Stuttering sign of intelligence
A Survey on Cognitive Functions of Students With Stuttering
1. Ward D. Stuttering and cluttering: Frameworks for understanding and treatment. Abingdon: Routledge. 2006.
2. Nippold MA. Stuttering and language ability in children: Questioning the connection. American Journal of Speech-Language Pathology. 2012; 21(3):183-96. [DOI:10.1044/1058-0360(2012/11-0078)] [DOI:10.1044/1058-0360(2012/11-0078)]
3. Healey EC. The CALMS: A multidimensional approach to assessing and treatment school-age children who stutter. The Bulletin. 2013; 11(1):1-22.
4. McDowell S, Whyte J, D'Esposito M. Working memory impairments in traumatic brain injury: Evidence from a dual-task paradigm. Neuropsychologia. 1997; 35(10):1341-53. [DOI:10.1016/S0028-3932(97)00082-1] [DOI:10.1016/S0028-3932(97)00082-1]
5. Afrooz Gh, Kamkary K. [Psychometric principles and intelligence: Tehran University Stanford-Binan Intelligence Test (Persian)]. Tehran: University of Tehran Press; 2009.
6. Aminloo S, Kamkary K, Shokrzadeh S. [The concurrent validity of the new version of the Tehran-Stanford-Binet Intelligence Scale with the Wechsler Intelligence Scale for children-revised (Persian)]. Journal of Exceptional Education. 2012; 13(7):50-61.
7. Baddely A. Working memory and language: an overview. Journal of Communication Disorders. 2003; 36(3):189-208. [DOI:10.1016/S0021-9924(03)00019-4] [DOI:10.1016/S0021-9924(03)00019-4]
8. Basi M, Farazi M, Bakhshi E. Evaluation of effects of Gradual Increase Length and Complexity of Utterance (GILCU) treatment method on the reduction of dysfluency in school-aged children with stuttering. Iranian Rehabilitation Journal. 2016; 14(1):59-62 [DOI:10.15412/J.IRJ.08140109] [DOI:10.15412/J.IRJ.08140109]
9. Saifpanahi S, Sobhani Rad D, Afzali M, Izanloo S, Mardani N, Gholamian M. [An investigation of the correlation between phonological and visual working memory with severity of stuttering in 6-12 years-old children (Persian)]. Journal of Paramedical Sciences & Rehabilitation. 2015; 4(4):20-6.
2015; 4(4):20-6.
10. Baezzat F, Moradi M, Motaghedifard M. The effect of phonological awareness on the auditory memory in students with spelling problems. Iranian Rehabilitation Journal. 2018; 16(1):83-9. [DOI:10.29252/nrip.irj.16.1.83] [DOI:10.29252/nrip.irj.16.1.83]
11. Oyoun HA, El Dessouky H, Shohdi S, Fawzy A. Assessment of working memory in normal children and children who stutter. Journal of American Science. 2010; 6(11):562-6.
12. Vameghi R, Sajedi F, Yadegari F, Zarifian T, Shahshahanipour S, Hatamizadeh N, et al. Production of a protocol on early intervention for speech and language delays in early childhood: A novice experience in Iran (Persian)]. Archives of Rehabilitation. 2016; 16(4):374-81.
13. Maddah M, AzadFallah P, Salmani M, RasoolZade Tabatabayi K. [Phonological working memory in children with normal non-fluency (Persian)]. Journal of Clinical Psychology. 2011; 3(3):1-6.
14. Vahab M, Shojaei K, Ahmadi A, Nasiri M. [Phonological working memory in 4-8 year-old Persian children who stutter (Persian)]. Journal of Rehabilitation Sciences and Research. 2015; 1(4):92-6.
Journal of Rehabilitation Sciences and Research. 2015; 1(4):92-6.
15. Jones RD, White AJ, Lawson KH, Anderson TJ. Visuoperceptual and visuomotor deficits in developmental stutterers: An exploratory study. Human Movement Science. 2002; 21(5):603-9. [DOI:10.1016/S0167-9457(02)00165-3] [DOI:10.1016/S0167-9457(02)00165-3]
16. Boberg E, Yeudall LT, Schopflocher D, Bo-Lassen P. The effect of an intensive behavioral program on the distribution of EEG alpha power in stutterers during the processing of verbal and visuospatial information. Journal of Fluency Disorders. 1983; 8(3):245-63. [DOI:10.1016/0094-730X(83)90038-4] [DOI:10.1016/0094-730X(83)90038-4]
17. Rahimi SS Farazi M, Darouie A, Bakhshi E, Abdi S, Valinejad V, Tiemori M. [Comparison the quality of life among adults with and without stuttering: An emohasis on the severity of stuttering (Persian)]. Journal of Rehabilitation. 2016; 17(4):300-6. [DOI:10.21859/jrehab-1704300] [DOI:10.21859/jrehab-1704300]
18. Furnham A, Davis S.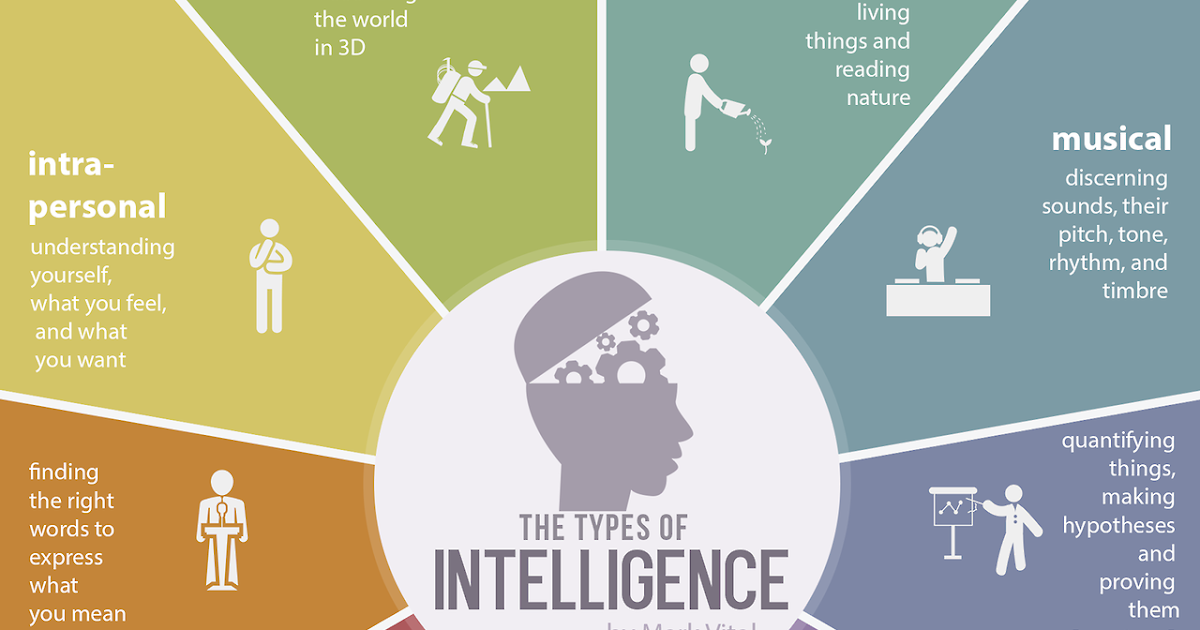 Involvement of social factors in stuttering: A review and assessment of current methodology. Stammering research: An Online Journal Published by the British Stammering Association. 2004; 1(2):112-22. [PMID] [PMCID]
Involvement of social factors in stuttering: A review and assessment of current methodology. Stammering research: An Online Journal Published by the British Stammering Association. 2004; 1(2):112-22. [PMID] [PMCID]
19. Farazi M, Sajedi F. [Speech and language intervention in children with speech disorder (Persian)]. Tehran: University of Social Welfare and Rehabilitation Sciences; 2016.
20. Farazi M, Sajedi F. [Stuttering in children (Persian)]. Speech and Language Pathology. 2014; 1(4):62-9.
21. Farazi M, Gholami Tehrani L, Khodabakhshi Kolaee A, Shemshadi H, Rahgozar M. The effect of a combination of cognitive therapy and speech in stutterers (Persian)]. Thought & Behavior in Clinical Psychology. 2014; 8(30):37-46.
