Therapy progress notes
How to Write Therapy Progress Notes (with Examples)
Article
Published Apr 13, 2022
Table of Contents
1.What are mental health progress notes?2.How to write therapy progress notes3.What should be included in a progress note?4.Sample therapy progress note5.What are some of the different mental health progress note types?6.Are progress notes the same thing as psychotherapy notes?7.How to use therapy progress notes with your EHRThere is no one size fits all method to completing progress notes, and they can be written in a number of ways. As you get to know your clients and their therapeutic needs, you’ll figure out the best method for your practice. But to start, here’s a breakdown of how to write therapy progress notes, and what to include in yours.
What are mental health progress notes?
Mental health progress notes are what clinicians use to document the details of every session, focusing on the client’s condition coming in, as well as what transpired during the clinician’s interaction with the client. Clinicians have a legal and ethical responsibility to document each treatment episode as part of the client’s official medical record. These notes describe any notable symptoms or other relevant factors in the client’s presentation, changes since their last visit, their response to treatment recommendations, and interventions related to their goals, as well as assessment of client risk.
How to write therapy progress notes
There are a lot of different ways you can write progress notes for therapy. Many clinicians find it ideal to utilize electronic health record systems in order to speed up the process by utilizing clickable checkboxes and fillable templates that hit all of the important elements required for documentation. Electronic notes also have the added benefit of being consistently legible, which is a major requirement of progress notes.
Others prefer to have a physical paper note, as they can complete some of it in-session. However, it is usually not possible to completely and thoroughly finish a progress note while also being attentive to your client, in addition to risking illegible handwriting.
However, it is usually not possible to completely and thoroughly finish a progress note while also being attentive to your client, in addition to risking illegible handwriting.
A hybrid approach might involve some handwritten notes to assist you in remembering some key details when you complete an electronic note later. This approach can also consist of incorporating a paper template form, containing sections for relevant information or checklists, that you can scan and attach to an electronic note. The hybrid approach may be particularly helpful for newer clinicians, in order to provide the added benefit of guiding your session, such as remembering to hit on or assess certain areas, so you’re not kicking yourself later for not asking a key question.
To help you learn how to write these notes, we’ve created a therapy progress note template, which you can customize as you need and put to use right away in your practice.
Download our free sample therapy progress note template!
What should be included in therapy progress notes?
So, how do you write a therapy progress note? The elements that need to be included in your progress notes will vary somewhat depending on requirements of your state, licensing board, professional organization, ethical code, the organization where you work, the modality you are using, and insurance company or third party contracts if applicable.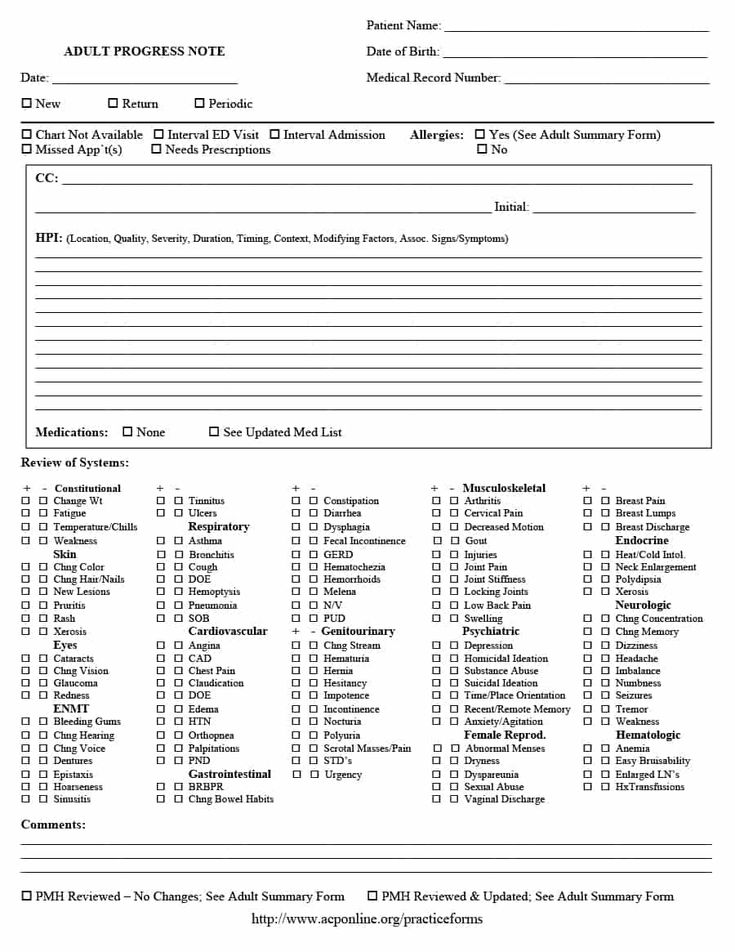 Each of these may require more specific information, so always check through each of these to add to your own format or templates.
Each of these may require more specific information, so always check through each of these to add to your own format or templates.
In general, all progress notes should include the following:
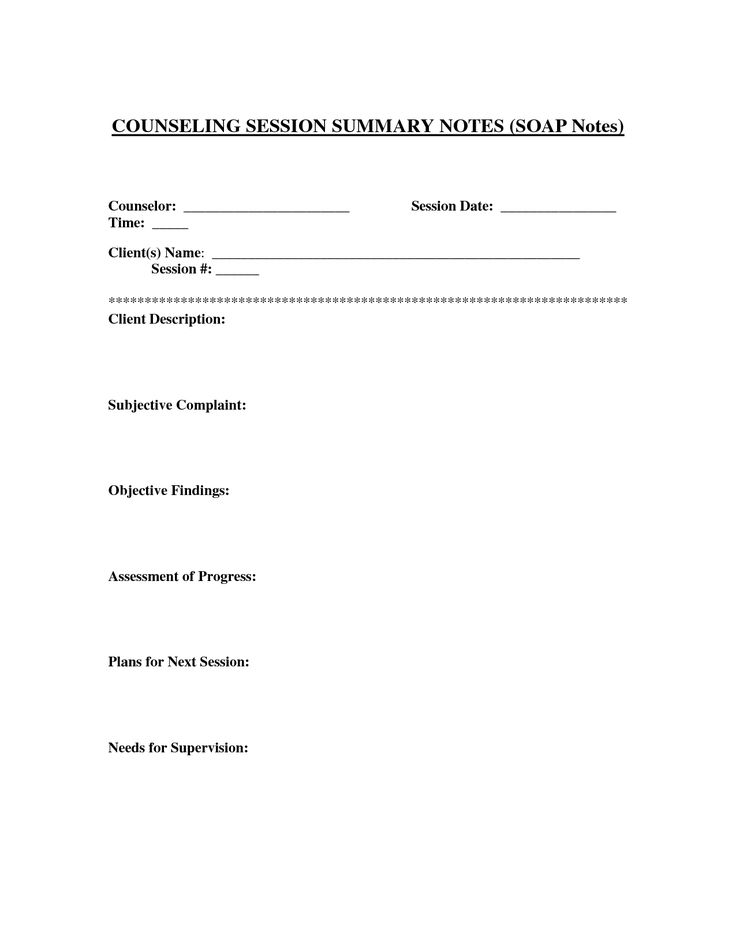
Demographic/identifying information
- Client’s name, and an identifier like date of birth
- Date of the session, and exact start and end time of the session
- Clinician’s name, and a handwritten or electronic signature
- For telehealth sessions, the location of the session/client
Description of your client’s behavior
- A description of the client’s presentation (their mood, affect, appearance, and behavior in the session), as well as relevant symptoms that are reported by the client and observed by the clinician
- A diagnosis
- A safety assessment.
