Otherwise specified dissociative disorder
Other Specified & Unspecified Dissociative Disorders
Other Specified Dissociative Disorder
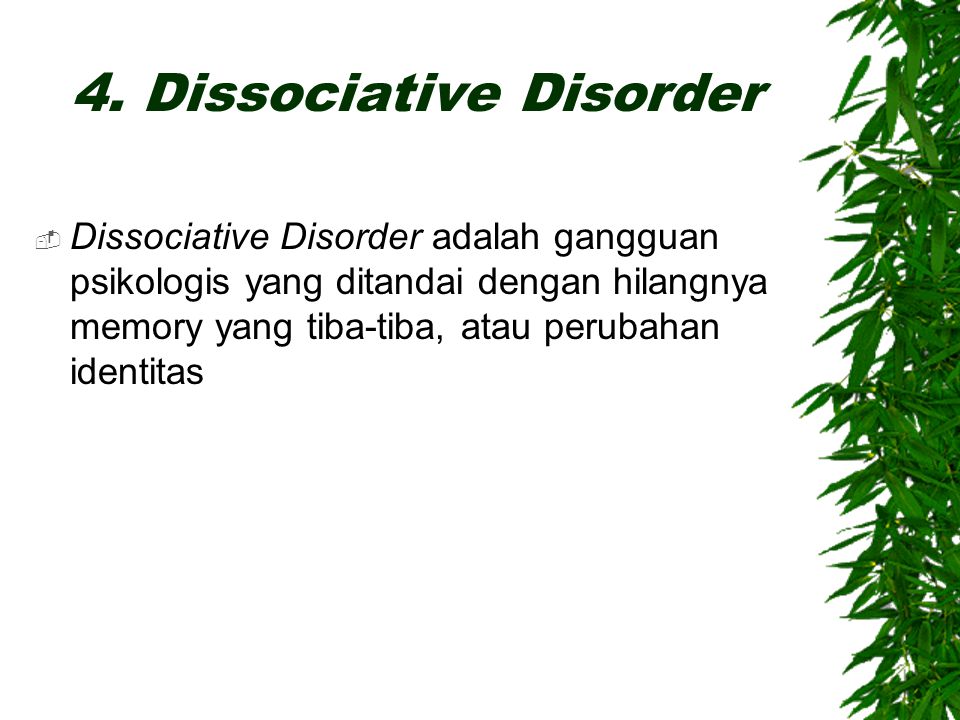
This disorder is characterized by a loss of awareness or orientation to their surroundings and/or identity. The functions of consciousness, memory, identity, or perception of one’s environment is disrupted.
In a dissociative trance, a person may be completely unresponsive to outside, surrounding stimuli (for instance, someone trying to talk to them may be ignored). This person may perceive that things around them are “surreal,” “blurred,” or moving around them while they remain paralyzed and unable to gain control over their environment.
The person may experience periods during which they question, reject, or detach from their awareness of who they are. These symptoms are rare and usually occur in those who have experienced prolonged stress of torture, abuse, or captivity.
These symptoms cannot be part of a culturally-accepted practice or religious ritual.
Others chronically or recurrently experience a combination of these states, termed syndrome of mixed dissociative symptoms.
Dissociative experiences that are of transient or brief nature most often occur as an acute reaction to an intensely stressful experience or traumatic event. Some common dissociative symptoms in these instances include:
- The feeling that time is slowing down
- Amnesia (recognized following the stressor as an inability to recall important parts of the event)
- A narrowing of consciousness or “tunnel vision”
- Feeling as if one were on chemical anesthetics or analgesics to some degree
Unspecified Dissociative Disorder
Sometimes, one may show signs of a noteworthy dissociative condition or an event that does not fit neatly into the typical presentation of a known dissociative disorder. At other times, the source of dissociative symptoms may be unclear. For example, in the ER after a car accident when the person has experienced a head trauma — here symptoms may be due to a medical injury.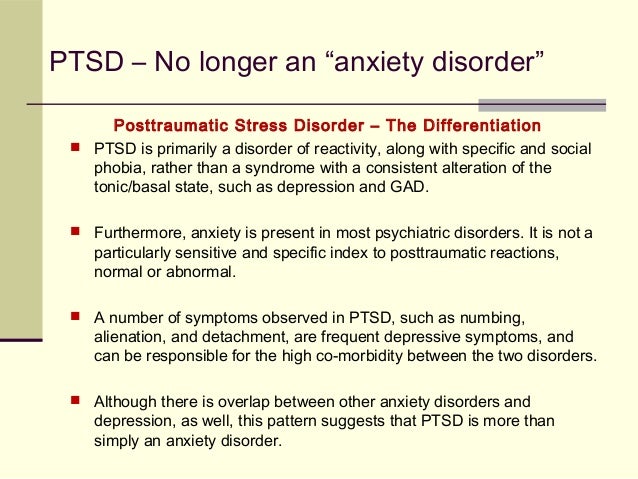
Sometimes, even in non-emergency settings, a patient may require an ongoing assessment of their symptoms in order for a clinician to gather sufficient evidence to confirm the existence of a dissociative disorder.
In these situations, the unspecified dissociative disorder may be used (often as a “working diagnosis”). Specifically, the unspecified category applies to a dissociative episode or experience that significantly distresses a person and/or impacts ability to function in daily life, yet does not meet all the criteria for one of the established, known dissociative disorders. For example, if a person had met all but one symptom criteria for a particular dissociative disorder, this diagnosis would be appropriate.
This criteria has been adapted for the 2013 DSM-5. Other specified dissociative disorder and unspecified dissociative disorder (diagnostic code 300.15) are new additions to the DSM-5.Dissociative Disorder: Not Otherwise Specified (NOS)
Dissociative disorder not otherwise specified historically refers to symptoms of a dissociative disorder that doesn’t quite meet full criteria. Currently, “other specified” or “unspecified” dissociative disorder is used.
