Vicarious posttraumatic stress disorder
Defining Vicarious Trauma and Secondary Traumatic Stress
What is Vicarious Trauma? What is Secondary Traumatic Stress?
Adapted from “The Compassion Fatigue Workbook”
What is Vicarious Trauma PDF?
Vicarious trauma (VT) and Secondary Traumatic Stress (STS) are frequently used interchangeably to refer to the indirect trauma that can occur when we are exposed to difficult or disturbing images and stories second-hand.
This can occur by viewing graphic news reports, gruesome or frightening television shows and various other media, hearing a detailed traumatic story from another person, viewing crime scene evidence, working in a court room, attending a debriefing or a conference where disturbing images are described or shown, and many other ways in which we can be indirectly affected by the content or visuals of some other living creature’s suffering.
The term Vicarious traumatization (VT) was coined by Pearlman & Saakvitne (1995) to describe the profound shift in world view that occurs in helping professionals when they work with individuals who have experienced trauma: helpers notice that their fundamental beliefs about the world are altered and possibly damaged by being repeatedly exposed to traumatic material. A domestic violence shelter worker may stop being able to believe that any relationship can be healthy. A child abuse investigator may lose trust in anyone who approaches their child. Again, examples of this abound and vary based on the type of work that we do.
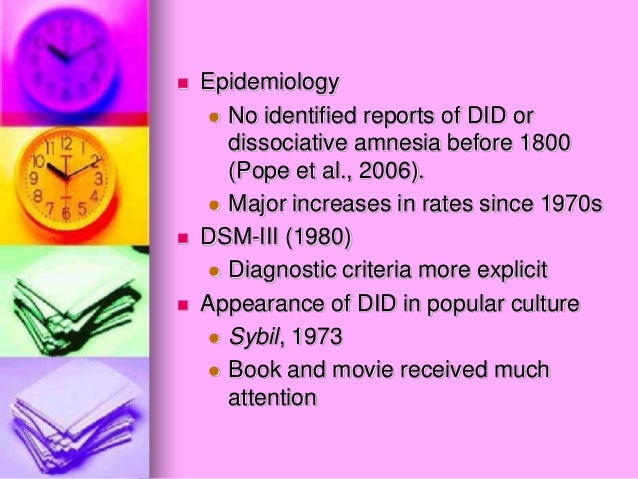
Secondary Traumatic Stress (STS) is a concept that was developed by trauma specialists Beth Stamm, Charles Figley and others in the early 1990s as they sought to understand why service providers seemed to be exhibiting symptoms similar to Post Traumatic Stress Disorder (PTSD) without having necessarily been exposed to direct trauma themselves.
VT/STS can occur in professionals who work in high-stress and trauma-exposed fields (child abuse investigators, prosecutors, judges, therapists, health care professionals, animal shelter workers and many others) but it can also affect civilians who do not work in high-trauma fields but are deeply impacted by stories that they are exposed to (maybe graphic news accounts, a friend sharing details of a traumatic event they experienced, again, there are many examples of ways in which this may occur.)
Direct trauma, in contrast, refers to a traumatic event that occurs directly to us. A paramedic who is called to a catastrophic car accident may have direct trauma as a result of what he/she sees at the crash site. The person in the car may also experience a direct trauma experience. Individuals who hear details of the crash after the fact, or see it on the news may have indirect trauma exposure as a result.
Whether someone will develop serious negative consequences as a result of VT/STS exposure depends on many factors which will we discuss below.
When you look through the literature, you may see these terms used interchangeably, and sometimes they are referred to as “Compassion Fatigue” or “Burnout”. At TEND, we believe that Compassion Fatigue and Burnout are related phenomenon but do not necessarily always co-occur. We discuss this at greater length in another post. Click Here
At the end of the day, whether you call it STS or VT, what we are referring to is the impact of indirect exposure to difficult, disturbing and/or traumatic images and stories of the suffering of others – humans and sometimes animals and they way that it might impact us as individuals and as professionals.
Over time, repeated exposure to difficult content can have a negative impact on our functioning and overall mental health, and it is important to develop a sense of our individual warning signs and develop tools to mitigate these negative effects.
Read more about Vicarious Trauma/Secondary Trauma through the links Below
Tools to Reduce Vicarious Trauma and Secondary Trauma
Warning Signs, Are You Experiencing Vicarious Trauma?
Extra Information About VT/ST
What is Vicarious Trauma - Vicarious Trauma Symptoms
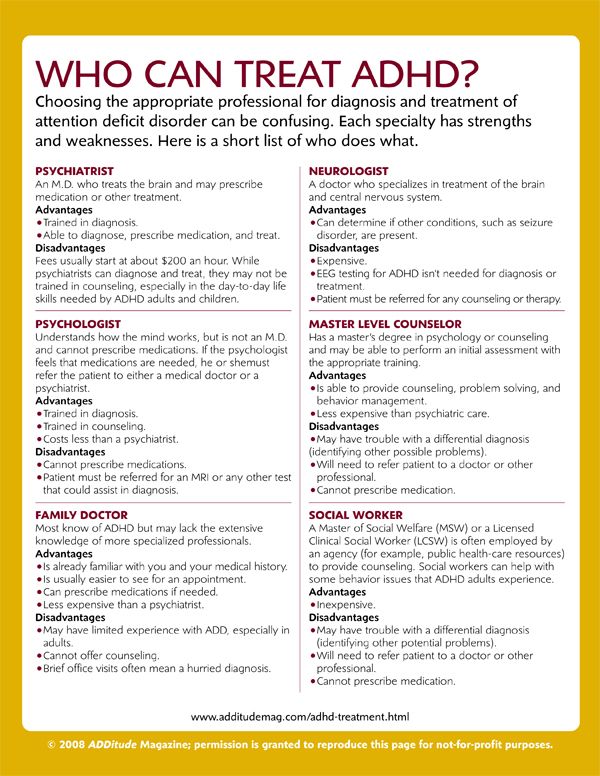
What is vicarious trauma? A negative mental health outcome on human service professionals includes compassion fatigue, which is made up of burnout and secondary traumatic stress. Secondary traumatic stress (STS) symptoms occur when an empathetic helper is exposed to another person’s trauma. Personal symptoms mimic Post Traumatic Stress Disorder (PTSD).
