What is acute mania
What Is It, Causes, Triggers, Symptoms & Treatment
Overview
What is mania?
Mania is a condition in which you have a period of abnormally elevated, extreme changes in your mood or emotions, energy level or activity level. This highly energized level of physical and mental activity and behavior must be a change from your usual self and be noticeable by others.
What's considered an “abnormal,” extreme change in behavior and what does it look like?
Abnormal manic behavior is behavior that stands out. It’s over-the-top behavior that other people can notice. The behavior could reflect an extreme level of happiness or irritation. For example, you could be extremely excited about an idea for a new healthy snack bar. You believe the snack could make you an instant millionaire but you’ve never cooked a single meal in your life, don’t know a thing about how to develop a business plan and have no money to start a business. Another example might be that you strongly disagree with a website “influencer” and not only write a 2,000 word post but do an exhaustive search to find all the websites connected to the influencer so you can post your letter there too.
Although these examples may sound like they could be normal behavior, a person with mania will expend a great deal of time and energy including many sleepless nights working on projects such as these.
What is a manic episode?
A manic episode is a period of time in which you experience one or more symptoms of mania and meet the criteria for manic episode (see “symptoms” and “diagnosis” sections). In some cases, you may need to be hospitalized.
Can I have a manic episode as its own condition or is it always part of another mental health condition?
Technically if you have a manic episode, you have a mental health condition. Mania can be a part of several mental health conditions including:
- Bipolar I disorder (most common condition for mania to occur).
- Seasonal affective disorder.
- Postpartum psychosis.
- Schizoaffective disorder.
- Cyclothymia.
What is bipolar I disorder?
Bipolar I disorder is a mental health illness in which a person has major high and low swings in mood, activity, energy and ability to think clearly. To be diagnosed with bipolar I disorder, you have to have at least one episode of mania that lasts for at least seven days or have an episode that is so severe that it requires hospitalization.
To be diagnosed with bipolar I disorder, you have to have at least one episode of mania that lasts for at least seven days or have an episode that is so severe that it requires hospitalization.
Most people have both episodes of both mania and depression, but you don’t have to have depression to be diagnosed with mania. Many people with a bipolar I disorder diagnosis have recurring, back-to-back manic episodes with very few episodes of depression.
What are the triggers of manic episodes?
Manic episode triggers are unique to each person. You’ll have to become a bit of a detective and monitor your mood (even keeping a “mood diary”) and start to track how you feel before an episode and when it occurs. Ask family and close friends who you trust and have close contact with to help identify your triggers. As outside observers, they may notice changes from your usual behavior more easily than you do.
Knowing your triggers can help you prepare for an episode, lessen the effect of an episode or prevent it from happening at all.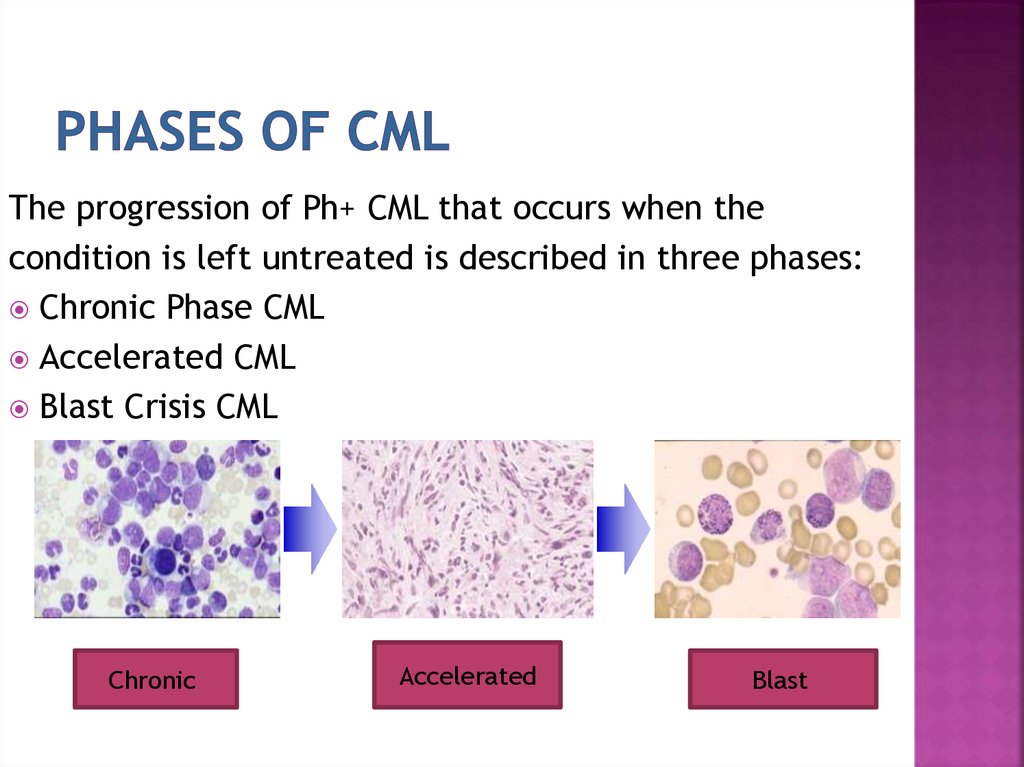
Common triggers to be aware of include:
- A highly stimulating situation or environment (for example, lots of noise, bright lights or large crowds).
- A major life change (such as divorce, marriage or job loss).
- Lack of sleep.
- Substance use, such as recreational drugs or alcohol.
What happens after a manic episode?
After a manic episode you may:
- Feel happy or embarrassed about your behavior.
- Feel overwhelmed by all the activities you’ve agreed to take on.
- Have only a few or unclear memories of what happened during your manic episode.
- Feel very tired and need sleep.
- Feel depressed (if your mania is part of bipolar disorder).
