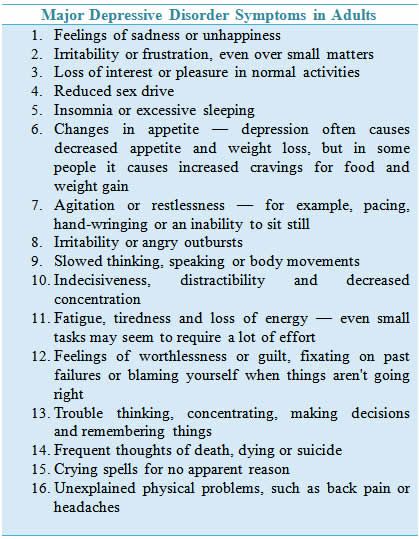
What are the symptoms of major depressive disorder
Depression (major depressive disorder) - Diagnosis and treatment
Diagnosis
Your doctor may determine a diagnosis of depression based on:
- Physical exam. Your doctor may do a physical exam and ask questions about your health. In some cases, depression may be linked to an underlying physical health problem.
- Lab tests. For example, your doctor may do a blood test called a complete blood count or test your thyroid to make sure it's functioning properly.
- Psychiatric evaluation. Your mental health professional asks about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
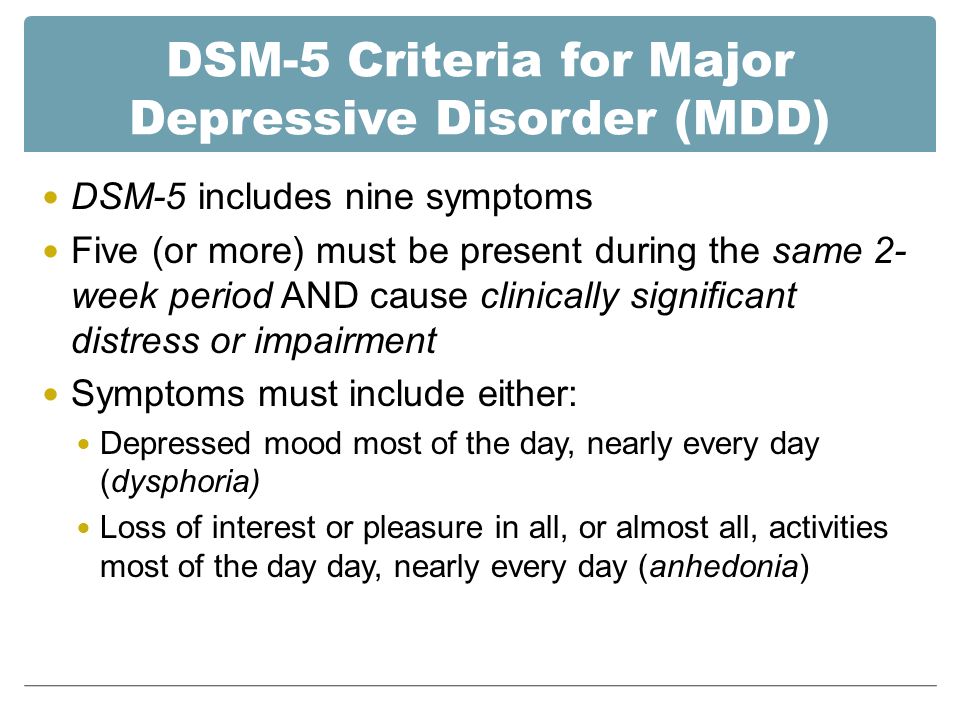
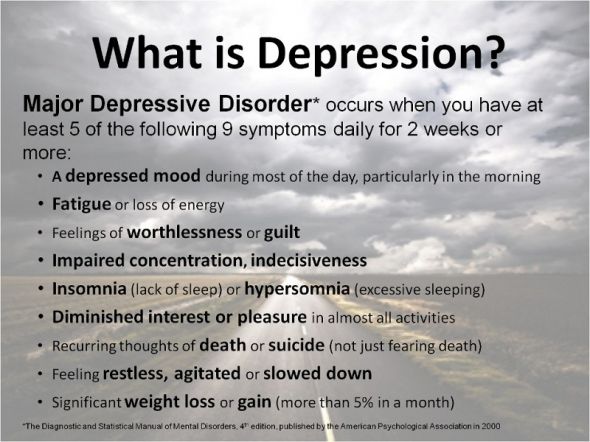
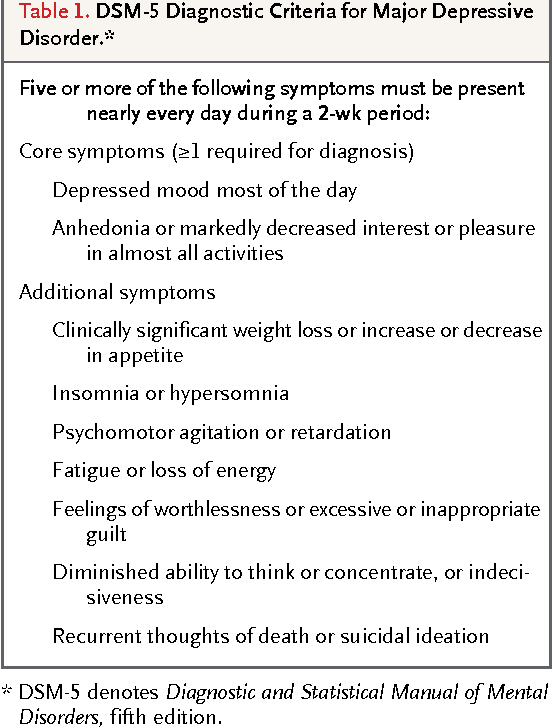
- DSM-5. Your mental health professional may use the criteria for depression listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
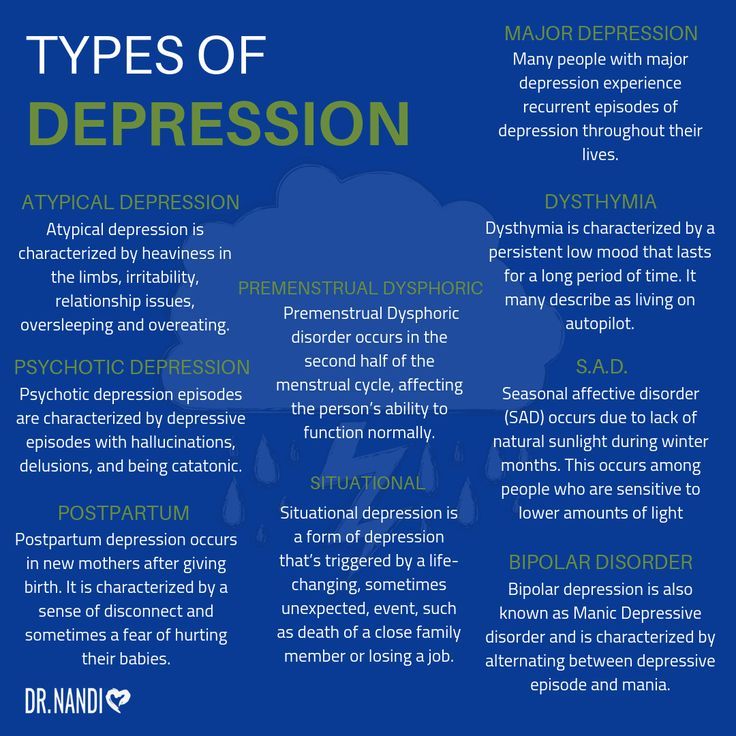
Types of depression
Symptoms caused by major depression can vary from person to person. To clarify the type of depression you have, your doctor may add one or more specifiers. A specifier means that you have depression with specific features, such as:
- Anxious distress — depression with unusual restlessness or worry about possible events or loss of control
- Mixed features — simultaneous depression and mania, which includes elevated self-esteem, talking too much and increased energy
- Melancholic features — severe depression with lack of response to something that used to bring pleasure and associated with early morning awakening, worsened mood in the morning, major changes in appetite, and feelings of guilt, agitation or sluggishness
- Atypical features — depression that includes the ability to temporarily be cheered by happy events, increased appetite, excessive need for sleep, sensitivity to rejection, and a heavy feeling in the arms or legs
- Psychotic features — depression accompanied by delusions or hallucinations, which may involve personal inadequacy or other negative themes
- Catatonia — depression that includes motor activity that involves either uncontrollable and purposeless movement or fixed and inflexible posture
- Peripartum onset — depression that occurs during pregnancy or in the weeks or months after delivery (postpartum)
- Seasonal pattern — depression related to changes in seasons and reduced exposure to sunlight
Other disorders that cause depression symptoms
Several other disorders, such as those below, include depression as a symptom.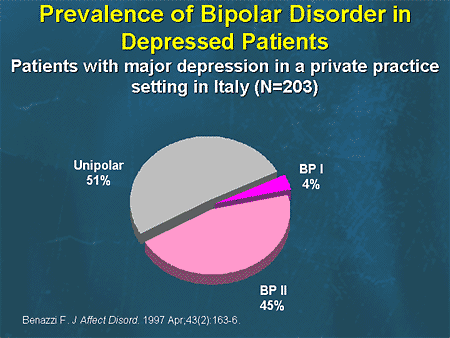 It's important to get an accurate diagnosis, so you can get appropriate treatment.
It's important to get an accurate diagnosis, so you can get appropriate treatment.
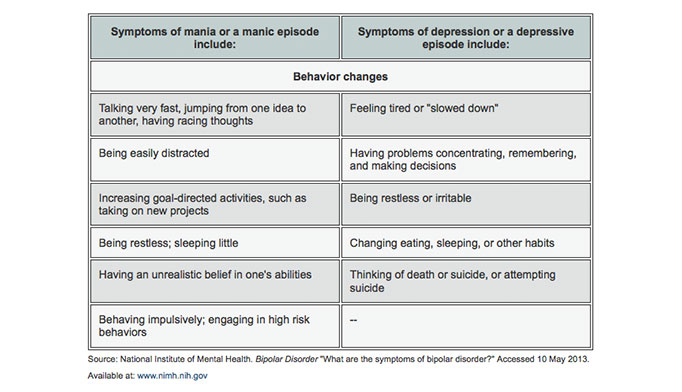
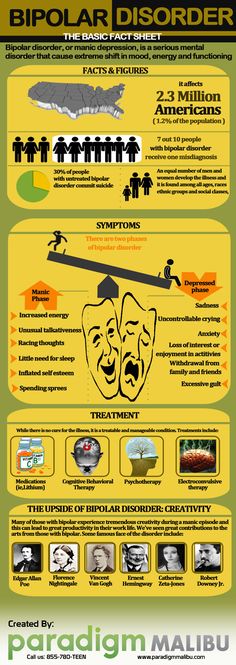
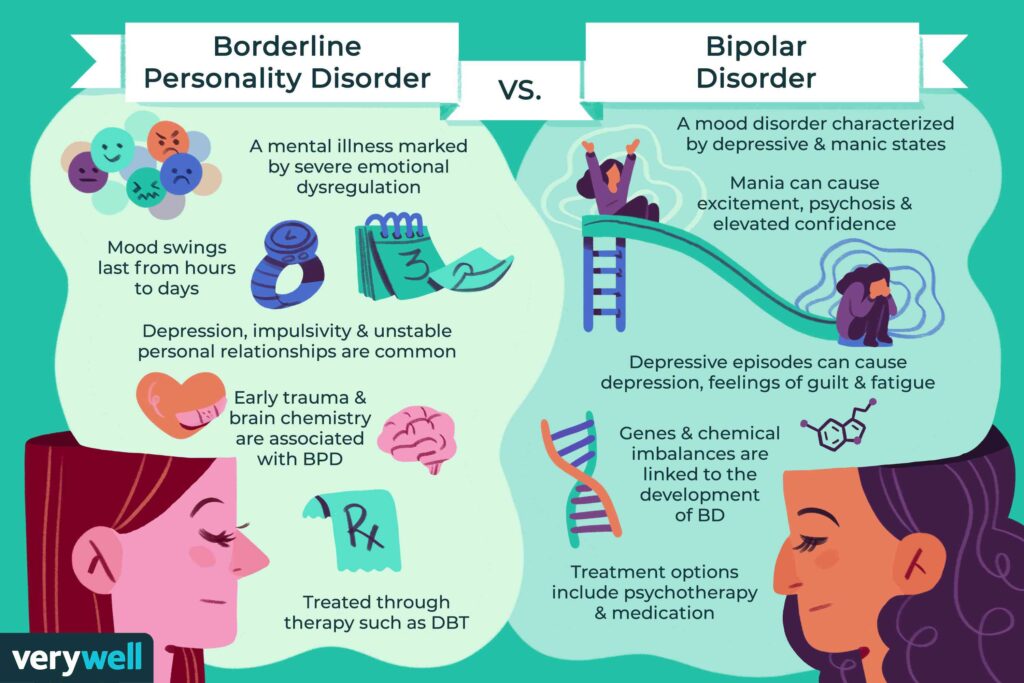
- Bipolar I and II disorders. These mood disorders include mood swings that range from highs (mania) to lows (depression). It's sometimes difficult to distinguish between bipolar disorder and depression.
- Cyclothymic disorder. Cyclothymic (sy-kloe-THIE-mik) disorder involves highs and lows that are milder than those of bipolar disorder.
- Disruptive mood dysregulation disorder. This mood disorder in children includes chronic and severe irritability and anger with frequent extreme temper outbursts. This disorder typically develops into depressive disorder or anxiety disorder during the teen years or adulthood.
- Persistent depressive disorder. Sometimes called dysthymia (dis-THIE-me-uh), this is a less severe but more chronic form of depression. While it's usually not disabling, persistent depressive disorder can prevent you from functioning normally in your daily routine and from living life to its fullest.
- Premenstrual dysphoric disorder. This involves depression symptoms associated with hormone changes that begin a week before and improve within a few days after the onset of your period, and are minimal or gone after completion of your period.
- Other depression disorders. This includes depression that's caused by the use of recreational drugs, some prescribed medications or another medical condition.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your depression (major depressive disorder)-related health concerns Start Here
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Complete blood count (CBC)
Treatment
Medications and psychotherapy are effective for most people with depression. Your primary care doctor or psychiatrist can prescribe medications to relieve symptoms.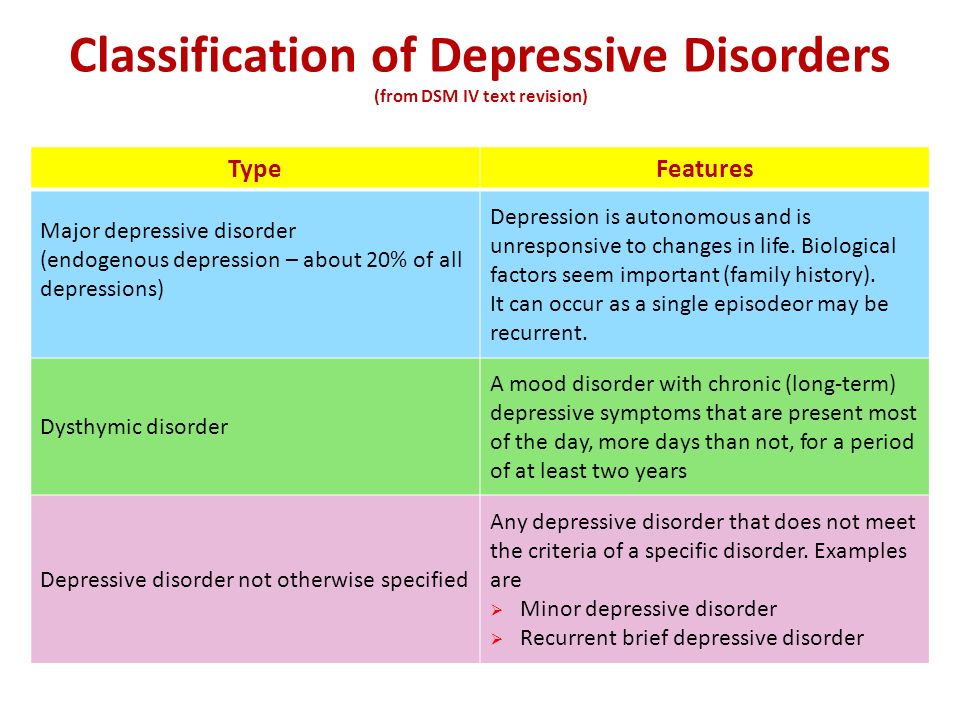 However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
If you have severe depression, you may need a hospital stay, or you may need to participate in an outpatient treatment program until your symptoms improve.
