Which is a negative symptom of schizophrenia
Symptoms - Schizophrenia - NHS
Schizophrenia changes how a person thinks and behaves.
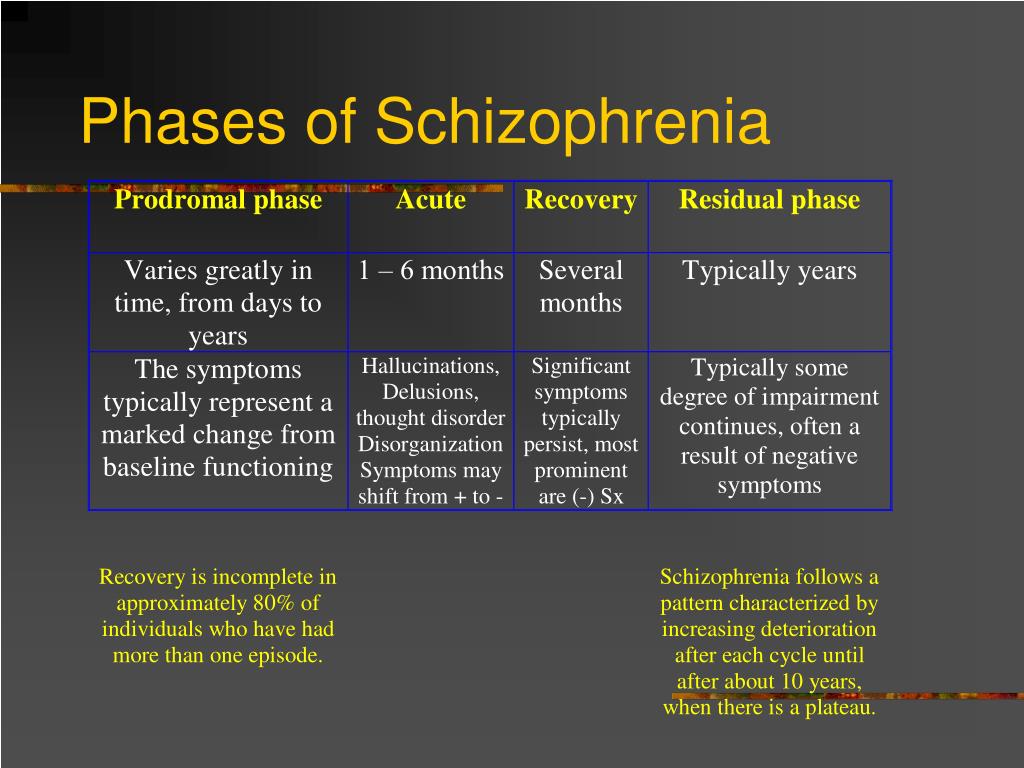
The condition may develop slowly. The first signs can be hard to identify as they often develop during the teenage years.
Symptoms such as becoming socially withdrawn and unresponsive or changes in sleeping patterns can be mistaken for an adolescent "phase".
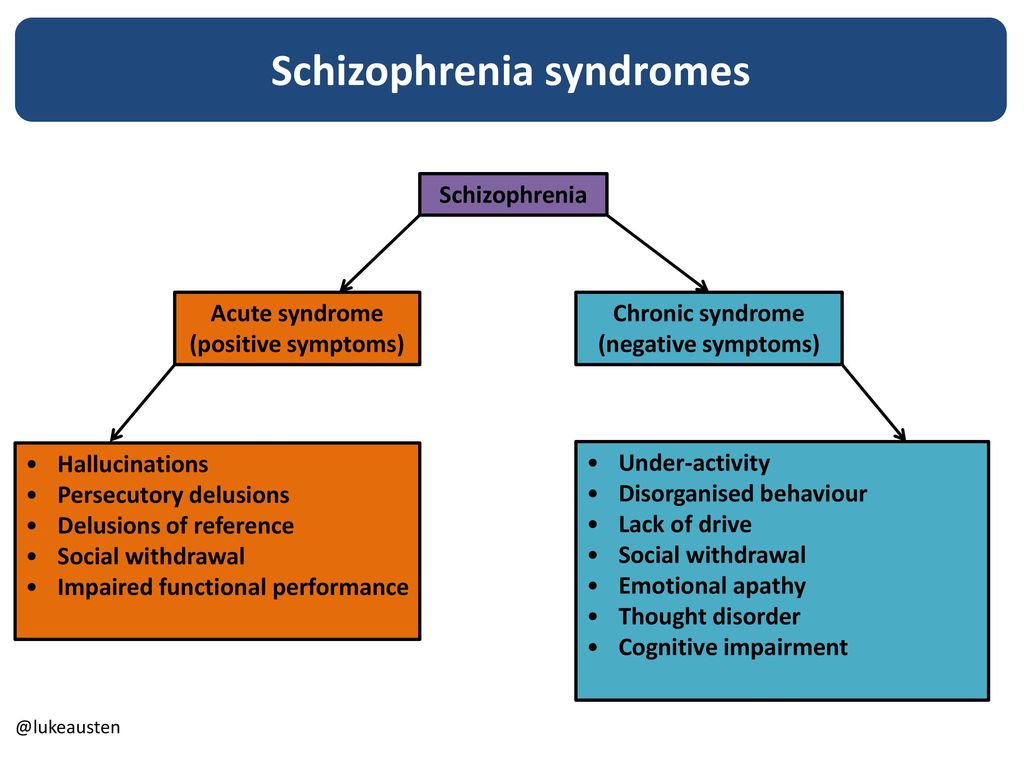
People often have episodes of schizophrenia, during which their symptoms are particularly severe, followed by periods where they experience few or no symptoms. This is known as acute schizophrenia.