Symptoms and Causes
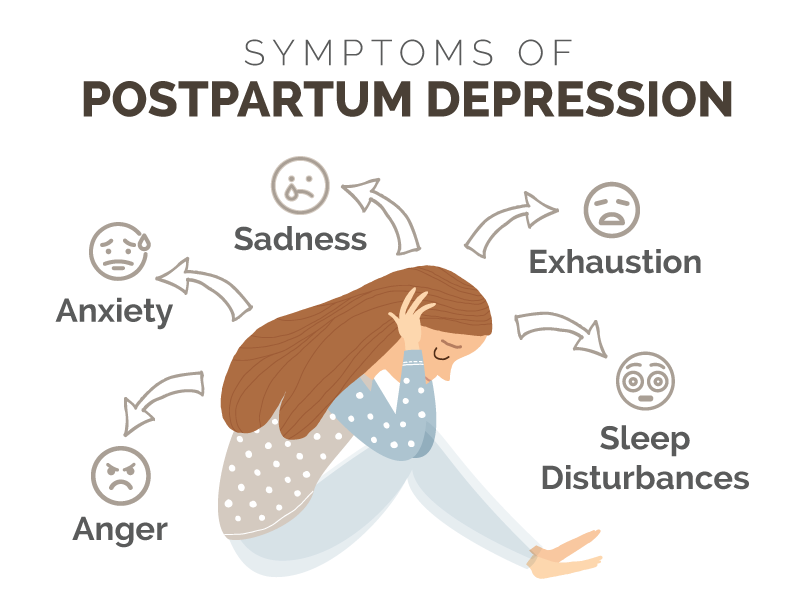
What are the symptoms of mania?
Symptoms of a manic episode
- Having an abnormally high level of activity or energy.
- Feeling extremely happy or excited — even euphoric.
- Not sleeping or only getting a few hours of sleep but still feeling rested.
- Having an inflated self-esteem, thinking you’re invincible.
- Being more talkative than usual. Talking so much and so fast that others can’t interrupt.
- Having racing thoughts — having lots of thoughts on lots of topics at the same time (called a “flight of ideas”).
- Being easily distracted by unimportant or unrelated things.
- Being obsessed with and completely absorbed in an activity.
- Displaying purposeless movements, such as pacing around your home or office or fidgeting when you’re sitting.
- Showing impulsive behavior that can lead to poor choices, such as buying sprees, reckless sex or foolish business investments.
Psychotic symptoms of a manic episode
- Delusions. Delusions are false beliefs or ideas that are incorrect interpretations of information. An example is a person thinking that everyone they see is following them.
- Hallucinations. Having a hallucination means you see, hear, taste, smell or feel things that aren’t really there.
 An example is a person hearing the voice of someone and talking to them when they’re not really there.
An example is a person hearing the voice of someone and talking to them when they’re not really there.
How long does a manic episode last?
Early signs (called “prodromal symptoms”) that you’re getting ready to have a manic episode can last weeks to months. If you’re not already receiving treatment, episodes of bipolar-related mania can last between three and six months. With effective treatment, a manic episode usually improves within about three months.
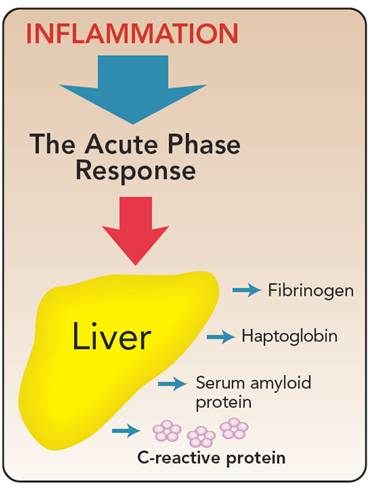
What causes mania?
Scientists aren’t completely sure what causes mania. However, there are several factors that are thought to contribute. Causes differ from person to person.
Causes may include:
- Family history. If you have a family member with bipolar illness, you have an increased chance of developing mania. This isn't definite though. You may never develop mania even if other family members have.
- A chemical imbalance in the brain.
- A side effect of a medication (such as some antidepressants), alcohol or recreational drugs.
- A significant change in your life, such as a divorce, house move or death of a loved one.
- Difficult life situations, such as trauma or abuse, or problems with housing, money or loneliness.
- A high level of stress and an inability to manage it.
- A lack of sleep or changes in sleep pattern.
- As a side effect of mental health problems including seasonal affective disorder, postpartum psychosis, schizoaffective disorder or other physical or neurologic condition such as brain injury, brain tumors, stroke, dementia, lupus or encephalitis.
Diagnosis and Tests
How is mania diagnosed?
Your healthcare provider will ask about your medical history, family medical history, current prescriptions and non-prescription medications and any herbal products or supplements you take. Your provider may order blood tests and body scans to rule out other conditions that may mimic mania. One such condition is hyperthyroidism. If other diseases and conditions are ruled out, your provider may refer you to a mental health specialist
To be diagnosed with mania, your mental health specialist may follow the criteria of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, DSM-5. Their criteria for manic episode is:
Their criteria for manic episode is:
- You have an abnormal, long-lasting elevated expression of emotion along with a high degree of energy and activity that lasts for at least one week and is present most of the day, nearly every day.
- You have three or more symptoms to a degree that they’re a noticeable change from your usual behavior (four symptoms if mood is only irritable). (See the symptoms section of this article for a list of the symptoms used as criteria.)
- The mood disturbance is severe enough to cause significant harm to your social, work or school functioning or there’s a need to hospitalize you to prevent you from harming yourself or others, or you have psychotic features, such as hallucinations or delusions.
- The manic episode can’t be caused by the effects of a substance (medications or drug abuse) or another medical condition.
Management and Treatment
How is mania treated?
Mania is treated with medications, talk therapy, self-management and family and friends support.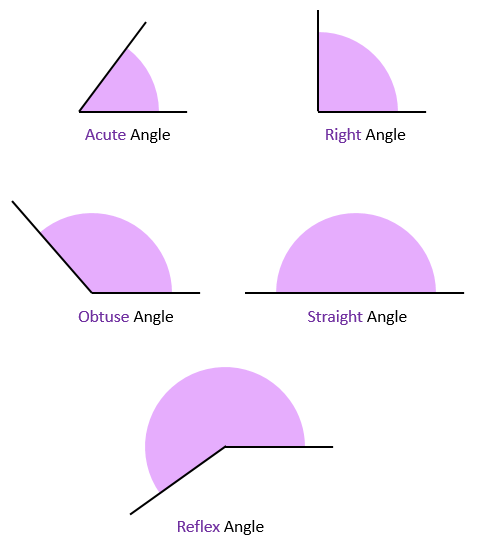
Medications
If you have mania only, your healthcare provider may prescribe an antipsychotic medication, such as ariprazole (Abilify®), lurasidone (Latuda®), olanzapine (Zyprexa®), quetiapine (Seroquel®) or risperridone (Risperdal®).
If you have mania as part of a mood disorder, your provider may add a mood stabilizer. Some examples include lithium, valproate (Depakote®) and carbamazepine (Tegretol®). (If you’re pregnant or plan to become pregnant, let your provider know. Valproate can increase the chance of birth defects and learning disabilities and shouldn’t be prescribed to individuals who are able to become pregnant.)
Sometimes antidepressants are also prescribed.
