Treatment for postpartum anxiety
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.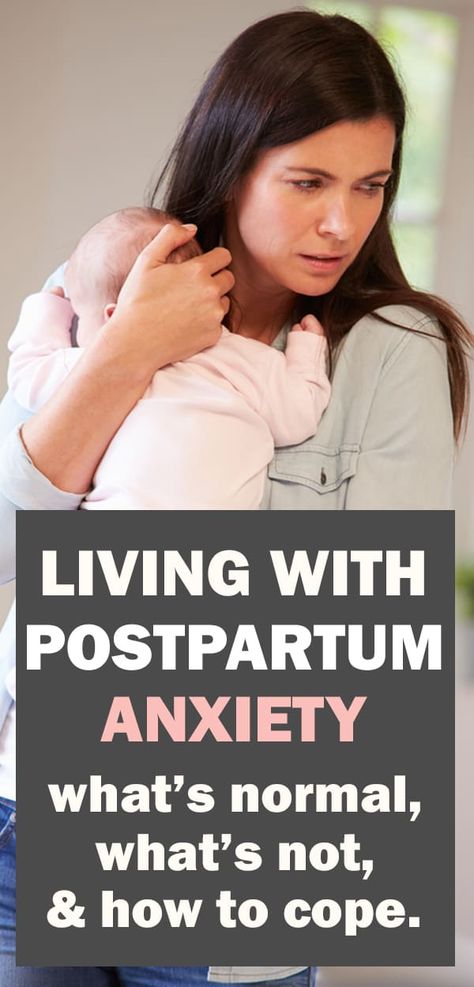 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.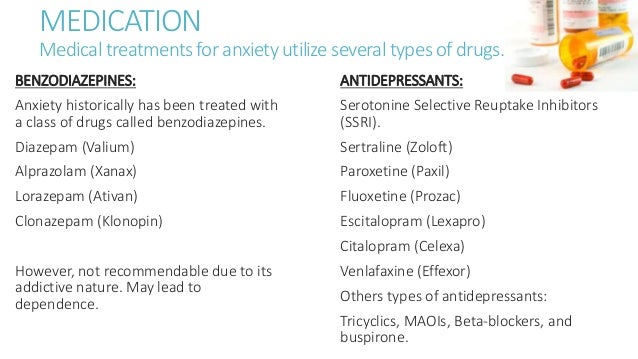
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Postpartum anxiety: difference from depression, symptoms, treatment
Pediatrician Dina Blanchard lives in Manhattan and, preparing to give birth to her second son two years ago, dreamed of making the most of four months of maternity leave: waking up in the morning next to the baby in an apartment in Upper West Side, go to postnatal yoga, and walk a lot in Central Park. “I was going to completely and completely immerse myself in the happiness of motherhood,” she recalls. Instead, Blanchard found herself consumed by anxiety at every moment.
She pestered her husband and doctor friends with calls. “I was constantly worried about something: sleeping too long - I was nervous, sleeping little - worried even more, endlessly drawing diagnoses in my head. Sometimes I dreamed of reflux, then I was allergic to milk protein. Against the background of all these fears, in two months she lost thirteen kilograms, she was tormented by insomnia. Dina recalls waiting with a baby in her arms for an appointment with a doctor and a lactation consultant. “The same thoughts constantly revolved in my head: what if something is wrong with him, and what if I don’t notice the symptoms and miss the development of some kind of disease.”
“I was constantly worried about something: sleeping too long - I was nervous, sleeping little - worried even more, endlessly drawing diagnoses in my head. Sometimes I dreamed of reflux, then I was allergic to milk protein. Against the background of all these fears, in two months she lost thirteen kilograms, she was tormented by insomnia. Dina recalls waiting with a baby in her arms for an appointment with a doctor and a lactation consultant. “The same thoughts constantly revolved in my head: what if something is wrong with him, and what if I don’t notice the symptoms and miss the development of some kind of disease.”
