The pain when will it end
SPY ETF: The Pain Will End In 2023
Dec. 31, 2022 9:00 AM ETSPDR S&P 500 Trust ETF (SPY)ACTV, AFMC, AFSM, AGG, ARKK, AVUV, BAPR, BAUG, BBMC, BFOR, BFTR, BJUL, BKMC, BKSE, BMAR, BMAY, BOCT, BOSS, BOUT, BUFF, BUL, CALF, CATH, CBSE, CSA, CSB, CSD, CSF, CSML, CSTNL, CWS, CZA, DDIV, DEEP, DES, DEUS, DFAS, DGRS, DIA, DIV, DJD, DJI, DON, DSPC, DVLU, DWAS, DWMC, EES, EFIV, EPS, EQAL, ESML, ETHO, EWMC, EZM, FAB, FAD, FDM, FFTY, FLQM, FLQS, FNDA, FNK, FNX, FNY, FOVL, FRTY, FSMD, FTA, FTDS, FYC, FYT, FYX, GLRY, GS, GSSC, HAIL, HIBL, HIBS, HLGE, HOMZ, HSMV, IJH, IJJ, IJK, IJS, IMCB, IMCG, IMCV, IPO, ISCB, ISCG, ISCV, ISMD, IUSS, IVDG, IVE, IVOG, IVOO, IVOV, IVV, IVW, IWC, IWM, IWN, IWO, IWP, IWR, IWS, IYY, JDIV, JHMM, JHSC, JPME, JSMD, JSML, KAPR, KJAN, KJUL, KNG, KOMP, KSCD, LSAT, MDY, MDYG, MDYV, MGMT, MID:IND, MIDE, NAPR, NDX, NJAN, NOBL, NUMG, NUMV, NUSC, NVQ, OMFS, ONEO, ONEQ, ONEV, ONEY, OSCV, OUSM, OVS, PAMC, PAPR, PAUG, PBP, PBSM, PEXL, PEY, PJAN, PJUN, PLTL, PRFZ, PSC, PTMC, PUTW, PWC, PY, QDIV, QMOM, QQC, QQD, QQEW, QQQ, QQQA, QQQE, QQQJ, QQXT, QTEC, QVAL, QVMS, QYLD, QYLG, REGL, RFG, RFV, RNMC, RNSC, ROSC, RPG, RPV, RSP, RVRS, RWJ, RWK, RWL, RYARX, RYJ, RYT, RZG, SCHD, SPX, VFFSX, VFIAX, VFINX, VOO, VTI71 Comments
JR Research
Marketplace
Summary
- With 2022's final trading day done and dusted, we move into 2023 with cautious optimism.
- Strategists have gotten their 2022 EPS target for the S&P 500 spot on. However, they didn't anticipate a valuation compression due to significant macro headwinds.
- Could 2023 be any different as the Fed moves into data-dependency mode? Will Jerome Powell and his FOMC heap more pain on investors?
- SPY's October lows look robust, with its recent pullback constructive.
- Investors need to decide which camp they are in (no recession, mild-to-moderate recession, deep recession) before assessing whether to add more positions.
- I do much more than just articles at Ultimate Growth Investing: Members get access to model portfolios, regular updates, a chat room, and more. Learn More »
wildpixel
SPY: Two Down Years Are Rare
With the final trading day of 2022 concluded on December 30, we enter 2023 with cautious optimism./pic1560675.png) The S&P 500 ETF (NYSEARCA:SPY) (SPX) posted a 2022 total return of about -18%, outperforming the tech-heavy Nasdaq's (QQQ) (NDX) -33% decline, but underperformed the Dow Jones Industrial Average's (DIA) (DJI) -6.8% downtick.
The S&P 500 ETF (NYSEARCA:SPY) (SPX) posted a 2022 total return of about -18%, outperforming the tech-heavy Nasdaq's (QQQ) (NDX) -33% decline, but underperformed the Dow Jones Industrial Average's (DIA) (DJI) -6.8% downtick.
Therefore, DJI's more defensive and less tech-exposed weighting helped its investors avoid the hammering seen in the Nasdaq. As such, we have also seen a proliferation of media updates hammering tech stocks and highlighting the perils of a second-year bear market.
Accordingly, Bloomberg emphasized that "two consecutive down years are rare for major equity markets - the S&P 500 index has fallen for two straight years on just four occasions since 1928. However, it also accentuated that "when they do occur, drops in the second year tend to be deeper than in the first."
Therefore optimists can seek solace with the rarity of a second-year bear market and see the Fed as "nearly done raising rates." In contrast, pessimists see further damage to the global economy. Notably, they expect the Fed to remain hawkish for an extended period, as Piper Sandler cautioned in a recent note:
Notably, they expect the Fed to remain hawkish for an extended period, as Piper Sandler cautioned in a recent note:
We see all rates, and especially short ones, as too low. At the moment, neither the stock market nor corporate debt appears to be pricing in the possibility of prolonged pain - WSJ
Yet, we also have the strategists from Goldman Sachs (GS) straddling between optimism and pessimism, seeing the S&P 500 vacillating "in a range of 3,750 to 4,000." Based on the SPX's 2022 close of 3,839, the midpoint of GS's forecast range implies an uptick of 0.01%.
