Natural treatments for narcolepsy
Natural Tips to Stay Alert With Narcolepsy
Medically Reviewed by Carol DerSarkissian, MD on October 01, 2022
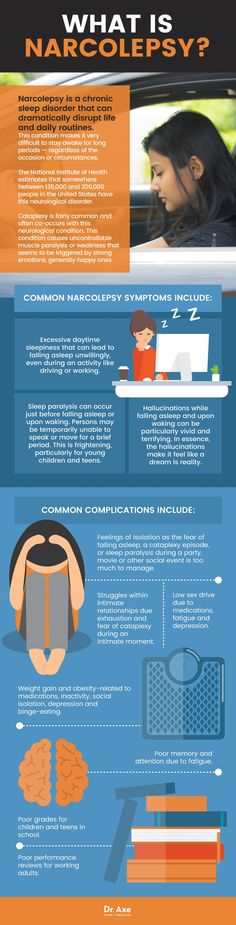
The world narcolepsy was coined in 1880s to mean “seized by somnolence,” or sleepiness. Just staying awake through the daylight hours can be difficult or impossible. Prescription drugs are often the go-to therapy for this brain disorder. But changes to your diet, habits, and environment also can help keep you alert without the side effects from medications.
It’s called “strategic napping.” Try to take several cat naps of about 15-20 minutes every day. But cap your dozes to no more than 30 minutes. Sleeping longer can make you more tired. If you have a job, the Americans With Disabilities Act requires your employer to make arrangements for you. For example, you might use your office, nursing lounge, or a wellness room to sneak quick rests.
Many people with narcolepsy sleep restlessly at night. Your body then needs to make the shortfall during the day. Try these tips to pack more quality ZZZs during your normal bedtime hours:
- Relax before turning in. Avoid alcohol close to bedtime.
- Try to go to bed at the same time each night.
- If you wake up during the night, avoid reaching for your phone or other electronics. Screens stimulate, not relax, you.
If you have a more severe type of condition called narcolepsy with cataplexy, you may be low on a hormone called hypocretin that helps you stay alert. The good news is that many foods contain hypocretin. They include sourdough bread, dark leafy greens, kimchi and other fermented vegetables, and salmon and other foods rich in omega-3 fatty acids.
Lots of people feel drowsy after a big meal. That can be especially true if you have narcolepsy. Limit sugar and other carbs to stay more alert. Eat smaller meals and snack on nuts, berries, and other nutritious foods in between.
Walk around every 20 minutes or so to stay alert. If you work at a desk, get up and visit the break room. Climb a flight of stairs and back. Other ideas to sneak in blood-flowing moments include:
Climb a flight of stairs and back. Other ideas to sneak in blood-flowing moments include:
- Pace while talking on the phone.
- Stand up when you read emails and texts.
- Walk to the bathroom even if you don’t need to go.
Those golden rays not only help you stay awake, they spark your brain to make feel-good chemicals. Sunshine helps your skin make vitamin D, a key nutrient in treating narcolepsy. Low vitamin D levels have been linked with poor sleep quality. Pair morning strolls with whole grains, scrambled eggs, and other foods that help put pep in your step.
Cold feet may help keep you awake. One study found that people with narcolepsy tend to have warmer skin temperatures in their fingers and toes. Cooler hands and feet made the people in the study more alert. You can dial down your body warmth with special cooling clothing, by avoiding warm drinks or meals, or using fans to keep your hands and feet chilled.
Coffee, tea, or other caffeine-fueled eye-openers may help prevent drowsiness. But take care if you take stimulant medications such as armodafinil (Nuvigil) or modafinil (Provigil) for your narcolepsy. Mixing them with caffeine can make your heart race or trigger jitters and anxiety. Avoid caffeine after 4 p.m.
But take care if you take stimulant medications such as armodafinil (Nuvigil) or modafinil (Provigil) for your narcolepsy. Mixing them with caffeine can make your heart race or trigger jitters and anxiety. Avoid caffeine after 4 p.m.
Regular physical activity ramps up your metabolism but also may help you rest better at night. Find something you can enjoy and stick with at least 20 minutes per day. Think tai chi, dancing, weight training, gardening, swimming, or tennis. Finish your workouts at least 3 hours before bedtime so you can wind down for restful slumber.
In a small survey, smokers who had narcolepsy all reported nicotine helped fight daytime sleepiness. There was a dangerous downside, though. One-third of the respondents said they’d fallen asleep while smoking, and many others had come close. Lit smoking materials led to burn injuries and property damage, and even larger fires. And it can be tough to quit because nicotine withdrawal causes drowsiness.
IMAGES PROVIDED BY:
1) Sanja Radin / Getty Images
2) fizkes / Getty Images
3) jacoblund / Getty Images
4) (Clockwise from top left) clubfoto / Getty Images, billnoll / Getty Images, naito8 / Getty Images, 4kodiak / Getty Images
5) Neydtstock / Getty Images
6) LL28 / Getty Images
7) adamkaz / Getty Images
8) Rike_ / Getty Images
9) Gregor Schuster / Photographer's Choice RR
10) PixelsEffect / Getty Images
11) alejandrophotography / Getty Images
SOURCES:
Progress in Neurobiology: “Challenges in the development of therapeutics for narcolepsy.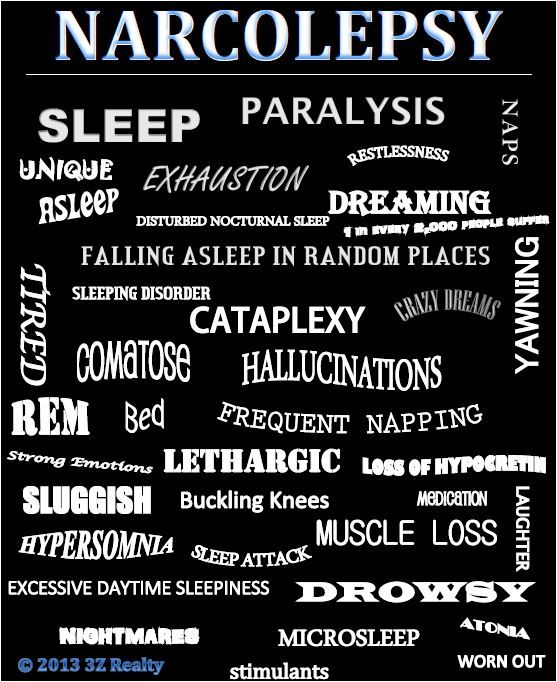 ”
”
Division of Sleep Medicine at Harvard Medical School: “Medications for Treating Daytime Sleepiness in Narcolepsy,” “Understanding Narcolepsy,” “Narcolepsy: Medications,” “Narcolepsy,” “Narcolepsy: At Work.”
Sleep Science: “Current and Future Treatment Options for Narcolepsy: A Review.”
Narcolepsy Network: “For Employees,” “Narcolepsy and Wakefulness: What’s the Connection?” “Lifestyle Adjustments.”
Sleep Foundation: “What Causes Narcolepsy?” “Cataplexy,” “Diet, Alcohol, Exercise, and Narcolepsy.”
Nutrients: “The Association Between Vitamin D Deficiency and Sleep Disorders: A Systematic Review and Meta-Analysis.”
Cleveland Clinic: “Narcolepsy: Management and Treatment.”
Journal of Clinical Sleep Medicine: “Narcoleptic Patients' Perceptions of Nicotine.”
© 2022 WebMD, LLC. All rights reserved. View privacy policy and trust info
Narcolepsy: Complementary and Alternative Treatments
Narcolepsy is a chronic sleep disorder that disrupts your wake-sleep pattern and brings about overwhelming drowsiness and periods of sudden sleep attacks during the daytime. The complex, lifelong condition affects 1 in 2,000 people but it often goes undiagnosed. There’s no cure for narcolepsy but medications and certain lifestyle changes may help manage the symptoms.
The complex, lifelong condition affects 1 in 2,000 people but it often goes undiagnosed. There’s no cure for narcolepsy but medications and certain lifestyle changes may help manage the symptoms.
