What does mdd stand for
Major Depressive Disorder - StatPearls
Continuing Education Activity
Major depressive disorder (MDD) has been ranked as the third cause of the burden of disease worldwide in 2008 by WHO, which has projected that this disease will rank first by 2030. It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. This activity reviews the evaluation and management of major depressive disorder which is one of the main causes of disability in the world and highlights the role of the interprofessional team.
Objectives:
Identify the etiology of major depressive disorder.
Review the appropriate management of major depressive disorder.
Outline the typical presentation of a patient with major depressive disorder.
Review the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by major depressive disorder.
Access free multiple choice questions on this topic.
Introduction
Major depressive disorder (MDD) has been ranked as the third cause of the burden of disease worldwide in 2008 by WHO, which has projected that this disease will rank first by 2030.[1] It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. Per the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), an individual must have five of the above-mentioned symptoms, of which one must be a depressed mood or anhedonia causing social or occupational impairment, to be diagnosed with MDD. History of a manic or hypomanic episode must be ruled out to make a diagnosis of MDD. Children and adolescents with MDD may present with irritable mood.
History of a manic or hypomanic episode must be ruled out to make a diagnosis of MDD. Children and adolescents with MDD may present with irritable mood.
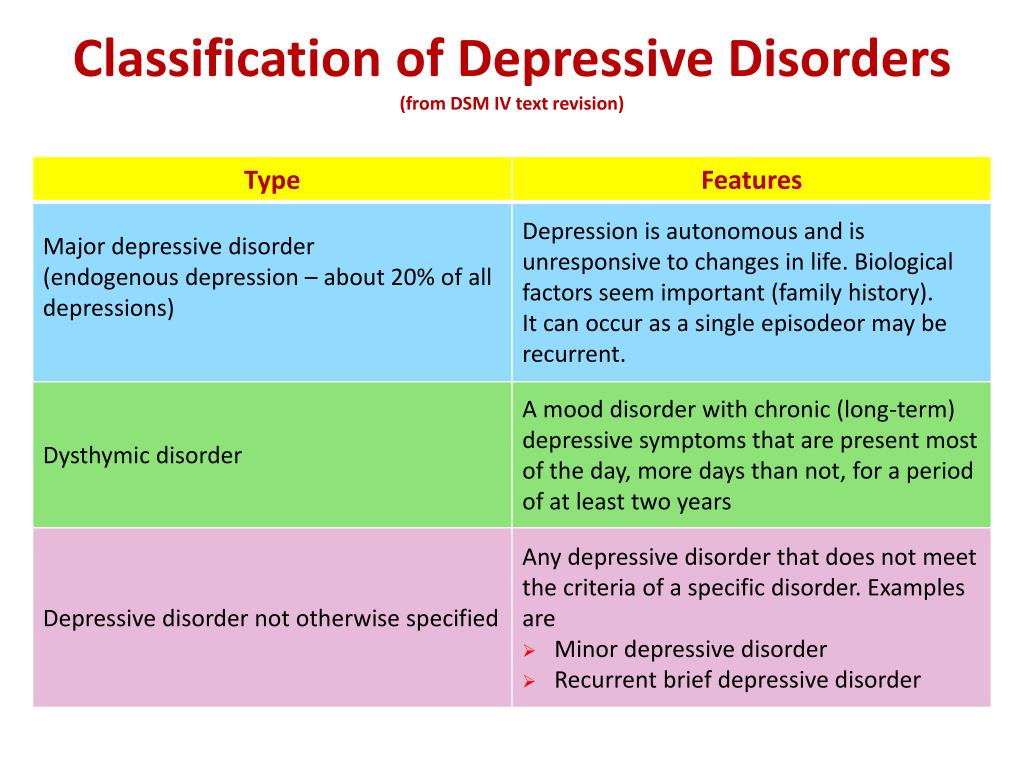
Per DSM-5, other types of depression falling under the category of depressive disorders are:
Persistent depressive disorder, formerly known as dysthymia
Disruptive mood dysregulation disorder
Premenstrual dysphoric disorder
Substance/medication-induced depressive disorder
Depressive disorder due to another medical condition
Unspecified depressive disorder
Etiology
The etiology of Major depressive disorder is believed to be multifactorial, including biological, genetic, environmental, and psychosocial factors. MDD was earlier considered to be mainly due to abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine. This has been evidenced by the use of different antidepressants such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, dopamine-norepinephrine receptor inhibitors in the treatment of depression. People with suicidal ideations have been found to have low levels of serotonin metabolites. However, recent theories indicate that it is associated primarily with more complex neuroregulatory systems and neural circuits, causing secondary disturbances of neurotransmitter systems.
People with suicidal ideations have been found to have low levels of serotonin metabolites. However, recent theories indicate that it is associated primarily with more complex neuroregulatory systems and neural circuits, causing secondary disturbances of neurotransmitter systems.
GABA, an inhibitory neurotransmitter, and glutamate and glycine, both of which are major excitatory neurotransmitters are found to play a role in the etiology of depression as well. Depressed patients have been found to have lower plasma, CSF, and brain GABA levels. GABA is considered to exert its antidepressant effect by inhibiting the ascending monoamine pathways, including mesocortical and mesolimbic systems. Drugs that antagonize NMDA receptors have been researched to have antidepressant properties. Thyroid and growth hormonal abnormalities have also been implicated in the etiology of mood disorders. Multiple adverse childhood experiences and trauma are associated with the development of depression later in life. [2][3]
[2][3]
Severe early stress can result in drastic alterations in neuroendocrine and behavioral responses, which can cause structural changes in the cerebral cortex, leading to severe depression later in life. Structural and functional brain imaging of depressed individuals has shown increased hyperintensities in the subcortical regions, and reduced anterior brain metabolism on the left side, respectively. Family, adoption, and twin studies have indicated the role of genes in the susceptibility of depression. Genetic studies show a very high concordance rate for twins to have MDD, particularly monozygotic twins.[4] Life events and personality traits have shown to play an important role, as well. The learned helplessness theory has associated the occurrence of depression with the experience of uncontrollable events. Per cognitive theory, depression occurs as a result of cognitive distortions in persons who are susceptible to depression.
Epidemiology
Major depressive disorder is a highly prevalent psychiatric disorder. It has a lifetime prevalence of about 5 to 17 percent, with the average being 12 percent. The prevalence rate is almost double in women than in men.[5] This difference has been considered to be due to the hormonal differences, childbirth effects, different psychosocial stressors in men and women, and behavioral model of learned helplessness. Though the mean age of onset is about 40 years, recent surveys show trends of increasing incidence in younger population due to the use of alcohol and other drugs of abuse.