Secondary traumatic stress (STS) symptoms occur when an empathetic helper is exposed to another person’s trauma. Personal symptoms mimic Post Traumatic Stress Disorder (PTSD).
Contents
- Secondary traumatic stress
- Occupational exposure to vicarious trauma
- Work-related vicarious trauma
- Recognize vicarious trauma symptoms
- Employers can help build resiliency
- Improving a workplace environment
- Prevent compassion fatigue
- Incorporate resilience training
Secondary traumatic stress
Secondary traumatic stress can occur in those who are new to trauma and mental health work, don’t get enough training, or have past traumas that have not been worked through.
Secondary traumatic stress and posttraumatic stress disorder have overlapping characteristics that are similar to vicarious trauma. Vicarious trauma is a psychological response that is associated with the disturbing experiences and traumatic events of another person, often victims or crime or abuse. The condition describes the indirect trauma or the result of identifying with a trauma survivor’s suffering.
The condition describes the indirect trauma or the result of identifying with a trauma survivor’s suffering.
Occupational exposure
I define trauma as when a person experiences an extremely stressful loss event or a repeated loss event that strongly affects their ability to cope. Occupational exposure to a person’s traumatic material can bring about a psychological response. An empathetic and engaged professional can embody a trauma survivor’s traumatic experience.
Although health and mental health practitioners can experience compassion satisfaction and vicarious post traumatic growth, they can also experience vicarious traumatization. This can happen while listening to a detailed narrative of people who have experienced trauma, ongoing exposure to the re-telling of traumatized events, or responding to a traumatic event. An actual shift in intrapersonal processes occurs when addressing vicarious trauma that is work-related.
Work-related exposure
Work-related trauma exposure is a potentially distressing situation for a human services worker who is confronted with highly complex topics (e.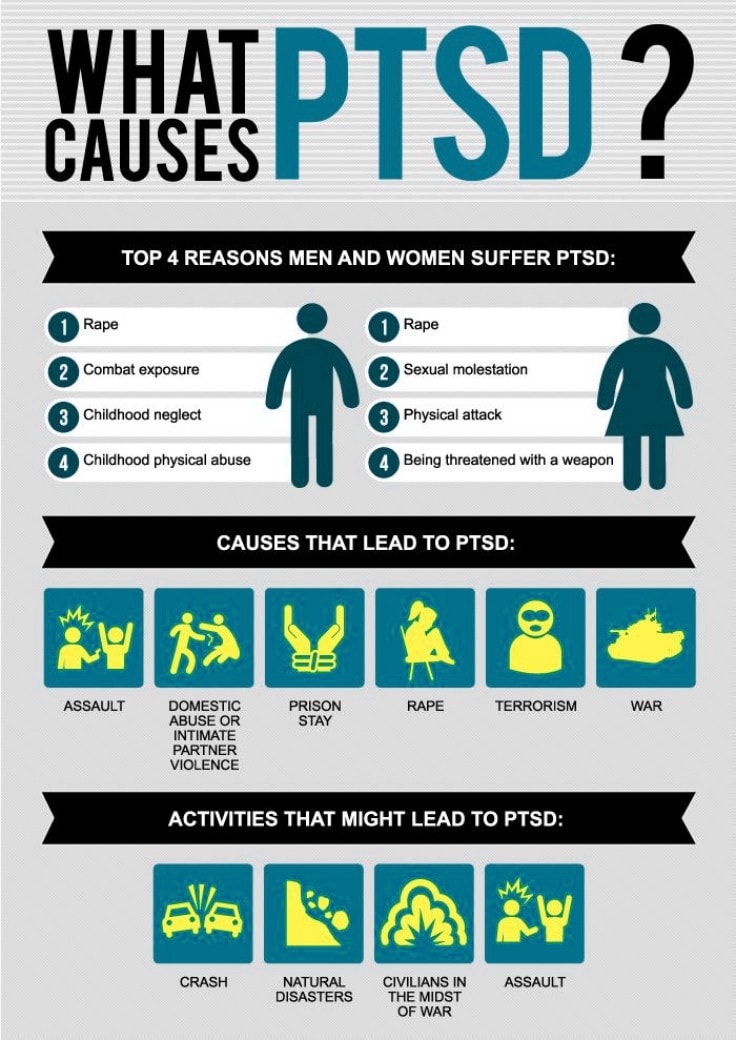 g. suicidality, physical abuse, sexual assault, mass violence). Those at a high risk for vicarious traumatization include clinicians researchers and educators, those who work in first responder agencies, law enforcement, fire services, child protective services, victim services, the courts, school systems, and mental health.
g. suicidality, physical abuse, sexual assault, mass violence). Those at a high risk for vicarious traumatization include clinicians researchers and educators, those who work in first responder agencies, law enforcement, fire services, child protective services, victim services, the courts, school systems, and mental health.
When a professional helper experiences secondary trauma, they experience changes in their world view, their role, and their perception of self. A sense of self gives them purpose in life when working in trauma-based services. They view their world based on how they grew up, and what they learned in life. When their sense of self deeply changes, their values and personal identify change with it. They become vicariously traumatized.
