Hallucinations and delusions in schizophrenia
Schizoprenia: Understanding Hallucinations and Delusions
Schizophrenia
Learn how to recognize the varying types of halluncinations and delusions that are among the most common symptoms of schizophrenia
Kathleen Smith, PhD, LPC
Medical ReviewerRandy Bressler, PsyD
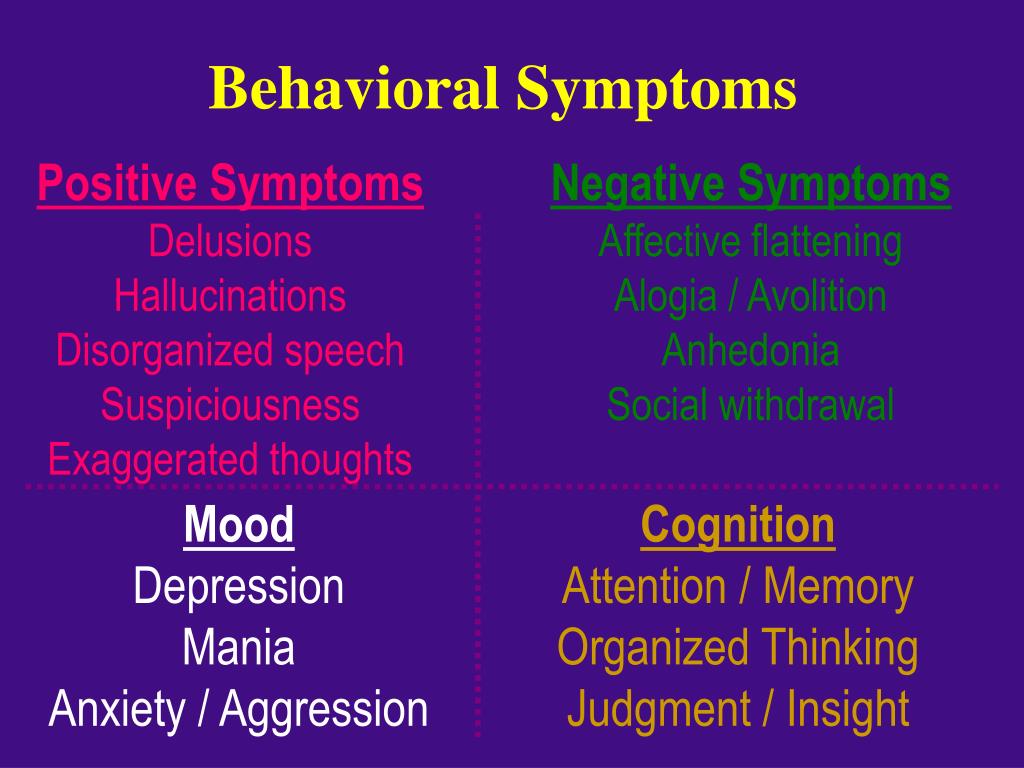
Hallucinations and delusions are among the most common symptoms of schizophrenia. Both are considered positive symptoms, meaning they are not seen in healthy people.
Though the words are sometimes used interchangeably, each is a different experience.
Hallucinations are defined as experiences and sensations that are not perceivable to others. To the person experiencing them, however, they may seem real, urgent, and vivid. Roughly 70% of people with schizophrenia will experience hallucinations.
Auditory hallucinations are most commonly experienced by people with schizophrenia and may include hearing voices—sometimes multiple voices—or other sounds like whispering or murmuring. Voices may seem angry or urgent and often make demands on the hallucinating person.
Visual hallucinations involve seeing objects, people, lights, or patterns that are not actually present. Visualizing dead loved ones, friends, or other people they knew can be particularly distressing. Perception may be altered as well, resulting in difficulty judging distance.
Olfactory hallucinations involve the sense of smell or taste, both good or bad, that are not actually present. This can be particularly dangerous if a person believes he is being poisoned and refrains from eating.
Tactile hallucinations are feelings of movement or sensation on your body that are not actually present, such as hands on your body or insects crawling around or inside you.
