Not getting rem sleep
REM & NREM, Sleep Stages, Good Sleep Habits & More
What is sleep?
You may think nothing is happening when you sleep. But parts of your brain are quite active during sleep. And enough sleep (or lack of it) affects your physical and mental health. When you sleep, your body has a chance to rest and restore energy. A good night’s sleep can help you cope with stress, solve problems or recover from illness. Not getting enough sleep can lead to many health concerns, affecting how you think and feel.
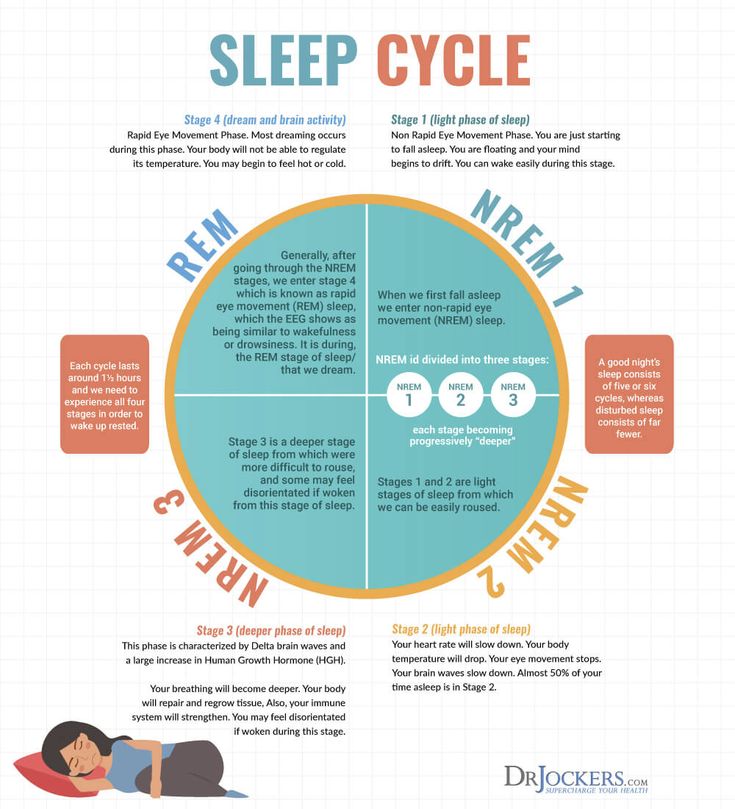
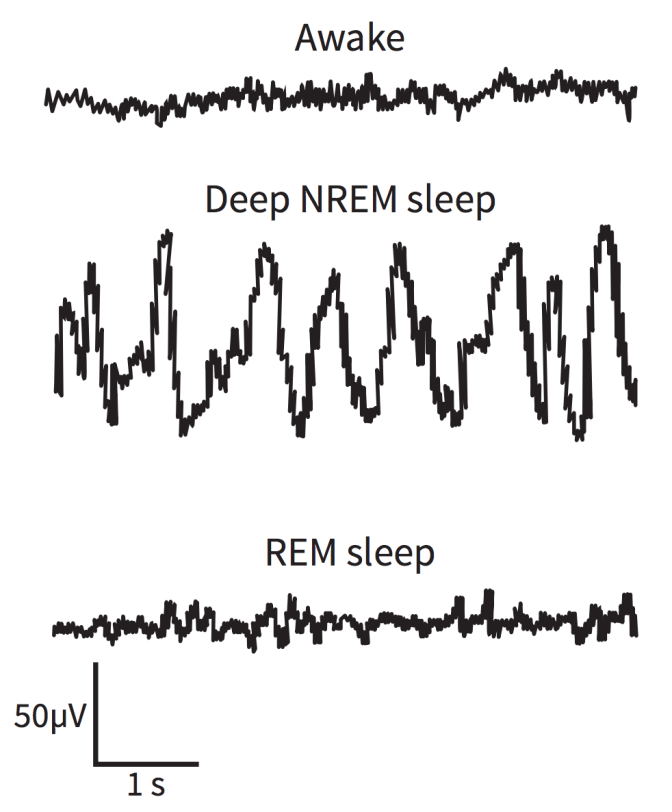
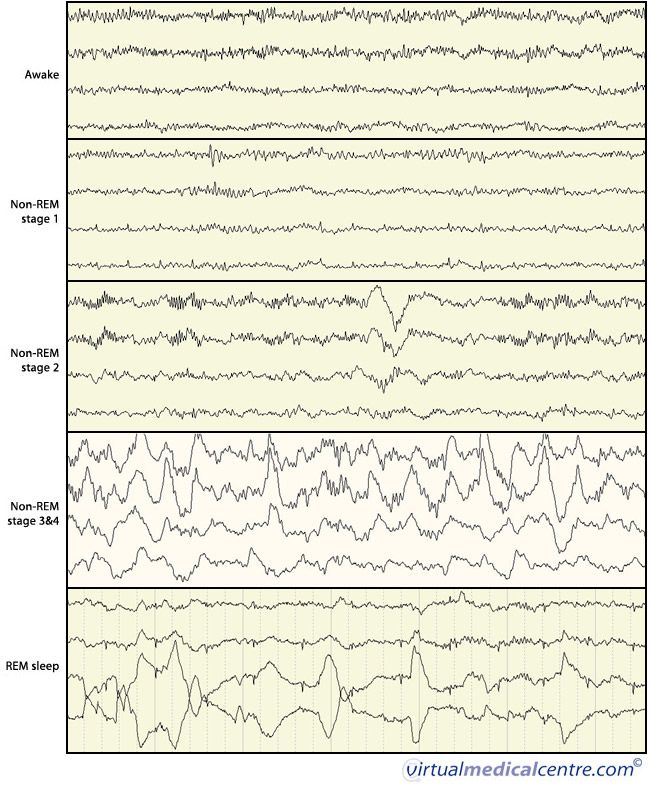
During the night, you cycle through two types of sleep: non-rapid eye movement (non-REM) sleep and rapid eye movement (REM) sleep. Your brain and body act differently during these different phases.
What happens in the brain during sleep?
Researchers continue to study sleep and its effect on us. While we’ve learned a lot about sleep, there’s still much that’s unknown.
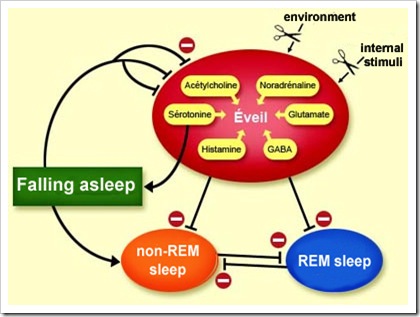
We know that brain chemicals are very involved in our sleep cycle. Neurotransmitters are chemicals that help the nerves communicate. They control whether we’re awake or asleep, depending on which neurons (nerve cells) they’re acting on:
- Neurons in the brainstem (where the brain and spinal cord meet) produce neurotransmitters called serotonin and norepinephrine. These chemicals keep our brain active when we’re awake.
- Neurons located at the base of the brain are responsible for us falling asleep. It seems these neurons turn off the signals that keep us awake.
Why do we need sleep?
Sleep helps us in many ways. We need it for:
- Growth: In children and young adults, deep sleep (sleep that’s harder to wake from) supports growth. The body releases growth hormone during this type of sleep. The body also increases production of proteins, which we need for cell growth and to repair damage.
- Nervous system function: A lack of sleep affects our memory, performance and ability to think clearly. If a person is severely sleep deprived, they may even experience neurological problems such as mood swings and hallucinations.
 Sleep also helps our nerve cells. They can repair themselves, so they function at their best. And certain nerve connections get a chance to turn on, strengthening our brain and thinking ability.
Sleep also helps our nerve cells. They can repair themselves, so they function at their best. And certain nerve connections get a chance to turn on, strengthening our brain and thinking ability. - Survival: Researchers don’t fully understand why sleep is so essential. But studies in animals have shown that getting deprived of REM sleep can shorten lifespans. Lack of sleep may harm the immune system, which protects us from infections.
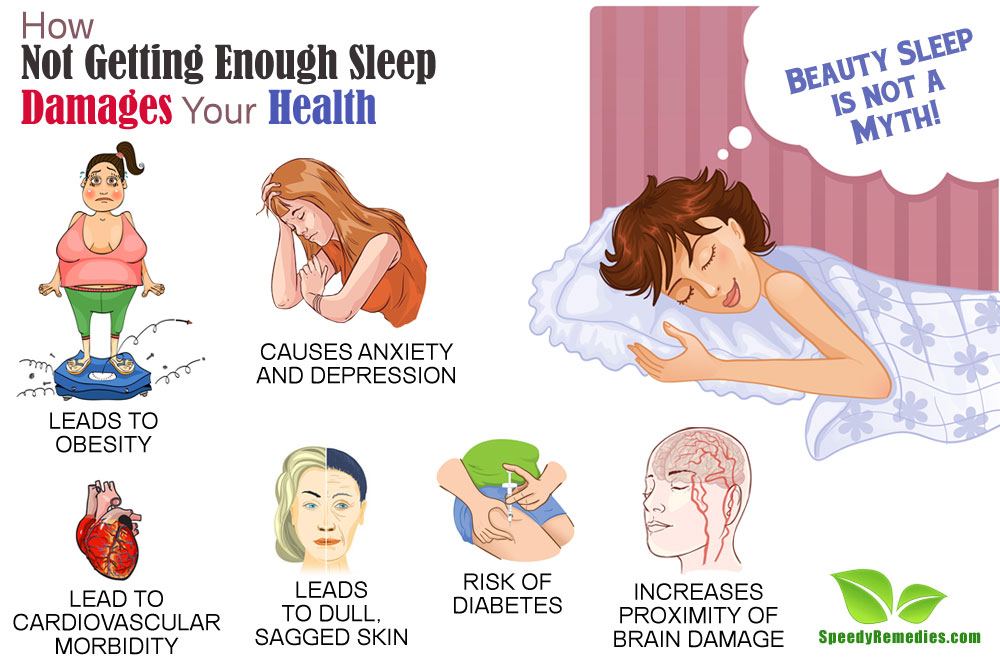
- Well-being: People who don’t get enough sleep are at higher risk for developing various health conditions including obesity, diabetes and heart problems.
What are the stages of sleep?
