Support for families with mental illness
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.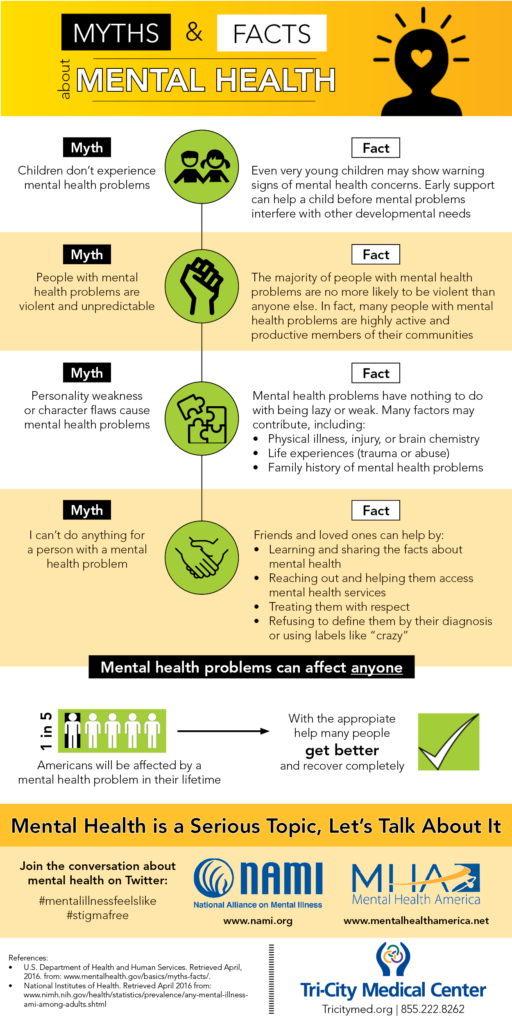
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Recovery and Recovery Support | SAMHSA
Recovery and Resilience
Resilience refers to an individual’s ability to cope with change and adversity. Resilience develops over time and gives an individual the capacity not only to cope with life’s challenges but also to be better prepared for the next stressful situation. Psychological resilience, the ability to cope with adversity and to adapt to stressful life events, varies widely from person to person and depends on environmental as well as personal factors. It refers to positive adaptation, or the ability to maintain mental and physical health despite participating in stressful situations. Resilience is playing up those protective factors so they can outweigh the risk factors. Optimism and the ability to remain hopeful are essential to resilience and the process of recovery.
Because recovery is a highly individualized process, recovery services and supports must be age appropriate and offered over the life course and flexible enough to ensure cultural relevancy. What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
Recovery and Relationships
The process of recovery is supported through relationships and social networks. This often involves family members who become the champions of their loved one’s recovery. They provide essential support to their family member’s journey of recovery and similarly experience the moments of positive healing as well as the difficult challenges. Families of people in recovery may experience adversities in their social, occupational, and financial lives, as well as in their overall quality of family life.
These experiences can lead to increased family stress, guilt, shame, anger, fear, anxiety, loss, grief, and isolation. The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
Peer support assists individuals to engage or stay connected to the recovery process through a shared understanding, respect, and mutual empowerment. Peer support extends beyond the reach of clinical treatment into the everyday environment providing non-clinical, strengths-based support. This relationship can help lay the foundation for SAMHSA’s four dimensions of recovery.
Recovery Support
SAMHSA advanced recovery support systems to promote partnering with people in recovery from mental and substance use disorders and their family members to guide the behavioral health system and promote individual, program, and system-level approaches that foster health and resilience; increase housing to support recovery; reduce barriers to employment, education, and other life goals; and secure necessary social supports in their chosen community.
Recovery support is provided in various settings. Recovery support services help people enter into and navigate systems of care, remove barriers to recovery, stay engaged in the recovery process, and live full lives in communities of their choice.
Recovery support services include culturally and linguistically appropriate services that assist individuals and families working toward recovery from mental and/or substance use problems. They incorporate a full range of social, legal, and other services (PDF | 409 KB). that facilitate recovery, wellness, and linkage to and coordination among service providers, and other supports shown to improve quality of life for people (and their families) in and seeking recovery.
Recovery support services may be provided before, during, or after clinical treatment, or may be provided to individuals who are not in treatment but seek support services.
These services, provided by professionals and peers, are delivered through a variety of community and faith-based groups, treatment providers, schools, and other specialized services. The broad range of service delivery options ensures the life experiences of all people are valued and represented.
