What meds cause depression
Medications That Can Cause Depression - Corticosteroids, Beta-Blockers
En español | Researchers have long known that many drugs can make us feel down or even depressed and that, as we age, our changing body chemistries put us at a greater risk for this side effect. But few doctors think to review the medications list when their patients have the telltale symptoms of depression: lack of energy, listlessness, feeling rundown, excessive fatigue, changes in appetite and sleeping patterns, sadness, despair. As a result, they often layer on top of the drugs causing those symptoms a new drug, such as an antidepressant, for treating them, which may in turn trigger additional side effects.
Stay informed: Get news and resources from the Health Newsletter.
Medication Side Effects
Your medications may be to blame if you're feeling blue. — Photo by Gerard Fritz/Getty Images
- Some prescription drugs may cause depression symptoms.
Read
- More from Dr. Armon B. Neel Jr. Read
- Find information on drug interactions with this tool. Do
Join AARP today – Receive access to exclusive information, benefits and discounts.
Are you feeling depressed? One of the drugs you're on could be the cause. Read below for the major classes of drugs that can cause depression. If you suspect that your depression symptoms are linked to a prescription drug you're taking, talk to your doctor or health care provider right away. It's important that you do not discontinue them on your own.
1. Beta-blockersWhy they're prescribed: Beta-blockers are typically prescribed to treat high blood pressure (hypertension). Examples: atenolol (Tenormin), carvedilol (Coreg), metoprolol, propranolol (Inderal), sotalol (Betapace), timolol (Timoptic) and some other drugs whose chemical names end with "-olol." These drugs slow the heart rate and lower blood pressure by blocking the effect of the hormone adrenaline. Beta-blockers are also used to treat angina and for other conditions, such as migraines, tremors, irregular heartbeat and, in eye-drop form, certain kinds of glaucoma.
Beta-blockers are also used to treat angina and for other conditions, such as migraines, tremors, irregular heartbeat and, in eye-drop form, certain kinds of glaucoma.
How they can cause depression: While scientists don't know exactly how beta-blockers cause depression, the three most commonly adverse effects reported with their use are fatigue, sexual dysfunction and depression.
Alternatives: For older people, benzothiazepine calcium channel blockers, another form of blood-pressure medication, are often safer and more effective than beta-blockers.
2. Corticosteroids
Why they're prescribed: Corticosteroids are used to treat inflammation of the blood vessels and muscles as well as rheumatoid arthritis, lupus, Sjögren's syndrome and gout. Examples: cortisone, methylprednisolone, prednisone and triamcinolone.
How they can cause depression: Research suggests that corticosteroids lower serotonin levels in the body, and it is known that lowered serotonin levels can cause depression and other psychiatric disorders. Withdrawal from corticosteroids can also trigger depression.
Withdrawal from corticosteroids can also trigger depression.
Alternatives: Acetaminophen (Tylenol), aspirin, tramadol (Ultram) or, if the situation requires it, a mild opiate like hydrocodone/acetaminophen (Vicodin). As we grow older, most joint pain from arthritis comes not from inflammation (for which corticosteroids may be used) but from immobility of the joint due to joint damage from years of inflammation.
3. Benzodiazepine hypnoticsWhy they're prescribed: These drugs, also known as benzodiazepine tranquilizers, are typically prescribed to treat anxiety and insomnia and to relax muscles. Examples: alprazolam (Xanax), diazepam (Valium), estazolam (ProSom), flurazepam (Dalmane), lorazepam (Ativan), temazepam (Restoril) and triazolam (Halcion).
How they can cause depression: Benzodiazepines are central nervous system depressants. If not fully metabolized in the liver, they can build up in the body to toxic levels. The resulting "hangover effect" can manifest itself as depression. Older people are more likely to experience these residual effects because their livers often lack a key enzyme needed to metabolize the drugs.
Older people are more likely to experience these residual effects because their livers often lack a key enzyme needed to metabolize the drugs.
Alternatives: Give yourself every chance to sleep well naturally: Go to bed and wake up at the same times every day, avoid meals within two hours of bedtime, allow 30 minutes before bedtime for a relaxing pre-sleep ritual, and so forth. Melatonin, a dietary supplement that helps control sleep and wake cycles, may also be worth trying.
4. Parkinson's drugs
Why they're prescribed: One approach to treating the symptoms of Parkinson's disease is to use drugs to adjust the levels of dopamine (a neurotransmitter) in the brain, as the motor symptoms associated with the disease result from the death of dopamine-generating cells in a region of the midbrain.
For example, levodopa, the most commonly prescribed Parkinson's medication, is converted into dopamine on entering the brain; it's typically combined with carbidopa, which helps prevent it from breaking down before it can reach the brain and take effect, in brand-name products such as Atamet, Sinemet and Stalevo.
Another approach is the use of dopamine agonists such as pramipexole (Mirapex) and ropinorole (Requip), which work by stimulating the dopamine receptors in the brain, thus mimicking the activity of dopamine.
How they can cause depression: Dopamine is one of three basic neurotransmitters that have been associated with depression (the others are serotonin and norepinephrine). Researchers believe that prolonged exposure to higher levels of dopamine may cause depression.
Alternatives: As many as 25 percent of all patients who are diagnosed with Parkinson's don't actually have the disease, so it's important to make sure that you're not among those misdiagnosed. Older people with essential tremors — involuntary trembling or quivering of the hands, limbs or other parts of the body — are often misdiagnosed as having Parkinson's. There's also drug-induced Parkinson's, which can often be reversed if the offending medication is discontinued early enough. (Older patients, for example, frequently develop parkinsonism after being prescribed antipsychotic drugs such as Haldol, Mellaril, Stelazine and Thorazine.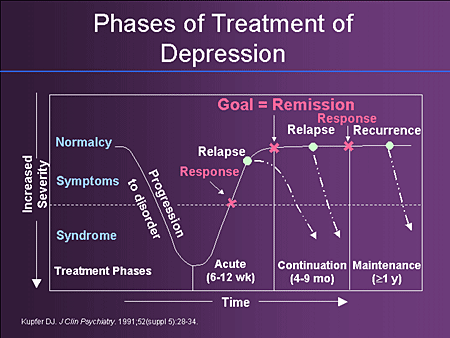 ) A systemic neurological examination is the best way to test for Parkinson's disease. And if you need to take levodopa, the dose can be reduced with the use of a COMT-inhibitor, a relatively new type of drug that blocks an enzyme in the body from metabolizing the levodopa before it reaches the brain.
) A systemic neurological examination is the best way to test for Parkinson's disease. And if you need to take levodopa, the dose can be reduced with the use of a COMT-inhibitor, a relatively new type of drug that blocks an enzyme in the body from metabolizing the levodopa before it reaches the brain.
Why they're prescribed: Hormone-altering drugs are used to treat a variety of conditions. Estrogen (Premarin), for example, is typically prescribed for hot flashes and other postmenopausal symptoms .
How they can cause depression: Manipulating hormone levels in the body can cause a variety of problems, particularly as medications interact with the central nervous system. Studies show that changes in hormonal levels are significantly associated with the appearance of symptoms of depression.
