What is mao inhibitors used for
Monoamine Oxidase Inhibitors (MAOI) - StatPearls
Tahrier Sub Laban; Abdolreza Saadabadi.
Author Information
Last Update: July 19, 2022.
Continuing Education Activity
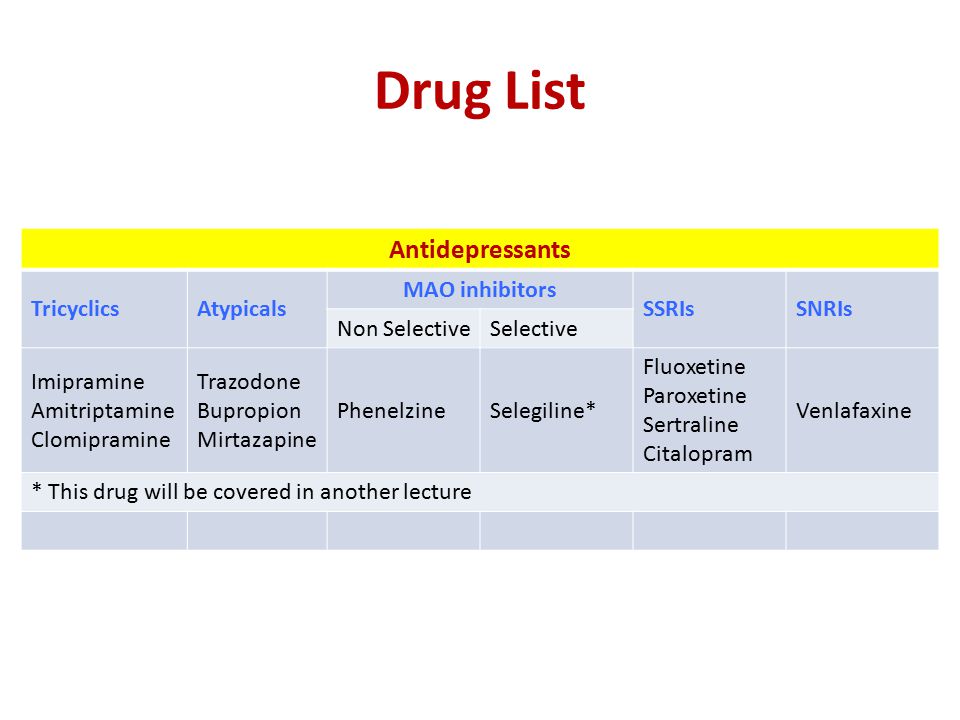
Monoamine oxidase inhibitors (MAOIs) are a separate class from other antidepressants, treating different forms of depression and other nervous system disorders such as panic disorder, social phobia, and depression with atypical features. Even though MAOIs were the first antidepressants introduced, they are not the first choice in treating mental health disorders due to several dietary restrictions, side effects, and safety concerns. MAOIs are only a treatment option when all other medications are unsuccessful. This activity will highlight the mechanism of action, adverse event profile, pharmacology, monitoring, and relevant interactions of MAOIs, pertinent for members of the interprofessional team in treating patients with conditions where this drug class has a therapeutic purpose.
Objectives:
Summarize the mechanisms of actions of the MAOI class of drugs.
Identify the approved and off-label indications for MAOI therapy.
Review the adverse event profile of MAOIs.
Outline the importance of collaboration and communication among interprofessional team members to improve outcomes and treatment efficacy for patients who might benefit from MAOI therapy.
Access free multiple choice questions on this topic.
Indications
Monoamine oxidase inhibitors (MAOIs) were first introduced in the 1950s.[1][2] They are a separate class from other antidepressants, treating different forms of depression as well as other nervous system disorders such as panic disorder, social phobia, and depression with atypical features.[3] Examples of atypical features are oversleeping and overeating. Even though MAOIs were the first antidepressants introduced, they are not the first choice in treating mental health disorders due to several dietary restrictions, side effects, and safety concerns. MAOIs are only a treatment option when all other medications are unsuccessful.
MAOIs are only a treatment option when all other medications are unsuccessful.
Furthermore, examples of neurological disorders that can benefit from MAOIs are patients with Parkinson disease and those diagnosed with multiple system atrophy.[4][5] Multiple system atrophy is a neurodegenerative disease that includes symptoms affecting movement as well as blood pressure.
Mechanism of Action
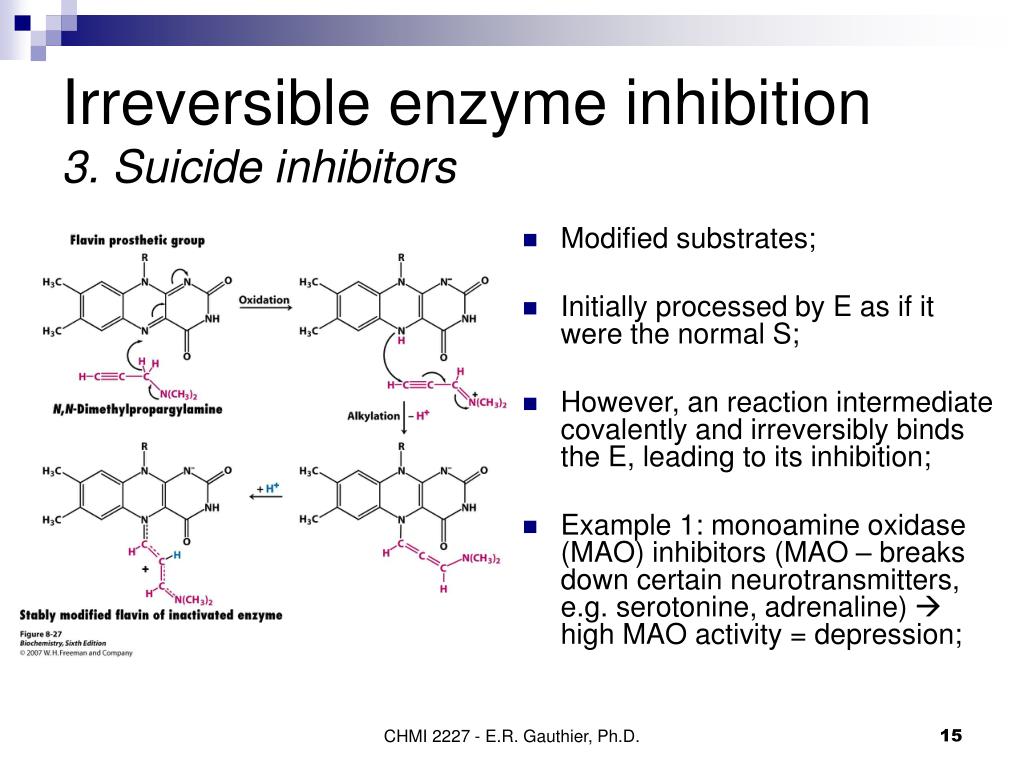
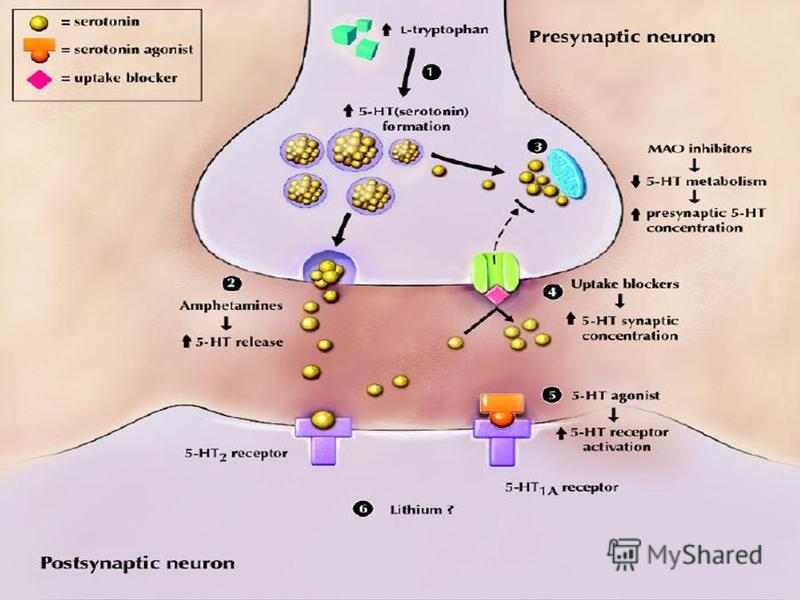
Monoamine oxidase inhibitors are responsible for blocking the monoamine oxidase enzyme. The monoamine oxidase enzyme breaks down different types of neurotransmitters from the brain: norepinephrine, serotonin, dopamine, and tyramine. MAOIs inhibit the breakdown of these neurotransmitters thus, increasing their levels and allowing them to continue to influence the cells that have been affected by depression.[6]
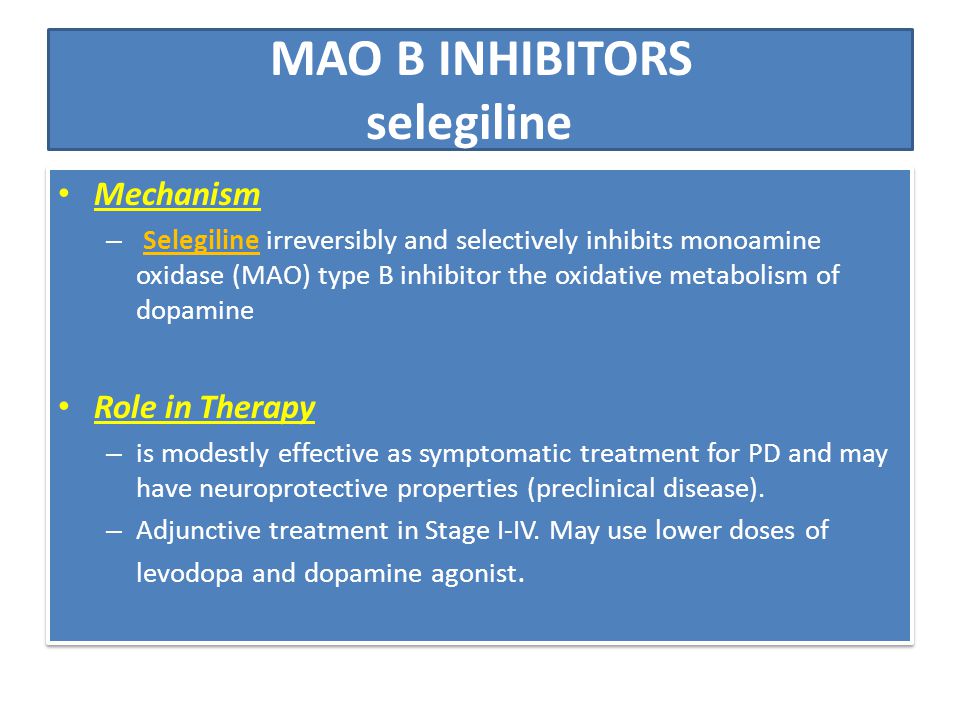
There are two types of monoamine oxidase, A and B. The MAO A is mostly distributed in the placenta, gut, and liver, but MAO B is present in the brain, liver, and platelets. Serotonin and noradrenaline are substrates of MAO A, but phenylethylamine, methylhistamine, and tryptamine are substrates of MAO B. Dopamine and tyramine are metabolized by both MAO A and B. Selegiline and rasagiline are irreversible and selective inhibitors of MAO type B, but safinamide is a reversible and selective MAO B inhibitor.[7]