SPY: Could Its October Lows Withstand A Recession?
Hence, with confusing commentary spanning a wide range and expectations of the FOMC as it moves into data-dependency mode in 2023, we believe investors could be even more confused about what to expect for the SPY.
Optimists could consider the battering in SPY as a "fantastic" opportunity to "buy the dips" as SPY pulled back from its recent December highs.
SPY price chart (weekly) (TradingView)
However, buying the dips hasn't worked since the market staged its first deep pullback in late January, as Russia had yet to invade Ukraine. But, when the index's recovery failed at its April highs, as sellers formed a bull trap, buying the dips (which worked marvelously from the COVID lows) turned out to be a losing strategy until June.
Therefore, even though analysts' bottom-up earnings estimates for the SPX were pretty much on-point, macro factors such as the Fed's hawkish stance and elevated inflation turned out to be the market's main focus. WSJ highlighted:
The FactSet consensus prediction [for the SPX's EPS] is for $221 a share this year, exactly as predicted, with the final quarter still based on estimates. The miss of less than $1 is the smallest in percentage terms for estimates at the end of the year since 1995, data from Refinitiv IBES show, while the consensus has on average been out by more than 9% since then.
- WSJ
S&P 500: Analysts Don't Expect A Deep Earnings Recession in 2023
S&P 500 earnings growth estimates % (Yardeni Research, Refinitiv)
Hence, we believe investors want to know what will the market focus on in 2023? With SPY's total return down nearly 20% YTD, could downgraded 2023 earnings estimates for the SPX help propel a recovery? Accordingly, analysts' 2023 earnings estimates for the S&P 500 suggest a growth of 3.4% before a recovery of 10.2% for 2024.
Hence, analysts remain upbeat about companies' ability to dodge a marked earnings recession.
But would the Fed play ball in 2023 to corroborate our thesis of a market bottom at its October lows, despite the recent pullback?
Our analysis indicates that SPX's NTM P/E of 16.7x is pretty well-balanced, slightly below its 10Y average of about 17.7x. Hence, given the downgraded estimates, SPX's October lows (implying an NTM P/E of 15.2x) seem reasonable if we could dodge a considerable earnings recession.
So The Critical Question Is Whether The Market Anticipates A Severe Recession
So, the question is whether the market concurs with our thesis of no severe recession, even though Tesla (TSLA) CEO Elon Musk warned investors to expect one in 2023 before green shoots of recovery could appear in 2024.
The market needs to retake its December highs before a potential re-test of the 4,300 levels (SPX's August highs), which we expect to see robust resistance.
Accordingly, SPY seems to be consolidating constructively above its October lows, suggesting that a higher-low price structure could be forming. Hence, the price action favors our thesis so far, as SPY also moved into medium-term oversold zones.
Takeaway
As such, we believe investors who missed SPY's October lows and looking to add to the pullbacks could consider the current levels appropriate.
But, if October lows were to be decisively breached (i.e., not a bear trap), then the market could likely be setting up shop for a deeper recession than anticipated.
Stay safe, and Happy New Year, everyone!
Rating: Buy (Revise from Hold)
Do you want to buy only at the right entry points for your growth stocks?
We help you to pick lower-risk entry points, ensuring you are able to capitalize on them with a higher probability of success and profit on their next wave up. Your membership also includes:
24/7 access to our model portfolios
Daily Tactical Market Analysis to sharpen your market awareness and avoid the emotional rollercoaster
Access to all our top stocks and earnings ideas
Access to all our charts with specific entry points
Real-time chatroom support
Real-time buy/sell/hedge alerts
Sign up now for a Risk-Free 14-Day free trial!
This article was written by
JR Research
22. 65K Followers
65K Followers
Author of Ultimate Growth Investing
Sifting through the ultimate growth stocks for your portfolio
JR research was featured as one of Seeking Alpha's leading contributors in 2022. See: https://seekingalpha.com/article/4578688-seeking-alpha-contributor-community-2022-by-the-numbers
Unlock the key insights to growth investing with JR Research - led by founder and lead writer JR. Our dedicated team is focused on providing you with the clarity you need to make confident investment decisions.
Transform your investment strategy with our popular Investing Groups service. Ultimate Growth Investing specializes in a price-action-based approach to uncovering the opportunities in growth and technology stocks, backed by in-depth fundamental analysis. Plus, stay ahead of the game with our general stock analysis across a wide range of sectors and industries.