Alternatives: Once again, it's important to try to identify the cause of the symptoms. Review the medications you're taking — prescription and over the counter — with your doctor to identify some problems that can be corrected without additional drugs.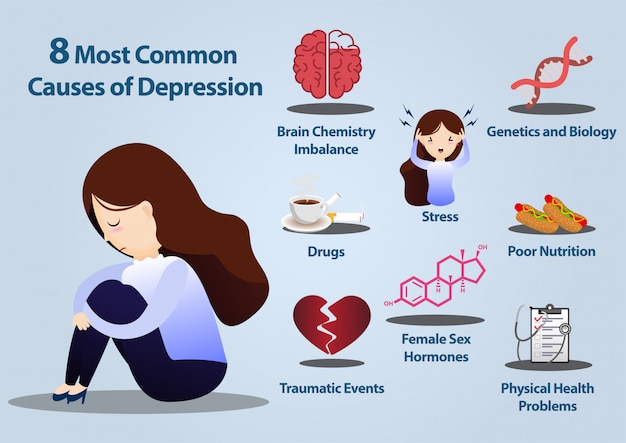
6. Stimulants
Why they're prescribed: Stimulant medications, such as methylphenidate (Ritalin) and modafinil (Provigil), are often prescribed to treat excessive daytime sleepiness, whether caused by hypersomnia, narcolepsy or sleep apnea. They're also prescribed for ADHD and fatigue.
How they can cause depression: Stimulant medications increase the level of dopamine in the body. Researchers believe that prolonged exposure to higher levels of dopamine may cause depression.
Alternatives: As with insomnia (see benzodiazepine hypnotics, above), it's important to identify the cause of excessive daytime sleepiness. Other medications you're taking — whether prescription or over the counter — could be responsible. Drugs with sedating effects, for example, are among the most common causes of excessive daytime sleepiness. (These include alpha- and beta-blockers, anti-diarrheal agents, antihistamines, antipsychotics, antispasmodics, cough suppressants, epilepsy drugs, skeletal muscle relaxants, Parkinson's drugs and some antidepressant medications. )
)
Nondrug causes of excessive daytime sleepiness include sleep deprivation, obstructive sleep apnea (when the throat muscles intermittently relax and block the airway during sleep) and depression. When such underlying conditions are treated appropriately, there's rarely, if ever, any need for the use of stimulants.
7. Anticonvulsants
Why they're prescribed: Anticonvulsant drugs, which have long been used to treat seizures, are increasingly being used to treat other medical conditions, including neuropathic pain, bipolar disorder, mood disorders and mania. Examples: carbamazepine (Tegretol), gabapentin (Neurontin), lamotrigine (Lamictal), pregabalin (Lyrica) and topiramate (Topamax).
How they can cause depression: Anticonvulsants are believed to work by affecting neurotransmitters, which act as chemical messengers in the brain. They may, for example, limit seizures from spreading by blocking the flow of signals from the central nervous system (CNS) rather than raise the threshold for seizures.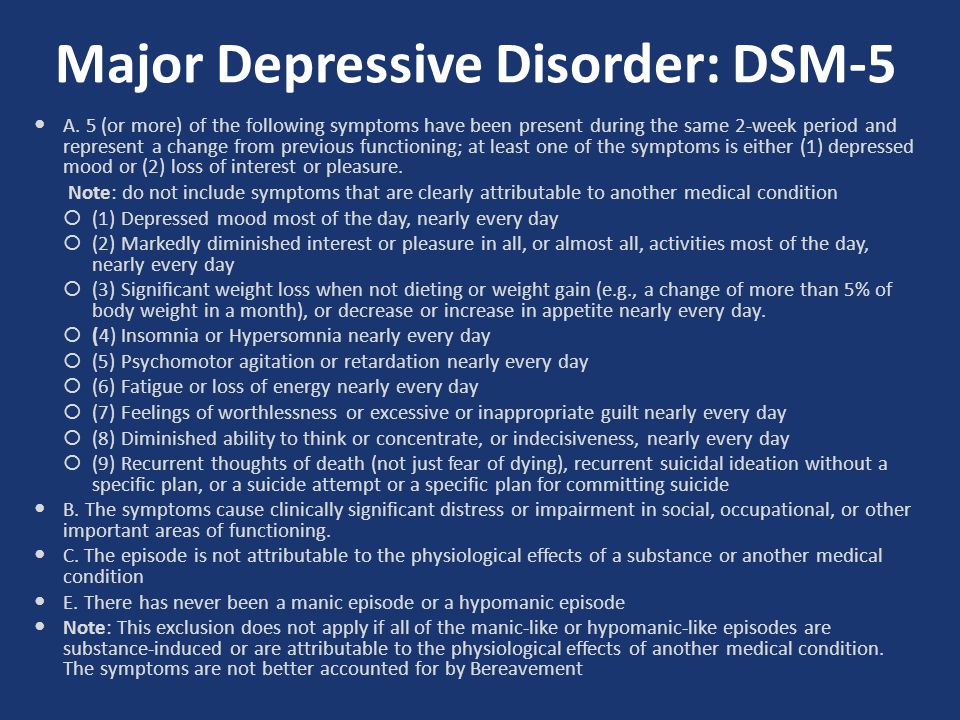 All CNS depressants, including anticonvulsants, can cause depression.
All CNS depressants, including anticonvulsants, can cause depression.
Alternatives: For seizures, phenytoin (Dilantin), which raises the seizure threshold; for chronic neuropathic pain, venlafaxine (Effexor), which affects the two neurotransmitters, serotonin and norepinephrine, that are thought to play roles in regulating pain.
8. Proton pump inhibitors and h3 blockersWhy they're prescribed: Doctors typically prescribe these medications, which suppress the secretion of gastric acid, to treat gastroesophageal reflux disease (GERD).
How they can cause depression: While these drugs are known to cause depression, scientists don't yet understand why they do. When any major body process is blocked, however, the body often rebels in an intense effort to fight back. Consequently, it's altogether likely that changing the pH of the stomach could bring on changes to the central nervous system and the brain.
Alternatives: Know which foods trigger your acid reflux (spicy or fried foods, for example) and avoid them, especially in the hours before bedtime.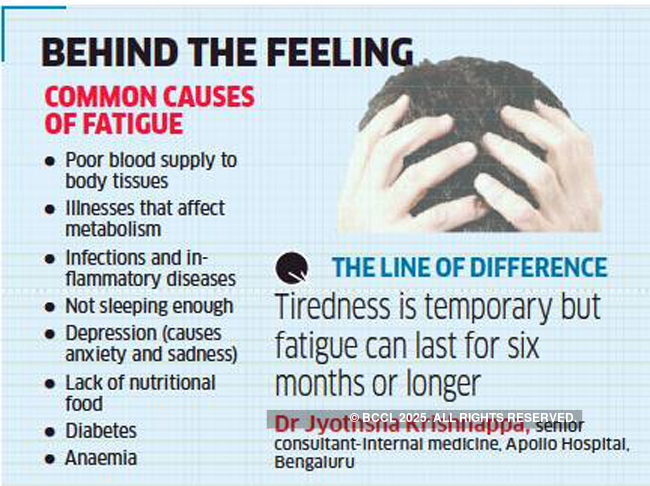 A non-calcium-carbonate-based antacid, such as Mylanta, may also help. Many of my patients have reported relief from the home remedy of apple cider vinegar and honey (typically one tablespoon each, taken together), though I know of no scientific research that confirms the effectiveness of this approach.
A non-calcium-carbonate-based antacid, such as Mylanta, may also help. Many of my patients have reported relief from the home remedy of apple cider vinegar and honey (typically one tablespoon each, taken together), though I know of no scientific research that confirms the effectiveness of this approach.
9. Statins and other lipid-lowering drugs
Why they're prescribed: Statins are the class of drugs most commonly prescribed to lower cholesterol levels, followed by fibrates and other drugs, such as ezetimibe, colesevelam and nicotinic acid.
How they can cause depression: Recent research suggests that lipid-lowering drugs may cause depression by depleting levels of cholesterol in the brain, where it plays an important role in the release of neurotransmitters.