Here's a closer look at depression treatment options.
Medications
Many types of antidepressants are available, including those below. Be sure to discuss possible major side effects with your doctor or pharmacist.
- Selective serotonin reuptake inhibitors (SSRIs). Doctors often start by prescribing an SSRI. These drugs are considered safer and generally cause fewer bothersome side effects than other types of antidepressants. SSRIs include citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft) and vilazodone (Viibryd).
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Examples of SNRIs include duloxetine (Cymbalta), venlafaxine (Effexor XR), desvenlafaxine (Pristiq, Khedezla) and levomilnacipran (Fetzima).
- Atypical antidepressants. These medications don't fit neatly into any of the other antidepressant categories. They include bupropion (Wellbutrin XL, Wellbutrin SR, Aplenzin, Forfivo XL), mirtazapine (Remeron), nefazodone, trazodone and vortioxetine (Trintellix).
- Tricyclic antidepressants. These drugs — such as imipramine (Tofranil), nortriptyline (Pamelor), amitriptyline, doxepin, trimipramine (Surmontil), desipramine (Norpramin) and protriptyline (Vivactil) — can be very effective, but tend to cause more-severe side effects than newer antidepressants. So tricyclics generally aren't prescribed unless you've tried an SSRI first without improvement.
- Monoamine oxidase inhibitors (MAOIs). MAOIs — such as tranylcypromine (Parnate), phenelzine (Nardil) and isocarboxazid (Marplan) — may be prescribed, typically when other drugs haven't worked, because they can have serious side effects. Using MAOIs requires a strict diet because of dangerous (or even deadly) interactions with foods ― such as certain cheeses, pickles and wines ― and some medications and herbal supplements.
 Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs.
Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs. - Other medications. Other medications may be added to an antidepressant to enhance antidepressant effects. Your doctor may recommend combining two antidepressants or adding medications such as mood stabilizers or antipsychotics. Anti-anxiety and stimulant medications also may be added for short-term use.
Finding the right medication
If a family member has responded well to an antidepressant, it may be one that could help you. Or you may need to try several medications or a combination of medications before you find one that works. This requires patience, as some medications need several weeks or longer to take full effect and for side effects to ease as your body adjusts.
Inherited traits play a role in how antidepressants affect you. In some cases, where available, results of genetic tests (done by a blood test or cheek swab) may offer clues about how your body may respond to a particular antidepressant.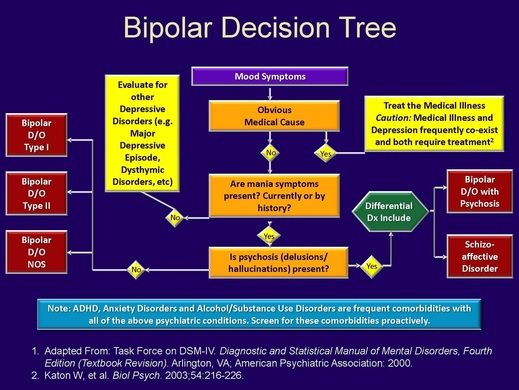 However, other variables besides genetics can affect your response to medication.
However, other variables besides genetics can affect your response to medication.
Risks of abruptly stopping medication
Don't stop taking an antidepressant without talking to your doctor first. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur.
Stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, and quitting suddenly may cause a sudden worsening of depression. Work with your doctor to gradually and safely decrease your dose.
Antidepressants and pregnancy
If you're pregnant or breast-feeding, some antidepressants may pose an increased health risk to your unborn child or nursing child. Talk with your doctor if you become pregnant or you're planning to become pregnant.
Antidepressants and increased suicide risk
Most antidepressants are generally safe, but the Food and Drug Administration (FDA) requires all antidepressants to carry a black box warning, the strictest warning for prescriptions.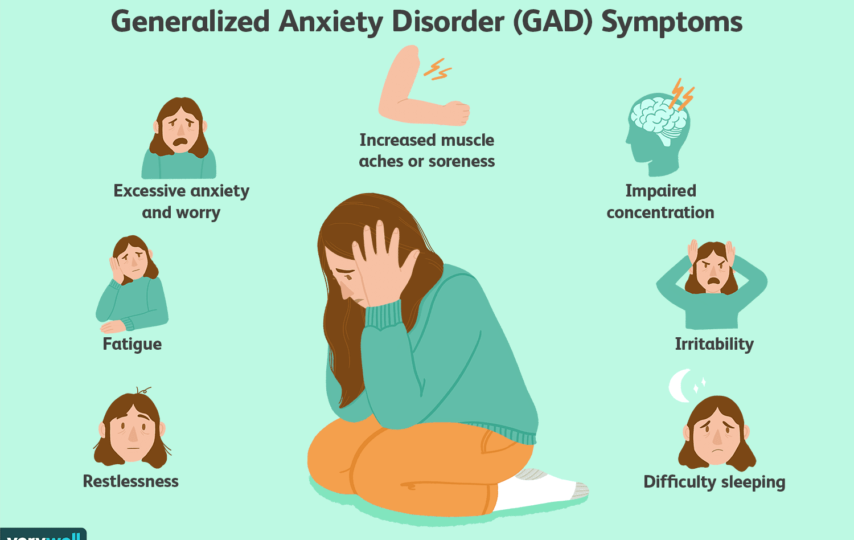 In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
Anyone taking an antidepressant should be watched closely for worsening depression or unusual behavior, especially when starting a new medication or with a change in dosage. If you or someone you know has suicidal thoughts when taking an antidepressant, immediately contact a doctor or get emergency help.
Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
Psychotherapy
Psychotherapy is a general term for treating depression by talking about your condition and related issues with a mental health professional. Psychotherapy is also known as talk therapy or psychological therapy.
Different types of psychotherapy can be effective for depression, such as cognitive behavioral therapy or interpersonal therapy.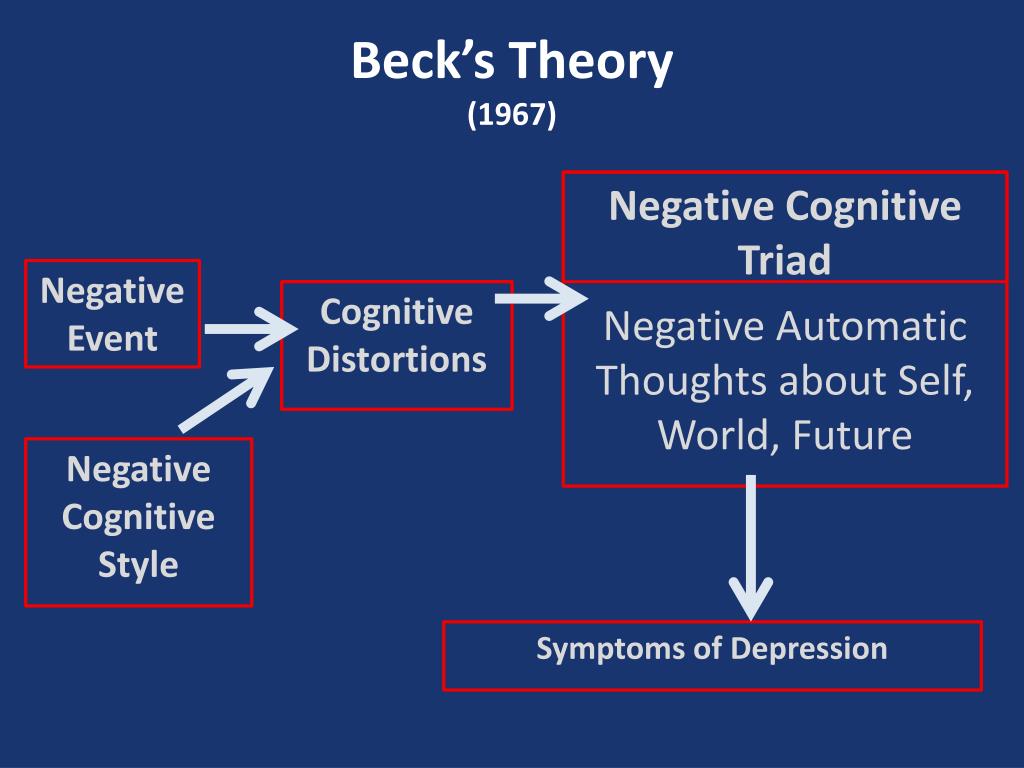 Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
- Adjust to a crisis or other current difficulty
- Identify negative beliefs and behaviors and replace them with healthy, positive ones
- Explore relationships and experiences, and develop positive interactions with others
- Find better ways to cope and solve problems
- Identify issues that contribute to your depression and change behaviors that make it worse
- Regain a sense of satisfaction and control in your life and help ease depression symptoms, such as hopelessness and anger
- Learn to set realistic goals for your life
- Develop the ability to tolerate and accept distress using healthier behaviors
Alternate formats for therapy
Formats for depression therapy as an alternative to face-to-face office sessions are available and may be an effective option for some people. Therapy can be provided, for example, as a computer program, by online sessions, or using videos or workbooks.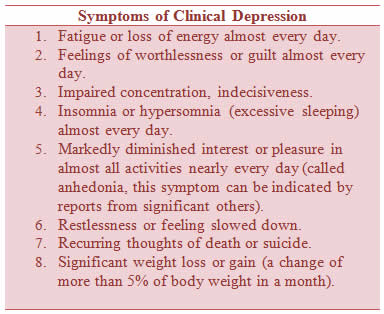 Programs can be guided by a therapist or be partially or totally independent.
Programs can be guided by a therapist or be partially or totally independent.
Before you choose one of these options, discuss these formats with your therapist to determine if they may be helpful for you. Also, ask your therapist if he or she can recommend a trusted source or program. Some may not be covered by your insurance and not all developers and online therapists have the proper credentials or training.
Smartphones and tablets that offer mobile health apps, such as support and general education about depression, are not a substitute for seeing your doctor or therapist.
Hospital and residential treatment
In some people, depression is so severe that a hospital stay is needed. This may be necessary if you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else. Psychiatric treatment at a hospital can help keep you calm and safe until your mood improves.
Partial hospitalization or day treatment programs also may help some people.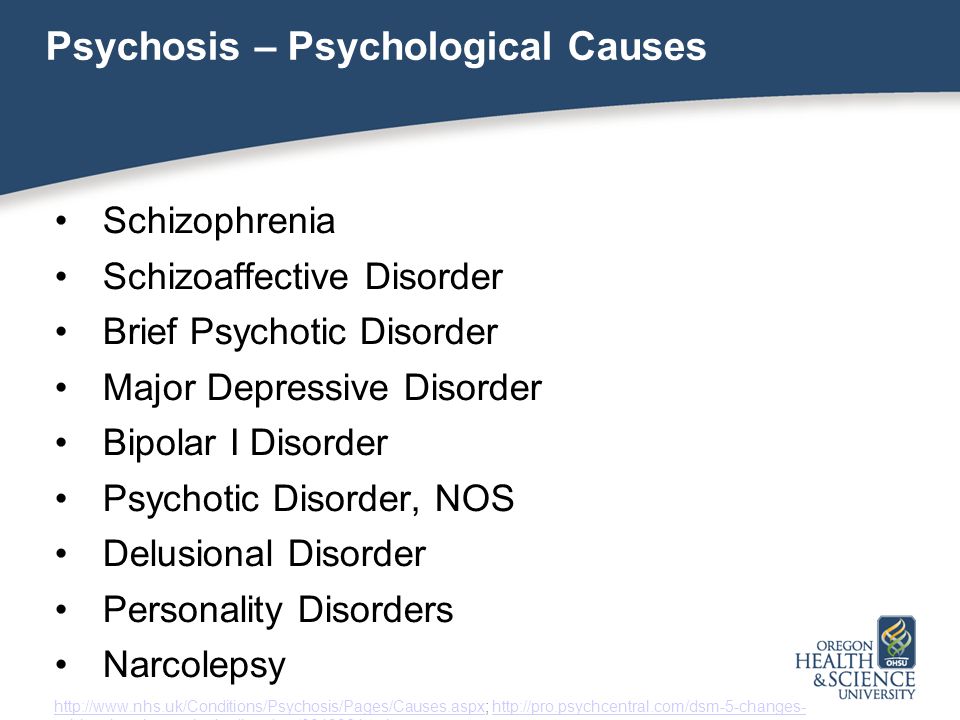 These programs provide the outpatient support and counseling needed to get symptoms under control.
These programs provide the outpatient support and counseling needed to get symptoms under control.
Other treatment options
For some people, other procedures, sometimes called brain stimulation therapies, may be suggested:
- Electroconvulsive therapy (ECT). In ECT, electrical currents are passed through the brain to impact the function and effect of neurotransmitters in your brain to relieve depression. ECT is usually used for people who don't get better with medications, can't take antidepressants for health reasons or are at high risk of suicide.
- Transcranial magnetic stimulation (TMS). TMS may be an option for those who haven't responded to antidepressants. During TMS, a treatment coil placed against your scalp sends brief magnetic pulses to stimulate nerve cells in your brain that are involved in mood regulation and depression.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Atypical antidepressants
- Monoamine oxidase inhibitors (MAOIs)
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- MAOIs and diet: Is it necessary to restrict tyramine?
