The following would be a cognitive symptom of schizophrenia
NIMH » Schizophrenia
Overview
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective treatments are available. Many people who receive treatment can engage in school or work, achieve independence, and enjoy personal relationships.
Onset and Symptoms
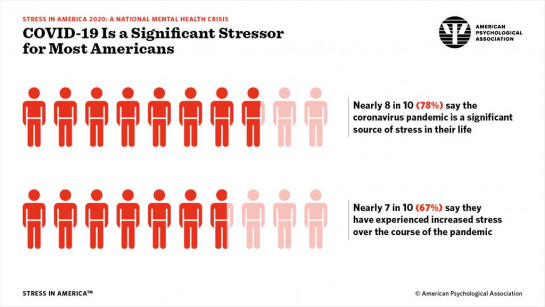
The Centers for Disease Control and Prevention (CDC) has recognized that having certain mental disorders, including depression and schizophrenia, can make people more likely to get severely ill from COVID-19. Learn more about getting help and finding a health care provider on NIMH's Help for Mental Illnesses webpage.
It’s important to recognize the symptoms of schizophrenia and seek help as early as possible. People with schizophrenia are usually diagnosed between the ages of 16 and 30, after the first episode of psychosis. Starting treatment as soon as possible following the first episode of psychosis is an important step toward recovery. However, research shows that gradual changes in thinking, mood, and social functioning often appear before the first episode of psychosis. Schizophrenia is rare in younger children.
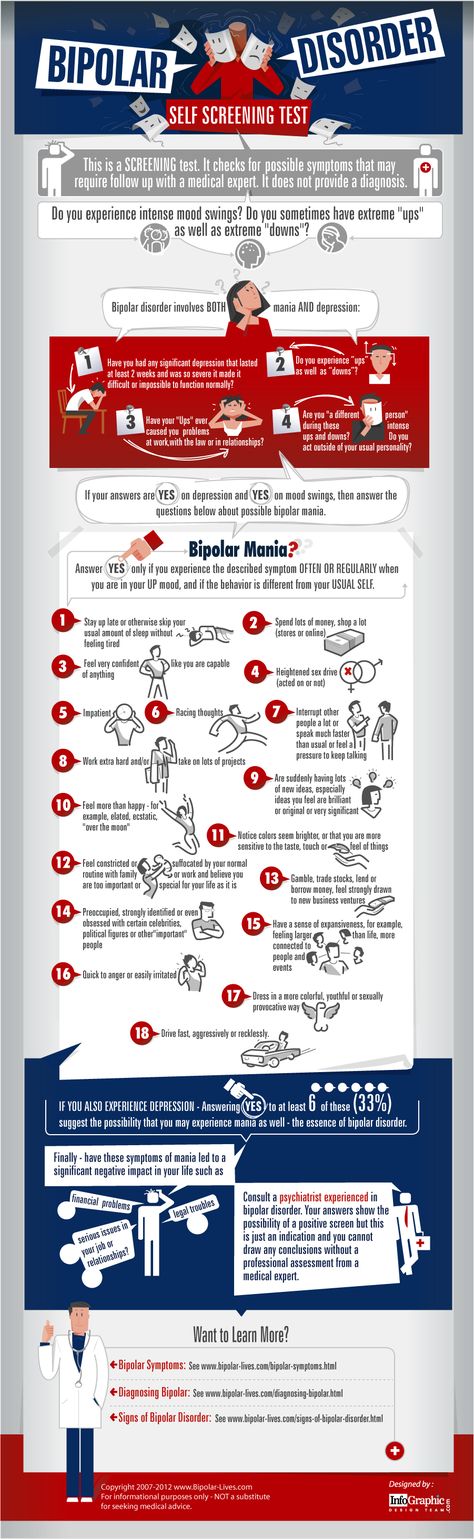
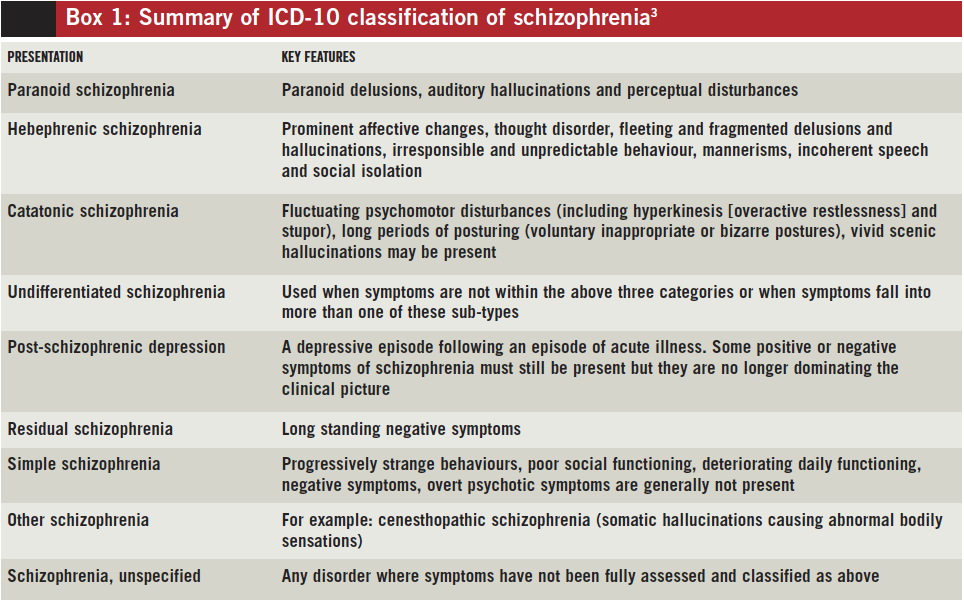
Schizophrenia symptoms can differ from person to person, but they generally fall into three main categories: psychotic, negative, and cognitive.
Psychotic symptoms include changes in the way a person thinks, acts, and experiences the world. People with psychotic symptoms may lose a shared sense of reality with others and experience the world in a distorted way. For some people, these symptoms come and go. For others, the symptoms become stable over time. Psychotic symptoms include:
- Hallucinations: When a person sees, hears, smells, tastes, or feels things that are not actually there.
 Hearing voices is common for people with schizophrenia. People who hear voices may hear them for a long time before family or friends notice a problem.
Hearing voices is common for people with schizophrenia. People who hear voices may hear them for a long time before family or friends notice a problem. - Delusions: When a person has strong beliefs that are not true and may seem irrational to others. For example, individuals experiencing delusions may believe that people on the radio and television are sending special messages that require a certain response, or they may believe that they are in danger or that others are trying to hurt them.
- Thought disorder: When a person has ways of thinking that are unusual or illogical. People with thought disorder may have trouble organizing their thoughts and speech. Sometimes a person will stop talking in the middle of a thought, jump from topic to topic, or make up words that have no meaning.
- Movement disorder: When a person exhibits abnormal body movements. People with movement disorder may repeat certain motions over and over.
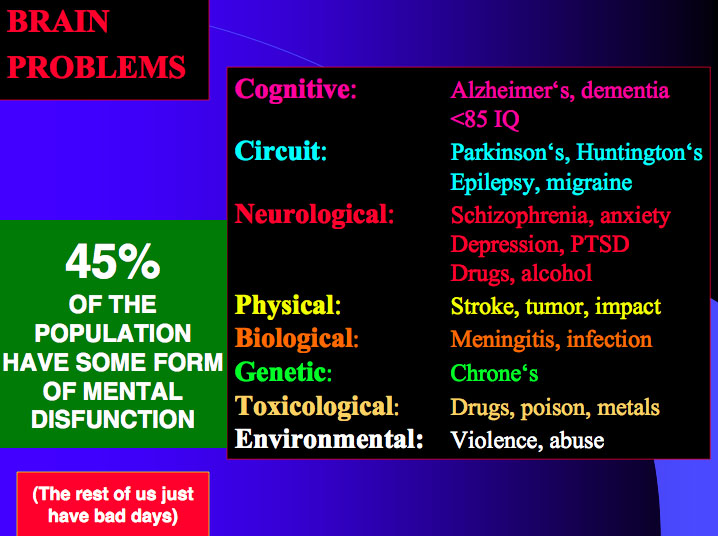
Negative symptoms include loss of motivation, loss of interest or enjoyment in daily activities, withdrawal from social life, difficulty showing emotions, and difficulty functioning normally. Negative symptoms include:
- Having trouble planning and sticking with activities, such as grocery shopping
- Having trouble anticipating and feeling pleasure in everyday life
- Talking in a dull voice and showing limited facial expression
- Avoiding social interaction or interacting in socially awkward ways
- Having very low energy and spending a lot of time in passive activities. In extreme cases, a person might stop moving or talking for a while, which is a rare condition called catatonia.
These symptoms are sometimes mistaken for symptoms of depression or other mental illnesses.
