Feeling hot after eating
Why Am I feeling Hot After Eating?
Content
- Overview
- Why humans sweat
- What is excessive sweating?
- Types of excessive sweating
- Diagnosis
- How is diabetes related to excessive sweating?
- Hyperhidrosis treatment
- When should I see a doctor?
- The lowdown
Excessive sweating may occur for several reasons. If you find that your sweating has increased since you've been diagnosed with diabetes, this may be because there are a couple of forms of hyperhidrosis (excessive sweating) that have been linked to the disease.
Your doctor will be able to help you determine whether your sweating is natural or whether diabetes or some other condition, may be at fault. Except for extreme cases, treatment options are simple and non-invasive.
Have you considered clinical trials for Diabetes?
We make it easy for you to participate in a clinical trial for Diabetes, and get access to the latest treatments not yet widely available - and be a part of finding a cure.
Check your eligibility
Humans are one of few mammals that are capable of removing excess heat through the use of sweat glands. While sweating is most commonly associated with hot weather, it serves two purposes within the body. To fully understand the process, let's look at both of them.
Thermoregulatory - Your body can get too hot for a number of reasons. The sun beating down on a hot day is a common cause, but physical exertion also raises your body temperature. When your body gets too warm, the eccrine sweat glands tell your body to release sweat. Eccrine glands are the sweat glands that cover most of your body, as opposed to apocrine sweat glands, which are found primarily around hair follicles. As the sweat from the eccrine glands begins to evaporate, your body temperature cools. This type of sweating is controlled mostly by a part of the brain called the hypothalamus.
Emotional - You can also start sweating in response to emotional stimuli.
 The mechanism for this type of sweating takes place largely in the limbic region of the brain. Emotional sweating tends to be limited to the face, armpits, palms, and soles of the feet. Although it's a different mechanism than thermoregulatory sweating, the two mechanisms do influence one another.
The mechanism for this type of sweating takes place largely in the limbic region of the brain. Emotional sweating tends to be limited to the face, armpits, palms, and soles of the feet. Although it's a different mechanism than thermoregulatory sweating, the two mechanisms do influence one another.
Sweating is a normal, and important, part of being human. In severe situations, your body will even sweat quite a bit. However, in some people, the body produces extreme levels of sweat without an underlying extreme cause. This condition, known as hyperhidrosis, can be annoying, embarrassing, and uncomfortable.
There are several types of excessive sweating and several underlying causes that may be at the root of the issue.
The medical name for excessive sweating is hyperhidrosis. There are two major types of hyperhidrosis, generalized and focal.
Generalized hyperhidrosis can be caused by conditions such as infection, endocrine imbalances, medications, intoxication, and withdrawals from alcohol or other substances. Generalized sweating affects the whole body.
Generalized sweating affects the whole body.
The second type of excessive sweating is called focal hyperhidrosis. This type of sweating can be broken down into four categories:
Primary focal hyperhidrosis - This form of hyperhidrosis often develops during puberty. It's also the most common form of the condition, making up over half of all cases. Primary focal hyperhidrosis affects mainly the armpit area, but can also impact the face, hands, and feet as well. In many cases, there's a family history of the condition among those who suffer from it.
Secondary focal hyperhidrosis - This type of hyperhidrosis is caused by damage to the nervous system. This can include nerves in the brain, or peripheral nerves outside the brain. Sweating of this nature is one of the many symptoms that can be a sign of other conditions, such as post-traumatic syringomyelia, which is the development of a cavity in the spinal cord filled with spinal fluid.
Harlequin syndrome - When a person develops Harlequin syndrome, one side of their face suffers nerve damage that prevents it from sweating properly.
 As a result, the other side of the face develops hyperhidrosis as a way of compensating for the reduced sweating. The result is one half of the face appearing dry and pale, while the other is moist and red.
As a result, the other side of the face develops hyperhidrosis as a way of compensating for the reduced sweating. The result is one half of the face appearing dry and pale, while the other is moist and red.Frey's syndrome - The parotid gland is a major salivary gland located below the ear. Damage to this gland can result in Frey's syndrome. Those who develop the condition sweat excessively after eating, or even thinking, about food. The sweating occurs around the area of the parotid gland: the cheek, temple, and ear area. Sweating triggered by food intake is known as gustatory sweating.
If you're sweating excessively, your doctor will first ask you about your medical history and may run some tests to see if any underlying causes might be causing you to sweat too much. Specific tests to check for and narrow down the specific type of hyperhidrosis can include an iodine starch test.
With this test, iodine is applied to the skin, and starch is placed on top of it. The solution will turn a purple color when it comes in contact with sweat. This test allows doctors to see exactly where you are sweating and what the pattern looks like.
The solution will turn a purple color when it comes in contact with sweat. This test allows doctors to see exactly where you are sweating and what the pattern looks like.
Doctors can measure the amount of sweat by placing a pre-weighed piece of filler paper over the affected area and then measuring again after it's been allowed to come in contact with the sweat. This information, along with the pattern exposed by the iodine starch test, can help doctors narrow down the severity and type of hyperhidrosis.
One of the risk factors for generalized hyperhidrosis includes endocrine imbalances. As diabetes is a disease affecting the endocrine system, it can be a cause of generalized hyperhidrosis.
Diabetics who are experiencing generalized hyperhidrosis will typically sweat all over, but diabetes is also a risk factor for a type of focal/gustatory hyperhidrosis, that is limited largely to the face, head, and upper body, though can also affect the whole body.
Diabetics who are experiencing this form of hyperhidrosis will notice the extra sweat after eating.
Why do I feel hot after eating?
Frey's syndrome isn't the only condition that can cause gustatory sweating. In some instances, the response is normal. For example, eating extremely spicy foods may trigger your body to begin sweating.