 While some clinicians do this as needed if a client reports suicidal ideation or self-harm behavior, if you work with high risk clients you may want to document that you checked on this in each session, and that a client denied these, as a safeguard.
While some clinicians do this as needed if a client reports suicidal ideation or self-harm behavior, if you work with high risk clients you may want to document that you checked on this in each session, and that a client denied these, as a safeguard. - Any additions or changes to medications that may impact the client’s mood or symptoms, or a statement about medication compliance or noncompliance for any client who is already taking medications
Treatment plans going forward
- What you did as a clinician (treatment modalities used, what you recommended, what you asked, what you prompted the client to consider, coping skills you taught, handouts or assignments you provided)
- The client’s response to interventions listed above
- The client’s progress toward established goals, in a more specific and short-term format than in their treatment plan, and whether any changes need to be made to the treatment plan
- The plan for the client following the session (what the client will work on, what will be discussed in the next session, when the next session is scheduled)
In addition to these elements, it’s important to keep in mind that progress notes should be primarily objective in nature, and completed with maintaining a client’s privacy in mind.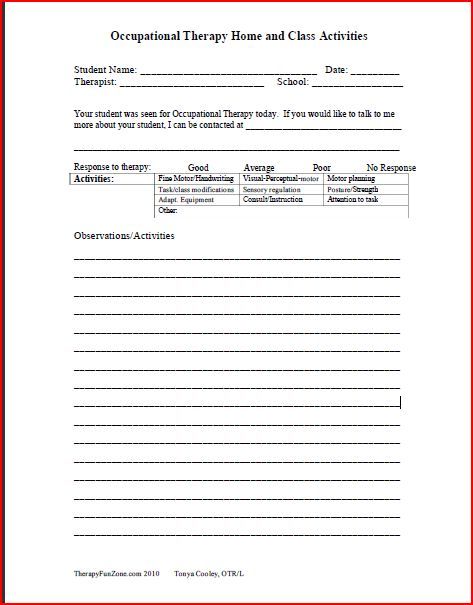 Progress notes are part of the documentation that could be requested by your client, or subpoenaed and read out loud in a court of law. Does a jury, a client’s soon to be ex-husband, need to hear the contents of your client’s sexual dream, the identifying information of another individual in their life, or your personal opinion about the childhood root of your client’s issue? Most likely not.
Progress notes are part of the documentation that could be requested by your client, or subpoenaed and read out loud in a court of law. Does a jury, a client’s soon to be ex-husband, need to hear the contents of your client’s sexual dream, the identifying information of another individual in their life, or your personal opinion about the childhood root of your client’s issue? Most likely not.
Client progress note example
Here’s an example of how some of these elements might be written in your progress note:
Clinician Name
Agency Name
1234 Office Address
Wherever, UR 12345
Client Name: Johnny Appleseed
Client DOB: 01/02/3456
Diagnosis: F 33.0, Major Depressive Disorder, Recurrent, Mild
Date: 03/04/5678
Start Time: 07:03 pm
End Time: 07:58 pm
Client’s Subjective Concerns/Chief Complaint: “I’m starting to feel more depressed.” Client noted concerns about his mood, endorsing depressed mood, lethargy, insomnia, loss of energy and motivation, and urges to isolate from his romantic partner.
Clinical Observations: Client appeared disheveled, which is unusual for him, and a marked change since last session. Client sat in a hunched position upon the beginning of the session, and appeared tired, with slowed movements and dysthymic mood. He was attentive and cooperative, and had congruent and appropriate affect. Client denies suicidal ideation.
Issues and Stressors Discussed/Session Description: Client discussed experiencing increased difficulty with depressive symptoms beginning last week, following an argument with his romantic partner. Client reviewed the details of the argument, and stated that it occurred late on Tuesday night, causing him to get only 4 hours of sleep. Client has continued to attend work, and reports compliance with prescribed medication. Client stated that the argument is now resolved, and he has been communicating with his partner, though he has had thoughts such as “What’s the point? He doesn’t understand me.” Upon further exploration, this writer learned that, since Tuesday night, the client has been spending more time than usual on his mobile device at night, continuing to get a less than ideal amount of sleep (5-6 hours), and negatively impacting his energy level and mood. While the client did roll his eyes upon this writer bringing up his mobile phone use, he then laughed and stated, “I know, I know, I’m doing it to myself.”
While the client did roll his eyes upon this writer bringing up his mobile phone use, he then laughed and stated, “I know, I know, I’m doing it to myself.”
Interventions/Methods Provided: Discussion of symptoms, supportive counseling, identification and exploration of emotions, Psychoeducation: Dialectical Behavior Therapy Emotion Regulation skills, discussion of vulnerabilities, ABC PLEASE handout provided. Review of client’s safety plan.
Assessment: While client’s endorsed symptoms and presentation are in keeping with depression, but are part of a sudden change prompted by an argument and reduction in sleep, it is likely that client’s emotional reaction to the argument with his partner and subsequent poor sleep hygiene are responsible for this sudden shift in mood and appearance. Client does not appear to be at risk of suicide at this time, discussing the importance of being available for his younger brother and pet dog, and is agreeable to following the steps outlined in his safety plan if symptoms increase or ideation occurs.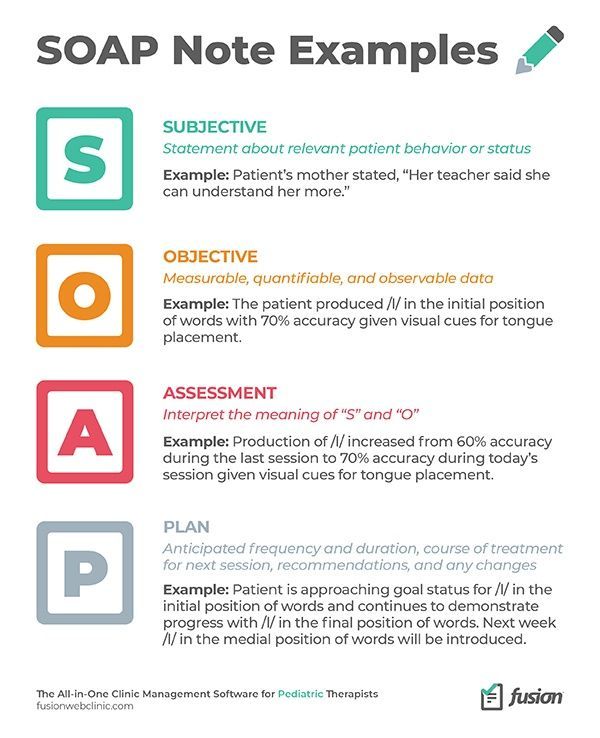 However, the client is at risk for worsening depression if he is unable to prevent further decompensation.
However, the client is at risk for worsening depression if he is unable to prevent further decompensation.
Plan: Client has committed to resuming a sleep schedule, beginning tonight, and agreed to turn off his smartphone an hour before the established 11PM bedtime. Client will monitor his symptoms, and reach out to this writer if symptoms increase. If symptoms worsen by the next session, this writer may encourage the client to outreach his psychiatrist for an earlier appointment, as their next follow up is not scheduled for another month.