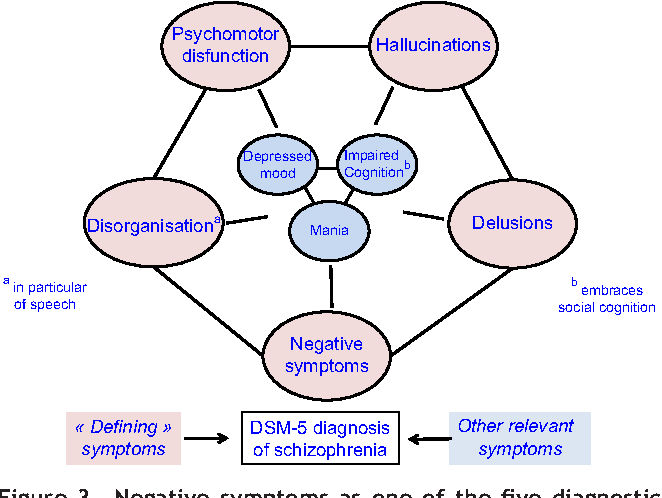
Positive and negative symptoms
The symptoms of schizophrenia are usually classified into:
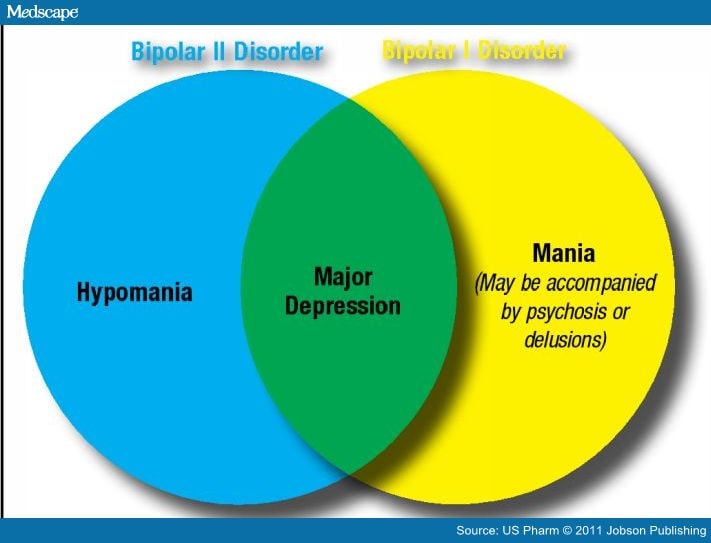
- positive symptoms – any change in behaviour or thoughts, such as hallucinations or delusions
- negative symptoms – where people appear to withdraw from the world around then, take no interest in everyday social interactions, and often appear emotionless and flat
Hallucinations
Hallucinations are where someone sees, hears, smells, tastes or feels things that do not exist outside their mind. The most common hallucination is hearing voices.
Hallucinations are very real to the person experiencing them, even though people around them cannot hear the voices or experience the sensations.
Research using brain-scanning equipment shows changes in the speech area in the brains of people with schizophrenia when they hear voices. These studies show the experience of hearing voices as a real one, as if the brain mistakes thoughts for real voices.
Some people describe the voices they hear as friendly and pleasant, but more often they're rude, critical, abusive or annoying.
The voices might describe activities taking place, discuss the hearer's thoughts and behaviour, give instructions, or talk directly to the person. Voices may come from different places or 1 place, such as the television.
Delusions
A delusion is a belief held with complete conviction, even though it's based on a mistaken, strange or unrealistic view. It may affect the way the person behaves.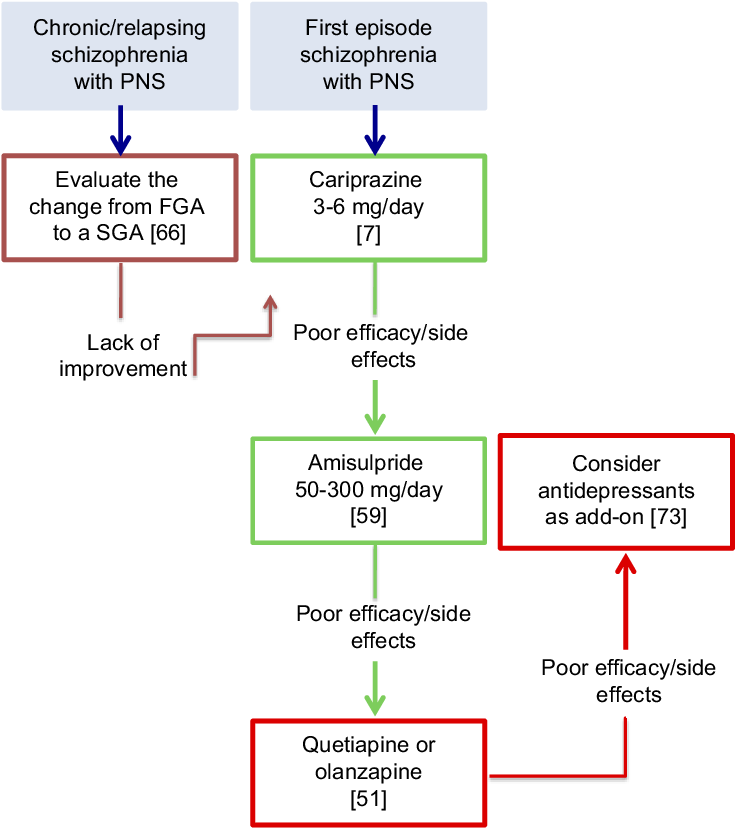 Delusions can begin suddenly or may develop over weeks or months.
Delusions can begin suddenly or may develop over weeks or months.
Some people develop a delusional idea to explain a hallucination they're having. For example, if they have heard voices describing their actions, they may have a delusion that someone is monitoring their actions.
Someone experiencing a paranoid delusion may believe they're being harassed or persecuted. They may believe they're being chased, followed, watched, plotted against or poisoned, often by a family member or friend.
Some people who experience delusions find different meanings in everyday events or occurrences.
They may believe people on TV or in newspaper articles are communicating messages to them alone, or that there are hidden messages in the colours of cars passing on the street.
Confused thoughts (thought disorder)
People experiencing psychosis often have trouble keeping track of their thoughts and conversations.