Recognize traumatization symptoms
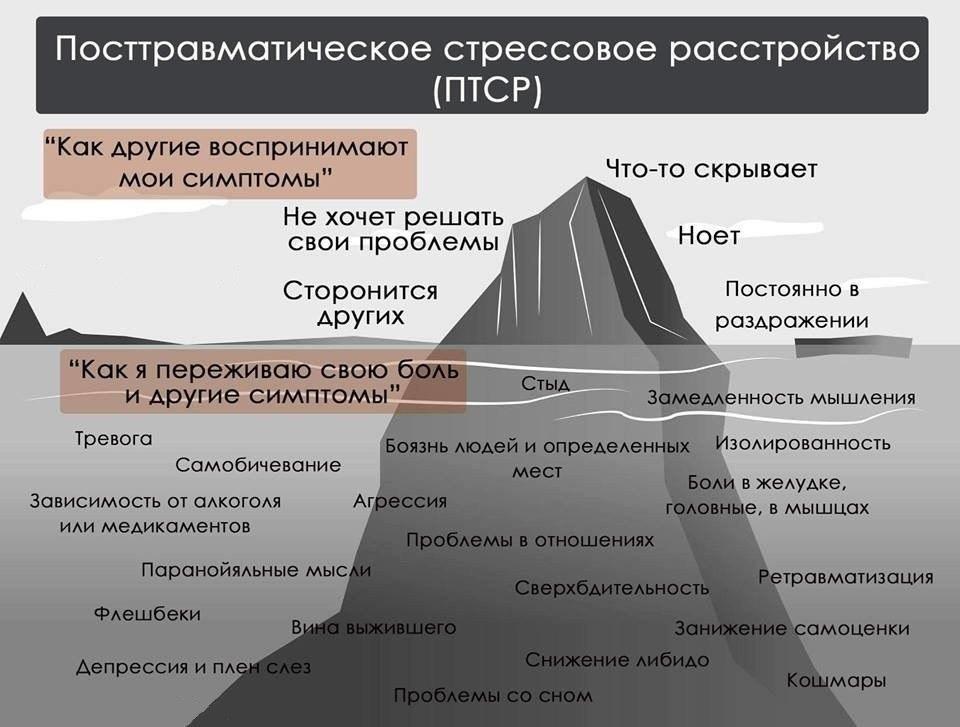
What is vicarious trauma? Symptoms include anxiety, anger, feeling isolated, depressed, unsafe, hopelessness, numbness, irritability, emotionally numb, losing control, not trusting others, powerless, fear, worried about a loved one’s safety, more sensitive to violence, being cynical, inattention, easily distracted, intrusive imagery, overwhelming negative changes in looking at one’s world, becoming forgetful about important details, loss of appetite, fatigue, risky behavior, can’t separate personal life from professional life, addictive behaviors, not wanting to talk with others about work, becoming aggressive, trouble with workplace boundaries, headaches, heartburn, loss of hope, and loss of meaning in life.
Employers can help build resiliency
Being that organizational factors influence psycho-social well-being, employers can mitigate the impact of traumatic stress before it wears away at an employee’s motivation to stay in their job. To build workforce resiliency, an employee retention strategy should focus fostering resilience and trauma treatment to prevent employee turnover and negative work environments. To function at maximum capacity when dealing with second-hand trauma, employers need to stress trauma training and self-care, and help employees develop coping mechanisms.
Employers can be proactive as they provide professional support and professional development, and a vicarious trauma toolkit. The organizational culture needs to focus on an approach to help employees, whether that is giving them additional resources and training, or educating them within the workplace about effective self-care.
Improving a workplace environment
To improve the workplace environment and stress organizational goals that focus on employee self-care, supervisors need to do the following: during orientation supply material about compassion fatigue and burnout, including a list of factors that contribute to distress in professionals who work with complex trauma survivors; pair a new employee with a mentor who has been on the job for a while; create a workplace culture that stresses shared norms around self-care; allow employees flexible working arrangements whether a compressed work week or flextime; and express an understanding of what a day is like working with those who are traumatized and how hard that is.
Employers can tell workers that they understand self-sacrifice and their guilty feelings of not working when they are at home; never allow those who work with trauma survivors to sacrifice their own well-being and self-care for that of those they support; provide trauma-informed care; give them permission to take care of themselves; show appreciation by offering occasional perks; connect with each employee on a regular basis; don’t wait for an annual review to discuss resilience and recovery; offer professional development on trauma and mental health management; and help employees be cognitively aware of the impact of vicarious trauma.
Prevent compassion fatigue
Supervision, training in emotional labor, and a team climate mitigate the impact of secondary trauma. To prevent compassion fatigue and burnout and increase job satisfaction, service providers need to practice self-care, which is a vital strategy to minimize the risk of vicarious trauma and build resilience. Employers need to motivate employees to focus on self-care to mitigate the impact of vicarious trauma and posttraumatic stress.
The right motivational keynote speaker understands how to put things in the proper perspective while enlightening professionals about new and inventive ways to foster resilience. Barbara offers the skills necessary to deal with selfcare issues for clinicians and how to develop a self-care plan. Being a keynote speaker on traumatic-bereavement-informed care, addressing vicarious traumatization, and mental well-being, means more than simply firing up a group of people about fostering resilience. It is about recognizing how aversive details of a client’s traumatic experiences has a long-lasting impact on a professional’s personal beliefs and world view.
It is about recognizing how aversive details of a client’s traumatic experiences has a long-lasting impact on a professional’s personal beliefs and world view.
Incorporate training
Contact Barbara today to learn more about burnout, secondary traumatic stress, resilience and recovery, compassion fatigue, and vicarious traumatization and incorporate trauma training in your program curricula.
Echo of Pain. What is post-traumatic stress disorder - Daria Varlamova - Psychology - Site materials - Snob
What is psychological trauma
In a broad sense, psychological trauma means any acute emotional impact that disrupts the normal functioning of the psyche. But we all differ in the degree of sensitivity, so an event that knocks down one person will not prevent another from adapting to reality and enjoying himself. In popular psychology, it is fashionable to talk about childhood traumas that affect a person’s behavior in adulthood (for example, “I had a cold father, so I don’t have relationships with the opposite sex”), but many experts are of the opinion that endlessly returning to the past and shifting all the responsibility to parental mistakes in education is not a very productive way and it is better to concentrate on changing your behavior for the better in the present. Unless, of course, we are not talking about really acute experiences that radically change the worldview.
Unless, of course, we are not talking about really acute experiences that radically change the worldview.
Does any trauma cause PTSD?
Post-traumatic stress disorder (PTSD) develops in people who have experienced a catastrophic or simply life-threatening event, from a natural disaster or war to sexual violence. Here in the first place is the loss of basic trust and a sense of security. Sometimes a person gives out acute reactions immediately after traumatization, but it happens that the symptoms appear within a few months or even years later. The repercussions of the stressful experience can cause serious problems in relationships, at work and in social life. Often, people who have experienced this have suicidal tendencies, eating disorders, or alcohol and drug abuse.
At the same time, not all mental troubles that you can get after a trauma are post-traumatic disorder: emotional shock can become a trigger for almost any mental illness, such as depression or schizophrenia. Also, not all victims of traumatic events get PTSD - this requires a combination of a genetic predisposition to mental disorders and a certain set of external factors. What matters is the duration of the stressful situation and the age at which a person experienced it (childhood injuries “heal” worse), whether there were people nearby who could provide support.
Also, not all victims of traumatic events get PTSD - this requires a combination of a genetic predisposition to mental disorders and a certain set of external factors. What matters is the duration of the stressful situation and the age at which a person experienced it (childhood injuries “heal” worse), whether there were people nearby who could provide support.