Improve your returns and stay ahead of the curve with our short- to medium-term stock analysis.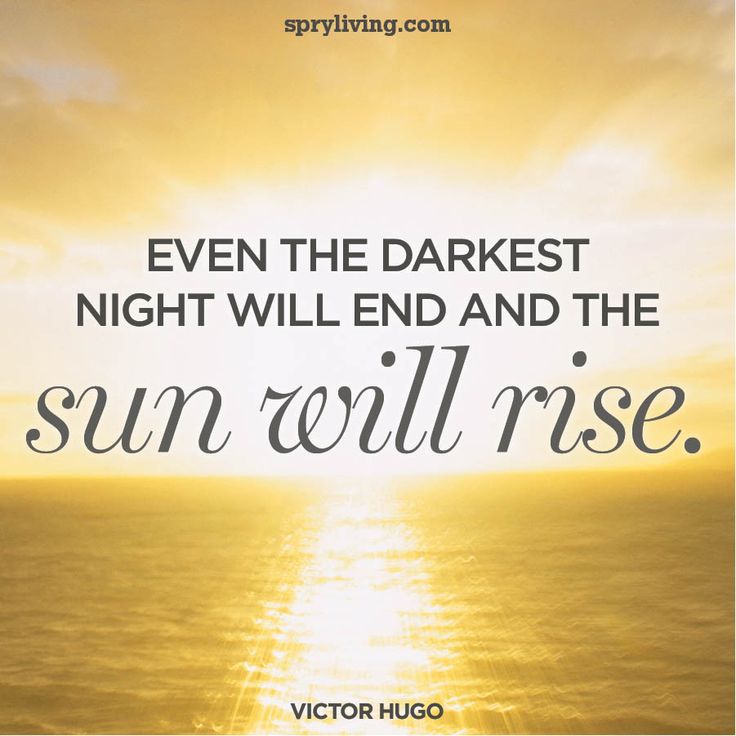 We not only identify long-term potential but also seize opportunities to profit from short-term market swings, using a combination of long and short set-ups. Join us and start seeing experiencing the quality of our service today.
We not only identify long-term potential but also seize opportunities to profit from short-term market swings, using a combination of long and short set-ups. Join us and start seeing experiencing the quality of our service today.
My LinkedIn: www.linkedin.com/in/seekjo
Disclosure: I/we have a beneficial long position in the shares of TSLA either through stock ownership, options, or other derivatives. I wrote this article myself, and it expresses my own opinions. I am not receiving compensation for it (other than from Seeking Alpha). I have no business relationship with any company whose stock is mentioned in this article.
Comments (71)Recommended For You
To ensure this doesn’t happen in the future, please enable Javascript and cookies in your browser.
Is this happening to you frequently? Please report it on our feedback forum.
If you have an ad-blocker enabled you may be blocked from proceeding. Please disable your ad-blocker and refresh.
Please disable your ad-blocker and refresh.
The pain will end. The tears will stop. Doors will open. A season of miracles and blessings is on the horizon. Don't give up...
The pain will end. The tears will stop. Doors will open. A season of miracles and blessings is on the horizon. Don’t give up.More Related Quotes:Never Lose Hope Just when you think it’s over, you’re sent a Miracle.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
When life gives you a hundred reasons to break down and cry, show life that you have a million reasons to smile and to be thankful for.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
 Stay Strong. To you reading this right now: It doesn’t matter where you are on the planet, I wish you a beautiful life full of love, happiness, and where all your dreams come true. Keep going.
Stay Strong. To you reading this right now: It doesn’t matter where you are on the planet, I wish you a beautiful life full of love, happiness, and where all your dreams come true. Keep going.Stop focusing on how stressed you are and remember How Blessed You Are.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
Life Is Saying To You Today: The pain will end.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
 The tears will stop. The doors will open. MIRACLES and BLESSINGS are coming. Don’t Give Up.
The tears will stop. The doors will open. MIRACLES and BLESSINGS are coming. Don’t Give Up. What is One Thing you are Grateful For Today?View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
This Is Your Weekly Reminder that you are Strong, Kind, Beautiful, Loved, and can handle anything this week throws at you.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on

Nothing Is Permanent Don’t stress yourself too much because no matter how bad the situation is… it will change.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
Don’t Lose Hope. You never know what tomorrow will bring. You are not too old, and it is not too late.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
I have felt alone when I couldn’t afford to be. But at the end of the day, I had to learn to love myself and be My Own Best Friend, because there’s going to be days when there will be no one there for me but myself. Positivity Pledge I shall no longer allow negative thoughts or feelings to drain me of my energy. Instead I shall focus on all the good that is in my life. I will think it, feel it and speak it. By doing so I will send out vibes of positive energy into the world and I shall be grateful for all the wonderful things it will attract into my life.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on

I opened Two Gifts this morning. They were My Eyes.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