22. St Clare T, Menzies RG, Onslow M, Packman A, Thompson, R, Block, S. Unhelpful thoughts and beliefs linked to social anxiety in stuttering: Development of a measure. International Journal of Language & Communication Disorders. 2009; 44(3):13. [DOI:10.1080/13682820802067529] [PMID] [DOI:10.1080/13682820802067529]
[DOI:10.1080/13682820802067529] [PMID] [DOI:10.1080/13682820802067529]
23. Karrass J, Walden TA, Conture EG, Graham CG, Arnold HS, Hartfield KN, Schwenk KA. Relation of emotional reactivity and regulation to childhood stuttering. Journal of Communication Disorders. 2006; 39(6):402-26. [DOI:10.1016/j.jcomdis.2005.12.004] [PMID] [PMCID] [DOI:10.1016/j.jcomdis.2005.12.004]
24. Watkins RV, Yairi E. Language production abilities of children who stuttering persisted or recovered. Journal of Speech, Language, and Hearing Research. 1997; 40(2):385-99. [DOI:10.1044/jslhr.4002.385] [DOI:10.1044/jslhr.4002.385]
25. Schwenk KA, Conture EG, Walden TA. Reaction to background stimulation of preschool children who do and do not stutter. Journal of Communication Disorders. 2007; 40(2):129-41. [DOI:10.1016/j.jcomdis.2006.06.003] [PMID] [PMCID] [DOI:10.1016/j.jcomdis.2006.06.003]
26. Yadegari F, Salehi A. [Diffevential diagnosis of frimary stuttering and normal nonfluency in children referring to Saba Clinic (Persian)]. Archives of Rehabilitation. 2003; 4(3):45-8.
Archives of Rehabilitation. 2003; 4(3):45-8.
27. Eggers K, De Nil, Vandenberg BR. Inhibitory control in childhood stuttering. Journal of Fluency Disorders. 2007; 38(1):1-13. [DOI:10.1016/j.jfludis.2012.10.001] [PMID] [DOI:10.1016/j.jfludis.2012.10.001] [DOI:10.1016/j.jfludis.2012.10.001]
28. Dhatri SD, Ajith U, Santosh M. Camparison of working memory abilities in adults who do and not stutter. Journal of Indian Speech, Language & Hearing Association. 2017; 31(2):42-7. [DOI:10.4103/jisha.JISHA_5_17] [DOI:10.4103/jisha.JISHA_5_17]
Stuttering: Myth vs. Fact
Stuttering: Myth vs. Fact
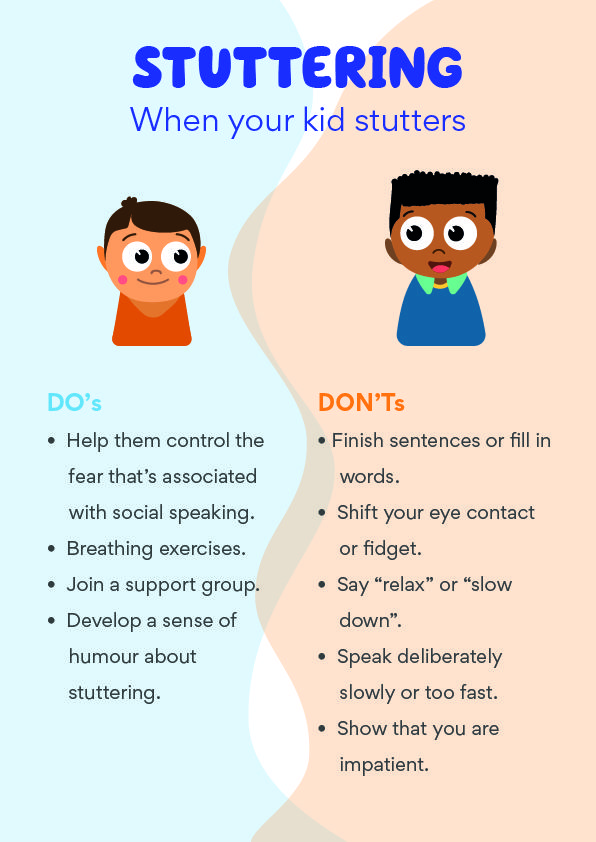
Stuttering specialist Catherine Montgomery had a blind patient who stuttered. Someone once asked him which was more difficult to deal with in life — blindness or stuttering.
“The man thought for a moment,” Montgomery recalls. “Then he replied, ‘Stuttering — because unlike my blindness, people don’t understand that stuttering is beyond my control.’”
“Interesting, isn’t it?” she says. “You’d never think of saying to a blind person, ‘Slow down and you’ll be able see,’ or ‘If you just tried a little harder you could see.’ But most of us think if a stutterer just relaxed and tried a little harder, he could speak fluently. That’s not the case,” says Montgomery, M.S., CCC-SLP, executive director and founder of The American Institute for Stuttering in New York City, N.Y.
“You’d never think of saying to a blind person, ‘Slow down and you’ll be able see,’ or ‘If you just tried a little harder you could see.’ But most of us think if a stutterer just relaxed and tried a little harder, he could speak fluently. That’s not the case,” says Montgomery, M.S., CCC-SLP, executive director and founder of The American Institute for Stuttering in New York City, N.Y.
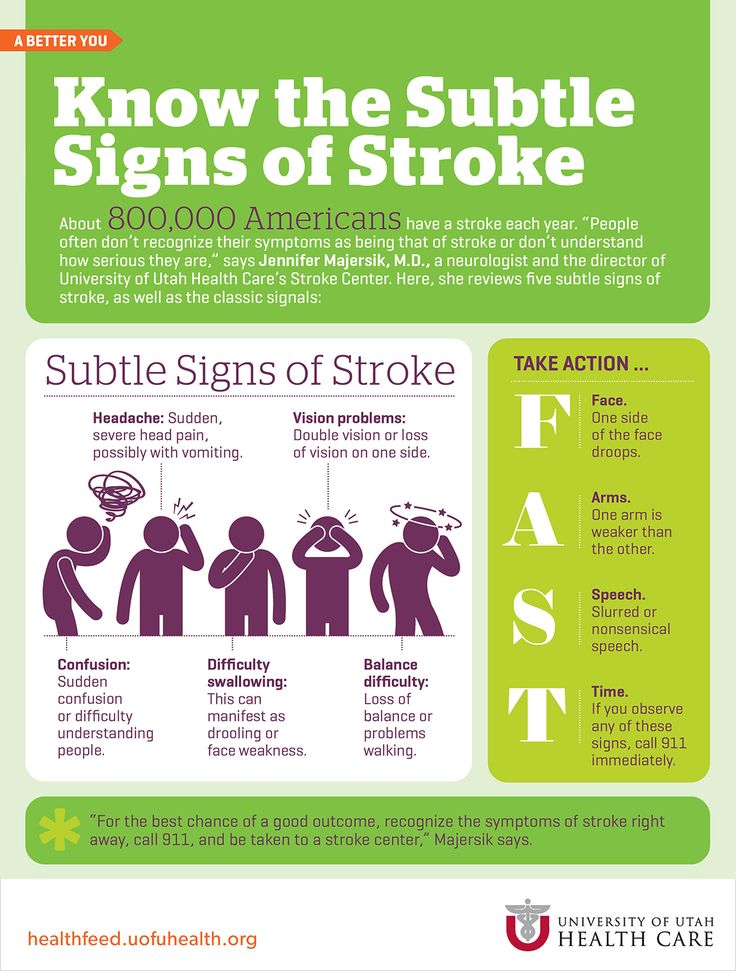
Stuttering is a chronic dysfluency or break in fluent speech. It’s characterized by sound, syllable, word or phrase repetitions; hesitations, fillers (um, ah) and revisions in word choices. It can also include unnatural stretching out of sounds and blocks in which a sound gets stuck and just won’t come out. Stuttering may be accompanied by muscle tension, facial tics and grimaces.
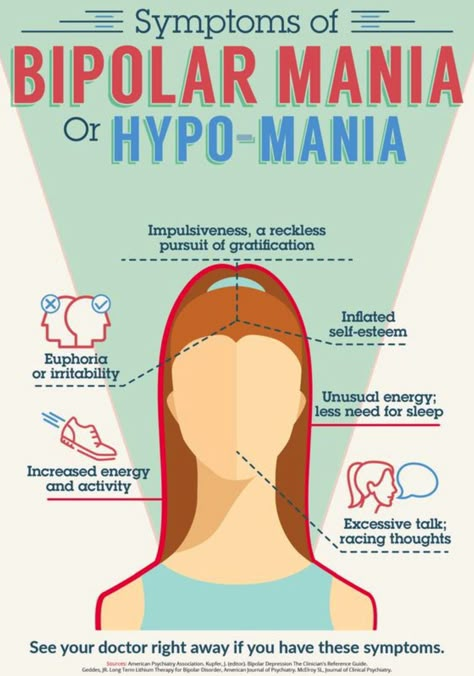
No one really knows for sure exactly what causes it, but researchers believe there’s a neurological basis with a strong genetic component. Currently, the medical community categorizes stuttering as a psychiatric disorder — just like they do schizophrenia and bipolar disorder.
“There are probably multiple factors that can cause stuttering,” says Gerald Maguire, M.D., assistant clinical professor and director of residency training in the department of psychiatry at the University of California at Irvine. “There is a strong genetic component — stuttering does run in families. But it may be a combination of genetics, something neurological and something environmental. Since about 99 percent of all stutterers develop the disorder in childhood — usually before age 9 or 10 — it indicates that something occurs in the developing brain.”
