Social anxiety dsm 5 code
Table 16, DSM-IV to DSM-5 Social Phobia/Social Anxiety Disorder Comparison - DSM-5 Changes
Table 16DSM-IV to DSM-5 Social Phobia/Social Anxiety Disorder Comparison
| DSM-IV | DSM-5 |
|---|---|
| Disorder Class: Anxiety Disorders | SAME |
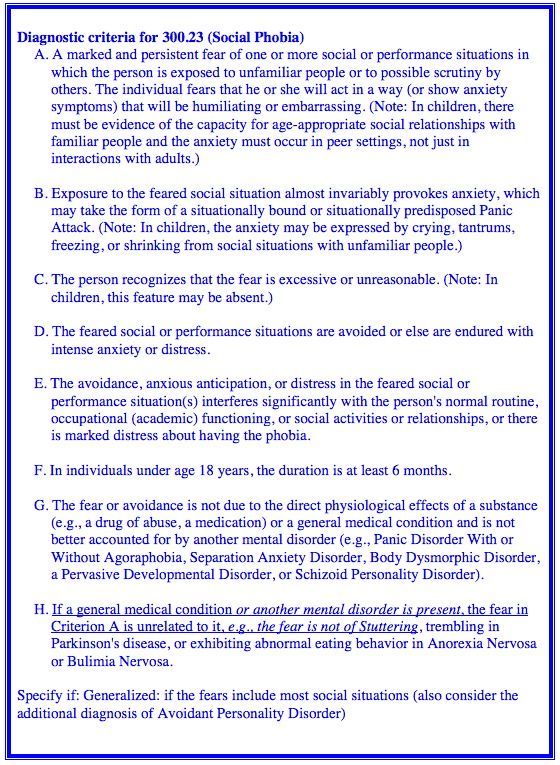
| A. A marked and persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others. The individual fears that he or she will act in a way (or show anxiety symptoms) that will be humiliating or embarrassing. Note: In children, there must be evidence of the capacity for age-appropriate social relationships with familiar people and the anxiety must occur in peer settings, not just in interactions with adults. | A. Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others. Examples include social interactions (e.g., having a conversation, meeting unfamiliar people), being observed (e.g., eating or drinking), and performing in front of others (e.g., giving a speech). Note: In children, the anxiety must occur in peer settings and not just during interactions with adults. The individual fears that he or she will act in a way or show anxiety symptoms that will be negatively evaluated (i.e., will be humiliating or embarrassing; will lead to rejection or offend others). |
| B. Exposure to the feared social situation almost invariably provokes anxiety, which may take the form of a situationally bound or situationally predisposed panic attack. Note: In children, the anxiety may be expressed by crying, tantrums, freezing, clinging, shrinking, or failing to speak in social situations. 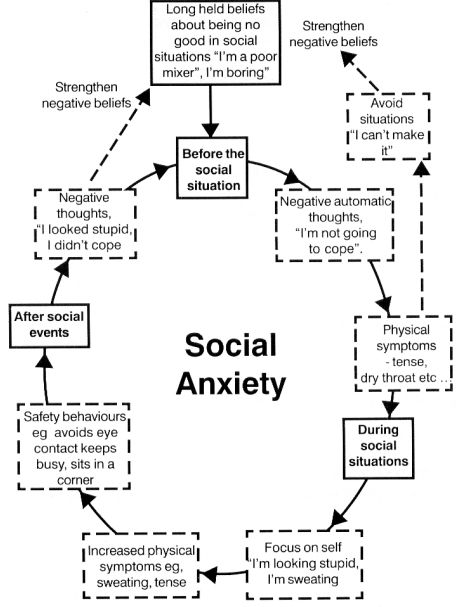 | C. The social situations almost always provoke fear or anxiety. Note: In children, the fear or anxiety may be expressed by crying, tantrums, freezing, clinging, shrinking, or failing to speak in social situations. |
| C. The person recognizes that the fear is excessive or unreasonable. Note: In children, this feature may be absent. | B. The fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context. |
| D. The feared social or performance situations are avoided or else are endured with intense anxiety or distress. | D. The social situations are avoided or endured with intense fear or anxiety. |
| t12_1_1_1_1" rowspan="1" colspan="1">E. The avoidance, anxious anticipation, or distress in the feared social or performance situation(s) interferes significantly with the person’s normal routine, occupational (academic) functioning, or social activities or relationships, or there is marked distress about having the phobia. | G. The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| F. In individuals under age 18 years, the duration is at least 6 months. | F. The fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more. |
G. The fear or avoidance is not due to the direct physiological effects of a substance (e.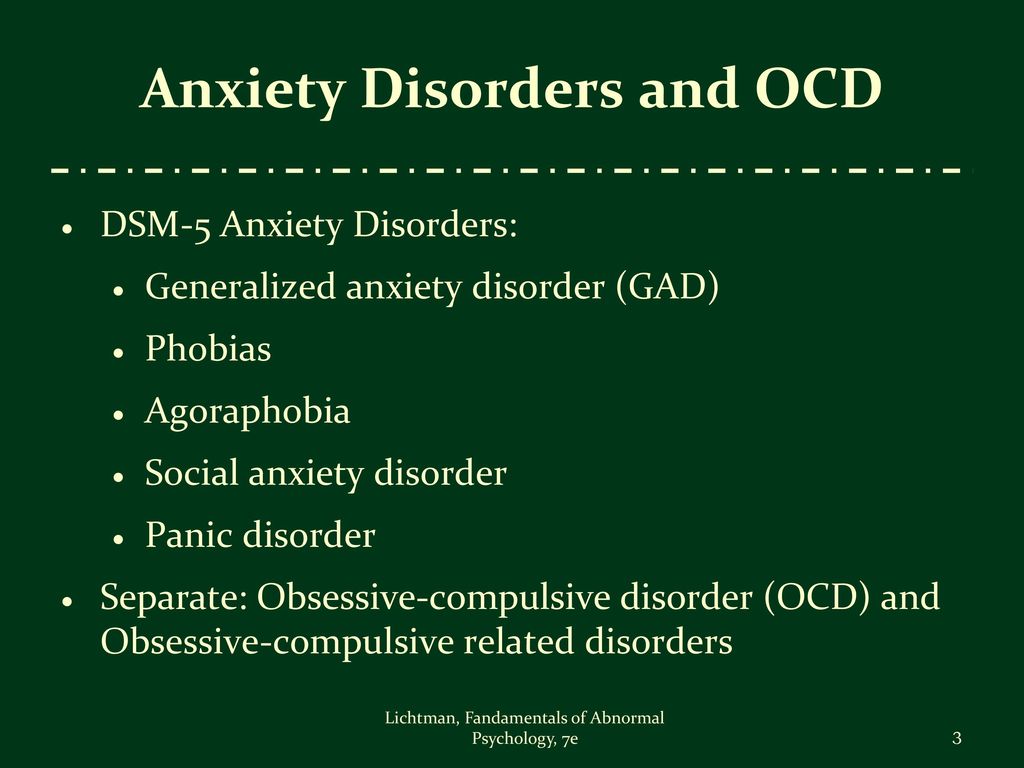 g., a drug of abuse, a medication) or a general medical condition and is not better accounted for by another mental disorder (e.g., panic disorder with or without agoraphobia, separation anxiety disorder, body dysmorphic disorder, a pervasive developmental disorder, or schizoid personality disorder). g., a drug of abuse, a medication) or a general medical condition and is not better accounted for by another mental disorder (e.g., panic disorder with or without agoraphobia, separation anxiety disorder, body dysmorphic disorder, a pervasive developmental disorder, or schizoid personality disorder). | H. The fear, anxiety, or avoidance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. |
| I. The fear, anxiety, or avoidance is not better explained by the symptoms of another mental disorder, such as panic disorder, body dysmorphic disorder, or autism spectrum disorder. | |
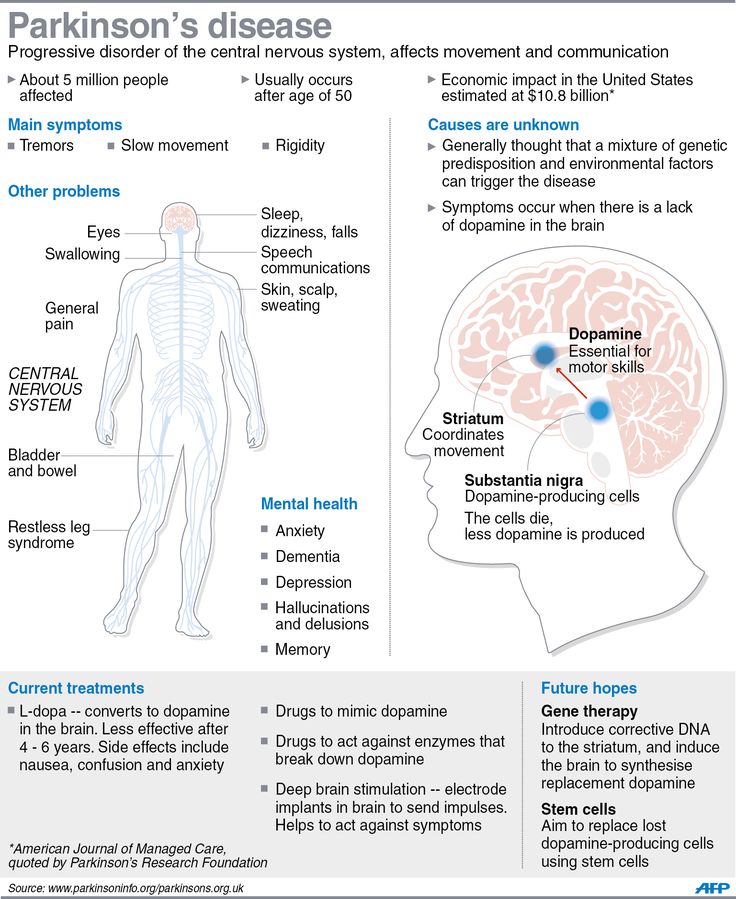
H. If a general medical condition or another mental disorder is present, the fear in Criterion A is unrelated to it (e. g., the fear is not of stuttering, trembling in Parkinson’s disease, or exhibiting abnormal eating behavior in anorexia nervosa or bulimia nervosa). g., the fear is not of stuttering, trembling in Parkinson’s disease, or exhibiting abnormal eating behavior in anorexia nervosa or bulimia nervosa). | J. If another medical condition (e.g., Parkinson’s disease, obesity, disfigurement from burns or injury) is present, the fear, anxiety, or avoidance is clearly unrelated or is excessive. |
