Supporting a friend with depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.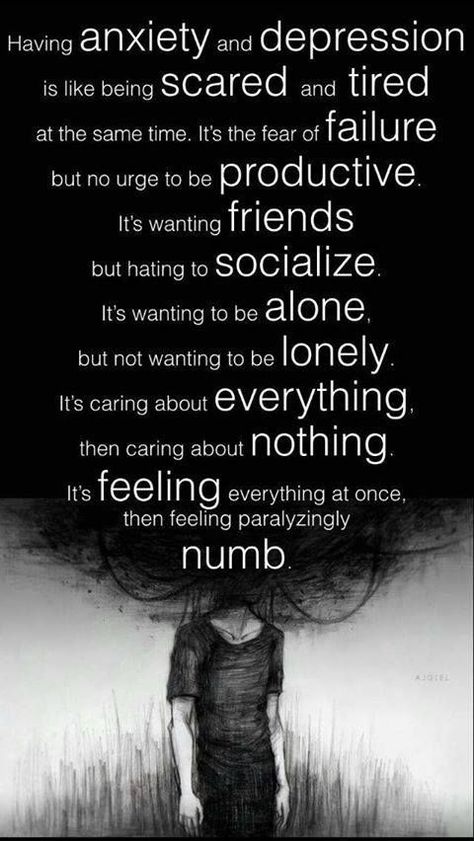 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.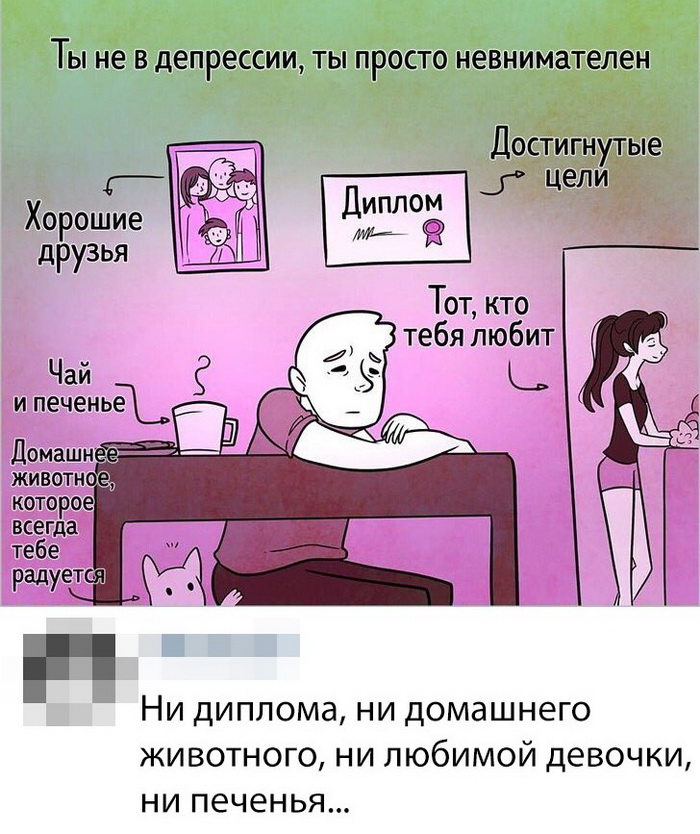 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
6 phrases to support a loved one in a difficult period
338 073
Practices how to Antistress
1. “Just know: I am always there”
Having made it clear that you are ready to be there in any situation, you are already providing support. A suffering person realizes how painful, and sometimes burdensome for others, his condition, and begins to close himself off from people. Your words will make him feel less alone and isolated.
You can even say nothing - just be there, listen, or just be silent together. Your presence will help a person overcome the internal blockade, will make him feel: he is still loved and accepted.
Your presence will help a person overcome the internal blockade, will make him feel: he is still loved and accepted.
2. “What can I do to help you?”
People experiencing a psychological breakdown are often unable to answer this question. However, your words will help someone who is going through a difficult period to listen to himself, to his desires.
Even if you are told that you don't need anything, believe me - it was very important to hear this question. And if a person decides to tell and you listen to him, it will be a huge help for him.
3. “I really like you…”
In moments of depression, we lose self-confidence and often self-respect. And if you make a compliment, pointing out the winning sides and qualities: delicate taste, attention and kindness, features of appearance, this will help you start treating yourself with more attention and love.