Having hallucinations, in and by itself, does not indicate schizophrenia. People with mood disorders, schizoaffective disorders, other mental health conditions, and neurodegenerative diseases such as Alzheimer's and Parkinson's may also hallucinate.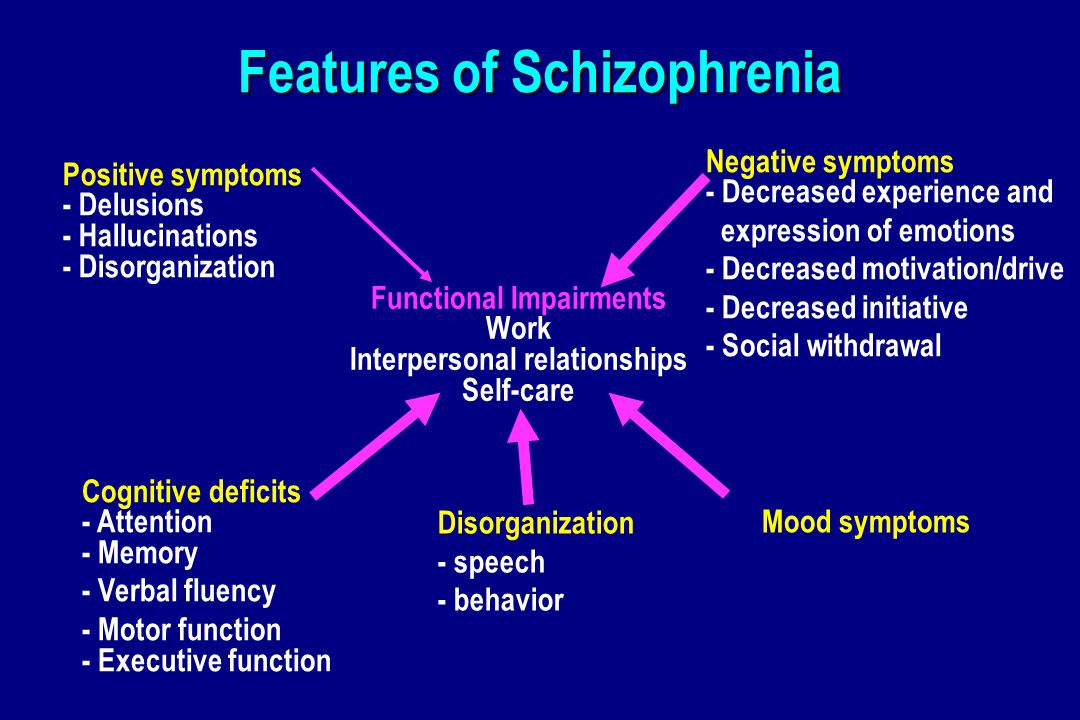 Hallucinations can occur when falling asleep (known as hypnagogic hallucinations) or when awaking (known as hypnopompic hallucinations). Those who consume psychoactive substances such as alcohol, marijuana, cocaine, and LSD may also experience sensory disturbances.
Hallucinations can occur when falling asleep (known as hypnagogic hallucinations) or when awaking (known as hypnopompic hallucinations). Those who consume psychoactive substances such as alcohol, marijuana, cocaine, and LSD may also experience sensory disturbances.
Delusions are defined as beliefs that conflict with reality. Delusions are one of the most common symptoms of schizophrenia. These beliefs might include:
Persecutory delusions: When a person believes a person, group, or organization is mistreating or harming them despite contradictory evidence.
Erotomanic delusions: When a person believes another is in love with them, despite no evidence. This other person is often a celebrity or person in power.
Somatic delusions: When a person believes they have an illness or their body is affected by a strange condition, despite contradictory evidence.
Grandiose delusions: When a person believes they have superior abilities or qualities (i.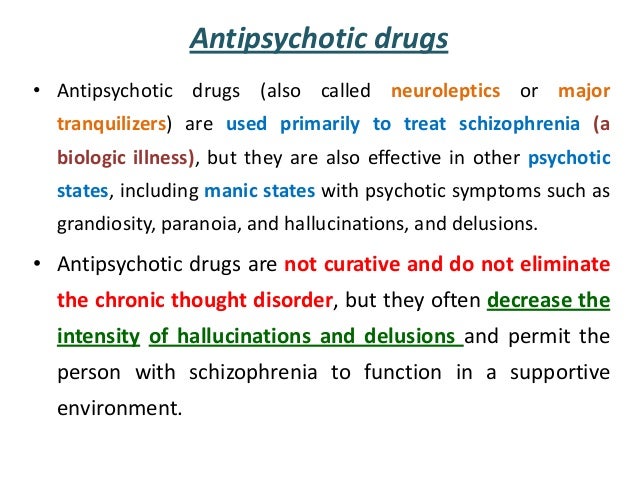 e. talent, fame, wealth) despite no evidence.
e. talent, fame, wealth) despite no evidence.
Sometimes a person will experience a recurring theme in their delusions over a period, which makes them seem more convincing to the individual experiencing them.
Try to stay calm and avoid feeling overwhelmed, confused, or fearful of someone experiencing hallucinations or delusions. A tranquil disposition can help the individual connect to reality. Here are some additional tips:
Encourage openness
Our understanding of hallucinations and delusions suggests that they can be triggered by a wide range of conditions. For those who experience them, they may feel shame and/or fear, which can make a productive conversation challenging. Try gently explaining that you cannot see or hear what they are experiencing and need help understanding it.