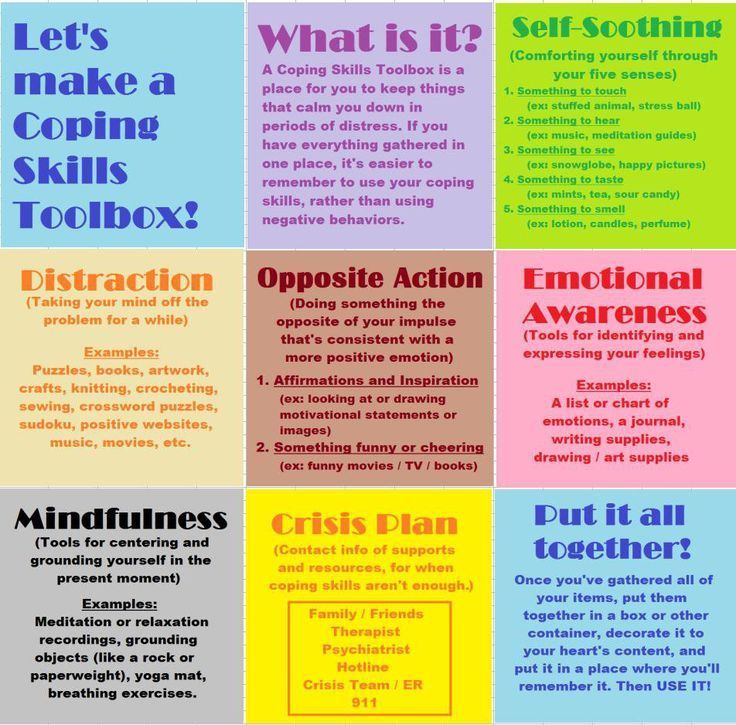
For some people with narcolepsy, conventional Western medication alone may not be enough to ease the day-to-day symptoms, which can take a toll on quality of life. Some choose to include complementary medicine or turn to alternative medicine to manage their condition.
Complementary medicine includes approaches that you take along with traditional Western medicine. While alternative medicine focuses on approaches you may take instead of conventional medicine your doctor uses. In some cases, your doctor may choose to combine different approaches to get the best results. This is called integrative medicine.
For narcolepsy, this can range from lifestyle changes, melatonin supplements, and natural herbal extracts to trying yoga or acupuncture for a better wake-sleep cycle.
Searching for an Alternative
For Gina Dennis, 49, intense sleepiness was something she struggled with since she was a teenager.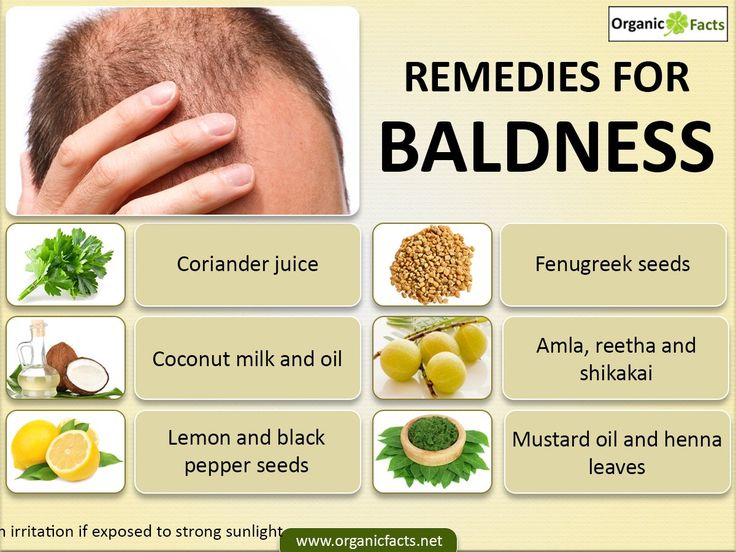 Getting out of bed each morning was an ordeal. It was something she shared in common with her mother. When her mother got diagnosed with narcolepsy later in life, Dennis decided to get checked out as well. Soon after, Dennis who was in her late 30s by then, was also diagnosed with narcolepsy.
Getting out of bed each morning was an ordeal. It was something she shared in common with her mother. When her mother got diagnosed with narcolepsy later in life, Dennis decided to get checked out as well. Soon after, Dennis who was in her late 30s by then, was also diagnosed with narcolepsy.
Her doctor put her on a regimen of drugs to help her stay awake through the day. But the drugs didn’t work as well as the Dallas native had hoped. But when her teenage son started to show symptoms, she came to find out that narcolepsy ran in her family. Turns out, her son and ex-husband also had the same sleeping disorder.
“It was breaking my heart, so we eventually got [my son] diagnosed. But here he is, a teenager, and he’s looking at a lifetime of medications. It just didn't seem good enough for me. So, I started to do some research,” Dennis says.
She went down the internet rabbit hole and stumbled upon another blogger who suggested the ketogenic diet to curb the daytime sleepiness. She decided to give it a try. In the ketogenic diet, the idea is to focus on getting your calories from high fat and moderate amounts of protein foods and cut back on most carbohydrates like sugar, bread, and pasta. It can be quite restrictive.
She decided to give it a try. In the ketogenic diet, the idea is to focus on getting your calories from high fat and moderate amounts of protein foods and cut back on most carbohydrates like sugar, bread, and pasta. It can be quite restrictive.
Dennis says she saw changes within a week. “I had a level of wakefulness that I had never had before, not even with the medication, it was cleaner, it didn't feel a buzz as some of the medications I had been taking,” Dennis says. In fact, over time, she stopped taking her medications altogether.
It’s been about 10 years since Dennis and her family started making dietary changes. While it’s helped bring a lot of the symptoms under control, she’s quick to add that it’s not a cure-all.
“I'm not saying I don't have symptoms because I do. But what I found through this entire journey is that diet is one component, the other component is some lifestyle changes.”
Alternative and Complementary Treatments
If you’re looking to try out or take on complementary or alternative approaches to manage your day-to-day narcolepsy symptoms, there are a few ways to go about it.
Yoga and meditation. A few studies point out that certain yoga positions can bring about relaxation, ease anxiety, and help with sleep issues. This may be because of its meditative properties such as breathing in and out and taking in the moment.
However, not all types of yoga are beneficial, says Rubin Naiman, PhD, a psychologist, sleep and dream specialist and clinical assistant professor of medicine at the University of Arizona Center for Integrative Medicine.
“I think yoga is helpful for anybody and everybody, because it really helps refashion our relationship with the body,” Naiman says. “There are 10 ways to do yoga, and not all are helpful. But when it’s done right, it’s almost like a friendly dialogue with our body.”
If you’re looking to try yoga to help you relax and sleep better at night, keep these things in mind:
- Find the right style of yoga. Hot yoga or vinyasa yoga require movements that will raise your heart rate. Doing this before bed will make your sleep worse.
 Instead, choose a relaxing technique.
Instead, choose a relaxing technique. - Set the scene for yoga and meditation. You can dim the light, put on soft, soothing music, and find a space to stretch out in comfy clothes.
- Focus on breathing. Pay attention to taking your breath in and out through your nose and mouth. This can be therapeutic and help you de-stress before you get to bed.
- Don’t push yourself too hard. Do only what you physically tolerate. You can work your way up over time.
Herbal remedies. Research shows that certain herbs can induce or regulate sleep. You can add them to beverages like tea or take them as supplements. For example, chamomile flower used in teas may help with poor sleep issues. The flower has several chemical compounds like apigenin that can have a mild tranquilizing effect. However, there needs to be more research done on chamomile’s effectiveness for conditions like narcolepsy. Some people are allergic to chamomile so it’s best to try in small amounts first.
Valerian root has natural sedative properties and has long been used as a sleep aid to help ease issues like stress, anxiety or headaches that disrupt your sleep cycle. But clinical trials on valerian root’s effects have had inconsistent results. Experts aren’t sure what effects long-term use may have on your body.
Other herbs used to improve sleep problems include passion flower, kava, red ginseng, lemon balm, and hops. If you’re taking prescription drugs, it’s important to note that certain herbs can interact with other drugs or cause side effects. It’s always a good idea to tell your doctor before you try any herbal remedies or supplements.
Melatonin. Your body naturally makes melatonin around 4 hours before you got to sleep. It’s triggered when your body’s exposure to light reduces naturally at night. But if you have narcolepsy, your sleep/wake cycle may not be properly regulated. Research shows that taking melatonin supplements can help regulate and induce sleep, increase rapid eye movement (REM) sleep time, and improve sleep quality. You can buy melatonin in pill form over the counter. If you’re not sure how much you take, ask the pharmacist or your doctor.
You can buy melatonin in pill form over the counter. If you’re not sure how much you take, ask the pharmacist or your doctor.
Lifestyle changes. When you have narcolepsy, one of the symptoms includes falling asleep or feeling excessively drowsy involuntarily during the day. This can be dangerous if you’re driving or out and about in public. To reduce the intense sleepiness during the day and sleep better at night, you can:
- Schedule small, regular naps during the day.
- Stick to a bedtime routine. Try to go to bed at the same time each night and wake up at the same time, too.
- Reduce any distractions in the room where you sleep at night.
- Avoid alcohol, smoking, and caffeine before bedtime.
- Don’t eat large meals for dinner before sleep.
- Exercise regularly to help you stay awake and alert during the day. But don’t work out or push yourself too much 2 hours before you go to bed.