“The idea that stuttering is a brain disorder in the same category as schizophrenia and bipolar disorder is very controversial,” says Maguire, a stutterer. In fact, there has been a push to recategorize stuttering as something other than psychiatric. “Some feel it attaches a stigma to a disorder that’s already very misunderstood by most,” Maguire said.
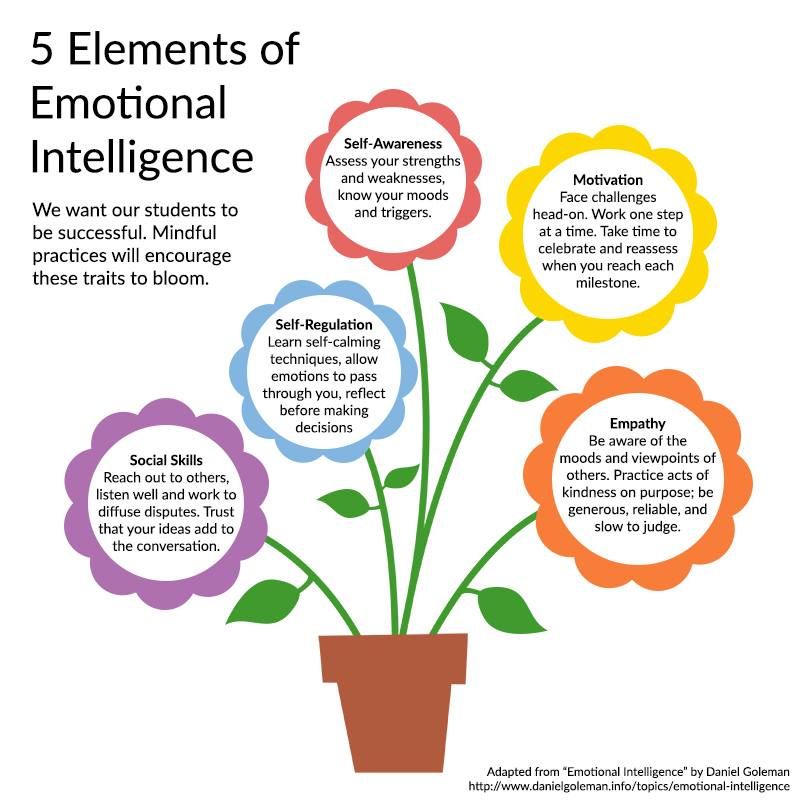
Among the things researchers do know about stuttering is that it’s not caused by emotional or psychological problems. It’s not a sign of low intelligence. The average stutterer’s IQ is 14 points higher than the national average. And it’s not a nervous disorder or a condition caused by stress. “If stress caused stuttering, we’d all be stutterers,” says Montgomery. Stuttering can, however, be made worse by anxiety or stress. And anxiety and stress can be a product of stuttering.
It’s not a sign of low intelligence. The average stutterer’s IQ is 14 points higher than the national average. And it’s not a nervous disorder or a condition caused by stress. “If stress caused stuttering, we’d all be stutterers,” says Montgomery. Stuttering can, however, be made worse by anxiety or stress. And anxiety and stress can be a product of stuttering.
Two Layers to Stuttering
Stuttering really has two layers, says Montgomery.
“There’s the neurological-genetic-environmental layer and then there’s the part that goes on inside your head layer, the conditioned or learned response,” Montgomery said. “For example, on the first day of preschool, Mommy takes little Michael by the hand to meet his teacher. Smiling, the teacher asks Michael, ‘What’s your name?’ And even though he’s never stuttered before, he says, ‘M-M-Michael.’ And he sees a response — maybe the teacher stops smiling for a minute or Mommy tightens her grip on his hand. Consciously or unconsciously, he may think, ‘I have trouble saying my name. ’
’
“So the next time someone asks his name, he has a memory flash of that first time he had trouble saying his name, which sets up a fight or flight response and he stutters over his name,” says Montgomery.
The pattern can continue without intervention. Studies show by age 7 children begin to develop attitudes and feelings about their speech difficulties, and by age 12 speech patterns are set — which makes it difficult to overcome stuttering.
“Lots of kids go through stuttering as a period in their development — and that’s OK for most kids,” says Scott Yaruss, Ph.D., an assistant professor at the University of Pittsburgh, clinical research consultant at Children’s Hospital of Pittsburgh and co-director of the Stuttering Center of Western Pennsylvania.
In fact, researchers say one in four American preschoolers stutter at some point. Only one in 30 in older children, however, actually develop real stuttering problems, according to the U.S. Department of Health and Human Services.
“Most get better — but some get worse,” Yaruss adds. “The problem is, at this time it’s difficult to tell who is stuttering normally in their development and who is at risk for problems. For years, the advice was to do nothing. Ignore it and it’ll probably go away. That’s not true anymore. Today, the best advice is to have your child evaluated by a speech language pathologist who specializes in stuttering.”
Speech language pathologists who are certified by the American Speech-Hearing-Language Association (that’s the equivalent of the American Medical Association for speech pathologists) have the letters CCC-SLP after their name. They mean “Certificate of Clinical Competence — Speech Language Pathologist.”
Most experts agree your child should be evaluated if he begins to demonstrate a physical awareness of his stuttering. Does he become frustrated, distressed or anxious? Does she become tense or tighten her muscles when she has trouble getting the words out?
The second signal is family history. “Not every child of a stutterer will become a stutterer,” says Yaruss. “But since stuttering runs in families, there’s no reason to wait.”
“Not every child of a stutterer will become a stutterer,” says Yaruss. “But since stuttering runs in families, there’s no reason to wait.”
Children don’t learn to stutter from a parent, researchers say. But they may learn the frustration that comes with stuttering from the parent.
Treatment usually varies according to the age of the stutterer, says Yaruss. And different therapies work for different children. A speech language pathologist who specializes in stuttering can match your child with the right therapy.
To treat a very young child, the speech pathologist usually works with the family to help stack the deck in the child’s favor to be as fluent as possible. This may include encouraging parents to create a calm setting for conversation, ensuring that only one person talks at a time and making sure the child doesn’t feel rushed to speak. “As the child approaches age 7, we begin to work more with the child and less with the family,” he says. “We encourage the child to speak more slowly and help shape the child’s speech with specific therapies. ”
”
In adults, the approach may include a three-pronged approach of cognitive-behavioral therapy (to help weaken the connection between stuttering and your reaction to it, and to help change your thinking patterns about what makes you feel badly about stuttering), speech therapy and medication.
At UC Irvine, Maguire is currently conducting clinical trials in adults on a new generation of drugs used to treat schizophrenia and Tourette’s Syndrome. These drugs — risperidone (Risperdal) and olanzapine (Zyprexa) — are dopamine blockers. Dopamine is a neurotransmitter chemical that sends messages from one cell to the next.
Research indicates that stutterers may have dopamine levels that are too high in one area of the brain. The drugs are designed to block the impulses that encourage stuttering. Maguire, who is also a participant in the trials, says the outcomes have been very positive.
But for now, Maguire says, the best bet in beating stuttering is early intervention. “The earlier the therapy occurs, the better the results in resolving stuttering,” he says.
“The earlier the therapy occurs, the better the results in resolving stuttering,” he says.
Yaruss agrees. “The key is to catch the disfluency before it becomes ingrained and the child begins to believe ‘I’m not good at talking.’ But it’s also important to know this: A person who stutters can still do anything in the world that a non-stutterer can,” he adds.
Fast Facts about Stuttering
- Stuttering affects more than 3 million Americans.
- The exact cause of stuttering is still unknown, but researchers believe it is neurologically based with a strong genetic component.
- One in 30 American children stutters. About 75 percent of them will outgrow it.
- Males are four times more likely to stutter than females.
- The average IQ of people who stutter is 14 points higher than the national average.
- Early intervention is critical. Research shows the likelihood of total recovery significantly diminishes as the child grows older.
- Parents should contact a specialist in stuttering treatment if their child shows signs of stuttering as early as age two.
Sources: The U.S. Department of Health and Human Services, The National Stuttering Association and The American Institute for Stuttering.
More Information, Please . . .
In addition to valuable nuts-and-bolts information, many organizations offer resources like referrals to speech language pathologists who specialize in stuttering, and support groups for stutterers and parents of stutterers. Want to learn more? Consider the following Web sites:
- To visit The Stuttering Home Page, sponsored by Minnesota State University in Mankato, log onto http://www.stutteringhomepage.com.
- Log on to the site of The National Stuttering Association at http://www.nsastutter.org.
- The site for The Stuttering Foundation of America can be visited at http://www.stutteringhelp.org.
- Visit the site for The American Institute for Stuttering at http://www.stutteringtreatment.org.
Andrei Aleksandrovich Kiselnikov - user, employee
Moscow State University named after M.