Some people find it hard to concentrate and will drift from one idea to another.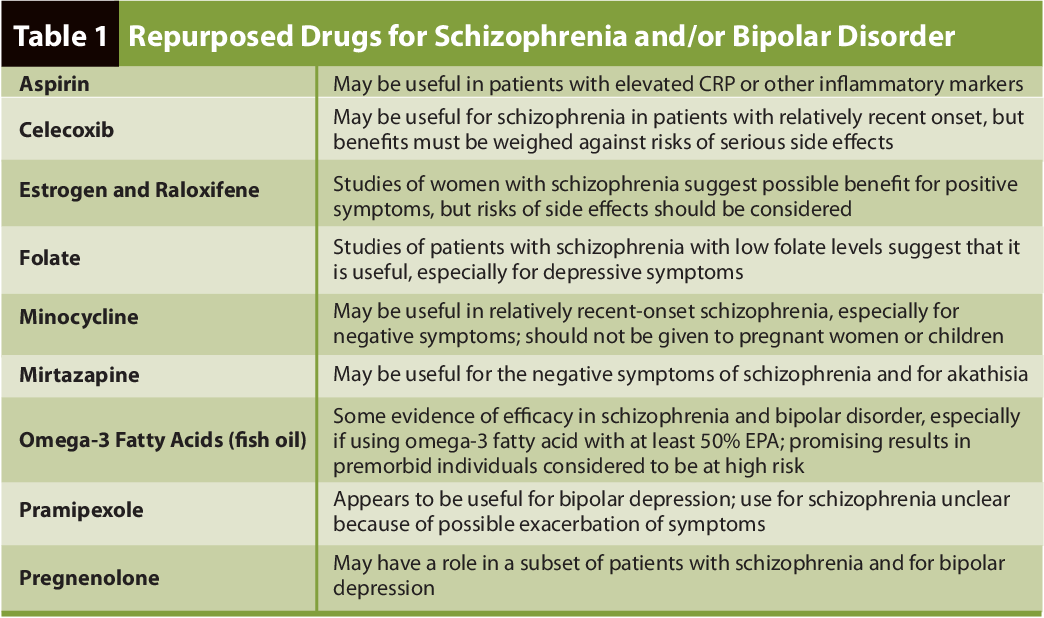 They may have trouble reading newspaper articles or watching a TV programme.
They may have trouble reading newspaper articles or watching a TV programme.
People sometimes describe their thoughts as "misty" or "hazy" when this is happening to them. Thoughts and speech may become jumbled or confused, making conversation difficult and hard for other people to understand.
Changes in behaviour and thoughts
A person's behaviour may become more disorganised and unpredictable.
Some people describe their thoughts as being controlled by someone else, that their thoughts are not their own, or that thoughts have been planted in their mind by someone else.
Another feeling is that thoughts are disappearing, as though someone is removing them from their mind.
Some people feel their body is being taken over and someone else is directing their movements and actions.
Negative symptoms of schizophrenia
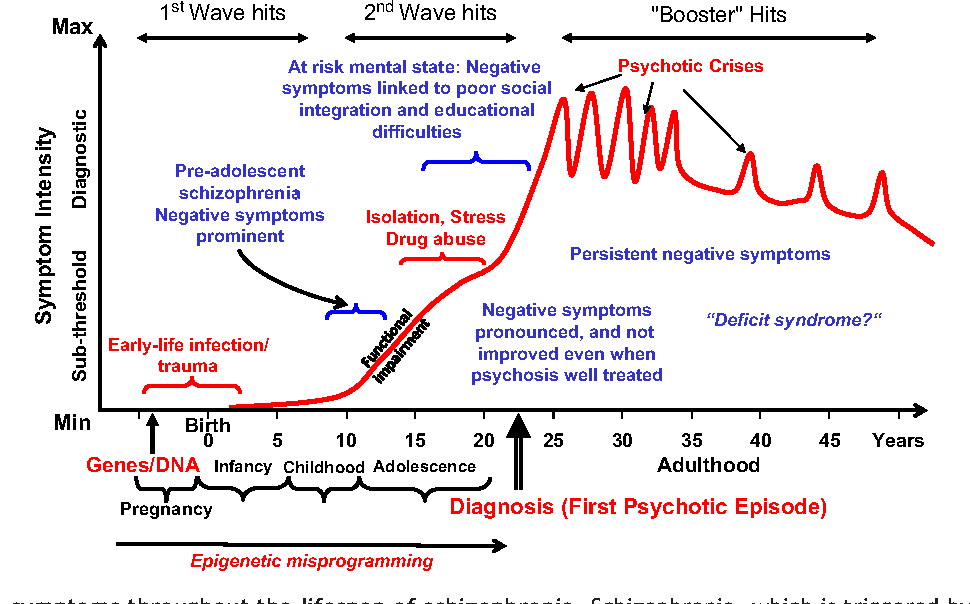
The negative symptoms of schizophrenia can often appear several years before somebody experiences their first acute schizophrenic episode.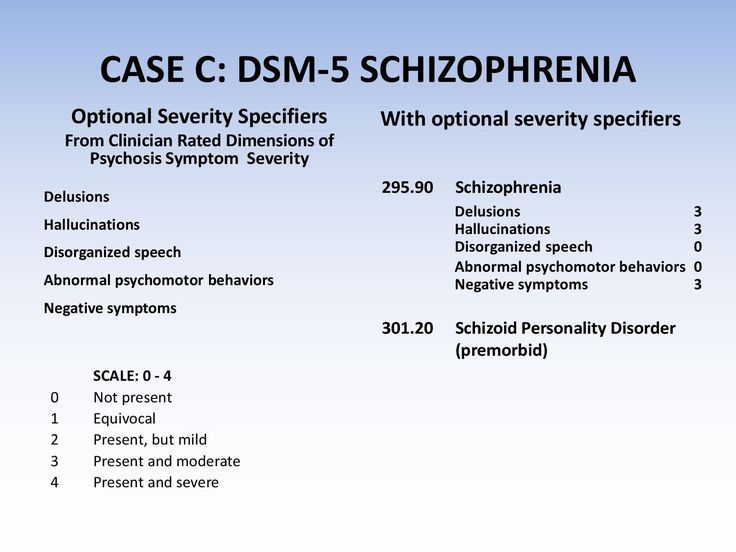
These initial negative symptoms are often referred to as the prodromal period of schizophrenia.
