What is hebephrenia
Hebephrenia Definition & Meaning - Merriam-Webster
he·be·phre·nia ˌhē-bə-ˈfrē-nē-ə
-ˈfre-nē-
: a form of schizophrenia characterized especially by incoherence, delusions lacking an underlying theme, and affect that is usually flat, inappropriate, or silly
hebephrenic
ˌhē-bə-ˈfre-nik
-ˈfrē-nik
adjective or noun
Example Sentences
Recent Examples on the Web His acceptance speech for the Best Actor prize was a more interesting performance than the hebephrenia Phoenix displayed in Joker. Armond White, National Review
, 5 Feb. 2020
These example sentences are selected automatically from various online news sources to reflect current usage of the word 'hebephrenia.' Views expressed in the examples do not represent the opinion of Merriam-Webster or its editors. Send us feedback.
Word History
Etymology
borrowed from German Hebephrenie "type of mental disorder occurring at puberty," from Greek hēbē- (probably extracted from hēbētḗs "having reached sexual maturity, adult," from hēbē-, variant stem of hēbáō, hēbân "to reach puberty, be in the prime of youth" —derivative of hḗbē "youth, vigor of youth, sexual maturity"— + -tēs, adjective suffix) + phren-, phrḗn "midriff, seat of the passions, mind, wits" + German -ie -ia entry 1; Greek hḗbē perhaps going back to Indo-European *(H)i̯ēgw-eh2, whence also Lithuanian jėgà "strength, force," Latvian ję̄ga "power, sense" — more at frenetic
Note: The term was apparently introduced by the German psychiatrist Karl Kahlbaum (1828-99), though first used in medical literature by Kahlbaum's associate Ewald Hecker (1843-1909), in "Die Hebephrenie. Ein Beitrag zur klinischen Psychiatrie," Archiv für pathologische Anatomie und Physiologie und für klinische Medicin (Virchows Archiv), 52. Band, 3. Heft (21. März 1871), p. 405: "Kahlbaum hat in seinen Vorlesungen zuerst darauf merksam gemacht, dass dieses gewiss auffälliges Merkmal auch einen anderen Krankheitsform zukommt, die mit der Paralyse im Uebrigen nicht viel gemeinsames hat: es ist die von ihm aufgestellte Hebephrenie, eine Form der Geistesstörung, die ebenfalls wechselnde Zustandsformen zeigt und im Anschluss an die Jahre der Pubertät auftretend, mit dem in dieser Zeit vor sich gehenden grossen Umschwung der körperlichen und geistigen Entwicklung in engen Zusammenhange steht." ("Kahlbaum was the first to draw attention in his lectures to the fact that this most striking feature [the onset of dementia associated with general paresis] is attached to another form of disease with which it otherwise has little in common: hebephrenia, a kind of mental disorder put forward by him that likewise exhibits changing states and, emerging in association with the years of puberty, is closely connected with the extreme alterations in physical and mental development at this time.
Ein Beitrag zur klinischen Psychiatrie," Archiv für pathologische Anatomie und Physiologie und für klinische Medicin (Virchows Archiv), 52. Band, 3. Heft (21. März 1871), p. 405: "Kahlbaum hat in seinen Vorlesungen zuerst darauf merksam gemacht, dass dieses gewiss auffälliges Merkmal auch einen anderen Krankheitsform zukommt, die mit der Paralyse im Uebrigen nicht viel gemeinsames hat: es ist die von ihm aufgestellte Hebephrenie, eine Form der Geistesstörung, die ebenfalls wechselnde Zustandsformen zeigt und im Anschluss an die Jahre der Pubertät auftretend, mit dem in dieser Zeit vor sich gehenden grossen Umschwung der körperlichen und geistigen Entwicklung in engen Zusammenhange steht." ("Kahlbaum was the first to draw attention in his lectures to the fact that this most striking feature [the onset of dementia associated with general paresis] is attached to another form of disease with which it otherwise has little in common: hebephrenia, a kind of mental disorder put forward by him that likewise exhibits changing states and, emerging in association with the years of puberty, is closely connected with the extreme alterations in physical and mental development at this time. ") There appear to be no precedents in Greek for the use of hḗbē "youth, vigor of youth, sexual maturity" as the initial element of a compound, but the expected form would be hēbo-, which does not occur in modern Greco-Latin word formation. The form hēbē-, on the other hand, can be found in a number of New Latin botanical terms dating from at least the early nineteenth century, as hebecarpus "having pubescent seeds," hebegynus "having pubescent ovaries," etc. The combining element -phrenia (German -phrenie, French -phrénie) was apparently used first in French paraphrénie "mental illness with delusional symptoms," introduced by the Belgian physician Joseph Guislain in Traité sur les phrénopathies (Brussels, 1833).
