What is binge and purge
Bulimia Nervosa | Johns Hopkins Medicine
What is bulimia?
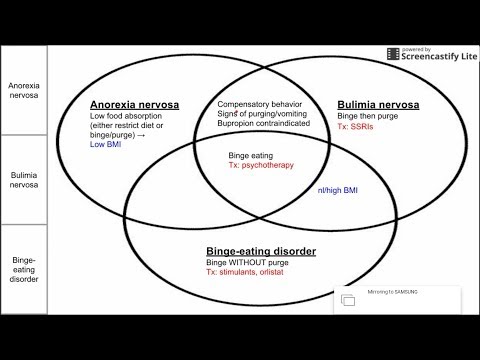
Bulimia is an eating disorder. It is characterized by uncontrolled episodes of overeating, called bingeing. This is followed by purging with methods such as vomiting or misuse of laxatives. Bingeing is eating much larger amounts of food than you would normally eat in a short period of time, usually less than 2 hours. You may feel like you can’t stop or control these episodes of binge eating.
The binge-purge cycles can happen from many times a day to several times a week.
Often, people with bulimia keep a normal or above normal body weight. This lets them hide their problem for years. Many people with bulimia don’t seek help until they reach the ages of 30 or 50. By this time, their eating behavior is deeply ingrained and harder to change.
There are 2 ways people with bulimia restrict calories:
- Purging type. The person engages in self-induced vomiting or misuse of laxatives, diuretics, or enemas, or other medicines that clear the intestines.
- Nonpurging type. The person uses other behaviors, such as fasting or excessive exercise, rather than purging behaviors.
Who is at risk for bulimia?
Bulimia most often affects females and starts during the teenage years. But, it can also affect males. People with bulimia are more likely to come from families with a history of eating disorders, physical illness, and other mental health problems. Other illnesses, such as substance abuse, anxiety disorders, and mood disorders are common in people with bulimia.
What causes bulimia?
The cause of bulimia is not known. Society and cultural ideals that assign value based on body weight and shape play a role. There is also a genetic link as eating disorders tend to run in families.
What are the symptoms of bulimia?
These are the most common symptoms of bulimia:
- Usually a normal or above average body weight
- Recurrent episodes of binge eating and fear of not being able to stop eating
- Self-induced vomiting (usually secretive)
- Excessive exercise
- Excessive fasting
- Peculiar eating habits or rituals
- Inappropriate use of laxatives or diuretics
- Irregular or absence of menstruation
- Anxiety
- Discouraged feelings related to dissatisfaction with themselves and the way their body looks
- Depression
- Preoccupation with food, weight, and body shape
- Throat is always inflamed or sore
- Tiredness and decreased energy
- Dental problems due to erosion of enamel from vomiting
Most people with eating disorders also share certain traits including:
- Low self-esteem
- Feelings of helplessness
- Fear of getting fat
- Intense unhappiness with their body shape and size
If you have bulimia, you may binge to reduce stress and ease anxiety.
- With binge eating comes guilt, disgust, and depression.
- Purging brings only short-term relief.
- You may be impulsive and more likely to take part in risky behaviors, such as alcohol and drug abuse.
The symptoms of bulimia may look like other medical problems or mental health conditions. Always talk with a healthcare provider for a diagnosis.
How is bulimia diagnosed?
You likely keep your binging and purging secret. This is so family, friends, and healthcare providers won’t know about it. If you seek help from a healthcare professional for bulimia, he or she will want to gather a detailed history of your behaviors from you, your family, parents, and others. Sometimes, psychological testing is done.
Blood tests may be done to check overall health and nutritional status.
Early treatment can often prevent future problems. Bulimia, and the malnutrition that results, can affect nearly every organ system in the body. Bulimia can be deadly.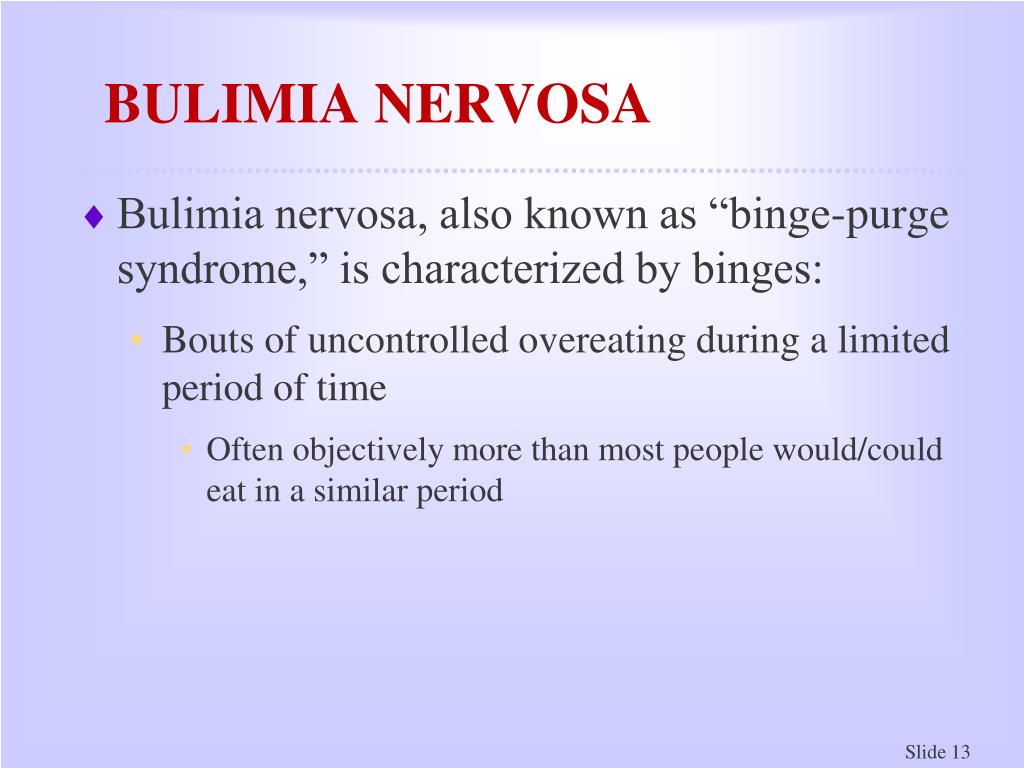 If you suspect bulimia, talk with a healthcare provider for more information.