However, some people sweat profusely after eating, even when foods that would trigger the condition aren't being consumed. This is a well-known side effect of diabetes mellitus, affecting twice as many diabetics as non-diabetics. At the moment, researchers are unsure of the exact pathophysiology that results in the condition among diabetics.
Often, hyperhidrosis doesn't require treatment, but many people find that excessive sweating has detrimental effects on their confidence and social lives. There are some medical options available that can reduce the sweating and allow those with hyperhidrosis to live a life they're more comfortable with. These methods include medication, and in extreme cases, surgery.
Medications
Medications that alleviate hyperhidrosis symptoms come in both systemic and topical forms. The most common options your doctor may try are listed below:
The most common options your doctor may try are listed below:
Anticholinergic drugs - This class of drugs has shown to be effective against hyperhidrosis. Side effects, which include, dry mouth, urinary retention, and memory problems are a limitation to more widespread use, however.
Antihypertensive drugs - Several drugs used to treat hypertension, such as beta-blockers and calcium channel blockers, are moderately effective at treating certain types of hyperhidrosis.
Antidepressants - Similarly to antihypertensive drugs, some antidepressants have shown to have a mild effect on reducing excessive sweating caused by hyperhidrosis.
Prescription antiperspirant - Most over-the-counter antiperspirants use aluminum salts at a concentration of around 1% to 2%. Prescription antiperspirants can go much higher, with concentrations reaching 25%.
Glycopyrrolate cream - Another topical option is glycopyrrolate cream.
 The substance is an anticholinergic that's particularly useful in gustatory sweating, such as that caused by Frey's syndrome or diabetes.
The substance is an anticholinergic that's particularly useful in gustatory sweating, such as that caused by Frey's syndrome or diabetes.Botulinum toxins - Injection of botulinum toxins to inhibit the release of acetylcholine is the most effective method of controlling focal hyperhidrosis. The injections are typically effective for 4-7 months.
Surgery
Treating hyperhidrosis with surgery is considered a last resort that should only be used when all other options have been exhausted. The two surgical procedures often used involve removing either the nerves responsible for the reaction or removing the sweat glands themselves.
Removal of the nerves ( sympathectomy) is most effective in sweat coming from the palms of the hands. Removal of the sweat glands is most effective in the armpit area, but is not a trivial operation and may cause complications such as infection, scarring, and skin necrosis or discoloration.
Seeing a doctor as soon as you notice that you're sweating more than you usually do can help ensure that no underlying conditions are causing this. Your doctor can prescribe medications that will help reduce the severity of the sweating. If you've recently developed diabetes, the conditions may be linked, and a doctor will be able to determine this connection.
Your doctor can prescribe medications that will help reduce the severity of the sweating. If you've recently developed diabetes, the conditions may be linked, and a doctor will be able to determine this connection.
There are several reasons your body may begin to sweat more than usual. A few of them may be related to your diabetes diagnosis. If you find yourself noticeably sweating more than usual, consult your doctor. An examination will help you determine the cause of the sweating and find the treatment option that best suits you.
Sweating After Eating: Here's Why it Can Happen
- Can certain foods make you sweat?
- Gustatory hyperhidrosis
- Managing sweating after eating
- Don’t brush it off
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Sometimes we do something for one outcome—and end up with the exact opposite. Yoga’s supposed to be relaxing, and yet many times, you’re left breaking a sweat. Massages can actually cause your muscles to cramp up if you don’t stretch afterward. And eating, which is also generally a relaxing experience, can cause you to perspire.
So what’s the deal with sweating after eating? After all, you’re probably not a competitive eater. It sort of makes sense, even without science, that downing 50 hot dogs in five minutes would activate someone’s sweat glands. But a nice sit-down dinner is different, and, apart from holidays like Thanksgiving, you’re generally not stuffing yourself. Here’s what might be making your shirt wet and how to prevent it. (Sorry, we can’t do anything about sweating on that dinner date if it’s about nerves.)
A solution for excessive sweating, delivered to your door
Drysol is a first-line prescription treatment for excessive sweating (hyperhidrosis).
Learn more
Yes, absolutely. Although the science is still torn on whether the meat sweats are real, experts agree certain foods can get the juices flowing. There are a couple of categories of foods that are the main culprits if you find yourself sweating after eating: spicy foods and (possibly) sugary foods. Acidic foods, like those that contain vinegar, may increase the likelihood of sweating as well as foods served hot, like soup. But the main triggers are outlined below and may cause facial sweating or excessive sweating in the armpits.
It’s widely known that spicy foods can make you sweat. That’s thanks to a compound in peppers that gives them their kick, called capsaicin. Our bodies sense the presence of this heat-inducing compound through a receptor called TRPV1. When TRPV1 is sensitized and picks up that there’s capsaicin around, it can cause thermal hyperalgesia. That’s a condition in which you perceive things as really hot or cold that are truly only warm or cool (O’Neill, 2012). This could explain why you’re suddenly sweating in a restaurant that was a comfortable temperature for you just moments ago.
This could explain why you’re suddenly sweating in a restaurant that was a comfortable temperature for you just moments ago.
Capsaicin also raises your body temperature, and this reaction may serve a purpose. There could be a good reason you see a lot of spicy food in hot, dry areas of the globe. “Spicy foods, especially from capsaicin-containing peppers, warm your body, which in turn makes you sweat,” explains Dana Hunnes, Ph.D., RD, MPH, senior dietitian at Ronald Reagan UCLA Medical Center and an adjunct assistant professor at the UCLA Fielding School of Public Health. “This, in turn, cools down your body, and this may be important in warmer climates.” (Unfortunately, she notes, that isn’t so effective at cooling you down in hot and humid climates. It needs to be dry).