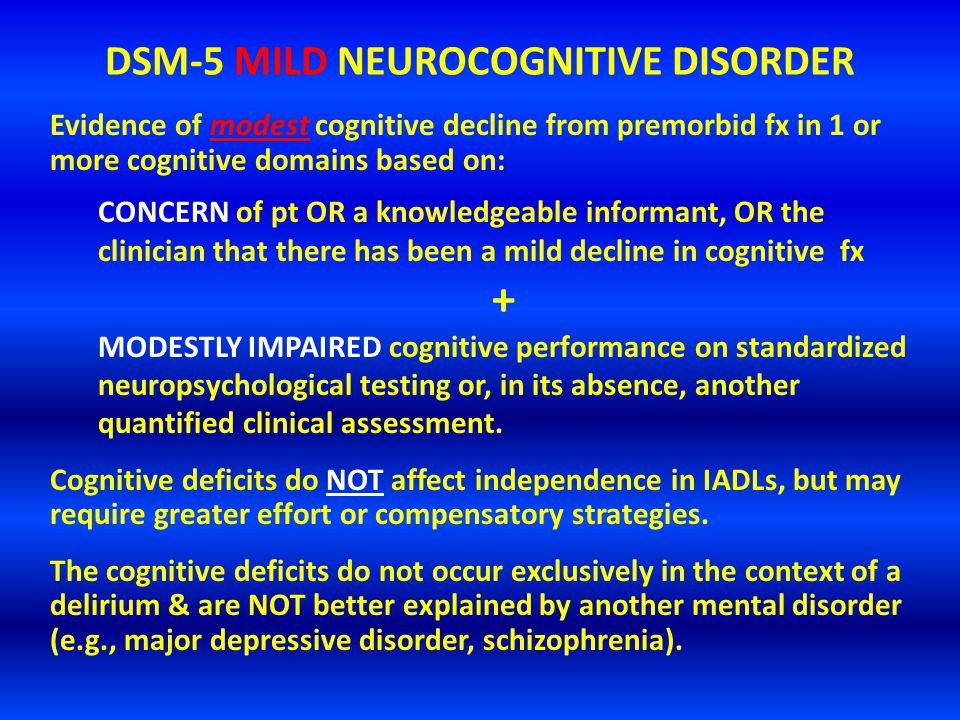
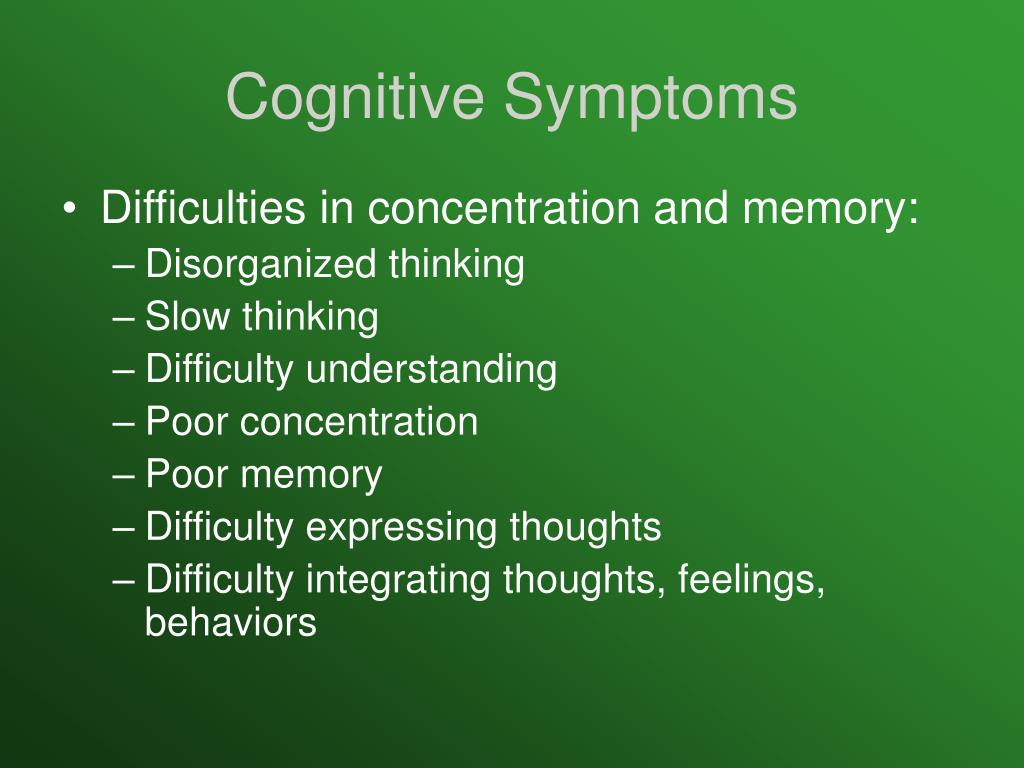
Cognitive symptoms include problems in attention, concentration, and memory. These symptoms can make it hard to follow a conversation, learn new things, or remember appointments.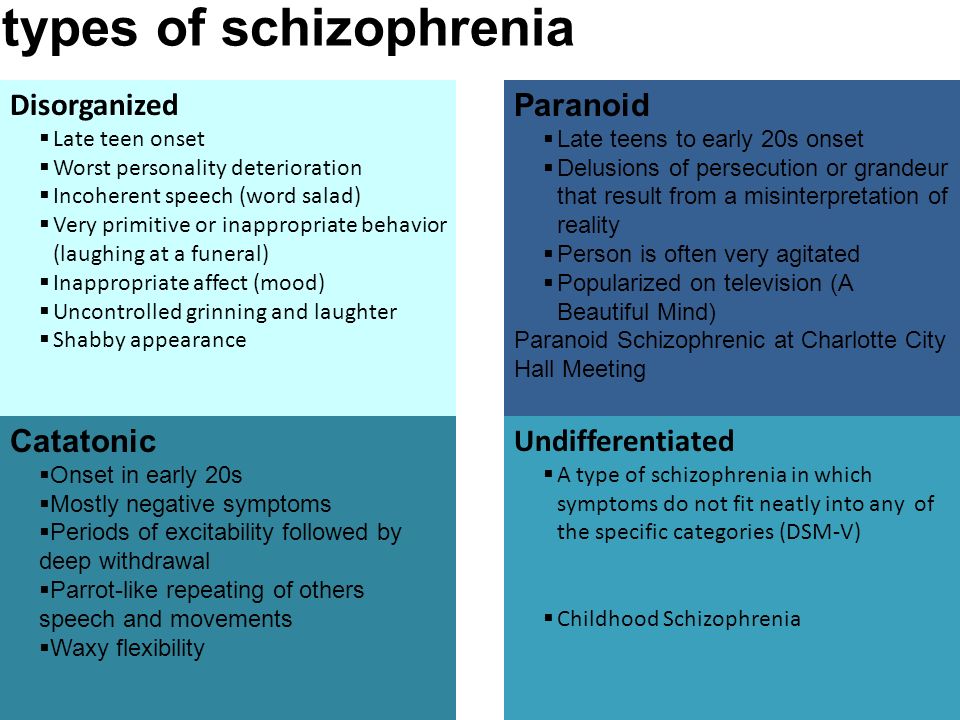 A person’s level of cognitive functioning is one of the best predictors of their day-to-day functioning. Cognitive functioning is evaluated using specific tests. Cognitive symptoms include:
A person’s level of cognitive functioning is one of the best predictors of their day-to-day functioning. Cognitive functioning is evaluated using specific tests. Cognitive symptoms include:
- Having trouble processing information to make decisions
- Having trouble using information immediately after learning it
- Having trouble focusing or paying attention
Risk of Violence
Most people with schizophrenia are not violent. Overall, people with schizophrenia are more likely than those without the illness to be harmed by others. For people with schizophrenia, the risk of self-harm and of violence to others is greatest when the illness is untreated. It is important to help people who are showing symptoms to get treatment as quickly as possible.
Schizophrenia vs. Dissociative Identity Disorder
Although some of the signs may seem similar on the surface, schizophrenia is not dissociative identity disorder (which used to be called multiple personality disorder or split personality).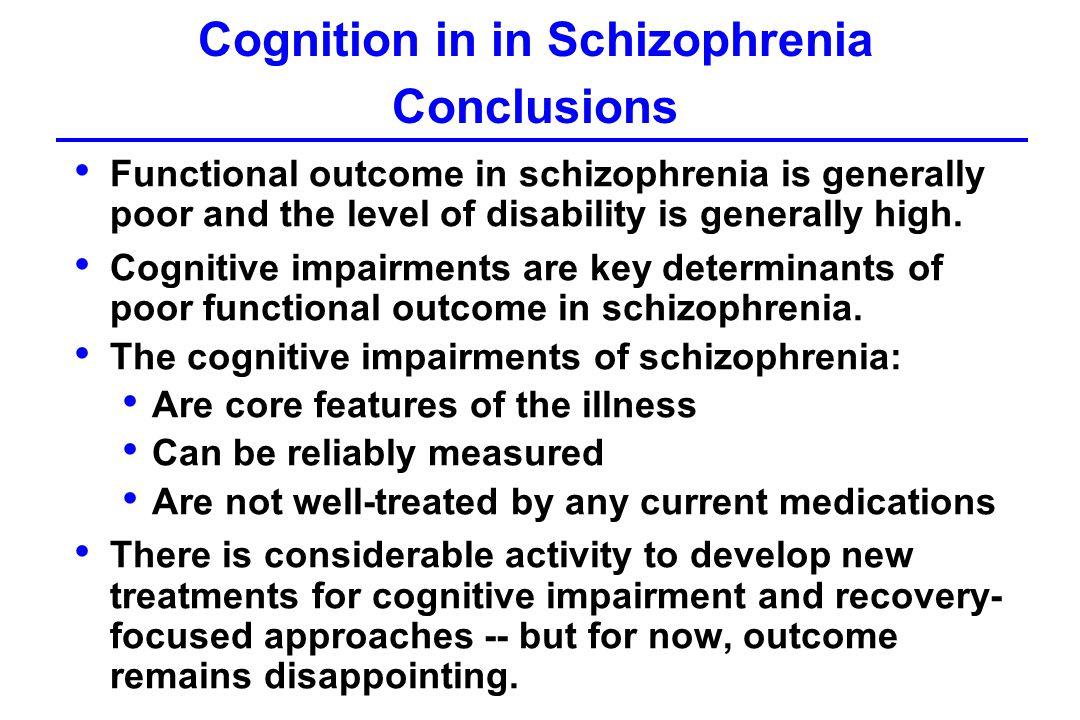 People with dissociative identity disorder have two or more distinct identities
that are present and that alternately take control of them.
People with dissociative identity disorder have two or more distinct identities
that are present and that alternately take control of them.
Risk Factors
Several factors may contribute to a person’s risk of developing schizophrenia, including:
Genetics: Schizophrenia sometimes runs in families. However, just because one family member has schizophrenia, it does not mean that other members of the family also will have it. Studies suggest that many different genes may increase a person’s chances of developing schizophrenia, but that no single gene causes the disorder by itself.