") There appear to be no precedents in Greek for the use of hḗbē "youth, vigor of youth, sexual maturity" as the initial element of a compound, but the expected form would be hēbo-, which does not occur in modern Greco-Latin word formation. The form hēbē-, on the other hand, can be found in a number of New Latin botanical terms dating from at least the early nineteenth century, as hebecarpus "having pubescent seeds," hebegynus "having pubescent ovaries," etc. The combining element -phrenia (German -phrenie, French -phrénie) was apparently used first in French paraphrénie "mental illness with delusional symptoms," introduced by the Belgian physician Joseph Guislain in Traité sur les phrénopathies (Brussels, 1833).
First Known Use
1883, in the meaning defined above
Time Traveler
The first known use of hebephrenia was in 1883
See more words from the same year
Dictionary Entries Near
hebephreniaHebei
hebephrenia
Heber
See More Nearby Entries
Cite this Entry
Style
MLAChicagoAPAMerriam-Webster
“Hebephrenia. ” Merriam-Webster.com Dictionary, Merriam-Webster, https://www.merriam-webster.com/dictionary/hebephrenia. Accessed 9 Nov. 2022.
” Merriam-Webster.com Dictionary, Merriam-Webster, https://www.merriam-webster.com/dictionary/hebephrenia. Accessed 9 Nov. 2022.
Copy Citation
Medical Definition
hebephrenia
he·be·phre·nia ˌhē-bə-ˈfrē-nē-ə -ˈfren-ē-
: a disorganized form of schizophrenia characterized especially by incoherence, delusions which if present lack an underlying theme, and affect that is flat, inappropriate, or silly
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!
Merriam-Webster unabridged
Disorganized (Hebephrenic) Schizophrenia: What Is It?
Schizophrenia is a complex and chronic disorder of the brain that affects about 1 percent of the U. S. population.
S. population.
Characterized by multiple symptoms such as distorted thinking, behavioral difficulties, or altered perceptions of reality, schizophrenia may be described based on these symptoms.
While no longer an official diagnosis, the term hebephrenic, or disorganized, schizophrenia is still used to describe a group of symptoms.
Disorganized or hebephrenic schizophrenia describes a person with schizophrenia who has symptoms including:
- disorganized thinking
- unusual speech patterns
- flat affect
- emotions that don’t fit the situation
- incongruent facial reactions
- difficulty performing daily activities
An individual with schizophrenia who is described as hebephrenic does not have hallucinations or delusions but instead has disorganized behavior and speech.
Once considered a diagnosis, in the newest version of the Diagnostic and Statistical Manual of Mental Disorders, Edition 5 (DSM-5), the official manual that psychiatrists and other mental health professionals use, hebephrenic schizophrenia is no longer an official diagnosis.
However, the term is still considered a diagnosis in another manual, the International Classification of Diseases and Related Health Problems (ICD-10), healthcare professionals use to categorize medical conditions.
What was previously a group of subtypes is now used to describe one main overarching diagnosis and help mental health professionals plan and provide care.
Read this article for more information about subtypes and schizophrenia.