4. “Yes, I also think that it is hard and unfair”
Deep experiences make you mentally return to the events that caused them again and again, and the environment begins to seem that he is exaggerating and it is high time to pull himself together.
Depressed people become hypersensitive, and in order for the interlocutor to trust you, it is important to make it clear that you share his emotions. You acknowledge that he has been treated unfairly and the circumstances he is going through are difficult. If he feels that his bitter feelings are accepted, and not devalued, he will more likely find the strength to move on.
5. "I'll help you find a way out"
If you see a person sinking into a deep depression, the best thing you can do is help them get professional support.
For many people who have never experienced therapy before, the prospect of going to a specialist is daunting. You can contact a psychotherapist yourself and invite a loved one to accompany him to the first appointment. In a state of depression, there is often no strength to turn to outside help, and your support will be invaluable.
6. “I understand you: it happened to me too”
If you or someone close to you has gone through similar ups and downs in life, tell us about it. Your openness will help the person become more outspoken.
Your openness will help the person become more outspoken.
The more and more freely he talks about what torments him, realizing that words resonate, the less helpless and lonely he feels. And gradually the situation will begin to be perceived not so hopeless.
About the Author: Gene Kim is Professor of Psychiatry at George Washington University.
Text: Sabina Safarova Photo Source: Getty Images
New on the site
Why we avoid doctors: 3 main reasons
“I can’t get a job because I’m afraid to go out”
How to use the archetype to find your superpower and find your ideal job humiliation. But how can I stop being sensitive?”
“I’m afraid to find my father dead in the apartment”
Global gender difference: how men and women choose work
Supporting a partner with depression
11/22/2019
Depression is one of the most common mental disorders, affecting more than 350 million people of all age groups.
Every year about 150 million people in the world lose their ability to work due to depression
The support of family and friends is essential in the treatment of mental disorders. However, depression can negatively impact relationships and leave loved ones feeling helpless, frustrated, or afraid.
There are ways people can support a partner with depression on their journey to recovery.
Questions to ask about symptoms
To understand the severity of a person's depression, it is helpful to study how these symptoms affect their life.
Asking about symptoms also shows a person that his partner is interested in his feelings and experiences.
Useful questions to ask include:
- Can you help me understand how you feel?
- What activities do you find enjoyable right now?
- Do you enjoy spending time with other people?
- What's wrong with your energy?
- Do you sleep more or less than usual?
- Do you eat more or less than usual?
- Can you focus on things right now?
- Do you have thoughts of death or suicide?
Questions to avoid
Avoid asking questions that seem judgmental or that place blame on the person with depression. They may already be blaming themselves for their symptoms and need support rather than further judgment.
They may already be blaming themselves for their symptoms and need support rather than further judgment.
It is also important not to oversimplify depression, which is a serious illness.
Examples of questions to avoid include:
- Why can't you just cheer up?
- Don't I make you happy?
- When will you feel better?
- Don't you realize that it's all in your head?
- Why do you attach such importance to this?
- Do you know that others are in a much worse situation than you?
Partner support
1. Learn about depression
Learning about depression can make it easier to support those with depression. Learning about symptoms often helps people recognize symptoms in their loved ones.
Symptoms can range from mild to severe and may change over time. However, symptoms must last at least 2 weeks before a doctor can diagnose depression.
Symptoms of depression may include:
- feelings of sadness, worthlessness or guilt
- loss of interest in previously enjoyable activities
- changes in appetite or weight
- changes in sleep habits
- fatigue and loss of energy
- difficulty concentrating or making decisions
- thoughts of death or suicide
2. Understand and acknowledge your partner's feelings
It is important to listen to a person with depression and express empathy, which is the ability to understand and share other people's feelings. One way to show empathy is to mirror what the person is saying.