Environment: Research suggests that a combination of genetic factors and aspects of a person’s environment and life experiences may play a role in the development of schizophrenia. These environmental factors that may include living in poverty, stressful or dangerous surroundings, and exposure to viruses or nutritional problems before birth.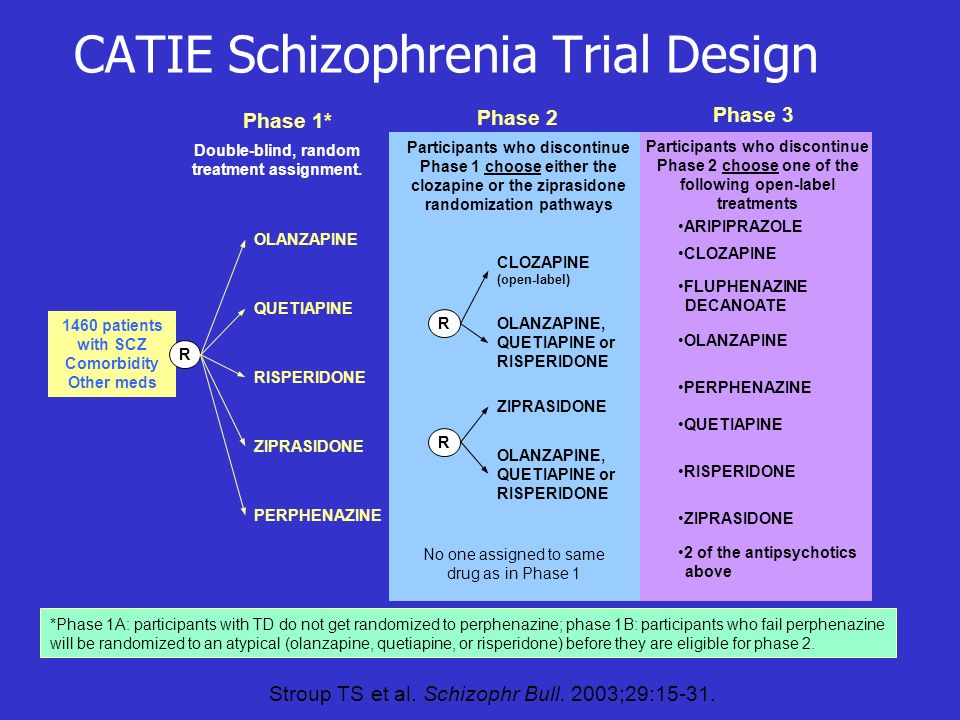
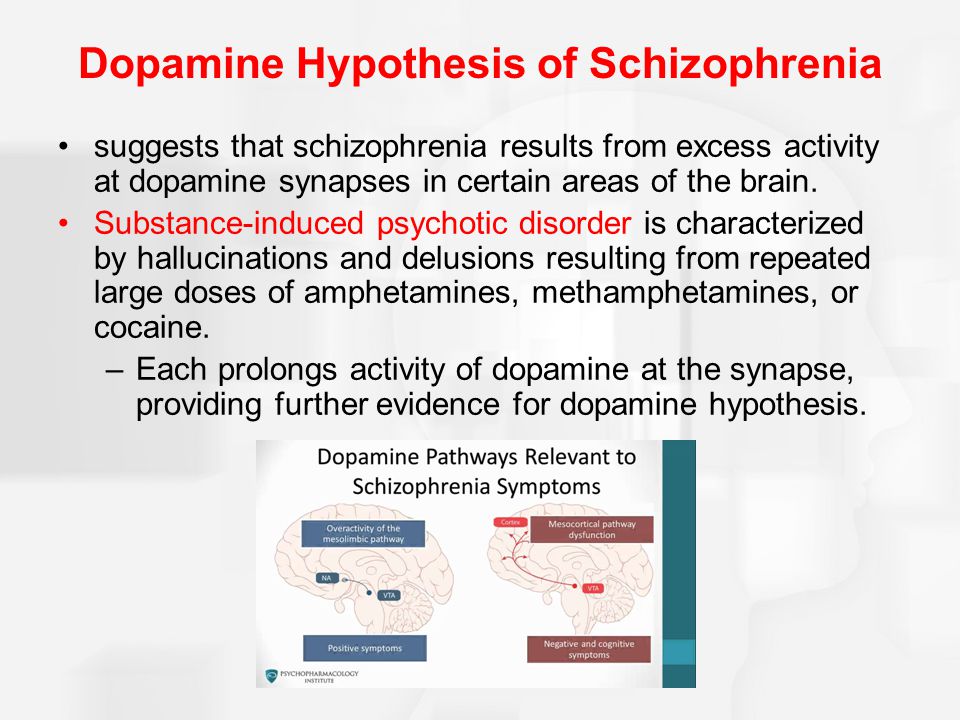
Brain structure and function: Research shows that people with schizophrenia may be more likely to have differences in the size of certain brain areas and in connections between brain areas. Some of these brain differences may develop before birth. Researchers are working to better understand how brain structure and function may relate to schizophrenia.
Treatments and Therapies
Current treatments for schizophrenia focus on helping individuals manage their symptoms, improve day-to-day functioning, and achieve personal life goals, such as completing education, pursuing a career, and having fulfilling relationships.
Antipsychotic Medications
Antipsychotic medications can help make psychotic symptoms less intense and less frequent. These medications are usually taken every day in a pill or liquid forms. Some antipsychotic medications are given as injections once or twice a month.
If a person’s symptoms do not improve with usual antipsychotic medications, they may be prescribed clozapine.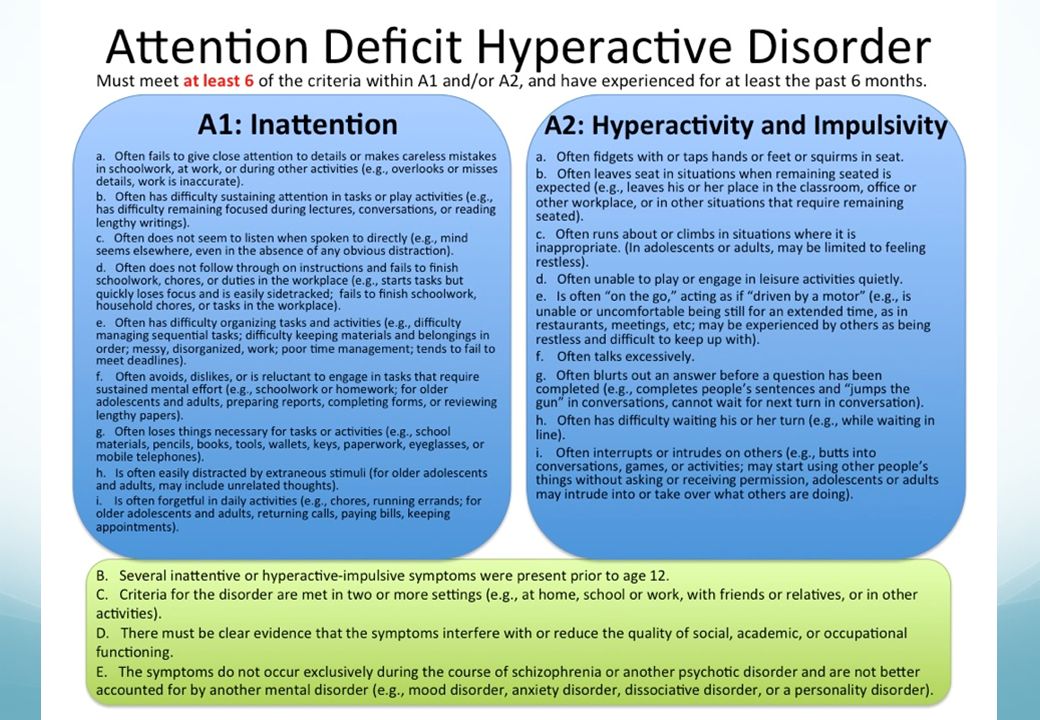 People who take clozapine must have regular blood tests to check for a potentially dangerous side effect that occurs in 1-2% of patients.
People who take clozapine must have regular blood tests to check for a potentially dangerous side effect that occurs in 1-2% of patients.
People respond to antipsychotic medications in different ways. It is important to report any side effects to a health care provider. Many people taking antipsychotic medications experience side effects such as weight gain, dry mouth, restlessness, and drowsiness when they start taking these medications. Some of these side effects may go away over time, while others may last.
Shared decision making between doctors and patients is the recommended strategy for determining the best type of medication or medication combination and the right dose. You can find the latest information on warnings, patient medication guides, or newly approved medications on the U.S. Food and Drug Administration (FDA) website.
Psychosocial Treatments
Psychosocial treatments help people find solutions to everyday challenges and manage symptoms while attending school, working, and forming relationships.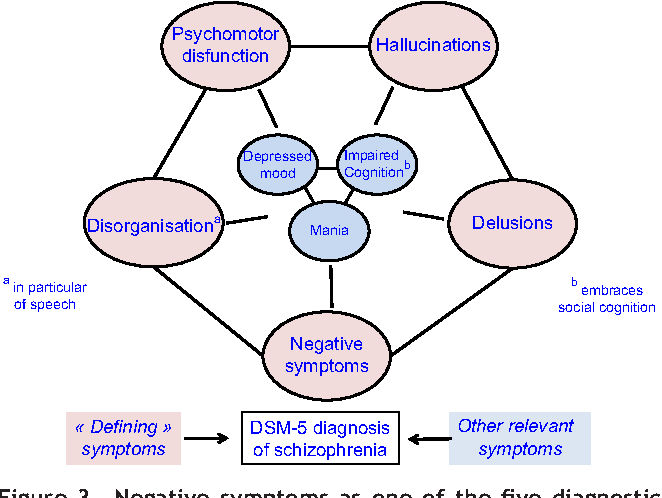 These treatments are often used together with antipsychotic medication. People who participate in regular psychosocial treatment are less likely to have symptoms reoccur or to be hospitalized.
These treatments are often used together with antipsychotic medication. People who participate in regular psychosocial treatment are less likely to have symptoms reoccur or to be hospitalized.
Examples of this kind of treatment include cognitive behavioral therapy, behavioral skills training, supported employment, and cognitive remediation interventions.
You can find information about psychosocial treatments on the National Institute of Mental Health (NIMH) psychotherapies webpage.