We're talking to Dina in a busy Flatiron office, wearing jeans and a lilac cashmere sweater, her hair in a sleek brown bob: she's a confident woman who knows her stuff. “Therein lies the trick,” she explains. — I consider myself a real professional, so I could not understand what was going on. This is not my first child, besides, I am a pediatrician!” Two weeks before the end of her maternity leave, Blanchard began to experience excruciating panic attacks and finally had to give in to a therapist. It turned out that she was suffering from postpartum anxiety, a disorder she had never heard of before.
It turned out that she was suffering from postpartum anxiety, a disorder she had never heard of before.
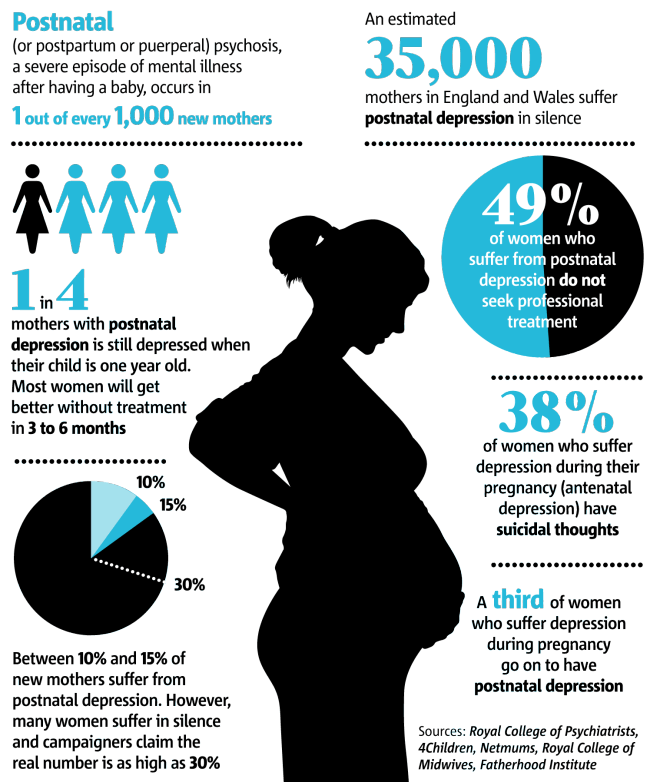
Ten out of 100 mothers develop increased anxiety after childbirth, according to Postpartum Support International, an international organization dedicated to informing and supporting those suffering from this disorder and postpartum depression. A 2016 University of British Columbia study found that it occurs more than twice as often as postpartum depression, which in turn can cause both relatively harmless feelings of hopelessness and sadness, as well as suicidal thoughts. In recent years, there has been a lot of talk and writing about postpartum depression, but so little is known about anxiety - Blanchard's case is an example of this - that doctors often do not recognize it or simply ignore it.
Popular
Another common mistake is mistaking anxiety for postpartum depression. “Everything is being called the term now,” says reproductive psychiatrist Katherine Birndorf of the Manhattan Maternity Center, which specializes in postpartum affective disorders.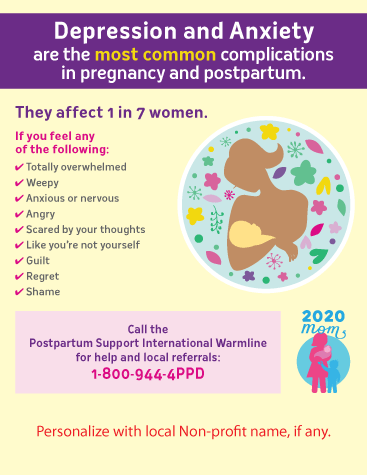 “There is a feeling that a lot of women with anxiety are generally overlooked. It often happens that at the doctor’s appointment they only talk about this: “I am constantly scared. I feel like a bad mother,” but unless even a hint of depression pops up, there will be no diagnosis.” Birndorf also elaborates that there is now a movement in America and Europe to replace the term "postpartum depression" with the more comprehensive term "perinatal affective and anxiety disorders." To make matters worse, many mothers with symptoms of anxiety, like Blanchard, don't even know there's something wrong with them—they think they're just not coping with motherhood.