Symptoms
PTSD may present with the following symptoms:
- Intrusive thoughts. These are memories of the traumatic event and re-experiencing it in the imagination, unpleasant dreams about what happened and acute reactions to anything reminiscent of a stressful situation.
- Avoidance. People with PTSD are often afraid to discuss the traumatic event and avoid places, people, and activities associated with it. This may lead to a change of job, partner or place of residence.
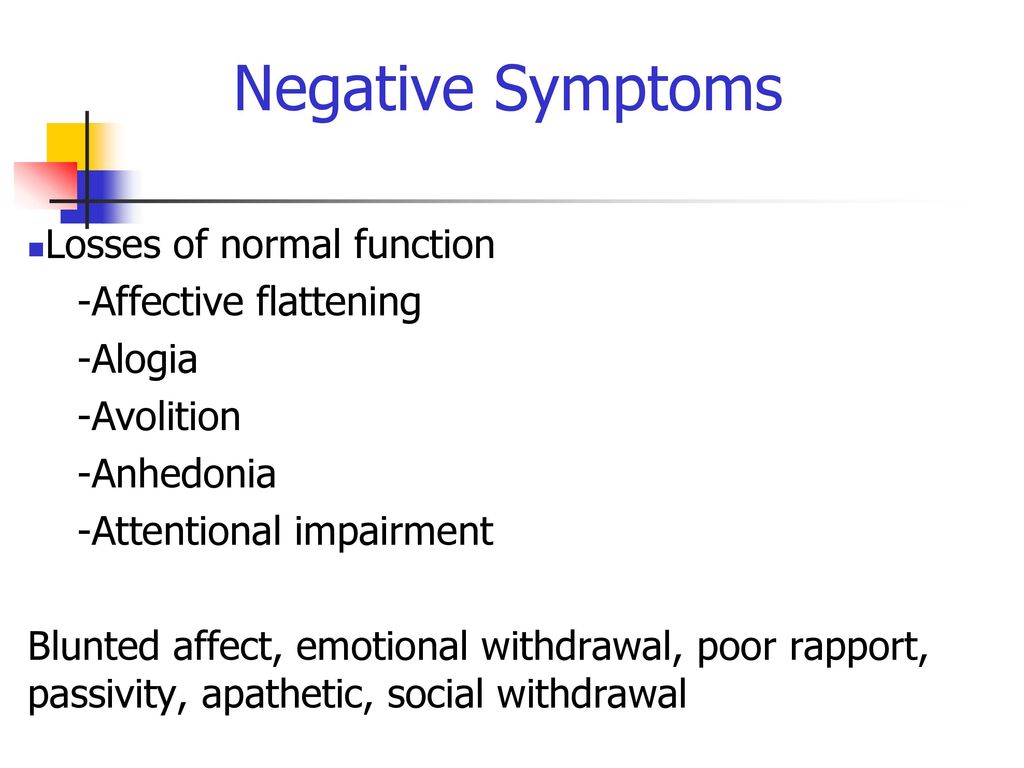
- Devastation and alienation. People who have experienced a traumatic event often lose the ability to experience positive emotions.
 They feel emotionally empty, hopeless, and lose their zest for life and interest in what used to hook them. In addition to the obvious discomfort for the patients themselves, this can cause problems with loved ones: friends and relatives may feel that the person has been changed. Now he hardly makes contact and in his thoughts he seems to be somewhere far away all the time.
They feel emotionally empty, hopeless, and lose their zest for life and interest in what used to hook them. In addition to the obvious discomfort for the patients themselves, this can cause problems with loved ones: friends and relatives may feel that the person has been changed. Now he hardly makes contact and in his thoughts he seems to be somewhere far away all the time. - Outbursts of anger.
- Anxiety/bravado. The patient may become obsessed with their own safety and become paranoid, or, conversely, constantly run into trouble, provoking situations similar to the one that caused the injury (for example, a person whose loved one died in an accident may become a street racer).
- Psychosomatics. Possible panic attacks, problems with concentration and sleep, tachycardia, fatigue, muscle tension. Often there is partial amnesia: a person does not remember some important and too frightening details of a fatal event.
See the DSM-5 for a complete version of the diagnostic criteria. But do not try to diagnose the disorder yourself - this should be done by a specialist.
Why it happens
According to one of the neurobiological theories, this disorder is caused by a malfunction in the functioning of the hippocampus, the part of the brain responsible for working with memory. It is assumed that a stressful memory is not “archived”, so the body relives it over and over again as if it were happening again in reality.
And if you think from a psychological point of view, a traumatic event deprives a person of a sense of security and trust in the world. Theoretically, we understand that life is unfair and any of us on Bronnaya can fall on the head with a brick, but we defend ourselves against these unpleasant thoughts, otherwise we would quickly cease to enjoy life. It is difficult for a person who has experienced incredibly strong stress to ignore the feeling that the surrounding reality can “set him up” at any moment.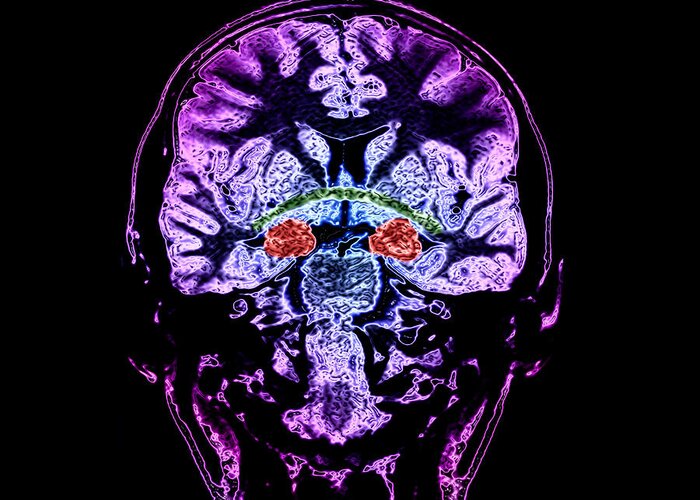
Scenario repeated
The saddest thing is that it is quite easy for a person with PTSD to get re-traumatized and fall into a vicious circle of anxiety and mistrust. Retraumatization can occur in two ways. Firstly, a person can unconsciously reproduce a sad situation from the past (for example, a victim of an abuser can find another partner with the same unpleasant qualities, and a war veteran can go as a mercenary to a “hot spot”). Secondly, trauma can be “resurrected” in the course of untimely frank conversation, inept psychotherapy, or reproduction of the circumstances where it was received. The problem is that each such circle will reinforce a negative attitude, and in the future it will be more difficult to treat a person.
