Types of brain images
Brain Imaging: What Are the Different Types?
Brain Scans
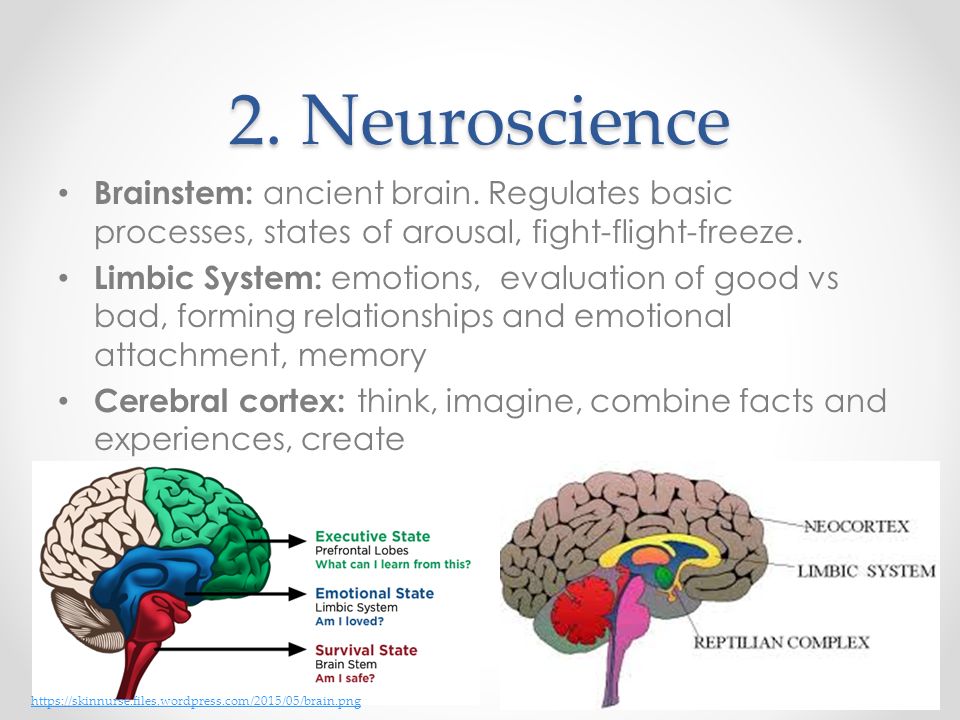
Neuroimaging—or brain scanning—includes the use of various techniques to either directly or indirectly image the structure, function, or pharmacology of the brain. Brain imaging methods allow neuroscientists to see inside the living brain. These methods help neuroscientists understand the relationships between specific areas of the brain and what function they serve.
Neuroimaging falls into two broad categories:
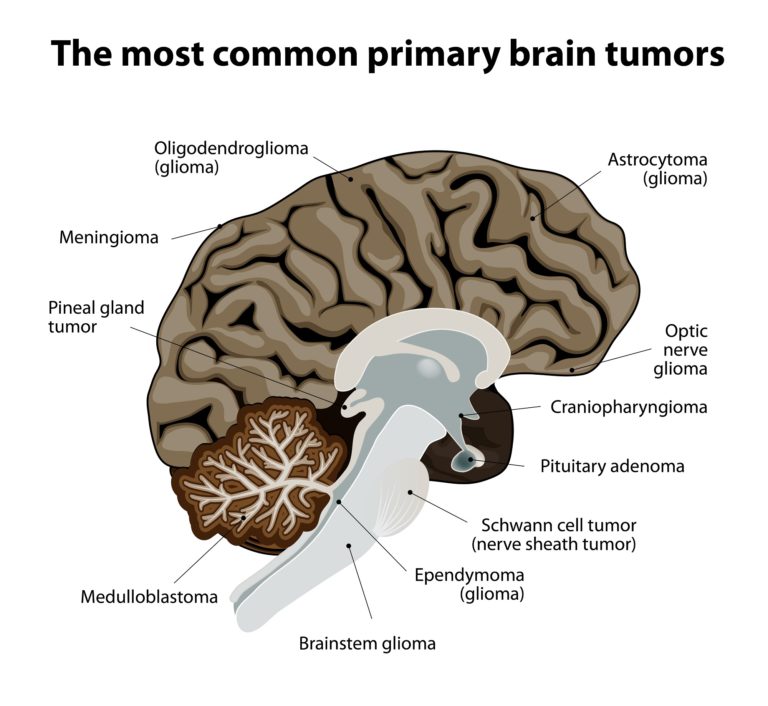
- structural imaging – deals with the structure of the brain and the diagnosis of large-scale intracranial disease—such as a tumor—as well as injury.
- functional imaging – measures an aspect of brain function, often with a view to understanding the relationship between activity in certain brain areas and specific mental functions. It is primarily used as a research tool in cognitive neuroscience and neuropsychology.
The main types of neuroimaging include:
- Computed Tomography Scan (CT)
- Magnetic Resonance Imaging (MRI)
- Functional Magnetic Resonance Imaging (fMRI)
- T1-Weighted MRI
- T2-Weighted MRI
- Diffusion-Weighted MRI (DWI)
- Fluid -Attenuated Inversion Recovery MRI (FLAIR)
- Gradient Record MRI (GRE)
- Positron Emission Tomography Scan (PET)
- Diffusion Tensor Imaging (DTI)
There is also an emerging technology called Transcranial Magnetic Stimulation (TMS), which is not a type of neuroimaging but is related.
Take a look at these slides and descriptions below to get a better understanding of the use of neuroimaging in the brain.
Computed Tomography Scan (CT)
Computed Tomography Scan (CT) scans use a series of X-ray beams passed through the head. The images are then developed on sensitive film. This method creates cross-sectional images of the brain and shows the structure of the brain, but not its function. It is the test of choice to evaluate for the four types of intracranial hemorrhage—subdural, epidural, intracerebral, or subarachnoid, which specifically means bleeding or swelling of the brain during the first 24 to 48 hours after injury. It is also used to detect a skull fracture.
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) scans use echo waves to discriminate among grey matter, white matter, and cerebrospinal fluid. These cans can show if there’s a fracture or bleeding. An MRI may be helpful if a person’s symptoms continue for 48 hours or more after the injury, or if symptoms get worse.
