What age group does ptsd affect
What Age Group Shows The Most PTSD? Statistics On Post-Traumatic Stress Disorder
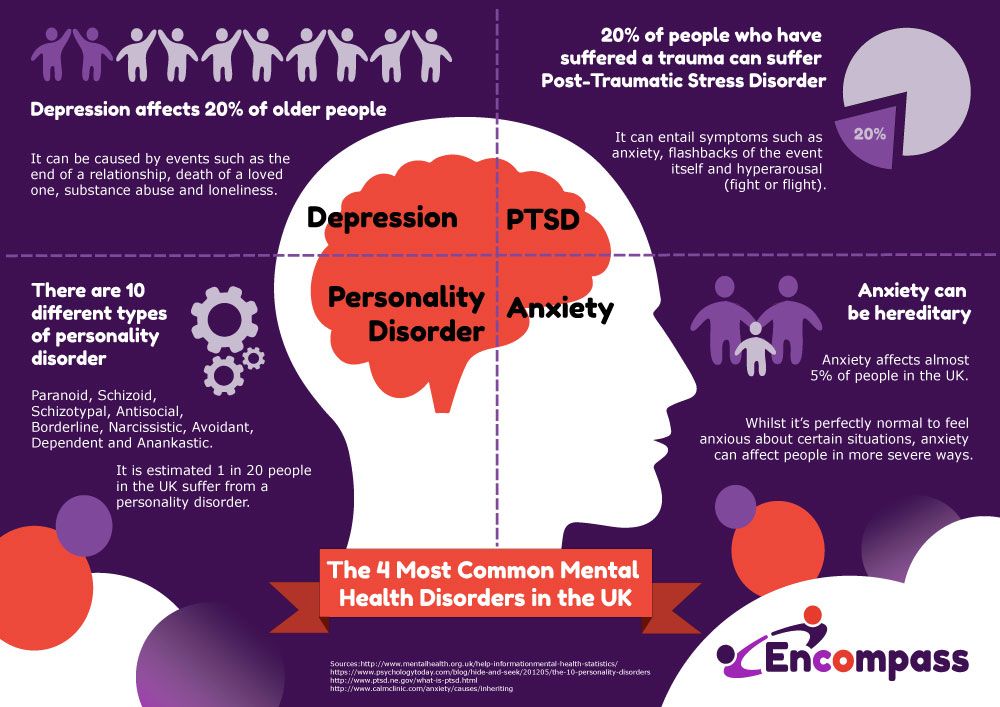
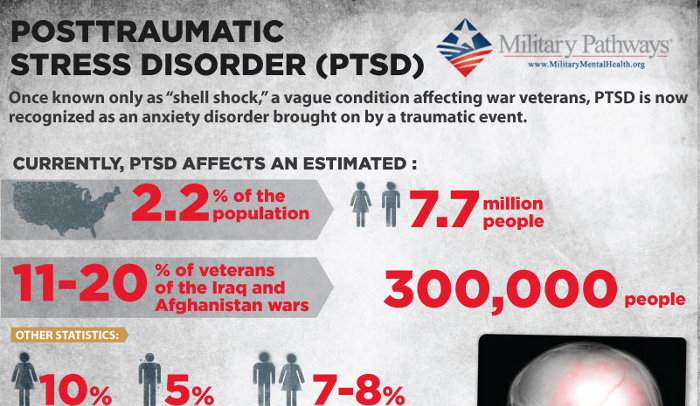
Research indicates that 3.6% of those 18 and older in the United States alone live with post-traumatic stress disorder or PTSD per year. PTSD is considered a common mental health disorder, but there are some misunderstandings about post-traumatic stress disorder and what it is. There are many stereotypes and assumptions made about PTSD. One of the most common assumptions made about PTSD is that it affects adults in the military and does not affect anyone else. This could not be more or false; post-traumatic stress disorder is a disorder that can affect anyone who has experienced a traumatic event, and it affects people of all ages. So, what age group shows the most PTSD? In this article, we will go over the average age of onset for post-traumatic stress disorder and other PTSD statistics.
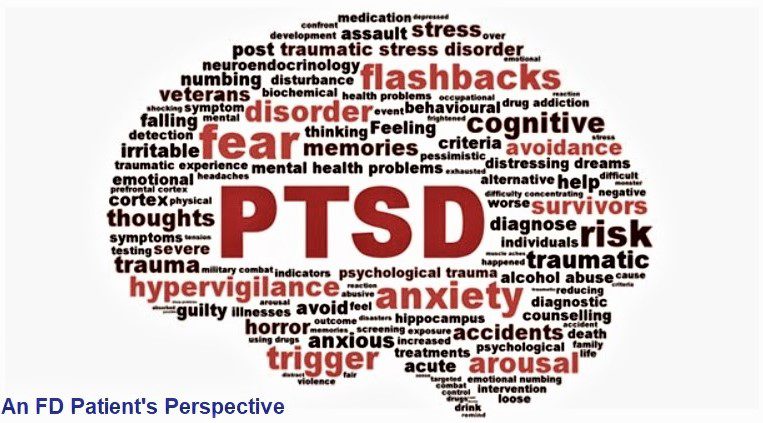
What Is PTSD?
Post-traumatic stress disorder or PTSD is a mental health condition or disorder that can develop after a traumatic event. Not all, or even most, survivors of traumatic events go on to develop post-traumatic stress disorder, but it is a disorder that is born out of trauma in some people
Symptoms or signs of post-traumatic stress disorder include but are not limited to:
- Hypervigilance
- Re-experiencing traumatic events, whether that is through flashbacks, nightmares, or something else
- Irritability or agitation
- Trouble sleeping or insomnia
- Social withdrawal or isolation from others
- Trouble focusing or concentrating
- Difficulty trusting other people
- Emotional detachment
- Feelings of guilt
- Self-destructive behaviors
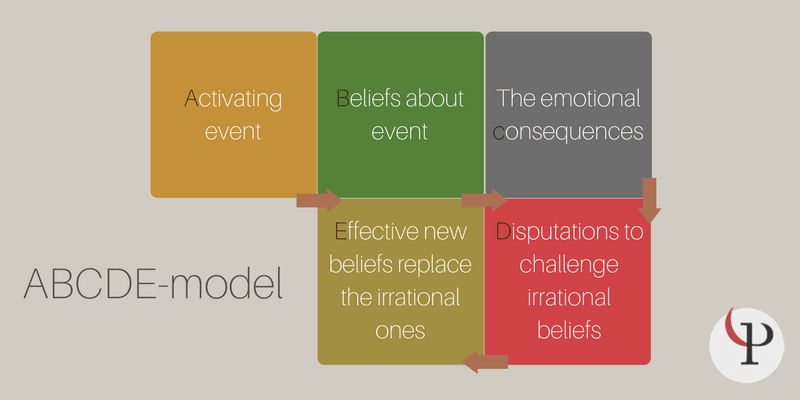
Diagnostically speaking, to be diagnosed with post-traumatic stress disorder, you have to have experienced or witnessed a traumatic event. Symptoms of PTSD must affect your life and ability to function in social relationships or social situations, work, school, self-care, and so on to be diagnosed. It is normal to experience emotional consequences after trauma, but PTSD is more severe, and the impact is long-lasting. The good news is that post-traumatic stress disorder is a treatable condition. There are several studied treatments for post-traumatic stress disorder, including therapies such as cognitive-behavioral therapy or CBT and eye movement desensitization and reprocessing therapy or EMDR. For all information regarding specific treatments and therapies, make sure to speak with a medical or mental health professional who can give you individual medical or mental health advice.
It is normal to experience emotional consequences after trauma, but PTSD is more severe, and the impact is long-lasting. The good news is that post-traumatic stress disorder is a treatable condition. There are several studied treatments for post-traumatic stress disorder, including therapies such as cognitive-behavioral therapy or CBT and eye movement desensitization and reprocessing therapy or EMDR. For all information regarding specific treatments and therapies, make sure to speak with a medical or mental health professional who can give you individual medical or mental health advice.
What Age Group Shows The Most PTSD?
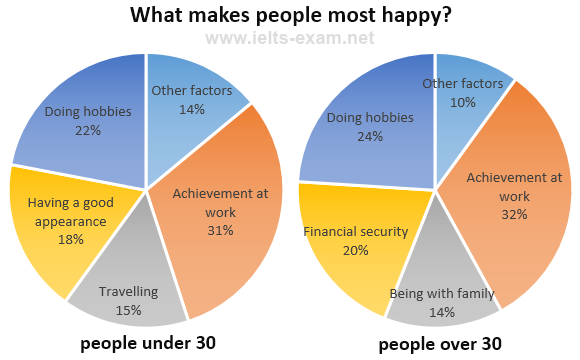
Statistics from the national institute of Mental Health NIMH suggest that individuals aged 45 to 59 have the highest prevalence of post-traumatic stress disorder, followed by those aged 18 to 29. Here are the percentages found in those studies:
- 4% of People ages 18 through 29 have post-traumatic stress disorder.
- 5% of people aged 30 to 44 have post-traumatic stress disorder.

- 3% of those 45 through 59 have post-traumatic stress disorder.
- 1% of those aged 60 or older have post-traumatic stress disorder.
It is important to note that children can also experience PTSD. Symptoms of PTSD and children can differ from those seen in adulthood with post-traumatic stress disorder PTSD. Though some symptoms are the same, children might experience other symptoms, such as reenacting traumatic events through play. Sources say that, out of the children who experience trauma, the development of post-traumatic stress disorder in kids is more likely to occur in girls than in boys. More specifically, 3%-15% of girls and 1-6% of boys develop PTSD after a traumatic event.
Other PTSD Facts and Statistics
Here are some other facts and statistics about post-traumatic stress disorder that might surprise you:
- Again, post-traumatic stress disorder impacts people of different genders disproportionately, in both children and adults—the reason why is unknown.
 Post-traumatic stress disorder is more common in females than in males, though it can affect all genders. More specifically, 5.2% of females experience PTSD, whereas 1.6% of males experience PTSD. That is where the statistic of 3.6% of all individuals is born.
Post-traumatic stress disorder is more common in females than in males, though it can affect all genders. More specifically, 5.2% of females experience PTSD, whereas 1.6% of males experience PTSD. That is where the statistic of 3.6% of all individuals is born. - Many people living with post-traumatic stress disorder have a comorbid mental health condition. Common comorbidities seen in post-traumatic stress disorder include anxiety disorders, substance use disorder, and depressive disorders.
- Before the most recent version of the diagnostic and statistical manual of mental disorders, the DSM-5, PTSD was diagnosed as an anxiety disorder. It is now diagnosed under a new category, which is called "trauma and stressor-related disorders."
- There are many different potential causes of PTSD. These causes include but are not limited to car accidents, illness or injury, sexual assault, natural disasters, domestic violence, witnessing violence, and more.
- According to the National Institute on Mental Health NIMH, 36.
 6% of those living with post-traumatic stress disorder experience serious impairment, while 30.2% experience moderate impairment, and 33.1% experience mild impairment. This statistic is derived from the prevalence of the impact of PTSD over a year, so the current numbers may differ.