To be clear right off the bat, we’re not saying sugary foods will always cause sweating after eating for some people. Even if you get sweaty after a sugary snack or meal, that doesn’t mean sugar is a trigger for you, rather, that perhaps you need to consciously balance your meals in order to slow digestion. If sugar is making you sweat, it’s likely because your body is producing too much insulin in response to what you ate. This, in turn, causes your blood sugar to plummet, a condition known as reactive hypoglycemia, or low blood glucose as a response to a meal rather than caused by diabetes. Sweating is a common side effect. But it’s worth noting that a food that triggers you alone may not cause sweating if eaten along with a source of quality fat or fiber to slow digestion. Talk to a healthcare professional about what you’re experiencing. They may take blood samples to look at blood glucose levels or offer lifestyle suggestions. Reactive hypoglycemia may require interventions.
Why do we sweat?
Hyperhidrosis Last updated: Feb 27, 2020 7 min read
In some cases, sweating after eating is related to your nerves and not to the food on the menu. There are several different kinds of hyperhidrosis. Primary hyperhidrosis is the most common cause of excessive sweating, but its cause isn’t known. Secondary hyperhidrosis, on the other hand, is excessive sweating due to some underlying cause. Gustatory hyperhidrosis is simply when it happens after you eat. Gustatory sweating is also called Frey’s syndrome, one type of secondary hyperhidrosis, and has to do with the nerves in and around the mouth.
There are several different kinds of hyperhidrosis. Primary hyperhidrosis is the most common cause of excessive sweating, but its cause isn’t known. Secondary hyperhidrosis, on the other hand, is excessive sweating due to some underlying cause. Gustatory hyperhidrosis is simply when it happens after you eat. Gustatory sweating is also called Frey’s syndrome, one type of secondary hyperhidrosis, and has to do with the nerves in and around the mouth.
Your chances of having Frey’s syndrome are higher if someone in your family has it, and it is generally caused by a previous surgery near the parotid glands, the body’s biggest salivary glands that are located just in front of the ears. Surgery may damage these nerves, causing the syndrome. While the condition is not entirely understood, one of the biggest signs is the development of sweating after eating within a year following surgery (Frey Syndrome, n.d.). Frey’s syndrome is also considered secondary hyperhidrosis because the sweating is a byproduct of underlying nerve damage.
Nerve damage, anxiety, alcoholism, and gout may all be underlying conditions causing secondary hyperhidrosis. Health conditions involving damage to the nervous system, such as Parkinson’s disease, may also cause gustatory hyperhidrosis. In some cases, diabetes can cause diabetic neuropathy, damage to the nerves that may also cause this sweating. It’s common with primary hyperhidrosis for sweating to be localized in certain parts of the body. This is called focal axillary hyperhidrosis and accounts for around 51% of cases of hyperhidrosis. In some cases, such as hyperhidrosis caused by Harlequin syndrome, the sweating can happen on just one side of the body (Schlereth, 2009).
The easiest option if you know your triggers is, of course, to avoid foods that make you sweat. Hunnes suggests easing up on the spice if peppers seem to cause sweating, and you’re adamant about not giving up these flavorful ingredients altogether. If reactive hypoglycemia (low blood sugar) is the culprit, you should speak with your healthcare provider. The excess insulin may be due to a medical condition that requires further testing.
The excess insulin may be due to a medical condition that requires further testing.
“If it is [an underlying medical condition], the only treatment I know of is botulinum toxin,” Hunnes says. (You likely know this better as Botox. Injections of this medication have shown promise in easing sweating after eating in one study. And the researchers suggest it as a first-line treatment since it appears to at least lessen the sweating and successfully diminish sweating with every reinjection (Laccourreye, 1999). (Medications like Botox wear off eventually, and the exact timeline differs from person to person.) You can discuss this treatment option with a dermatologist.
If your symptoms aren’t severe or you’re not ready to try Botox injections as a solution, over the counter (OTC) or prescription antiperspirants, and deodorants can help. There are special antiperspirants made in sprays and wipes for your face, hands, and feet as well. “Other potential ways to work around this might be having ice-cold beverages at the table so that you can cool off from the inside out,” Hunnes suggests. For people with Parkinson’s disease, some medications that manage symptoms of the disease (called anticholinergics) may lessen excessive sweating. But these medications aren’t without their own side effects, so you should discuss your treatment options with a healthcare professional.
For people with Parkinson’s disease, some medications that manage symptoms of the disease (called anticholinergics) may lessen excessive sweating. But these medications aren’t without their own side effects, so you should discuss your treatment options with a healthcare professional.
Understanding what causes excessive sweating
Hyperhidrosis Last updated: Feb 28, 2020 4 min read
Hyperhidrosis can significantly affect quality of life. Having primary hyperhidrosis is associated with an increased risk of having anxiety by 49.6%, one study found (Braganca, 2014). And although that study didn’t find an association between hyperhidrosis and depression, a 2016 study did. The study found that of the participants questioned, only 9.7% of those without hyperhidrosis experienced depression compared to 27.2% with the condition (Bahar, 2016). If you feel like your sweating is interfering in your daily life, consider consulting a medical professional to discuss your treatment options.
If you feel like your sweating is interfering in your daily life, consider consulting a medical professional to discuss your treatment options.