Next Appointment: 03/11/5678
Clinician Signature: ____________________________________
Clinician Printed Name, LCSW
What are some of the different mental health progress note types?
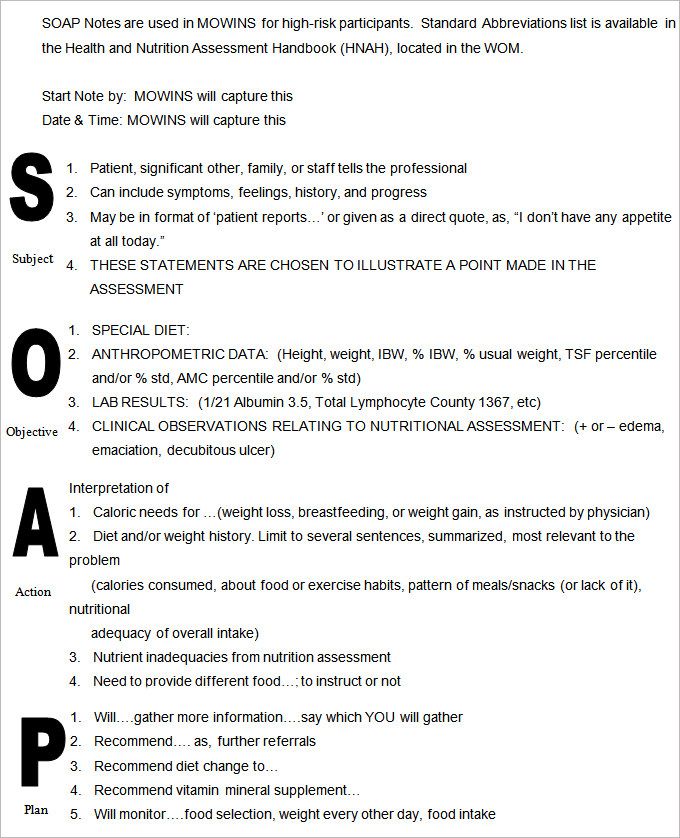
There are several widely used formats for progress notes that can provide a template for making your note-keeping more efficient, while including all of the necessary key points:
- DAP (Description, Assessment, Plan)
- BIRP (Behavior, Intervention, Response, Plan)
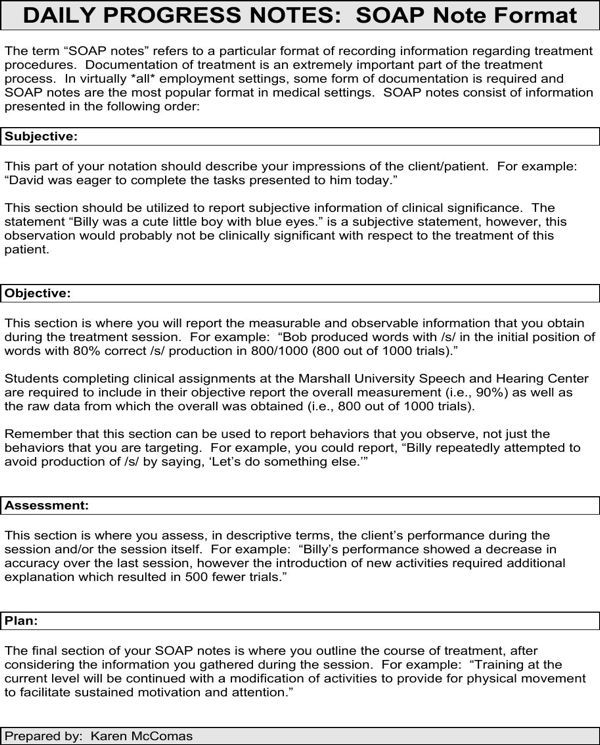
- SOAP (Subjective, Objective, Assessment, Plan)
Each kind of note template is similar, but there are some differences that might lead you to choose one format over another. For example, since SOAP notes were created for healthcare settings, some may find that they prefer DAP notes, which allow for a bit more subjectivity around the elements of mental health that are less black and white. Conversely, some clinicians can easily veer off-course with an open-ended description section like in the DAP note, preferring the more concrete objective or behavioral categories in the SOAP or BIRP notes.
For example, since SOAP notes were created for healthcare settings, some may find that they prefer DAP notes, which allow for a bit more subjectivity around the elements of mental health that are less black and white. Conversely, some clinicians can easily veer off-course with an open-ended description section like in the DAP note, preferring the more concrete objective or behavioral categories in the SOAP or BIRP notes.
Both SOAP and DAP notes contain an assessment section, unlike BIRP notes, which focus on the response to the in-session interventions, but not the overall condition of the client. Since this type of assessment may be required, particularly for health insurance companies or if you are in a setting that requires you to justify the need for more treatment on a regular basis, many clinicians opt for the SOAP or DAP formats.
Ultimately, you might consider your strengths and difficulties as a note taker. If your notes tend to be lengthy without guidance, or you easily find yourself getting lost in the details and including too much personal client information or subjective opinion, choose a format that helps you to be more succinct, like SOAP or DAP notes. If these formats cause you to feel boxed in, you might prefer to create your own template that includes all of the factors required, without having to fit them into the categories of any of these formats.
If these formats cause you to feel boxed in, you might prefer to create your own template that includes all of the factors required, without having to fit them into the categories of any of these formats.
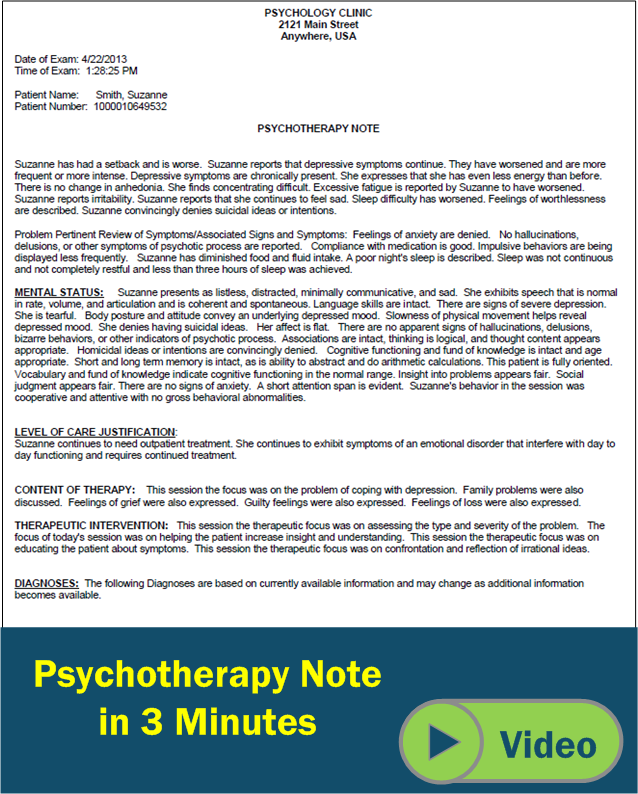
Are progress notes the same thing as psychotherapy notes?