Be patient
Try to be sympathetic. Hallucinating is a very consuming experience. Speak slowly and clearly and frequently use the person’s name. Managing your own anxiety will encourage the hallucinating person to be more responsive.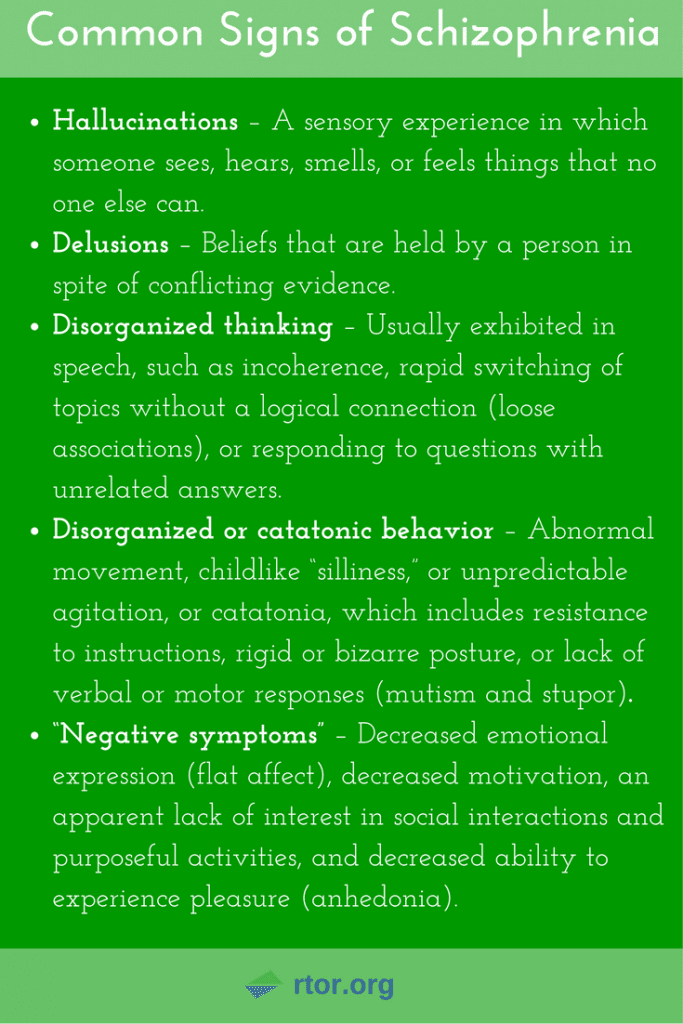
Reinforce reality
Don’t argue with the hallucinations or deluded observations. It isn’t useful to challenge the person who is struggling. Instead, refrain from being judgmental; work to stay engaged, talking with a calm voice and making concerted efforts to understand what the person is experiencing; express to them that you each have your own perceptions of the world; do not focus on correcting their psychotic thinking or encourage their distorted reality; and emphasize that you are there as a support and can get help, if need be.
Ask for help
If you feel ill-equipped to help someone experiencing psychosis, get help. Find out if there is a trusted friend, family member, community resource, or mental health expert/health care provider that is monitoring their care, whom you can reach out to. If safety is a concern, whether it involves you or the one who is experiencing thought disturbances, call 911 or, if you feel safe, bring them to an emergency room at your local medical center.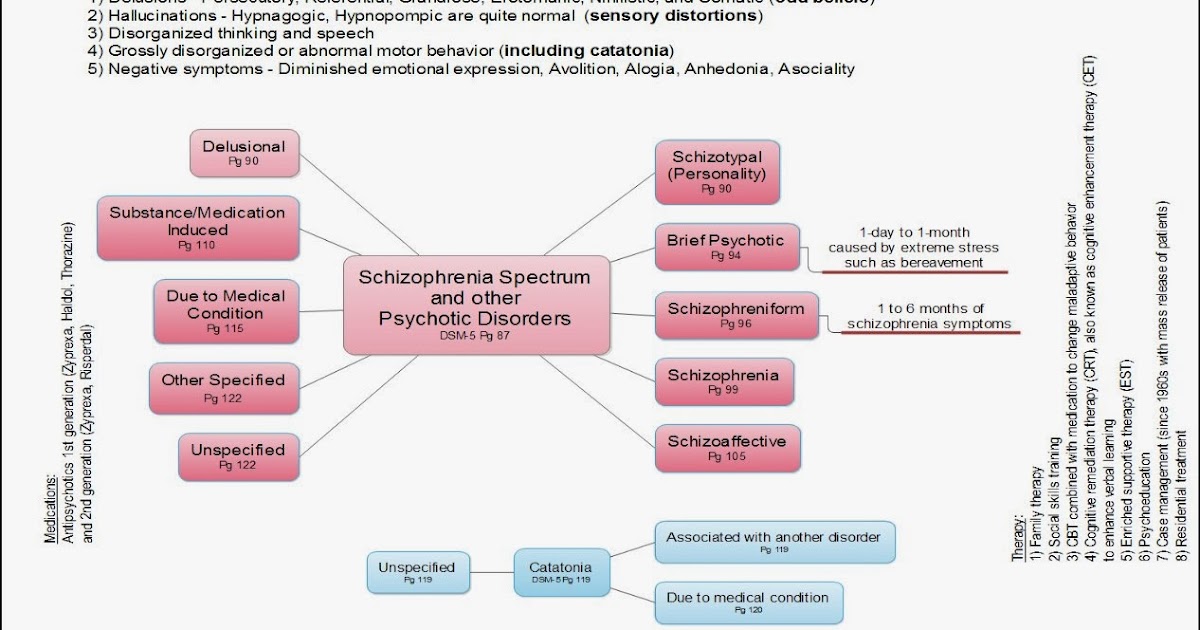
Helpful online resources include the National Institute of Mental Health, National Alliance on Mental Illness (NAMI) (which also offers support groups and other in-person resources), and The Child Mind Institute.
Hallucination and delusion can be scary to witness, but medication, therapy, psychoeducation, and family support can make a difference. The symptoms may never disappear completely, but people plagued by these problems can learn to manage them. If you know someone with schizophrenia, seek out more education and training to help your loved one cope and even thrive with schizophrenia.
- https://www.livingwithschizophreniauk.org/symptoms-of-schizophrenia/
- http://www.nytimes.com/health/guides/disease/schizophrenia/print.html
- https://medlineplus.gov/ency/article/003258.htm
Notes: This article was originally published November 28, 2017 and most recently updated September 14, 2022.
