Who can diagnose schizophrenia
Diagnosis - Schizophrenia - NHS
There's no single test for schizophrenia and the condition is usually diagnosed after assessment by a specialist in mental health.
If you're concerned you may be developing symptoms of schizophrenia, see a GP as soon as possible. The earlier schizophrenia is treated, the better.
The GP will ask about your symptoms and check they're not the result of other causes, such as recreational drug use.
Community mental health team
If a diagnosis of schizophrenia is suspected, the GP should refer you to your local community mental health team (CMHT).
CMHTs are made up of different mental health professionals who support people with complex mental health conditions.
A member of the CMHT team, usually a psychiatrist or a specialist nurse, will carry out a more detailed assessment of your symptoms. They'll also want to know your personal history and current circumstances.
To make a diagnosis, most mental healthcare professionals use a diagnostic checklist.
Schizophrenia can usually be diagnosed if:
- you've experienced 1 or more of the following symptoms most of the time for a month: delusions, hallucinations, hearing voices, incoherent speech, or negative symptoms, such as a flattening of emotions
- your symptoms have had a significant impact on your ability to work, study or perform daily tasks
- all other possible causes, such as recreational drug use or bipolar disorder, have been ruled out
Related illnesses
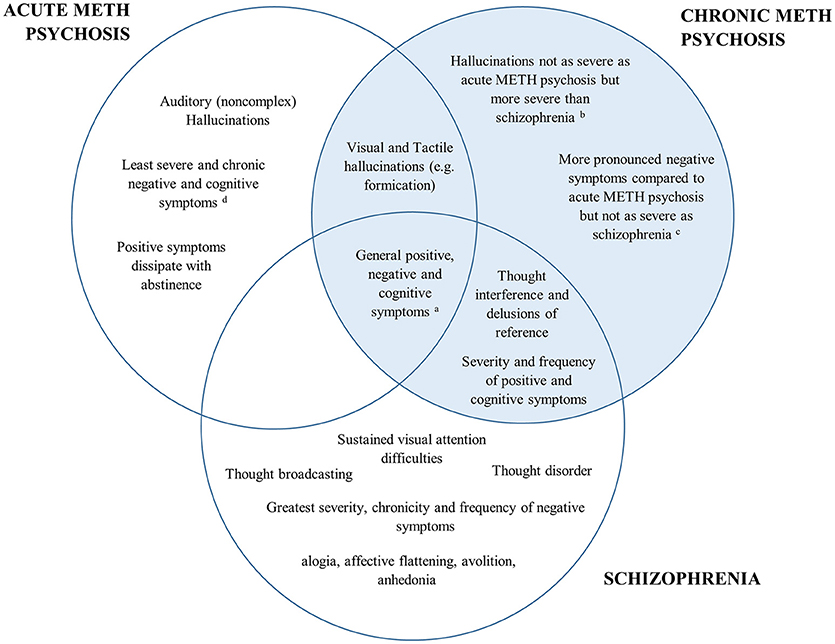
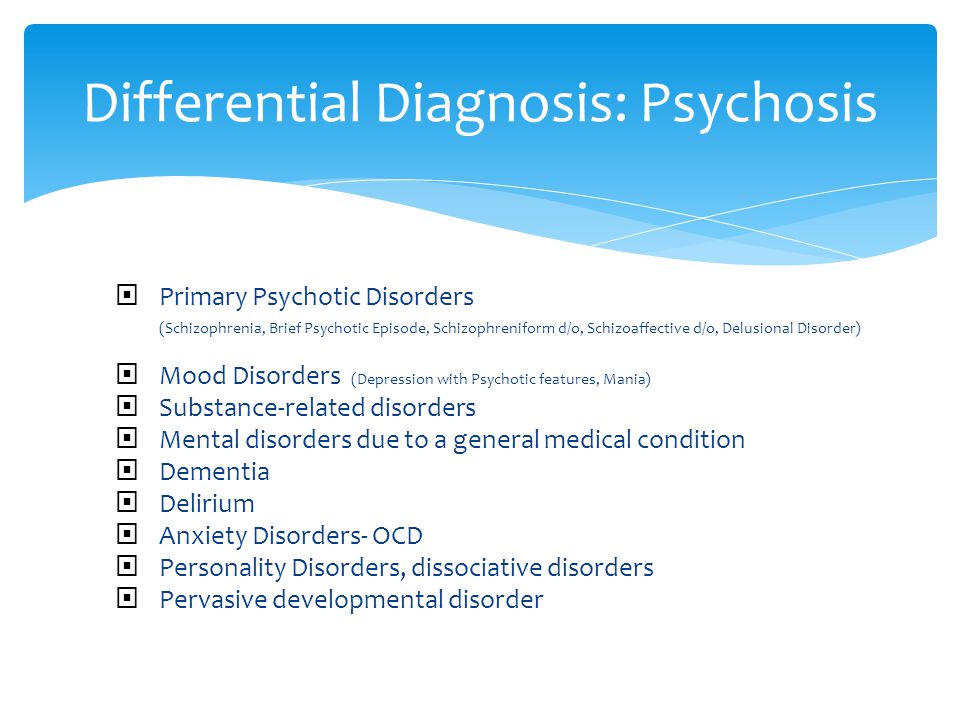
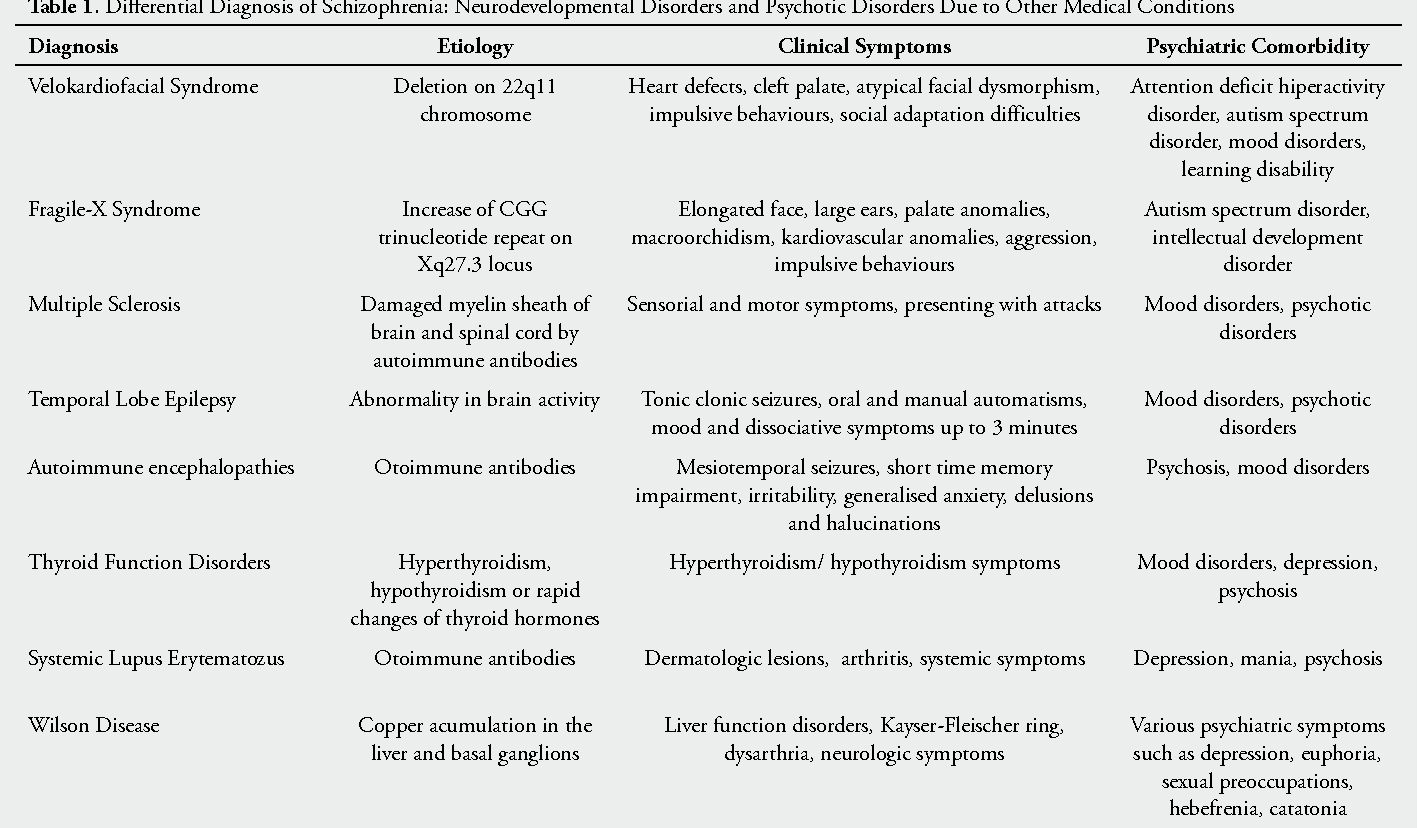
Sometimes it might not be clear whether someone has schizophrenia. If you have other symptoms at the same time, a psychiatrist may have reason to believe you have a related mental illness, such as:
- bipolar disorder – people with bipolar disorder swing from periods of elevated moods and extremely active, excited behaviour (mania) to periods of deep depression; some people also hear voices or experience other kinds of hallucinations, or may have delusions
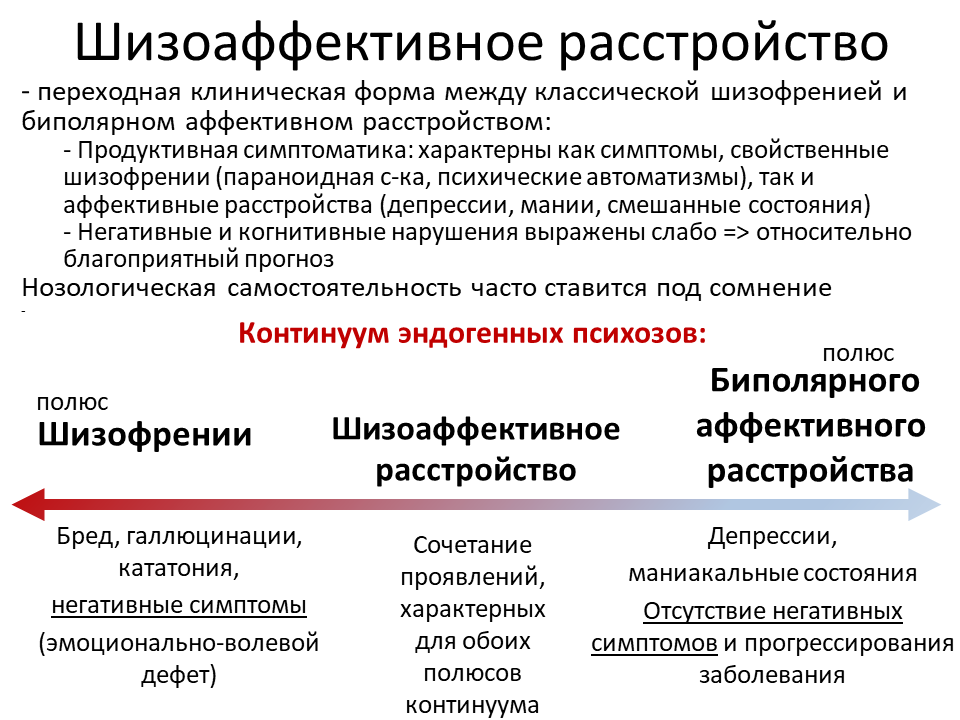
- schizoaffective disorder – this is often described as a form of schizophrenia because its symptoms are similar to schizophrenia and bipolar disorder, but schizoaffective disorder is a mental illness in its own right; it may occur just once in a person's life, or come and go and be triggered by stress