It has a lifetime prevalence of about 5 to 17 percent, with the average being 12 percent. The prevalence rate is almost double in women than in men.[5] This difference has been considered to be due to the hormonal differences, childbirth effects, different psychosocial stressors in men and women, and behavioral model of learned helplessness. Though the mean age of onset is about 40 years, recent surveys show trends of increasing incidence in younger population due to the use of alcohol and other drugs of abuse.
MDD is more common in people without close interpersonal relationships, and who are divorced or separated, or widowed. No difference in the prevalence of MDD has been found among races and socioeconomic status. Individuals with MDD often have comorbid disorders such as substance use disorders, panic disorder, social anxiety disorder, and obsessive-compulsive disorder. The presence of these comorbid disorders in those diagnosed with MDD increases their risk of suicide. In older adults, depression is prevalent among those with comorbid medical illnesses. [6] Depression is found to be more prevalent in rural areas than in urban areas.
[6] Depression is found to be more prevalent in rural areas than in urban areas.
History and Physical
Major depressive disorder is a clinical diagnosis; it is mainly diagnosed by the clinical history given by the patient and mental status examination. The clinical interview must include medical history, family history, social history, and substance use history along with the symptomatology. Collateral information from a patient's family/friends is a very important part of psychiatric evaluation.
A complete physical examination, including neurological examination, should be performed. It is important to rule out any underlying medical/organic causes of a depressive disorder. A full medical history, along with the family medical and psychiatric history, should be assessed. Mental status examination plays an important role in the diagnosis and evaluation of MDD.
Evaluation
Although there is no objective testing available to diagnose depression, routine laboratory work including complete blood account with differential, comprehensive metabolic panel, thyroid-stimulating hormone, free T4, vitamin D, urinalysis, and toxicology screening is done to rule out organic or medical causes of depression.
Individuals with depression often present to their primary care physicians for somatic complaints stemming from depression, rather than seeing a mental health professional. In almost half of the cases, patients deny having depressive feelings, and they are often brought for treatment by the family or sent by the employer to be evaluated for social withdrawal and decreased activity. It is very important to evaluate a patient for suicidal or homicidal ideations at each visit.
In primary care settings, the Patient Health Questionnaire-9 (PHQ-9), which is a self-report, standardized depression rating scale is commonly used for screening, diagnosing, and monitoring treatment response for MDD.[7] The PHQ-9 uses 9 items corresponding to the DSM-5 criteria for MDD and also assesses for psychosocial impairment. The PHQ-9 scores 0 to 27, with scores of equal to or more than 10, indicate a possible MDD.
In most hospital settings, the Hamilton Rating Scale for Depression (HAM-D), which is a clinician-administered depression rating scale is commonly used for the assessment of depression. The original HAM-D uses 21 items about symptoms of depression, but the scoring is based only on the first 17 items.
The original HAM-D uses 21 items about symptoms of depression, but the scoring is based only on the first 17 items.
Other scales include the Montgomery-Asberg Depression Rating Scale (MADRS), the Beck Depression Inventory (BDI), the Zung Self-Rating Depression Scale, the Raskin Depression Rating Scale, and other questionnaires.
Treatment / Management
Major depressive disorder can be managed with various treatment modalities, including pharmacological, psychotherapeutic, interventional, and lifestyle modification. The initial treatment of MDD includes medications or/and psychotherapy. Combination treatment, including both medications and psychotherapy, has been found to be more effective than either of these treatments alone.[8][9] Electroconvulsive therapy is found to be more efficacious than any other form of treatment for severe major depression.[10]
FDA-approved medications for the treatment of MDD are as follows: All antidepressants are equally effective but differ in side-effect profiles.
Selective serotonin reuptake inhibitors (SSRIs) include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. They are usually the first line of treatment and the most widely prescribed antidepressants.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) include venlafaxine, duloxetine, desvenlafaxine, levomilnacipran, and milnacipran. They are often used for depressed patients with comorbid pain disorders.
Serotonin modulators are trazodone, vilazodone, and vortioxetine.
Atypical antidepressants include bupropion and mirtazapine. They are often prescribed as monotherapy or as augmenting agents when patients develop sexual side-effects due to SSRIs or SNRIs.
Tricyclic antidepressants (TCAs) are amitriptyline, imipramine, clomipramine, doxepin, nortriptyline, and desipramine.
Monoamine oxidase inhibitors (MAOIs) available are tranylcypromine, phenelzine, selegiline, and isocarboxazid.
 MAOIs and TCAs are not commonly used due to the high incidence of side-effects and lethality in overdose.
MAOIs and TCAs are not commonly used due to the high incidence of side-effects and lethality in overdose.Other medications include mood-stabilizers, antipsychotics which may be added to enhance antidepressant effects.