If you suspect bulimia, talk with a healthcare provider for more information.
How is bulimia treated?
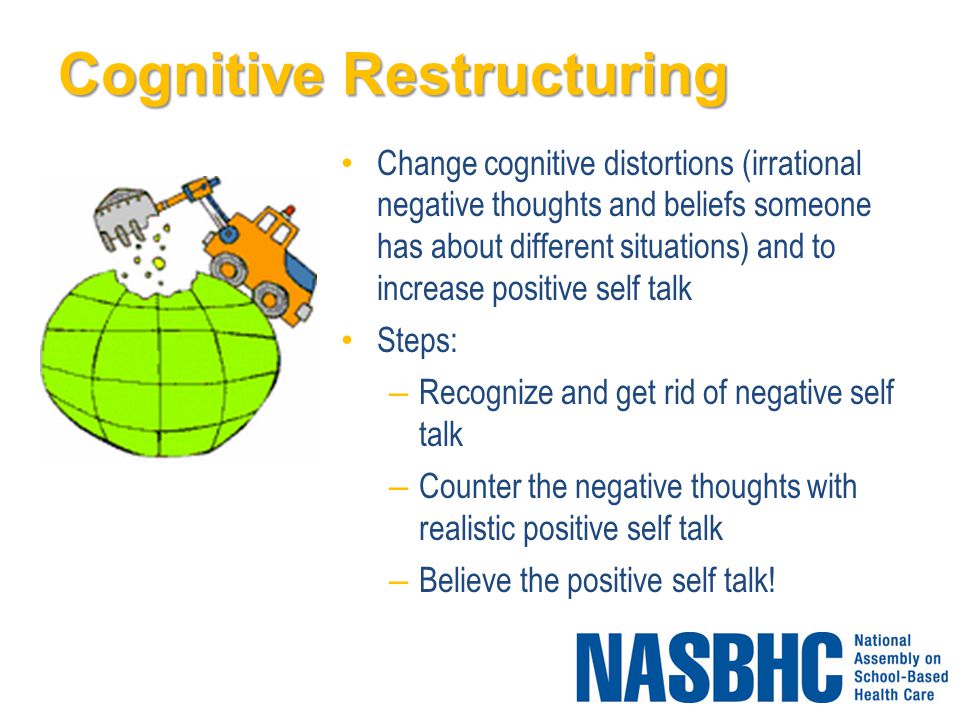
Bulimia is usually treated with both individual therapy and family therapy. The focus is on changing your behavior and correcting any nutritional problems.
Therapy looks at the link between your thoughts, feelings, and behaviors. The therapist will explore the patterns of thinking that lead to self –destructive actions and help change that thinking.
Medicine (usually anti-depressants or anti-anxiety medicines) may help if you are also anxious or depressed.
A healthcare provider and a nutritionist will be part of your care.
Your family can play a vital supportive role in any treatment process.
In some cases, a hospital stay may be needed to treat electrolyte problems.
What are the complications of bulimia?
Complications of bulimia include:
- Stomach rupture
- Heart problems due to loss of vital minerals and electrolytes, such as potassium and sodium
- Dental problems, the acid in vomit wears down the outer layer of the teeth
- Inflamed esophagus
- Swollen glands near the cheeks
- Irregular menstrual periods
- Kidney problems
- Diminished sex drive
- Addictions, substance abuse, and/or compulsive behavior
- Depression, anxiety, obsessive-compulsive disorder, and other mental health problems
- Suicidal behavior
Living with bulimia
It’s important to follow your healthcare provider’s advice for treating your bulimia. Support is necessary. Try to involve your family and friends in your care.
Support is necessary. Try to involve your family and friends in your care.
When should I call my healthcare provider?
If your symptoms get worse or you have new symptoms, tell your healthcare provider.
Key points about bulimia
- Bulimia is an eating disorder. It is characterized by uncontrolled episodes of overeating (called bingeing). This is followed by purging by self-induced vomiting, misuse of laxatives, and other methods.
- Bulimia typically affects females and starts during the teenage years. But, it can also affect males. Society and cultural ideals that assign value based on body weight and shape play a role in the cause. So does genetics.
- People with bulimia keep it very private and hidden.
