What are the signs of psychosis
Symptoms - Psychosis - NHS
Someone who develops psychosis will have their own unique set of symptoms and experiences, according to their particular circumstances.
But in general, 3 main symptoms are associated with a psychotic episode:
- hallucinations
- delusions
- confused and disturbed thoughts
Hallucinations
Hallucinations are where someone sees, hears, smells, tastes or feels things that do not exist outside their mind.
- sight – seeing colours, shapes or people
- sounds – hearing voices or other sounds
- touch – feeling touched when there is nobody there
- smell – an odour that other people cannot smell
- taste – a taste when there is nothing in the mouth
Delusions
A delusion is where a person has an unshakeable belief in something untrue.
A person with persecutory delusions may believe an individual or organisation is making plans to hurt or kill them.
A person with grandiose delusions may believe they have power or authority. For example, they may think they're the president of a country or they have the power to bring people back from the dead.
People who have psychotic episodes are often unaware that their delusions or hallucinations are not real, which may lead them to feel frightened or distressed.
Confused and disturbed thoughts
People with psychosis sometimes have disturbed, confused, and disrupted patterns of thought. Signs of this include:
- rapid and constant speech
- disturbed speech – for example, they may switch from one topic to another mid-sentence
- a sudden loss in their train of thought, resulting in an abrupt pause in conversation or activity
Postnatal psychosis
Postnatal psychosis, also called puerperal psychosis, is a severe form of postnatal depression, a type of depression some women experience after having a baby.
It's estimated postnatal psychosis affects around 1 in every 1,000 women who give birth.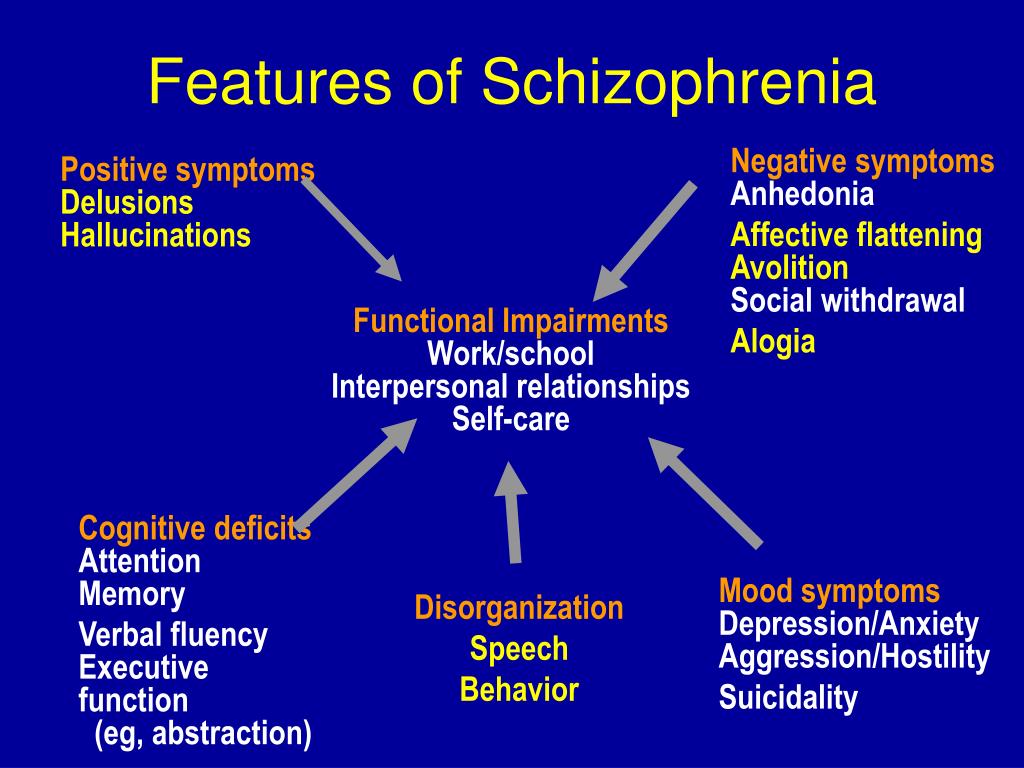 It most commonly occurs during the first few weeks after having a baby.
It most commonly occurs during the first few weeks after having a baby.
Postnatal psychosis is more likely to affect women who already have a mental health condition, such as bipolar disorder or schizophrenia.
As well as the symptoms of psychosis, symptoms of postnatal psychosis can also include changes in mood:
- a high mood (mania) – for example, feeling elated, talking and thinking too much or too quickly
- a low mood – for example, feeling sad, a lack of energy, loss of appetite, and trouble sleeping
Contact a GP immediately if you think you or someone you know may have developed postnatal psychosis as it is a medical emergency. If this is not possible, call NHS 111 or your local out-of-hours service.
If you think there's an imminent danger of harm, call 999 and ask for an ambulance.
Psychosis is not the same as psychopath
The terms "psychosis" and "psychopath" should not be confused.
Someone with psychosis has a short-term (acute) condition that, if treated, can often lead to a full recovery.
A psychopath is someone with an antisocial personality disorder, which means they:
- lack empathy – the capacity to understand how someone else feels
- are manipulative
- often have a total disregard for the consequences of their actions
People with an antisocial personality can sometimes pose a threat to others because they can be violent. Most people with psychosis are more likely to harm themselves than others.
Page last reviewed: 10 December 2019
Next review due: 10 December 2022
NIMH » Understanding Psychosis
What is psychosis?
Psychosis refers to a collection of symptoms that affect the mind, where there has been some loss of contact with reality. During an episode of psychosis, a person’s thoughts and perceptions are disrupted and they may have difficulty recognizing what is real and what is not.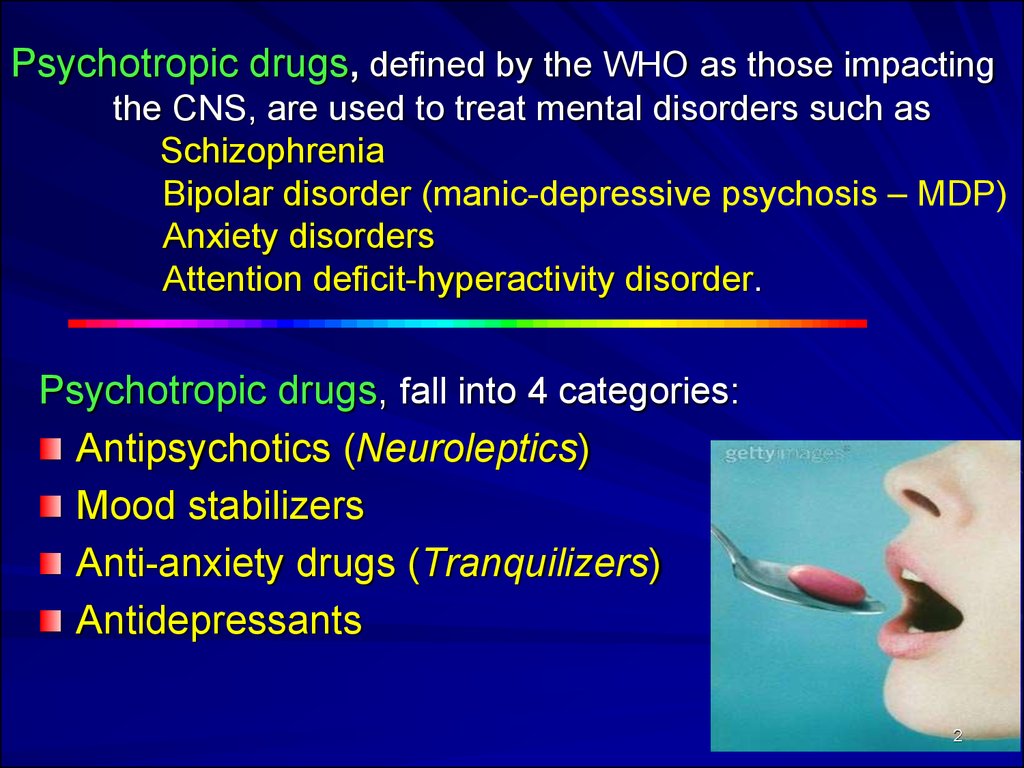
Who develops psychosis?