- Bahar, R., Zhou, P., Liu, Y., Huang, Y., Phillips, A., Lee, T. K., … Zhou, Y. (2016). The prevalence of anxiety and depression in patients with or without hyperhidrosis (HH). Journal of the American Academy of Dermatology, 75(6), 1126–1133. doi: 10.1016/j.jaad.2016.07.001, https://www.ncbi.nlm.nih.gov/pubmed/27567033
- Bragança, G. M. G., Lima, S. O., Neto, A. F. P., Marques, L. M., Melo, E. V. D., & Reis, F. P. (2014). Evaluation of anxiety and depression prevalence in patients with primary severe hyperhidrosis. Anais Brasileiros De Dermatologia, 89(2), 230–235. doi: 10.1590/abd1806-4841.20142189, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4008051/
- Frey Syndrome. (n.d.). Retrieved February 11, 2020, from https://rarediseases.org/rare-diseases/frey-syndrome/
- Laccourreye, O., Akl, E., Gutierrez-Fonseca, R.
 , Garcia, D., Brasnu, D., & Bonan, B. (1999). Recurrent Gustatory Sweating (Frey Syndrome) After Intracutaneous Injection of Botulinum Toxin Type A. Archives of Otolaryngology–Head & Neck Surgery, 125(3), 283. doi: 10.1001/archotol.125.3.283, https://www.ncbi.nlm.nih.gov/pubmed/10190799
, Garcia, D., Brasnu, D., & Bonan, B. (1999). Recurrent Gustatory Sweating (Frey Syndrome) After Intracutaneous Injection of Botulinum Toxin Type A. Archives of Otolaryngology–Head & Neck Surgery, 125(3), 283. doi: 10.1001/archotol.125.3.283, https://www.ncbi.nlm.nih.gov/pubmed/10190799 - O’Neill, J., Brock, C., Olesen, A. E., Andresen, T., Nilsson, M., & Dickenson, A. H. (2012). Unravelling the Mystery of Capsaicin: A Tool to Understand and Treat Pain. Pharmacological Reviews, 64(4), 939–971. doi: 10.1124/pr.112.006163, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3462993/
- Schlereth, T., Dieterich, M., & Birklein, F. (2009). Hyperhidrosis—Causes and Treatment of Enhanced Sweating. Deutsches Aerzteblatt Online, 106(3), 32–37. doi: 10.3238/arztebl.2009.0448b, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695293/
Feeling hot
I confirm More
- INVITRO
- Library
- Symptoms
- Feeling hot
Menopause
Diabetes mellitus
Climax
Thyrotoxicosis
Pheochromocytoma
51098 24 August
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
The feeling of heat that a person experiences arises from a sharp expansion and blood filling of small subcutaneous vessels. This condition is called arterial hyperemia. The skin turns red and becomes hot.
The lumen of the vessels is regulated by the sympathetic and parasympathetic nervous system. Its changes depend on the signals of the vasomotor (vasomotor) center of the central nervous system, hormones, pyrogenic (heat-causing) substances entering the blood, and a number of other factors.
Feelings of heat
The vessels are constantly influenced by factors that have a vasoconstrictor or vasodilating effect. For example, under stress, blood vessels under the influence of the hormone adrenaline narrow, the skin turns pale. At the end of a stressful situation, the vessels relax and fill with blood.
Pathological arterial hyperemia, which is accompanied by a feeling of heat, develops either under the influence of irritants (infections, toxins, tissue breakdown products during burns, pyrogenic substances), or in violation of nervous regulation.
Distinguish neurogenic arterial hyperemia (occurring in response to irritation of nerve endings) and metabolic (due to the action of local chemical factors). An example of neurogenic arterial hyperemia is the reddening of the face and neck with hypertension, menopausal syndrome, and also with strong emotions.
Blood electrolytes have a metabolic effect on vascular tension: calcium and sodium constrict blood vessels and increase blood pressure, while potassium and magnesium, on the contrary, expand. Metabolic regulators include carbon dioxide, organic acids, hormones.
Possible Causes of Feeling Hot
Hot, spicy and spicy foods can cause flushing and feeling hot.
The same effect on the body has alcohol , which promotes the expansion of blood vessels.
Taking certain medications may also cause a sensation of heat spreading through the body. These include vasodilators, hormonal agents, antidepressants, etc.
These include vasodilators, hormonal agents, antidepressants, etc.
The causes of arterial hyperemia and, as a result, feelings of heat can be different. If the regulation of vascular tone is disturbed, arterial hypertension may develop, accompanied by a sudden increase in blood pressure - a hypertensive crisis. The most common cause of this condition is hypertension. However, in a third of cases, arterial hypertension is caused by diseases of the internal organs: acute glomerulonephritis and other kidney damage, adrenal tumors and other diseases of the endocrine system. The magnitude of the rise in blood pressure during a hypertensive crisis depends on the age and individual characteristics of the person. At a young age, the symptoms of a crisis may occur at a lower level of blood pressure, and in the elderly - at a higher one.
A sharp increase in blood pressure is accompanied by headache, dizziness, nausea, vomiting, visual disturbances (“flies”, doubling). Perhaps numbness of the limbs, a feeling of goosebumps, palpitations, shortness of breath.:strip_icc():format(webp)/kly-media-production/medias/3409770/original/009673600_1616563590-WhatsApp_Image_2021-03-24_at_08.07.16.jpeg)
Due to a violation of the nervous regulation, chills occur, followed by fever, increased sweating. Completion of the crisis is accompanied by frequent urination.
An increase in blood pressure and the symptoms accompanying this condition also occur with a tumor of the adrenal gland - pheochromocytoma and other hormone-producing tumors. The tumor secretes large amounts of catecholamines (epinephrine and norepinephrine).
Clinical signs of pheochromocytoma may include headache, sweating, palpitations, irritability, weight loss, chest pain, nausea, vomiting, weakness, fatigue. In some cases, patients may experience fever, shortness of breath, hot flashes, increased thirst, frequent urination, dizziness, and tinnitus.