“For diagnostic purposes, and even for characterization of the extent of injury, we predominantly rely upon magnetic resonance imaging. This is our standard imaging modality. With an MRI, our standard measures are good at characterizing whether there's been blood, whether there's been a contusion or a bruise to the brain, or whether there is significant damage to axons that actually result in lesions that we characterize in the brain. It's also, of course, very good at tumor, at stroke, at ischemic damage.” — Deborah Little, PhD, professor, Department of Psychiatry and Behavioral Sciences, director of research for the Trauma and Resilience Center, McGovern Medical School, University of Texas
Functional MRI (fMRI)
Functional magnetic resonance imaging (fMRI) scans are a series of MRIs measuring brain function via a computer’s combination of multiple images taken less than a second apart. For this imaging test, doctors ask patients to do something while in the MRI machine like opening and closing their right hand for 30 seconds and then opening and closing their left hand for 30 seconds.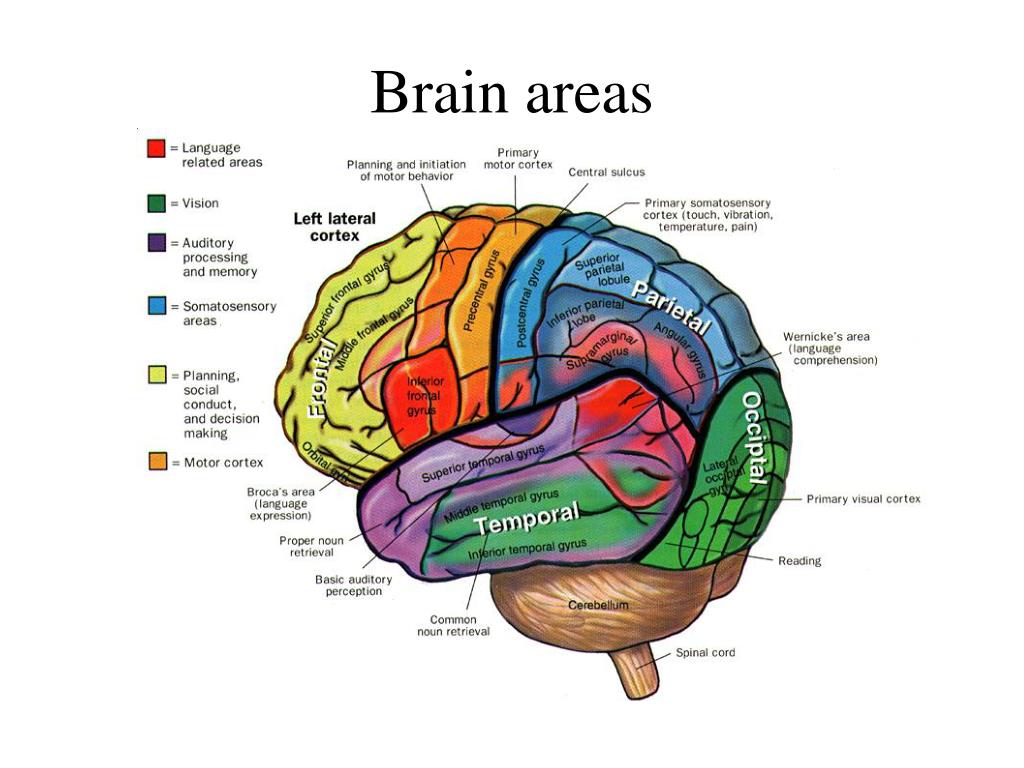 Then, the doctors model the change in signal associated with an increase in blood related to that task. So, areas involved in opening the right hand will show increased signal. This allows images to be created that reveal how the brain does tasks. This is potentially useful in brain injury when the brain structures all appear normal but the brain is functioning in a different way. It is important to know that fMRI is not approved for clinical use for diagnosis of TBI.
Then, the doctors model the change in signal associated with an increase in blood related to that task. So, areas involved in opening the right hand will show increased signal. This allows images to be created that reveal how the brain does tasks. This is potentially useful in brain injury when the brain structures all appear normal but the brain is functioning in a different way. It is important to know that fMRI is not approved for clinical use for diagnosis of TBI.
T1-Weighted MRI
The T1-Weighted MRI is the standard imaging test and part of every general MRI exam. It provides doctors with a very clear view of brain anatomy and structure. It can also show damage in brain injury but generally only when the damage is very significant.
T2-Weighted MRI
The T2-Weighted MRI is also a standard part of every MRI exam. But unlike T1-weighted imaging, the T2 allows visualization of severe diffuse axonal injury such as what is expected following severe TBI. T2-weighted scans are used to measure white matter and cerebrospinal fluid in the brain, as this type of scan is more suited to measure fluid rather than soft tissues.
Diffusion Weighted MRI (DWI)
Diffusion Weighted MRI (DWI) shows alterations in tissue integrity— the ability of body tissues to regenerate and/or repair to maintain normal physiological processes. In ischemic injury—such as many types of stroke or when blood is not able to get to all parts of the brain—there is a chemical reaction in the cells. As the cells die because of lack of blood flow (with oxygen), there is an increase in sodium and this changes (increases) the amount of water in the tissue. DWI is very sensitive to this change. In fact, using DWI, doctors can identify a stroke or ischemic injury within seconds of occurrence.
Fluid-Attenuated Inversion Recovery (FLAIR) MRI
Fluid-Attenuated Inversion Recovery (FLAIR) MRI is also sensitive to water content in brain tissue. This is very useful in patients who have reductions in brain tissue following an injury. Most commonly, however, FLAIR is used to visualize alterations in tissue in diseases such as multiple sclerosis.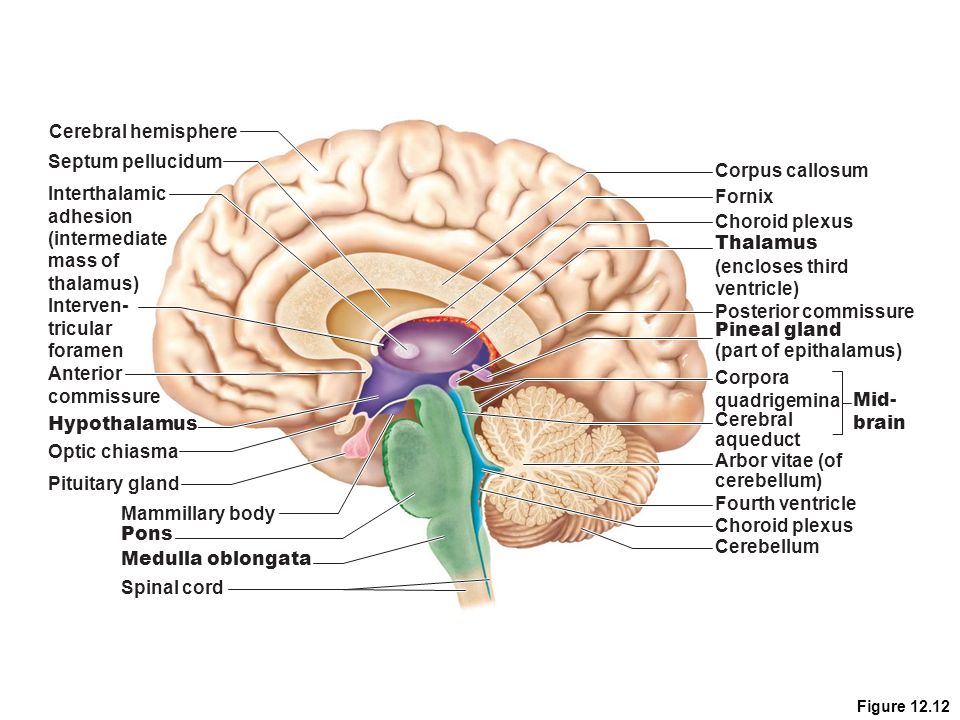
Gradient Record MRI (GRE)
Gradient Record MRI (GRE) shows blood or hemorrhaging in the brain tissue. This is very important in acute brain injury. CT scans are also very useful in this stage but sometimes miss very small bleeds—or so called microbleeds—in the brain. Other types of MRI cannot easily detect these types of injury, so GRE is particularly useful to physicians who suspect these injuries may be present in a patient.