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.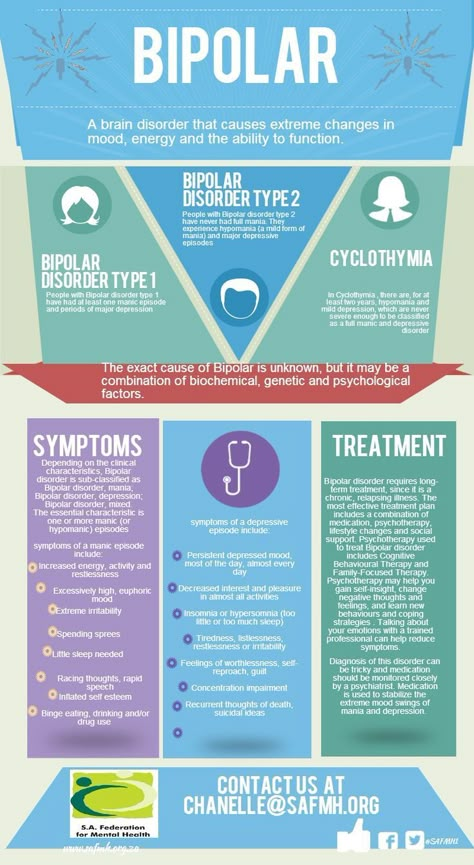
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.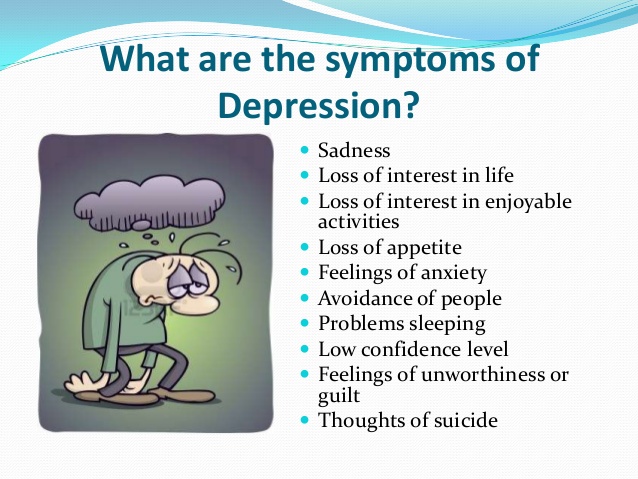
Lifestyle and home remedies
Depression generally isn't a disorder that you can treat on your own. But in addition to professional treatment, these self-care steps can help:
- Stick to your treatment plan. Don't skip psychotherapy sessions or appointments. Even if you're feeling well, don't skip your medications. If you stop, depression symptoms may come back, and you could also experience withdrawal-like symptoms. Recognize that it will take time to feel better.
- Learn about depression. Education about your condition can empower you and motivate you to stick to your treatment plan. Encourage your family to learn about depression to help them understand and support you.
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your depression symptoms. Make a plan so that you know what to do if your symptoms get worse. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
 Ask relatives or friends to help watch for warning signs.
Ask relatives or friends to help watch for warning signs. - Avoid alcohol and recreational drugs. It may seem like alcohol or drugs lessen depression symptoms, but in the long run they generally worsen symptoms and make depression harder to treat. Talk with your doctor or therapist if you need help with alcohol or substance use.
- Take care of yourself. Eat healthy, be physically active and get plenty of sleep. Consider walking, jogging, swimming, gardening or another activity that you enjoy. Sleeping well is important for both your physical and mental well-being. If you're having trouble sleeping, talk to your doctor about what you can do.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Depression, anxiety and exercise
Alternative medicine
Alternative medicine is the use of a nonconventional approach instead of conventional medicine. Complementary medicine is a nonconventional approach used along with conventional medicine — sometimes called integrative medicine.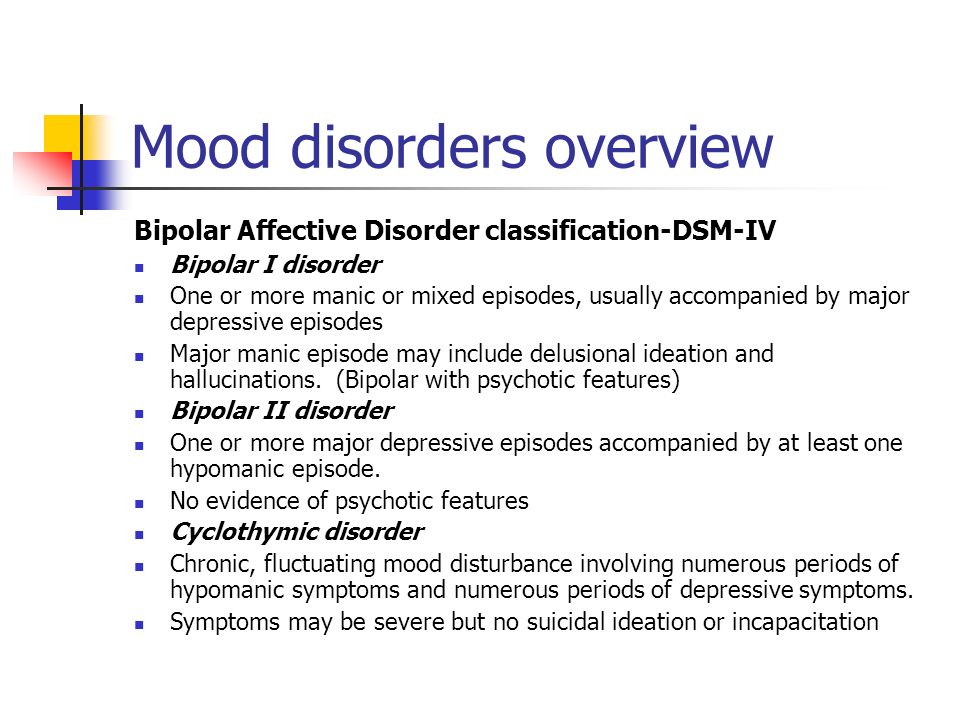
Make sure you understand the risks as well as possible benefits if you pursue alternative or complementary therapy. Don't replace conventional medical treatment or psychotherapy with alternative medicine. When it comes to depression, alternative treatments aren't a substitute for medical care.
Supplements
Examples of supplements that are sometimes used for depression include:
- St. John's wort. Although this herbal supplement isn't approved by the Food and Drug Administration (FDA) to treat depression in the U.S., it may be helpful for mild or moderate depression. But if you choose to use it, be careful — St. John's wort can interfere with a number of medications, such as heart drugs, blood-thinning drugs, birth control pills, chemotherapy, HIV/AIDS medications and drugs to prevent organ rejection after a transplant. Also, avoid taking St. John's wort while taking antidepressants because the combination can cause serious side effects.
- SAMe.
 Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder.
Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder. - Omega-3 fatty acids. These healthy fats are found in cold-water fish, flaxseed, flax oil, walnuts and some other foods. Omega-3 supplements are being studied as a possible treatment for depression. While considered generally safe, in high doses, omega-3 supplements may interact with other medications. More research is needed to determine if eating foods with omega-3 fatty acids can help relieve depression.
Nutritional and dietary products aren't monitored by the FDA the same way medications are. You can't always be certain of what you're getting and whether it's safe. Also, because some herbal and dietary supplements can interfere with prescription medications or cause dangerous interactions, talk to your doctor or pharmacist before taking any supplements.
Mind-body connections
Integrative medicine practitioners believe the mind and body must be in harmony for you to stay healthy. Examples of mind-body techniques that may be helpful for depression include:
- Acupuncture
- Relaxation techniques such as yoga or tai chi
- Meditation
- Guided imagery
- Massage therapy
- Music or art therapy
- Spirituality
- Aerobic exercise
Relying solely on these therapies is generally not enough to treat depression. They may be helpful when used in addition to medication and psychotherapy.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Natural remedies for depression: Are they effective?
Coping and support
Talk with your doctor or therapist about improving your coping skills, and try these tips:
- Simplify your life. Cut back on obligations when possible, and set reasonable goals for yourself.
 Give yourself permission to do less when you feel down.
Give yourself permission to do less when you feel down. - Write in a journal. Journaling, as part of your treatment, may improve mood by allowing you to express pain, anger, fear or other emotions.
- Read reputable self-help books and websites. Your doctor or therapist may be able to recommend books or websites to read.
- Locate helpful groups. Many organizations, such as the National Alliance on Mental Illness (NAMI) and the Depression and Bipolar Support Alliance, offer education, support groups, counseling and other resources to help with depression. Employee assistance programs and religious groups also may offer help for mental health concerns.
- Don't become isolated. Try to participate in social activities, and get together with family or friends regularly. Support groups for people with depression can help you connect to others facing similar challenges and share experiences.
- Learn ways to relax and manage your stress. Examples include meditation, progressive muscle relaxation, yoga and tai chi.
- Structure your time. Plan your day. You may find it helps to make a list of daily tasks, use sticky notes as reminders or use a planner to stay organized.
- Don't make important decisions when you're down. Avoid decision-making when you're feeling depressed, since you may not be thinking clearly.
Preparing for your appointment
You may see your primary care doctor, or your doctor may refer you to a mental health professional. Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for your appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins or other supplements that you're taking, including dosages
- Questions to ask your doctor or mental health professional
Take a family member or friend along, if possible, to help you remember all of the information provided during the appointment.
Some basic questions to ask your doctor include:
- Is depression the most likely cause of my symptoms?
- What are other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatment is likely to work best for me?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a psychiatrist or other mental health professional?
- What are the main side effects of the medications you're recommending?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first notice your symptoms of depression?
- How long have you felt depressed? Do you generally always feel down, or does your mood fluctuate?
- Does your mood ever swing from feeling down to feeling intensely happy (euphoric) and full of energy?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with depression or another mood disorder?
- What other mental or physical health conditions do you have?
- Do you drink alcohol or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
Major Depressive Disorder - StatPearls
Continuing Education Activity
Major depressive disorder (MDD) has been ranked as the third cause of the burden of disease worldwide in 2008 by WHO, which has projected that this disease will rank first by 2030.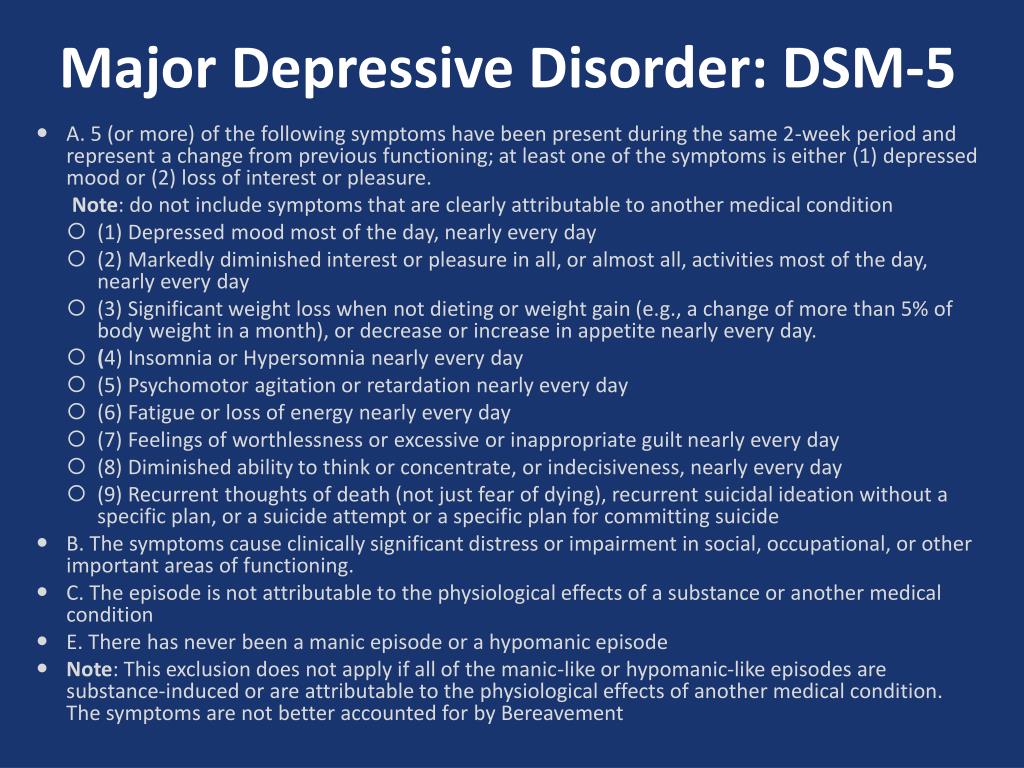 It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. This activity reviews the evaluation and management of major depressive disorder which is one of the main causes of disability in the world and highlights the role of the interprofessional team.
It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. This activity reviews the evaluation and management of major depressive disorder which is one of the main causes of disability in the world and highlights the role of the interprofessional team.
Objectives:
Identify the etiology of major depressive disorder.
Review the appropriate management of major depressive disorder.
Outline the typical presentation of a patient with major depressive disorder.
Review the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by major depressive disorder.
Access free multiple choice questions on this topic.
Introduction
Major depressive disorder (MDD) has been ranked as the third cause of the burden of disease worldwide in 2008 by WHO, which has projected that this disease will rank first by 2030.[1] It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. Per the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), an individual must have five of the above-mentioned symptoms, of which one must be a depressed mood or anhedonia causing social or occupational impairment, to be diagnosed with MDD. History of a manic or hypomanic episode must be ruled out to make a diagnosis of MDD. Children and adolescents with MDD may present with irritable mood.
Per DSM-5, other types of depression falling under the category of depressive disorders are:
Persistent depressive disorder, formerly known as dysthymia
Disruptive mood dysregulation disorder
Premenstrual dysphoric disorder
Substance/medication-induced depressive disorder
Depressive disorder due to another medical condition
Unspecified depressive disorder
Etiology
The etiology of Major depressive disorder is believed to be multifactorial, including biological, genetic, environmental, and psychosocial factors.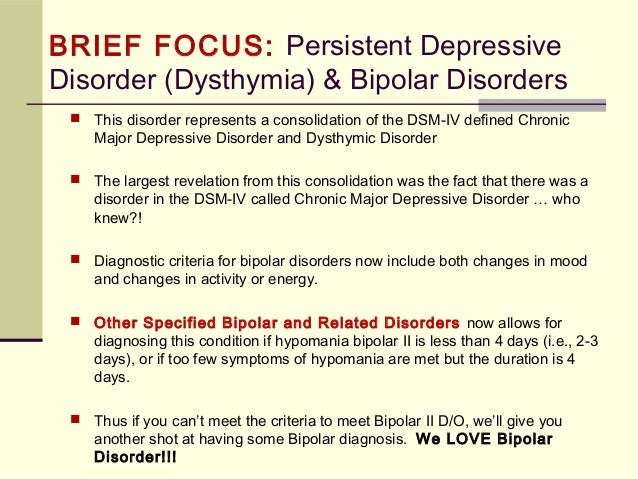 MDD was earlier considered to be mainly due to abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine. This has been evidenced by the use of different antidepressants such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, dopamine-norepinephrine receptor inhibitors in the treatment of depression. People with suicidal ideations have been found to have low levels of serotonin metabolites. However, recent theories indicate that it is associated primarily with more complex neuroregulatory systems and neural circuits, causing secondary disturbances of neurotransmitter systems.
MDD was earlier considered to be mainly due to abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine. This has been evidenced by the use of different antidepressants such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, dopamine-norepinephrine receptor inhibitors in the treatment of depression. People with suicidal ideations have been found to have low levels of serotonin metabolites. However, recent theories indicate that it is associated primarily with more complex neuroregulatory systems and neural circuits, causing secondary disturbances of neurotransmitter systems.