- Bulimia is usually treated with a combination of individual therapy and family therapy. The focus is on changing behavior and correcting any nutritional deficits.
- Complications may include heart and kidney problems, inflamed esophagus, dental problems, and others.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.

- Know how you can contact your provider if you have questions.
Bulimia: All About Bingeing and Purging
Bulimia is an eating disorder characterized by its cycle of binge eating and purging. But what does it mean to binge and purge?
Bulimia nervosa is a type of eating disorder where people typically binge eat and then purge.
Someone living with bulimia may feel a lack of control when eating large amounts of food in a short time. Or they may feel powerless over life’s stressors, seeing their eating habits and weight as the only things they can control. To compensate for overeating, they may purge, like vomiting or using laxatives.
To be classified as bulimia by a doctor, someone must binge eat and purge — or use other ways to prevent or control their weight — once a week for at least 3 months.
Some people living with bulimia compensate for binge eating with excessive exercise or fasting, rather than purging. Or they mix purging and non-purging behaviors.
Bulimia is associated with an intense dissatisfaction and obsession with body weight and shape. You may feel shame or feel isolated.
Binge eating and purging behaviors can have health side effects that not everyone knows of. Bulimia can also be a heavy condition to deal with on your own.
Having an eating disorder is not your fault. You can find support and treatment options that can help you manage this condition.
Binge eating is when you eat a large amount of food in a short period of time while feeling out of control.
It’s not the same as having a second helping of Thanksgiving dinner. Many people have had the experience of indulging in extra servings during a special meal. That is not binge eating.
Binge eating in bulimia happens regularly, on ordinary days as well as on special occasions.
According to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) — the guide mental health professionals use to diagnose conditions like eating disorders — bulimia is characterized by:
- the binge eating episode occurs within a 2-hour time frame
- the amount of food a person eats within that 2-hour period is more than someone else in the same situation would usually eat in 2 hours
- the person binge eating feels out of control, like they cannot stop eating or control how much they eat
You may not even be hungry when binge eating. Instead, bingeing can be used as a coping mechanism for stress or upsetting emotions. Eating helps take your mind off what’s bothering you.
Instead, bingeing can be used as a coping mechanism for stress or upsetting emotions. Eating helps take your mind off what’s bothering you.
People who binge eat often do so in secret, sometimes hiding food.
Because binge eating is driven by emotions rather than hunger, you might binge eat even if you feel full. You may even eat to the point where you feel uncomfortable or ill.
When you binge eat, you might be driven to continue eating by thoughts like, “I’ve already blown my diet, I might as well go all-in on bingeing and start dieting again tomorrow.”
Side effects and risks
When someone binge eats, they typically consume more calories than they need in a short amount of time. It overwhelms the body with calories which affect blood sugar levels, digestion, energy, and more.
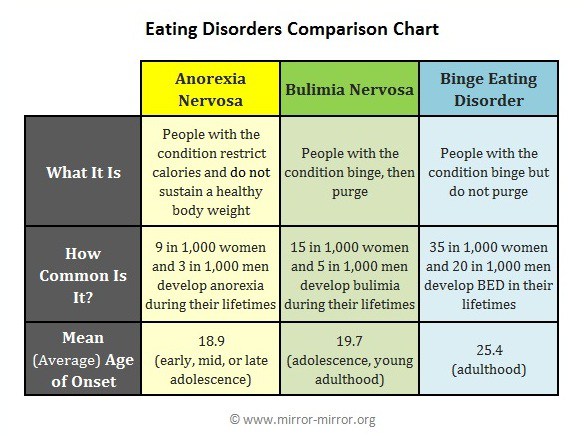
Regular binge eating is usually connected with two eating disorders: bulimia and binge eating disorder (BED). The main difference is that people with BED don’t purge like people with bulimia do.
People with bulimia often report feelings of shame and guilt after they binge eat. This drives them to purge — to “undo” their overeating.
Side effects of binge eating include:
- bloating, abdominal cramping, and nausea
- acid reflux or heartburn
- diarrhea
- lethargy
- gallstones
- resistance to insulin or type 2 diabetes
Binge eating can sometimes cause medical emergencies. According to the National Eating Disorders Association (NEDA), eating too much at once can cause the stomach to rupture. Eating too quickly can also raise your chances of choking.
Purging means getting rid of something unwanted. For a person living with bulimia, purging is how someone controls or “makes up for” bingeing on food.