Positron Emission Topography (PET)
Positron Emission Tomography Scan (PET) measures brain metabolism. Different applications of PET allow one to "see" pathology associated with Alzheimer's disease, for instance, that cannot be visualized any other way. Used in a different way, PET also allows doctors to see how different areas of the brain use oxygen or glucose—both very important in understanding not just what the damage might look like but also how the brain provides energy to itself. In brain injury research, PET scans are used to identify how metabolic processes may be changed after a brain injury. For instance, the brain may absorb less glucose (sugar) after a brain injury, which may affect how an individual processes information. PET has recently been used in tandem with MRI to identify (with a high degree of spatial accuracy) specific brain regions that may be experiencing metabolic changes after injury.
For instance, the brain may absorb less glucose (sugar) after a brain injury, which may affect how an individual processes information. PET has recently been used in tandem with MRI to identify (with a high degree of spatial accuracy) specific brain regions that may be experiencing metabolic changes after injury.
“PET scans look at metabolism in the brain. We inject the radiotracer glucose, and the glucose is utilized in the brain, and areas of the brain that use more glucose light up stronger, and areas that use less glucose do not light up as strong. So, we can see areas of the brain that are potentially damaged and not utilizing glucose as much as they should be.” — Gerard Riedy, MD, PhD, neuroradiologist, National Intrepid Center of Excellence (NICoE), Walter Redd National Military Medical Center Bethesda
Diffusion Tensor Imaging (DTI)
Diffusion Tensor Imaging (DTI) shows white matter tracts in brain tissue. These tracts allow different parts of the brain to talk to each other. Think of the brain as if it were a computer. With DTI, doctors can see and measure the "cables" connecting parts of the brain. DTI can provide information about damage to parts of the nervous system as well as about connections among brain regions.
Think of the brain as if it were a computer. With DTI, doctors can see and measure the "cables" connecting parts of the brain. DTI can provide information about damage to parts of the nervous system as well as about connections among brain regions.
Transcranial Magnetic Stimulation (TMS)
Although not an neuroimaging technique, per se, TMS is an FDA-cleared noninvasive treatment that uses gentle magnetic pulses to activate areas of the brain involved in mental health and addiction conditions. The treatment is well-tolerated, has no systemic side effects.
“Though still in the research stages, TMS may be a useful non-invasive brain stimulation tool to study the effects of targeted TMS treatment on individuals with chronic symptoms after brain injury.” — Cooper Hodges, PhD, Polytrauma Research fellow at the DC VA hospital
Posted on BrainLine April 22, 2011. Reviewed October 25, 2021.
Brain Imaging Techniques: Types and Uses
Many brain imaging techniques are used today, each one visualizing your brain in a unique way.
If your doctor has recently ordered a brain imaging scan, you might wonder what your upcoming session will be like or what types of brain imaging techniques might be used.
Experts have gradually improved techniques throughout the years to map out different parts of the brain and various brain functions.
There’s a lot that your doctor can learn from brain imaging, and the information that these scans provide can be helpful in forming a diagnosis and building a treatment plan.
While it may seem stressful to go in for brain imaging, you can take comfort in knowing that this is a safe and painless procedure.
The year 1924 marked the first human electroencephalography (EEG), recorded by German psychiatrist Hans Berger. This early EEG was able to detect electrical waves in the brain that would rise and fall as different brain cells communicated with each other.
Since then, neuroimaging techniques have gotten increasingly more sophisticated, and are an important tool for neurology and mental health specialists.
Commonly used brain imaging techniques are:
- functional magnetic resonance imaging (fMRI)
- computerized tomography (CT)
- positron emission tomography (PET)
- electroencephalography (EEG) and magnetoencephalography (MEG)
- functional near-infrared spectroscopy (fNIRS)
One of the benefits of brain imaging is how easily it can be performed. It doesn’t require invasive steps and often simply involves laying down and being still while the scan takes place around you.
These modern brain imaging techniques enable doctors to map out the regions and functions of your brain in a non-invasive way.
Brain imaging has many roles in health care and makes the jobs of diagnosticians easier. Some uses of brain imaging techniques include:
- identifying the effects of a stroke
- locating cysts and tumors
- finding swelling and bleeding
Doctors use a particular type of imaging method based on what they need to see in your brain. For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
Brain imaging can also connect certain mental health issues to biological causes as well. According to a 2020 study, people with high levels of anxiety also displayed differences in brain connectivity when compared to people without anxiety. In addition, brain imaging can detect conditions such as early-stage psychosis.
fMRI
Functional magnetic resonance imaging (fMRI) can detect changes in blood flow and oxygen levels that result from your brain’s activity. It uses the magnetic field of the scanner to affect the magnetic nuclei of hydrogen atoms, so they can be measured and converted into images.
MRIs display anatomic structure and fMRIs measure metabolic function.
fMRIs have many uses, such as:
- assessing brain activity
- finding brain abnormalities
- creating pre-surgical brain maps
CT
A computerized tomography (CT) scan is a series of X-ray images converted into cross-sectional images of your brain.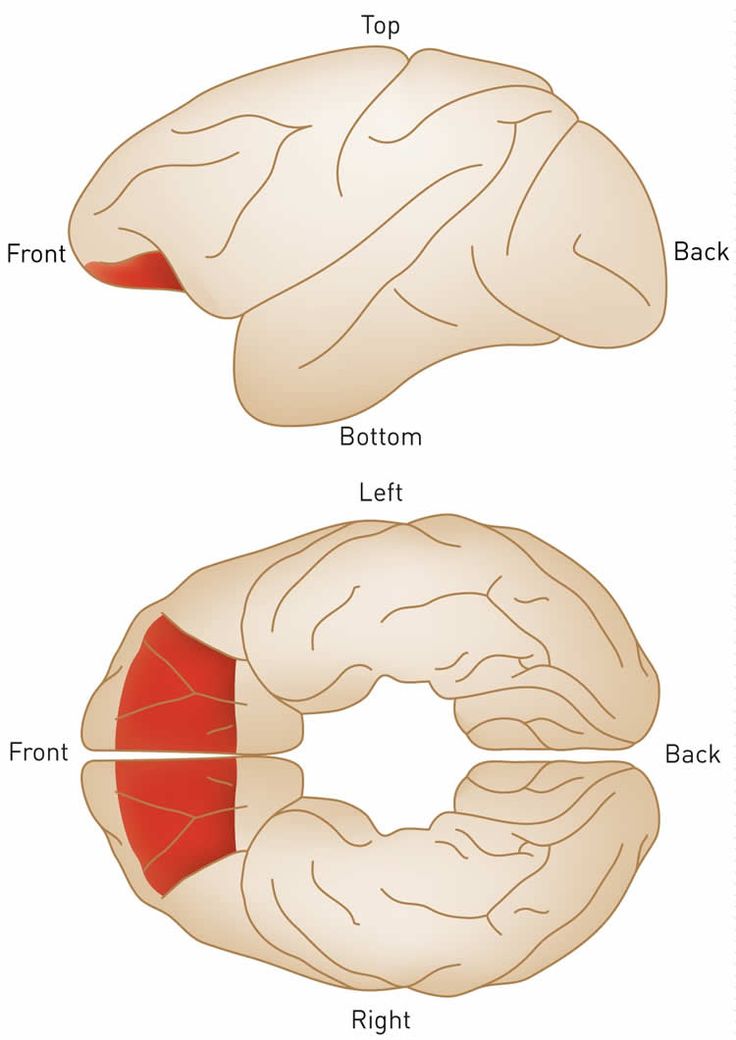 These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
CT scans can:
- find certain types of brain injuries
- identify cancer
- locate brain swelling or bleeding
- reveal structural brain changes from schizophrenia
PET
A positron emission tomography (PET) scan uses a radioactive tracer that attaches to the glucose in your bloodstream. Since your brain uses glucose as its primary fuel source, the tracer accumulates in areas of higher brain activity.