It is difficult to know the number of people who experience psychosis. Studies estimate that between 15 and 100 people out of 100,000 develop psychosis each year.
Psychosis often begins in young adulthood when a person is in their late teens to mid-20s. However, people can experience a psychotic episode at younger and older ages and as a part of many disorders and illnesses. For instance, older adults with neurological disorders may be at higher risk for psychosis.
What are the signs and symptoms of psychosis?
People with psychosis typically experience delusions (false beliefs, for example, that people on television are sending them special messages or that others are trying to hurt them) and hallucinations (seeing or hearing things that others do not, such as hearing voices telling them to do something or criticizing them). Other symptoms can include incoherent or nonsense speech and behavior that is inappropriate for the situation.
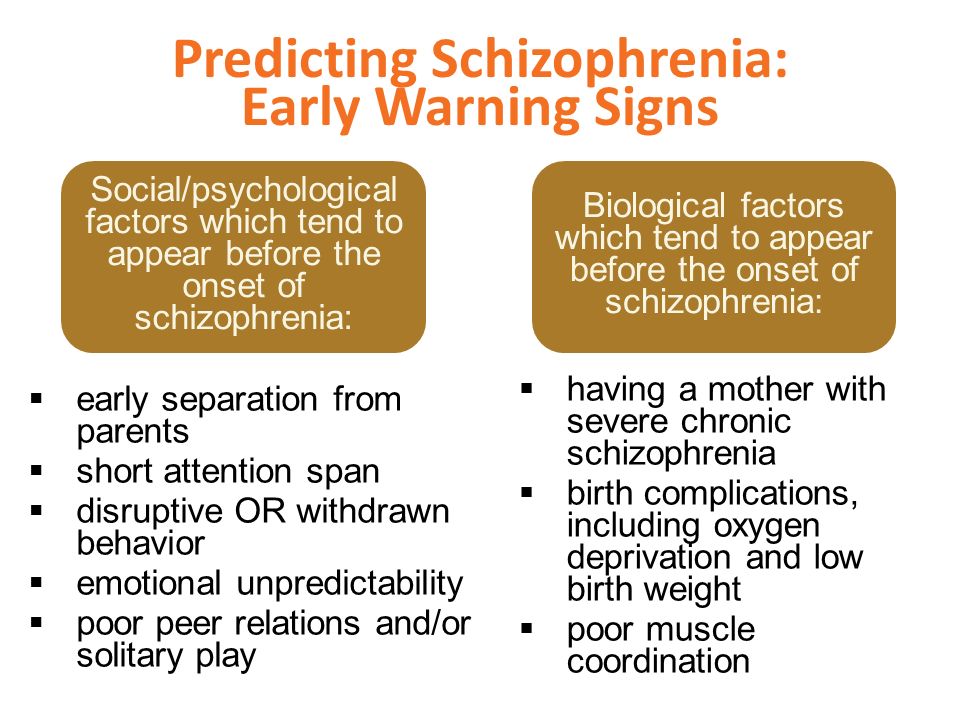
However, a person will often show changes in their behavior before psychosis develops. Behavioral warning signs for psychosis include:
- Suspiciousness, paranoid ideas, or uneasiness with others
- Trouble thinking clearly and logically
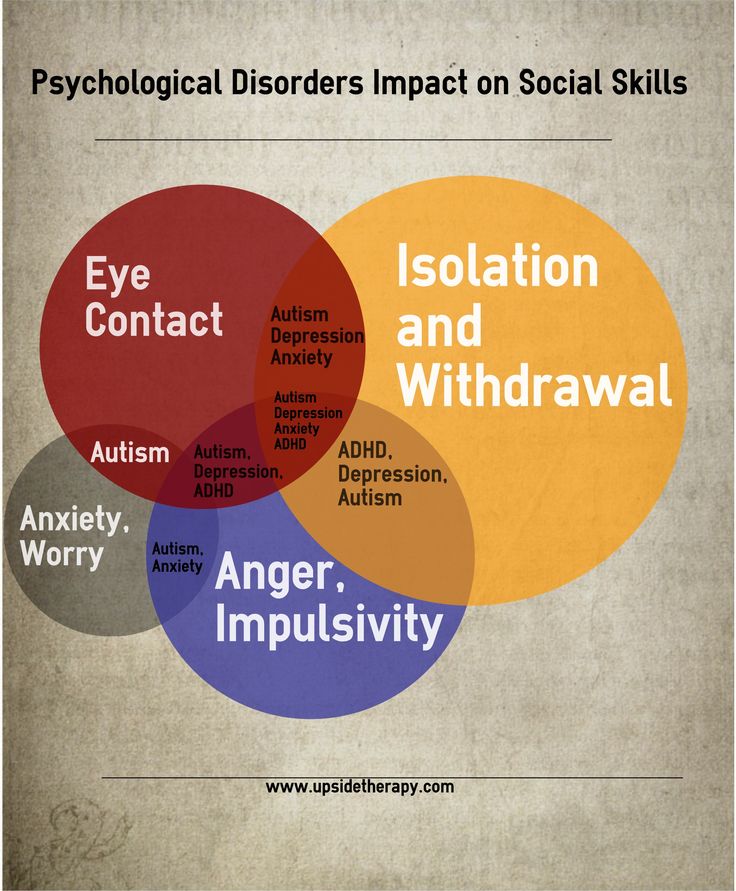
- Withdrawing socially and spending a lot more time alone
- Unusual or overly intense ideas, strange feelings, or a lack of feelings
- Decline in self-care or personal hygiene
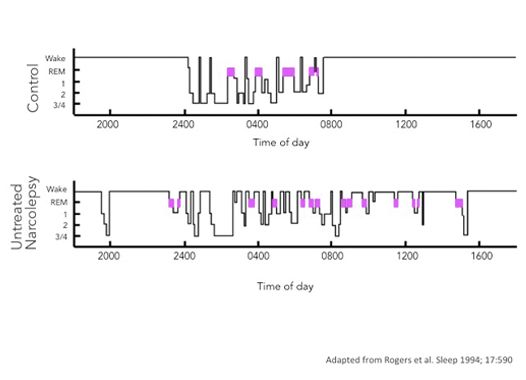