Purging behaviors include:
- making yourself vomit
- misusing laxatives, diuretics, or enemas
Some people use non-purging behaviors to compensate for binge eating, including:
- fasting
- excessive exercise
Some people use only one purging or non-purging method, while others use several.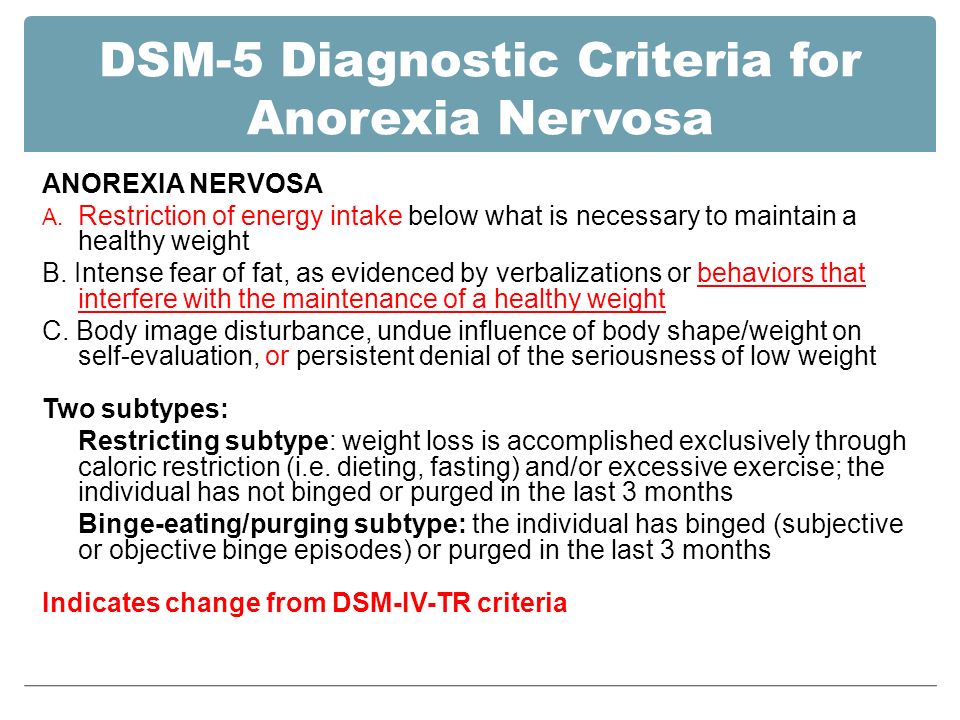
In a 2018 study on adolescents with bulimia, 41.3% reported purging while the rest (58.7%) reported non-purging behaviors.
You might feel relief when you purge, believing you’re getting rid of the excess calories you ate while bingeing. When you purge, you “fix” the issue.
Many people living with bulimia vow that this purge is the last one, until the next binge eating episode starts the cycle all over again.
The DSM-5 uses the frequency of purging behaviors to determine the severity level of bulimia:
- Mild: 1 to 3 times per week
- Moderate: 4 to 7 times per week
- Severe: 8 to 13 times per week
- Extreme: 14 or more times per week
Sometimes healthcare professionals increase the severity rating based on how much the condition interferes with your life.
Side effects and risks
Purging behaviors have many side effects that can be dangerous. If left untreated, eating disorders like bulimia nervosa can be life threatening.
If left untreated, eating disorders like bulimia nervosa can be life threatening.
When you vomit, the contents of your stomach are forcefully propelled back up through your esophagus. Regular vomiting can cause problems, such as:
- tooth decay
- a hoarse voice and swollen throat or face
- oral bleeding
- chronic cough
- digestive issues like acid reflux, diarrhea, and stomach pain
- esophageal tears
- low blood pressure and heart rate
- an irregular heart rhythm
- difficulty regulating body temperature
- kidney failure
- pregnancy complications
Purging can also disrupt hormone levels. A small 2013 study involving 74 females revealed hormonal changes in the 31 participants who regularly purged.
You may also develop Russell’s sign — scarring on your hands from scraping them against your teeth during induced vomiting.
The amount of dental erosion you experience can depend on your diet. For example, if your diet contains a lot of sweetened or acidic foods, purging will likely affect your teeth more.
Rare but possible complications of regular, forced vomiting include hiatal hernias and gastroesophageal intussusception, a condition where your stomach slides up into your esophagus.
Vomiting isn’t the only harmful purging method, though. If you regularly use laxatives or diuretics, you can become dependent on them and be unable to have a bowel movement naturally. Overuse of diuretics can also cause kidney damage.
Purging, fasting, and excessive exercising can result in nutritional imbalances and dehydration, which can contribute to other health issues, such as:
- fatigue
- electrolyte imbalances
- seizures
- drying and thinning hair
- brittle nails
- reproductive complications
- muscle weakness
Compulsively exercising can also lead to more than nutritional imbalances and dehydration.
Pushing yourself physically to burn extra calories can also cause reduced bone density, along with chronic joint and bone pain. You may also have chronic muscle soreness and regular overuse injuries.
You may also have chronic muscle soreness and regular overuse injuries.
Over-exercising can even cause you to have upper respiratory tract infections more often, and more illnesses in general.
While some side effects of purging are serious, remember that people do recover from bulimia — and so can you.
An eating disorder is not a choice, and it’s not your fault. Many people are able to move past eating disorders to live without the guilt and shame the comes along with them.
Bulimia is a serious mental health condition. About 94.5% of people living with bulimia also have at least one other mental health condition, like depression or anxiety.
Both binge eating and purging can have negative effects on your health. To prevent unwanted health effects, you can find support through a doctor or therapist and learn more about treatment options.
If you need help now and don’t know where to start, you can call, text, or chat online with NEDA.
Binge drinking - what is it, classification, treatment and prognosis
Article reviewed by an expert:
MAKE AN APPOINTMENT
Binge - drinking alcohol for a day or more with the development of severe alcohol intoxication. Develops with alcoholism. The average duration of binge is 3-10 days, binge drinking lasting up to a month or more is sometimes observed.