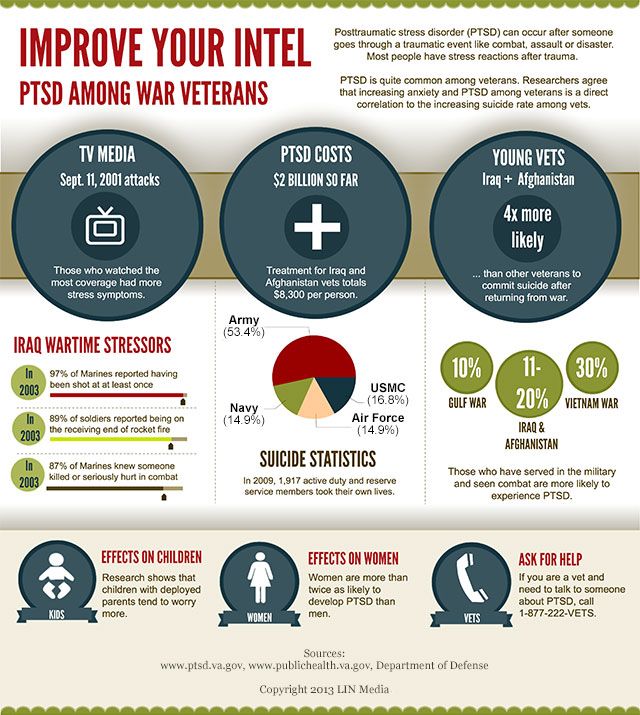
6% of those living with post-traumatic stress disorder experience serious impairment, while 30.2% experience moderate impairment, and 33.1% experience mild impairment. This statistic is derived from the prevalence of the impact of PTSD over a year, so the current numbers may differ. - Roughly, 30%of veterans are said to have post-traumatic stress disorder.
PTSD Support
There are several ways that you can gain support for post-traumatic stress disorder or PTSD. Of course, treatment is the most important thing to pursue if you are experiencing post-traumatic stress disorder symptoms that are affecting your life. Peer support, in conjunction with therapy, can be highly beneficial as well. It is never a replacement for treatment, but peer support does have a special place because it provides individuals living with post-traumatic stress disorder or other mental health disorders with a sense of community and understanding.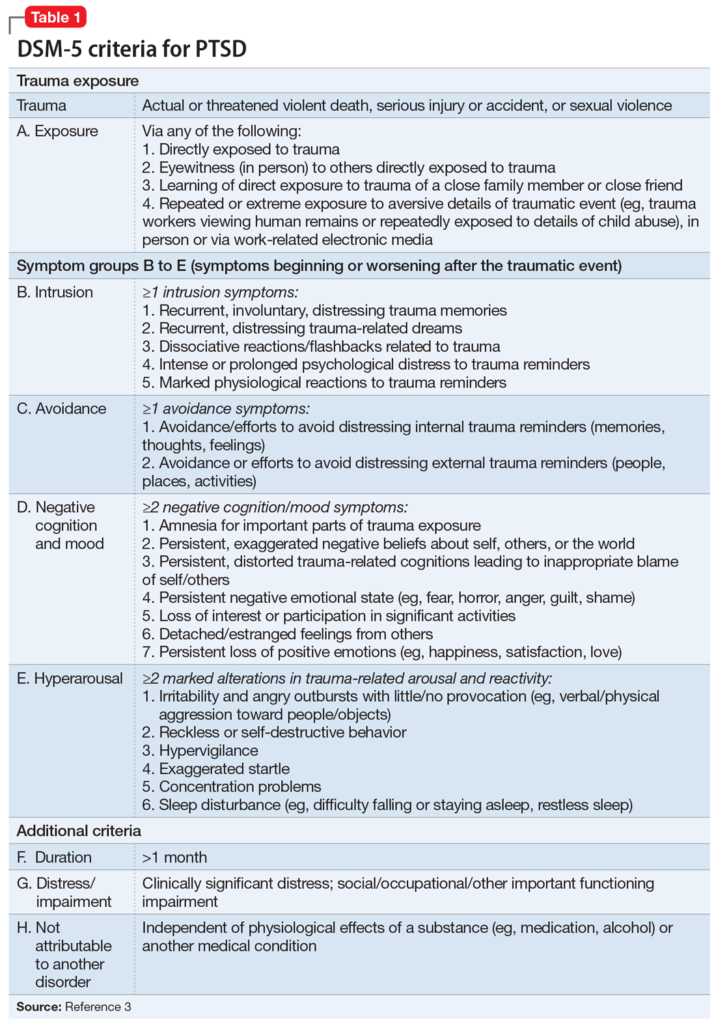
Finding Peer Support
Here are some ways to find peer support for post-traumatic stress disorder:
Visit Post-Traumatic Stress Disorder Forums Online:
There are several support forums online that you can use. Where support groups meet at specific times, forums can often be used anywhere at any time, as long as you have an Internet connection. Here are some active online forums for people living with post-traumatic stress disorder:
My PTSD forum
My PTSD forum is an online forum-based community for those living with post-traumatic stress disorder.
The mentalhealthforum.net Post-Traumatic Stress Disorder Forum
Mentalhealthforum.net is a website with forums for various mental health conditions and concerns, including anxiety disorders, depression, post-traumatic stress disorder, and more.
The Beyond Blue PTSD and Trauma Forum
Beyond Blue is an Australian-based organization. Their website has mental health forums, including one for post-traumatic stress disorder and trauma, among other resources. Click here to go to the Beyond Blue post-traumatic stress disorder forum.
Their website has mental health forums, including one for post-traumatic stress disorder and trauma, among other resources. Click here to go to the Beyond Blue post-traumatic stress disorder forum.
The psychforums.com Post-Traumatic Stress Disorder Forum
Like mentalhealthforum.net, psychforums.com is a website with various forums for many mental health conditions or concerns, including anxiety disorders, obsessive-compulsive disorder (OCD), depressive disorders, post-traumatic stress disorder, and more. Click here to go to the psychforums.com post-traumatic stress disorder forum.
Find a Support group In Your Area
To find a support group near you, you may ask a trauma-informed mental health provider who specializes in trauma or post-traumatic stress disorder for recommendations. Another way to find a support group in your area is to search for "trauma support groups near me" or "PTSD support groups near me" using your search engine of choice. In some cases, you will find support groups for PTSD or trauma surrounding specific sources of trauma. For example, if you have survived a car accident, you may be able to find a group of car accident survivors. The same is true for other traumas, like domestic violence and natural disasters.
In some cases, you will find support groups for PTSD or trauma surrounding specific sources of trauma. For example, if you have survived a car accident, you may be able to find a group of car accident survivors. The same is true for other traumas, like domestic violence and natural disasters.
No matter what route you take, make sure to remember that it is possible to heal from post-traumatic stress disorder. If you are searching for a counselor or therapist in your area, there are several ways that you can go about finding one. You may decide to go to your doctor and ask for a referral to a therapist or counselor. Another option is to search the web for "trauma therapist near me" or "PTSD counselors near me" using your search engine of choice. If you are interested in remote therapy or services, consider using an online therapy company like Better Help.
Take the Mind Diagnostics PTSD Test
Are you wondering if you could have symptoms of post-traumatic stress disorder or PTSD? If so, consider taking the Mind Diagnostics post-traumatic stress disorder test. Although taking the test is not a replacement for a diagnosis from a medical or mental health professional, the Mind Diagnostics post-traumatic stress disorder test can give your insight into your symptoms and what you're going through, and taking the test might just be the first step to getting the help that you need. While PTSD can affect people of all ages, the Mind Diagnostics post-traumatic stress disorder test is for those aged 18 and older.
Although taking the test is not a replacement for a diagnosis from a medical or mental health professional, the Mind Diagnostics post-traumatic stress disorder test can give your insight into your symptoms and what you're going through, and taking the test might just be the first step to getting the help that you need. While PTSD can affect people of all ages, the Mind Diagnostics post-traumatic stress disorder test is for those aged 18 and older.
To take the Mind Diagnostics post-traumatic stress disorder test, click the following link or copy and paste it into your browser: https://www.mind-diagnostics.org/ptsd-test.
Frequently Asked Questions (FAQs)
What are 5 statistics about PTSD?
What percent of the population has PTSD?
Who suffers from PTSD the most?
How much has PTSD increased over the years?
Why is PTSD more common now?
What age group is most affected by PTSD?
Is PTSD a mental illness or disorder?
Is PTSD a disability?
Is PTSD curable?
Why do psychologists believe PTSD is overdiagnosed?
51 PTSD Statistics & Facts: How Common Is PTSD?
Key PTSD Statistics & Facts
- An estimated 70% of adults in the United States have experienced at least one traumatic event in their lifetime.

- Up to 20% of these people go on to develop post-traumatic stress disorder.
- An estimated 5% of Americans – more than 13 million people – have PTSD at any given time.
- Around 8.7% of all adults – 1 in 13 people in the U.S. will develop PTSD at some point in their lifetime.
- Around 3.6% of adults in the U.S. suffer from PTSD in a given year.
- Approximately 1 in 9 women will get PTSD at some point in their lifetime, and women are around twice as likely as men to develop the disorder.
- Surprisingly, 23% of women in the military report being sexually assaulted. And 55% of female veterans and 38% of male veterans experienced sexual harassment while in the military.
- Researchers found the estimated prevalence of PTSD among veterans ranges from 1.09% to 34.84%.
- Post-traumatic stress disorder (PTSD) can occur after any traumatic event, not only trauma from wartime.
- 16% of emergency physicians meet diagnostic criteria of PTSD.
- Around 5% of adolescents experience PTSD.