Symptoms of schizophrenia may include:
- hallucinations: hearing, seeing, or feeling things that aren’t there
- delusions: false beliefs or suspicions not shared by others, even in the face of contradictory evidence
- negative symptoms: emotionally flat, no relationships, dull or disconnected speaking voice, apathy
- cognitive issues or disorganized thinking: struggle to complete tasks or thoughts, lack of insight
- abnormal behavior: laughing to self, self-neglect or unkempt appearance, wandering aimlessly
While people with schizophrenia described as disorganized don’t have hallucinations and delusions, they usually have several other symptoms in addition to negative symptoms and disorganized thinking.
Diagnosing schizophrenia can be difficult. There is no specific lab test or physical exam that can diagnose it.
To diagnose it, a doctor or healthcare professional must see symptoms for at least 6 months. Other options need to be ruled out, such as brain tumor, other mental illness, substance-induced psychosis, or other medical conditions.
A diagnosis of schizophrenia means that a person has at least two of the following symptoms consistently, along with reduced functioning:
- delusions
- hallucinations
- disorganized behavior
- catatonia
- negative symptoms
Symptoms that could be considered disorganized schizophrenia include:
- flat affect
- speech disturbances
- disorganized thinking
- inappropriate emotions
- facial expressions that don’t fit the situation
- difficulty with daily activities
Related conditions that may need to be ruled out before a diagnosis can be made include:
- schizoaffective disorder
- psychosis
- bipolar disorder
- schizophreniform disorder
- delusional disorder
- substance use
The exact cause of schizophrenia is unknown. Researchers think there are several contributing factors:
Researchers think there are several contributing factors:
- biological factors
- genetics
- environmental factors
- substance use
Many of these variables are thought to interact with each other in some way to cause schizophrenia. It is also thought that different factors cause different types of schizophrenia.
Risk factors and causes often overlap, since the exact cause of schizophrenia is unknown.
Having a risk factor for a disease or condition does not mean that an individual will definitively develop that condition, but they are at higher risk.
Risk factors for schizophrenia include:
- genetics
- substance use
- environment
There’s no one gene for schizophrenia, but there is thought to be an interaction between genetics and environment. Individuals with a close relative with schizophrenia, like a parent or sibling, are more than six times more likely to develop it as well.
Mind-altering drugs used during adolescence may increase the risk of developing schizophrenia. The younger an individual is and the more frequent the substance use occurs, the higher the risk.
The younger an individual is and the more frequent the substance use occurs, the higher the risk.
Exposure to viruses or malnutrition in utero, especially in the first and second trimesters, has been shown to increase the risk of later developing schizophrenia.
Treatment goals for schizophrenia include:
- targeting symptoms
- preventing relapse
- increasing adaptive functioning so the person can be in the community
This is usually done with both medications and other treatments.
Treatment options
Treatment options can include:
- psychotherapy
- cognitive-behavioral therapy (CBT)
- individual therapy
- group therapy
- pharmacological therapy
- antipsychotic medications are the first-line treatments
- assertive community treatment
- a multidisciplinary therapeutic team approach
- help reduce hospitalizations and homelessness
Depending on the specific symptoms, sometimes a combination of medications may be used. Medication and therapy are often used together since support systems help increase the likelihood of sticking to a medication routine. Job training and social skills training may also be part of psychotherapy or social supports.
Medication and therapy are often used together since support systems help increase the likelihood of sticking to a medication routine. Job training and social skills training may also be part of psychotherapy or social supports.
While there are no treatments specific to hebephrenic schizophrenia, CBT can help address disorganized thinking and behaviors and help provide support.
Schizophrenia is a chronic illness, and there is no cure. There are treatments, and sticking to a treatment plan is a good way to help manage these symptoms.
Above-average financial, social, and health concerns may be associated with a schizophrenia diagnosis due to:
- limited access to a nutrient-dense, balanced diet
- increased likelihood of being a smoker and having substance use disorder
- limited access to medical care
- increased risk of suicidal thoughts and attempts
- increased likelihood for treatment-related negative effects
- approximately half of all people with schizophrenia also having other mental health disorders
Combined, these factors can contribute to a higher risk of death for those diagnosed with this disorder.