You may also be assessed for post-traumatic stress disorder, depression, anxiety and substance misuse.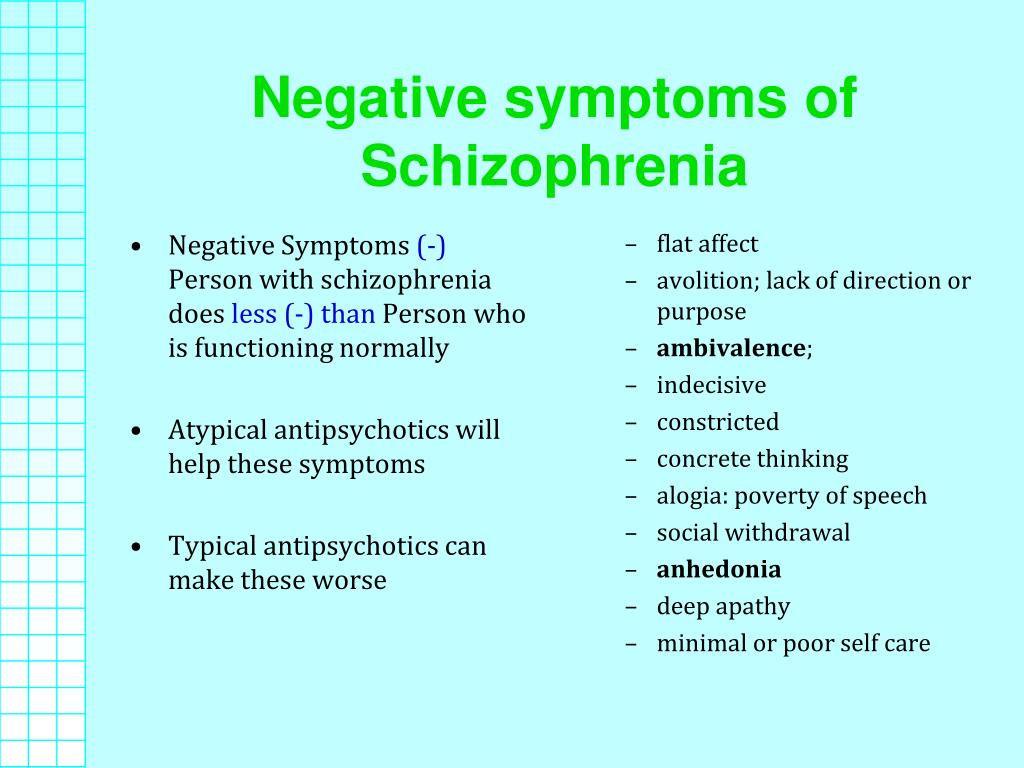
Getting help for someone else
As a result of their delusional thought patterns, people with schizophrenia may be reluctant to visit their GP if they believe there's nothing wrong with them.
It's likely someone who has had acute schizophrenic episodes in the past will have been assigned a care co-ordinator. If this is the case, contact the person's care co-ordinator to express your concerns.
If someone is having an acute schizophrenic episode for the first time, it may be necessary for a friend, relative or another loved one to persuade them to visit their GP.
In the case of a rapidly worsening schizophrenic episode, you may need to go to the accident and emergency (A&E) department, where a duty psychiatrist will be available.
If a person who is having an acute schizophrenic episode refuses to get help, their nearest relative can request that a mental health assessment is carried out. The social services department of your local authority can advise how to do this. Find your local authority.
Find your local authority.
In severe cases, people can be compulsorily detained in hospital for assessment and treatment under the Mental Health Act (2007).
After diagnosis
If you or a friend or relative are diagnosed with schizophrenia, you may feel anxious about what will happen. You may be worried about the stigma attached to the condition, or feel frightened and withdrawn.
It's important to remember that a diagnosis can be a positive step towards getting good, straightforward information about the illness and the kinds of treatment and services available.
Diagnosing children and young people
Children and young people with a first episode of schizophrenia should be referred urgently to a specialist mental health service.
This should be either children and young people's mental health services (CYPMHHS) for those aged up to 17, or an early intervention service for those aged 14 years or over, that includes a consultant psychiatrist with training in children and young people's mental health.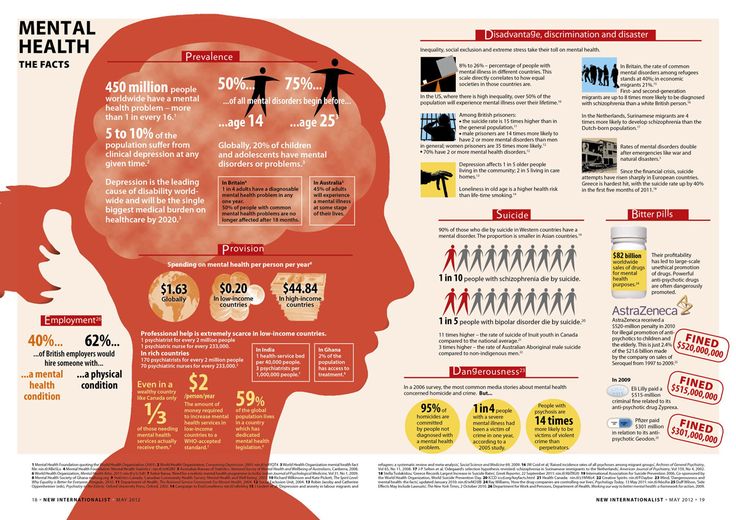
For more information, see the National Institute for Health and Care Excellence (NICE) guidelines on psychosis and schizophrenia in children and young people.