Many women complain of hot flashes during menopause . A change in the hormonal background occurs even before the cessation of menstruation, during the period of premenopause (menopausal transition). At first, its manifestations are insignificant, and most often they are not given importance or are attributed to the consequences of fatigue and mental overstrain. Hormonal and metabolic changes, in particular, a decrease in the level of estrogens, progesterone and an increase in the production of GnRH, are accompanied by hot flashes, which can be repeated several times a day.
At first, its manifestations are insignificant, and most often they are not given importance or are attributed to the consequences of fatigue and mental overstrain. Hormonal and metabolic changes, in particular, a decrease in the level of estrogens, progesterone and an increase in the production of GnRH, are accompanied by hot flashes, which can be repeated several times a day.
Women describe them as a periodic short-term sensation of heat, followed by chills, increased sweating, and rapid heartbeat.
In most cases, hot flashes slightly interfere with well-being. Arterial hyperemia and a feeling of heat may be a sign of a dysfunction of the thyroid gland, for example, in thyrotoxicosis . Patients with thyrotoxicosis complain of general weakness, fatigue, irritability, sleep disturbance, sweating, finger trembling, palpitations, and sometimes pain in the region of the heart.
Despite increased appetite, patients with thyrotoxicosis lose weight.
Violation of thermoregulation, which occurs due to accelerated metabolism, leads to an increase in body temperature and causes a constant feeling of heat. The skin becomes warm and moist, the skin vessels dilate, which is accompanied by reddening of the face. Sweating increases, nails become brittle, hair falls out.
Sometimes hot flashes and a feeling of heat in combination with high blood pressure occur at diabetes mellitus . These symptoms are accompanied by general malaise, sweating, thirst, increased urine output.
Which doctors should I contact?
If you experience symptoms such as fever and hot flashes on a regular basis, you should contact therapist, who, on the basis of complaints and analyzes, will refer to gynecologist or endocrinologist.
Diagnostics and examinations
The appearance of periodic hot flashes, accompanied by a feeling of heat, sweating, redness of the skin of the face, requires a mandatory diagnosis.
The doctor evaluates the patient's complaints, taking into account age, gender and concomitant diseases. With an increase in blood pressure, turning into crises, it is necessary to determine the nature of the pathology - primary (associated with impaired nervous regulation) or secondary (due to diseases of the internal organs). For this, a clinical blood test and a general urinalysis, a Nechiporenko urinalysis, a blood test for glucose, cholesterol, and creatinine are prescribed.
Clinical blood test: general analysis, leukogram, ESR (with microscopy of a blood smear in the presence of pathological changes)
Synonyms: Complete blood count, KLA. Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram. Brief description of the study Clinical blood test: general...
Up to 1 business day
Available with house call
RUB 810
Add to cart
General urinalysis (Urine analysis with sediment microscopy)
Method of determination Determination of physical and chemical parameters is carried out on an automatic analyzer using the "dry chemistry" method.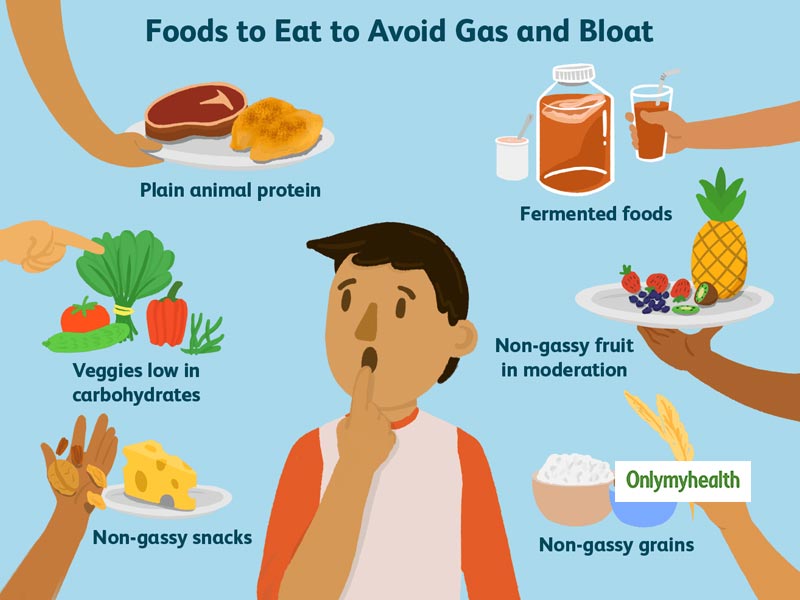 Hardware microscope...
Hardware microscope...
Up to 1 business day
Available with house call
410 RUB
Add to cart
Nechiporenko Urine Test
Synonyms: Determination of the amount of blood cells in the urine sediment; Sample of Nechiporenko; Urinalysis by the Nechiporenko method. Analysis of urine Nechiporenko; Urinalysis; Urine...
Up to 1 business day
Available with house call
475 RUB
Add to cart
Glucose (in the blood) (Glucose)
Research material Serum or blood plasma. If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation...
If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation...
Up to 1 business day
Available with house call
335 RUB
Add to cart
Cholesterol total (cholesterol, Cholesterol total)
Synonyms: Cholesterol, cholesterol. Blood cholesterol, Cholesterol, Chol, Cholesterol total. Brief characteristics of the analyte Total cholesterol Approximately 80% of total cholesterol is synthetic...
Up to 1 business day
Available with house call
370 RUB
Add to cart
Creatinine (in the blood) (Creatinine)
Synonyms: Blood test for creatinine; Serum creatinine; Serum creatinine, GFR estimate. Creat; Cre; Blood Creatinine; Serum Creatinine; Serum Creat. Brief description of the definition ...
Creat; Cre; Blood Creatinine; Serum Creatinine; Serum Creat. Brief description of the definition ...