Symptoms during the prodromal period usually appear gradually and slowly get worse.
They include the person becoming more socially withdrawn and increasingly not caring about their appearance and personal hygiene.
It can be difficult to tell whether the symptoms are part of the development of schizophrenia or caused by something else.
Negative symptoms experienced by people living with schizophrenia include:
- losing interest and motivation in life and activities, including relationships and sex
- lack of concentration, not wanting to leave the house, and changes in sleeping patterns
- being less likely to initiate conversations and feeling uncomfortable with people, or feeling there's nothing to say
The negative symptoms of schizophrenia can often lead to relationship problems with friends and family as they can sometimes be mistaken for deliberate laziness or rudeness.
Psychosis
Schizophrenia is often described by doctors as a type of psychosis.
A first acute episode of psychosis can be very difficult to cope with, both for the person who is ill and for their family and friends.
Drastic changes in behaviour may occur, and the person can become upset, anxious, confused, angry or suspicious of those around them.
They may not think they need help, and it can be hard to persuade them to visit a doctor.
Read more about understanding psychotic experiences.
Positive and Negative Symptoms of Schizophrenia
Written by Terri D'Arrigo
Schizophrenia changes how you think, feel, and act. It might affect you differently from someone else. The symptoms can come and go, too. No one has all of them all of the time.
They usually start between ages 16 and 30. Men often get them earlier than women. Oftentimes there is a gradual change in the person before obvious symptoms start. This is sometimes called the prodrome phase.
This is sometimes called the prodrome phase.
When the disease is in full swing and symptoms are severe, the person with schizophrenia can't tell when certain ideas and perceptions they have are real or not. This happens less often as they get older.
People with the condition usually aren't aware that they have it until a doctor or counselor tells them. They won't even realize that something is seriously wrong. If they do happen to notice symptoms, like not being able to think straight, they might chalk it up to things like stress or being tired.
If you're concerned that you or someone you know is showing signs of schizophrenia, talk to a doctor or counselor.
Positive Symptoms of Schizophrenia: Things That Might Start Happening
Positive symptoms are highly exaggerated ideas, perceptions, or actions that show the person can’t tell what’s real from what isn’t. Here the word "positive" means the presence (rather than absence) of symptoms. They can include:
- Hallucinations.
 People with schizophrenia might hear, see, smell, or feel things no one else does. The types of hallucinations in schizophrenia include:
People with schizophrenia might hear, see, smell, or feel things no one else does. The types of hallucinations in schizophrenia include:- Auditory. The person most often hears voices in their head. They might be angry or urgent and demand that they do things. It can sound like one voice or many. They might whisper, murmur, or be angry and demanding.
- Visual. Someone might see lights, objects, people, or patterns. Often it’s loved ones or friends who are no longer alive. They may also have trouble with depth perception and distance.
- Olfactory and gustatory. This can include good and bad smells and tastes. Someone might believe they’re being poisoned and refuse to eat.
- Tactile. This creates a feeling of things moving on your body, like hands or insects.
- Delusions. These are beliefs that seem strange to most people and are easy to prove wrong.
 The person affected might think someone is trying to control their brain through TVs or that the FBI is out to get them. They might believe they're someone else, like a famous actor or the president, or that they have superpowers. Types of delusions include:
The person affected might think someone is trying to control their brain through TVs or that the FBI is out to get them. They might believe they're someone else, like a famous actor or the president, or that they have superpowers. Types of delusions include:- Persecutory delusions. The feeling someone is after you or that you’re being stalked, hunted, framed, or tricked.
- Referential delusions. When a person believes that public forms of communication, like song lyrics or a gesture from a TV host, are a special message just for them.
- Somatic delusions. These center on the body. The person thinks they have a terrible illness or bizarre health problem like worms under the skin or damage from cosmic rays.
- Erotomanic delusions. A person might be convinced a celebrity is in love with them or that their partner is cheating. Or they might think people they’re not attracted to are pursuing them.
- Religious delusions.
 Someone might think they have a special relationship with a deity or that they’re possessed by a demon.
Someone might think they have a special relationship with a deity or that they’re possessed by a demon. - Grandiose delusions. They consider themselves a major figure on the world stage, like an entertainer or a politician.
- Confused thoughts and disorganized speech. People with schizophrenia can have a hard time organizing their thoughts. They might not be able to follow along when you talk to them. Instead, it might seem like they're zoning out or distracted. When they talk, their words can come out jumbled and not make sense.
- Trouble concentrating. For example, someone might lose track of what's going on in a TV show as they're watching.
- Movement disorders. Some people with schizophrenia can seem jumpy. Sometimes they'll make the same movements over and over again. But sometimes they might be perfectly still for hours at a stretch, which experts call being catatonic.
 Contrary to popular belief, people with the disease usually aren't violent.
Contrary to popular belief, people with the disease usually aren't violent.
Negative Symptoms of Schizophrenia: Things That Might Stop Happening
Negative symptoms refer to an absence or lack of normal mental function involving thinking, behavior, and perception. You might notice:
- Lack of pleasure. The person may not seem to enjoy anything anymore. A doctor will call this anhedonia.
- Trouble with speech. They might not talk much or show any feelings. Doctors call this alogia.
- Flattening: The person with schizophrenia might seem like they have a terrible case of the blahs. When they talk, their voice can sound flat, like they have no emotions. They may not smile normally or show usual facial emotions in response to conversations or things happening around them. A doctor might call this affective flattening.
- Withdrawal. This might include no longer making plans with friends or becoming a hermit.
 Talking to the person can feel like pulling teeth: If you want an answer, you have to really work to pry it out of them. Doctors call this apathy.
Talking to the person can feel like pulling teeth: If you want an answer, you have to really work to pry it out of them. Doctors call this apathy. - Struggling with the basics of daily life. They may stop bathing or taking care of themselves.
- No follow-through. People with schizophrenia have trouble staying on schedule or finishing what they start. Sometimes they can't get started at all. A doctor might call this avolition.