Treatment with medications, behavioral therapy, and social support are important in helping to manage symptoms of schizophrenia. Treatment may change over time due to medication side effects or if symptoms change. An individual’s doctor can adjust or change medications if a specific drug causes side effects.
For people with hebephrenic schizophrenia, negative symptoms can be associated with higher risks because of the disturbance to behavior and emotions. This is why having a treatment plan and plenty of social supports is essential for management.
Schizophrenia is a complex, serious, and chronic mental health illness. While hebephrenic schizophrenia is no longer its own separate diagnosis through the DSM-5, the features of the illness still remain.
While there is no cure for schizophrenia, there are treatments available that may help manage symptoms and improve quality of life.
Treatment of hebephrenic schizophrenia in St. Petersburg
- Main
- Psychiatry
- Treatment of schizophrenia
- Hebephrenic schizophrenia
We diagnose and treat hebephrenic schizophrenia in adults and adolescents (girls from 14 years old, boys from 15-16 years old can be hospitalized). Due to the intensification of treatment, the selection of pharmacotherapy and its correction in a hospital takes no more than 10–15 days.
Treatment of hebephrenic schizophrenia in adolescents is carried out under the supervision of Aleksey Viktorovich Bocharov, a child psychiatrist, Doctor of Medical Sciences, a recognized expert in the field of pharmacotherapy of mental disorders, associate professor of the North-Western State Medical University. I.I. Mechnikov and SPbMAPO.
I.I. Mechnikov and SPbMAPO.
In addition to the selection of pharmacotherapy in safe effective dosages, our patients receive psychotherapeutic assistance. This approach to the treatment of hebephrenic schizophrenia makes it possible to quickly achieve deep remission and correct pathological personality traits that develop against the background of the disease.
After discharge, in order to prevent the development of side effects and correct pharmacotherapy, control examinations are prescribed: in the first month after discharge - 2 times; then - once with an interval of 2-3 months for at least a year. We recommend that you do not neglect the recommendations of the attending physician on taking the prescribed medications and attend follow-up examinations in a timely manner.
Doctor's consultation on the treatment of hebephrenic schizophrenia:
+7 (812) 407-18-00
Thank you for your trust!
- Post-discharge care
- Prevention of relapses
- Anonymous, without registration
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A.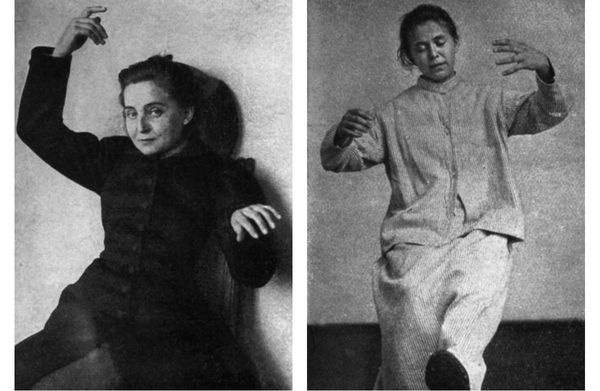 V. (Associate Professor, PhD) V. (Associate Professor, PhD) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | Is free | |
| Standard Chamber | 8 900 ₽ | |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | Is free | |
Signs of hebephrenic schizophrenia
Treatment of hebephrenic schizophrenia in our clinic
Pharmacotherapy is the main treatment for hebephrenic schizophrenia. For differential diagnosis, removal of an acute condition and rapid selection of drug therapy, hospitalization is necessary.
For differential diagnosis, removal of an acute condition and rapid selection of drug therapy, hospitalization is necessary.