Serotonin and noradrenaline are substrates of MAO A, but phenylethylamine, methylhistamine, and tryptamine are substrates of MAO B. Dopamine and tyramine are metabolized by both MAO A and B. Selegiline and rasagiline are irreversible and selective inhibitors of MAO type B, but safinamide is a reversible and selective MAO B inhibitor.[7]
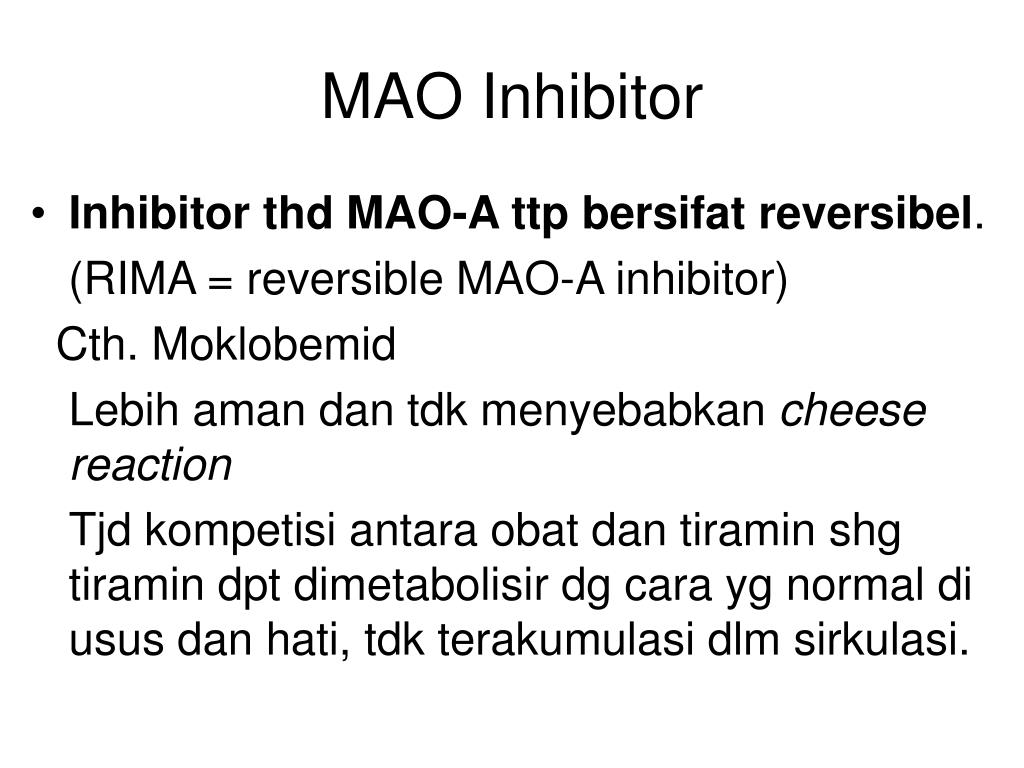
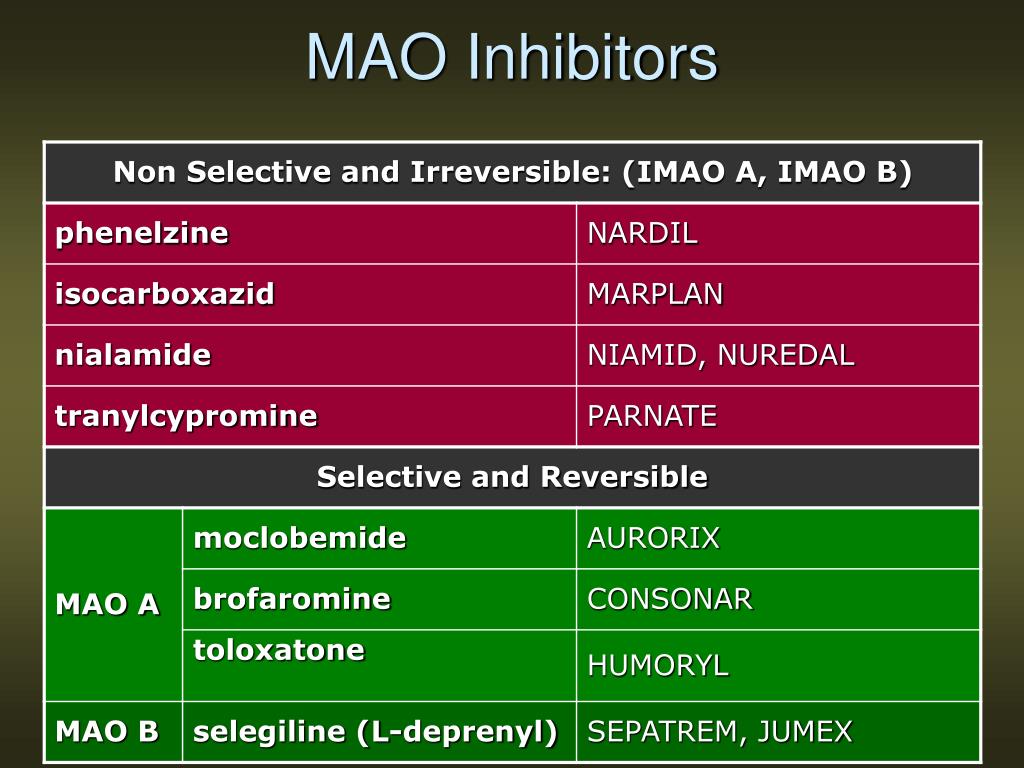
MAOIs are reversible or irreversible. Moclobemide is an example of a reversible MAOI I (RIMA), tranylcypromine, phenelzine, isocarboxazid, and selegiline irreversibly inhibit MAO. Selegiline in low doses is a selective, irreversible MAO B inhibitor, but it is no longer selective at higher doses.[8]
Administration
MAOI administration is almost always orally but sometimes comes in the form of a skin patch.[1] The skin patches were FDA approved and can be more beneficial to patients than oral dose forms. An example of this is selegiline, which can be given in a skin patch and causes fewer side effects than oral administration.[1] Patients with lower doses of MAOIs may not have to be as strict with their diet as those with higher doses.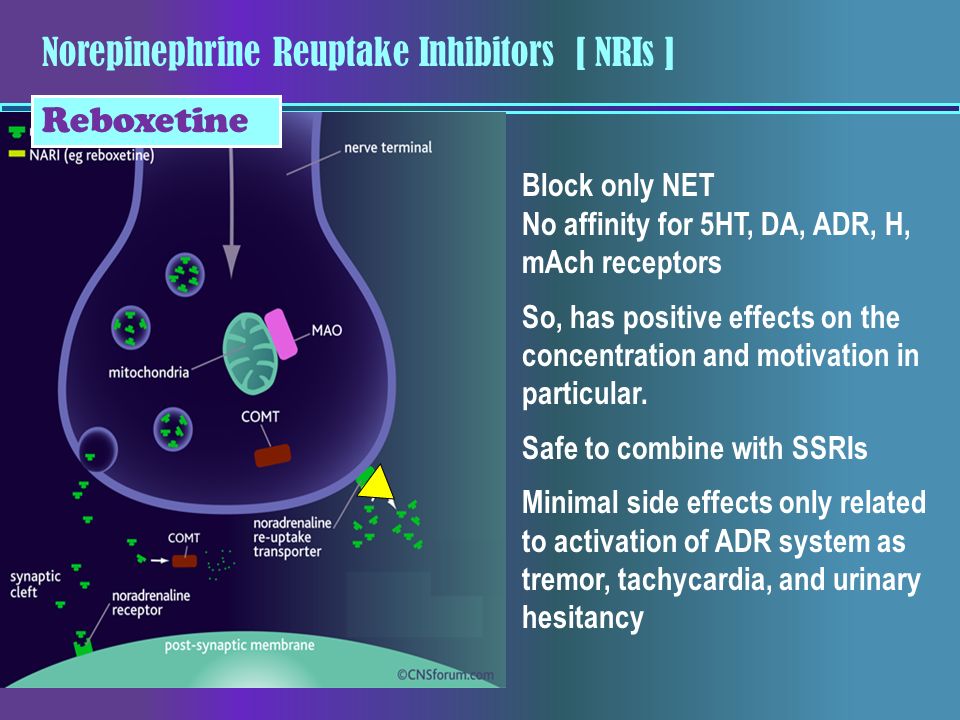
The different types of MAOIs approved by the FDA include isocarboxazid, phenelzine, selegiline, and tranylcypromine.[9] When patients are prescribed antidepressants like MAOIs, they must be aware of the time it takes to start experiencing the therapeutic effects of the drug. Usually, the medication starts to become effective within two to three weeks. However, patients should take the antidepressant for at least six months for the maximal therapeutic benefit. Patients who take an antidepressant for less than six months are shown to have a high symptomatic relapse rate.
Adverse Effects
The most frequently encountered side effects are dry mouth, nausea, diarrhea, constipation, drowsiness, insomnia, dizziness, and/or lightheadedness. Furthermore, if applied via patch, a skin reaction may occur at the patch site.[9] Recommendations are that any patient scheduled for an elective surgery that requires general anesthesia should not take MAOIs for at least ten days before the surgery to avoid any drug interaction.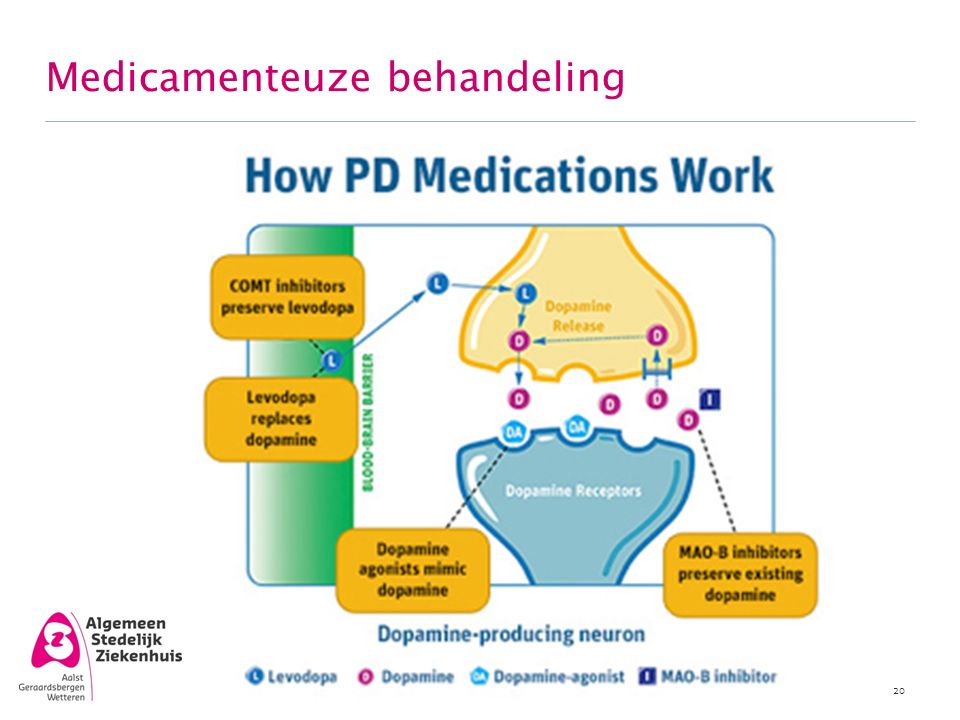 [10][11]
[10][11]
Contraindications
MAOIs can potentially cause drug-to-drug interactions, drug-food interaction, and overdoses, of which the patient should be aware.[9] For example, patients should not be mixing MAOIs with other antidepressants like selective serotonin reuptake inhibitors (SSRIs).[12] These two drugs combined can cause serotonin syndrome, which is potentially fatal. The first cases of serotonin syndrome were reported during the 1960s when patients were on MAOIs and tryptophan. Patients showed signs and symptoms of fever, confusion, increased perspiration, muscle rigidity, seizures, liver or kidney problems, fluctuation of heart rhythms, and blood pressure. Furthermore, when changing MAOIs to another antidepressant, patients should give themselves 14 days to pass before initiating the new treatment, to prevent any drug interaction.