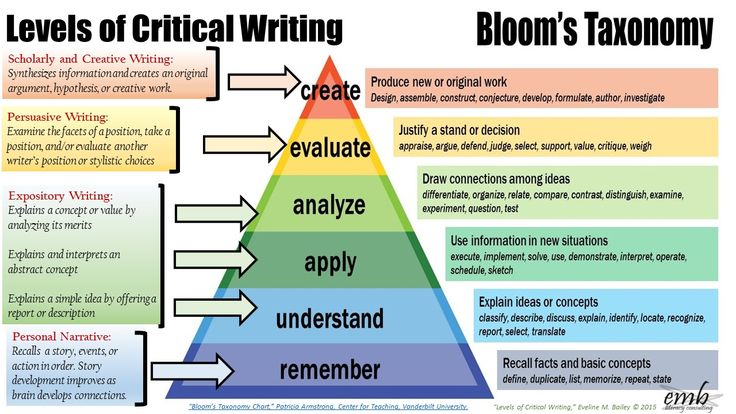
Psychotherapy
Cognitive-behavioral therapy
Interpersonal therapy
Electroconvulsive Therapy (ECT)
Acute suicidality
Severe depression during pregnancy
Refusal to eat/drink
Catatonia
Severe psychosis
Transcranial Magnetic Stimulation (TMS)
FDA-approved for treatment-resistant/refractory depression; for patients who have failed at least one medication trial
Vagus Nerve Stimulation (VNS)
FDA-approved as a long-term adjunctive treatment for treatment-resistant depression; for patients who have failed at least 4 medication trials
Esketamine
Nasal spray to be used in conjunction with an oral antidepressant in treatment-resistant depression; for patients who have failed other antidepressant medications
Differential Diagnosis
While evaluating for MDD, it is important to rule out depressive disorder due to another medical condition, substance/medication-induced depressive disorder, dysthymia, cyclothymia, bereavement, adjustment disorder with depressed mood, bipolar disorder, schizoaffective disorder, schizophrenia, anxiety disorders, and eating disorders for the appropriate management. Depressive symptoms can be secondary to the following causes:
Depressive symptoms can be secondary to the following causes:
Neurological causes such as cerebrovascular accident, multiple sclerosis, subdural hematoma, epilepsy, Parkinson disease, Alzheimer disease
Endocrinopathies such as diabetes, thyroid disorders, adrenal disorders
Metabolic disturbances such as hypercalcemia, hyponatremia
Medications/substances of abuse: steroids, antihypertensives, anticonvulsants, antibiotics, sedatives, hypnotics, alcohol, stimulant withdrawal
Nutritional deficiencies such as vitamin D, B12, B6 deficiency, iron or folate deficiency
Infectious diseases such as HIV and syphilis
Malignancies
Prognosis
Untreated depressive episodes in major depressive disorder can last from 6 to 12 months. About two-thirds of the individuals with MDD contemplate suicide, and about 10 to 15 percent commit suicide. MDD is a chronic, recurrent illness; the recurrence rate is about 50% after the first episode, 70% after the second episode, and 90% after the third episode. About 5 to 10 percent of the patients with MDD eventually develop bipolar disorder.[11] The prognosis of MDD is good in patients with mild episodes, the absence of psychotic symptoms, better treatment compliance, a strong support system, and good premorbid functioning. The prognosis is poor in the presence of a comorbid psychiatric disorder, personality disorder, multiple hospitalizations, and advanced age of onset.
About 5 to 10 percent of the patients with MDD eventually develop bipolar disorder.[11] The prognosis of MDD is good in patients with mild episodes, the absence of psychotic symptoms, better treatment compliance, a strong support system, and good premorbid functioning. The prognosis is poor in the presence of a comorbid psychiatric disorder, personality disorder, multiple hospitalizations, and advanced age of onset.
Complications
MDD is one of the leading causes of disability worldwide. It not only causes a severe functional impairment but also adversely affects the interpersonal relationships, thus lowering the quality of life. Individuals with MDD are at a high risk of developing comorbid anxiety disorders and substance use disorders, which further increases their risk of suicide. Depression can aggravate medical comorbidities such as diabetes, hypertension, chronic obstructive pulmonary disease, and coronary artery disease. Depressed individuals are at high risk of developing self-destructive behavior as a coping mechanism. MDD is often very debilitating if left untreated.
MDD is often very debilitating if left untreated.
Deterrence and Patient Education
Patient education has a profound impact on the overall outcome of major depressive disorder. Since MDD is one of the most common psychiatric disorders causing disability worldwide and people in different parts of the world are hesitant to discuss and seek treatment for depression due to the stigma associated with mental illness, educating patients is very crucial for their better understanding of the mental illness and better compliance with the mental health treatment. Family education also plays an important role in the successful treatment of MDD.
Enhancing Healthcare Team Outcomes
An interdisciplinary approach is essential for the effective and successful treatment of MDD. Primary care physicians and psychiatrists, along with nurses, therapists, social workers, and case managers, form an integral part of these collaborated services. In the majority of cases, PCPs are the first providers to whom individuals with MDD present mostly with somatic complaints. Depression screening in primary care settings is very imperative. The regular screening of the patients using depression rating scales such as PHQ-9 can be very helpful in the early diagnosis and intervention, thus improving the overall outcome of MDD. Psychoeducation plays a significant role in improving patient compliance and medication adherence. Recent evidence also supports that lifestyle modification, including moderate exercises, can help to improve mild-to-moderate depression. Suicide screening at each psychiatric visit can be helpful to lower suicide incidence. Since patients with MDD are at increased risk of suicide, close monitoring, and follow up by mental health workers becomes necessary to ensure safety and compliance with mental health treatment. The involvement of families can further add to a better outcome of the overall mental health treatment. Meta-analyses of randomized trials have shown that depression outcomes are superior when using collaborative care as compared with usual care.
Depression screening in primary care settings is very imperative. The regular screening of the patients using depression rating scales such as PHQ-9 can be very helpful in the early diagnosis and intervention, thus improving the overall outcome of MDD. Psychoeducation plays a significant role in improving patient compliance and medication adherence. Recent evidence also supports that lifestyle modification, including moderate exercises, can help to improve mild-to-moderate depression. Suicide screening at each psychiatric visit can be helpful to lower suicide incidence. Since patients with MDD are at increased risk of suicide, close monitoring, and follow up by mental health workers becomes necessary to ensure safety and compliance with mental health treatment. The involvement of families can further add to a better outcome of the overall mental health treatment. Meta-analyses of randomized trials have shown that depression outcomes are superior when using collaborative care as compared with usual care.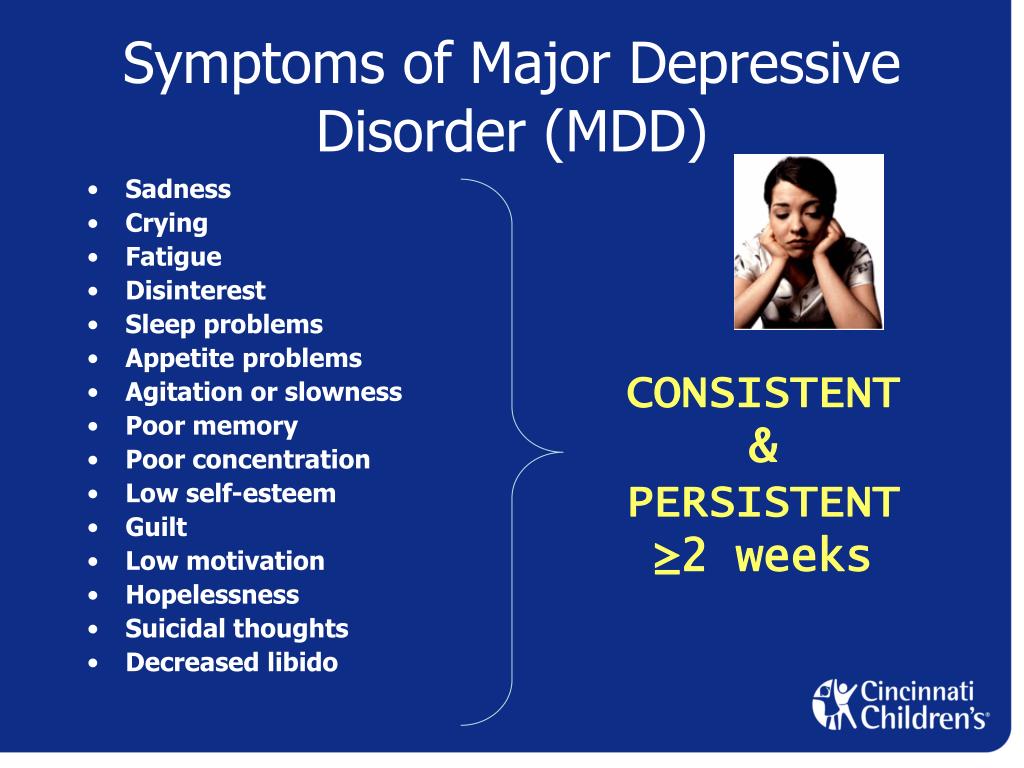 [12]
[12]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Malhi GS, Mann JJ. Depression. Lancet. 2018 Nov 24;392(10161):2299-2312. [PubMed: 30396512]
- 2.
Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, Gillespie CF, Berg T, Evces M, Newport DJ, Stowe ZN, Heim CM, Nemeroff CB, Schwartz A, Cubells JF, Ressler KJ. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008 Feb;65(2):190-200. [PMC free article: PMC2443704] [PubMed: 18250257]
- 3.
Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010 Feb;67(2):113-23. [PMC free article: PMC2822662] [PubMed: 20124111]
- 4.
Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000 Oct;157(10):1552-62. [PubMed: 11007705]
- 5.
Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, Mortensen PB, Eaton WW. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014 May;71(5):573-81. [PubMed: 24806211]
- 6.
Lyness JM, Niculescu A, Tu X, Reynolds CF, Caine ED. The relationship of medical comorbidity and depression in older, primary care patients. Psychosomatics. 2006 Sep-Oct;47(5):435-9. [PubMed: 16959933]
- 7.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003 Nov;41(11):1284-92. [PubMed: 14583691]
- 8.
Cuijpers P, Dekker J, Hollon SD, Andersson G. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis.
 J Clin Psychiatry. 2009 Sep;70(9):1219-29. [PubMed: 19818243]
J Clin Psychiatry. 2009 Sep;70(9):1219-29. [PubMed: 19818243]- 9.
Cuijpers P, van Straten A, Warmerdam L, Andersson G. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety. 2009;26(3):279-88. [PubMed: 19031487]
- 10.
Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J ECT. 2004 Mar;20(1):13-20. [PubMed: 15087991]
- 11.
Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, McGorry PD, Scott J, Berk M, Cotton SM. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. 2017 Apr;135(4):273-284. [PubMed: 28097648]
- 12.
Sighinolfi C, Nespeca C, Menchetti M, Levantesi P, Belvederi Murri M, Berardi D. Collaborative care for depression in European countries: a systematic review and meta-analysis.
 J Psychosom Res. 2014 Oct;77(4):247-63. [PubMed: 25201482]
J Psychosom Res. 2014 Oct;77(4):247-63. [PubMed: 25201482]
Depression (Major Depressive Disorder): Symptoms and More
Major depressive disorder (MDD), or clinical depression, is a common mood disorder that can affect anyone. Its most prevalent symptom includes persistent sadness or irritability.
Sadness is a natural part of the human experience. People may feel sad or depressed when a loved one passes away or when they’re going through a life challenge, such as a divorce or serious illness.
These feelings are usually short-lived. When someone experiences persistent and intense feelings of sadness for extended periods, then they may have a mood disorder such as major depressive disorder (MDD).
MDD, also referred to as clinical depression, is a significant medical condition that can affect many areas of your life. It impacts mood and behavior as well as various physical functions, such as appetite and sleep.
MDD is one of the most common mental health conditions in the United States. Data suggests that more than 8.4% of U.S. adults experienced a major depressive episode in 2020.
Data suggests that more than 8.4% of U.S. adults experienced a major depressive episode in 2020.
Some people with MDD never get treatment. However, most people with the disorder can learn to cope and function with treatment. Medications, psychotherapy, and other methods can effectively treat people with MDD and help them manage their symptoms.
When to seek emergency help
If you think you may hurt yourself or attempt to take your own life, call 911 or your local emergency number immediately.
You may also want to consider these options:
- Call a doctor or mental health professional.
- Call a suicide hotline, such as the 988 Suicide & Crisis Lifeline at 988. Use 988 and press “1” to reach the Veterans Crisis Line.
- Reach out to a close friend or loved one.
If you have a loved one who’s thinking about suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately.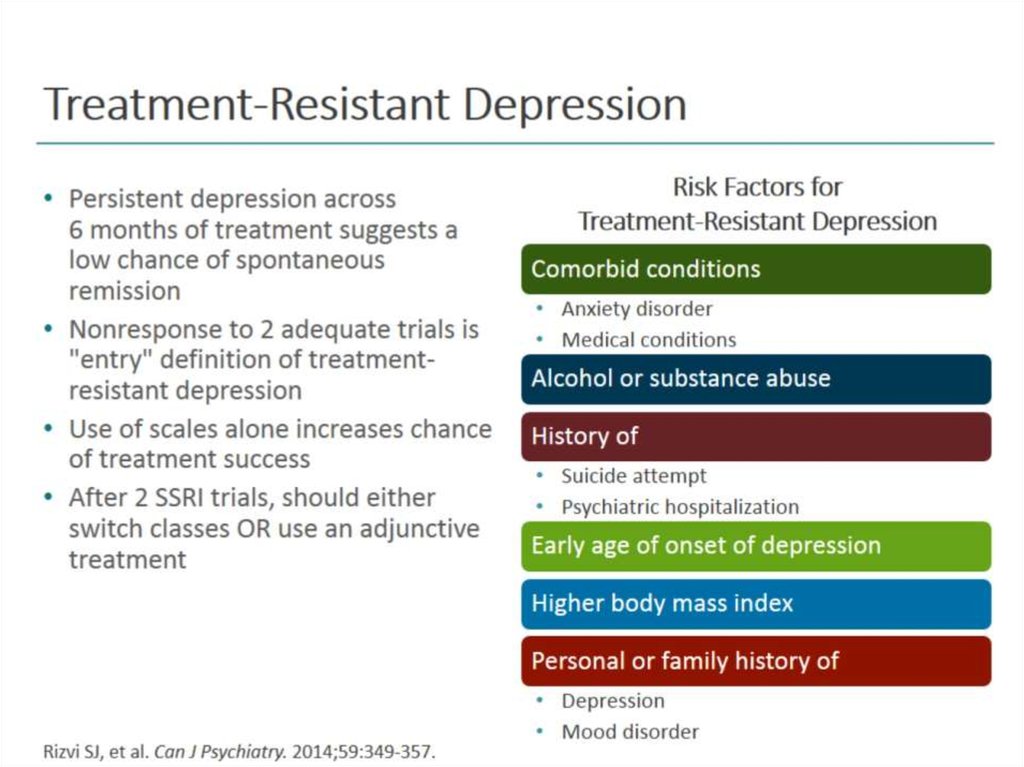 Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Types of depression
MDD is one type of depression. Other types include:
- Persistent depressive disorder
- Bipolar disorder
- Seasonal affective disorder
- Psychotic depression
- Peripartum (postpartum) depression
- Premenstrual dysphoric disorder
- Situational depression
- Atypical depression
- Treatment-resistant depression
A doctor or a mental health professional can diagnose MDD based on your symptoms, feelings, and behaviors.