- Disruption of sleep, including difficulty falling asleep and reduced sleep time
- Difficulty telling reality from fantasy
- Confused speech or trouble communicating
- Sudden drop in grades or job performance
Alongside these symptoms, a person with psychosis may also experience more general changes in behavior that include:
- Emotional disruption
- Anxiety
- Lack of motivation
- Difficulty functioning overall
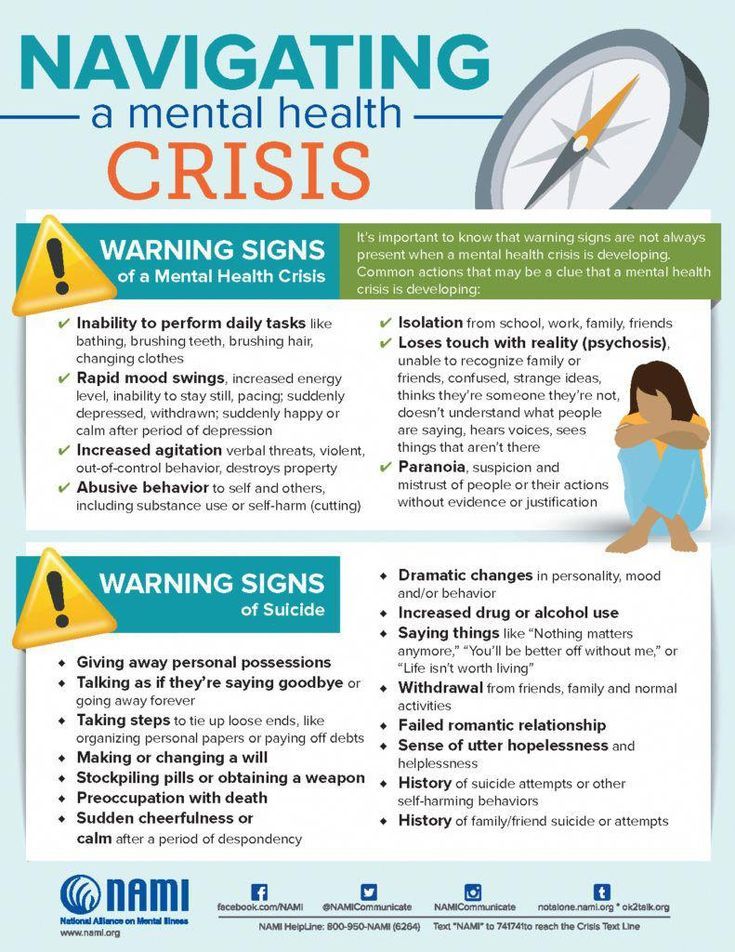
In some cases, a person experiencing a psychotic episode may behave in confusing and unpredictable ways and may harm themselves or become threatening or violent toward others.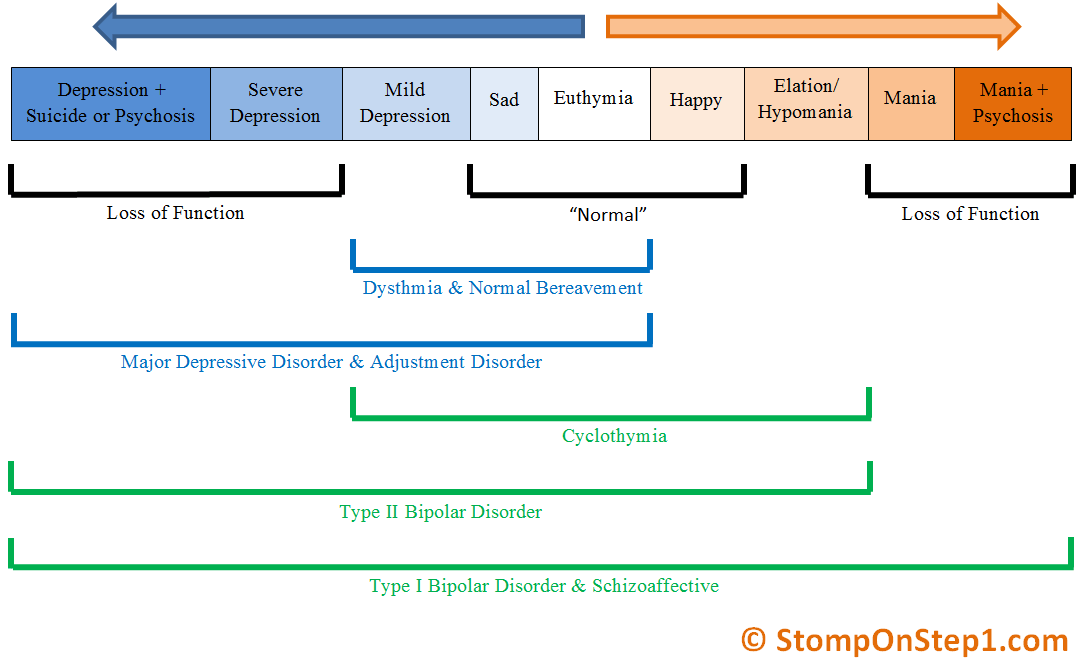 The risk of violence and suicide decreases with treatment for psychosis, so it is important to seek help. If you find that you are experiencing these changes in behavior or notice them in a friend or family member and they begin to intensify or do not go away, reach out to a health care provider.
The risk of violence and suicide decreases with treatment for psychosis, so it is important to seek help. If you find that you are experiencing these changes in behavior or notice them in a friend or family member and they begin to intensify or do not go away, reach out to a health care provider.
The National Institute of Mental Health (NIMH) has information on ways to get help and find a health care provider or access treatment. If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org. In life-threatening situations, call 911.