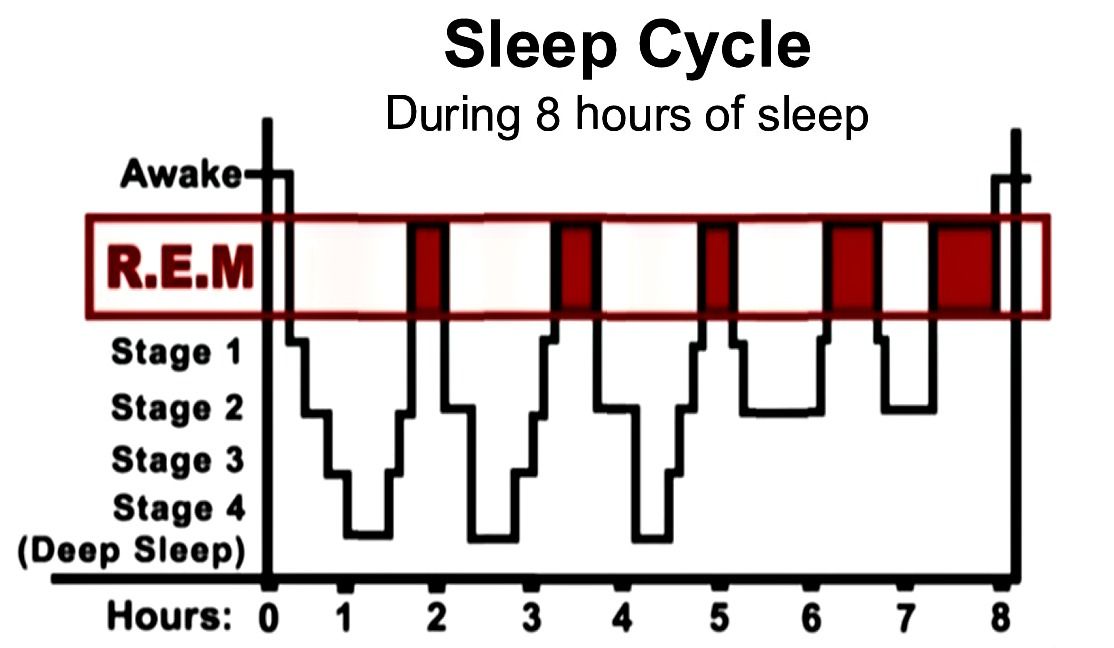
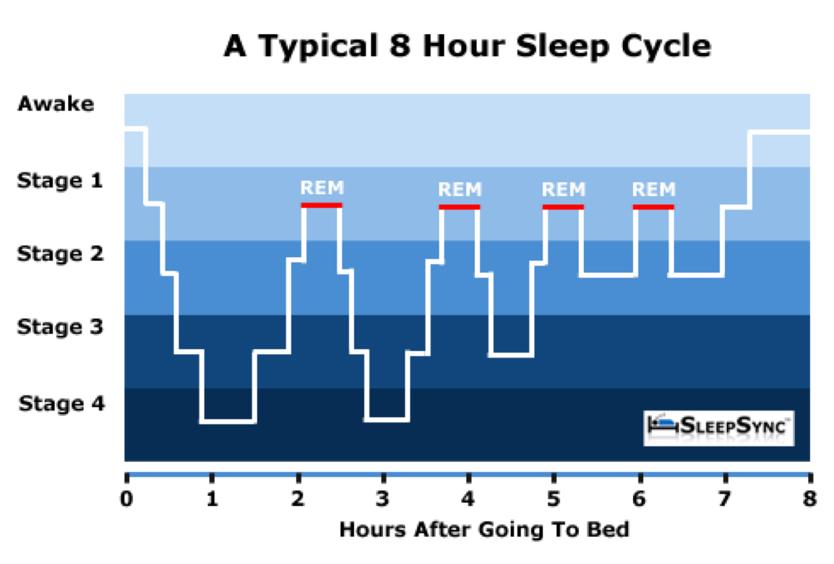
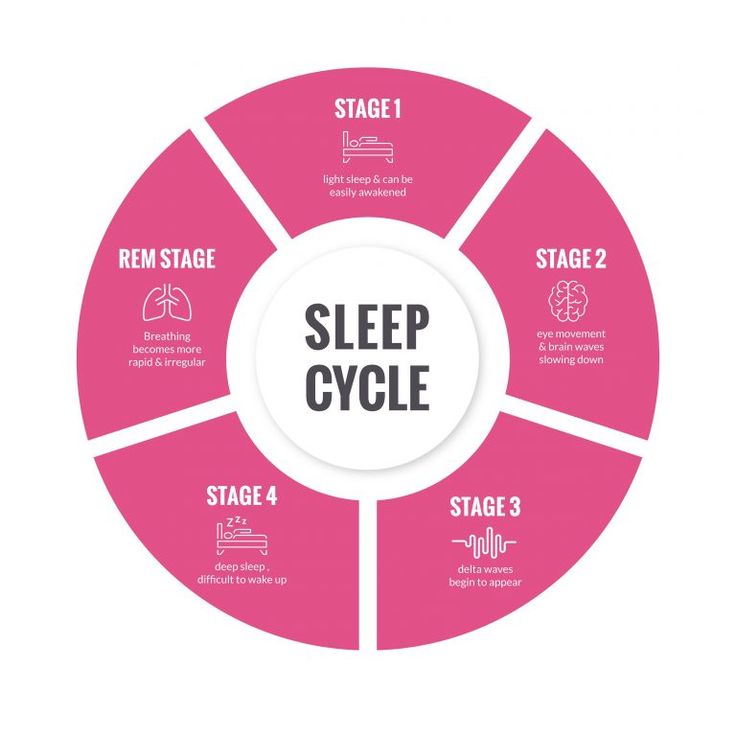
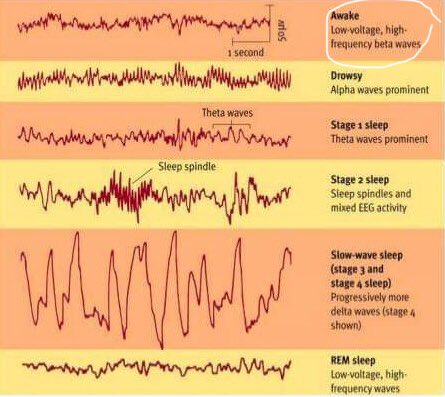
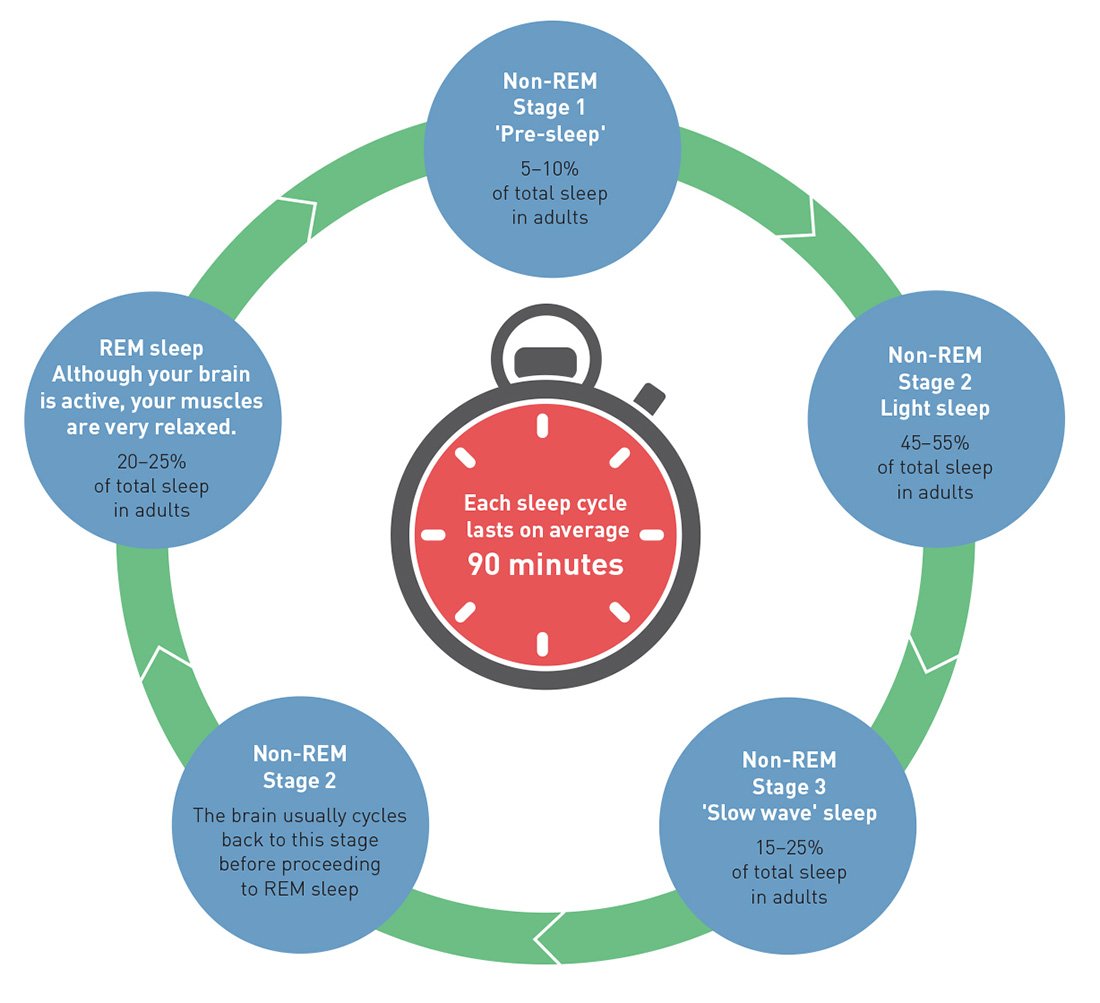
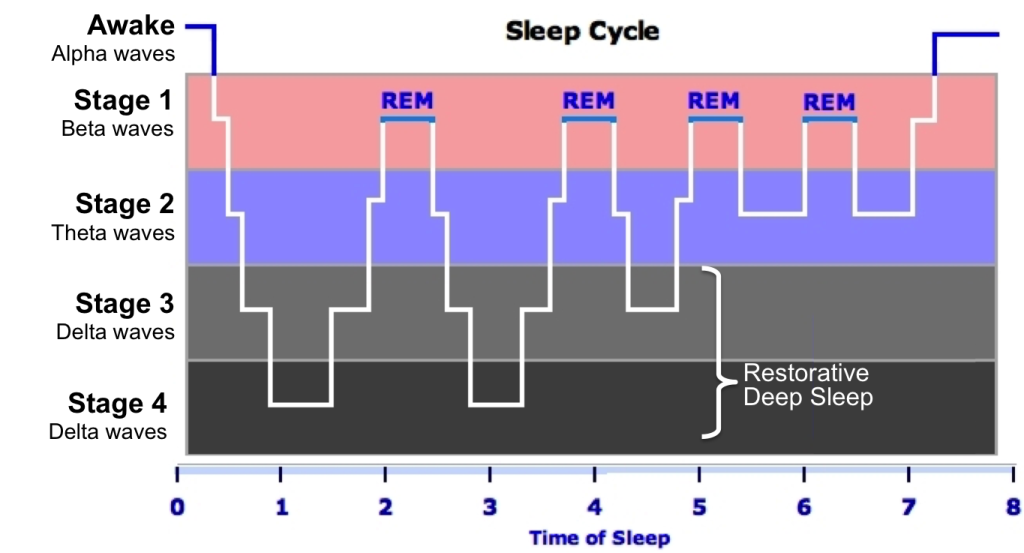
When you sleep, your brain goes through natural cycles of activity. There are four total stages of sleep, divided into two phases:
- Non-REM sleep happens first and includes three stages. The last two stage of non-REM sleep is when you sleep deeply. It’s hard to wake up from this stage of sleep.
- REM sleep happens about an hour to an hour and a half after falling asleep. REM sleep is when you tend to have vivid dreams.
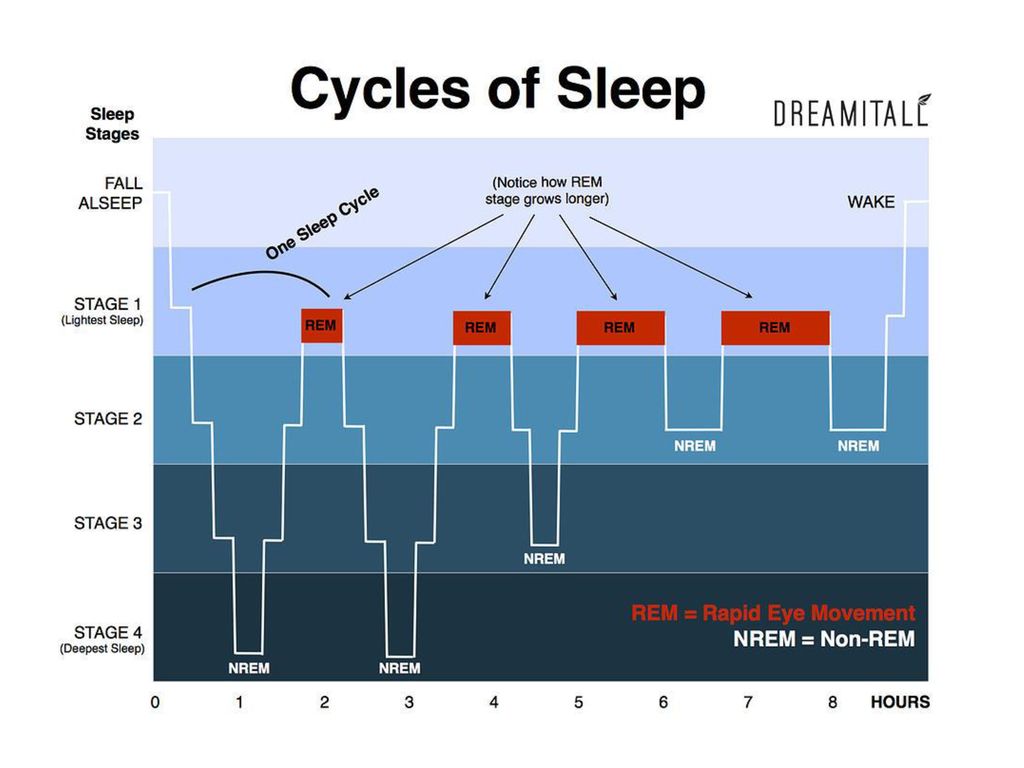
As you sleep, your body cycles through non-REM and REM sleep. You usually start the sleep cycle with stage 1 of non-REM sleep. You pass through the other stages of non-REM sleep, followed by a short period of REM sleep. Then the cycle begins again at stage 1.
A full sleep cycle takes about 90 to 110 minutes. Your first REM period is short. As the night goes on, you’ll have longer REM sleep and less deep sleep.
What is non-REM sleep?
Three stages make up non-REM sleep.
Stage 1:
This stage of light sleeping lasts for five to 10 minutes.