| Specify if: Generalized: if the fears include most social situations (also consider the additional diagnosis of avoidant personality disorder) | Specify if: Performance only: if the fear is restricted to speaking or performing in public. |
300.23 Social Anxiety Disorder (Social Phobia) Symptoms and Related Diagnosis
Social Anxiety Disorder and the DSM-5
Social phobia was first classified as a mental disorder in the DSM-III.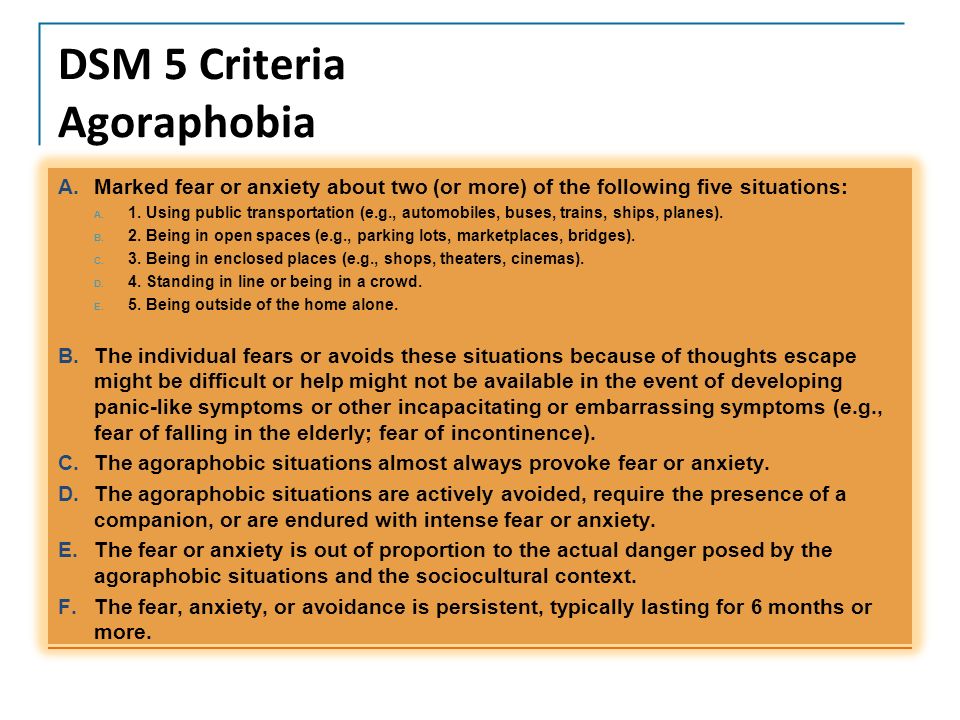 More recently it has been reclassified in the DSM-5 (Diagnostic And Statistical Manual of Mental Disorders-Fifth edition) as social anxiety disorder. It is one of the most common anxiety disorders with some researchers believing that it has a lifetime prevalence rate of a little more than 10%. Most people are diagnosed with social anxiety disorder in childhood or in the earlier adolescent years. This anxiety disorder is frequently comorbid with other mental health disorders such as major depressive disorder, substance use disorders and other anxiety disorders.
More recently it has been reclassified in the DSM-5 (Diagnostic And Statistical Manual of Mental Disorders-Fifth edition) as social anxiety disorder. It is one of the most common anxiety disorders with some researchers believing that it has a lifetime prevalence rate of a little more than 10%. Most people are diagnosed with social anxiety disorder in childhood or in the earlier adolescent years. This anxiety disorder is frequently comorbid with other mental health disorders such as major depressive disorder, substance use disorders and other anxiety disorders.
Main Characteristics of Social Anxiety Disorder:
Some of the key features of social anxiety disorder include an ongoing fear and worry of social situations. If you have social anxiety disorder, you may have a fear of negative evaluation by others, performance anxieties or fear of being observed in various social circumstances. The DSM-5 also included a performance only specifier which needs to be experienced for a minimum of six months. Children and adolescents also share the same minimum duration as adults.
Children and adolescents also share the same minimum duration as adults.
While both genders seem to share the same intense fears and worries, women tend to be diagnosed with social anxiety disorder more often than men. An interesting anecdote is that people with social anxiety disorder tend to never marry or have children. This anxiety disorder is highest among Caucasian and Native Americans, and studies have found it to also be high among Latino and Caucasian youth.
Some people may believe shyness to be a social anxiety disorder, but it is not. Shyness is not pathological and does not result in the severe impairment that you would see in someone who has social anxiety disorder. Also, when comparing social anxiety disorder to specific phobias, phobic individuals typically do not worry about being judged in social situations. Individuals with social anxiety disorder seem to have a capacity for age-appropriate interactions as well as social relationships, although they sometimes avoid them and may experience significant personal distress at times.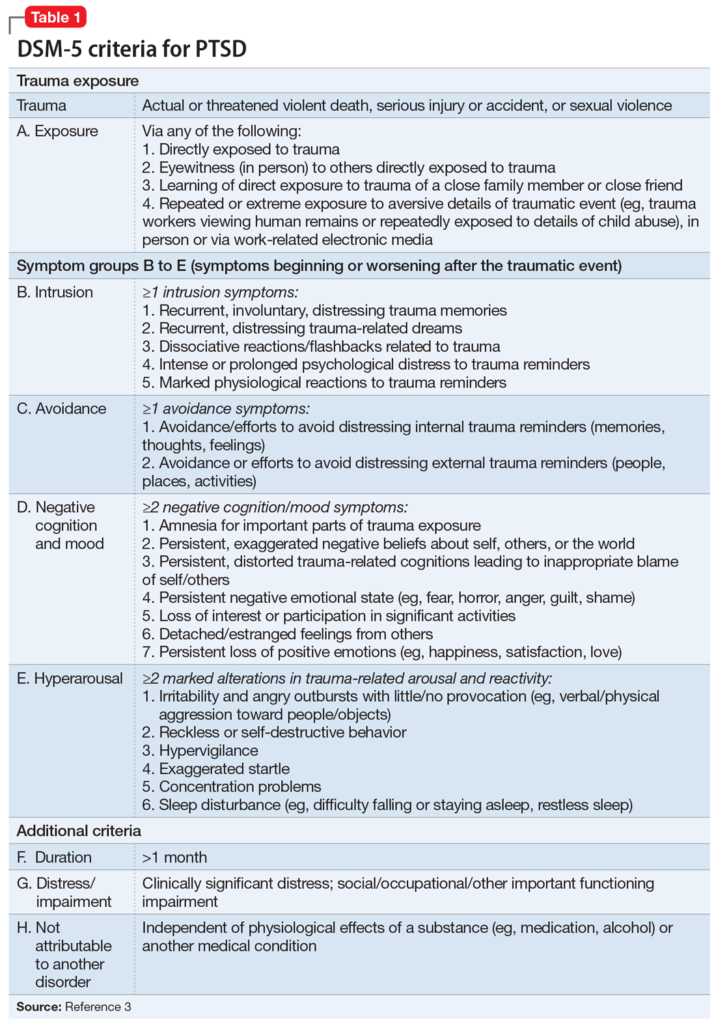 Individuals diagnosed with social anxiety disorder often have significant insight into the disproportionate fear and anxiety they experience in social situations.
Individuals diagnosed with social anxiety disorder often have significant insight into the disproportionate fear and anxiety they experience in social situations.
Social Anxiety and Public Speaking:
The most common and most easily recognizable social anxiety disorder is fear of public speaking. This disorder is experienced by approximately three out of four or about 75% of the overall population. Most people have some anxiety about speaking in public, while individuals with this performance related social anxiety disorder may have very intense almost disabling ability to speak in front of other people.