Family Education and Support
Educational programs can help family and friends learn about symptoms of schizophrenia, treatment options, and strategies for helping loved ones with the illness. These programs can help friends and family manage their distress, boost their own coping skills, and strengthen their ability to provide support. For more information about family-based services in your area, you can visit the family education and support groups page on the National Alliance on Mental Illness website.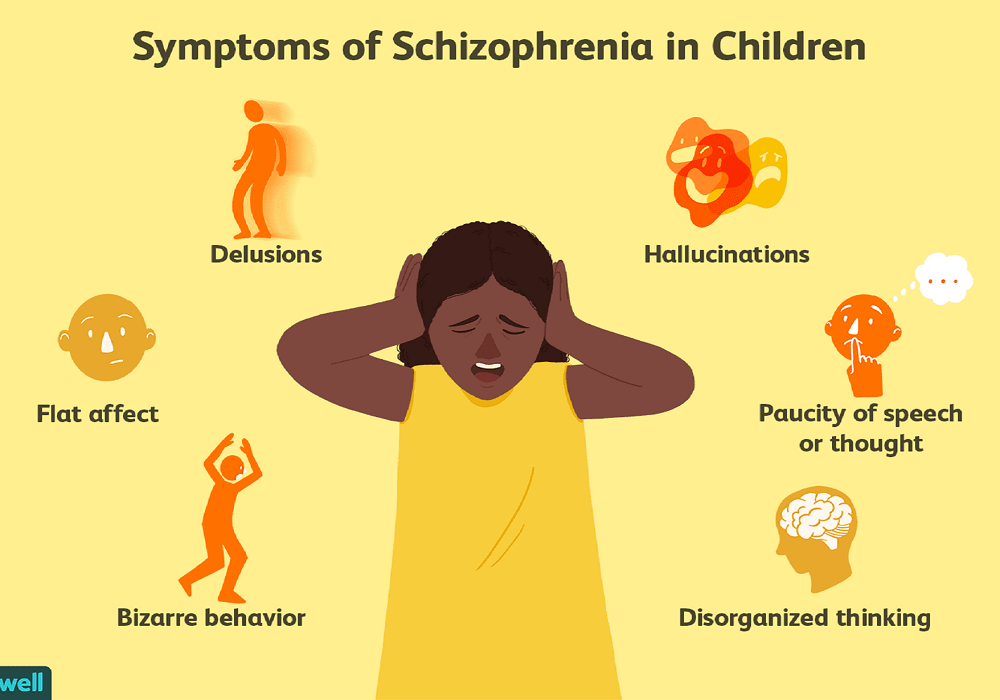
Coordinated Specialty Care
Coordinated specialty care (CSC) programs are recovery-focused programs for people with first episode psychosis, an early stage of schizophrenia. Health professionals and specialists work together as a team to provide CSC, which includes psychotherapy, medication, case management, employment and education support, and family education and support. The treatment team works collaboratively with the individual to make treatment decisions, involving family members as much as possible.
Compared with typical care, CSC is more effective at reducing symptoms, improving quality of life, and increasing involvement in work or school. Check here for more information about CSC programs.
Assertive Community Treatment
Assertive Community Treatment (ACT) is designed especially for individuals with schizophrenia who are likely to experience multiple hospitalizations or homelessness. ACT is usually delivered by a team of health professionals who work together to provide care to patients in the community.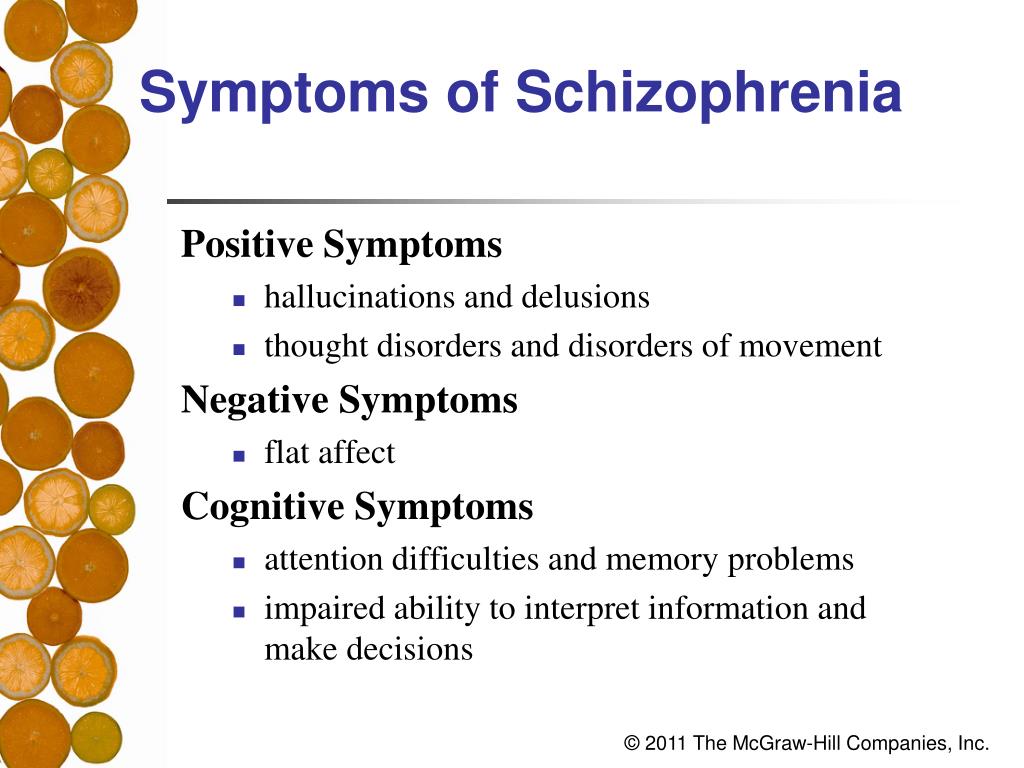 Check here for more information about ACT programs.
Check here for more information about ACT programs.
Treatment for Drug and Alcohol Misuse
It is common for people with schizophrenia to have problems with drugs and alcohol. A treatment program that includes treatment for both schizophrenia and substance use is important for recovery because substance use can interfere with treatment for schizophrenia.
How can I help a friend or relative with schizophrenia?
It can be difficult to know how to help someone who is experiencing psychosis.
Here are some things you can do:
- Help them get treatment and encourage them to stay in treatment.
- Remember that their beliefs or hallucinations seem very real to them.
- Be respectful, supportive, and kind without tolerating dangerous or inappropriate behavior.
- Look for support groups and family education programs, such as those offered by the National Alliance on Mental Illness.
Some symptoms require immediate emergency care. If your loved one is thinking about attempting suicide or otherwise harming themselves or others, seek help right away:
If your loved one is thinking about attempting suicide or otherwise harming themselves or others, seek help right away:
- Call 911 for emergency services or go to the nearest emergency room.
- Call the National Suicide Prevention Lifeline (Lifeline) at 1-800-273-TALK (8255) or text the Crisis Text Line (text HELLO to 741741).
Finding Help
If you’re not sure where to get help, your health care provider is a good place to start. Your health care provider can refer you to a qualified mental health professional, such as a psychiatrist or psychologist who has experience treating schizophrenia. You can learn more about getting help on NIMH's Help for Mental Illness webpage.
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides the Behavioral Health Treatment Services Locator, an online tool to help you find mental health services in your area. You can find information about treatment facilities that offer coordinated specialty care by using SAMHSA’s Early Serious Mental Illness Treatment Locator.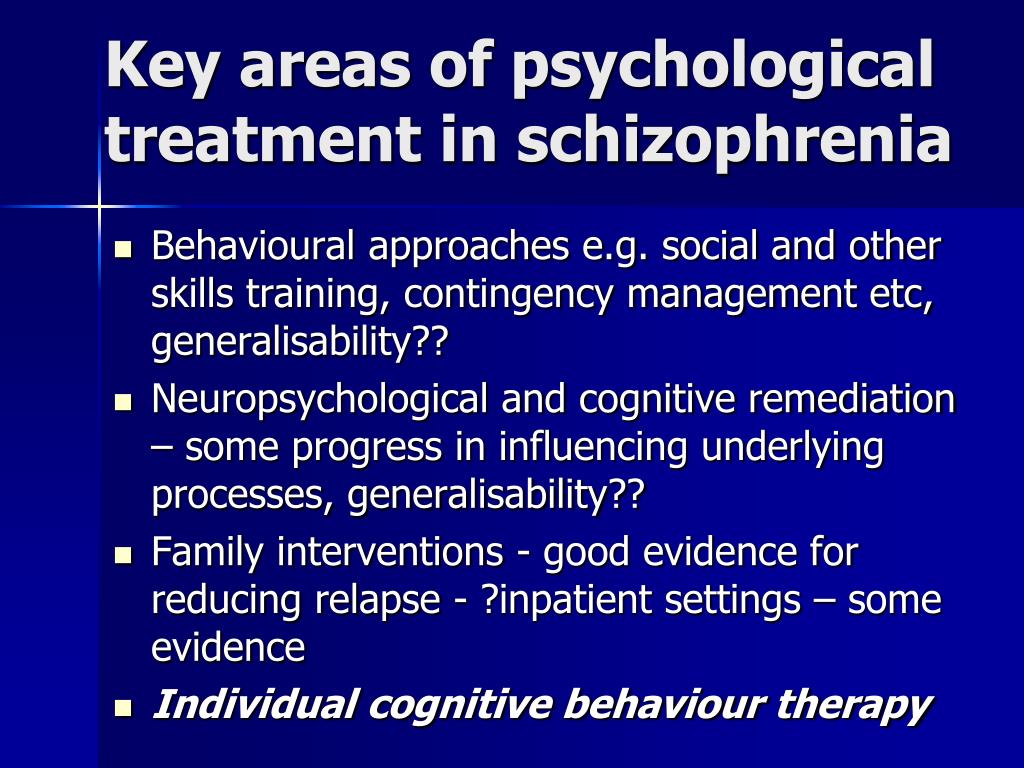
For tips on talking with your health care provider about your mental health and getting the most out of your visit, read NIMH’s fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.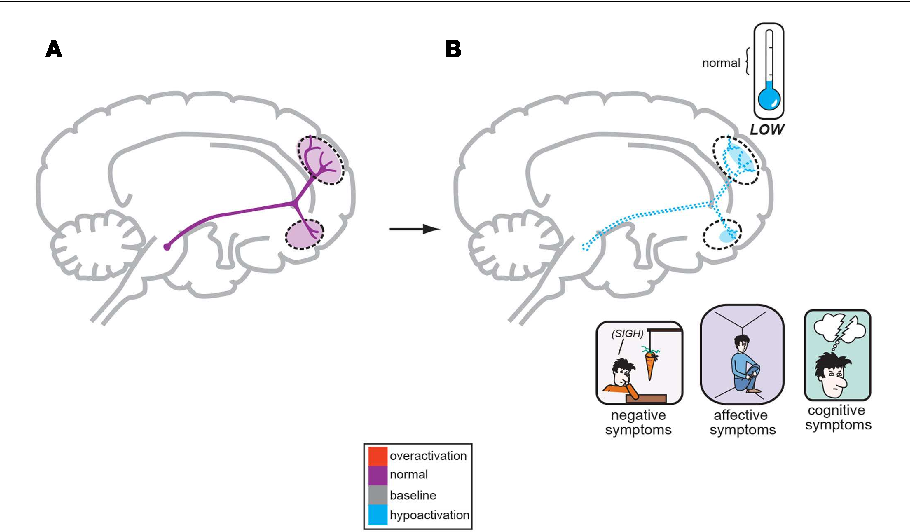
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Schizophrenia: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Schizophrenia: List of studies being conducted on the NIH Campus in Bethesda, MD
Learn More
Free Brochures and Shareable Resources
- Schizophrenia: A brief brochure on schizophrenia that offers basic information on signs and symptoms, treatment, and finding help. Also available en español.