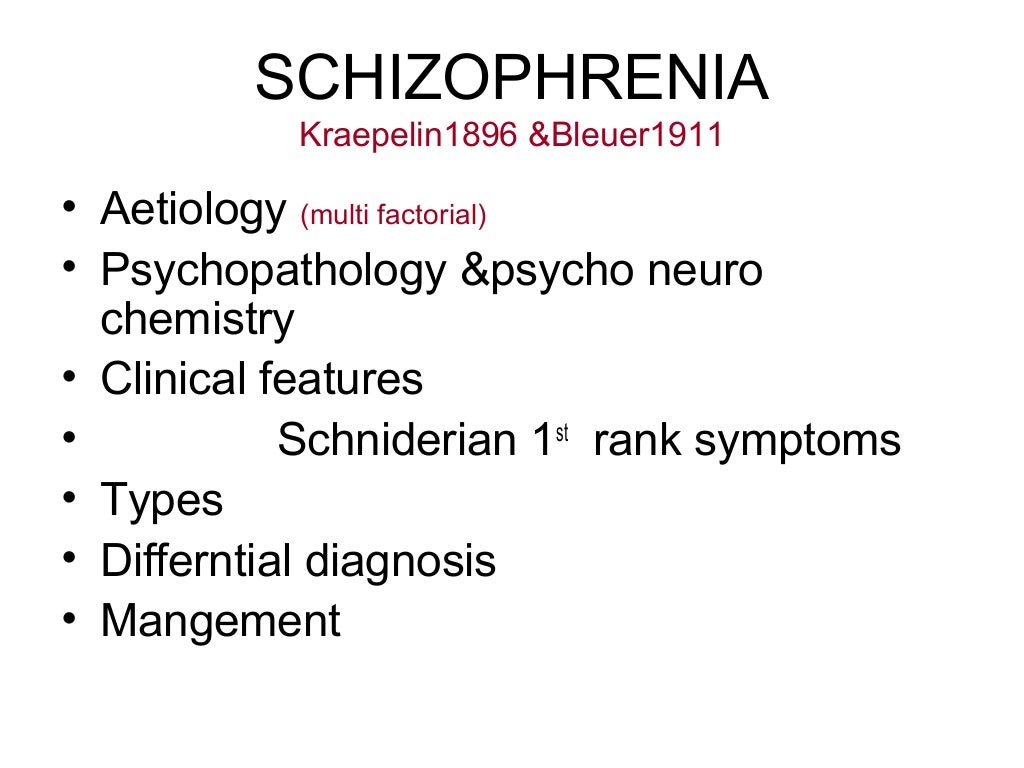
What causes psychosis?
There is no one cause of psychosis. Psychosis appears to result from a complex combination of genetic risk, differences in brain development, and exposure to stressors or trauma. Psychosis may be a symptom of a mental illness, such as schizophrenia, bipolar disorder, or severe depression.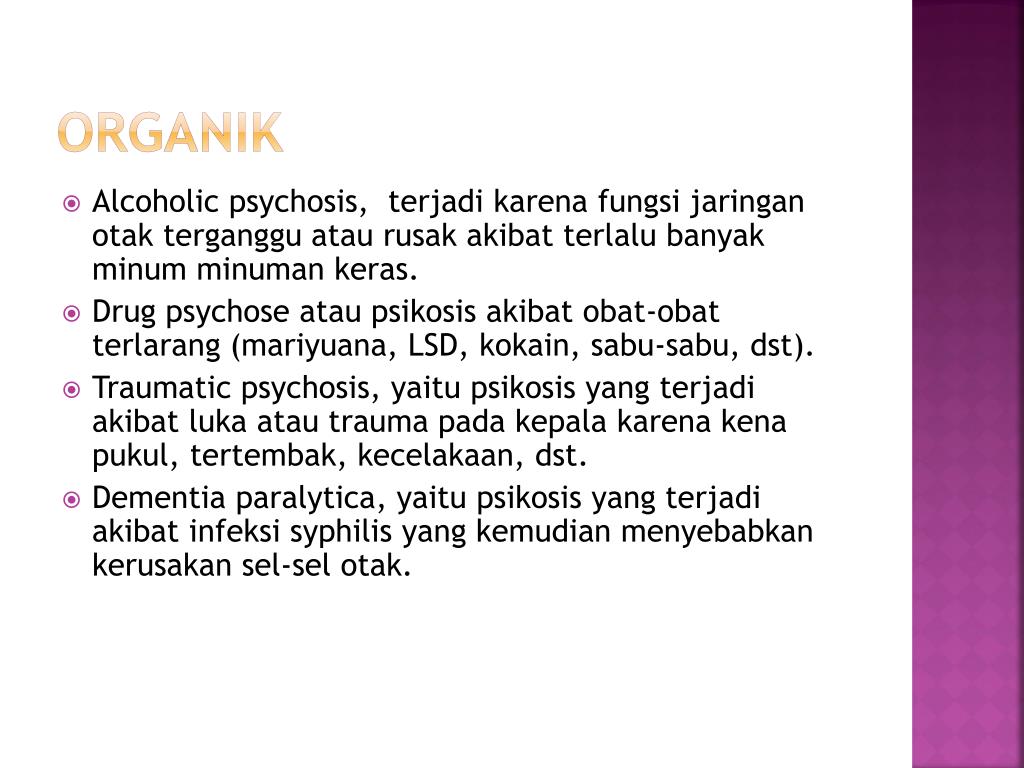 However, a person can experience psychosis and never be diagnosed with schizophrenia or any other disorder.
However, a person can experience psychosis and never be diagnosed with schizophrenia or any other disorder.
For older adults, psychosis symptoms can be part of a physical or mental illness that emerges later in life. Psychosis can also be a symptom of some diseases of older age, including Parkinson's disease, Alzheimer’s disease, and related dementias.
Other possible causes of psychosis include sleep deprivation, certain prescription medications, and the misuse of alcohol or drugs. A mental illness, such as schizophrenia, is typically diagnosed by excluding these other causes.
A qualified mental health professional (such as a psychologist, psychiatrist, or social worker) can provide a thorough assessment and accurate diagnosis. Find tips to help prepare for and get the most out of your visit. For additional resources, including questions to ask your health care provider, visit the Agency for Healthcare Research and Quality.
How is psychosis treated?