10 SIGNS YOU’RE DOIN WELL IN LIFE:View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
1. You have a roof over your head.
2. You ate today.
3. You have a good heart.
4. You wish good for others.
5. You have clean water.
6. Someone cares for you.
7. You forgive others.
8. You have clothes to wear.
9. You smile.
10. You’re breathing.Be Thankful For The Little Things
At the end of the day, I Am Thankful that my blessings are bigger than my problems.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
Everything will work out in the end. You don’t need to know exactly how, you just have to trust that it will.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
Laugh Your Heart Out, Dance in the Rain, Cherish the Moment, Ignore the Pain, Live, Laugh, Love, Forgive and Forget, Life is not Meant to be lived with Regrets.View this post on Instagram
❤️
A post shared by Understanding Compassion (@understanding_compassion) on
 No matter how you feel: Get Up, Dress Up, Show Up, and Never Give Up! You are Loved.Watch this video of a kind child who uses his allowance to feed the homeless:
No matter how you feel: Get Up, Dress Up, Show Up, and Never Give Up! You are Loved.Watch this video of a kind child who uses his allowance to feed the homeless:Subscribe to YouTube
Postoperative pain: how to reduce the use of non-steroidal anti-inflammatory drugs
Author, editor and medical expert - Muraeva Yulia Yuryevna.
Views: 206 763
Last update date: 02/21/2023 G.
Average reading time: 9000
Content:
- Why postoperative pain
- How to reduce postoperative pain
- How long does postoperative pain last
The number of surgical interventions is growing 1 , surgical techniques and methods of anesthesia are being improved. However, postoperative pain remains an expected phenomenon and still requires the attention of doctors. Intense pain syndrome, which is observed in at least 40% of patients 1 , aggravates the course of the recovery period, contributes to the development of complications 2 , increases the recovery time, can turn into a chronic process 3 .
The International Association for the Study of Pain (IASP) adopted a declaration in 2010 that recognized adequate pain management as a fundamental human right 3 .
According to large studies 4 high intensity of postoperative pain is noted by patients after obstetric, gynecological, orthopedic and abdominal (on the abdominal cavity) surgical interventions, which are associated with postoperative pain in the abdomen, chest, joints. The characteristics of pain in the first day are very important, it is she who determines how the pain syndrome will develop in the future and whether it will become chronic 4 .
The characteristics of pain in the first day are very important, it is she who determines how the pain syndrome will develop in the future and whether it will become chronic 4 .
Up to content
Why postoperative pain occurs
Postoperative pain according to ICD-10 (International Classification of Diseases) refers to unspecified types of pain and does not carry any signal information either for the patient or for the doctor, since its causes and mechanisms are clear occurrence. Therefore, the modern principles of managing patients after surgery provide for maximum relief from unpleasant pain. Moreover, pain has a negative impact not only on healing, but also on vital processes in the body: the work of the cardiovascular, respiratory, digestive, central nervous systems, as well as blood coagulation 4 .
The formation of painful sensations is provided by a multilevel reaction that connects the immediate area of damage (wound surface) and the central nervous system. It starts with mechanical stimuli in the area of the incision and the release of biologically active substances (prostaglandins, bradykinins and others) 4 , and ends with the processing of information in the cerebral cortex and the connection of emotional and psychological components.
It starts with mechanical stimuli in the area of the incision and the release of biologically active substances (prostaglandins, bradykinins and others) 4 , and ends with the processing of information in the cerebral cortex and the connection of emotional and psychological components.
Pain syndrome develops as a result of the appearance of areas of increased pain sensitivity (hyperalgesia). Primary hyperalgesia is directly related to injury and forms near the wound. The area of secondary hyperalgesia covers a larger area and occurs later, within the next 12-18 hours 4 , as it is associated with stimulation of other types of receptors. It is she who is responsible for the preservation and intensification of pain sensations on the second or third day after the operation, and subsequently, for the development of chronic pain syndrome 7 .
Up to content
How to reduce postoperative pain
Specialists refer to the tasks of postoperative pain relief 4 :
- quality recovery period,
- acceleration of rehabilitation and discharge from the hospital,
- reduction in the number of complications, including the development of chronic postoperative pain.
The most effective is the so-called multimodal scheme 4 postoperative pain relief, the concept of which involves the use of the optimal combination of drugs from different groups in minimal doses 4 .
Groups of drugs used as pain relievers after surgery:
- Opioid analgesics. Traditionally considered the basis for surgical anesthesia, however, their isolated use gives the expected result in only 25-30% of cases 4 , and the introduction of the maximum effective dose is associated with a high risk of side effects 4 , including respiratory depression. Also, after their cancellation, even greater pain sensitivity often occurs.
- Non-steroidal anti-inflammatory drugs (NSAIDs). The formation of postoperative pain syndrome is directly related to tissue injury and inflammation. Therefore, the appointment of NSAIDs, as drugs with a powerful anti-inflammatory and analgesic effect, is indicated from the first minutes after surgery, and sometimes during surgery.
They act directly on the cause of the development of hypersensitivity, namely the production of prostaglandins and other biologically active substances involved in the inflammatory process. There are methods that suggest using NSAIDs 20-30 minutes before the incision, which reduces the intensity of pain in the area of postoperative sutures. 4
When prescribed with drugs from the previous group, NSAIDs make it possible to reduce the dose and enhance the effect of opioids and prevent their side effects 4 .