Alternatives: A combination of vitamin B12 (injectable or sublingual), vitamin B6, folic acid and fish oil can lower homocysteine levels in the body. Homocysteine, an amino acid, inflicts damage to the inner arterial lining (endothelium) and other cells of the body, elevating lipids levels. While there are many studies that substantiate this nondrug approach and many that reject it, I've found that it works consistently well in older patients without posing the risk of serious side effects.
While there are many studies that substantiate this nondrug approach and many that reject it, I've found that it works consistently well in older patients without posing the risk of serious side effects.
10. Anticholinergic drugs used to treat stomach cramps and other GI disorders
Why they're prescribed: Anticholinergic medications slow the action of the intestine, thereby reducing the amount of stomach acid produced. They do this mostly by blocking the effects of acetylcholine, the neurotransmitter that causes muscles — including those in the intestine — to contract. Dicyclomine (Bentyl), for example, is widely used to treat the symptoms of irritable bowel syndrome.
How they can cause depression: Anticholinergics, as central nervous system depressants, can cause depression, sedation and cognitive impairment in older patients.
Alternatives: Using an h3 blocker such as ranitidine (Zantac) in the lower-dose formulation (75mg) can work well for the occasional attack of heartburn and acid indigestion. A calcium-free antacid (Gelusil or Mylanta, for example) may help.
A calcium-free antacid (Gelusil or Mylanta, for example) may help.
Member Discounts! Save on eye exams, prescription drugs, hearing aids and more
Drugs That Cause Depression | hims
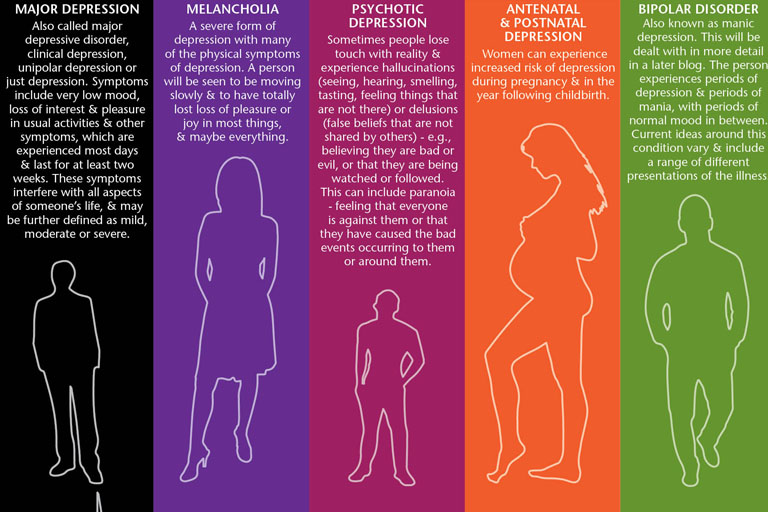
Major depressive disorder (MDD, or clinical depression) is a common mood disorder. In fact, it’s one of the most common forms of mental illness, with an estimated 21 million adults in the US, or 8.4 percent of the entire adult population, experiencing a depressive episode in 2020.
Depression has several potential causes, including genetic factors, sudden negative changes in your life and certain personality traits, such as childhood anxiety.
Certain drugs, including over the counter medications and prescription drugs used to treat many common diseases and medical conditions, can either cause or contribute to depression.
This means that If you’ve recently started using a new medication and feel down, tired or simply less interested in your hobbies and activities than normal, it’s possible that the medication could be to blame.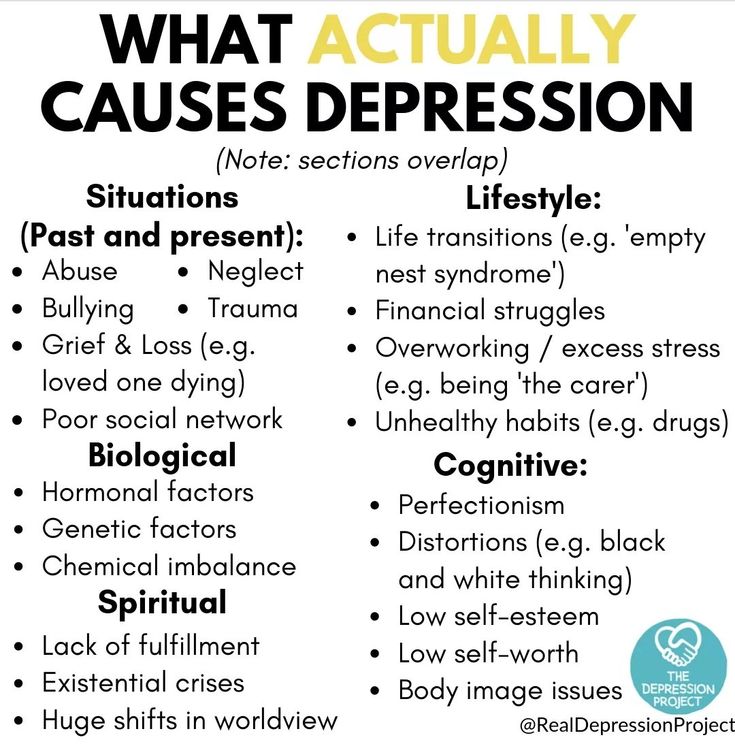
Below, we’ve discussed how you may feel if you’re depressed and listed medications and drugs that can cause or worsen depression.
We’ve also explained your options for treating depression, from antidepressants to therapy, new habits and more.
Symptoms of Depression
Depression can have a serious impact on the way you think, feel and behave. While it’s normal to occasionally feel down, major depression involves severe symptoms that affect your life on a daily or near-daily basis for a period of two weeks or longer.
Common symptoms of depression include:
Severe pessimistic or hopeless feelings
A persistent sad, empty or anxious mood
Reduced interest in or pleasure from your hobbies
Feeling like you’re worthless, guilty or unable to improve your life
Difficulty concentrating on tasks or remembering information
Finding it challenging to think clearly or make decisions
Thoughts involving death, or suicidal thoughts and/or behavior
Difficulty falling asleep, staying asleep or waking up
Slowed movements and/or speech
Irritability and a “shorter fuse” with other people
Pains, cramps and other physical symptoms without a clear cause
Changes in your appetite, eating habits and/or weight
Our guide to the signs of clinical depression discusses these symptoms and the effects they can have on your daily life in more detail.
Medications That May Cause Depression
Many common medications can affect your moods and thoughts, often by affecting your levels of certain hormones or brain chemicals called neurotransmitters.
In some cases, using certain types of medication may increase your risk of developing clinical depression. Some medications can even contribute to severe depression and/or an increased risk of suicide.
According to research published in the Journal of the American Medical Association, as many as 37.2 percent of US adults report using medications that are linked to depression.
Below, we’ve listed 10 classes of medication below that can cause or contribute to depression, with detailed information on how each type of medication works, what it’s used to treat and the effects it may have on your moods and behavior.
online counseling
the best way to try counseling
Benzodiazepines
Benzodiazepines are prescription medications that are used to treat anxiety disorders, seizure disorders, agitation and insomnia. They work by binding to receptors throughout your nervous system and slowing down activity.
They work by binding to receptors throughout your nervous system and slowing down activity.
Widely-used benzodiazepines include diazepam (Valium®), alprazolam (Xanax®), clonazepam (Klonopin®) and others.
Although many benzodiazepines are safe when used as directed for short periods, there is an association between benzodiazepine use and depressive symptoms. In some cases, this can even potentially involve suicidal ideation.