A PET scan is able to see these tracers and observe how they move and accumulate in your brain. This allows doctors to see trouble spots where glucose isn’t moving correctly.
PET scans can evaluate:
- seizures
- Alzheimer’s
- tumors
EEG
An electroencephalography (EEG) test measures your brain waves. Before the scan, clinicians will attach small electrodes to your scalp that are attached to wires. These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
EEG can detect issues such as:
- anxiety
- head injuries
- epilepsy
- sleep disruption
MEG
Magnetoencephalography (MEG) measures the magnetic field from neuron electrical activity. This type of scan can locate and identify malfunctioning neurons in your brain. Doctors use MEG to evaluate both spontaneous brain activity, as well as neuronal responses triggered by stimuli.
MEG allows doctors to assess areas such as:
- epilepsy sources
- motor areas
- sensory areas
- language and vision
NIRS
Near-infrared spectroscopy (NIRS) monitors your brain’s oxygen saturation. It uses infrared light to detect variations in hemoglobin oxygen levels in your blood. Since oxygen is critical for your brain to function properly, NIRS can assist doctors in any clinical setting where brain oxygen levels may fluctuate.
NIRS is used to monitor:
- brain oxygen levels during cardiac surgery
- brain function and oxygenation levels in preterm infants in a neonatal intensive care unit (NICU) setting
Brain imaging methods offer medical professionals a view of your brain to see if it’s structurally and functionally typical. There are several different brain scan types that map out different parts of your brain, but your specialist will know which one to use for the issue they’re investigating.
Brain imaging techniques do more than simply find medical issues, though. They can also identify brain differences associated with certain mental health conditions, such as schizophrenia, early-stage psychosis, and anxiety disorders.
If your doctor is sending you in for brain imaging, remember that this is a non-invasive procedure that will help your doctor have a clearer understanding of how your brain is functioning. After they receive the results, they can create the best and most accurate treatment plan specific to your needs.
What are the projections in MRI?
- Main
- Articles
- What are the projections in MRI?
EXPERTISE
Radiologists with experience up to 36 years
QUALITY
Tomograph Siemens 1.5 Tl expert class
OPERATION
MRI interpretation as early as
in 30 minutes*
EXPERIENCE
We have been working since 2008, over 55,000 studies
EXPERTISE
Radiologists with experience up to 36 years
QUALITY
Tomograph Siemens 1.5 Tl expert class
OPERATION
MRI interpretation as early as
in 30 minutes*
EXPERIENCE
We have been working since 2008, over 55,000 studies nine0013
- Awards
If you have any questions about the work of the center, you can write a letter to the director. Due to the possibility of obtaining images of the area under study in any projection, MRI is one of the most accurate and informative diagnostic methods.
Due to the possibility of obtaining images of the area under study in any projection, MRI is one of the most accurate and informative diagnostic methods.
There are 3 main projections:
- Ax - axial (transversal) projection. Section in the transverse plane of the body. nine0004
- Cag - sagittal view. Section along the anterior-posterior axis of the body.
- Cor - coronal (frontal) projection. The cut is in the plane of bilateral symmetry of the body, perpendicular to the sagittal.
For each organ, one of the listed projections is leading, and the other two are clarifying. In some cases, to detail the identified changes, it is possible to conduct diagnostics in any non-standard projection.
Experienced doctors
Medicenologist
17 years old
Machekhin
Grigory
Sergeevich
Rentgenologist
years old
Tomograph expert class
One MRI-study-from Visit to the result-occupies more than 1 hour
Book an MRI
Skip the line
Arrive on time
Get your procedure
without stress or pain
Get your MRI results in 30 minutes
Book an MRI
Skip the line
Arrive at your scheduled appointment
Complete your procedure
without stress or pain
Get your MRI results in 30 minutes
One MRI exam - from
visit to result - takes no more than 45 minutes minutes
As MRI results you will receive:
Exam record of your choice*
| nine0147 | ||
| for disc | on film | to flash drive |
Radiologist report
What are "artifacts" on MRI scans?
Artifacts (from lat. artefactum) are errors made by a person in the process of research. Artifacts significantly degrade image quality. There is an extensive group of physiological (in other words, related to human behavior) artifacts: motor, respiratory, artifacts from swallowing, blinking, random uncontrolled movements (tremor, hypertonicity). All artifacts associated with the human factor can be easily overcome if a person is completely relaxed during the study, breathes evenly and freely, without deep swallowing movements and frequent blinking. However, in medical practice, cases of using light anesthesia are not uncommon. nine0013
artefactum) are errors made by a person in the process of research. Artifacts significantly degrade image quality. There is an extensive group of physiological (in other words, related to human behavior) artifacts: motor, respiratory, artifacts from swallowing, blinking, random uncontrolled movements (tremor, hypertonicity). All artifacts associated with the human factor can be easily overcome if a person is completely relaxed during the study, breathes evenly and freely, without deep swallowing movements and frequent blinking. However, in medical practice, cases of using light anesthesia are not uncommon. nine0013
At what age can children have an MRI?
Magnetic resonance imaging has no age restrictions, so it can be performed on children from birth. But due to the fact that during the MRI procedure it is necessary to remain still, the examination of young children is carried out under conditions of anesthesia (surface anesthesia). In our center, examination under anesthesia is not carried out, therefore, we examine children only from the age of seven. nine0013
nine0013
What are the contraindications for MRI?
All contraindications to MRI can be divided into absolute and relative.
Absolute contraindications for MRI are the following features of the patient: the presence of a pacemaker (heart pacemaker) and other implantable electronic devices, the presence of ferrimagnetic (iron-containing) and electrical prostheses of the stirrup (after reconstructive operations on the middle ear), hemostatic clips after operations on the vessels brain, abdominal cavity or lungs, metal fragments in the orbit, large fragments, shot or bullets near the neurovascular bundles and vital organs, as well as pregnancy up to three months. nine0021 Relative contraindications include: claustrophobia (fear of closed space), the presence of massive non-ferrimagnetic metal structures and prostheses in the patient's body, the presence of an IUD (intrauterine device). In addition, all patients with magnetically compatible (not ferrimagnetic) metal structures can be examined only after a month after the surgical intervention.
Do I need to have a doctor's referral to get an MRI? nine0013
A doctor's referral is not a prerequisite for visiting an MRI center. Your concern for your health, your consent to the examination, as well as the absence of contraindications for an MRI is important to us.
I get headaches often. Which area should have an MRI?
Any person is familiar with a headache, but if it recurs suspiciously often, it certainly cannot be ignored. We recommend that a patient with severe headaches undergo an MRI of the brain and its vessels. In some cases, this may not be enough, because the cause of headaches is not always associated with the pathology of the brain. Headaches can be the result of cervical osteochondrosis, so our specialists additionally advise to undergo MRI of the cervical spine and neck vessels. nine0013
How long does an MRI exam take?