Schizophrenia - Symptoms and causes
Overview
Schizophrenia is a serious mental disorder in which people interpret reality abnormally.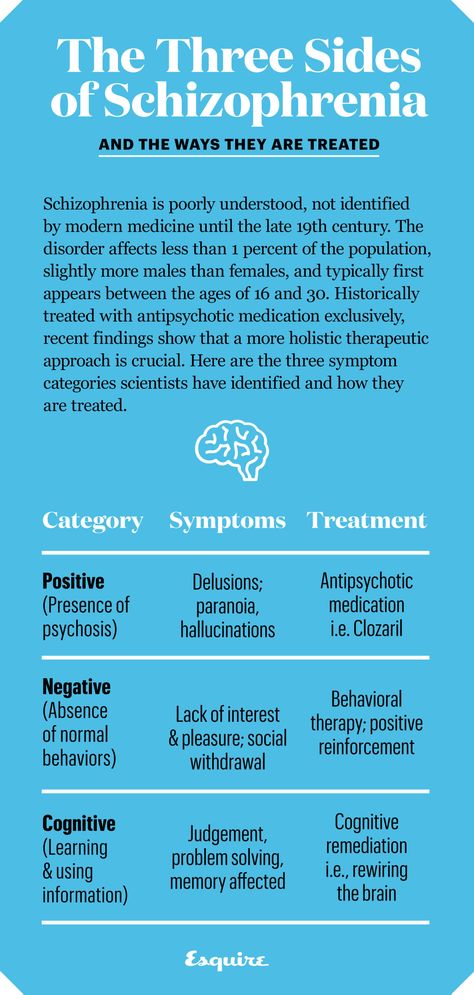 Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
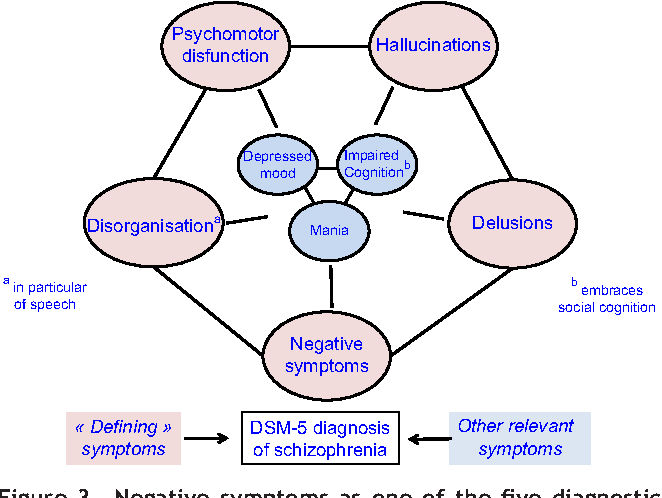
Schizophrenia involves a range of problems with thinking (cognition), behavior and emotions. Signs and symptoms may vary, but usually involve delusions, hallucinations or disorganized speech, and reflect an impaired ability to function. Symptoms may include:
- Delusions. These are false beliefs that are not based in reality. For example, you think that you're being harmed or harassed; certain gestures or comments are directed at you; you have exceptional ability or fame; another person is in love with you; or a major catastrophe is about to occur.
 Delusions occur in most people with schizophrenia.
Delusions occur in most people with schizophrenia. - Hallucinations. These usually involve seeing or hearing things that don't exist. Yet for the person with schizophrenia, they have the full force and impact of a normal experience. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganized thinking (speech). Disorganized thinking is inferred from disorganized speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated. Rarely, speech may include putting together meaningless words that can't be understood, sometimes known as word salad.
- Extremely disorganized or abnormal motor behavior. This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement.
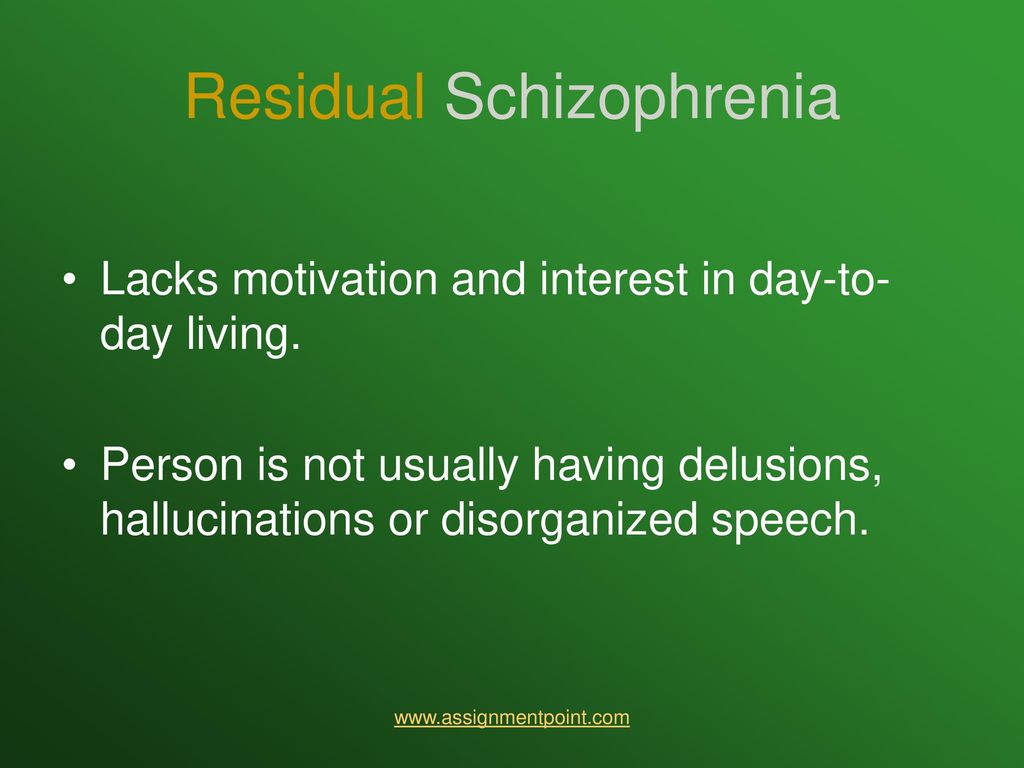
- Negative symptoms. This refers to reduced or lack of ability to function normally. For example, the person may neglect personal hygiene or appear to lack emotion (doesn't make eye contact, doesn't change facial expressions or speaks in a monotone). Also, the person may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Symptoms can vary in type and severity over time, with periods of worsening and remission of symptoms. Some symptoms may always be present.