Currently, “other specified” or “unspecified” dissociative disorder is used.
If you’re experiencing dissociative symptoms that don’t seem to match the major types of dissociative disorder, you may have what mental healthcare professionals previously called dissociative disorder not otherwise specified (DDNOS).
The term DDNOS was used until 2013, when the most recent version of the Diagnostic and Statistical Manual of Mental Disorders (DSM) introduced new criteria for classifying dissociative disorders.
Thus, people who once would have received a diagnosis of DDNOS would now be diagnosed with one of several other conditions.
Dissociative disorder not otherwise specified is a former condition classification that mental healthcare professionals no longer use.
Before the classification change, older studies found that 8.3% of people experienced DDNOS. In contrast, studies have found that the most severe form of dissociative disorder, dissociative identity disorder (DID), is present in about 1% of the population.
Thus, DDNOS and the conditions that have replaced this former classification are fairly common.
The DSM-5 now includes five conditions in the category of dissociative disorders:
- dissociative identity disorder (DID)
- dissociative amnesia (DA), including dissociative fugue (DF)
- depersonalization/derealization disorder (DPDRD)
- other specified dissociative disorder (OSDD)
- unspecified dissociative disorder (UDD)
What used to be called dissociative disorder not otherwise specified (DDNOS) now falls mainly into the above categories of “other specified dissociative disorder” and “unspecified dissociative disorder,” although some people’s conditions may fall into other categories.
Other diagnostic classifications
This definition of DDNOS is specifically from the DSM-5.
Other diagnostic authorities, such as the International Classification of Diseases, 11th edition (ICD-11), have their own overlapping but distinct diagnostic criteria for dissociative disorders.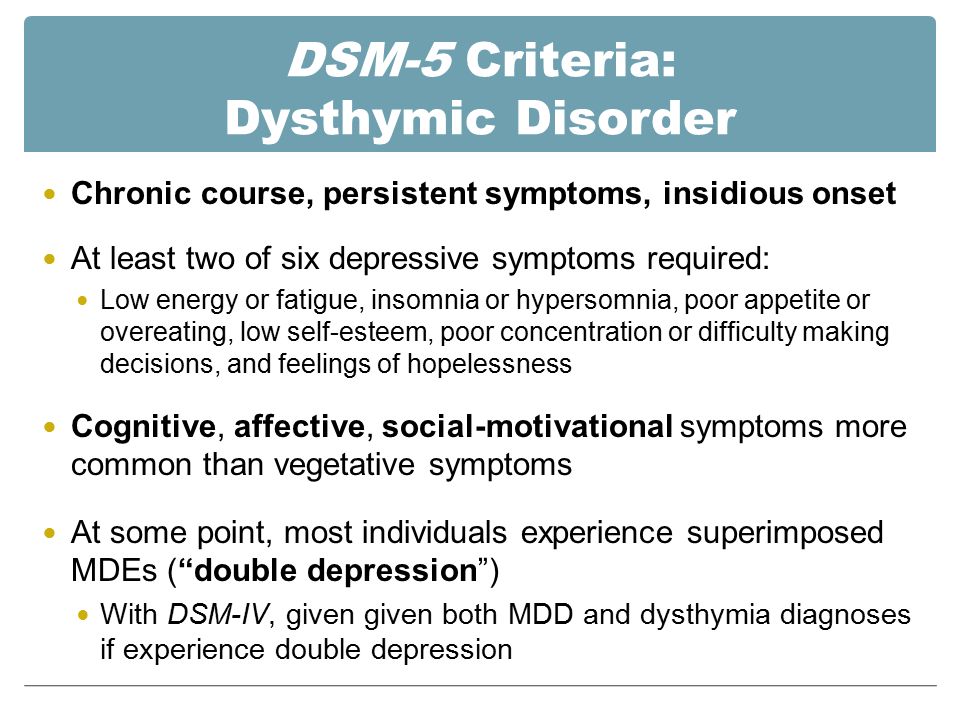
Dissociative identity disorder not otherwise specified is no longer a diagnosable disorder, according to the latest version of the DSM.
However, in all cases of dissociative disorders, the person would have dissociative symptoms that cause them significant problems or distress in key areas of their life, like with family, friends, or at work.