PTSD Prevalence: How Common Is PTSD?
| Statistic | Data |
| % Of Americans Who’ve Experienced At Least One Traumatic Event | 70% |
| % Of Americans Who Have PTSD | 5% |
| % Of American Adults Who Have PTSD | 5% (More Than 13 Million) |
| % Of Americans Who Experience Trauma That Will Develop PTSD | 20% |
| % Of PTSD Cases That Are Severe | 36.6% |
| % Of PTSD Cases That Are Moderate | 33.1% |
| % Of PTSD Cases That Are Mild | 30.2% |
| % Of Women Who Will Get PTSD | 11% (1 in 9) |
| % Of Women Who Get Sexually Assaulted In The Military | 23% |
| % Of Male Veterans Who Experienced Sexual Harassment | 38% |
| PTSD Prevalence In 45- to 59-Year-Olds | 5.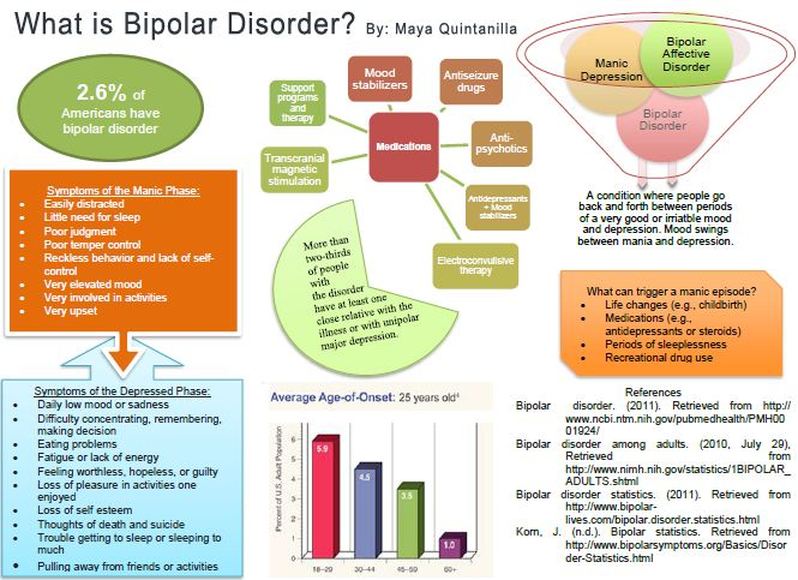 3% 3% |
| PTSD Prevalence In Female Adolescents Aged 13 to 18 | 8% |
| PTSD Prevalence In Adults Aged 60 Or Older | 1% |
| PTSD Prevalence In Blacks | 8.7% |
| PTSD Prevalence In Hispanics | 7.0% |
| PTSD Prevalence In Whites | 7.4% |
| PTSD Prevalence In Asians | 4.0% |
Prevalence Of PTSD By Country
Source: Therecoveryvillage.comU.S PTSD Statistics
- Around 70% of adults in the United States have experienced at least one traumatic event in their lifetime.
- Up to 20% of these people go on to develop post-traumatic stress disorder.
- Approximately 5% of Americans – more than 13 million people – have PTSD at any given time.
- Approximately 8.7% of all adults – 1 in 13 people in the U.S. will develop PTSD at some point in their lifetime.
- Approximately 3.6% of adults in the U.S. suffer from PTSD in a given year.
- Of people in the U.S. who experience a traumatic event, 1 in 5 of them will develop the condition.
- 36.6% of PTSD cases are severe, 33.1% are moderate, and 30.2% are mild according to a study by Harvard Medical School in 2007.
Canada PTSD Statistics
- Canada has the highest rates of PTSD of 24 countries that were studied by the British Journal of Psychiatry in 2016.
- 9% of Canadians will suffer from PTSD in their lifetime.
PTSD Statistics By Gender
- Around 1 in 9 women will get PTSD at some point in their lifetime.
- Women are around twice as likely as men to develop the disorder.
- Surprisingly, 23% of women in the military report being sexually assaulted.
- 55% of female veterans and 38% of male veterans experienced sexual harassment while in the military.
PTSD Statistics By Age
- PTSD in adults was highest in 45- to 59-year-olds (5.3%) as of 2001-2003.
- PTSD in adolescents was highest in female adolescents aged 13 to 18 (8%) as of 2001-2004.
- PTSD prevalence was lowest in adults aged 60 or older (1%) as of 2001-2003.
PTSD Statistics By Race
- A study found that the lifetime prevalence of PTSD was highest among Blacks (8.7%), intermediate among Hispanics and Whites (7.0% and 7.4%) and lowest among Asians (4.0%).
PTSD Statistics By Trauma
Post-traumatic stress disorder is rooted in traumatic events, so we’ve compiled the latest data which illustrates the percentage of people who will likely develop the disorder after experiencing these traumatic events:
| Trauma | % Of People Who Will Likely Develop PTSD |
| Sexual assault | 49% |
| Severe physical assault | 32% |
| Serious accidents | 16.8% |
| Shoot and stabbing victims | 15.4% |
| The unexpected death of a loved one | 14. 3% 3% |
| Parents of children with life-threatening illnesses | 10.4% |
| Witnesses of violence | 7.3% |
| Natural disaster victims | 3.8% |
PTSD In Adults
In the past year, PTSD affected around 3.6% of American adults over the age of 18 according to studies. The symptoms of PTSD in adults are grouped as serious, moderate or mild, and there are approximately 36.6% of adults who experience serious impairment, 33.1% of adults who experience a moderate impairment, and 30.2% of adults who experience mild impairment. All age groups can be affected even though most statistics focus on PTSD in adults.
Source: Cohen Veterans BioscienceIt’s possible for the disorder to occur in children, though sometimes childhood trauma doesn’t result in the disorder until after the brain has more time to develop in the individual’s early adulthood.
PTSD Among Adolescents
Around 5% of adolescents experience PTSD. Studies on PTSD in teenagers have found that just 1.5% experience severe impairment. Unsurprisingly, PTSD in adolescents is more than twice as prevalent in the later teen years, as the prevalence of PTSD for teens aged 13-4 is 3.7%. In the 17-18 age group, the PTSD prevalence increases to 7%.
Studies on PTSD in teenagers have found that just 1.5% experience severe impairment. Unsurprisingly, PTSD in adolescents is more than twice as prevalent in the later teen years, as the prevalence of PTSD for teens aged 13-4 is 3.7%. In the 17-18 age group, the PTSD prevalence increases to 7%.
PTSD & Domestic Violence
The connection between PTSD and domestic violence is clear even if PTSD might not always develop immediately following abuse. There are several factors which influence the probability of domestic violence victims developing post traumatic stress disorder, including the severity and duration of violence, and the age of the victim.
Whether or not someone feels their life is in danger can also influence the chance of PTSD developing in the victim. The intense emotional connection victims might have with the abuser is probably a big part of what makes the violence such a traumatic experience for the victim.
Veteran PTSD Statistics
Many researchers have worked to understand the prevalence of PTSD among military veterans. The result of their efforts are statistics that we’ve compiled. Estimates of prevalence in veterans vary widely because the field of psychiatry has defined and assessed PTSD in multiple ways over time.
The result of their efforts are statistics that we’ve compiled. Estimates of prevalence in veterans vary widely because the field of psychiatry has defined and assessed PTSD in multiple ways over time.
In one recent analysis of 32 scientific scientific articles, researchers found the estimated prevalence of PTSD among veterans ranges from 1.09% to 34.84%.
A 2017 study involving 5,826 U.S. veterans showed that 12.9% were diagnosed with PTSD. This is a shockingly high prevalence rate compared to the prevalence of PTSD among the general population: only 8.7% of the U.S. population will experience PTSD in their lives. And around 3.6% of adults in the U.S. suffer from PTSD in a given year.
Source: Hill & Ponton Disability AttorneysAnd in a 2014 study involving 3,157 U.S. veterans, 87% reported exposure to at least one potentially traumatic event in their lifetime. Veterans reported 3. 4 potentially traumatic events during their lifetime, on average.
4 potentially traumatic events during their lifetime, on average.
Surprisingly, nearly 1 in 4 women in the military report being sexually assaulted. And 55% of female veterans and 38% of male veterans experienced sexual harassment while in the military.
Source: Hill & Ponton Disability Attorneys- Around 30% of Vietnam veterans have had PTSD in their lifetime. (according to American Psychological Association in 1990)
- Approximately 354 million adult war survivors globally have PTSD and/or major depression. (according to European Journal of Psychotraumatology in 2019)
- PTSD prevalence of around 14% was present in veterans who served in Iraq in one study of 1,938 veterans. (according to U.S. Department of Veterans Affairs)
- A 10% prevalence of PTSD has been extrapolated for all Gulf War veterans in a 2003 report by American Journal of Epidemiology.
PTSD Symptoms
PTSD symptoms may include unwanted memories of the trauma, avoidance of situations that bring back memories of the trauma, nightmares, anxiety, depressed mood, or heightened reactions.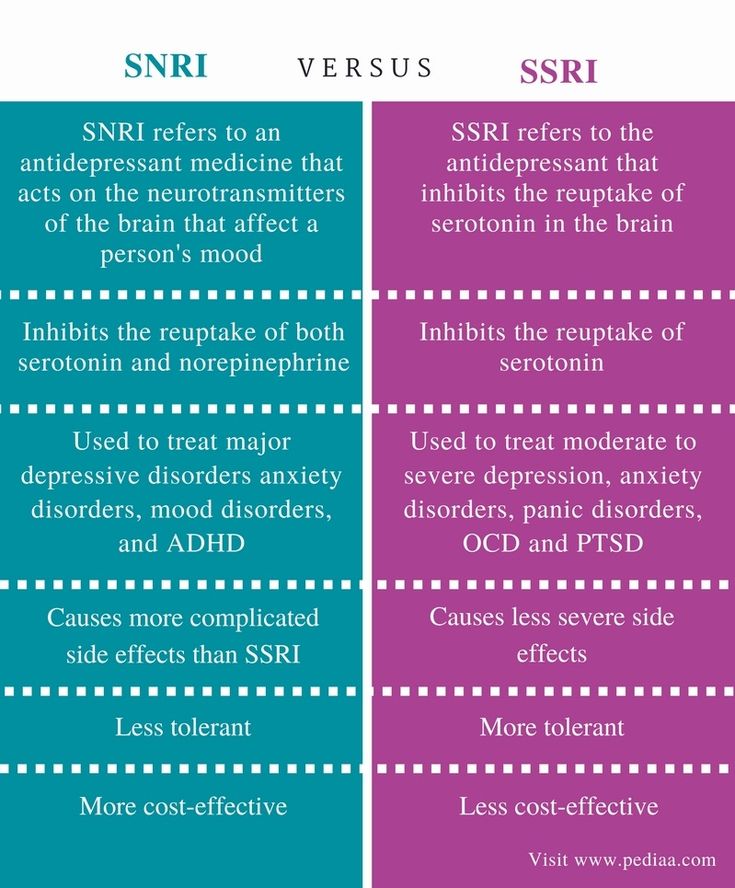
People may experience these symptoms:
- Intrusion of thoughts, flashbacks, memories, and dreams
- Avoidance of reminders of traumatic events
- Alterations in mood and cognition
- Alterations in reactivity and arousal
- Insomnia or nightmares
- Emotional detachment or unwanted thoughts
- Self-destructive behavior, social isolation, irritability, agitation
- Loss of interest in activities, loneliness, or guilt
PTSD & Co-Occurring Conditions
It’s possible for many mental health disorders to co-occur with PTSD in part, to the significant changes in brain functioning following trauma that leads to the disorder. The most common conditions someone with PTSD may experience include:
- Depression
- Suicidal thoughts
- Trauma
- Anxiety
- Substance use disorders
We’ll go into more detail on each condition in this section.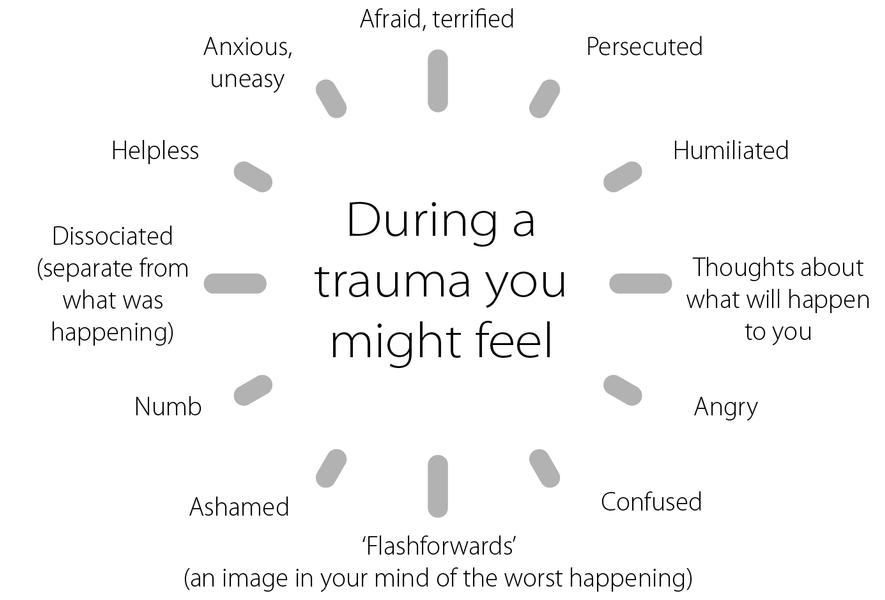
PTSD & Depression
Approximately 1 in 10 people have some form of depressive disorder every year, making it a common mental health condition. It’s more common among people who’ve experienced traumatic experiences.