Cognitive behavioral therapy (CBT). This type of psychological treatment attempts to change your thinking patterns. This may help you cope with symptoms for several health conditions, including narcolepsy. Naiman says it’s especially helpful for people who have cataplexy, a core symptom in which you may have a sudden muscle weakness and collapse. It can be triggered by emotions like laughter, surprise, or negative things like stress and anxiety.
This type of psychological treatment attempts to change your thinking patterns. This may help you cope with symptoms for several health conditions, including narcolepsy. Naiman says it’s especially helpful for people who have cataplexy, a core symptom in which you may have a sudden muscle weakness and collapse. It can be triggered by emotions like laughter, surprise, or negative things like stress and anxiety.
“When people begin to have symptoms of cataplexy, there is a reaction of anxiety like, ‘oh God, I’m about to fall off,’ and then the anxiety spirals into this adversarial relationship with narcolepsy,” Naiman says. “With CBT, we talk about meeting cataplexy in a mindful way. It’s about understanding that if I tense up each time, it makes the cataplexy worse.”
For some patients, Naiman says he uses CBT to help them consciously work through a narcolepsy episode when it comes on. This helps them learn skills to handle it better the next time they have a sudden episode.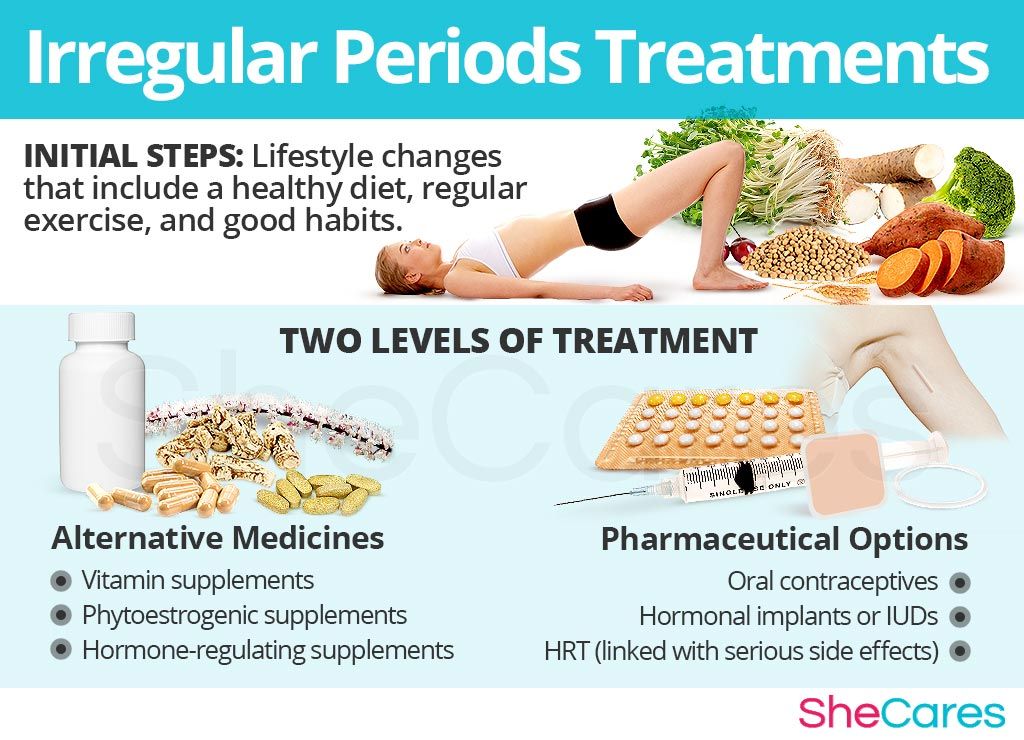
CBT may include learning other strategies like:
- Learning how to use problem-solving skills to manage difficult situations
- Evaluating thoughts and experiences in a realistic way
- Developing confidence
If you plan to try CBT, ask your doctor or a psychologist if it’s right for you.
Acupuncture. As part of traditional Chinese medicine, acupuncture practitioners insert thin needles at specific points on your body. The idea is for the needles to stimulate certain pressure points that bring about pain relief and reduce narcolepsy symptoms like headache. However, researchers say there’s not enough evidence to know if it helps with sleep problems.
Acupuncture is relatively safe if it’s done by someone who’s experienced. However, if it’s done incorrectly, nonsterile needles can cause infections or other dangerous health problems. If you’re going to try acupuncture, make sure to visit an experienced acupuncturist.
Emotional freedom technique (EFT). Similar to acupuncture, EFT is a simple, self-therapeutic manual tapping therapy used to relieve stress and anxiety. To do it, you have to tap certain meridian points on your face and body while saying out loud whatever is concerning you to work through distressing situations or the onset of anxiety or depression. It combines other psychological therapies like talk therapies, exposure therapy, and cognitive behavioral therapy. It promotes self-acceptance.
Similar to acupuncture, EFT is a simple, self-therapeutic manual tapping therapy used to relieve stress and anxiety. To do it, you have to tap certain meridian points on your face and body while saying out loud whatever is concerning you to work through distressing situations or the onset of anxiety or depression. It combines other psychological therapies like talk therapies, exposure therapy, and cognitive behavioral therapy. It promotes self-acceptance.
It was founded in the 1995 and the idea behind the tapping is that it stimulates the pressure points to signal the brain and the central nervous system to release chemicals to ease stress or fear.
While there are few studies that show EFT’s effects and benefits psychologically, there is limited evidence if it positively impacts physical health to improve conditions like narcolepsy and others. But EFT is safe, harmless, and a cheap, affordable option you can use anywhere if you want to calm your emotions and center yourself.
Things to Be Aware of Before You Try Complementary or Alternative Medicine
Most complementary and alternative treatments like yoga or EFT are safe to use and harmless. But not all alternative medicine options, particularly herbal remedies, products, and supplements, are safe even if they are “natural.”
Many herbs or over-the-counter supplements may interact or suppress prescription medication you may be taking and may cause dangerous side effects. The FDA does not regulate dietary supplements like it oversees and regulates prescription drugs.
Thinking about trying a complementary or alternative medicine or product for narcolepsy?
- Talk to your doctor about it. Ask if it will affect or interact with any drugs you may be taking for narcolepsy or other conditions you may have. Tell them if you’re planning to use a certain product or technique. This will help them get a full picture of your health and medical history when they treat you.
- Look up potential side effects or safety for long-term use before you try any herbs.
 If you’re not sure, ask your doctor about it.
If you’re not sure, ask your doctor about it. - If you’re pregnant or planning to get pregnant, ask your doctor before trying something new.
- Ask your health insurance provider if they cover complementary or alternative treatment options like CBT or acupuncture. This may help avoid any surprise bills or expenses.
- Talk to your doctor before you cut back or stop taking your prescription drugs or treatments.
If you experience side effects or an allergic reaction from certain products or supplements, get medical attention as soon as possible or tell your doctor about it.
what is it, symptoms, treatment, causes of daytime sleepiness
Font size Color scheme Images
x
Make an appointment
Name* Phone* Adult Child (under 18)x
Sign up for analysis
Name* Phone* ☆ st. Malaya Balkanskaya, 23 (m. Kupchino)
Kupchino)
Dunaisky ave., 47 (m. Dunaiskaya)
Udarnikov ave., 19 (m. Ladozhskaya)
st. Marshala Zakharova, 20 (metro station Leninskiy pr-t)
Vyborgskoe shosse, 17 (metro Prospect of Enlightenment)
- Call
435 55 55 -
Make an appointment
This disease is treated by Somnologist
The information provided on this page should not be used for self-treatment or self-diagnosis. If you suspect a disease, you should seek help from a qualified specialist. Only your doctor can diagnose and prescribe treatment.
Article content:
- Causes
- Symptoms of narcolepsy
- Diagnostics
- Narcolepsy treatment
- Prognosis and prevention
What is narcolepsy?
Narcolepsy is a pathological condition characterized by an inability to control sleep and wakefulness. Sudden onset of excessive daytime sleepiness and other symptoms of narcolepsy can occur at any time, even in situations that require extreme concentration, such as driving. The risk group for the development of narcolepsy is men, the frequency of cases is 1 in 2 thousand people. But there is an opinion that the prevalence is higher due to the fact that not all patients do not seek medical help and treatment. Narcolepsy Source:
The risk group for the development of narcolepsy is men, the frequency of cases is 1 in 2 thousand people. But there is an opinion that the prevalence is higher due to the fact that not all patients do not seek medical help and treatment. Narcolepsy Source:
description of the clinical observation. Remizevich R.S., Kurasov E.S. Bulletin of the National Medical and Surgical Center. N. I. Pirogova, Volume 8, No. 4, 2013. pp. 141-145 - not a fatal pathology, but accidents still happen during attacks.