Dissociative symptoms the person might have depend on the specific disorder. They include:
- gaps in memory about certain events, time periods, or people
- you don’t feel a consistent sense of identity and might perceive that other personalities (or alters) sometimes take control of your actions
- you feel emotionally detached or numb
- you frequently feel like you are separated from your body and watching yourself from afar
- you experience other mental healthcare conditions and situations, such as depression, anxiety, and suicidal thoughts
Researchers have found that dissociative disorders are strongly associated with psychological trauma, particularly prolonged traumatic experiences in childhood.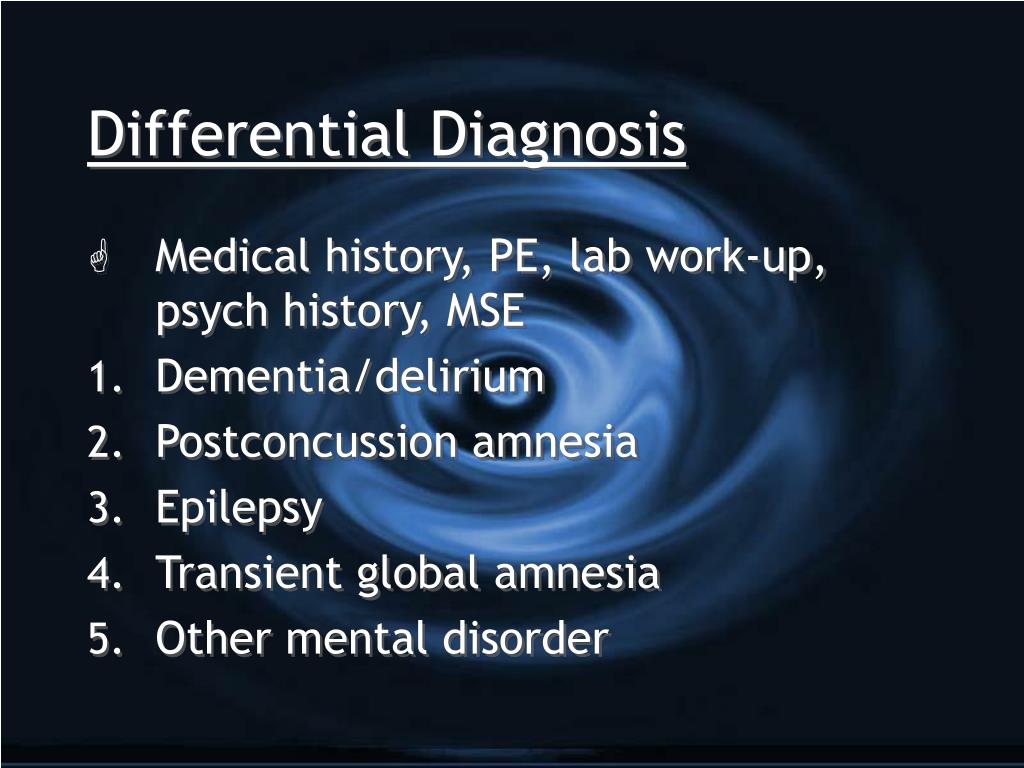
Every version of the DSM seeks to improve upon previous versions so that mental healthcare professionals can use the classification system to provide diagnoses that are as accurate and precise as possible.
To serve that purpose, in its newest edition published in 2013, the DSM has broken down the classification of DDNOS into the classifications we list above.
A mental healthcare professional might diagnose someone who would have formerly been diagnosed with DDNOS with one of the following conditions:
- dissociative identity disorder (DID), which has broader criteria in the DSM-5 compared with before
- depersonalization/derealization disorder, which now also has broader criteria
- other specified dissociative disorder
- unspecified dissociative disorder
The last two in this list are new classifications created to replace DDNOS.
In both of these conditions, the person shows dissociative symptoms that cause them significant problems or distress. However, their dissociative symptoms may be less defined or frequent than the symptoms of someone with DID, for example.
However, their dissociative symptoms may be less defined or frequent than the symptoms of someone with DID, for example.
Other specified dissociative disorder
Most people who would have been diagnosed with DDNOS with the previous version of the DSM would now be diagnosed with this condition.
Mental healthcare professionals use this classification in situations where they decide to specify the reason why the person doesn’t meet criteria to be diagnosed with a specific dissociative disorder.
Reasons a healthcare professional might specify include:
- The person has long-term changes in or questions about their identity after they experience prolonged, intense coercive persuasion, such as brainwashing, cult indoctrination, political imprisonment, or torture.
- The person frequently and repeatedly experiences dissociative symptoms, but they don’t have amnesia, or it’s hard to determine when or whether they felt breaks from their sense of self or felt like someone else was in control.
- The person experiences strong dissociative symptoms in reaction to stressful events.
- The person experienced a dissociative trance in which they became unresponsive but not as part of a normal cultural or religious practice.
Unspecified dissociative disorder
A person diagnosed with unspecified dissociative disorder would also have dissociative symptoms but would not satisfy all the standard indicators to be diagnosed with any of the other dissociative disorders.
It’s different than otherwise specified dissociative disorder (OSDD) in that the diagnosing healthcare professional decides they don’t want to specify why the person doesn’t meet the criteria.
Reasons for this could be:
- There’s not enough information available to make a specific diagnosis, such as in cases where a person has just come into the emergency room.
- The clinician decides for some other reason not to specify how the person did not meet the criteria.
If you think you might have a dissociative disorder, such as other specified dissociative disorder or unspecified dissociative disorder, consider reaching out to a licensed psychotherapist who has experience treating dissociative disorders.
You could ask a doctor to recommend a therapist or search for an expert yourself online. You can also try using this therapist search tool.
The National Alliance on Mental Illness offers this list of resources for getting help with dissociative disorders.
You can also learn more about dissociative disorders from these organizations:
- The National Alliance on Mental Illness (NAMI)
- The American Psychiatric Association (APA)
Whether you’re a mental healthcare professional or you’re experiencing dissociative symptoms yourself, you may be looking for more information on how DDNOS is diagnosed.
Though healthcare professionals no longer use DDNOS as a diagnosis, they have other ways to more accurately diagnose and treat people experiencing these dissociative conditions.
📖 List of diagnostic headings of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, 1995 (ICD-10), including borderline conditions.
 20, Clinical features of the main forms of borderline mental disorders, Section II. Clinic of borderline mental disorders. Borderline mental disorders. Tutorial. Aleksandrovsky Yu. A. Page 14. Read online
20, Clinical features of the main forms of borderline mental disorders, Section II. Clinic of borderline mental disorders. Borderline mental disorders. Tutorial. Aleksandrovsky Yu. A. Page 14. Read online List of diagnostic rubrics International Statistical Classification of Diseases and health problems, tenth revision, 1995 (ICD-10), including boundary conditions.
2020 edition WHO. Russian translation S.-P., 1994, 1995; adapted option for use in the Russian Federation. M., 1998.
F3 Affective mood disorders
F30 Manic Episode
F30.0 Hypomania
Psychology bookap
F30.1 Mania without psychotic symptoms
F30.2 Mania with psychotic symptoms
F30.