- Everything starts to slow down, including your eye movement and muscle activity.
- Your eyes stay closed. If you get woken from stage 1 sleep, you may feel as if you haven’t slept at all. You may remember pieces of images.
- Sometimes, you may feel like you’re starting to fall and then experience a sudden muscle contraction.
 Healthcare providers call this motion hypnic myoclonic or hypnic jerk. Hypnic jerks are common and not anything to be concerned about as this occurrence is unlikely to cause any complications or side effects.
Healthcare providers call this motion hypnic myoclonic or hypnic jerk. Hypnic jerks are common and not anything to be concerned about as this occurrence is unlikely to cause any complications or side effects.
Stage 2:
- This period of light sleep features periods of muscle tone (muscles partially contracting) mixed with periods of muscle relaxation.
- Your eye movement stops, heart rate slows and body temperature decreases.
- Brain waves become slower. Occasionally, you’ll have a burst of rapid waves called sleep spindles.
- Your body prepares to enter deep sleep.
Stages 3
- This stage is deep sleep.
- During this stage, your brain produces delta waves, very slow brain waves.
- It’s hard for someone to wake you up during this stage.
- You have no eye movement or muscle activity.
- If you’re woken up, you may feel groggy and disoriented for a few minutes.
What happens during non-REM sleep?
During non-REM stages, your body:
- Builds bone and muscle.

- Repairs and regenerates tissues.
- Strengthens the immune system.
As you age, you get less non-REM sleep. Older adults get less deep sleep than younger people.
What is REM sleep?
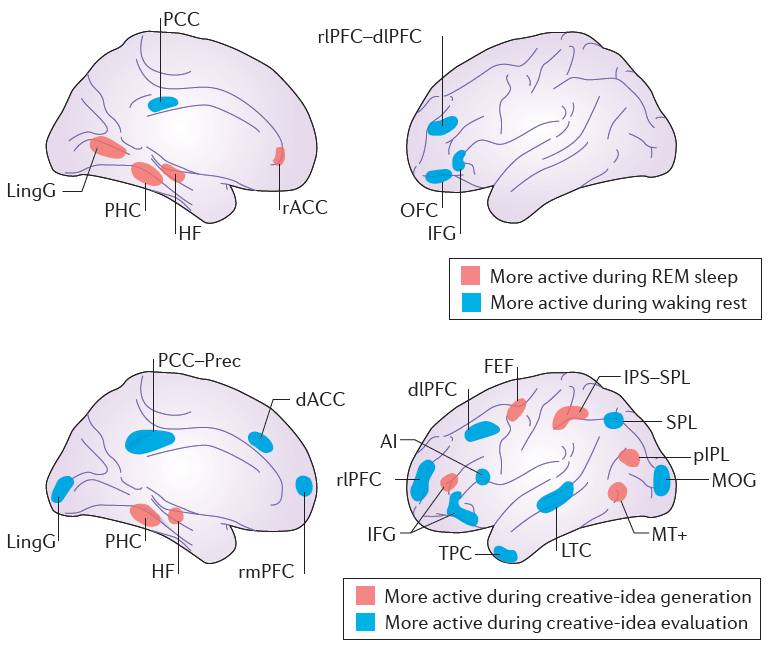
When you enter REM sleep, brain activity increases again, meaning sleep is not as deep. The activity levels are like when you’re awake. That’s why REM sleep is the stage where you’ll have intense dreams.
At the same time, major muscles that you normally control (such as arms and legs) can’t move. In effect, they become temporarily paralyzed.
Usually, REM sleep arrives about an hour and a half after you go to sleep. The first REM period lasts about 10 minutes. Each REM stage that follows gets longer and longer.
The amount of REM sleep you experience changes as you age. The percentage of REM sleep:
- Is highest during infancy and early childhood.
- Declines during adolescence and young adulthood.
- Declines even more as you get older.
What else happens to the body in REM sleep?
Besides increased brain activity and muscle relaxation, your body goes through a series of changes during REM sleep. These changes include:
- Faster breathing.
- Increased heart rate and blood pressure.
- Penile erections.
- Rapid eye movement.
What affects sleep quality?
Chemical signals in the brain influence our sleep and wake cycles. Anything that shifts the balance of these neurotransmitters can make us feel drowsier or more awake. For example:
- Alcohol may help people fall into a light sleep. But it reduces the deeper stages of sleep and REM sleep and leads to more disrupted sleep.
- Caffeine and pseudoephedrine (drug ingredient) can stimulate the brain. They may cause insomnia, an inability to sleep. Watch out for caffeinated drinks such as coffee and drugs such as diet pills and decongestants.
- Medications such as antidepressants can cause less REM sleep.
- People who smoke heavily often sleep lightly and have less REM sleep. They may wake up after a few hours because they experience nicotine withdrawal.
- Very hot or cold temperatures can disrupt REM sleep. We’re less able to regulate body temperature during REM sleep.
How much sleep do I need?
Many factors affect how much sleep you need. Age is a big factor:
- Infants need about 16 hours a day.
- Toddlers and preschoolers need about 12 hours.
- Teenagers need about nine hours.
- Adults need seven to eight (though some are fine with five and others need closer to 10).
- Pregnant people often need more sleep during the first trimester.
What is a sleep debt?
If you haven’t slept well or long enough for a few days, you might create a sleep debt. Once your debt builds up, you may feel physically and mentally exhausted. Try to make sure you get enough sleep every night to avoid creating this debt. You can’t necessarily make up your debt by sleeping a lot on the weekends. It’s best to get enough sleep all week long.
You can’t necessarily make up your debt by sleeping a lot on the weekends. It’s best to get enough sleep all week long.
Can we adapt to needing less sleep?
Generally, people don’t adapt to getting less sleep than they need. You may feel like you’re used to reduced sleep, but it still affects your function. For example, it can harm your judgment and reaction time.
What is sleep deprivation?
When you’re sleep deprived, you’re not getting the total amount of sleep you need. Signs of sleep deprivation include:
- Falling asleep within a few minutes of lying down.
- Feeling drowsy during the day.
- Nodding off for microsleeps — short periods of sleep during the day when you’re otherwise awake.
- Sleep deprivation can be dangerous. Driving while tired causes about 100,000 car accidents each year, according to the National Highway Traffic Safety Administration. It also causes 1,500 deaths. If you feel tired on the road, pull over. It’s not safe to drive if you’re drowsy.

What are sleep disorders?
According to the American Sleep Association, at least 40 million Americans experience sleep disorders each year. Another 20 million have occasional sleep issues. These disorders cause sleep deprivation, leading to problems with work, school, driving and social activities.
There are more than 70 sleep disorders. A few, known as disruptive sleep disorders, lead to moving around or making sounds. Other sleep disorders involve food. And some sleep disorders overlap with psychiatric conditions. If you have problems with sleep or feel very tired, talk to your healthcare provider about a possible sleep disorder.
Some of the most common sleep disorders include:
- Insomnia disorder: Many people experience insomnia at some point in their lives, with trouble falling or staying asleep. Sleeping pills can help in the short-term but behavioral strategies to improve sleep including cognitive behavioral therapy for Insomnia (CBT-i) is a much better long term solution.
- Narcolepsy: You may suddenly fall asleep during the day, even if you had a good sleep the night before. These “sleep attacks” can last a few seconds or up to 30 minutes. Talk to your provider about your symptoms and additional testing will need to be completed to diagnosis this sleep disorder.
- Restless legs syndrome (RLS): You may feel unpleasant sensations in your legs (such as prickling or tingling). You may also have an urge to move your legs to get relief. If you have RLS, talk to your healthcare provider about medication to help improve symptoms.
- Sleep apnea:
You may experience periods of interrupted breathing while you sleep, a condition called sleep apnea. Often, getting polysomnography (sleep study) in a sleep center is the best way to get properly diagnosed and treated. Sometimes, weight loss or not sleeping on your back can help. But you may need a special device to help you breathe while you sleep.
- Snoring: People who regularly snore can have disturbed sleep. They can also disturb the sleep of their bed partner. Snoring often leads to feeling tired during the day. Several treatment options are available for snoring.
What are good sleep habits?
Good sleep habits, also called good sleep hygiene, are practices to help you get enough quality sleep.
Do:
- Have a sleep schedule: Go to sleep and wake up around the same time every day, even on weekends and vacations.
- Clear your mind before bed: Make a to-do list early in the evening, so you won’t stay awake in bed and worry about the next day.
- Create a good sleep environment: Make sure your bed and pillows are comfortable. Turn down the lights and avoid loud sounds. Keep the room at a comfortable temperature.
- Exercise every day: Stay active but try to avoid exercising during the few hours right before bed.

- Relax: Before bed, take a warm bath, read or do another relaxing activity.
- See your healthcare provider: If you’ve been having trouble sleeping or feel extra drowsy during the day, talk to your provider. There are many treatments available for sleep disorders.
Don’t:
- Consume caffeine, nicotine and alcohol late in the day: These substances can interfere with your ability to fall and stay asleep.
- Lie in bed awake: It’s better to do a soothing activity, like reading, until you feel tired.
- Nap during the day: A short nap (less than 30 minutes) is OK if you’re very sleepy. But try to avoid naps after 3 p.m.
- Think negative thoughts: Try to avoid a negative mindset when going to bed, such as, “If I don’t get enough sleep now, I won’t get through my day tomorrow!”
- Use electronics right before bed: Electronics, such as your phone or tablet, can interfere with your body’s production of melatonin.
 This hormone gets released before bed to help you feel tired.
This hormone gets released before bed to help you feel tired.
A note from Cleveland Clinic
Far from being a state of doing nothing, sleep is an essential part of our lives. It helps our body rest, recharge and repair. There are four sleep stages — three in the non-REM phase plus REM sleep. Many factors can affect sleep quality, including the food and drink you consume before bed and room temperature. Many people experience trouble sleeping now and then. But if you think you may have a sleep disorder, talk to your healthcare provider. Common sleep disorders include insomnia (trouble falling asleep) and sleep apnea (breathing trouble during sleep). Your provider can help you get the diagnosis and treatment you need.
8 Tips, Medications, and Supplements to Try
How to Get More REM Sleep: 8 Tips, Medications, and Supplements to Try- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Raj Dasgupta, MD — By Jaime Herndon, MS, MPH, MFA on June 29, 2021
Insomnia, undiagnosed sleep disorders and chronic sleep deprivation can result in a lack of rapid eye movement (REM) sleep, which can have a serious impact on your quality of life — and your health.
Good sleep is important for our bodies and minds. Without it, it’s hard to concentrate, our immune system is weakened, and we can become short-tempered, just to name a few things.
There are ways to get better sleep, with or without medications.
There are some things you can do to help you get better REM sleep. You might have to try one or more to see what works for you.
- Develop a sleep schedule. Go to bed and wake up at the same time every day. This primes your body for sleep and waking.
- Don’t drink caffeine or smoke cigarettes later in the day. These are stimulants and can interfere with sleep.
- Avoid alcoholic drinks at night. Though they may initially make you sleepy, they actually interfere with sleep, particularly REM sleep.
- Put together a relaxing sleep routine before bed. Warm baths, relaxing music like classical music, or quietly reading are all good activities.
- Get regular exercise. Try to get about 20 to 30 minutes a day, but do so several hours before bed.
- Create an ideal environment for sleep. That means no bright lights, not too hot and not too cold, and don’t watch television or work on the computer in the bedroom.
- If you can’t sleep, don’t lie in bed awake. Get up and go into another room and do something quietly, like read or listen to relaxing music, until you’re sleepy.
- Replace your pillows. If you’ve had your pillows for more than a year, consider replacing them. This might make you more comfortable for sleep. Want suggestions? Browse our market, filled with editor-trusted and expert-verified pillow recommendations.
If nothing works, talk with a medical professional. They may have other suggestions, run some tests to see if there’s an underlying cause for your sleep issues, or talk with you about prescribing medication.
Without deep sleep and REM sleep, you might find yourself becoming cranky, unable to focus, and it may impair your work performance and quality of life. Chronic sleep deprivation can be very unpleasant.
Chronic sleep deprivation can be very unpleasant.
It’s essential to make sure you’re getting not only the appropriate quantity of sleep but quality of sleep also. So, be sure to be evaluated by your doctor or primary care provider before taking any medications or supplements to help you sleep. Especially because some sleep medications can be addictive.
Mental health conditions
Certain psychiatric conditions are known to affect sleep and REM sleep. These include schizophrenia, bipolar disorder, and major depressive disorder. All have been associated with disturbances in REM sleep. Treating the underlying psychiatric condition along with cognitive behavioral therapy (CBT) both help to normalize sleep.
