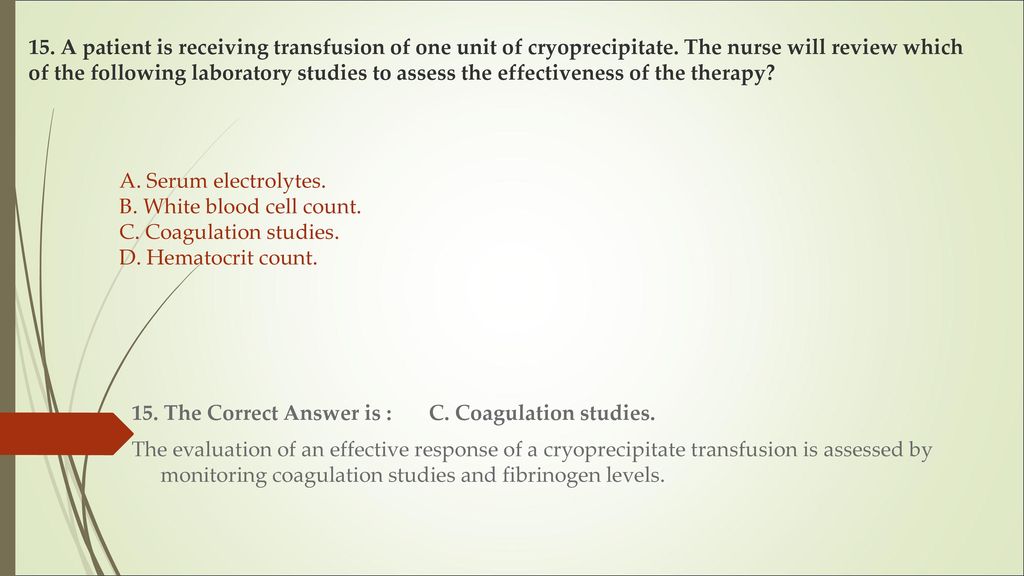
How is depression diagnosed?
The most popular test in clinical practice is the Hamilton scale. A person can go through it himself, calculate the points, and if he shows depression, then seek help. This is a significant aid to clinicians in identifying depression.
But psychiatrists and psychotherapists do not use scales in their work. They ask in great detail about the symptoms. Psychiatry and psychotherapy is the only branch of medicine that does not lend itself to any objective research methods. To diagnose depression, you can’t do, say, an ultrasound or MRI of the brain or a blood test. Will show nothing. Only a subjective, descriptive way of collecting information.
It is good if a person comes to an appointment with a specialist together with someone who will confirm and clarify the information. In principle, the diagnosis is made in one visit. If you suspect depression in a loved one, then you can give a test and persuade him to visit a specialist.
Who else can help?
The good news is that today in Kazakhstan not only psychotherapists and psychiatrists, but also therapists (GPs), neuropathologists, and endocrinologists can prescribe antidepressants. According to the order currently in force according to the standard of psychiatric care, general practitioners can treat borderline mental disorders: anxiety, fears, depression.
The first step in diagnosing depression for a person can be a psychologist. However, a truly competent specialist always cooperates with a psychiatrist, to whom he will redirect to confirm the diagnosis and prescribe medication. And after that, he will make a plan for his work.
Earlier in an interview with our publication, Zhibek Zholdasova spoke about the difference between a psychologist, psychotherapist and psychiatrist:
Psychologist helps healthy people to solve issues of emotions, interpersonal relationships, that is, to live better. A psychologist does not write prescriptions or make diagnoses.
Psychotherapist is a doctor with a specialization in psychotherapy, he prescribes drugs and carries out psychocorrection. He deals with neurosis and borderline mental disorders, when a person's condition significantly interferes with communication, work and raising children.
Psychiatrist - a more general medical education in mental disorders. Psychiatrists are divided into psychotherapists, narcologists, sex therapists, clinical and medical psychologists. People go to a psychiatrist with impaired attention, thinking, memory, perception, feelings, emotions, behavior and sensations. A psychiatrist deals with manifestations of a person that help to live in the world around him - to set goals and achieve them.
People with depression who do not reach specialists tend to self-medicate: they seek help from magicians, practice spiritual practices, go to healers and psychics, exorcise genies. But in fact, only a few manage to cope with depression on their own.
How is depression treated?
The main treatment for depression is antidepressants. Rumors about their harm are a post-Soviet myth: the old drugs did have a number of pronounced side effects. The current generation of antidepressants has a good level of tolerance. There are individual reactions, but by contacting a doctor, you can always change the drug or adjust the dosage.
There are individual reactions, but by contacting a doctor, you can always change the drug or adjust the dosage.
Drug treatment is prescribed for a course of 5-6 months. The effect of antidepressants appears after a week of taking: a person feels that life has improved, some kind of joy has appeared, sensations have changed, thoughts have become more blissful, not as pessimistic as before. Plus, a visit to a psychologist / psychotherapist is required.
The main treatment for all mental disorders - including depression, anxiety, fears - is psychotherapy. I explain to my patients this way: medicines do not solve problems, they only remove symptoms. This is a kind of crutch that will help to cope with unwanted symptoms, improve the quality of life. It becomes easier to go to work, anxiety goes away, sleep normalizes. A person, in principle, begins to better cope with life, remembers what it is to make plans, and enjoys life.
If the drugs are canceled, but the psychotherapist is not visited, then there is a possibility that the condition will return.