8 Other manic episodes
F30.9 Manic episodes, unspecified
F31 Bipolar affective disorder
F31.0 Bipolar affective disorder, current hypomanic episode
Psychology bookap
F31.1 Bipolar affective disorder, current episode of mania without psychotic symptoms
F31.2 Bipolar affective disorder, current manic episode with psychotic symptoms
F31.3 Bipolar affective disorder, current episode of moderate or mild depression
.30 without somatic symptoms
.31 with somatic symptoms
F31.4 Bipolar affective disorder, current episode of severe depression without psychotic symptoms
Psychology bookap
F31.5 Bipolar affective disorder, current episode of severe depression with psychotic symptoms
F31.6 Bipolar affective disorder, current episode mixed
F31.7 Bipolar affective disorder, condition remissions
Psychology bookap
F31.
8 Other bipolar affective disorders
F31.9 Bipolar affective disorder, unspecified
F32 Depressive episode
F32.0 Mild depressive episode
.00 without somatic symptoms
.01 with somatic symptoms
F32.1 Moderate depressive episode
.10 without somatic symptoms
.11 with somatic symptoms
F32.2 Severe depressive episode without psychotic symptoms
Psychology bookap
F32.3 Major depressive episode with psychotic symptomatic
F32.8 Other depressive episodes
F32.9 Depressive episodes, unspecified
F33 Recurrent depressive disorder
F33.0 Recurrent depressive disorder, current mild episode
.00 without somatic symptoms
.01 with somatic symptoms
F33.
1 Recurrent depressive disorder, current moderate episode
.10 without somatic symptoms
.11 with somatic symptoms
F33.2 Recurrent depressive disorder, current severe episode without psychotic symptoms
Psychology bookap
F33.3 Recurrent depressive episode, current severe episode with psychotic symptoms
F33.4 Recurrent depressive disorder, condition remission
F33.8 Other recurrent depressive disorders
F33.9 Recurrent depressive disorder, unspecified
F34 Chronic (affective) mood disorders
F34.0 Cyclothymia
Psychology bookap
F34.1 Dysthymia
F34.8 Other chronic affective disorders F34.9 Chronic (affective) mood disorder, unspecified
F38 Other (affective) mood disorders
F38.0 Other single (affective) disorders moods
.
00 mixed affective episode
F38.1 Other recurrent (affective) disorders moods
.10 recurrent short-term depressive disorder
F38.8 Other specified (affective) disorders moods
F39 Unspecified (affective) mood disorders
F4 Neurotic, stress-related and somatoform disorders
F40 Anxiety-phobic disorders
F40.0 Agoraphobia
.00 without panic disorder
.01 with panic disorder
F40.1 Social phobias
Psychology bookap
F40.2 Specific (isolated) phobias
F40.8 Other phobic anxiety disorders
F40.9 Phobic anxiety disorder, unspecified
F41 Other anxiety disorders
F41.0 Panic disorder (episodic paroxysmal anxiety)
Psychology bookap
F41.
1 Generalized anxiety disorder
F41.2 Mixed anxiety and depressive disorder
F41.3 Other mixed anxiety disorders
Psychology bookap
F41.8 Other specified anxiety disorders
F41.9 Anxiety disorder, unspecified
F42 Obsessive-compulsive disorder
F42.0 Predominantly intrusive thoughts or ruminations (mental gum)
Psychology bookap
F42.1 Predominantly compulsive actions (obsessional rituals)
F42.2 Mixed obsessive thoughts and actions
F42.8 Other obsessive-compulsive disorders
F42.9 Obsessive-compulsive disorder, unspecified
F43 Severe stress reactions and adjustment disorders 21
21 Socially stressful disorders (CVD) are described in detail in the relevant section of this manual. In ICD-10, SSRs are not distinguished, however, more and more evidence is accumulating to consider their inclusion in the classification schemes for mental illness.
F43.0 Acute stress reaction
Psychology bookap
F43.1 Post-traumatic stress disorder
F43.2 Adjustment disorders
.20 short-term depressive reaction
Psychology bookap
.21 prolonged depressive response
.22 mixed anxiety and depressive reaction
.23 with predominant disturbance of other emotions
Psychology bookap
.24 with predominance of behavioral disorder
.25 mixed disorder of emotions and conduct
.28 other specific predominant symptoms
F43.8 Other reactions to severe stress 22
22 B this group includes nosogenic reactions that occur due to a serious somatic illness (the last is a traumatic event in these cases).