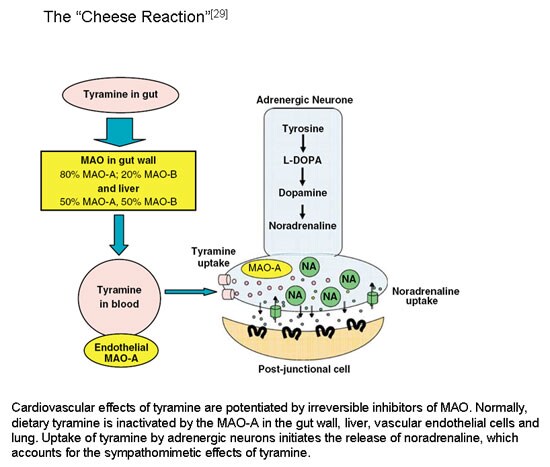
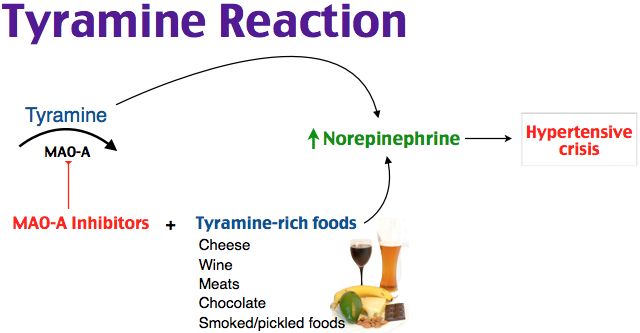
MAOIs prevent the breakdown of tyramine found in the body and certain foods, drinks, and other medications. Patients that take MAOIs and consume tyramine-containing foods or drinks will exhibit high serum tyramine level.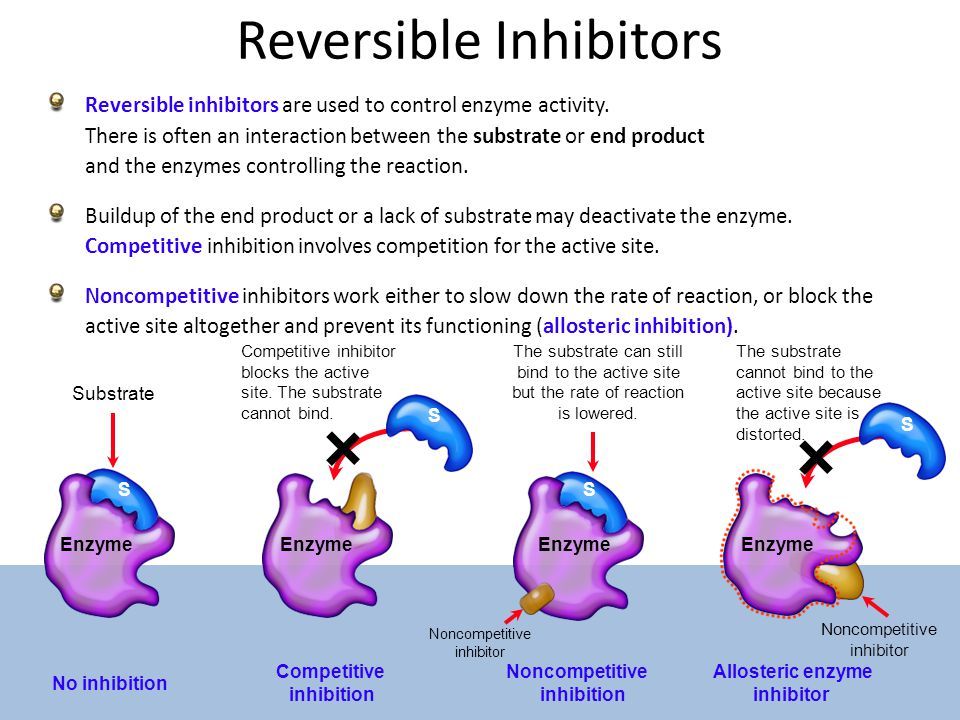 [13][14] A high level of tyramine can cause a sudden increase in blood pressure, called the tyramine pressor response.[14] Even though it is rare, a high tyramine level can trigger a cerebral hemorrhage, which can even result in death.
[13][14] A high level of tyramine can cause a sudden increase in blood pressure, called the tyramine pressor response.[14] Even though it is rare, a high tyramine level can trigger a cerebral hemorrhage, which can even result in death.
Eating foods with high tyramine can trigger a reaction that can have serious consequences.[14] Patients should know that tyramine can increase with the aging of food; they should be encouraged to have fresh foods instead of leftovers or food prepared hours earlier. Examples of high levels of tyramine in food are types of fish and types of meat, including sausage, turkey, liver, and salami.[15][16] Also, certain fruits can contain tyramine, like overripe fruits, avocados, bananas, raisins, or figs. Further examples are cheeses, alcohol, and fava beans; all of these should be avoided even after two weeks of stopping MAOIs.[16] Anyone taking MAOIs is at risk for an adverse hypertensive reaction, with accompanying morbidity.
Tramadol, meperidine, dextromethorphan, and methadone are contraindicated in patients on MAOIs as they are at high risk for causing serotonin syndrome.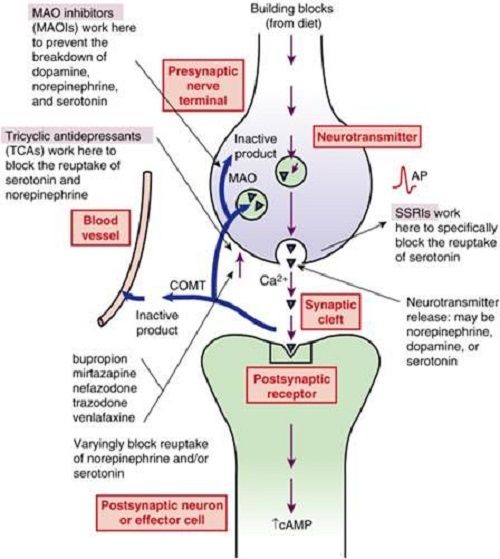 [8]
[8]
In general, SSRIs, SNRIs, TCAs, bupropion, mirtazapine, St. John's Wort and, sympathomimetic amines, including stimulants, are contraindicated with MAOIs.[8]
Monitoring
Even though MAOIs are no longer a first-line treatment option, they are still in use, and it is essential to note the precautions when initiating treatment.[12] Patients should be encouraged by health providers to carry identification cards or wear a wristband.[9] Patients always need to notify every doctor they encounter, whether dental or medical, to avoid any health consequences, especially due to the medications' influence on the vasculature.
Toxicity
Patients taking MAOIs can overdose and may show similar side effects, as stated above, except with more severe presentation.[17] Anyone on MAOIs may experience symptoms slowly within the first 24 to 48 hours. However, symptoms can be nonspecific, which range from mild to severe to even life-threatening. Depending on the MAOI prescribed, some can cause patients to go into a coma, and others (e.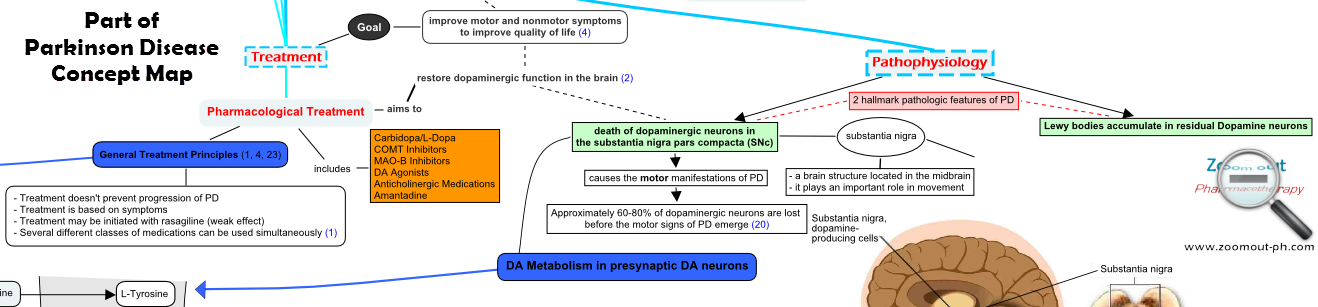 g., overdosing on tranylcypromine) can result in death.[9] The severity depends on the amount consumed and the type of MAOIs the patient took. For example, phenelzine and tranylcypromine being nonselective and nonreversible, increase the risk of a patient experiencing a hypertensive crisis when ingested with tyramine. However, selegiline is a selective MAO-B inhibitor with less hypertensive risk.[4] Any patient experiencing any of the following: agitation, flushing, tachycardia, hypotension or hypertension, palpations, twitching, increased deep tendon reflexes, seizures, or high fevers should immediately report to a health provider.[9]
g., overdosing on tranylcypromine) can result in death.[9] The severity depends on the amount consumed and the type of MAOIs the patient took. For example, phenelzine and tranylcypromine being nonselective and nonreversible, increase the risk of a patient experiencing a hypertensive crisis when ingested with tyramine. However, selegiline is a selective MAO-B inhibitor with less hypertensive risk.[4] Any patient experiencing any of the following: agitation, flushing, tachycardia, hypotension or hypertension, palpations, twitching, increased deep tendon reflexes, seizures, or high fevers should immediately report to a health provider.[9]
Enhancing Healthcare Team Outcomes
Safety and optimal treatment are vital to patient health. Patients with a history of seizures or epilepsy should avoid MAOIs; these medications can increase the occurrence of seizures. Also, people with a history of alcoholism, angina, severe headaches, blood vessel disease, diabetes, kidney or liver disease, history of a recent heart attack or stroke, overactive thyroid, and pheochromocytoma should not receive MAOI therapy; since this may cause a hypertensive crisis.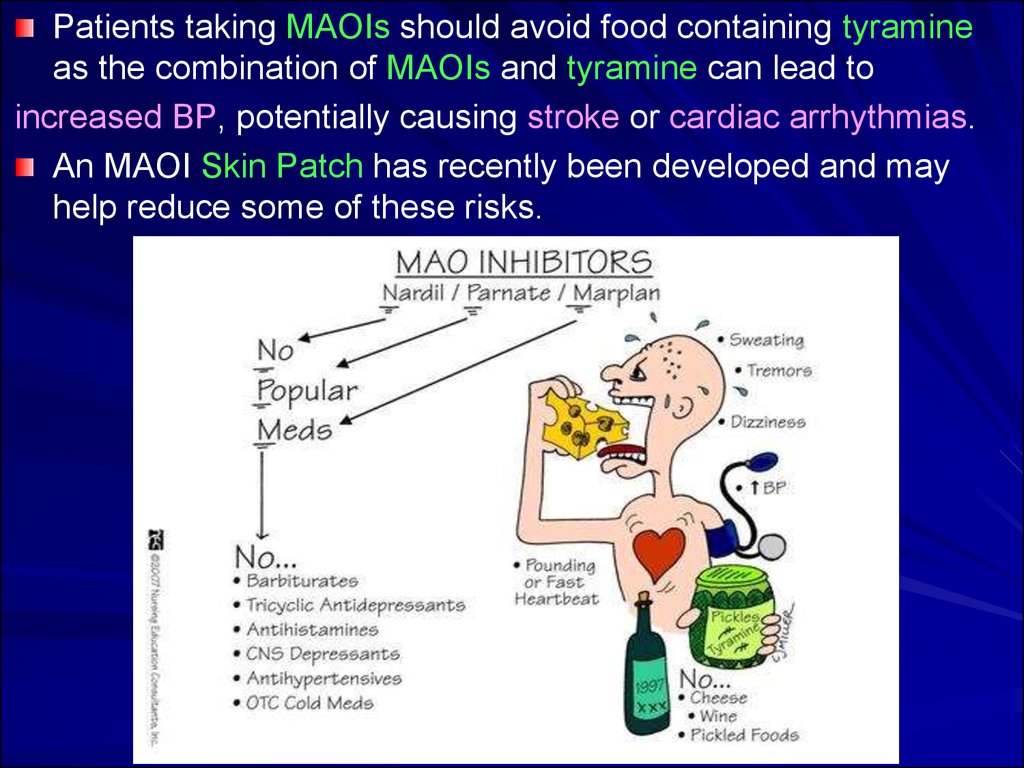 [2] This caution is also necessary for patients with a family history of depression, any neurological disorders, or even if any family members have attempted suicide. Due to the high risks, patients must provide a complete family history. Educating the patient on the importance of possible risks and side effects of the drug is critical for their well-being. It provides them an opportunity for a better outcome.
[2] This caution is also necessary for patients with a family history of depression, any neurological disorders, or even if any family members have attempted suicide. Due to the high risks, patients must provide a complete family history. Educating the patient on the importance of possible risks and side effects of the drug is critical for their well-being. It provides them an opportunity for a better outcome.