Chronic insomnia
Chronic insomnia often has multiple causes and the correct assessment and treatment of all contributing causes is critical for maximum therapeutic benefit. A broad assessment should be performed in all patients to identify predisposing and precipitating factors such as depression, anxiety, pain, and medications that may be interfering with sleep.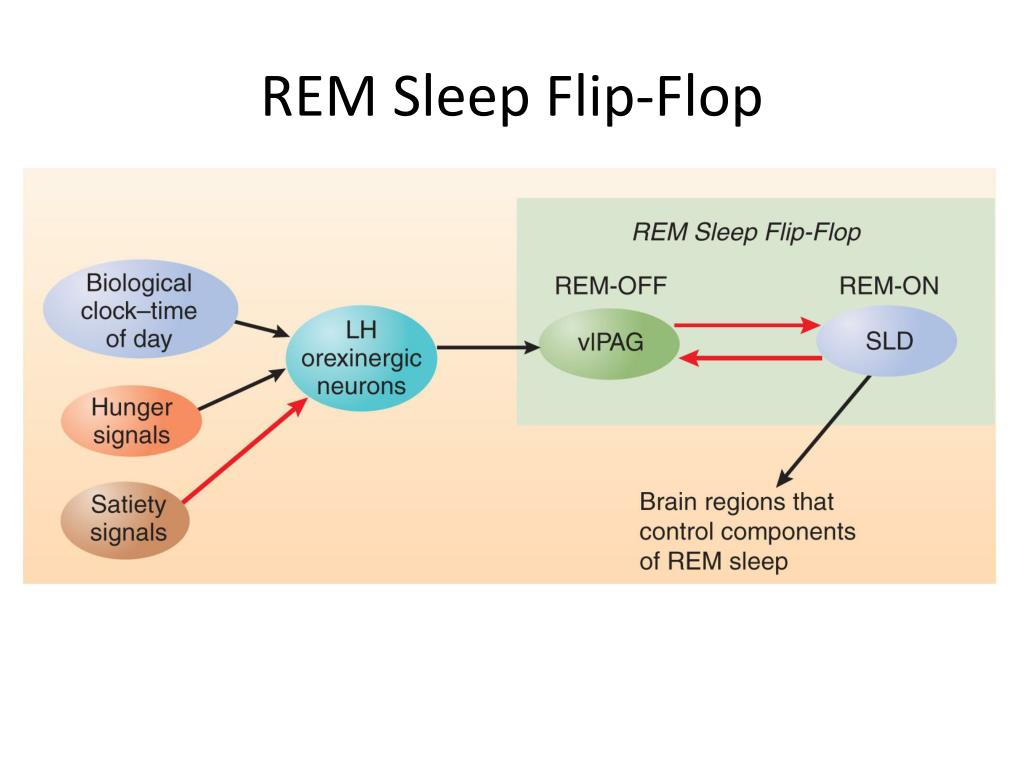
If you’re living with chronic insomnia the main treatment is cognitive behavioral therapy as first-line therapy, rather than medications. If your doctor prescribes a sleep aid, the specific medication they prescribe will depend on things like:
- your symptoms
- the goals of treatment
- your medical history and preferences
- the cost
- potential adverse effects
There are also supplements you can use to help with sleep in combination with good sleep hygiene. It’s important to remember that even though they aren’t prescription and they may be considered all-natural, that it doesn’t mean they’re necessarily safe.
Talk with a medical professional before using any supplements to make sure they’re safe and won’t interfere with any medications you may be taking.
Supplements that may be helpful with sleep include:
- melatonin
- valerian root
- magnesium
- chamomile
- tryptophan
- glycine
- L-theanine
- gingko biloba
We all need sleep — good sleep — in order to function.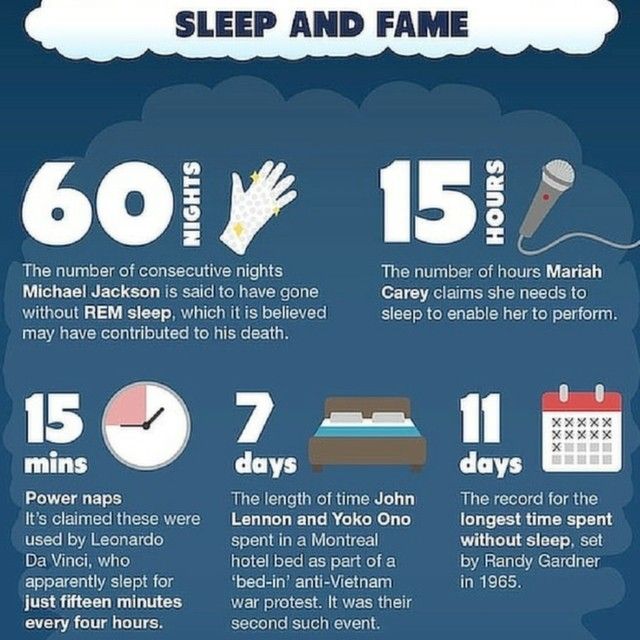 Sleep restores our bodies and minds, and without enough REM sleep, you won’t feel rested or rejuvenated. If you have daytime sleepiness or exhaustion that’s interfering with your work or day-to-day functioning, talk with a medical professional.
Sleep restores our bodies and minds, and without enough REM sleep, you won’t feel rested or rejuvenated. If you have daytime sleepiness or exhaustion that’s interfering with your work or day-to-day functioning, talk with a medical professional.
They might want to run sleep tests or do a physical to rule out any underlying causes.
Adequate REM sleep is necessary for good health and proper functioning. Chronic sleep deprivation can negatively impact your quality of life — but it doesn’t have to. There are ways to get better sleep. If lifestyle changes don’t help with sleep, talk with your doctor about medications, either over-the-counter or prescription, that might be helpful to you.
Last medically reviewed on June 29, 2021
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.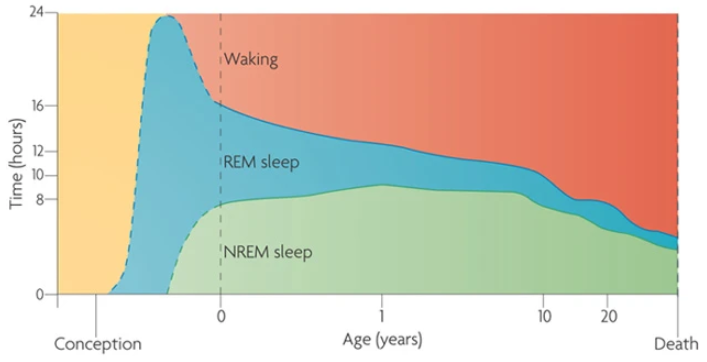
- Abbasi B, et al. (2012). The effect of magnesium supplementation on primary insomnia in the elderly: A double-blind placebo-controlled clinical trial.
ncbi.nlm.nih.gov/pmc/articles/PMC3703169/ - Boyle NB, et al. (2017). The effects of magnesium supplementation on subjective anxiety and stress – a systematic review.
ncbi.nlm.nih.gov/pmc/articles/PMC5452159/ - Brain basics: Understanding sleep. (2019).
ninds.nih.gov/Disorders/patient-caregiver-education/Understanding-sleep#8 - Feriante J, et al. (2021). Physiology, REM sleep.
ncbi.nlm.nih.gov/books/NBK531454/ - Ferracioli-Oda E, et al. (2013). Meta-analysis: Melatonin for the treatment of primary sleep disorders.
journals.plos.org/plosone/article?id=10.1371/journal.pone.0063773 - Hemmeter U, et al. (2001). Polysomnographic effects of adjuvant gingko biloba therapy in patients with major depression medicated with trimipramine.
 DOI:
DOI:
10.1055/s-2001-15182 - Kim S, et al. (2019). GABA and L-theanine mixture decreases sleep latency and improves NREM sleep.
ncbi.nlm.nih.gov/pmc/articles/PMC6366437/ - Lie JD, et al. Pharmacological treatment of insomnia.
ncbi.nlm.nih.gov/pmc/articles/PMC4634348/ - Roehrs T, et al. (n.d.). Sleep, sleepiness, and alcohol use.
pubs.niaaa.nih.gov/publications/arh35-2/101-109.htm - Yamadera W, et al. (2007). Glycine ingestion improves subjective sleep quality in human volunteers, correlating with polysomnographic changes.
onlinelibrary.wiley.com/doi/full/10.1111/j.1479-8425.2007.00262.x
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Jun 29, 2021
Written By
Jaime R. Herndon, MS, MPH, MFA
Edited By
Allison Tsai
Medically Reviewed By
Raj Dasgupta, M.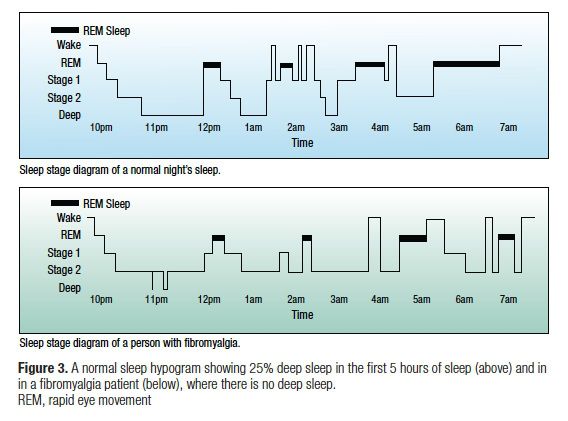 D.
D.
Copy Edited By
Naomi Farr
Share this article
Medically reviewed by Raj Dasgupta, MD — By Jaime Herndon, MS, MPH, MFA on June 29, 2021
Read this next
What Is the Purpose of Sleep?
Medically reviewed by Raj Dasgupta, MD
Research has shown that sleep helps your body and brain repair, restore, and reenergize. Lack of sleep can lead to many negative effects.
READ MORE
Best Sleeping Positions for a Good Night’s Sleep
Knowing your best sleeping position can be harder than you think. It may be worth trying a new position. You might gain more than just a good night’s…
READ MORE
The 8 Sleep Trackers that Will Assure You Get the Beauty Sleep You Need
Sleep trackers are equipped with tools and features, such as sleep duration and quality, heart rate, blood oxygen level, that can help you make…
READ MORE
7 Podcasts for Sleep, Relaxation, and Sleep Science
Medically reviewed by Alana Biggers, M.
 D., MPH
D., MPHWhether you’re looking for a “boring” podcast to put you to sleep, something lighthearted to fall asleep to, ambient noise, or want to learn more…
READ MORE
The Best Mattresses for Back and Neck Pain in 2023
Medically reviewed by Gregory Minnis, DPT
Tired of missing out on good sleep because of back and neck pain? A new mattress can be a good place to start.
READ MORE
The 11 Best Full-Size Mattresses in 2023
Looking to upgrade your full-size mattress this year? Check out our top picks for the best options to consider in 2023.
READ MORE
Find Your Mattress Match with This Mattress Quiz
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Take our five-question quiz to get mattress recommendations made just for you, plus mattress shopping basics to get you started.
READ MORE
The 10 Best Mattresses for Pressure Point Relief
Medically reviewed by Gregory Minnis, DPT
These 10 mattresses are some of the best for pressure point relief. No matter how you like to sleep, you’re sure to find a great fit.
READ MORE
These Common Medications May be Silently Damaging Your Kidneys
Commonly used prescription and over-the-counter drugs, including some antibiotics and blood pressure medications, can cause significant damage to your…
READ MORE
what to do if sleep is bad, how to get rid of the problem
We all need proper sleep to be productive and enjoy life. The quality of the night's rest determines how joyful the morning rise will be, as well as whether our spirit will be cheerful, and the view will be blooming. In the article we will talk about the causes of sleep disturbance, about ways to prevent and solve problems with sleep
In the article we will talk about the causes of sleep disturbance, about ways to prevent and solve problems with sleep
“Sleep mode” is an opportunity for the body to replenish energy and bring the functions of all systems in order. At night, the load on the organs decreases, their work slows down, the muscles relax - in a word, complete peace sets in.