Differential diagnostics
Differential diagnostics in our clinic includes an examination by doctors of narrow specializations (gastroenterologist, cardiologist, neuropsychiatrist), clinical-psychopathological, psychometric and psychological testing, advanced laboratory tests, EEG, MRI and (or) CT.
Differential testing is necessary to confirm the diagnosis and to rule out some somatic and viral diseases, as well as brain tumors, which can cause symptoms similar to hebephrenic schizophrenia.
Selection of pharmacotherapy
In our clinic, it is possible to quickly select pharmacotherapy through the use of infusion therapy and plasmapheresis (the so-called intensification of the treatment of hebephrenic schizophrenia). Correction of the prescribed treatment with access to psychotherapy requires about 2-3 weeks, after which the patient can be discharged.
Psychotherapy
All of our patients attend group psychotherapy sessions. Psychotherapy allows you to speed up the process of treatment of hebephrenic schizophrenia and begin to work out addictive attitudes that have formed during the course of the disease (for example, fears, phobias, pathological patterns of behavior).
Post discharge management
Sources
Nursing process/nursing of schizophrenic patients with hebephrenic schizophrenia — https://pubmed.ncbi.nlm.nih.gov
Modern antipsychotic pharmacotherapy of schizophrenia — https://www.rmj.ru
Hebephrenia - a viable psychopathological construct? — https://pubmed.ncbi.nlm.nih.gov
Update date: 08/26/2022
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
November 09
Tomorrow
November 10
Friday
November 11
Saturday
November 12
Sunday
November 13
Monday
November 14
Tuesday
November 15
Wednesday
November 16
Thursday
November 17
Friday
November 18
Saturday
November 19
Sunday
November 20
Monday
November 21
Tuesday
November 22
Wednesday
November 23
Thursday
November 24
Friday
November 25
Saturday
November 26
Sunday
November 27
Monday
November 28
Tuesday
November 29
Wednesday
November 30
Hebephrenic schizophrenia is treated on
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 41 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Work experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Work experience 33 years
Psychiatrist
Work experience 33 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb. department
department
Work experience 15 years
Psychiatrist
Work experience 15 years
Voronina Elvira
Vladimirovna
Psychiatrist
First category
Experience 27 years
Psychiatrist
Work experience 27 years
Efimova Evgenia
Vladimirovna
Psychiatrist
Second category
Work experience 19 years
Psychiatrist
Work experience 19 years
Gorobets Elena
Vasilievna
Psychiatrist
First category
Work experience 16 years
Psychiatrist
Work experience 16 years
Travnikova Oksana
Mikhailovna
Psychiatrist
First category
Work experience 21 years
Psychiatrist
Work experience 21 years
Kurochkina Nadezhda
Pavlovna
Psychiatrist
First category
Work experience 19 years
Psychiatrist
Work experience 19years
Suslennikova Elena
Viktorovna
Psychiatrist, psychotherapist
First category
Work experience 25 years
Psychiatrist, psychotherapist
Work experience 25 years
Chuban Olga
Ivanovna
Psychiatrist, psychotherapist
First category
Work experience 13 years
Psychiatrist, psychotherapist, psychologist
Work experience 13 years
Popov Andrey
Petrovich
Psychiatrist
Top category
Experience 35 years
Psychiatrist
Experience 35 years
Stetsiv Ludmila
Gennadievna
Psychiatrist, psychotherapist
PhD
Experience 31 years
Psychiatrist, psychotherapist
Work experience 31 years
Prokhorchev Konstantin
Sergeevich
Psychiatrist, psychotherapist
First category
Work experience 12 years
Psychiatrist, psychotherapist
Work experience 12 years
Gulevsky Roman
Aleksandrovich
Psychiatrist, narcologist
Head of Hospital
Work experience 25 years
Psychiatrist, narcologist
Work experience 25 years
Konoplin Dmitry
Alekseevich
Narcologist, psychiatrist
PhD
Work experience 24 years
Narcologist, psychiatrist