Ads with other illnesses, depression, and other psychiatric treatment plans pose multiple dilemmas for physicians.[17] These patients may need to try various medication regimens before achieving effective treatment. Someone experiencing depression or panic attacks may have significant life changes, and usually, the family physician is aware of these changes. While a psychiatric physician is almost always involved with patients dealing with different types of mental health issues, it is important to consult with an interprofessional group specialist that includes a family physician, internal medicine, specialty-trained mental health nurse, neurologist, and pharmacist.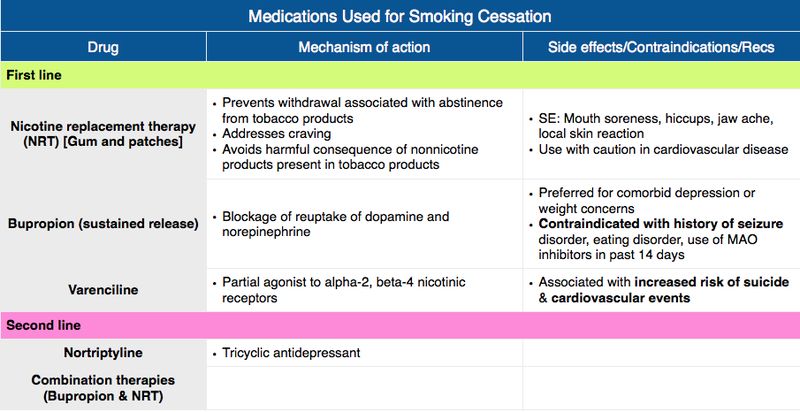 [18] Also, all other health providers involved in the patient's care are vital members of the interprofessional team, for example, other nurses and social workers. Each member provides an essential element to the patient's treatment plan. Evidence has shown that promoting interprofessional communication by consulting specialists can improve the outcome of a patient's health and their adherence to the plan.[19] [Level 5]
[18] Also, all other health providers involved in the patient's care are vital members of the interprofessional team, for example, other nurses and social workers. Each member provides an essential element to the patient's treatment plan. Evidence has shown that promoting interprofessional communication by consulting specialists can improve the outcome of a patient's health and their adherence to the plan.[19] [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Culpepper L. Reducing the Burden of Difficult-to-Treat Major Depressive Disorder: Revisiting Monoamine Oxidase Inhibitor Therapy. Prim Care Companion CNS Disord. 2013;15(5) [PMC free article: PMC3907330] [PubMed: 24511450]
- 2.
Rapaport MH. Dietary restrictions and drug interactions with monoamine oxidase inhibitors: the state of the art. J Clin Psychiatry. 2007;68 Suppl 8:42-6.
 [PubMed: 17640157]
[PubMed: 17640157]- 3.
Thase ME. MAOIs and depression treatment guidelines. J Clin Psychiatry. 2012 Jul;73(7):e24. [PubMed: 22901357]
- 4.
Volz HP, Gleiter CH. Monoamine oxidase inhibitors. A perspective on their use in the elderly. Drugs Aging. 1998 Nov;13(5):341-55. [PubMed: 9829163]
- 5.
McFarland NR. Diagnostic Approach to Atypical Parkinsonian Syndromes. Continuum (Minneap Minn). 2016 Aug;22(4 Movement Disorders):1117-42. [PMC free article: PMC5567217] [PubMed: 27495201]
- 6.
Baker GB, Coutts RT, McKenna KF, Sherry-McKenna RL. Insights into the mechanisms of action of the MAO inhibitors phenelzine and tranylcypromine: a review. J Psychiatry Neurosci. 1992 Nov;17(5):206-14. [PMC free article: PMC1188458] [PubMed: 1362653]
- 7.
Müller T, Riederer P, Grünblatt E. Determination of Monoamine Oxidase A and B Activity in Long-Term Treated Patients With Parkinson Disease. Clin Neuropharmacol.
 2017 Sep/Oct;40(5):208-211. [PubMed: 28682929]
2017 Sep/Oct;40(5):208-211. [PubMed: 28682929]- 8.
Thomas SJ, Shin M, McInnis MG, Bostwick JR. Combination therapy with monoamine oxidase inhibitors and other antidepressants or stimulants: strategies for the management of treatment-resistant depression. Pharmacotherapy. 2015 Apr;35(4):433-49. [PubMed: 25884531]
- 9.
Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004 Jul;10(4):239-48. [PMC free article: PMC2075358] [PubMed: 15552546]
- 10.
Saraghi M, Golden LR, Hersh EV. Anesthetic Considerations for Patients on Antidepressant Therapy-Part I. Anesth Prog. 2017 Winter;64(4):253-261. [PMC free article: PMC5715313] [PubMed: 29200376]
- 11.
Saraghi M, Golden L, Hersh EV. Anesthetic Considerations for Patients on Antidepressant Therapy - Part II. Anesth Prog. 2018 Spring;65(1):60-65. [PMC free article: PMC5841487] [PubMed: 29509514]
- 12.

Flockhart DA. Dietary restrictions and drug interactions with monoamine oxidase inhibitors: an update. J Clin Psychiatry. 2012;73 Suppl 1:17-24. [PubMed: 22951238]
- 13.
Brown C, Taniguchi G, Yip K. The monoamine oxidase inhibitor-tyramine interaction. J Clin Pharmacol. 1989 Jun;29(6):529-32. [PubMed: 2666453]
- 14.
Sathyanarayana Rao TS, Yeragani VK. Hypertensive crisis and cheese. Indian J Psychiatry. 2009 Jan;51(1):65-6. [PMC free article: PMC2738414] [PubMed: 19742203]
- 15.
Walker SE, Shulman KI, Tailor SA, Gardner D. Tyramine content of previously restricted foods in monoamine oxidase inhibitor diets. J Clin Psychopharmacol. 1996 Oct;16(5):383-8. [PubMed: 8889911]
- 16.
Sullivan EA, Shulman KI. Diet and monoamine oxidase inhibitors: a re-examination. Can J Psychiatry. 1984 Dec;29(8):707-11. [PubMed: 6394124]
- 17.
Thorp M, Toombs D, Harmon B. Monoamine oxidase inhibitor overdose.
 West J Med. 1997 Apr;166(4):275-7. [PMC free article: PMC1304212] [PubMed: 9168689]
West J Med. 1997 Apr;166(4):275-7. [PMC free article: PMC1304212] [PubMed: 9168689]- 18.
Culpepper L. The use of monoamine oxidase inhibitors in primary care. J Clin Psychiatry. 2012;73 Suppl 1:37-41. [PubMed: 22951241]
- 19.
Agius M, Murphy CL, Zaman R. Does shared care help in the treatment of depression? Psychiatr Danub. 2010 Nov;22 Suppl 1:S18-22. [PubMed: 21057395]
Monoamine Oxidase Inhibitors (MAOI) - StatPearls
Tahrier Sub Laban; Abdolreza Saadabadi.
Author Information
Last Update: July 19, 2022.
Continuing Education Activity
Monoamine oxidase inhibitors (MAOIs) are a separate class from other antidepressants, treating different forms of depression and other nervous system disorders such as panic disorder, social phobia, and depression with atypical features. Even though MAOIs were the first antidepressants introduced, they are not the first choice in treating mental health disorders due to several dietary restrictions, side effects, and safety concerns.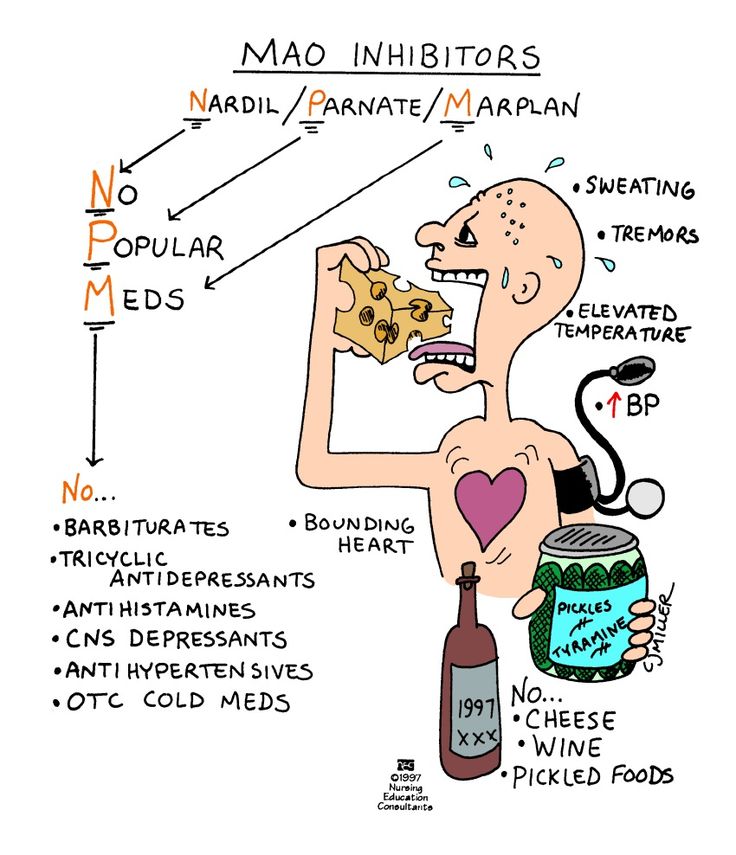 MAOIs are only a treatment option when all other medications are unsuccessful. This activity will highlight the mechanism of action, adverse event profile, pharmacology, monitoring, and relevant interactions of MAOIs, pertinent for members of the interprofessional team in treating patients with conditions where this drug class has a therapeutic purpose.
MAOIs are only a treatment option when all other medications are unsuccessful. This activity will highlight the mechanism of action, adverse event profile, pharmacology, monitoring, and relevant interactions of MAOIs, pertinent for members of the interprofessional team in treating patients with conditions where this drug class has a therapeutic purpose.
Objectives:
Summarize the mechanisms of actions of the MAOI class of drugs.
Identify the approved and off-label indications for MAOI therapy.
Review the adverse event profile of MAOIs.
Outline the importance of collaboration and communication among interprofessional team members to improve outcomes and treatment efficacy for patients who might benefit from MAOI therapy.
Access free multiple choice questions on this topic.
Indications
Monoamine oxidase inhibitors (MAOIs) were first introduced in the 1950s.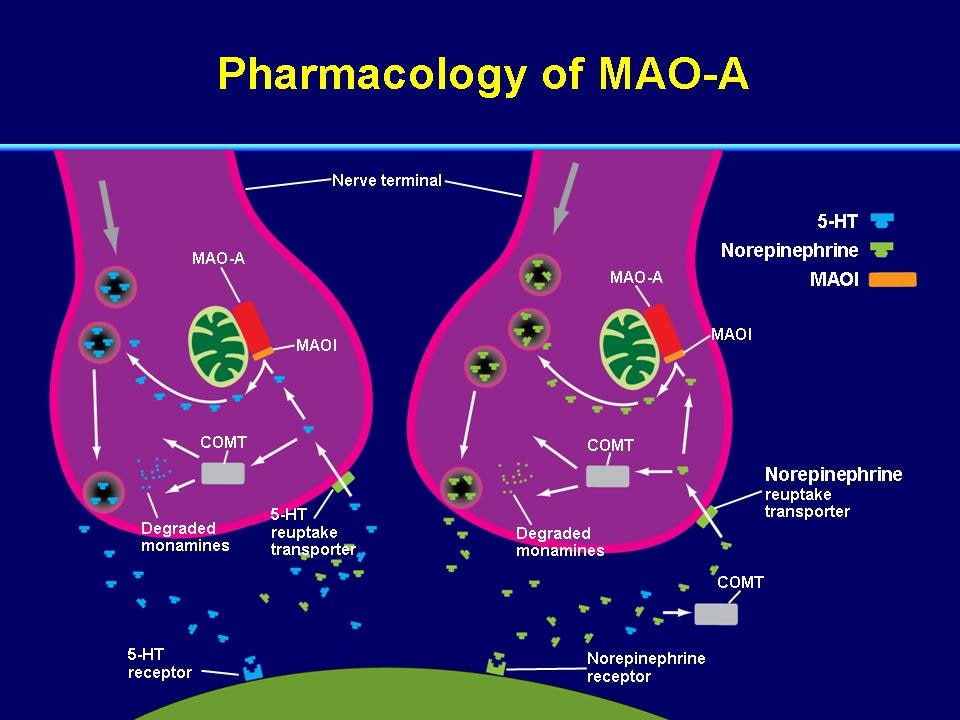 [1][2] They are a separate class from other antidepressants, treating different forms of depression as well as other nervous system disorders such as panic disorder, social phobia, and depression with atypical features.[3] Examples of atypical features are oversleeping and overeating. Even though MAOIs were the first antidepressants introduced, they are not the first choice in treating mental health disorders due to several dietary restrictions, side effects, and safety concerns. MAOIs are only a treatment option when all other medications are unsuccessful.