Causes
The exact causes of narcolepsy are unknown, although it has been established that heredity plays a role, as well as a lack of the neurotransmitter orexin, which is responsible for wakefulness.
REM sleep literally invades the periods of wakefulness and the transition to sleep. Symptoms of narcolepsy are associated with a sharp loss of muscle tone, the appearance of vivid visions, which are just characteristic of the phase of REM sleep. nine0003
It was not possible to establish the exact reasons for the decrease in the production of the neurotransmitter, but the predisposing factors for the development of the pathology were identified:
- serious craniocerebral injuries and their consequences;
- infectious diseases affecting the nervous system Source:
Autonomic disorders in narcolepsy (review of foreign literature). Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. pp. 165-168;
Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. pp. 165-168; - pronounced hormonal changes; nine0025
- autoimmune diseases;
- chronic stress and severe emotional upheaval;
- nervous and physical exhaustion.
As a rule, the development of a disease requires the combined action of several factors at once. Great importance in the mechanism of the development of the state is given to the work of immunity. An immune response is triggered, as a result of which its own cells are mistakenly destroyed, which leads to the onset of symptoms.
Symptoms of narcolepsy
The most common symptom is excessive daytime sleepiness, as well as persistent sleep disturbances at night. This creates inconvenience, spoils the quality of life, affects success in work and social relations.
Over time, the clinical picture changes, other signs join:
- The first and most common symptom is sudden falling asleep during the day.
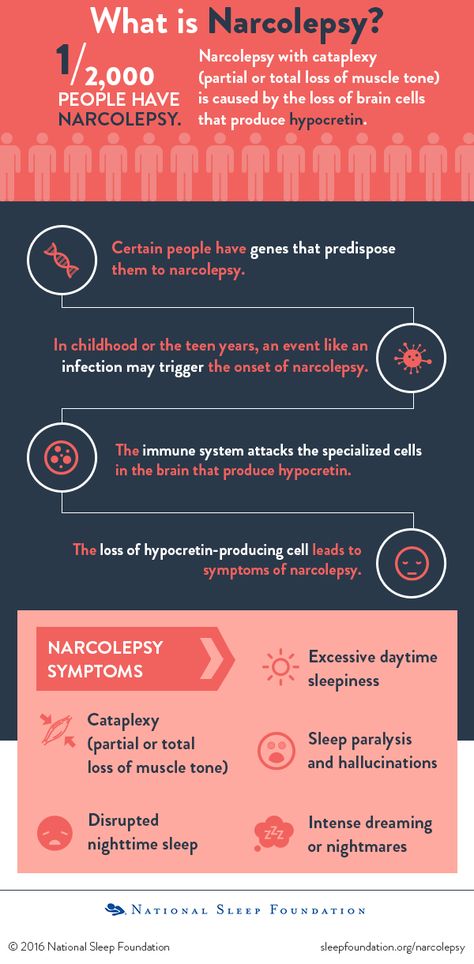 Drowsiness is severe, patients fall asleep against their will, even in unsuitable surroundings. But after waking up, they feel a surge of strength, there is no drowsiness. This state can be deceptive - after a short time they fall asleep again. At the same time, waking up the patient is no more difficult than during normal sleep. nine0025
Drowsiness is severe, patients fall asleep against their will, even in unsuitable surroundings. But after waking up, they feel a surge of strength, there is no drowsiness. This state can be deceptive - after a short time they fall asleep again. At the same time, waking up the patient is no more difficult than during normal sleep. nine0025 - Cataplexy Source:
Narcolepsy with prepubertal onset cataplexy. Gromova D.O., Zinovieva O.E., Rogovina E.G., Poluektov M.G. Neurological journal No. 4, 2012. pp. 22-27 - sudden muscle weakness after strong emotional outbursts. The resulting weakness can be explained by a sharp loss of muscle tone, which often ends in injuries associated with a fall. The duration of the attack varies and lasts up to several minutes, followed by falling asleep. nine0025 - Hallucinations on falling asleep and waking up. They are characterized as vivid acoustic or visual visions, which correspond to REM sleep. This state is sometimes called "waking sleep", and the patient himself does not realize that he is sleeping and dreaming.
 This is a dangerous condition that creates confusion between reality and dream.
This is a dangerous condition that creates confusion between reality and dream. - Sleep paralysis is a condition characterized by the inability to move after waking up, but the ability to breathe and blink remains. The patient is conscious, understands where he is. Most often, sleep paralysis is formed in the morning, less often in the evening and at night. Sleep paralysis is aggravated by hallucinations without the ability to move. The condition goes away after a few minutes. nine0025
Only 10% of patients present with all symptoms at once. Usually first appear in young people, with no previous diseases. Although they can be associated with strong emotional upheavals or chronic stress. After the first onset of symptoms, narcolepsy is permanent, but does not affect life expectancy.
In clinical practice, it is customary to distinguish 2 types of narcolepsy:
- the first occurs due to orexin deficiency, the appearance of cataplexy is characteristic Source:
Narcolepsy-cataplexy. Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. pp. 53-55;
Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. pp. 53-55; - the second is characterized by a normal level of the neurotransmitter and cataplexy does not occur.
Diagnostics
The main thing is to detect the pathology in time to prevent risks to the patient's physical health and harm to others. The patient cannot control narcolepsy, attacks occur even at the time of hard work and maximum concentration of attention, as well as performing tasks that involve risks to health and even life. nine0003
When visiting a doctor, the symptoms that characterize the diagnosis are studied in detail. The doctor is interested in:
- the patient's complaints, when the attack first occurred and how long it lasted, what symptoms are present;
- neurological examination data, some tests;
- results of additional examination methods to confirm the diagnosis.
These include polysomnography.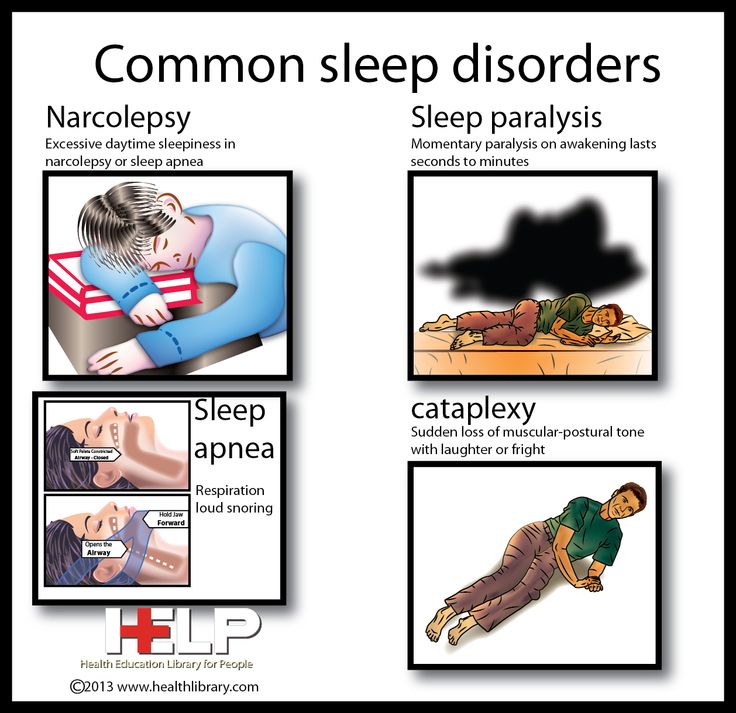 Source:
Source:
Problems in the differential diagnosis of epileptic seizures and narcolepsy (clinical observation). Dmitrenko D.V., Alekseeva O.V., Sapronova M.R., Usoltseva A.A., Areshkina I.G. Bulletin of the North-Eastern Federal University. M. K. Ammosov. Series: Medical Sciences No. 4(13), 2018. pp. 44-51 with EEG data. This method of examination allows you to objectively assess the activity of the brain and sleep phases. The survey continues throughout the night. Electrodes are placed on the patient's head, which fix the indicators and give them out in the form of curves - the doctor analyzes the data. nine0003
Additionally, CT and MRI are recommended to assess brain function and condition. In some cases, it may be necessary to analyze the cerebrospinal fluid, which is aimed at determining the concentration of orexin.
Treatment tactics are determined by the data obtained during the examination. This takes into account the severity of concomitant pathology, acquired diseases.
Treatment of narcolepsy
Drug treatment prescribed by specialists is constant, but the number of drugs depends on the clinical picture and the characteristics of the manifestation of the disease. Doctors usually prescribe:
- stimulants;
- sleeping pills to help normalize night sleep;
- antidepressants;
- means to combat daytime sleepiness.