“There is a feeling that a lot of women with anxiety are generally overlooked. It often happens that at the doctor’s appointment they only talk about this: “I am constantly scared. I feel like a bad mother,” but unless even a hint of depression pops up, there will be no diagnosis.” Birndorf also elaborates that there is now a movement in America and Europe to replace the term "postpartum depression" with the more comprehensive term "perinatal affective and anxiety disorders." To make matters worse, many mothers with symptoms of anxiety, like Blanchard, don't even know there's something wrong with them—they think they're just not coping with motherhood.
All new parents struggle with persistent fears, especially when it comes to their first child: for every sneeze they rush to call a doctor. Hormonal storms and lack of sleep can bring even a woman with the healthiest mind in the world to the handle, and anxiety from this is exacerbated many times over. If a new mother begins to suspect something is wrong, she is often embarrassed to seek help: according to a recent study by the University of North Carolina, twenty-one percent of women suffering from postpartum disorders, including anxiety, do not tell their doctor about them.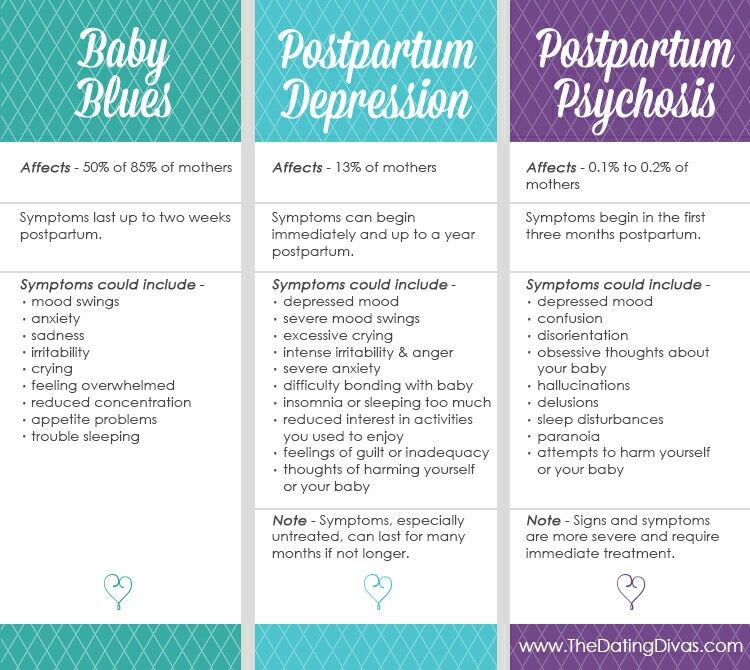 Those who already suffered from anxiety disorders not related to motherhood are at higher risk of postpartum anxiety. Cultural factors also play a role: the colossal pressure of the stereotype “the first months of a mother with a new baby is the happiest time in life”, the habit of “self-diagnosis” using the Internet (an endless search on Google for medical symptoms can just lead to a real disorder - cyberchondria) and a constant stream of news about all sorts of terrible things that could happen to your child.
Those who already suffered from anxiety disorders not related to motherhood are at higher risk of postpartum anxiety. Cultural factors also play a role: the colossal pressure of the stereotype “the first months of a mother with a new baby is the happiest time in life”, the habit of “self-diagnosis” using the Internet (an endless search on Google for medical symptoms can just lead to a real disorder - cyberchondria) and a constant stream of news about all sorts of terrible things that could happen to your child.
Popular
But anxiety can be treated, says Jonathan Abramovitz, professor of psychology and neuroscience at the University of North Carolina at Chapel Hill. “This is not due to dysfunction of the brain or neurotransmitters,” he says. - Anxiety is not a disease caused by physiological disorders or hormonal imbalances, such as postpartum depression. It's a psychological problem."