Studies have shown that it is common for a person to have psychotic symptoms for more than a year before receiving treatment.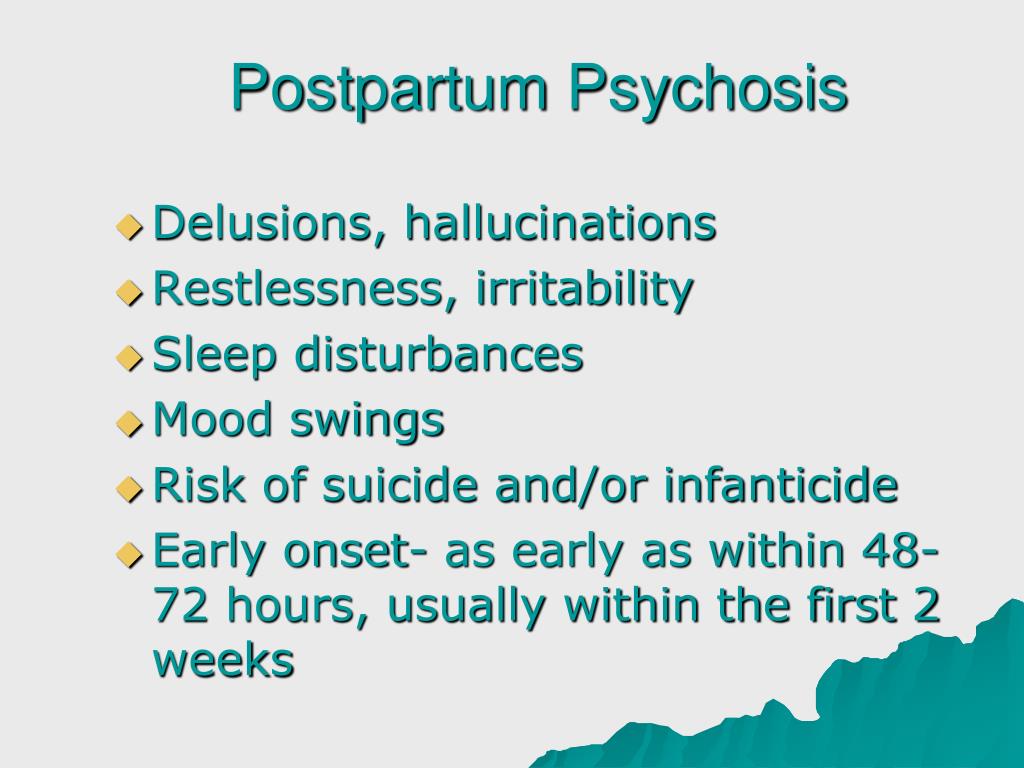 Reducing this duration of untreated psychosis is critical because early treatment often means better recovery. A qualified psychologist, psychiatrist, or social worker can make a diagnosis and help develop a treatment plan.
Reducing this duration of untreated psychosis is critical because early treatment often means better recovery. A qualified psychologist, psychiatrist, or social worker can make a diagnosis and help develop a treatment plan.
Treatment of psychosis usually includes antipsychotic medication. There are several different types of antipsychotic medications, and they have different side effects, so it is important to work with a health care provider to determine the medication that is most effective with the fewest side effects.
Treatment also often includes other elements. There is substantial research support for coordinated specialty care, which is a multi-element, recovery-oriented team approach to treating psychosis that promotes easy access to care and shared decision-making among specialists, the person experiencing psychosis, and family members. People experience better outcomes from coordinated specialty care if they begin treatment as soon as possible after psychotic symptoms emerge.
Coordinated specialty care is now the standard of care for early psychosis, according to “The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia.”
NIMH research on coordinated specialty care
The Recovery After an Initial Schizophrenia Episode (RAISE) research project, supported by NIMH, established coordinated specialty care as an effective treatment for early psychosis and identified important elements for helping people lead productive, independent lives. Learn more about the RAISE studies.
NIMH continues to prioritize research on and expansion of treatments for early psychosis with the launch of the Early Psychosis Intervention Network (EPINET) in 2019. Through EPINET, NIMH funded awards to establish a national data coordinating center and regional scientific hubs connected to more than 100 coordinated specialty care programs that provide early psychosis treatment in 17 states.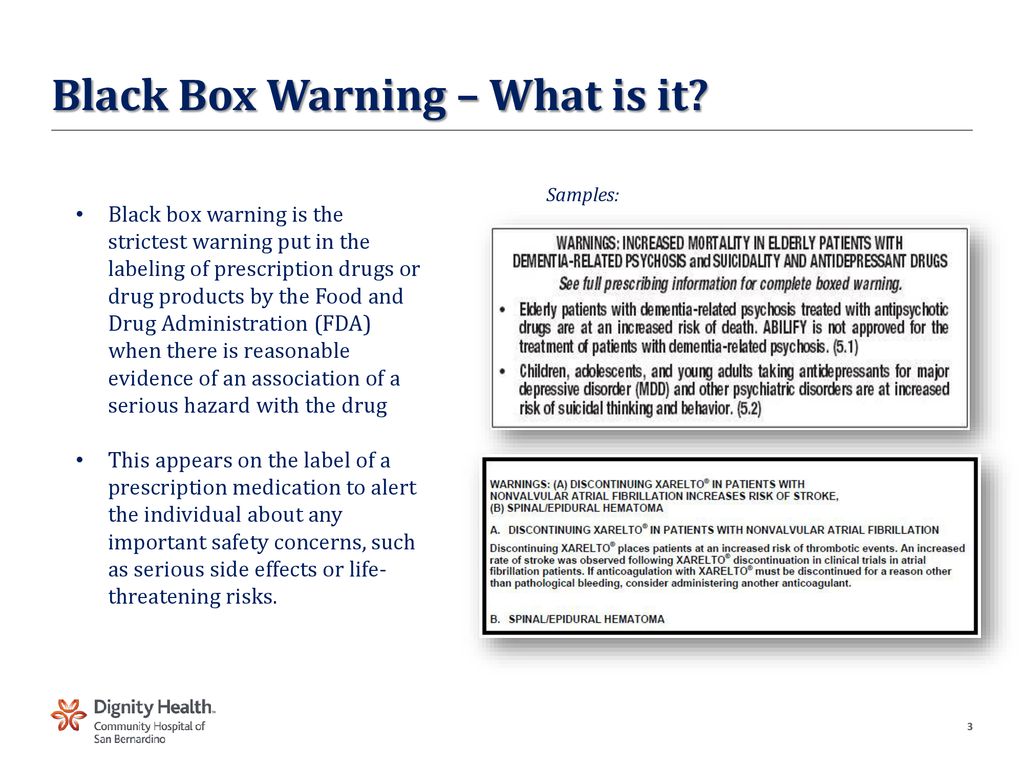 The EPINET website provides resources for researchers, health care providers, administrators, and people experiencing psychosis and their families.
The EPINET website provides resources for researchers, health care providers, administrators, and people experiencing psychosis and their families.
Coordinated specialty care consists of multiple components:
- Individual or group psychotherapy is tailored to a person’s recovery goals. Cognitive and behavioral therapies focus on developing the knowledge and skills necessary to build resilience and cope with aspects of psychosis while maintaining and achieving personal goals.
- Family support and education programs teach family members about psychosis as well as coping, communication, and problem-solving skills. Family members who are informed and involved are more prepared to help loved ones through the recovery process.
- Medication management (also called pharmacotherapy) means tailoring medication to a person’s specific needs by selecting the appropriate type and dose of medication to help reduce psychosis symptoms.
 Like all medications, antipsychotic medications have risks and benefits. People should talk with a health care provider about side effects, medication costs, and dosage preferences (daily pill or monthly injection).
Like all medications, antipsychotic medications have risks and benefits. People should talk with a health care provider about side effects, medication costs, and dosage preferences (daily pill or monthly injection). - Supported employment and education services focus on return to work or school, using the support of a coach to help people achieve their goals.
- Case management provides opportunities for people with psychosis to work with a case manager to address practical problems and improve access to needed support services.
