How to get sleep in depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs.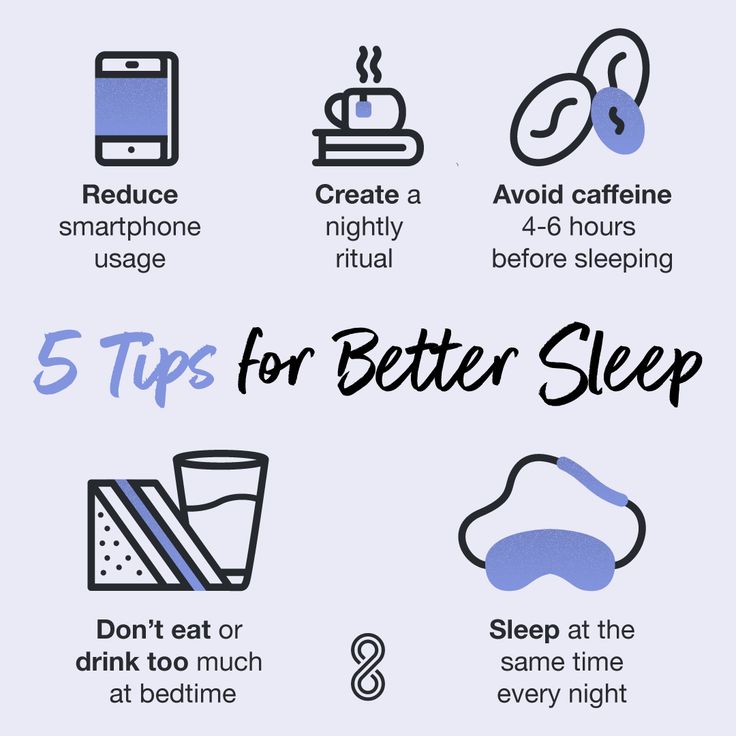 In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
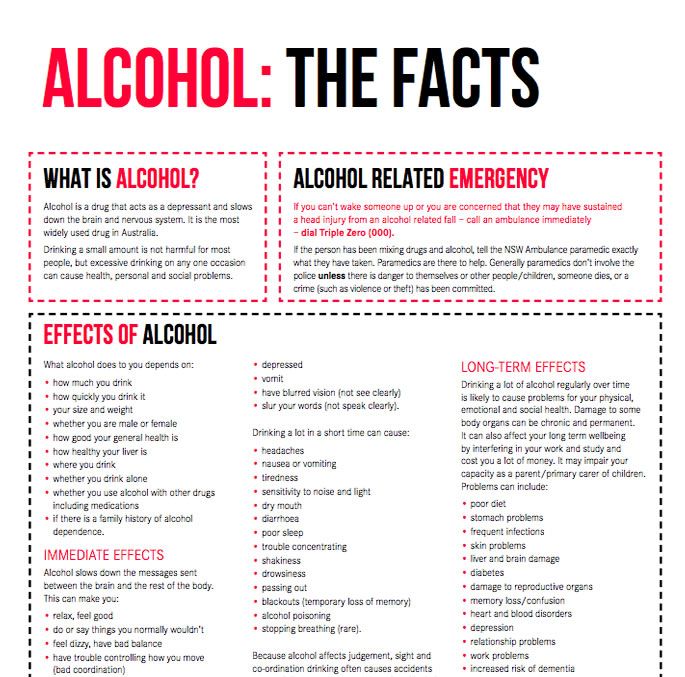
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 03/22/2023
Treatment of insomnia in neurosis, depression, stress in St. Petersburg
- Main
- Neurology
- Treatment of sleep disorders
- Treatment of insomnia
- For neurosis
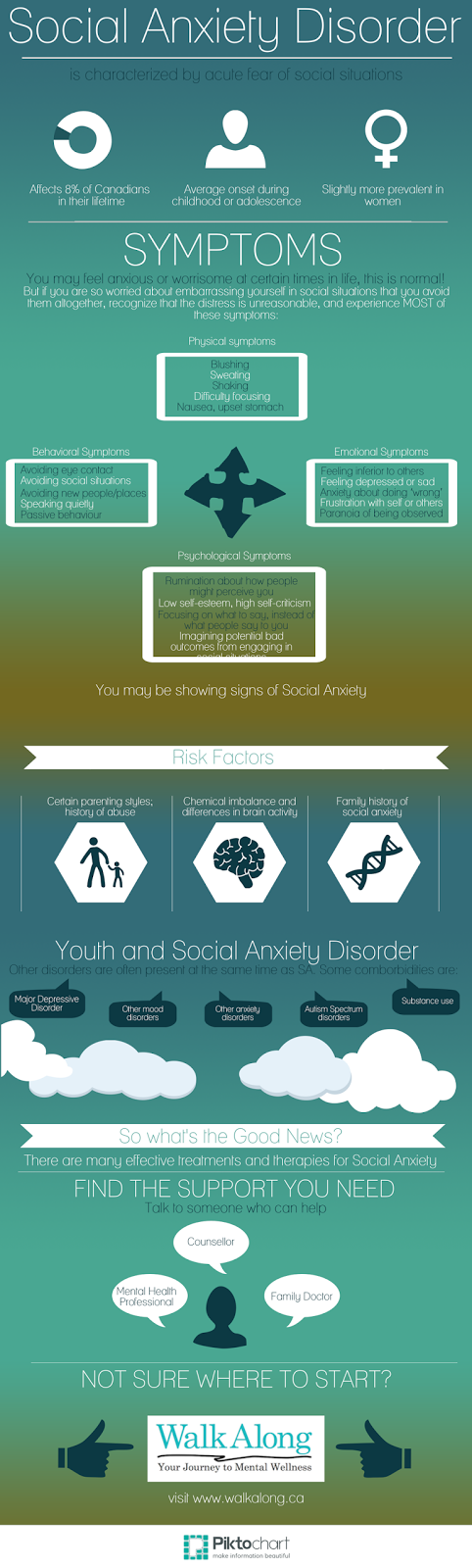
Insomnia is a symptomatic manifestation characterized by sleep disturbance or inability to fall asleep. There are many causes of insomnia, but they are divided into only 2 groups: physiological and psychological factors.
In order to prescribe the right treatment, our specialists first determine the true cause of the disorder. If a patient has insomnia against a background of neurosis, we begin to treat the underlying disease that caused the sleep disorder. Otherwise, the therapeutic effect will be ineffective: the eliminated symptoms will return again after a certain time.
Insomnia in neurosis requires long-term complex treatment, in severe cases of manifestation of the disease - with the use of medications (hypnotics and sedatives). Tranquilizers can also be shown to the patient - when prescribing a remedy for insomnia, stress and depression to the patient, the doctor takes into account the clinical picture of the disease and the characteristics of the patient's body.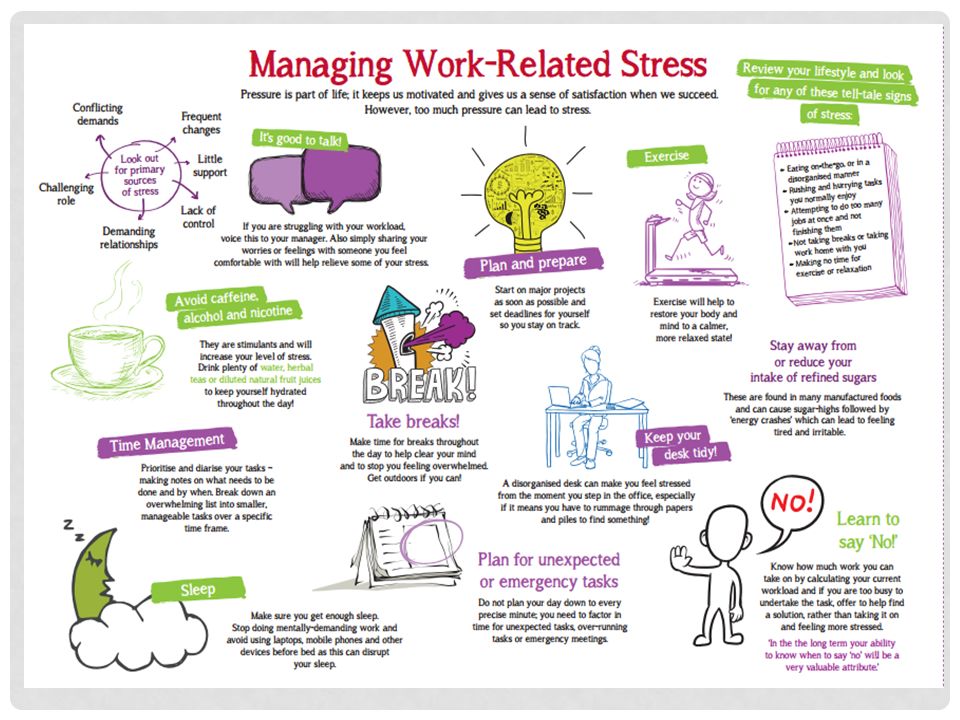