[1][2] They are a separate class from other antidepressants, treating different forms of depression as well as other nervous system disorders such as panic disorder, social phobia, and depression with atypical features.[3] Examples of atypical features are oversleeping and overeating. Even though MAOIs were the first antidepressants introduced, they are not the first choice in treating mental health disorders due to several dietary restrictions, side effects, and safety concerns. MAOIs are only a treatment option when all other medications are unsuccessful.
Furthermore, examples of neurological disorders that can benefit from MAOIs are patients with Parkinson disease and those diagnosed with multiple system atrophy.[4][5] Multiple system atrophy is a neurodegenerative disease that includes symptoms affecting movement as well as blood pressure.
Mechanism of Action
Monoamine oxidase inhibitors are responsible for blocking the monoamine oxidase enzyme. The monoamine oxidase enzyme breaks down different types of neurotransmitters from the brain: norepinephrine, serotonin, dopamine, and tyramine.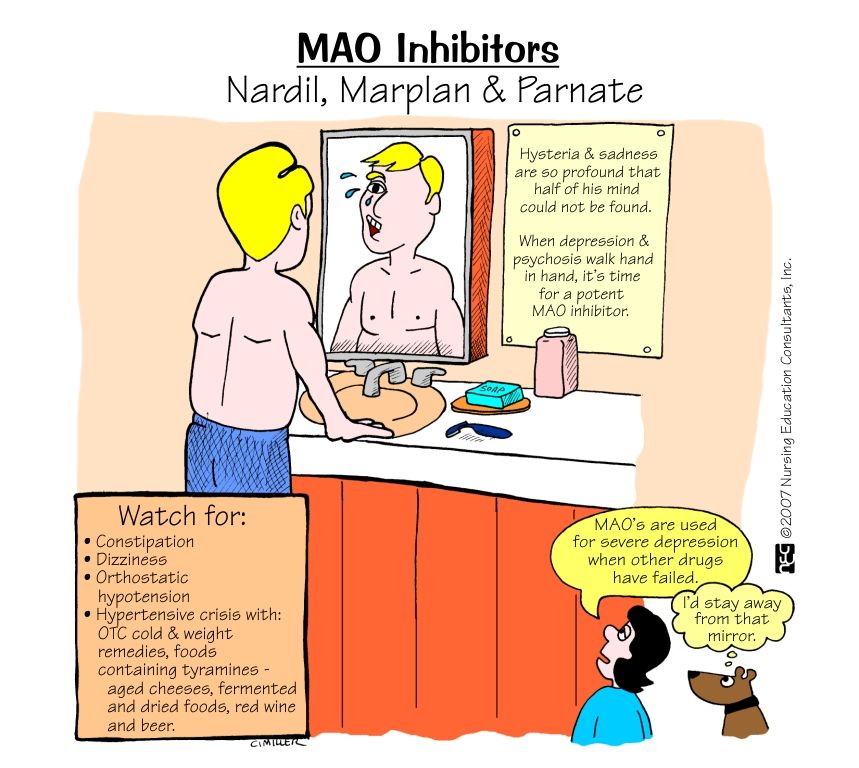 MAOIs inhibit the breakdown of these neurotransmitters thus, increasing their levels and allowing them to continue to influence the cells that have been affected by depression.[6]
MAOIs inhibit the breakdown of these neurotransmitters thus, increasing their levels and allowing them to continue to influence the cells that have been affected by depression.[6]
There are two types of monoamine oxidase, A and B. The MAO A is mostly distributed in the placenta, gut, and liver, but MAO B is present in the brain, liver, and platelets. Serotonin and noradrenaline are substrates of MAO A, but phenylethylamine, methylhistamine, and tryptamine are substrates of MAO B. Dopamine and tyramine are metabolized by both MAO A and B. Selegiline and rasagiline are irreversible and selective inhibitors of MAO type B, but safinamide is a reversible and selective MAO B inhibitor.[7]
MAOIs are reversible or irreversible. Moclobemide is an example of a reversible MAOI I (RIMA), tranylcypromine, phenelzine, isocarboxazid, and selegiline irreversibly inhibit MAO. Selegiline in low doses is a selective, irreversible MAO B inhibitor, but it is no longer selective at higher doses.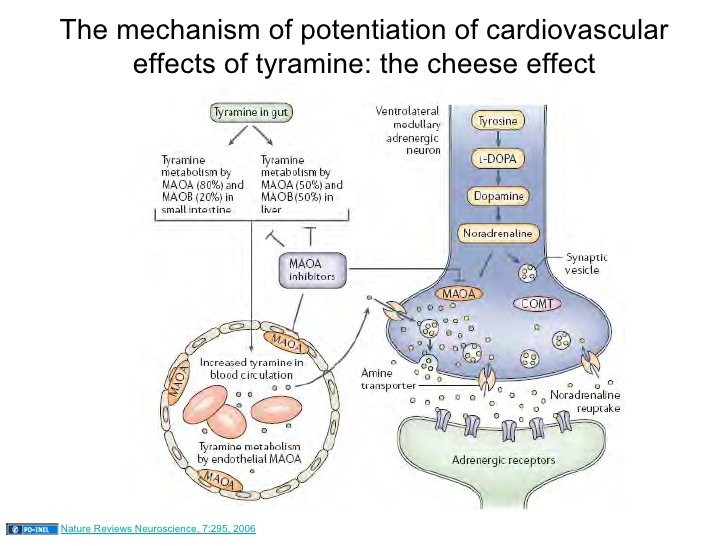 [8]
[8]
Administration
MAOI administration is almost always orally but sometimes comes in the form of a skin patch.[1] The skin patches were FDA approved and can be more beneficial to patients than oral dose forms. An example of this is selegiline, which can be given in a skin patch and causes fewer side effects than oral administration.[1] Patients with lower doses of MAOIs may not have to be as strict with their diet as those with higher doses.
The different types of MAOIs approved by the FDA include isocarboxazid, phenelzine, selegiline, and tranylcypromine.[9] When patients are prescribed antidepressants like MAOIs, they must be aware of the time it takes to start experiencing the therapeutic effects of the drug. Usually, the medication starts to become effective within two to three weeks. However, patients should take the antidepressant for at least six months for the maximal therapeutic benefit. Patients who take an antidepressant for less than six months are shown to have a high symptomatic relapse rate.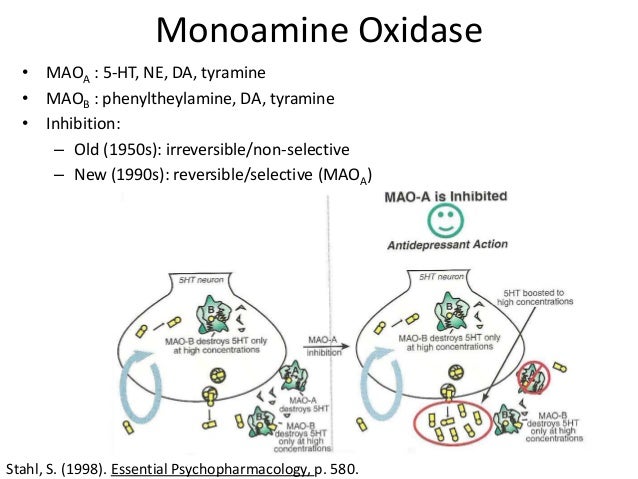
Adverse Effects
The most frequently encountered side effects are dry mouth, nausea, diarrhea, constipation, drowsiness, insomnia, dizziness, and/or lightheadedness. Furthermore, if applied via patch, a skin reaction may occur at the patch site.[9] Recommendations are that any patient scheduled for an elective surgery that requires general anesthesia should not take MAOIs for at least ten days before the surgery to avoid any drug interaction.[10][11]
Contraindications
MAOIs can potentially cause drug-to-drug interactions, drug-food interaction, and overdoses, of which the patient should be aware.[9] For example, patients should not be mixing MAOIs with other antidepressants like selective serotonin reuptake inhibitors (SSRIs).[12] These two drugs combined can cause serotonin syndrome, which is potentially fatal. The first cases of serotonin syndrome were reported during the 1960s when patients were on MAOIs and tryptophan. Patients showed signs and symptoms of fever, confusion, increased perspiration, muscle rigidity, seizures, liver or kidney problems, fluctuation of heart rhythms, and blood pressure.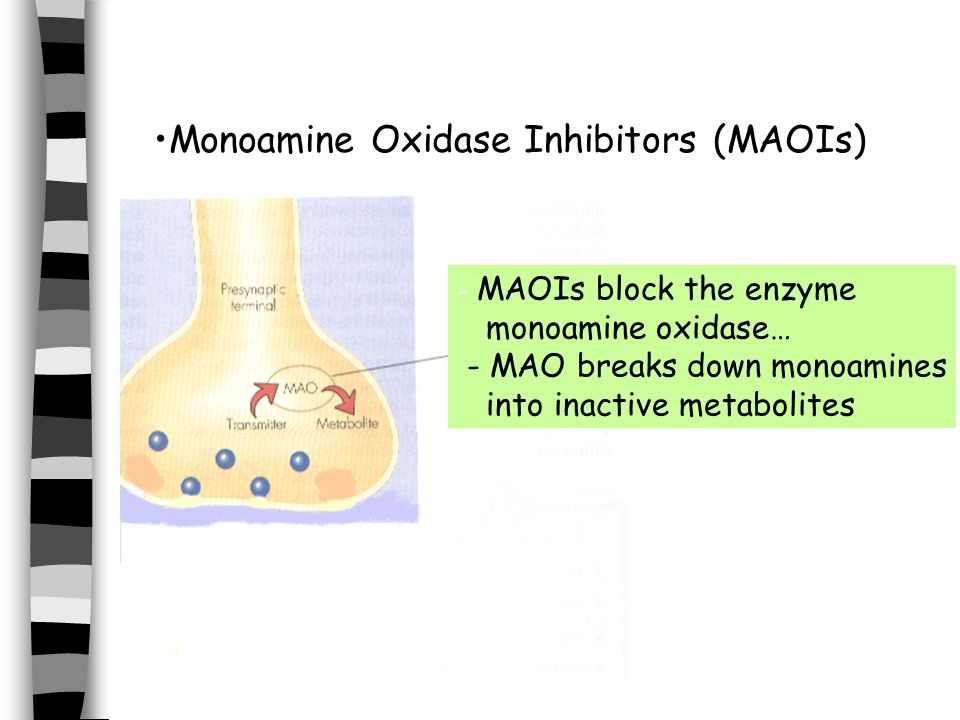 Furthermore, when changing MAOIs to another antidepressant, patients should give themselves 14 days to pass before initiating the new treatment, to prevent any drug interaction.
Furthermore, when changing MAOIs to another antidepressant, patients should give themselves 14 days to pass before initiating the new treatment, to prevent any drug interaction.
MAOIs prevent the breakdown of tyramine found in the body and certain foods, drinks, and other medications. Patients that take MAOIs and consume tyramine-containing foods or drinks will exhibit high serum tyramine level.[13][14] A high level of tyramine can cause a sudden increase in blood pressure, called the tyramine pressor response.[14] Even though it is rare, a high tyramine level can trigger a cerebral hemorrhage, which can even result in death.