 V. Lomonosov, Faculty of Psychology, Department of Psychophysiology, Senior Researcher, since September 19, 2006
V. Lomonosov, Faculty of Psychology, Department of Psychophysiology, Senior Researcher, since September 19, 2006 Candidate of Psychological Sciences since 2006
Previous jobs (Click to display)
Moscow State University named after M.V. Lomonosov, Faculty of Psychology, Department of Psychophysiology, responsible for the system
Co-authors: Vartanov A.V., Kozlovsky S.A., Glozman Zh.M., Marakshina Yu.A., Buldakova N.S., Sergeev A.A., Kiselnikova N.V., Pyasik M.M., Ushakov V.L., Danina M.M., Vinitsky D.A., Volkova N.V., Shirenova S.D. show full..., Chernorizov A.M., Neklyudova A.K., Slovenko E.D., Kartashov S.I., Mitiureva D.G., Danilova N.N., Zubko V.M., Komarova A.V., Terlichenko E.O., Kabanova P., Komarova A., Mitiureva D.
 , Shcherbakova E., Tan I, Yurlova M., Dolgorukova A.P., Zheymo A.Yu., Karpova N.L., Kovalev A.I., Myasnichenko A.O., Rasskazova E.I., Yurlova M.I., Geguchadze T., Skiteva L., Baev A.A., Bespalov B.I., Zaitsev D.V., Zaitseva N.V., Izmailov Ch.A., Kostanyan D.G., Menshikova G.Ya., Sokolov E.N., Cheburashkin-Antipov D.N., Shaigerova L.A., Shilko R.S., Isakova J., Korotkova A., Nurieva E., Galanina A., Karpova N.L., Korosteleva A., Povorova K.G., Popova A.V., Shevchenko I.A., Skripkina S.M., Tan I, Bezzubik E.G., Vakhantseva O.V., Dolgikh A.G., Zinchenko Yu.P., Lebedev V.V., Nikonova E.Yu., Pastushkova L.M., Pozdnyakov I.S., Sadovnichaya V.S., Beuzeron-Mangina H.
, Shcherbakova E., Tan I, Yurlova M., Dolgorukova A.P., Zheymo A.Yu., Karpova N.L., Kovalev A.I., Myasnichenko A.O., Rasskazova E.I., Yurlova M.I., Geguchadze T., Skiteva L., Baev A.A., Bespalov B.I., Zaitsev D.V., Zaitseva N.V., Izmailov Ch.A., Kostanyan D.G., Menshikova G.Ya., Sokolov E.N., Cheburashkin-Antipov D.N., Shaigerova L.A., Shilko R.S., Isakova J., Korotkova A., Nurieva E., Galanina A., Karpova N.L., Korosteleva A., Povorova K.G., Popova A.V., Shevchenko I.A., Skripkina S.M., Tan I, Bezzubik E.G., Vakhantseva O.V., Dolgikh A.G., Zinchenko Yu.P., Lebedev V.V., Nikonova E.Yu., Pastushkova L.M., Pozdnyakov I.S., Sadovnichaya V.S., Beuzeron-Mangina H. , Bure-Reyes A., Head E., Gorshkova T.A., Irina T., Kiselev S., Mangina C.A., Mikheykin M.E., Popov V.V., Salazar G., Udartseva V.K., Usaeva E.M., Ushakov V.G., Vladimir P., Zhejmo A., Abrosimova V.D., Alymkulov D.E., Asmolov A.G., Barabanshchikova V.V., Berezkina S.Yu., Vaitkyavichus G.G., Varako N.A., Verkholaz D.M., Vinogradova M.G., Vovnenko A.E., Vorobieva A.N., Gadelshina D.F., Garusev A.V., Grechenko T.N., Gromova D.S., Gudkov V.N., Huseynov M.M., Demkina E.I., Dubrovsky V.E., Evtikhin D.V., Ermusheva (Malyutina) A.A., Zimachev M.M., Izmailov Ch.A., Kabanova P.I., Kipiani A.Yu., Kovyazina M.S., Korobkova A.A., Korosteleva A., Krivchenkova E.V.
, Bure-Reyes A., Head E., Gorshkova T.A., Irina T., Kiselev S., Mangina C.A., Mikheykin M.E., Popov V.V., Salazar G., Udartseva V.K., Usaeva E.M., Ushakov V.G., Vladimir P., Zhejmo A., Abrosimova V.D., Alymkulov D.E., Asmolov A.G., Barabanshchikova V.V., Berezkina S.Yu., Vaitkyavichus G.G., Varako N.A., Verkholaz D.M., Vinogradova M.G., Vovnenko A.E., Vorobieva A.N., Gadelshina D.F., Garusev A.V., Grechenko T.N., Gromova D.S., Gudkov V.N., Huseynov M.M., Demkina E.I., Dubrovsky V.E., Evtikhin D.V., Ermusheva (Malyutina) A.A., Zimachev M.M., Izmailov Ch.A., Kabanova P.I., Kipiani A.Yu., Kovyazina M.S., Korobkova A.A., Korosteleva A., Krivchenkova E.V. , Kuzmina Yu.V., Lartseva A.V., Latanov A.V., Makarcheva E.B., Maslenko N.S., Mikhailova O.M., Motovilina N.V., Osin E.N., Pankratova A.A., Panova E.L., Pligina A.M., Pokidko A.B., Polyansky V.B., Rogachev A.O., Sozinova E.V., Stanikounas R.A., Strabykina E.A., Turkovsky A.A., Ushkov F.I., Khludova L.K., Black E.V., Zhang Q., Chudina Yu.A., Churilina E.V., Shatinskas R.V., Shvegzhda A.A., Shekhter E.D.
, Kuzmina Yu.V., Lartseva A.V., Latanov A.V., Makarcheva E.B., Maslenko N.S., Mikhailova O.M., Motovilina N.V., Osin E.N., Pankratova A.A., Panova E.L., Pligina A.M., Pokidko A.B., Polyansky V.B., Rogachev A.O., Sozinova E.V., Stanikounas R.A., Strabykina E.A., Turkovsky A.A., Ushkov F.I., Khludova L.K., Black E.V., Zhang Q., Chudina Yu.A., Churilina E.V., Shatinskas R.V., Shvegzhda A.A., Shekhter E.D. 151 articles, 4 books, 130 conference papers, 38 abstracts, 25 research projects, 18 scientific reports, 17 awards, 1 scientific society membership, 1 internship, 24 program committee memberships, 2 dissertation council memberships, 1 dissertation , 13 theses, 116 term papers, 40 training courses
The number of citations of articles in journals according to the data Web of Science: 36, Scopus: 4
RSCI:
IstinaResearcherID (IRID): 502463
ResearcherID: G-8475-2012
Scopus Author ID: 8387330500
ORCID: 0000-0001-9848-5322
FGBNU NTsPZ.
(86).jpg) ‹‹Pathology of mental development››
‹‹Pathology of mental development›› Psychopathological features of mental retardation, including the intellectual defect itself, are polymorphic both in nature and in severity. However, there are general symptoms that primarily characterize the so-called nuclear mental retardation.
The concept of "nuclear oligophrenia" was introduced in 1938 by N.I. Ozeretsky on the basis of the massiveness of the defect and the characteristics of both intellectual underdevelopment and the patient's personality as a whole. Mental underdevelopment in nuclear oligophrenia has two main features: the developmental disorder is poorly differentiated, more or less uniform, diffuse; evolutionarily youngest, intensively developing systems of the brain are affected. As subsequent studies have shown, with nuclear oligophrenia, even more ancient brain formations can be affected [Isaev D. N., 1982; Marnicheva G. S., Glezerman T. B., 1986].
A typical oligophrenia is always characterized by the totality of mental underdevelopment, which concerns not only intellectual activity, but the entire psyche as a whole, and the insufficiency of higher forms of cognitive activity - abstract thinking - comes to the fore.
In children of the first years of life with a deep mental retardation, the insufficiency of thinking is most of all manifested in the underdevelopment of those functions that reflect the formation of cognitive activity. Prior to this, in early childhood, mental underdevelopment is expressed mainly in the insufficiency of the affective-volitional sphere and motor skills of the child, the distortion and slowing down of the formation of visual and auditory reflexes, the inferiority of the “revitalization complex”, the later manifestation of emotional response to the environment. In the 2nd-3rd year, intellectual insufficiency manifests itself in the peculiarities of behavior and play activity. Children slowly master the skills of self-care, do not differ in liveliness, inquisitiveness, interest in surrounding objects and phenomena that are characteristic of a healthy child. Their games are characterized by simple manipulation, lack of understanding of the elementary requirements of the game, weakness of contacts with children, and less emotionality. Preschool age is characterized by a lack of motivation for intellectual forms of play activity and an increased interest in mobile, non-purposeful games. In the emotional sphere, primitive reactions and insufficient differentiation of higher emotions are noted - manifestations of sympathy, shame, personal attachments. At school age, intellectual disorders are increasingly coming to the fore, which manifest themselves in various areas of activity and behavior of patients, mainly in educational activities.
Preschool age is characterized by a lack of motivation for intellectual forms of play activity and an increased interest in mobile, non-purposeful games. In the emotional sphere, primitive reactions and insufficient differentiation of higher emotions are noted - manifestations of sympathy, shame, personal attachments. At school age, intellectual disorders are increasingly coming to the fore, which manifest themselves in various areas of activity and behavior of patients, mainly in educational activities.