Work experience 24 years
Stavitskaya Svetlana
Yurievna
Psychiatrist
Top category
Work experience 24 years
Psychiatrist
Work experience 24 years
Pylskaya Anna
Nikolaevna
Psychiatrist
Second category
Work experience 7 years
Psychiatrist
Work experience 7 years
Trofimova Alexandra
Olegovna
Psychiatrist, child psychiatrist
First category
Experience 28 years
Psychiatrist, child psychiatrist
Experience 28 years
Zhelobetskaya Maria
Sergeevna
Psychiatrist, psychotherapist
Top category
Work experience 22 years
Psychiatrist, psychotherapist
Work experience 22 years
Endrzheevskaya Diana
Vadimovna
Psychiatrist, psychotherapist
Second category
Work experience 14 years
Psychiatrist, child psychiatrist, psychotherapist
Work experience 14 years
Ivanov Alexander
Nikolaevich
Psychiatrist, narcologist
Top category
Work experience 20 years
Psychiatrist, narcologist
Experience 20 years
Semenov Andrey
Nikolaevich
Psychiatrist, narcologist
Leading specialist of clinic
Work experience 24 years
Psychiatrist, narcologist, transfusiologist
Work experience 24 years
Leave a request for a call:
+7 (812) 407-18-00
FGBNU NTsPZ.
 ‹‹Schizophrenia in adolescents››
‹‹Schizophrenia in adolescents›› Feedback form
Question about the work of the siteQuestion to a specialistQuestion to the administration of the clinic
email address
Name
Message text
Epidemiological evidence suggests that it is likely that malignant juvenile schizophrenia has become less common in recent decades than it used to be. In the 40s G. V. Morozov (1950) found that catatonic-hebephrenic syndrome is the second most common after hypochondriacal syndrome in schizophrenia at the age of 16-18 years. In the 60s, M. Ya-Tsutsulkovskaya and T. A. Druzhinina (1966) found that malignant schizophrenia accounts for 28% of all cases of continuous forms.
Among all cases of schizophrenia, according to data published in 1972, the malignant form was 6.5% [Zharikov N. M., 1972], and in 1983 — 4.5% [Nadzharov R. A., Smulevich A . B., 1983].
In 63%, the malignant form begins at the age of 10-19 years [Zharikov N. M., 1972]; ages 15 to 19 are especially vulnerable. After 30 years, the debuts of this form are very rare; only 7% also fall on childhood. That is why this form is called malignant juvenile.
M., 1972]; ages 15 to 19 are especially vulnerable. After 30 years, the debuts of this form are very rare; only 7% also fall on childhood. That is why this form is called malignant juvenile.
Clinical picture and course. Malignant schizophrenia, which quickly leads to a defect, was called "schizocaric" [Mauz F., 1930]. R. A. Nadzharov (1965) identified malignant juvenile schizophrenia as a special form. Him (1972), 6 main features of this form were formulated:
-
Beginning in pre- and puberty.
-
The appearance of negative signs, in particular, a "drop in energy potential", emotional changes, etc., even before the process has manifested itself violently.
-
The speed of development of the disease.
-
"Syndromic incompleteness" at the time of manifestation, i.e., the psychotic picture includes symptoms from different syndromes.
-
resistance to therapy.

-
The severity of the final states, i.e. the formation of a pronounced defect.
From our point of view, among the listed signs, the appearance of negative signs before manifestation and resistance to therapy with antipsychotic neuroleptics have the greatest diagnostic value.
Three variants of malignant juvenile schizophrenia were also described, depending on the predominant symptoms: 1) hebephrenia, in which not only hebephrenic, but also catatonic disorders are expressed; 2) malignant paranoid form; 3) malignant simple form. With hebephrenia, the defect is formed in a year and a half from the moment of manifestation, with a malignant paranoid form - more slowly, in 2-4 years. There is a view on a simple form that it is “malignant schizophrenia that stopped at the initial stage” [Tsutsulkovskaya M. Ya., Druzhinina T. A., 1966].