You may have also heard about psychotherapy notes, and it’s important to note that these aren’t the same as progress notes. Psychotherapy notes are private notes, kept separate from the client’s medical record or chart, that are for the clinician’s eyes only. Psychotherapy notes cannot be subpoenaed and aren’t part of the record that gets shared with the client or other providers. This option is helpful to keep in mind when you want to remember some personal details the client shared, a direction you’re thinking of moving in treatment, or some internal experiencing to discuss with your clinical supervisor—but the information would be inappropriate to place in the client’s progress note.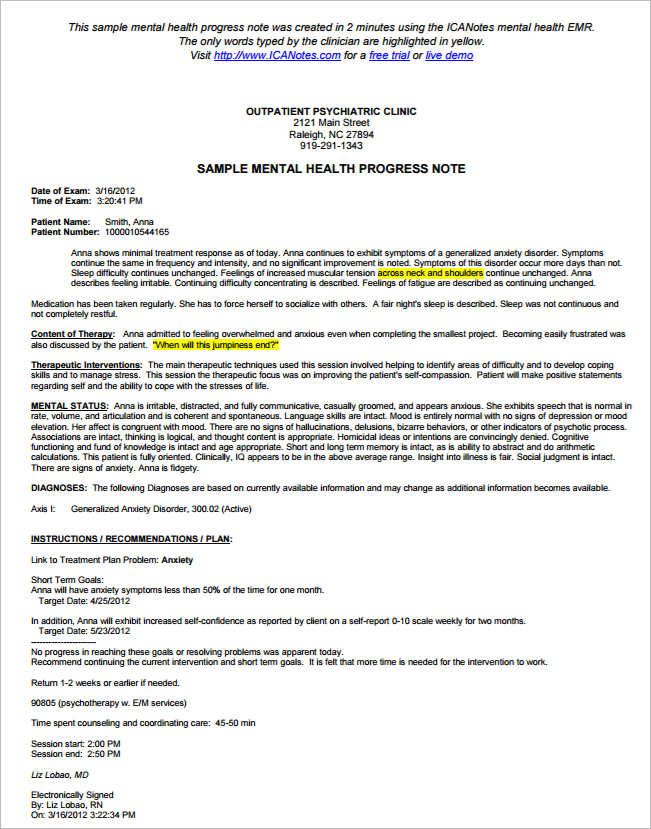
For those clinicians that want a way to document a lot of detail, and have recognized they are likely sharing too much in the description section of their DAP progress note, psychotherapy notes are a great solution as an addendum to the progress note.
How to use therapy progress notes with your EHR
There are several ways you can incorporate digital notes with your EHR. You can either upload a template, or follow the structure within your software. A top-rated EHR will have a dedicated section for notes and documentation, as well as easy-to-use templates that are built right into the platform.
If you’re looking for a fully integrated EHR that works for behavioral health practitioners like you, try SimplePractice for a free 30 days. SimplePractice makes it easy to streamline your notes and documentation, while also improving your clients’ experience.
Sign up for emails from SimplePractice
Build the best practice you can.
Our resources to help you & your practice take the next step.
Article
Benefits of an EHR: How Software Can Support Private Practice
Article
What is an EHR System?
Article
Self-Care Worksheets: 3 Tools to Help Your Clients
Article
5 Free Coping Skills Worksheets
Article
How to Build Self-Esteem: 5 Free Self-Esteem Worksheets
Article
Child Anger Management Worksheets (Free Download)
Article
Cognitive Behavioral Therapy (CBT) Worksheets
Article
5 Anxiety Worksheets (Free Download)
Article
Group Therapy Activities (with Examples)
Article
How to Write Therapy Progress Notes (with Examples)
Manage and grow your private practice, all in one place.
Free 30-day trial. No contracts. Change anytime. Tax deductible.
Start For Free- List CheckmarkNo credit card needed
- List CheckmarkAccess all features
- List CheckmarkHIPAA-compliant
How to Write DAP Notes (with Examples)
Article
Published Feb 16, 2022
Table of Contents
1. What is a DAP note?2.What’s the difference between SOAP notes and DAP notes?3.How long should a DAP note be?4.How to write a DAP note5.DAP notes therapy example6.How to use DAP notes with your EHR
What is a DAP note?2.What’s the difference between SOAP notes and DAP notes?3.How long should a DAP note be?4.How to write a DAP note5.DAP notes therapy example6.How to use DAP notes with your EHRThere are many different formats and structures available for psychotherapy and counseling progress notes. One of those formats is DAP notes. Bear in mind that the requirements for documentation vary by clinician, clientele, and a number of other factors. Simply put, there’s no single right way to do documentation, but your documentation format and content should be aligned to your specific practice and needs.
What is a DAP note?
A DAP note is one of the most popular and current ways to write a psychotherapy or progress note. So what is a DAP note? DAP stands for Data, Assessment, and Plan, and is used by counselors and psychotherapists everywhere. DAP notes provide a standardized way to document your sessions and follow the D-A-P format every time.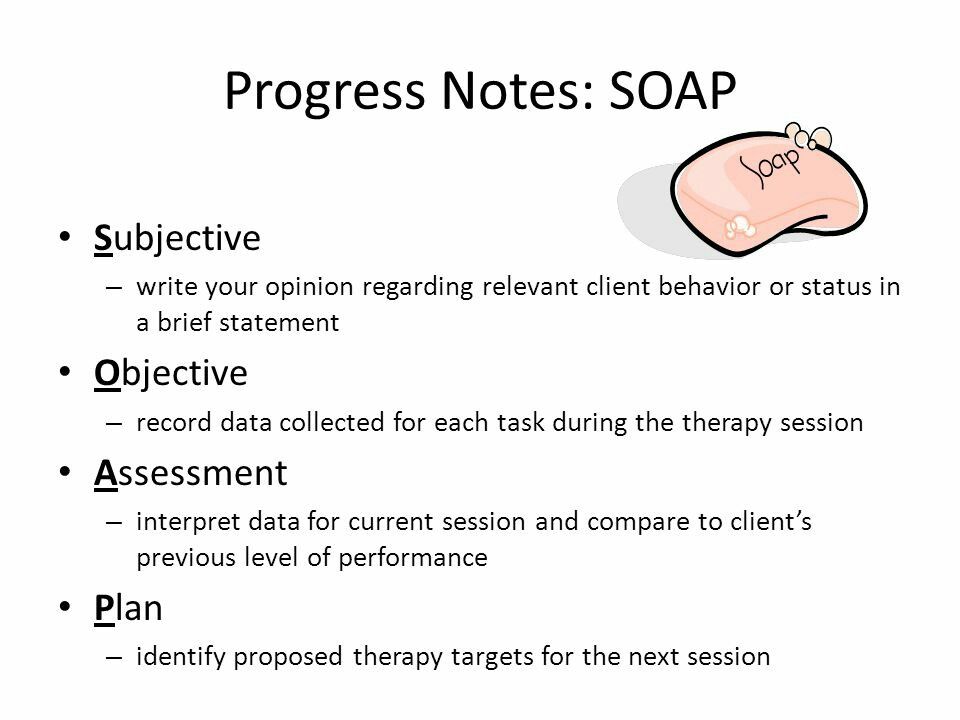 This note structure also helps clinicians develop documentation that is both brief and complete. Done well, each section should make good logical sense based on the information in previous sections.
This note structure also helps clinicians develop documentation that is both brief and complete. Done well, each section should make good logical sense based on the information in previous sections.
Download our Free DAP Note template!
What’s the difference between SOAP notes and DAP notes?