In men, schizophrenia symptoms typically start in the early to mid-20s. In women, symptoms typically begin in the late 20s. It's uncommon for children to be diagnosed with schizophrenia and rare for those older than age 45.
Symptoms in teenagers
Schizophrenia symptoms in teenagers are similar to those in adults, but the condition may be more difficult to recognize. This may be in part because some of the early symptoms of schizophrenia in teenagers are common for typical development during teen years, such as:
- Withdrawal from friends and family
- A drop in performance at school
- Trouble sleeping
- Irritability or depressed mood
- Lack of motivation
Also, recreational substance use, such as marijuana, methamphetamines or LSD, can sometimes cause similar signs and symptoms.
Compared with schizophrenia symptoms in adults, teens may be:
- Less likely to have delusions
- More likely to have visual hallucinations
When to see a doctor
People with schizophrenia often lack awareness that their difficulties stem from a mental disorder that requires medical attention. So it often falls to family or friends to get them help.
Helping someone who may have schizophrenia
If you think someone you know may have symptoms of schizophrenia, talk to him or her about your concerns. Although you can't force someone to seek professional help, you can offer encouragement and support and help your loved one find a qualified doctor or mental health professional.
If your loved one poses a danger to self or others or can't provide his or her own food, clothing, or shelter, you may need to call 911 or other emergency responders for help so that your loved one can be evaluated by a mental health professional.
In some cases, emergency hospitalization may be needed. Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and behavior are common among people with schizophrenia. If you have a loved one who is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you.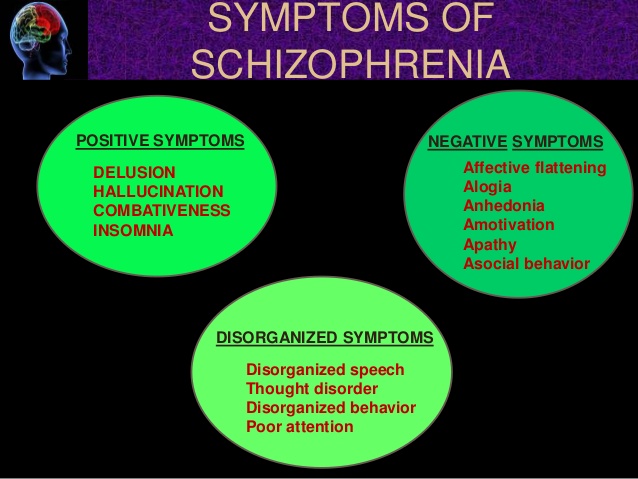 If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
It's not known what causes schizophrenia, but researchers believe that a combination of genetics, brain chemistry and environment contributes to development of the disorder.