The broad range of service delivery options ensures the life experiences of all people are valued and represented.
For example, in the United States there are 34 recovery high schools that help reduce the risk in high school environments for youth with substance use disorders. These schools typically have high retention rates and low rates of students returning to substance use.
Additionally, SAMHSA's Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS) advances effective recovery supports and services for people with mental or substance use disorders and their families.
Find more Publications and Resources on Recovery and Recovery Support.
Information for families with mentally ill people
We, psychiatrists, often ask relatives of people with "our" illnesses what they most often lack in their situation. Often I hear answers: “Information”, “Understanding”.
The family has always existed in the social environment that every person needs, whether he is healthy or ill (even with a mental disorder). At the same time, he often falls out of it. And every individual (healthy or sick) in this environment has rights and obligations. The sick person has a special claim to help and a precautionary attitude, like other members of his family, who also have the same, but they cannot be left unattended for a long time, unless he (the sick person) does not want to risk the breakdown of family ties. In such a special situation, help from outside is required, and then we will talk about overcoming crises, about treatment, about rehabilitation, about the social security of the patient, or about the financial and moral hardships of relatives.
At the same time, he often falls out of it. And every individual (healthy or sick) in this environment has rights and obligations. The sick person has a special claim to help and a precautionary attitude, like other members of his family, who also have the same, but they cannot be left unattended for a long time, unless he (the sick person) does not want to risk the breakdown of family ties. In such a special situation, help from outside is required, and then we will talk about overcoming crises, about treatment, about rehabilitation, about the social security of the patient, or about the financial and moral hardships of relatives.
The common notion that "a person, once mentally ill, remains ill forever" is erroneous. It often happens that the disease disappears again, or at least it can be successfully overcome.
It is also encouraging that in recent decades significant progress has been made in the research and treatment of mental illness, thanks to the emergence of new drugs.
Erroneous sentences include the idea that patients with mental (mental) disorders should be equated with "mentally retarded persons" and during fascism they were exterminated by the thousands. This is also completely false. As one look at the many mentally ill and yet talented people who have made outstanding contributions to art and achieved success in other fields shows: Fyodor Dostoevsky, Hans Christian Andersen, Franz Schubert, Alfred Schnittke, Salvador Dali, Leonardo da Vinci, Nicolo Paganini, Johann Sebastian Bach, Sigmund Freud, Rudolf Diesel, Johann Wolfgang Goethe, Claude Henri Saint-Simon, Immanuel Kant, Charles Dickens, Albrecht Dürer, Sergei Rachmaninoff, Wolfgang Amadeus Mozart, Lope de Vega, Nostradamus, Jean Baptiste Molière, Francisco Goya, Honore de Balzac, Friedrich Nietzsche and others
Today, the concept of "mentally ill" is no longer used, but it is said about "mental illness" and "mentally ill" in order to clarify the change of views, knowledge. Despite the existing, fortunately, positive processes, a relatively high percentage of patients suffer from relapses or remain impaired for a long time. This means that the lives of families where there are such people proceed differently than expected, and plans and desires remain in the background, and all participants must go through painful processes of adaptation, learning, until eventually, perhaps, balance is restored.
This means that the lives of families where there are such people proceed differently than expected, and plans and desires remain in the background, and all participants must go through painful processes of adaptation, learning, until eventually, perhaps, balance is restored.
This is based on the experience of families with such relatives. Well, if you are a relative only recently and have come into conflict with a mental illness, then you will probably find these descriptions depressing. However, perhaps in this you will gain your own experience, and your suffering will be justified.
We, the specialists, would like to give information and evoke understanding without delusion, and point out the possibilities for assistance that you can seek without hiding problems - sometimes out of shame, more often out of good will, in order to somehow spare the patient or cause greater understanding from the outside world. The flip side of this behavior is that problems and ailments are underestimated and not taken seriously - "it's just the psyche . ..", as many say and at the same time believe: this is not so bad and if you pull yourself together, everything will work out . The consequences of such views can be completely unforeseen and are the basis for insufficient assistance, which families usually complain about.
..", as many say and at the same time believe: this is not so bad and if you pull yourself together, everything will work out . The consequences of such views can be completely unforeseen and are the basis for insufficient assistance, which families usually complain about.