As mentioned earlier, PTSD and depression frequently co-occur. Specifically, people with PTSD are 3-5 times more likely to have depression.
PTSD & Suicide
In general, people diagnosed with PTSD who struggle to express their emotions have a higher risk of suicide. Other common co-occurring conditions such as depression or anxiety can make a negative impact on the chances of suicide for someone with the disorder.
PTSD & Trauma
Disruptions and changes in brain chemistry caused by an individuals’ trauma is the main reason why PTSD and trauma are interconnected. The condition can occur in response to traumas besides military combat (example: sexual abuse).
However, there are other traumatic events which can happen in a person’s life that might lead to the disorder:
- 49% of rape victims will develop PTSD.

- Almost 32% of physical assault victims will develop PTSD.
- 16.8% of people involved in serious vehicle accidents develop PTSD.
- 15.4% of shooting and stabbing victims develop PTSD.
- 14.3% of people who unexpectedly and suddenly experience the death of a close loved one develop PTSD.
- 7.3% of people who’ve witnessed the murder or serious injury of another person will develop PTSD.
- 3.8% of people who experience natural disasters develop PTSD.
PTSD & Anxiety
Currently, PTSD is considered a separate type of disorder, but in the past it was categorized as an anxiety disorder because PTSD and anxiety disorders share some symptoms, many of which can impair sleep and other biological functions. For example, someone with anxiety related to PTSD can frequently feel on edge and be easily startled.
Similarly, anxiety caused by the disorder can make it challenging for an individual to concentrate, and it can also increase their agitation.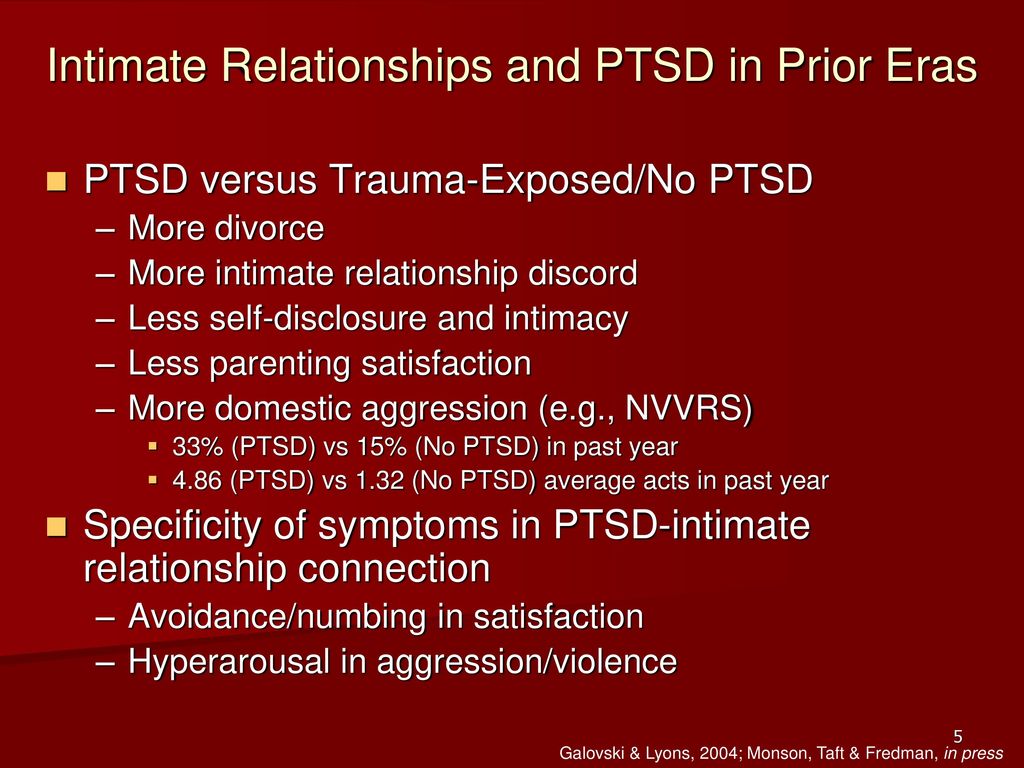
PTSD & Substance Abuse
One study estimates that 46.4% of people diagnosed with the disorder also meet the criteria for a substance use disorder. Another study found that women with the disorder were 2.48 times more likely to suffer from alcohol abuse, while men with the disorder were 2.06 times more likely.
PTSD Treatment Statistics
Medication, psychotherapy, or a combination of both can treat PTSD. Even though there’s more than one type of psychotherapy used to treat the disorder, trauma-focused psychotherapies with a mental healthcare professional are the most recommended.
That’s primarily because this type of treatment assists people to process their experiences by helping them focus on the memory of the traumatic event or the meaning behind it.
In fact, studies have demonstrated that up to 46% of people diagnosed with the disorder show improvement within the first six weeks of psychotherapy.
Another treatment option that can alleviate the symptoms of PTSD, including anxiety, are antidepressants. Interestingly, studies show up to 62% of people who receive medication for PTSD show improvement. (American Family Physician, 2003)
Interestingly, studies show up to 62% of people who receive medication for PTSD show improvement. (American Family Physician, 2003)
First Responder PTSD Statistics
If you’re wondering how common is PTSD among first responders, this section will show you the up-to-date stats.
Surprisingly, more than 80% of first responders experience traumatic events on the job. The challenging and dangerous situations they face cause them to be at a high risk of developing PTSD as a work-related injury or condition.
In fact, according to the Substance Abuse and Mental Health Services Administration, an estimated 30% of first responders develop behavioral health conditions including, but not limited to, depression and PTSD, as compared with 20% in the general population.
9/11 PTSD Statistics
More than 21% of residents enrolled in the WTC Health Registry reported new PTSD symptoms 5 to 6 years after the tragic day. PTSD among residents increased from more than 13% 2-3 years after the attacks to more than 16% 5-6 years later. The main risk factors associated with 9/11 were:
The main risk factors associated with 9/11 were:
- Intense dust cloud exposure
- Returning to a home with a heavy layer of dust
- Witnessing horror
- Job loss
- Lack of social support
Firefighter PTSD Statistics
Studies have shown that anywhere between around 7% and 37% of firefighters meet the criteria for a current PTSD diagnosis.
World War 2 PTSD Prevalence
Among individuals who had previously sought psychiatric treatment, 37% of the World War 2 veterans and 80% of the Korean War veterans had current PTSD. It was found that 54% of a group of psychiatric patients who had been in combat during World War 2 met criteria for PTSD. At the time, the prevalence for PTSD was 27%.
Frequently Asked Questions
What is PTSD?
PTSD stands for post-traumatic stress disorder, and the disorder develops in some who have experienced a dangerous or shocking event and have a challenging time recovering from the trauma the incident caused.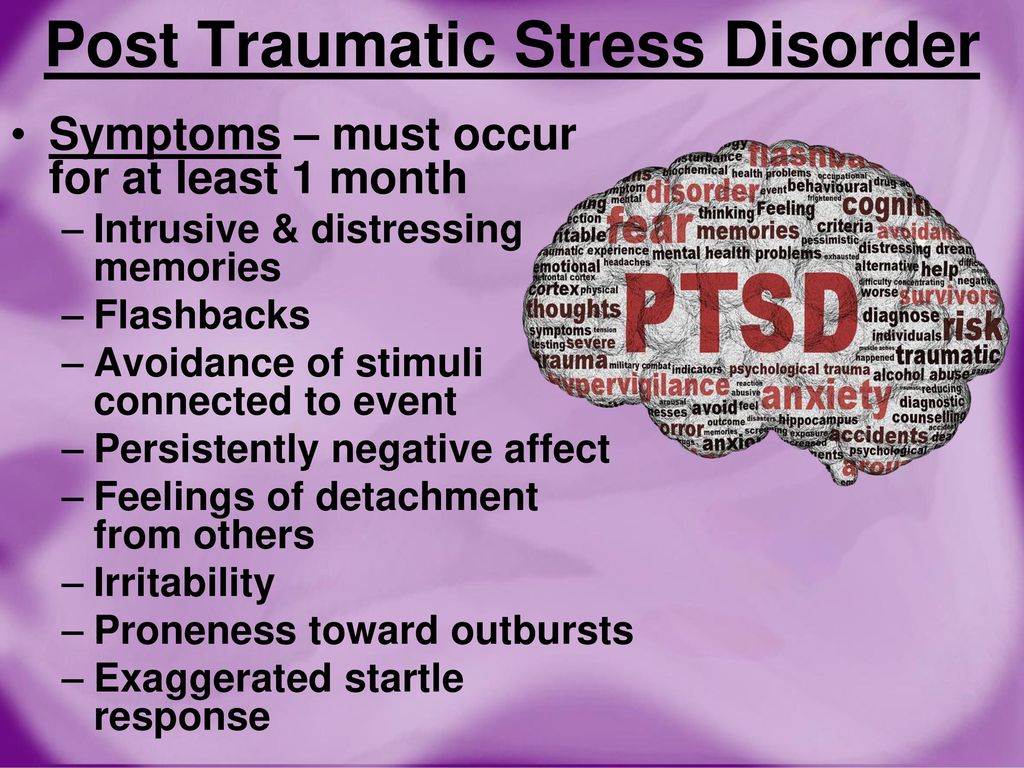
Life-threatening events are common risk factors for PTSD. For example, military personnel who have experienced violence, people who have lived through natural disasters, victims of sexual abuse, and those who were involved in a car accident have an unfortunate high chance for developing the disorder.
What does PTSD do to a person?
People diagnosed with PTSD have disturbing, intense thoughts and feelings related to their experience that can last long after the traumatic event occurred. They may even relive the event through nightmares or flashbacks, they may feel sadness or even depression, anger, fear, and they may feel detached from others.
What are 3 things that can lead to PTSD?