- Centrally acting non-opioid analgesics. They do not affect the mechanisms of inflammation, but are able to suppress secondary increased pain sensitivity at the level of transmission of nerve impulses. Their use half an hour before the end of the operation ensures a calm and painless awakening after anesthesia 4 . They have proven themselves in complex anesthesia.
- Drugs that affect the perception of pain.
 Introduced to prevent hypersensitivity and the development of chronic pain syndrome 4 .
Introduced to prevent hypersensitivity and the development of chronic pain syndrome 4 . - Regional anesthesia (analgesia). Application of the method is based on interrupting the flow of pain impulses from the damaged area to the spinal cord and brain 4 .
For each patient, a comprehensive pain relief scheme is selected individually. Factors such as age, gender, volume of surgical intervention, comorbidities, mental characteristics, sensitivity to pain and its presence before surgery are taken into account.
Up to contents
How long does postoperative pain last
This question cannot be answered unambiguously, but acute pain and discomfort disappear completely when scar tissue is formed and there are no more grounds for the occurrence of pain impulses. How long this period will last depends on the patient himself - the ability of his body's tissues to regenerate (recovery), the adequacy of pain relief, psychological mood and general condition.
If pain in the area of postoperative sutures lasts more than 3 months, with or without interruptions, and is not associated with the healing process, then these are signs of the development of a chronic pain syndrome. It is based on nerve damage or the formation of pathological impulses 6 . The frequency of its development ranges from 5 to 50% (on average, every fifth patient 6 ) and is one of the indicators of the success of surgical treatment 7 . This difference is explained by the difference in the methods of intervention and their trauma 7 .
For the formation of chronic postoperative pain, including scars, predisposing factors are 6 :
- female;
- under 35 years old 6 ;
- stress, preoperative anxiety, preoperative pain;
- type of intervention - if surgical treatment is associated with a high probability of damage to large nerves (amputation of limbs, operations on the chest organs, removal of the mammary glands), then the risk of chronic pain is much higher;
- duration of operation;
- during the postoperative period - intense acute pain, large doses of analgesics, the use of radiation and chemotherapy;
- excessive guardianship and support from loved ones in the recovery period,
- prolonged bed rest.

Prevention of the development of chronic pain syndrome is carried out in several stages:
- Primary - associated with the surgical intervention itself: if possible, the choice of a non-surgical method of treatment, the operation is performed in the least traumatic way, for example, the use of endoscopic techniques.
- Secondary - intensive pain relief after surgery. This is the most promising method that can be supplemented with the preoperative administration of analgesics, which contributes to the weakening of pain impulses after the intervention. Various analgesics, NSAIDs, regional anesthesia, sedatives are used as painkillers after surgery 7 .
Motrin® is one of the drugs in the group that helps to fight acute and chronic postoperative pain. Available in tablets of 250 mg. It has a pronounced anti-inflammatory and analgesic effect, which can last up to 12 hours 9 . In the postoperative period (in traumatology, orthopedics, gynecology, maxillofacial surgery) it can be taken by adults and children over 15 years old 8 .
If you do not know exactly the causes of pain in the postoperative wound, but it is not possible to consult a doctor quickly, then you can take Motrin® on your own for no more than 5 days 9 . Be sure to contact the doctor and find out the cause of the pain.
Modern complex (multimodal) pain relief tactics include the use of a combination of non-steroidal anti-inflammatory drugs, local anesthetics, centrally acting analgesics and drugs that act at the level of nerve impulse conduction. It should be applied throughout the entire period of existence of the zone of damaged tissues until the final healing.
Back to Contents
The information in this article is for reference only and does not replace professional medical advice. For diagnosis and treatment, contact a qualified specialist.
You may also be interested in:
- Pain in everyday life
- Treatment of pain with exercise therapy
- Arthritis of the knee
this is how my life will end” What do people experience when they suddenly wake up during an operation, and why does this happen?0001
General anesthesia is needed to make medical procedures painless. However, in vanishingly rare cases, it fails, and the patient may suddenly wake up during the operation. Being in a paralyzed state, he is unable to move or even open his eyes. To his horror, the man feels every touch of the scalpel, unable to give a distress signal. What people actually experience during intraanesthetic awakening and what is the reason for this phenomenon - in the material "Lenta.ru".
Donna Penner Awakening
Donna Penner from Altona, Canada never recovered from the psychological trauma she received 13 years ago. In 2008, shortly before her 45th birthday, she experienced heavy bleeding during her period and sought medical attention.
The doctor referred her for exploratory laparoscopy, a surgical operation in which an incision is made in the patient's abdomen to examine the abdominal organs for injury or disease. Penner was reassured that there was nothing to fear, as she was waiting for an ordinary procedure. However, something went wrong, and the woman woke up seconds before the surgeon made the first incision with a scalpel.