Social Anxiety Disorder Treatments:
Some of the treatments available for social anxiety disorder include both psychological treatments and medication. Psychological treatments include cognitive behavioral therapy, relaxation therapy and the use of exposure treatment. Medications treatments include the use of depression medications such as the SSRIs, and anxiety medication such as Xanax and Klonopin.
Social Anxiety Disorder Coding and Specifiers:
Social anxiety disorder has only one diagnostic code: 300.23 (F40.10). However, a performance only specifier may also be included with this disorder if it is specifically related to speaking or performing in public. In most cases these individuals do not avoid social situations and fear evaluation or scrutiny except for when public speaking or performing in front of others. If people experience panic attacks in conjunction with social anxiety disorder, they may also be given the specifier with panic attacks, which should be added to the actual diagnosis.
The specific symptoms of social anxiety disorder follow below.
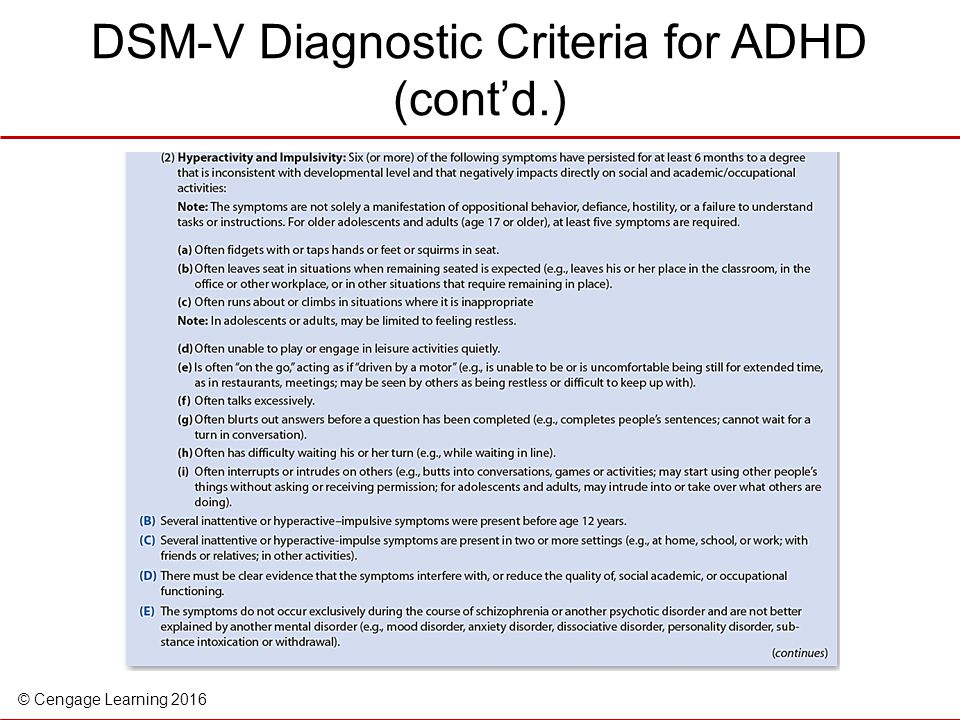
Social Anxiety Disorder (Social Phobia) diagnostic criteria 300.23 (F40.10):
A. Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others. Examples include social interactions such as having a conversation, meeting unfamiliar people, being observed eating or drinking, and performing in front of others such as giving a speech.
B. Individual fears that he or she will act in a way or show anxiety symptoms that will be negatively evaluated such as feeling humiliated or embarrassed or will lead to rejection or offend others.
C. The social situations almost always provoke fear or anxiety.
Note: In children, the fear or anxiety may be expressed by crying, tantrums, freezing, clinging, shrinking, or failing to speak in social situations.
D. The social situations are avoided or endured with intense fear or anxiety.
E. The fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context.
F. The fear, anxiety, or avoidance is persistent, typically lasting for six months or more.
G. The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
H. The fear, anxiety, or avoidance is not attributable to the physiological effects of a substance such as drug of abuse, a medication or another medical condition.
I. The fear, anxiety, or avoidance is not better explained by the symptoms of another mental disorder, such as panic disorder, body dysmorphic disorder, or autism spectrum disorder.
J. If another medical condition such as Parkinson’s disease, obesity, disfigurement from burns or injury is present, the fear, anxiety, or avoidance is clearly unrelated or is excessive.
Specify if:
Performance only: If the fear is restricted to speaking or performing in public.
Diagnostic Information and Criterion adaptedfrom the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition American Psychological Association by Paul Susic Ph.D. Licensed Psychologist
See Related Posts:
Treatment of social anxiety disorder - PsyAndNeuro.ru
Social anxiety disorder (SAD) is one of the most common anxiety disorders (8-12% of the global population). It is more common in women than in men; more often in developed countries than in developing ones. STR begins at a young age (average age 12) and continues as a chronic disease. In epidemiological studies, the following factors that increase the risk of SAD have been noted: low educational level, low socioeconomic status, celibacy, and comorbid depression.
STR begins at a young age (average age 12) and continues as a chronic disease. In epidemiological studies, the following factors that increase the risk of SAD have been noted: low educational level, low socioeconomic status, celibacy, and comorbid depression.
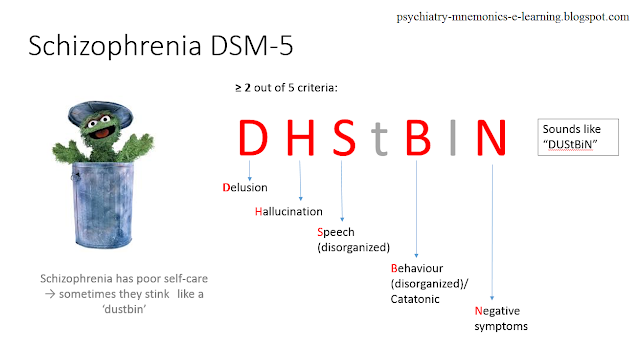
Up to 72% of patients with SAD suffer from another psychiatric disorder. The most common are depression and other anxiety disorders. Also diagnosed with SAD are anxiety disorder, body dysmorphic disorder, substance abuse, ADHD, and schizophrenia.
Here is an overview translation of the clinical guidelines for the treatment of social anxiety disorder, compiled by the experts of the Canadian Association of Anxiety Disorders. The translation was prepared jointly by the scientific Internet portal "Psychiatry & Neuroscience" and the Clinic of Psychiatry "Doctor SAN" (St. Petersburg). You can download the whole recommendation file from the link.
Diagnosis
SAD is characterized by a constant fear that in a social situation a person will say or do something that will cause a negative evaluation from other people.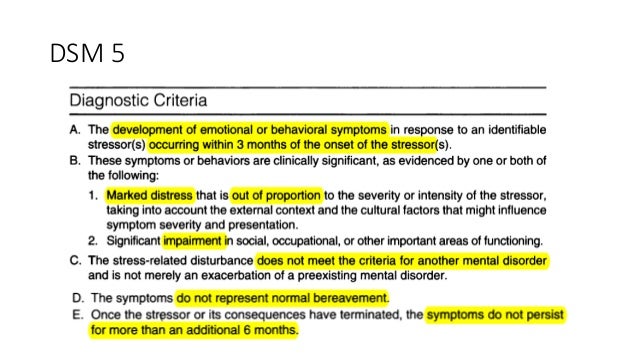 Social situations are avoided or experienced in a state of distress, while the person understands that his fear is excessive and irrational. Avoidance behavior and anxiety lead to significant functional impairment.
Social situations are avoided or experienced in a state of distress, while the person understands that his fear is excessive and irrational. Avoidance behavior and anxiety lead to significant functional impairment.
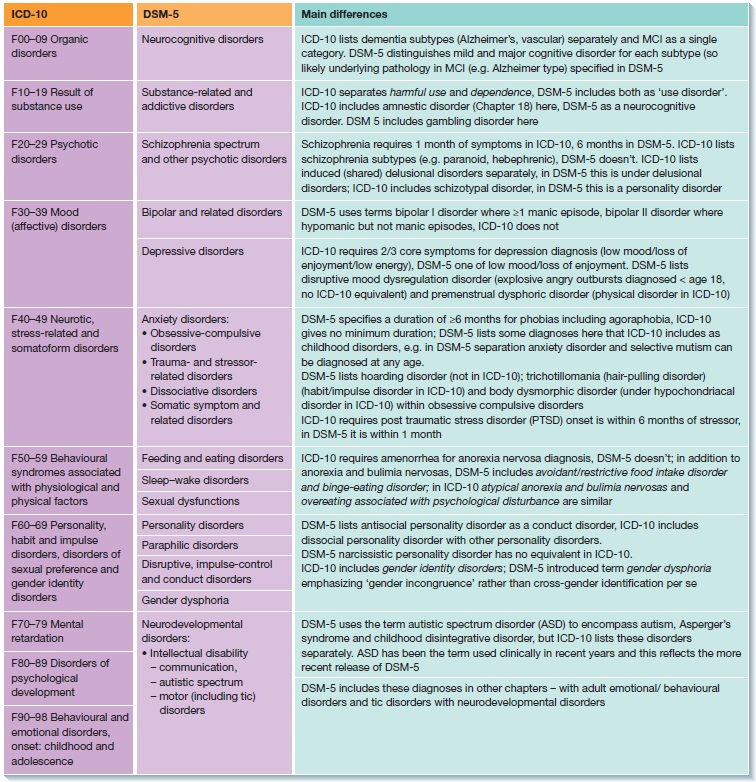
The DSM-IV-TR did not mention fear and avoidance associated with medical problems, but the DSM-V indicates that SAD may be secondary to physical illness. Some patients experience social anxiety due to symptoms of their illnesses (e.g. stuttering, shaking from Parkinson's disease, obesity, burn or injury marks).