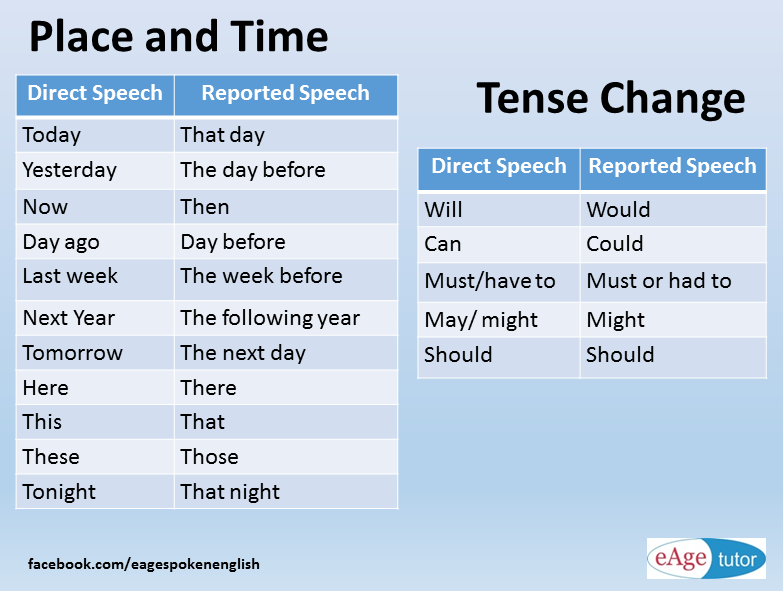
For example, if he says, "I just feel like things will never get better," their partner might reflect this by saying, "that sounds like you're not hopeful for the future."
Constant attempts to cheer up a person are useless, as this devalues his condition and feelings. Phrases like “tomorrow will be better” or “try to cheer up” do not take into account the nature of the disease.
Phrases like “tomorrow will be better” or “try to cheer up” do not take into account the nature of the disease.
3. Ask your partner what they want from you
To show further understanding and support, ask the person what they need. He may need:
- medication reminders
- company when visiting a doctor or visiting therapy
- homemade meals
- encouragement to socialize or exercise
- hug or hold the hand
- to sometimes be left alone
Useful questions to ask include:
- How can I help you?
- Would it be helpful if I...?
4. Encourage your partner to heal
Depression can cause a person to lose their motivation, which can be a barrier to seeking treatment. However, most people with depression need treatment to get better.
Those who support someone with depression can play an important role in their recovery by encouraging them to seek medical help.
To inspire a partner to seek treatment, a person can try:
- joint detection and documentation of your partner's symptoms
- expression of desire to help
- discussion of treatment options such as medication, psychotherapy and lifestyle changes
- accompaniment to doctor appointments
5. Support your partner during recovery
Recovery from depression can sometimes be difficult. To support a partner in the recovery process:
- help them keep track of their prescriptions and medications
- do some physical exercise together
- plan and prepare healthy meals together
- try to reduce stressors at home
- make your goals small and achievable
- encourage them to socialize with other people
- plan fun activities together
- pay attention to the person's progress towards recovery
- avoid forcing treatment on a person
Let your partner know they are not alone when you say:
- I'm here for you.

- We'll deal with this together.
6. Accept that there will be bad days
People with depression have good days and bad days. To cope with bad days:
- expect them to happen
- understand that this is a normal part of depression
- don't give up love and support at this time
- take some time and do something nice, either alone or with others
- remember that not every day will be like this - there will be good days
7. Take care of yourself
When a person supports a partner with depression, it is very important to take the time to enjoy hobbies and other activities for yourself.
Caring for a partner with depression can be draining, frustrating and intimidating.
Research shows that having a spouse with depression increases a person's risk of developing depressive symptoms. This risk is especially high when a man is supportive of a depressed woman.
Those caring for someone with a mental illness should also take care of their own mental health. They can do it:
- trying to stay positive
- having realistic expectations about the recovery process
- knowing that they also have the right to be heard and respected
- taking time out and doing pleasurable activities and hobbies
- interacting with other people besides their partner
- seeking help from friends or relatives
- doing regular exercise
- eating healthy
- trying to get more sleep and rest
- visiting a psychologist or psychological support groups
Professional support
Professional treatment is an important part of the recovery process. The first step is often to see a doctor, who can recommend treatment, psychotherapy, or both.
For particularly severe depressive symptoms or in life-threatening situations, seek emergency care.
Beginning of form
People with depression may be at risk of suicide. According to the American Foundation for Suicide Prevention, more than half of those who die by suicide suffer from major depression.
Partners of those who suffer from depression should be aware of the warning signs of suicide so that they can take prompt action if necessary. Warning signs include:
- talking about death or suicide
- having a suicide plan
- preparation of means of suicide, e.g. collection of pills
- preparation for death, e.g. by making a will
- distribution of things
- farewell to family and friends
- engaging in risky or reckless behavior
- extreme changes in mood or personality
- leaving society
If a person suspects that someone is in imminent risk of suicide, they should seek emergency help.
If someone believes that a loved one is contemplating suicide but is not in immediate danger, they should contact the person's doctor and seek support from other family members or a support group.