Thus, in children suffering from oligophrenia, as they grow older, the insufficiency of abstract thinking, the weakness of the prerequisites for intelligence, in particular attention, memory, and mental performance, are more and more clearly revealed. But at the same time, sensations and perception are slowly formed [Vygotsky L. S., 1956; Leontiev A.N., 1965; Rubinshtein S. Ya., 1970, etc.]. Insufficiency and slowdown in the development of visual, auditory, kinesthetic and other processes of perception violate the orientation of children in the environment, prevent the establishment in the mind of the patient of complete and adequate connections and relationships between objects of the real world. Insufficiency of perception in oligophrenia is largely due to violations of purposeful voluntary attention; the attention of such children is hardly attracted and fixed, easily dissipated. Children with typical oligophrenia are also characterized by a slowdown and "fragility" of memorization. Particularly affected is logical, mediated memorization, i.e., the highest level of memory, while mechanical memory can be preserved or even hypertrophied developed. Poor understanding of perceived impressions leads to the fact that patients remember only external signs of objects and phenomena and hardly retain memories of internal connections and verbal explanations.
Insufficiency of perception in oligophrenia is largely due to violations of purposeful voluntary attention; the attention of such children is hardly attracted and fixed, easily dissipated. Children with typical oligophrenia are also characterized by a slowdown and "fragility" of memorization. Particularly affected is logical, mediated memorization, i.e., the highest level of memory, while mechanical memory can be preserved or even hypertrophied developed. Poor understanding of perceived impressions leads to the fact that patients remember only external signs of objects and phenomena and hardly retain memories of internal connections and verbal explanations.
A special place in the structure of mental underdevelopment is occupied by speech disorders, which in most cases reflect the depth of mental retardation: in the most severe cases, patients not only do not speak, but also do not understand the speech addressed to them. With a lesser degree of severity of oligophrenia, patients have a limited vocabulary, but do not have sufficient phrasal speech. They use the words they know in the most elementary connection, relating them to specific objects or actions; the generalizing meaning of words is almost inaccessible to them. Even in patients with a mild degree of oligophrenia, who have a sufficient vocabulary, the semantic side of speech is noticeably impaired. Verbal definitions that are not related to a specific, familiar situation are assimilated with great difficulty and very slowly. The grammatical structure of speech is also slowly formed. Since active speech suffers especially with a limited vocabulary, even with a shallow mental retardation, the speech of patients is usually inexpressive, monosyllabic, speech stamps, short, often agrammatically constructed phrases predominate in it. Characterized by incorrect semantic use of words. There may also be defects such as tongue-tied tongue, dysarthria, etc. In cases of oligophrenia complicated by residual effects of organic brain damage, there are focal speech disorders such as motor and sensory alalia, pseudobulbar dysarthria, etc.
They use the words they know in the most elementary connection, relating them to specific objects or actions; the generalizing meaning of words is almost inaccessible to them. Even in patients with a mild degree of oligophrenia, who have a sufficient vocabulary, the semantic side of speech is noticeably impaired. Verbal definitions that are not related to a specific, familiar situation are assimilated with great difficulty and very slowly. The grammatical structure of speech is also slowly formed. Since active speech suffers especially with a limited vocabulary, even with a shallow mental retardation, the speech of patients is usually inexpressive, monosyllabic, speech stamps, short, often agrammatically constructed phrases predominate in it. Characterized by incorrect semantic use of words. There may also be defects such as tongue-tied tongue, dysarthria, etc. In cases of oligophrenia complicated by residual effects of organic brain damage, there are focal speech disorders such as motor and sensory alalia, pseudobulbar dysarthria, etc. Even with a relatively well-developed in the history of speech in patients with oligophrenia, it is usually possible to establish a significant delay in the timing of its development (understanding, pronunciation of individual words, phrasal speech, etc.).
Changes in the emotional-volitional sphere in oligophrenia are quite characteristic. While elementary emotions may be relatively intact, higher emotions, primarily moral ones, turn out to be underdeveloped and insufficiently differentiated. Mostly direct experiences prevail, emotions arising from a specific situation and activity that are relevant only at the moment. The degree of emotional underdevelopment in nuclear oligophrenia is in accordance with the depth of the intellectual defect and the insufficiency of other components of mental activity and personality. Volitional activity of patients is characterized by weakness of motives and initiative, insufficient independence.
The actions of oligophrenic children are characterized by a lack of purposefulness, impulsiveness (without any struggle of motives) and negativism. They are also distinguished by increased imitation, suggestibility and lack of independence of behavior, they are dependent on drives and affects, as well as on the situation and circumstances.
The formation of the personality of mentally retarded children is determined not only by the degree of intellectual underdevelopment and age, but also by the conditions of upbringing, training, and other factors. The level of adaptation of patients with oligophrenia varies depending on the depth of the defect. With mild mental retardation, patients are well versed in familiar everyday situations and they have a relative preservation of practical orientation. E.Kraepelin (19)23) wrote on this occasion that a characteristic feature of oligophrenics is "the ability to navigate much better in simple circumstances than one would expect, judging by the scarcity of the stock of ideas and the weakness of judgment." According to the definition of E. Kraepelin, "an oligophrenic can, undoubtedly, more than he knows. "
Among the most frequent and constant manifestations of oligophrenia are also signs of underdevelopment in the motor sphere. The underdevelopment of psychomotor is manifested primarily in the delay and slowdown in the rate of development of locomotor functions, in the unproductiveness and insufficient expediency of successive movements, in motor restlessness and fussiness. The movements of children are poor, angular and not smooth enough. The lack of development of the motor sphere is especially manifested in subtle and precise movements, gestures and facial expressions.
Such, in general terms, is the psychopathological structure of underdevelopment in typical oligophrenia.
But the structure of mental underdevelopment can be uneven and not exhausted by the symptoms characteristic of typical oligophrenia. In this regard, atypical and complicated variants of oligophrenia are distinguished [Mnukhin S. S., 1958; Sukhareva G. E., 1965; Pevzner M. S., 1969]. Atypical forms include cases of oligophrenia with an uneven structure of a mental defect, manifested in the unilateral development of any mental function or in signs of partial mental underdevelopment.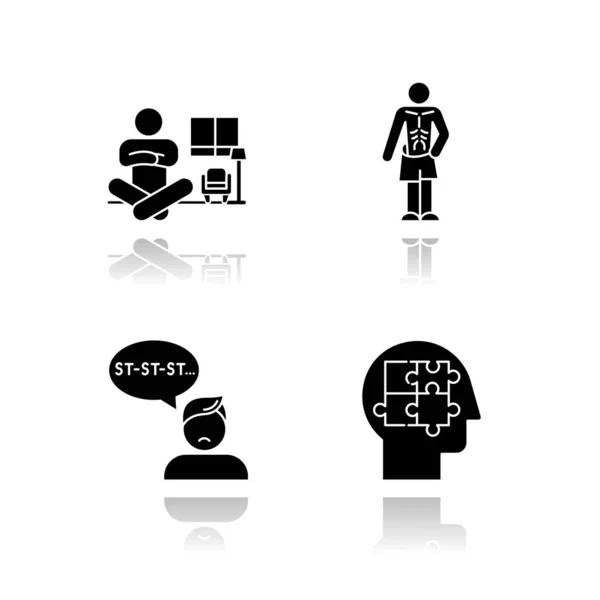
Diagnosis of mental retardation is not limited to assessing the degree of mental underdevelopment. Somatic examination occupies an important place in the diagnostic process.
Some mentally retarded children have an abnormal appearance. This external abnormality is due not only to the dysplasticity of the structure of the face and body, which is often observed in mentally retarded children, but also to the presence of severe neurological disorders, secondary deformities of the skull (with organic brain damage), hypomia, etc. The degree of change in the appearance of patients is associated with the depth of intellectual defect and the nature of brain pathology. With mild intellectual underdevelopment, patients may have a normal appearance. But it should be borne in mind that even with a deep intellectual defect, patients may not have gross anomalies in addition. They are sometimes quite harmoniously built and even pretty. But in most cases, the study of the somatic characteristics of a mentally retarded patient makes it possible not only to diagnose some nosological forms of intellectual underdevelopment, but also to assess the timing of brain damage. Somatic examination reveals congenital malformations and so-called minor anomalies, which are very common in patients with mental retardation, which indicates the intrauterine nature of the lesion. These anomalies are the result of incomplete, less often distorted morphogenesis (some of them may also be an expression of the normal variability of one or another morphological trait). Their number and diversity are so great that it is not possible to compile a list of them, especially since such anomalies are found not only during an external examination of the child, but also during additional examinations - when examined by an ophthalmologist, with x-rays of the skull, spine, limbs.