Other recommendations are added to medications - lifestyle changes that help control symptoms. Patients with narcolepsy are recommended to:
- strictly observe the daily regimen: go to bed and get up at the same time, regardless of holidays and weekends; nine0025
- give up alcohol completely and stop smoking;
- Minimize your intake of coffee, sugary sodas, energy drinks, and junk food;
- introduce a short daytime nap into your schedule;
- lead an active lifestyle, play sports, for example, exercise therapy, yoga.
Prognosis and prevention
Unfortunately, there is no cure for narcolepsy.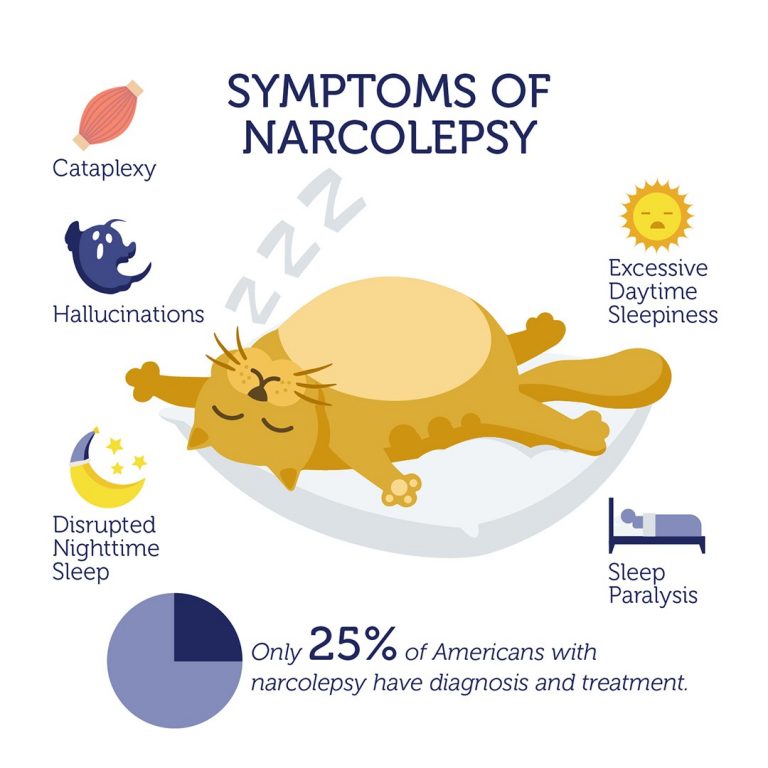 All treatment is aimed at controlling and maximizing symptom relief. After the course of treatment, the patient returns to his usual way of life, although there are still some restrictions. nine0003
All treatment is aimed at controlling and maximizing symptom relief. After the course of treatment, the patient returns to his usual way of life, although there are still some restrictions. nine0003
There are some prohibitions for all narcolepsy patients. They are forbidden to drive a car, as well as to occupy positions related to hazardous industries, for example, to work with machine tools, in large factories, etc. After all, an attack can happen at any moment, regardless of what a person is doing.
- Narcolepsy-cataplexy. Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. p.53-55
- Narcolepsy with cataplexy with onset in prepubertal age. Gromova D.O., Zinovieva O.E., Rogovina E.G., Poluektov M.G. Neurological journal №4, 2012. pp.22-27
- Modern concepts of narcolepsy with a description of clinical observation. Remizevich R.S., Kurasov E.S. Bulletin of the National Medical and Surgical Center. N. I. Pirogova, Volume 8, No.
 4, 2013. p.141-145
4, 2013. p.141-145 - Autonomic disorders in narcolepsy (review of foreign literature). Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. p.165-168
- Problems of differential diagnosis of epileptic seizures and narcolepsy (clinical observation). Dmitrenko D.V., Alekseeva O.V., Sapronova M.R., Usoltseva A.A., Areshkina I.G. Bulletin of the North-Eastern Federal University. M. K. Ammosov. Series: Medical Sciences No. 4(13), 2018. p.44-51
Article published : 31/05/2017
Last updated : 30/11/2022
See also
Nightmares
Sleep disorders
Snoring treatment
Licenses
Medicom LLC
(Udarnikov Avenue)
Medicom LLC
(Vyborgskoye Highway)
Medi Len LLC
(Marshal Zakharov St.)
MediProf LLC
avenue)
Medi Prof LLC
(Malaya Balkanskaya St.)
Go to the license section Go to the legal information section
record from website DISCOUNT 10%
Enrollment is only possible through the contact center.
To register, fill out the form below and you will be contacted.
By clicking on the button, you consent to the processing of your personal data by
nine0003
You are enrolling:
Clinic: {{department}}
Specialty: {{specialty}}
Doctor: {{doctor}}
Date and time: {{form.date | setTime(form.time) | dateTimeFormatted}}
Date of birth: {{age | dateFormatted}}
{{appointmentReply}}
By clicking "Sign up", I accept the terms of the user agreement, the provisions on the protection of personal data and give my consent to the processing of personal data. nine0003
In order to pass the mandatory registration, you must come to the registration desk 10 minutes before the time of your appointment with your passport.
If the patient is a minor (children under 18), it is mandatory to be accompanied by one of the parents with the presentation of his passport and birth certificate of the child.
Relatives and third parties accompanying a minor must have a notarized consent of the parents or legal representatives.
If you have booked an appointment with a coloproctologist, please read the information about preparing for an appointment
The price of the consultation includes:
History taking, preliminary diagnosis and examination appointment. All additional doctor's manipulations at the appointment are paid according to the price list.
If you change your mind, please unsubscribe from the appointment by phone +7 (812) 435-55-55
The price of the consultation includes:
History taking, preliminary diagnosis and examination appointment. All additional doctor's manipulations at the appointment are paid according to the price list. nine0003
If you change your mind, please unsubscribe from the appointment using your Personal Account or by phone +7 (812) 435-55-55.
Are you sure you want to stop recording?
If you have any questions, call us at +7 (812) 435-55-55
Are you sure you want to change the current entry?
If you have any questions, call us at +7 (812) 435-55-55
You are subject to some restrictions on online booking. nine0003
nine0003
Appointment possible via contact center.
You can sign up by phone +7 (812) 435-55-55
The specialist does not see patients of the specified age. To register please fill out the form below and you will be contacted.
Make an appointment
Would you like us to call you
?
Name Phone
By clicking on the button, you consent
to process their personal data
You will be contacted to confirm your application.
Making an appointment
Preliminary appointment through the site
Our employee will contact you to confirm the appointment with a specialist
By clicking on the button, you consent to the processing of your personal data by
Learn more about quality assurance of medical services
Would you like us to call you
?
By clicking on the button, you consent to the processing of your personal data by
Leave a request and our specialist
will select a convenient time for a communication session with a doctor
By clicking on the button, you consent to the processing of your personal data by
Screenshot of a review from Yandex. Maps*
Maps*
By clicking on the button, you consent to the processing of your personal data by
Sign up
for a consultation
Choose a clinic 1st. Marshal Zakharov, house 20Vyborg highway, house 17, bldg. 1
By clicking on the button, you consent
to process their personal data
Learn more about the quality assurance of medical services
Appointment for tests
Preliminary appointment through the site
Our employee will contact you to confirm the appointment with a specialist
By clicking on the button, you consent to the processing of your personal data by
Write to manager
customer support services SM-Clinic
By clicking on the button, you consent to the processing of your personal data by
We use cookies. This allows us to analyze the interaction of visitors with the site and make it better. By continuing to use the site, you agree to the use of cookies.
This allows us to analyze the interaction of visitors with the site and make it better. By continuing to use the site, you agree to the use of cookies.
To accept
Multimodal clinical effects of orexin
Despite a long history of studying the mechanisms of regulation of sleep and wakefulness, today there is no absolutely accurate picture of the cause-and-effect relationships of sleep mechanisms. Every year there are new hypotheses and discoveries in somnology, on the one hand, allowing you to get closer to understanding the subtle nuances of the brain, and on the other hand, raising new questions.
A striking example is the evolution of research on orexin, a substance of great importance as a regulator of the neurohumoral system. Since the end of the 20th century, there has been an avalanche-like increase in the number of publications devoted to this topic. nine0003
A Brief History of the Evolution of Orexin Research
In 1998, two independent companies using very different approaches reported the discovery of orexin/hypocretin. L. De Lecea et al. [1], using a special molecular biological technique of the complementary DNA coding strand, determined that the transcript expressed in the hypothalamus encodes 2 neuropeptides called hypocretin-1 and -2. Sakurai T. et al. [2] used the “reverse pharmacology” approach — molecular screening using recombinantly expressed receptors for which natural ligands are unknown. It has been shown that the penetration of orexin, A or B into the lateral ventricles of the brain in rats increases during meals. nine0003
L. De Lecea et al. [1], using a special molecular biological technique of the complementary DNA coding strand, determined that the transcript expressed in the hypothalamus encodes 2 neuropeptides called hypocretin-1 and -2. Sakurai T. et al. [2] used the “reverse pharmacology” approach — molecular screening using recombinantly expressed receptors for which natural ligands are unknown. It has been shown that the penetration of orexin, A or B into the lateral ventricles of the brain in rats increases during meals. nine0003
Subsequently, the importance of orexin in the regulation of the sleep-wake cycle was suggested. L. Lin et al. [3] in the study of the genotype identified mutations in the orexin-2 receptor genes in dogs that were involved in narcolepsy with cataplexy. Other authors [4] have reported that preproorexin in gene-knocked mice exhibits a phenotype strikingly similar to human narcolepsy with cataplexy.