GABA, an inhibitory neurotransmitter, and glutamate and glycine, both of which are major excitatory neurotransmitters are found to play a role in the etiology of depression as well. Depressed patients have been found to have lower plasma, CSF, and brain GABA levels. GABA is considered to exert its antidepressant effect by inhibiting the ascending monoamine pathways, including mesocortical and mesolimbic systems.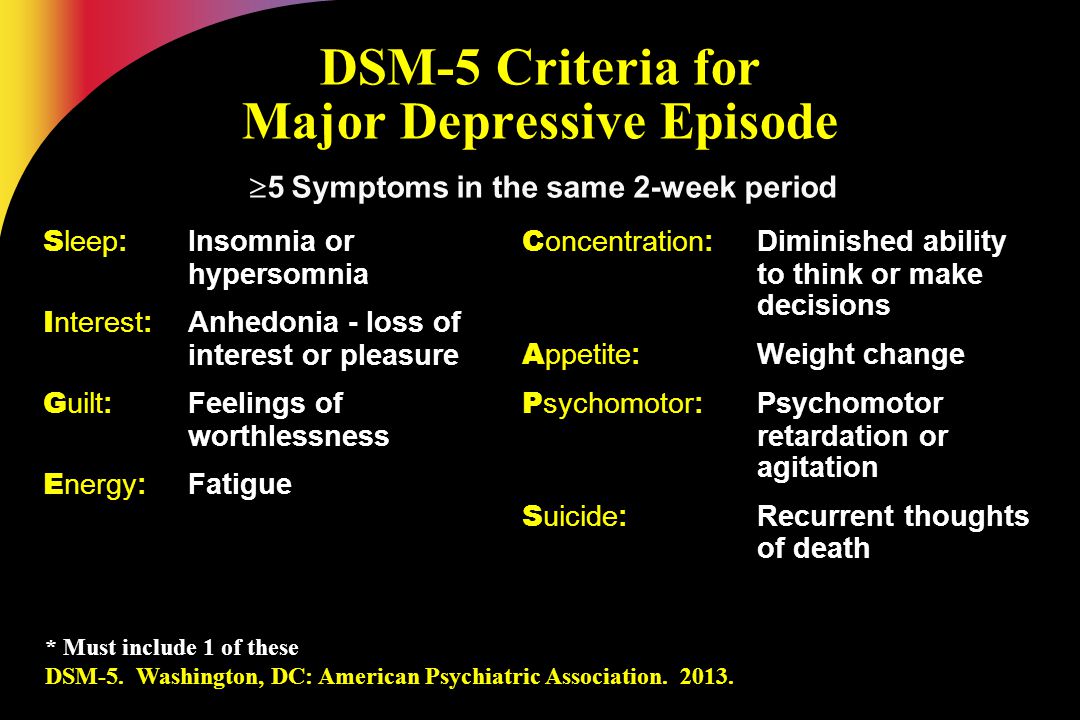 Drugs that antagonize NMDA receptors have been researched to have antidepressant properties. Thyroid and growth hormonal abnormalities have also been implicated in the etiology of mood disorders. Multiple adverse childhood experiences and trauma are associated with the development of depression later in life.[2][3]
Drugs that antagonize NMDA receptors have been researched to have antidepressant properties. Thyroid and growth hormonal abnormalities have also been implicated in the etiology of mood disorders. Multiple adverse childhood experiences and trauma are associated with the development of depression later in life.[2][3]
Severe early stress can result in drastic alterations in neuroendocrine and behavioral responses, which can cause structural changes in the cerebral cortex, leading to severe depression later in life. Structural and functional brain imaging of depressed individuals has shown increased hyperintensities in the subcortical regions, and reduced anterior brain metabolism on the left side, respectively. Family, adoption, and twin studies have indicated the role of genes in the susceptibility of depression. Genetic studies show a very high concordance rate for twins to have MDD, particularly monozygotic twins.[4] Life events and personality traits have shown to play an important role, as well.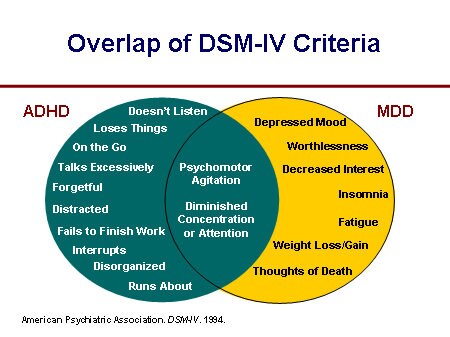 The learned helplessness theory has associated the occurrence of depression with the experience of uncontrollable events. Per cognitive theory, depression occurs as a result of cognitive distortions in persons who are susceptible to depression.
The learned helplessness theory has associated the occurrence of depression with the experience of uncontrollable events. Per cognitive theory, depression occurs as a result of cognitive distortions in persons who are susceptible to depression.
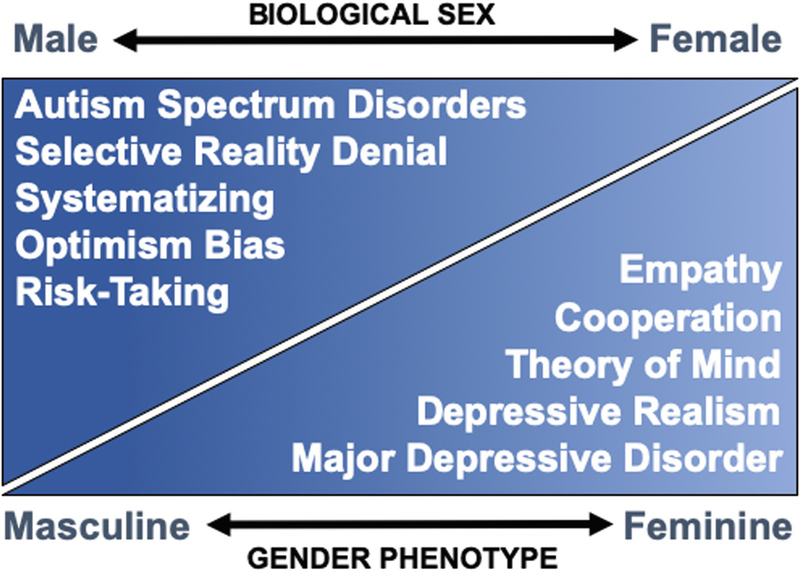
Epidemiology
Major depressive disorder is a highly prevalent psychiatric disorder. It has a lifetime prevalence of about 5 to 17 percent, with the average being 12 percent. The prevalence rate is almost double in women than in men.[5] This difference has been considered to be due to the hormonal differences, childbirth effects, different psychosocial stressors in men and women, and behavioral model of learned helplessness. Though the mean age of onset is about 40 years, recent surveys show trends of increasing incidence in younger population due to the use of alcohol and other drugs of abuse.
MDD is more common in people without close interpersonal relationships, and who are divorced or separated, or widowed. No difference in the prevalence of MDD has been found among races and socioeconomic status.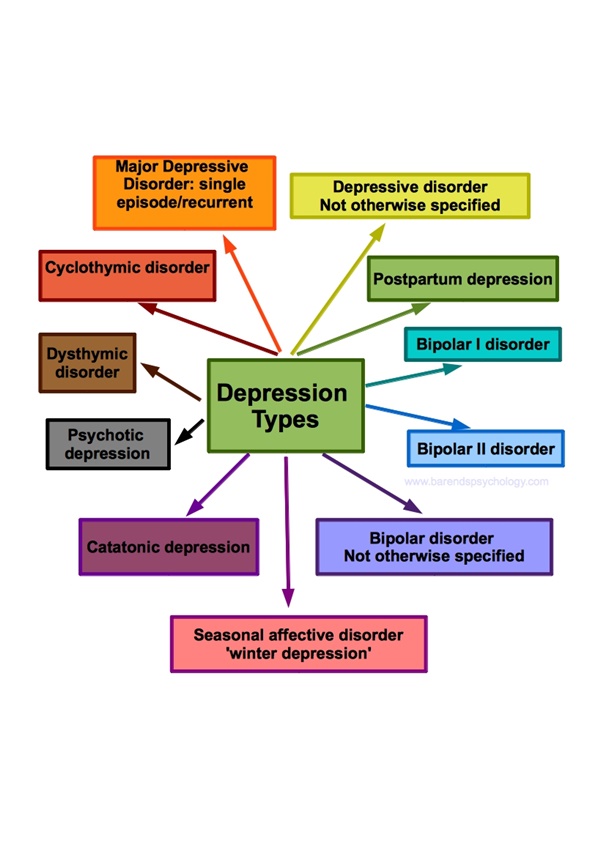 Individuals with MDD often have comorbid disorders such as substance use disorders, panic disorder, social anxiety disorder, and obsessive-compulsive disorder. The presence of these comorbid disorders in those diagnosed with MDD increases their risk of suicide. In older adults, depression is prevalent among those with comorbid medical illnesses.[6] Depression is found to be more prevalent in rural areas than in urban areas.
Individuals with MDD often have comorbid disorders such as substance use disorders, panic disorder, social anxiety disorder, and obsessive-compulsive disorder. The presence of these comorbid disorders in those diagnosed with MDD increases their risk of suicide. In older adults, depression is prevalent among those with comorbid medical illnesses.[6] Depression is found to be more prevalent in rural areas than in urban areas.
History and Physical
Major depressive disorder is a clinical diagnosis; it is mainly diagnosed by the clinical history given by the patient and mental status examination. The clinical interview must include medical history, family history, social history, and substance use history along with the symptomatology. Collateral information from a patient's family/friends is a very important part of psychiatric evaluation.
A complete physical examination, including neurological examination, should be performed. It is important to rule out any underlying medical/organic causes of a depressive disorder.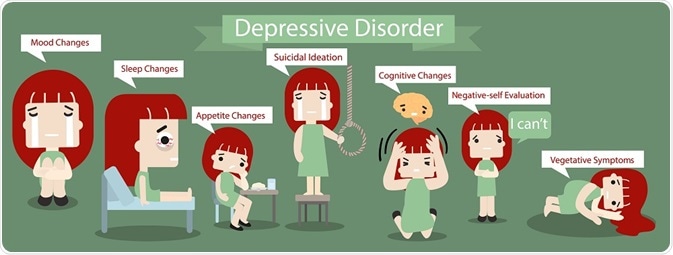 A full medical history, along with the family medical and psychiatric history, should be assessed. Mental status examination plays an important role in the diagnosis and evaluation of MDD.
A full medical history, along with the family medical and psychiatric history, should be assessed. Mental status examination plays an important role in the diagnosis and evaluation of MDD.
Evaluation
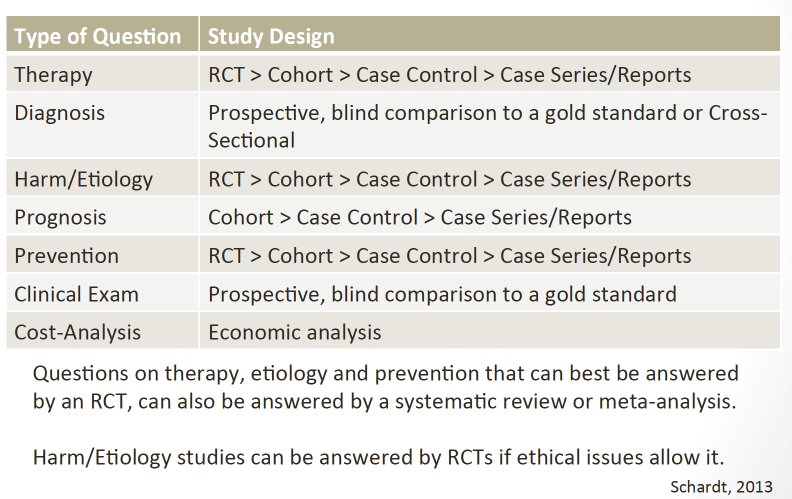
Although there is no objective testing available to diagnose depression, routine laboratory work including complete blood account with differential, comprehensive metabolic panel, thyroid-stimulating hormone, free T4, vitamin D, urinalysis, and toxicology screening is done to rule out organic or medical causes of depression.
Individuals with depression often present to their primary care physicians for somatic complaints stemming from depression, rather than seeing a mental health professional. In almost half of the cases, patients deny having depressive feelings, and they are often brought for treatment by the family or sent by the employer to be evaluated for social withdrawal and decreased activity. It is very important to evaluate a patient for suicidal or homicidal ideations at each visit.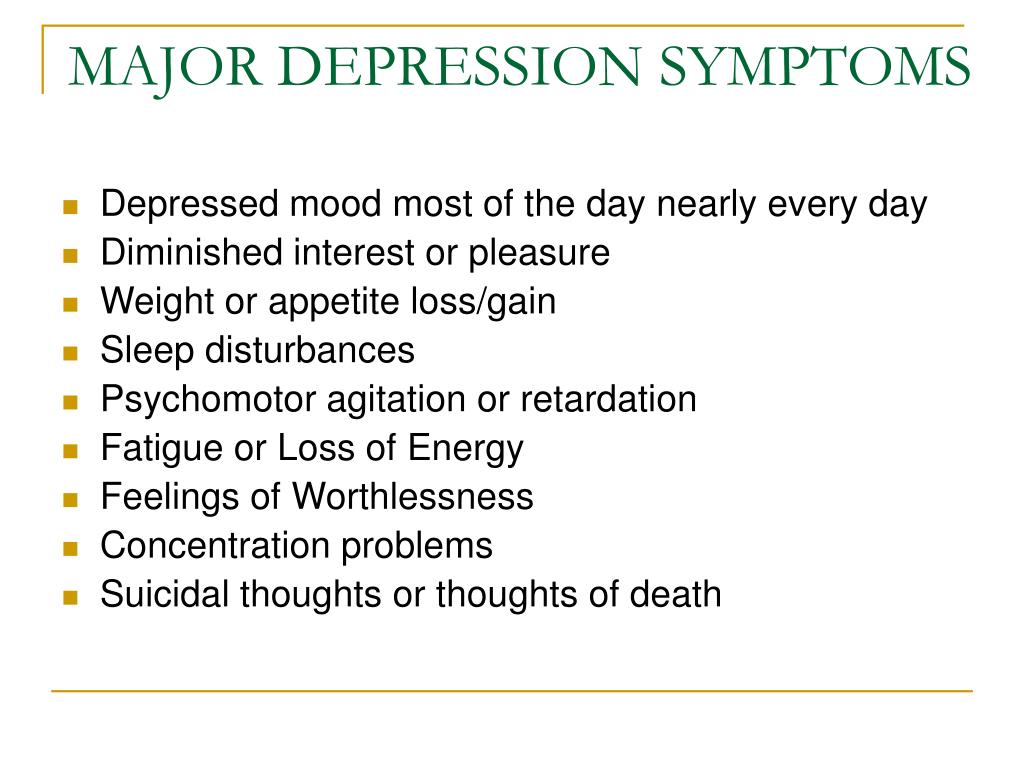
In primary care settings, the Patient Health Questionnaire-9 (PHQ-9), which is a self-report, standardized depression rating scale is commonly used for screening, diagnosing, and monitoring treatment response for MDD.[7] The PHQ-9 uses 9 items corresponding to the DSM-5 criteria for MDD and also assesses for psychosocial impairment. The PHQ-9 scores 0 to 27, with scores of equal to or more than 10, indicate a possible MDD.
In most hospital settings, the Hamilton Rating Scale for Depression (HAM-D), which is a clinician-administered depression rating scale is commonly used for the assessment of depression. The original HAM-D uses 21 items about symptoms of depression, but the scoring is based only on the first 17 items.
Other scales include the Montgomery-Asberg Depression Rating Scale (MADRS), the Beck Depression Inventory (BDI), the Zung Self-Rating Depression Scale, the Raskin Depression Rating Scale, and other questionnaires.