Problems with certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neuroimaging studies show differences in the brain structure and central nervous system of people with schizophrenia.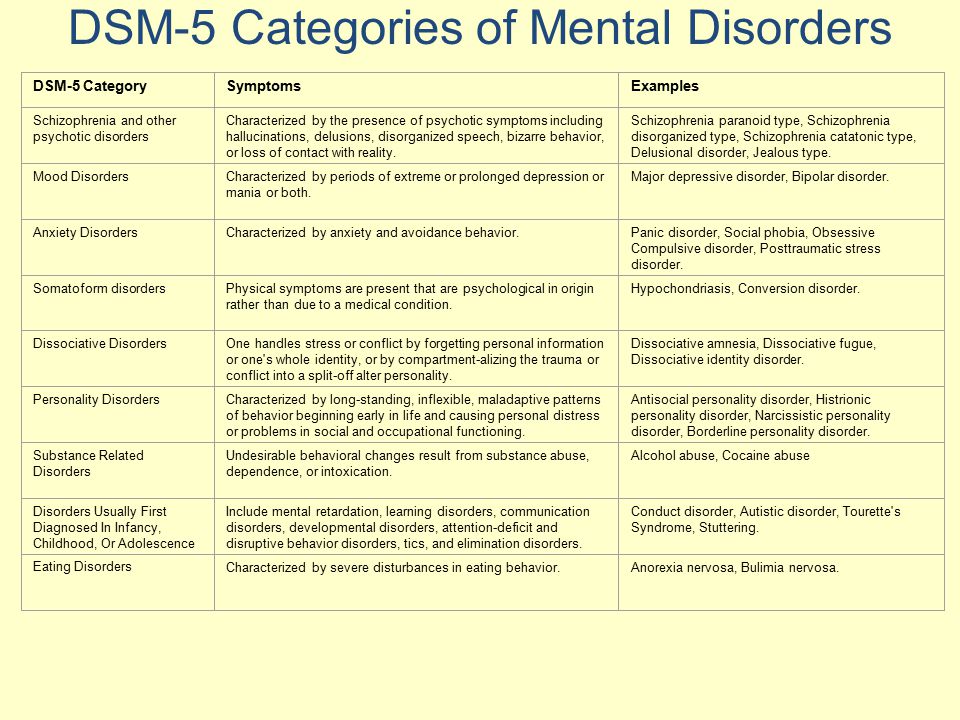 While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
Risk factors
Although the precise cause of schizophrenia isn't known, certain factors seem to increase the risk of developing or triggering schizophrenia, including:
- Having a family history of schizophrenia
- Some pregnancy and birth complications, such as malnutrition or exposure to toxins or viruses that may impact brain development
- Taking mind-altering (psychoactive or psychotropic) drugs during teen years and young adulthood
Complications
Left untreated, schizophrenia can result in severe problems that affect every area of life. Complications that schizophrenia may cause or be associated with include:
- Suicide, suicide attempts and thoughts of suicide
- Anxiety disorders and obsessive-compulsive disorder (OCD)
- Depression
- Abuse of alcohol or other drugs, including nicotine
- Inability to work or attend school
- Financial problems and homelessness
- Social isolation
- Health and medical problems
- Being victimized
- Aggressive behavior, although it's uncommon
Prevention
There's no sure way to prevent schizophrenia, but sticking with the treatment plan can help prevent relapses or worsening of symptoms.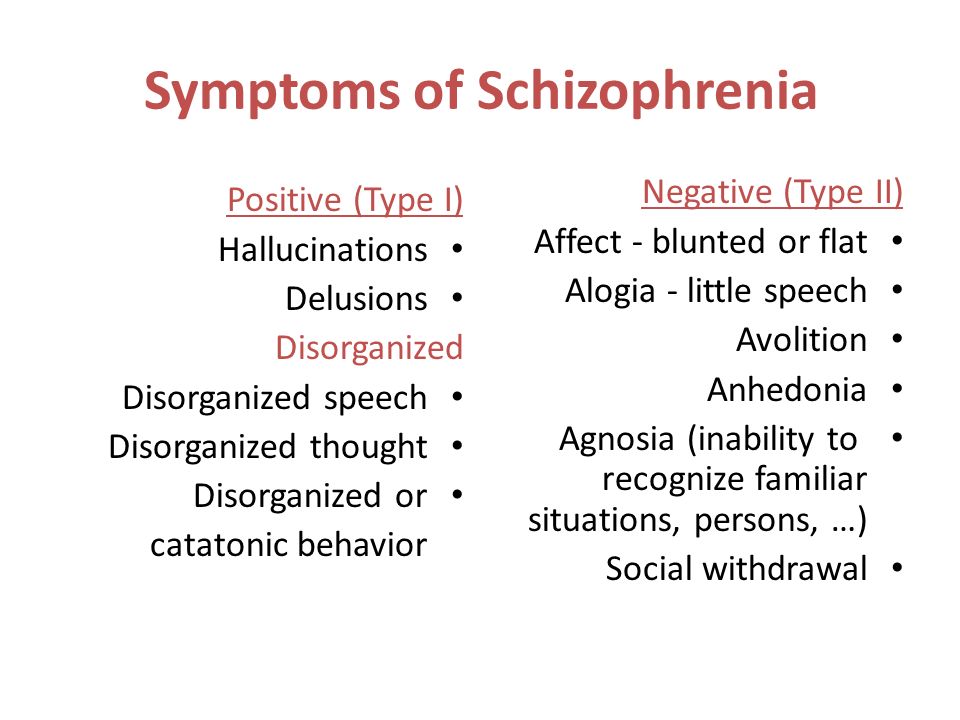 In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
PKB No. 5 - Schizophrenia
Moscow State Budgetary Institution of Healthcare
Psychiatric Clinical Hospital No. 5 of the Moscow City Health Department
+7 (495) 445-55-25, +7 (496) 724-33 -33
Moscow region, Chekhov, s. Troitskoe, 5
Medical Tourism
Site search
Schizophrenia is a chronic mental illness, which is characterized by a violation of the unity of thought processes, with a relatively intact intellect, which is combined with significant emotional impoverishment and a decrease in will.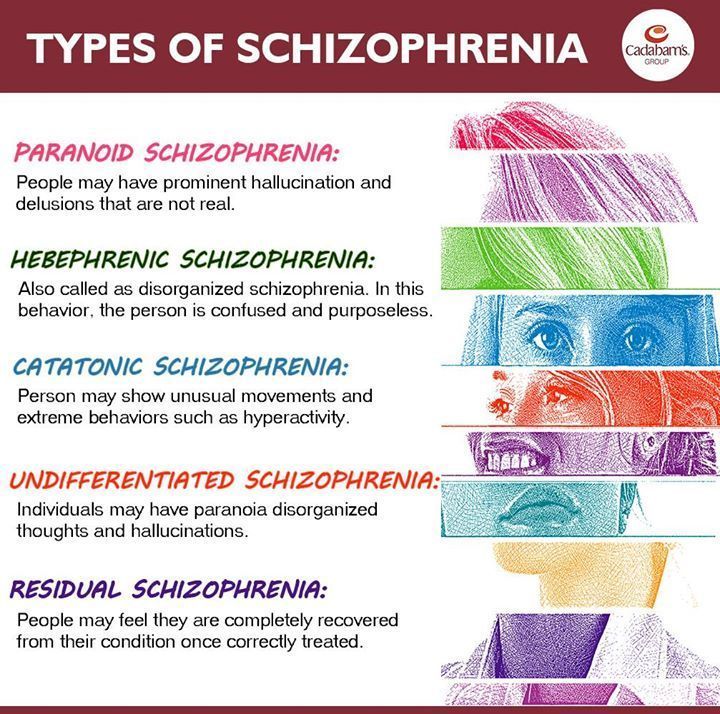 Often hallucinatory and delusional disorders join.