Here are the most common events that can lead to PTSD:
- Physical or sexual assault
- Serious accidents
- Abuse, including childhood or domestic abuse
How long does PTSD last for?
Some people with PTSD recover within just 6 months, while others have symptoms that can last much longer.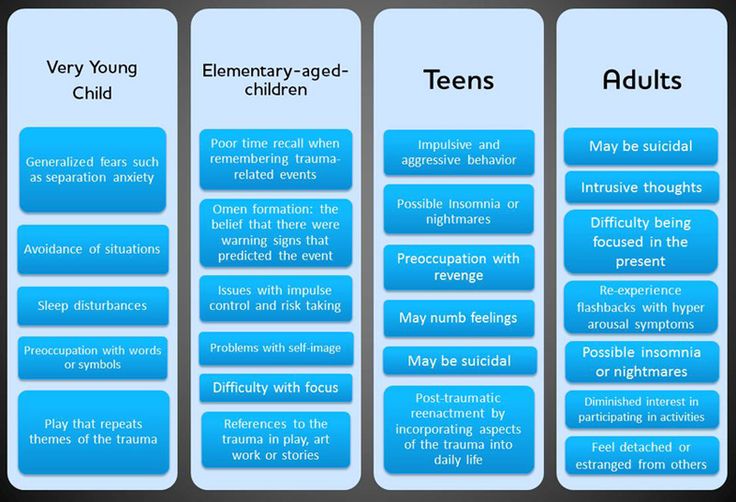 In some people, the condition becomes chronic and can result in depression and anxiety. A doctor, such as a psychologist or psychiatrist, who has experience helping people with mental illnesses can diagnose PTSD.
In some people, the condition becomes chronic and can result in depression and anxiety. A doctor, such as a psychologist or psychiatrist, who has experience helping people with mental illnesses can diagnose PTSD.
Is PTSD a cause of death?
Post-traumatic stress disorder more than doubles a veteran’s risk of death from any cause. It’s also an independent risk factor for cardiovascular disease, according to research presented in 2010 at the American Heart Association’s Scientific Sessions.
Can PTSD change your personality?
Yes, a study published by the National Library of Medicine concluded that PTSD is a risk of development enduring personality changes with serious individual and social consequences.
Can PTSD be cured?
As with the majority of mental illnesses, no cure exists for PTSD. However, it’s possible to effectively manage the symptoms to help the affected individual restore themself to normal functioning. A combination of therapy and medication is the best hope for treating the disorder.
Does PTSD affect memory?
If you have PTSD, you might notice that it’s challenging for you to concentrate or that you have memory issues such as memory loss. In fact, memory and concentration problems are common symptoms of PTSD.
Can PTSD last a lifetime?
As with the majority of mental illnesses, PTSD is very personal and no two cases are the same. In fact, according to Dr. Kriegeskotten, “When PTSD is not treated, it can last a very long time, perhaps a lifetime.”
PTSD Research & Sources
- Post-traumatic stress disorder
- National Center for PTSD
- Post-traumatic stress disorder
- Diagnosis and management of post-traumatic stress disorder
- Epidemiology of PTSD
- PTSD and Veterans: Exploring The Statistics
- Post Traumatic Stress
Post-traumatic stress disorder in young children
Alexandra De Young, PhD, Justin Kenardi, PhD
National Research Center for Disorders and Rehabilitation, Faculty of Medicine, University of Queensland, Australia
(English).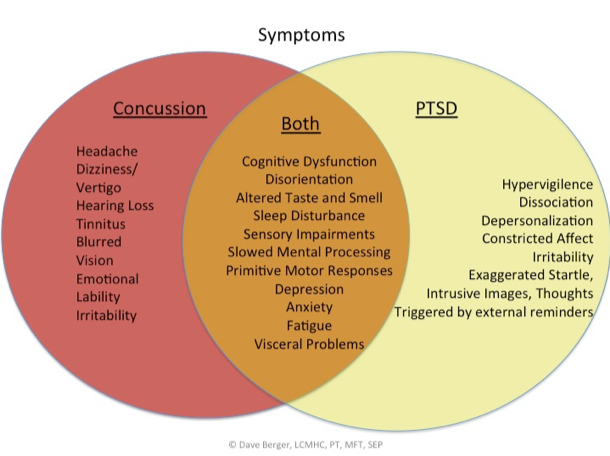 Translation: June 2015 nine0008 PDF document
Translation: June 2015 nine0008 PDF document
Introduction
Post-traumatic stress disorder (PTSD) is one of the most severe and debilitating disorders associated with trauma. According to research, young children, as well as older children and adolescents, commonly exhibit three of the traditional symptoms of PTSD: re-experiencing the event (through nightmares or acting out traumatic events), seeking to avoid being reminded of the event, and psychological overexcitation (for example, , irritability, sleep disturbance, unmotivated shivering). nine0014 1 However, research suggests that the PTSD features listed in The Diagnostic and Statistical Manual of Mental Disorders 2 do not adequately reflect the specificity of onset of symptoms in infants and preschool children. The Guidelines also underestimate the number of children experiencing post-traumatic stress and subsequent deterioration in health. nine0014 3 Accordingly, new research is encouraging the inclusion of a subtype of PTSD occurring in preschool children in the 5th edition of the Diagnostic and Statistical Manual. 4.5
nine0014 3 Accordingly, new research is encouraging the inclusion of a subtype of PTSD occurring in preschool children in the 5th edition of the Diagnostic and Statistical Manual. 4.5
Frequency, course and consequences of reactions to trauma months after the traffic accident (RTA) 6 or burn injuries 7 ; in 14.3–25% of cases, within two months after receiving various types of injuries (for example, burns, bullet wounds, road accidents, injuries during sports or during the game), 8.9 in 10% of cases, within six months after an accident or burn injuries 6.8 and in 13.2% of cases - within 15 months on average after burn injuries.10 Signs of age-specific PTSD appear in 26-60% 1,3,11 cases as a result of physical or sexual abuse. Our study has shown that young children develop depression, separation anxiety disorder, oppositional defiant disorder (ODD), and specific phobias due to burn injuries, 8 , and that these disorders are highly co-morbid symptoms of PTSD.
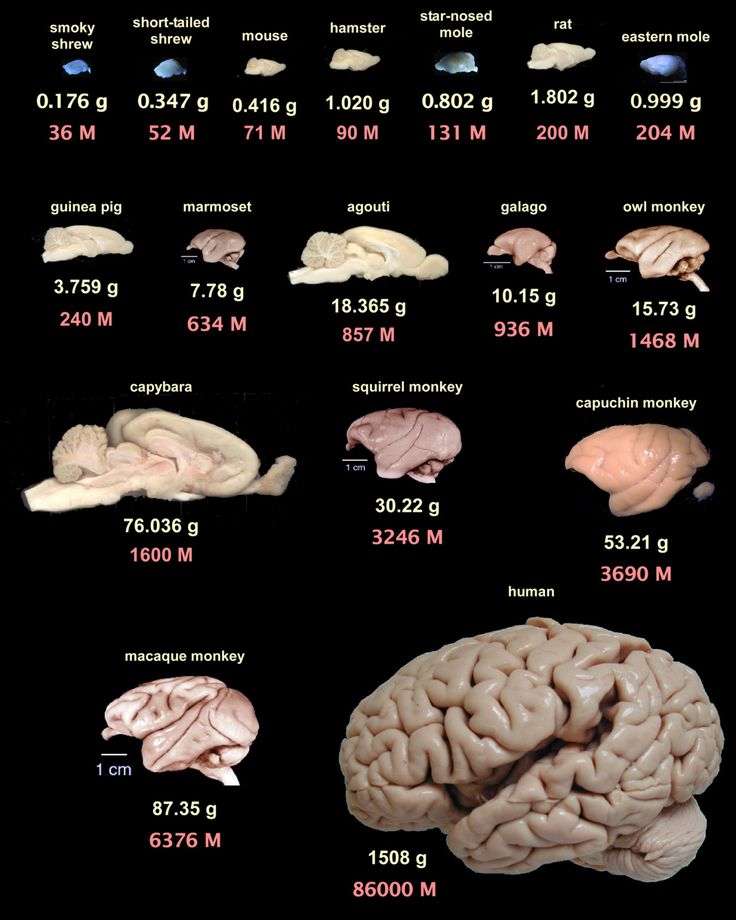
Studies in children of all ages have shown that, if left untreated, PTSD can develop into a chronic, debilitating form. nine0014 8,12,13 The results of this study are troubling given the fact that neurophysiological systems in young children, including stress modulation and emotion regulation, are still in rapid development. 14 In addition, childhood trauma is associated with permanent structural 15 and functional 16 brain damage, as well as with the onset of psychiatric disorders, 17 health risk behavior and related physical health status in adults. 18 Thus, trauma in early childhood can have much more severe consequences on the developmental trajectory than trauma sustained later in development.
