My head feels foggy
Brain Fog: Solutions to Help You Improve Concentration
Most people have experienced mental fog or brain fog. It is often described as a cloudy-headed feeling. Forgetfulness is a common complaint among older adults. As we grow older, we experience physiological changes that can cause glitches in brain functions we have always taken for granted. It takes longer to learn and recall information. We are not as quick as we used to be. Also, lack of sleep, overworking, and stress can cause brain fog. Brain fog can be frustrating, but relief is possible. Do not ignore your symptoms. If left untreated, brain fog can impact the quality of your life and lead to other conditions such as Parkinson’s disease, memory loss, and Alzheimer’s disease.
What is brain fog syndrome?
Brain fog is characterized by confusion, forgetfulness, and a lack of focus and mental clarity. This can be caused by overworking, lack of sleep, stress, and spending too much time on the computer. On a cellular level, brain fog is believed to be caused by high levels inflammation and changes to hormones that determine your mood, energy and focus. The imbalanced levels of hormones make the whole system to be thrown off. Also, brain fog syndrome can lead to other conditions such as obesity, abnormal menstruation, and diabetes mellitus.
Causes
Brain fog is typically rooted in a lifestyle that promotes hormonal imbalances and is exacerbated by stress.
- Electromagnetic radiation – from computer, mobile phone, tablets
- Stress – reduce blood flow to the brain causing poor memory
- Lack of sleep, no exercise
- Diet – amino acids, vitamins, minerals, and antioxidants
- Toxins, pollution, chemical substances, and insecticides
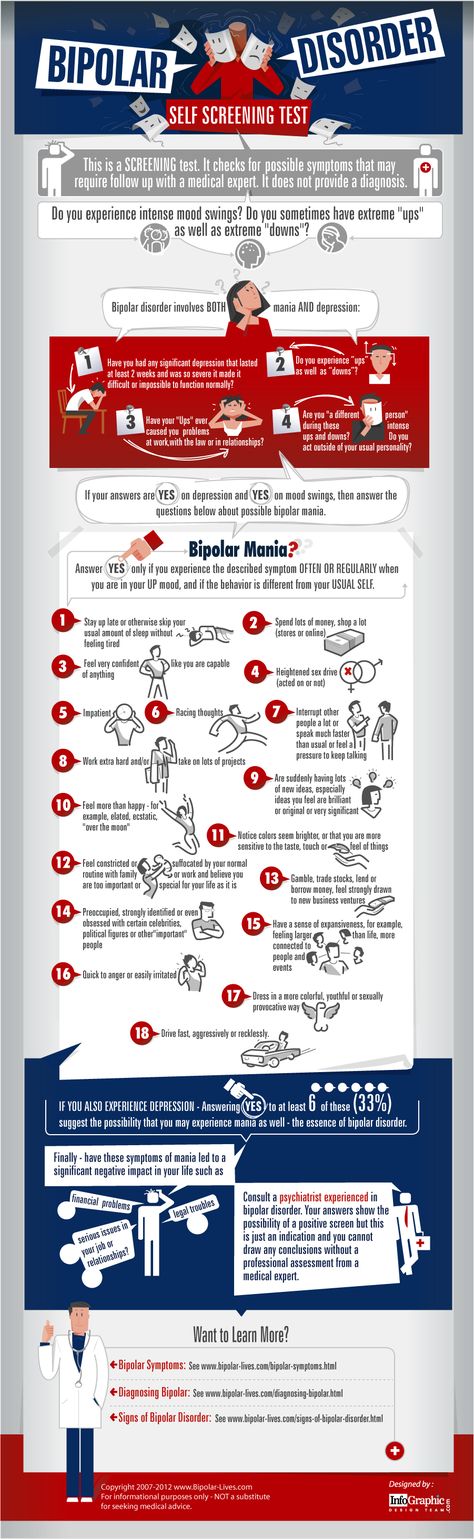
Symptoms
- Trouble sleeping, insomnia
- Headaches
- Low energy or fatigue
- Impaired cognitive function
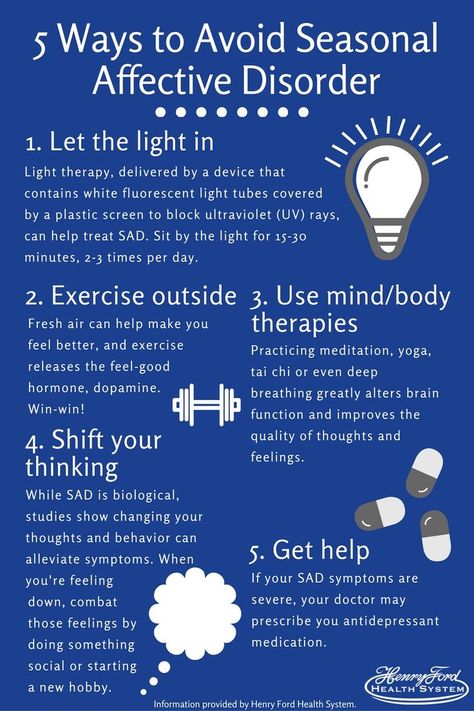
- Mood swings
- Irritables
- Forgetfulness
- Trouble concentrating
- Low motivation, lack of ideas
- Excessive absences
- Mildly depress
Treatment – ways to end brain fog
Brain fog treatment depends on the cause. Lifestyle modifications can also help.
Lifestyle modifications can also help.
- Spend less time on computer and mobile phone – remind yourself to take a break
- Positive thinking, reduce stress
- Change your diet
- Get enough sleep – 7-8 hours a day, go to bed at 10pm or no later than midnight
- Regular exercise
- Avoid alcohol, smoking, and drinking coffee in the afternoon
- Finding enjoyable activities
Supplements to help stop brain fog
- Fish Oil – contains long chain omega 3 fatty acids, DHA.
 The source is salmon, tuna, mackerel, and sardines. It can improve brain function, motor skills, and vision.