Page last reviewed: 11 November 2019
Next review due: 11 November 2022
Schizophrenia - Diagnosis and treatment
Diagnosis
Diagnosis of schizophrenia involves ruling out other mental health disorders and determining that symptoms are not due to substance abuse, medication or a medical condition. Determining a diagnosis of schizophrenia may include:
- Physical exam. This may be done to help rule out other problems that could be causing symptoms and to check for any related complications.
- Tests and screenings. These may include tests that help rule out conditions with similar symptoms, and screening for alcohol and drugs. The doctor may also request imaging studies, such as an MRI or CT scan.
- Psychiatric evaluation. A doctor or mental health professional checks mental status by observing appearance and demeanor and asking about thoughts, moods, delusions, hallucinations, substance use, and potential for violence or suicide. This also includes a discussion of family and personal history.
- Diagnostic criteria for schizophrenia. A doctor or mental health professional may use the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
More Information
- CT scan
- MRI
Treatment
Schizophrenia requires lifelong treatment, even when symptoms have subsided. Treatment with medications and psychosocial therapy can help manage the condition. In some cases, hospitalization may be needed.
A psychiatrist experienced in treating schizophrenia usually guides treatment. The treatment team also may include a psychologist, social worker, psychiatric nurse and possibly a case manager to coordinate care.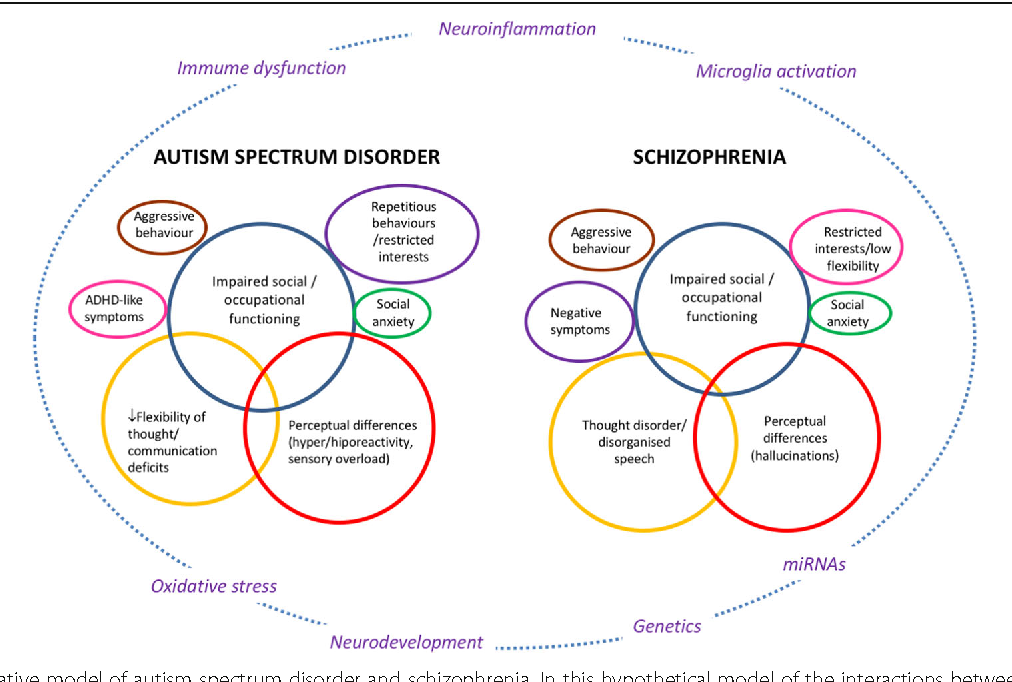 The full-team approach may be available in clinics with expertise in schizophrenia treatment.
The full-team approach may be available in clinics with expertise in schizophrenia treatment.
Medications
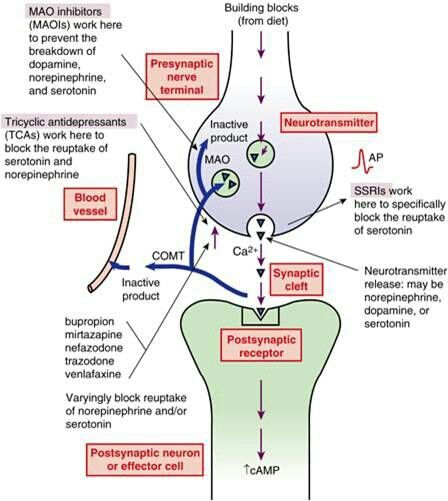
Medications are the cornerstone of schizophrenia treatment, and antipsychotic medications are the most commonly prescribed drugs. They're thought to control symptoms by affecting the brain neurotransmitter dopamine.
The goal of treatment with antipsychotic medications is to effectively manage signs and symptoms at the lowest possible dose. The psychiatrist may try different drugs, different doses or combinations over time to achieve the desired result. Other medications also may help, such as antidepressants or anti-anxiety drugs. It can take several weeks to notice an improvement in symptoms.
Because medications for schizophrenia can cause serious side effects, people with schizophrenia may be reluctant to take them. Willingness to cooperate with treatment may affect drug choice. For example, someone who is resistant to taking medication consistently may need to be given injections instead of taking a pill.
Ask your doctor about the benefits and side effects of any medication that's prescribed.
Second-generation antipsychotics
These newer, second-generation medications are generally preferred because they pose a lower risk of serious side effects than do first-generation antipsychotics. Second-generation antipsychotics include:
- Aripiprazole (Abilify)
- Asenapine (Saphris)
- Brexpiprazole (Rexulti)
- Cariprazine (Vraylar)
- Clozapine (Clozaril, Versacloz)
- Iloperidone (Fanapt)
- Lurasidone (Latuda)
- Olanzapine (Zyprexa)
- Paliperidone (Invega)
- Quetiapine (Seroquel)
- Risperidone (Risperdal)
- Ziprasidone (Geodon)
First-generation antipsychotics
These first-generation antipsychotics have frequent and potentially significant neurological side effects, including the possibility of developing a movement disorder (tardive dyskinesia) that may or may not be reversible.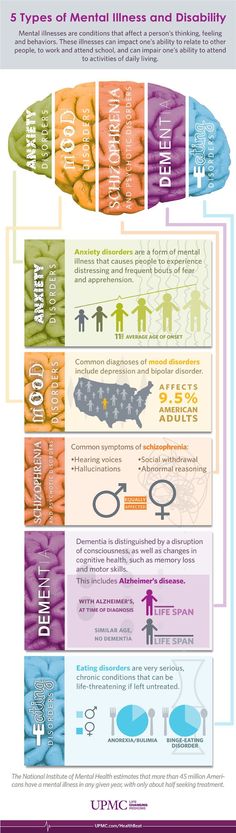 First-generation antipsychotics include:
First-generation antipsychotics include:
- Chlorpromazine
- Fluphenazine
- Haloperidol
- Perphenazine
These antipsychotics are often cheaper than second-generation antipsychotics, especially the generic versions, which can be an important consideration when long-term treatment is necessary.
Long-acting injectable antipsychotics
Some antipsychotics may be given as an intramuscular or subcutaneous injection. They are usually given every two to four weeks, depending on the medication. Ask your doctor about more information on injectable medications. This may be an option if someone has a preference for fewer pills and may help with adherence.
Common medications that are available as an injection include:
- Aripiprazole (Abilify Maintena, Aristada)
- Fluphenazine decanoate
- Haloperidol decanoate
- Paliperidone (Invega Sustenna, Invega Trinza)
- Risperidone (Risperdal Consta, Perseris)
Psychosocial interventions
Once psychosis recedes, in addition to continuing on medication, psychological and social (psychosocial) interventions are important.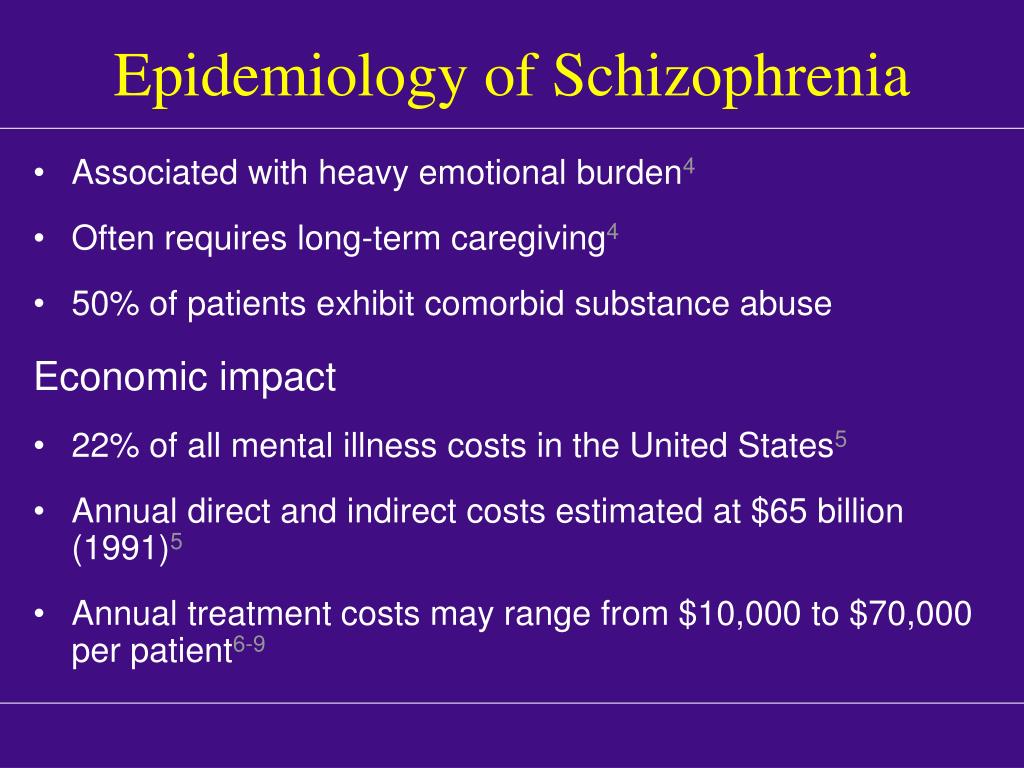 These may include:
These may include:
- Individual therapy. Psychotherapy may help to normalize thought patterns. Also, learning to cope with stress and identify early warning signs of relapse can help people with schizophrenia manage their illness.