F43.9 Severe stress response, unspecified
F44 Dissociative (conversion) disorders 23
23 B ICD-10 the term "hysteria" is not used because of its many and varied meanings. The term "dissociative" is used instead. It combines the disorders described earlier in within the framework of hysteria and includes both properly dissociated, and conversion disorders.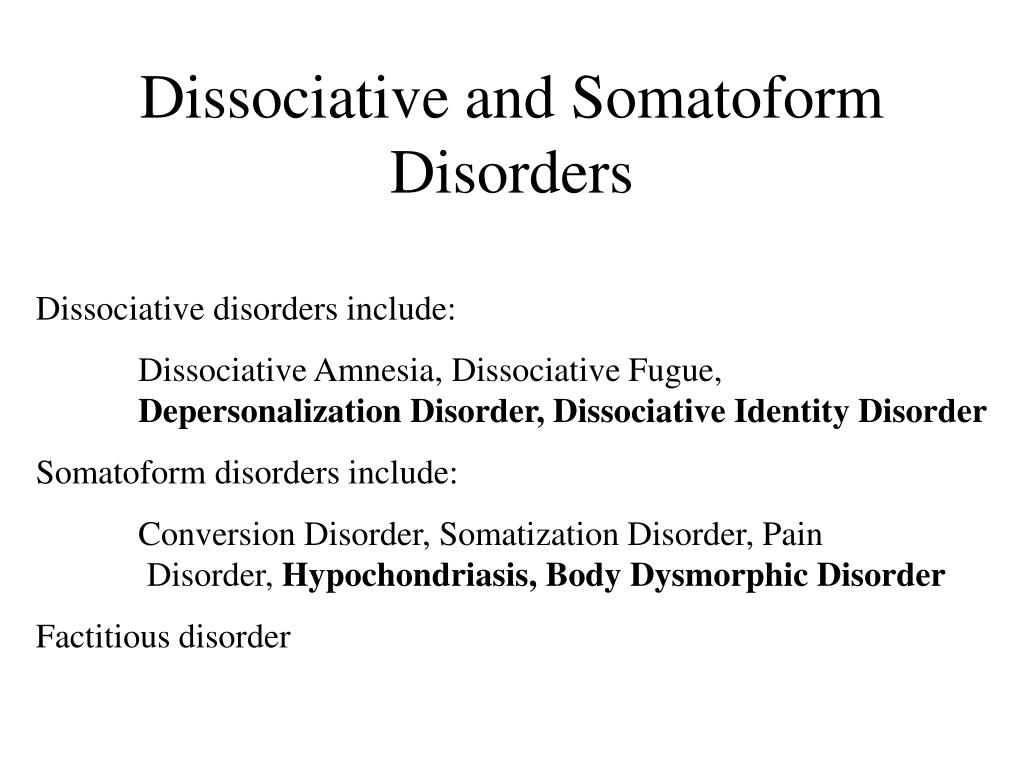
F44.0 Dissociative amnesia
Psychology bookap
F44.1 Dissociative fugue
F44.2 Dissociative stupor
F44.3 Trances and states of mastery
Psychology bookap
F44.4 Dissociative motor disorders
F44.5 Dissociative convulsions
F44.6 Dissociative anesthesia and sensory loss perception
Psychology bookap
F44.7 Mixed dissociative (conversion) disorders
F44.8 Other dissociative (conversion) disorders
.80 Ganser syndrome
Psychology bookap
.81 multiple personality disorder
.82 transient dissociative (conversion) disorders that occur in childhood and adolescence aged
.88 other specified dissociative (conversion) disorders
F44.9 Dissociative (conversion) disorder, unspecified
F45 Somatoform disorders 24
24 Common in domestic medicine, the term "psychosomatic disorder" in ICD-10 is not used due to ambiguity of its definition in different languages and in the presence of unequal psychiatric traditions. In addition, psychological factors are important and broader in the origin and the course of various diseases, and not only included among the "psychosomatic". In ICD-10 for designation of "association" of physical or somatic manifestations with mental disorders the concept of "somatoform disorders" is used.
F45.
0 Somatization disorder
Psychology bookap
F45.1 Undifferentiated somatoform disorder
F45.2 Hypochondriacal disorder
F45.3 Somatoform autonomic dysfunction
.30 heart and cardiovascular system
Psychology bookap
.31 upper gastrointestinal tract
.32 lower gastrointestinal tract
.33 respiratory system
Psychology bookap
.34 urogenital system
.38 other body or system
F45.4 Chronic somatoform pain disorder
Psychology bookap
F45.8 Other somatoform disorders
F45.9 Somatoform disorder, unspecified
F48 Other neurotic disorders
F48.0 Neurasthenia
Psychology bookap
F48.1 Depersonalization-derealization syndrome
F48.8 Other specific neurotic disorders
F48.9 Neurotic disorder, unspecified
F5 Behavioral syndromes associated with physiological disorders and physical factors
F50 Eating disorders
F50.
0 Anorexia nervosa
Psychology bookap
F50.1 Atypical anorexia nervosa
F50.2 Bulimia nervosa
F50.3 Atypical bulimia nervosa
Psychology bookap
F50.4 Overeating associated with other psychological violations
F50.5 Vomiting associated with other psychological violations
F50.8 Other eating disorders
F50.9 Eating disorder, unspecified
F51 Inorganic sleep disorders
F51.0 Insomnia of inorganic nature
Psychology bookap
F51.1 Hypersomnia of inorganic nature
F51.2 Nonorganic sleep-wake disorder nature
F51.3 Sleepwalking (somnambulism)
Psychology bookap
F51.4 Night terrors (night terrors)
F51.5 Nightmares
F51.8 Other nonorganic sleep disorders
F51.9 Inorganic sleep disorder, unspecified
F52 Non-organic sexual dysfunction disorder or disease
F52.
0 Absence or loss of sexual desire
F52.1 Sexual aversion and lack of sexual satisfaction
.10 sexual disgust
. 11 lack of sexual satisfaction
F52.2 No genital response
Psychology bookap
F52.3 Orgasmic dysfunction
F52.4 Premature ejaculation
F52.5 Vaginismus of inorganic origin
Psychology bookap
F52.6 Nonorganic dyspareunia
F52.7 Increased sexual desire
F52.8 Other sexual dysfunction, not due to organic disorder or disease
F52.9 Unspecified sexual dysfunction, not due to organic disorder or disease
F53 Mental and behavioral disorders, associated with the postpartum period, not classified in other sections
F53.0 Mild mental and behavioral disorders, associated with the postpartum period, not classified in other sections
Psychology bookap
F53.