Treatment / Management
Major depressive disorder can be managed with various treatment modalities, including pharmacological, psychotherapeutic, interventional, and lifestyle modification.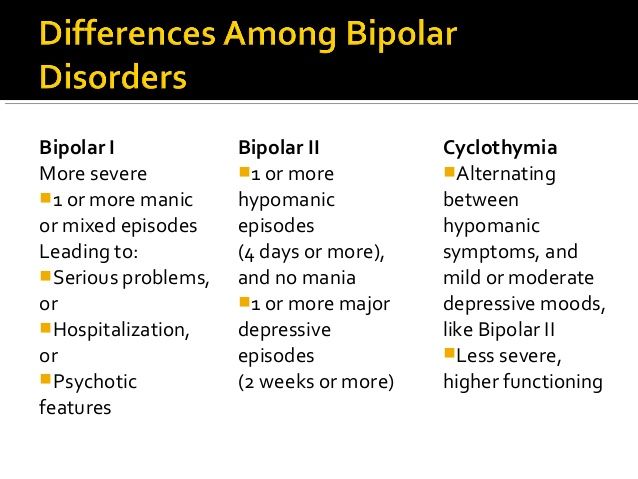 The initial treatment of MDD includes medications or/and psychotherapy. Combination treatment, including both medications and psychotherapy, has been found to be more effective than either of these treatments alone.[8][9] Electroconvulsive therapy is found to be more efficacious than any other form of treatment for severe major depression.[10]
The initial treatment of MDD includes medications or/and psychotherapy. Combination treatment, including both medications and psychotherapy, has been found to be more effective than either of these treatments alone.[8][9] Electroconvulsive therapy is found to be more efficacious than any other form of treatment for severe major depression.[10]
FDA-approved medications for the treatment of MDD are as follows: All antidepressants are equally effective but differ in side-effect profiles.
Selective serotonin reuptake inhibitors (SSRIs) include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. They are usually the first line of treatment and the most widely prescribed antidepressants.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) include venlafaxine, duloxetine, desvenlafaxine, levomilnacipran, and milnacipran. They are often used for depressed patients with comorbid pain disorders.
Serotonin modulators are trazodone, vilazodone, and vortioxetine.
Atypical antidepressants include bupropion and mirtazapine. They are often prescribed as monotherapy or as augmenting agents when patients develop sexual side-effects due to SSRIs or SNRIs.
Tricyclic antidepressants (TCAs) are amitriptyline, imipramine, clomipramine, doxepin, nortriptyline, and desipramine.
Monoamine oxidase inhibitors (MAOIs) available are tranylcypromine, phenelzine, selegiline, and isocarboxazid. MAOIs and TCAs are not commonly used due to the high incidence of side-effects and lethality in overdose.
Other medications include mood-stabilizers, antipsychotics which may be added to enhance antidepressant effects.
Psychotherapy
Cognitive-behavioral therapy
Interpersonal therapy
Electroconvulsive Therapy (ECT)
Acute suicidality
Severe depression during pregnancy
Refusal to eat/drink
Catatonia
Severe psychosis
Transcranial Magnetic Stimulation (TMS)
FDA-approved for treatment-resistant/refractory depression; for patients who have failed at least one medication trial
Vagus Nerve Stimulation (VNS)
FDA-approved as a long-term adjunctive treatment for treatment-resistant depression; for patients who have failed at least 4 medication trials
Esketamine
Nasal spray to be used in conjunction with an oral antidepressant in treatment-resistant depression; for patients who have failed other antidepressant medications
Differential Diagnosis
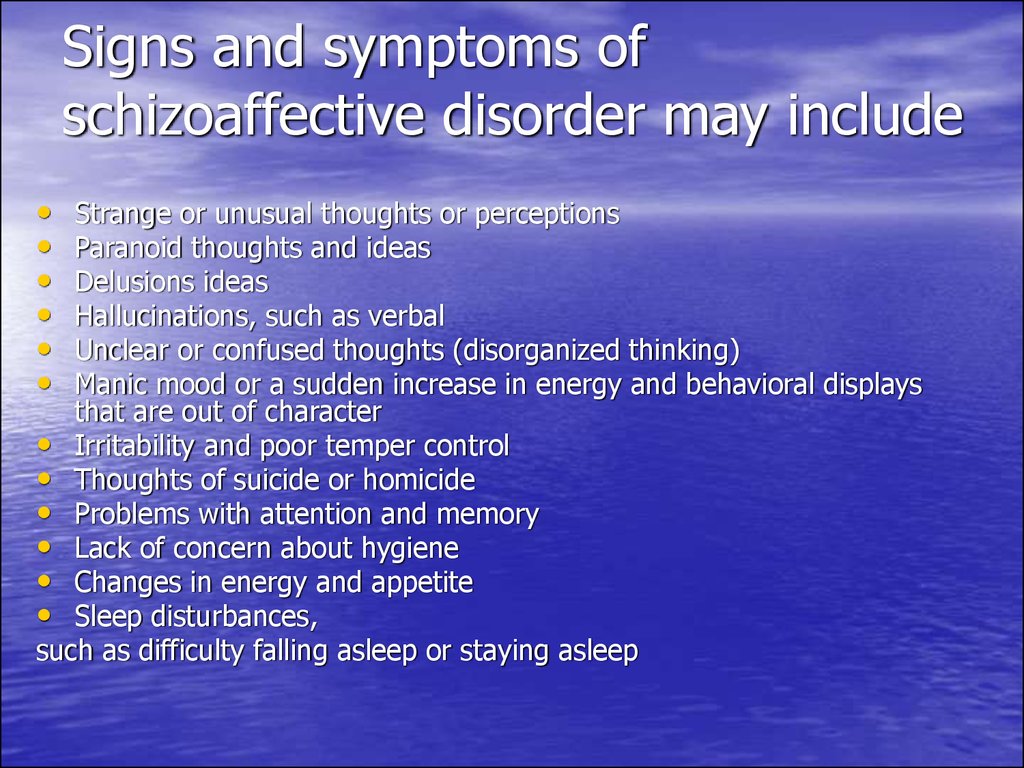
While evaluating for MDD, it is important to rule out depressive disorder due to another medical condition, substance/medication-induced depressive disorder, dysthymia, cyclothymia, bereavement, adjustment disorder with depressed mood, bipolar disorder, schizoaffective disorder, schizophrenia, anxiety disorders, and eating disorders for the appropriate management. Depressive symptoms can be secondary to the following causes:
Depressive symptoms can be secondary to the following causes:
Neurological causes such as cerebrovascular accident, multiple sclerosis, subdural hematoma, epilepsy, Parkinson disease, Alzheimer disease
Endocrinopathies such as diabetes, thyroid disorders, adrenal disorders
Metabolic disturbances such as hypercalcemia, hyponatremia
Medications/substances of abuse: steroids, antihypertensives, anticonvulsants, antibiotics, sedatives, hypnotics, alcohol, stimulant withdrawal
Nutritional deficiencies such as vitamin D, B12, B6 deficiency, iron or folate deficiency
Infectious diseases such as HIV and syphilis
Malignancies
Prognosis
Untreated depressive episodes in major depressive disorder can last from 6 to 12 months. About two-thirds of the individuals with MDD contemplate suicide, and about 10 to 15 percent commit suicide. MDD is a chronic, recurrent illness; the recurrence rate is about 50% after the first episode, 70% after the second episode, and 90% after the third episode.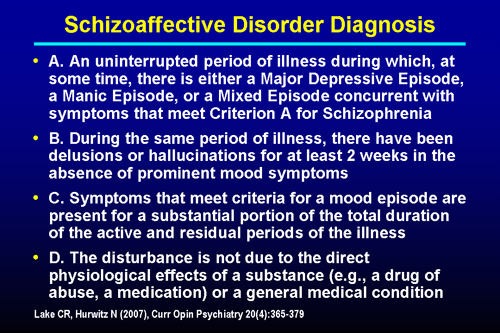 About 5 to 10 percent of the patients with MDD eventually develop bipolar disorder.[11] The prognosis of MDD is good in patients with mild episodes, the absence of psychotic symptoms, better treatment compliance, a strong support system, and good premorbid functioning. The prognosis is poor in the presence of a comorbid psychiatric disorder, personality disorder, multiple hospitalizations, and advanced age of onset.
About 5 to 10 percent of the patients with MDD eventually develop bipolar disorder.[11] The prognosis of MDD is good in patients with mild episodes, the absence of psychotic symptoms, better treatment compliance, a strong support system, and good premorbid functioning. The prognosis is poor in the presence of a comorbid psychiatric disorder, personality disorder, multiple hospitalizations, and advanced age of onset.
Complications
MDD is one of the leading causes of disability worldwide. It not only causes a severe functional impairment but also adversely affects the interpersonal relationships, thus lowering the quality of life. Individuals with MDD are at a high risk of developing comorbid anxiety disorders and substance use disorders, which further increases their risk of suicide. Depression can aggravate medical comorbidities such as diabetes, hypertension, chronic obstructive pulmonary disease, and coronary artery disease. Depressed individuals are at high risk of developing self-destructive behavior as a coping mechanism. MDD is often very debilitating if left untreated.
MDD is often very debilitating if left untreated.
Deterrence and Patient Education
Patient education has a profound impact on the overall outcome of major depressive disorder. Since MDD is one of the most common psychiatric disorders causing disability worldwide and people in different parts of the world are hesitant to discuss and seek treatment for depression due to the stigma associated with mental illness, educating patients is very crucial for their better understanding of the mental illness and better compliance with the mental health treatment. Family education also plays an important role in the successful treatment of MDD.
Enhancing Healthcare Team Outcomes
An interdisciplinary approach is essential for the effective and successful treatment of MDD. Primary care physicians and psychiatrists, along with nurses, therapists, social workers, and case managers, form an integral part of these collaborated services. In the majority of cases, PCPs are the first providers to whom individuals with MDD present mostly with somatic complaints.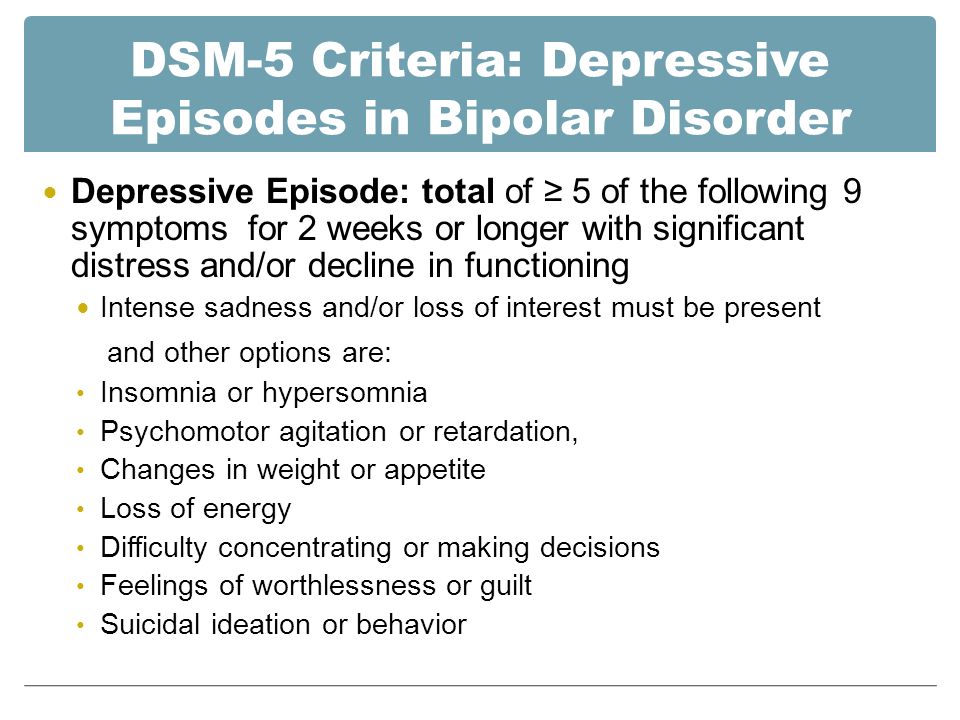 Depression screening in primary care settings is very imperative. The regular screening of the patients using depression rating scales such as PHQ-9 can be very helpful in the early diagnosis and intervention, thus improving the overall outcome of MDD. Psychoeducation plays a significant role in improving patient compliance and medication adherence. Recent evidence also supports that lifestyle modification, including moderate exercises, can help to improve mild-to-moderate depression. Suicide screening at each psychiatric visit can be helpful to lower suicide incidence. Since patients with MDD are at increased risk of suicide, close monitoring, and follow up by mental health workers becomes necessary to ensure safety and compliance with mental health treatment. The involvement of families can further add to a better outcome of the overall mental health treatment. Meta-analyses of randomized trials have shown that depression outcomes are superior when using collaborative care as compared with usual care.
Depression screening in primary care settings is very imperative. The regular screening of the patients using depression rating scales such as PHQ-9 can be very helpful in the early diagnosis and intervention, thus improving the overall outcome of MDD. Psychoeducation plays a significant role in improving patient compliance and medication adherence. Recent evidence also supports that lifestyle modification, including moderate exercises, can help to improve mild-to-moderate depression. Suicide screening at each psychiatric visit can be helpful to lower suicide incidence. Since patients with MDD are at increased risk of suicide, close monitoring, and follow up by mental health workers becomes necessary to ensure safety and compliance with mental health treatment. The involvement of families can further add to a better outcome of the overall mental health treatment. Meta-analyses of randomized trials have shown that depression outcomes are superior when using collaborative care as compared with usual care.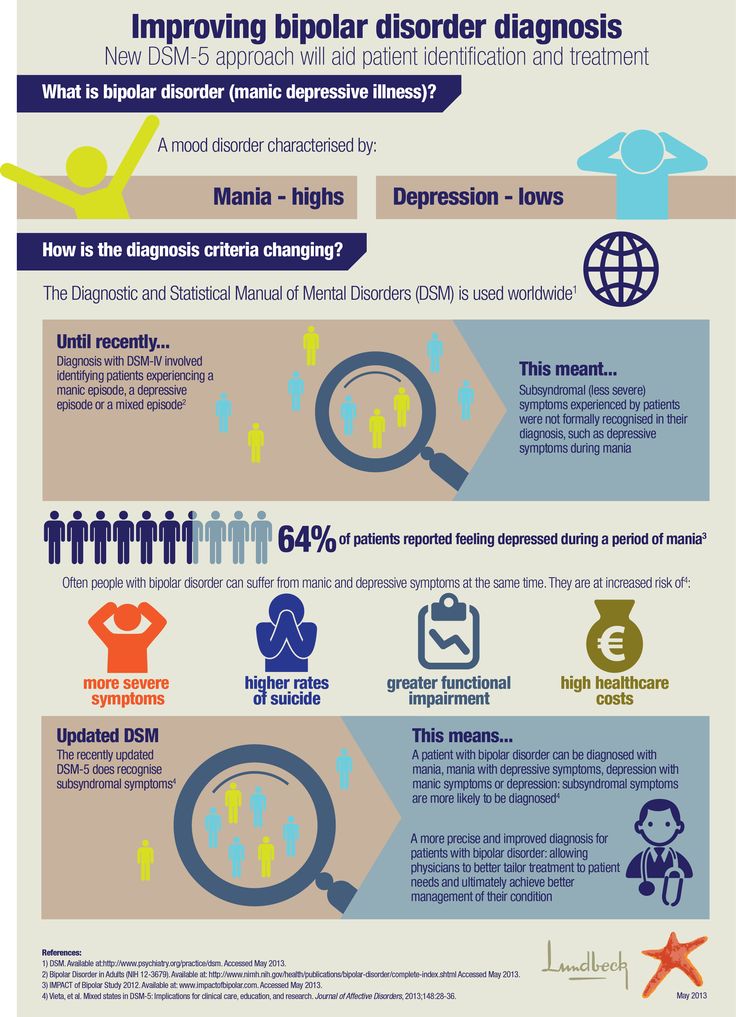 [12]
[12]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Malhi GS, Mann JJ. Depression. Lancet. 2018 Nov 24;392(10161):2299-2312. [PubMed: 30396512]
- 2.
Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, Gillespie CF, Berg T, Evces M, Newport DJ, Stowe ZN, Heim CM, Nemeroff CB, Schwartz A, Cubells JF, Ressler KJ. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008 Feb;65(2):190-200. [PMC free article: PMC2443704] [PubMed: 18250257]
- 3.
Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010 Feb;67(2):113-23. [PMC free article: PMC2822662] [PubMed: 20124111]
- 4.
Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000 Oct;157(10):1552-62. [PubMed: 11007705]
- 5.
Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, Mortensen PB, Eaton WW. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014 May;71(5):573-81. [PubMed: 24806211]
- 6.
Lyness JM, Niculescu A, Tu X, Reynolds CF, Caine ED. The relationship of medical comorbidity and depression in older, primary care patients. Psychosomatics. 2006 Sep-Oct;47(5):435-9. [PubMed: 16959933]
- 7.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003 Nov;41(11):1284-92. [PubMed: 14583691]
- 8.
Cuijpers P, Dekker J, Hollon SD, Andersson G. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis.
 J Clin Psychiatry. 2009 Sep;70(9):1219-29. [PubMed: 19818243]
J Clin Psychiatry. 2009 Sep;70(9):1219-29. [PubMed: 19818243]- 9.
Cuijpers P, van Straten A, Warmerdam L, Andersson G. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety. 2009;26(3):279-88. [PubMed: 19031487]
- 10.
Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J ECT. 2004 Mar;20(1):13-20. [PubMed: 15087991]
- 11.
Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, McGorry PD, Scott J, Berk M, Cotton SM. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. 2017 Apr;135(4):273-284. [PubMed: 28097648]
- 12.
Sighinolfi C, Nespeca C, Menchetti M, Levantesi P, Belvederi Murri M, Berardi D. Collaborative care for depression in European countries: a systematic review and meta-analysis.
 J Psychosom Res. 2014 Oct;77(4):247-63. [PubMed: 25201482]
J Psychosom Res. 2014 Oct;77(4):247-63. [PubMed: 25201482]
Types of depression - iFightDepression [EN]
There are different types of depression, which are different.
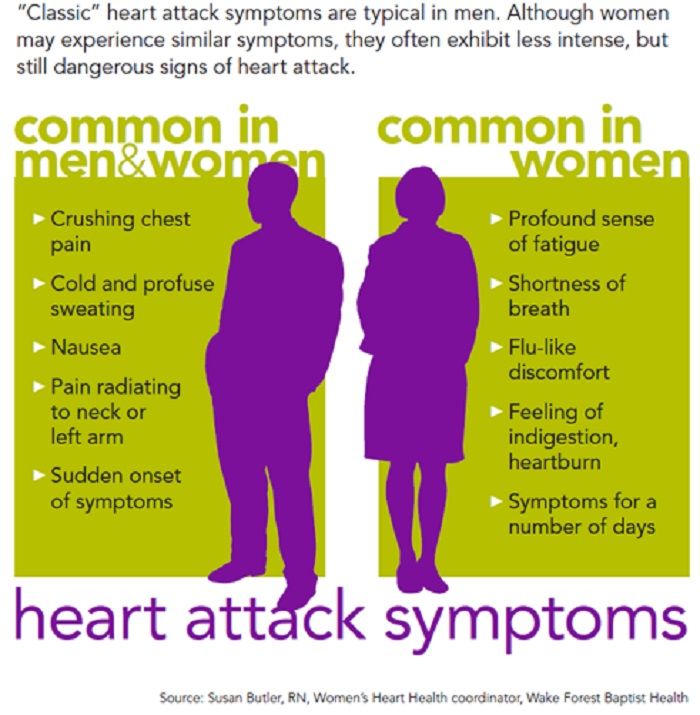
Signs and symptoms vary in number, time, severity and frequency, but are generally very similar. Because different types of depression are treated differently, it is important to pinpoint the type of depression. Depending on gender, age and cultural characteristics, people have different symptoms and severity of depression.
Neurotic, reactive (minor) depression is treated with psychotherapy.
Somatic and psychotic - medication. These terms are used by psychiatrists.
Studies have shown that depression has a phasic course. Periods of normal mood alternate with depressive episodes. Sometimes, instead of a depressive phase,
there may be a manic phase, which is manifested by irritability and high mood. If so, then it is not depression, but bipolar disorder (a more serious illness).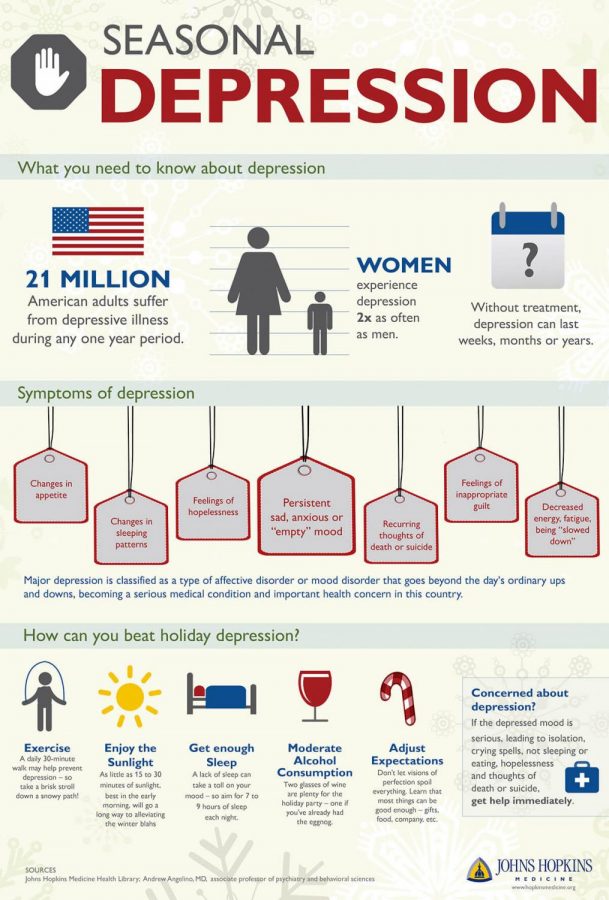
1. Depressive episode
The most common and typical form of depression is the depressive episode. An episode lasts from a few weeks to a year, but is always longer than 2 weeks. A single depressive episode is called a unipolar episode. Approximately one third of affected people experience only one episode, or "phase", during their lifetime. However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
2. Intermittent (recurrent) depressive disorder
When a depressive episode recurs, it is recurrent depressive disorder or major depressive disorder, which usually begins in adolescence or early adulthood. With this kind of depression, depressive phases, which can last from several months to several years, alternate with phases of normal mood. This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
This is the so-called "classic" or "clinical" depression.
3. Dysthymia
Dysthymia presents with milder and less severe symptoms than a depressive episode or recurrent depression. However, the disorder is permanent, with symptoms lasting much longer, at least 2 years, sometimes decades, which is why it is called "chronic depression". This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
4. Bipolar depression, type I
This is the type of depression in bipolar disorder, formerly called manic-depressive illness, and is less common than unipolar depression. It consists of alternating depressive phases, phases of normal mood and so-called manic phases.
Manic phases are characterized by excessively high mood associated with hyperactivity, anxiety, and decreased need for sleep.
Mania affects thinking, judgment and social behavior causing serious problems and difficulties.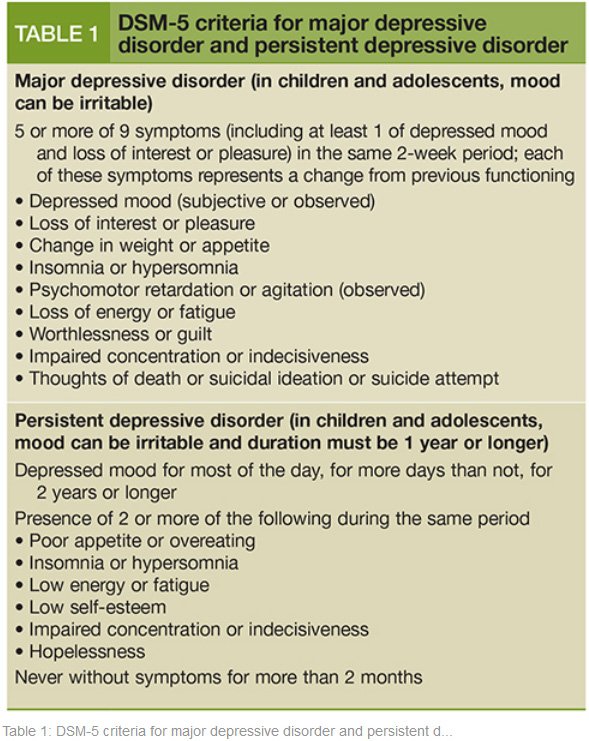 When a person is in a manic phase, he makes frequent casual unsafe sex, makes unwise financial decisions. After a manic episode, such people often experience depression.
When a person is in a manic phase, he makes frequent casual unsafe sex, makes unwise financial decisions. After a manic episode, such people often experience depression.
The best way to describe these "emotional upheavals" is "to be on top of the world and fall into the depths of despair".
Symptoms of the phases of depression in bipolar disorder are sometimes difficult to distinguish from unipolar depression.
5. Bipolar depression type II
More like recurrent depressive disorder than bipolar disorder. In this disorder, multiple depressive phases alternate with phases of mania, but with less pronounced euphoria. During these phases, family and loved ones may even mistakenly assume that the person is doing well.
6. Mixed anxiety-depressive disorder
In anxiety-depressive disorder, the clinical picture is very similar to depression, however, in depression, depressive syndromes always come first. In this case, both anxious and depressive symptoms are evenly combined.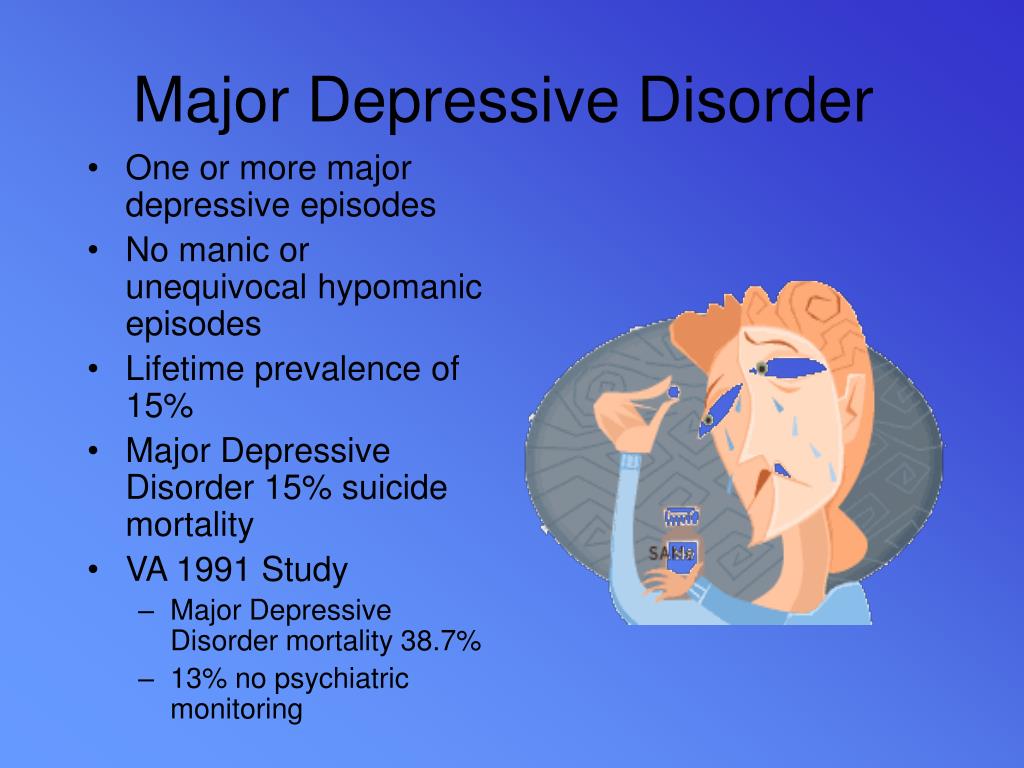
7. Depressive psychotic episode
A special form of depressive episode is psychotic or delusional depression. Psychosis is a condition in which people see or hear things that do not exist (hallucinations) and/or have false ideas or beliefs (delusions). There are various types of delusions such as self-accusation for no reason (delusion of guilt), financial ruin (delusions of poverty), feeling of an incomprehensible illness (hypochondriac delusions). People with delusional depression almost always require inpatient psychiatric treatment. Psychotic episodes can be either unipolar or bipolar.
8. Atypical depression
This type of depression is characterized by hypersensitivity and mood swings, overeating and drowsiness, panic attacks. This type of depression is mild and can be bipolar.
9. Seasonal depressive disorder
This type of depression is similar to atypical depression and comes on seasonally with climate change, usually in autumn or winter.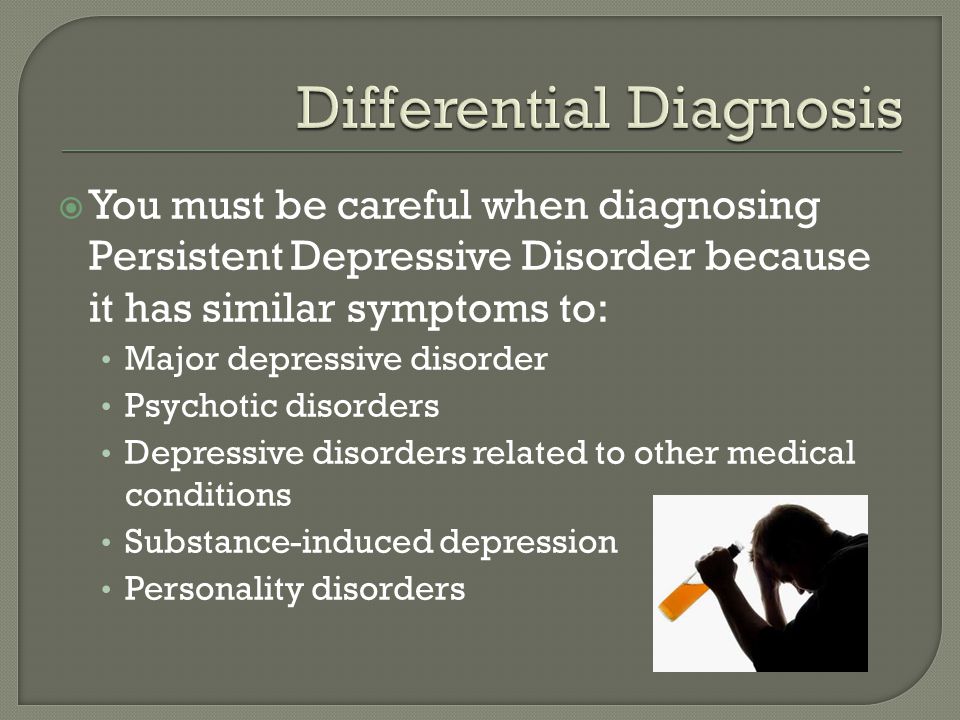 Usually, when the season ends, people return to normal functioning again.