- Social skills training. This focuses on improving communication and social interactions and improving the ability to participate in daily activities.
- Family therapy. This provides support and education to families dealing with schizophrenia.
- Vocational rehabilitation and supported employment. This focuses on helping people with schizophrenia prepare for, find and keep jobs.
Most individuals with schizophrenia require some form of daily living support. Many communities have programs to help people with schizophrenia with jobs, housing, self-help groups and crisis situations. A case manager or someone on the treatment team can help find resources.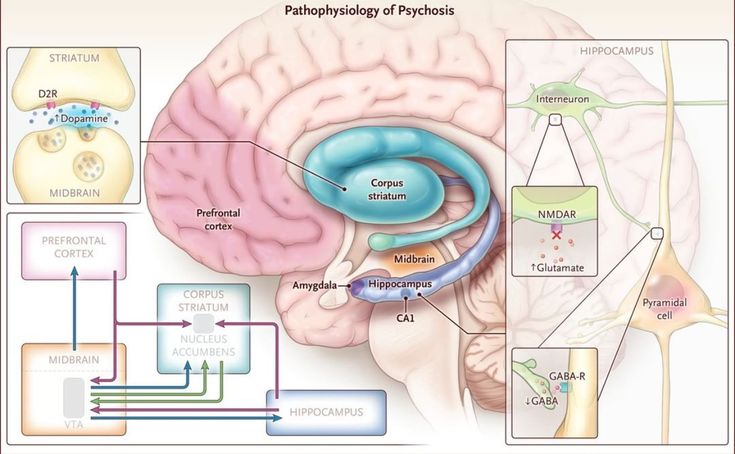 With appropriate treatment, most people with schizophrenia can manage their illness.
With appropriate treatment, most people with schizophrenia can manage their illness.
Hospitalization
During crisis periods or times of severe symptoms, hospitalization may be necessary to ensure safety, proper nutrition, adequate sleep and basic hygiene.
Electroconvulsive therapy
For adults with schizophrenia who do not respond to drug therapy, electroconvulsive therapy (ECT) may be considered. ECT may be helpful for someone who also has depression.
More Information
- Family therapy
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.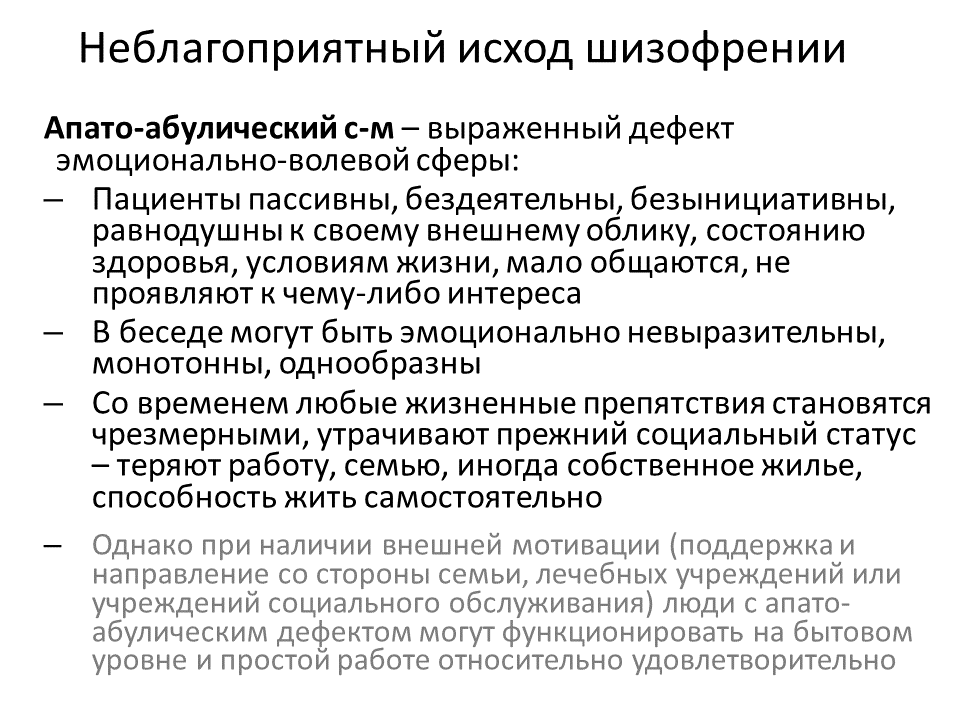 If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Coping and support
Coping with a mental disorder as serious as schizophrenia can be challenging, both for the person with the condition and for friends and family. Here are some ways to cope:
- Learn about schizophrenia. Education about the disorder can help the person with schizophrenia understand the importance of sticking to the treatment plan. Education can help friends and family understand the disorder and be more compassionate with the person who has it.
- Stay focused on goals. Managing schizophrenia is an ongoing process. Keeping treatment goals in mind can help the person with schizophrenia stay motivated. Help your loved one remember to take responsibility for managing the disorder and working toward goals.
- Avoid alcohol and drug use. Using alcohol, nicotine or recreational drugs can make it difficult to treat schizophrenia. If your loved one is addicted, quitting can be a real challenge. Get advice from the health care team on how best to approach this issue.
- Ask about social services assistance. These services may be able to assist with affordable housing, transportation and other daily activities.
- Learn relaxation and stress management. The person with schizophrenia and loved ones may benefit from stress-reduction techniques such as meditation, yoga or tai chi.
- Join a support group. Support groups for people with schizophrenia can help them reach out to others facing similar challenges.
 Support groups may also help family and friends cope.
Support groups may also help family and friends cope.
Preparing for your appointment
If you're seeking help for someone with schizophrenia, you may start by seeing his or her family doctor or health care professional. However, in some cases when you call to set up an appointment, you may be referred immediately to a psychiatrist.
What you can do
To prepare for the appointment, make a list of:
- Any symptoms your loved one is experiencing, including any that may seem unrelated to the reason for the appointment
- Key personal information, including any major stresses or recent life changes
- Medications, vitamins, herbs and other supplements that he or she is taking, including the dosages
- Questions to ask the doctor
Go with your loved one to the appointment. Getting the information firsthand will help you know what you're facing and what you need to do for your loved one.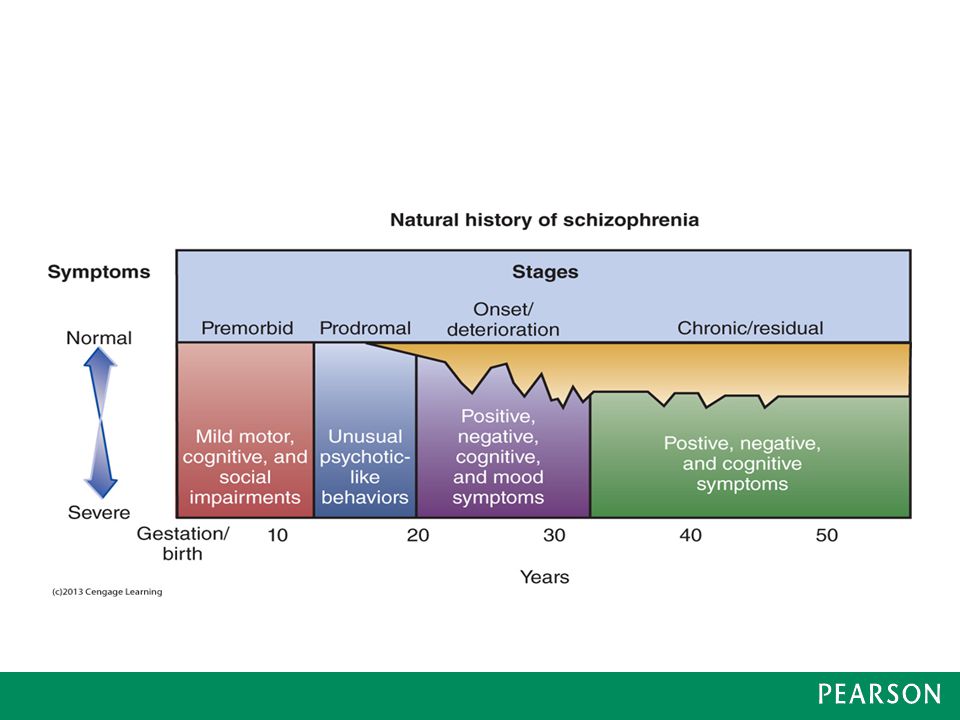
For schizophrenia, some basic questions to ask the doctor include:
- What's likely causing the symptoms or condition?