The average duration of one examination in our center is from 10 to 20 minutes, however, it all depends on the changes detected: sometimes, to clarify the disease, the radiologist may extend the examination protocol and resort to the use of contrast enhancement. In such cases, the study time is increased.
In such cases, the study time is increased.
Is Magnetic Resonance Imaging Harmful?
Magnetic resonance imaging is a completely harmless and safe method of radiation diagnostics. MRI imaging is based on the ionizing radiation inherent in computed tomography (CT) imaging. But there are contraindications that you need to familiarize yourself with before signing up for an examination. nine0013
Is pregnancy a contraindication for MRI?
An absolute contraindication to MRI is pregnancy up to three months. If an urgent (life-threatening) disease of a woman is suspected, the decision to conduct an MRI in the early stages of pregnancy is made by a gynecologist.
In our center, you can get an MRI during pregnancy in the second and third trimester - for this you need to provide a referral from the attending physician who ordered the MRI, as well as a certificate from the obstetrician-gynecologist that magnetic resonance imaging is allowed.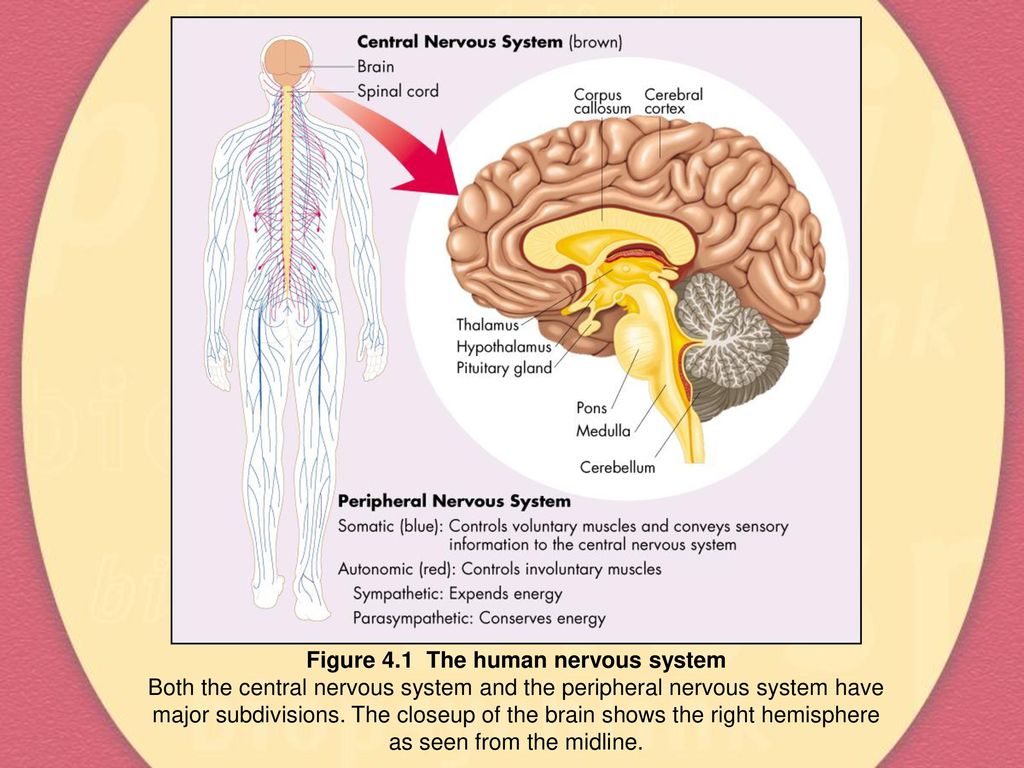 nine0013
nine0013
Decoding within 30 minutes
After the procedure, an experienced radiologist will decipher in half an hour.
Recording test results
You can receive the study in a medium that is convenient for you, as well as select several options.
By clicking on the "Sign up" button, you consent to the processing of personal data in accordance with the Federal Law of July 27, 2006 No. 152-FZ "On Personal Data". nine0013
Feedback on the work of the center
We came to the center from Estonia, Tallinn. My husband and I did many procedures: the brain, blood vessels, abdominal cavity, soft tissues of the neck. Everything is fast, high quality, the answer is on hand. Thank you! I will recommend your center to my friends. And if you need another MRI, we will come to you.
Nadezhda Marchuk, Andrey Nesterov
I would like to thank all the staff for their attentive service. Everything was very "Petersburg". Thank you! All health! Keep up the brand in the future!!! Good luck in all your endeavors! nine0013
Thank you! All health! Keep up the brand in the future!!! Good luck in all your endeavors! nine0013
Brodyagina L.I.
The center impressed me with its new renovation and new modern equipment. The examination procedure, two sections of the spine was held under classical music and a light "breeze", it was calm and comfortable.
Dukich E.N.
I really like your center, services, maintenance. Checked for the 6th time in 2 years. I only go to you. Very convenient, comfortable. Qualified personnel. Thanks a lot, everyone. Separately, I would like to note Dr. Cherkasova S.A.
Ignatieva I.P.
Signed up for the study at night. I arrived ahead of time, but everything was done quickly, clearly and as agreed at a lower price. Thanks a lot for the great service.
Kobycheva V.A.
I had an MRI with you a week ago. Everything is very fast, polite, and most importantly - a high-quality transcript and a doctor's conclusion. Thank you! I also subscribed to your VK group, what if I need it again?)))
Natalya Kiyanovskaya
I was very worried before the examination, but the clinic staff calmed me down and everything went well, thank you! The result was ready almost immediately, which is very pleased! Good and cozy environment! nine0013
Elena
all reviews
Benefits for patients
Possible presence accompanying person in the MRI room
wifi, tea and coffee for visitor center
Convenient schedule center work
Headphones with music for a comfortable MRI experience
Feedback on the work of the center
We arrived at the center from Estonia, Tallinn. My husband and I did many procedures: the brain, blood vessels, abdominal cavity, soft tissues of the neck. Everything is fast, high quality, the answer is on hand. Thank you! I will recommend your center to my friends. And if you need another MRI, we will come to you.
My husband and I did many procedures: the brain, blood vessels, abdominal cavity, soft tissues of the neck. Everything is fast, high quality, the answer is on hand. Thank you! I will recommend your center to my friends. And if you need another MRI, we will come to you.
Nadezhda Marchuk, Andrey Nesterov
I would like to thank all the staff for their attentive service. Everything was very "Petersburg". Thank you! All health! Keep up the brand in the future!!! Good luck in all your endeavors! nine0013
Brodyagina L.I.
The center impressed me with its new renovation and modern equipment. The procedure for examining 2 sections of the spine was accompanied by classical music and a light "breeze", it was calm and comfortable.
Dukich E.N.
I really like your center, services, maintenance. Checked for the 6th time in 2 years. I only go to you. Very convenient, comfortable. Qualified personnel. Thanks a lot, everyone. Separately, I would like to note Dr. Cherkasova S.A.
Cherkasova S.A.
Ignatieva I.P. nine0013
Signed up for the study at night. I arrived ahead of time, but everything was done quickly, clearly and as agreed at a lower price. Thanks a lot for the great service.
Kobycheva V.A.
I had an MRI with you a week ago. Everything is very fast, polite, and most importantly - a high-quality transcript and a doctor's conclusion. Thank you! I also subscribed to your VK group, what if I need it again?)))