The main difference between SOAP notes and DAP notes is the last section. If you’re familiar with the SOAP note structure, DAP notes are very similar. DAP notes take the Subjective and Objective sections of a SOAP note and combine them into a single section: data.
How long should a DAP note be?
There’s no rule for exactly how long DAP notes should be. The note length depends on a lot of factors, and it’ll vary based on your individual client and the treatment plan you come up with together.
As a guideline though, DAP notes can be shorter when the client is making routine, expected progress.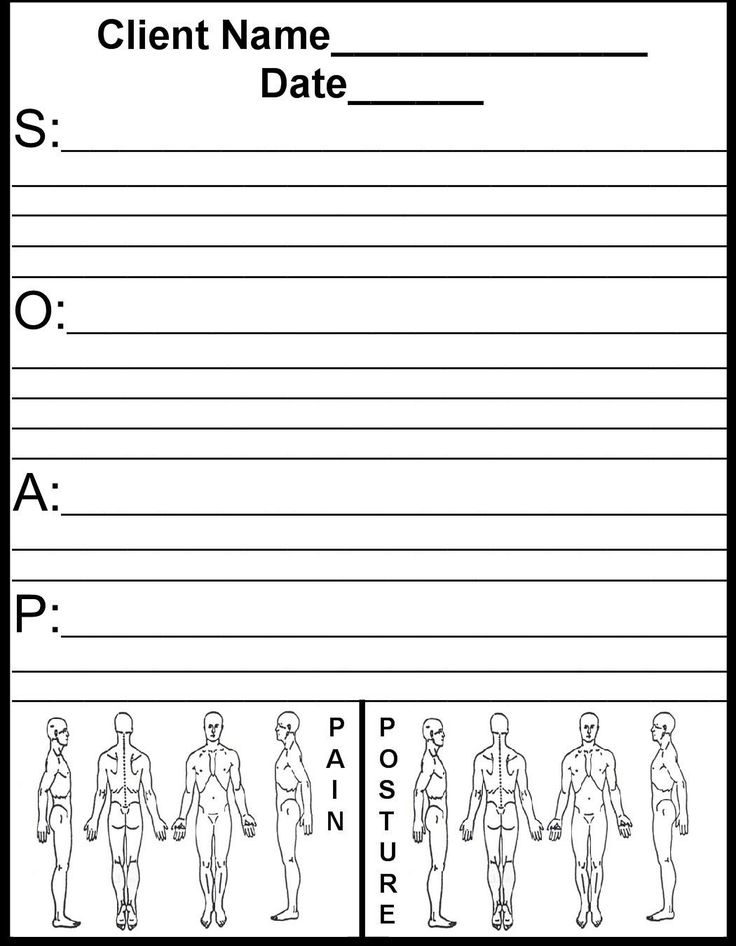 This can be toward treatment goals, if they present low risk for suicide or other violence, and if there are no changes to their diagnosis or treatment. Longer notes typically are the result of a client not making expected progress, if their symptoms change, if they present heightened risk, or when changes appear necessary to the diagnosis or treatment plan.
This can be toward treatment goals, if they present low risk for suicide or other violence, and if there are no changes to their diagnosis or treatment. Longer notes typically are the result of a client not making expected progress, if their symptoms change, if they present heightened risk, or when changes appear necessary to the diagnosis or treatment plan.
How to write a DAP note
When you write a DAP note, it will always follow the same format no matter who your client is. However, the content that’s included in each section of the DAP note can vary based on a number of factors. We’ll go through what each section of a DAP note should include, and how they would be applied with an example.
D – Data
This section is where you add data from your counseling or psychotherapy session. This could include:
- Reason for the visit
- Client presentation/appearance
- Client mental status
- Client reports of current symptoms or important events since the last session
- Results of screening or other measures
- Interventions applied in session
- Client responses to interventions applied
It’s important to note that this section should be limited to information, not interpretation.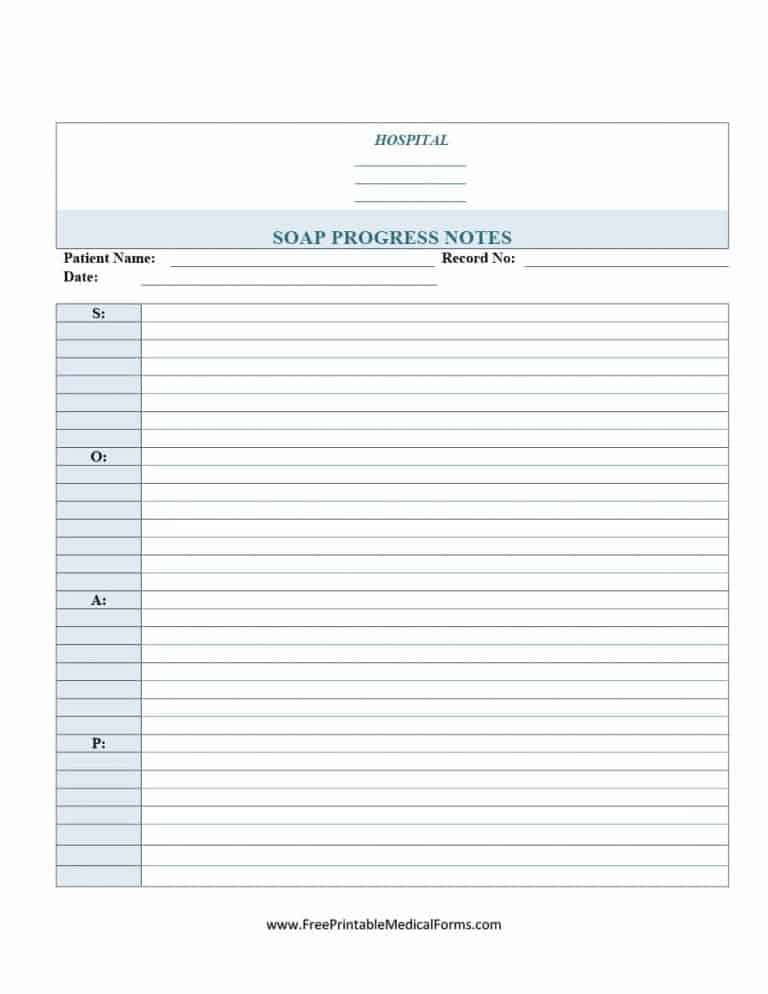 Speak factually, and if appropriate, use direct quotes.
Speak factually, and if appropriate, use direct quotes.
A – Assessment
This section is where you take the data from the first section and apply your clinical judgment to it. This could include:
- How the client is progressing
- How the client’s status relates to their treatment goals
- How the client responded
- Changes to the client’s diagnosis
Every note typically includes some evaluation of risk in this section, to ensure that potential indicators of suicide or other forms of risk have been assessed and the clinician has responded appropriately.
All conclusions in this section should be clearly supported by the data in the first part of the note. In fact, when the Data section is done well, the Assessment section will read to clinicians as obvious conclusions based on that Data.
P – Plan
Given the observed data and your interpretation of it, where does treatment go from here? This section could include:
- The date, time, and location of the next scheduled session
- Homework assigned to the client
- Referrals provided to the client
- Consultation or other third-party contact planned by the clinician
- Changes to the treatment plan based on the client’s progress so far
- Additional steps related to the treatment that the client or clinician is expected to take
Related How to Pick a Therapy Notes and Billing Software
DAP notes therapy example
We’ve created DAP note example to help give each section more context.