DSM-5 criteria for diagnosis of pages (sociophobia)
1- Fear and anxiety about social situations in which other people can be evaluated by
2- Fear that anxiety symptoms will be negatively assessed by other people
3 - Social situation:
- Almost always provokes fear or anxiety
- Avoided or experienced with fear or anxiety
4 - Fear, anxiety or avoidance:
- Not commensurate with the actual danger of a particular social situation
- Lasts for a long time, usually more than 6 months and functional impairment
5 – If any medical condition (e. g. stuttering, obesity) is present, anxiety is not adequate to its severity
g. stuttering, obesity) is present, anxiety is not adequate to its severity
A specific type of SAD - fear associated exclusively with public speaking
Psychological support The cognitive techniques of CBT target maladaptive thoughts and attitudes, the behavioral component is usually reduced to exposure therapy. The effectiveness of CBT has been proven by many RCTs and meta-analyses. There are studies showing similar efficacy of CBT and pharmacotherapy in the treatment of acute SAD. It is reported that after completion of treatment, the improvement achieved with CBT lasts longer, compared with the results of pharmacotherapy. CBT for STR can be done individually or in a group. Although several studies favor individual psychotherapy, meta-analyses have not found a significant difference in effectiveness.
The effectiveness of CBT components has also been studied. Exposure therapy has been proven to work without the addition of other components of CBT.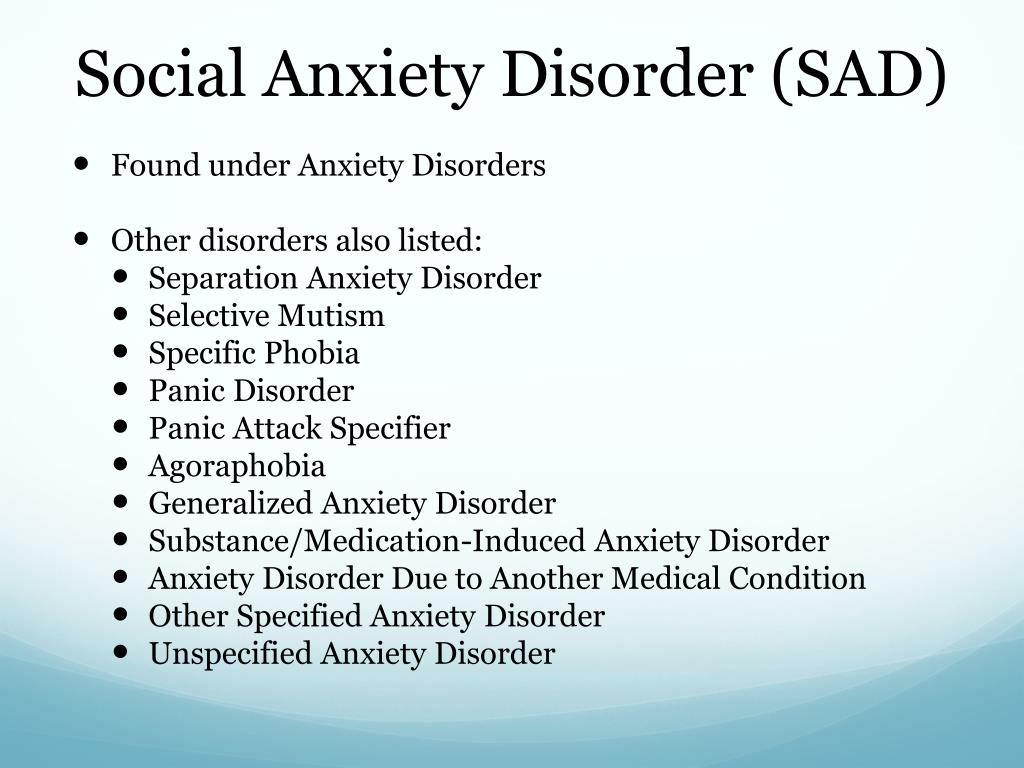
CBT with an emphasis on interpersonal relationships produces the same results as standard CBT, but it also increases relationship satisfaction. The effectiveness of interpersonal psychotherapy in CBT does not have a sufficient evidence base, there are studies that say that it is ineffective. It appears to be less effective than traditional CBT.
Mindfulness-based cognitive therapy is also less effective than CBT, but still able to improve the condition in SAD.
ICBT (Internet-assisted CBT) is a new type of psychotherapy that makes CBT more accessible to patients with anxiety and mood disorders. Studies have compared ICBT and CBT (individual and group). ICBT has been shown to be effective in the treatment of STR. Most ICBT programs involve minimal contact with a psychotherapist via email or telephone. Many programs include participants communicating on Internet forums. It remains unclear whether the participation of a psychotherapist is a prerequisite for ICBT.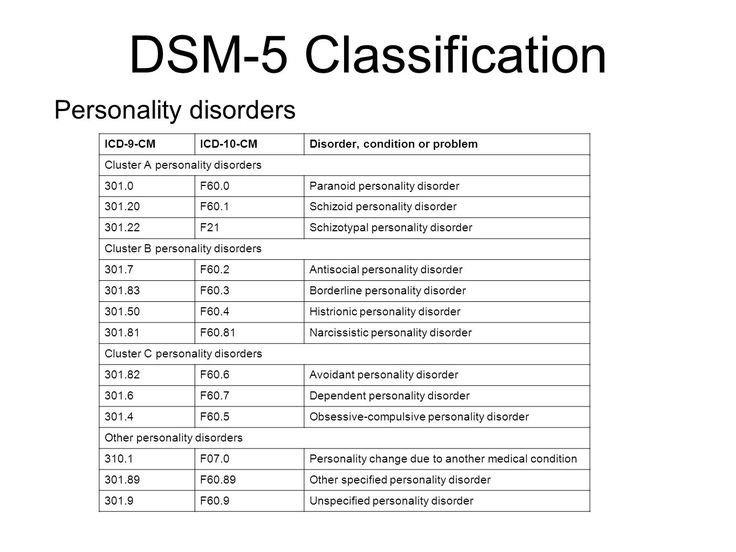 Studies comparing psychotherapist-led ICBT and non-psychotherapist-guided ICBT provide conflicting results. All RCTs assumed that before starting ICBT, the patient had previously communicated with a psychotherapist in person or by phone and contacted him after the end of the course. Little is known about the effectiveness of self-treatment (ICBT or self-help books) that is given without prior conversation and follow-up contact with a psychotherapist.
Studies comparing psychotherapist-led ICBT and non-psychotherapist-guided ICBT provide conflicting results. All RCTs assumed that before starting ICBT, the patient had previously communicated with a psychotherapist in person or by phone and contacted him after the end of the course. Little is known about the effectiveness of self-treatment (ICBT or self-help books) that is given without prior conversation and follow-up contact with a psychotherapist.
Combination of psychotherapy and pharmacological treatment
Pharmacotherapy does not enhance the effects of CBT, although one study found that the combination of phenelzine with CBT worked better than phenelzine and CBT alone. D-cycloserine taken during exposure enhances their therapeutic effect. There is also a study proving that the combination of psychodynamic group therapy with clonazepam works better than clonazepam without psychotherapy.
Duration of effect of psychotherapy
The results achieved with CBT are noted during visits to the doctor for 6-12 months.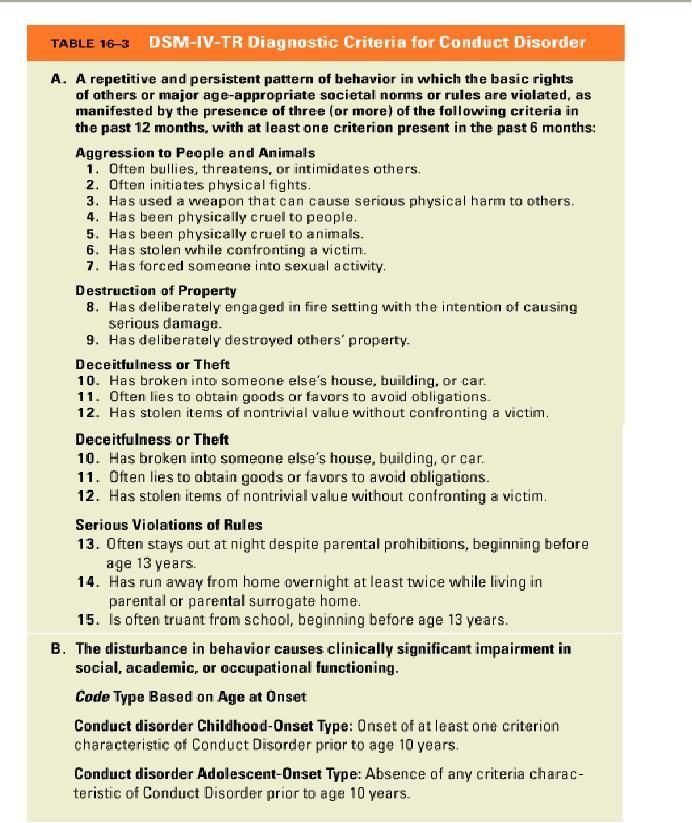 Sustained improvement has been reported for five years after treatment. Improvement after ICBT is noted at follow-up visits one to five years after the end of treatment. The long-term effect of psychotherapy is longer than the effect of pharmacotherapy remaining after stopping treatment.