How to treat
PTSD is considered a type of anxiety disorder, and patients with anxiety respond well to drug treatment with selective serotonin reuptake inhibitors (SSRIs, the latest generation of antidepressants). Sharp attacks of anxiety are relieved by tranquilizers - first of all, drugs from the benzodiazepine group. But dependence quickly arises from them, and they can be used only for a short time, about which the doctor prescribing such drugs should warn the patient. Psychotherapy also gives good results, and, as in the case of depression, from the point of view of evidence-based medicine, cognitive-behavioral therapy is considered the most reliable. But there are no universal recipes, and the patient may have to change several therapists and techniques before he finds an option that suits him personally.
But dependence quickly arises from them, and they can be used only for a short time, about which the doctor prescribing such drugs should warn the patient. Psychotherapy also gives good results, and, as in the case of depression, from the point of view of evidence-based medicine, cognitive-behavioral therapy is considered the most reliable. But there are no universal recipes, and the patient may have to change several therapists and techniques before he finds an option that suits him personally.
Contagious stress
PTSD can be transmitted: psychotherapists working with such patients sometimes experience similar symptoms, lose faith in their own safety, sense of harmony and trust in the world. This phenomenon is called "secondary" or "vicar" traumatization. In this case, the therapist may also need help in the form of communication with colleagues or a course of therapy under the supervision of a supervisor.
"A very powerful feeling of guilt for having survived.
 " What to do with PTSD
" What to do with PTSD © Illustration by Diana Dnepr
25 Oct 2022, 13:00
Three out of four frontline combatants in the Vietnam War developed post-traumatic stress disorder (PTSD). Now Russian society is threatened by the return to civilian life of tens of thousands of injured people. What this can lead to and what to do with their loved ones, psychologist Evgenia Dashkova told Taiga.info.
Taiga.info: What is PTSD, how does it manifest itself?
- Post-traumatic stress disorder - now this is the official name, but in Russian it is more often called "trauma". In short: PTSD (post-traumatic stress disorder) is the consequences of a traumatic event on the psyche.
The key to PTSD is that the person experiences or witnesses an extremely traumatic or extremely powerful negative event. Usually with a threat to life, health, for himself, or he can watch how a threat to the life of his loved ones or other people in general appears. This very event is key. It may be an accident, some kind of natural disaster, but this is not as scary for the people themselves as the events that people themselves commit. The most traumatic events are what people do to other people. These are any manifestations of violence, rape, murder.
This very event is key. It may be an accident, some kind of natural disaster, but this is not as scary for the people themselves as the events that people themselves commit. The most traumatic events are what people do to other people. These are any manifestations of violence, rape, murder.
The second side of PTSD is the consequences for the psyche. The psyche, under the influence of a traumatic event, does not withstand, and, by and large, it collapses, all aspects of its functioning are violated. On the one hand, without trauma, without a traumatic event, there can be no PTSD. It may be that there is a traumatic event, but PTSD did not happen. That is, there must also be an impact on the psyche. What is it? There are three main consequences for the psyche.
The first is the so-called intrusion. As if the psyche experiences this [event] again and again and again. These are memories of what happened. When people say that it is "as if standing in front of their eyes." What is called "flashbacks", it can be in the form of dreams, nightmares, some causeless feelings of fear. A person may not see it, not remember it, but you are in a panic for no reason. For no reason, horrified. All of a sudden, blood pressure starts to scale, literally a hypertensive crisis. It can also be memories at the level of words. When you hear any words, voices. This happens especially strongly in the first months, hours, years after a traumatic event. This is such a groundhog day, only the most terrible in life.
A person may not see it, not remember it, but you are in a panic for no reason. For no reason, horrified. All of a sudden, blood pressure starts to scale, literally a hypertensive crisis. It can also be memories at the level of words. When you hear any words, voices. This happens especially strongly in the first months, hours, years after a traumatic event. This is such a groundhog day, only the most terrible in life.
The second is the opposite tendency, avoidance. A person tries with all his might not to feel it, not to think about it, somehow distract himself. Then avoid anything that contains memories. Since this is also reminded by one's own feelings, one's own experiences, a person begins to move away from experiences. He tries not to feel fear, not to feel affection. Because, for example, you lost someone you loved, and then attachment reminds you of that pain. And the person avoids. He can avoid it in different ways. Purely behavioral - don't go somewhere, don't do something, and so on, don't talk about it. You can hear from so many people that grandfathers and great-grandfathers never talked about military operations. They were silent, remained silent, left, did not speak. This is the most typical everyday case of avoidance. Among those people who have experienced violence in everyday life - this is manifested in the refusal to speak, the refusal to even remember about this [traumatic event]. Through silence, a person tries to get rid of this, and there can be a variety of ways to avoid it - alcohol, drugs, sticking to social networks, extreme sports.
You can hear from so many people that grandfathers and great-grandfathers never talked about military operations. They were silent, remained silent, left, did not speak. This is the most typical everyday case of avoidance. Among those people who have experienced violence in everyday life - this is manifested in the refusal to speak, the refusal to even remember about this [traumatic event]. Through silence, a person tries to get rid of this, and there can be a variety of ways to avoid it - alcohol, drugs, sticking to social networks, extreme sports.
The third is overstimulation. The nervous system becomes overexcited at the moments of a traumatic event, especially if there were several of them or if it is a childhood trauma. At the moment of a threat to life, the nervous system is excited to make efforts to somehow cope with this, but nothing happens. A person still remains in trouble, still remains in a situation of threat. And this state of overexcitation does not end. A person in trauma seems to be in that overexcitation all the time that never ends.
Taiga.info: What does it mean?
- Firstly, very strong sensitivity to everything, great anxiety. Especially in women who have experienced mistreatment, the nervous system is constantly looking for threats everywhere, you are constantly on your guard. You are constantly "cutting the clearing".