DAP note example for depression
D- Data
Client reported on time for a third session of CBT to address symptoms of depression. Client was well-groomed and fully oriented. The client reported feeling “a little bit better here and there” since the last session, and noted that they have had an easier time getting to sleep at night. Client also noted recent financial stressors. The client scored a 14 on the BDI-II, scoring in the moderate range. In session, challenged the client’s automatic negative thoughts around their work performance and relationship functioning. Client reported feeling increasingly agitated but understanding that this was “part of the work.” When offered the opportunity to stop the intervention, the client asked instead to continue. Client neither displayed nor reported any other current risk factors for suicide or violence.
A – Assessment
Client reports of reduced sleep symptoms and improved mood, and their improved score on the BDI-II relative to initial assessment, suggest improvement toward treatment goal of reducing depressive symptoms below diagnostic threshold.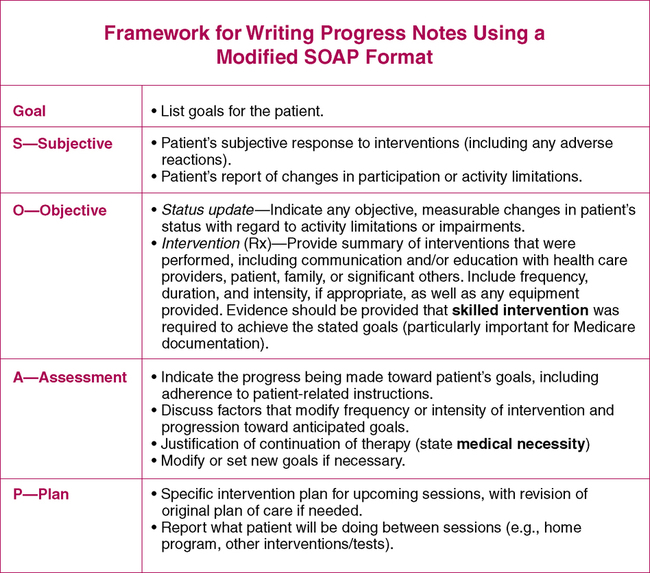 Client responded well overall to interventions, and appears to be well-motivated to continue. Client appears to demonstrate low risk level for suicide or violence; the safety plan established with the client at the first session remains in effect.
Client responded well overall to interventions, and appears to be well-motivated to continue. Client appears to demonstrate low risk level for suicide or violence; the safety plan established with the client at the first session remains in effect.
P – Plan
Our next session is scheduled for Thursday, March 17 at 10:00 am via telehealth. Assigned the client a thought record chart to specifically log instances of automatic negative thoughts regarding relationship functioning. Provided the client with referrals to three potential financial advisors to address reported recent financial stressors. No changes indicated to the treatment plan. Client to follow steps of established safety plan if symptoms significantly worsen prior to the next scheduled session.
How to use DAP notes with your EHR
Now that you have an understanding of the question “what is a dap note,” it’s time to explore how to put them to use in your practice.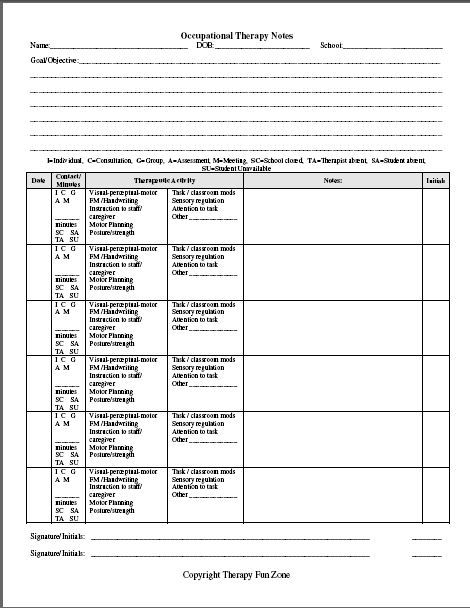 To use DAP notes with your EHR, you can either upload a template, or follow the note structure within your software. A top-rated EHR will have a dedicated section for notes and documentation, as well as easy-to-use templates that are built right into the platform.
To use DAP notes with your EHR, you can either upload a template, or follow the note structure within your software. A top-rated EHR will have a dedicated section for notes and documentation, as well as easy-to-use templates that are built right into the platform.
If you’re looking for a fully integrated EHR that works for behavioral health practitioners like you, try SimplePractice for a free 30 days. SimplePractice makes it easy to streamline your notes and documentation, while also improving your clients’ experience.
Sign up for emails from SimplePractice
Build the best practice you can.
Our resources to help you & your practice take the next step.
Article
Benefits of an EHR: How Software Can Support Private Practice
Article
What is an EHR System?
Article
Self-Care Worksheets: 3 Tools to Help Your Clients
Article
5 Free Coping Skills Worksheets
Article
How to Build Self-Esteem: 5 Free Self-Esteem Worksheets
Article
Child Anger Management Worksheets (Free Download)
Article
Cognitive Behavioral Therapy (CBT) Worksheets
Article
5 Anxiety Worksheets (Free Download)
Article
Group Therapy Activities (with Examples)
Article
How to Write Therapy Progress Notes (with Examples)
Manage and grow your private practice, all in one place.
Free 30-day trial. No contracts. Change anytime. Tax deductible.
Start For Free- List CheckmarkNo credit card needed
- List CheckmarkAccess all features
- List CheckmarkHIPAA-compliant
Archive. About me and the channel “Notes of the Evil…” | by Elizaveta Musatova
Archive. About me and the channel “Notes of the Evil…” | by Elizaveta Musatova | MediumAbout me and the channel “Notes of an Evil Therapist”
Why did I start this channel
Why is the therapist evil?
A
“And if he makes fun/shame/scolds me”: why we are afraid to go to a psychologist — and absolutely in vain0003
B
Visible and invisible work in the field of psychological assistance
General harmony: why psychologists do not teach how to achieve it
You have decided to change a psychotherapist: what can be done before you make this decision
D
Gender and psychotherapy: to choose a man or a woman?
Gender scenarios: where they come from, how they affect our lives, and what to do now, when everything is messed up
Speaking out loud to destroy power over yourself
Limits in therapy and beyond
Y
Two types of knowledge in psychotherapy
Directive and non-directive approaches in psychotherapy
Depression: how to recognize it and what to do with it
Acceptable and unacceptable in psychotherapy: how to find boundaries 9003
C
Therapist's notes: is it necessary to take them during sessions?
Inquiry in psychorapy: with what do we go to a specialist?
What do we pay a therapist for?
What do we pay a therapist for? Postscript
I
Internalization of the therapist
Artificial intelligence in psychotherapy: how advanced technologies continue to change our lives
C
The therapist's office as a reflection of his personality
Is every therapist a wounded healer?