If you’re prescribed a benzodiazepine, it’s important to take it exactly as directed and tell your healthcare provider about any side effects you experience.
Beta-Blockers
Beta-blockers are common medications that are used to treat cardiovascular diseases. They’re also used off-label to treat certain forms of anxiety, such as performance anxiety.
Your healthcare provider may prescribe a beta-blocker if you have tachycardia (overly fast heart rate), hypertension (high blood pressure), congestive heart failure, a heart arrhythmia, coronary artery disease, or if you’re recovering from a heart attack.
Popular beta-blockers include atenolol (Tenormin®), acebutolol (Sectral®), nadolol (Corgard®), metoprolol (Lopressor®), propranolol (Inderal®) and others.
Beta-blockers have long been associated with depression, although study results on the link between their use and a person’s depression risk are mixed.
For example, a study involving elderly people with hypertension found that use of a beta-blocker was associated with a higher average depression score.
However, a large review and meta-analysis published in the journal Hypertension recently found no significant association between use of beta-blockers and depression (it did, however, identify a link between beta-blockers and fatigue, insomnia and sleep disorders).
Overall, the science is mixed. Some beta-blockers are also associated with erectile dysfunction, changes in sexual performance and other symptoms similar to those of depression.
Stimulants
Stimulants are medications that increase activity in your central nervous system.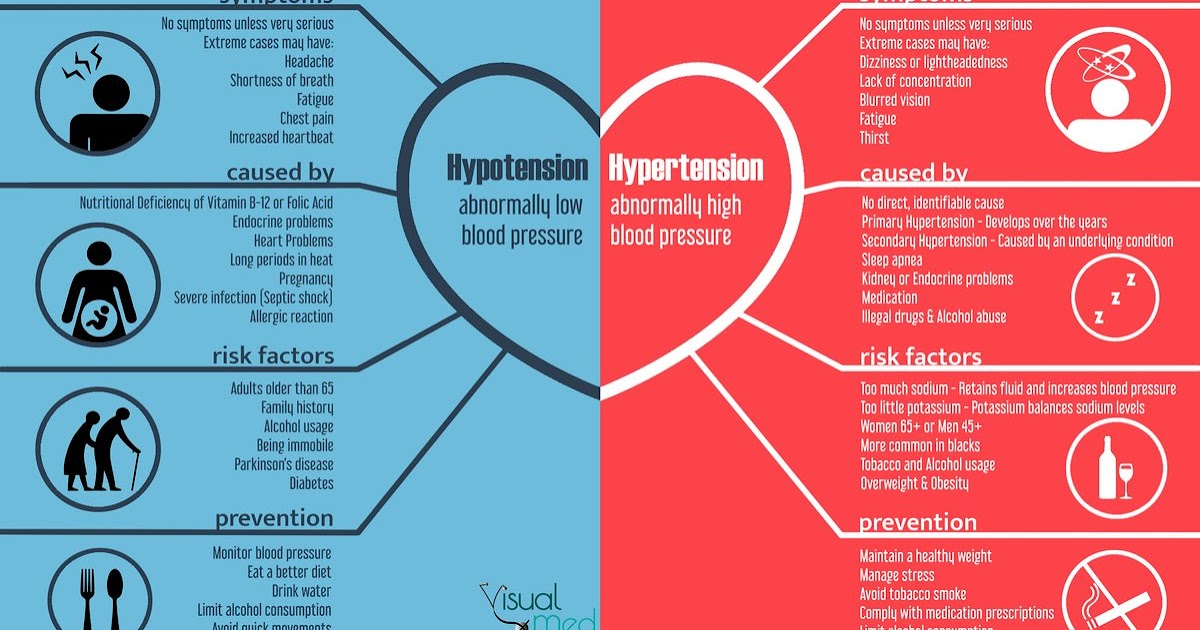 They’re used to treat attention deficit hyperactivity disorder (ADHD), asthma, obesity, narcolepsy, nasal/sinus congestion and hypotension (low blood pressure) caused by anesthesia.
They’re used to treat attention deficit hyperactivity disorder (ADHD), asthma, obesity, narcolepsy, nasal/sinus congestion and hypotension (low blood pressure) caused by anesthesia.
Common stimulants include caffeine and prescription medications such as dextroamphetamine (Dexedrine®), dextroamphetamine/amphetamine (Adderall®) and methylphenidate (Ritalin® or Concerta®).
Depression is a known side effect of some prescription stimulant medications. When misused or stopped suddenly, stimulants can cause withdrawal symptoms that include depression, sleep difficulties and fatigue.
Other adverse effects of stimulants include paranoia, anxiety, psychosis and physical problems such as headaches, weight loss and jitteriness.
Statins
Statins are prescription medications for lowering cholesterol levels. Your healthcare provider may prescribe a statin if you have risk factors for coronary artery disease.
Common statins include rosuvastatin (Crestor®), atorvastatin (Lipitor®), fluvastatin (Lescol®), simvastatin (Zocor®) and others.
Some research suggests that statins can cause depressed mood, anxiety, sleep problems and suicide attempts. However, a large-scale review that involved data from more than 70 studies found that statins do not appear to lead to depression symptoms in the general population.
Anticonvulsants
Anticonvulsants, or anti-seizure medications, are used to treat epilepsy. They’re also frequently prescribed as treatments for mental disorders, including bipolar disorder. Some anticonvulsant medications are used to treat migraines and neuropathic pain.
Some anticonvulsant medications are associated with depression, although results from studies are inconsistent overall. In 2008, research published by the FDA stated that people who used anticonvulsant drugs had an elevated risk of suicidal ideation or behavior.
Because of these findings, anticonvulsant medications are sold with labeling informing users of these safety risks.
Parkinson’s Disease Medications
Some medications used to treat the nervous system disorder Parkinson’s disease may cause or contribute to depression.
Common medications for Parkinson’s disease include levodopa and combination medications that contain levodopa, such as carbidopa/levodopa (Sinemet®).
Research shows a significant increase in depression among people with Parkinson’s disease who use levodopa. (It should be noted that the study examined only a small percentage of patients.)
Some medications used as adjunctive therapy for Parkinson’s, including amantadine (Gocovri®) may also contribute to depression symptoms.
Other common medications for managing Parkinson’s disease symptoms include pramipexole (Mirapex®) and ropinirole (Requip®).
These medications generally aren’t associated with depression. In fact, research suggests that they may have antidepressant properties.
Corticosteroids
Corticosteroids are anti-inflammatory medications. They’re synthetic forms of natural hormones produced in the adrenal glands. Corticosteroids are used to treat several conditions, including autoimmune diseases, neurological disorders and skin issues.
Widely-used corticosteroid medications include hydrocortisone, prednisolone, dexamethasone, betamethasone, prednisone and many others. These medications are available in many forms, including tablets, capsules, eye drops, injections and topical creams and gels.
Many corticosteroids can cause psychological side effects, including euphoria and, when used over the long term, depression. Some corticosteroids may also cause psychotic symptoms to develop, although this generally only occurs with high-dose, long-term use.
If you’re prescribed a corticosteroid, your healthcare provider will likely recommend using it for the shortest possible duration to minimize your risk of depression and other side effects.