In children who have experienced violence, this usually manifests itself in the fact that all adults around can be dangerous. In people who were prone to aggression before the injury, this manifests itself in outbursts of anger - they can be beaten for any reason, explode, flare up, throw things, anything. It's almost always a bad dream. Because the nervous system almost never calms down. Nightmares, some kind of tremors, jumps, and due to constant overexcitation, the body literally cannot stop, and in order to start resting and recovering, you need to calm down, but the nervous system cannot do this. A person becomes one who is constantly in a situation of danger.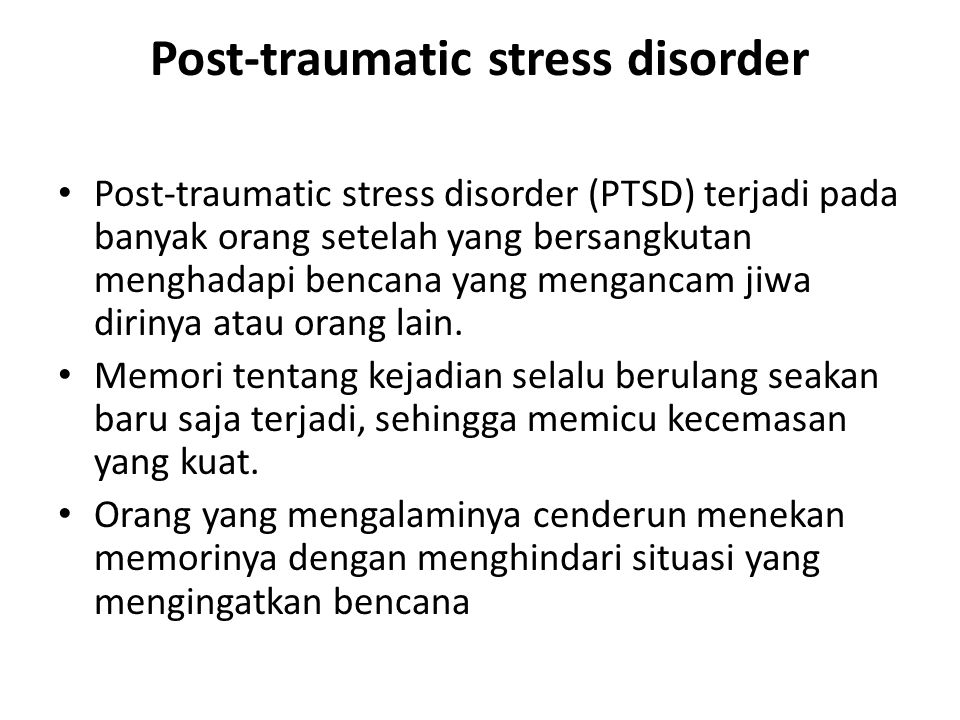
With the passage of time, these intrusive symptoms slowly subside and begin to gain strength in avoidance. But in general, a traumatized psyche is a constant push and pull, a constant contradiction.
Taiga.info: A person needs to both experience an event and try not to remember it.
- Yes, this manifests itself in life in such constant inconsistency. A person may be very sensitive to violence, but may flare up. If he saw something wrong somewhere, he flared up, he is furious and at the same time cannot survive violence - he is trying to save bunnies or kittens. The back and forth trend persists constantly and unwinds very strongly.
But there is also such a super-symptom — what happens outside of behavior, this is the destruction of the “I”, the identity is destroyed. Belief in oneself as a person who is worthy collapses, the physical integrity of a person collapses, he begins to think "it is not clear who I am." Usually it is a very powerful feeling of guilt for having survived. Or it is a feeling of shame because you allowed something to be done to you. Faith in people is completely destroyed, in general, faith in humanity in such a global world. And faith in God, in some higher powers, in the fact that the world is worthy to live in it, to give birth to children. It's all just falling apart. We get the ruins of personality and a completely destroyed nervous system.
Or it is a feeling of shame because you allowed something to be done to you. Faith in people is completely destroyed, in general, faith in humanity in such a global world. And faith in God, in some higher powers, in the fact that the world is worthy to live in it, to give birth to children. It's all just falling apart. We get the ruins of personality and a completely destroyed nervous system.
Taiga.info: Can it be argued that people involved in activism do not often experience their trauma in this way?
— Yes, many traumatized people find themselves in altruism. In volunteering, in helping others. And this is natural, because they become very sensitive. And sometimes, as you may have seen, one can observe rage, hatred and temper in activists. This, however, may be a manifestation of trauma. But the symptoms of trauma can be maladaptive, for example, if you go into drugs. But it can also be adaptive if you find yourself in volunteering, activism, helping others. And this helps to bring meaning to life and bring faith in people to life.
And this helps to bring meaning to life and bring faith in people to life.
Taiga.info: There seems to be a feeling of "need".
- And an attempt to restore one's own "I", one's own identity. Then volunteering can be a way to heal from trauma, because the person regains their identity. Plus, there is an important feature in trauma - in trauma, a person is helpless, he cannot do anything. And this is what is traumatic - you will die now, and there is nothing you can do.
Data show that those who have tried to fight in some way are less likely to experience PTSD. He has a lower risk of PTSD, and, in fact, this is what we do in activism. On the one hand, we establish connections with other people, which is insanely important when working with trauma, on the other hand, we restore the feeling of "I can do something." We struggle with our own helplessness.
Taiga.info: Does everyone develop PTSD? Maybe there should be precise conditions for this? Or does age play a big role?
- The key thing that affects whether there will be a trauma or not is the characteristics of the traumatic event itself. All the data I'm talking about is research on Vietnam veterans. The Vietnam War went on for a long time and began to be heavily recorded, research was carried out. The data is such that among those who were on the front line, who directly participated in the hostilities, PTSD will be in three out of four cases.
All the data I'm talking about is research on Vietnam veterans. The Vietnam War went on for a long time and began to be heavily recorded, research was carried out. The data is such that among those who were on the front line, who directly participated in the hostilities, PTSD will be in three out of four cases.
You can fight in different ways. You can fight while sitting at the headquarters and launching rockets - that is, you yourself do not participate in this, you do not see it.
Taiga.info: Often by others.
- You can't see anything with your eyes. You brought the installation up and fired, you don't see what happened. And you are not directly in danger at this moment. Here among them, in my opinion, only about 9% of PTSD. That is, the key is the events themselves, how dangerous, painful they were, where you were.