It is worth noting that in some cases, treatment can be carried out without the use of drugs, but with the help of psychotherapeutic influence, both group and individual.
At the same time, the main task of psychotherapy is to change the perception of patients to the environment, which helps to weaken the influence of traumatic factors on them. In the case of observation of insomnia in a patient with neurosis, therapy includes the patient's compliance with sleep hygiene.
Causes of insomnia in neurosis, depression, stress
The psychological causes of insomnia include the following:
- Stress associated with the patient's professional activities, difficulties within the family and domestic conflicts. Under their influence, the patient's nervous system works inefficiently, resulting in insomnia due to stress;
- Psychotrauma. As practice shows, insomnia, depression, neurosis go away on their own when a person accepts a problem;
- Strong mental experiences accompanying the loss of loved ones.
 Of the non-drug methods of therapy in this case, only time and the support of loved ones help. Often, insomnia after stress is treated with antidepressants prescribed strictly by a specialist;
Of the non-drug methods of therapy in this case, only time and the support of loved ones help. Often, insomnia after stress is treated with antidepressants prescribed strictly by a specialist; - Personality traits. In the risk group, patients are prone to anxiety - unreasonable fear. Anxiety before the next day negatively affects the psycho-emotional state of the patient, causing sleep disorders.
Symptoms of insomnia
You can easily recognize insomnia by the appearance of a person. Insomnia is characterized by redness of the eyes, pallor of the skin, the appearance of bags under the eyes, dry lips. A person suffering from insomnia shows lethargy, depression, and in some cases apathy.
The main symptoms of the disease are as follows:
- Difficulty falling asleep, lasting up to several hours;
- Partial or complete lack of sleep at night;
- Light sleep, which does not give the body and psyche a good rest;
- Interrupted sleep or early awakening, after which it is impossible to fall asleep again.

Remember that frequent lack of sleep is dangerous for the body. Insomnia during depression causes malfunctions of the central nervous system, which is accompanied by irritability, decreased performance. With persistent sleep disturbances, there is a risk of premature death.
Insomnia associated with various types of depression
There are several types of depressive conditions characterized by sleep disorders:
- Endogenous depression. In this case, falling asleep is normal, but there are sharp nocturnal awakenings, and further attempts to fall asleep remain fruitless. Upon awakening, there are often bouts of anxiety, fear, hopelessness, which do not allow you to fall asleep again. A state of drowsiness may occur, but it does not give a good rest. In the morning the patient experiences a bad mood, heaviness in the head.
- Latent depression (masked). With it, early awakenings occur, sleep is often interrupted, the patient feels tired and exhausted.