Eating foods with high tyramine can trigger a reaction that can have serious consequences.[14] Patients should know that tyramine can increase with the aging of food; they should be encouraged to have fresh foods instead of leftovers or food prepared hours earlier. Examples of high levels of tyramine in food are types of fish and types of meat, including sausage, turkey, liver, and salami.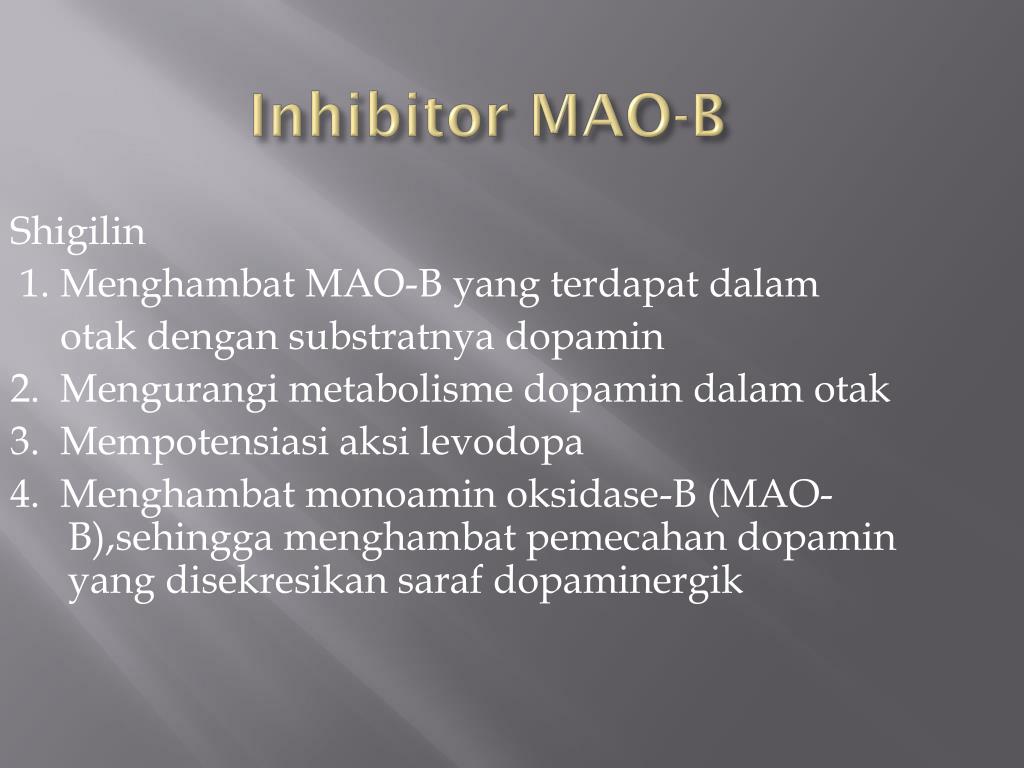 [15][16] Also, certain fruits can contain tyramine, like overripe fruits, avocados, bananas, raisins, or figs. Further examples are cheeses, alcohol, and fava beans; all of these should be avoided even after two weeks of stopping MAOIs.[16] Anyone taking MAOIs is at risk for an adverse hypertensive reaction, with accompanying morbidity.
[15][16] Also, certain fruits can contain tyramine, like overripe fruits, avocados, bananas, raisins, or figs. Further examples are cheeses, alcohol, and fava beans; all of these should be avoided even after two weeks of stopping MAOIs.[16] Anyone taking MAOIs is at risk for an adverse hypertensive reaction, with accompanying morbidity.
Tramadol, meperidine, dextromethorphan, and methadone are contraindicated in patients on MAOIs as they are at high risk for causing serotonin syndrome.[8]
In general, SSRIs, SNRIs, TCAs, bupropion, mirtazapine, St. John's Wort and, sympathomimetic amines, including stimulants, are contraindicated with MAOIs.[8]
Monitoring
Even though MAOIs are no longer a first-line treatment option, they are still in use, and it is essential to note the precautions when initiating treatment.[12] Patients should be encouraged by health providers to carry identification cards or wear a wristband.[9] Patients always need to notify every doctor they encounter, whether dental or medical, to avoid any health consequences, especially due to the medications' influence on the vasculature.
Toxicity
Patients taking MAOIs can overdose and may show similar side effects, as stated above, except with more severe presentation.[17] Anyone on MAOIs may experience symptoms slowly within the first 24 to 48 hours. However, symptoms can be nonspecific, which range from mild to severe to even life-threatening. Depending on the MAOI prescribed, some can cause patients to go into a coma, and others (e.g., overdosing on tranylcypromine) can result in death.[9] The severity depends on the amount consumed and the type of MAOIs the patient took. For example, phenelzine and tranylcypromine being nonselective and nonreversible, increase the risk of a patient experiencing a hypertensive crisis when ingested with tyramine. However, selegiline is a selective MAO-B inhibitor with less hypertensive risk.[4] Any patient experiencing any of the following: agitation, flushing, tachycardia, hypotension or hypertension, palpations, twitching, increased deep tendon reflexes, seizures, or high fevers should immediately report to a health provider.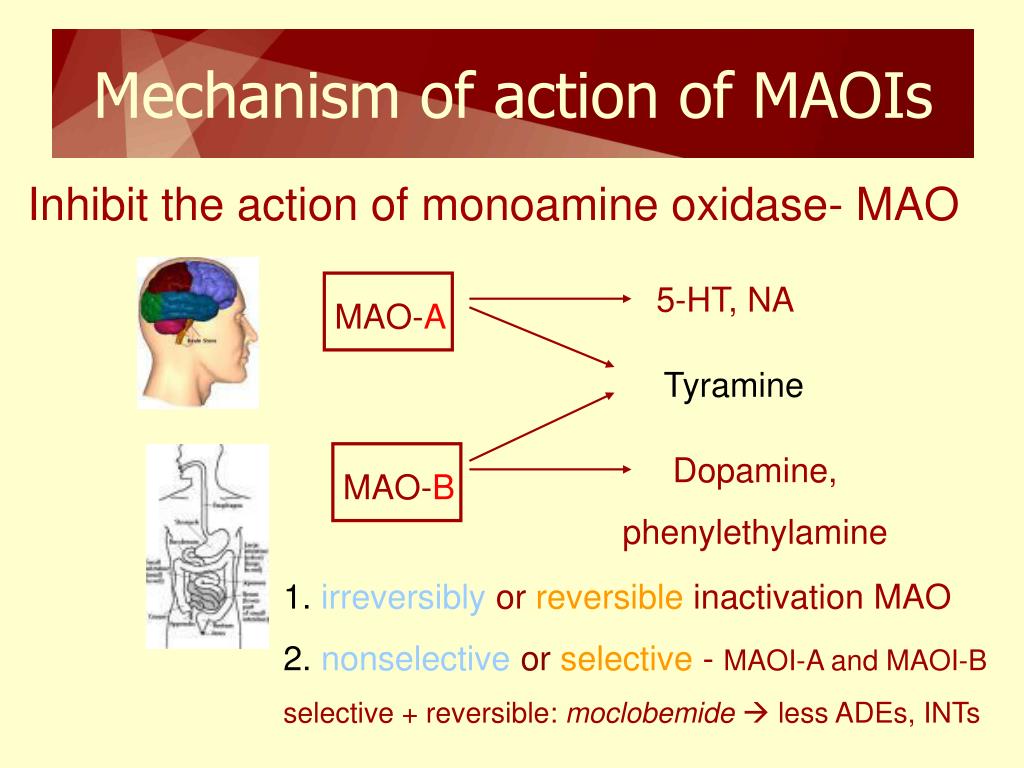 [9]
[9]
Enhancing Healthcare Team Outcomes
Safety and optimal treatment are vital to patient health. Patients with a history of seizures or epilepsy should avoid MAOIs; these medications can increase the occurrence of seizures. Also, people with a history of alcoholism, angina, severe headaches, blood vessel disease, diabetes, kidney or liver disease, history of a recent heart attack or stroke, overactive thyroid, and pheochromocytoma should not receive MAOI therapy; since this may cause a hypertensive crisis.[2] This caution is also necessary for patients with a family history of depression, any neurological disorders, or even if any family members have attempted suicide. Due to the high risks, patients must provide a complete family history. Educating the patient on the importance of possible risks and side effects of the drug is critical for their well-being. It provides them an opportunity for a better outcome.
Ads with other illnesses, depression, and other psychiatric treatment plans pose multiple dilemmas for physicians.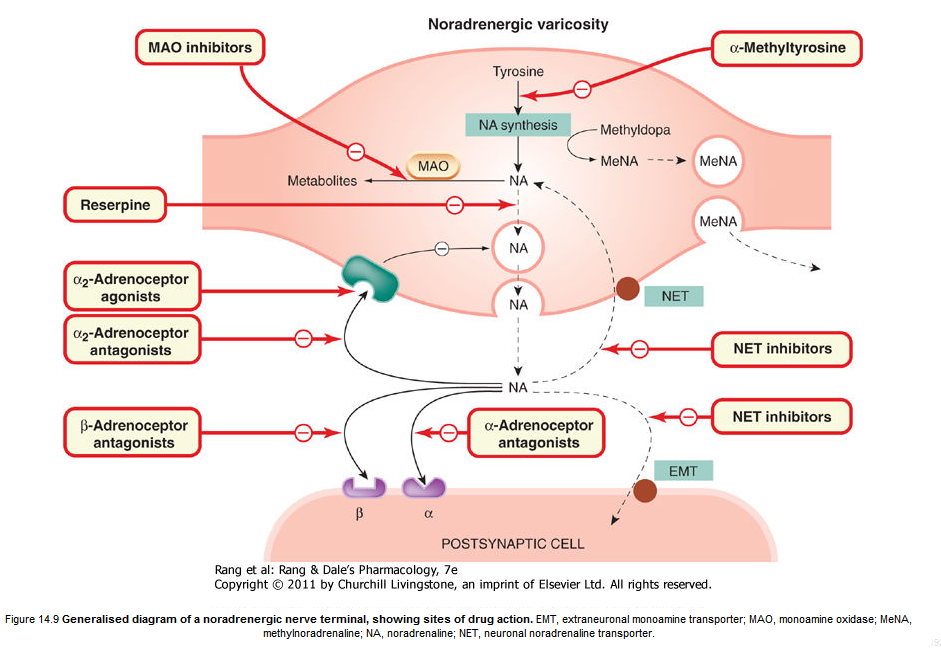 [17] These patients may need to try various medication regimens before achieving effective treatment. Someone experiencing depression or panic attacks may have significant life changes, and usually, the family physician is aware of these changes. While a psychiatric physician is almost always involved with patients dealing with different types of mental health issues, it is important to consult with an interprofessional group specialist that includes a family physician, internal medicine, specialty-trained mental health nurse, neurologist, and pharmacist.[18] Also, all other health providers involved in the patient's care are vital members of the interprofessional team, for example, other nurses and social workers. Each member provides an essential element to the patient's treatment plan. Evidence has shown that promoting interprofessional communication by consulting specialists can improve the outcome of a patient's health and their adherence to the plan.[19] [Level 5]
[17] These patients may need to try various medication regimens before achieving effective treatment. Someone experiencing depression or panic attacks may have significant life changes, and usually, the family physician is aware of these changes. While a psychiatric physician is almost always involved with patients dealing with different types of mental health issues, it is important to consult with an interprofessional group specialist that includes a family physician, internal medicine, specialty-trained mental health nurse, neurologist, and pharmacist.[18] Also, all other health providers involved in the patient's care are vital members of the interprofessional team, for example, other nurses and social workers. Each member provides an essential element to the patient's treatment plan. Evidence has shown that promoting interprofessional communication by consulting specialists can improve the outcome of a patient's health and their adherence to the plan.[19] [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Culpepper L. Reducing the Burden of Difficult-to-Treat Major Depressive Disorder: Revisiting Monoamine Oxidase Inhibitor Therapy. Prim Care Companion CNS Disord. 2013;15(5) [PMC free article: PMC3907330] [PubMed: 24511450]
- 2.
Rapaport MH. Dietary restrictions and drug interactions with monoamine oxidase inhibitors: the state of the art. J Clin Psychiatry. 2007;68 Suppl 8:42-6. [PubMed: 17640157]
- 3.
Thase ME. MAOIs and depression treatment guidelines. J Clin Psychiatry. 2012 Jul;73(7):e24. [PubMed: 22901357]
- 4.
Volz HP, Gleiter CH. Monoamine oxidase inhibitors. A perspective on their use in the elderly. Drugs Aging. 1998 Nov;13(5):341-55. [PubMed: 9829163]
- 5.
McFarland NR. Diagnostic Approach to Atypical Parkinsonian Syndromes. Continuum (Minneap Minn). 2016 Aug;22(4 Movement Disorders):1117-42. [PMC free article: PMC5567217] [PubMed: 27495201]
- 6.