1 Severe mental and behavioral disorders, associated with the postpartum period, not classified in other sections
F53.8 Other mental and behavioral disorders, associated with the postpartum period, not classified in other sections
F53.9 Postpartum mental disorder, unspecified
F54 Psychological and behavioral factors associated with disorders or diseases classified elsewhere in other sections
F55 Abuse of non-causing substances dependencies
F55.0 Antidepressants
Psychology bookap
F55.1 Laxatives
F55.2 Analgesics
F55.3 Deacidifiers
Psychology bookap
F55.4 Vitamins
F55.5 Steroids or hormones
F55.6 Specific herbs and folk remedies
Psychology bookap
F55.8 Other non-addictive substances
F55.9 Unspecified
F59 Unspecified behavioral syndromes associated with with physiological disorders and physical factors
F6 Disorders of mature personality and behavior in adults 25
25 Disorders mature personality and behavior in adults, including in this category, are stable and are expression of the characteristics inherent in the individual lifestyle and way of relating to oneself and others ("models behavior"). In most cases, these disorders ontogenetically formed, appear in childhood or adolescence and persist into adulthood. They are not secondary to other mental disorders or diseases of the brain.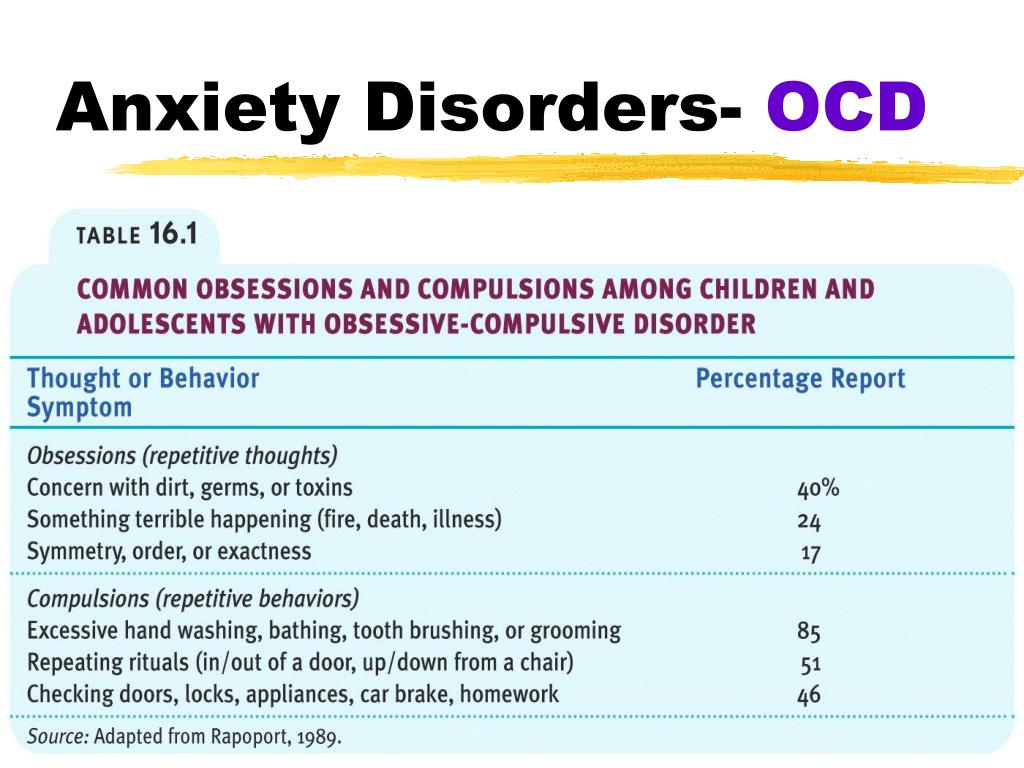 extreme conditions and other psychotraumatic factors contribute to decompensation (reaction) of existing disorders of mature personality. In our country, most of those attributed to this category of disorders is traditionally considered in within psychopathy and pathological personality development.
extreme conditions and other psychotraumatic factors contribute to decompensation (reaction) of existing disorders of mature personality. In our country, most of those attributed to this category of disorders is traditionally considered in within psychopathy and pathological personality development.
F60 Specific personality disorders
F60.0 Paranoid personality disorder
Psychology bookap
F60.1 Schizoid personality disorder
F60.2 Antisocial personality disorder
F60.3 Emotionally unstable personality disorder
.30 impulsive type
.31 border type
F60.4 Histrionic personality disorder
Psychology bookap
F60.5 Anancaste (obsessive-compulsive) disorder personalities
F60.6 Anxious (avoidant) personality disorder
F60.7 Dependent personality disorder
Psychology bookap
F60.8 Other specific personality disorders
F60.
9 Personality disorder, unspecified
F61 Mixed and other personality disorders
F61.0 Mixed personality disorders
F61.1 Disturbing personality changes
F62 Chronic personality changes, unrelated with brain damage or disease
F62.0 Chronic personality change after experience disasters
Psychology bookap
F62.1 Chronic personality change after mental diseases
F62.8 Other chronic personality changes
F62.9 Chronic personality change, unspecified
F63 Disorders of habits and impulses
F63.0 Pathological gambling
Psychology bookap
F63.1 Pathological arson (pyromania)
F63.2 Pathological theft (kleptomania)
F63.3 Trichotilomania
Psychology bookap
F63.8 Other disorders of habits and drives
F63.9 Disorder of habits and drives, unspecified
F64 Gender identity disorders
F64.
0 Transsexualism
Psychology bookap
F64.1 Dual role transvestism
F64.2 Gender identity disorder in children
F64.8 Other gender identity disorders
F64.9 Gender identity disorder, unspecified
F65 Disorders of sexual preference
F65.0 Fetishism
Psychology bookap
F65.1 Fetish transvestism
F65.2 Exhibitionism
F65.3 Voyeurism
Psychology bookap
F65.4 Pedophilia
F65.5 Sadomasochism
F65.6 Multiple disorders of sexual preference
Psychology bookap
F65.8 Other disorders of sexual preference
F65.9 Disorder of sexual preference, unspecified
F66 Psychological and behavioral disorders, related to sexual development and orientation
F66.0 Disorder of puberty
Psychology bookap
F66.1 Ego-dystonic sexual orientation
F66.