The source is salmon, tuna, mackerel, and sardines. It can improve brain function, motor skills, and vision. - Ginkgo Biloba Extract – widely studied for its effective anti-inflammatory, antioxidant, platelet-forming and circulation-boosting effects. Ginkgo biloba benefits include improved cognitive function, positive mood, increased energy, improved memory and reduced symptoms related to multiple chronic diseases. It can also reduce the risk of Alzheimer’s disease.
- Choline Bitartrate – Choline is chemically related to the B group of vitamins. Choline is important for cell membranes and for the production of the neurotransmitter acetylcholine, which has a role in memory and muscle control.
- Gamma Oryzanol – have been shown to raise the levels of neurotransmitters in central nervous system. It also promotes mood relaxation and restful sleep.
- L-Theanine – promotes relaxation and facilitates sleep by increasing level of serotonin, dopamine, and GABA.
 L-theanine is known as an anxiolytic—it works to reduce anxiety.
L-theanine is known as an anxiolytic—it works to reduce anxiety. - Phosphatidylserine – is an important chemical with widespread functions in the body. It is part of the cell structure and is key in the maintenance of cellular function, especially in the brain. Taking phosphatidylserine can improve some of the symptoms of Alzheimer’s disease and dementia. Also, it helps improve thinking ability, attention, impulse control, and hyperactivity in children and teens with attention deficit hyperactivity disorder (ADHD).
- Inositol – is once considered a member of vitamin B complex. It has a role in nervous system and fat metabolism. It helps in production of healthy cells in the bone marrow and cell membrane production – myelin sheath. Also, it is important for hair growth.
- Ginseng Extract – Ginseng effectively regulates the immune response and the hormonal changes due to stress, thus maintaining homeostasis.
 In addition to suppressing the occurrence of psychological diseases such as anxiety and depression, ginseng also prevents stress-associated physiological diseases.
In addition to suppressing the occurrence of psychological diseases such as anxiety and depression, ginseng also prevents stress-associated physiological diseases. - Soy Lecithin – composed of phosphatidylcholine. It improves memory and learning ability. It also helps reduce the risk of gall stones and improve liver function. Research shows that it helps improve brain function and can prevent dementia.
- L-Carnitine L-Tartrate – has an important role in acetylcholine production. It helps improve brain function and dementia. This amino acid can pass through blood brain barrier (BBB) and regulates neurotransmitter level in the brain.
- Vitamin C (Calcium Ascorbate) – plays an important role in the body. It is needed to maintain the health of skin, cartilage, teeth, bone, and blood vessels. It is also used to protect your body’s cells from damage. It is known as an antioxidant. Also, it helps regulate body temperature and hormonal production.
- Vitamin A Acetate – is an important fat-soluble vitamin. It promotes good vision and counteracts night blindness and eye disorders. Vitamin A aids in proper function of immune system. It is also necessary for normal cell growth and development. Another important role is it is an antioxidant that protect cells from free-radical damage.
- Vitamin E DL-Alpha-Tocopheryl Acetate) – fights free radicals and prevents disease development. Certain isomers of vitamin E have powerful antioxidant abilities that have the power to reduce free radical damage, fight inflammation, and therefore help naturally slow aging in your cells and fight off health issues like heart disease, hypertension, aging, and cancer.
- Vitamin B Complex – B complex vitamins help your body make energy from the food you eat, form red blood cells, and play an essential role in certain bodily functions. Vitamin B1 is a therapeutic agent for neuropathy.
 Vitamin B2 helps convert food into energy. Vitamin B3 helps enzymes in the body function properly by helping the body use other B vitamins. Vitamin B5 promotes digestive system and healthy skin. Vitamin B6 involves in immune function and brain development. It aids in the formation of neurotransmitters. Vitamin B12 is required for the formation of red blood cells and DNA. It is important for protein metabolism.
Vitamin B2 helps convert food into energy. Vitamin B3 helps enzymes in the body function properly by helping the body use other B vitamins. Vitamin B5 promotes digestive system and healthy skin. Vitamin B6 involves in immune function and brain development. It aids in the formation of neurotransmitters. Vitamin B12 is required for the formation of red blood cells and DNA. It is important for protein metabolism.
Every brain changes with age, and mental function changes along with it. Mental decline is common, and it’s one of the most feared consequences of aging. There are ways you can help to maintain brain function: reducing the use of smartphone, tablet, and computer, getting enough rest, eating healthy food, and taking essential supplements that prepared by a team of experts. These can help improve memory, reduce stress, and maintain emotional balance.
Reasons You May Have Brain Fog
Medically Reviewed by Brunilda Nazario, MD on June 22, 2021
“Brain fog” isn’t a medical condition. It’s a term used for certain symptoms that can affect your ability to think. You may feel confused or disorganized or find it hard to focus or put your thoughts into words.
It’s a term used for certain symptoms that can affect your ability to think. You may feel confused or disorganized or find it hard to focus or put your thoughts into words.
Many women find it’s harder to remember things during pregnancy. Carrying a baby can change your body in lots of ways, and chemicals released to protect and nourish your baby may bring on memory problems.
This disease affects your central nervous system and can change the way your brain “talks” to the rest of your body. About half the people who have MS have issues with memory, attention, planning, or language. Learning and memory exercises can help, and a therapist can give you new ways to handle the tasks you have trouble with.
Some kinds of drugs -- over-the-counter and prescribed -- can cause brain fog. If you take medicine and notice that your thinking isn’t as clear as it should be or you suddenly can’t remember things, call your doctor. Be sure to let them know all the medications you take. It is suspected that sensitivity to some chemicals (both natural and man-made) can also cause brain fog, a possibility that is debated in the medical community..
It is suspected that sensitivity to some chemicals (both natural and man-made) can also cause brain fog, a possibility that is debated in the medical community..