Natalya Kiyanovskaya
I was very worried before the examination, but the clinic staff reassured me and everything went well, thank you! The result was ready almost immediately, which is very pleased! Good and cozy environment! nine0013
Elena
all reviews
Magnetic resonance imaging
| Magnetic resonance imaging (MRI) − method of obtaining tomographic medical imaging for the study of internal organs and tissues with using the phenomenon of nuclear magnetic resonance. Nuclear Magnetic ResonanceNuclear magnetic resonance is realized on nuclei with nonzero backs. The most interesting for medicine are hydrogen nuclei ( 1 H), carbon ( 13 C), sodium ( 23 Na) and phosphorus ( 31 P), since they are all present in the body person. It has the most (63%) hydrogen atoms, which are contained in fat and water, which are the most abundant in the human body. For these reasons modern MRI scanners are most often "tuned" to hydrogen nuclei are protons. nine0013
In the absence of an external field, the spins and magnetic moments protons are randomly oriented (Fig. 8a). If we place a proton in the outer magnetic field, then its magnetic moment will either be codirectional or opposite to the magnetic field (Fig. 8b), and in the second case, its energy will be higher. A particle with spin placed in a magnetic field, intensity B, can absorb a photon, with frequency ν, which depends on its gyromagnetic ratio γ. nine0013 ν = γ B For hydrogen, γ = 42.58 MHz/T E = hν In NMR, the quantity ν is called resonant or Larmor frequency. ν = γB and E = hν, therefore, in order to cause a transition between two spin states, the photon must have an energy of E = hγB When the energy of a photon corresponds to the difference between two spin states, energy is absorbed. tension constant magnetic field and frequency radio frequency magnetic field must strictly match each other (resonance). In NMR experiments, the photon frequency corresponds to radio frequency (RF) range. In clinical MRI, for display hydrogen, ν as the rule is between 15 and 80 MHz. nine0021 At room temperature, the number of protons spins at the lower energy level slightly exceeds their number per top level. The signal in NMR spectroscopy is proportional to the difference in level populations. The number of excess protons is proportional to B 0 . This difference in a field of 0.5 T is only 3 protons per million, in a field of 1. At equilibrium, the net magnetization vector is parallel to the direction applied magnetic field B 0 and is called the equilibrium magnetization M 0 . AT this state, the Z-component of the magnetization M Z is equal to M 0 . Another M Z is called longitudinal magnetization. In this case, transverse (M X or M Y ) no magnetization. By sending an RF pulse at the Larmor frequency, it is possible to rotate the total magnetization vector in the plane, perpendicular to the Z axis, in this case the X-Y plane. T1 Relaxation M Z = M 0 ( 1 - e -t/T 1 ) T1 relaxation occurs in a volume containing protons. However, proton bonds molecules are not the same. These bonds are different for each tissue. One atom 1 H can be bound very strongly, as in fatty tissue, while another atom may have a weaker bond, for example in water. Strongly bound protons release energy much faster than weakly bound protons. Every tissue releases energy at different speeds, which is why MRI has such a good contrast resolution. nine0013 T2 Relaxation
Time constant describing the behavior of transverse magnetization, M XY , is called the spin-spin relaxation time, T 2 . M XY =M XYo e -t/T 2 T 2 always less than T 1 . Table 1
Magnetic resonance imaging devicenine0308 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Fig.  10. Scheme MRI 10. Scheme MRI | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The scheme of the magnetic resonance tomograph is shown in fig. 10. The MRI consists of a magnet, gradient coils and RF coils.
Permanent magnet
MRI scanners use powerful magnets. From the value field strength depends on the quality and speed of image acquisition. AT modern MRI scanners either permanent or superconducting magnets are used. permanent magnets cheap and easy to operate, but do not allow you to create magnetic fields with strength greater than 0.7 T. Most magnetic resonance imaging scanners are models with superconducting magnets (0.5 - 1.5 T). Tomographs with super strong field (above 3.0 T) are very roads are in operation. On MR tomographs with a field below 1 T, it is impossible to qualitatively do tomography of internal organs, since the power of such devices is too low for high resolution images. On tomographs with magnetic field strength < 1 T can be carried out only studies of the head, spine and joints. nine0013
nine0013
| |
Gradient coils
Gradient coils are located inside the magnet. gradient coils allow you to create additional magnetic fields that are superimposed on main magnetic field B 0 . There are 3 sets of coils. Each set can create a magnetic field in a certain direction: Z, X or Y. For example, when the current enters the Z gradient, in the Z direction (along the long axis body) a uniform linear change in the field is created. In the center magnet field has strength B 0 , and the resonant frequency is ν 0 , but at a distance ΔZ the field changes by ΔB, and the resonant frequency changes accordingly (Fig. 11). By adding to the overall uniform magnetic field gradient magnetic perturbation, localization of the NMR signal is provided. The action of the gradient providing slice selection provides selective excitation of protons in the right region. From the power and speed of action coils depends on the speed, signal-to-noise ratio, resolution tomograph. nine0013
From the power and speed of action coils depends on the speed, signal-to-noise ratio, resolution tomograph. nine0013
RF coils
RF coils create field B 1 , which rotates the total magnetization in a pulse sequence. They also register transverse magnetization while it precesses in the XY plane. RF coils come in three main categories: transmitting and receiving, only receiving, only transmitting. The RF coils serve as field emitters B 1 and receivers of RF energy from the object under study.
Signal coding
When the patient is in a uniform magnetic field B 0 , all protons from head to toes align along B 0 . They all revolve with Larmorova frequency. If you generate an RF excitation pulse to translate magnetization vector into the X-Y plane, all protons react and a response signal occurs, but there is no localization of the signal source.
Slice encoding gradient
additional magnetic field G Z , superimposed on B 0 . A stronger field means more high Larmor frequency. Along the entire slope of the gradient, the field B is different and, therefore, the protons rotate at different frequencies. Now if we generate RF pulse with a frequency ν + Δν, only protons in a thin section will react, because that they are the only ones rotating at the same frequency. response signal will only come from protons from this slice. Thus the signal source is localized along the Z axis. Protons in this slice rotate with the same frequency and have the same phase. In the cut is a huge number of protons, and the localization of sources along the axes is unknown X and Y. Therefore, for the exact determination of the immediate source of the signal requires further coding. nine0013
A stronger field means more high Larmor frequency. Along the entire slope of the gradient, the field B is different and, therefore, the protons rotate at different frequencies. Now if we generate RF pulse with a frequency ν + Δν, only protons in a thin section will react, because that they are the only ones rotating at the same frequency. response signal will only come from protons from this slice. Thus the signal source is localized along the Z axis. Protons in this slice rotate with the same frequency and have the same phase. In the cut is a huge number of protons, and the localization of sources along the axes is unknown X and Y. Therefore, for the exact determination of the immediate source of the signal requires further coding. nine0013
| Fig. 12. |
Phase encoding gradient
For further coding protons, the gradient G Y turns on for a very short time. During this time, in the axial direction Y, an additional gradient magnetic field is created. In this case, the protons will have slightly different velocities rotation. They no longer rotate in phase. The phase difference will accumulate. When the gradient is G Y off, protons in cut will rotate at the same frequency, but have a different phase. This called phase encoding.