Depression has some of the same symptoms, too. They can be hard to spot, especially in teens, because even healthy teens can have big emotional swings between highs and lows.
Cognitive Symptoms & Thinking Problems
These symptoms reflect how well the person’s brain learns, stores, and uses information.
Someone with schizophrenia might have a hard time with their working memory. For example, they may not be able to keep track of different kinds of facts at the same time, like a phone number plus instructions.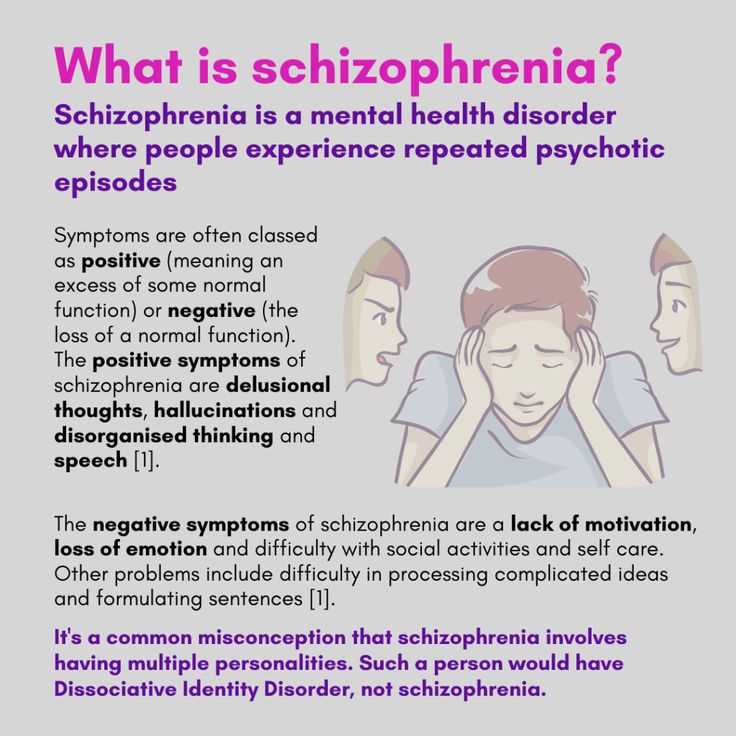
Along with having trouble paying attention, it can be hard for them to organize their thoughts and make decisions.
Next In Schizophrenia Overview
Schizophrenia TestsSchizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- in
- F
- x
- 9 h
- K.
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- Ф
- x
- C hours
- Sh
- Sh.
- K
- E 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0005
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0005
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/ nine0004 Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations. nine0286
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others; nine0005
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which is manifested, for example, by the patient performing actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms. nine0322