2 Sexual relations disorder
F66.8 Other psychosocial developmental disorders
F66.9 Psychosocial development disorder, unspecified
F68 Other disorders of adult personality and behavior in adults
F68.0 Exaggeration of physical symptoms by psychological reasons
Psychology bookap
F68.1 Intentional induction or feigning of symptoms or disability, physical or psychological (faking disorder)
F68.8 Other specific disorders of the mature personality and behavior in adults
What is dissociative identity disorder?
Dissociative identity disorder is a mental disorder characterized by either having two or more personalities, or a state of disconnection from the outside world, one's identity, and an inability to remember certain daily life events and important personal information. This disorder is often mistaken for depression, anxiety, or psychosis.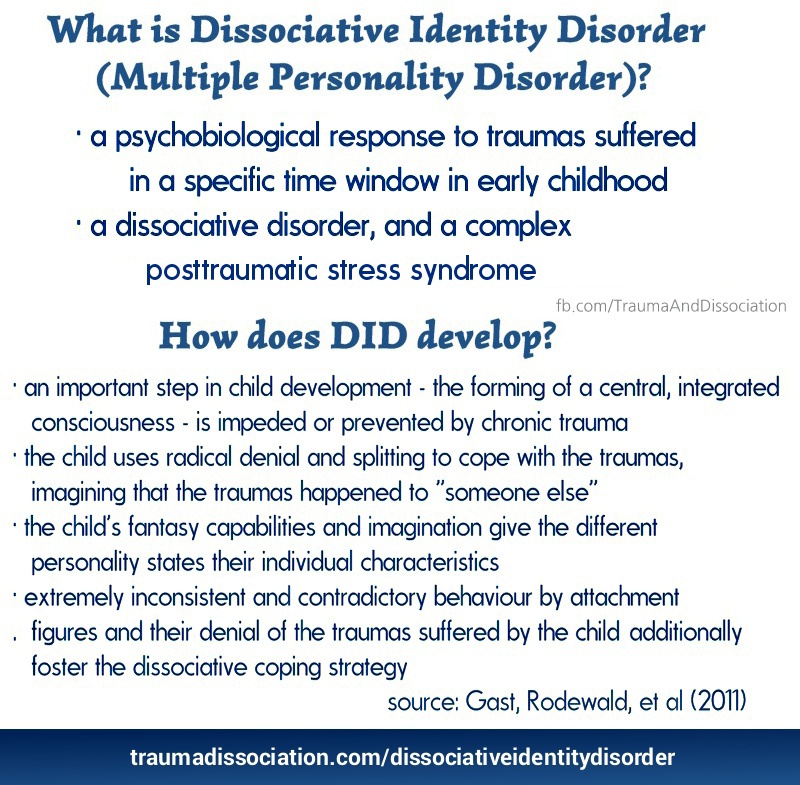 Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
Types of dissociative identity disorder
There are several types of dissociative disorders, which are characterized by different symptoms and manifestations. One of them is dissociative fugue, a disorder in which a person can find himself in a completely unfamiliar place and not remember how he got there. In this case, a person may forget some important information about himself and not even remember his name. At the same time, memory for some information, such as literature, science, and other things, can be preserved. In a state of fugue, a person assumes a different personality and identity with a different character, mannerisms and behavior. While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
A person who has a dissociative disorder is actually suffering a lot from their condition.
Another type of dissociative disorder is the presence of several personalities in which a person finds himself in turn or simultaneously. At such moments, he disconnects from himself and stops feeling his own body, and also cannot see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments, and behave in completely different ways. Often these personalities can even have different physiological manifestations. For example, while in one personality, a person can see poorly and wear glasses, and in another, have excellent vision and walk without glasses or lenses (or think that he sees perfectly and does without glasses).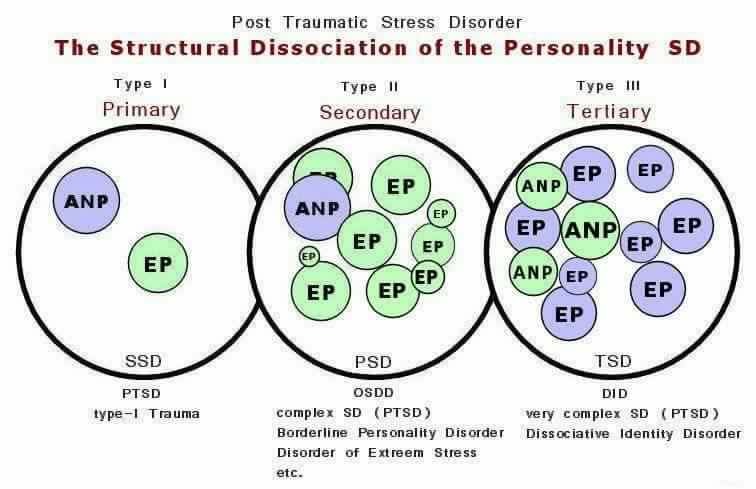 Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Manifestations of dissociative identity disorder
This disease affects both children (adolescents) and adults and presents with similar symptoms. However, dissociative disorder with multiple personalities in adolescents is quite rare. In old age, dissociation practically does not develop. When a specialist suspects a person of dissociative identity disorder, he usually asks if it happened that the person suddenly found himself in some place and did not understand how he got there. Also, the patient may suddenly speak in a completely different voice, he may have a different handwriting. For example, a person who has one of his personalities as a child may suddenly begin to write in a child's handwriting. Such phenomenal manifestations can be evoked in a patient suffering from dissociative personality disorder, and in a state of hypnosis.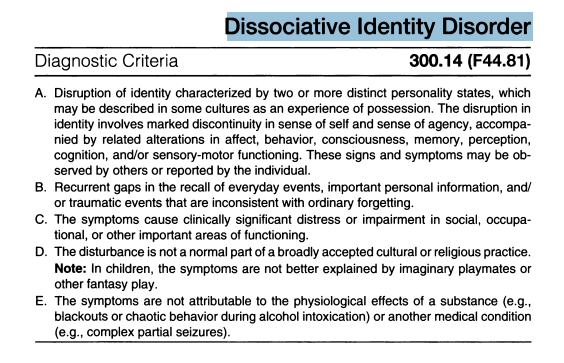 That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