- Seasonal depression. The patient often experiences bouts of weakness and drowsiness in the morning and afternoon hours, sleep at night is normal, but does not bring rest.
- Sad depression. It is characterized by a feeling of fatigue and a breakdown that occurs towards the end of the day. The patient's sleep becomes sensitive, during which a person cannot fully relax. Usually there are early awakenings, but the person cannot find the strength to get out of bed, and continues to lie until the sound of the alarm clock.
Fatigue and lethargy do not go away even after getting up, they can often be accompanied by headaches. During sleep, the patient often sees painful, monotonous dreams of a gloomy nature, usually associated with his problems and defeats.
- Apathetic depression. In this case, the patient's sleep differs in duration - the rise occurs much later than usual, but during the day the person is overcome by drowsiness and a feeling of severe fatigue.
 The patient may not get out of bed all day because of a breakdown. Dreams occur rarely, they are faded and not emotional, but often the patient can lose the border between dreams and reality.
The patient may not get out of bed all day because of a breakdown. Dreams occur rarely, they are faded and not emotional, but often the patient can lose the border between dreams and reality. - Anxious depression. It is accompanied by the appearance of disturbing thoughts, often preventing sleep. Sleep is mostly intermittent, with a negative emotional coloring, nightmares are possible.
Diagnosis of insomnia
Comprehensive examination of the patient helps our specialists to reliably determine the cause of insomnia. It includes examination of the patient by the doctors of the clinic, questioning, history taking, laboratory and instrumental examinations. Our patients are usually assigned the following types of examinations:
- Magnetic resonance imaging;
- Ultrasonic examination;
- Electrocardiography;
- Laboratory tests.
Treatment of insomnia in depression in the clinic Dr. SAN
Before starting the treatment of insomnia in neurosis, the doctors of the clinic conduct a thorough comprehensive examination of the patient. Based on the indications, specialists establish the necessary type of therapeutic effect, taking into account the characteristics of the patient's body, the mechanism of the development of the disease and the reasons for the development of insomnia, stress, and depression. In some cases, patients are prescribed psychotherapeutic sessions or treatment of insomnia neurosis with hypnosis. In extreme cases, the treatment of insomnia in depression requires the appointment of a number of medications by a specialist.
Based on the indications, specialists establish the necessary type of therapeutic effect, taking into account the characteristics of the patient's body, the mechanism of the development of the disease and the reasons for the development of insomnia, stress, and depression. In some cases, patients are prescribed psychotherapeutic sessions or treatment of insomnia neurosis with hypnosis. In extreme cases, the treatment of insomnia in depression requires the appointment of a number of medications by a specialist.
If there is a suspicion of damage to the patient's internal organs caused by overwork and lack of quality sleep, the patient is assigned an additional examination, with the involvement of specialized specialists: an endocrinologist, a therapist, a neurologist-epileptologist. Also in the Doctor SAN clinic there is an appointment with a somnologist, a polysomnography service is provided.
Cost of treatment of insomnia in case of neurosis
| Service | Price | |
|---|---|---|
| Appointment with a neurologist specializing in the treatment of sleep disorders | 2 840 ₽ | |
| Appointment with a psychiatrist who treats insomnia | 5 000 ₽ |
Update date: 02/14/2018
- Memory disorders
- Dizziness
- Epilepsy
Make an appointment
Date and time: (not set)
Make an appointment with a neurologist
Make an appointment with a neurologist
Select the date and time of your appointment
Tuesday
04 April
Thursday
06 April
Tuesday
April 11
Wednesday
April 12
Thursday
April 13
Saturday
April 15
Monday
April 17
Tuesday
April 18
Wednesday
April 19
Thursday
April 20
Saturday
April 22
Monday
April 24
Tuesday
April 25
Wednesday
April 26
Thursday
April 27
Friday
April 28
Saturday
April 29
Treatment of insomnia in neurosis is carried out
Fedosova Svetlana
Narzulloevna
Neurologist, epileptologist
Top category
Experience 37 years
Neurologist, epileptologist, vertebrologist
Experience 37 years
Belyasnik Andrey
Sergeevich
Neurologist, doctor of functional diagnostics
First category
Work experience 14 years
Neurologist, doctor of functional diagnostics
Work experience 14 years
Leave a request for a call:
+7 (812) 407-18-00
No sleep, no rest for the tormented soul
Sleep is one of the basic needs of the human body, and its lack leads to severe psychological and physical stress: not only mood and cognitive abilities suffer, but also the cardiovascular system and metabolism. Nevertheless, for almost 50 years, sleep deprivation has been trying to treat one of the most difficult and terrible conditions for the human psyche - depression. We set out to explore what forced sleep therapy for psychiatric disorders is, why it can be effective, and why it should be used with caution.