Develops with alcoholism. The average duration of binge is 3-10 days, binge drinking lasting up to a month or more is sometimes observed.
- Binge drinking - what is it?
- Classification and types of hard drinking
- Short drinking binges
- Long binges
- Treatment of binge drinking
- Prognosis for drinking binges
Alcohol intake is accompanied by denial of the problem and the development of depression. Refusal to work, decrease or loss of appetite, neglect of hygiene rules, etc. are possible. The reason for stopping alcohol consumption in the later stages of alcoholism is an exacerbation of somatic pathology and general fatigue of the body. With abrupt withdrawal, psychosis often develops. nine0003
Drinking alcohol - what is it?
Binge is drinking large amounts of alcohol for a day or more. Single short binges can occur in people who do not suffer from alcoholism or are in the prodrome stage. The reason may be the holidays or an attempt to relieve tension resulting from severe or prolonged stress. However, in most cases, binges are observed in alcoholics. As alcoholism deepens, there is an increase in the duration and severity of binges, the likelihood of developing alcoholic delirium and exacerbation of chronic diseases increases. nine0003
The reason may be the holidays or an attempt to relieve tension resulting from severe or prolonged stress. However, in most cases, binges are observed in alcoholics. As alcoholism deepens, there is an increase in the duration and severity of binges, the likelihood of developing alcoholic delirium and exacerbation of chronic diseases increases. nine0003
Drinking is one of the most characteristic signs of alcoholism. They are part of a vicious circle from which it is very difficult to get out without the help of a drug specialist. These conditions are accompanied by severe intoxication of the body. They often cause absenteeism, subsequent dismissal and loss of social status, followed by accelerating degradation. Treatment is carried out by specialists in the field of narcology. Home care, outpatient or inpatient therapy is available. nine0003
Classification, types and stages of hard drinking
In domestic medical literature, the concepts of "false binge" (pseudo-binge) and "true binge" are often encountered. What is a pseudo binge? Pseudo-drinking refers to cases where the duration of alcohol intake does not exceed 7-10 days. The patient usually stops drinking alcohol due to external circumstances (the need to go to work or solve accumulated domestic problems, obligations towards family members, etc.). In addition, the cause of getting out of a false binge can be fatigue, not reaching the degree of exhaustion. nine0003
What is a pseudo binge? Pseudo-drinking refers to cases where the duration of alcohol intake does not exceed 7-10 days. The patient usually stops drinking alcohol due to external circumstances (the need to go to work or solve accumulated domestic problems, obligations towards family members, etc.). In addition, the cause of getting out of a false binge can be fatigue, not reaching the degree of exhaustion. nine0003
What is the difference between a true hard drinking and a false one?
A true binge usually lasts at least 2 weeks, sometimes its duration is 1.2 and sometimes 3 months. The patient stops drinking alcohol due to severe poisoning of the body (a situation where a person is physically unable to drink anymore). Other reasons, including the need to go to work, take care of everyday life, fulfill any obligations in relation to others, and even observe elementary hygiene standards during this period become insignificant. All the interests of an alcoholic center around drinking alcohol. nine0003
nine0003
Despite some differences between false and true binges, there is currently a point of view according to which such a division should be recognized as unlawful. Firstly, polar variants of true and false binges are quite rare. Usually, the same patient has a mixture of two types of hard drinking with a predominance of one variant. Secondly, both types of binges are caused by the same mechanism - they arise due to an increased release of catecholamines, the effect of which the patient neutralizes by drinking alcohol. nine0003
From this position, all binges, regardless of their duration, are considered as one and the same pathological condition. The reason for the short duration of binges in stage II of alcoholism is the preservation of natural protective and compensatory mechanisms. As alcoholism progresses, these mechanisms gradually weaken, and the duration of binges increases. A gradual change in the clinical picture is also associated with a decrease in tolerance to alcohol, progressive mental degradation and a change in the patient's personality. nine0003
nine0003
Both short-term and long-term binges are characterized by an irresistible craving for alcohol. When the first signs of sobering appear, the patient feels the need not just to "drink a little", but to take an intoxicating amount of alcohol. Craving for alcohol uncontrollable, uncontrollable. Episodes of relative sobriety are so short that this period of time is only enough to find a new portion of alcohol. As a result, the withdrawal syndrome does not have time to develop, withdrawal symptoms practically do not bother the patient until the alcohol is stopped. nine0003
Short drinking binges
Short-term binges can occur episodically even in the period of the prodrome and at stage I of alcoholism. In stage II, they become regular. Their duration usually does not exceed 2-3 days, drinking bouts lasting 5-7 days are less common. As a rule, the beginning of alcohol consumption (at least formally) is associated with some kind of event, since the patient still needs to justify his drinking. The reason can be a holiday, a meeting of friends, a vacation trip, stress at work or in the family, etc. nine0003
The reason can be a holiday, a meeting of friends, a vacation trip, stress at work or in the family, etc. nine0003
Weekend drinking is a common variant. On Friday, the patient drinks, motivating alcohol intake by the need to relax after a hard week at work. On Saturday and Sunday, he tries to hangover to get rid of the withdrawal symptoms, but an irresistible craving for alcohol pushes him to drink a large dose of alcohol. On Sunday evening the patient is forced to stop drinking, on Monday he suffers from withdrawal.