Somatic examination reveals congenital malformations and so-called minor anomalies, which are very common in patients with mental retardation, which indicates the intrauterine nature of the lesion. These anomalies are the result of incomplete, less often distorted morphogenesis (some of them may also be an expression of the normal variability of one or another morphological trait). Their number and diversity are so great that it is not possible to compile a list of them, especially since such anomalies are found not only during an external examination of the child, but also during additional examinations - when examined by an ophthalmologist, with x-rays of the skull, spine, limbs.
The physical development of patients with oligophrenia often lags behind the age norm and often, even in the absence of obvious intrauterine dysplasticity, is characterized by a disproportionate structure of the trunk and limbs, curvature of the spine, signs of cerebro-endocrine insufficiency (obesity, underdevelopment of the genital organs, a violation of the pace and timing of the formation of secondary sexual characteristics ).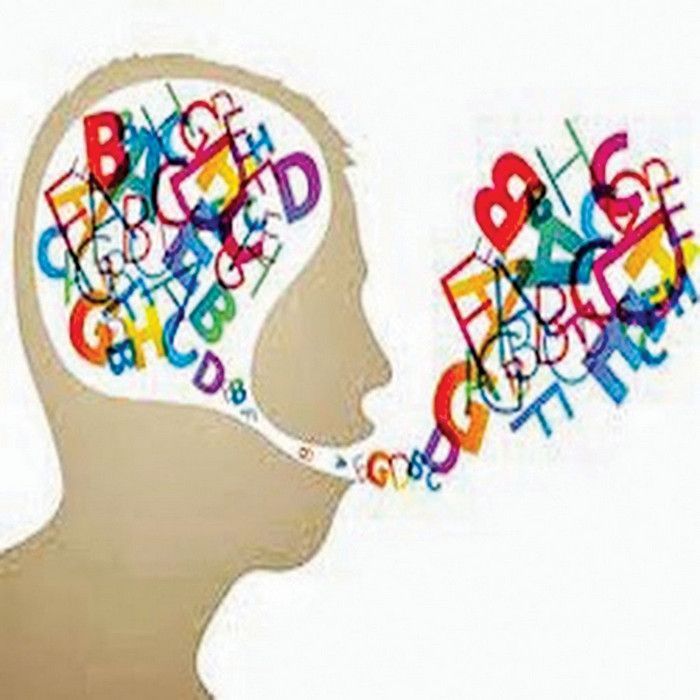 Neurological disorders occupy a particularly large place. It can be not only such gross symptoms as paralysis, paresis, ataxia, hyperkinesis, but also neurological microsymptomatics.
Neurological disorders occupy a particularly large place. It can be not only such gross symptoms as paralysis, paresis, ataxia, hyperkinesis, but also neurological microsymptomatics.
Of great importance in the diagnosis of mental retardation are ophthalmological and radiographic studies (especially X-ray computed tomography). Examination of the eye often reveals symptoms such as chorioretinitis, pigmentary retinal degeneration, cataracts, glaucoma, as well as some microanomalies indicating intrauterine dysgenesis - gliosis of the optic discs, anomalies in the structure of the retinal vessels, etc. In many cases, when examining the eye bottom, the degree of intracranial hypertension and its dynamics are determined. X-ray of the skull is very important for detecting signs of increased intracranial pressure, localization of atrophy of the brain parenchyma and deformations of the cerebrospinal fluid spaces, hidden anomalies in the structure of the skull, especially for the diagnosis of craniostenosis.
Since most cases of mental retardation remain etiologically unclear, for doctors in contact with mentally retarded children, the question is very acute: is it possible to distinguish between hereditary and exogenous forms based on the nature of the clinical features of oligophrenia. Apparently, the answer to this question can be as follows: as long as the patient is not diagnosed with any specific nosologically specific form of damage (as a rule, hereditary, less often exogenous), the etiological diagnosis can only be made presumably, the lesion can be classified as "probably exogenous" or "probably hereditary".
In foreign literature, there are a large number of works aimed at searching for features of the psychological structure of a defect in familial constitutional mental retardation and criteria for its differentiation from exogenously caused organic lesions [Zigler E., 1967; Kirman B., Bichnele J., 1975; Casper! E., 1977]. We are talking about identifying the features of cognitive activity, the level of motivation, etc. Some interesting findings, however, did not contribute to the development of clear diagnostic criteria.
Some interesting findings, however, did not contribute to the development of clear diagnostic criteria.
In domestic psychiatry, the differentiation of family-hereditary oligophrenia from that caused by organic brain damage is based on the clinical picture of mental underdevelopment as a whole, taking into account not only the features of the violation of the structure of cognitive activity, but also all psychopathological and neurological manifestations. But even in this case, the differentiation of these forms is only indicative, often the researcher proceeds from the diagnosis of an organic brain lesion.
Among the most common perinatal hazards that cause organic damage to the central nervous system with impaired mental development are birth trauma and especially neonatal asphyxia. Mechanical birth trauma and asphyxia cause brain damage similar in pathogenesis - circulatory disorders and intracranial hemorrhages, but there are some differences, which depend on which of these two factors was leading [Mastyukova E. M., 1964; Sukhareva G. E., 1965]. If the disease is caused only by asphyxia, the clinical picture is dominated by asthenic manifestations in combination with lethargy, weakness of impulses, slowing down of mental processes, emotional lability, fatigue and exhaustion. With a birth injury, a state of sharp psychomotor agitation, explosiveness, more severe disorders of memory and attention, speech disorders, disinhibition of gross drives, as well as focal neurological symptoms and convulsive seizures are more often observed. In the neurological status, focal symptoms (paresis and paralysis of the cranial nerves, often the phenomena of cerebral palsy, convulsive seizures, etc.) may be noted, the severity of which depends on the severity of brain damage.
M., 1964; Sukhareva G. E., 1965]. If the disease is caused only by asphyxia, the clinical picture is dominated by asthenic manifestations in combination with lethargy, weakness of impulses, slowing down of mental processes, emotional lability, fatigue and exhaustion. With a birth injury, a state of sharp psychomotor agitation, explosiveness, more severe disorders of memory and attention, speech disorders, disinhibition of gross drives, as well as focal neurological symptoms and convulsive seizures are more often observed. In the neurological status, focal symptoms (paresis and paralysis of the cranial nerves, often the phenomena of cerebral palsy, convulsive seizures, etc.) may be noted, the severity of which depends on the severity of brain damage.
Among the postnatal diseases that lead to the development of mental retardation, a large place is occupied by encephalitis, encephalomyelitis, meningoencephalitis (less often meningitis), as well as trauma to the skull, postnatal hypoxia. In post-infectious lesions of the central nervous system, the nature of residual clinical manifestations depends not so much on the characteristics of the etiological factor, but on the reactivity of the nervous tissue, due to individual and age characteristics. A profound intellectual defect is observed more often in children who have had a disease in the first 2 years of life. At this age, due to the immaturity of the protective mechanisms, the process often takes on a diffuse character and is accompanied by extensive damage to the brain tissue. In the genesis of post-infectious and post-traumatic disorders of mental development, the formation of cysts, scars and proliferation of connective tissue, circulation disorders of the cerebrospinal fluid, congestion and, due to circulatory disorders, secondary sclerotic changes in the brain tissue play a role. But the main features of the clinical manifestations of post-infectious and post-traumatic variants of mental retardation are determined primarily by the severity and prevalence of organic brain damage.
In post-infectious lesions of the central nervous system, the nature of residual clinical manifestations depends not so much on the characteristics of the etiological factor, but on the reactivity of the nervous tissue, due to individual and age characteristics. A profound intellectual defect is observed more often in children who have had a disease in the first 2 years of life. At this age, due to the immaturity of the protective mechanisms, the process often takes on a diffuse character and is accompanied by extensive damage to the brain tissue. In the genesis of post-infectious and post-traumatic disorders of mental development, the formation of cysts, scars and proliferation of connective tissue, circulation disorders of the cerebrospinal fluid, congestion and, due to circulatory disorders, secondary sclerotic changes in the brain tissue play a role. But the main features of the clinical manifestations of post-infectious and post-traumatic variants of mental retardation are determined primarily by the severity and prevalence of organic brain damage. In a more remote period, there may be signs of hydrocephalus or microcephaly, other secondary skull deformities, delayed physical development, as well as cerebral and focal symptoms that are very diverse in manifestation and severity. The degree of depth and structure of the intellectual defect in these disorders are extremely diverse. In some cases, the symptoms of underdevelopment, characteristic of typical forms of oligophrenia, predominate, in others, intellectual deficiency is uneven, mosaic in nature, approaching in structure to organic dementia [Ozeretsky N.I., 1938; Yurkova I. A., 1958; Sukhareva G. E., 1965, etc.]. The presence in the structure of the defect of signs of a psychoorganic syndrome, psychopathic behavior and other additional psychopathological symptoms is characteristic. The described lesions are, as a rule, atypical forms of oligophrenia [Pevzner M. S., 1959; Kirichenko E.I., 1965; Sukhareva G. E., 1965, etc.].