Sustained improvement has been reported for five years after treatment. Improvement after ICBT is noted at follow-up visits one to five years after the end of treatment. The long-term effect of psychotherapy is longer than the effect of pharmacotherapy remaining after stopping treatment.
Pharmacological treatment
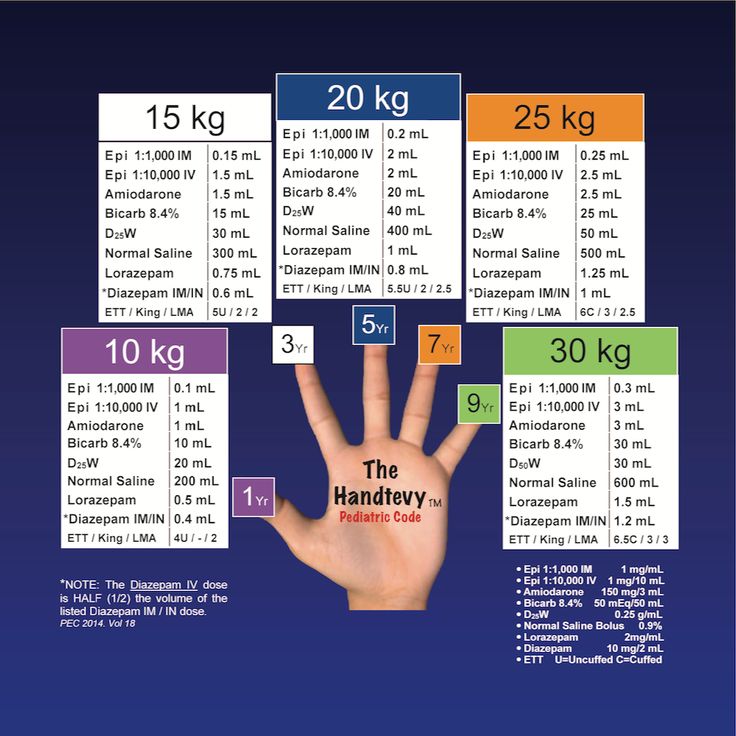
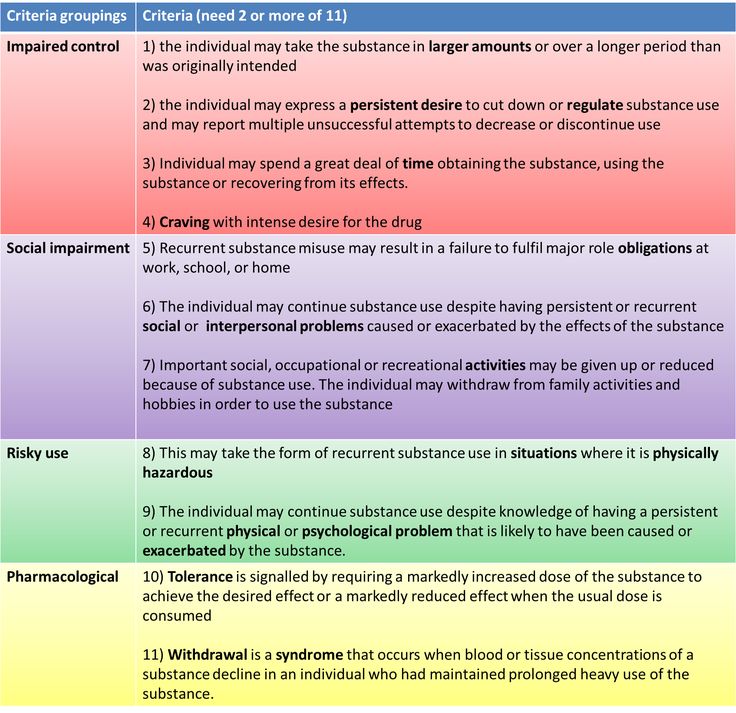
Providence levels
1-at least 2 RCTs with a placebo control
2-at least 1 RCT with a placebo control or active control of
9000 3 3,000 3 3,000 3 – Study without control group, with at least 10 participants4 – Case reports or expert opinion
Evidence levels do not tell the nature of the result (positive, negative, questionable), they tell the quality of the analysis performed.
Recommended treatment
The first line - Processing levels 1 or 2, as well as clinically proven efficiency and safety
, second line - Process level 3, as well as clinically proven efficiency and safety
Third line - Evidence level 4 and clinically proven efficacy and safety
Not recommended - No effect with evidence level 1 or 2
First line
SSRIs, SNRIs, anticonvulsants, and benzodiazepines have been shown to be effective in treating STR.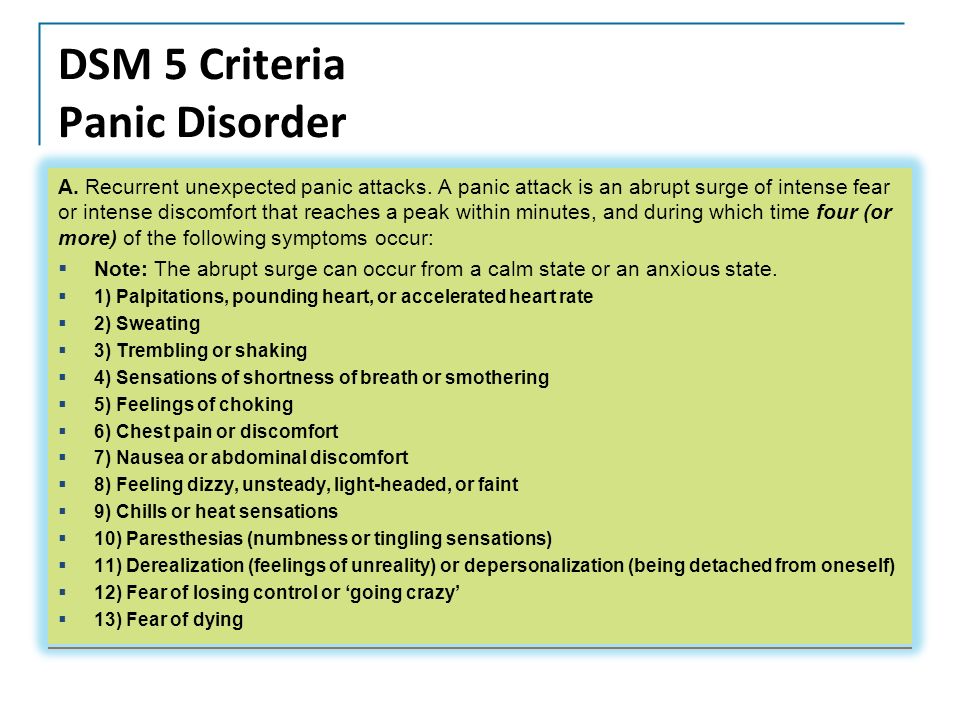 Evidence for the effectiveness of citalopram in SR is low, but it is probably as effective as other SSRIs, in contrast to fluoxetine, which has been shown to be ineffective in SR in studies and therefore can be considered the least effective SSRI.
Evidence for the effectiveness of citalopram in SR is low, but it is probably as effective as other SSRIs, in contrast to fluoxetine, which has been shown to be ineffective in SR in studies and therefore can be considered the least effective SSRI.
Pregabalin: Pregabalin is effective in the treatment of SAD at high doses (600 mg/day) but not at low doses (150–300 mg/day). Although the effectiveness of pregabalin is level 1 evidence, it is not clear how effective it is compared to that of SSRIs. In addition, the effectiveness of SSRIs has a wider spectrum in relation to typical comorbid conditions.
Second line
Benzodiazepines: Meta-analysis showed that benzodiazepines are as effective as SSRIs, but because they have little effect on typical addiction conditions and may form comorbid conditions in individuals substance abusers, benzodiazepines are recommended as second-line treatment.
Antidepressants: RCTs have shown citalopram to be as effective as moclobemide. Phenelzine has been shown to be effective, but due to dietary restrictions, drug interactions, and the risk of hypertensive crisis, it is recommended as a second-line agent. Anticonvulsants: There is (second level) evidence that gabapentin is as effective as tiagabine.
Phenelzine has been shown to be effective, but due to dietary restrictions, drug interactions, and the risk of hypertensive crisis, it is recommended as a second-line agent. Anticonvulsants: There is (second level) evidence that gabapentin is as effective as tiagabine.