Nevertheless, for almost 50 years, sleep deprivation has been trying to treat one of the most difficult and terrible conditions for the human psyche - depression. We set out to explore what forced sleep therapy for psychiatric disorders is, why it can be effective, and why it should be used with caution.
Anyone who has not slept for a long time at least once knows perfectly well what this is fraught with: lethargy appears, attention decreases, mood deteriorates and severe physical fatigue occurs. Available stimulants like caffeine stop working (their mechanism of action is rather limited), and the only way out is to take a break and still rest.
In chronic sleep deprivation and insomnia (we talked about it in detail in the material “Your words rock well”, prepared for World Sleep Day last year), deeper and more serious conditions and diseases are added to superficial symptoms.
For example, the consequences of lack of sleep include cardiovascular disease, nutritional and metabolic problems (from overeating to type 2 diabetes), and various mental disorders. Last but not least, lack of sleep is closely associated with depression, which is surprising in its own way, because sleep deprivation is often used to treat it, and at times quite successfully.
Last but not least, lack of sleep is closely associated with depression, which is surprising in its own way, because sleep deprivation is often used to treat it, and at times quite successfully.
At least that's what the meta-analyses suggest. One, conducted in 2017, focuses on 66 studies published since 1974 to 2016: it states that sleep deprivation is effective in 50 percent of patients in randomized control trials and 45 percent in other studies. The effect did not depend on what experimental technique was used, on what preparations the patient was sitting, and also on his gender and age.
The authors of the study call the effect significant, but given the fact that the side variables that would provide the desired effect could not be found, the result can be called random - of course, if we consider the use of sleep deprivation as a binary variable. In other words, when psychiatrists give patients with depression forced sleep therapy, it can either help or not - as luck would have it.
At the same time, sleep deprivation is still considered a fairly effective way to treat depression, and why this is so (even if it is intuitively clear that lack of sleep is more likely to be harmful) should still be understood.
Intervene experimentally
The relationship between sleep quality and mental disorders is complex. First of all, the relationship between them is two-way: insomnia, as well as hypersomnia - excessive sleep duration and daytime sleepiness, are considered both symptoms of depression and factors that largely affect its development.