How to choose “your” therapist and understand that he can be trusted.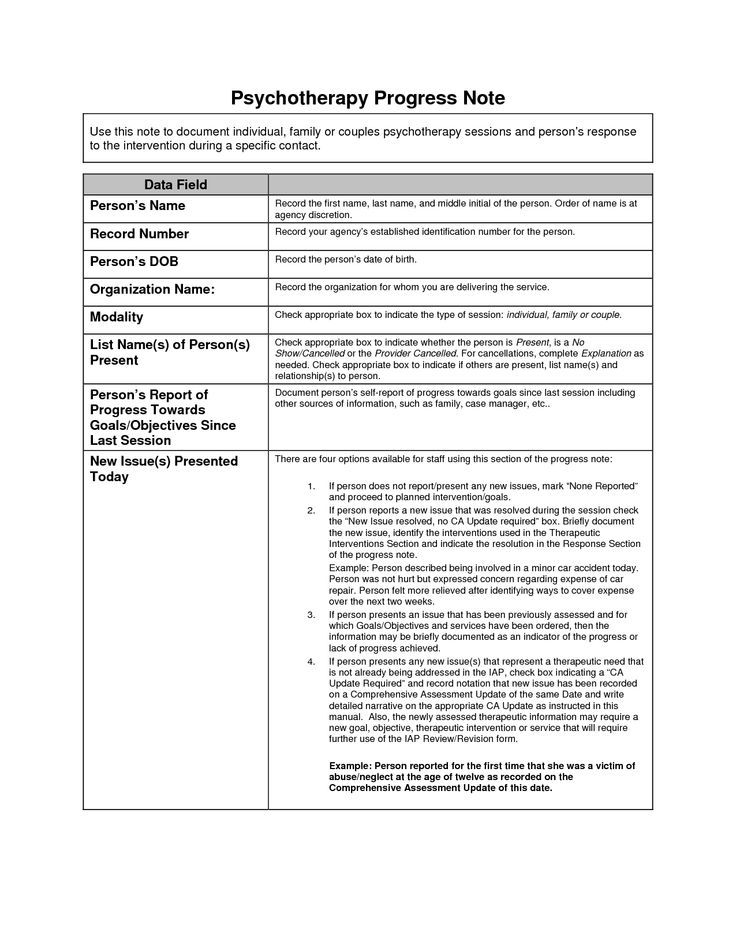 Which experts should not be trusted? Are psychologists and psychotherapists the same thing? Myths about psychotherapy
Which experts should not be trusted? Are psychologists and psychotherapists the same thing? Myths about psychotherapy
How the client's request changes during therapy
How to maintain therapy during a pandemic?
When it gets worse in psychotherapy, and this is normal
Containers in psychotherapy
Crutch or beacon? What is a psychologist for a client
Coaching and psychotherapy: similarities and differences
Brief psychological dictionary
What does the devaluation of feelings lead to: “It seems that everything is fine with me, but ...”
L
Personal recommendations: why they are not always help in choosing a therapist
In person or remotely: what is the best way to work with a therapist?
M
Metaphor in therapy: when working with a psychologist is like going down into a coal mine
The myth of absolute harmony: why you should not believe advertising
Can a psychologist forbid something to a client?
Is it possible to be a harmonious person without getting rid of the “inner devils”?
Can you trust reviews of a psychologist?
N
Hope in psychotherapy
Narrative approach and classical psychoanalysis
Getting started with a psychologist: not “what to do?” but “what is happening?”
Non-ideal parents: six types of parent-child relationships that cause trauma
Non-violent relationships with oneself: how to learn it
Non-obvious results of psychotherapy
About
About the utopia of the norm working with him can help the client
Communication with loved ones is not a substitute for psychotherapy - and vice versa
On the importance of inner work between sessions
On “fireproof sums” in psychotherapy
Organic factors of depression
On the role of dignity in therapy
Reviews of psychotherapy: can they be trusted
Relationship between client and therapist.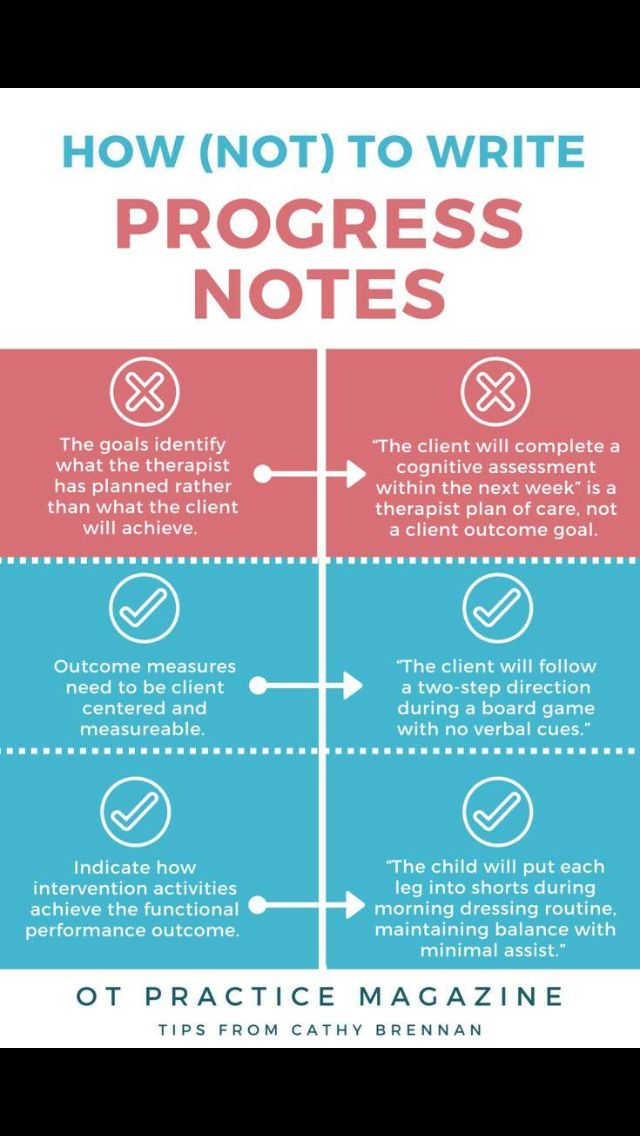 Live broadcast recording
Live broadcast recording
“Tangible results in a month”, or why you should not approach therapy from the position of an effective manager
P
First session with a therapist: what to tell about yourself
First session: what it is like and what can be expected from it
Transference in psychotherapy
Let's talk at the threshold: why do we say the most important things on the way to the door
Understanding what the problem is means coping with it? And why not?
Popular myths about psychotherapy
Psychologist's similar life experience: how important is it?
Why you shouldn't turn psychotherapy into a religion
Why a therapist won't "fix" you
Why the therapist is silent during the session
Why the therapist does not give advice
Psychologist's professional identity: different approaches to therapy
Mental health in the modern world
Psychological care in Serbia (compared to Russia)
Psychological research: what they say about psychotherapy scientists?
Psychosomatics: answers to frequently asked questions
Psychotherapy and promotion. Why does not happen at the session what is promised in advertising
Why does not happen at the session what is promised in advertising
Psychotherapy: what, why and for whom?
Is psychotherapy a service or not? And why work on insurance can be ineffective
R
Advertising psychological help in the Russian online space and what is wrong with it
С
Therapist himself: is it possible to heal yourself without going to a psychologist?
The most frequent requests for therapy
Separation. What is it and how to survive it if you are already an adult and want to finally live your life
How long does it take to visit a psychologist to solve a problem
Resistance in therapy: what it is and how to work with it
A remedy for chaos, or how therapy will not make the world consistent
Statistics: how millennials approach psychotherapy differs and baby boomers
Suicidal clients: how to work with them
T
So how many sessions does it take to solve a problem?
Therapy and goal setting: how working with a psychologist helps you understand which of your life goals are really yours
Therapy or toxic crap: how to tell the difference?