Up to 1 business day
Available with house call
370 RUB
Add to cart
Diagnosis of thyrotoxicosis is based on the clinical manifestations of the disease and the results of laboratory and instrumental examinations. These include determining the level of TSH, free T4 and T3, the level of antibodies to the TSH receptor (AT-rTTG) and the level of antibodies to thyroid peroxidase (AT-TPO).
Thyroid gland: extended examination
Up to 1 business day
Available with house call
RUB 3,185
Add to cart
Anti-Thyroid Peroxidase Autoantibodies
Synonyms: Blood test for AT-TPO; Antibodies to microsomal antigen; ATPO. Antimicrosomal Antibodies; Antithyroid Microsomal Antibodies; Thyroid Peroxidase Autoantibodies; TPO Antibodies; Thyroid Peroxidase Test; Thyroid microsomal a...
Antimicrosomal Antibodies; Antithyroid Microsomal Antibodies; Thyroid Peroxidase Autoantibodies; TPO Antibodies; Thyroid Peroxidase Test; Thyroid microsomal a...
Up to 1 business day
Available with house call
790 RUB
Add to cart
In addition, an ultrasound of the thyroid gland, a scintigraphic examination, and in the presence of nodes, a fine-needle biopsy are performed.
Ultrasound of the thyroid gland, parathyroid glands and regional lymph nodes
Examination of the thyroid and parathyroid glands, which allows to evaluate their structure, as well as to detect pathological changes in these organs and regional lymph nodes. ..
..
2,040 rubles Sign up
With symptoms of an adrenal tumor, stimulating tests are performed, the level of catecholamines in the daily urine and blood plasma, and metanephrines in the daily urine test are determined.
Catecholamines, daily urine: epinephrine, norepinephrine, dopamine
Catecholamines are biologically active substances from the group of biogenic amines. Adrenaline is the main hormone of the adrenal medulla, which is formed here in ...
Up to 4 working days
Available with house call
2 645 RUB
Add to cart
Plasma catecholamines (epinephrine, norepinephrine, dopamine)
The study is used in the diagnosis of pheochromocytoma, differential diagnosis of hypertensive conditions, with dysfunctions of the sympathadrenal system and pathology. ..
..
Up to 4 working days
Available with house call
2 645 RUB
Add to cart
Metanephrines fractionated, free and conjugated, 24-h urine
Intermediate metabolites of epinephrine and norepinephrine. A sensitive screening test in the diagnosis of pheochromocytoma. See also tests – Plasma catecholamines (p...
Up to 4 business days
Available with house call
3 425 RUB
Add to cart
An MRI of the abdominal organs and retroperitoneal space is also necessary, usually with the use of contrast.
Injection of a contrast agent (MRI)
Intravenous administration of a contrast agent.
RUB 5,840 Sign up
Treatment
The feeling of heat and hot flashes are only symptoms of the disease, so the doctor prescribes treatment after diagnosing the underlying pathology.
What should I do if I have a fever?
If the feeling of fever is caused by an increase in temperature due to infectious processes and intoxication, it is necessary to lower the body temperature and start treating the disease. In case of a hypertensive crisis, you need to call an ambulance. The feeling of heat that occurs with a sharp expansion of blood vessels due to neuroendocrine disorders does not require drug therapy.
Nevertheless, measures aimed at restoring vascular tone (contrast shower, normalization of sleep, daily exercise, healthy eating) lead to a decrease in the symptoms of hyperemia and an improvement in well-being.
Sources:
- Kasyan V.N., Adamyan L.V. Pathophysiology of hot flashes. Focus on neurohormonal regulation. reproduction problems. 2017;1:115-121. doi:10.17116/repro2017231115-121
- Maksimovich N.A. Analysis of the sensitivity and specificity of the test with reactive hyperemia in the diagnosis of endothelial dysfunction in children with vegetative disorders. Journal of the Grodno State Medical University "To the Practicing Doctor". 2012;2:101-103.
- Clinical guidelines "Menopause and menopause in women." Developed by: Russian Society of Obstetricians and Gynecologists. – 2021.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
Laryngeal edema
1450 07 November
-
Gastrointestinal bleeding
976 29 September
-
Intestinal colic
5524 28 September
Show 9 more0003
Scarlet fever
Diphtheria
Thrush
Gastritis
Pancreatitis
Diabetes mellitus
Worms
Plaque on the tongue
Plaque on the tongue: causes of appearance, in what diseases it occurs, diagnosis and methods of treatment.
More
Myositis
COVID-19
Tuberculosis
Toxoplasmosis
Hypothyroidism
Hyperthyroidism
Diabetes mellitus
Obesity
Systemic lupus erythematosus
Multiple sclerosis
Myalgia
Myalgia: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
More
Diabetes mellitus
Insulin
Diet
Dehydration
Diarrhea
Hyperhidrosis
Aldosterone
Convulsions
Thirst
Cushing's syndrome
Geophagia
Hypokalemia
Hypokalemia: causes, in which diseases it occurs, diagnosis and methods of treatment.
More
Diabetes mellitus
Human papillomavirus (HPV)
Fungus
Menopause
Climax
Thickening of the skin, or hyperkeratosis
Thickening of the skin: causes, in which diseases it occurs, diagnosis and methods of treatment.
More
Menopause
Climax
Pregnancy
Burn
Frostbite
Fungus
Mycosis
Psoriasis
Lichen planus
Brittle nails
Brittle nails cause significant discomfort. Traumatization and inflammation of the base of the nail plate is the first cause of fragility. Fragility and layering of the nail plate can be a symptom of a number of pathological conditions.
Traumatization and inflammation of the base of the nail plate is the first cause of fragility. Fragility and layering of the nail plate can be a symptom of a number of pathological conditions.