Many have heard the statement that the duration of healthy sleep is eight hours, but the norm is different for everyone: someone needs six, someone needs all nine to feel good. Much depends on the way of life: for example, after active physical and mental work, more time is needed for rest. In particular, the norm of healthy sleep depends on age. Babies sleep 10-16 hours a day, by the age of three, the duration of rest decreases to ten hours. From the age of 13, seven to nine hours is already enough, and this will continue until old age: after 65 years, as a rule, it takes only five to six hours to sleep.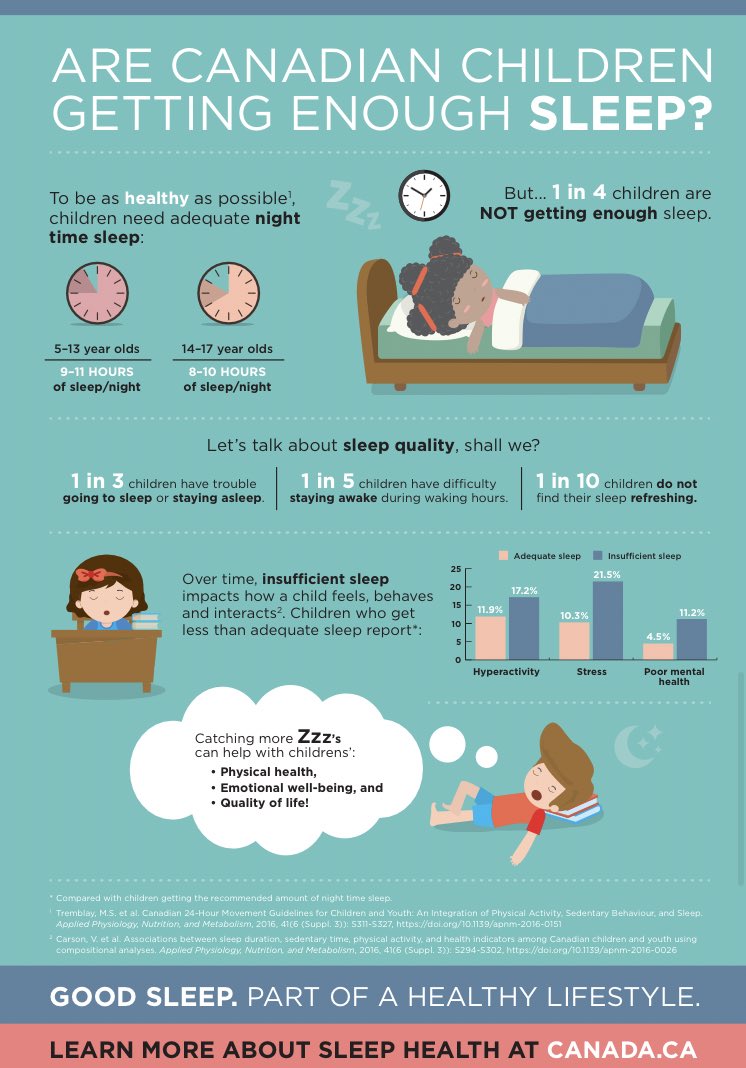
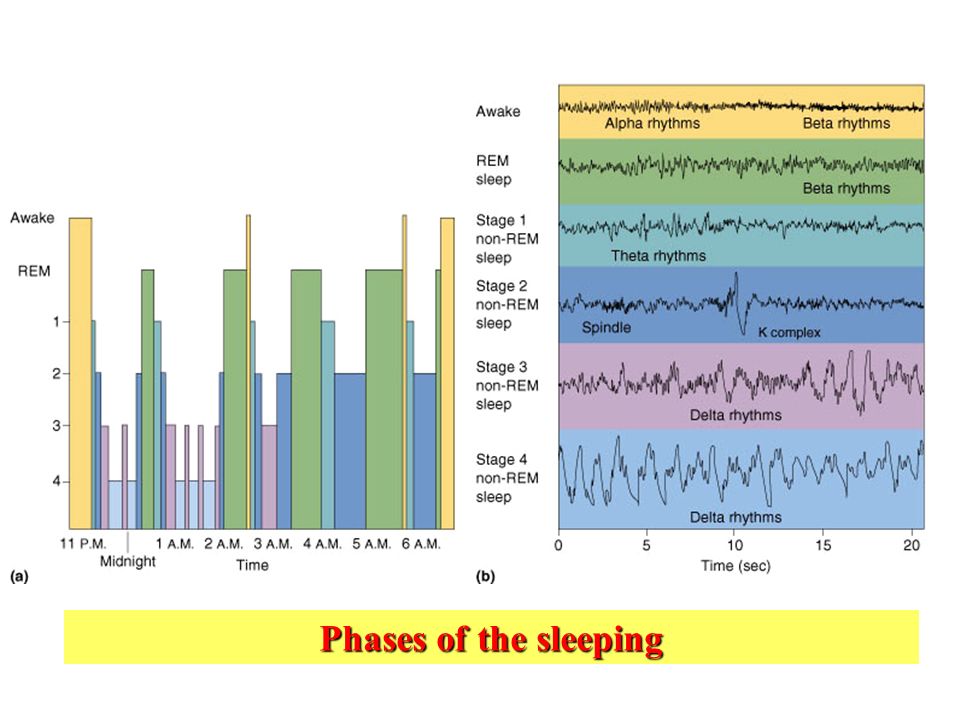
The most favorable time for going to bed is between 10:00 pm and 2:00 am. Sleep is cyclical, all night there is an alternation of two phases - slow and REM sleep, and normally there should be four to five cycles.
Phase slow sleep begins right after falling asleep. The duration is about one and a half hours, and this is the most relaxed state of the body: breathing becomes less frequent, blood pressure decreases and metabolism, brain and muscle activity, and temperature slow down. The body restores physical strength. Slow-wave sleep is very important, because it is during this phase that our body fully rests, immune cells are restored. In addition, being in the phase of deep sleep, the brain performs a “night cleaning” - it gets rid of the accumulated toxic waste products.
REM sleep follows deep sleep and lasts about 20 minutes. The eyeballs move rapidly under the eyelids, which is why this phase is also called the rapid eye movement stage (REM sleep).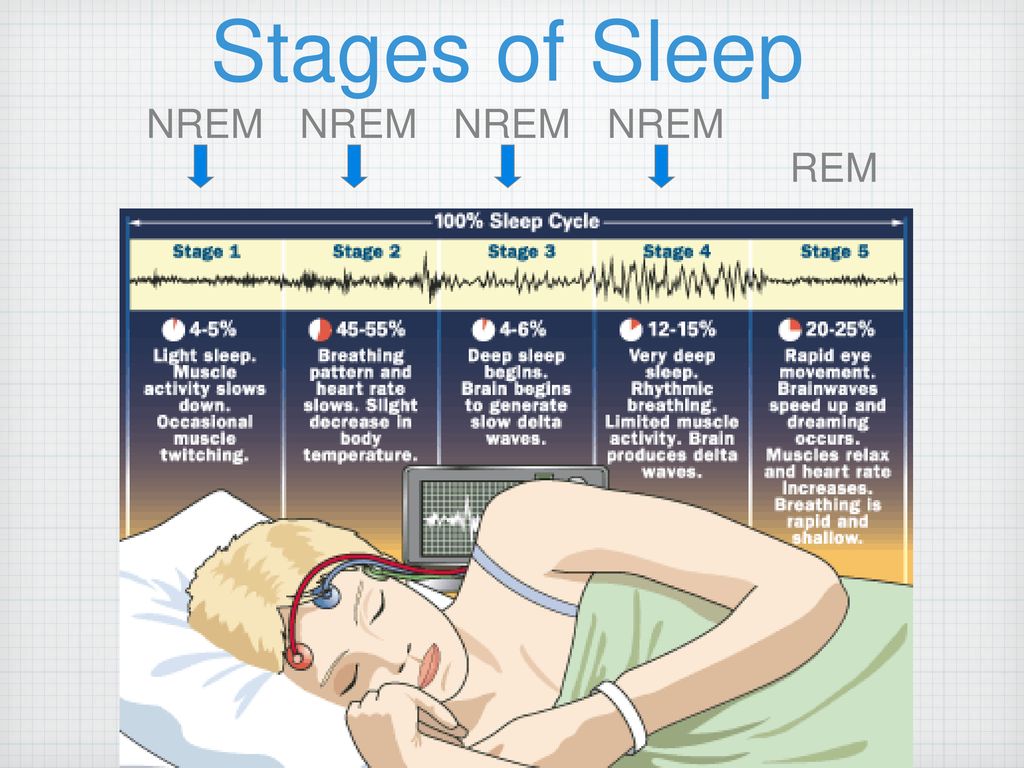 The pressure rises slightly, brain activity increases, and the secretion of adrenal hormones increases. If we wake up at this time, we remember the dream very vividly. However, the chances are not so much - only 20% of a night's sleep falls on the "fast" phase.
The pressure rises slightly, brain activity increases, and the secretion of adrenal hormones increases. If we wake up at this time, we remember the dream very vividly. However, the chances are not so much - only 20% of a night's sleep falls on the "fast" phase.
Problems with sleep at night, unfortunately, cannot remain without consequences: it can be a deterioration in memory, attention, a decrease in overall productivity. With a lack of sleep, the risks of getting sick increase, because there are fewer immune cells. A sleepy person is prone to overeating, which leads to problems with being overweight, as well as to disruption of the cardiovascular system. The emotional state becomes unstable: even what previously seemed interesting can annoy. Lack of sleep also affects the appearance: the skin ages prematurely, bags under the eyes appear.
Too much sleep is also a problem. So, with more than nine hours of nightly rest, biorhythms go astray, which leads to a constant feeling of fatigue.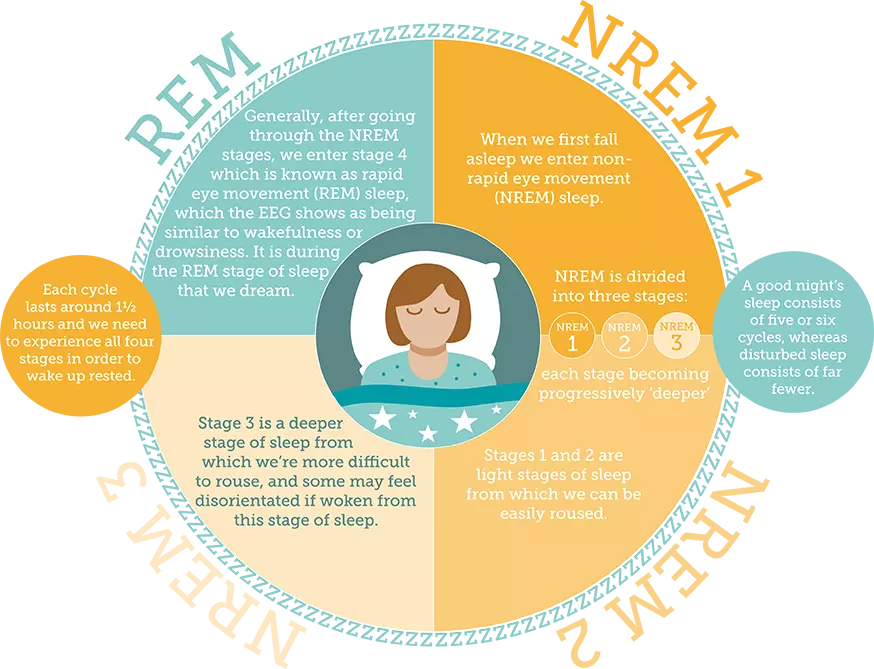 Also, excess sleep is closely related to depression: it is both one of the causes and a consequence of depressive states. In addition, too much sleep increases the risk of coronary disease and diabetes, leads to pain in the neck, lower back and spine.
Also, excess sleep is closely related to depression: it is both one of the causes and a consequence of depressive states. In addition, too much sleep increases the risk of coronary disease and diabetes, leads to pain in the neck, lower back and spine.
What causes sleep problems?
The causes of poor sleep usually lie in the daily routine, the influence of stress. Here are the most common factors:
- Sleep disturbance . If after a five-day work week you get ten hours of sleep on the weekend, your circadian rhythms get off.
- Poor sleep hygiene . Stuffiness in the bedroom, light, noise can contribute to the appearance of insomnia.
- Chronic and acute stress . Problems at work and in the family often affect health and, in particular, the quality of sleep. Thinking about the coming day can increase nervous excitability, which also makes it difficult to fall asleep.
- Taking medications that list insomnia as a side effect.

Ways to deal with the problem
Simple methods will help prevent the problem and ensure healthy deep sleep. Here are some recommendations:
- Go to bed and wake up at the same time and . The regime is developed within two months, do not break this rule even on weekends, when there is an opportunity to stay in bed longer. As a reward, you will receive an easy awakening and cheerfulness.
Note
Our ancestors went to bed and got up with the sun, just the way nature intended. A modern person in the winter has to get up and go to work long before dawn. To prepare the body for awakening, you can use a special alarm clock that simulates dawn.
- Ventilate the bedroom . Fresh air and a comfortable temperature (not higher than 22°C) will ensure deep sleep and a gentle rise.
- Do not use gadgets before bed .
 Phones, tablets, TVs emit blue light, which inhibits the production of melatonin. This is the so-called darkness hormone, which transmits information to the brain that the night has come, which means it's time to sleep.