The role of parents
When working with children, it is very important to realize that the trauma itself and the child's reaction to it is a serious test for parents, which can also become a source of chronic stress. Research has shown that approximately 25% of parents experience clinically elevated levels of acute stress, PTSD, anxiety, depression, and stress within the first six months of a child's trauma. nine0014 19-21 Although most parents remain relatively resilient and their stress levels return to clinical normal over time, parental distress during the acute stress stage contributes to the development and persistence of traumatic symptoms in affected children. 19,20,22
Research has shown that approximately 25% of parents experience clinically elevated levels of acute stress, PTSD, anxiety, depression, and stress within the first six months of a child's trauma. nine0014 19-21 Although most parents remain relatively resilient and their stress levels return to clinical normal over time, parental distress during the acute stress stage contributes to the development and persistence of traumatic symptoms in affected children. 19,20,22
It is generally accepted that the quality of the attachment of children and parents to each other, the mental health of parents and their parenting actions are key factors influencing a child's recovery from trauma. nine0014 14,23,24 For young children, relationships with parents are especially important because children do not have sufficient adaptive capacity to regulate strong emotions on their own. Thus, they depend on a sensitive and emotionally open educator who can help them regulate their emotional response in times of distress.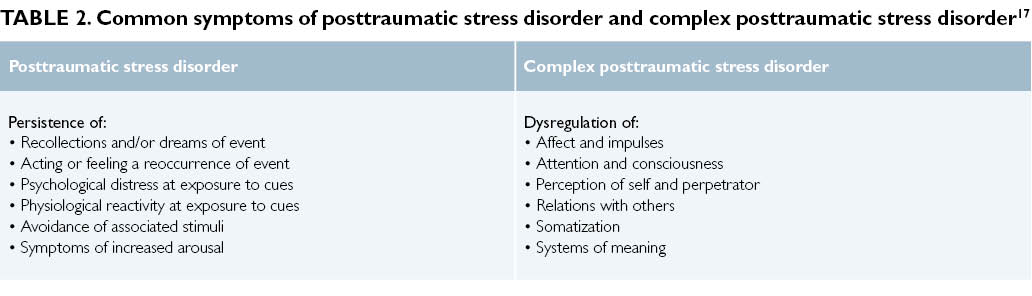 14.23 In addition, young children especially rely on their parents' emotions to understand how to interpret or respond to an event. In the future, children can imitate their parents' reaction to fear and their inadequate adaptive reactions. nine0014 25 Parents can also directly influence the child's contact with the trauma memories (for example, avoiding discussion of what happened) and thus hinder the child's adaptation to the event. 25
14.23 In addition, young children especially rely on their parents' emotions to understand how to interpret or respond to an event. In the future, children can imitate their parents' reaction to fear and their inadequate adaptive reactions. nine0014 25 Parents can also directly influence the child's contact with the trauma memories (for example, avoiding discussion of what happened) and thus hinder the child's adaptation to the event. 25
The influence of adverse psychological reactions on the relationship between children and parents, the development of traumatic symptoms in the child, combined with the mental suffering of parents, are important arguments for paying more attention to the needs of parents in order to reduce their level of experience and stimulate their ability to support children in difficult times. Adequate measures aimed at alleviating the mental illness of the child and parents, as well as improving relations between them, will have a beneficial effect on the process of inhibiting the development of post-traumatic reactions in parents and children.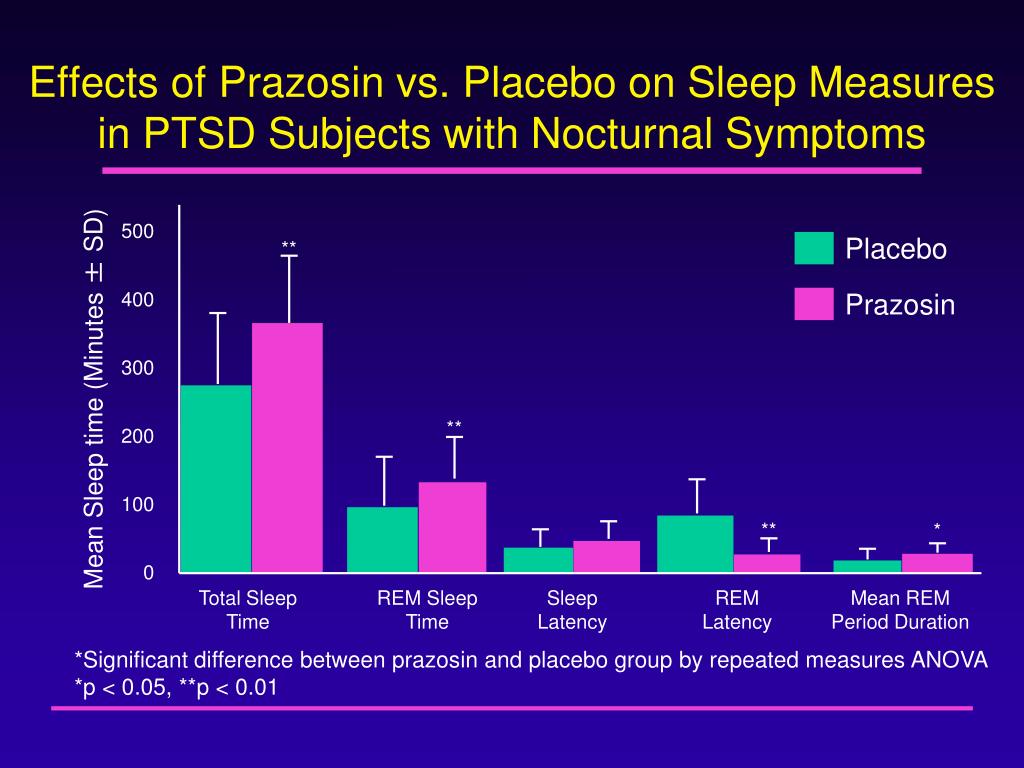 However, there is only preliminary evidence to support these types of interventions during an exacerbation, and more research is needed on this issue. nine0008
However, there is only preliminary evidence to support these types of interventions during an exacerbation, and more research is needed on this issue. nine0008
Early prevention and correction measures
Unfortunately, most children and their parents who experience psychological difficulties after trauma are not diagnosed with characteristic symptoms, as a result of which both children and parents do not receive adequate support. Taking into account the prevalence of injuries, as well as the fact that early childhood is a sensitive period of brain development, it is necessary to introduce effective measures that can reduce the risk of developing chronic post-traumatic stress reactions in children and parents. It is advisable to take such measures in an environment with an increased risk of stress reactions, for example, in a medical institution. This solution would reduce the risk of traumatic stress reactions or even prevent them by conducting an examination and implementing a program of preventive measures. nine0014 26 Early detection of severe symptoms and appropriate action in families at risk will help prevent problems from occurring and entrenching, or at least minimize the impact of these problems on the child, family and society. However, the primary task is to learn to distinguish between categories of patients experiencing a short-term mental disorder and those at risk of developing chronic PTSD, 13 without creating additional overload for filled medical institutions. Psychometrically verified examination methods for very young children do not exist, which is a significant shortcoming in this area. nine0008
nine0014 26 Early detection of severe symptoms and appropriate action in families at risk will help prevent problems from occurring and entrenching, or at least minimize the impact of these problems on the child, family and society. However, the primary task is to learn to distinguish between categories of patients experiencing a short-term mental disorder and those at risk of developing chronic PTSD, 13 without creating additional overload for filled medical institutions. Psychometrically verified examination methods for very young children do not exist, which is a significant shortcoming in this area. nine0008
To date, most research has focused on the treatment of chronic PTSD rather than early prevention of its symptoms. Both in children's and adult literature, there is no data on which categories of patients need preventive measures at an early stage, what duration and content these measures should have. 27 To date, systematic reviews suggest that continuous cognitive-behavioral trauma therapy (CBT) is most effective when administered within the first three months after the event.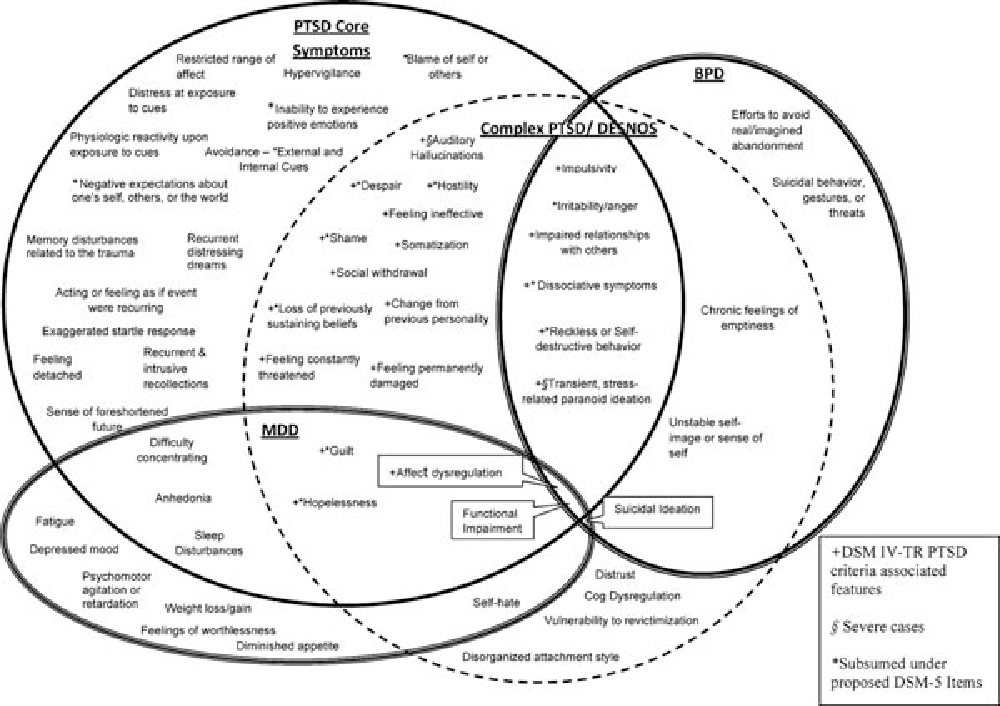 nine0014 27
nine0014 27
Research involving children suggests that preventive action based on incident information up to two weeks after an injury can reduce anxiety symptoms in children at 1 28 and 6 months after the event developments. 29 In addition, Landolt et al received a positive response to a single session of preventive therapy aimed at managing symptoms of depression and behavioral problems in a group of preteens (7-11 years old) affected by road traffic accidents. nine0014 30 Berkowitz and colleagues 31 created the only individualized prevention program (4 sessions for a child with a parent/guardian, including diagnostics, psychological self-help training and coping skills) for children 7-17 years old. The program has shown its effectiveness in reducing the manifestations of PTSD and various post-traumatic symptoms.
However, there are no published studies on the effectiveness of preventive post-traumatic psychological interventions for young children (under six years of age). However, Scheering's research has shown that 12 sessions of cognitive-behavioral therapy, built in accordance with a special plan for PTSD, conducted with children aged 3-6 years who experienced a variety of traumatic events, showed their appropriateness and effectiveness in reducing existing post-traumatic stress symptoms. nine0014 32
However, Scheering's research has shown that 12 sessions of cognitive-behavioral therapy, built in accordance with a special plan for PTSD, conducted with children aged 3-6 years who experienced a variety of traumatic events, showed their appropriateness and effectiveness in reducing existing post-traumatic stress symptoms. nine0014 32
Few studies look at the preventive therapy component for adults to prevent post-trauma disorders in children. Kenardy et al found that psychological self-help training provided to parents within 72 hours of an accident was effective in reducing parental post-traumatic symptoms up to 6 months after the accident. 28 Melnyk et al. 33 examined the effectiveness of a prevention program in parents of children aged 2-7 years under close pediatric supervision. The researchers found that parents in the prevention group had markedly reduced levels of stress, depression, and PTSD symptoms, and their children experienced fewer internalizing and externalizing behavioral problems after discharge. nine0008
nine0008
Evidence-based recommendations for the prevention of PTSD in young children require research. However, Landolt et al., based on the results of a recent meta-analysis, argue that early preventive measures help identify children at risk. These activities include several sessions of training in psychological self-help, individual adaptation skills, involvement of parents in the process and familiarization with various forms of traumatic phenomena. nine0014 34
Advice for parents, services and policy
The phenomenon of post-traumatic stress disorder in young children has received little attention so far. Health care providers should monitor children more closely for signs of post-traumatic stress disorder. This may require training and retraining of staff. Mass standardized screening is ideal, but diagnosing groups of children at risk may be more cost-effective. In addition, any screening program must be integrated with a clinical setting that provides opportunities for appropriate care. Parental distress is a significant factor influencing post-traumatic reactions in children. However, in medical institutions this criterion is given insufficient attention. The reason for this may be the fact that the distress of the parents against the background of the child's injury may not reach the level of clinical diagnosis, or the fact that it is customary to pay more attention to the needs of the child than the family as a whole. nine0014 22 Caregivers should pay more attention to the fact that the consequences of trauma can have a more serious impact on the family system as a whole.