This can go on for years, while patients do not consider themselves alcoholics, because they manage to keep their jobs and their usual social status. They consider the ability to stop drinking before starting work as confirmation of the ability to control alcohol intake. Meanwhile, alcoholism is gradually progressing. After some time, the duration of binges increases, the patient begins to drink alcohol not only on weekends, but also on weekdays. Sooner or later, there comes a moment when, due to a long binge, he simply does not go to work. nine0003
Sooner or later, there comes a moment when, due to a long binge, he simply does not go to work. nine0003
A short-term binge can be quite easily interrupted. In addition to going to work, a scandal with the wife, complaints from neighbors, lack of money for alcohol, a visit from the district police officer, etc. can become the reason for stopping alcohol intake. For the patient, such an intervention looks like an attempt to “spoil the holiday”. Alcohol withdrawal is usually accompanied by a sharp deterioration in mood. The patient splashes out his discontent on others (usually on family members), but cools down quickly enough.
Short-term binges alternate with episodes of a single use of alcohol with a hangover or without a hangover (depending on external conditions). Withdrawal syndrome is expressed moderately, to eliminate the main manifestations, it is enough for patients to get drunk with a small amount of alcohol. The amount of alcohol drunk during binges and one-day excesses can vary significantly. The duration of periods of sobriety is determined by the patient's living conditions: the amount of cash, work schedule, etc. nine0003
The duration of periods of sobriety is determined by the patient's living conditions: the amount of cash, work schedule, etc. nine0003
Long binges
At stage II of alcoholism, tolerance to alcohol increases and eventually reaches a "plateau". At this stage, the amount of alcohol gradually increases, binges become longer and last 1-3 weeks. There is a decrease in the duration of "sober periods", the frequency of hard drinking becomes more pronounced. Each intake of alcoholic beverages turns into a binge, solitary excesses disappear and the usual drunkenness with a hangover the next morning. During the binge, the patient consumes alcohol relatively evenly. nine0003
The amount drunk per day usually ranges from 0.8-1.5 liters of vodka, in some cases, patients drink up to 2-3 liters daily. The craving for alcohol is so strong that it forces the patient to wake up at night to take a new dose. The quality of alcohol becomes unimportant, patients are ready to use "everything that burns", including cologne, technical liquids, any alcohol tinctures for medical (including external) use.
Everything else becomes insignificant. Patients stop going to work, do not leave the house as long as there is alcohol in it, do not wash, do not shave, can sleep without undressing, etc. They not only spend on alcohol the money set aside for food, rent or the needs of children , but also sell things and jewelry in order to purchase another portion of alcohol. Patients no longer need to look for reasons to justify their own actions - the need for alcohol becomes so significant that other needs, in comparison with it, seem unimportant or even far-fetched. nine0003
If at the stage of short-term binges the patients drank “for pleasure”, now physical dependence comes to the fore. Patients no longer view drinking as a holiday. On the contrary, they can be oppressed, depressed and inhibited. The withdrawal symptoms are becoming more and more vivid and are not completely eliminated even when taking a large amount of alcohol. Patients drink not to achieve a state of euphoria, but to relieve physical and mental suffering. nine0003
nine0003
Intoxication of the body with alcohol decay products gradually increases. The amount of alcohol consumed decreases. Sleep disorders progress. Initially, sleep becomes superficial, unstable, the patient manages to fall asleep only after drinking a large dose of alcohol. By the end of the binge, insomnia develops. Even in a state of intoxication, the patient only briefly "falls" into a short sleep, accompanied by nightmares. At the time of falling asleep and waking up, hallucinations occur in the form of fragmentary phrases, car horns, bells and other noises. nine0003
Vestibular disturbances are possible in the form of a feeling of falling or falling. There are affective disorders. The patient feels anxiety, anxiety and fear, suffers from guilt and remorse. Alcoholic depression often develops. Mental disorders are combined with progressive motor and somatovegetative disorders. There is nausea, lack of appetite, vomiting and stool disorders.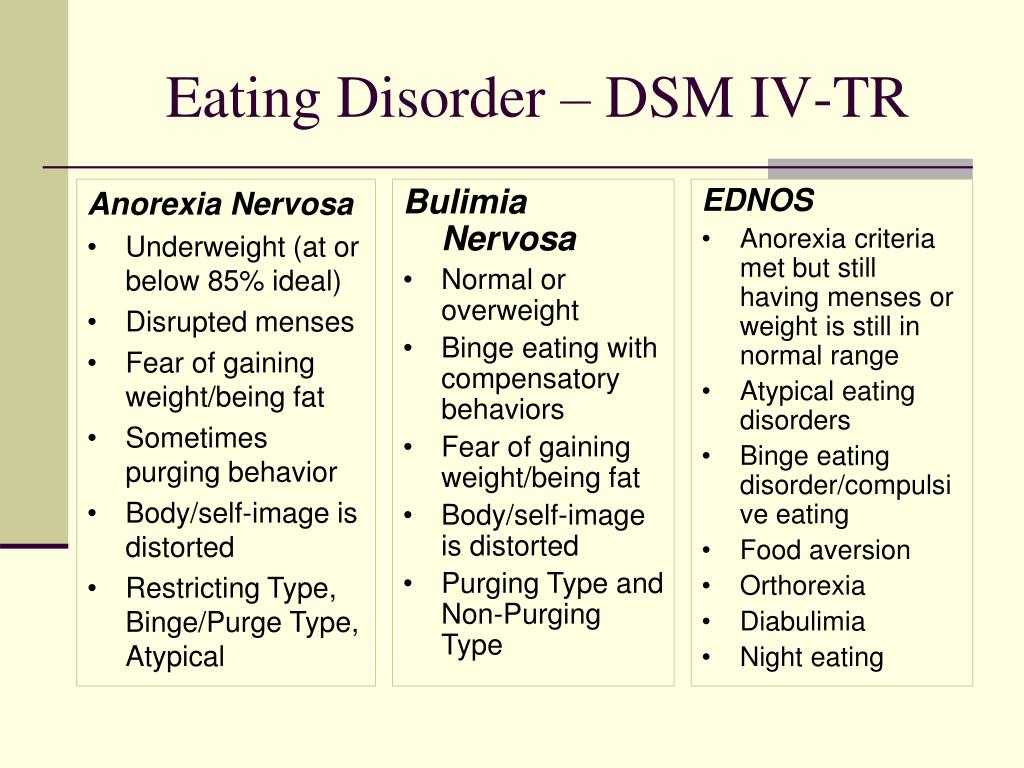 There may be pain in the epigastric region and right hypochondrium, as well as girdle pain in the upper abdomen. nine0003