Baker GB, Coutts RT, McKenna KF, Sherry-McKenna RL. Insights into the mechanisms of action of the MAO inhibitors phenelzine and tranylcypromine: a review. J Psychiatry Neurosci. 1992 Nov;17(5):206-14. [PMC free article: PMC1188458] [PubMed: 1362653]
- 7.
Müller T, Riederer P, Grünblatt E. Determination of Monoamine Oxidase A and B Activity in Long-Term Treated Patients With Parkinson Disease. Clin Neuropharmacol. 2017 Sep/Oct;40(5):208-211. [PubMed: 28682929]
- 8.
Thomas SJ, Shin M, McInnis MG, Bostwick JR. Combination therapy with monoamine oxidase inhibitors and other antidepressants or stimulants: strategies for the management of treatment-resistant depression. Pharmacotherapy. 2015 Apr;35(4):433-49. [PubMed: 25884531]
- 9.
Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004 Jul;10(4):239-48. [PMC free article: PMC2075358] [PubMed: 15552546]
- 10.

Saraghi M, Golden LR, Hersh EV. Anesthetic Considerations for Patients on Antidepressant Therapy-Part I. Anesth Prog. 2017 Winter;64(4):253-261. [PMC free article: PMC5715313] [PubMed: 29200376]
- 11.
Saraghi M, Golden L, Hersh EV. Anesthetic Considerations for Patients on Antidepressant Therapy - Part II. Anesth Prog. 2018 Spring;65(1):60-65. [PMC free article: PMC5841487] [PubMed: 29509514]
- 12.
Flockhart DA. Dietary restrictions and drug interactions with monoamine oxidase inhibitors: an update. J Clin Psychiatry. 2012;73 Suppl 1:17-24. [PubMed: 22951238]
- 13.
Brown C, Taniguchi G, Yip K. The monoamine oxidase inhibitor-tyramine interaction. J Clin Pharmacol. 1989 Jun;29(6):529-32. [PubMed: 2666453]
- 14.
Sathyanarayana Rao TS, Yeragani VK. Hypertensive crisis and cheese. Indian J Psychiatry. 2009 Jan;51(1):65-6. [PMC free article: PMC2738414] [PubMed: 19742203]
- 15.
Walker SE, Shulman KI, Tailor SA, Gardner D.
 Tyramine content of previously restricted foods in monoamine oxidase inhibitor diets. J Clin Psychopharmacol. 1996 Oct;16(5):383-8. [PubMed: 8889911]
Tyramine content of previously restricted foods in monoamine oxidase inhibitor diets. J Clin Psychopharmacol. 1996 Oct;16(5):383-8. [PubMed: 8889911]- 16.
Sullivan EA, Shulman KI. Diet and monoamine oxidase inhibitors: a re-examination. Can J Psychiatry. 1984 Dec;29(8):707-11. [PubMed: 6394124]
- 17.
Thorp M, Toombs D, Harmon B. Monoamine oxidase inhibitor overdose. West J Med. 1997 Apr;166(4):275-7. [PMC free article: PMC1304212] [PubMed: 9168689]
- 18.
Culpepper L. The use of monoamine oxidase inhibitors in primary care. J Clin Psychiatry. 2012;73 Suppl 1:37-41. [PubMed: 22951241]
- 19.
Agius M, Murphy CL, Zaman R. Does shared care help in the treatment of depression? Psychiatr Danub. 2010 Nov;22 Suppl 1:S18-22. [PubMed: 21057395]
| 04/13/12 MAO inhibitors are used to treat depression, some anxiety disorders, and other illnesses. PrecautionsTell your doctor if you are allergic to any drugs, if you are pregnant, intend to become pregnant, or are breastfeeding, before taking these medicines. While taking MAO inhibitors, it is generally best for you to check with your doctor before taking any other medicine, whether or not prescribed by other doctors. Make sure all your doctors, including dentists, know about all the medicines you take. Possible side effects Many patients do not experience any side effects while taking MAO inhibitors. In some cases, patients experience mild and transient side effects. Usually these include dizziness, feeling of lightheadedness, especially when getting up from a lying or sitting position (you should get up slowly), drowsiness, gastrointestinal disturbances, decreased appetite, muscle twitching, sexual dysfunction. Tell your doctor if side effects become bothersome. Your dosage or treatment regimen may be changed to reduce side effects. You should also tell your doctor if you experience any side effects such as dark urine, diarrhea, severe dizziness, skin rash, swelling of the feet, legs, unusual nervousness, jaundice of the eyes or skin. Stop taking this medicine and seek emergency care immediately if you experience any of the following side effects: severe chest pain, dilated pupils, severe headache, eye sensitivity to light, nausea and vomiting, stiffness or tenderness in the neck, unusually rapid or slow heartbeat, drastically increased sweating. Be patient if the remedy doesn't work right away. In some cases, at least four weeks must pass before the drug from the group of MAO inhibitors will give an effect. Carefully follow the instructions of your doctor, do not stop taking medication without his advice. Your patience may be rewarded with improved well-being. Foods, drinks and drugs to avoid while taking MAO inhibitors. The following foods, drinks, and drugs are not recommended while taking MAO inhibitors and for two weeks after stopping them. Meat and fish
vegetables and fruits, vegetables and fruits Franks broad beans | |
Monoamine oxidase inhibitors
A special group is drugs for the treatment of depression, the therapeutic effect of which is associated with inhibition of the activity of the mitochondrial enzyme monoamine oxidase, accompanied by a decrease in the breakdown of catecholamines, as well as indole amines. Most monoamine oxidase inhibitors (MAOIs) act indiscriminately and therefore increase the level of not only catecholamines and serotonin, but also dopamine.
Most monoamine oxidase inhibitors (MAOIs) act indiscriminately and therefore increase the level of not only catecholamines and serotonin, but also dopamine.
Monoamine oxidase inhibitors (iproniazid), like tricyclic antidepressants, appeared in the 1950s, in the process of finding drugs needed to treat tuberculosis.
The effectiveness of these antidepressants is controversial. In some cases, they are effective in depressions resistant to other antidepressants, with increased appetite, drowsiness, and an atypical course of depression.
The effect of MAOIs on arterial arterial pressure is unpredictable, since these drugs increase the level of norepinephrine and adrenaline in the blood, then blood pressure numbers increase. At the same time, MAOIs inhibit vasomotor centers and thereby reduce sympathetic activity (Anthony P., et al., 2002). The first signs of an increase in blood pressure may be pain in the occipital region, heaviness in the region of the heart, a tense pulse, and fainting.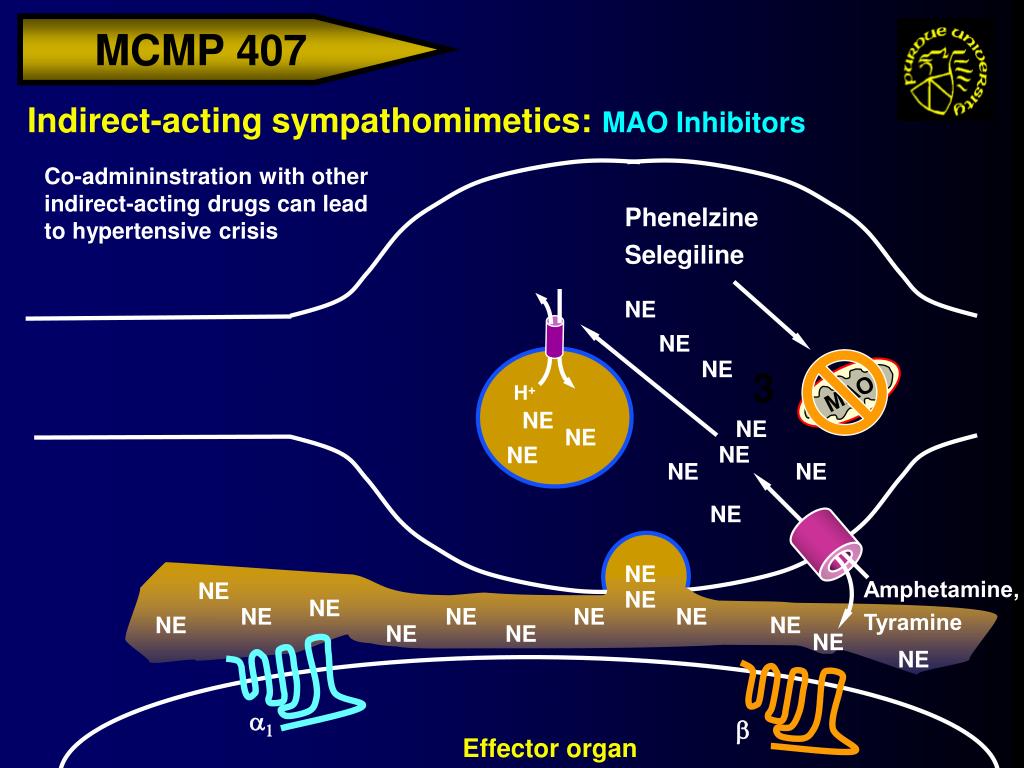
In order to prevent a sharp increase in blood pressure while taking these drugs, certain medications (desensitizing agents, anesthetics and painkillers), as well as foods containing tyramine (cheese, pizza, sour cream, smoked beef, sauerkraut) should be excluded , legumes, avocados, yeast products, soy sauce, etc.), drinks (champagne, beer, whiskey, coffee, chocolate). Normally, tyramine is destroyed by MAOI even before absorption, while under conditions of inhibition of monoamine oxidase activity, tyramine contained in food is absorbed. In the future, it is captured by adrenergic neurons, participates in synthetic processes and turns into a "false mediator" - octopamine, which in turn leads to a massive release of norepinephrine and can cause a hypertensive crisis (Anthony P., et al., 2002). MAOI preparations are metabolized in the liver and, if this organ is diseased, can cause its toxic damage.
According to L. Elkin et al. (1989), non-selective MAO inhibitors are secondary in the treatment of depression and are used only for simple and mild depression and when other, safer methods of treatment do not help.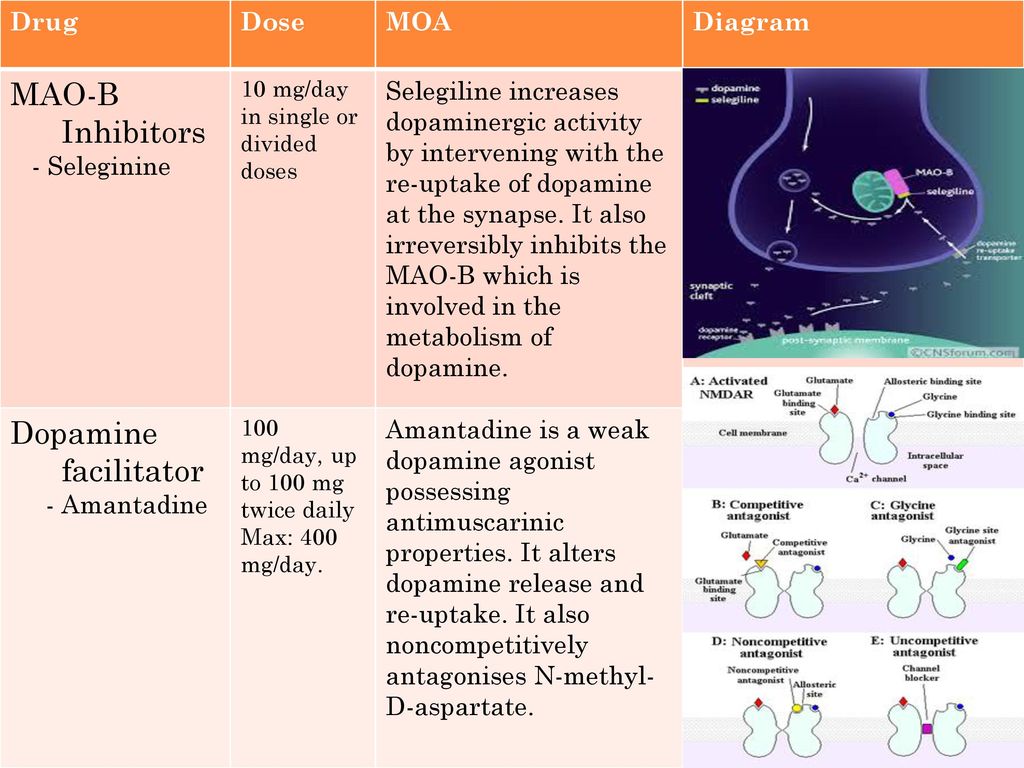 These are old, currently rarely used inhibitors - phenelzine (Nardil), isocarboxazid (Marplan), tranylcypromine (Parnate).