Typically, you’ll be asked specific questions or given a questionnaire so health professionals can better determine whether you have MDD or another condition.
To be diagnosed with MDD, you need to meet the symptom criteria listed in the “Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).” This manual helps medical professionals diagnose mental health conditions.
According to its criteria:
- You must experience a change in your previous functioning.
- Symptoms must occur for a period of 2 or more weeks.
- At least one symptom is either depressed mood or loss of interest or pleasure.
You must also experience five or more of the following symptoms in the 2-week period:
- You feel sad or irritable most of the day, nearly every day.
- You’re less interested in most activities you once enjoyed.
- You suddenly lose or gain weight or have a change in appetite.
- You have trouble falling asleep or want to sleep more than usual.
- You experience feelings of restlessness.
- You feel unusually tired and have a lack of energy.
- You feel worthless or guilty, often about things that wouldn’t usually make you feel that way.
- You have difficulty concentrating, thinking, or making decisions.
- You think about harming yourself or suicide.
Symptoms in different age groups
Symptoms in teens
Symptoms parents should be aware of in their teens include the following:
- onset or increased use of substances (i.
 e., alcohol, smoking)
e., alcohol, smoking) - poorer academic performance
- problems with peers
- increased social withdrawal/isolation
Symptoms in older adults
Depression symptoms in older adults are similar to other age groups. It’s often the cause of physical pain in older adults that’s not explained by other medical conditions.
Depression is common in people with Alzheimer’s and related dementias. It’s sometimes called geriatric depression.
Older adults with one chronic health condition are 80% more at risk of developing depression than the average person, especially if their function becomes limited.
The exact cause of MDD isn’t known. However, several factors can increase your risk of developing the condition.
A combination of genes and stress can affect brain chemistry and lower your ability to maintain mood stability.
Changes in the balance of hormones might also contribute to the development of MDD.
MDD may also be triggered by:
- alcohol or drug use
- certain medical conditions, such as cancer or hypothyroidism
- particular types of medications, including steroids
- abuse during childhood
MDD is often treated with medication and psychotherapy. Some lifestyle adjustments can also help ease certain symptoms.
Some lifestyle adjustments can also help ease certain symptoms.
People who have severe MDD or have thoughts of harming themselves may need to stay in a hospital during treatment. Some might also need to take part in an outpatient treatment program until symptoms improve.
Medications
Primary care professionals often start treatment for MDD by prescribing antidepressant medications.
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs are a frequently prescribed type of antidepressant. SSRIs work by helping inhibit the breakdown of serotonin in your brain, resulting in higher amounts of this neurotransmitter.
Serotonin is a brain chemical that’s believed to be responsible for mood. It may help improve mood and produce healthy sleeping patterns.
People with MDD are often thought to have low levels of serotonin. An SSRI may relieve symptoms of MDD by increasing the amount of serotonin available in your brain.
SSRIs include well-known drugs such as fluoxetine (Prozac) and citalopram (Celexa). They have a relatively low incidence of side effects that most people tolerate well.
They have a relatively low incidence of side effects that most people tolerate well.
Similar to SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs) are another type of antidepressant that are often prescribed. These affect serotonin and norepinephrine, which helps manage your fight-or-flight response.
Other medications
Tricyclic antidepressants and medications known as atypical antidepressants, such as bupropion (Wellbutrin), may be used when other drugs haven’t helped.
These drugs can cause several side effects, including weight gain and sleepiness. As with any medication, benefits and side effects need to be weighed carefully with a healthcare professional.
Stopping medications immediately can cause withdrawal symptoms. It’s important not to stop taking your medications unless a mental health or healthcare professional advises you to.
Some medications used to treat MDD aren’t safe while you’re pregnant or nursing. Make sure you speak with a healthcare professional if you become pregnant, you’re planning to become pregnant, or you’re nursing.
Psychotherapy
Psychotherapy, also known as psychological therapy or talk therapy, can effectively treat people with MDD. It involves meeting with a mental health professional regularly to talk about your condition and related issues.
Psychotherapy can help you:
- adjust to a crisis or other stressful event
- working toward achieving a balanced perspective of a given situation and acting in accordance with values instead of based on mood
- improve your communication skills
- find better ways to cope with challenges and solve problems
- increase your self-esteem
- regain a sense of satisfaction and control in your life
A mental health professional may also recommend other types of therapy, such as cognitive behavioral therapy or interpersonal therapy. If you don’t already have a mental health professional, the Healthline FindCare tool can help you find a professional in your area.
Another possible treatment is group therapy, which allows you to share your feelings with people who can relate to what you’re going through.
Online therapy options
Read our review of the best online therapy options to find the right fit for you.
Lifestyle changes
In addition to taking medications and participating in therapy, you can help improve MDD symptoms by making some changes to your daily habits.
Dietary changes
Nutritious foods benefit your mind and body. While no foods can cure depression, certain healthful food choices can benefit your mental well-being.
Consider eating foods:
- containingomega-3 fatty acids, such as salmon
- rich in B vitamins, such as beans and whole grains
- withmagnesium, which is found in nuts, seeds, and yogurt
These can also be found in supplement form, but the Food and Drug Administration (FDA) hasn’t approved any natural products for depression. Speak with a healthcare professional before starting new supplements, especially if you take other medications.