Phones, tablets, TVs emit blue light, which inhibits the production of melatonin. This is the so-called darkness hormone, which transmits information to the brain that the night has come, which means it's time to sleep. - Do not eat at night . It takes energy to digest heavy meals, hence sleep time is delayed. In addition, it is better to refuse dinner with coffee, strong tea, dark chocolate: the caffeine contained in these products excites the nervous system. Don't go to bed hungry either. Light cottage cheese or yogurt will be useful both for healthy sleep and for the figure.
If the problem already exists, poor sleep in an adult will help to correct:
- Meditation, breathing practices. They reduce the level of stress, emotional stress, it facilitates the process of falling asleep and prevents night rises.
- Refusal of bad habits. The use of any alcohol leads to dehydration, shortens REM sleep. After nicotine, the body rests more superficially, night rises become more frequent.
- Phytotherapy. Decoctions with chamomile, lemon balm, hops, motherwort or oregano will help you calm down and relax after a busy day. A warm bath with a few drops of lavender, lemon balm or bergamot essential oil will give the same effect.
- Dietary supplements and over-the-counter medications to improve sleep. As a rule, such products are made on a plant basis. But in comparison with homemade decoctions and herbal tinctures, they are more convenient to use: the pharmaceutical market offers tablets, syrups, and drops.
The recipe for healthy sleep is quite simple. But if the observance of the daily regimen and the correction of lifestyle depend solely on the person himself, then with such a “culprit” of insomnia as stress, the situation is more complicated. Unfortunately, it is far from always possible to protect yourself from it, but it is still possible to cope with psycho-emotional stress. This can be done with the help of mild sedative drugs - most importantly, do not forget to consult a specialist before starting the reception.
How does the sleep mechanism work, and what can go wrong in it? - Personal experience on vc.ru
Let's figure out what components a healthy sleep consists of. Reminder edition material.
16,887 views
Unsplash
The list of sleeping pills available from pharmacies with a prescription is long: barbiturates, benzodiazepines, Z-hypnotics - and these are just the names of drug groups. But the best treatments for sleep problems are still sleep hygiene and cognitive behavioral therapy for insomnia.
Sleeping pills help you fall asleep, but not sleep well. The state of the brain after taking the pills is not like natural sleep, and insomnia increases rather than disappears. Why sleeping pills don't work? To understand this, you must first understand how sleep works. Then it will immediately become clear where sleep problems come from and how to properly influence them.
The problem is that scientists still have not figured out the mechanism of sleep and cannot even identify one main "sleep center".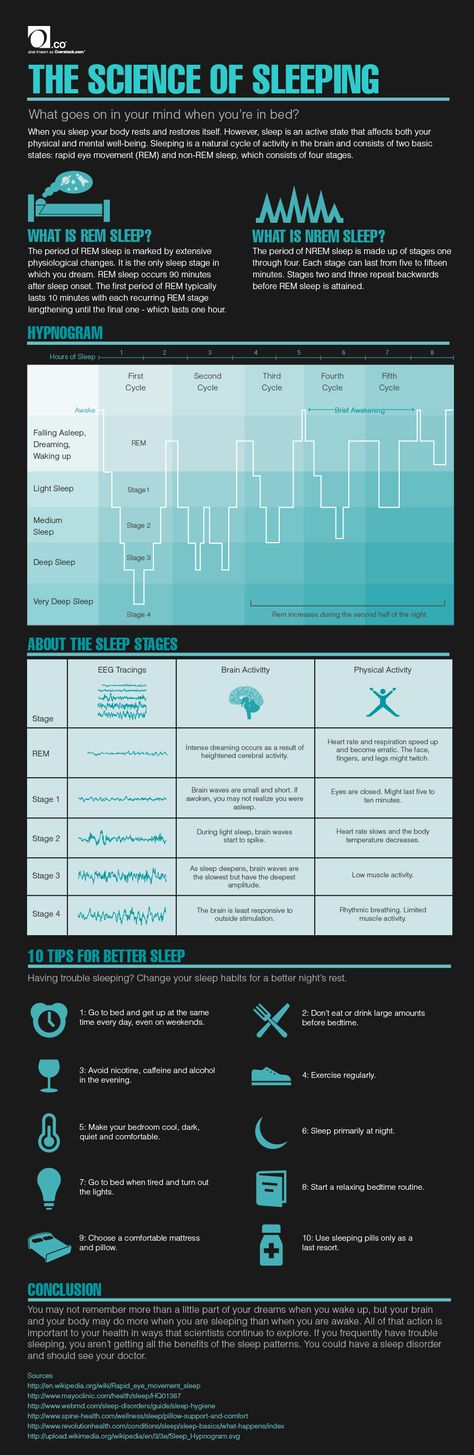 So that we can fall asleep, live in a dream world and wake up, a complex system works in the body 24/7. Some of its mechanisms operate in parallel to each other, while others are more closely connected and function in a chain.
So that we can fall asleep, live in a dream world and wake up, a complex system works in the body 24/7. Some of its mechanisms operate in parallel to each other, while others are more closely connected and function in a chain.
Imagine a factory: in one workshop they work on proteins of the circadian rhythm, in another they synthesize melatonin from serotonin, in the third they cool and warm the body, in the fourth they activate or calm the nervous system. If there is a strike in one department or equipment breaks down, the final product (dream) becomes wrong. Crooked or broken. This is not only about the problem with falling asleep: it is also about nighttime awakenings, and about daytime sleepiness, and about sleep that does not bring rest - that is, both about the quantity and quality of sleep at the same time.
Department of slow and REM sleep
It seems that our body has two main states: sleep and wakefulness. Actually it is not. At this point, somnologists often refer to the ancient Indian treatises of the Upanishads, and this is a truly fascinating story.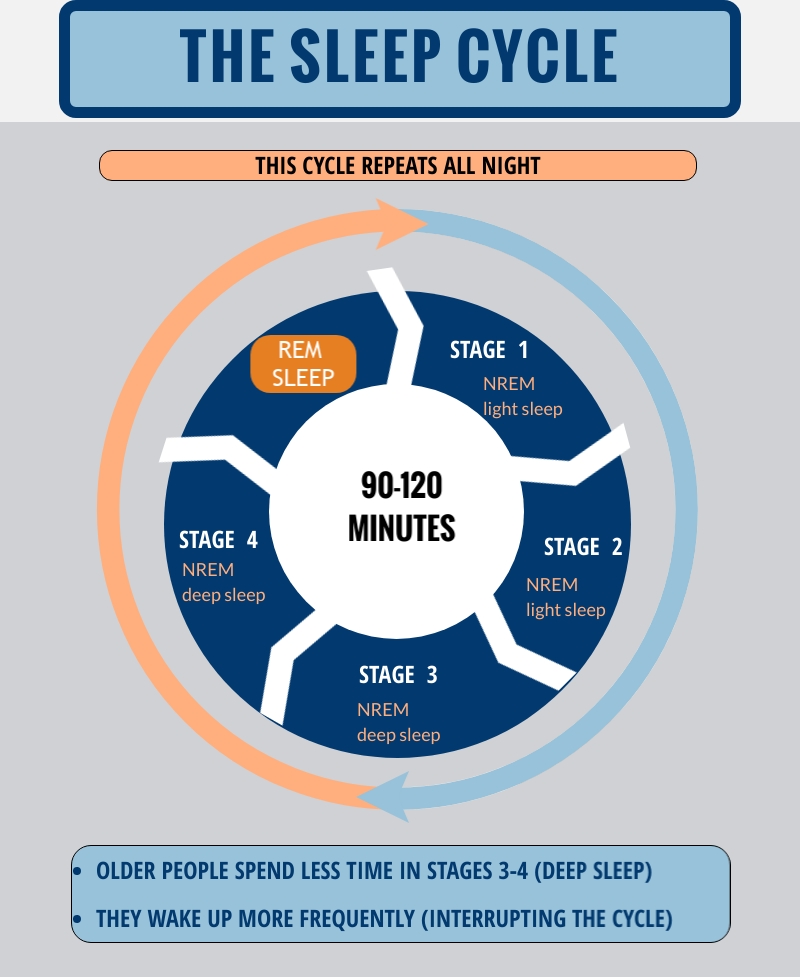
The Upanishads say that there is wakefulness, when a person becomes aware of the world around him, slumber with dreams, where he forms a new world from what he sees in wakefulness, and sleep, in which we are freed from desires, anxieties of the bonds of the body, merge with Brahman and experience bliss . These three forms of consciousness are combined in the form of a superconscious true Self - but, alas, scientists have not found it. But they proved that we really experience the first three states as in the Upanishads: wakefulness, deep slow-wave sleep (Non-REM-sleep, the one that is most similar to the standard idea of sleep as a rest of the body) and REM sleep (REM sleep, REM sleep, in which our brain works in a very special way).
Why such difficulties? Nobody knows for sure. A beautiful explanation of sleep phase changes is given by a British neuroscientist, professor at the University of California at Berkeley and author of the book Why We Sleep. The New Science of Sleep and Dreams Matthew Walker: Sleep is a general cleaning of the brain.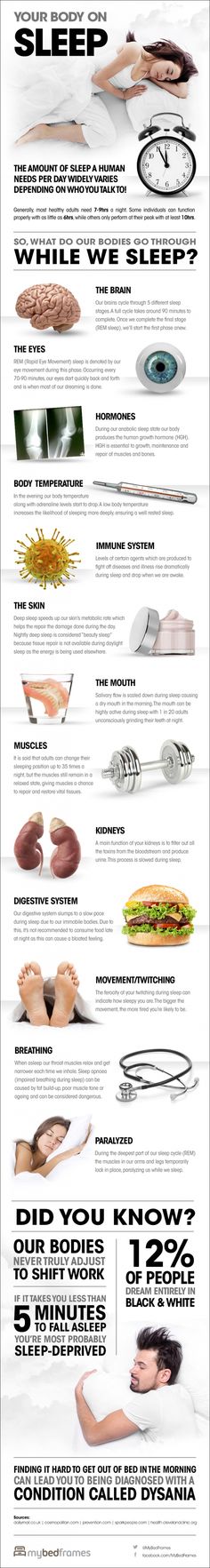 Unnecessary memories are deleted, relevant ones are played again and transferred from short-term memory to long-term memory. During non-REM sleep, the brain detects junk - unnecessary neural connections - and removes them. During REM sleep, we reflect and strengthen neural connections, which may be why we dream.
Unnecessary memories are deleted, relevant ones are played again and transferred from short-term memory to long-term memory. During non-REM sleep, the brain detects junk - unnecessary neural connections - and removes them. During REM sleep, we reflect and strengthen neural connections, which may be why we dream.
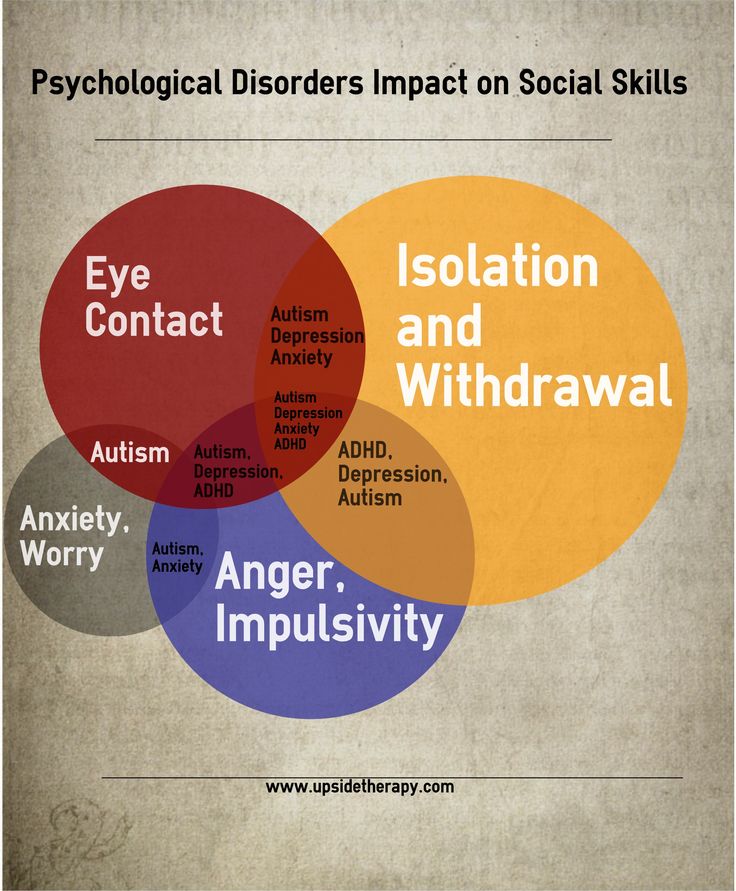
It is important that both phases are present in our sleep. Lack of REM sleep makes us less able to discern other people's emotions and regulate our own—that is, lowers emotional IQ. Interestingly, children with autism have less REM sleep than children without the disorder (although it is too early to talk about a causal relationship). Selective deprivation of rat pups in REM sleep experiments distorted the formation of synapses between neurons in the nervous system and made them withdrawn and depressed in adulthood.