More
Nothing found
Try changing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing your request or select medical office from the list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Try changing your query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Subscribe to our newsletters
Enter e-mail
I consent to processing of personal data
Subscribe
Why throws in a fever / What does severe sweating without fever mean / Should I visit a doctor when sweating | 74.
“I don’t see them realizing what they have done”: Maria Zakharova told students how badly the West lives with children
The head of the Ministry of Labor told how maternity capital will grow in 2023
Mi-2 helicopter crashed in the Kostroma region
In the Chelyabinsk region, security forces identified a teenager who sent a threatening letter to school ”: one of the Siamese twins born in Chelyabinsk became a mother
A criminal case was opened against a minivan driver who caused a fatal accident with migrants near Chelyabinsk
“I am selling an apartment in the Crimea. Urgently! ”: Russians began to get rid of real estate on the peninsula
What is Ariant sausage made of: the agricultural holding revealed all the secrets of production
Which of the servicemen will receive the presidential 195,000? The Ministry of Defense answered
Families from neighboring countries were traveling in a minivan that got into a fatal accident near Chelyabinsk
The Ministry of Health told how many people went to emergency centers in Chelyabinsk because of sleet
A search party was named in memory of her. The story of Irina Bukhanova, who was killed by an ex-boyfriend - now he can get out on parole
The story of Irina Bukhanova, who was killed by an ex-boyfriend - now he can get out on parole
Mobilized from the Chelyabinsk region died a month after being called up for service
The Ministry of Defense explained when the mobilized will receive payments
Renault Logan driver who drove into the oncoming lane died on M-5 near Ashoy, the accident was caught on video
". The mobilized stated that they were forced to change their military service under threats
The Ministry of Defense supported the idea of returning primary military training to schools
The authorities decided on a decision regarding two years of military service
A conflict in a minibus, after which a schoolgirl was hospitalized with a head injury, escalated into a criminal case
As a result of a collision between a minivan and a truck near Chelyabinsk, two people died, six more were injured
Do you need a TIN? What documents may be required from you when applying for a job?0003
When eating less and moving more doesn’t help: what you need to know about the surgical treatment of obesity most often Russians die and how to prevent the disease
“We are not obliged to plaster them”: the head of a large management company explained the status of bomb shelters in Chelyabinsk
Midlife crisis: who in Russia rushed for loans
How many mobilized people are taking part in the battles and will they be recruiting more: NVO news for November 7
The plane flying to Yekaterinburg made an emergency landing in Sochi. There was a depressurization on board
There was a depressurization on board
The plane flying to Yekaterinburg suffered a cabin depressurization. The liner is being prepared for an emergency landing
The head of the TFR became interested in the incident with the schoolgirl thrown out of the minibus in Chelyabinsk
Putin promised to personally discuss with the Russians the payments to the mobilized
Volunteers from Troitsk who died at the front were the stepfather and father of one girl
I’m ashamed to admit it: the revelations of a mother who constantly yells at children (and advice on how to stop yelling) the whole country discussed
All news
Stress, problems with the heart and blood vessels can make themselves felt through excessive sweating
Photo: depositphotos.ru
Share
The body is covered with skin that must sweat in certain situations, such as when it is hot. This is a cooling system that prevents overheating. But sometimes we sweat even in the cold or under air conditioning, why? This is what Doctor Peter is about.
If we didn't know how to sweat, it would be very difficult for us in the warm season or with sudden changes in temperature, says Dr. Piter. Sweat, evaporating from the surface of the skin, allows you to give off excess heat, preventing overheating. In addition, with sweat during a fever, part of the salts, metabolic products, is excreted, due to sweating, the body temperature gradually decreases. But if attacks of severe sweating occur quite suddenly and it literally pours in hail, throws you into a fever or instantly breaks through cold sweat, the skin becomes cold and sticky - this is a reason to visit a doctor. These can be signs of stress, excessive fatigue, problems with the heart, blood vessels, and the endocrine system.
Why am I sweating? This question has come up a lot in recent years. A person feels healthy, leads an active lifestyle, but episodes of weakness and sweating come in waves at the most crucial moments. Is it familiar to you?
Is it familiar to you?
Elizaveta Melnikova, general practitioner, cardiologist.
Sweat is a natural secretion of our sweat glands and was created to protect the body from overheating. There are different types of glands in our body with you - some are thermoregulators and produce a hypotonic solution, which is sweat, during periods of elevated temperatures or physical exertion, while others secrete this specific secret of the body in moments of stress or fear.
The work of the sweat glands throughout the body is regulated by a part of the brain - the hypothalamus and sympathetic nerve fibers.
When the human body overheats, the thermoregulation center in the hypothalamus gives a signal to the peripheral nerves: it is necessary to increase heat transfer. To achieve this, there is an expansion of blood vessels on the surface of the skin and the process of secretion of a liquid watery secret - sweat is activated. It is this process that causes excessive sweating of a person during ARVI or other pathological conditions accompanied by an increase in body temperature.
In the female body, many processes are determined by the hormonal background, and therefore, when it changes (during menopause, pregnancy), the work of the autonomic nervous system is restructured. This leads to a short-term sensation of heat, hot flashes, increased sweating. During such periods, a woman needs to consult a gynecologist in order to alleviate the symptoms of her condition.
For the same reason, people suffering from other endocrine pathologies - overweight, hyperthyroidism, insulin resistance, diabetes mellitus - are prone to excessive sweating.
Observation of an endocrinologist, correction of the hormonal profile and lifestyle changes significantly reduce the manifestations of hyperhidrosis (as pathological sweating is called in medicine) and improve the general condition of a person.