Often hallucinatory and delusional disorders join.
The term "schizophrenia" itself is made up of two Greek words - "schizo" - splitting and "freni" - mind reason.
This term was first used by the Swiss psychiatrist Eigen Bleuler in 1908y. Schizophrenia, of course, existed before, but only by the beginning of the 20th century did the idea of it as a special kind of psychosis mature.
In the mass consciousness there is an unreasonable identification of schizophrenia with a "split personality" - that is, in fact, with a very rare mental disorder in which different "I"s are alternately activated in one person.
Schizophrenia, unfortunately, is quite common. Its prevalence among the Russian population is 35 per 10,000 people, with no significant difference between the sexes. Thus, in Russia there are at least half a million patients with this serious pathology.
Schizophrenia refers to endogenous mental illness, which means that it is an internal breakdown of the psyche.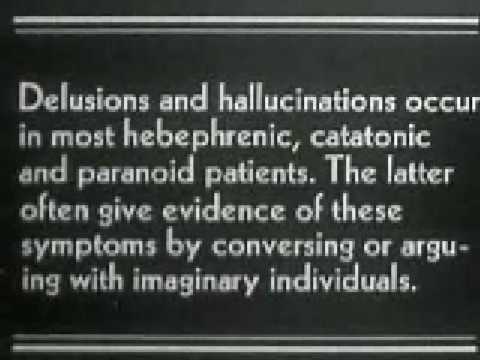 It cannot be caused by any factors acting on the brain from the outside (trauma, intoxication, severe stress). Of course, these factors can affect the rate of development of schizophrenia, but not its occurrence. However, the mechanism of development of the schizophrenic process has not yet been established with certainty. There are several hypotheses about this. Thus, there is evidence of a relationship between schizophrenia and a violation of the distribution of dopamine in the central nervous system.
It cannot be caused by any factors acting on the brain from the outside (trauma, intoxication, severe stress). Of course, these factors can affect the rate of development of schizophrenia, but not its occurrence. However, the mechanism of development of the schizophrenic process has not yet been established with certainty. There are several hypotheses about this. Thus, there is evidence of a relationship between schizophrenia and a violation of the distribution of dopamine in the central nervous system.
The role of heredity is very great. So, if one of the twins fell ill with schizophrenia, then the risk of getting sick for the other twin is 17% in a fraternal couple and 48% in an identical one. However, it is believed that in half of the cases of schizophrenia arises from a random mutation, that is, on the basis of genetic changes that were absent in the parents and appeared after conception.
Symptoms can develop at any age (possibly even in utero), but usually its onset is timed to coincide with the third pubertal crisis, that is, by the age of 12-18 years or several years later (up to about 30 years).
Most often, the disease begins with negative symptoms associated with the loss of normal functioning - a person changes in character for no apparent reason, becomes closed, fenced off, loses social contacts, emotional warmth in relation to relatives disappears. Former interests disappear, school or university performance drops sharply, or official duties are not fulfilled. Thus, from the very beginning of clinical manifestations there is a very high risk of disability. In the most unfavorable variant, which is designated as simple schizophrenia, the patient can lie for days on end, staring at the ceiling, and with a clear mind and normal physical strength, he is not able to simply serve himself. Even with more favorable options, thinking disorders increase, which are expressed in the influx of thoughts or in the feeling that there are no thoughts at all. Reasoning becomes unproductive, unfocused, an ambivalent attitude to life phenomena (ambivalence) is formed. Speech is distinguished by ornateness, sometimes with neologisms that the patient himself comes up with.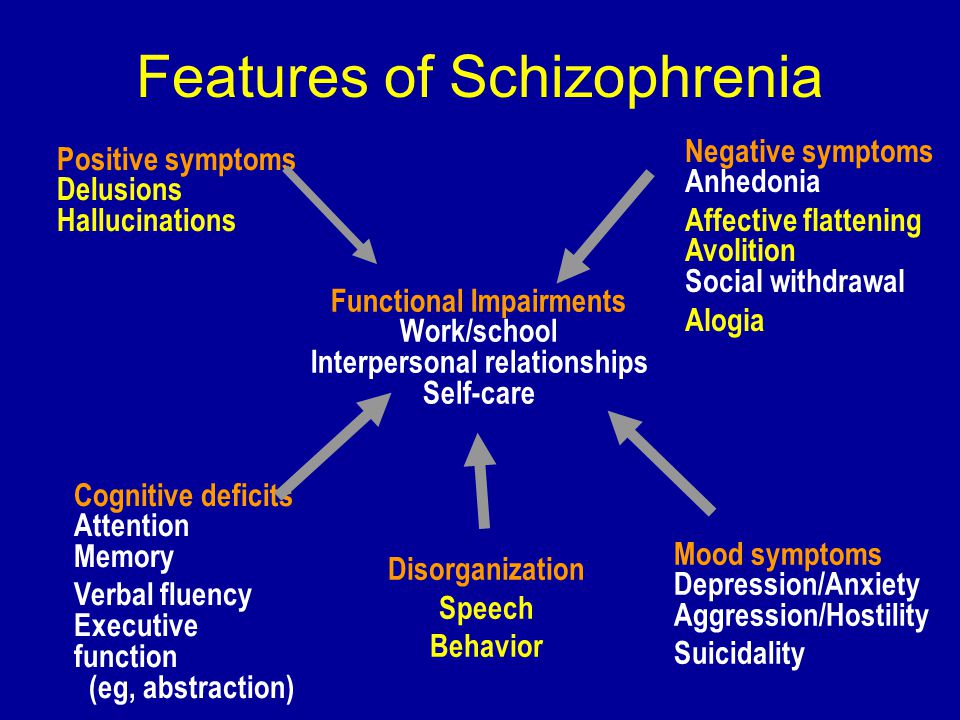 During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics. People with schizophrenia tend to be somewhat cynical about many aspects of their environment.