Similar studies with deep sleep deprivation slowed brain development in rat pups and made them less socially active. As for the sleep of adults, it is ineffective even without the intervention of scientists: by the age of 40, a person loses 60-70% of deep sleep, by the age of 70 - 80-90%.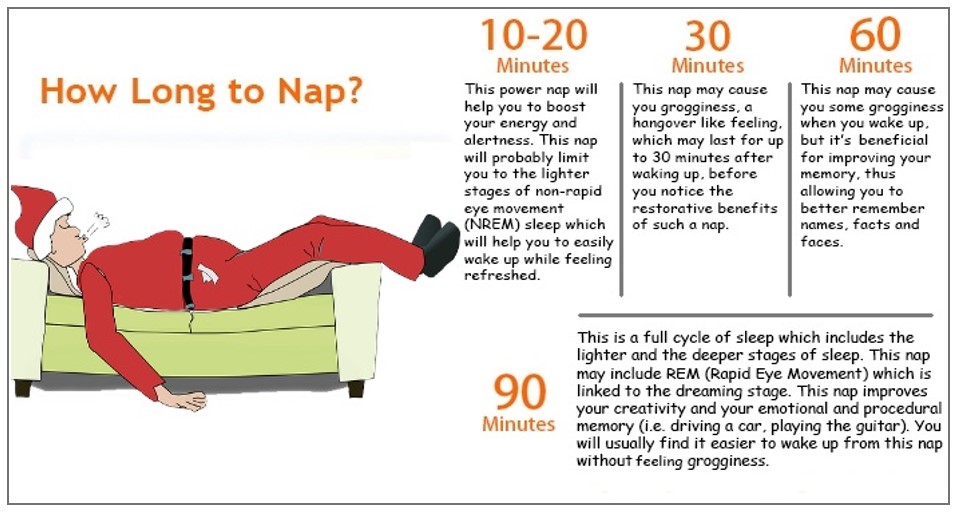 These numbers are not harmless: along with deep sleep, we lose the ability to learn and remember, and we also accumulate toxic amyloid protein in the brain and because of this we risk developing Alzheimer's.
These numbers are not harmless: along with deep sleep, we lose the ability to learn and remember, and we also accumulate toxic amyloid protein in the brain and because of this we risk developing Alzheimer's.
You don't have to wait until the age of 70 to experience the effects of sleep deprivation. In the first half of the night we experience non-REM sleep with short intervals of REM sleep, in the second half we experience REM sleep with interspersed slow-wave sleep. Falling asleep at midnight and sleeping six hours instead of eight, we lose not 25% of sleep, but 60-90% REM sleep. And falling asleep at two in the morning and waking up at eight in the morning - some share of slow sleep. REM sleep is also blocked by alcohol, many antidepressants, and sleeping pills. But more on that later.
Department of biorhythms
Each of our cells is subject to a biological clock that regulates circadian rhythms. Those adapt the body to different stages of the day. This is not only switching from “sleep” to “wake” mode, but also everything that happens to the body during the day: temperature, pressure and pulse, how fast the metabolism goes, and even want to eat or not.
This is not only switching from “sleep” to “wake” mode, but also everything that happens to the body during the day: temperature, pressure and pulse, how fast the metabolism goes, and even want to eat or not.
It is worth keeping in mind that, in general, a person's biological day is not 24 hours, but approximately 24 hours: an average of 24 hours and 15 minutes. (On average, because the period of the circadian rhythm differs from person to person. So both with a partner and with a cat we live at different times, even if we sleep in the same bed.) The “internal clock” is in a hurry, and we inevitably experience mini- jetlag. Every day.
Suprachiasmatic nucleus workshop
Above the intersection of the optic nerves in the very center of our brain, in the anterior lobe of the hypothalamus, there is a small but important area - the suprachiasmatic nucleus. All 20,000 of its neurons analyze light signals every second and adjust the "biological clock".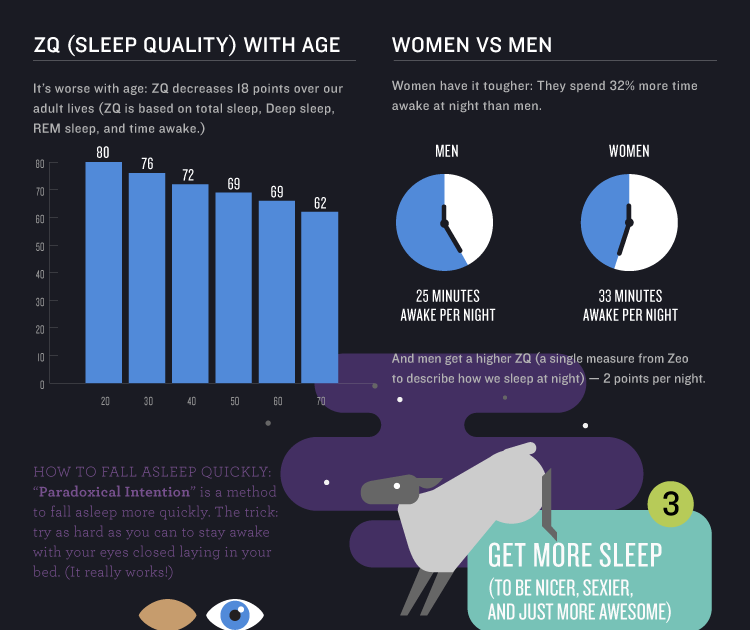
Even blindness does not prevent the suprachiasmatic nucleus from understanding whether it is day, evening or night: light is recognized by special neurons in the structure of the retina, photosensitive ganglion cells (pRGC).
Complete and partial blindness is most often caused by damage to other photoreceptors of the eye, rods and cones, and does not affect light-sensitive ganglion cells - therefore, if the eyes are in place, the body knows whether it is day or evening.
Melatonin workshop
The signal about light or its absence goes from the neurons of the suprachiasmatic nucleus through the hypothalamus and spinal cord to the superior cervical ganglion and the pineal gland or the pineal gland (it is interesting that in Ayurveda it is called the "third eye chakra"). The pineal gland synthesizes the familiar neurotransmitter serotonin, and after a signal from the superior cervical ganglion, it turns it into the “sleep hormone” melatonin (the same one that you buy in a pharmacy without a prescription – only natural).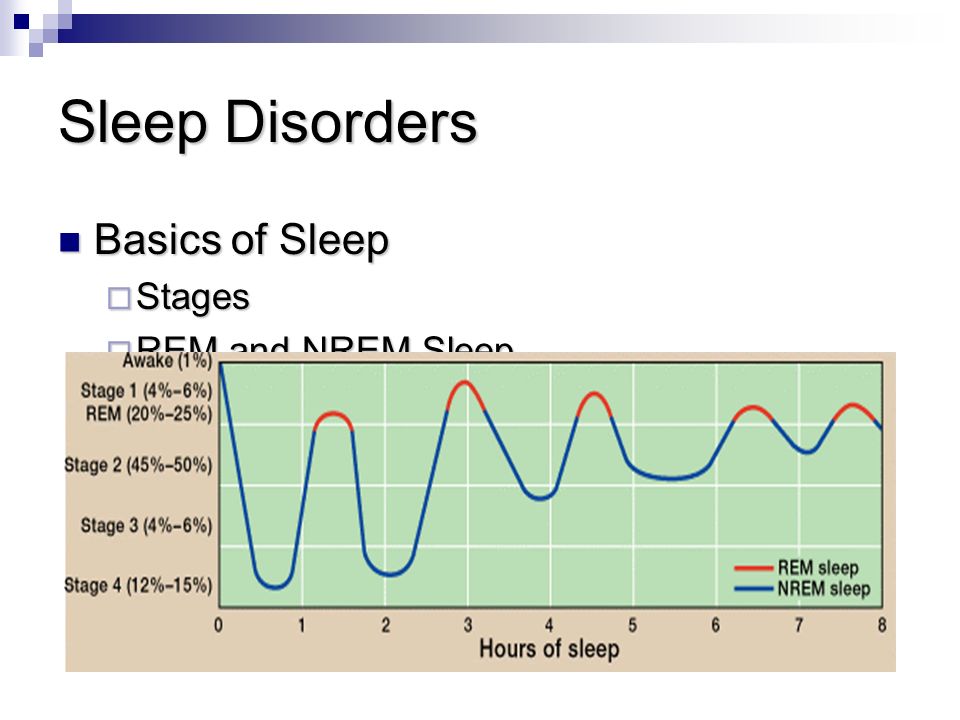
Melatonin does not create a state of sleep, but only tells the body: "Now is the time for this beneficial action!" Its concentration gradually increases at dusk, reaches a maximum at about 4-5 am local solar time (about 05:00-06:30 in Moscow) and then slowly decreases. With dawn, which signals the pineal gland to turn off the melatonin tap, we wake up.
A small luminous object with a power of 8 lux or more is enough to confuse our suprachiasmatic nucleus and delay the synthesis of melatonin. For comparison: the most modest 20 W incandescent lamp or 3 W LED produces 250 lux.
"Circadian" protein shop
The “circadian” gene, period, encodes the PER protein, which accumulates at night, decomposes during the day and determines whether we feel alert or tired. The PER protein is assisted by two accessory proteins, TIM (encoded by the timeless gene) and DBT (encoded by the doubletime gene). TIM stimulates the accumulation of PER in the body, DBT, on the contrary, blocks this accumulation. Because of this mutual work or, one might even say, the constant struggle between TIM and DBT, the PER level during the day is unstable and fluctuates - in accordance with circadian rhythms. Mutations in PER lead to sleep problems.
Because of this mutual work or, one might even say, the constant struggle between TIM and DBT, the PER level during the day is unstable and fluctuates - in accordance with circadian rhythms. Mutations in PER lead to sleep problems.
In general, today not even three “clock” genes are known, but 14, and there are also more “circadian” proteins. For example, the CRY protein is activated by light and affects TIM, while TIM affects PER. The interaction of these and similar proteins forms our chronotype - a way of life in a biological day according to an individual circadian rhythm.
Imagine a scale with two poles: at one end - "larks", who go to bed early and rise early, at the other - "owls". Most people are not at the poles, but somewhere in between - such "middle peasants" from 60 to 80%. Having explored this space "between", chronobiologists have identified seven chronotypes. (You can find out yours with the Munich Chronotype Questionnaire (MCTQ).)
So the “department of biorhythms” works according to the following scheme:
Circadian proteins set the general rhythm, that is, the chronotype → no light → light-sensitive ganglion cells have calmed down and no longer transmit nerve impulses → the suprachiasmatic nucleus has calmed down → the pineal gland increases the secretion of melatonin → it’s time sleep.

Sleep problems that occur in the “jorhythm department” correlate with a variety of diseases: depression and bipolar disorder, diabetes, glucose intolerance, and even cancer. The International Agency for Research on Cancer at WHO has already called night shift work "probably carcinogenic". That being said, “night shift” is just a convenient definition. In fact, this is about everyone who is somehow forced to stay awake during the time that their internal clock considers night (for example, getting up at 6 in the morning if you are a “night owl”), or often crosses time zones.
'Circadian' sleep disorders are called circadian rhythm sleep disorders (CRSD) but are difficult to diagnose. For example, delayed sleep phase syndrome / delayed sleep phase disorder: a person falls asleep in the morning and feels tired simply because he had to rise too early according to his biological clock. This syndrome is associated with a genetic mutation and does not interfere with life if you sleep, say, from 4 to 13 hours.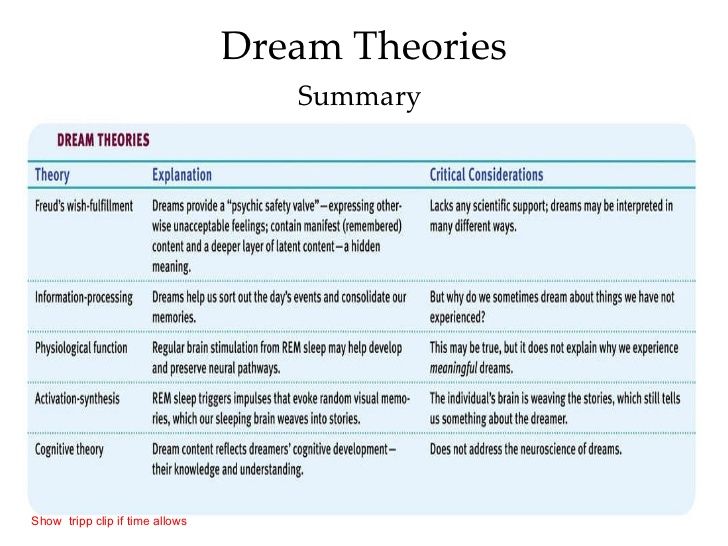 A non-specialist, and a specialist too, can confuse delayed sleep syndrome with insomnia.