Learn more about the components of coordinated specialty care.
People with psychosis should be involved in their treatment planning and consulted in making decisions about their care. Their needs and goals should drive the treatment programs, which will help them stay engaged throughout the recovery process.
It is important to find a mental health professional who is trained in psychosis treatment and who makes the person feel comfortable.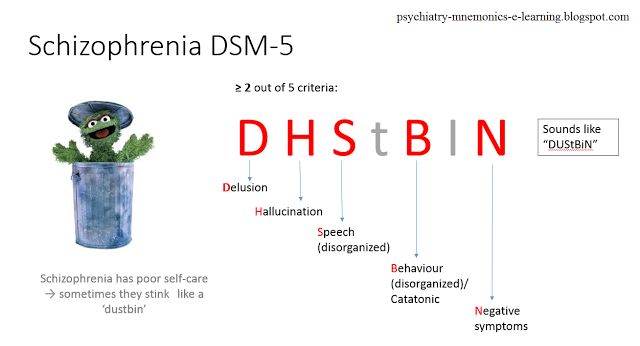 With early diagnosis and appropriate treatment, it is possible to recover from psychosis. Some people who receive early treatment never have another psychotic episode. For other people, recovery means the ability to lead a fulfilling and productive life, even if psychotic symptoms sometimes return.
With early diagnosis and appropriate treatment, it is possible to recover from psychosis. Some people who receive early treatment never have another psychotic episode. For other people, recovery means the ability to lead a fulfilling and productive life, even if psychotic symptoms sometimes return.
Clinical trials studying psychosis and related disorders
NIMH supports a wide range of research, including clinical trials that look at new ways to prevent, detect, or treat diseases and conditions, such as psychosis and disorders that involve psychosis (like schizophrenia). The goal of a clinical trial is to determine if a new test or treatment works and is safe. Although people may benefit from being part of a clinical trial, they should know that the primary purpose of a clinical trial is to gain new scientific knowledge so that others can be better helped in the future.
Researchers at NIMH and around the country conduct clinical trials with people experiencing psychosis and healthy volunteers. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you. Learn more about participating in clinical trials.
Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you. Learn more about participating in clinical trials.
How can I find help?
NIMH does not endorse specific psychosis clinics or evaluate individual practitioners’ professional qualifications or competencies. However, several organizations are available to assist in finding a treatment program in your area. The following is not a comprehensive list of all programs, and a program’s inclusion on the list does not constitute an endorsement by NIMH.
- Early Assessment and Support Alliance (EASA): EASA offers a National Early Psychosis Directory that lists early psychosis programs across the United States.
- Early Psychosis Intervention Network (EPINET): EPINET’s Early Psychosis Intervention Network Clinics provide treatment and services to individuals with early psychosis across 17 states.

- National Alliance on Mental Illness (NAMI): The NAMI HelpLine can connect you with the NAMI office in your state and help you find programs close to home. Also, you can talk with someone at the NAMI HelpLine, Monday–Friday, 10:00 a.m.–10:00 p.m. ET, by:
- Calling 1-800-950-NAMI (6264)
- Texting “HelpLine” to 62640
- Emailing [email protected]
- Psychosis-Risk and Early Psychosis Program Network (PEPPNET): PEPPNET supports an Early Psychosis Program Directory that provides services to people at risk for or experiencing early psychosis.
- Substance Abuse and Mental Health Services Administration (SAMHSA): SAMHSA has an Early Serious Mental Illness Treatment Locator for finding mental health treatment facilities and programs.
Reprints
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy the images in the publication. If you do use our materials, we request that you cite the National Institute of Mental Health. To learn more about using NIMH publications, refer to NIMH’s reprint guidelines.
However, you may not reuse or copy the images in the publication. If you do use our materials, we request that you cite the National Institute of Mental Health. To learn more about using NIMH publications, refer to NIMH’s reprint guidelines.
For more information
MedlinePlus (National Library of Medicine) (en español)
ClinicalTrials.gov (en español)
National Institutes of Health
NIH Publication No. 23-MH-8110
SIGNS OF MENTAL DISORDERS (WHEN TO SEE A DOCTOR)
Signs of mental disorders, and also the frequency of their occurrence is a common question, exciting people in recent years. This is especially true in connection with the fact that the pace of life is steadily growing, and the resources of human nervous system remain unchanged. Very often mental violations develop gradually, stepwise, introducing features into the psyche a person who was previously not peculiar to him, respectively, there are good chances to notice them in time and provide proper medical care.
According to the latest data, mental disorders are detected in 25-30% of the population, that is, one in four in the world. However, it is noteworthy that while 75-80% are sick non-psychotic, mild mental disorders. serious mental illnesses such as schizophrenia occur in 6-17% cases. Alcoholism - in 60%.
It must be remembered that mental disorder is not a sentence, because with sufficient and timely treatment by a specialist, as well as a responsible attitude and attention to their condition, the symptoms of mental disorders can be stopped, (and often the disorder itself can be completely cured), which will help to maintain the former social, professional status and quality of life.
SIGNS
Asthenic syndrome.
This condition may accompany any mental disorders and many of the somatic diseases. Asthenia expressed in weakness, low performance, mood swings, increased sensitivity. A person starts crying easily, instantly gets irritated and loses his temper. Often asthenia is accompanied sleep disturbances, feeling of weakness, increased fatigue, inability to cope with the usual workload, study.
Often asthenia is accompanied sleep disturbances, feeling of weakness, increased fatigue, inability to cope with the usual workload, study.
Obsessive states.
A wide range of obsessions includes many manifestations: from constant doubts, unpleasant thoughts, "stuck, spinning in the head", fears with which a person does not able to cope, to an irresistible desire for purity or performing certain unusual actions. Under the control of the obsessive state, a person can return home several times in order to check whether he turned off the iron, gas, water, whether he closed the door with a key. An obsessive fear of an accident can force the patient to perform some rituals that, according to the sufferer, can avert trouble. If you notice that your friend or relative washes his hands for hours, became overly squeamish and is always afraid of getting infected with something - this also obsession. The desire not to step on cracks in the asphalt, joints tiles, avoidance of certain modes of transport or people in clothing a certain color or type is also an obsessive state.
Mood changes.
It is especially important to pay attention not to how much for short-term changes under the influence of momentary factors, how much for mood changes that were not previously characteristic a person, long-term, from 2 weeks or more.
- Longing, depression, longing for self-accusations, talk about their own worthlessness, sinfulness, about death, lack of future, hope for the best, etc.
- Unnatural frivolity, carelessness.
- Foolishness, not characteristic of age and character.
- Euphoric state, optimism without any basis.
- Apathy, painful feeling of lack of emotions.
- Fussiness, talkativeness, inability to concentrate, confused thinking.