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease. nine0322
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2).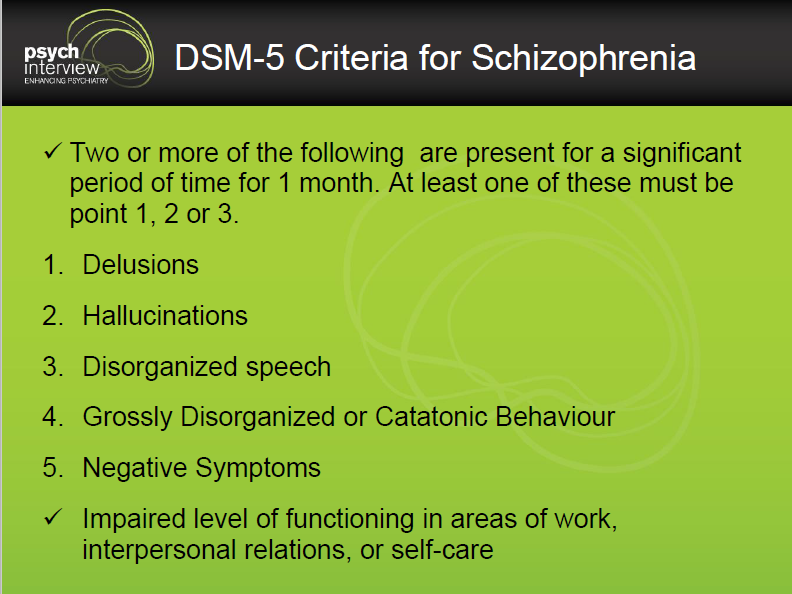 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment. nine0322
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.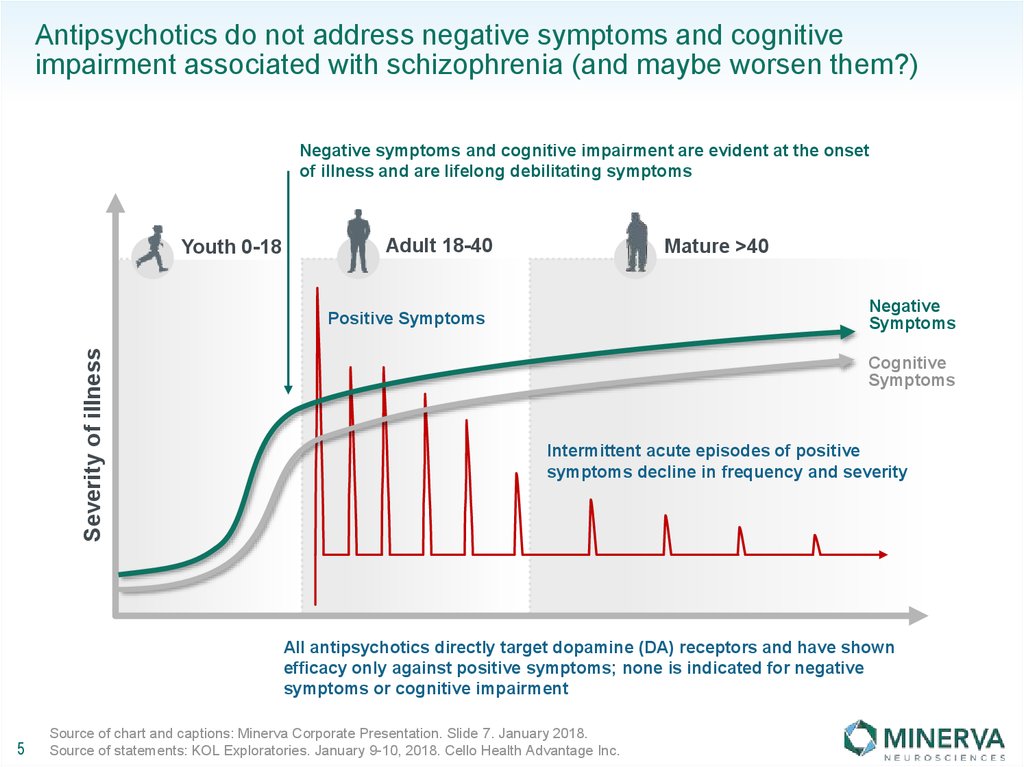 nine0322
nine0322
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia.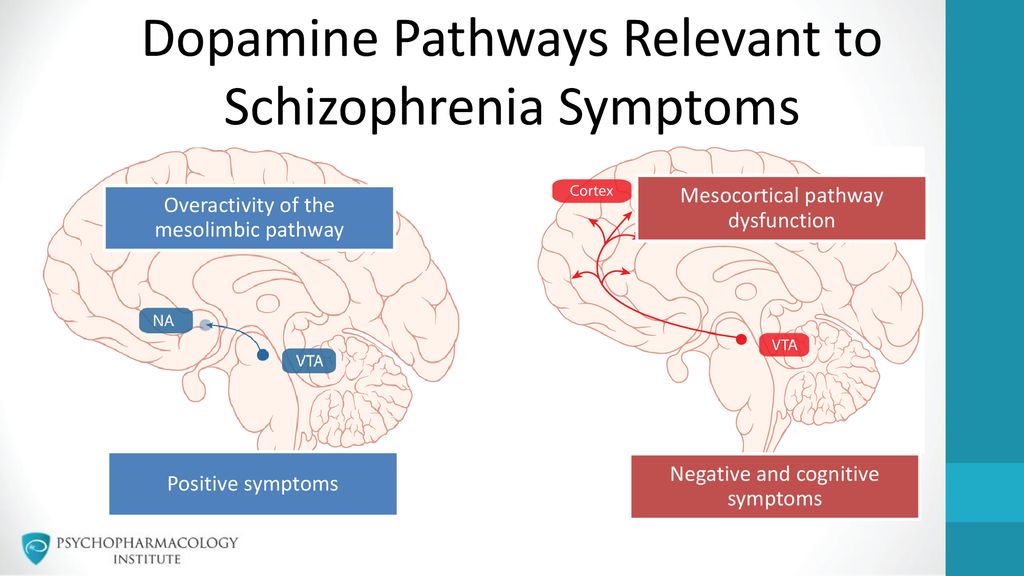 Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0322
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0322
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).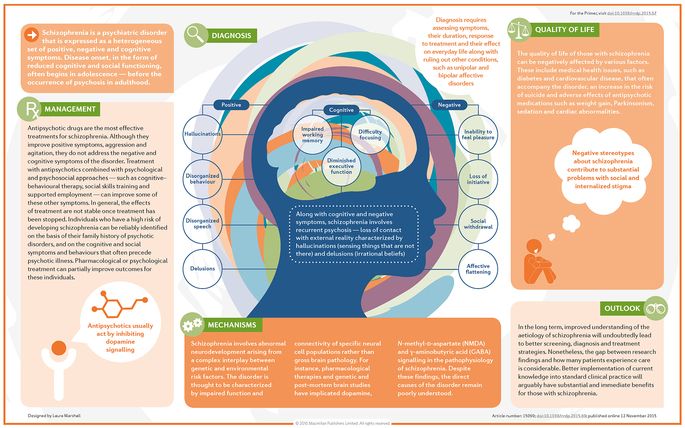 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0322
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0322
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care. nine0322
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.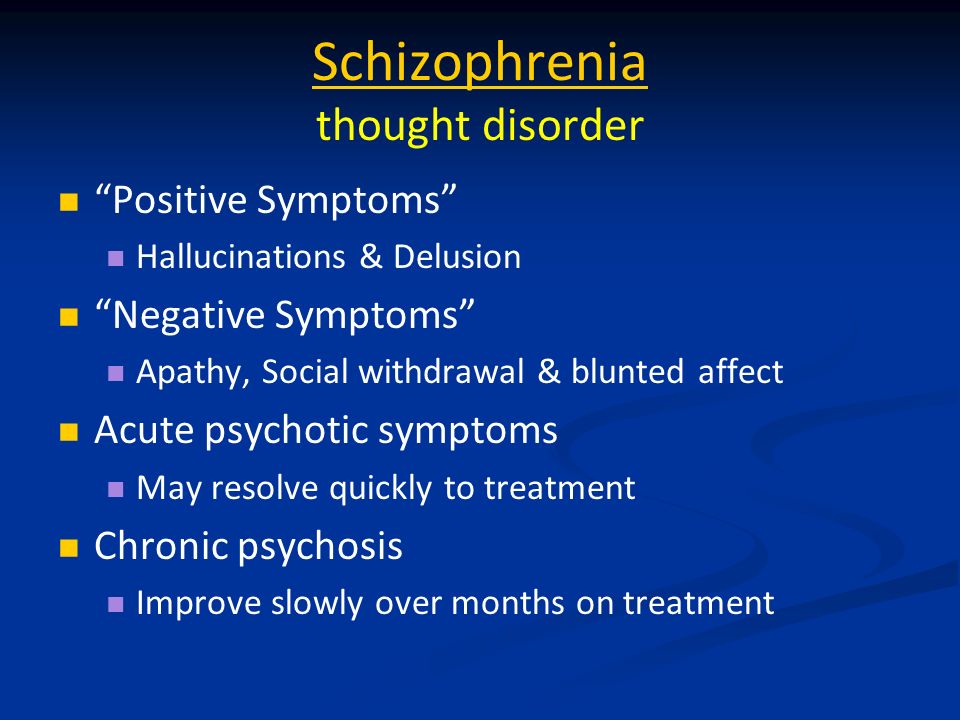 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0322
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0322
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities. nine0322
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.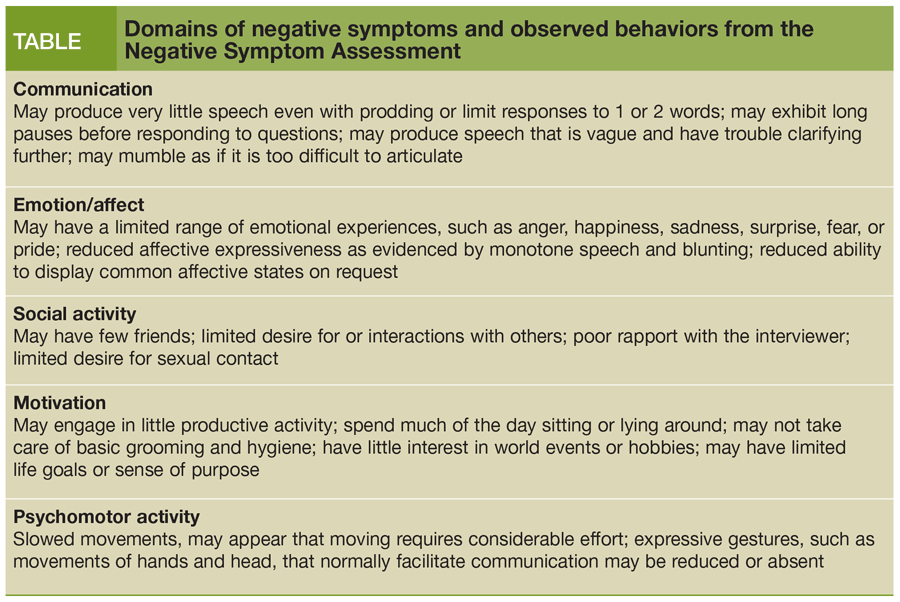 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Negative symptoms of schizophrenia
Negative symptoms of schizophrenia consist in a gradually increasing emotional and volitional decline.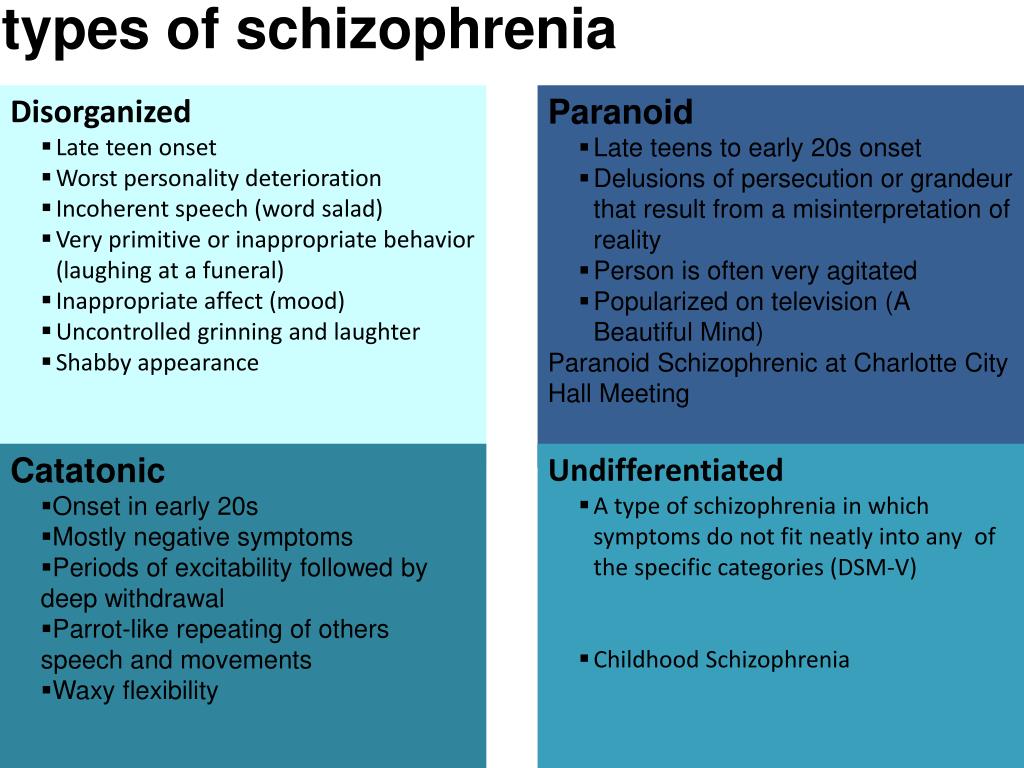