It is appropriate to talk about the conflicting feelings of relatives towards the mentally ill. On the one hand, they treat him with understanding and want to protect him, and on the other hand, irritation and dissatisfaction may appear if, as a result of the patient’s behavior, all family life goes haphazardly, although it is known that one must always restrain oneself in illness. Some relatives take the side of the patient and oppose the "rest of the world", others act quite the opposite: they get so upset and nervous that they contribute to the isolation of the sick person, while others hesitate between understanding and sympathy, on the one hand, and refusal, and anger , on the other hand.
Patients themselves, doctors, support staff participate in this game, and the "stumbling block" adjoins either one or the other. Everything in this complex and constantly changing situation is understandable, but this certainly does not make it easier for a solution that is acceptable to all participants.
Everything in this complex and constantly changing situation is understandable, but this certainly does not make it easier for a solution that is acceptable to all participants.
The motto of the German Relatives Association brings this goal together in the thesis: "In order to live together with the mentally ill, it is necessary to be self-confident and in solidarity." However, there is an experience acquired by many relatives before you: “Your most important assistant is yourself!”. Therefore, it is so important that you take care not only of the patient, but also of yourself.
The first step in self-help is gathering information. The one who receives more information about the disease can better manage it and overcome its consequences. Relatives can turn to doctors, read specialized literature, etc. However, when it comes to the numerous and dubious issues that arise in daily communication with the mentally ill, the "expert assessment" of other relatives is an indispensable source of help and Information.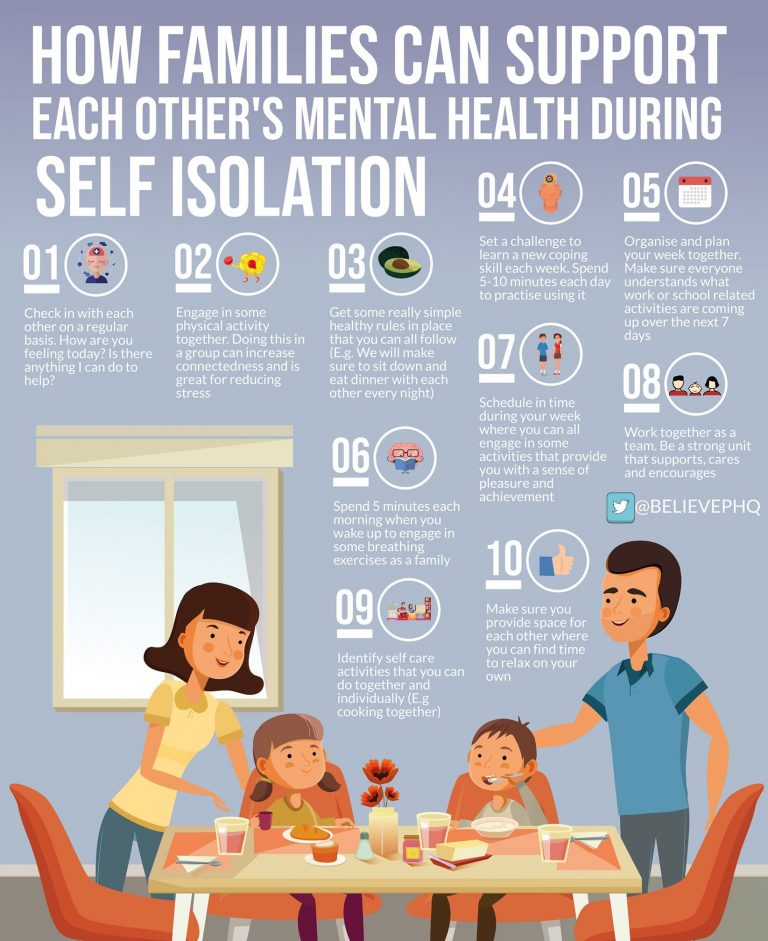
All of the above can be summarized in ten basic rules, such a "game" is worth the candle. Thanks to her, we can all avoid stress and conflict in the family and ensure peace in our relationships with each other.
So, 10 basic rules to avoid stress and conflict in the family and ensure peace in relationships with each other:
1. Try to limit yourself to the most important things and at first close your eyes to some behavioral problems.
2. Leave the patient alone - excessive care will not benefit him or us. Do not protect him or take care of him beyond measure and give him as much independence as possible. However, it is important to let him know that you are at his disposal at any moment when he needs you.
3. Give yourself and the patient time, especially after the acute phase of the illness. Don't wait impatiently for a "quick leap forward" but promote small steps and enjoy them.