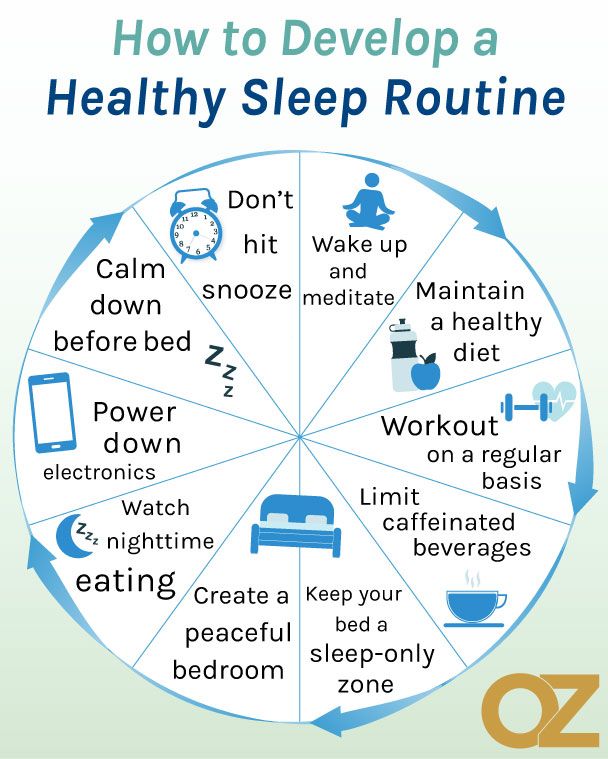
First of all, therefore, in case of depression, it is necessary to restore normal sleep hygiene: do not eat a few hours before going to bed, go to bed at the same time, sleep the number of hours recommended for age (for an adult - about seven to eight hours a day). day) and do not put off rest for the weekend in anticipation of a cumulative effect.
Obviously this can be quite difficult; in this case, patients with depression are prescribed drugs from the group of neuroleptics or other substances with anti-anxiety (trouble, as you know, does not come alone: with depression, the risk of developing anxiety is higher) or sedative effect.
In the early 1970s, the German psychiatrist Walter Schulte discovered and studied that sleep deprivation could have a therapeutic effect on depression. He observed three patients diagnosed with depressive disorder: two teachers and one doctor. Each of them reported to Schulte that after a sleepless night at work or playing sports, they feel an improvement in their mental state.
Of course, it is impossible to base an entire psychiatric practice on three cases, so after the first statements about the benefits of sleep deprivation (after Schulte, two more of his colleagues managed to achieve a significant effect in 23 of 34 patients), scientists began to actively conduct research.
First, it was necessary to determine exactly how many hours of sleep deprivation it takes to achieve at least some effect - and at what time to start the experiment. Usually, sleep deprivation therapy involves a whole day (or even more: sometimes up to 36-40 hours) of forced wakefulness: the patient is woken up at about one in the morning, after which he does not sleep the whole next day and sometimes the whole next night.
With this therapy, the intake of any CNS stimulants (even coffee) is excluded, and it is also recommended to combine forced insomnia with light therapy (however, both are considered branches of chromotherapy - artificial "tuning" of sleep and wake cycles).
The effect comes fairly quickly: with sleep deprivation in a depressed patient, visible improvements are immediately observed. However, this is a rather deceptive success: studies indicate that in 50-80 percent of patients the state returns to the usual depressive state after they do get some sleep. At the same time, in 10-15 percent of patients, improvements, on the contrary, appear only after sleep following deprivation. In 2-7 percent of patients, the condition may worsen, and symptoms of mania may be added to depression (sleep deprivation, therefore, is not recommended for people with bipolar disorder - even in the depressive phase).
Some vagueness of the effect can be explained by the fact that a day or more without sleep is still quite painful for the body. Therefore, scientists tried to reduce the time of forced wakefulness to a few hours at night. To do this, for example, you can wake up the patient in the middle of the night and keep him awake for a couple of hours. Such a study was conducted in the early 1990s, but forced wakefulness until five in the morning after waking up at three did not give any special effect.
Although meta-analyses indicate that there are no precise confounding variables that would provide the desired effect of sleep deprivation, anecdotal studies still state that several conditions must be met for this method to be effective.
For example, sleep deprivation works best on patients with endogenous depression, rather than depression caused by external factors. In addition, the variation in the patient's mood during the day must also be taken into account: sleep deprivation works most effectively in those who feel better in the evening, rather than during the day.
The mechanism of the therapeutic effect of sleep deprivation has not been fully established. For example, recent research suggests the role of the neurotransmitter adenosine, which accumulates in the brain during the day and is ultimately responsible for making us feel tired and fall asleep.