During this time, in the axial direction Y, an additional gradient magnetic field is created. In this case, the protons will have slightly different velocities rotation. They no longer rotate in phase. The phase difference will accumulate. When the gradient is G Y off, protons in cut will rotate at the same frequency, but have a different phase. This called phase encoding.
Frequency encoding gradient
For coding left-right direction, the third gradient G X is enabled. Protons on the left side rotate at a lower frequency than with right. They accumulate additional phase shift due to differences in frequencies, but the already acquired phase difference obtained with the phase encoding of the gradient in the previous step is preserved. nine0013
So for source localization signals that are received by the coil, gradients are used magnetic field.
- G Z Gradient selects the axial slice.
- G Y gradient creates lines with different phases.
- G X gradient forms columns with different frequencies.
In one step, phase encoding is performed for only one line. To scan a whole slice full cut, phase and frequency encoding process must be repeated repeatedly. nine0021 This is how small volumes (voxels) are created. Each a voxel has a unique combination of frequency and phase (Fig. 12). Quantity protons in each voxel determines the amplitude of the RF wave. Received the signal coming from different areas of the body contains a complex combination of frequencies, phases and amplitudes.
Pulse trains
| Fig. 13. Diagram of the simplest sequence |
On fig. 13 shows a diagram of the simplest sequence. First, the cut-selective gradient (1) (Gss) is turned on. Simultaneously 9 is generated with it0 0 Cutoff select RF pulse (2), which "flips" the total magnetization into the X-Y plane. Then the phase-coding gradient (3) (Gpe) is switched on for performing the first step of phase encoding. After that, it is served frequency encoding or reading gradient (4) (Gro) during which the free induction decay signal (5) (FID) is registered. Subsequence pulses are usually repeated 128 or 256 times to collect all the necessary data to build an image. Time between sequence repetitions is called the repetition time (TR). With each repetition of the sequence changes the value of the phase-coding gradient. However, in this case, the signal (FID) was extremely weak, so the resulting image was bad. To increase signal strength a spin echo sequence is applied. nine0013
Then the phase-coding gradient (3) (Gpe) is switched on for performing the first step of phase encoding. After that, it is served frequency encoding or reading gradient (4) (Gro) during which the free induction decay signal (5) (FID) is registered. Subsequence pulses are usually repeated 128 or 256 times to collect all the necessary data to build an image. Time between sequence repetitions is called the repetition time (TR). With each repetition of the sequence changes the value of the phase-coding gradient. However, in this case, the signal (FID) was extremely weak, so the resulting image was bad. To increase signal strength a spin echo sequence is applied. nine0013
Spin echo sequence
After excitation pulse 90 0 the total magnetization is in the X-Y plane. Starts right away phase shift due to T2 relaxation. It is because of this dephasing that the signal decreases sharply. Ideally, it is necessary to maintain phase coherence, providing the best signal.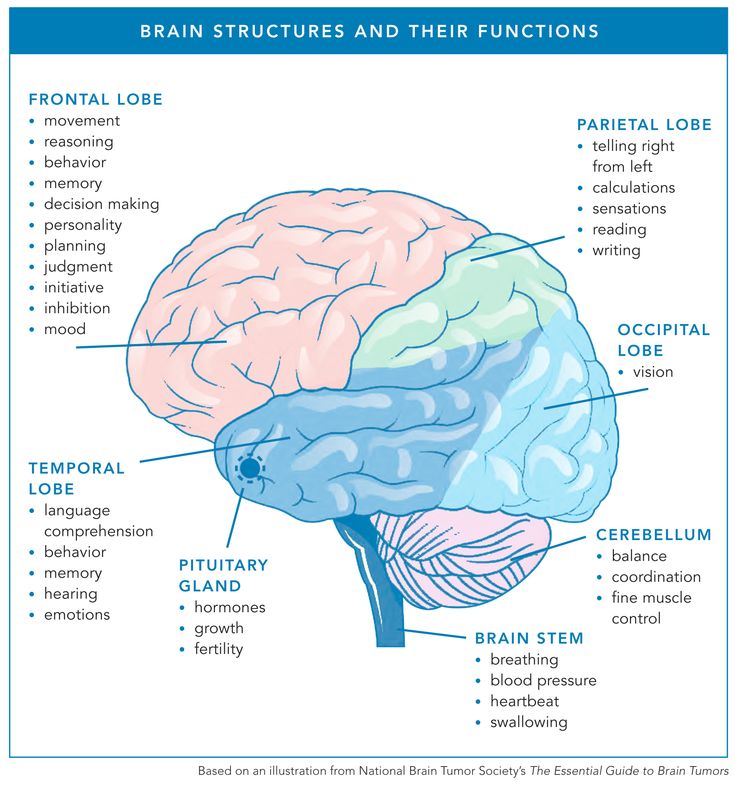 To do this, a short time after 90 0 RF pulse applied 180 0 pulse. 180 0 impulse causes spin rephasing. When all spins are restored in phase, the signal becomes high again and the image quality is much better.
To do this, a short time after 90 0 RF pulse applied 180 0 pulse. 180 0 impulse causes spin rephasing. When all spins are restored in phase, the signal becomes high again and the image quality is much better.
In fig. 14 shows a diagram of the pulse sequence spin echo.
Fig. 14. Diagram of the spin-echo pulse sequence
Slice-selective gradient is switched on first (1) (GSS). Simultaneously a 90º RF pulse is applied with it. Then the phase encoding is turned on. gradient (3) (Gpe) to perform the first phase encoding step. Gss (4) turn on again during 180º rephasing pulse (5), thus, the effect is to the same protons that were excited 90º pulse. After that a frequency encoding or reading gradient (6) (Gro) is applied, during which the signal (7) is received.
TR (Repeat time). The complete process must be repeated repeatedly. TR is the time between two 90º excitation pulses. TE (Echo time). This is the time between the 90º excitation pulse and the echo.
Image Contrast
NMR scan two relaxation processes T1 and T2 occur simultaneously. And
T1 >>T2. Image Contrast strongly depends on these processes and on how fully each of them appears at the selected scanning time parameters TR and TE. Consider obtaining a contrast image on the example of a brain scan. nine0013
T1 contrast
Fig. 15. a) spin-spin relaxation and b) spin-lattice relaxation in various brain tissues
| CSF (Cerebrospinal fluid, CSF, cerebrospinal liquid) - a clear, colorless liquid that fills cavities of the ventricles of the brain, subarachnoid space brain and spinal canal, perivascular and pericellular spaces in brain tissue. | nine0153
Choose the following scan parameters: TR = 600 ms and TE = 10 ms. That is, T1 relaxation takes 600 ms, and T2 relaxation takes only
5 ms (TE/2). As can be seen from fig. 15a after 5ms offset phases is small and it does not differ much in different tissues. image contrast, therefore, depends very weakly on T2 relaxation. As for T1 relaxation, after 600 ms fat almost completely relaxed, but CSF needs some more time
As can be seen from fig. 15a after 5ms offset phases is small and it does not differ much in different tissues. image contrast, therefore, depends very weakly on T2 relaxation. As for T1 relaxation, after 600 ms fat almost completely relaxed, but CSF needs some more time
(Fig. 15b). This means that the contribution from the CSF to the overall signal will be insignificant. Image contrast becomes process dependent T1 relaxation. The image is "T1 weighted" because the contrast is more dependent on the T1 relaxation process. The resulting CSF image will be dark, adipose tissue will be bright, and the intensity of the gray matter will be something in between. nine0013
T2 contrast
Fig. 16. a) spin-spin relaxation and b) spin-lattice relaxation in various brain tissues
Now set the following parameters: TR = 3000 ms and TE = 120 ms, that is, T2 relaxation to proceed for 60 ms. As follows from Fig. 16b, practically all tissues underwent complete T1 relaxation. Here TE is the dominant factor for image contrast. The image is "weighted by T2". On the CSF image will be bright while other fabrics will have different shades of grey. nine0013
Here TE is the dominant factor for image contrast. The image is "weighted by T2". On the CSF image will be bright while other fabrics will have different shades of grey. nine0013
Proton density contrast
There is another type of image contrast called proton density (PD).