Talk therapy (psychotherapy)
- Psychotherapy involves a variety of techniques. During psychotherapy, you’ll talk with a mental health professional who'll help you identify and work through factors that may be triggering your mania and/or depression (if you’re diagnosed with bipolar I disorder).
- Cognitive behavioral therapy can be useful in helping you change inaccurate perceptions that you have about yourself and the world around you.
- Family therapy is important since it’s very helpful for your family members to understand your behavior and what they can do to help.
Ask your provider for contact information for local support groups. You might find it helpful to talk with other people who have similar medical experiences and share problems, ideas for coping and strategies for living and caring for yourself.
Other treatments
Electroconvulsant therapy (ECT) may be considered in rare cases in individuals who have severe mania or depression (if bipolar). ECT involves applying brief periods of electric current to your brain.
Prevention
What steps can I take to better cope with or manage my mania?
Although episodes of mania can’t always be prevented, you can make a plan to better manage your symptoms and prevent them from getting worse when you feel a manic episode may be starting.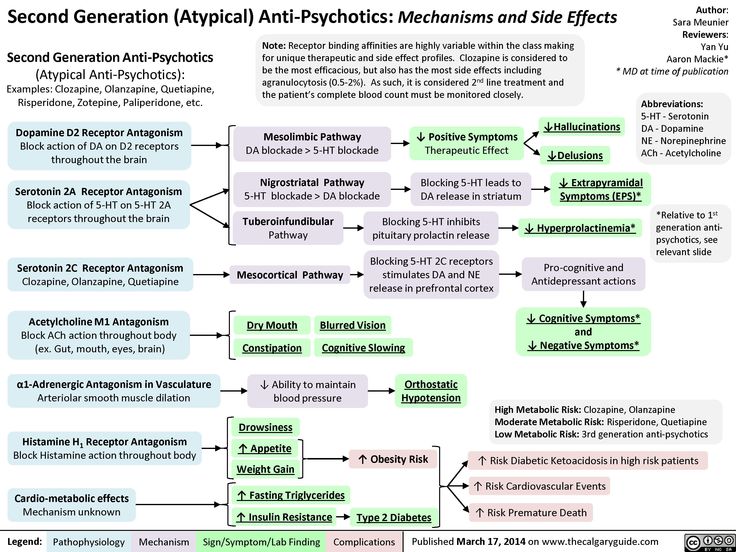
Some ideas to try during this time include:
- Avoid stimulating activities and environment – such as loud or busy places or bright places. Instead choose calm and relaxing activities and environments.
- Stick to routines. Go to bed at a set time, even if you’re not tired. Also, stick to the same times for eating meals, taking medications and exercising.
- Limit the number of social contacts to keep you from getting too stimulated and excited.
- Postpone making any major life decisions and big purchases.
- Avoid people and situations that might tempt you to make poor or risky choices, such as taking recreational drugs or drinking alcohol.
- Consider selecting someone to manage your finances during a manic episode.
If you ever have thoughts of harming yourself, tell family or friends, call you healthcare provider or contact the National Suicide Prevention Lifeline at 800-273-(TALK) (1-800-273-8255). Counselors are available 24/7.
Outlook / Prognosis
What outcome can I expect if I’ve been diagnosed with mania?
If your mania is related to a diagnosis of bipolar I disorder, this is a lifelong disease. Although there’s no cure for mania, medication and talk therapy (psychotherapy) can manage your condition in most cases.
Living With
How can I involve family and friends in understanding my mania?
It’s important to have an honest conversation with your family and closest friends.
- Let your family and friends know what you do and don’t find helpful. For example, if you’d appreciate a friendly reminder about taking your daily medications or a question about if you are getting enough sleep, let them know. On the other hand, if you don’t like always being asked if your current state of happiness is a sign you’re having a manic episode, discuss this.
- Ask your family and friends if they can help identify your triggers if you can’t. They may be able to spot triggers that you can’t spot yourself.
 Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change.
Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change. - Describe how your symptoms feel to you. Your family and friends will have a better understanding of your condition.
- Let family and friends know what type of help you’d like from them and when you’d like it. There may be times when you feel you can cope on your own. Knowing the difference will be helpful for everyone.
Frequently Asked Questions
What is acute mania?
Acute mania is the manic phase of bipolar I disorder. It is defined as an extremely unstable euphoric or irritable mood along with excess activity or energy level, excessively rapid thought and speech, reckless behavior and feeling of invincibility.
What is unipolar mania?
Unipolar mania is a disorder in which only excitement, excess activity or energy level and euphoric symptoms are seen. This is a rare condition.
What’s the difference between mania and hypomania?
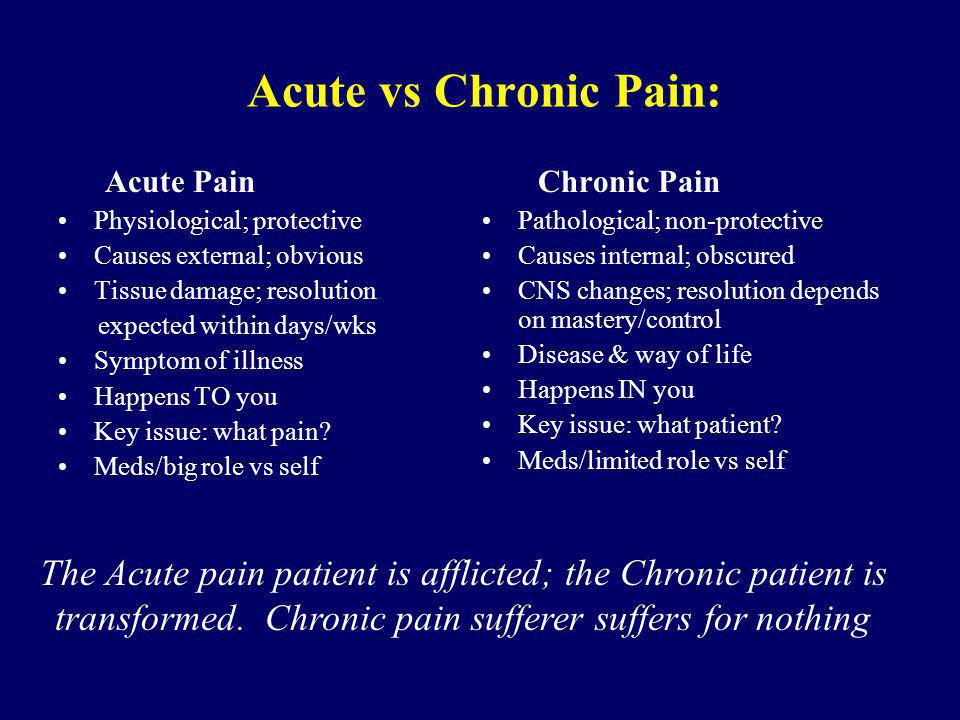
Hypomania is a less severe form of mania. The criteria that healthcare professionals use to make the diagnosis of either hypomania or mania is what sets them apart. The differences between these two conditions is as follows:
| Mania | Hypomania | |
|---|---|---|
| How long the episode lasts. | At least one week. | At least four consecutive days. |
| Severity of episode. | Causes severe impact on social or work/school functioning. | Not severe enough to significantly affect social or work/school functioning. |
| Need for hospitalization. | Possibly. | No. |
| Psychotic symptoms present (delusions or hallucinations). | Is among possible symptoms. | Can’t be present for a diagnosis of hypomania. |
Can my diagnosis change between bipolar I disorder and bipolar II disorder?