Chemotherapy -- a treatment for cancer that uses strong drugs -- can lead to what’s sometimes called “chemo brain.” You may have trouble remembering details like names or dates, have a hard time multi-tasking, or take longer to finish things. It usually goes away fairly quickly, but some people can be affected for a long time after treatment. Cancer itself can also cause “brain fog,” for instance, if the cancer has affected the brain.
Women may find it harder to learn or remember things when they reach this stage of life. It happens about a year after their last period, usually around age 50. Along with brain fog, they also may have hot flashes -- sudden sweating with a higher heart rate and body temperature -- and other body changes. Hormone supplements and other types of medication may help.
With this condition, your body and mind are tired for a long time. You may feel confused, forgetful, and unable to focus. There’s no known cure for CFS, but medication and talk therapy may help.
You may feel confused, forgetful, and unable to focus. There’s no known cure for CFS, but medication and talk therapy may help.
You may not remember things well or be able to think through problems easily. It’s hard to know if this is linked to the loss of energy and motivation that comes with depression, or if depression affects your brain in a way that causes the fog. Treatment for your depression, which includes medication and talk therapy, should help get you back on track.
You need sleep to help your brain work the way it should, but too much can make you feel foggy, too. Aim for 7 to 9 hours. To get good rest at bedtime, you may want to avoid caffeine and alcohol after lunch or right before bedtime and keep the computer and smartphone out of your bedroom. It also can help to get to bed and wake up at the same time every day. Talk to your doctor if you think your brain fog might be caused by a sleep disorder like apnea, insomnia, or narcolepsy.
This long-term disease causes your immune system to attack your body, and the symptoms can be different in different cases. About half the people with lupus have problems with memory, confusion, or trouble concentrating. There’s no cure, but medication and talking with a therapist can help.
About half the people with lupus have problems with memory, confusion, or trouble concentrating. There’s no cure, but medication and talking with a therapist can help.
IMAGES PROVIDED BY:
1) Getty
2) Getty
3) Science Source
4) Getty
5) Getty
6) Getty
7) Getty
8) Getty
9) Getty
10) Medical Images
SOURCES:
American Cancer Society: “Chemo Brain.”
Brain and Cognition: “Assessment of cognitive function across pregnancy using CANTAB: A longitudinal study.”
CDC: “Sleep and Sleep Disorders.”
Health Guidance.org: “Brain Fog Causes.”
Journal of Hypertension: “Flavanol-rich chocolate acutely improves arterial function and working memory performance counteracting the effects.”
LiveScience: “Menopausal 'Foggy Brain' Confirmed in Tests.”
Lupus Research Alliance: “Can Lupus Affect My Brain?” “About Lupus.”
Mayo Clinic: “Chronic Fatigue Syndrome,” “Depression,” “Menopause. ”
”
National Institutes of Health: “The Risks of Sleeping 'Too Much'. Survey of a National Representative Sample of 24671 Adults (INPES Health Barometer),” “What is brain fog? An evaluation of the symptom in postural tachycardia syndrome,” “Cognition in perimenopause: The effect of transition stage.”
National Sleep Foundation: “Debunking Sleep Myths: Does Alcohol Help or Hurt Your Sleep?”
Marin Optimal Health: “Brain Fog: Anxiety, Depression, Insomnia.”
American Sleep Apnea Association: “Brain Awareness.”
Nature and Science of Sleep: “New developments in the management of narcolepsy.”
© 2021 WebMD, LLC. All rights reserved. View privacy policy and trust info
“Unclear head” syndrome, its complex diagnostics and treatment
“Unclear head” is one of the main signs of astheno-neurotic syndrome
If "Unclear head", "Muddy head" - the feeling with which you get up and lie down, and if increased irritability, fatigue and poor sleep are added to this - most likely, we are talking about astheno-neurotic syndrome .
Main symptoms: A lot of people complain about "fog in the head", "head like cotton wool", "unclear head" and similar symptoms.
If you notice overwork, sleep disturbance, constant irritability, then you may have a mental disorder called astheno-neurotic syndrome.
Prevalence: This disease is one of the most common "diseases of civilization". It is often referred to as the "management flu".
The disease affects people who are educated and prosperous. The most characteristic age is from 20 to 40 years. These are entrepreneurs, managers, doctors, teachers. In a special risk group are people whose work is associated with increased responsibility, for example, air traffic controllers.
In the past, astheno-neurotic syndrome was called "nervous exhaustion"
Also at risk are creative individuals.
Causes of occurrence: The main causes of occurrence are stress, prolonged nervous excitement, chronic lack of sleep, constant overwork. Also, factors contributing to the emergence of astheno-neurotic syndrome are past diseases, including colds, some viruses, poisoning, and poor environmental conditions.
Also, factors contributing to the emergence of astheno-neurotic syndrome are past diseases, including colds, some viruses, poisoning, and poor environmental conditions.
Similar symptomatology: What diseases can be manifested as "head as if in a fog", poor sleep, weakness and irritability, except for neurasthenia? First of all, these are asthenic conditions with incipient serious illnesses. In the second - masked depression, which at the beginning can easily be confused with astheno-neurotic syndrome. And chronic fatigue syndrome can manifest itself in a similar way.
So the correct diagnosis can only be made by a psychotherapist or psychiatrist. To make a diagnosis, professional psychological diagnostics (psychotests) are usually used, which you can go through on your own (following this link).
How the disease develops: The syndrome occurs gradually, with a combination of emotional and physical overstrain, constant fatigue. Most often, patients complain of a breakdown, general weakness, increased irritability, "fog" in the head, inability to cope with the usual amount of work.
If a person continues to be stressed further and does not seek medical help, his condition worsens - tearfulness, complaints about the heart, fog in the head join the usual set of complaints about a "cotton" head. Irritability increases to an extreme degree, but irritation is quickly replaced by weakness. Sleep is usually unstable, does not bring a feeling of rest, after sleep the head is “like cotton wool”. Appetite worsens, constipation or diarrhea may disturb. Sexual desire decreases in both men and women. The condition worsens before a change in the weather (the so-called "weather sensitivity"). In the absence of treatment at this stage, apathy, lethargy, severe weakness and a persistent decrease in mood follow. Interest in life is reduced, the patient thinks only about his painful condition, about his "obscure" head.