In 2000, the role of disturbances in the orexin system in the development of narcolepsy-cataplexy was proved. S. Nishino et al. [5] found that the level of orexin, A (hypocretin-1) is reduced in the cerebrospinal fluid (CSF) in about 95% of narcolepsy patients with cataplexy. C. Peyron et al. [6] and T. Thannickal et al. [7] also showed in their works a sharp decrease in the level of orexin mRNA and the phenomenon of immunoreactivity in the brain during postmortem autopsy of patients with narcolepsy with cataplexy.
S. Nishino et al. [5] found that the level of orexin, A (hypocretin-1) is reduced in the cerebrospinal fluid (CSF) in about 95% of narcolepsy patients with cataplexy. C. Peyron et al. [6] and T. Thannickal et al. [7] also showed in their works a sharp decrease in the level of orexin mRNA and the phenomenon of immunoreactivity in the brain during postmortem autopsy of patients with narcolepsy with cataplexy.
In 2003, J. Willie et al. [8] demonstrated the important role of orexin receptor subtypes in the regulation of sleep and wakefulness. A. Yamanaka et al. proved [9] that orexin receptors are activated under the influence of negative energy balance and are necessary for awakening. nine0003
In 2004, M. Mieda et al. [10] found that ectopic expression of the preproorexin transgene or administration of orexin A into the brains of mice with “off” orexin neurons suppresses the narcoleptic phenotype of these mice.
In less than 10 years, the path from experimental work to the emergence of a hypothesis about the possibility of using the "orexin pathway" for the correction of sleep disorders was covered: in 2007, C.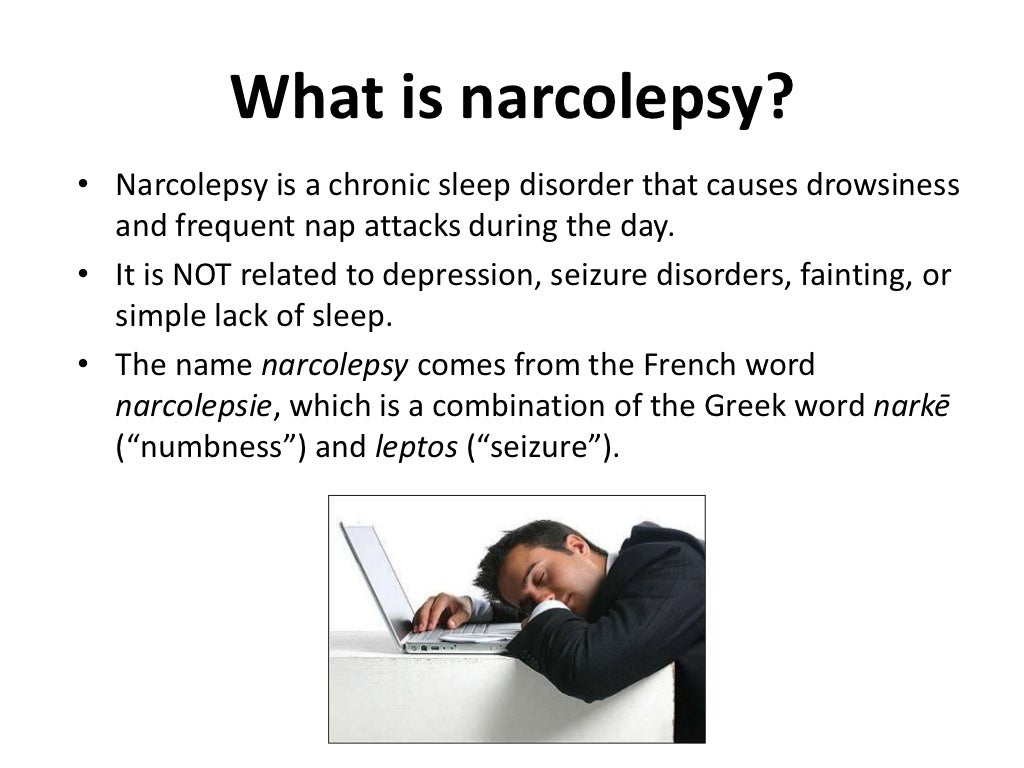 Brisbare-Roch et al. [11] demonstrated that an orexin antagonist for oral administration, blocking both types of its receptors, acts as a hypnotic. nine0003
Brisbare-Roch et al. [11] demonstrated that an orexin antagonist for oral administration, blocking both types of its receptors, acts as a hypnotic. nine0003
Clinical effects of orexin
The most promising is the use of orexin in insomnia, but the revealed multi-vector action of this molecule suggests its wider use in clinical practice.
Osteoporosis and orexin
Orexin and leptin affect bone remodeling. As a team of scientists from the University of Texas Southwestern Medical Center (UT Southwestern Medical Center) found out [12], orexins, protein neurotransmitters, also play an important role in bone formation. The data obtained may allow the development of new treatments for osteoporosis. Orexins, or hypocretins, are a special type of protein that nerve cells use to communicate with each other. Due to a lack of bone-forming osteoblast cells, orexin-deficient mice have thinner, more brittle bones that break easily. nine0003
nine0003
It turned out that orexins play a dual role: they both promote bone formation and prevent its formation (Fig. 1). Rice. 1. Clinical impact of orexin. Directly in the skeleton itself, they interact with another protein, the orexin OX1R receptor, which reduces the level of ghrelin, the hormone responsible for feeling hungry. This process slows down the production of new osteoblasts and therefore hinders the formation of bone cells. At the same time, in the brain, orexins interact with the OX2R receptor, leading to a decrease in the levels of leptin, a hormone that promotes bone destruction, which is ultimately a positive factor. nine0003
Thus, the prevention and treatment of osteoporosis can be achieved by suppressing the activity of OX1R or by stimulating OX2R. Neuropeptides manage to regulate bone formation through two different receptors located in two different tissues.
Neurological pathology associated with disorders in the orexin system
Narcolepsy nine0055
Currently, the occurrence of most cases of narcolepsy with cataplexy is explained by an autoimmune lesion of orexin (hypocretin) neurons of the hypothalamus. Confirmation of the autoimmune nature of the disease can be an association with certain histocompatibility antigens, a connection with a previous infectious disease or immunization, the presence of an elevated level of C-reactive protein in the blood plasma. The death of hypocretin neurons is accompanied by a decrease in the level of hypocretin-1 in the CSF in the majority (90%) of patients with narcolepsy with cataplexy [12] .
Confirmation of the autoimmune nature of the disease can be an association with certain histocompatibility antigens, a connection with a previous infectious disease or immunization, the presence of an elevated level of C-reactive protein in the blood plasma. The death of hypocretin neurons is accompanied by a decrease in the level of hypocretin-1 in the CSF in the majority (90%) of patients with narcolepsy with cataplexy [12] .
Despite the vivid clinical picture, nocturnal polysomnographic examination is required to confirm the diagnosis, followed by a multiple sleep latency test, which is the “gold standard” for diagnosing narcolepsy [12].
In some cases, confirmation of the diagnosis of "narcolepsy with cataplexy" requires determination of the level of hypocretin-1 in the CSF (≤110 pg / ml).