4. Match your expectations and aspirations to the situation, avoid overstimulation and do not make excessive demands.
5. If you want to do something (for example, tidy up your room), first think about how to act more delicately and wait for the most favorable moment. Express your thoughts clearly and concisely. If you act with irritation or direct pressure, then the chances of achieving the intended goal decrease, and we create additional stress for ourselves.
6. Consider that the symptoms of illness are not an expression of ill will, but an attempt to cope with a disturbed lifestyle.
7. Reflect on the fact that the sick person himself is trying to protect the still healthy parts of his body from the disease and help him strengthen and develop them.
8. Take care of a quiet way of life - even if it is sometimes difficult. Work hard to minimize conflicts and strained relationships in the family. Ask yourself if a walk in the fresh air will help you get out of a difficult situation or if you need to give free rein to your own feelings.
9. Take a well-thought-out attitude towards medicines. In many cases they are necessary and can help, partly at long intervals. In principle, taking medication is the business of the patient and his doctor. If necessary, we can point the patient to medications, but should avoid feeling full responsibility for taking them or putting pressure on them.
In many cases they are necessary and can help, partly at long intervals. In principle, taking medication is the business of the patient and his doctor. If necessary, we can point the patient to medications, but should avoid feeling full responsibility for taking them or putting pressure on them.
10. And finally: take good care of yourself! Carefully save your strength, maintain contacts and engage in hobbies, as well as allow yourself some benefits - this is very important!
Kachurin Artem Aleksandrovich,
doctor psychiatrist, psychiatrist-narcologist of the highest qualification category, chief freelance psychiatrist of SURDZ
,twitter,vkontakte,gplus">
Help for a loved one with a mental disorder
Basic concepts
There is a lot of talk these days about the rise in the number of mental disorders in society, but many people have very vague ideas about this very vague concept. Despite the fact that now psychiatrists are doing everything possible to inform the population as best as possible about stress, depression, anxiety, neuroses, more severe mental disorders, there is very little literature written by experts for the average layman, and on the Internet there is an abundance of information written either difficult language, or simply illiterate. All this ultimately leads to the fact that such information is not only contrary to reality, but also harmful.
Despite the fact that now psychiatrists are doing everything possible to inform the population as best as possible about stress, depression, anxiety, neuroses, more severe mental disorders, there is very little literature written by experts for the average layman, and on the Internet there is an abundance of information written either difficult language, or simply illiterate. All this ultimately leads to the fact that such information is not only contrary to reality, but also harmful.
It is impossible to sort everything out in one article and give clear instructions on the relationship between the patient and his relatives, but it is possible to bring to a holistic picture the idea of this complex group of diseases (the terms "disease" and "disorder" from a medical point of view are largely close, but not identical*). Therefore, my task is to acquaint the reader with this complex problem, primarily related to relationships and assistance to those suffering from severe mental illnesses.
* It is desirable to know the most basic terms, then it will be easier for the doctor to help both the patient himself and his relatives. In addition, you should not use terms that are not well known to you, it is better to describe the situation or condition as you understand it.
So, mental (or mental, because psyche - translated from Greek means soul ) disorders - are painful conditions of a person with psychopathological (i.e., with mental disorders) and behavioral (i.e., they do not always appear, for example, in case of neurosis, when a person, by an effort of will, keeps himself within the cultural society up to a certain point) manifestations due to the influence of biological, psychological, social and other factors.