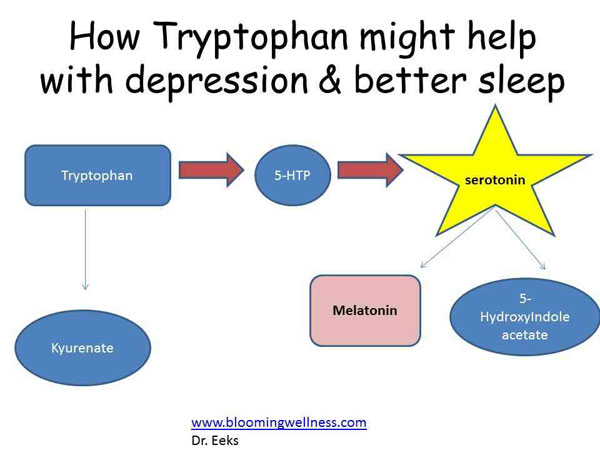
Other studies point to the involvement of the serotonergic system, the main one in the pathology of depression, in such therapy. When taking the drug pindolol, which blocks serotonin autoreceptors and improves the effect of antidepressants from the group of selective serotonin reuptake inhibitors, sleep deprivation more effectively improves well-being in depression.
A logical reason for the effectiveness of lack of sleep seems to be its comparison with the use of psychostimulants (eg, amphetamine). Indeed, in the absence of sleep, effects similar to taking psychoactive substances are sometimes observed (you may be familiar with this: sometimes, with a long wakefulness, it seems that there is more strength and energy).
In both cases, the concentration of monoamines in the brain increases (primarily, however, not serotonin, but dopamine), due to which the work of the limbic system stabilizes, and mental well-being improves. Such a theory is consistent with the fact that the effect of sleep deprivation is often unstable and short-lived - like psychostimulants. However, this is still just a theory.
Use with caution
Despite a fairly long history of study and use in psychiatric practice, sleep deprivation still remains an experimental treatment for depression and is not included in the standard treatment recommendations on a par with antidepressant drugs and psychotherapy. This is evidenced both by the fact that depression is often treated with sleep deprivation only under controlled conditions (under the supervision of doctors), and by the fact that sleepless nights have many negative consequences.
One of the most serious is the possible increased risk of developing Alzheimer's disease even from one night of sleeplessness. Two proteins play a key role in the development of the disease: beta-amyloid, which forms plaques in the brain, and tau, which contributes to the formation of intracellular neurofibrillary cords.
Studies show that just one sleepless night significantly increases the concentration of beta-amyloid in the brain and tau in the blood. The mechanism of such an action is not fully known in either case, and it is also not clear whether there are actually any negative consequences.
It is also interesting that lack of sleep leads to increased feelings of loneliness and social isolation. Here the effect, however, is more psychological: the lack of sleep makes people look for a variety of ways to escape from the accumulated fatigue, which increases the need for communication. Other people, on the contrary, find a sleepy person more repulsive and do not want to make contact with him.
A rather understandable conflict arises, which makes it difficult to establish communication with others - hence the feeling of loneliness appears. And with depression (unless, of course, it was not there before, since loneliness is one of the common psychological symptoms of a disorder), it is definitely not necessary.
In addition, a recent study showed that a sleepless night reduces the activity of the prefrontal cortex, which is responsible, among other things, for cognitive control. With a decrease in cognitive control, in turn, anxiety increases significantly - and it can significantly worsen the condition of depression.
However, it should be borne in mind that the use of sleep deprivation for the treatment of insomnia and the same technique for behavioral research are two different things. Healthy people without mental disorders take part in the latter; in them, control studies of sleep deprivation therapy show that not getting a night's rest only increases irritability—and doesn't work the way it does for people with depression, even in the short term.
Therefore, it is logical to assume that lack of sleep may not bring negative behavioral and mental aspects to people with depression: review studies also speak about the severity of the presence of mental disorders for the effectiveness of sleep deprivation.