- What are other possible causes for the symptoms or condition?
- What kinds of tests are needed?
- Is this condition likely temporary or lifelong?
- What's the best treatment?
- What are the alternatives to the primary approach you're suggesting?
- How can I be most helpful and supportive?
- Do you have any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
The doctor is likely to ask you a number of questions. Anticipating some of these questions can help make the discussion productive. Questions may include:
- What are your loved one's symptoms, and when did you first notice them?
- Has anyone else in your family been diagnosed with schizophrenia?
- Have symptoms been continuous or occasional?
- Has your loved one talked about suicide?
- How well does your loved one function in daily life — is he or she eating regularly, going to work or school, bathing regularly?
- Has your loved one been diagnosed with any other medical conditions?
- What medications is your loved one currently taking?
The doctor or mental health professional will ask additional questions based on responses, symptoms and needs.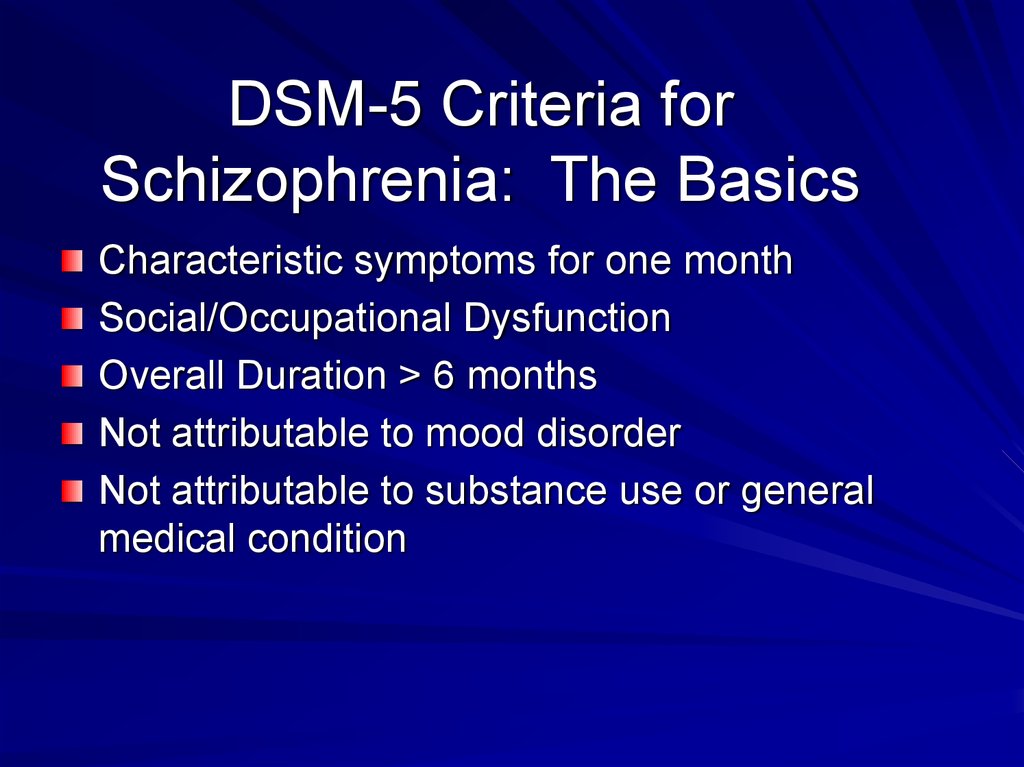
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Schizophrenia
Schizophrenia is a serious mental disorder in which the patient suffers from hallucinations (most often auditory), his interpretation of reality is distorted, delirium begins (false fixed beliefs), impaired thinking, behavior. The social activity of a person depends on the severity of the disease. Approximately 10% of patients commit suicide, about 80% experience depression at least once in their lives.
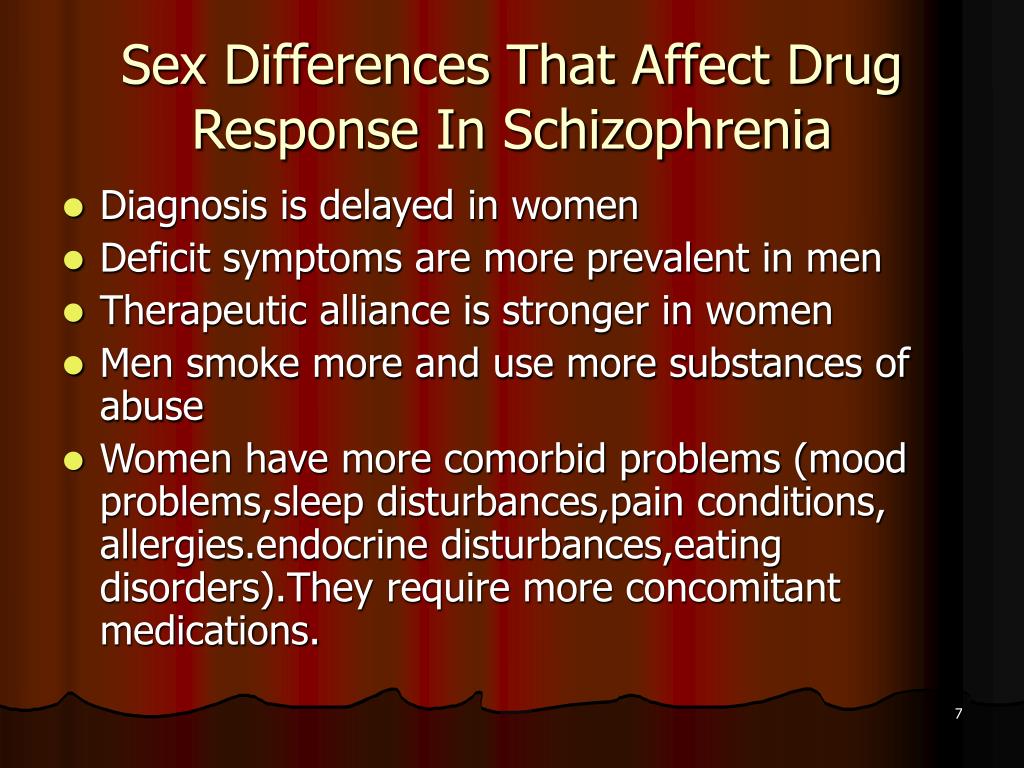
The average age of onset of the disease in men is 18 years, in women - 25. Over the years, the severity of the disease may decrease, the most difficult period is the first 5-10 years.
Contrary to popular belief, schizophrenia is not a split personality disorder.
This is a life-long chronic disease that requires constant treatment: medication and psychotherapy.