Third line
Antidepressants: Fluoxetine efficacy studies are inconsistent. A large RCT showed a positive effect as strong as CBT. But two other, smaller RCTs showed no effect. Therefore, it can be assumed that fluoxetine is less effective than other SSRIs.
Same situation with moclobemide. Several RCTs showed a positive effect, a few did not. Moclobemide is more effective than CBT at the beginning of psychotherapy, but after 6 months CBT shows a stronger effect than moclobemide. Two small RCTs of mirtazapine produced conflicting results, one was effective, the other was not. Comparison of the efficacy of 60 mg/day duloxetine with 120 mg/day duloxetine showed no benefit from the higher dose.
All of these drugs, as well as anticonvulsants, olanzapine, selegelin, atomoxetine, can be recommended as third-line agents for patients who have not responded to first-line and second-line drugs as monotherapy and in combination with additional drugs.
Additive drugs
The strategy of using additional drugs has been studied in patients who have not responded adequately to antidepressant treatment and can be used in cases of resistant SAD.
Preparation | Level of evidence |
| SSRI | 1 |
| Escitalopram | 1 |
| Fluvoxamine | 1 |
| Paroxetine | 1 |
| Sertraline | 1 |
| Fluoxetine | 1 (inconsistent data) |
| Citalopram | 2 |
| Paroxetine as adjunct | 3 |
| SNRI | |
| Venlafaxine | 1 |
| Duloxetine | 2 |
| TCA | |
| Clomipramine | 3 |
| Imipramine | 3 (negative) |
| IMAO and OIMAO | |
| Phenelzine | 1 |
| Moclobemide | 1 (inconsistent data) |
| Other antidepressants | |
| Mirtazapine | 1 (inconsistent data) |
| Bupropion | 3 |
| Benzodiazepines | |
| Clonazepam | 1 |
| Alprazolam | 2 |
| Bromazepam | 2 |
| Clonazepam as add-on | 2 (negative) |
| Anticonvulsants | |
| Pregabalin | 1 |
| Gabapentin | 2 |
| Levetiracetam | 2 (negative) |
| Divalproex | 3 |
| Tiagabin | 3 |
| Topiramate | 3 |
| Other drugs | |
| Atenolol | 1 (negative result) |
| Buspirone | 1 (negative result) |
| Atomoxetine | 1 (inconsistent data) |
| Propranolol | 2 (negative result) |
| Selegiline | 3 |
| Pergolide | 3 (negative) |
| Buspirone as add-on | 3 |
| Pindolol as adjuvant | 2 (negative) |
| Atypical antipsychotics | |
| Olanzapine | 2 |
| Quetiapine | 2 (negative result) |
| Aripiprazole as add-on | 3 |
| Risperidone as add-on | 3 |
| First line: Escitalopram, fluvoxamine, paroxetine, pregabalin, sertraline, venlafaxine Second line: Alprazolam, bromazepam, citalopram, clonazepam, gabapentin, phenelzine Third line: Atomoxetine, bupropion, clomipramine, divalproex, duloxetine, fluoxetine, mirtazapine, moclobemide, olanzapine, selegiline, tiagabine, topiramate Complementary drugs (third line): Aripiprazole, buspirone, paroxetine, risperidone Not recommended as adjuncts: Clonazepam, pindolol Not recommended: Atenolol*, Buspirone, Imipramine, Levetiracetam, Propranolol*, Quetiapine *Beta-blockers have been successfully used during public speaking. |
Maintenance pharmacological therapy
Meta-analysis showed that long-term use of SSRIs (3-6 months) effectively prevented relapse (relative risk = 0.39). Pregabalin has also been shown to be effective in preventing relapse. There are studies showing the effectiveness of long-term use of moclobemide in preventing relapse.
Biological and alternative therapies
Biological therapy: Neuro-Psychophysical Optimization Radioelectric Asymmetric Brain Stimulation (NPPO-REAC) protocol has been shown to be as effective as sertraline.
Alternative therapy: St. John's wort is not effective in the treatment of CRT and is not recommended for use (Evidence level 2).
Translated by: Filippov D.S.
Source: Katzman et al.: Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessivecompulsive disorders.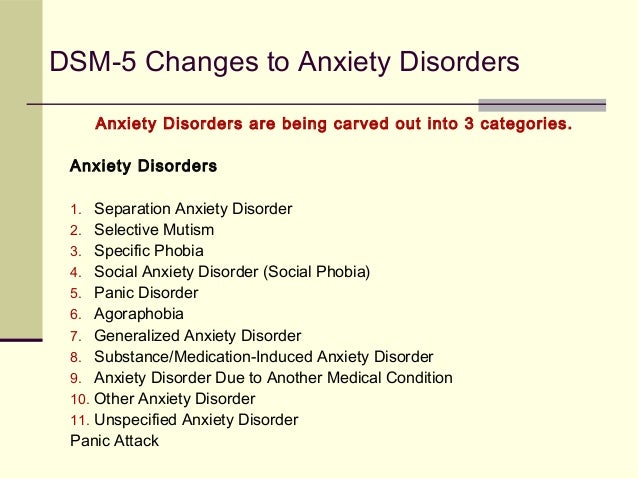 BMC Psychiatry 2014 14
BMC Psychiatry 2014 14
Anxious personality disorder - symptoms, causes, stages
Anxious personality disorder is a disorder in which a person is characterized by isolation, feelings of inferiority, asociality, avoidance of communication with others because of fear of being criticized. Often associated with symptoms of other anxiety spectrum disorders.
The disease most often occurs in people aged 15 to 35 years.
Disease definition
The most common types of disorder are anxiety avoidant personality disorder and phobic disorders. Such a state is characterized by a feeling of anxiety - anxiety of ongoing events and fear - a reaction to what is happening.
Anxiety is an individual feature of a person, therefore it does not manifest itself in everyone. A person with increased anxiety tends to worry about every trifle.
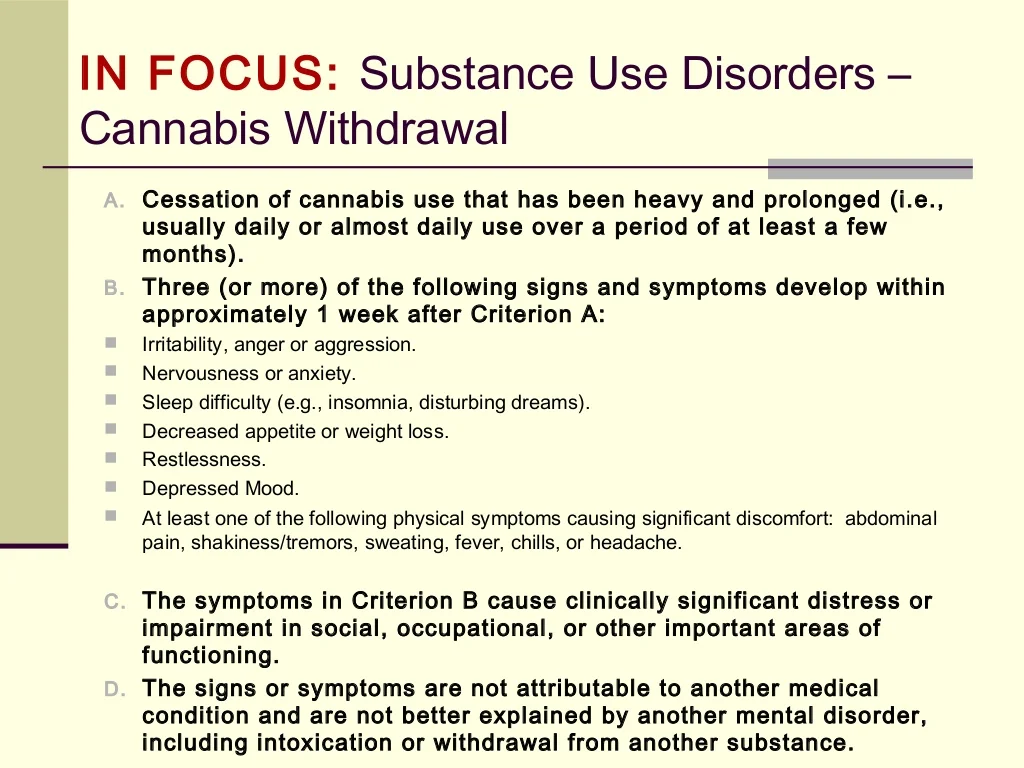
The condition can be diagnosed if its symptoms appear for six months and significantly worsen the quality of a person’s life.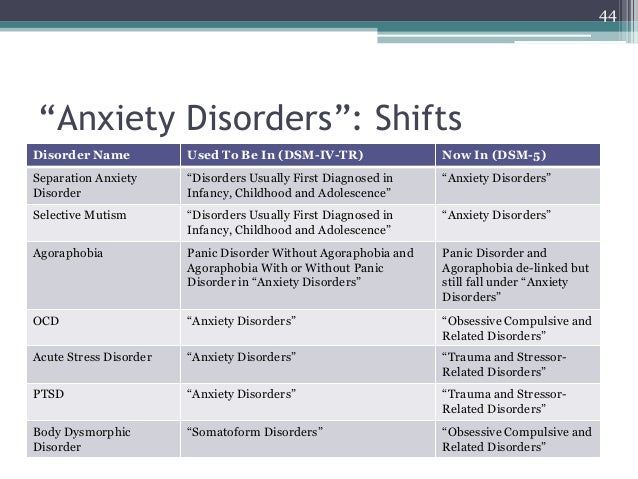 Among the physical disorders that can lead to such disorders are hyperthyroidism, ischemia, caffeine, alcohol and drug addiction (from cannabis), and drug withdrawal symptoms.