There are two more clinical forms of narcolepsy - narcolepsy without cataplexy and secondary narcolepsy. Narcolepsy without cataplexy accounts for about 10% of all forms of narcolepsy. In such patients, a decrease in the level of hypocretin-1 in the CSF occurs much less frequently (in 10–20% of cases), which implies the preservation of the main number of hypocretin-producing neurons. In secondary narcolepsy with cataplexy, characteristic clinical symptoms appear against the background of an obvious underlying disease: a tumor or sarcoidosis of the hypothalamus, multiple sclerosis, stroke, paraneoplastic syndrome, Niemann-Pick disease [12]. nine0003
In such patients, a decrease in the level of hypocretin-1 in the CSF occurs much less frequently (in 10–20% of cases), which implies the preservation of the main number of hypocretin-producing neurons. In secondary narcolepsy with cataplexy, characteristic clinical symptoms appear against the background of an obvious underlying disease: a tumor or sarcoidosis of the hypothalamus, multiple sclerosis, stroke, paraneoplastic syndrome, Niemann-Pick disease [12]. nine0003
Kleine-Levin Syndrome (KLS)
SCL is characterized by sleep attacks lasting hours or days, with an imperative onset and difficulty waking up. the syndrome belongs to rare and little-studied diseases not only in our country, but throughout the world [13]. The etiology of the syndrome remains unknown. Great importance is attached to the study of the role of certain neuropeptides (orexin, neuropeptide Y, leptins) in the pathogenesis of the disease. Recent studies [14] link the development of SCL with apoptosis of orexin (hypocretin) neurons, which reduces the ability to wake up and shortens the REM sleep phase. Orexin-producing neurons regulate the activity of neurons that produce monoamines by the type of reciprocal connection. Monoamines excite the thalamus and cerebral cortex, maintaining the state of wakefulness. In the state of sleep, there is a constant inhibition of orexin neurons by the ventrolateral nucleus of the preoptic region. nine0003
Orexin-producing neurons regulate the activity of neurons that produce monoamines by the type of reciprocal connection. Monoamines excite the thalamus and cerebral cortex, maintaining the state of wakefulness. In the state of sleep, there is a constant inhibition of orexin neurons by the ventrolateral nucleus of the preoptic region. nine0003
Parkinson's disease (PD).
There is an assumption about the primary nature of daytime sleepiness in PD [15]. In this regard, the attention of researchers was attracted by narcolepsy, since, in general, sleep disorders in PD are very similar to those in narcolepsy, especially in the so-called "narcolepsy without cataplexy", which made it possible to put forward a hypothesis about a narcoleptic-like (i.e., orexinergic) mechanism of drowsiness in parkinsonism [ 16-18]. Immediately after the discovery of the orexin system, an assumption arose about its destruction in PD as well [19]. This hypothesis was confirmed only in 2007, when a significant degeneration of orexin neurons was found in the brain of patients with PD during a postmortem study [20–23]. Moreover, it has been shown that PD is also accompanied by the destruction of Melatonin-concentrating hormone (MCH) of the brain, a system that is reciprocal with respect to the orexin/hypocretin system, which remains unaffected in patients with narcolepsy [22, 24]. At the same time, the stage of the disease turned out to be associated with the degree of destruction of orexin and MCH neurons, rather than dopaminergic neurons. According to some authors [25], dopaminergic neurons only mediate motor disturbances caused by the destruction of the orexin system. These data, revolutionary for understanding the nature of PD, are now generally recognized [26–30]. nine0003
Moreover, it has been shown that PD is also accompanied by the destruction of Melatonin-concentrating hormone (MCH) of the brain, a system that is reciprocal with respect to the orexin/hypocretin system, which remains unaffected in patients with narcolepsy [22, 24]. At the same time, the stage of the disease turned out to be associated with the degree of destruction of orexin and MCH neurons, rather than dopaminergic neurons. According to some authors [25], dopaminergic neurons only mediate motor disturbances caused by the destruction of the orexin system. These data, revolutionary for understanding the nature of PD, are now generally recognized [26–30]. nine0003
Anti-narcotic potential of orexin
As a result of the studies [31], new data were obtained on some general mechanisms of formation of dependence on psychoactive drugs in the experiment based on the study of the role of orexins in the narcogenic effects of psychostimulants (phenamin, dizocilpine) and sedatives with a hypnotic component (trimeperidine). It has been shown that orexin, A modulates the reinforcing (narcogenic) properties of these psychoactive substances through the structures of the dilated amygdala (the central nucleus of the amygdala, the nuclei of the bed of the terminal strip and the medial part of the nucleus accumbens). The mechanisms of this modulation involve the orexin OX1R and dopamine receptors, which mediate direct activation of the lateral hypothalamus through specific pathways (the anterior ventral cerebral dopaminergic bundle) (Fig. 2). Rice. 2. Schematic representation of the connections between the lateral hypothalamus (orexin), monoaminergic neurons and VLPO (ventrolateral preoptic area) of the hypothalamus (GABA). SCN - suprachiasmatic nucleus; VLPN, ventrolateral preoptic nucleus; GABA is gamma-aminobutyric acid. nine0003
It has been shown that orexin, A modulates the reinforcing (narcogenic) properties of these psychoactive substances through the structures of the dilated amygdala (the central nucleus of the amygdala, the nuclei of the bed of the terminal strip and the medial part of the nucleus accumbens). The mechanisms of this modulation involve the orexin OX1R and dopamine receptors, which mediate direct activation of the lateral hypothalamus through specific pathways (the anterior ventral cerebral dopaminergic bundle) (Fig. 2). Rice. 2. Schematic representation of the connections between the lateral hypothalamus (orexin), monoaminergic neurons and VLPO (ventrolateral preoptic area) of the hypothalamus (GABA). SCN - suprachiasmatic nucleus; VLPN, ventrolateral preoptic nucleus; GABA is gamma-aminobutyric acid. nine0003
By blocking OX1R in dilated amygdala structures, the reinforcing effects of the NMDA antagonist MK-801 can be abolished, as well as the effects of phenamine and trimeperidine can be significantly reduced. At the same time, the systemic blockade of OX1R when their antagonist SB-408124 is administered into the brain ventricles has a less pronounced effect compared to intrastructural administration. The OX1R antagonist SB-408124 potentiates the inhibitory effects of the dopamine D2 receptor antagonist sulpiride. Co-administration of the OX1R antagonist SB-408124 and sulpiride suppresses the psychoactivating effect of phenamine, dizocilpine, and trimeperidine on the self-stimulation response. The proposed molecular mechanism of this phenomenon can be considered the formation of a dimeric (heteromeric) structure between the orexin OX1R and the dopamine D2 receptor on the membranes of brain neurons. This phenomenon of enhancement (potentiation) of the antinarcotic action of orexin and dopamine antagonists is important for the development of methods for the biological prevention of dependence on various narcotics, the essence of which is the search and study of agents that eliminate or reduce the reinforcing properties of narcotics.
At the same time, the systemic blockade of OX1R when their antagonist SB-408124 is administered into the brain ventricles has a less pronounced effect compared to intrastructural administration. The OX1R antagonist SB-408124 potentiates the inhibitory effects of the dopamine D2 receptor antagonist sulpiride. Co-administration of the OX1R antagonist SB-408124 and sulpiride suppresses the psychoactivating effect of phenamine, dizocilpine, and trimeperidine on the self-stimulation response. The proposed molecular mechanism of this phenomenon can be considered the formation of a dimeric (heteromeric) structure between the orexin OX1R and the dopamine D2 receptor on the membranes of brain neurons. This phenomenon of enhancement (potentiation) of the antinarcotic action of orexin and dopamine antagonists is important for the development of methods for the biological prevention of dependence on various narcotics, the essence of which is the search and study of agents that eliminate or reduce the reinforcing properties of narcotics.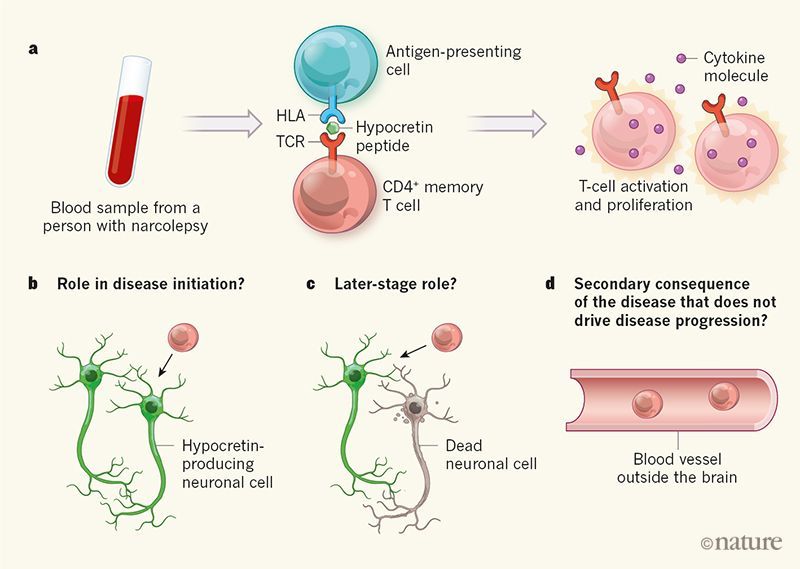 nine0003
nine0003
Sleep improvement for insomnia
Of particular importance is the use of the neurohumoral effects of orexin in insomnia disorders. It is this vector of clinical use that is by far the most studied and ultimately implemented in terms of practical application. We are talking about the use of a synthetic highly selective orexin receptor antagonist, suvorexant, in patients with sleep disorders. The difficulties faced by doctors in the care of patients with insomnia are well known: on the one hand, the apparent freedom of maneuver when using a number of hypnotic drugs in patients with insomnia, on the other hand, any experienced doctor who has encountered this group of patients knows how difficult there is their management. nine0003
The pharmacological action of suvorexant is based on the blocking of the orexin system due to the reversible antagonism of the orexin OX1R and OX2R receptors, which leads to the suppression of wakefulness and improvement in the quality of sleep [31]. Unlike benzodiazepines, which activate GABA receptors and have associated side effects such as visual hallucinations, memory problems, drug addiction, and aftereffect syndrome, suvorexant is believed to selectively reversibly block orexin neurons, affecting only the wakefulness system. and reducing the risk of developing complications that are characteristic of other hypnotics that affect the sleep system [32]. This drug has a linear pharmacokinetics, its maximum plasma concentration is reached on average 2 hours after administration, the half-life is about 12 hours. The drug reaches a stationary concentration in 3 days when taken 1 time per day 1 . Suvorexant is actively bound to plasma proteins (more than 99%). It can be taken with or without food, however, to achieve a faster onset of sleep, the drug should not be taken during or immediately after a meal, as its effect may come later.