These are old, currently rarely used inhibitors - phenelzine (Nardil), isocarboxazid (Marplan), tranylcypromine (Parnate).
Combination of MAO inhibitors with TCAs has been shown to be effective in depression refractory to the latter drugs (Pande A., et al., 1991). Non-selective MAO inhibitors can also be effective in atypical depressions (hyperphagia, hypersomnia, anxiety and phobias) (Puzhinskiy S., 2000). It is believed that MAOIs are more effective than TCAs in the treatment of atypical depression.
The half-life of MAOIs is approximately 2.5 hours, the maximum binding of MAOIs (maximum effectiveness) is observed 14 hours after the absorption of MAOIs, however, the antidepressant effect of these drugs does not appear until 4 weeks after the start of therapy.
Modern selective monoamine oxidase inhibitors that inhibit the activity of an isolated isoenzyme A or B include: selective monoamine oxidase inhibitors of type A - pyrazidol, moclobemide, selective monoamine oxidase inhibitors of type B - selegiline (used in the early stages of Parkinson's disease).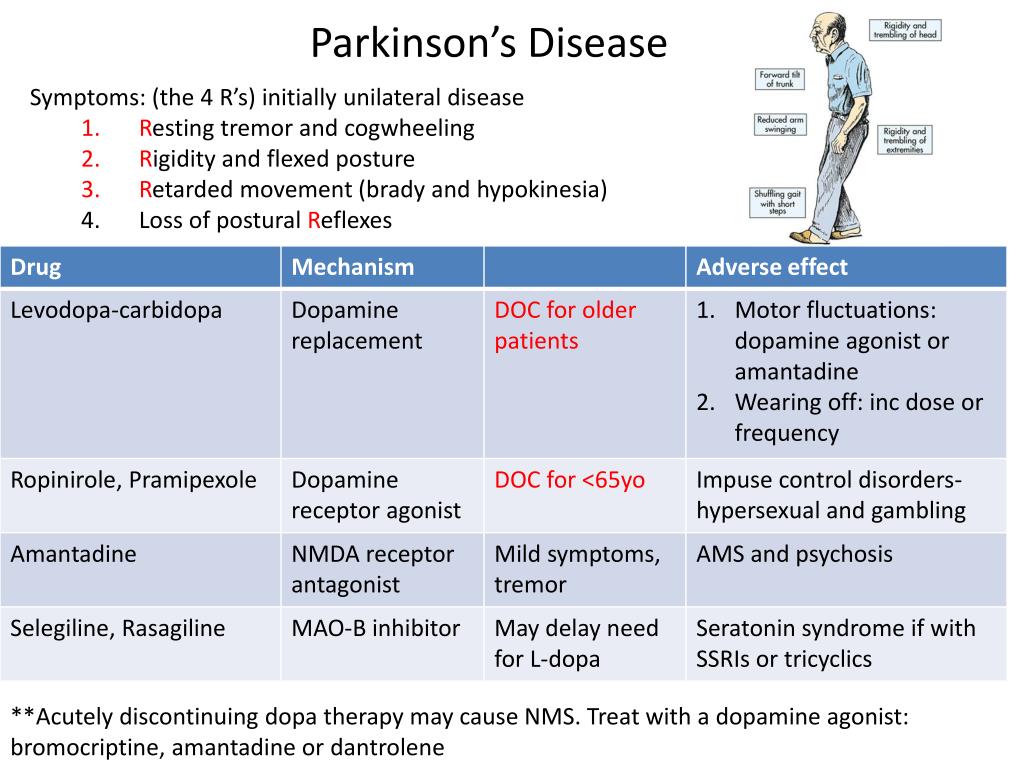
Pyrazidol
Pyrazidol is a domestic antidepressant of balanced action, it selectively inhibits type A MAO (short-term and completely reversible). The thymoanaleptic effect is manifested in the relief of depressive symptoms, primarily vital anguish, mental anesthesia and psychomotor retardation.
This drug normalizes the metabolism of monoamine neurotransmitters, blocks the deamination of serotonin, to a lesser extent - norepinephrine, and to a small extent - tyramine, partially inhibits the reuptake of monoamines. It exhibits nootropic properties and improves cognitive functions. It should be borne in mind that pyrazidol is mainly used for mild depression or its moderate forms, including neurotic and masked depressions, and may be ineffective in severe depression accompanied by manifestations of agitation (up to 50% of patients with deep depressions of the melancholic type give a positive response to therapy). pyrazidol). The drug is also used for Alzheimer's disease, "organic" depression, alcohol withdrawal syndrome.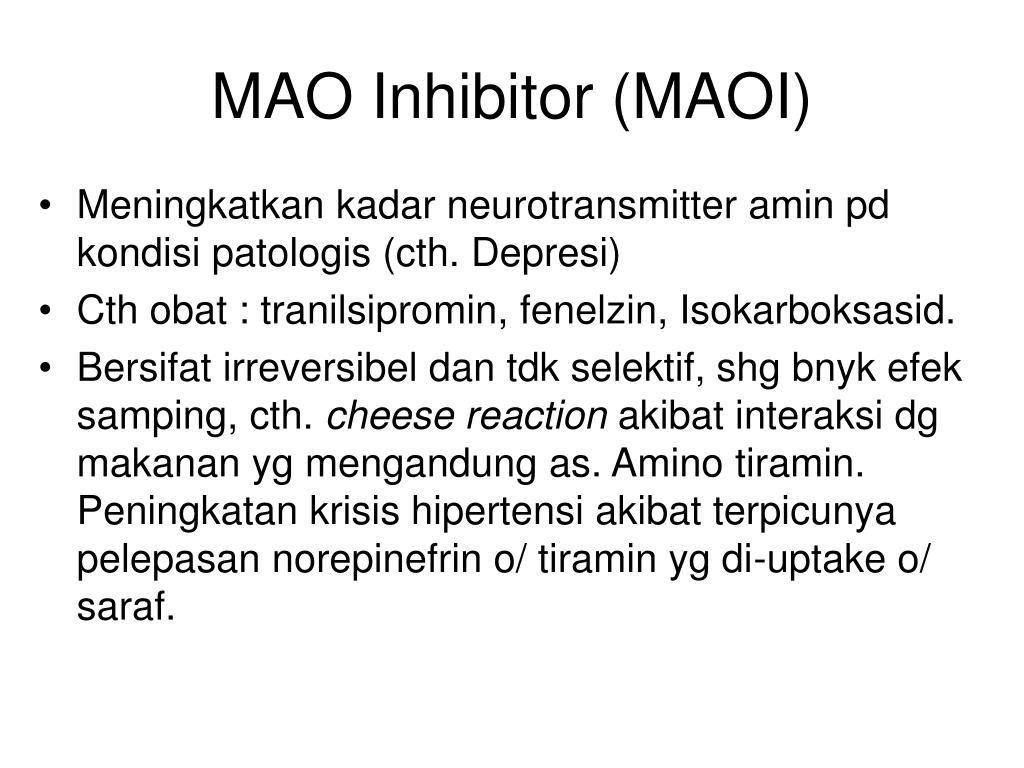 Pyrazidol is also used in the treatment of psychosomatic disorders, with astheno-depressive symptoms that have developed against the background of myocardial infarction and cerebral atherosclerosis (the drug goes well with other medicines). The drug has a normalizing effect on the lungs with manifestations of hypoxia.
Pyrazidol is also used in the treatment of psychosomatic disorders, with astheno-depressive symptoms that have developed against the background of myocardial infarction and cerebral atherosclerosis (the drug goes well with other medicines). The drug has a normalizing effect on the lungs with manifestations of hypoxia.
The therapeutic effect after taking pyrazidol appears after 3-5 days after the start of therapy. The optimal daily dose of the drug is 15-300 mg. (begin treatment with 50-75 mg in two divided doses). With a dosage of the drug over 200 mg. its sedative effect begins to dominate, and more than 400 mg. the drug may have an effect on severe endogenous depression.
The balance of action of pyrazidol is characterized by a combination of an antidepressant effect with an activating effect in adynamia and apathy and a sedative effect in an agitated state. As a result of the foregoing, the drug is effective in mixed, atypical depressions.
In the process of treatment, such comorbid depression symptoms as: manifestations of senesto-hypochondria, obsessive-compulsive states, signs of depersonalization also disappear.
Side effects of pyrazidol are mild and limited to dry mouth, sweating, weakness, tachycardia. More rarely, allergic reactions and dizziness occur. Unlike TCAs, the drug does not have an anticholinergic effect. Contraindications to the appointment of the drug are acute hepatitis and blood diseases.
Moclobemide
The psychotropic profile of a reversible selective MAO inhibitor type A (MAO-A selectively destroys serotonin, norepinephrine and dopamine) - moclobemide approaches TCAs that have a disinhibitory effect (imipramine, desipramine). Indications for the use of moclobemide are depressive states with a predominance of apathy, lethargy, anergy (Fitton A., et al. 1992).
Moclobemide is given at a dose of 300-450 mg. inside once a day after meals. If there is no effect, increase the dosage by 150 mg. per day, at intervals of 2-3 weeks (maximum daily dose - 600 mg twice a day).
Despite the fact that moclobemide inhibits MAO-A, within therapeutic doses, its interaction with sympathomimetics and tyramine-containing products is unlikely, since the main pathway of tyramine metabolism is via monoamine oxidase type B (MAO-B).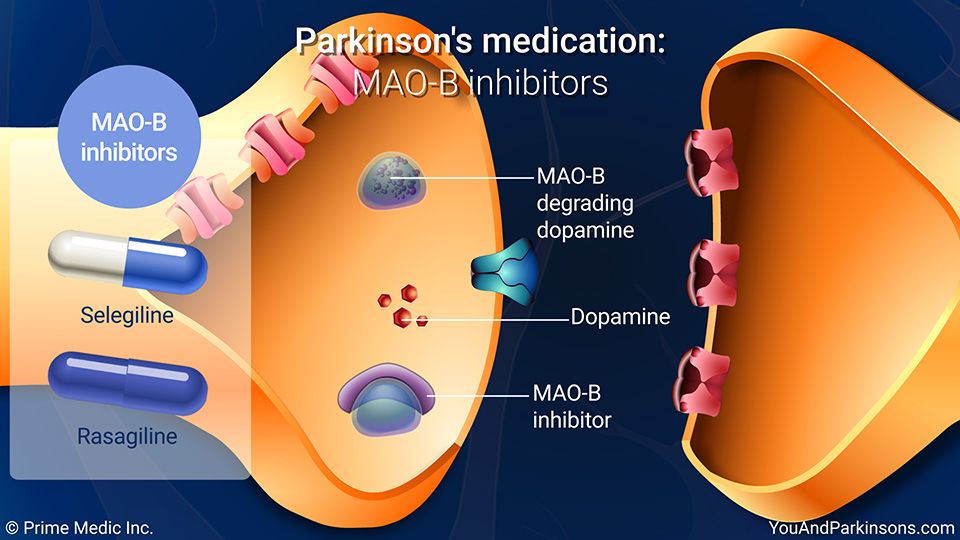 After the abolition of this antidepressant, MAO-A activity is relatively quickly restored (24-48 hours).
After the abolition of this antidepressant, MAO-A activity is relatively quickly restored (24-48 hours).
Placebo-controlled studies have shown that moclobemide has a therapeutic effect in major depression and dysthymia. J. Angst, M. Stabl (1992) and J. Angst, F. Jhonson (1994) indicate that moclobemide can be used to treat severe depression.
Due to its low toxicity and good tolerance, moclobemide is the drug of choice in the clinic of depression in the elderly. Moclobemide does not interact with alcohol.
Numerous researchers point to the good tolerability of moclobemide, due in particular to the absence of peripheral and central anticholinergic effects (Fitton A., et al., 1992; Baldwin D., Rudge S., 1994; Pujynski S., Rybakowski J., 1995).
The most common side effects of moclobemide include: dry mucous membranes (especially the oral cavity), dizziness, headaches, drowsiness, nausea, insomnia. Less common are constipation, discomfort in the stomach. Very rarely there are muscle twitches, visual impairment.