No. Once you have a diagnosis of bipolar I disorder — even if you never have another manic episode or a psychotic event (delusions or hallucinations) — your diagnosis can never be changed to bipolar II disorder. You’ll always have a bipolar I disorder diagnosis.
A note from Cleveland Clinic
Problems can develop in your social life, work/school functioning and home life when you have symptoms of mania, which include mood swings and an abnormal level of energy and activity. You may require hospitalization if you have severe hallucinations or delusions, or to prevent you from harming yourself or others. It’s important to have a good understanding of mania, mania symptoms, your particular triggers and ways to better manage your manic episodes. Medications, talk therapy and support groups as well as support from your family and friends can help manage your mania.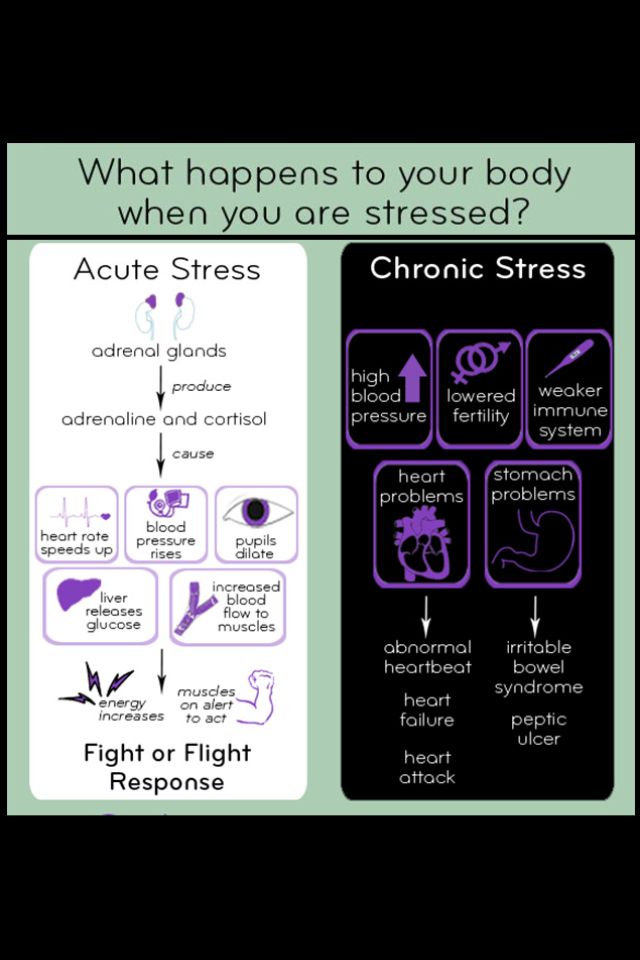 Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
What Causes A Manic Episode?
Learn more about what mania is, what causes it and how you can tell if you have it.
Mania is an extreme, elevated mood state. Someone in a state of mania may describe their sensory experiences as more vivid and pleasant and experience increases in energy and alertness.
Typically, mania is a symptom of bipolar disorder, a condition characterized by periods of mania called “manic episodes” that experienced periodically. In the past, people referred to bipolar disorder as “mania disorder,” since mania is one of the primary signs of bipolar disorder. While mania commonly occurs with bipolar disorder, other conditions and factors can also trigger episodes of mania.
Article at a Glance:
- A common bipolar disorder symptom is mania, an extremely elevated mood state with increased alertness and energy.

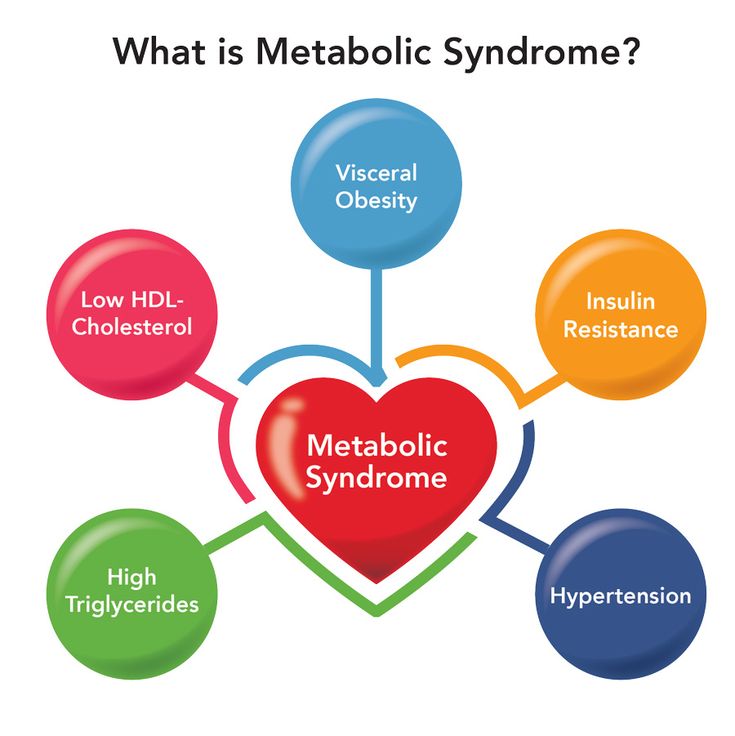
- There are three stages of mania: hypomania, acute mania and delirious mania.
- Classifications of mania are mixed states, hypomania and associated disorders.
- Mania can occur in cycles over several weeks or months with no predictable triggers.
- Treatment for mania is often part of bipolar disorder treatment and may involve therapy, hospitalization and medications.
What Is Mania?