Left untreated, psychotic disorders can develop.
Treatment: Treatment prospects are positive, usually psychotherapeutic methods give excellent results up to a complete cure. In severe cases, a combination of psychotherapy with psychopharmacotherapy is used.
In severe cases, a combination of psychotherapy with psychopharmacotherapy is used.
Self-medication usually worsens the condition and leads to the progression of the disease.
At the initial stage of the disease, a psychotherapist, in order to make a correct diagnosis, needs to exclude all diseases in which similar symptoms appear, because the more accurate the diagnosis, the more successful the treatment will be.
Different diseases with similar symptoms need to be treated differently. Therefore, it is necessary to consult a psychotherapist. A good psychotherapist selects therapy that is appropriate for the specific manifestations of the disease and the individual characteristics of each patient.
Astheno-neurotic syndrome is one of the most common "diseases of civilization". It is often referred to as the "management flu".
The treatment of the syndrome depends on the severity of the painful symptoms, but is primarily aimed at eliminating psychotraumatic factors. It is necessary to reduce both mental and physical stress. This is the most important condition for treatment, without such measures it will not be possible to defeat the disease. In the early stages of the development of the disease, normalization of the rhythm of life, elimination of stress and psychotherapy may be enough to significantly improve the state of health. And, of course, at this stage, psychotherapy methods that do not use drugs give a very good effect - cognitive-behavioral, psychoanalysis, group psychotherapy methods are very effective.
It is necessary to reduce both mental and physical stress. This is the most important condition for treatment, without such measures it will not be possible to defeat the disease. In the early stages of the development of the disease, normalization of the rhythm of life, elimination of stress and psychotherapy may be enough to significantly improve the state of health. And, of course, at this stage, psychotherapy methods that do not use drugs give a very good effect - cognitive-behavioral, psychoanalysis, group psychotherapy methods are very effective.
In any case, you need to contact a psychotherapist.
In more advanced cases, additional psychopharmacotherapy may be required. General tonic drugs, tranquilizers, if necessary, sleeping pills and antidepressants are used. Psychotherapy is also actively used in the treatment of advanced astheno-neurotic syndrome.
The first indicator of improvement is the normalization of sleep and the disappearance of the feeling of "fog" in the head. With timely prescribed treatment, the problem can usually be completely overcome, however, if the tense situation and stress at work and in personal life continue to persist, various complications are possible.
With timely prescribed treatment, the problem can usually be completely overcome, however, if the tense situation and stress at work and in personal life continue to persist, various complications are possible.
Terminology and other names: In the past, astheno-neurotic syndrome, together with diseases of similar symptoms, was called "nervous exhaustion".
In modern psychiatry, the term "neurasthenia" is more often used to refer to neuro-asthenic syndrome (synonyms). In the everyday sense, neurasthenia is usually perceived as a painfully nervous, unbalanced state, characteristic of weak-willed people, easily amenable to various influences and moods, in a state of acute mental crisis. And in the medical sense, this is a state of depression, irritability, "a vague head."
FGBNU NTSPZ. ‹‹Depersonalization››
Among the cases of psychogenic changes in consciousness according to the type of mental alienation, there were cases with the presence of pathological development of the asthenic type, affectogenic reactions of an asthenic and hysterical nature, and protracted reactions in psychopathic personalities. Patients were observed not only in the course of clinical treatment, but also follow-up.
Patients were observed not only in the course of clinical treatment, but also follow-up.
Let's move on to the presentation of clinical observations.
1. Patient O, 22 years old, student, was admitted with complaints that it seemed to him that "the crown of the head is not his", his hands often get cold, blood goes somewhere. Obsessive states, respiratory constitution, somatically somewhat weak, neurologically hyperreflexia, vegetative lability. There is no pathology in the genus. Developed as a frail, sickly child, often sick. He suffered measles, tonsillitis, influenza. But the character is closed, impressionable, suspicious. After finishing school, he worked as a telegraph operator. He studied at fitter courses, but dropped out due to dizziness and weakness. Soon he developed an anxiety state, the fear of death, arising paroxysmal. This condition arose after intense studies: preparing for exams, sleeping little, not eating regularly. Did not pass the exams; for a long time and extremely strongly worried about this. At times, he suddenly felt a rapid heartbeat - "everything was pounding inside." “The view was obscured by fog, everything seemed unreal, the head was as if not my own”, an influx of strange thoughts: “why do I live”, “what kind of wall”, walked around the room like an automaton, sang. He thought he had a heart defect, he was afraid to go crazy.
At times, he suddenly felt a rapid heartbeat - "everything was pounding inside." “The view was obscured by fog, everything seemed unreal, the head was as if not my own”, an influx of strange thoughts: “why do I live”, “what kind of wall”, walked around the room like an automaton, sang. He thought he had a heart defect, he was afraid to go crazy.
In the clinic: the patient is anxious, often asks the doctor about the state of his heart. He says that at home he carefully studied the anatomy of the heart. Sleeps badly, sudden fears at night, “arms and legs get cold, heart stops”. With the arrival of the doctor quickly calms down. He constantly complains that he does not feel his head, especially the top of his head, often doubts: "My body or not mine." It seems that the face is covered with dirt, becomes wrinkled, alien. Sudden onset of fear causes general weakness, dizziness, it seems that a fainting state sets in, the environment seems strange, incomprehensible, distant, the voice feels alien. Seems like he's in a dream. He asks himself the question: do I exist or not? However, "intelligence" he understands that this is a painful condition. Despite some emotional lethargy and indifference to the environment, the patient has a constant feeling of internal tension, unaccountable anxiety, restlessness and an obsessive fear of death.