Hormonal Medications
Some hormonal medications, including birth control pills, are associated with an increased risk of developing depression. However, researchers aren’t sure if the link is causal (meaning birth control pills cause depression) or if it’s related to a factor other than contraceptive use.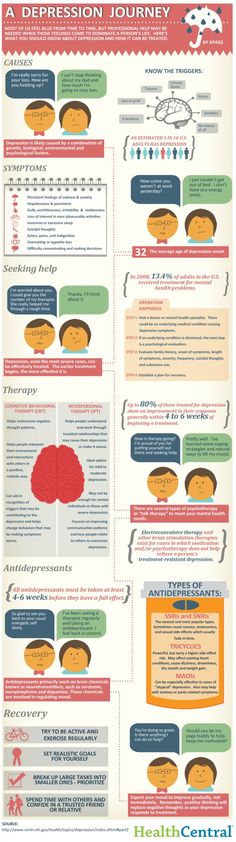
Common birth control pills include drospirenone-ethinyl estradiol (sold as Yaz®, Yasmin® and under other brand names), norgestimate-ethinyl estradiol (Ortho Tri-Cyclen®), norethisterone acetate-ethinyl estradiol (Estrostep®) and many others.
In a study published in JAMA Psychiatry in 2016, researchers found an increased risk of being diagnosed with depression among women who used hormonal contraceptives, with the highest rates of depression observed among adolescent women.
However, a systematic review and meta-analysis published in 2021 concluded that use of birth control pills and other types of hormonal contraceptives was not associated with any increased risk of depression in adult women.
In addition to birth control pills, other hormonal medications are also associated with a high risk of developing depression.
For example, research suggests that antiandrogen medications (drugs that reduce testosterone and other androgen levels) used in prostate cancer treatment increase the risk of depression in men.
Anticholinergic Drugs
Anticholinergic medications work by blocking the effects of the neurotransmitter acetylcholine — a naturally-occurring chemical that’s involved in brain and muscle function.
Medications of this type are used to treat respiratory health issues such as asthma and chronic obstructive pulmonary disease (COPD), as well as heart disease, Parkinson’s disease, mental disorders, allergies and urge incontinence (a sudden need to urinate).
Some scientific research suggests that long-term use of anticholinergic medications may play a role in reduced cognitive function late in life.
Healthcare providers are instructed to use caution when prescribing anticholinergic medications to people with depression or schizophrenia. However, while old studies have suggested a link between their use and depression, more recent research doesn’t show a clear association.
Make sure to inform your healthcare provider if you notice any changes in your moods, feelings or thoughts if you’re prescribed any type of anticholinergic medication.
Proton Pump Inhibitors (PPIs)
Proton pump inhibitors are medications that reduce the amount of acid produced by the glands inside your stomach lining. They’re used to treat gastroesophageal reflux disease (GERD) and ulcers that develop in the stomach and small intestine.
Widely used proton pump inhibitors include omeprazole (Prilosec®), lansoprazole (Prevacid®), esomeprazole (Nexium®), rabeprazole (AcipHex®), pantoprazole (Protonix®) and others.
Research suggests that use of proton pump inhibitors is linked to depression, with people who use PPIs in high dosage more likely to develop depressive symptoms.
Other research has found a potential link between proton pump inhibitor use and neurological issues, such as dementia.
If you’re prescribed a proton pump inhibitor, it’s important to talk with your healthcare provider before adjusting your dosage, stopping treatment or making any other changes to your use of medication.
Want to learn more? We answer "can antibiotics cause depression?" in our blog.
How to Treat Depression
Even when it involves severe, persistent symptoms, depression is treatable. If you think you’re depressed, it’s important to reach out to a mental health professional to learn more about your options.
You can get help for depression by talking to your primary care provider by contacting a licensed psychiatrist in your area or from home using our online psychiatry service.
Depression is usually treated with medications called antidepressants, therapy and changes to your habits and lifestyle. If a medication is involved in your symptoms, your healthcare provider may adjust your dosage or switch you to a medication that’s less likely to cause depression.
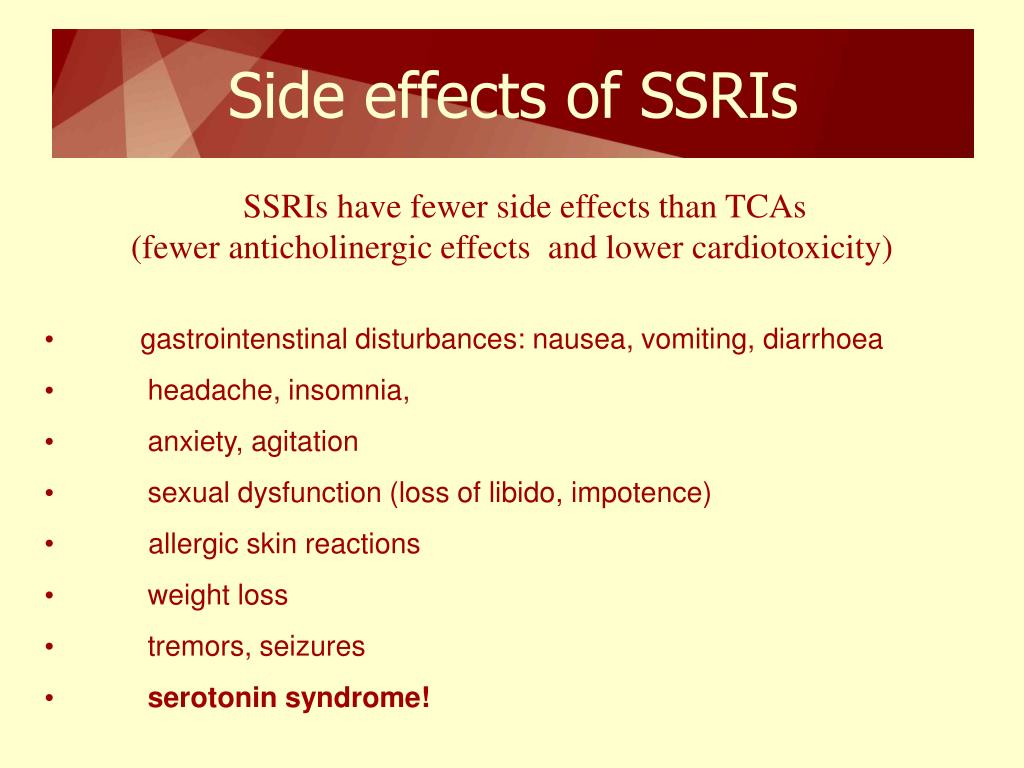
Antidepressants
If you’ve been diagnosed with clinical depression, your healthcare provider will likely prescribe an antidepressant.