Parental distress is a significant factor influencing post-traumatic reactions in children. However, in medical institutions this criterion is given insufficient attention. The reason for this may be the fact that the distress of the parents against the background of the child's injury may not reach the level of clinical diagnosis, or the fact that it is customary to pay more attention to the needs of the child than the family as a whole. nine0014 22 Caregivers should pay more attention to the fact that the consequences of trauma can have a more serious impact on the family system as a whole.
Literature
- Scheeringa, M., et al., New findings on alternative criteria for PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry , 2003. 42(5): p. 561-570.
- American Psychiatric Association, Diagnostic and statistical manual of mental disorders, (4th edition, Text Revision). nine0025 2000, Washington, DC: Author.
- Scheeringa, M.S., et al., Two approaches to the diagnosis of posttraumatic stress disorder in infancy and early childhood. Journal of the American Academy of Child and Adolescent Psychiatry , 1995. 34(2): p. 191-200.
- Scheeringa, M.S., C.H. Zeanah, and J.A. Cohen, PTSD in Children and Adolescents: Toward an Empirically Based Algorithm. Depression and Anxiety , 2011. 28(9): p. 770-782.
- De Young, A.C., J.A. Kenardy, and V.E. Cobham, Diagnosis of Posttraumatic Stress Disorder in Preschool Children. nine0024 Journal of Clinical Child and Adolescent Psychology , 2011. 40(3): p. 375-384.
- Meiser-Stedman, R., et al., The posttraumatic stress disorder diagnosis in preschool- and elementary school-age children exposed to motor vehicle accidents. American Journal of Psychiatry , 2008. 165(10): p. 1326-1337.
- Stoddard, F.J., et al., Acute stress symptoms in young children with burns. Journal of the American Academy of Child and Adolescent Psychiatry , 2006.
 45(1): p. 87-93.
45(1): p. 87-93. - De Young, A.C., et al., Prevalence, comorbidity and course of trauma reactions in young burn-injured children. Journal of Child Psychology and Psychiatry , 2012. 53(1): p. 56-63.
- Scheeringa, M.S., et al., Factors affecting the diagnosis and prediction of PTSD symptomatology in children and adolescents. American Journal of Psychiatry , 2006. 163(4): p. 644-651.
- Graf, A., C. Schiestl, and M.A. Landolt, Posttraumatic Stress and Behavior Problems in Infants and Toddlers With Burns. nine0024 Journal of Pediatric Psychology , 2011. 36(8): p. 923-931.
- Levendosky, A.A., et al., Trauma symptoms in preschool-age children exposed to domestic violence. Journal of Interpersonal Violence , 2002. 17(2): p. 150-164.
- Scheeringa, M.S., et al., Predictive validity in a prospective follow-up of PTSD in preschool children. J ournal of the American Academy of Child and Adolescent Psychiatry , 2005.
 44(9): p. 899-906.
44(9): p. 899-906. - Le Brocque, R.M., J. Hendrikz, and J.A. Kenardy, The Course of Posttraumatic Stress in Children: Examination of Recovery Trajectories Following Traumatic Injury. nine0024 Journal of Pediatric Psychology , 2010. 35(6): p. 637-645.
- Carpenter, G.L. and A.M. Stacks, Developmental effects of exposure to Intimate Partner Violence in early childhood: A review of the literature. Children and Youth Services Review , 2009. 31(8): p. 831-839.
- Carrion, V.G., C.F. Weems, and A.L. Reiss, Stress predicts brain changes in children: A pilot longitudinal study on youth stress, posttraumatic stress disorder, and the hippocampus. nine0024 Pediatrics , 2007. 119(3): p. 509-516.
- Perry, B.D., et al., Childhood trauma, the neurobiology of adaptation, and ''use-dependent'' development of the brain: How ''states'' become ''traits''. Infant Mental Health Journal , 1995. 16(4): p. 271-291.
- Green, J.G., et al.
 , Childhood Adversities and Adult Psychiatric Disorders in the National Comorbidity Survey Replication I Associations With First Onset of DSM-IV Disorders. Archives of General Psychiatry , 2010. 67(2): p. 113-123.
, Childhood Adversities and Adult Psychiatric Disorders in the National Comorbidity Survey Replication I Associations With First Onset of DSM-IV Disorders. Archives of General Psychiatry , 2010. 67(2): p. 113-123. - Felitti, V.J., et al., Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults - The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine , 1998. 14(4): p. 245-258.
- De Young, A.C., Psychological impact of burn injury on young children and their parents: Implications for diagnosis, assessment and treatment (Unpublished Doctoral dissertation), 2011, School of Psychology, University of Queensland: Brisbane. nine0133
- Landolt, M.A., et al., The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry , 2012. 53(7): p. 767-774.
- Hall, E., et al.
 , Posttraumatic stress symptoms in parents of children with acute burns. Journal of Pediatric Psychology , 2006. 31(4): p. 403-412.
, Posttraumatic stress symptoms in parents of children with acute burns. Journal of Pediatric Psychology , 2006. 31(4): p. 403-412. - Le Brocque, R.M., J. Hendrikz, and J.A. Kenardy, Parental response to child injury: Examination of parental posttraumatic stress symptom trajectories following child accidental injury. nine0024 Journal of Pediatric Psychology , 2010. 35(6): p. 646-655.
- Lieberman, A.F., Traumatic stress and quality of attachment: Reality and internalization in disorders of infant mental health. Infant Mental Health Journal , 2004. 25(4): p. 336-351.
- Scheeringa, M.S. and C.H. Zeanah, A relational perspective on PTSD in early childhood. Journal of Traumatic Stress , 2001. 14(4): p. 799-815.
- Nugent, N.R., et al., Parental posttraumatic stress symptoms as a moderator of child's acute biological response and subsequent posttraumatic stress symptoms in pediatric injury patients. nine0024 Journal of Pediatric Psychology , 2007.
 32(3): p. 309-318.
32(3): p. 309-318. - Kazak, A.E., et al., An integrative model of pediatric medical traumatic stress. Journal of Pediatric Psychology , 2006. 31(4): p. 343-355.
- Roberts, N.P., et al., Systematic Review and Meta-Analysis of Multiple-Session Early Interventions Following Traumatic Events. American Journal of Psychiatry , 2009. 166(3): p. 293-301.
- Kenardy, J., et al., Information-provision intervention for children and their parents following pediatric accidental injury. nine0024 European Child & Adolescent Psychiatry , 2008. 17(5): p. 316-325.
- Cox, C.M., J.A. Kenardy, and J.K. Hendrikz, A Randomized Controlled Trial of a Web-Based Early Intervention for Children and their Parents Following Unintentional Injury. Journal of Pediatric Psychology , 2010. 35(6): p. 581-592.
- Zehnder, D., M. Meuli, and M.A. Landolt, Effectiveness of a single-session early psychological intervention for children after road traffic accidents: a randomized controlled trial.
 nine0024 Child and adolescent psychiatry and mental health , 2010. 4: p. 7.
nine0024 Child and adolescent psychiatry and mental health , 2010. 4: p. 7. - Berkowitz, S.J., C.S. Stover, and S.R. Marans, The Child and Family Traumatic Stress Intervention: Secondary prevention for youth at risk of developing PTSD. Journal of Child Psychology and Psychiatry , 2011. 52(6): p. 676-685.
- Scheeringa, M.S., et al., Trauma-focused cognitive-behavioral therapy for posttraumatic stress disorder in three-through six year-old children: a randomized clinical trial. nine0024 Journal of Child Psychology and Psychiatry , 2011. 52(8): p. 853-860.
- Melnyk, B.M., et al., Creating opportunities for parent empowerment: Program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics , 2004. 113(6): p. E597-E607.
- Kramer, D.N. and M.A. Landolt, Characteristics and efficacy of early psychological interventions in children and adolescents after single trauma: a meta-analysis.
 nine0024 European journal of psychotraumatology , 2011. 2.
nine0024 European journal of psychotraumatology , 2011. 2.
For citation:
De Young A, Kenardi D. Post-traumatic stress disorder in young children. In: Tremblay RE, Buavan M, Peters RDeV, eds. Rapi RM, ed. themes. Encyclopedia of early childhood development [online]. https://www.encyclopedia-deti.com/trevozhnost-i-depressiya/ot-ekspertov/posttravmaticheskoe-stressovoe-rasstroystvo-u-detey-mladshego. Published: March 2013 (English). Viewed on December 31, 2022 nine0008
Text copied to clipboard ✓
A gene has been discovered that affects the likelihood of developing post-traumatic syndrome
Post-traumatic stress disorder (PTSD) is a complex mental disorder that develops in some (but not all) people after severe traumatic experiences. American scientists have found that the likelihood of developing PTSD in women is partly hereditary and depends on a gene that affects the sensitivity of cells to one of the "stress hormones". The activity of this gene depends on the level of estrogens (female sex hormones). The discovery provides a key to understanding the causes of women's increased susceptibility to PTSD and may help develop new treatments for it. nine0279
The activity of this gene depends on the level of estrogens (female sex hormones). The discovery provides a key to understanding the causes of women's increased susceptibility to PTSD and may help develop new treatments for it. nine0279
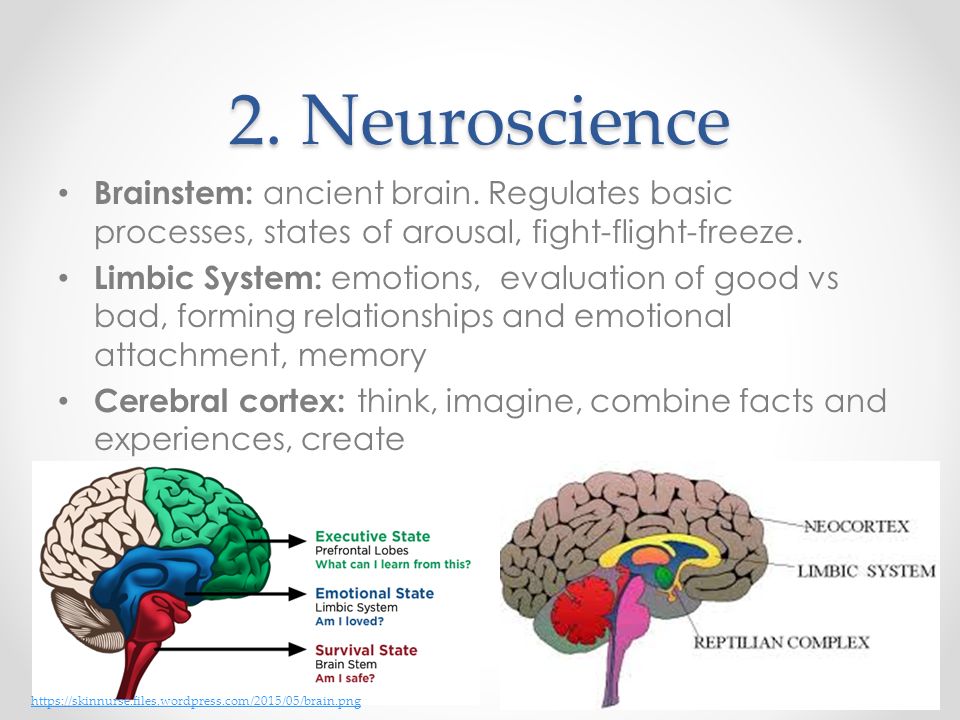
Pituitary adenylate-cyclase activating polypeptide (PACAP) is one of the hormones that regulate the response of the mammalian body to stress. PACAP is a 38 amino acid peptide. It is synthesized in the central nervous system, especially in the limbic system of the brain (see lymbic system), as well as in immune cells, sex glands, adrenal glands, gastrointestinal tract, and some other organs and tissues. Neurons and other body cells perceive this signal peptide with the help of a special PAC1 receptor. nine0008
The functions of PACAP are numerous and varied (they are not limited to the regulation of the response to stress), but only a few of them have been studied in detail. In particular, there is still a lot of uncertainty about the role of the PACAP-PAC1 signaling system in the psychological (and not just physiological) reactions of people to severe stress.