A non-specialist, and a specialist too, can confuse delayed sleep syndrome with insomnia.
Department of braking and activation
Real sleep is caused by neurotransmitters that inhibit or activate the central nervous system. If there are few “brake” mediators or a lot of “activating” mediators, we toss and turn in bed for a long time without sleep - even if we didn’t fly to another time zone, put gadgets aside in time, and everything is in order with biorhythms.
Two competing blocks within the autonomic nervous system are responsible for the processes of activation and inhibition. The first block, the sympathetic nervous system, mobilizes the body: it makes the heart beat faster, speeds up metabolism, and dilates the pupils. Sounds like a fight-or-flight state, right? Not in vain. Stress is the element that activates the sympathetic nervous system. The second block, the parasympathetic nervous system, prepares us for rest.
Norepinephrine shop
When the signal about the absence of light goes to the “melatonin workshop”, it passes through the superior cervical ganglion.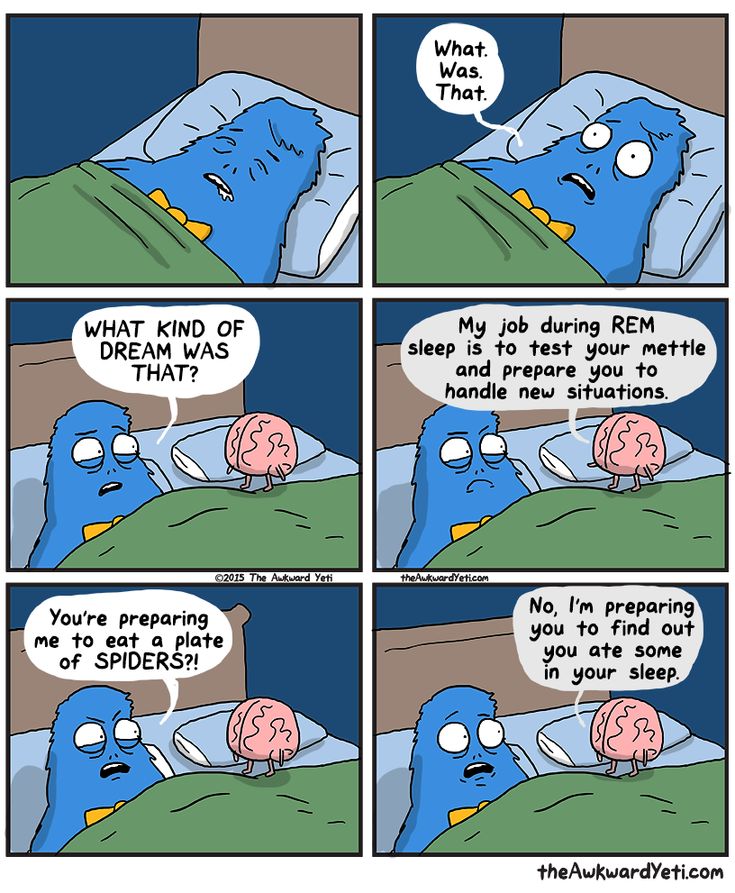 He not only gives a signal to the pineal gland that it is time to press the "melatonin" button, but also reduces the synthesis of the neurotransmitter norepinephrine. Norepinephrine is produced in response to stress along with adrenaline and cortisol, which inhibits sleep centers and activates the central nervous system. This is the main mediator of the sympathetic nervous system, and therefore, after quarrels or on the eve of an important day, it is so difficult to forget: it's all about an extra dose of norepinephrine.
He not only gives a signal to the pineal gland that it is time to press the "melatonin" button, but also reduces the synthesis of the neurotransmitter norepinephrine. Norepinephrine is produced in response to stress along with adrenaline and cortisol, which inhibits sleep centers and activates the central nervous system. This is the main mediator of the sympathetic nervous system, and therefore, after quarrels or on the eve of an important day, it is so difficult to forget: it's all about an extra dose of norepinephrine.
Thalamus shop
When we forget natural and healthy sleep, or rather, its deep slow-wave phase, we do not hear the noise of cars outside the window, we do not realize whether it is cold or hot in the room, and we do not feel that we lay down on our hand and squeezed it. Sensory signals are blocked by the thalamus, the thalamus in the center of the brain. It does not pass signals to the cerebral cortex and does not allow it to consciously perceive them.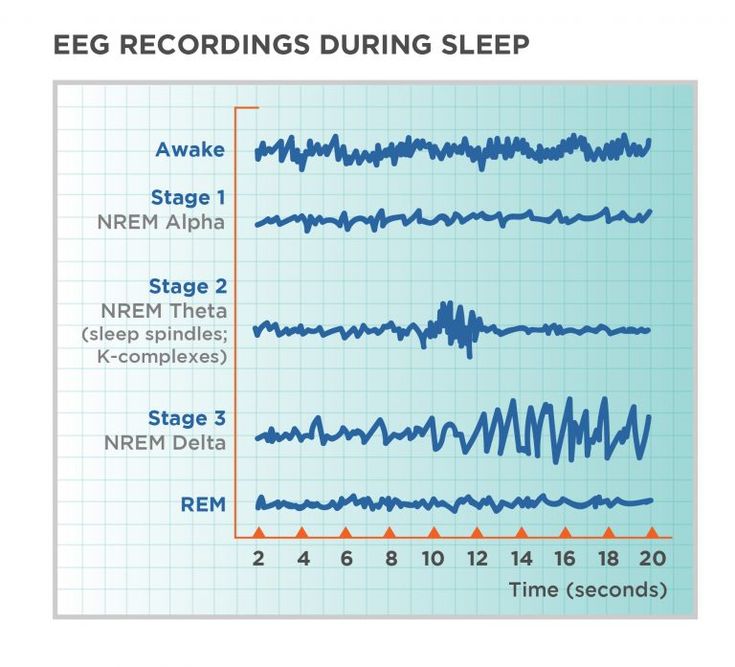 Roughly speaking, you hear - but do not listen, look - but do not see. The cerebral cortex is resting and not concentrating on trifles.
Roughly speaking, you hear - but do not listen, look - but do not see. The cerebral cortex is resting and not concentrating on trifles.
If the thalamus fails and its “sensory gates” do not close at night, sleep does not come. This happens with fatal familial insomnia (FFI, Fatal familial insomnia) - a rare genetic disease in which a mutation in one gene turns normal protein molecules into infectious prions. As a result of the attack of prions, amyloid plaques appear on the thalamus, it ceases to block sensory sensations, the patient cannot sleep, and eventually dies.
Orexin shop
The neurotransmitter orexin helps to increase the pressure of the brain stem on the thalamus and open its “sensory gates”. Getting from the hippocampus to the brain stem, it turns on wakefulness and perception - and vice versa, blocks contact with the outside world when it does not enter it. If there is not enough orexin and its receptors on the brainstem, a process begins that is the reverse of fatal family insomnia: the sensory gates of the thalamus are constantly closed, narcolepsy appears - a disease in which a person cannot fully wake up and then plunges into sleep, then emerges from it.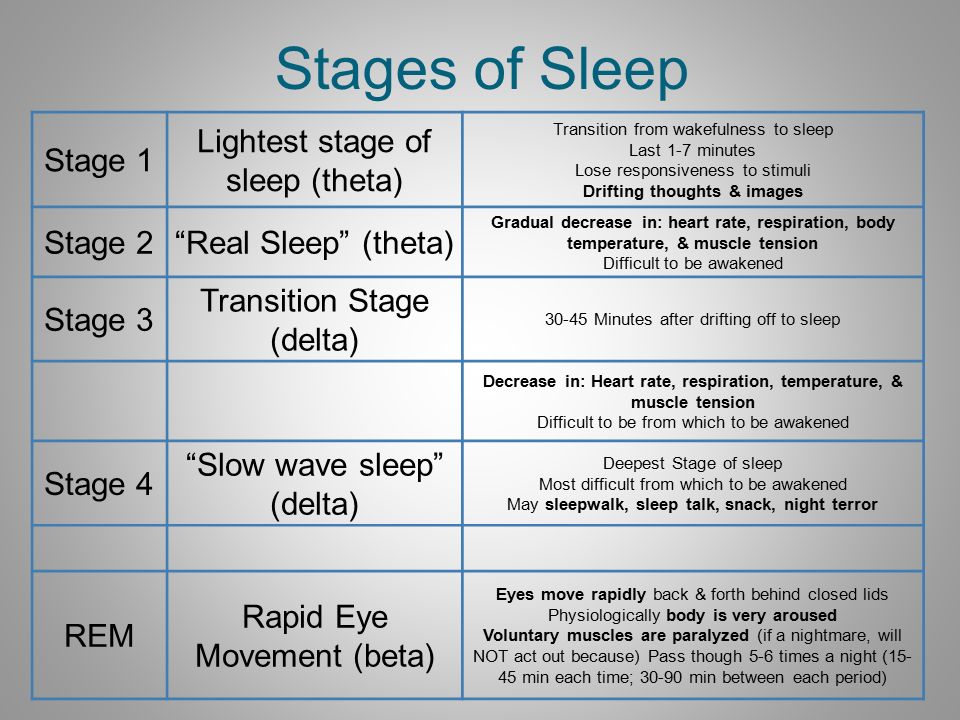
Adenosine shop
While we are awake and expending energy, the helper neuron cells of the brain, astrocytes, secrete adenosine. With every second of non-sleep, the concentration of adenosine rises until we feel sleep pressure: the eyelids stick together, and the jaw uncontrollably yawns. Caffeine blocks adenosine-sensitive receptors, that is, the feeling of fatigue - but not the fatigue itself and the need for sleep.
The peak of adenosine concentration after which we switch off (unless we drank coffee) occurs 16-20 hours after waking up - that is, waking up at 8 o'clock in the morning, you will feel sleepy around midnight. While we sleep, the concentration of adenosine drops to a minimum level. In order for the body to deal with the fatigue of the past day and be ready to get tired again, you need about 8 hours of sleep - that is, having fallen asleep at midnight, by 8 in the morning we dealt with adenosine and are ready to stay awake.
Acetylcholine workshop
The nerve endings of the parasympathetic nervous system produce acetylcholine, a neurotransmitter that lowers the level of arousal when it's time to rest, or, on the contrary, slows down the brain if it is too lethargic. Therefore, its effect on the body is called normalizing. During deep sleep, the concentration of acetylcholine drops by 50%, in REM sleep it increases to a value twice as high as during wakefulness.
Therefore, its effect on the body is called normalizing. During deep sleep, the concentration of acetylcholine drops by 50%, in REM sleep it increases to a value twice as high as during wakefulness.
Interaction of acetylcholine with other “workshops” of sleep looks something like this:
Adenosine accumulates → acetylcholine level decreases → we fall asleep and fall into deep sleep.
Acetylcholine is released during sleep → we move from deep sleep to REM sleep.
Acetylcholine is released + orexin is released → we wake up and stay awake.
In patients with Alzheimer's disease, the concentration of acetylcholine is always reduced - therefore, scientists believe that it is acetylcholine that helps us remember something new through sleep.
Workshop GABA
The processes of acetylcholine neurons reach the hippocampus and already tell other neurotransmitters in it that it is time to work or, on the contrary, to rest. So they act on gamma-aminobutyric acid, the neurotransmitter GABA - the most important element of sleep in terms of pharmacology: it is this that most sleeping pills activate.
So they act on gamma-aminobutyric acid, the neurotransmitter GABA - the most important element of sleep in terms of pharmacology: it is this that most sleeping pills activate.
When GABA binds to the corresponding receptor in the nerve cell, negatively charged chloride ions enter the cell. Due to this, the cell "slows down". GABA constantly dampens the action of glutamate and other excitatory mediators - for 40% of the cells in our body, so its importance is enormous. This happens not only in sleep, but also when, for example, we need to concentrate: brain neurons release GABA, they inhibit the central nervous system, and we focus on the main thing.
When GABA is not enough to slow down our movements and emotions, anxiety and insomnia appear. Attention deficit disorder (ADHD) is also associated with a lack of GABA, when it is difficult for a child or an adult to sit in one place, and epilepsy, when a single area of the brain is overexcited and initiates an epileptic seizure.