Is therapy science or magic?
Three Questions to Ask Your Therapist
F
The Philosophy of Nonviolent Communication
Finance and Therapy Part 1: Financial Boundaries in the Psychologist's Office
Finance and Therapy Part 2: Why Money Is More Than a Medium of Exchange
Finance and Therapy Part 3: Pricing
Finance and Therapy Part 4: Resistance and Money
Finance and therapy, part 5: when the cost of the session can change
X
I want to find a psychologist.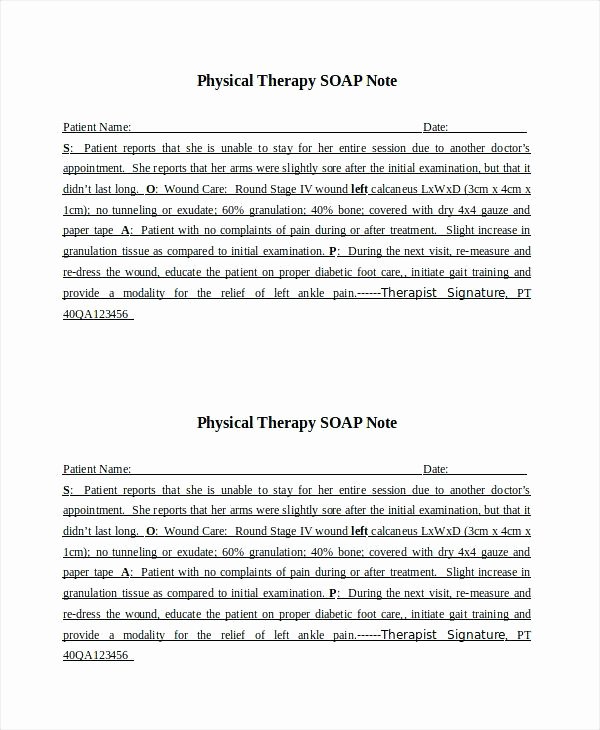 Where to begin?
Where to begin?
P
What to expect and what not to expect from psychotherapy
Man is always more than a problem
Honesty in psychotherapy
How can a therapist help a client in times of crisis?
Feeling of inclusion in the world: what it is and how it manifests itself
Feeling of separation from others: why do we think that our problems are unique?
What happens if you yell at a therapist?
What makes us human?
What is mental health and what factors affect it
E
Is it ethical to give gifts to your therapist? What could be behind this?
Effectiveness of psychotherapy in numbers
Language and cultural differences in psychotherapy
Love podcasts or audiobooks? Learn on the go with our new app.
Try Knowable
Get the Medium app
Elizaveta Musatova
Status
Careers
Knowable
THIRD AND SUBSEQUENT SESSIONS.
 Cognitive therapy. Complete guide
Cognitive therapy. Complete guide Starting from the third, the sessions are held in the same format. The content varies depending on the patient's complaints, concerns and goals, as well as the goals of the therapist. In this section, we will touch on the course of therapy throughout the sessions. More information about treatment planning can be found in chapter 16.
As we have already mentioned, in the beginning the therapist takes over setting the agenda, actively assisting the patient in identifying and evaluating automatic thoughts, assigning homework and debriefing the session. Over time, responsibility gradually shifts to the patient. By the end of therapy, most of the agenda is set by the patient. He also uses tools such as the Dysfunctional Thought Worksheet (DDM) to assess his own thinking (see Chapter 9), sets a homework assignment for himself and sums up the final conclusion of the therapy session.
During the course of therapy, the focus shifts from automatic thoughts to an exploration of the patient's ingrained beliefs (see chapters 10 and 11).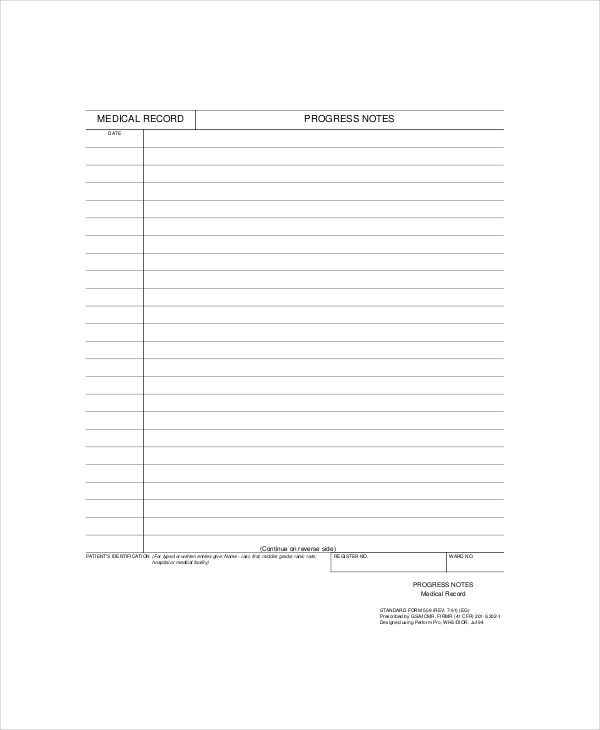 There are also changes in the relative emphasis of behavioral
There are also changes in the relative emphasis of behavioral
aspects, although they are less predictable. Patients with depression should be encouraged from the start of therapy to plan their activities and lead a more active lifestyle (see Chapter 12). (Patients suffering from major depression may initially be unable to do cognitive work, so the therapist tries to increase their behavioral activity and refrains from cognitive interventions until the patient's condition improves at least to some extent.) When therapy approaches the final stage , the focus shifts to preparing the patient for the end of treatment and teaching them how to prevent relapse (see Chapter 15).
When planning an individual session, the therapist takes into account the current stage of therapy. As emphasized in chapter 2, he guides the therapy process using the patient's conceptualization. Before the session begins, the therapist enters the items on the agenda on the "Therapy Notes" form (see Figure 4. 3), but is prepared to disregard them if necessary. As the client talks about his mood, how the week went, and sets out agenda items, the therapist mentally formulates a specific goal or goals for the session. For example, in the third session, the therapist's goals are to train Sally to evaluate her automatic thoughts in a structured way and to convince her to continue planning for enjoyable leisure activities. During the fourth session, the therapist discusses with the patient problems with finding a part-time job and teaches how to properly respond to negative automatic thoughts. The therapist constantly seeks to align his goals with the issues proposed by the patient as an agenda. So he teaches her problem solving and cognitive restructuring skills in the context of the situations she brings to therapy. This combination of problem solving and helping the patient respond to his thoughts usually gives both the therapist and the patient sufficient time to consider only one or two issues on the agenda for a given session.
3), but is prepared to disregard them if necessary. As the client talks about his mood, how the week went, and sets out agenda items, the therapist mentally formulates a specific goal or goals for the session. For example, in the third session, the therapist's goals are to train Sally to evaluate her automatic thoughts in a structured way and to convince her to continue planning for enjoyable leisure activities. During the fourth session, the therapist discusses with the patient problems with finding a part-time job and teaches how to properly respond to negative automatic thoughts. The therapist constantly seeks to align his goals with the issues proposed by the patient as an agenda. So he teaches her problem solving and cognitive restructuring skills in the context of the situations she brings to therapy. This combination of problem solving and helping the patient respond to his thoughts usually gives both the therapist and the patient sufficient time to consider only one or two issues on the agenda for a given session.