Avoid alcohol and certain processed foods
It’s beneficial to avoid alcohol because it’s a nervous system depressant that worsens your symptoms. It has also been identified as a potential risk factor for depression.
It has also been identified as a potential risk factor for depression.
Ultra-processed foods have also been associated with depressive symptoms.
Get plenty of exercise
Although MDD can make you feel very tired, it’s essential to be physically active. Exercising, especially outdoors and in moderate sunlight, can boost your mood and make you feel better.
Sleep well
It’s vital to get enough sleep each night. This can vary from person to person but typically ranges between 7 to 9 hours.
People with depression often have trouble sleeping. Speak with a doctor if you’re having trouble sleeping or oversleeping.
SAMHSA’s National Helpline
The Substance Abuse and Mental Health Services Administration has a free, confidential helpline for people and family members of those facing substance misuse or mental health conditions. They’re available 24 hours a day at 1-800-662-HELP (4357).
While someone with MDD can feel hopeless at times, it’s important to remember that the disorder can be treated successfully. There is hope.
There is hope.
Sticking with a treatment plan is a critical part of improving your outlook. Try not to miss therapy sessions or follow-up appointments with your mental health professional.
Similarly, it’s important not to stop taking your medications unless a mental health or healthcare professional advises you to.
On days when you feel particularly depressed despite treatment, it can be helpful to call a local crisis or mental health service. Resources are available.
A friendly, supportive voice could be just what you need to get you through a difficult time.
Read this article in Spanish.
Suicidal thoughts
If you start taking antidepressants and have suicidal thoughts, call your doctor or 911 or local emergency services right away. Although it’s a rare occurrence, some MDD medications can cause suicidal thoughts in people who have just started treatment.
Talk with a doctor about concerns you may have about taking medications that pose this risk.
Duchenne/Becker muscular dystrophy - DNA diagnostics
Duchenne myodystrophy (DMD) is a hereditary disease that begins at the age of 2-5 years and is characterized by progressive muscle weakness, weakness, atrophy and pseudohypertrophy proximal muscles often 90.03 accompanied by cardiomyopathy and intellectual impairment. In the early stages of the disease, there is increased fatigue when walking, a change in gait (“duck gait”). In this case, there is a gradual degradation of muscle tissue. 95% of patients stop walking at the age of 8-12 years. At the age of 18-20 years, patients usually die, often from respiratory failure. There is an allelic form of DMD - Becker muscular dystrophy (BMD, OMIM 310200), which is characterized by similar clinical manifestations, a later onset (at about 10-16 years) and a milder course. Such patients often remain able to walk up to 20 years, and some - up to 50-60 years, although the same muscles are involved in the pathological process as in DMD. The life expectancy of such patients is reduced slightly.
The life expectancy of such patients is reduced slightly.
A biochemical marker of the disease is an increased (100-200) times the level of creatine phosphokinase ( CPK ) in the blood. In carriers of the damaged gene, the level of CPK is also slightly increased on average.
The mode of inheritance of Duchenne muscular dystrophy is X-linked recessive, i.e. it affects almost exclusively boys, while women with a damaged gene in one of the X chromosomes are carriers of DMD. But in rare cases, girls can also get Duchenne muscular dystrophy. The reasons for this may be the predominant inactivation of the X chromosome with a normal allele in heterozygous carriers of the mutant DMD gene, X-autosomal translocation affecting this gene, hemizygosity for the mutant allele, and the presence of phenocopies (diseases associated with a violation of other proteins included in the dystrophin-glycoprotein complex ). In approximately 2/3 of cases, the son receives a damaged chromosome from the carrier mother; in other cases, the disease occurs as a result of a de novo mutation in the germ cells of the mother or father, or in the precursors of these cells. Duchenne muscular dystrophy (DMD) occurs in approximately one in 2500-4000 newborn boys.
Duchenne muscular dystrophy (DMD) occurs in approximately one in 2500-4000 newborn boys.
The DMD gene responsible for progressive Duchenne/Becker muscular dystrophy (DMD/MDD) is located at the Xp21.2 locus and has a size of 2.6 million bp. and consists of 79 exons. In 60% of cases, mutations leading to DMD/MDD are extended deletions (from one to several tens of exons), in 30% of cases - point mutations, and in 10% of cases - duplications. Due to the presence of so-called "hot spots" of deletions, amplification of 27 exons and the promoter region of the DMD gene makes it possible to detect approximately 98% of all large deletions. The search for point mutations is difficult due to the large size of the gene and the absence of major mutations.
The Center for Molecular Genetics measures the level of CPK in the blood, as well as direct diagnosis of DMD/MDD, which is the search for large deletions/duplications in all exons of the DMD gene and the search for "point" mutations of the DMD gene using the NGS (next generation sequencing) method. An NGS study also makes it possible to detect deletions of all exons of the DMD gene in sick boys. Analysis of all exons of a gene makes it possible to determine the exact exon boundaries of a deletion in the event of its detection, and thus determine whether this deletion leads to a protein reading frame shift, which in turn is important for predicting the form of the disease - Duchenne or Becker myodystrophy. Thus, a combination of various research methods makes it possible to detect almost all mutations in the DMD gene.
An NGS study also makes it possible to detect deletions of all exons of the DMD gene in sick boys. Analysis of all exons of a gene makes it possible to determine the exact exon boundaries of a deletion in the event of its detection, and thus determine whether this deletion leads to a protein reading frame shift, which in turn is important for predicting the form of the disease - Duchenne or Becker myodystrophy. Thus, a combination of various research methods makes it possible to detect almost all mutations in the DMD gene.
The presence of any type of mutation (deletions/duplications in one or more exons, "point" mutations) is a molecular genetic confirmation of the clinical diagnosis of Duchenne/Becker myodystrophy and allows prenatal diagnosis in this family.
Attention! To measure the level of CPK, the blood must be fresh (not frozen)!
In the case of prenatal diagnosis, a fetal biomaterial is required, which can be used as chorionic villi (from the 8th to the 12th week of pregnancy), amniotic fluid (from the 16th to the 24th week of pregnancy) or umbilical cord blood (from 22 th week of pregnancy).
We have developed kits for DNA diagnostics of progressive Duchenne/Becker muscular dystrophy. The kits are intended for use in diagnostic laboratories of the molecular genetic profile.
When conducting prenatal (antenatal) DNA diagnostics for a specific disease, it makes sense to diagnose frequent aneuploidies (Down syndrome, Edwards syndrome, Shereshevsky-Turner syndrome, etc.) on the already existing fetal material, paragraph 54.1. The relevance of this study is due to the high total frequency of aneuploidy - about 1 per 300 newborns, and the absence of the need for repeated sampling of fetal material.