Set the following parameters: TR = 2000 ms and TE 10 ms. So way, as in the first case T2, relaxation introduces insignificant contribution to image contrast. With TR = 2000 ms, the total magnetization of most tissues recover along the Z-axis. Image contrast in PD images is independent of from T2, nor from T1 relaxation. The received signal depends entirely on the amount protons in tissue: a small number of protons means a low signal and a dark image, while a large number of them produce a strong signal and bright image. nine0013
| Fig. 17. |
All images have combinations of T1 and T2 contrasts.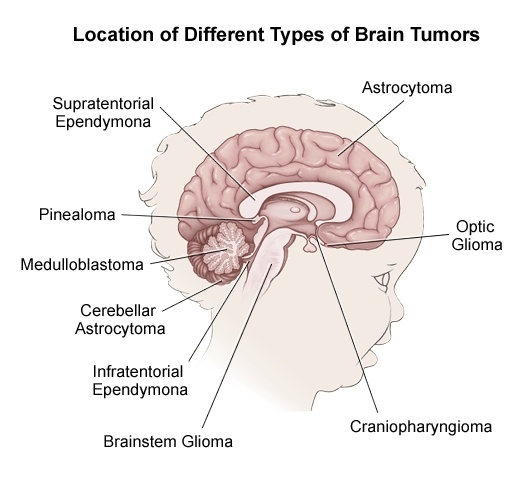 The contrast only depends on how long T2 is allowed to flow. relaxation. The spin echo (SE) sequences are most important for contrast images TR and TE times.
The contrast only depends on how long T2 is allowed to flow. relaxation. The spin echo (SE) sequences are most important for contrast images TR and TE times.
In fig. 17 shows schematically how TR and TE are connected in in terms of image contrast in the SE sequence. Short TR and short TEs give T1 weighted contrast. Long TR and short TE give PD contrast. A long TR and a long TE result in a T2-weighted contrast. nine0013
Fig. 18. Images with different contrasts: T1 weighted, proton density and weighted by T2. Note the differences in tissue signal intensity. CSF dark on T1, gray on PD and bright on T2.
| Fig. nineteen. Magnetic resonance tomograph |
MRI good displays soft tissue while CT is better visualizes bone structures. Nerves, muscles, ligaments and tendons are seen much more clearly in MRI than in CT.
 For inventing the MRI method, Peter Mansfield and Paul Lauterbur received in 2003 Nobel Prize prize in the field of medicine.
For inventing the MRI method, Peter Mansfield and Paul Lauterbur received in 2003 Nobel Prize prize in the field of medicine. 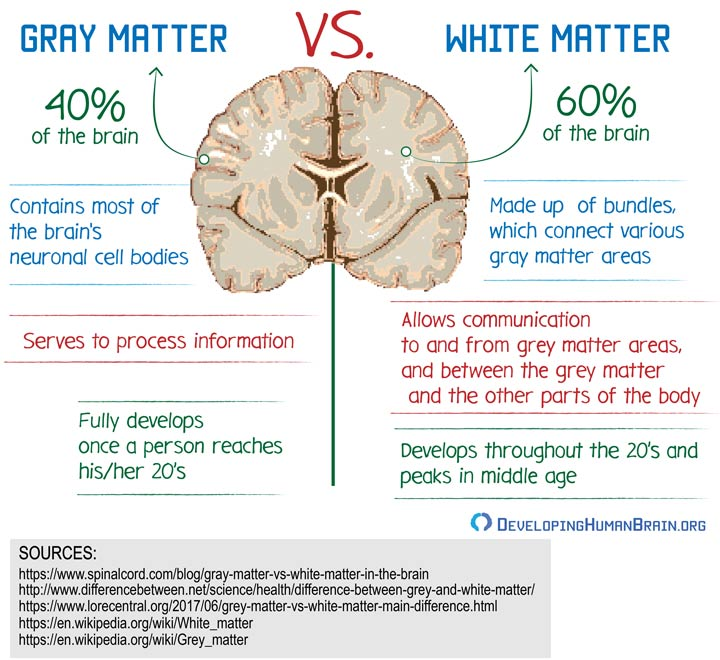 8. a) protons in the absence of an external field,
8. a) protons in the absence of an external field,  626 10 -34 J s). nine0013
626 10 -34 J s). nine0013  5 T - 9 protons per million million. However, the total number of excess protons in 0.02 ml of water in the field 1.5 T – 6.02 10 15 . Than The greater the magnetic field strength, the better the image.
5 T - 9 protons per million million. However, the total number of excess protons in 0.02 ml of water in the field 1.5 T – 6.02 10 15 . Than The greater the magnetic field strength, the better the image.  Time constant describing how M Z is returned to the equilibrium value is called the spin-lattice relaxation time (T 1 ).
Time constant describing how M Z is returned to the equilibrium value is called the spin-lattice relaxation time (T 1 ).  All vectors have the same direction because they are in phase. However they don't save that state. The total magnetization vector begins to shift along phase (out of phase) due to the fact that each spin packet experiences a magnetic field slightly different from the magnetic field experienced by others packets, and rotates at its own Larmor frequency. Quantity first dephased vectors will be small, but rapidly increasing until the moment when the phase coherence disappears: there will be no a vector that has the same direction as another. Total the magnetization in the XY plane tends to zero, and then the longitudinal magnetization increases to as long as M 0 not will be along Z.
All vectors have the same direction because they are in phase. However they don't save that state. The total magnetization vector begins to shift along phase (out of phase) due to the fact that each spin packet experiences a magnetic field slightly different from the magnetic field experienced by others packets, and rotates at its own Larmor frequency. Quantity first dephased vectors will be small, but rapidly increasing until the moment when the phase coherence disappears: there will be no a vector that has the same direction as another. Total the magnetization in the XY plane tends to zero, and then the longitudinal magnetization increases to as long as M 0 not will be along Z.  T2 relaxation called spin-spin relaxation because it describes interactions between protons in their immediate environment (molecules). T2 relaxation is a damping process, meaning a high phase coherence at the beginning of the process, but rapidly decreasing to complete disappearance of coherence at the end. Signal strong at the beginning, but quickly weakens due to T2 relaxation. Signal called the decline in magnetic induction (FID - Free Induction Decay) (Fig. 9).
T2 relaxation called spin-spin relaxation because it describes interactions between protons in their immediate environment (molecules). T2 relaxation is a damping process, meaning a high phase coherence at the beginning of the process, but rapidly decreasing to complete disappearance of coherence at the end. Signal strong at the beginning, but quickly weakens due to T2 relaxation. Signal called the decline in magnetic induction (FID - Free Induction Decay) (Fig. 9).