Among the physical disorders that can lead to such disorders are hyperthyroidism, ischemia, caffeine, alcohol and drug addiction (from cannabis), and drug withdrawal symptoms.
The ICD-10 code for avoidant personality disorder is F60.6. In order to make this diagnosis, the patient must have the following behavioral symptoms (at least 4):
- Constant tension and anxiety.
- Low self-esteem and feelings of inadequacy.
- Increased suspiciousness and a feeling of criticism from others.
- Communication only with those people who, in the opinion of the patient, like him.
- Avoiding active interpersonal contact for fear of criticism.
Another type of disorder is distinguished - anxious depressive personality disorder, in which the patient equally has symptoms of both anxiety and depression, however, individually they are not so pronounced as to diagnose the disorder. Such a diagnosis should be made only by an experienced doctor, with an appeal to which one cannot delay. This type of disease often causes suicidal thoughts, which many patients translate into reality.
This type of disease often causes suicidal thoughts, which many patients translate into reality.
Symptoms and signs of anxiety disorder
Symptoms of an anxious personality disorder manifest themselves in childhood, when the child is shy, fearful, afraid to meet people, go to the blackboard, be the center of attention. Closer to adolescence, the symptoms become more pronounced. Such people do not have many friends, they avoid social events, preferring to spend time alone with books or a computer. Patients with anxiety disorder distance themselves from others, fearing criticism and disapproval, worry about any minor trifles.
In the future, such patients do not develop a career because of their awkwardness and inexperience in relationships. They prefer quiet, inconspicuous work, in which they do not have to manage people and speak in public.
Internal tension does not allow them to communicate with others. From the outside, they seem ridiculous, closed, strange and even arrogant, which often causes negativity in the interlocutor. Such a condition prevents the patient from turning even to a psychologist. If it seems to him that the doctor does not approve of his behavior or does not accept, then the patient may abruptly interrupt therapy and close even more. Therefore, it is so important that the specialist is qualified and has experience working with such patients.
Such a condition prevents the patient from turning even to a psychologist. If it seems to him that the doctor does not approve of his behavior or does not accept, then the patient may abruptly interrupt therapy and close even more. Therefore, it is so important that the specialist is qualified and has experience working with such patients.
Signs of an anxious personality disorder may be accompanied by tachycardia, abdominal pain, excessive sweating, migraine, dizziness, stool disturbance, and muscle pain.
Among the symptoms that can give out an anxiety disorder are the following:
- The problem is concentration.
- Insomnia.
- Lack of energy.
- Nervous state.
- Feeling of anxiety.
- Tearfulness.
- Pessimistic mood.
- Low self-esteem, a tendency to belittle.
- Excessive tension in all aspects.
- Decreased mood, apathy.
It can be difficult to diagnose the disorder due to concomitant somatic diseases - digestive disorders, headaches, and so on. Often, therapists, without revealing a somatic pathology, diagnose vegetovascular dystonia, which completely deprives the patient of the opportunity to visit a psychotherapist or psychiatrist, since the disorder is mental in nature. According to statistics, only 1/3 of patients reach these doctors, the rest are treated for somatic manifestations of an anxiety disorder. Therefore, it is so important to contact a specialized clinic, where highly specialized doctors work, who can establish an accurate diagnosis.
Often, therapists, without revealing a somatic pathology, diagnose vegetovascular dystonia, which completely deprives the patient of the opportunity to visit a psychotherapist or psychiatrist, since the disorder is mental in nature. According to statistics, only 1/3 of patients reach these doctors, the rest are treated for somatic manifestations of an anxiety disorder. Therefore, it is so important to contact a specialized clinic, where highly specialized doctors work, who can establish an accurate diagnosis.
Causes of disease manifestation
The causes of anxiety disorder are not fully understood by experts. It is assumed that the basis of the disease is hereditary predisposition, character trait and temperament, as well as the style of education in the family.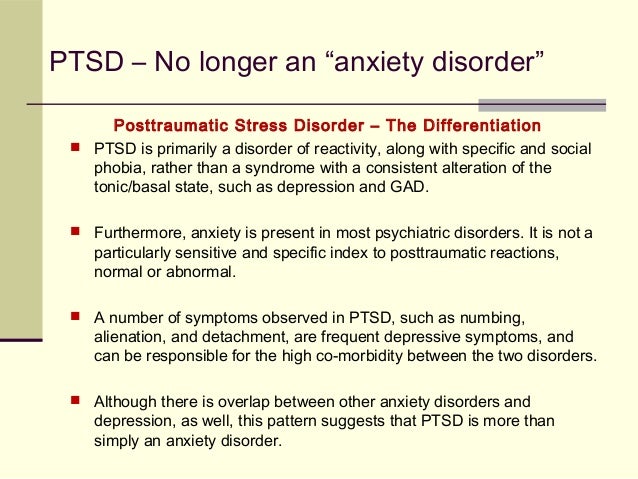 At a younger age, a person is shy, shy, withdrawn, it is difficult for him to get used to everything new. Although, in some cases, these signs are not direct indicators of the presence of an anxiety state. The timidity of a child is a natural stage in the development of his psyche, which, as he grows up, disappears without a trace.
At a younger age, a person is shy, shy, withdrawn, it is difficult for him to get used to everything new. Although, in some cases, these signs are not direct indicators of the presence of an anxiety state. The timidity of a child is a natural stage in the development of his psyche, which, as he grows up, disappears without a trace.
Sometimes an anxiety disorder manifests itself in conditions of constant criticism from others, rejection and rejection of society. The atmosphere in the family also plays a significant role.
The pathogenesis of anxiety personality disorder lies in the biological aspect. Low levels of GABA and neurotransmitters that reduce the activity of the central nervous system provoke feelings of anxiety. The amygdala plays a significant role in the processing of fear. Violation of its performance, also, can lead to an alarming state.
Stages of anxiety disorder
There are 3 main stages of anxiety:
- Anxiety stage.
 On it, a person does not realize the presence of this disorder in himself, takes it for suspiciousness. The patient regularly experiences anxiety, however, does not find anything wrong with this. In this state, a person can be a long time, until the end of life.
On it, a person does not realize the presence of this disorder in himself, takes it for suspiciousness. The patient regularly experiences anxiety, however, does not find anything wrong with this. In this state, a person can be a long time, until the end of life. - In some cases, the first stage smoothly passes into the second. Anxiety is growing, fear is already beginning to manifest itself physically - fever, chills, muscle tension, tachycardia, dizziness, weakness, nausea, loss of a sense of reality. Symptoms manifest themselves at first in a stressful situation, and then in everyday life. The second stage is accompanied by recurrent symptoms in a normal situation and increased anxiety during the day. The person is aware of his anxiety. It can be reduced at this stage by getting rid of negative emotions, using relaxation methods, and forming the right lifestyle.
- In the third stage, panic attacks join the feeling of anxiety, which can be both episodic in nature and accompany a person constantly.
 The patient also has difficulty sleeping and eating.
The patient also has difficulty sleeping and eating.
If a person has been at this stage for more than 2 years, then it gradually develops into the last stage and becomes a stable state for him. At this stage, you will need not only psychotherapy, but also medication. However, even at stage 1, a consultation with a psychotherapist is required, which will help either exclude or establish a diagnosis of an anxiety disorder, prescribe an effective treatment so that the disease does not develop further.
Types of anxiety disorder
Experts identify 9 main types of anxiety personality disorder.
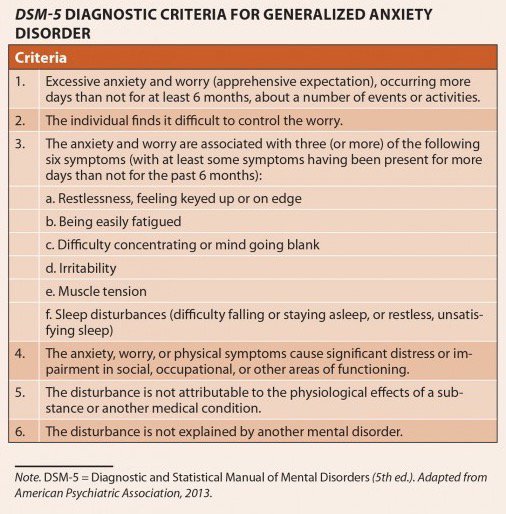
- Generalized anxiety disorder is the most common subtype of AD. Patients with this diagnosis feel constant anxiety throughout the day, worry about any household trifles.
- Phobias. This type of anxiety combines fears and anxieties associated with a particular situation. Phobias are observed in 10% of the population worldwide. The patient is terrified of the upcoming object that causes negative events in him - a place or an animal.
- Panic attacks. When they occur, a person experiences brief bouts of fear and anxiety, often accompanied by tremors in the body, dizziness, nausea, or difficulty breathing.