Publications on the topic of the section
Duchenne-Becker muscular dystrophy
Duchenne muscular dystrophy (muscular dystrophy) - ALL about the disease
Duchenne myodystrophy is a hereditary neuromuscular disease that manifests itself in boys and is characterized by progressive muscle weakness and fatigue, symmetrical pseudohypertrophy of the legs and symmetrical atrophy of other muscles in combination with osteoarticular deformities, cardiovascular and respiratory disorders. Duchenne muscular dystrophy has an X-linked recessive type of inheritance, the English abbreviation DMD is denoted as the name of the gene dystrophin , and the name of the disease is Duchenne muscular dystrophy.
Duchenne muscular dystrophy has an X-linked recessive type of inheritance, the English abbreviation DMD is denoted as the name of the gene dystrophin , and the name of the disease is Duchenne muscular dystrophy.
If you are a relative, doctor, or just know someone with Duchenne or Becker muscular dystrophy, please tell them about the MyMyo National Registry. In the Register, we combine data on all patients with DMD/BMD in Russia. The data will make it possible to collect statistics to argue the problems of a rare patient, which in turn will increase the level of argumentation in protecting the rights of people with Duchenne/Becker muscular dystrophy, help build a model of medical care, and therefore help such patients more and more efficiently.
Together we are stronger, join us!
Basic information about the disease
- This disease (previously the term Duchenne myopathy was often used) progresses rapidly.
 On average, at the age of 8-12 years, the ability to move independently occurs. Cardiomyopathy develops and cardiac and respiratory failure progresses.
On average, at the age of 8-12 years, the ability to move independently occurs. Cardiomyopathy develops and cardiac and respiratory failure progresses. - Corticosteroid therapy allows the patient to prolong the time of ability to move independently
- Proactive administration of ACE inhibitors and beta-blockers will help protect the heart
- Proper rehabilitation measures (use of technical rehabilitation aids (RTD) and physical management) can prevent early spinal curvature, chest deformity, and multiple large joint contractures.
Causes of Duchenne muscular dystrophy
Etiology and pathogenesis The DMD dystrophin gene is localized on the short arm of the X chromosome (Xp21.2–p21.1 locus). This is one of the largest human genes, which is why sporadic mutations occur so often in it (up to 40%). The disease in 60% of cases is inherited by boys from female carriers, as a typical X-linked recessive inheritance.
That's why we often say Duchenne is a boy's disease. Women have 2 X chromosomes, and if a gene breaks on one chromosome, the second will produce dystrophin.
The absence of dystrophin (as occurs in Duchenne muscular dystrophy) entails a violation of the integrity of the sarcolemma, the destruction of myocytes and their replacement with adipose and connective tissue. Clinically, this process is expressed by a progressive decrease in the ability of muscles to contract, loss of muscle strength and tone, and muscle atrophy.
The pathogenesis of Duchenne myodystrophy includes immunopathological processes. The process of regeneration is disturbed in the body, and almost immediately after birth, a cascade of inflammatory reactions is launched. Due to the resulting defect in the lipid layer of the sarcolemma, its permeability increases, which provokes rhabdomyolysis. Through the missing protective cell barrier, intracellular CPK enters the blood, and extracellular calcium enters myocytes.
Duchenne myopathy symptoms
Clinical disease cardThere are 5 stages of the disease.
| Stage | Description, features | |
|---|---|---|
| 1 | Presymptomatic | Increased levels of CPK, LDH, AST and ALT in a biochemical blood test. |
| 2 | Early (outpatient) The ability to move independently is preserved | Use of the Gowers technique when standing up, myopathic "duck" gait, walking on toes. The child climbs the steps with a side step and / or with support. |
| 3 | Late (outpatient) The ability to move independently is preserved | Increasing difficulty walking, loss of ability to climb stairs and get up from the floor. |
| 4 | Early (non-ambulatory) Lost the ability to move independently | The patient is able to move independently for some time, is able to maintain the position of the body. High risks of developing skeletal deformities, cardiomyopathy and respiratory disorders. |
| 5 | Late (non-ambulatory) Lost the ability to move independently | Increasing limitation of upper limb function, skeletal deformities, cardiomyopathy and respiratory disorders. Difficulty maintaining body position. Difficulty maintaining body position. |
Newborns with Duchenne may have no significant or noticeable abnormalities. Then, for the first months and even a year, the motor development of the child occurs within the normal range or with a slight delay. Up to 30% of patients in the first year of life have a lag in psychoverbal development. Also, these children, more often than the average in the population, are diagnosed with autism spectrum disorders.
Up to 10% of patients with Duchenne PMD may have clinical manifestations in the 1st year of life in the form of a “sluggish child” symptom complex. The main symptoms are weakness of the muscles of the pelvic girdle, pathological muscle fatigue during exercise. Change in gait according to the "duck" type - by the age of 4-5, a gait defect is formed: the patient spreads his legs wide, when walking he rolls from side to side, moves on his toes, patients help themselves with their hands, waving them strongly when walking. On average, patients with Duchenne myopathy lose the ability to move independently from 8 to 12 years of age. However, there are patients who have lost the ability to move independently at the age of 6, and patients who move independently at the age of 16-17. Apparently, this depends on the individual characteristics of the course of the disease.
On average, patients with Duchenne myopathy lose the ability to move independently from 8 to 12 years of age. However, there are patients who have lost the ability to move independently at the age of 6, and patients who move independently at the age of 16-17. Apparently, this depends on the individual characteristics of the course of the disease.
Cardiovascular disorders - pulse lability, blood pressure, muffled tones, expansion of the boundaries of the heart, heart failure. Approximately 73% of the population have manifestations of cardiac pathology. The cardiovascular system is involved in the pathological process quite early. There are changes in the myocardium (blockade of the legs of the bundle of His, etc.).
Duchenne Muscular Dystrophy Diagnosis
The first step in the diagnosis of suspected Duchenne Study of the activity of CPK in blood serum.
In Duchenne myopathy, myocytes break down (rhabdomyolysis) and release CPK and other cytolysis products into the blood. Therefore, the level of CPK in the blood is significantly increased. Deviations in the level of CPK activity by 100 or more times. Thus, the study of the activity of CPK in the blood serum can be the first step in the diagnosis of the disease.
Therefore, the level of CPK in the blood is significantly increased. Deviations in the level of CPK activity by 100 or more times. Thus, the study of the activity of CPK in the blood serum can be the first step in the diagnosis of the disease.