There may be pain in the epigastric region and right hypochondrium, as well as girdle pain in the upper abdomen. nine0003
Movement disorders are revealed: gait instability, static ataxia, trembling of the limbs, eyelids and tongue. There are violations of the cardiovascular system: increased heart rate and unstable blood pressure with a tendency to increase. Some patients experience arrhythmia and pain in the heart. Due to a decrease in alcohol tolerance, the patient takes alcohol in small quantities and gradually comes out of the binge through "nurturing". Asthenia persists for several days, the patient may experience an aversion to alcohol. With a sharp cancellation, the likelihood of developing alcoholic delirium increases. nine0003
Gradually, the disgust fades away, the craving for alcohol becomes more and more unbearable. The patient tries to abstain from drinking, because he knows that even a small amount of alcohol will be the beginning of a new binge. After a while, a breakdown occurs, and the cycle repeats. The duration of the inter-binge period ranges from several days to several months. Neither the patient nor the people around him can accurately predict the moment of the next breakdown. One can only take into account the circumstances that will surely push the patient to take alcohol, and if possible try to prevent them, but this is a temporary measure that does not solve the problem of alcoholism. nine0003
After a while, a breakdown occurs, and the cycle repeats. The duration of the inter-binge period ranges from several days to several months. Neither the patient nor the people around him can accurately predict the moment of the next breakdown. One can only take into account the circumstances that will surely push the patient to take alcohol, and if possible try to prevent them, but this is a temporary measure that does not solve the problem of alcoholism. nine0003
Sometimes patients during the entire binge retain a sufficiently high resistance to alcohol. The manifestations of the withdrawal syndrome do not increase. Patients drink alcohol several times a day and at the same time retain their ability to work. This form of binges resembles constant drunkenness, but differs from it in a certain frequency. After a few months, somatovegetative disorders appear. Progressive asthenia is noted, depression occurs. As a result, patients stop drinking alcohol for a while. nine0003
Treatment for binge drinking
Depending on the patient's condition, both withdrawal from binge at home and inpatient treatment are possible. Withdrawal from binge at home is allowed in the II stage of alcoholism, short-term binge and the absence of signs of gross violations of the activity of internal organs. With prolonged continuous use of alcohol, severe withdrawal syndrome and severe somatovegetative disorders, hospitalization in a drug treatment hospital is indicated. There are several treatment regimens: standard cleansing of the body, double cleansing of the body, deep cleansing of the body and quick sobering up. The choice of treatment regimen is carried out by a narcologist. nine0003
Withdrawal from binge at home is allowed in the II stage of alcoholism, short-term binge and the absence of signs of gross violations of the activity of internal organs. With prolonged continuous use of alcohol, severe withdrawal syndrome and severe somatovegetative disorders, hospitalization in a drug treatment hospital is indicated. There are several treatment regimens: standard cleansing of the body, double cleansing of the body, deep cleansing of the body and quick sobering up. The choice of treatment regimen is carried out by a narcologist. nine0003
To restore water-salt metabolism and acid-base balance, saline solutions are injected intravenously. Glucose solution is used to improve brain nutrition. Enterosorbents are administered orally - drugs that combine with alcohol in the intestine and prevent the absorption of ethanol. They use vitamins B1 and B6, ascorbic acid, nootropics, sleeping pills and sedatives. If necessary, treatment of somatic pathology is carried out.
Prognosis for binge drinking
The prognosis depends on the duration and severity of binge drinking, the stage of alcoholism, the mental and physical condition of the patient. Exacerbations of chronic somatic diseases are possible. During the period of cessation of alcohol consumption, the likelihood of developing strokes and heart attacks increases. Often there are alcoholic depression. One of the most serious complications is alcohol delirium, which can lead to death, harm to yourself or others.