Seems like he's in a dream. He asks himself the question: do I exist or not? However, "intelligence" he understands that this is a painful condition. Despite some emotional lethargy and indifference to the environment, the patient has a constant feeling of internal tension, unaccountable anxiety, restlessness and an obsessive fear of death.
This case is a typical, most common manifestation of the alienation syndrome among neurotics. Characteristically, an asthenic personality, as a result of sharp mental experiences about life's failures and the presence of somatic exhaustion and overwork, gives a typical picture of an obsessive state. Moreover, during the period of exacerbation of obsessive fears, the patient experiences alienation phenomena in the sphere of perceptions of his body, voice and environment. The experience of dreamlikeness and a decrease in the experience of one's own existence is characteristic. 9some emotional lethargy and indifference to the environment are striking. Emotions become vague, amorphous, their main content becomes an unconscious fear of death.
Emotions become vague, amorphous, their main content becomes an unconscious fear of death.
Similar emotional states in this group of patients are especially characteristic. So, in one of our patients, the obsessive fear was so unconscious and intense that she exclaimed in despair: “I’m afraid of myself, I want to run away from fear, but I understand that you can’t run away from yourself anywhere.” Emotional expressiveness is quite preserved. Patients talk about the loss of feelings for loved ones, for children, while they really suffer from the fact of losing these feelings.
During paroxysmal states of alienation, patients also experience changes in the shape, size of individual parts of the body and surrounding objects (macro-micropsy, metamorphopsia). Often accompanied by peculiar sensations in the head, on the surface of the body in the form of colic, numbness, heat in the center of the brain, a feeling of fullness from the inside of the head, etc.
2. Patient B. , 16 years old, a schoolboy, was admitted with complaints of headaches, feeling of heat in the eyes and on the face, fatigue, depressed mood. There is nothing pathological in the family. The patient grew up as a sickly child, suffered three times pneumonia, diphtheria, measles, whooping cough, tonsillitis, influenza and malaria. By nature he was cheerful, sociable, studied well at school. From the age of 13 he began to help his mother, worked and studied at the same time. At the age of 14, he lost his mother and father. The tragic death of his parents had an unusual effect on the sensitive and somatically weak young man. The patient fell into a deep apathy, lost the desire to live, headaches appeared, it seemed that the brain was turning over. There were strange sensations for him that his soul was leaving him, but his body remained; felt like in a dream, it seemed that he did not exist.
, 16 years old, a schoolboy, was admitted with complaints of headaches, feeling of heat in the eyes and on the face, fatigue, depressed mood. There is nothing pathological in the family. The patient grew up as a sickly child, suffered three times pneumonia, diphtheria, measles, whooping cough, tonsillitis, influenza and malaria. By nature he was cheerful, sociable, studied well at school. From the age of 13 he began to help his mother, worked and studied at the same time. At the age of 14, he lost his mother and father. The tragic death of his parents had an unusual effect on the sensitive and somatically weak young man. The patient fell into a deep apathy, lost the desire to live, headaches appeared, it seemed that the brain was turning over. There were strange sensations for him that his soul was leaving him, but his body remained; felt like in a dream, it seemed that he did not exist.
In the clinic, the patient constantly complains of headaches pressing from the inside, of feeling as if he "has only eyes and nothing else. " When he reads a book, it seems that he does not exist, but reads about himself in the book. While working in workshops, he does not feel himself and works like an automatic machine. In the evenings, thoughts flow mechanically, he loses his will over them. “My thoughts scatter, overtake each other, I want to say something and do not have time to put them into words.” Often tries to convince himself of the reality of the environment. He says in his mind: “This is a garden, these are trees, this is a house,” but still he does not really perceive them: “everything is vague, like in a fog.” These states are painful and painful. The patient experiences a slowdown in body movement. Sometimes it seems to him that if he jumps from the second floor into the garden, then nothing will happen to him, since he will slowly, smoothly, go down. I did not feel my weight, while walking it seems that I am floating in the air. There are a number of obsessive thoughts and fears. By the end of his stay at the clinic, his condition improved.
" When he reads a book, it seems that he does not exist, but reads about himself in the book. While working in workshops, he does not feel himself and works like an automatic machine. In the evenings, thoughts flow mechanically, he loses his will over them. “My thoughts scatter, overtake each other, I want to say something and do not have time to put them into words.” Often tries to convince himself of the reality of the environment. He says in his mind: “This is a garden, these are trees, this is a house,” but still he does not really perceive them: “everything is vague, like in a fog.” These states are painful and painful. The patient experiences a slowdown in body movement. Sometimes it seems to him that if he jumps from the second floor into the garden, then nothing will happen to him, since he will slowly, smoothly, go down. I did not feel my weight, while walking it seems that I am floating in the air. There are a number of obsessive thoughts and fears. By the end of his stay at the clinic, his condition improved. Somatically recovered well.
Somatically recovered well.
This observation of an asthenic reaction occurs as a result of a sharp mental trauma that deeply shakes the emotional sphere of a sensitive and somatically weak young man. Along with hypochondriacal complaints and the experience of alienation, derealization of external objects, there is a deautomatization of the thought process, the phenomenon of mentism. The patient loses control over his thoughts. Curious are the experiences that often occur in a dream, especially in adolescents: the patient did not feel the weight of his body, it seemed that he was not walking, but floating in the air; I thought that if he jumped from the second floor, he would not break, but smoothly and slowly go down.
After somatic strengthening, the patient's condition improves rapidly.
3. Patient D., 28 years old, accountant, was admitted with complaints of colic and heaviness in the head, strong heartbeat, tinnitus, ringing and beeping in the head, and beating in the abdomen. The patient is of a muscular physique, from the side of somatics - nothing pathological. Increased muscle excitability, hyperreflexia, vasomotor lability. There is no pathology in the genus. Developed as a lively, impressionable, suspicious boy. After finishing school, he worked in a shop. A year later, he was removed from work and exiled for embezzling money. For good work, after 2.5 years, he was released ahead of schedule. Married. Family life was unsuccessful. At home there were frequent quarrels and fights. Gradually, he began to feel increased fatigue, heaviness in the head, it seemed that the body was being filled with something, obsessive fears, sweating, chills, fainting, subfebrile temperature. Cardiopalmus. In the clinic: the patient was very willing and spoke in detail about his experiences. Complaints about a feeling of pressure in the head, pain in the temples and heart, a feeling of unreality of the surroundings, it seems that "things are breathing, they are about to fall on me.