Antidepressants work by increasing the levels of neurotransmitters in your brain that regulate your moods, thoughts and feelings. Common types of antidepressants include:
Selective serotonin reuptake inhibitors (SSRIs)
Serotonin-norepinephrine reuptake inhibitors (SNRIs)
Tricyclic antidepressants (TCAs)
Monoamine oxidase inhibitors (MAOIs)
Antidepressants are usually effective at reducing the severity of physical and mood symptoms caused by depression, but their effects aren’t immediate.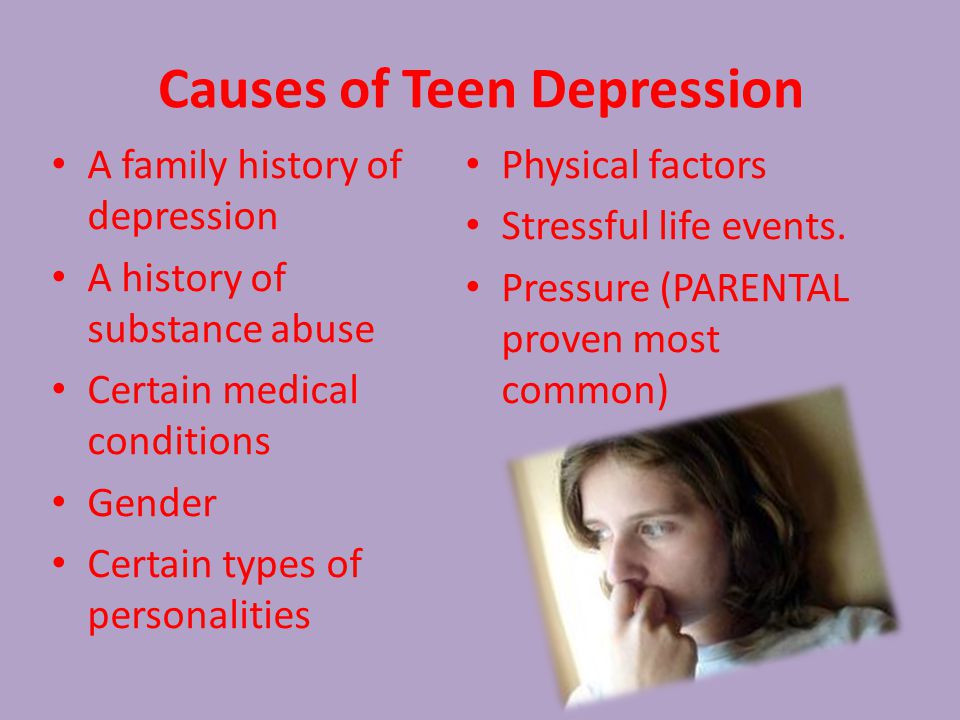 It may take two to four weeks before you notice any effects from your medication.
It may take two to four weeks before you notice any effects from your medication.
Most people use antidepressants for six to 12 months. Stopping treatment for depression too early can increase your risk of experiencing a relapse.
If you’re prescribed an antidepressant, make sure to take it exactly as directed by your mental health provider. Inform your mental health provider if you experience any side effects or would like to stop using your medication.
Our full list of antidepressants provides more information about the most effective medications for treating depression.
Psychotherapy
Psychotherapy, or talk therapy, often helps to treat depression. This type of treatment involves working with a mental health professional to identify and change the specific thoughts, feelings and behaviors that may be contributing to your depression symptoms.
A variety of forms of psychotherapy are used to treat depression, including cognitive behavioral therapy (CBT), problem-solving therapy and interpersonal therapy (IPT).
Your mental health provider may recommend therapy on its own or in combination with the use of antidepressants.
Habits and Lifestyle Changes
Sometimes, making changes to your habits and daily life can make recovering from depression an easier process.
Simple things such as staying physically active, spending time with friends and family, avoiding social isolation and setting realistic goals for your recovery can often have a big impact on your progress.
Our list of 11 ways to help depression shares simple but effective techniques you can try in combination with medication and therapy to assist in your recovery.
online psychiatrist prescriptions
talk to a psychiatry provider. it’s never been easier
Get Expert Help for Depression
If you’ve recently started to notice the signs of depression and think that a medication you use could be responsible, you might be right.
Even if you think a medication may be causing you to feel depressed, it’s important not to stop using it abruptly. Instead, you should seek expert help to learn more about your options.
Instead, you should seek expert help to learn more about your options.
You can get help for depression by talking to your primary care provider, visiting a psychiatrist locally or using our online mental health services. It’s especially important to seek help if your symptoms are severe, or if you have suicidal thoughts.
If your provider thinks your symptoms are caused by your medication, they might recommend adjusting your dosage or changing to something else. They may also suggest antidepressants or therapy to help you deal with your symptoms more effectively.
Depression is a serious mental illness, but it is treatable. With the right combination of mindset, medication and ongoing care, you can regain control over your life and leave depression where it belongs — in the rearview mirror.
30 Sources
Hims & Hers has strict sourcing guidelines to ensure our content is accurate and current. We rely on peer-reviewed studies, academic research institutions, and medical associations. We strive to use primary sources and refrain from using tertiary references.
We strive to use primary sources and refrain from using tertiary references.
- Major Depression. (2021, October). Retrieved from https://www.nimh.nih.gov/health/statistics/major-depression
- Depression. (2018, February). Retrieved from https://www.nimh.nih.gov/health/topics/depression
- Bains, N. & Abdijadid, S. (2021, April 20). Major Depressive Disorder. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Qato, D.M., Ozenberger, K. & Olfson, M. (2018). Prevalence of Prescription Medications With Depression as a Potential Adverse Effect Among Adults in the United States. JAMA. 319 (22), 2289-2298. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2684607
- Bounds, C.G. & Nelson, V.L. (2021, November 14). Benzodiazepines. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470159/
- Longo, L.P. & Johnson, B. (2000, April 1).
 Addiction: Part I. Benzodiazepines—Side Effects, Abuse Risk and Alternatives. American Family Physician. 61 (7), 2121-2128. Retrieved from https://www.aafp.org/afp/2000/0401/p2121.html
Addiction: Part I. Benzodiazepines—Side Effects, Abuse Risk and Alternatives. American Family Physician. 61 (7), 2121-2128. Retrieved from https://www.aafp.org/afp/2000/0401/p2121.html - Farzam, K. & Jan, A. (2021, December 13). Beta Blockers. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Ringoir, L., et al. (2014, June). Beta-blockers and depression in elderly hypertension patients in primary care. Family Medicine. 46 (6), 447-53. Retrieved from https://pubmed.ncbi.nlm.nih.gov/24911300/
- Riemer, T.G., et al. (2021). Do β-Blockers Cause Depression? Systematic Review and Meta-Analysis of Psychiatric Adverse Events During β-Blocker Therapy. 77, 1539-1548. Retrieved from https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.16590
- Prescription Stimulants DrugFacts. (2018, June). Retrieved from https://nida.nih.gov/publications/drugfacts/prescription-stimulants
- ADDERALL XR®.
 (2013, November). Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021303s026lbl.pdf
(2013, November). Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021303s026lbl.pdf - Farzam, K., Faizy, R.M. & Saadabadi, A. (2021, December 13). Stimulants. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539896/
- Sizar, O., Khade, S., Jamil, R.T. & Talati, R. (2021, October 29). Statin Medications. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430940/
- Cham, S., Koslik, H.J. & Golomb, B.A. (2016, December). Mood, Personality, and Behavior Changes During Treatment with Statins: A Case Series. Drug Safety - Case Reports. 3, 1. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5005588/
- De Giorgi, R., et al. (2021). Statins in Depression: An Evidence-Based Overview of Mechanisms and Clinical Studies. Frontiers in Psychiatry. 12, 702617. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8353114/
- Cascade, E.
 , Kalali, A.H. & Weisler, R.H. (2008, June). Varying Uses of Anticonvulsant Medications. Psychiatry. 5 (6), 31–33. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695747/
, Kalali, A.H. & Weisler, R.H. (2008, June). Varying Uses of Anticonvulsant Medications. Psychiatry. 5 (6), 31–33. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695747/ - Mula, M. & Hesdorffer, D.C. (2011). Suicidal behavior and antiepileptic drugs in epilepsy: analysis of the emerging evidence. Drug, Healthcare and Patient Safety. 3, 15–20. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3132858/
- STATISTICAL REVIEW AND EVALUATION: ANTIEPILEPTIC DRUGS AND SUICIDALITY. (2008, May 23). Retrieved from https://www.fda.gov/files/drugs/published/Statistical-Review-and-Evaluation--Antiepileptic-Drugs-and-Suicidality.pdf
- Celano, C.M., et al. (2011, March). Depressogenic effects of medications: a review. Dialogues in Clinical Neuroscience. 13 (1), 109–125. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181967/
- Hodgens, A. & Sharman, T. (2021, October 16). Corticosteroids.
 StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554612/
StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554612/ - Skovlund, C.W., et al. (2016, November). Association of Hormonal Contraception With Depression. JAMA Psychiatry. 73 (11), 1154–1162. Retrieved from https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2552796
- De Wit, A.E., et al. (2021, July). Hormonal contraceptive use and depressive symptoms: systematic review and network meta-analysis of randomised trials. BJPsych Open. 7 (4), e110. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8220855/
- Nowakowska, M.K., et al. (2021, December). Association of Second-generation Antiandrogens With Depression Among Patients With Prostate Cancer. JAMA Network Open. 4 (12), e2140803. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34940861/
- Ghossein, N., Kang, M. & Lakhkar, A.D. (2021, May 17). Anticholinergic Medications. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK555893/
- Wouters, H.
 , et al. (2020, February). Long-Term Exposure to Anticholinergic and Sedative Medications and Cognitive and Physical Function in Later Life. The Journals of Gerontology: Series A. 75 (2), 357-365. Retrieved from https://academic.oup.com/biomedgerontology/article/75/2/357/5298370
, et al. (2020, February). Long-Term Exposure to Anticholinergic and Sedative Medications and Cognitive and Physical Function in Later Life. The Journals of Gerontology: Series A. 75 (2), 357-365. Retrieved from https://academic.oup.com/biomedgerontology/article/75/2/357/5298370 - Welk, B & McArthur, E. (2020, December). Are anticholinergic medications used for overactive bladder associated with new onset depression? A population-based matched cohort study. Pharmacoepidemiology and Drug Safety. 29 (12), 1710-1714. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33015899/
- Proton pump inhibitors. (2021, April 22). Retrieved from https://medlineplus.gov/ency/patientinstructions/000381.htm
- Laudisio, A., et al. (2018, January). Use of proton-pump inhibitors is associated with depression: a population-based study. International Psychogeriatrics. 30 (1), 153-159. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28899441/
- Novotny, M.
 , Klimova, B. & Valis, M. (2018). PPI Long Term Use: Risk of Neurological Adverse Events? Frontiers in Neurology. 9, 1142. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6331532/
, Klimova, B. & Valis, M. (2018). PPI Long Term Use: Risk of Neurological Adverse Events? Frontiers in Neurology. 9, 1142. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6331532/ - Psychotherapies. (2021, June). Retrieved from https://www.nimh.nih.gov/health/topics/psychotherapies
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
Medicines that can cause depression and mania - HealthInfo
Home Mental health Depression and mania Medicines that can cause depression and mania
Some medicines can cause sadness, despair and sadness as side effects. These are just the feelings that come with depression. Other drugs, on the contrary, can cause a manic state - excessive excitement and joy, which is noted in bipolar disorder. nine0009
nine0009
The thing is that such drugs affect the biochemical processes in the brain. And although in many cases these drugs must be taken to cure them, they can cause side effects that are more serious than the disease itself. For example, roaccutane, which is used to treat acne, can provoke the development of depression. Oral contraceptives, blood pressure medications, and statins (medications to lower cholesterol) can have the same effect. nine0006
How can I avoid medications that can cause depression or mania?
The surest way is to find out what drugs can cause these conditions. After that, you need to discuss with your doctor the possibility of replacing the drug. But, as a rule, the doctor will warn you in advance about all side effects.
Medicines that can cause mania
The following medicines can cause manic symptoms:
- Corticosteroids, eg hydrocortisone, triamcinolone, prednisone, nasonex, azmacort.
 These drugs reduce inflammation and swelling and reduce the activity of the immune system.
These drugs reduce inflammation and swelling and reduce the activity of the immune system. - Cyclosporine. The drug prevents rejection of transplanted organs by suppressing the immune system.
- Lioresal. A muscle relaxant and antispasmodic used to treat multiple sclerosis and spinal cord injuries.
- Selective serotonin reuptake inhibitors such as Prozac and Paxil are used to treat depression. nine0029
- Trihexyphenidyl. The drug is used to treat Parkinson's disease.
- Other drugs for the treatment of Parkinson's disease can cause excessive excitement.
- Yohimbine. It is prescribed for impotence.
Other drugs may have this effect: drugs to treat attention deficit hyperactivity disorder (ADHD), drugs to treat underactive thyroid, some monoamine oxidase inhibitors (used to treat depression). nine0006
Medicines that can cause depression
The following medicines can contribute to depression:
- Roaccutane.
 The drug is used to treat severe acne.
The drug is used to treat severe acne. - Alcohol.
- Antabuse. The medicine is used to treat alcoholism.
- Some anticonvulsants used for epileptic seizures.
- Barbiturates, eg phenobarbital. Barbiturates have a depressing effect on the central nervous system and inhibit brain activity. Used to treat anxiety and prevent epileptic seizures. nine0029
- Benzodiazepines, eg Librium, Valium, Xanax. Benzodiazepines inhibit the activity of the central nervous system, are used to treat anxiety and insomnia, and as muscle relaxants.
- Certain beta-blockers (or beta-blockers), such as tenormin. Beta-blockers are used to treat many cardiovascular conditions, including hypertension, heart failure, angina pectoris, and irregular heart rhythms. In addition, they are used for migraines. nine0029
- Bromocriptine, parlodel - drugs for the treatment of Parkinson's disease.
- Certain calcium channel blockers. Calcium channel blockers are used to treat hypertension, angina, heart failure, and arrhythmias.
 They dilate blood vessels and slow down the rhythm of heart contractions.
They dilate blood vessels and slow down the rhythm of heart contractions. - Estrogens, eg premarin. These are female sex hormones that are used as hormone replacement therapy for menopause, as well as for the prevention and treatment of osteoporosis. nine0029
- Some fluoroquinolone antibiotics.
- Interferon alfa. This drug is used to treat certain types of cancer and hepatitis B.
- Norplant. Contraceptive.
- Opioids such as codeine and morphine. Opioids are used to relieve moderate to severe pain and are addictive.
- Statins, eg mevacor, zocor, leskol. Statins are prescribed to lower cholesterol levels and prevent myocardial infarction.
- Zovirax. It is used to treat shingles and herpes. nine0029
It should be noted that an increased risk of depression with these drugs is observed in older people.
What should I do if a prescribed medication causes symptoms of mania or depression?
If a drug has caused manic or depressive symptoms, the doctor will stop the drug or reduce its dosage.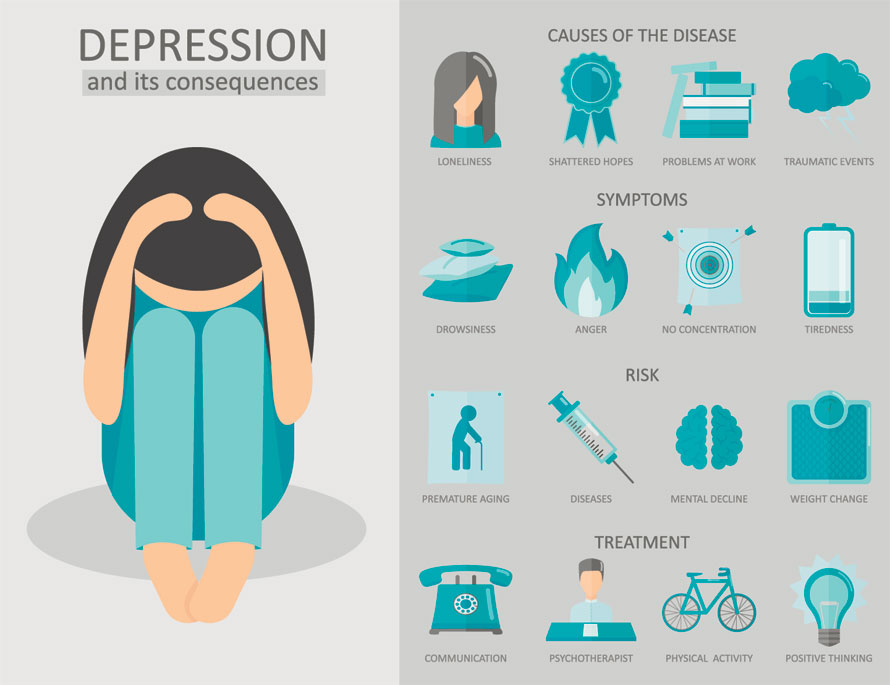 If stopping the drug is not an option, your doctor will prescribe medication to treat the symptoms of mania or depression.