Forms of negative symptoms of schizophrenia
1. Change in emotional state. In the early stages it can be depression, fear, frequent mood swings, guilt. Later, emotions are smoothed out, there is a decrease in emotional sensitivity. Sometimes it seems that the patient has no emotions at all. Because of this, it becomes difficult to communicate with the patient, as a result of which he closes, moves away from social contacts. This is often aggravated by the fact that the patient ceases to understand the emotions of other people. nine0322
2. Cognitive decline. Thinking disorders occur: the patient cannot concentrate, is not able to build logical chains and draw conclusions. Draws attention to the minor features of the object to the detriment of the main ones. Pays more attention to emotional perception than logical. Memory deteriorates, which causes difficulty in planning and decision making. Due to the deterioration of thinking processes, speech disorders appear.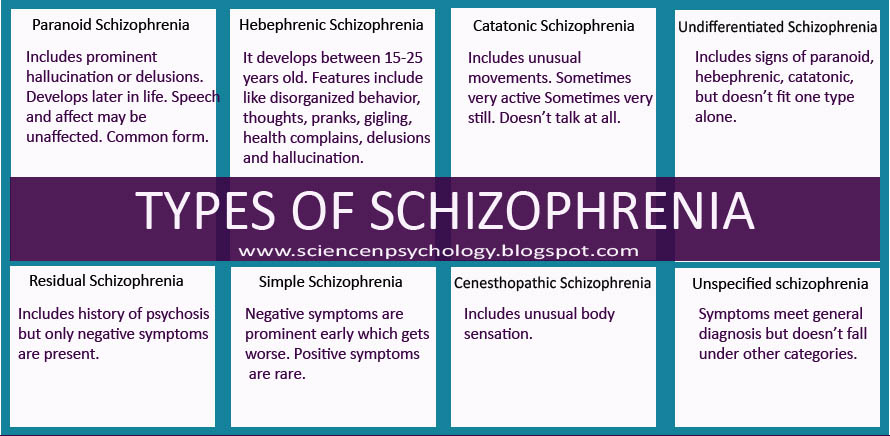 It becomes incoherent, slow, with a lot of pauses between words. nine0322
It becomes incoherent, slow, with a lot of pauses between words. nine0322
3. Decay of will. The patient becomes passive, lack of initiative, lethargic, apathetic. The circle of interests of the patient narrows, interest in previously important goals disappears.