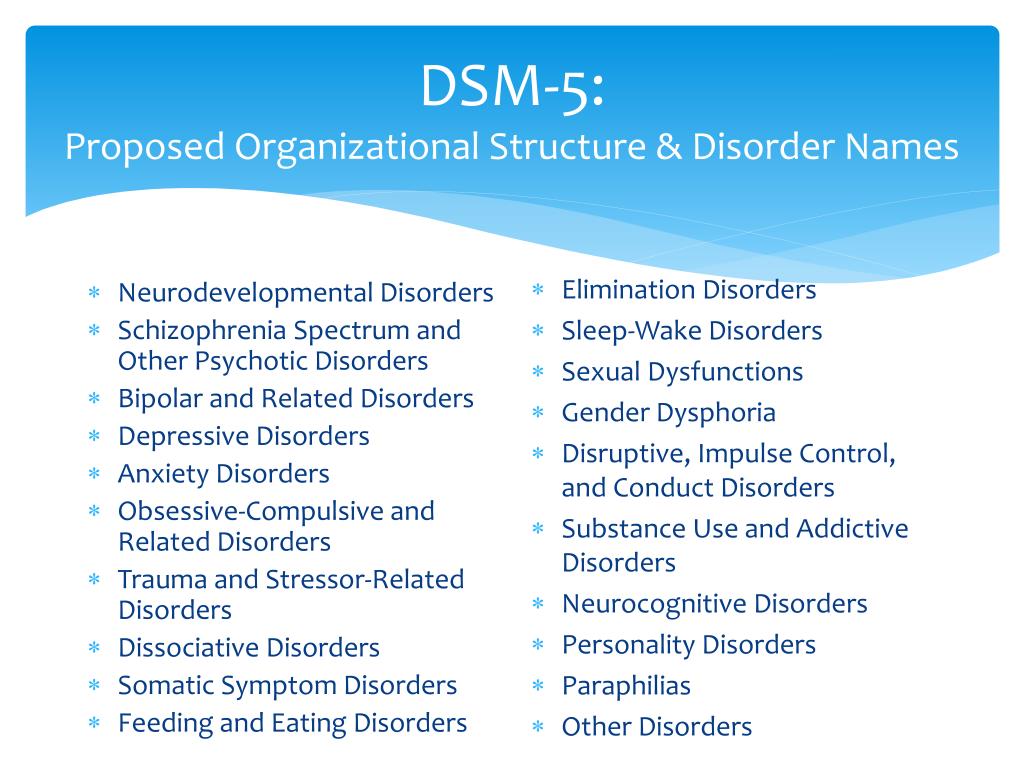
Let's not confuse with psychosis (or psychotic) disorders, which are characterized by gross and contradictory environmental disorders of thinking, perception and behavior (delusions, in a medical, not philistine view; hallucinations; psychomotor agitation; suicidal behavior, etc. ).
).
It is important to note that the problem of mental disorders is interdisciplinary and even interdepartmental, social. Rehabilitation is needed, not just treatment.
As for the diagnosis. Diagnosis - definition and recognition, an indication of the disease. In medicine, and especially in psychiatry, diagnosis does not always mean treatment in strict accordance with the diagnosis. Diagnosis is often a statistical category needed to understand, roughly speaking, how the condition of one patient is similar to another.
I am sometimes puzzled by the desire of a person to look at the records of a doctor. After all, a special interpretation, justification of the diagnosis, terminology can not only frighten and offend an unprepared person, but cause unreasonable distrust of a specialist and, even worse, aggravate disturbed mental balance, upset not only the patient, but also relatives.
It is much more important to trust each other (the doctor, the patient, his relatives), to ask questions of interest. It is on trust that the desired result is achieved - a cure or a stable remission, if the disorder is chronic.
It is on trust that the desired result is achieved - a cure or a stable remission, if the disorder is chronic.
I will not decipher concepts and terms much in this article. Let's talk about the topic corresponding to the title. We will talk about such diseases as schizophrenia, dementia, severe depression, drug addiction (alcoholism, drug addiction), etc. I will try to give basic, a kind of "universal" recommendations.
Recommendations
1 situation: a relative (both a 16-year-old child and an old grandfather, a researcher in the past or present) became “somehow not like that”, began to withdraw, get annoyed for no apparent reason, although “he had never been aggressive before ', to talk, to talk to oneself.
Usually, such behavior is first perceived as a joke, then surprise, then a discussion with a sick person begins, which can lead to serious conflicts and distrust. If you suspect that a person close to you has a mental disorder (we do not take emergency situations, for example, in case of severe aggression, the police and medical workers are already intervening here), you cannot argue.
It is also desirable not to support the painful delusions of a person, to try to be patient and caring, to persuade a loved one to seek medical help. Unfortunately, in our society, when it comes to psychiatry, in most cases it causes a smile, fear, surprise, but not sympathy and a desire to help a sick person, especially if it refers to a relative. Only later, when a sick person can feel and even understand that the help of a psychiatrist is for his benefit, will he himself reach out to her.
At the initial stage, it is worth trying to persuade a person to calm down, assess his degree of adequacy (if he used to trust you, but now he doesn’t groundlessly, whether he understands you or is completely in his experiences, etc.), to understand whether there are threats to him and surrounding.
It is impossible to forcibly help a person (involuntary hospitalization in a psychiatric hospital is carried out only by a court decision), but everything possible must be done: to involve relatives who will correctly understand and support people who are authoritative for the patient, consult a doctor.