The patient is of a muscular physique, from the side of somatics - nothing pathological. Increased muscle excitability, hyperreflexia, vasomotor lability. There is no pathology in the genus. Developed as a lively, impressionable, suspicious boy. After finishing school, he worked in a shop. A year later, he was removed from work and exiled for embezzling money. For good work, after 2.5 years, he was released ahead of schedule. Married. Family life was unsuccessful. At home there were frequent quarrels and fights. Gradually, he began to feel increased fatigue, heaviness in the head, it seemed that the body was being filled with something, obsessive fears, sweating, chills, fainting, subfebrile temperature. Cardiopalmus. In the clinic: the patient was very willing and spoke in detail about his experiences. Complaints about a feeling of pressure in the head, pain in the temples and heart, a feeling of unreality of the surroundings, it seems that "things are breathing, they are about to fall on me. " The sounds of his voice are unclear, vague. “I perceive the voices of people not as sounds, but as injections on the body.” The head at times seems large, as if separated from the body, falling into the abyss. Something makes you push, touch and interfere with people. At times he feels his body is alien, inanimate. Expresses a lot of hypochondriacal complaints. Emotionally quite alive, intelligence is preserved By the end of the third month, the patient's condition has improved significantly.
" The sounds of his voice are unclear, vague. “I perceive the voices of people not as sounds, but as injections on the body.” The head at times seems large, as if separated from the body, falling into the abyss. Something makes you push, touch and interfere with people. At times he feels his body is alien, inanimate. Expresses a lot of hypochondriacal complaints. Emotionally quite alive, intelligence is preserved By the end of the third month, the patient's condition has improved significantly.
In this observation, the presence of somato-vegetative disorders and the mass of hypochondriacal complaints regarding bodily sensations, significant hyperesthesia are striking. The phenomena of alienation, mainly in the sphere of perceptions of one's own body and the environment, and they are of a more elementary nature. Psychopathological symptoms disappeared after strengthening the somato-vegetative sphere as a result of treatment.
4. Patient D., 38 years old, office worker. She was admitted to the clinic with complaints of anxiety and fear about a change in the sense of the body - a feeling of a change in the shape of the thigh and buttocks, a violation of the sense of self by obsessive states. The patient is respiratory addition with digestive components. There are no deviations from the internal organs. There are significant changes in the autonomic nervous system - a sharp vasomotor lability, intense, diffuse dermography, skin depigmentation in separate areas, dry skin, increased reflex excitability, the thyroid gland is noticeably palpable. The patient developed in childhood lively, impressionable, modest. At school, she was sociable, she studied well. Parents married early, against her wishes, to a man much older in age and with amputated legs. Despite the good material living conditions, the patient very often worried because of the rude and despotic character of her husband. In addition, the husband led a dissolute life and did not hide his ties from his wife.
She was admitted to the clinic with complaints of anxiety and fear about a change in the sense of the body - a feeling of a change in the shape of the thigh and buttocks, a violation of the sense of self by obsessive states. The patient is respiratory addition with digestive components. There are no deviations from the internal organs. There are significant changes in the autonomic nervous system - a sharp vasomotor lability, intense, diffuse dermography, skin depigmentation in separate areas, dry skin, increased reflex excitability, the thyroid gland is noticeably palpable. The patient developed in childhood lively, impressionable, modest. At school, she was sociable, she studied well. Parents married early, against her wishes, to a man much older in age and with amputated legs. Despite the good material living conditions, the patient very often worried because of the rude and despotic character of her husband. In addition, the husband led a dissolute life and did not hide his ties from his wife. The only consolation was the child, whom she loved excessively. The relationship between the spouses gradually became so aggravated that she had to leave her husband. Lived in the next room; the child remained with the father. This caused extremely severe suffering. There were headaches, irritability, depressed mood, insomnia. One morning, meeting her son in the corridor, she was struck by his appearance: it seemed to her that he had changed (face, height), became somehow alien and distant; felt with horror that she had no feeling of love for him. This painful condition subsequently entrenched. In a state of painful experiences, the patient was admitted to the clinic). Here, in a conversation with a doctor, she remembered that she already had similar experiences of alienation and indifference to the child some time after the birth, but then this condition disappeared within a few weeks.
The only consolation was the child, whom she loved excessively. The relationship between the spouses gradually became so aggravated that she had to leave her husband. Lived in the next room; the child remained with the father. This caused extremely severe suffering. There were headaches, irritability, depressed mood, insomnia. One morning, meeting her son in the corridor, she was struck by his appearance: it seemed to her that he had changed (face, height), became somehow alien and distant; felt with horror that she had no feeling of love for him. This painful condition subsequently entrenched. In a state of painful experiences, the patient was admitted to the clinic). Here, in a conversation with a doctor, she remembered that she already had similar experiences of alienation and indifference to the child some time after the birth, but then this condition disappeared within a few weeks.
In the clinic, the patient underwent a course of physiotherapy, hypnotherapy and was discharged with significant improvement.