If stopping the drug is not an option, your doctor will prescribe medication to treat the symptoms of mania or depression.
Should I stop taking a medication that has caused symptoms of mania or depression? nine0017
If symptoms of mania or depression appear during treatment with the above or any other drugs, you should immediately consult a doctor. You can stop taking the medicine that caused these symptoms only on the recommendation of a doctor. The doctor will assess the risk of stopping the medication and, if necessary, replace it with another one.
if ( strpos( $_SERVER['REQUEST_URI'], 'komu-nuzhna-povtornaya-vakcinaciya-a-komu-ne-nuzhna' ) === false ) { ?> } ?>Registered with the Federal Service for Supervision of Communications, Information Technology and Mass Communications on October 21, 2010. Registration certificate El No. FS77-42371. © 2023 Copyright HealthInfo
Can medications cause depression?
- Alex Therrien
- BBC health reporter
Photo credit, Getty Images
Photo caption,Experts say doctors must provide full information about which drugs you take06
When we hear about the side effects of medications, most often the first thing that comes to our mind is the physical reaction of our body, such as a headache or a rash.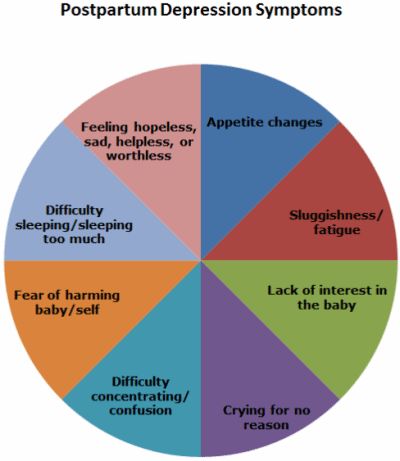 nine0119
nine0119
However, US scientists have provided new evidence that many prescription drugs can cause depression.
These include heart medications, oral contraceptives, and even some painkillers.
The study involved 26,000 people - and more than a third of the drugs they took provoked depression.
What does the study say?
In a study published in the Journal of the American Medical Association, researchers analyzed medical data from people who used at least one prescription drug between 2005 and 2014. nine0006
In 37% of the drugs taken by the subjects, depression was among the side effects.
- Is fast food a sure way to depression?
- Can you get quality health care if you are a woman?
Moreover, those who took only one drug with such a possible side reaction, the risk of developing depression increased by 7%.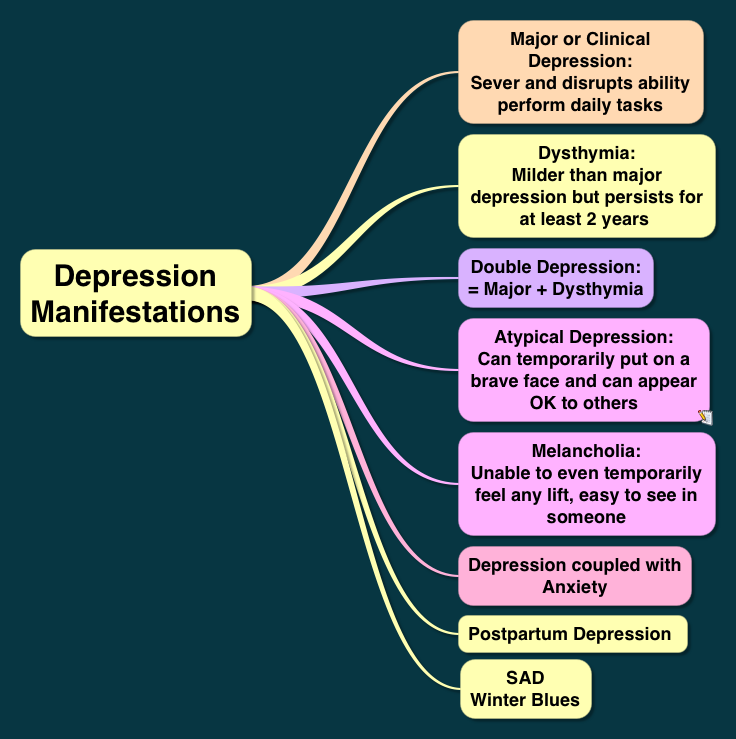 For those who took two drugs - by 9%, and for those who took three drugs - by 15%.
For those who took two drugs - by 9%, and for those who took three drugs - by 15%.
"It will surprise many that their medications, despite the fact that they may have nothing to do with mood changes or any other condition that is commonly associated with depression, can increase the risk of depressive symptoms and even lead to a diagnosis of depression" - notes Dima Kato of the University of Illinois, who led the research. nine0006
At the same time, it should be noted that any disease can negatively affect mood. In addition, some participants in the study may have experienced depression before.
What do other experts say?
British experts note that a study by their American colleagues indicates a link between drugs and an increased risk of depression, but not that drugs can cause this condition.
"It is not surprising that the use of drugs to treat physical ailments, such as heart problems or lung disease, may be associated with depressive symptoms, since these physical ailments are already associated with an increased risk of depression," explains Professor David Baldwin of the British Royal college of psychiatrists.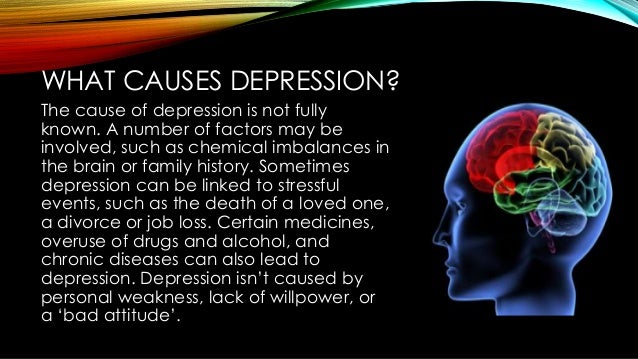 nine0006
nine0006
At the same time, Professor Helen Stokes-Lampard, chairman of the Royal College of Physicians, notes that the study indicates "how important it is for patients to tell their doctors or pharmacists about all the drugs they take."
Is there a risk?
Side effects depend on the pharmacological properties of the drug. For example, depression can be a common side effect of some oral contraceptives, meaning it affects up to 1 in 10 patients. nine0006
In turn, rare side effects may occur in 1 patient in 10 thousand.
Professor David Taylor of the British Royal Society of Pharmacy says that what's important here is whether there is a "reliable explanation" for why a particular drug causes depression.
- How bacteria affect our mood
- How hormones, immunity, microbes and pulse affect our character mood. nine0006
In other cases, it may be difficult to determine whether a drug is causing depression - or whether it is the illness for which it is prescribed.