In a more remote period, there may be signs of hydrocephalus or microcephaly, other secondary skull deformities, delayed physical development, as well as cerebral and focal symptoms that are very diverse in manifestation and severity. The degree of depth and structure of the intellectual defect in these disorders are extremely diverse. In some cases, the symptoms of underdevelopment, characteristic of typical forms of oligophrenia, predominate, in others, intellectual deficiency is uneven, mosaic in nature, approaching in structure to organic dementia [Ozeretsky N.I., 1938; Yurkova I. A., 1958; Sukhareva G. E., 1965, etc.]. The presence in the structure of the defect of signs of a psychoorganic syndrome, psychopathic behavior and other additional psychopathological symptoms is characteristic. The described lesions are, as a rule, atypical forms of oligophrenia [Pevzner M. S., 1959; Kirichenko E.I., 1965; Sukhareva G. E., 1965, etc.].
It must be emphasized that, in general, the differentiation of forms of intellectual underdevelopment into exogenously conditioned and hereditary-constitutional forms on the basis of only psychopathological features is extremely difficult.![]() In the absence of a pronounced "organic" radical, such differentiation is generally impossible; in particular, the uneven structure of mental underdevelopment is not a criterion for an exogenously caused lesion: the literature describes familial hereditary forms with local cortical disorders [Glezerman T. B., 1983; Lewitter p., 1975].
In the absence of a pronounced "organic" radical, such differentiation is generally impossible; in particular, the uneven structure of mental underdevelopment is not a criterion for an exogenously caused lesion: the literature describes familial hereditary forms with local cortical disorders [Glezerman T. B., 1983; Lewitter p., 1975].
The dynamics of mental retardation is determined by the processes of compensation developing in the central nervous system and the evolution of age-related maturation. The dynamics of oligophrenia as a whole is usually defined as "non-progredient" (according to P. B. Gannushkin, 1933) or "evolutionary" (according to G. E. Sukhareva, 1965). Deviations from this course of the disease can, however, sometimes be observed under the influence of adverse internal and external factors (including factors of education).
Positive evolutionary dynamics in mental retardation can be associated primarily with the natural growth and development of the organism, which leads to an increase in its adaptive capabilities. Naturally, such an improvement is limited by the depth of mental underdevelopment and is less pronounced, the greater the developmental delay: favorable dynamics in idiocy is practically impossible; on the contrary, with debility, the therapeutic and corrective effect can have a great influence on the course of the disease. O. Connor and J. Tizard (1953) found that if such active influences are carried out, then approximately 80% of persons who were diagnosed with debility in childhood, becoming adults, almost did not differ in many respects from people with normal intelligence. Follow-up studies conducted by domestic authors [Portia L.I., 1961; Pevzner M. S., Lubovsky V. I., 1963; Freyerov O. E., 1964; Sukhareva G. E., 1965; Yurkova I.A., 1970] also showed that many students of auxiliary schools, i.e., persons with debility, turned out to be able-bodied by the end of their studies, mastered certain progressions and adapted to life relatively well. According to D. E. Melekhov (1970), 77% of adults with debility are "systematically able-bodied".
Naturally, such an improvement is limited by the depth of mental underdevelopment and is less pronounced, the greater the developmental delay: favorable dynamics in idiocy is practically impossible; on the contrary, with debility, the therapeutic and corrective effect can have a great influence on the course of the disease. O. Connor and J. Tizard (1953) found that if such active influences are carried out, then approximately 80% of persons who were diagnosed with debility in childhood, becoming adults, almost did not differ in many respects from people with normal intelligence. Follow-up studies conducted by domestic authors [Portia L.I., 1961; Pevzner M. S., Lubovsky V. I., 1963; Freyerov O. E., 1964; Sukhareva G. E., 1965; Yurkova I.A., 1970] also showed that many students of auxiliary schools, i.e., persons with debility, turned out to be able-bodied by the end of their studies, mastered certain progressions and adapted to life relatively well. According to D. E. Melekhov (1970), 77% of adults with debility are "systematically able-bodied".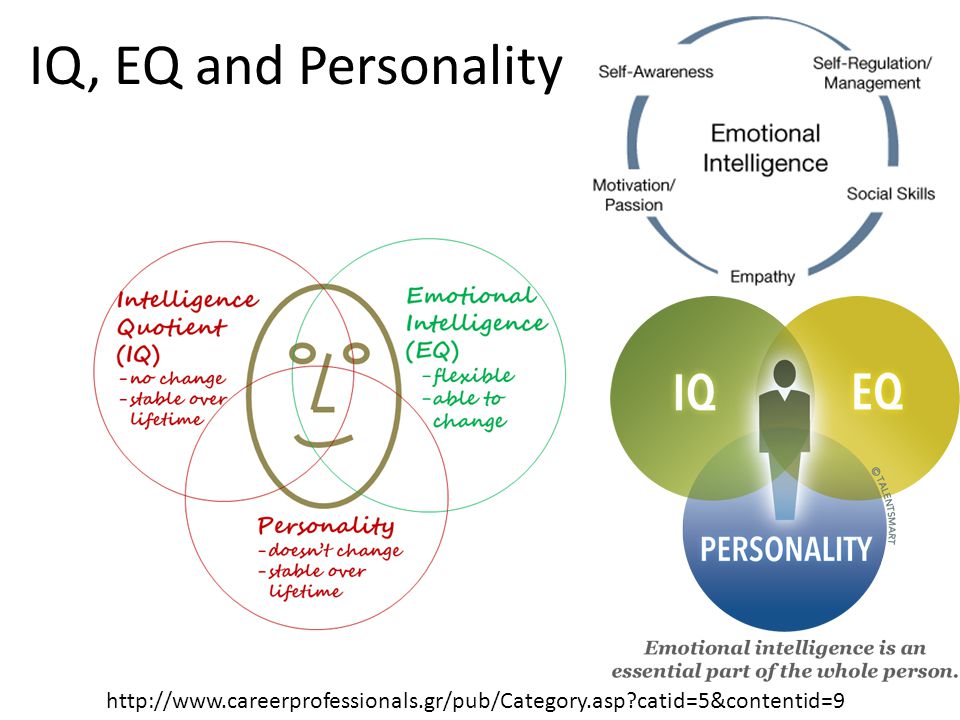
The dynamics of the disease also depends on the level of personality development and the characteristics of the emotional-volitional sphere of the patient. Even in cases of imbecility, in the absence of severe personality and behavioral disorders, relatively good compensation and social adaptation are possible. So, according to D. E. Melekhov (1970), 66% of imbeciles are able to work in specially organized conditions.
In some patients, in the process of age evolution and under the influence of therapeutic and corrective measures, there is a reverse development of such disorders as motor disinhibition, impulsivity, negativism, cerebrasthenic phenomena, and neurological symptoms.
The negative dynamics of oligophrenia is more often observed in more severe forms, in particular with gross anomalies in the development of the brain and other organs and systems, in complicated forms, when mental underdevelopment is combined with a psychoorganic syndrome, convulsive seizures and severe neurological symptoms. Negative dynamics in mental retardation is facilitated by various additional hazards that lead to decompensation of the condition (comorbidities and injuries, psychogenic disorders, unfavorable microsocial environment), as well as the lack of therapeutic and corrective measures. The negative dynamics of oligophrenia may be associated with decompensation during periods of age-related crises, especially puberty.
Negative dynamics in mental retardation is facilitated by various additional hazards that lead to decompensation of the condition (comorbidities and injuries, psychogenic disorders, unfavorable microsocial environment), as well as the lack of therapeutic and corrective measures. The negative dynamics of oligophrenia may be associated with decompensation during periods of age-related crises, especially puberty.
Periods of decompensation in oligophrenia are characterized by different phenomena. Most often, asthenic conditions occur with adynamia, increased exhaustion of mental processes, irritable weakness, emotional lability, etc. Neurotic disorders are also common - tics, stuttering, sleep and appetite disturbances, enuresis, fears, hysteroform phenomena. During these periods, affective disorders (in the form of dysphoria, dysthymia, euphoria, etc.) and behavioral disorders such as psychopathic reactions can also be observed. Sometimes decompensation appears in the form of hypochondriacal disorders, pathological behavioral reactions and psychopathic behavior (motor disinhibition, irritability, protest reaction, running away from home and vagrancy, the desire for arson and other pathological drives).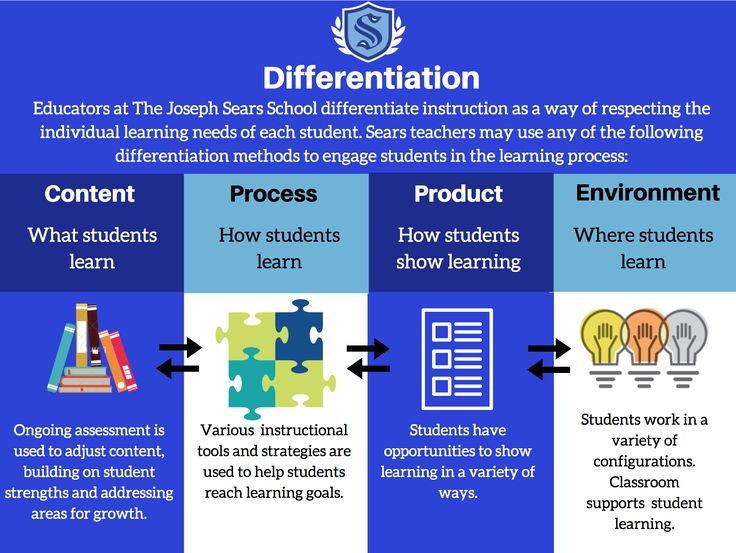 Sometimes intellectual abilities are significantly reduced, which leads to an incorrect conclusion about the growth of an intellectual defect, which in reality does not happen. A temporary decrease in intellectual abilities as a result of decompensation of the state should be distinguished from the reaction of pseudodementia in oligophrenics [Freyerov O. E., 1964]. In the first case, intellectual capabilities improve as the state compensates for the elimination or weakening of the influence of unfavorable factors.