A large team of American neuroscientists, physicians and psychologists set out to find out if there is a connection between the PACAP-PAC1 system and the formation of post-traumatic stress disorder (PTSD), or post-traumatic syndrome, a complex of mental disorders that develop in some people after severe traumatic experiences . The results of the study were published in the latest issue of the journal Nature .
PTSD can be caused by severe physical injury (eg, in a car accident), combat, childhood abuse, sexual abuse. People suffering from PTSD cannot get rid of obsessive fears associated with memories of an experienced event.
Fortunately, most (approximately 80-90%) of people who have experienced severe traumatic events recover after some time and return to normal life. Only the remaining 10-20% develop PTSD, and women are much more susceptible to this disease than men. For the same amount of trauma, women are about twice as likely to develop PTSD as men.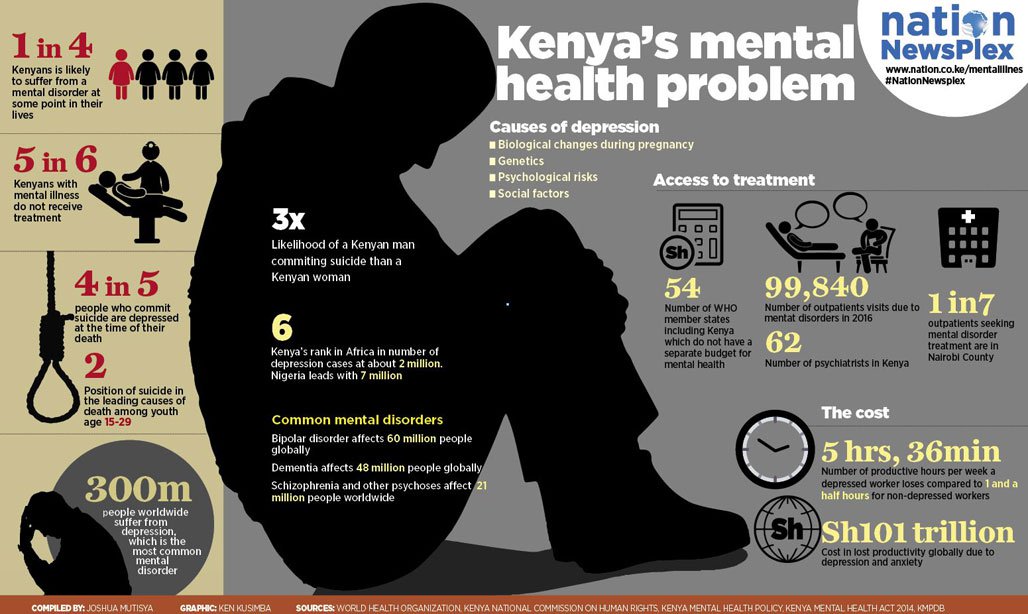 Until now, very little is known about the genetic and physiological factors that influence the likelihood of developing PTSD. Previously identified risk factors include a reduced volume of the hippocampus and some abnormalities in the amygdala and insula (see: insular cortex). The lack of scientific data hinders the development of effective methods for the treatment of post-traumatic syndrome. The means at the disposal of physicians - psychotherapeutic procedures and antidepressants - help only a small part of patients. nine0008
Until now, very little is known about the genetic and physiological factors that influence the likelihood of developing PTSD. Previously identified risk factors include a reduced volume of the hippocampus and some abnormalities in the amygdala and insula (see: insular cortex). The lack of scientific data hinders the development of effective methods for the treatment of post-traumatic syndrome. The means at the disposal of physicians - psychotherapeutic procedures and antidepressants - help only a small part of patients. nine0008
The authors compared the severity of PTSD symptoms with the state of the PACAP-PAC1 system in a large sample of Americans who experienced severe traumatic events. When diagnosing PTSD, three groups of symptoms are used: 1) constant obsessive memories of the trauma experienced, 2) avoidance of everything that is associated with the traumatic event, 3) hyperexcitability, manifested, in particular, in increased fearfulness. Depression, which often accompanies PTSD, is not included in its composition and is considered as a separate phenomenon.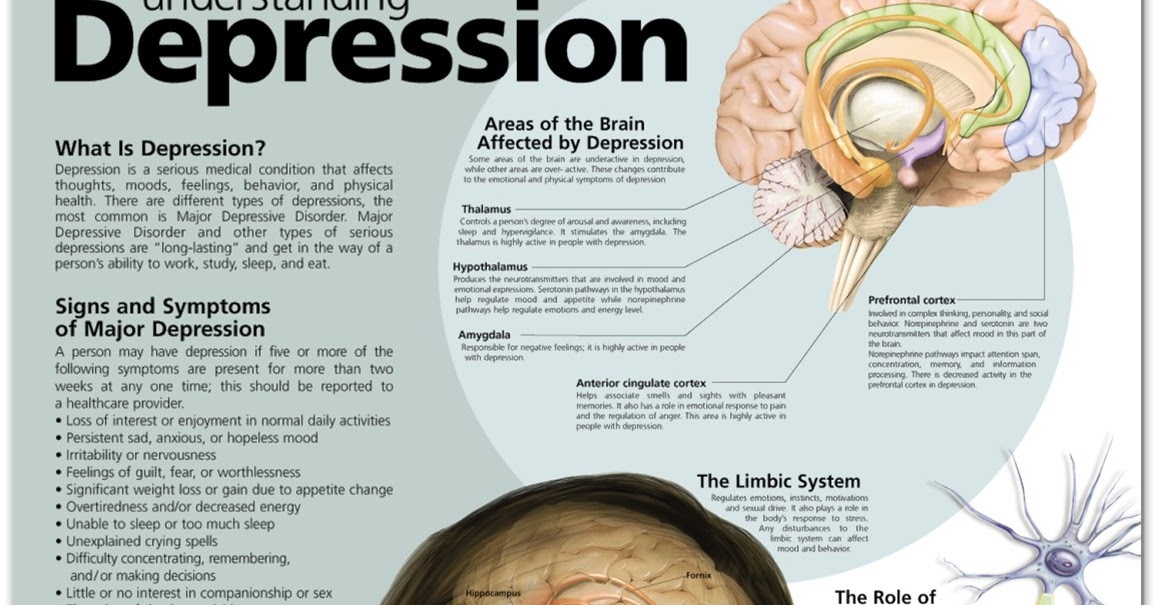 nine0008
nine0008
During the statistical analysis of the results, of course, age and gender differences were taken into account, as well as the nature and severity of the injuries suffered. The study showed a close relationship between PTSD and the PACAP-PAC1 system, with this relationship being much more pronounced in women than in men.
In women (but not in men), researchers found a strong positive correlation between blood levels of PACAP and the severity of all three groups of PTSD symptoms. Symptoms of depression, however, are independent of PACAP levels. This result showed that the researchers are on the right track and that the PACAP-PAC1 system does indeed have something to do with PTSD. nine0008
The authors then undertook a targeted search for hereditary (genetic) factors influencing the risk of developing PTSD. For this, the genes encoding the hormone PACAP and the PAC1 receptor were studied in 1237 patients who survived severe trauma. A total of 44 variable nucleotide positions (see: single nucleotide polymorphism) present in these two genes were analyzed: 14 in the hormone gene and 30 in the receptor gene.
After all the necessary statistical adjustments, it turned out that one (and only one) of these single nucleotide polymorphisms significantly affects the likelihood of developing PTSD (but not depression) after a traumatic event. Moreover, as in the case of the level of PACAP in the blood, this dependence was found only in women. nine0008
Women with a C (cytosine) nucleotide in a certain position in the PAC1 receptor gene are significantly more likely to develop PTSD after a traumatic event than women with a G (guanine) nucleotide in this position. More precisely, women with the CC genotype have the highest risk of developing PTSD, those with the CG genotype have an average risk, and those with the GH genotype have a minimal risk (see figure).
Then the authors analyzed the nucleotide sequence of the region of the PAC1 receptor gene in which this single nucleotide polymorphism is located. It turned out that this region of the gene is similar to the so-called estrogen-effector elements (oestrogen response elements, EREs) - DNA fragments, through which gene activity can be regulated by the female sex hormones estrogen. Estrogen binds to special proteins - estrogen receptors, which then attach to the ERE and thereby regulate the activity of the gene. Estrogen has previously been shown to affect the activity of the gene encoding the PAC1 receptor. nine0008
Estrogen binds to special proteins - estrogen receptors, which then attach to the ERE and thereby regulate the activity of the gene. Estrogen has previously been shown to affect the activity of the gene encoding the PAC1 receptor. nine0008
Thus, a quite logical picture emerges. Apparently, this region of the PAC1 gene is indeed an estrogen effector element. Which nucleotide is there - G or C - depends on the extent to which estrogen can affect the expression of this gene. Its expression, in turn, determines the sensitivity of cells to the PACAP hormone. Finally, the strength of the cell response to PACAP (and the concentration of PACAP) depends on the likelihood of developing PTSD.
The authors tried to find a connection between this single nucleotide polymorphism and other mental disorders (depression, Alzheimer's disease, schizophrenia, bipolar affective disorder, drug addiction) - and found nothing. This polymorphism appears to have a rather specific effect, affecting only the likelihood of PTSD in women. nine0008
nine0008
Of all the symptoms of PTSD in women with the CC genotype, increased shyness is most pronounced (which is determined, in particular, by the physiological reaction to an unexpected sound, see: Political beliefs depend on shyness, "Elements", 09/26/2008).
In the course of numerous additional experiments, the authors were able to establish the following facts:
1) The degree of methylation of the PAC1 receptor gene positively correlates with the severity of PTSD symptoms, and this dependence, unlike all others, can be traced not only in women, but also in men. nine0008
2) The activity levels of the PACAP hormone genes and its PAC1 receptor in the brain are inversely related: the more hormone, the less receptor molecules are produced, and vice versa. Such negative feedbacks are characteristic of many hormonal systems.
3) The development of a conditioned fear reflex in mice (see: Neuroscientists have figured out how to permanently get rid of terrible memories, "Elements", 11/25/2010) is accompanied by an increase in the activity of the PAC1 receptor gene in the amygdala (a part of the brain that plays a key role in the formation of a stable fear of certain conditioned stimuli).