Synonyms Russian
Bleuler's disease, discordant psychosis, schizophrenic psychosis, latent schizophrenia, paranoid schizophrenia, dementia praecox.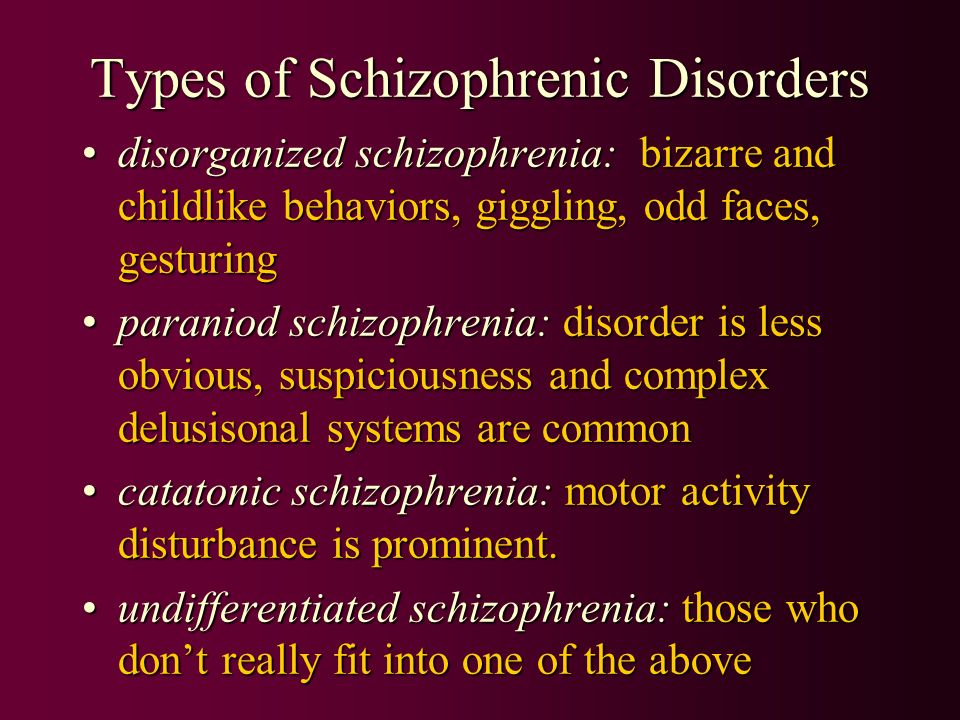
English synonyms
Schizophrenia, Schizophrenic disorder, Schizophrenic psychosis, Dementia praecox.
Symptoms
12-24 months before the onset of the disease, in some cases, there may be slight distortions in perception, cognitive function, decreased ability to experience pleasure, difficulty in solving problems, irritability, suspicion, social isolation. In men, the first symptoms of schizophrenia most often appear at the age of 16-20, in women - at about 25. In childhood and after 45 years, schizophrenia begins extremely rarely.
Symptoms of the disease are divided into groups.
1. Positive symptoms.
- Delirium - false beliefs. The patient may feel threatened, followed, followed. It may seem to him that excerpts from books, newspapers, films are addressed directly to him. The schizophrenic may believe that others are able to read his thoughts, that thoughts and actions are put into him by external forces.
- Hallucinations are images that appear in the mind. They can be auditory, visual, olfactory, gustatory, tactile. The most common in schizophrenia are auditory: the patient can hear voices commenting on his actions, talking to each other, making critical or offensive remarks. Hallucinations can be extremely unpleasant for the patient and even lead to threatening consequences, for example, if voices order him to do something that could harm others.
- Thinking disorders - disorganized thinking with incoherent speech, with constant transitions from one topic to another.
- Inadequate behavior can be manifested by childish naivety, stupidity, excitement, inappropriate appearance and actions, unreasonable joy or sadness.
2. Negative symptoms.
- Loss of interest in daily activities, neglect of personal hygiene.
- Absence of emotions.
- Violation of the ability to plan one's actions.
- Social isolation, lack of facial expressions, expressionlessness of the face, lack of eye contact when communicating.
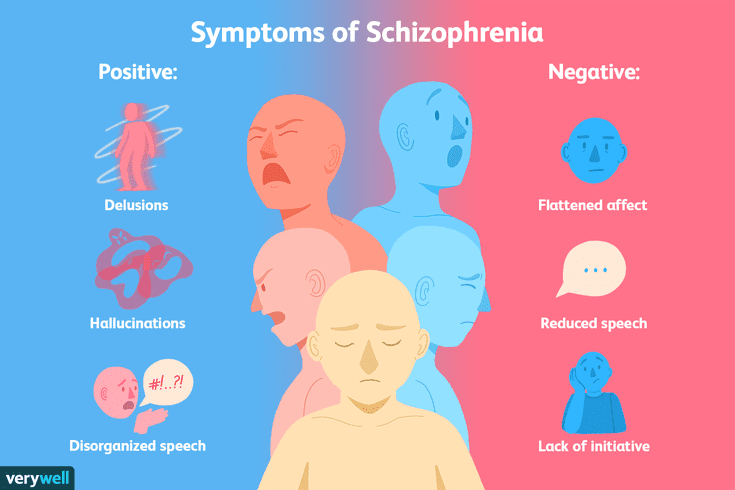
- Poverty of speech: monosyllabic answers, laconicism.
- Problems with comprehending information, abstract thinking, understanding social connections. The ability to solve problems, understand other people's points of view, and analyze one's own experience is lost.
- Disorders of attention, memory.
Symptoms of schizophrenia often lead to a violation of the socialization of the patient: he may lose his job, family, friends, stop taking care of himself.
It is noteworthy that people with schizophrenia are often unaware of their illness and consider themselves healthy, refusing treatment.
General information about the disease
Schizophrenia is a serious mental disorder in which the patient has hallucinations, the interpretation of reality is distorted, there is delirium, thinking, behavior, and social adaptation are disturbed.
Although the causes of the disease have not yet been established, it is known that schizophrenia has a biological basis - damage to the brain structure: an increase in the ventricles of the brain, a decrease in some of its areas, a violation of the activity of biologically active substances (dopamine and glutamate).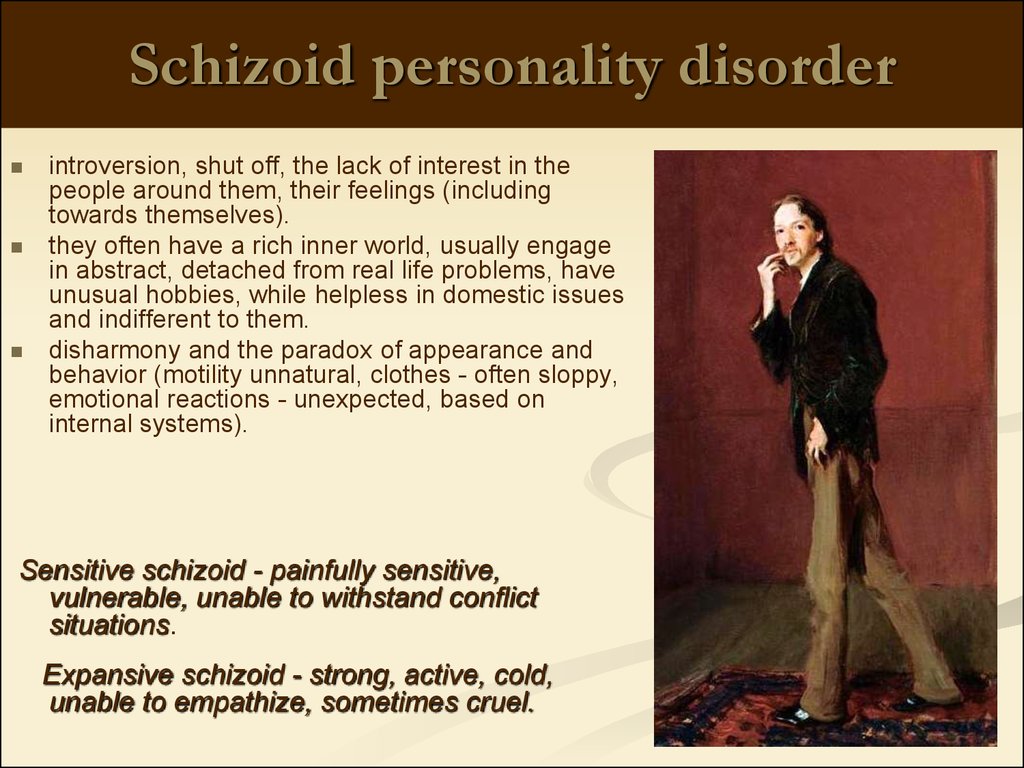
It is believed that schizophrenia can be caused by genetic factors and factors affecting the fetus during pregnancy and childbirth:
- genetic predisposition - if both parents have schizophrenia, the risk of developing schizophrenia in a child is 40%;
- complications during pregnancy, childbirth or the first years of life, such as maternal malnutrition during pregnancy, flu in the 2nd trimester of pregnancy, Rh incompatibility of the child with the mother, low birth weight, hypoxia (oxygen deprivation), and others