- Understanding Psychosis: A fact sheet that presents information on psychosis, including causes, signs and symptoms, treatment, and resources for help. Also available en español.
- Shareable Resources on Schizophrenia: Help support schizophrenia awareness and education in your community.
 Use these digital resources, including graphics and messages, to spread the word about schizophrenia.
Use these digital resources, including graphics and messages, to spread the word about schizophrenia.
Research and Statistics
- Accelerating Medicines Partnership® Program - Schizophrenia (AMP® SCZ): This AMP public-private collaborative effort aims to promote the development of effective, targeted treatments for those at risk of developing schizophrenia. More information about the program is also available on the AMP SCZ website.
- Early Psychosis Intervention Network (EPINET): This broad research initiative aims to develop models for the effective delivery of coordinated specialty care (CSC) services for early psychosis.
- Journal Articles: This webpage provides information on references and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Psychotic Disorders Research Program: This program supports research into the origins, onset, course, and outcome of schizophrenia spectrum disorders and other psychotic illnesses.
- Recovery After an Initial Schizophrenia Episode (RAISE): The NIMH RAISE research initiative included two studies examining different aspects of coordinated specialty care treatments for people who were experiencing early psychosis.
- Schizophrenia Statistics: This webpage provides information on the best statistics currently available on the prevalence and treatment of schizophrenia in the U.S.
Last Reviewed: May 2022
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge. Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
Cognitive Symptoms of Schizophrenia: Types and Treatments
Cognitive, negative, and positive are the three types of schizophrenia symptoms. Cognitive symptoms affect how you think and remember.
Negative symptoms represent a decrease in something, such as reduced energy or social withdrawal.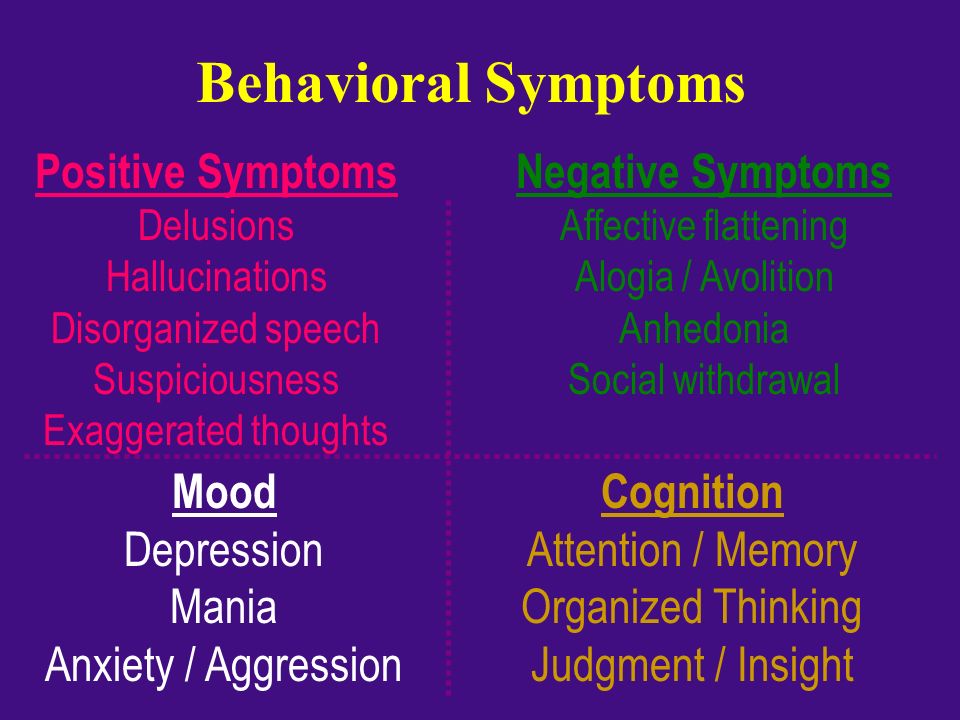 Positive symptoms are those that are new or increased experiences, like delusions or hearing voices.
Positive symptoms are those that are new or increased experiences, like delusions or hearing voices.
Doctors also recognize cognitive symptoms as a third category. Any symptom that affects your thought process is included in this category.
Schizophrenia is chronic and lifelong, but treatable. The earlier treatment is started, the easier it is to manage symptoms.
Doctors identify cognitive symptoms of schizophrenia using neurocognitive tests, which are tests to identify your capabilities across different areas of mental functioning.
Examples of cognitive symptoms of schizophrenia include:
- processing speed
- working memory
- attention and vigilance
- verbal learning
- reasoning and problem solving
- social cognition
The cognitive symptoms of schizophrenia are usually present at the first onset of psychosis, so they’re not a side effect of antipsychotic medication.
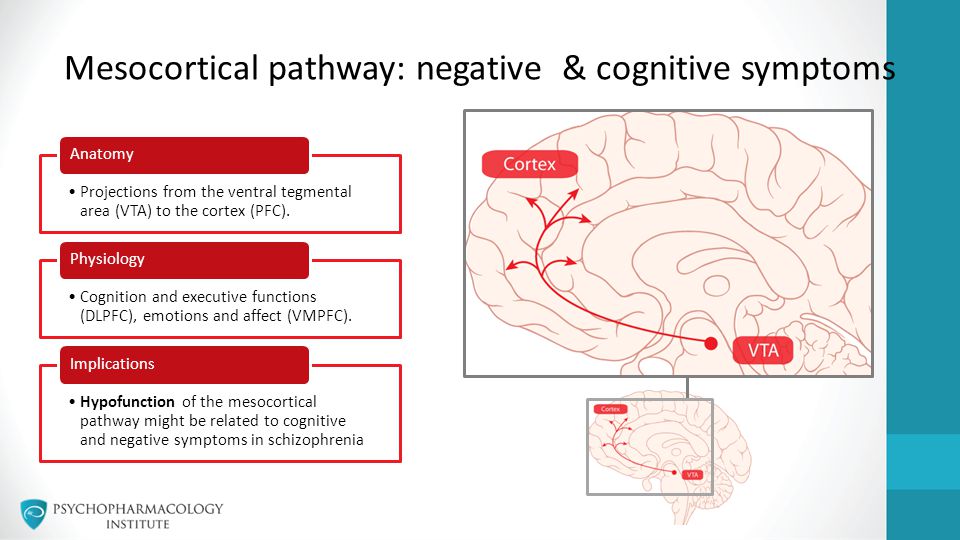
The cognitive symptoms of schizophrenia may, in part, be related to changes in the brain.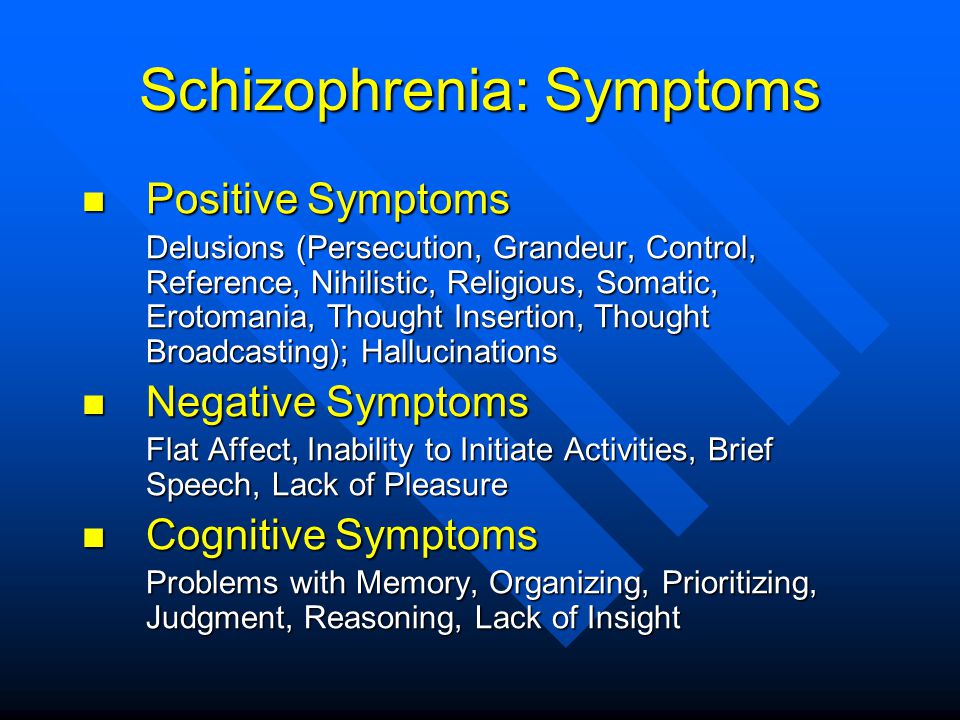 Research, including a 2021 study, shows that people with schizophrenia have reduced cortical thickness, which may contribute to changes in thinking and memory.
Research, including a 2021 study, shows that people with schizophrenia have reduced cortical thickness, which may contribute to changes in thinking and memory.
The cortex is the outer surface of your brain, with gray matter on the outside and white matter underneath. Gray and white matter support cognitive functions like attention, memory, and language.
A 2019 study reported that people with schizophrenia had less brain matter in several areas, including gray matter in the cortex, than people without schizophrenia.
Some people with schizophrenia don’t experience changes in cognitive domains. A 2011 study showed that the people with no cognitive symptoms had a brain cortex similar to people without schizophrenia.
The rate at which you receive, assess, and respond to new information is called your processing speed. This cognitive quality impacts how quickly you think, learn, and respond to your environment.
The volume of white matter in the brain affects processing speed.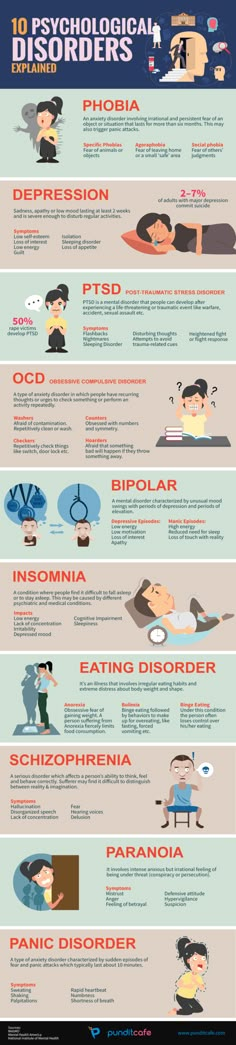 White matter contains nerve cell axons, which transmit signals through brain cells.