Situation 2: patients were brought to a psychiatrist. There can be 2 ways here. The doctor will help to understand the situation, make a diagnosis, prescribe treatment, give recommendations. Everything here is very individual. But it may also be that the doctor gives a recommendation, but not only the patient (due to inadequacy), but also a relative does not want to follow it.
I can give an example. A mother brings her 20-year-old daughter to a psychotherapist. The daughter has painful sensations in her body: the bones, according to her, “go back and forth, fall through and hurt.” All specialists were examined, all studies were carried out, including MRI, no diseases were found, the symptoms do not correspond to the alleged physical pathology.
A mental illness was diagnosed, drugs were prescribed, and after a couple of months there was a significant improvement. The patient stops taking the medicine, after a while she comes to the doctor with her mother, complains about the deterioration, assures that the medicines do not help, refuses help, runs out of the office, rushes about, says that she does not want to live. Hospitalization is proposed, since adequate dosages of drugs can only be prescribed in a hospital, in response - a categorical refusal.
Hospitalization is proposed, since adequate dosages of drugs can only be prescribed in a hospital, in response - a categorical refusal.
With difficulty he manages to calm down, persuade him to give an injection, agrees to resume taking medications. The doctor suggests that the mother call a psychiatric team to resolve the issue of hospitalization, in connection with the suicidal risk, to which he receives the answer: “Well, she will kill herself, then this is her fate, I will not put her in a psychiatric hospital.” On receipt released home. The mother calls the next day, the daughter gets a little better, then disappears for six months. Another call to the doctor's personal phone: the daughter lies in bed, does not want to get up, complains about "movements in the body of some creatures" that cause severe pain.
Recommendations were given, the patient was finally hospitalized in a psychiatric hospital with schizophrenia. She was discharged with improvement, criticism of her condition appeared, adequate therapy was selected.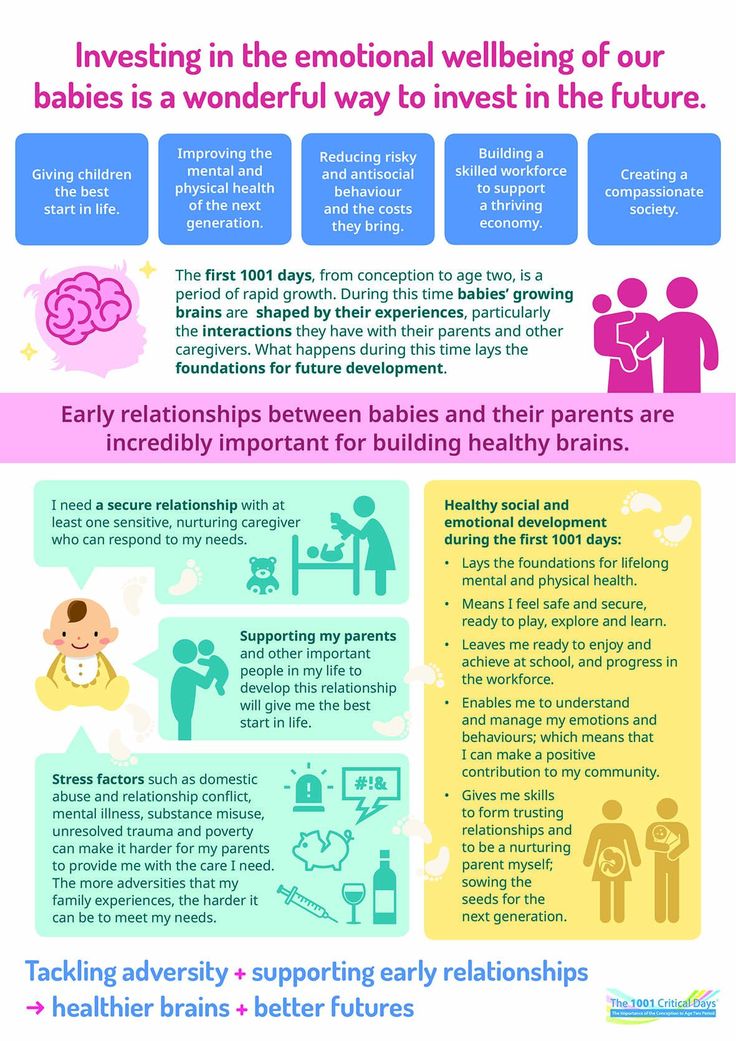
Bottom line: fortunately, this story ended happily, but the patient suffered for several months, while the mother believed in the need for hospitalization; I had to prescribe heavier drugs, the treatment was delayed.