- Irritability, anger, aggressiveness
- Inability to control emotions, tearfulness, slight breakdowns in conversation natural bashfulness, inability to restrain sexual desires or vice versa, the disappearance of libido, the absence of a morning erection in men
Unusual sensations in the body.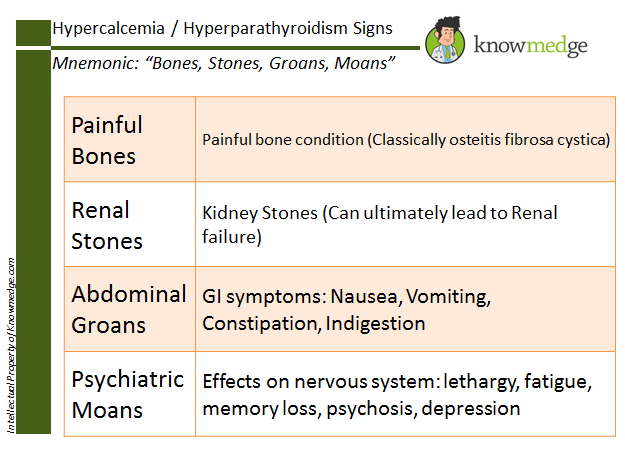
Stinging, burning in the skin, sensations burning, “twisting” pressure in the body, stirring “something inside”, "rustling in the head", the presence of foreign objects in the body - can signal disturbances in the nervous system.
Hypochondria.
Expressed in an obsessive, obsessive search for themselves of serious illnesses and disorders, painful "listening" to the slightest change in the state of your body. At the same time, the patient often does not trust doctors, requires repeated and deeper research, completely focused on finding difficult diseases, requires to be treated as a patient.
Appetite disorders.
It is important to note how sudden increased appetite - "wolfish appetite", and its sharp decrease and perversion of taste preferences. The reason may be as in the disease gastrointestinal tract, and in the general depression of the state, or painful conviction of excessive fullness in its absence.![]() Also it is important if previously tasty food has lost its taste, has become bland, tasteless, "like cardboard."
Also it is important if previously tasty food has lost its taste, has become bland, tasteless, "like cardboard."
Illusions
Do not confuse illusions with hallucinations. Illusions force a person to perceive real objects and phenomena in distorted form, while in hallucinations a person feels something that in reality does not exist.
Examples of illusions:
- the pattern on the wallpaper seems to be an interweaving of snakes or worms;
- sizes of objects are perceived in a distorted form;
- the sound of raindrops on the windowsill seems to be the careful steps of someone terrible;
- the shadows of the trees turn into terrible creatures crawling up with frightening intentions, etc.
Hallucinations not guess, then susceptibility to hallucinations can manifest itself more noticeable. Hallucinations can affect all the senses, that is be visual and auditory, tactile and gustatory, olfactory and common, as well as combined in any combination.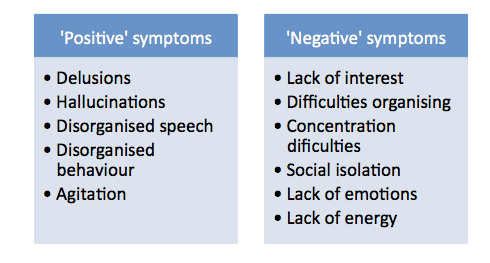 To the sick all he is sees, hears and feels, seems completely real. He may not believe that all this is not felt, not heard, not seen by others. Their he can perceive bewilderment as a conspiracy, deceit, mockery, get irritated at not being understood.
To the sick all he is sees, hears and feels, seems completely real. He may not believe that all this is not felt, not heard, not seen by others. Their he can perceive bewilderment as a conspiracy, deceit, mockery, get irritated at not being understood.
- Auditory hallucinations human hears various kinds of noise, fragments of words or coherent phrases. Voices can give commands or comment on every action of the patient, laugh at him or discuss his thoughts.
- Taste and olfactory hallucinations often cause a sensation of an unpleasant quality: a disgusting taste or smell.
- For tactile hallucinations, the patient it seems that someone is biting him, touching him, strangling him, that they are crawling on him insects that some creatures are introduced into his body and there move or eat the body from the inside.
- Outwardly subject to hallucinations expressed in conversations with an invisible interlocutor, sudden laughter or constant intense listening to something.
 The patient can always to shake off something, to cry out, to examine oneself with preoccupied look or ask others if they see something on his body or in the surrounding space.
The patient can always to shake off something, to cry out, to examine oneself with preoccupied look or ask others if they see something on his body or in the surrounding space.
Changes in thinking
Previously uncharacteristic overestimation own abilities or abilities, confidence in one's own exclusivity, passion for esotericism, magic, suddenly appeared belief in the supernatural. The rate at which thoughts flow in the head can also change, or become uncomfortably slow, or so fast that sometimes it is very difficult to concentrate on one thought.
Delusional thoughts.
Delusional states often accompany psychoses. Delusion is based on erroneous judgments, and the patient stubbornly maintains its false belief, even if there are obvious contradictions with reality. Crazy ideas acquire significance that determines everything behavior. Delusional disorders can be expressed in an erotic form, or in the conviction of one's great mission, in descent from a noble kind or aliens. It may seem to the patient that someone is trying to kill or poison, rob or kidnap. Sometimes the development of delusional state is preceded by a feeling of unreality of the surrounding world or own personality.
It may seem to the patient that someone is trying to kill or poison, rob or kidnap. Sometimes the development of delusional state is preceded by a feeling of unreality of the surrounding world or own personality.
Desocialization.
There are people who are unsociable and unsociable in strength of his character. This is normal and should not arouse suspicion. mental disorders. But if a born merry fellow, the soul company, a family man and a good friend suddenly begins to destroy social connections, becomes unsociable, shows coldness towards those who have recently was dear to him - this is a reason to worry about his mental health. A person becomes sloppy, stops taking care of himself, maybe quit your job for no good reason, abandon your career, former goals and interests, in society can begin to behave shockingly - commit acts that are considered indecent and unacceptable.
Gathering or excessive generosity
Yes, any collector can be suspicion.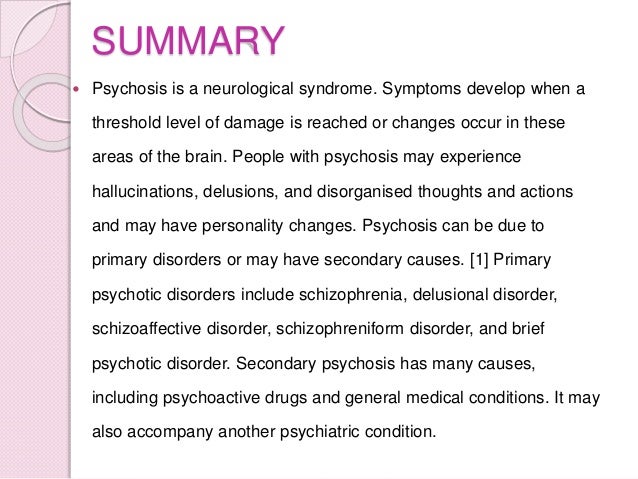 Especially in cases where the gathering becomes obsession, subjugates the whole life of a person. It may expressed in the desire to drag into the house things found in the garbage, hoarding products without paying attention to expiration dates, or pick up stray animals in numbers that exceed the ability provide them with proper care and maintenance.