Usually, when the season ends, people return to normal functioning again.
10. Brief depressive disorder
This is a milder variant of depression that more often affects young people and is characterized by short depressive episodes lasting less than 2 weeks.
Types of depression and their classification
Depression - what is it, what is its etiology, what is the relevance of depressive disorders. Symptoms and classification of depression. What are the characteristics of certain types of depression? These topics formed the basis of our interview with the Chief Physician of the Health Harmony Medical Center, psychiatrist, psychiatrist-narcologist and psychotherapist Vladislav Sipovich.
What is depression, how common is it and what are its causes?
Depression in Latin means to suppress, put pressure on something. As a medical term, it is used to define a mental disorder characterized by low mood, manifested by a depressed, depressed, sad, anxious, or indifferent state.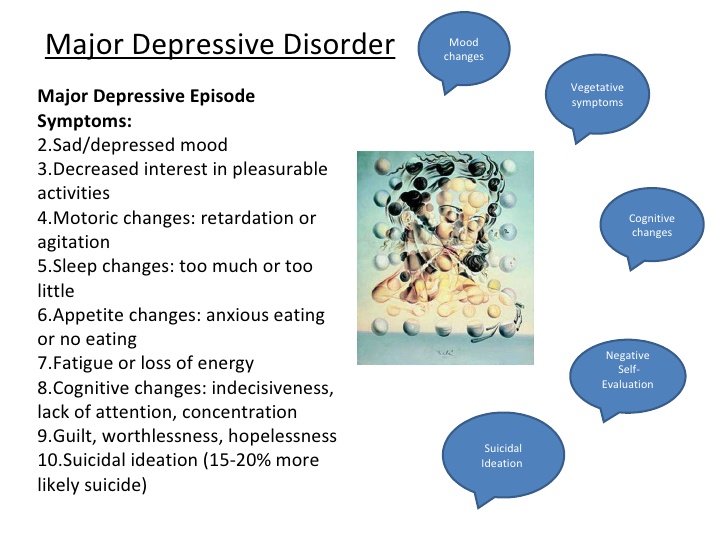 Accompanied by anhedonia - a reduced or completely lost ability to enjoy life and have fun.
Accompanied by anhedonia - a reduced or completely lost ability to enjoy life and have fun.
The main symptoms of depression are:
• Low self-esteem.
• Loss of interest in normal activities.
• Exaggerated sense of guilt.
• Decreased mood.
• Pessimistic outlook on life.
• Fatigue and lack of energy.
• Violation of concentration, sleep and appetite.
• Suicidal thoughts.
Severe forms of depression are characterized by the so-called depressive triad:
• Low mood.
• Inhibited thinking.
• Decreased motor activity with a predominance of inhibition processes.
Temporary depression can be a normal response to negative life circumstances such as job loss, divorce, financial loss, illness, or bereavement. In such cases, a person sometimes begins to abuse alcohol, drugs, antidepressants and other psychoactive substances.
Depressive disorder may be a symptom of physical illness or a side effect of certain medications.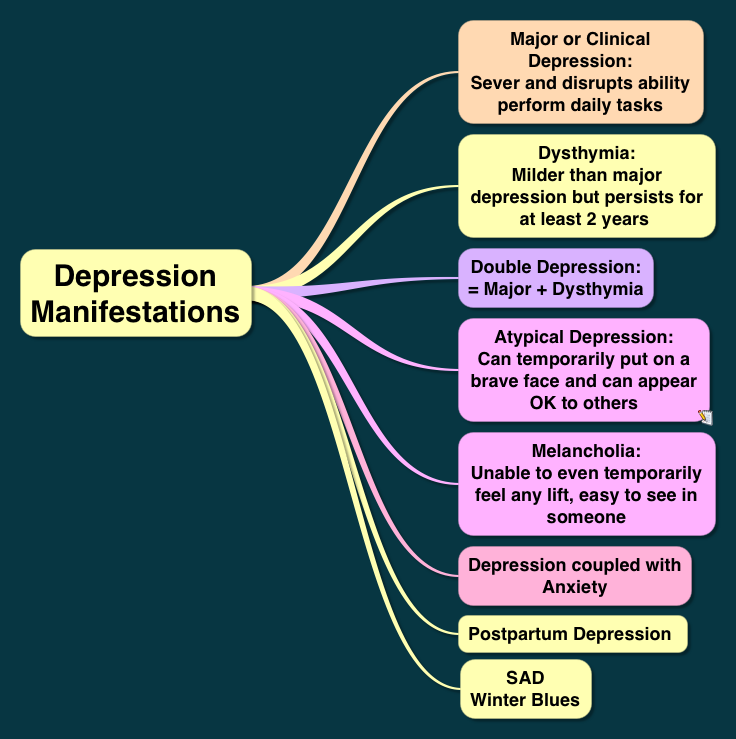 If the cause of depression is not identified, then it is differentiated as endogenous. Screening for types of depression is done using self-assessment tests such as the Zang or Beck scale, a large depression questionnaire. By the way, the main symptoms of depression were described by Hippocrates, who defined this condition as melancholy.
If the cause of depression is not identified, then it is differentiated as endogenous. Screening for types of depression is done using self-assessment tests such as the Zang or Beck scale, a large depression questionnaire. By the way, the main symptoms of depression were described by Hippocrates, who defined this condition as melancholy.
The relevance of identifying and diagnosing depression is explained not only by the fact that it significantly reduces the quality of life of a person, but is also the most common mental disorder. Every tenth person over the age of 40 suffers from it, and 2/3 of them are women. Children are less susceptible to depression, but nevertheless, 5% of adolescents aged 10-16 experience a depressive disorder. Depression is a major cause of morbidity and disability in children and young people, and significantly increases the risk of suicide in these age groups.
The etiology of depression is multifactorial. The main causes can be combined into the following groups:
• Social and psychological leading to the so-called reactive (psychogenic) depression.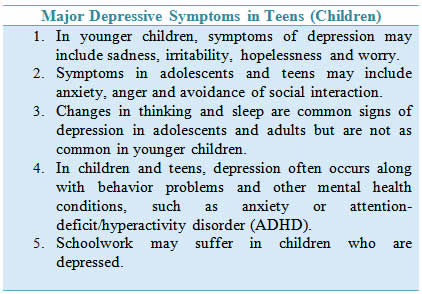 Depression in this case develops as a response to the external impact of events, situations and stress.
Depression in this case develops as a response to the external impact of events, situations and stress.
• Somatic , more precisely somatogenic. An example is Alzheimer's disease, atherosclerosis of the cerebral arteries, TBI, viral infections, endocrinological disorders, especially in hypothyroidism (7 times higher than in healthy people), etc.
• Iatrogenic developing in response to taking certain drugs - corticosteroids, benzodiazepines, neuroleptics, sedatives and hypnotics. This group also includes depressions provoked by the abuse of alcohol, cocaine, opiates, and other psychostimulants. They usually heal on their own or go away when the drugs are stopped.
• Endogenous , arising without any apparent external cause, as if from within the body. About 35% of depressions develop autochthonously without any external influences.
Risk factors for depression are:
• Dramatic childhood experiences including abuse, loss of parents or their antisocial behavior, physical anomalies in the child, bullying and cyberbullying by peers or teachers.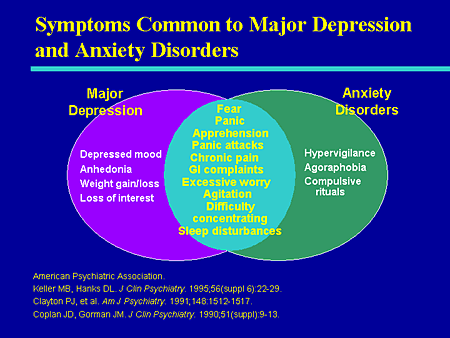
• Personal characteristics of the patient , for example, perfectionism.
• Periods of hormonal adjustment - adolescence, menopause, as well as pregnancy and childbirth. About 10% of pregnant women may suffer from depression, and postpartum depression occurs in 12-16% of women who have given birth.
As for the neurobiological mechanisms of the development of major depressive disorder, there are several hypotheses, among which the most popular is monoamine, linking depression with a lack of amine neurotransmitters - serotonin, norepinephrine, dopamine. This theory has not yet received a convincing evidence base.
There is also an evolutionary theory of depression, which considers it as a survival mechanism and the least painful solution to urgent problems. Avoidance behavior in depression helps to solve problems such as:
• avoid unpleasant moments in the process of understanding negative situations and making often compelled compromise decisions;
• adapt to unpleasant circumstances, and in a social environment in which there are opportunities for avoiding them.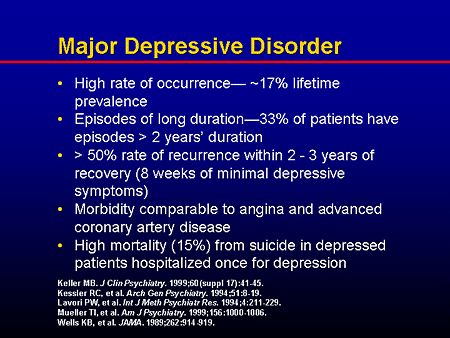
Also noteworthy is such a type of depression as seasonal affective disorder, which develops as a result of prolonged sunless weather in autumn and winter, as well as in people who are in rooms with twilight lighting for a long time. Seasonal depression is treated with walks in the sun or light therapy. Perhaps the seasonality of the disease is due to a deficiency in the formation of vitamin D in the skin with a lack of sunlight in the UV spectrum.
According to the cognitive model of depression, it is caused by dysfunctional beliefs that are formed in childhood and are activated in adulthood under certain life circumstances. According to this theory, the distortion of thinking in depression manifests itself in the form of a cognitive triad:
• Low self-esteem, confidence in one's own worthlessness.
• Low opinion of the surrounding reality.
• Disbelief in one's own "bright" future.
Distorted thinking and ideas also manifest themselves in the “tyranny of duties” characteristic of depressive patients in the form of a firm conviction that they should know everything, understand, foresee, make quick and correct decisions, etc.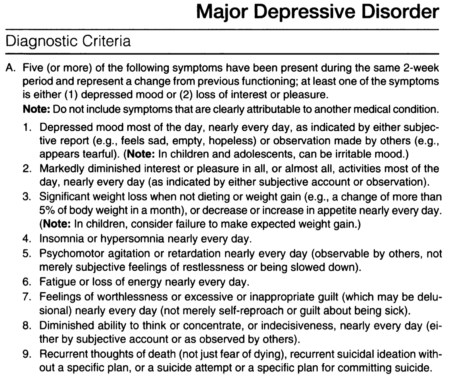 At the same time, there are random inferences, exaggerations, generalization or selective abstraction from events and situations.
At the same time, there are random inferences, exaggerations, generalization or selective abstraction from events and situations.
What is the diagnosis of depression based on?
Difficulties in diagnosing depressive disorders are primarily due to the fact that patients try not to advertise their condition and often hide the symptoms of depression. This is explained by the fear of prescribing antidepressants and the occurrence of side effects from taking them, as well as fixing the diagnosis in the medical record, followed by referral to a psychiatrist or psychotherapist and a possible report to the employer.
Depression is diagnosed in the following areas:
• Screening for the presence of a disorder.
• Test and clinician's clinical assessment.
• Determination of the severity of individual symptoms - anxiety, anhedonia, suicidal tendencies.
As I said, various tests (Zange or Beck scale) and questionnaires (short and long) are used to screen and determine the severity of depression.
Clinical judgment is important in the choice of treatment and management. Based mainly on medical experience, the role of instrumental or laboratory criteria is relevant only in the diagnosis of somatic depression caused by diseases of an infectious, neurological, endocrinological nature. To differentiate the latter, it is important in depressed patients to conduct an examination of the thyroid gland to diagnose hypo- or hyperthyroidism.
According to ICD-10 (International Classification of Diseases, 10th Revision), symptoms of depression are divided into major and minor. To make a diagnosis, you must have 2 main and at least 3 additional.
The main (typical) symptoms of depression are:
• Unreasonably depressed mood for more than 2 weeks.
• Anhedonia with loss of interest in life and inability to enjoy previously pleasant moments and activities.
• Loss of strength, increased fatigue, stably fixed for a month.
Additional symptoms include:
• Pessimistic outlook on life.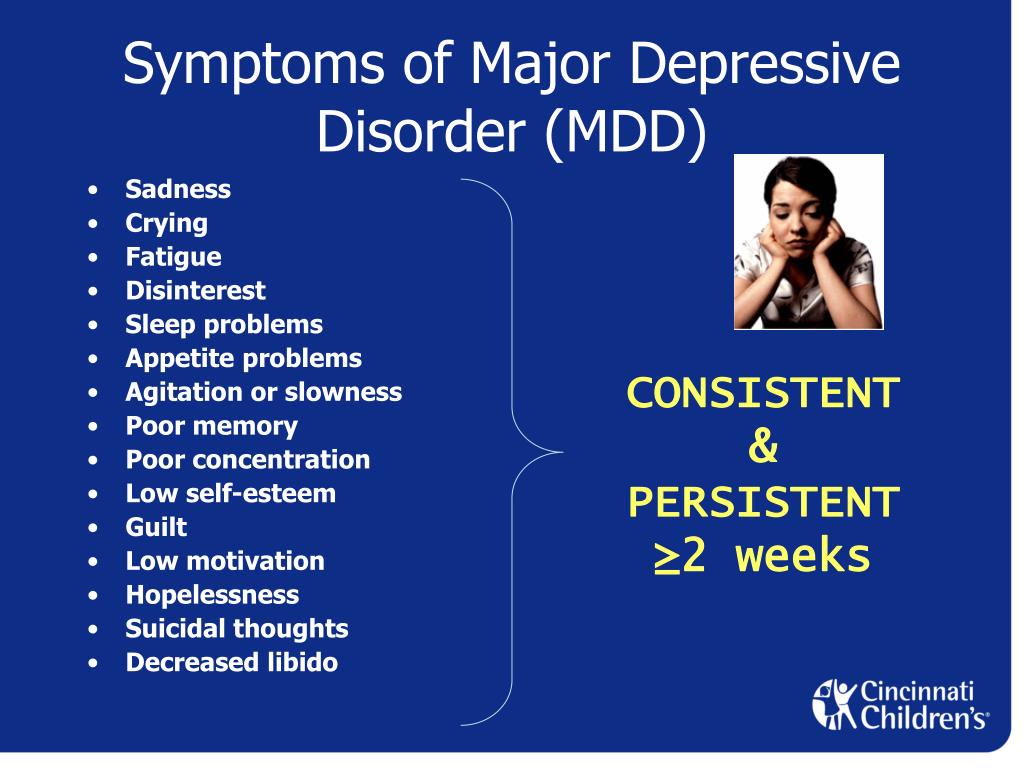
• Anxiety, fear, sense of worthlessness and pronounced guilt.
• Low self-esteem.
• Decreased ability to concentrate and make decisions.
• Appetite disorders, decreased or increased weight.
• Sensation of a sweet taste in the mouth (glycogeusia).