There is nothing wrong if the patient refuses this doctor (for example, the patient has included the doctor in his delusional system) or the doctor himself understands that he will not be able to provide adequate assistance. Then it is necessary to attract colleagues, send them to a hospital, together with relatives, think over options for assistance and choose the best one. It happens that the patient returns after treatment, apologizes for his behavior, because he did not understand the pain and inadequacy at that time.
You should not change specialists (sometimes people come to me with dozens of recommendations from different doctors of the same specialty, which is puzzling). Well, 2-3 opinions is understandable, but more than 10!? The most common reason is that medications do not immediately help, side effects.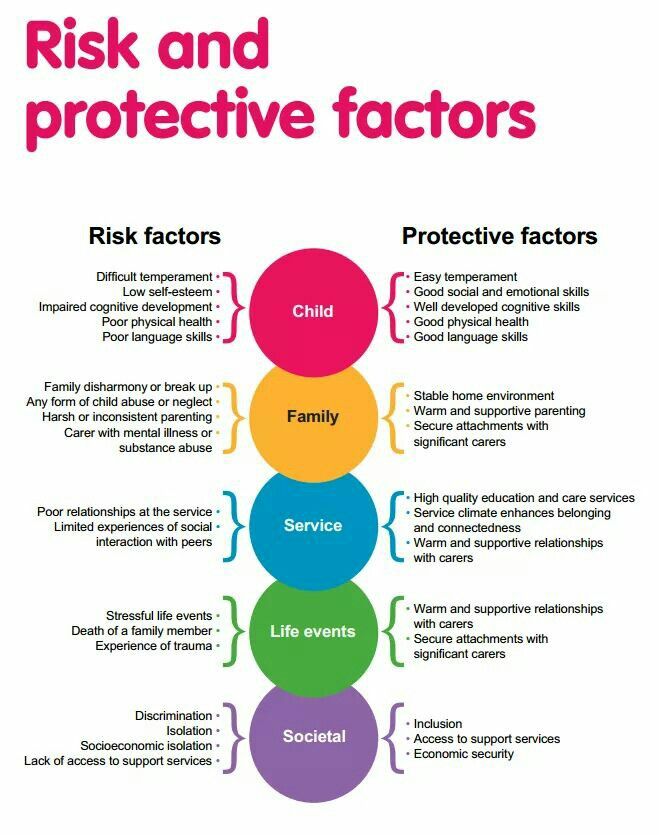
Some patients soon stop taking their medications, and many diseases are chronic and require many months or even years of maintenance therapy. A natural deterioration sets in, the new doctor does not yet know the specifics of the course of the disorder in this patient, experiments with treatment begin, a new selection of medicines begins, resistance to treatment is formed, and previously effective drugs cease to work.
And one more thing: it is desirable, at the initial visit to the doctor, to bring, if not all, then the main examinations, extracts, and tests. A psychiatrist is a doctor like everyone else, and the more information about the patient, the easier it is to understand the diagnosis. For example, if a person has a pathology of the thyroid gland, it is advisable to bring the last tests for hormones, since when the hormonal background changes, the state of mind also changes (irritability, sleep disturbances, mood swings, etc.).
In some cases, antidepressants are not only not needed, but can be harmful, it may be worth limiting yourself to the appointments of an endocrinologist and psychotherapy. Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
3 situation: the patient has been examined for a long time, the diagnosis is known, but the disease is progressing. Relatives begin to "look for a miracle": consult the patient with leading specialists, go to the main scientific centers, someone is looking for help abroad.
I have had a number of cases where patients have returned from the US, Europe, Israel, etc. with complaints that the prescription of drugs selected in Russia was refused, or that the treatment was simply ineffective, worsened. Here I would advise you to find a specialist you trust and coordinate your actions with him. Only together can we help sick people provide adequate assistance and, if not cured, then improve the quality of life as much as possible.