Mania is a heightened mood state that causes hyperactivity and a decreased need for sleep. Other common features of mania include:
- Mood changes
- Sudden increases in energy and activity
- Rapid speech that is difficult or impossible to interrupt
- Impaired judgment
- Flighty thoughts or thoughts that jump from topic to topic
In more severe cases of mania, people may also experience hallucinations and delusions. Many people who suspect they or someone they love has mania may ask, “What is mania disorder?” Mania disorder is sometimes used as another term for bipolar disorder and is typically the reason that mania occurs. However, while bipolar disorder often causes mania, it is not the only reason that mania occurs.
However, while bipolar disorder often causes mania, it is not the only reason that mania occurs.
Stages of Mania
There are three stages of mania that may be experienced. People often first experience more mild forms of mania — like hypomania and acute mania — before progressing into a potentially dangerous delirious mania state.
- Hypomania (Stage I). Hypomania is a mild form of mania that may not be recognized as a significant symptom by those around the person experiencing it. While hypomania affects sleep and activity and may lead to increased impulsivity, it usually doesn’t require hospitalization or cause psychosis.
- Acute Mania (Stage II). During acute mania, an individual may experience increased impulsivity that causes them to act in a way that is brash, inappropriate or promiscuous. People with acute mania will also likely have increased energy, get little to no sleep and talk very quickly, often jumping from topic to topic.
 They may experience some symptoms of psychosis, where they are not fully aware of or connected to reality.
They may experience some symptoms of psychosis, where they are not fully aware of or connected to reality. - Delirious Mania (Stage III). Delirious mania is the most severe of the three stages of mania. Its symptoms are similar to acute mania, with the addition of delirium. Delirium is temporary confusion and a decreased ability or inability to connect with reality. This stage can also involve a combination of mania and psychosis. Because delirious mania can be profoundly disorienting, many people experiencing it need to be hospitalized to prevent injury to themselves or others.
Mania Classifications
In addition to the stages of mania, different classifications of mania are also used to describe the various types of mania. These include mixed state mania, hypomania and mania caused by associated disorders.
Mixed States
Mixed state mania is an episode of mania that includes either hypomania or mania and depressive symptoms. This state does not usually produce the same elevation in mood that mania would produce by itself. The depressive features of mixed state mania may increase the risk of suicidal ideation while also increasing energy and impulsivity, which further increases the likelihood of a suicide attempt.
The depressive features of mixed state mania may increase the risk of suicidal ideation while also increasing energy and impulsivity, which further increases the likelihood of a suicide attempt.
Hypomania
While hypomania is the first stage of mania, it is also a classification of mania. Those experiencing hypomania undergo significant changes in mood and may have disruptions in sleep, activity and impulsivity. The effects of hypomania, however, are not so severe that they will significantly impact people’s normal daily activities. Hypomania does not cause symptoms of psychosis, including hallucinations or a disconnect from reality.
Related Topic: Hypomanic treatment
Associated Disorders
Mania associated with bipolar disorder is not the only form of mania; there are also symptoms of other mental health conditions that mania mimics. Aside from bipolar disorder, other common causes of mania may include mania from other psychiatric conditions, mania due to an underlying medical condition — especially those that affect the thyroid — and mania caused by drugs or medications.
Many people wonder, “What does mania feel like?” There are multiple signs of mania that are experienced during a manic episode. These mania symptoms include:
- Increased energy
- Increased activity
- Significant changes in mood
- Decreased inhibition
- Flighty thought processes
- Extreme talkativeness
- Decreased sleep
The signs of bipolar mania include these manic episode symptoms over a prolonged period, normally for at least one week.
Causes of Mania
In any discussion about mania, people usually wonder, “What causes mania?” While there may be multiple causes of mania, the most common cause is bipolar disorder. Those with bipolar disorder tend to experience cycles of mania and depression over several weeks or months. In many cases, those with bipolar disorder don’t have any predictable mania triggers, making the onset of manic episodes unpredictable.
In addition to bipolar disorder, mania may also be caused by drugs or medications, especially stimulants. Certain other medical conditions, especially thyroid conditions or mental health diseases, may also cause episodes of mania.
Certain other medical conditions, especially thyroid conditions or mental health diseases, may also cause episodes of mania.
Diagnosing Mania
Any diagnosis for a psychological syndrome, such as mania, is done using specific criteria listed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). An individual must experience at least three of the following symptoms for at least a week to meet the criteria for bipolar disorder:
- Reduced need for sleep
- Increased rate of speech
- Being easily distracted
- Raised self-esteem
- Increased interest in goal-oriented activities
- Psychomotor agitation (such as pacing or hand-wringing)
- Increased pursuit of risky or dangerous activities
Mania Risk Factors
The most significant risk factors for mania are the risk factors for bipolar disorder, which commonly causes mania. These include having close relatives with bipolar disorder or having a history of substance abuse. Other risk factors of mania include using drugs recreationally or failing to treat underlying mental health conditions that may cause mania. Drug-induced mania is quite rare but is still something that may be experienced.
Other risk factors of mania include using drugs recreationally or failing to treat underlying mental health conditions that may cause mania. Drug-induced mania is quite rare but is still something that may be experienced.
Because there is such a strong relationship between bipolar and mania, most mania statistics are tied to bipolar disorder statistics. Most research seems to report that statistically, 0.4–1.6% of adults will have an episode of mania at some point in their lives. There is some more recent research that reports this rate may be as high as 5–7%.
Mania Treatment and Recovery
Typically, acute mania treatment is part of a broader bipolar disorder treatment. The initial focus is usually placed on the more short-term mania recovery so that the person suffering from the manic episode can resume normal activities. Mania management may involve hospitalization and therapy with a psychiatrist. Long-term treatment to address the symptoms of bipolar disorder typically involves continued therapy and medications, such as lithium, anticonvulsants and antipsychotics. While this may be the typical course of treatment for many people, each person’s situation is unique, and someone with specific questions should seek the advice of a doctor.
While this may be the typical course of treatment for many people, each person’s situation is unique, and someone with specific questions should seek the advice of a doctor.
If you or a loved one live with the symptoms of mania and addiction, consider reaching out to The Recovery Village. Call a representative today for more information.
If you’re experiencing symptoms of bipolar disorder, such as mania, the Nobu app is a great tool to to add to your treatment plan. It is free and for anyone that is looking to reduce anxiety, work through depression, build self-esteem, get aftercare following treatment, attend teletherapy sessions and so much more. Download the Nobu app today!