Among women who have experienced violence, almost 100% will be traumatized in one form or another.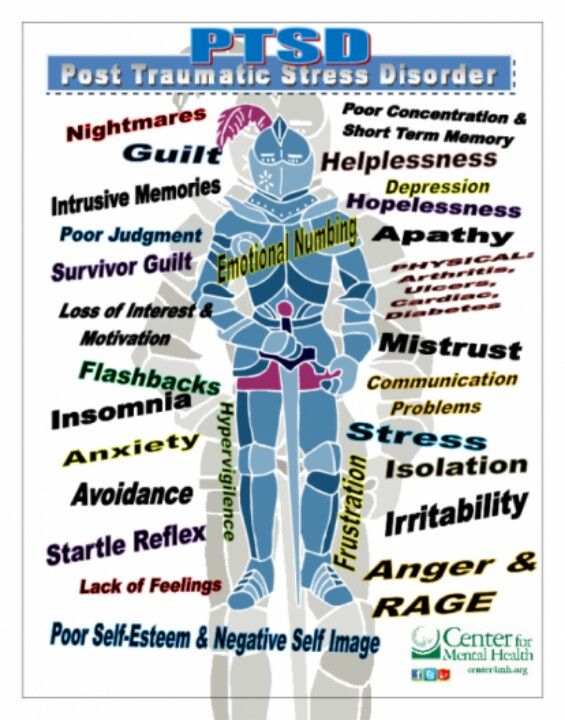 The most traumatic events are where the violence is committed by someone you treated well. Or it is violence against the defenseless. Even soldiers suffer the most when they see them killing women, children, civilians, and so on. Paradoxically, those who themselves participate in the killing of civilians have the highest probability of PTSD in the future - almost 100%. If your loved ones, comrades in the company, died, if your commander or comrades betrayed you, this is also the highest risk [of developing PTSD].
The most traumatic events are where the violence is committed by someone you treated well. Or it is violence against the defenseless. Even soldiers suffer the most when they see them killing women, children, civilians, and so on. Paradoxically, those who themselves participate in the killing of civilians have the highest probability of PTSD in the future - almost 100%. If your loved ones, comrades in the company, died, if your commander or comrades betrayed you, this is also the highest risk [of developing PTSD].
During the First World War, when the word "injury" did not even exist, it was believed that this was a loss of military spirit, a loss of face. Such people were treated with beatings and lectures on how to restore the warrior spirit. The data from there is as follows: if a soldier stayed on the front line for 200 days, not a single one left unbroken. There are conditions that no one can stand.
But there are some events that predict how quickly a person will break down. The fastest are children, because they are small, weak, and the world around is strong. Plus, children instantly become defenseless.
The fastest are children, because they are small, weak, and the world around is strong. Plus, children instantly become defenseless.
Taiga.info: Is it possible to get PTSD without any direct contact with violence, but, for example, watching it on the news every day?
— Yes, you can. It even has a name - vicarious trauma. When we observe cruelty, violence for a long time. We are experiencing at this moment the same helplessness, we are experiencing the same loss of faith in the world. Our body experiences almost the same emotions and sensations. Yes, in fact, it will be the same trauma, but there is a difference.
First, the injury will still be less because the body has not had direct contact with violence. Accordingly, at the level of the body, it has not been so strongly imprinted, so it will be easier to work with it. More prone to vicarious trauma are journalists, the same volunteers, activists, psychologists, all those who often see violence.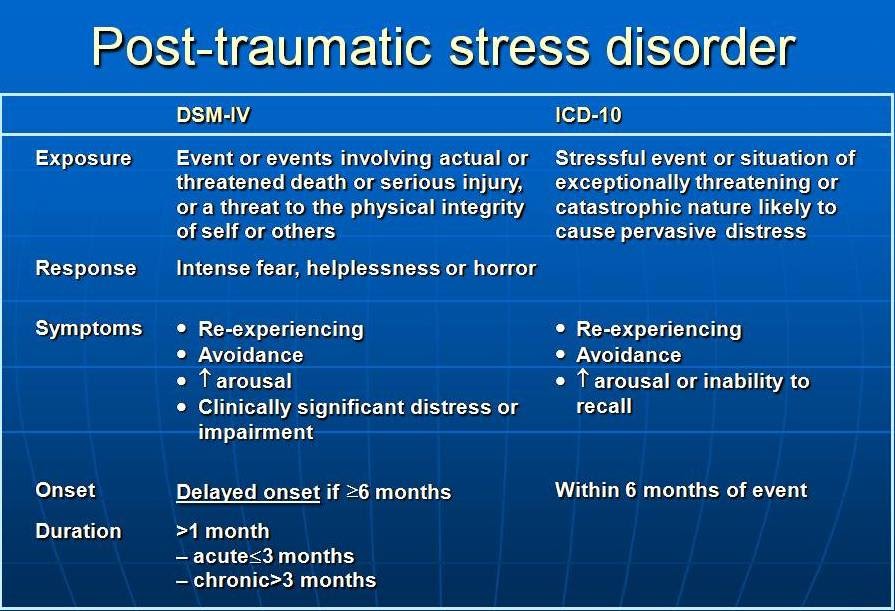 The simplest thing in the prevention of vicarious trauma is to minimize the similarity of the picture to real life. Mute the sound, if possible, turn the screen to black and white. If possible, do not watch the video, but read the texts. Make the situation as unlike reality as possible.
The simplest thing in the prevention of vicarious trauma is to minimize the similarity of the picture to real life. Mute the sound, if possible, turn the screen to black and white. If possible, do not watch the video, but read the texts. Make the situation as unlike reality as possible.
Taiga.info: People who will constantly be in contact with the injured can also get a vicarious injury?
- Of course. They can be traumatized either by the constant uncertainty about what is happening with your loved one, some terrible information about him, his fate. Or they may be traumatized by this loved one himself, who returned [from the war]. And their propensity for violence, of course, increases dramatically.
Taiga.info: Accordingly, the consequences of injury are also similar?
Yes.
Taiga.info: If we are talking about people who got PTSD through direct contact with violence, what strategy of communication with them should we choose? If we constantly observe outbursts of anger or they go into alcohol, drugs, how should we behave in general? If this is a loved one, how to help him, how to alleviate the pain?
- Probably the most honest answer would be - I don't know. It's like living with a broken person. I think the first thing is to pay attention to your feelings. Because if this is your loved one and you communicate with him, live, it is very painful if you love him. It's the same as living day by day with your father's ghost, only it still beats you up.