4 situation: terminally ill patient in the final stage.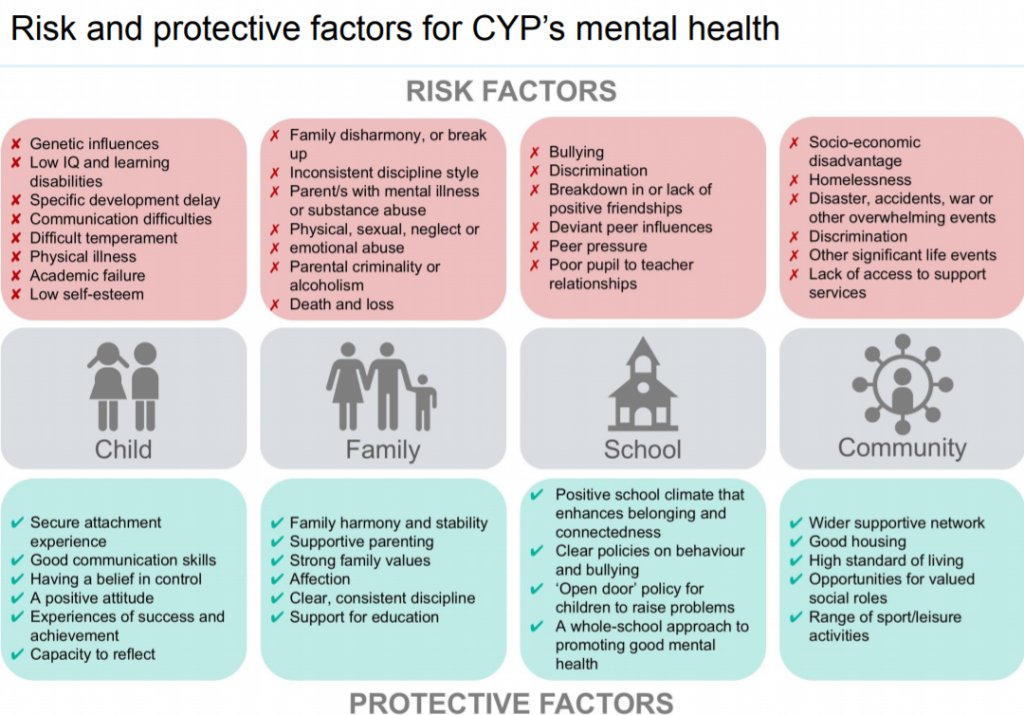 There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case.
There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case.
“If a person cannot be cured, this does not mean that he cannot be helped.”
If you are destined to die, it is easier to do this among loving relatives on your bed, even if a person does not understand anything and does not recognize anyone. But he FEELS the attitude towards him. How a small child feels the caress of his mother, smiles or cries when his mother is gone. You will say - there is no comparison, children are our future, and here is a dying person who does not understand anything. Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ...
Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ...
Nursing staff
Well, a few words about help for those who care for the sick. It is difficult to give specific recommendations here, only one thing is clear: you cannot take the position of either a rescuer or a victim, you just need to fulfill your human duty to the best of your ability and ability. Don't forget yourself.
Any person who lives with a sick person, and even more so caring for him, experiences enormous personal and emotional stress. Therefore, you should think about how you will cope with the disease in the future. By understanding your own emotions properly, you will be able to deal more effectively with both the patient's problems and your own problems. You may have to experience emotions such as grief, shame, anger, embarrassment, loneliness and others.
For some people who care for the sick, the family is the best helper, for others it brings only grief.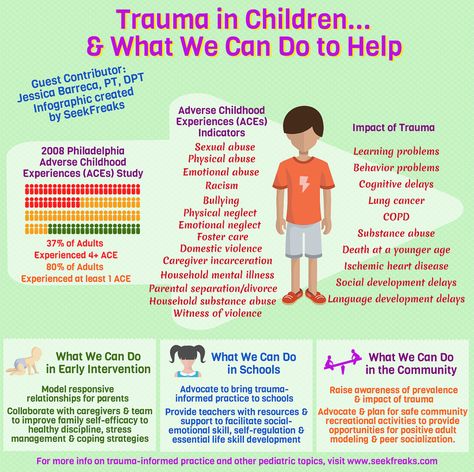 It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
If family members upset you with their unwillingness to help, or criticize your work because of the lack of information about this disorder, you can form a family council to discuss care problems. In particular, make a decision to involve an employee, at least for the period of time necessary for your rest and recuperation, and, if necessary, treatment.
And the last. Don't keep problems to yourself. Feeling that your emotions are a natural reaction in your position, it will be easier for you to cope with your problems. Don't reject the help and support of others, even if you feel like you're making it difficult. Even psychotherapists themselves (seemingly knowing how to minimize stress as much as possible) often have their own psychotherapist, and it is bad for the doctor who neglects the help of his colleagues.