If you suspect that this is your diagnosis, try to analyze your behavior, not moods - they are too changeable.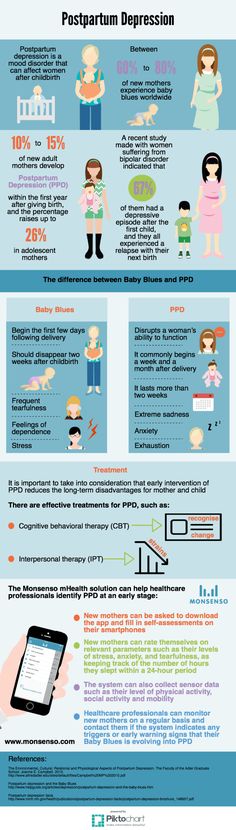 Birndorf likes to ask mothers if they can rest while someone else looks after the sleeping baby. “If the mother says no, then she needs treatment,” she explains. Recovery will require at least one or more of this list: more self-care, behavioral therapy, social support (such as a hotline), and possibly antidepressants, which should first be discussed in detail with a doctor. especially if you are breastfeeding. With the permission of the doctor Dean Blanchard began to take antidepressants, and the experience gradually dissipated. Soon, her pediatric clinic began testing mothers for postpartum anxiety. “After I got the help I needed, I began to enjoy breastfeeding, swaddling, bathing, walking, and even sleep sickness did not bother me,” she says. “Finally, I have become the same as before,” she smiles and corrects herself: “No, not the same - better. Both as a mother and as a doctor. Now I tell patients that they are not alone and that self-care is the best thing a mother can give her child.
Birndorf likes to ask mothers if they can rest while someone else looks after the sleeping baby. “If the mother says no, then she needs treatment,” she explains. Recovery will require at least one or more of this list: more self-care, behavioral therapy, social support (such as a hotline), and possibly antidepressants, which should first be discussed in detail with a doctor. especially if you are breastfeeding. With the permission of the doctor Dean Blanchard began to take antidepressants, and the experience gradually dissipated. Soon, her pediatric clinic began testing mothers for postpartum anxiety. “After I got the help I needed, I began to enjoy breastfeeding, swaddling, bathing, walking, and even sleep sickness did not bother me,” she says. “Finally, I have become the same as before,” she smiles and corrects herself: “No, not the same - better. Both as a mother and as a doctor. Now I tell patients that they are not alone and that self-care is the best thing a mother can give her child. ”
”
Popular
Subscribe and become one step closer to fashion professionals.
Postpartum depression
Page 2 of 7
At least one in 10 mothers suffer from postpartum depression. It is one of the most frequent postpartum complications and occurs in 10-13% of women in labor. As a rule, in such cases it is not always possible to make a correct diagnosis, because mothers are reluctant to seek medical help. Psychotic states in the postpartum period occur in no more than 0.1-0.3% of cases. That is, out of every thousand women who give birth, from 1 to 3 suffer from an even more severe form of depression - postpartum psychosis, in which a woman develops delusions or hallucinations, often accompanied by an obsession with harming herself or the child. The psychotic state significantly impairs the woman's ability to function naturally in family and social life, and also poses a significant risk of committing a suicide attempt. In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
Most often, depression appears 30-35 days after birth and in some cases can last up to 1.5-2 years. However, in most cases, a depressive episode ends spontaneously safely 3-6 months after birth. Symptoms of postpartum depression meet the diagnostic criteria for depressive disorder. The patient has a deterioration in mood, a decrease in energy, activity, the ability to rejoice, have fun, a decrease in interests and difficulty in long-term concentration of attention. Severe fatigue is common, even after minimal effort. As a rule, sleep is disturbed and appetite worsens. Self-esteem and self-confidence are almost always reduced, even in mild forms of the disease. Often there are thoughts of one's own guilt and worthlessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.
Often there are thoughts of one's own guilt and worthlessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.
In most cases, postpartum depression remains unrecognized in the initial period. The most typical example is the prevailing idea of the "natural whims" or character flaws of a woman in labor who turns to her relatives for help instead of actively caring for the child. Loss of initiative and energy or fear of being judged and discussed by others often prevents a woman from seeking medical help. However, even when contacting a doctor, the disease often remains unrecognized, since some doctors tend to consider this condition as a temporary and natural reaction to the stress that childbirth is, especially for primiparas.