See also
Myths about hypnosis
A person who has a dissociative disorder is actually very distressed by his condition. He sees the negative or dismissive attitude of those around him: they look at him strangely, they reject him, no one finds a common language with him, because of him the family can collapse, and so on. At the moment of a dissociative state, a person does not have the opportunity to critically look at himself and his own behavior. That is, in a situation where one of the alternative personalities appears, he is in an inadequate state.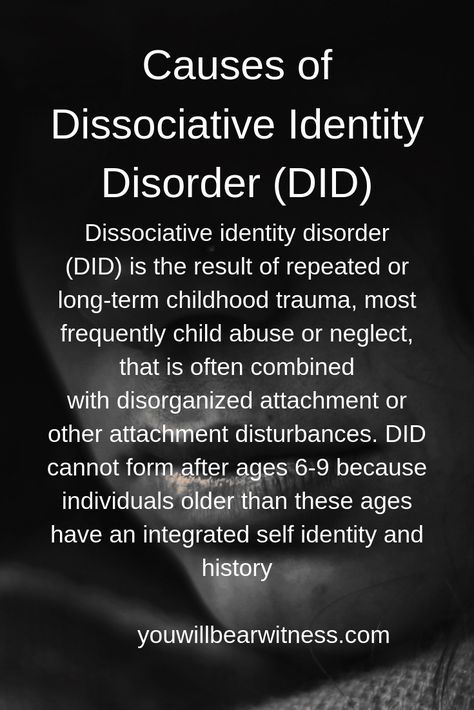
The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence.
Dissociation is one of three conditions in which the patient is exempt from criminal liability, along with psychosis and mental retardation. There were cases when people in a dissociative state committed murder and rape. In such situations, even taking into account the severity of the crimes, patients are not sent to prison, but are sent to a psychiatric hospital or, in extreme cases, to a special ward of the psychiatric department of the prison.
Causes of dissociative identity disorder
Scientists have not yet found the genetic causes of dissociative personality disorder. The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence. However, even this theory does not explain all 100% of cases of dissociative states. There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
Diagnosis of dissociative personality disorder
Diagnosis of dissociative identity disorder is made through clinical interviews with several specialists. Sometimes the diagnosis requires not one, but several meetings with psychologists and psychiatrists, so that they have the opportunity to identify different aspects of the disorder, look at the patient's condition from several points of view and assemble a consultation. However, the specialist who identifies this disorder must have a great deal of experience and qualifications, since this disease can often be confused with others. In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder.
In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder.
Medications do not cure dissociative identity disorder, but only relieve some of the symptoms.
See also
Mental norm and pathology
A separate task for a specialist in the process of diagnosing dissociation in a child is to distinguish diseases from the presence of imaginary friends in a child, which very often appear in perfectly healthy children at a certain age. To do this, a specialist must be highly qualified in the field of developmental psychology and clearly be able to recognize a dissociative disorder not only in adults, but also in children.
Treatment for dissociative identity disorder
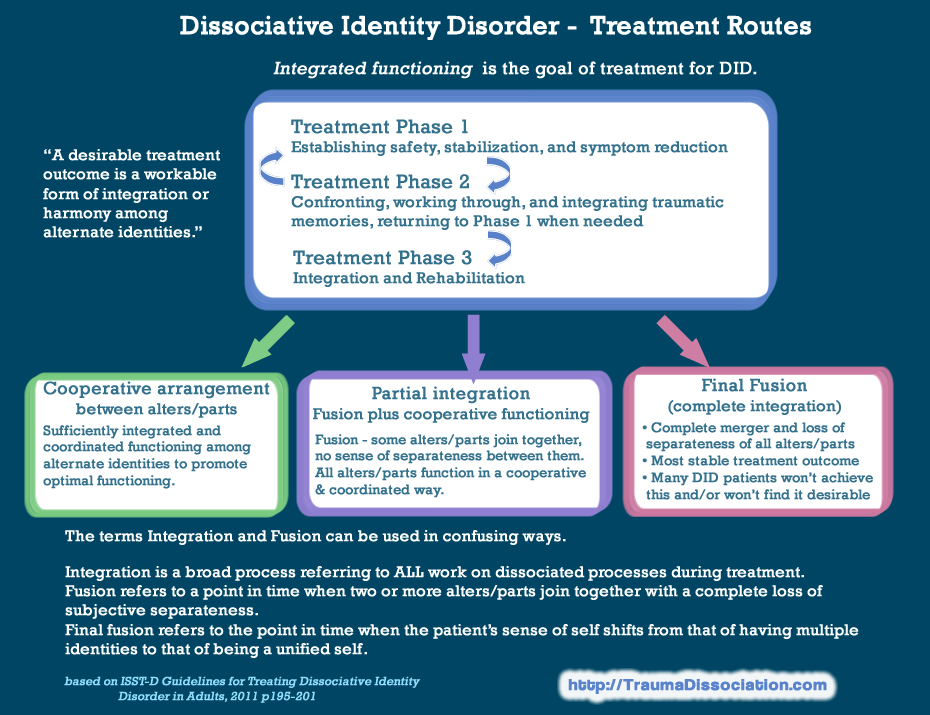
The main treatment for dissociative identity disorder is hypnosis.