Due to the neuromuscular blocking drugs given at the same time as anesthesia, Penner's body became completely paralyzed. She was conscious and felt the surgeon making incisions in her abdomen. And while the doctors examined her body, the patient was pierced by indescribable pain. “I thought, ‘That’s it, this is how my life will end, right here on the operating table, and the family will never know what I experienced in the last few hours of my life, because no one will even notice what happened to me. the Canadian admitted.0003
Donna Penner
Photo: personal archive
Painful memories still keep her from sleeping peacefully. She wakes up several times a night from nightmares. Penner has stopped wearing neck-tight clothes and accessories because they make her feel like she's suffocating. What she had to experience shortly before the anniversary, she calls a life sentence, which can hardly be canceled.
Medical breakthrough
Penner's medical case is undeniably rare, but not an isolated one. A 2017 study of 260 people by University of Wisconsin anesthesiologist Robert Sanders shows that about five percent of patients can regain consciousness on the operating table despite being placed under anesthesia.
It is true that due to the effects of anesthesia, many of the patients eventually forget about the experience of intraanesthetic awakening. Now more than ever, it is important for doctors to investigate such cases, given how often anesthesia is used in the treatment of patients.
In the UK alone, nearly three million anesthetics are administered per year. I assume that right now in some part of the world a patient is conscious during an operation
Peter Odor Receptionist at St George's Hospital in London
Anesthesiology appeared two centuries ago and became a real breakthrough in the world of medicine. On October 16, 1846, Boston dentist William Morton was the first in the world to successfully perform ether anesthesia in the removal of a submandibular tumor in a patient, Gilbert Abbott. Although the patient could still mutter under his breath, he no longer felt pain, just a faint sensation of being "scratched with a hoe" on his skin.
In Russia, the first operation under anesthesia was performed by a friend of Nikolai Pirogov at the professorial institute, Fedor Inozemtsev, in February 1847. A week later, Pirogov himself performed the operation using an anesthetic. Soon he took part in military operations in the Caucasus. There, for the first time in the history of medicine, he began to operate on the wounded under ether anesthesia. In total, the surgeon performed about 10 thousand operations with ether anesthesia.
Before the advent of anaesthesia, surgery was considered the last and most cruel way to treat a patient. At the same time, the areas in which the surgeon could practice were strictly limited: minor surgery, amputation of limbs, excision of necrotic tissues and removal of stones from the bladder. The abdomen and chest were forbidden areas.
Many patients died on the operating table, unable to bear the pain. Some patients survived only due to the fact that they lost consciousness due to agony
The success of the operation without anesthesia was determined only by the speed of the surgeon. However, with the advent of general anesthesia, surgery has moved to a new level. Now doctors could operate on patients more slowly, and therefore more accurately and accurately. Anesthesiology has also made it possible to treat restricted areas. Over time, ether began to be replaced by more modern inhalation anesthetics.
Anesthesiologists now have a wide range of pain medications available. The choice of one or another means, as well as the dose, depend on the procedure and the needs of the particular patient.
William Morton performs the world's first anesthesia (October 16, 1846)
Photo: Granger / Diomedia
As a rule, the task for surgeons is not to make the patient unconscious, but to reduce or completely block the sensitivity of a certain part of the body. For example, to “freeze” the lower half of the body, regional anesthesia is used: spinal or epidural anesthesia. It is most commonly used during childbirth, bladder surgery, and hip arthroplasty.
Pitfalls of anesthesia
Drugs that are injected into the patient's body during general anesthesia intravenously or inhalation completely turn off consciousness. Under anesthesia, a person does not feel pain and most often experiences amnesia. The exact mechanisms of general anesthesia are still not fully understood. There is a theory that anesthetics blunt neurotransmitters - substances that regulate brain function.
For example, the short-term hypnotic propofol is used in general anesthesia as a sedative. It enhances the work of gamma-aminobutyric acid (GABA) - the most important inhibitory neurotransmitter of the central nervous system.
Related content:
“It's possible that anesthesia interferes with active communication,” says University of Wisconsin anesthesiologist Robert Sanders. In this case, the mind turns off, turning into a turned off TV, unable to process and respond to body signals.
However, it is important for the anesthesiologist to consider many factors when treating each patient. The specialist may use one drug to put the patient into a medically induced coma and another to keep the patient in that state. In addition, the age and build of the patient, whether he smoked, what medications he took, and the cause of the disease are important in order to determine the appropriate dosage.
Doctors often administer muscle relaxants to patients - drugs that reduce muscle tone up to complete immobilization of a person. For example, in the UK, almost half of general anesthesia includes neuromuscular blockers. These medicines temporarily paralyze the patient to eliminate the possibility of spasms and reflex movements during surgery.
Anesthesiology has been working wonders for more than 170 years, saving the lives of millions of people. However, as with other medical procedures, there are complicating factors. Some people have a high threshold for anesthetics. In this case, the drugs do not reduce brain activity, and the person remains conscious. In difficult cases, for example, with injuries with a large loss of blood, the doctor has to manage with smaller doses of anesthetics so as not to aggravate the patient's condition.