The patient remarried, but her life was again unsuccessful. The husband turned out to be an apathetic, inert and sexually impotent person. He earned little. I had to endure financial hardship. The patient entered shorthand courses, studied well, but did not complete them because of the deterioration of her condition. Thoughts of divorce arose; she communicated this decision to her husband. He categorically refused a divorce. She was sure now that he had only married because of her room. Haven't had sex with him for over a year. Her condition began to worsen again, a depressed mood arose, obsessive thoughts, "self-digging" in her experiences. One day, the patient, going naked to the mirror, was surprised by the change in the shape of the thigh and buttocks: it seemed to her that one side of this part of the body had become much thinner. I began to think. Gradually, a feeling of alienation began to arise, to "extra" one's buttocks and thighs. She literally felt this strange state, although she was critical of it. There was a fear of myself.” She began to feel the absence of personality, “as if I didn’t exist”, especially strongly she felt alienation and even at times the absence of the gluteal region of the body. The patient became frigid. Her suffering over these conditions was so excruciating that thoughts of suicide repeatedly arose. Re-entered the clinic. In the clinic: the patient constantly complains of obsessive experiences of changes in the gluteal region of the body and a sense of "self". Contact, sociable, neat, takes good care of her appearance. Anxious, depressed. He tries to distract himself from painful sensations by work and reading. Takes physiotherapy and hypnosis sessions. Easily falls into a hypnotic state. During the session, it was experimentally possible to repeatedly suggest the absence of individual parts of the body, such as the head, arms, etc.; in a hypnotic state, she was inspired by a full-fledged sense of reality, the physicality of the gluteal region. Gradually, the patient began to feel better, obsessive states disappeared, fear, anxiety, the feeling of the gluteal region was restored.
There was a fear of myself.” She began to feel the absence of personality, “as if I didn’t exist”, especially strongly she felt alienation and even at times the absence of the gluteal region of the body. The patient became frigid. Her suffering over these conditions was so excruciating that thoughts of suicide repeatedly arose. Re-entered the clinic. In the clinic: the patient constantly complains of obsessive experiences of changes in the gluteal region of the body and a sense of "self". Contact, sociable, neat, takes good care of her appearance. Anxious, depressed. He tries to distract himself from painful sensations by work and reading. Takes physiotherapy and hypnosis sessions. Easily falls into a hypnotic state. During the session, it was experimentally possible to repeatedly suggest the absence of individual parts of the body, such as the head, arms, etc.; in a hypnotic state, she was inspired by a full-fledged sense of reality, the physicality of the gluteal region. Gradually, the patient began to feel better, obsessive states disappeared, fear, anxiety, the feeling of the gluteal region was restored. Discharged from the clinic in good condition.
Discharged from the clinic in good condition.
This patient is of exceptional interest in relation to the mechanism of occurrence of experiences of alienation. Constant psycho-traumatic moments during a life together with her first husband were the cause of sharp affective experiences of an impressionable, easily excitable woman. These states of a long-term nature led to a pronounced disorder of the vegetative-endocrine sphere. On this basis, the phenomena of alienation grow. Moreover, a characteristic feature of the manifestation of these states is that the content of alienated images is always dependent on traumatic moments and follows logically from these traumatic situations. So, a sudden experience. alienation of the perception of the child and the loss of feelings for him occurs after a short period of time after the divorce from the first husband.
Further, a new experience of alienation of the gluteal region of one's body with irradiated phenomena of alienation of the whole body and even one's personality arises after a second unsuccessful marriage. Constant need, apathetic, inert nature of her husband, his indifference to her and complete sexual impotence - all this led to frequent family conflicts.
Constant need, apathetic, inert nature of her husband, his indifference to her and complete sexual impotence - all this led to frequent family conflicts.
As a result of these long-term affective traumas, states of alienation reappear, which begin with a feeling of alienation of one half of the gluteal region of the body and frigidity; then there are sensations of the unreality of the whole body and of one's personality. These states are accompanied by excruciating suffering.
How can one explain that the content of the experience of alienation follows so logically and understandably from a traumatic situation? Is this not a voluntaristic tendency to repress the sexual nature of type of Freudian mechanisms? Schilder, explaining depersonalization in this spirit, considers it "an unsuccessful escape from unbearable reality." Gaug reasonably objects to this view, saying that patients do not have any benefit from this, the advantage from the fact that they change one unpleasant experience for another unpleasant experience. This, in his opinion, (is just a figuratively symbolic metaphorical way of considering the problem.
This, in his opinion, (is just a figuratively symbolic metaphorical way of considering the problem.
Indeed, this mechanism cannot be explained by voluntarism alone. It is well known that if you fix your attention on a certain part of the body, you can clearly feel it, highlighting it from others. However, with a long, affectively saturated concentration of attention on a separate part of the body in a vegetatively labile personality, it can easily lead to the opposite result, i.e., to a pathological form of inhibition of an ultra-paradoxical nature (Pavlov): the patient completely ceases to feel this area of the body. It is very likely that the mechanism of alienation of the gluteal region of the body in our patient occurs according to the indicated type. This type is closely related to the mechanism of hypnotic inhibition.
In our other patient, along with the state of dreamlikeness and unreality of the surroundings, peculiar experiences of the loss of the semantic meaning of words were observed, which became strange and incomprehensible. The patient also developed phenomena of deautomatization of the respiratory act: her attention was compulsively riveted to observing the act of breathing and regulating its rhythm.
The patient also developed phenomena of deautomatization of the respiratory act: her attention was compulsively riveted to observing the act of breathing and regulating its rhythm.
In the third patient, under the influence of sharp emotional experiences, fallout of a hysterical functional nature occurs. Against the background of these fallouts, the phenomena of alienation, splitting of one's personality and the phenomenon of a "double" (autoscopy) appear.
5 Patient K., aged 24, a final year student at the Construction Institute. He was admitted to the clinic with complaints of general lethargy, weakness, heaviness in the head, unrealistic perceptions, obsessive thoughts, and fear. From the side of the nervous system: cyanosis and small tremor of the fingers, twitching of individual muscles of the limbs, high tendon reflexes, red, persistent dermographism.