4. Sleep disorder. Patients with schizophrenia often suffer from sleep disorders. It can be problems with falling asleep, ragged sleep, nighttime wakefulness. The aggravation of sleep problems may be one of the harbingers of an imminent exacerbation of schizophrenia.
5. Physical syndromes. nine0286 Stupor, twitching of limbs. Critical decrease or increase in muscle tone: constant tension or relaxation. Frequent headaches, dizziness. Nausea and weakness are also characteristic of schizophrenia. Vestibular disorders are not uncommon: the patient's gait becomes uncertain, he often stumbles upon objects.
6. Perception changes. Sounds may seem too loud, reality is blurry.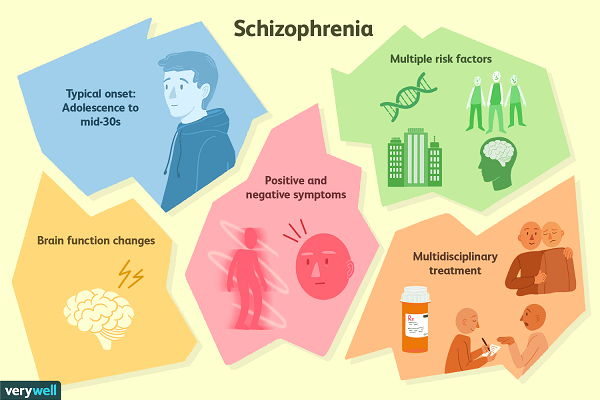 A person is constantly “in himself”, often to the detriment of the perception of the outside world. The speed of perception slows down. Spatial images are fuzzy. This leads to anxiety and even greater isolation in patients with schizophrenia. nine0322
A person is constantly “in himself”, often to the detriment of the perception of the outside world. The speed of perception slows down. Spatial images are fuzzy. This leads to anxiety and even greater isolation in patients with schizophrenia. nine0322
Negative symptoms progress over time and are a true companion of schizophrenia.
Primary and secondary negative symptoms in schizophrenia
Primary negative symptoms of schizophrenia are disorders resulting from the course of the disease itself. These are violations of thinking, perception, emotional decline, somatic and vegetative disorders.
Secondary negative symptoms of schizophrenia appear as a result of external influences. Their development is strongly influenced by the attitude towards the patient of the surrounding people, members of his family, the side effects of drugs, a long stay in the hospital. The use of neuroleptics often contributes to the development of secondary negative symptoms of schizophrenia.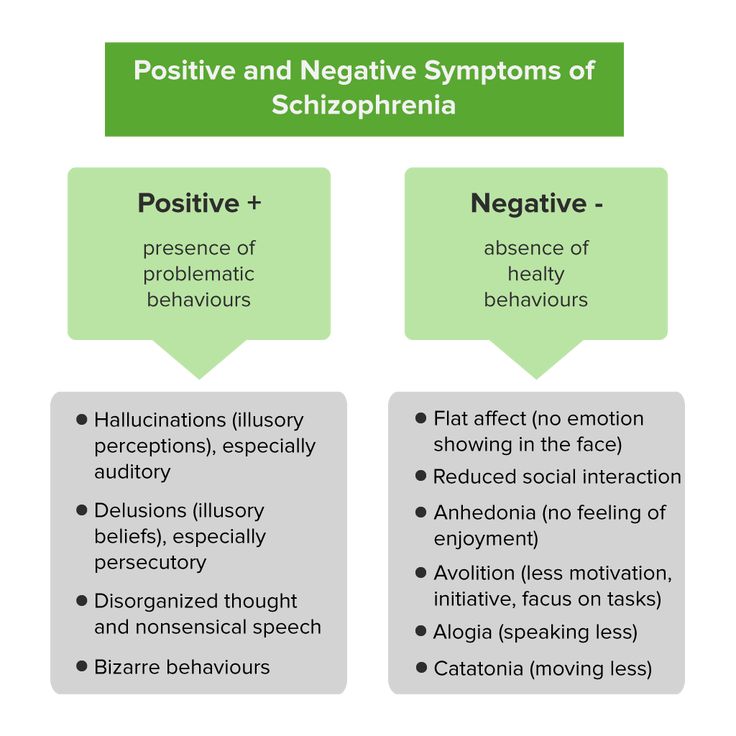 Therefore, in modern medicine, they are practically replaced by antipsychotics - a new generation of drugs that do not cause an increase in the symptoms of schizophrenia.
Therefore, in modern medicine, they are practically replaced by antipsychotics - a new generation of drugs that do not cause an increase in the symptoms of schizophrenia.
Drug-induced secondary negative symptoms of schizophrenia disappear when the drug is stopped. However, often such symptoms cause the patient to stop taking medication, which leads to new exacerbations. nine0322
Our clinic does not use conventional antipsychotics for the treatment of schizophrenia. We use only new generation antipsychotics, which allows us to reduce negative symptoms.
Primary negative symptoms are irreversible. You can only stop its progression by using the right methods of treating schizophrenia. Treatment of schizophrenia should begin on time, because over time, negative symptoms only increase.
Secondary negative symptoms can be resolved with the right treatment and support from loved ones. nine0322
The negative symptoms of schizophrenia are not yet decisive for the diagnosis.