In addition to determining CPK in a biochemical blood test, it is necessary to determine the activity of such enzymes as lactate dehydrogenase (LDH), and the so-called "liver enzymes" alanine aminotransferase (ALT) and aspartate aminotransferase (AST). In Duchenne PMD, the activity of the LDH enzyme is increased by 3-5 times. The activity of AST and ALT enzymes, which are of extrahepatic origin, can be increased tenfold.
Diagnosis verification Progressive Duchenne muscular dystrophy requires genetic diagnostics.
DNA analysis Genetic testing usually begins with a simple MLPA (Multiplex ligation-dependent probe amplification) method that allows you to check the presence of all 79 exons in the DMD gene - this way deletion of exons / s can be detected .
Identification duplications of are carried out by modified MLPA. If the mutation has not been identified, sequencing of the DMD gene is used to detect point mutations. Various types of genetic studies provide more detailed information about changes in the structure (mutations) of DNA in Duchenne PMD. For the study, 2 ml of venous blood is needed. Confirmation of the diagnosis by the results of a genetic study allows the child to be included in clinical trials, and for his parents to develop recommendations for prenatal diagnosis in future pregnancies. After determining the mutation (changes in the dystrophin gene), the mother of the child is invited to undergo a genetic test to identify the carriage of the mutation in the DMD gene. Such information is important for other female relatives on the mother's side (her sisters, daughters, aunts, cousins), as they may also be carriers of this mutation.
It is possible to carry out prenatal diagnosis of Duchenne PMD by methods of molecular genetic research (material for research from the mother must be taken before the 12th week of pregnancy), as well as preimplantation gene diagnosis in the case of in vitro fertilization.
Treatment of Duchenne muscular dystrophy
Glucocorticoids (or glucocorticosteroids)The current anti-inflammatory treatment with corticosteroids is the gold standard described in the international guidelines for the management of patients with Duchenne.
Data from randomized controlled trials have shown the benefit of corticosteroids in restoring muscle strength. In addition to the main anti-inflammatory effect (relieves swelling and inflammation, stabilizes the muscle membrane), corticosteroid therapy allows the patient to extend the time of the ability to move independently (walk). Currently, corticosteroids are maintained even after the patient has lost the ability to walk. Continued therapy will help curb the development of scoliosis, maintain muscle strength in the upper limbs, and support respiratory and cardiac function. Because corticosteroids have been used in patients with Duchenne for a long time, it is important to monitor adverse events and complications of such therapy (eg, weight gain, behavioral changes, growth and/or puberty retardation, etc. ).
).
Cardiomyopathy and heart failure are major causes of death in patients with DMD.
The goal of cardioprotective therapy is to reduce the load on the myocardium. The effectiveness of the appointment of ACE inhibitors for the prevention of dilated cardiomyopathy has been proven. For example, one of the first was a study by the Institute of Myology in Paris, which showed that with the early appointment of ACE inhibitors by the age of 15, cardiomyopathy formed in only 20-30 percent of patients instead of 70 percent, as it was before. Also prescribed drugs that reduce heart rate - beta-blockers. This refers to the stage of compensation.
Cardiometabolic therapy (L-carnitine, coenzyme Q10)At the stage of decompensation, the specialist may recommend additional drugs (eg, cardiotonic).
Metabolic therapy For the prevention of osteoporosis, the appointment of drugs containing vitamin D3 and calcium is indicated.
The goal of etiotropic treatment is to eliminate the cause of the disease - a mutation in the DMD gene, thereby restoring the synthesis of dystrophin. Currently, several drugs that restore protein synthesis are approved in the world.
Nonsense mutation. Stop codonApproximately 10-15% of DMD is caused by point mutations leading to the formation of a premature stop codon, that is, a premature stop in the synthesis of the dystrophin protein. Ataluren (Translarna, PTC Therapeutics, USA) is designed to skip premature stop codons. Ataluren binds to ribosomal RNA and impairs premature stop codon recognition, which allows restoration of translation and synthesis of modified dystrophin.
Skipping exon/s The violation of the reading frame (the process of synthesis of the protein dystrophin) in most cases is associated with deletions and duplications, so the main strategy of gene therapy being developed was the method of skipping an exon or exons. This method leads to the restoration of the reading frame, in other words, the resumption of expression of the truncated dystrophin. Restoration of expression of partially functional dystrophin should convert the malignant form of DMD with severe phenotypic presentation to BMD, Becker muscular dystrophy. This treatment can help most patients with Duchenne muscular dystrophy. Exceptions are deletions that destroy actin-binding domains in the N-terminal region or affect the first or last exons and large chromosomal rearrangements. Such mutations are quite rare and together make up less than 10% of all described mutations in the DMD gene. Currently, three drugs have been approved using exon skipping with AOH antisense oligonucleotides.
This method leads to the restoration of the reading frame, in other words, the resumption of expression of the truncated dystrophin. Restoration of expression of partially functional dystrophin should convert the malignant form of DMD with severe phenotypic presentation to BMD, Becker muscular dystrophy. This treatment can help most patients with Duchenne muscular dystrophy. Exceptions are deletions that destroy actin-binding domains in the N-terminal region or affect the first or last exons and large chromosomal rearrangements. Such mutations are quite rare and together make up less than 10% of all described mutations in the DMD gene. Currently, three drugs have been approved using exon skipping with AOH antisense oligonucleotides.
The most anticipated is a universal drug or method that can be used for any kind of mutation in the dystrophin gene.
Mini and microdystrophin or method CRISPR/Cas9 can be called such preparation.
Disease prognosis
The introduction of a multidisciplinary approach and adherence to standards of care has increased the life expectancy of patients with Duchenne muscular dystrophy in the world according to a retrospective analysis to an average of 27.9years (from 23 to 38.6 years).
Links to used articles:Saito T, Kawai M, Kimura E et al. Study of Duchenne muscular dystrophy long-term survivors aged 40 years and older living in specialized institutions in Japan. Neuromuscul Discord. 2017 Feb;27(2):107-114. doi: 10.1016/j.nmd.2016.11.012.
Passamano L., Taglia A., Palladino A. Improvement of survival in Duchenne Muscular Dystrophy: a retrospective analysis of 835 patients. Acta Myol. 2012 Oct; 31(2): 121–125.
Skuk D, Goulet M, Roy B, Chapdelaine P, Bouchard JP, Roy R, et al. Dystrophin expression in muscles of Duchenne muscular dystrophy patients after high-density injections of normal myogenic cells.