Editor – Megan Hull
Megan Hull is a content specialist who edits, writes and ideates content to help people find recovery. Read more
Medically Reviewed By – Benjamin Caleb Williams, RN
Benjamin Caleb Williams is a board-certified Emergency Nurse with several years of clinical experience, including supervisory roles within the ICU and ER settings.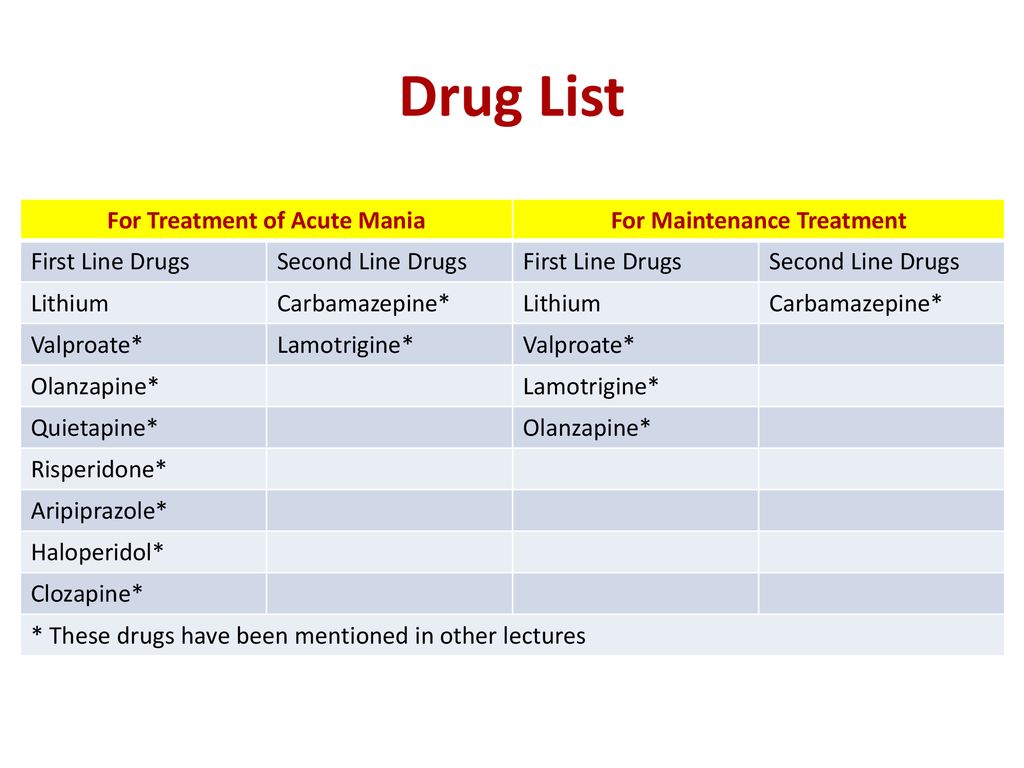 Read more
Read more
World Health Organization. “Mental and Behavioral Disorders.” March 6, 2003. Accessed May 11, 2019.
Reliawire. “What is Mania?” December 7, 2013. Accessed May 11, 2019.
Purse, Marcia. “Symptoms of Mania in Bipolar Disorder.” Very Well Mind, May 10, 2019. Accessed May 11, 2019.
Merck Manuals Professional Edition. “Some Causes of Symptoms of Depression and Mania.” 2019. Accessed May 11, 2019.
Yutzy, Sean H. et al. “The Increasing Frequency of Mania and Bipolar Disorder.” The Journal of Nervous and Mental Diseases, May 2012. Accessed May 11, 2019.
Vieta, Eduard. “Acute and Long-Term Treatment of Mania.” Dialogues in Clinical Neuroscience, June 2008. Accessed May 11, 2019.
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.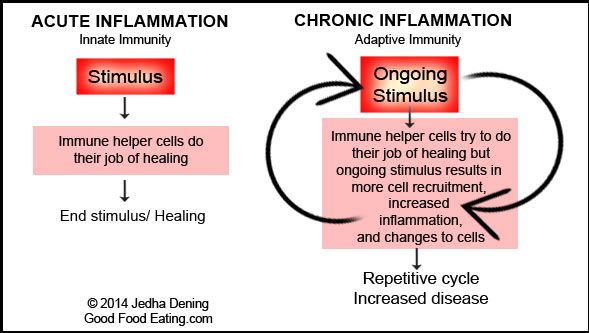 nine0003
nine0003
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. These may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life. nine0003
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode. nine0015 Cyclothymic disorder.
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke. nine0018
 You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression). Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time. nine0003
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy nine0015 Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others. The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons. nine0003
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons. nine0003
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships. nine0003
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Mania of persecution - causes of occurrence, in what diseases it occurs, diagnosis and methods of treatment
I confirm More nine0003
- INVITRO
- Library
- Symptoms
- Persecution mania
Stroke
19679 20 August
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0127 For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Mania of persecution: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
Definition
Persecution mania (delusions of persecution) is a mental disorder, which is expressed in a person's obsession about a threat to his own safety, about the presence of surveillance of him. No protection (isolation, relocation) saves such patients from delusional ideas. nine0003
Varieties of persecution mania
Mental disorders that manifest as delusions can vary significantly depending on the disease that caused them. Often, by the type and structure of delusions, one can draw a conclusion about the cause of its occurrence. Delirium can be systematized, logical , well linked to the environment. In these cases, it can be identified only by the obsession of the state. Such nonsense accompanies the formation of a new "I" in schizophrenia. Sometimes delirium wears fragmentary, unsystematized character and can be supplemented by illusory perception, pseudo-hallucinations ("pseudo" - because the patient understands that they are unreal) of certain "enemies", "spies" or "murderers", which is characteristic of acute alcoholic psychosis. Delirium may be accompanied by sensory sensations . So, for example, with an obsessive idea of the penetration of harmful creatures into the body, the patient feels their physical passage through the skin, mouth. With a combination of diseases that affect the patient's psyche, n application of delusional ideas. This is the case, for example, with alcoholic psychosis that occurs in patients with schizophrenia.
Delirium may be accompanied by sensory sensations . So, for example, with an obsessive idea of the penetration of harmful creatures into the body, the patient feels their physical passage through the skin, mouth. With a combination of diseases that affect the patient's psyche, n application of delusional ideas. This is the case, for example, with alcoholic psychosis that occurs in patients with schizophrenia.
Diseases in which delusions appear, or persecution mania
Organic vascular disease , which is accompanied by sclerotic changes, encephalopathy, stroke, quite often causes a change in the patient's personality. The clinical picture of such changes may be accompanied by the emergence of various psychoses and delusions. In addition, mental disorders are aggravated by age-related changes. Since the disorder is based on compensation and decompensation of brain nutrition, the clinical picture of the disease is periodic. nine0003
In the case of the habitual stereotype of life under standard loads, the patient copes with the situation, but with any deviations from the norm or the presentation of new requirements, psychosis may occur.