It's like living with a broken person. I think the first thing is to pay attention to your feelings. Because if this is your loved one and you communicate with him, live, it is very painful if you love him. It's the same as living day by day with your father's ghost, only it still beats you up.
I think the first thing you can do is take care of yourself. If a person commits violence, you need to seek salvation from this violence, to protect yourself physically. Secondly, it is to secure yourself financially, if your husband came and he has depression or hard drinking, you will have to somehow get out. After all, close people with PTSD have little strength, everything is bad, there are many difficulties in life, and if we throw all our strength into helping another person, we ourselves can remain stranded after a while. Therefore, the first thing is to protect yourself by any means.
Secondly, when a person is more or less stable, there is no point in doing something when he is in a fit of rage. When he is calm, talk to him about the injury and try to convince him to seek help or seek this help with him. Do not take [responsibility] completely on yourself, but at least discuss with him that he needs help. It, unfortunately, cannot be provided simply by a close person. No matter how much you love your father, brother, husband, wife, a loved one cannot become the one who cures. You need to seek help, and this is not necessarily professional help.
When he is calm, talk to him about the injury and try to convince him to seek help or seek this help with him. Do not take [responsibility] completely on yourself, but at least discuss with him that he needs help. It, unfortunately, cannot be provided simply by a close person. No matter how much you love your father, brother, husband, wife, a loved one cannot become the one who cures. You need to seek help, and this is not necessarily professional help.
The very first organized help groups, which started the history of PTSD treatment at all, were connected with the Vietnam War. The then medicine could offer nothing to the soldiers, and they began to unite themselves. They told each other about what was happening just to hear each other. The same was done by female rape victims who organized small groups, met and talked. This is the first part of dealing with trauma so that you can be heard. Accordingly, what can you do for a loved one with a trauma - ask him to tell you about what he sees, what kind of horrors, what kind of nightmares. Do not insist and believe him, express it with all your words and gestures. Relatives can help provide a sense of security, because this is categorically lacking for a person with PTSD, since the psyche is constantly under threat.
Do not insist and believe him, express it with all your words and gestures. Relatives can help provide a sense of security, because this is categorically lacking for a person with PTSD, since the psyche is constantly under threat.
When a person is sausage, he lies, sobs and shouts - come up, cover him with a blanket, such the simplest things. Tell him that you are here now, look around, you are safe, nothing threatens you. During nightmares, during falling into a stupor, you need to constantly repeat "you are safe, I am with you, everything is fine." Tactility helps. Touch this blanket, touch this, bring any warm drink. Let him not even drink, just give it to his hands. You know, like in American films - they cover the victims of some disasters with a blanket, they cover with a blanket with a head and something warm in their hands - this gives a feeling of security. This can be done at home, it helps a person to see that he has returned from the places of violence, from the street where she was caught and raped, that the person is no longer at home with the father who beat him, that he is safe here and now.
It is clear that it is possible and necessary to insist on a psychiatrist. It won't help heal the injury, but it will help support the nervous system. Antidepressants increase resistance in general to some difficulties. They restore disturbed excitation-inhibition systems, help to somehow stop the symptoms and help a little. To summarize: the first is to take care of yourself, the second is to ensure the safety of the person, help him understand that he is safe, the third is the psychiatrist.
Taiga.info: Another collective experience with people.
- Yes, maybe I'm exaggerating a lot now, but swimming in pools and shouting "For the Airborne Forces!" can be considered for…
Taiga.info: Collective therapy?
Yes.
Taiga.info: Is it possible to completely recover from this type of injury? Or is it already becoming part of a person's identity, and he somehow bases his life on it?
- It depends on what it means to be completely cured. A person will not become what he was. Because, imagine, you were run over by a truck, all your life he ran over, after that you will not be the same, but your bones can grow together, you can learn to walk, live, enjoy something, you can learn to be safe and restore social ties. Yes, they will be completely different.
A person will not become what he was. Because, imagine, you were run over by a truck, all your life he ran over, after that you will not be the same, but your bones can grow together, you can learn to walk, live, enjoy something, you can learn to be safe and restore social ties. Yes, they will be completely different.
This is a huge misfortune for people who come from military operations, you can often hear: I returned, everything has changed for me, but here everything remains the same. And then this rupture of all previous social ties occurs. People often go into alcohol, into some violent acts, into crime, and so on. You can make some new contacts, find new connections. And if you ask “is it possible to live a long, meaningful, fulfilling life after an injury?”, The answer is yes, but this life will never be the same as before the injury.
Taiga.info: Is there psychological rehabilitation for people in Russia after staying in places with an increased level of violence?
- She is not there as such. To have a well-established system of rehabilitation, you need to admit that there is a problem. And the state needs to allocate money, funds and resources to solve this problem. And we don't have this problem. Why help with something that is already good.
To have a well-established system of rehabilitation, you need to admit that there is a problem. And the state needs to allocate money, funds and resources to solve this problem. And we don't have this problem. Why help with something that is already good.
As such, we do not have training for psychologists and psychiatrists in working with war trauma, for example. Everything that Russian psychologists know about working with trauma is the result of their own initiative. All the trainings that were paid. They can be counted on the fingers of two hands. By injury, they will usually understand something like “it’s your own fault” and they will offer you to play in the sandbox, draw mandalas.
Taiga.info: Drink weed.
- Or breathe. No finances, no recognition of the problem, no trained professionals. I think the last thing veterans do right now is turn to a psychologist, because there is no history of public discussion as such.
Taiga. info: There is no culture of discussion.
info: There is no culture of discussion.
Yes. Only a few who have money go to psychologists, but, as a rule, people who have some money do not go to serve. To serve in the army now, many go just from lack of money in order to somehow earn money on the contract. Therefore, I think that this is a completely lost situation. I think that people who have returned now will just drink too much. There are two options. If a person before the injury had a tendency to illegal behavior, then these will be outbursts of aggression and trauma to everyone around him. If a person, let's say, of high moral qualities, then it will most likely be depression, some kind of quiet alcoholism and a lot of suicide attempts.
Taiga.info: So it will hit everyone?
- This will have huge consequences for the whole society. When one part, in this case not a person, but a society, is insanely sick, and they scream that this is horror, a horror, a nightmare happened to us, look at this, and the second part of society is unbearable to look at it, I want not to encounter, not to have nothing in common.