White matter contains nerve cell axons, which transmit signals through brain cells.
Axons are covered with a substance called myelin, which helps to speed up the transmission of signals. Schizophrenia is associated with disruptions in myelin, resulting in less white matter and a slower processing speed.
If you have slow processing speed, you may need extra time to respond to questions. You might feel overwhelmed with too much information at once, and you might need instructions or information repeated.
Working memory is the information you retain to complete an immediate task. Examples of what you might hold in your working memory include:
- multistep instructions
- a short shopping list
- a new phone number you don’t already have memorized
- mental math
Impaired working memory is a common characteristic of schizophrenia. It’s linked to lower levels of activity in an area of the brain called the prefrontal cortex.
If you have trouble repeating something you’ve just heard or remembering directions, this might indicate difficulties with your working memory.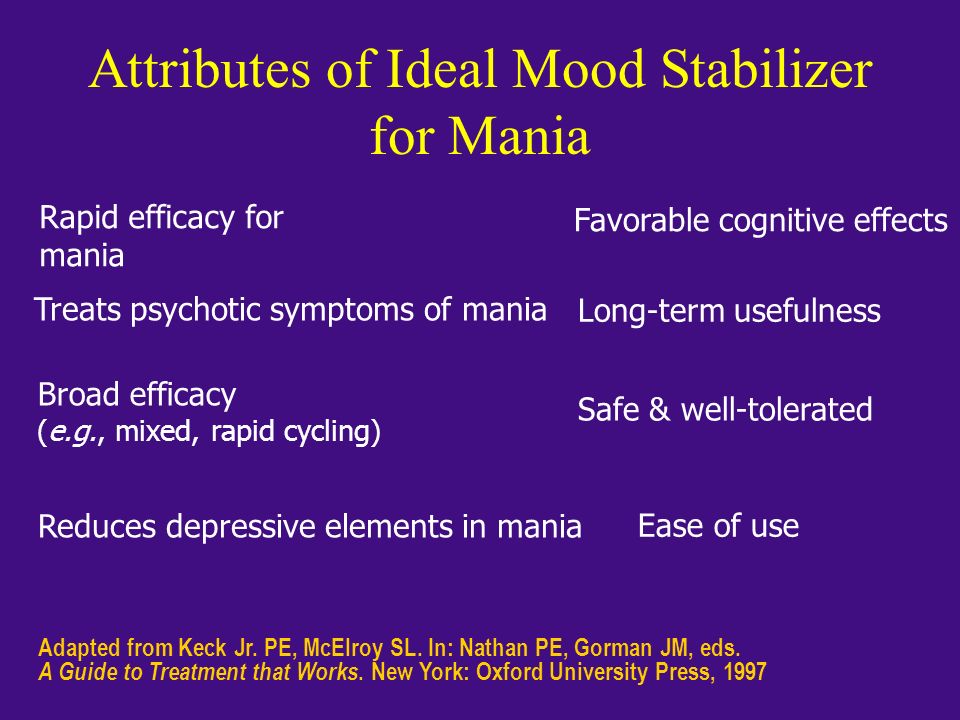
Attention and vigilance both mean to focus on something. With attention, you focus on a task or something that is happening, whereas vigilance means to focus on watching for something that might happen.
If you have schizophrenia, you may have reduced attention and vigilance ability regardless of whether you’re experiencing psychosis.
Verbal learning is based on verbal elements like:
- words
- syllables
- letters
- digits
A verbal learner is someone who remembers what they’ve heard and read, and who expresses themselves well using language.
A 2018 review of 17 studies linked immediate and delayed verbal learning to reductions in the volume of the brain region called the hippocampus — a key area for memory. Dysfunction in this area, resulting in reduced verbal learning, is one of the cognitive symptoms of schizophrenia.
In addition, a 2000 study shows that decreases in brain activity — specifically in the prefrontal cortex — is associated with verbal memory abilities.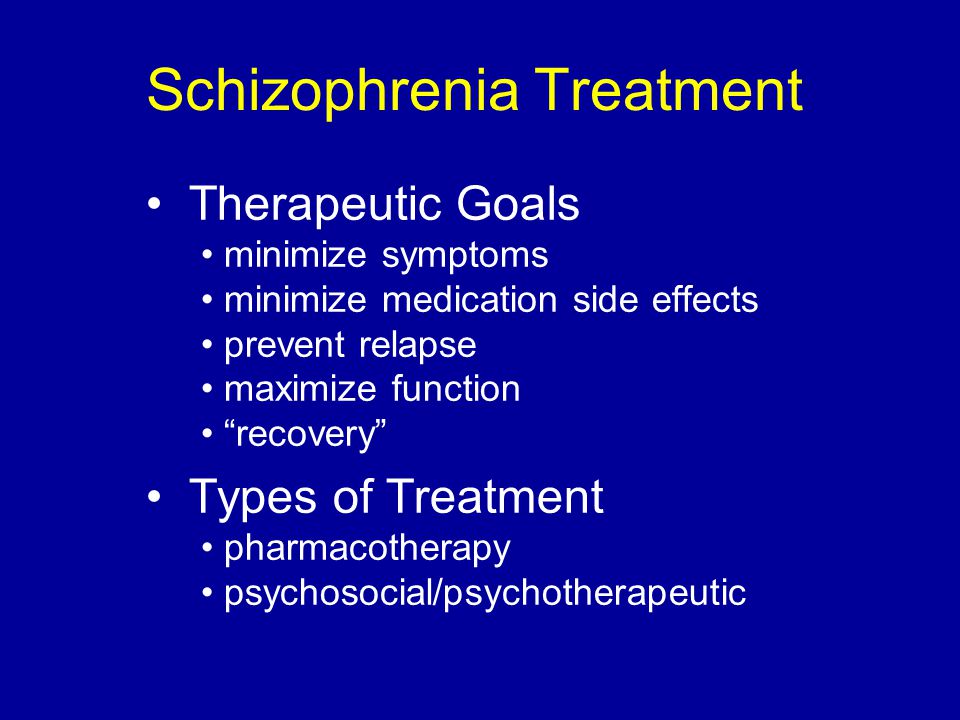
Executive functioning includes higher level cognitive abilities like reasoning and problem solving, a complex skill with multiple steps. To solve a problem you must first identify and analyze it, and ultimately find a solution.
Reasoning stems from perception. A person with schizophrenia who experiences psychosis may have trouble identifying the truth from their hallucinations and delusions. This makes it difficult to perform reasoning tasks.
When we interact with people, our brains process and store information about them. We then use this information to understand others and to decide how to interact with them. This is called social cognition.
For example, social cognition is how we understand another person’s beliefs and attitudes about us and the world. It’s also how we let others know about our emotions, and how we communicate our emotions to others.
Social cognitive impairment can cause issues with daily functioning. If you have schizophrenia, you may have difficulties in social cognition areas that make it difficult to interact with others, like:
- regulating your emotions
- understanding the feelings of others, known as mentalizing
- noticing emotions and social signals in other people’s faces and voices
Schizophrenia is a complex condition with treatments that aim to help with positive, negative, and cognitive symptoms.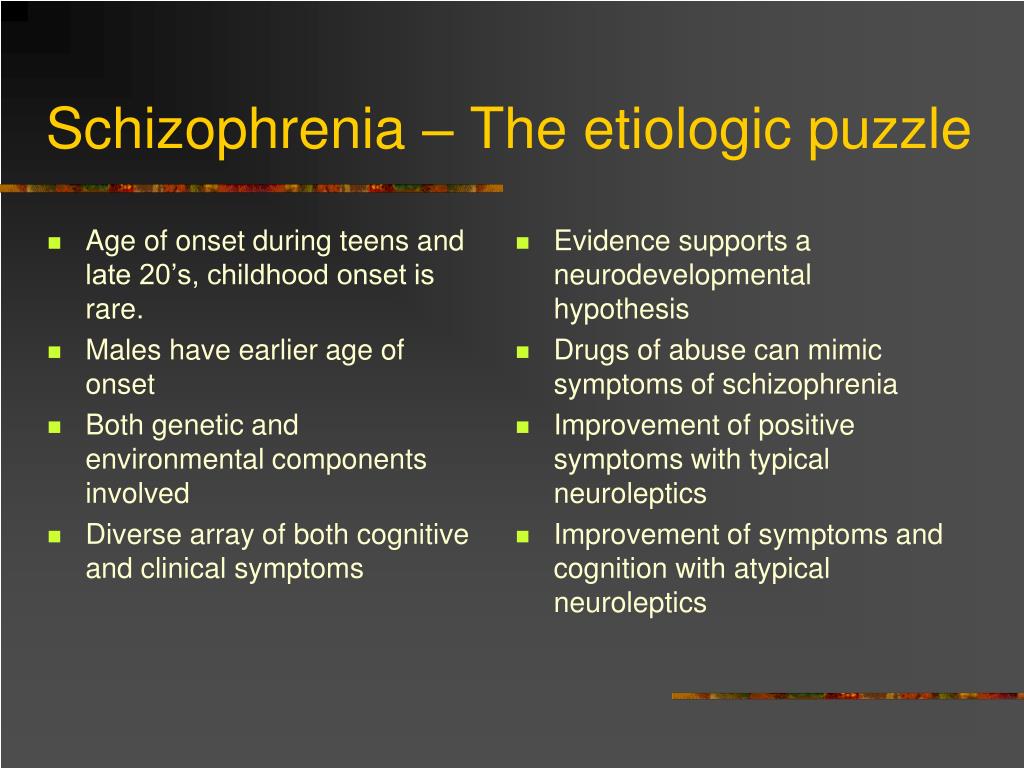
Medication and therapy are common treatment strategies. For cognitive symptoms, executive function training may also help, though it usually takes several months to take effect.
Medication
Unlike the positive and negative symptoms, the cognitive symptoms of schizophrenia are less responsive to antipsychotic medications.