As for the male half of the population, according to statistics, men are more likely to face stressful situations, and their sensitivity to adrenaline is higher than that of women.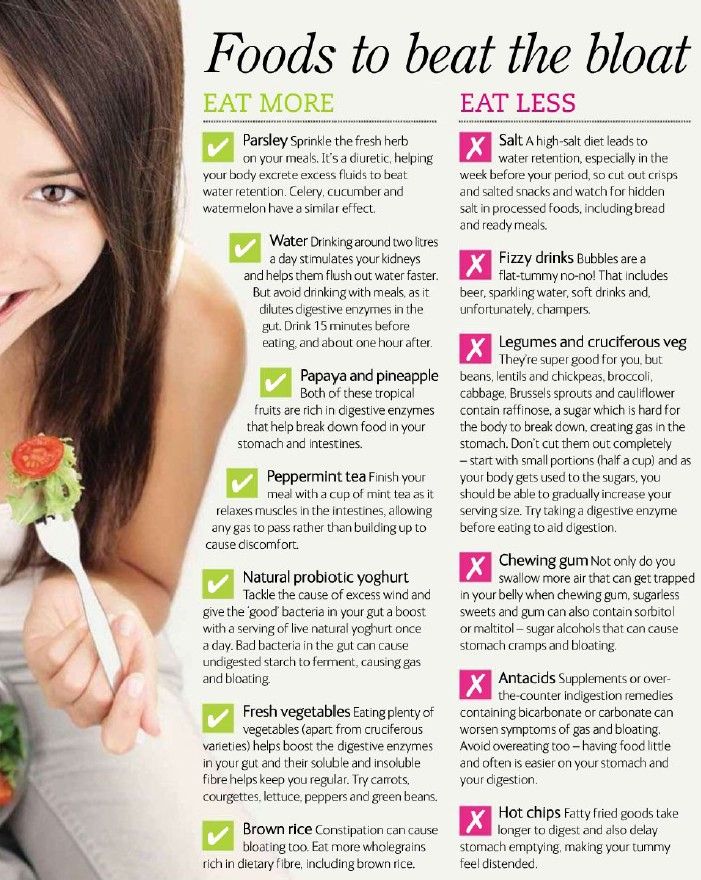 In this regard, in the male body, in response to stress, tachycardia develops, sweating increases, breathing quickens.
In this regard, in the male body, in response to stress, tachycardia develops, sweating increases, breathing quickens.
Smokers also tend to sweat more, as nicotine is a direct stimulant of acetylcholine, which irritates sweat gland receptors.
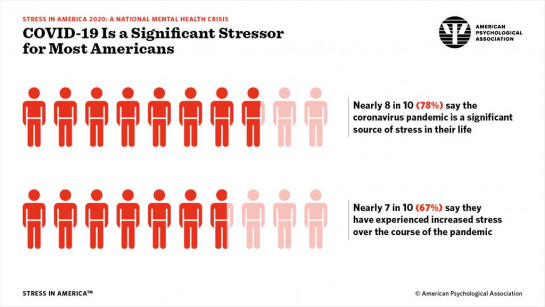
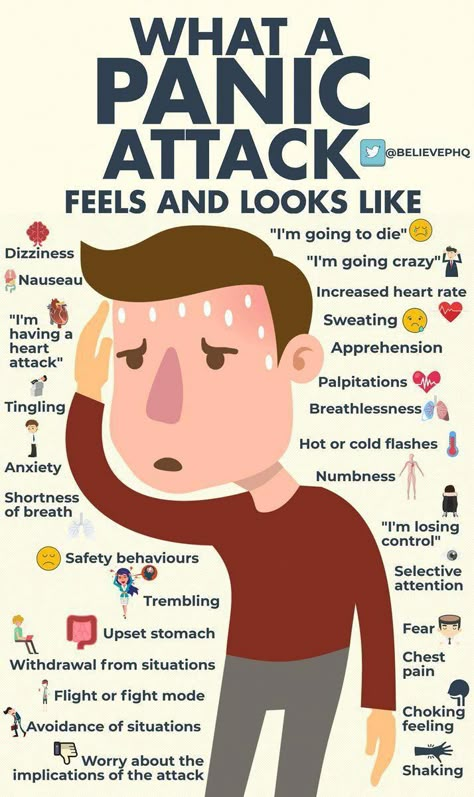
During the COVID-19 pandemic, cases of depression, anxiety disorders, panic attacks, in which sweating is an almost constant attribute, have become more frequent. A panic attack is most often manifested by an autonomic crisis, which may be accompanied by:
- anxiety,
- fear of death,0006
- shortness of breath,
- shortness of breath,
- chills,
- increased sweating,
- pre-syncope,
- frequent urination
- and other manifestations.
This is due to a sharp release of large amounts of adrenaline and dopamine into the blood, which stimulates a sharp increase in heart rate, respiratory rate, and the production of liquid secretions in the sweat glands throughout the body. The correction of these conditions is carried out by a psychotherapist, who helps to choose therapy to reduce the level of emotional stress, anxiety, leading to the development of panic attacks.
The correction of these conditions is carried out by a psychotherapist, who helps to choose therapy to reduce the level of emotional stress, anxiety, leading to the development of panic attacks.
Thus, sweating is most often a natural reaction of the body, which is an adaptive function of the body. In most cases, this condition does not require medical correction and manifests itself as a response to an adequate stimulus.
However, in a situation where you constantly and profusely sweat almost everywhere, you should consult a doctor for diagnosis and possible detection of diseases that require drug therapy.
Alena Paretskaya
SweatingHeat
- LIKE12
- LAUGHTER4
- SURPRISE2
- ANGER5
- SAD10
See the typo? Select a fragment and press Ctrl+Enter
COMMENTS22
Read all comments
What can I do if I log in?
COMMENT RULES
0 / 1400 This site is protected by reCAPTCHA and Google.