Disability is established in 70% of patients, including 23% - disability of group I and 41% - of group II [Zharikov N. M., 1972]. Thus, about a quarter of patients need vigilant professional supervision and care and usually become permanent residents of psychiatric hospitals.
M., 1972]. Thus, about a quarter of patients need vigilant professional supervision and care and usually become permanent residents of psychiatric hospitals.
According to our data, hebephrenia is not only the most common among malignant forms, but also in other variants of malignant juvenile schizophrenia (paranoid, simple form), in most cases, hebephrenic symptoms are sufficiently represented. The appearance of these symptoms against the background of apatoabulic, catatonic, incoherent (acute polymorphic syndrome), paranoid and even psychopathic disorders serves as a prognostically unfavorable sign.
Against the background of the apatoabulic syndrome in these cases, one can see not only a drop in activity, initiative, growing isolation and isolation from the environment, emotional impoverishment with poor facial expressions and a voice devoid of emotional modulations, but also ridiculous senseless actions combined with them. For example, a 17-year-old defecated in a shoe and tied it to a chandelier in the room when the restroom was occupied for too long, he said. Closure, unwillingness to enter into a conversation is accompanied by obscene cynical abuse or shouting out certain phrases. The poverty of mimic reactions does not exclude ridiculous pretentious grimaces. The monotonous "wooden" voice is suddenly interrupted by unnatural pompous and pathetic exclamations.
Closure, unwillingness to enter into a conversation is accompanied by obscene cynical abuse or shouting out certain phrases. The poverty of mimic reactions does not exclude ridiculous pretentious grimaces. The monotonous "wooden" voice is suddenly interrupted by unnatural pompous and pathetic exclamations.
Against the background of paranoid disorders, hebephrenic symptoms are manifested primarily by a sharp discrepancy between facial expressions, intonation of the voice, manner of behaving, and the content of delusional statements. Ridiculously giggling and grimacing, the teenager declares that he “heard the guys agree to cut off his penis at night.” Another teenager, with a contemptuous expression on his face and a majestically proud look, declares that intelligence from one of the foreign powers is poisoning him, putting poison in his food, from which he feels a “chemical smell and taste”, which, however, does not interfere with him. to devour this food with greed.
According to M. Ya. Tsutsulkovskaya et al. (1982), in 57% of premorbid patients with malignant juvenile schizophrenia, there is a personality type called "exemplary" [Pekunova L. G., 1974]. Even E. Kraepelin (1912) noted that their parents spoke of those who fell ill with hebephrenia as “exemplary children”. From here, apparently, the name was taken for the premorbid type of adolescents and young men. However, it is unlikely that this type of teenagers deserves such a name. They were "home children", obedient and did not cause any particular disturbance. Becoming teenagers, they were always distinguished by “correct” behavior, complaisance. However, their interests were limited, they were deprived of creative activity and initiative. From our point of view, in such cases it is more correct to speak of a “conformal type of character accentuation” [Lichko A.E., 1977, 1983]. Their "exemplary" is the result of passive assimilation of the mode of behavior in the immediate familiar environment, in their own family, above all.
Ya. Tsutsulkovskaya et al. (1982), in 57% of premorbid patients with malignant juvenile schizophrenia, there is a personality type called "exemplary" [Pekunova L. G., 1974]. Even E. Kraepelin (1912) noted that their parents spoke of those who fell ill with hebephrenia as “exemplary children”. From here, apparently, the name was taken for the premorbid type of adolescents and young men. However, it is unlikely that this type of teenagers deserves such a name. They were "home children", obedient and did not cause any particular disturbance. Becoming teenagers, they were always distinguished by “correct” behavior, complaisance. However, their interests were limited, they were deprived of creative activity and initiative. From our point of view, in such cases it is more correct to speak of a “conformal type of character accentuation” [Lichko A.E., 1977, 1983]. Their "exemplary" is the result of passive assimilation of the mode of behavior in the immediate familiar environment, in their own family, above all.