In some cases, the patient may move their limbs and even speak to alert the surgeon that the drugs are not working. However, if the patient was injected with muscle relaxants, it is no longer possible to give a signal. It is for this reason that a small percentage of people become hostages of their body and are conscious on the operating table. Most often, they hear sounds and feel pain, but cannot call for help.
The operation is not over yet
Penner recalls how nervous she was before the laparoscopy, although in the past she had undergone operations under anesthesia, and everything went without any problems. She was taken to the operating room, placed on the table and given the first dose of medication. Soon she began to fall asleep, having time to think: "Well, that's it, it worked."
When the Canadian regained consciousness, she heard the nurses fussing around the operating table. Penner felt a touch on her stomach and decided that the examination was over and the medical staff was rubbing her skin. “I thought, ‘Well, you needlessly worried,’” she says. And then, to her horror, she heard the surgeon ask the nurse to give him a scalpel. The operation isn't over yet, she suddenly realized. In fact, it hasn't even started yet.
The next thing the patient felt was a sharp pain from a knife piercing her body. She tried desperately to move and speak, but the muscle relaxants kept her body immobilized.
I felt so...so helpless. I couldn't do anything. Don't move, don't scream, don't open your eyes. I tried to cry so that tears would run down my cheeks, hoping that they would notice this and understand that something was wrong. But I couldn't cry
Donna Penner
Penner put all her strength into moving one foot, and succeeded. The Canadian felt relieved when the nurse touched her leg with her hand. However, before she could move her foot again, the paramedic withdrew her hand. The patient tried three times to draw attention to herself, but to no avail. “I lost all hope, realizing that I only have one way to communicate, and even that doesn’t work,” she admits.
Photo: Christopher Furlong / Getty Images
It seemed that immediately after the operation her suffering should have ended. But as soon as the effect of the muscle relaxants began to fade, Penner began to move her tongue near the tube inserted into her throat. In this way, she wanted to hint to the staff that she was conscious all this time.
The health worker misunderstood her message and prematurely took out the oxygen tube, before the muscle relaxants finally wore off and her lungs began to work on their own. “I was lying on the operating table, and he took away what kept me afloat, my oxygen. I couldn't breathe,” she says.
Penner began to lose consciousness, at which point she said she thought she felt the presence of God. Fortunately, she was put back on the oxygen machine, after which she woke up in tears
Memories of the experience and a sense of insecurity haunt the woman to this day. Psychological trauma forced her to temporarily leave her job and take a sick leave. “It’s hard to sit at home and see how the neighbors come out of the house in the morning, get into their cars and leave for work, and realize that I can’t,” she complained in 2019year in an interview.
A little-studied phenomenon
There are various organizations around the world investigating such incidents. However, the Anesthesia Awareness Registry at Washington State Research University is considered to provide the most detailed analysis. Operating since 2007, the university organization has collected information on hundreds of medical cases of intraanesthetic awakening.
Although all stories are strictly anonymous, they shed light on this little-studied phenomenon. Nearly all patients who experienced inadvertent awakening from general anesthesia reported hearing voices and other sounds.
“I heard songs in one genre and tried to understand why my surgeon chose it,” recalls one of the patients. Another patient noted that he also heard different voices, and it seemed to him that people were excited. “They said they were losing me,” he recounted.
Photo: BSIP / Universal Images Group via Getty Images
More than 70 percent of those who experienced intraoperative recovery from anesthesia complained of pain. “I felt sharp pain and burning from four incisions, it felt like a finger cut with a sharp knife,” the patient recalls. “And then the burning, unbearable pain.”
It is the paralyzing effect of muscle relaxants that scares patients more than anything else. According to the stories of patients, due to muscle blockers, a person has a feeling that he stops breathing. And to all this - devastating helplessness. “To myself, I shouted something like: “Don’t they understand that I’m not sleeping, open your eyes and give them a signal,” one of the victims noted. The panic is exacerbated by the fact that patients experiencing intraanesthetic awakening do not know what is happening to them and think that they are dying.
Fortunately, judging by the statistics, such incidents are indeed extremely rare.
One of the largest and most detailed studies was the fifth draft national audit conducted by the British and Irish Associations of Anesthesiologists. Under the agreement, each public hospital in the UK and Ireland had to report any cases of intraanesthetic awakening known to them within a year.
Results published in 2014 showed that this phenomenon occurs in one in 19thousands of patients undergoing general anesthesia. At the same time, if paralyzing drugs were administered during anesthesia, intraoperative exit from anesthesia occurred more often - in one in eight thousand patients - because people could not warn doctors about the problem.
Related materials:
The findings and expert opinion confirm that the risk of experiencing intraanesthetic awakening is vanishingly small. However, Peter Odor from St George's Hospital in London believes that the results of the study are not correct enough to assess the risks of general anesthesia based on them.
The draft national audit took into account the stories of only those patients who were willing to share their experiences. According to Odor, many victims simply could not or did not want to talk about the trauma they received during the operation in order to leave negative memories in the past.