Treating binge is an emergency measure. It is necessary to fight the root cause of the problem - alcoholism, otherwise the binges will be aggravated, causing more and more harm to the patient's body. There are many methods for treating alcoholism: installation of a coding implant, drug treatment with provocation, Dovzhenko coding, etc. After eliminating the withdrawal symptoms, you need to contact a narcologist who will select a therapy regimen that is best suited for a particular patient. nine0003
nine0003
Alcoholism. Binge drinking, detoxification
Binge drinking is a condition accompanied by irresistible craving for alcohol and inability to stop its consumption, which is typical for the second stage of alcoholism.
A drunken state is a natural continuation of the formed hangover syndrome. In a binge, alcohol intoxication practically does not deliver a man of habitual pleasure. A sick organism makes a person drink another dose to relieve suffering for a short time. nine0003
Drinking binges can last from several days to several weeks and even months. To stop the abuse of alcohol does not force a person to willpower, but severe poisoning of the body caused by alcoholic poison acetaldehyde. A person can get out of a binge both independently and by resorting to doctor's help. However, with the cessation of the drunken state, the disease does not end, but goes into a latent form. If you do not start anti-relapse complex treatment (drugs + psychotherapy), then binges will resume, because. in the body with a certain frequency, the biological mechanism of exacerbation of alcoholism will begin to work. nine0003
in the body with a certain frequency, the biological mechanism of exacerbation of alcoholism will begin to work. nine0003
It is necessary to get out of binge not only physiologically under the influence of the negative factor of intoxication, but also in your mind, when the binge state passes and an illusory feeling of complete well-being appears. If the image of alcohol as a universal means of salvation and obtaining the highest pleasure remains to dominate in the mind, then the next binge is only a matter of time, since the physiology and biochemistry of the drinking person is constantly ready to adapt to the fulfillment of his secret desire. nine0003
Relief (interruption) of binges can only begin at the end drunken state. An experienced narcologist will not go, for example, to put dropper on the second day of binge, if this patient usually has it lasts a week or more. In this case, the dropper will only temporarily remove alcohol poisoning, not complete the binge. And the "purified" patient with renewed vigor will run "add". You can successfully stop the binge only at the end of the binge states when the body of the drinker is "satiated" with alcohol, and the patient himself is exhausted by the disease and asks for help. nine0003
And the "purified" patient with renewed vigor will run "add". You can successfully stop the binge only at the end of the binge states when the body of the drinker is "satiated" with alcohol, and the patient himself is exhausted by the disease and asks for help. nine0003
Cleansing the body of toxins. There are many ways to derive alcohol poisons from the body: hemosorption (method of removing toxins from the body by passing blood through special filters), plasmapheresis (obtaining plasma blood with the return of formed elements to the bloodstream), the introduction intravenous drip of various medicinal solutions. However, the first two should be used only in case of extremely severe alcohol poisoning, dangerous for the patient's life. In all other cases, the body only needs help to cope with elimination of alcoholic toxins in gentle ways. Many are mistaken that having undergone such methods of cleansing the body of alcoholic poisons, in fact the alcohol problem will disappear by itself.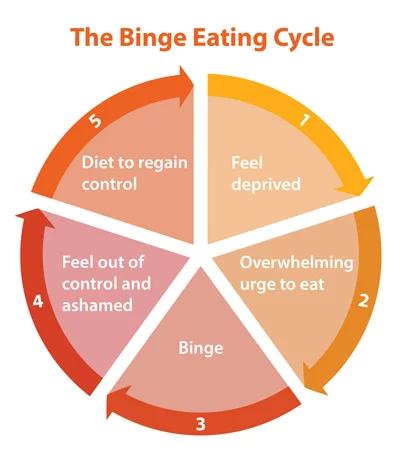 Detox is just the very first step. on the road to recovery. After all, a drunken state is not a banal alcohol poisoning, but an attack of an alcoholic recurrent disease. nine0003
Detox is just the very first step. on the road to recovery. After all, a drunken state is not a banal alcohol poisoning, but an attack of an alcoholic recurrent disease. nine0003
If a person acquired alcoholic hepatitis as a result of alcohol abuse (inflammation of the liver), then the temporary removal of toxins will not lead to serious recovery, since the liver is the main factory for processing poisons in the body continues to hurt. In outpatient (home) conditions for cleansing the body and restoration of the liver, special sorbents are successfully used, hepatoprotectors, amino acids and vitamins.
The body has the ability to self-cleanse and restore, you only need help him in his time of need. For example, the formed elements of the blood (erythrocytes) are updated naturally by the end of 3-4 months, and the metabolism returns to a relative norm by the end of the 6th month after the complete rejection of alcohol. The nervous system and the psychological state of a person recover the longest, which requires long-term observation by a psychotherapist. nine0003
nine0003
Alcohol dependence is a complex disease that affects the entire body in in general. Therefore treatment should be complex and phased .
Magalif Alexey Alexandrovich.
- Modern treatment for alcoholism
- Alcoholism in the family
- Stress and alcohol: how not to break loose?
- Alcohol and addiction
- Don't drown your sorrows
- Everything starts with a buffet
- Alcoholic aggression, or why do women grow mustaches from beer?
- Drunkards on Fridays
- Alcohol myths
- Where do bad habits come from?
- Female alcoholism
- You can't feed a snake with a pill
- Delirium tremens - alcoholic psychosis
- Alcoholism.
Learn more