However, some newer antipsychotic medications may be helpful in treating the cognitive impairment caused by schizophrenia. These include:
- Paliperidrone
- Lurasidone
- Aripiprazole
- Ziprasidone
- BL-1020
Research is ongoing, with other medications emerging as potential cognitive symptom treatments. These include:
- Varenicline
- Encenicline
- D-serine
- Sodium benzoate
- L-carnosine
- Raloxifene
Sex differences exist in schizophrenia, with males developing the condition younger than females. 2017 research suggests that estrogen might have a neuroprotective (brain-based) effect against cognitive symptoms.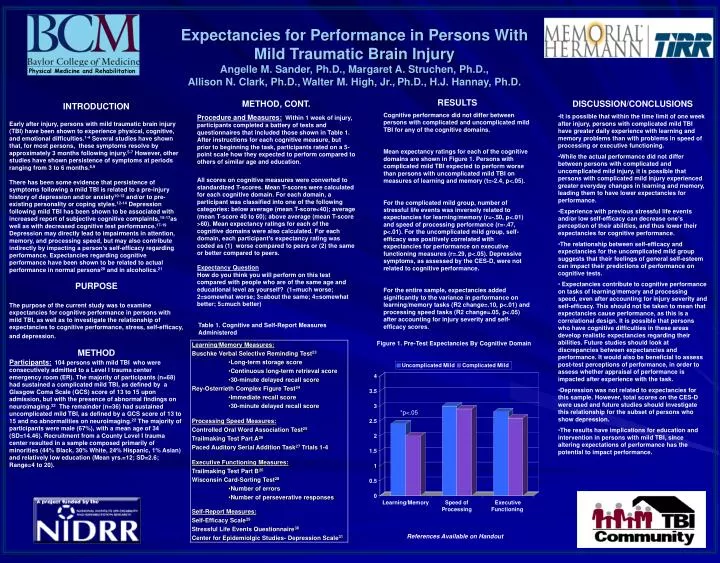
Psychotherapy
Cognitive enhancement therapy
Cognitive enhancement therapy (CET) works toward the goal of improving the functioning of the prefrontal brain. This is one of the areas that causes cognitive symptoms because of reduced function.
A small 18-month randomized trial showed improvements to the prefrontal cortex, limbic, and striatal brain regions in participants with schizophrenia who underwent CET.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is effective for supporting people with many mental health issues. Your therapist helps you identify thoughts and patterns of thought that lead to distress and counterproductive behavior. You then work with your therapist to reshape those thoughts into those that create a positive and proactive mindset.
Social cognitive training
Many people with schizophrenia report a need for more social interaction. Social cognitive training aims to improve social cognition and social abilities in people with schizophrenia.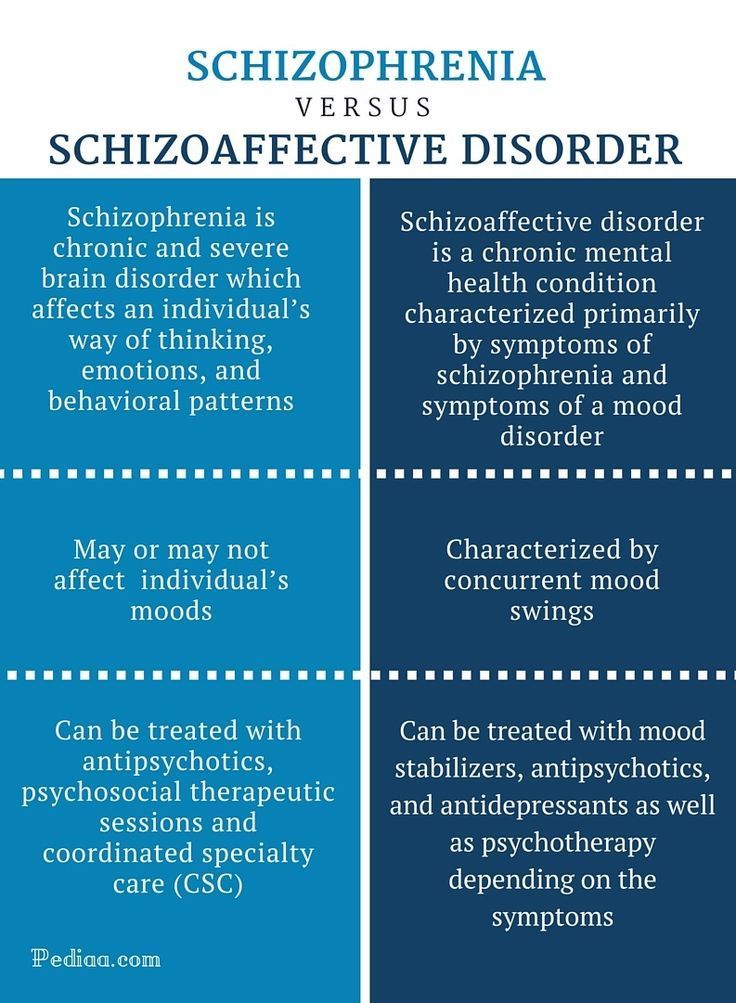
This therapy helps you understand and perceive the emotions of others, figure out social situations, and then helps you put this into practice.
Family support and education
With support and education, family members and caregivers are better equipped to navigate the landscape of a schizophrenia diagnosis. Learning to recognize symptoms, combined with strategies that are proven to help, can reduce the stress of managing schizophrenia.
Schizophrenia is a serious and complex condition, but there is treatment and support available.
If you or someone you know is newly diagnosed and is looking for a treatment facility, the Substance Abuse and Mental Health Services Administration (SAMHSA) has a treatment locator directory and a behavioral health services locator you can try.
SAMHSA also has a national helpline at 800-662-HELP (4357).
The Schizophrenia and Psychosis Action Alliance has a support group finder tool where you can join a group via conference call or in person.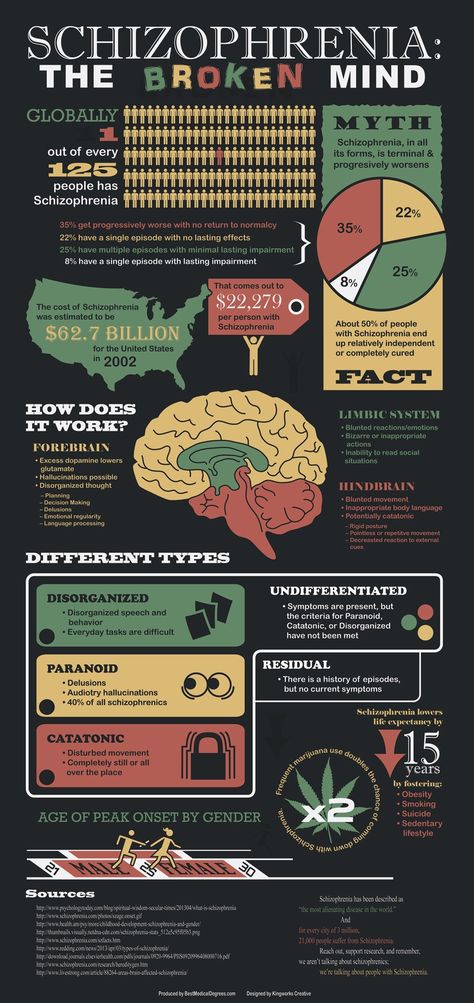
The National Suicide Prevention Lifeline at 800-273-8255 is available 24/7 with free confidential support for anyone in distress. Text HOME to 741741 to reach the Crisis Text Line where you can speak to a crisis counselor 24/7.
Schizophrenia
Schizophrenia- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- E
- e
- ё 9000
- x
- C
- h
- Sh
9000 WHO in countries » - Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Globally, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- sensation of external influence, control or passivity: the presence in the patient of the sensation that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness by someone else's will, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2).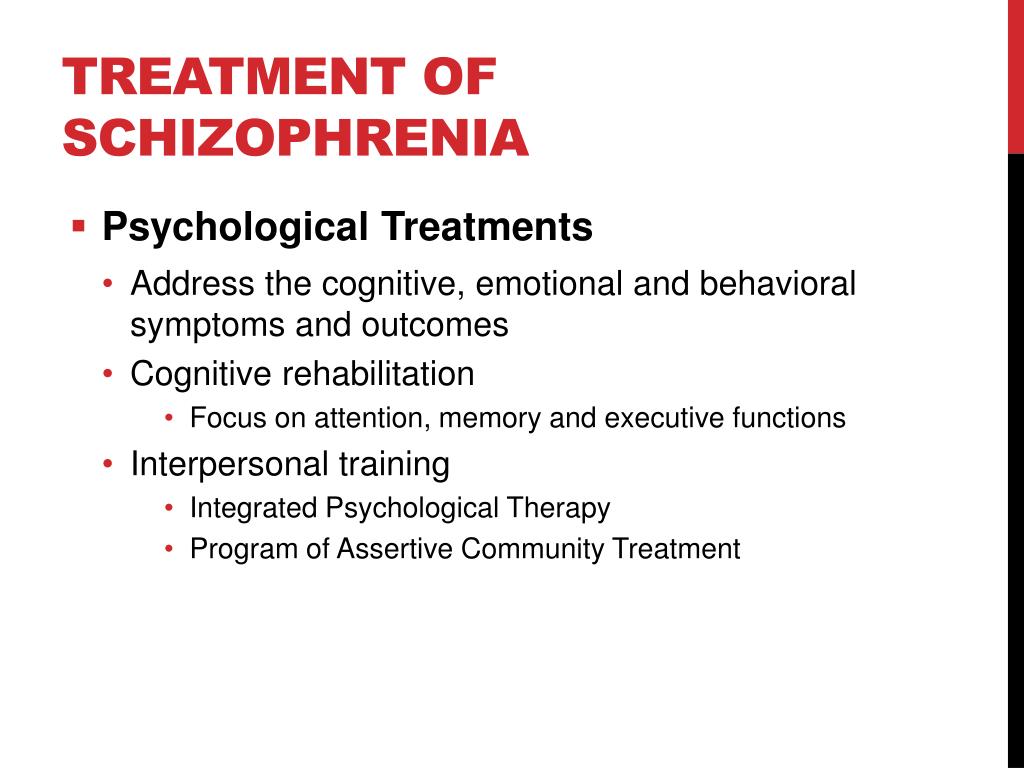 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia.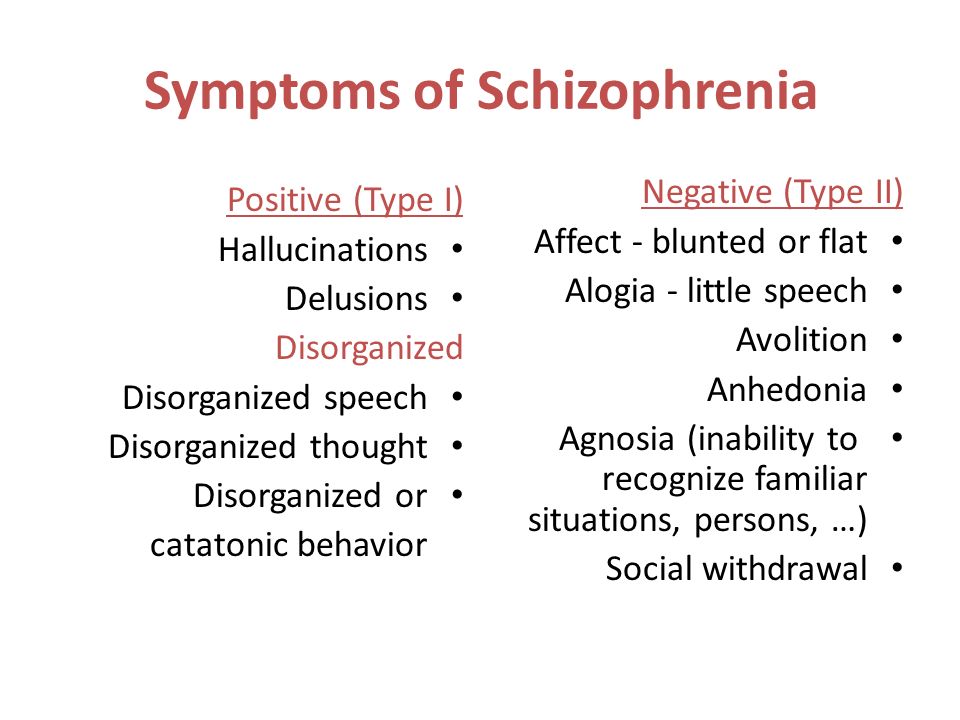 Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg life skills education).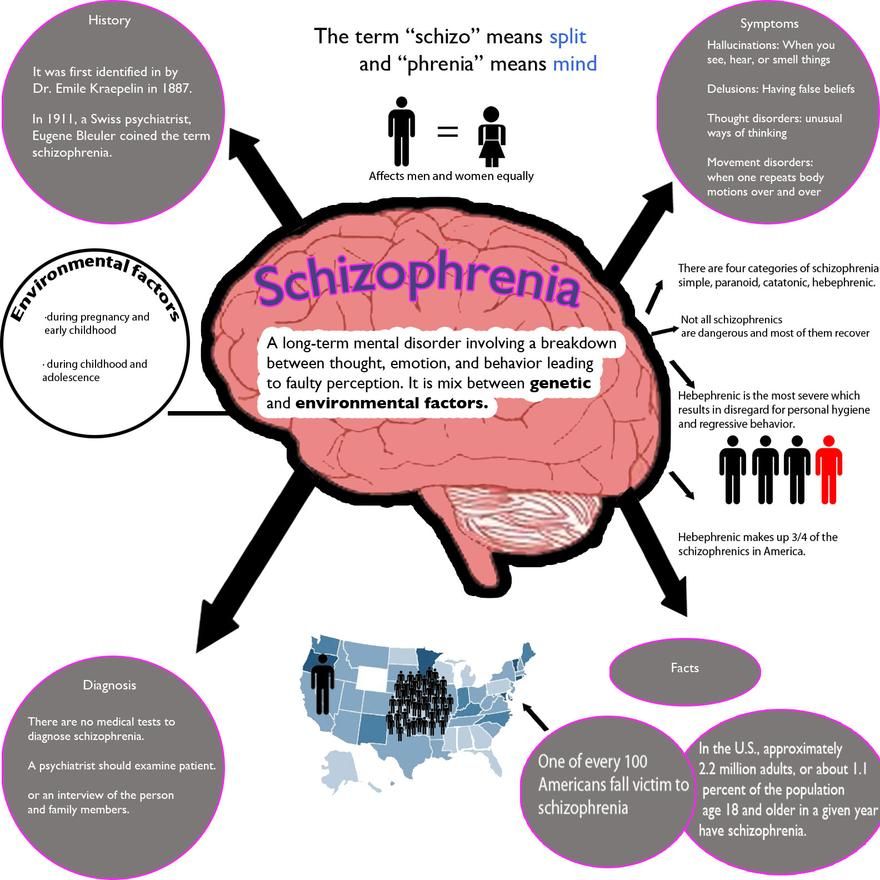 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO activities