By nature, soft, impressionable, prone to daydreaming, intellectually gifted. At the age of 14 - phenomena of alienation and unreality of the external world and obsessive fears. In the fifth year, these states reappeared with even greater force. There was a feeling of some kind of withering, "twilight worldview", vague anxiety. All movements in the environment seem to him mechanical, as if "in another mental dimension." The patient at the same time says that "the environment seems to be glassy, retains the duality of the photographic image - movement and stillness." In the clinic, the patient is tense, confused, attention is riveted to his experiences. He especially complains about the unreal nature of perceptions, uncertainty, vagueness and alienation of figurative representations, a feeling of a split personality: “as if there are two “I”s in me, one “I” acts, and the other observes.” At times it seems that the body, as well as the voice, is not his own, but someone else's. All impressions seem to him "as if weighed in the mind, that automatic immutability, the organic perception that was characteristic of me disappears." The patient compares the unreal nature of his perceptions with the perception of the lunar landscape, “frozen lighting, sharply defined shadows, cold glare of bright light, everything bears the stamp of a strange, disturbing immobility, a cold dead feeling.
In the fifth year, these states reappeared with even greater force. There was a feeling of some kind of withering, "twilight worldview", vague anxiety. All movements in the environment seem to him mechanical, as if "in another mental dimension." The patient at the same time says that "the environment seems to be glassy, retains the duality of the photographic image - movement and stillness." In the clinic, the patient is tense, confused, attention is riveted to his experiences. He especially complains about the unreal nature of perceptions, uncertainty, vagueness and alienation of figurative representations, a feeling of a split personality: “as if there are two “I”s in me, one “I” acts, and the other observes.” At times it seems that the body, as well as the voice, is not his own, but someone else's. All impressions seem to him "as if weighed in the mind, that automatic immutability, the organic perception that was characteristic of me disappears." The patient compares the unreal nature of his perceptions with the perception of the lunar landscape, “frozen lighting, sharply defined shadows, cold glare of bright light, everything bears the stamp of a strange, disturbing immobility, a cold dead feeling. It seems that all things and phenomena have lost some kind of inner meaning inherent in them, and I insensibly contemplate only the dead shell inherent in them, the form. In the evenings in bed, with eyes closed, he notes the sudden appearance of vivid images in a strange absurd combination, for example, a lamp, a wheel, a window, and some strange physiognomy. The patient often talks about the spread of thoughts, the lack of synthesis. He fights with the spread of thoughts with the help of "thinking aloud", that is, talking with himself and writing thoughts. Gradually, he develops an uncharacteristically preparedness for supernatural phenomena and mysticism. He complains about the growing emotional insufficiency not only to those around him, but also to his relatives. “When I see my relatives, whom I also perceive insufficiently realistically and concretely, some kind of alienation and indifference to these people close to me arise in my mind.” By the end of the stay in the clinic, the patient's condition improved somewhat.
It seems that all things and phenomena have lost some kind of inner meaning inherent in them, and I insensibly contemplate only the dead shell inherent in them, the form. In the evenings in bed, with eyes closed, he notes the sudden appearance of vivid images in a strange absurd combination, for example, a lamp, a wheel, a window, and some strange physiognomy. The patient often talks about the spread of thoughts, the lack of synthesis. He fights with the spread of thoughts with the help of "thinking aloud", that is, talking with himself and writing thoughts. Gradually, he develops an uncharacteristically preparedness for supernatural phenomena and mysticism. He complains about the growing emotional insufficiency not only to those around him, but also to his relatives. “When I see my relatives, whom I also perceive insufficiently realistically and concretely, some kind of alienation and indifference to these people close to me arise in my mind.” By the end of the stay in the clinic, the patient's condition improved somewhat. He stated that the improvement is due to getting used to his painful experiences, he became somewhat more alive, however, the activity is still insufficient in the patient after treatment in the clinic over the past three years, these conditions periodically appear.
He stated that the improvement is due to getting used to his painful experiences, he became somewhat more alive, however, the activity is still insufficient in the patient after treatment in the clinic over the past three years, these conditions periodically appear.
This clinical observation is of great interest.
Even at puberty, the patient has obsessive states with phenomena of alienation of the perceptions of the outside world. Intensified intellectual studies in the fifth year of the institute again cause these states, but in a pronounced form. A gifted and intellectually developed patient vividly conveys his experiences of alienation not only of perceptions, ideas of his body and the outside world, but also of the alienation of his personality, his "I", which seems to him to be bifurcated. These states are not paroxysmal, but constant, last for more than a year, and then in subsequent years occur periodically, briefly and less intensely.
It is very important to note that such patients, if in the first period of the disease they experience anxiety and excruciating fear, then later they get used to these conditions.
In another case observed by us, it was remarkable that the patient experienced pronounced phenomena of mental alienation for almost one year and at the same time worked well in production as an engineer. He came out of this state one day suddenly: during the exacerbation of the obsessive state of fear of death. Sometimes he felt how the “fog in his eyes” disappeared and the whole world cleared up. However, the patient's joy at the return of a sense of reality is overshadowed by a sharp increase in obsession and hypochondriacal experiences.
The entire group of patients with a psychogenic picture of the alienation syndrome, overwhelmingly in the premorbid state, is characterized by pronounced asthenic character. The morbid state proceeds, as a rule, in a non-psychotic form. Patients are well oriented in the environment, the consciousness is clear, the intellectual processes are preserved, the behavior is correct. They can even work in this state. One of our patients in this condition even passed the state exams at the institute with excellent marks.
Patients complain of a state of alienation in almost all of its forms. When explaining their experiences, they always add the word “seems” or “as if”. They say that with their minds they understand that the world has not changed, but they feel differently. They understand well that their consciousness is still there, but it “seems” that their personality and I disappear, split into two. These conditions often occur paroxysmal, but often proceed continuously throughout the year and even several years.
Patients speak of a decrease and even loss of their senses; most often they suffer from the consciousness of “loss of feeling”. However, objectively sick people can experience even very deep emotions. The expressiveness of facial and pantomimic movements is intact.
Affectivity in patients often manifests itself in the form of inexplicable, unaccountable and vague states of intense anxiety, anxiety and fear. The phenomena of alienation are most often accompanied by obsession and hypochondria.