• Suicidal thoughts and obsessive thoughts about death.
• Sleep disorders in the form of insomnia or, conversely, drowsiness and oversleeping.
The duration of symptoms for a reliable diagnosis should be at least 2 weeks, although a shorter period of their manifestation is allowed with especially pronounced severity and intensity.
According to the diagnostic criteria of the American classification of mental illness DSM-IV-TR, it is necessary to identify and save for 2 weeks 5 of these 9-ty symptoms:
• Suppressed depressive mood, which in adolescence may be manifested by irritability.
• Anhedonia.
• Increase or decrease in appetite and weight.
• Insomnia - difficulty falling asleep, dissatisfaction with the quality of sleep, as well as hypersomnia (sleep intoxication), manifested by a difficult transition from sleep to wakefulness.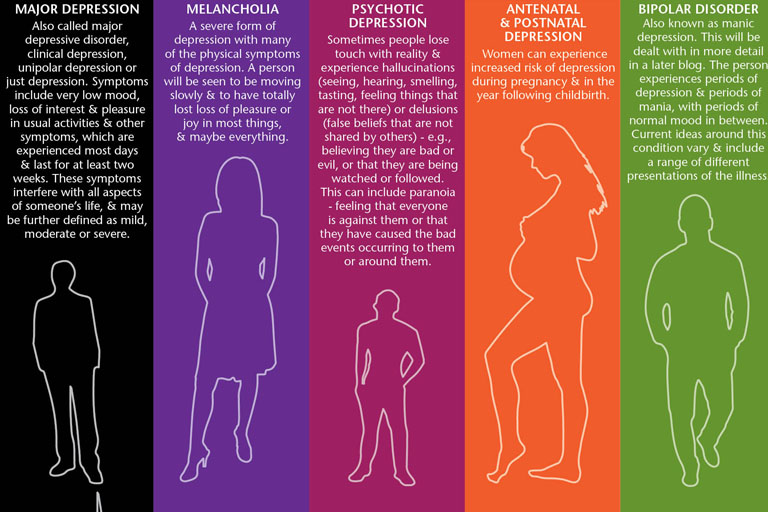
• Psychomotor inhibition or excitation.
• Inhibition of thought processes and decreased attention, especially the ability to concentrate.
• Feelings of insignificance, low self-esteem, inflated guilt.
• Increased fatigue, loss of energy, decreased vitality.
• Persistent thoughts of death and suicide, marked suicidal tendencies.
As part of the 5 significant symptoms, at least one of the 2 main symptoms must be present - anhedonia and / or depressive mood.
How are the different types of depression classified?
The classification of the main types of depression is based on the etiology, clinical picture, prevailing symptoms, frequency of occurrence, duration of the course and other features.
If the mood remains stably lowered, then such depressive disorders are referred to as unipolar, if episodes of depression are interspersed with manic (enthusiastic mood and arousal) - they speak of mixed or bipolar depression, more likely related to bipolar disorder (OCD).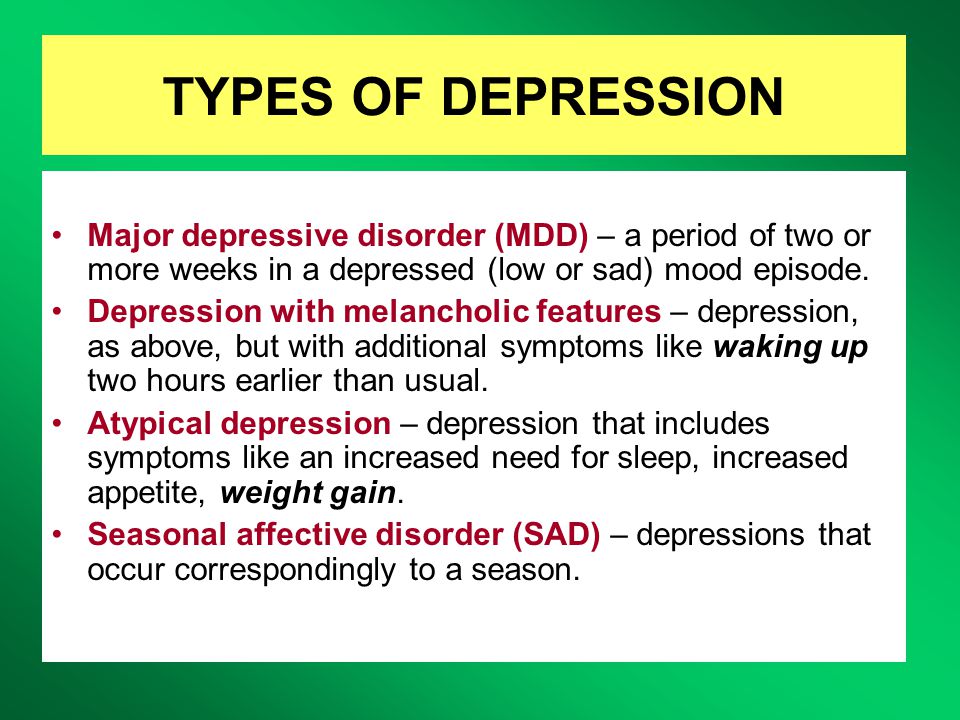
The following types of unipolar depression are classified in the DSM-IV:
• Major depressive disorder (clinical depression) with all of the characteristic symptoms described above.
• Minor depression in which not all symptoms of clinical depression are present, but 2 major depression criteria are present for at least 2 weeks.
• Atypical form , in which, along with the typical symptoms of a depressive disorder, there are also atypical ones - increased appetite, weight gain, emotional reactivity.
• Recurrent transient form depression (RBD) with a characteristic course. Episodes develop about once a month and last less than 2 weeks, most often 2-3 days. Diagnosis requires regular occurrence of episodes throughout the year without reference to MC in women.
• Dysthymia is a mild form of mood disorder characterized by milder and less severe symptoms than clinical depression.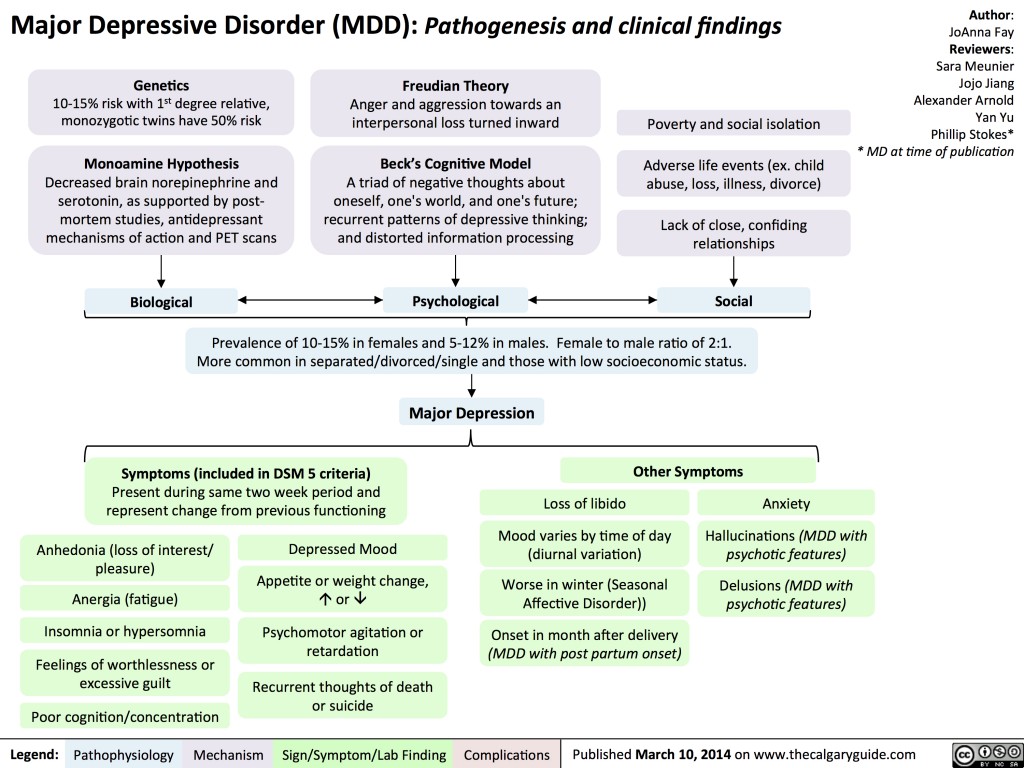 Despite this, it has a protracted course, lasts much longer, at least 2 years, sometimes stretches for decades. Therefore, it is often referred to as chronic depression. Sometimes it develops into major depressive disorder, in which case it is called double depression.
Despite this, it has a protracted course, lasts much longer, at least 2 years, sometimes stretches for decades. Therefore, it is often referred to as chronic depression. Sometimes it develops into major depressive disorder, in which case it is called double depression.
• In domestic medicine, the concept of 9 is widespread0095 vital, i.e. life depression . It is characterized by pronounced melancholy and anxiety, which can manifest itself even at the physical level, for example, pain in the solar plexus, lack of need for food and sleep. Therefore, it is also called "dreary depression." It proceeds quite hard, but has a favorable prognosis, as it responds well to treatment with antidepressants.
• The resistant form , in contrast to the vital form, does not give a pronounced clinical effect when even two 4-week courses of antidepressants are used.
• Anxiety and depressive disorder . Reminds depressive, but in contrast to it, anxiety and depressive syndromes in the clinical picture are equally represented.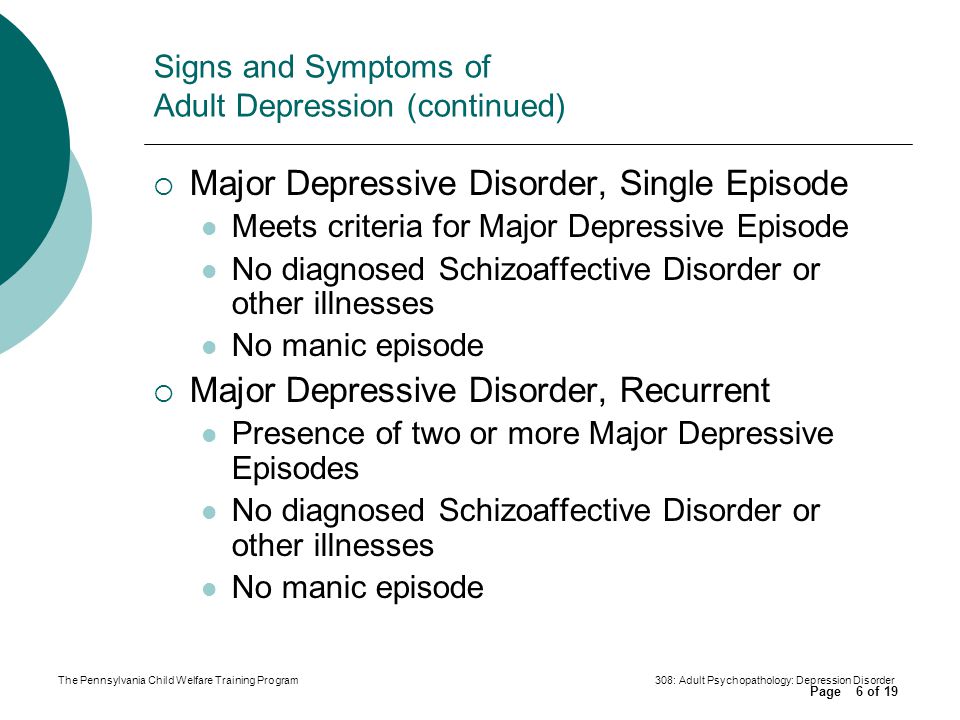
• The neurotic form of is characterized by low self-esteem, lack of confidence in one's strengths and abilities, and an acute sense of guilt.
• Autonomic depression with severe physical symptoms such as tachycardia, BP fluctuations, tinnitus.
• Masked with hidden, mild signs of apathy, with a desire for solitude and self-isolation, reduced interest in life. It masquerades as chronic fatigue.
• Asthenic . It proceeds with weakness, lethargy, sleep disturbances, emotional instability, aggravated by stress, physical and mental overload.
• Postpartum . It develops 10-14 days after childbirth against the background of hormonal changes, anxiety for the baby, constant lack of sleep and excessive fatigue.
• Somatogenic . It is a consequence of endocrine disorders, neoplasms, brain injuries, impaired blood supply, and some psychotic conditions.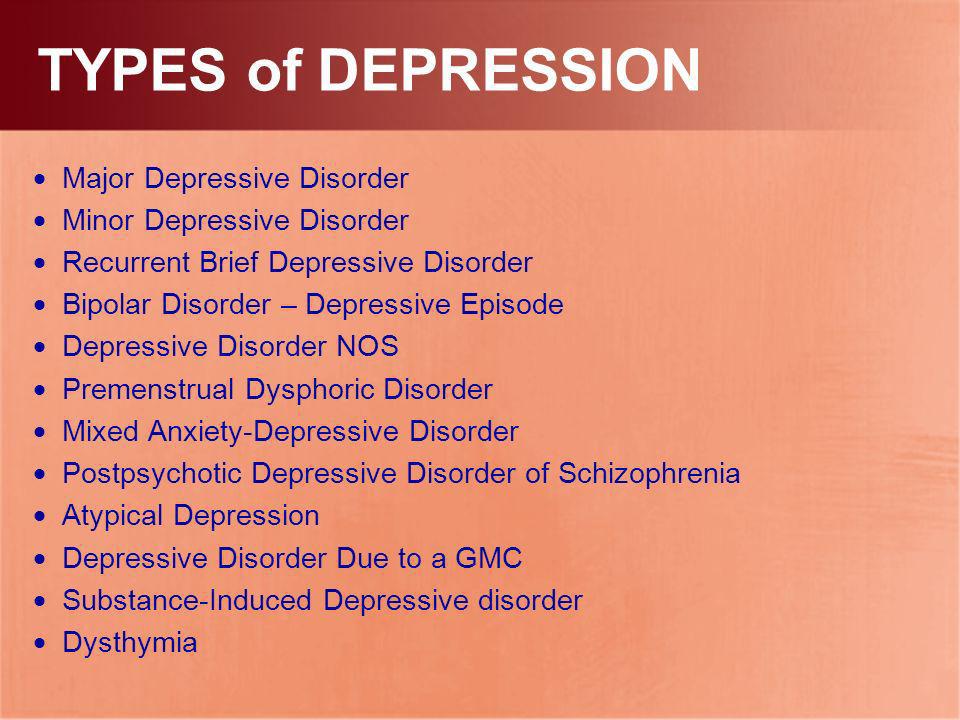
• Alcoholic depression . It is a mental disorder, accompanied by dependence on alcohol, detachment, non-recognition of the problem and often self-flagellation, an acute sense of guilt. Women are at particular risk due to their increased emotionality.
The following forms are distinguished among bipolar depressive disorders:
• Type I bipolar depression. Rare, characterized by alternating phases of depression, normal mood and manic phases. The latter are characterized by an elevated, almost euphoric mood, hyperactivity, increased excitability, and reduced need for sleep. In the manic phase, a person often commits rash acts, engages in casual sexual relationships, and often takes irrational financial steps. In fact, bipolar depression can be characterized as being periodically on top of the world, followed by a plunge into the abyss of despair.
• Bipolar depression type II. More similar to recurrent depression in terms of milder symptoms and frequency of episodes.