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.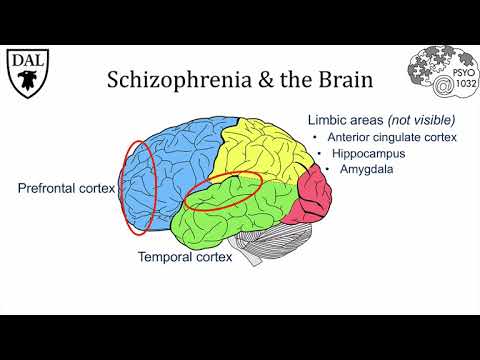 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.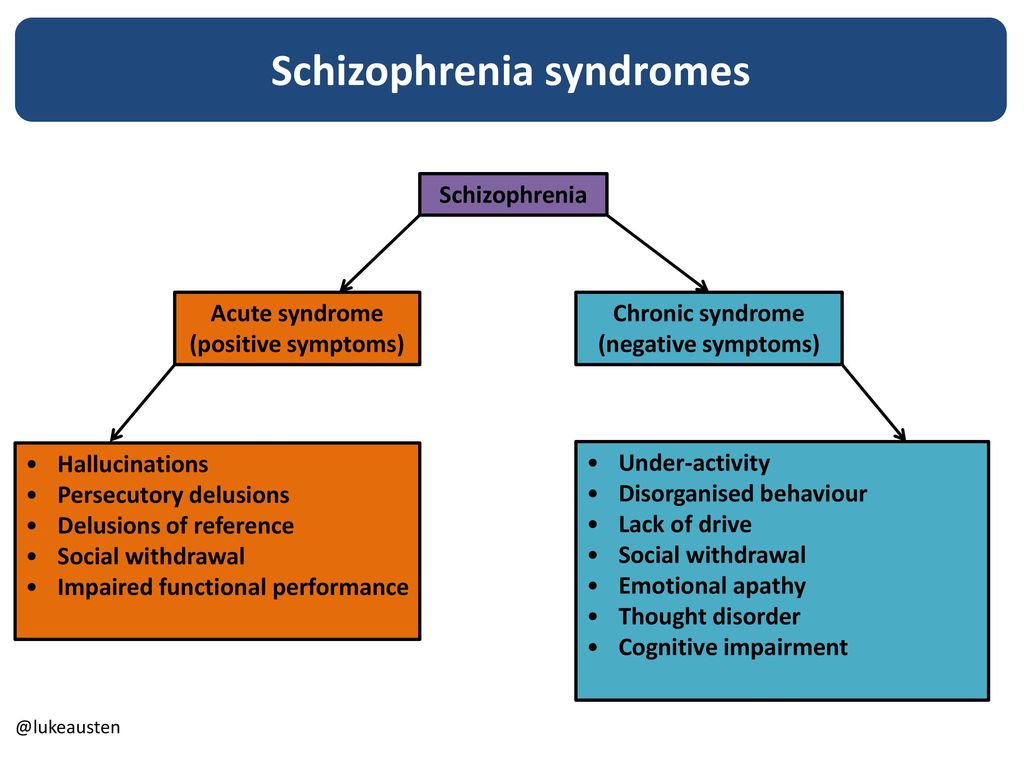 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Video games for schizophrenia | Cochrane
Survey question
Are video games an effective treatment (as a stand-alone treatment or as an adjunct to existing treatment) to improve the well-being and functioning of people with schizophrenia or schizoaffective disorder?
Relevance
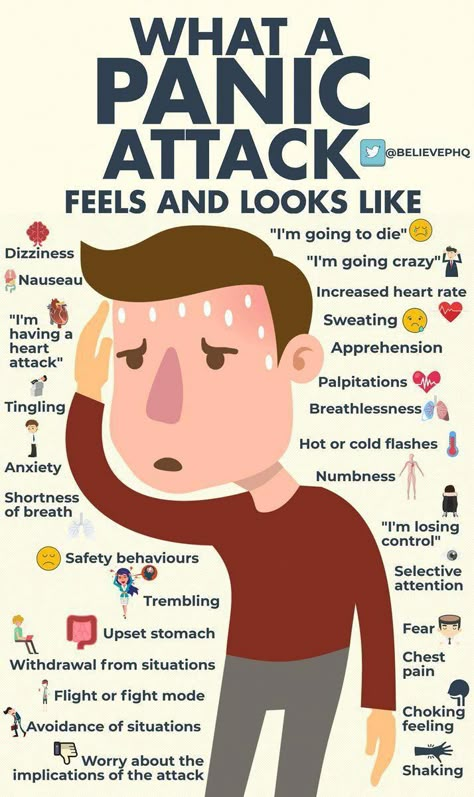
Schizophrenia is a severe mental illness affecting people all over the world. People with schizophrenia often have a distorted view of reality—perceiving things that don't really exist (hallucinations) and believing things that aren't true (delusions). People with schizophrenia may experience difficulty with motivation, as well as anxiety and depression. In addition, they experience cognitive symptoms, often having difficulty concentrating on daily activities and becoming disoriented. Delusions and hallucinations are usually treated with antipsychotic drugs, while other symptoms are difficult to manage with medication alone.
People with schizophrenia often have a distorted view of reality—perceiving things that don't really exist (hallucinations) and believing things that aren't true (delusions). People with schizophrenia may experience difficulty with motivation, as well as anxiety and depression. In addition, they experience cognitive symptoms, often having difficulty concentrating on daily activities and becoming disoriented. Delusions and hallucinations are usually treated with antipsychotic drugs, while other symptoms are difficult to manage with medication alone.
Psychotherapy is sometimes used in addition to medication to manage some symptoms, but this can be difficult and expensive. Video games are a relatively inexpensive and, for many, fun treatment. Their use has been proposed to correct cognitive impairments such as problems with concentration or memory, which are often seen in individuals with schizophrenia. If effective, video games could serve as a simple and relatively inexpensive complementary treatment for people with schizophrenia.
Search
We searched for randomized controlled trials (a type of study in which participants are randomly assigned to one of two or more treatment groups) in people with schizophrenia who receive either video games or another type of treatment, such as cognitive ( conversational) therapy or placebo (sham treatment). We searched in March 2017, August 2018 and August 2019.
Results
Seven trials met our inclusion criteria and provided useful data. Interventions using video games were divided into those that included body movements ("exergames") and those that did not include them ("non-exergames"). In clinical trials of non-movement video games, direct video game intervention has been compared to "brain training," also known as cognitive remediation. One trial compared motion-enabled video games with standard assistance, and another compared motion-enabled video games with non-motion video games.