In addition, anesthetics can cause memory lapses in patients. “Anesthetic drugs interfere with the ability to remember,” says Odor. “And the dose used to dull the memory is less than what is used to knock a person out of consciousness.” It follows from this that a larger percentage of people could also come out of anesthesia during the operation, but then forget about it.
Controversial facts
To investigate this phenomenon, experts use what they call the hand isolation technique. During the injection of anesthesia, the patient's shoulder is tightened with a belt that does not allow muscle relaxants to block the arm. Thanks to this, for some time the patient can still move his arm and answer the doctor's questions: is he conscious and does he feel pain.
In one of the largest studies of its kind, University of Wisconsin anesthesiologist Robert Sanders collaborated with colleagues from six hospitals in the US, Europe, and New Zealand. Of the 260 patients who participated in the experiments, 4.6 percent confirmed that they were still conscious, despite the effect of general anesthesia.
The data obtained is inconsistent with the indicators noted in the framework of the 2014 national audit project. Approximately four out of ten patients treated with the isolated hand technique - 1.9 percent of the entire study group - also said they felt pain. These results call into question the ethical aspect of the use of anesthesia.
Whenever I talk to trainees, I discuss this philosophical question with them. If the patient does not remember anything, is it worth worrying about?
Robert Sanders anesthesiologist at the University of Wisconsin
According to Sanders, there is no evidence to date that patients who respond to pain during arm-tightening experiments but do not remember the experience later do not experience post-traumatic stress disorder and others. psychological problems, such as in the case of Penner. After all, if a person does not experience adverse consequences in such a case and does not remember anything, one might think that intraanesthetic awakening is an unpleasant, but most often not a fearful experience.
Sanders decided to conduct a survey among ordinary people and was surprised to hear mixed opinions. A surprisingly large number of respondents stated that they would take such a sudden exit from anesthesia calmly if the painful experience would surely disappear from their memory upon awakening.
I believe that the patient is hoping that he will be unconscious; and as researchers who want to understand the mechanisms of this phenomenon, as well as doctors who want to provide quality care and meet patient expectations, we have an obligation to study this process and find out what the true impact of intraanesthetic awakening is on a person, and also to learn how we can reduce the likelihood of its manifestation
Robert Sanders anesthesiologist at the University of Wisconsin
Statistics can lie
Undoubtedly, various articles and studies on intraanesthetic awakening can frighten patients preparing for surgery. Some even refuse anesthesia and subsequent treatment in order to avoid the possible consequences of general anesthesia. However, it should be remembered that the risk of sudden withdrawal from drug sleep is extremely low.
Physicians are convinced that this phenomenon should be known to as many people as possible. In some cases, described in medical journals, patients were unaware of the existence of such a phenomenon and upon awakening were convinced that they were dying. Perhaps with greater awareness, patients will be able to experience this experience less painfully.
Greater awareness of this issue may also help clinicians treat patients who have experienced intraanesthetic awakening. Many patients, including Penner, claim that their behavior on the operating table was perceived by doctors incorrectly.
Photo: Klar / ullstein bild via Getty Images
According to a study by scientists from the University of Washington, 75 percent of patients who experienced an unplanned awakening from anesthesia were dissatisfied with the staff's response to their complaints. 51 percent of people claimed that neither the anesthesiologist nor the surgeon expressed sympathy for them. Only 10 percent of the victims said the hospital apologized to them, and only 15 percent were referred to specialists who helped them cope with psychological trauma.
When Penner tried to tell the nurses what had happened, they stood in confusion and remained silent. “I will never forget the look on their faces – they seemed to be in total shock,” she says. “They don’t know what to do in a situation like this.” The Canadian believes that doctors should study this phenomenon more.
Penner hopes that further research on intraanesthetic awakening will help to better understand the effects of general anesthesia and, as a result, reduce the number of sudden awakenings during surgery. Scientists believe that with a deeper study of drug-induced sleep, doctors will be able to use this phenomenon for the benefit of patients.
Clinical studies confirm that some types of therapeutic hypnosis have a beneficial effect on patients. Thus, anesthesia can be an ideal way to put the patient into a state of hypnotic trance. And although the brain goes into deep sleep under the influence of anesthetics, it has been proven that some areas continue to function, for example, the auditory zone. This suggests that doctors can communicate with an unconscious patient during surgery
There is very little research on this theory, but Jenny Roosendahl and her colleagues at the University Hospital in Jena, Germany, tried to collect all the available evidence. Their meta-analysis showed a small but significant improvement in postoperative symptoms in patients, in particular nausea and vomiting, as well as less morphine use during the rehabilitation period.
Recovering slightly from her injury, Penner volunteered to help Canadian universities educate physicians about intraanesthetic awakening and the best ways to treat patients. “I want them to be shod,” she emphasizes. - After all, when the operation does not go according to plan, you need to know how to react; this is essential for the well-being of the patient.