Unlike benzodiazepines, which activate GABA receptors and have associated side effects such as visual hallucinations, memory problems, drug addiction, and aftereffect syndrome, suvorexant is believed to selectively reversibly block orexin neurons, affecting only the wakefulness system. and reducing the risk of developing complications that are characteristic of other hypnotics that affect the sleep system [32]. This drug has a linear pharmacokinetics, its maximum plasma concentration is reached on average 2 hours after administration, the half-life is about 12 hours. The drug reaches a stationary concentration in 3 days when taken 1 time per day 1 . Suvorexant is actively bound to plasma proteins (more than 99%). It can be taken with or without food, however, to achieve a faster onset of sleep, the drug should not be taken during or immediately after a meal, as its effect may come later.
Animal studies (rodents, dogs, Rhesus macaques) [33-36] have shown the ability of suvorexant to reduce the time of active wakefulness and increase the duration of REM sleep and slow-wave activity. The delayed effects of these observations are not yet fully understood, but presumably have practical implications. nine0003
The delayed effects of these observations are not yet fully understood, but presumably have practical implications. nine0003
To date, four randomized, double-blind, placebo-controlled patient studies have demonstrated the efficacy and safety of suvorexant in the treatment of insomnia. The first clinical trials on the selection of effective doses of the drug were carried out by W. Herring et al. [37] in 2012 in adult patients (18–64 years of age) who received one of 4 doses of the drug for 4 weeks and then placebo for the next 4 weeks. This regimen was designed to allow for a one-week washout period between the 2 phases of the clinical trial. The primary endpoint was sleep efficiency, calculated as total sleep time divided by total time spent in bed (minutes). The second endpoint included time spent awake after sleep onset and time to fall asleep. The results showed a significant dose-dependent improvement in both measures during treatment with suvorexant compared with placebo ( p = 0. 001). Side effects were dose dependent but minimal. The most common adverse event (AE) was somnolence, which was registered in 1.6-11.5% of patients taking different doses of suvorexant. In 2016, the same authors conducted a phase III [38] study of suvorexant, in which patients with insomnia of two age groups took part for 3 months: 18–64 years and older than 65 years. Suvorexant 20/15 mg was shown to improve sleep quality and symptoms of insomnia by questionnaires and repeat polysomnography (PSG), in contrast to placebo. Also, a 3-month course of taking the drug showed the greatest efficiency. At the same time, after a sharp cessation of taking suvorexant, there was no exacerbation of insomnia and / or withdrawal syndrome even after 3-6 months. There was no significant effect of the drug on the emotional sphere. The main side effect was daytime sleepiness, which resolved after 7–30 days of treatment [38]. nine0003
001). Side effects were dose dependent but minimal. The most common adverse event (AE) was somnolence, which was registered in 1.6-11.5% of patients taking different doses of suvorexant. In 2016, the same authors conducted a phase III [38] study of suvorexant, in which patients with insomnia of two age groups took part for 3 months: 18–64 years and older than 65 years. Suvorexant 20/15 mg was shown to improve sleep quality and symptoms of insomnia by questionnaires and repeat polysomnography (PSG), in contrast to placebo. Also, a 3-month course of taking the drug showed the greatest efficiency. At the same time, after a sharp cessation of taking suvorexant, there was no exacerbation of insomnia and / or withdrawal syndrome even after 3-6 months. There was no significant effect of the drug on the emotional sphere. The main side effect was daytime sleepiness, which resolved after 7–30 days of treatment [38]. nine0003
In 2014, the results of the work of D. Michelson et al. were published. [39]. The study involved patients younger than 65 years of age who took suvorexant at two different doses for 1 year, including a 2-month washout period of the drug from the body, in order to identify withdrawal syndrome and rebound phenomena. The results of the study showed that these phenomena did not develop after discontinuation of the drug. In the suvorexant group, there was a significant increase in total sleep duration compared to placebo (38.7 min vs. 16 min; 95% CI 16.4–29.0; p = 0.0001). Also, compared with the placebo group, the suvorexant group reduced the duration of falling asleep from 18 to 8.4 minutes (95% CI 14.6–4.5, p = 0.0002). In 2016, the authors [40] evaluated the effects of long-term use of suvorexant (for 1 year) in patients with insomnia. It was noted that suvorexant was well tolerated by patients and had a favorable safety profile. In a small percentage of patients, AEs in the form of hallucinations associated with sleep and sleep paralysis were noted, which is generally characteristic of the use of sedative hypnotics as well.
[39]. The study involved patients younger than 65 years of age who took suvorexant at two different doses for 1 year, including a 2-month washout period of the drug from the body, in order to identify withdrawal syndrome and rebound phenomena. The results of the study showed that these phenomena did not develop after discontinuation of the drug. In the suvorexant group, there was a significant increase in total sleep duration compared to placebo (38.7 min vs. 16 min; 95% CI 16.4–29.0; p = 0.0001). Also, compared with the placebo group, the suvorexant group reduced the duration of falling asleep from 18 to 8.4 minutes (95% CI 14.6–4.5, p = 0.0002). In 2016, the authors [40] evaluated the effects of long-term use of suvorexant (for 1 year) in patients with insomnia. It was noted that suvorexant was well tolerated by patients and had a favorable safety profile. In a small percentage of patients, AEs in the form of hallucinations associated with sleep and sleep paralysis were noted, which is generally characteristic of the use of sedative hypnotics as well. The study did not assess daily productivity or quality of life and work using objective tests. However, the patients did not complain of driving difficulties or emotional lability. nine0003
The study did not assess daily productivity or quality of life and work using objective tests. However, the patients did not complain of driving difficulties or emotional lability. nine0003
In August 2014, US Food and Drug Administration (FDA) 2 approved 5, 10, 15 and 20 mg suvorexant under the brand name Belsomra. Since 2016 Belsomra (suvorexant) has been registered in Japan, Australia and Russia. In Russia, the drug is registered for the treatment of insomnia characterized by difficulty falling asleep and / or maintaining sleep in dosages of 20 mg for patients under 65 years of age, 15 mg for patients 65 years of age and older. nine0003
For patients taking inhibitors of cytochrome P 450 3A (ketoconazole, clarithromycin, ritonavir, etc.), the recommended dose of suvorexant is 10 mg (5 mg starting dose). For patients taking cytochrome P stimulants 450 3A (rifampicin, phenytoin, carbamazepine), a higher dose of suvorexant may be required. Co-administration with other sedative drugs is strictly prohibited.
Co-administration with other sedative drugs is strictly prohibited.
The presented data allow us to declare a new direction in the treatment of various nosological forms associated with a violation of the mechanisms of regulation of the orexin system. The pleiotropy of orexin is the key to a broad approach to its clinical use. Undoubtedly, a very important practical direction is the relief of sleep disorders using the synthetic orexin receptor antagonist suvorexant. The results of clinical studies show that suvorexant accelerates falling asleep, reduces the number of nocturnal awakenings, lengthens the total time of sleep and improves its efficiency. Upon discontinuation of suvorexant, withdrawal syndrome and rebound insomnia are not observed. nine0003
The use of the drug will improve the quality of life of a significant number of patients suffering from sleep disorders. In addition, the multidimensional nature of the problem of insomnia disorders, presented through the diversity of neuromorphological and neurohumoral connections, should force physicians to consider insomnia disorders more widely, from a multidisciplinary position, and use the entire arsenal of tools, including both new drug directions and non-drug options for correcting widespread and difficult to treat diseases.