Schizophrenia is a chronic disease that must be treated throughout a person's life. Approximately 1-2 years before the onset of the disease, distortions of perception and thinking of the patient may appear, difficulties in solving problems, irritability, suspicion, and social isolation are observed. The onset of the disease (delusions, hallucinations) can be sudden (over weeks or months) or slow (over several years). The severity of the disease can vary from mild to severe.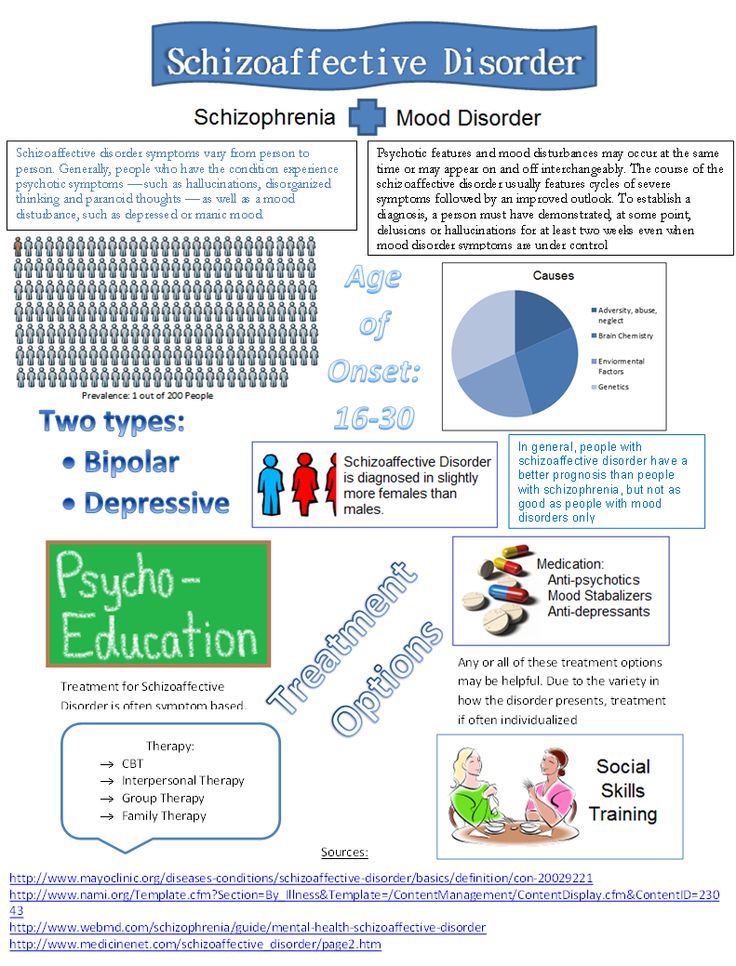
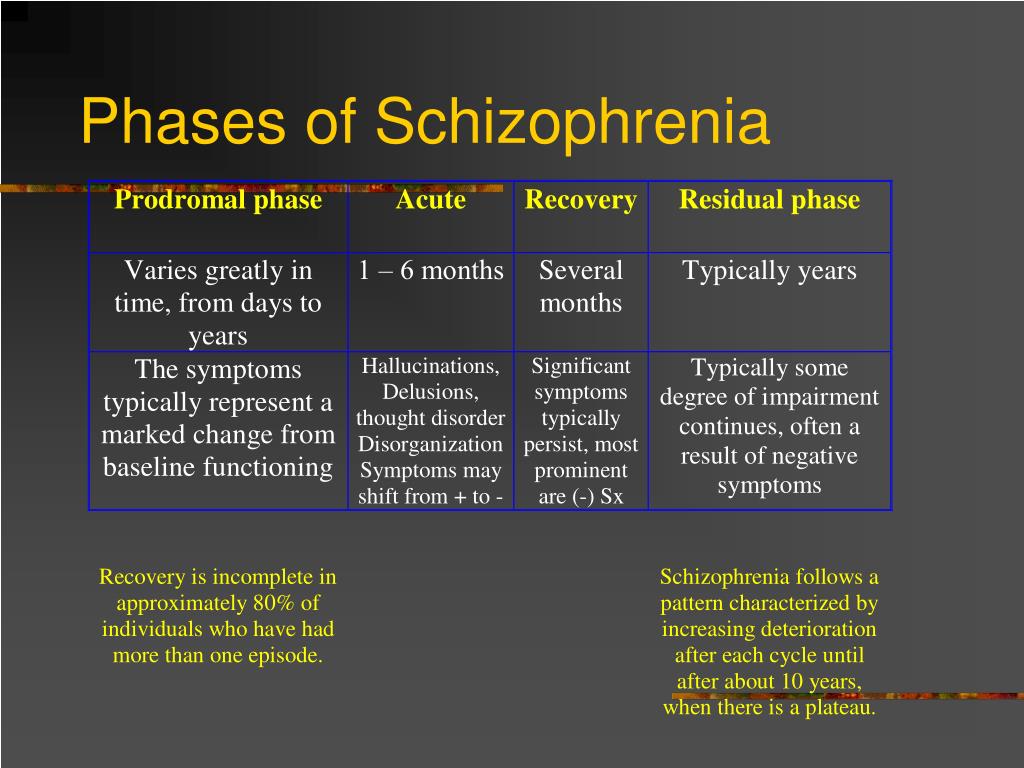
Types of schizophrenia course: a) episodic - with exacerbations and remissions, b) continuous. The most difficult period of the disease is the first 5-10 years from the onset of schizophrenia, after which approximately 10 years of stability occurs. Then the severity of the disease may decrease.
The following forms of schizophrenia are distinguished:
- paranoid - characterized by delusions and auditory hallucinations, while thinking and emotional sphere do not suffer;
- disorganized - characterized by disorganization of speech, behavior, inadequacy;
- catatonic - impaired activity - either immobility or excessive activity and the adoption of frilly postures;
- undifferentiated - a combination of various symptoms of the disease;
- residual - when schizophrenia with pronounced symptoms is followed by a long period of moderately severe negative symptoms.
If left untreated, schizophrenia can lead to serious mental and behavioral problems:
- suicide, harm to one's own health, about 10% of patients commit suicide;
- depression - 80% of schizophrenics have it at least once in their lives;
- abuse of alcohol, drugs;
- homelessness, asociality;
- aggressiveness - with delusional ideas of persecution; hallucinations calling for violence and non-compliance with the prescribed treatment.
Who is at risk?
- Having relatives with schizophrenia.
- Exposure to viruses, toxins, malnutrition (especially in the first and second trimesters) during the mother's pregnancy.
- Persons who have undergone severe stressful situations, shocks.
- Persons whose father's age at the time of conception was over 60 years.
- Substance users.
Diagnosis
The diagnosis of "schizophrenia" is made by a psychiatrist on the basis of a long-term comprehensive study of the history of the disease, the mental state of a person, his behavior, the symptoms of the disease. There are no changes in the analyzes characteristic of schizophrenia.
Additional testing, including a neurological consultation, may be done to rule out other medical conditions or substance abuse.
Laboratory tests
- Complete blood count
- Thyroid-stimulating hormone (TSH), which characterizes the function of the thyroid gland.

In some situations, determination may be indicated:
- Blood and urine levels of drugs and heavy metals
- The level of cortisol, a hormone produced by the adrenal glands. With its excess or deficiency in the body, the mental status of a person can change.
Other research methods
- Computed tomography (CT) and magnetic resonance imaging (MRI) of the brain. These studies are performed in order to exclude volumetric formations of the brain, hemorrhages.
- Electroencephalography (EEG). In some cases, an EEG is required, a research method that evaluates the electrical potentials of the brain.
In all cases, the extent of the examination is determined by the attending physician.
Treatment
Schizophrenia is a chronic disease that requires lifelong treatment, even if symptoms are rare and less severe. Treatment involves taking medications (neuroleptics), psychotherapy and rehabilitation of a schizophrenic.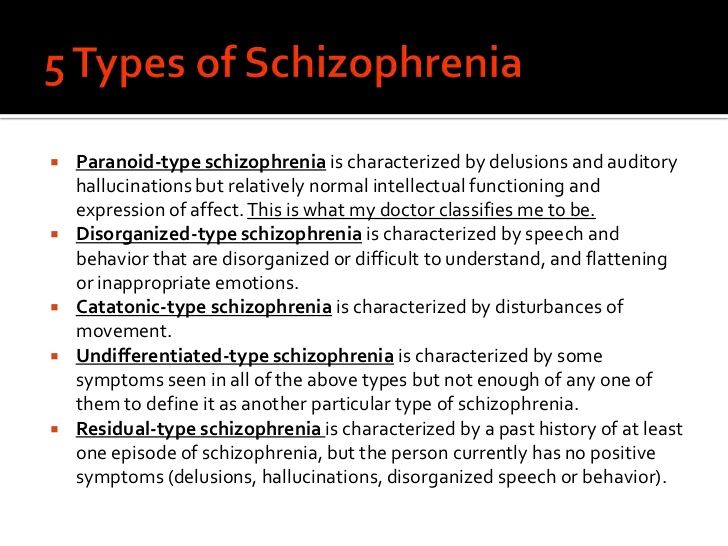
The patient may need to be hospitalized in a neuropsychiatric dispensary, especially during exacerbations and attacks of schizophrenia.