Along with depression, anxiety, they often coexist with delusional states: paranoia, auditory hallucinations. Psychoses are aggravated in the evening and at night and are accompanied by neurological disorders. Syndromes that develop against the background of vascular disorders may include manic, anxious, depressive components. It is possible to attach delusional ideas of persecution, especially if the patients' ability to analyze and abstract is sharply reduced. Therefore, the delirium of such persons is characterized by a rough structure and lack of logic. Most often they develop delusions of jealousy, poisoning and persecution mania. nine0003
With schizophrenia persecutory delusions are considered the most common. As a rule, this condition is observed in paranoid schizophrenia. In the analysis of delirium, its logic and good linkage with external circumstances are noted. Often delusions are supplemented by sensory sensations, especially if there is an obsession with poisoning. Patients feel a suspicious taste, burning, smell, which, in their opinion, indicate poisoning. Thus, the picture of delirium is characterized by complexity, the inclusion of various emotional components in the plot - “hints”, “insults”, “ridicule”. This developed "decoration" of persecution mania distinguishes the delirium in schizophrenia from the intoxication lesion in alcoholism. Intelligence in patients with schizophrenia does not suffer, which is also a characteristic feature of the disease. nine0003
Patients feel a suspicious taste, burning, smell, which, in their opinion, indicate poisoning. Thus, the picture of delirium is characterized by complexity, the inclusion of various emotional components in the plot - “hints”, “insults”, “ridicule”. This developed "decoration" of persecution mania distinguishes the delirium in schizophrenia from the intoxication lesion in alcoholism. Intelligence in patients with schizophrenia does not suffer, which is also a characteristic feature of the disease. nine0003
Often, the development of persecution mania is preceded by the appearance of an unmotivated fear of people and social phobia.
Such fear makes you avoid others, be afraid of people walking behind.
Persecution mania can develop in bipolar affective disorder - a mental illness, the symptom of which is the alternation of depression and manic episodes. Moreover, in women, the disease often begins with periods of depression, in men - with the development of mania. The period of depression is accompanied by tearfulness, despondency, complaints of lack of strength. Such patients are characterized by a violation of concentration, memory, and a decrease in cognitive abilities. After a while, depression is replaced by a manic syndrome. Despondency turns into excessive gaiety, talkativeness. A person makes many plans that remain unrealized. Self-control of one's condition in these two phases of the disease changes significantly. During depression, patients tend to be aware that there is no reason for such a condition and seek medical help, while during a manic period, self-criticism decreases, and any advice to visit a doctor is perceived extremely negatively. Psychotic symptoms are a characteristic feature of bipolar disorder. During the depressive phase, delusions of guilt or hypochondriacal delusions (confidence in the violation of the state of one's body) may form. During the manic phase, inflated self-esteem leads to the formation of delusions of grandeur, and lack of criticality and suspicion develop into delusions of persecution.
The period of depression is accompanied by tearfulness, despondency, complaints of lack of strength. Such patients are characterized by a violation of concentration, memory, and a decrease in cognitive abilities. After a while, depression is replaced by a manic syndrome. Despondency turns into excessive gaiety, talkativeness. A person makes many plans that remain unrealized. Self-control of one's condition in these two phases of the disease changes significantly. During depression, patients tend to be aware that there is no reason for such a condition and seek medical help, while during a manic period, self-criticism decreases, and any advice to visit a doctor is perceived extremely negatively. Psychotic symptoms are a characteristic feature of bipolar disorder. During the depressive phase, delusions of guilt or hypochondriacal delusions (confidence in the violation of the state of one's body) may form. During the manic phase, inflated self-esteem leads to the formation of delusions of grandeur, and lack of criticality and suspicion develop into delusions of persecution. nine0003
nine0003
Epilepsy that develops in children can also be accompanied by persecution mania. The clinical picture of the disease is characterized not only by the occurrence of repeated spontaneous seizures, but also by various neurological and mental personality changes. Patients with epilepsy are characterized, on the one hand, by a tendency to the viscosity of thinking, and on the other, impulsiveness.
Epileptics often show egocentrism, obsession with their needs, excessive attention to their health, cruelty and aggressiveness, and are in a depressed mood. nine0003
Mental disorders also include sensory, psychosensory and speech disorders, fears, sleep disturbance and disorientation. Among the delusional syndromes in children with epilepsy, there may be paranoid delirium with plots of persecution, excessive attention to one's health. Sometimes it can be mania, including hallucinations or ideas of fantastic events.
Delusions of persecution may be a manifestation of disease Bourneville-Pringle disease (tuberous sclerosis) - a genetically determined disease in which there is an overgrowth of the skin and blood vessels, damage to the nervous system and the growth of benign tumors in various organs. Clinical signs of the disease appear either from birth or in the first year of life. nine0003
Clinical signs of the disease appear either from birth or in the first year of life. nine0003
A characteristic skin symptom is hypomelanotic spots (discolored areas of the skin or a spot in the form of a leaf of a tree), which are observed in all patients in the second year of life.
Neurological symptoms include convulsive paroxysms. They cannot be controlled with anticonvulsant therapy and tend to be the main cause of disability. In the future, mental retardation and behavioral changes are detected.
The earlier epileptic seizures occur, the more severe mental retardation is. If the development of the nervous system is ahead of the pathological process, then various psychoses (fear, persecution mania, intrusive behavior) are more pronounced in patients. nine0003
Acute paranoid, which is manifested by delusions of persecution and hallucinations, occurs with alcohol and drug intoxication . In the subacute period of the disease, hallucinations are absent in patients, and the structure of mania becomes more ordered and logical. As a rule, against the background of isolation and suspiciousness, inexplicable attacks of fear and aggression occur in patients with alcoholism.
As a rule, against the background of isolation and suspiciousness, inexplicable attacks of fear and aggression occur in patients with alcoholism.
Which doctors to contact in case of persecution mania
It is very difficult to induce a patient who imagines surveillance or persecution to see a doctor. However, this must be done using a variety of reasons. If you can't overcome your fear of seeing a therapist or neurologist, you need to contact therapist or a pediatrician who can make a preliminary diagnosis. In some cases, consultation with a dermatologist and ophthalmologist may be required. nine0003
Diagnosis and examination of persecutory mania
Only a thorough examination of persons with persecutory obsession can help to make a correct diagnosis. The results of CT and MRI of the brain testify to vascular pathologies that can contribute to the development of delusions of persecution.