Especially in cases where the gathering becomes obsession, subjugates the whole life of a person. It may expressed in the desire to drag into the house things found in the garbage, hoarding products without paying attention to expiration dates, or pick up stray animals in numbers that exceed the ability provide them with proper care and maintenance.
Desire to distribute all one's property, excessive spending can also be regarded as suspicious symptom. Especially in the case when a person was not different before generosity or altruism. Particular attention should be paid to this a condition, especially when a person begins to unexpectedly actively attend banks and make loans.
Psychosis. What are the signs of a disorder? | Psychology
Psychosis is a group of mental disorders that cause a distorted perception of the picture of the world, as a result of which a person behaves inappropriately to the situation.
Depending on the cause of psychosis, there are two large groups of disorders.
- The first group includes disorders that were caused by an organic lesion of the nervous system. For example, such psychoses are typical for patients with atherosclerosis, syphilis of the brain, some types of tumors can provoke such disorders.
- The second group of psychoses is caused by the genetic characteristics of the nervous system, psychological factors.
All types of psychosis have such symptoms as inappropriate psychotic behavior, strange affective reactions, detachment, inadequate perception of reality, problems with generalization and understanding of what is happening, a tendency to hypochondria.
A manifestation of psychosis are cardinal changes in attitude towards people, phenomena, objects of reality. Often, change results in a hostile or detached perception of the world. Ksenia Kit, Manic-Depressive Psychosis, 2015
Photo: artchive. ru
ru
The first phase of the development of psychosis is characterized by hypochondria, the patient is concerned about his state of health, he is sure that terrible diagnoses are being hidden from him, and so on. The second phase of is characterized by delusional or hallucinogenic constructions and attempts to establish relations with the outside world. The problem is that the patient seeks to build relationships in a fictional world, while those around him, and he himself, live in the real world.
People prone to psychosis often show some abnormalities even before the onset of the active phase of the disease. A person's character deteriorates, irritability and excessive sensitivity are noticeable, appetite disappears, sleep disturbances are observed, he falls into depression, becomes inactive and careless in relation to himself.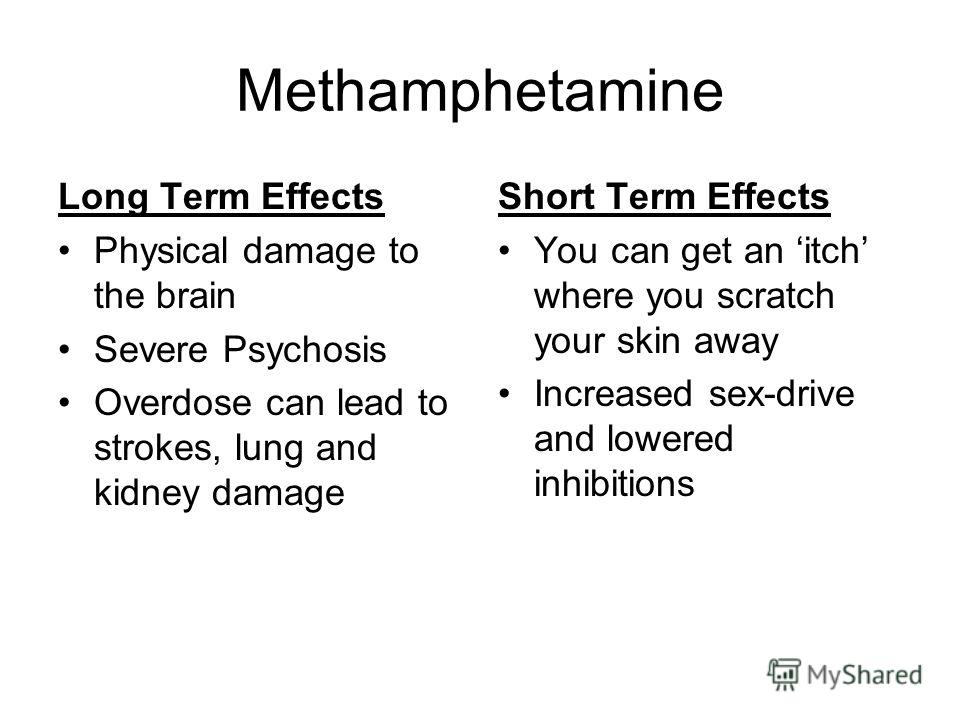 Decreased performance and stress tolerance.
Decreased performance and stress tolerance.
Many psychotic people become interested in religion, the occult, and become interested in the supernatural. From the point of view of social relationships, a person who develops psychosis changes dramatically: he withdraws into himself, breaks ties with many people, becomes suspicious. The patient has a feeling that he hears and sees something that other people cannot perceive. In addition, there is confidence in the supernatural influence of extraneous people and objects on him (for example, suspicions arise that someone is reading his thoughts).
If someone close to you has at least half of the described symptoms, you should not postpone a visit to specialists.
Photo: Depositphotos My experience shows that it is very difficult to convince a patient that he should see a psychiatrist or psychotherapist.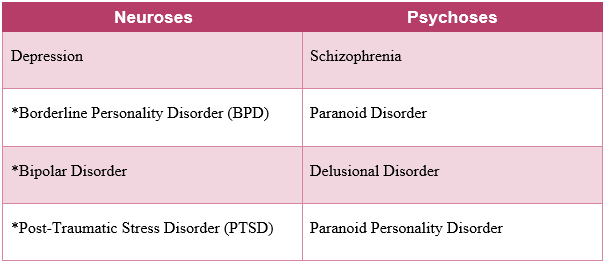 Do not immediately insist on such a visit, it is better to suggest, for example, a visit to a psychologist to combat depression. A psychologist or psychotherapist will be able to convince the patient that there is nothing wrong with a visit to the doctor, medications are not a way to poison a problematic member of society.
Do not immediately insist on such a visit, it is better to suggest, for example, a visit to a psychologist to combat depression. A psychologist or psychotherapist will be able to convince the patient that there is nothing wrong with a visit to the doctor, medications are not a way to poison a problematic member of society.
In addition, while psychosis at the initial stage, it is possible to get by with little bloodshed. Namely: a good psychoanalyst or psychotherapist and sparing, not always chemical, drugs. Combination therapy, during which the use of mood stabilizers, antidepressants, antipsychotics, or other drugs is combined with psychotherapy sessions, can make life much easier for the patient and those around him.
People who constantly communicate with a psychotic should also consult a psychotherapist. The fact is that psychoses are treated, as a rule, on an outpatient basis, which means that the environment of the person being treated will go through a series of difficult tests, and you need to be prepared for them and know how to behave in different situations, be able to withstand stress.