Side effects of antipsychotics include weight gain, diabetes, and high blood cholesterol levels.
Rehabilitation of the patient is aimed at the socialization of the patient, instilling in him social skills, professional rehabilitation, training.
Prevention
There is no way to prevent schizophrenia.
People at increased risk of developing schizophrenia should stop using alcohol, drugs, psychotropic substances; avoid exposure to mental and emotional stress, overwork, lack of sleep. At the first signs of the disease, it is necessary to consult a specialist and begin treatment.
To prevent severe attacks and complications of schizophrenia, the treatment plan prescribed by the doctor must be strictly followed, lifelong therapy and periodic stay in a medical institution are possible to avoid attacks and exacerbations of the disease.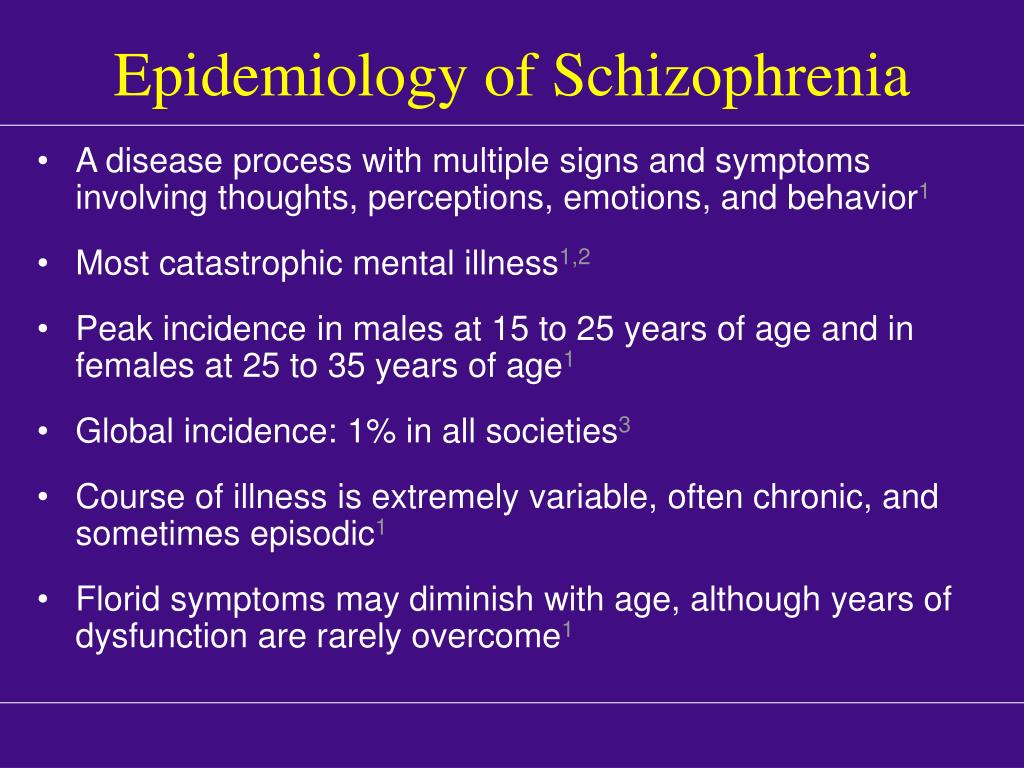
Recommended tests
- CBC
- Thyroid Stimulating Hormone (TSH)
- Cortisol
- Screening for the presence of narcotic, psychotropic and potent substances
Literature
- Dan L. Longo, Dennis L. Kasper, J. Larry Jameson, Anthony S. Fauci, Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill Medical Publishing Division, 2011.
Schizophrenia - Adamant Medical Clinic
Adamant
medical clinic
St. Petersburg, Moika river embankment, 78.
+7 (812) 740-20-90
Content:
Schizophrenia is a mental disorder in which there is a breakdown of thought processes and emotional reactions. The disease does not cause disturbances in consciousness and does not change many intellectual processes, however, with its prolonged course, perception, memory and attention are disturbed.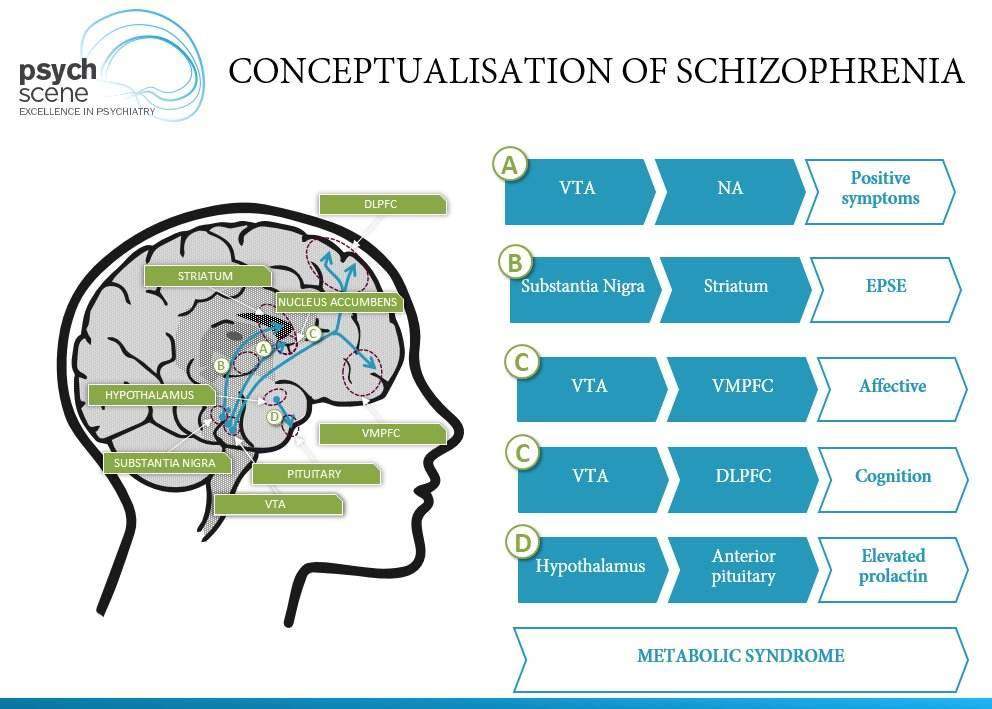
Lack of treatment leads to a complete loss of a sense of one's own "I", the loss of the integrity of a person's personality. In order to avoid this, it is necessary to diagnose the signs of schizophrenia in a timely manner and start treatment as soon as possible.
Symptoms of schizophrenia
Schizophrenia develops for a long time and imperceptibly for the patient. The first signs appear when a person is sure that he is completely healthy.
Early symptoms of schizophrenia:
- Isolation from society, unsociableness.
- Indifference to yourself, friends and family.
- Emotional coldness.
- Gradual loss of interest in everything that previously worried.
- Sleep disorders.
Adolescents often experience these symptoms during the transition period. However, in any case, take a closer look at your child and consult a doctor if you suspect.
As the disease progresses, common symptoms and signs of schizophrenia occur:
-
Psychotic (positive):
- Hallucinations - the patient sees and hears what is not there.
- Nonsense - illogical beliefs in which the patient cannot be persuaded.
- Disorderly thinking - the patient either speaks too quickly, then stops in the middle of a thought and at the same time names non-existent words.
- Unnatural movements - a patient with schizophrenia moves slowly and freezes in an unnatural position, or vice versa moves too quickly and jerkily.
- Hallucinations - the patient sees and hears what is not there.
-
Negative:
- Inability to express emotions - the patient constantly looks depressed and out of touch with reality.
- Violation of the thought process - the patient does not absorb information well, cannot concentrate and forgets everything.
In order to alleviate the situation of the patient, it is necessary to urgently consult a doctor and not push the patient away from himself. Remember that all changes in a person's personality are not his fault, but a manifestation of the disease.
Treatment of schizophrenia
Unfortunately, there is currently no cure for schizophrenia. The doctor can only alleviate the course of the disease. However, this is not a reason to put an end to yourself or your loved one. In the UK, people with schizophrenia even find employment, work successfully and lead a normal life.
From a medical point of view, the ideal solution for the treatment of schizophrenia is the placement of a patient in a hospital. Especially during an exacerbation of the disease. However, it should be borne in mind that hospitalizations are a great stress for a person who is associated with a restriction of freedom. Before doing so, consider possible alternatives.
The main treatment for schizophrenia is drug therapy. After a thorough diagnosis, the doctor individually prescribes a set of drugs that extinguishes the manifestations of the disease.
In addition to drug therapy, the patient needs professional psychological help and support from loved ones.