 Already 10 minutes after the start, they reach their peak and can last several hours. In order to be diagnosed with panic disorder, it must have chronic consequences: fear of future attacks, changes in behavior, heart palpitations. By the way, patients often confuse the latter sign with heart problems, the thought of which can cause a second panic attack.
Already 10 minutes after the start, they reach their peak and can last several hours. In order to be diagnosed with panic disorder, it must have chronic consequences: fear of future attacks, changes in behavior, heart palpitations. By the way, patients often confuse the latter sign with heart problems, the thought of which can cause a second panic attack. - Agoraphobia. Another type of anxiety disorder in which people are afraid of public places and open spaces. Agoraphobia is closely related to panic disorder and is often the result of its manifestation.
- Social anxiety disorder or social phobia usually occurs under certain circumstances, such as before public speaking. The person is embarrassed, fearful and humiliated.
 The disorder can manifest itself physically: redness, sweating, difficulty speaking. People experiencing social phobia try to avoid the source of anxiety, which often leads to complete social isolation.
The disorder can manifest itself physically: redness, sweating, difficulty speaking. People experiencing social phobia try to avoid the source of anxiety, which often leads to complete social isolation. - Post-traumatic stress disorder (PTSD) as a result of a negative event: from rape to a natural disaster. It occurs as a result of prolonged stress and is accompanied by sleep disturbance.
- Situational anxiety arising from a change in environment and changing events that makes a person uncomfortable. This type of disorder is common among a certain type of people. They may experience anxiety in crowds, dark spaces, shops, and other public places. Often this anxiety leads to panic attacks.
- Obsessive-compulsive disorder (OCD) is a condition of obsessions, thoughts, images and repeated performance of certain actions (rituals). OCD causes feelings of anxiety and impaired socialization. A person realizes the unreasonableness of his actions and tries to fight thoughts and behavior.
- selective mutism. Another type of disorder that occurs in people who are shy and have social anxiety. The disorder is manifested by the silence of a person who is able to talk, in certain situations and with certain people.
To make such a diagnosis, the patient must have at least 3 signs of the disease: anxiety, fatigue, irritability, insomnia, muscle tension, impaired concentration. The most common type of generalized anxiety disorder occurs in older people. Often, anxiety is a consequence of another disease, or occurs as a result of the use of narcotic and psychotropic substances. Outwardly, a person looks tense, he has hyperhidrosis, tearfulness, a depressive state are manifested.
Often, anxiety is a consequence of another disease, or occurs as a result of the use of narcotic and psychotropic substances. Outwardly, a person looks tense, he has hyperhidrosis, tearfulness, a depressive state are manifested.
Among the most common phobias are the fear of flying in airplanes, the sight of blood, water, heights, darkness, closed spaces, reptiles and spiders. A person is fettered by fear, the heartbeat quickens, he experiences trembling and shortness of breath at the sight of what causes horror in him. As a rule, it is impossible to overcome a phobia in a person on his own.
Sometimes the term is used to refer to avoidance behavior after a panic attack. For example, if after the next attack a person is afraid to drive a car, then he will continue to avoid doing it. Such behavior is a direct path to even greater fear.
Sequelae of anxiety disorder
Anxiety should not be left unattended. Their diagnosis, treatment and control are best entrusted to competent doctors in a specialized clinic. Among the socio-psychological complications of TR can be identified: sleep disturbance, low self-esteem, accompanying feelings of hopelessness, social isolation. Lack of energy and depressed mood do not allow a person to actively develop and change under the realities of our time. Job loss, financial difficulties, family breakup can be the consequences of such conditions and further aggravate the condition. Often, anxiety provokes the onset of depression - a condition fraught with suicidal thoughts and attempts to carry it out.
Feelings of anxiety also arise as a result of the use of drugs, alcohol or nicotine.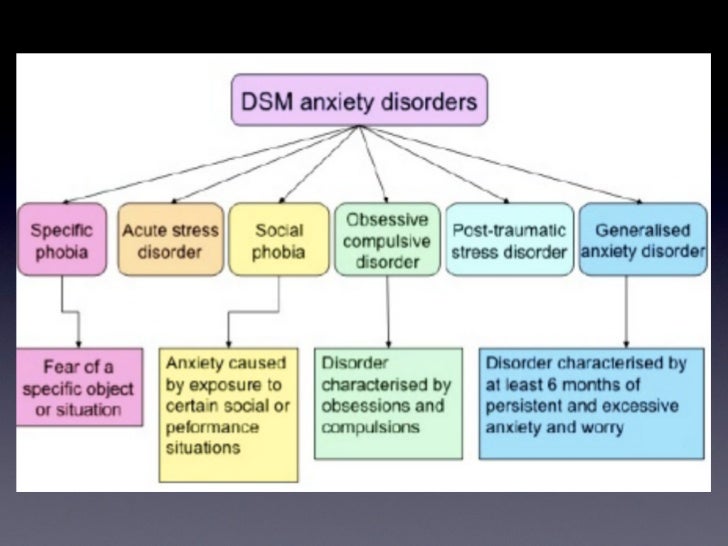
Complications of anxiety personality disorder are also physical in nature. The patient experiences pain in the intestines, heartburn, problems with stools, insomnia, migraine. Often, the disorder is accompanied by a loss of sexual interest in a partner and fluctuations in weight, a decrease in immunity and white blood cells. According to researchers, stress can also trigger the appearance of allergies and autoimmune diseases.
A constant feeling of anxiety, restlessness and insecurity is a clear sign to contact an experienced psychiatrist. Sometimes patients, due to their individual characteristics and due to illness, cannot do this. Relatives should take on this role, gently and tactfully point out to a loved one the presence of the disease. The specialist will help to overcome psycho-emotional dependence and restore strength.
Diagnostics
The diagnosis of anxiety disorder is difficult due to the lack of specific biomarkers. In order to detect anxiety symptoms, the specialist conducts a conversation with the patient and special psychological testing using the Beck Anxiety Scale, the Tsung Self-Assessment Anxiety Scale, and the Taylor Anxiety Scale.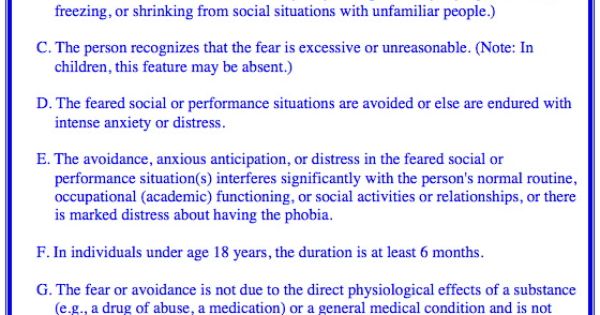
The criteria for making a diagnosis are the following persistent signs that haunt the patient for a long time:
- social awkwardness;
- belittling one's own value;
- internal tension;
- restriction in social communication for fear of criticism and disapproval.
The treatment of this disorder is carried out by a psychotherapist who, if necessary, will prescribe a consultation with a psychiatrist. Anxiety disorders sometimes occur along with depression, while sharing the same symptomatology.
According to studies, anxiety disorders often occur in those people whose relatives have also been diagnosed with such a diagnosis. The disorder is sometimes accompanied by a sexual disorder or arises from a common mass of causes. This is especially true in patients with panic disorder.
When making a diagnosis, first of all, it is necessary to exclude a medical pathology with similar symptoms:
- endocrine diseases;
- metabolic dysfunction;
- deficiency of vitamin D and folic acid;
- diseases of the gastrointestinal tract, blood and heart;
- dementia, sclerosis and other brain diseases.
Anxiety Personality Disorder Treatment
The goal of treatment is to reduce the level of anxiety and improve the quality of life of the patient. The doctor, with the help of special psychoanalytic techniques, helps a person to realize the presence of a disorder and understand the reasons that prompted him.
Some of the most effective treatments for anxiety disorder symptoms include:
- Cognitive behavioral therapy, which aims to change the patient's thinking and behavior. A psychotherapist in the course of therapy helps a person not only to detect this disorder and identify its causes, but also to form new thinking, teach how to communicate with people and form adaptive patterns of behavior.
- Family therapy. The family plays a significant role in the treatment of any mental illness, especially when it comes to a child or adolescent. Family therapy is aimed at identifying problems in the family and methods of dealing with them, eliminating negative factors that contribute to the development of an anxiety disorder.
- Medical therapy. Your doctor may prescribe antidepressants and benzodiazepines, psychoactive drugs that have sedative and sedative effects.
In no case should you use drugs on your own. They are selected individually and only as prescribed by a doctor, after a thorough examination and identification of symptoms of an anxiety disorder.
+7 (495) 121-48-31
Prevention of Anxiety Personality Disorder
With anxiety attacks, the patient should try to cope on their own. To do this, you can perform certain breathing exercises, belly breathing, nostril breathing techniques and mindfulness "here and now" techniques.
Among the main recommendations of an anxious personality disorder is a change in the patient's lifestyle. This is a set of measures aimed at eliminating negative factors that provoke anxiety:
- Physical exercises.
- Observance of sleep and rest.
- Reducing caffeine intake.
- Rejection of bad habits.