CT scan of the brain and skull
Scanning of the brain, skull and surrounding tissues, which allows diagnosing various pathologies. nine0003
nine0003
RUB 4,590 Sign up
MRI of the brain
Safe and informative scanning of brain structures for the diagnosis of its pathologies.
RUB 5,140 Sign up
The presence of foci of excitation in epilepsy is confirmed by echoencephalography. In addition, x-rays of the skull, CT and MRI of the brain are performed. nine0127 Diagnosis of Bourneville-Pringle disease includes x-rays of the chest, skull, hands and feet, electroencephalography, CT, MRI, and urinalysis.
Electroencephalography (EEG)
EEG is a safe and painless method for studying the functional state of the brain.
RUB 2,840 Sign up
Skull x-ray
X-ray examination of the skull to detect violations of the structure and integrity of the bones of the skull of various nature.
RUB 2,090 Sign up
CT scan of the brain and skull
Scanning of the brain, skull and surrounding tissues, which allows diagnosing various pathologies.
RUB 4,590 Sign up nine0003
MRI of the brain
Safe and informative scanning of brain structures for the diagnosis of its pathologies.
RUB 5,140 Sign up
X-ray of the thoracic spine
X-ray examination to assess the condition and structural integrity of the vertebrae.
RUB 2,440 Sign up nine0003
X-ray of the skull
X-ray examination of the skull to detect structural and integrity disorders of the skull bones of various nature.
RUB 2,090 Sign up
X-ray of the bones of the hand
X-ray examination of the bones of the hand is intended for the diagnosis of traumatic injuries, pathological changes, as well as the assessment of bone development ...
RUB 2,340 Sign up
X-ray of the bones of the foot
X-ray examination of the foot in two projections allows diagnosing injuries and other pathological changes, including flat feet.
RUB 2,340 Sign up nine0003
General urinalysis (Urine analysis with sediment microscopy)
Method of determination Determination of physical and chemical parameters is carried out on an automatic analyzer using the "dry chemistry" method.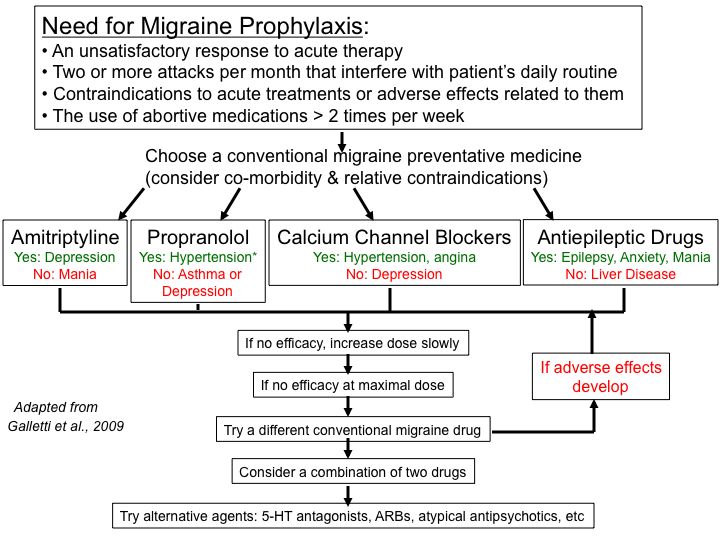 Hardware microscope...
Hardware microscope...
Up to 1 business day
Available with home visit
410 RUB nine0003
In garbage
Diagnosis of schizophrenia and alcoholic paranoid requires a careful medical history taking from the physician.
What to do in case of persecution mania
The main principle to be followed when detecting persecution mania is psychiatric alertness.
Communicating with such people should be as friendly as possible in order to prevent suicidal attempts and not provoke aggression. nine0003
Advice to visit a doctor can be justified by the presence of other diseases.
Treatment of persecutory mania
When treating patients with delusions of persecution, a systematic approach is necessary, since delusions are only one of the symptoms of an organic lesion of the central nervous system. Acute mental disorders require urgent medical attention, as they can provoke suicidal events. To stop the excitation, antipsychotics-antipsychotics are used. For patients with vascular lesions, the doctor may also prescribe drugs that improve blood circulation and brain nutrition. nine0003
Acute mental disorders require urgent medical attention, as they can provoke suicidal events. To stop the excitation, antipsychotics-antipsychotics are used. For patients with vascular lesions, the doctor may also prescribe drugs that improve blood circulation and brain nutrition. nine0003
Sources:
- The World Federation of Societies for Biological Psychiatry (WFSBP) Guidelines for the Biological Therapy of Schizophrenia / A. Hassan, P. Falkai, T. Wobrok et al. // Contemporary Therapy of Mental Disorders: Thematic Issue. – № 2, 2014.
- Studenikin V.M. Epilepsy in childhood // The attending physician. No. 5, 2015.
- Pringle-Bourneville disease: diagnostics at the intersection of disciplines / Kuklin I.A., Kenikfest Yu.V., Volkova N.V., Tolstaya A.I., Bochkarev Yu.M., Glazkova L.K., Rimar O. G., Krupina N.E. // Modern problems of dermatovenereology, immunology and medical cosmetology. No. 4, 2010. – P. 51–58. nine0018
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes. nine0003
Recommendations
-
Cholesterol plaques
6611 November 18th
-
Hepatic colic
4317 09 November
- nine0002 Laryngeal edema
3628 07 November
Show more
Stroke
Angina
nine0002 Parkinson's diseaseEsophageal dyskinesia
Tumor
Diverticulum
Dysphagia
Violation of the act of swallowing, or dysphagia, is due to the impossibility of passing the food bolus formed in the oral cavity through the oropharyngeal or pharyngeal-esophageal part into the stomach. nine0003
nine0003
More
Cerebral ischemia
Stroke
Cerebral infarction
Intoxication
nine0002 HeadacheConvulsions
Encephalopathy
Cerebral edema
Cerebral edema: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
More
nine0002 StrokeHypoxia
Traumatic brain injury
Dyslexia
Dyslexia: causes of occurrence, in what diseases it occurs, diagnosis and methods of treatment.
More
nine0002 EncephalitisMigraine
Meningitis
Stroke
Rabies
Brain tumor
Influenza
Conjunctivitis
Keratitis
Uveitis
Glaucoma
nine0002 Corneal ulcerPhotophobia
Photophobia (photophobia, photophobia, photophobia) - increased sensitivity of the eye to light (natural or artificial light), accompanied by discomfort, tearing and / or pain in the eyes.