Sometimes intellectual abilities are significantly reduced, which leads to an incorrect conclusion about the growth of an intellectual defect, which in reality does not happen. A temporary decrease in intellectual abilities as a result of decompensation of the state should be distinguished from the reaction of pseudodementia in oligophrenics [Freyerov O. E., 1964]. In the first case, intellectual capabilities improve as the state compensates for the elimination or weakening of the influence of unfavorable factors.
States of decompensation must be differentiated from psychopathic disorders. With the right approach and medical and pedagogical influences, these violations, including in the conditions of auxiliary schools, are quite easily compensated [Lebedinskaya K. S., 1982].
Especially often, neurotic disorders arise when a mentally retarded child is mistakenly placed in a public school or when a class is chosen incorrectly without sufficient consideration for the degree of intellectual deficiency. In such cases, a state of school maladaptation sets in, interest in learning is lost, fear and anxiety appear, sleep disorders, enuresis, etc. Some children experience reactions of passive protest in the form of negative behavior, refusal to study, leaving school.
In such cases, a state of school maladaptation sets in, interest in learning is lost, fear and anxiety appear, sleep disorders, enuresis, etc. Some children experience reactions of passive protest in the form of negative behavior, refusal to study, leaving school.
In the pubertal period, situations associated with the experience of one's own inferiority, the inability to take part in the life of healthy teenagers, and the wrong attitude of others towards a mentally retarded teenager acquire a psychotraumatic character. In more severe cases, it is possible to develop reactive states with subdepression, suicidal thoughts and even attempts.
Wrong conditions of education and training can cause pathocharacterological reactions, the consolidation of which sometimes becomes the basis for the appearance of pathological character traits [Kovalev V.V., 1971, 1995; Voronkov B.V., 1976; Trippi J., 1973; Komender J., 1974; Psarska A., 1974].
Until now, the question of the nosological affiliation of psychoses in oligophrenics remains unclear: whether they belong to specific psychoses characteristic of mental retardation or are only a modification of "ordinary" psychoses (reactive, symptomatic, endogenous). Supporters of the nosological independence of psychoses in oligophrenia explain their pathogenesis in different ways: by constitutional factors, psychological mechanisms, liquorodynamic disorders and other manifestations of residual cerebral insufficiency. Most domestic researchers associate the occurrence of psychosis in oligophrenia with decompensation of the state under the influence of various unfavorable (often psychogenic or exogenous-organic) factors [Freyerov O. E., 1964; Sukhareva G. E., 1965; Isaev D. N., 1976; Kovalev V.V., 1979, etc.]. Such a diversity of views in itself rather indicates that psychoses in oligophrenics do not fundamentally differ from psychoses in persons with normal intelligence. Apparently, we are talking about ordinary psychoses (psychogenic-reactive, exogenous-organic, endogenous) arising on pathological grounds, which explains the atypical nature of their clinical manifestations and course.
Supporters of the nosological independence of psychoses in oligophrenia explain their pathogenesis in different ways: by constitutional factors, psychological mechanisms, liquorodynamic disorders and other manifestations of residual cerebral insufficiency. Most domestic researchers associate the occurrence of psychosis in oligophrenia with decompensation of the state under the influence of various unfavorable (often psychogenic or exogenous-organic) factors [Freyerov O. E., 1964; Sukhareva G. E., 1965; Isaev D. N., 1976; Kovalev V.V., 1979, etc.]. Such a diversity of views in itself rather indicates that psychoses in oligophrenics do not fundamentally differ from psychoses in persons with normal intelligence. Apparently, we are talking about ordinary psychoses (psychogenic-reactive, exogenous-organic, endogenous) arising on pathological grounds, which explains the atypical nature of their clinical manifestations and course.
Many clinicians emphasize the dependence of the clinical picture of psychoses in oligophrenia on the severity of intellectual underdevelopment, and some even separate psychoses with severe mental retardation and psychoses with debility [Freyerov O. E., 1964]. Most authors adhere to the syndromic principle in the systematics and description of psychoses in the mentally retarded. There are psychoses with a predominance of affective disorders (in the form of dysphoric, dysthymic, anxiety-depressive, depressive-hypochondriac states), psychoses with a predominance of movement disorders and hallucinatory-delusional psychoses. The latter are rare and only in the form of short-term episodes. O. E. Freierov (1964) distinguished, in addition, psychoses that proceed according to the type of hysterical twilight disorder of consciousness, and acute psychotic reactions in oligophrenics (states of acute fear and confusion, the reaction of homesickness - nostalgia, especially specific for morons, reactions of pseudodementia and puerilism). The reactive states described by O.E. Freyerov in morons do not differ in clinical manifestations from situationally determined reactive states in healthy people, but in oligophrenia they are most often associated with a change in the habitual life stereotype.
E., 1964]. Most authors adhere to the syndromic principle in the systematics and description of psychoses in the mentally retarded. There are psychoses with a predominance of affective disorders (in the form of dysphoric, dysthymic, anxiety-depressive, depressive-hypochondriac states), psychoses with a predominance of movement disorders and hallucinatory-delusional psychoses. The latter are rare and only in the form of short-term episodes. O. E. Freierov (1964) distinguished, in addition, psychoses that proceed according to the type of hysterical twilight disorder of consciousness, and acute psychotic reactions in oligophrenics (states of acute fear and confusion, the reaction of homesickness - nostalgia, especially specific for morons, reactions of pseudodementia and puerilism). The reactive states described by O.E. Freyerov in morons do not differ in clinical manifestations from situationally determined reactive states in healthy people, but in oligophrenia they are most often associated with a change in the habitual life stereotype.![]()
Common features for all psychoses in oligophrenia are the rudimentary and fragmentary productive symptoms, the poverty and primitiveness of statements in connection with painful experiences. The clinical picture of psychosis as a whole is relatively simple and monotonous. Many authors emphasize the specificity and figurativeness of sensory and delusional disorders, the abundance of senestopathically colored somatic complaints. With complicated oligophrenia, the signs of organically altered soil are more pronounced: complacency or malice, uncriticality and particular importunity (“stickiness”), exhaustion, headache [Sukhareva G. E., 1965].
According to most researchers, a common feature of psychosis in oligophrenics is the reversibility and transience of psychotic disorders. The most characteristic are episodic and recurrent psychoses described by many domestic [Serbsky V.P., 1912; Felinskaya N.I., 1950; Freyerov O. E., 1964; Sosyukalo O.D., 1964; Sukharev G. E., 1965] and foreign authors [Nevstadt R. , 1931; Meadow W., 1935; Brendel J., 1954, etc.]. Their clinical picture and course differ from mental illnesses (schizophrenia, circular psychosis, exogenous psychoses), which can develop on the basis of mental retardation. Psychoses of this group were described by different authors under various names: "psychoses in oligophrenics", "psychoses in debility", "amorphous psychoses", etc. The high frequency of their occurrence in puberty and adolescence is emphasized [Sukhareva G. E., 1965; Sosyukalo O.D., 1966].
, 1931; Meadow W., 1935; Brendel J., 1954, etc.]. Their clinical picture and course differ from mental illnesses (schizophrenia, circular psychosis, exogenous psychoses), which can develop on the basis of mental retardation. Psychoses of this group were described by different authors under various names: "psychoses in oligophrenics", "psychoses in debility", "amorphous psychoses", etc. The high frequency of their occurrence in puberty and adolescence is emphasized [Sukhareva G. E., 1965; Sosyukalo O.D., 1966].
The etiology and pathogenesis of psychosis in people with mental retardation is not yet clear enough. The role of vascular and liquorodynamic disorders is assumed. The frequency of occurrence of such psychoses during puberty also indicates the pathogenetic role of the shifts characteristic of pubertal crises. A certain role in the development of psychosis can be played by pathogenetic mechanisms specific to one form or another. Thus, there is an increased frequency of psychosis with subsequent regression of mental functions in adults and adolescents with Down's disease.