During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics. People with schizophrenia tend to be somewhat cynical about many aspects of their environment.
Patients have a painful feeling that everything around is somehow changed, devoid of naturalness, harmony (- derealization), the same feelings can arise in relation to their personality (- depersonalization). With depersonalization, the consciousness (but not the personality!) seems to split in two: one part of it looks at what is happening from the side, and the other is horrified by the realization of the loss of control over oneself.
One's own thoughts and ideas begin to be perceived as alien. According to modern views, this is why schizophrenia has verbal hallucinations (“voices”), and it is not surprising that the sound of “voices” inside the head is typical for this disease. For the same reason, it seems to the patient that someone controls him from the outside, up to the control of movements and the work of internal organs. Visions are less common.
For the same reason, it seems to the patient that someone controls him from the outside, up to the control of movements and the work of internal organs. Visions are less common.
Such a growing wave of unusual sensations is very painful. In many cases, internal tension is somewhat relieved by the formation of delusional ideas (quickly - like an insight - the crystallization of delirium occurs). It suddenly becomes “clear” to the patient that what is happening to him is, for example, the “intrigues” of some “organization”, which, with the help of modern equipment, “influences” him from the outside (delusions of persecution, influence). There is also delusions of jealousy, damage. It is clear that the plot of experiences is influenced by the level of development of society, including the plots of popular works of literature and cinema.
This whole clinical picture often develops acutely, in the form of an attack that lasts from several days to several months, and then may recur.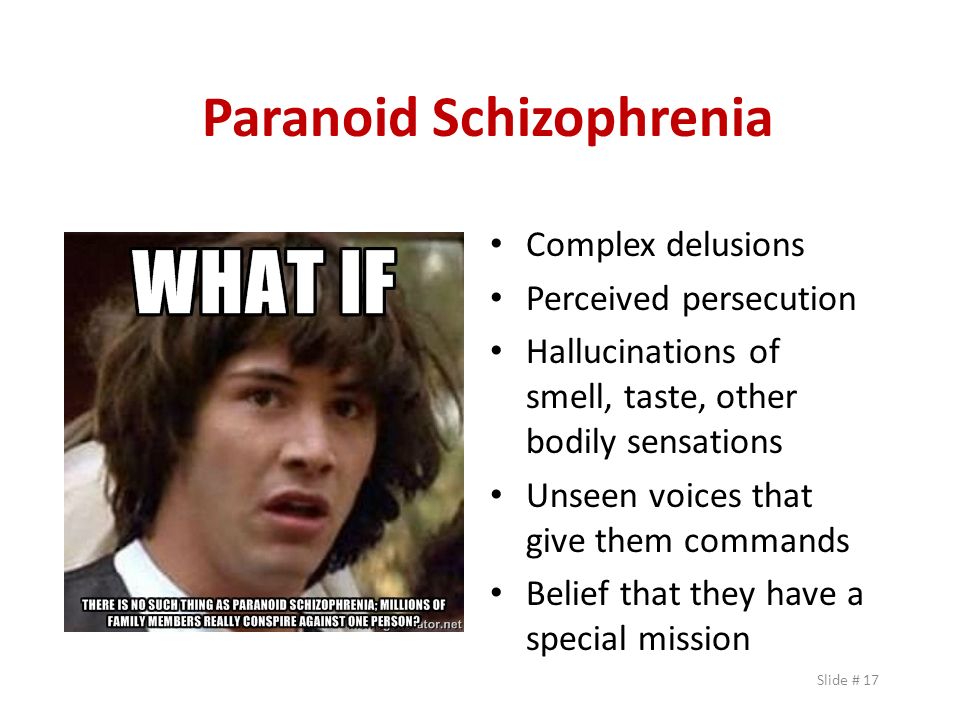 Attack-like forms of schizophrenia are more favorable, in terms of prognosis, than continuous ones. The intervals between attacks are very long (sometimes - tens of years), and between them the person looks almost the same as before, before the illness. But this is rather an exception. Much more often, exacerbations of symptoms are repeated annually or several times a year, and after each new attack, it turns out that the will has become even weaker and emotions have faded even more. Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia.
Attack-like forms of schizophrenia are more favorable, in terms of prognosis, than continuous ones. The intervals between attacks are very long (sometimes - tens of years), and between them the person looks almost the same as before, before the illness. But this is rather an exception. Much more often, exacerbations of symptoms are repeated annually or several times a year, and after each new attack, it turns out that the will has become even weaker and emotions have faded even more. Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia.
Patients either do not recognize themselves as ill or have conflicting thoughts about it. As a rule, they negatively meet the persuasion of relatives about the need to contact a psychiatrist. There are attempts to alleviate their condition with alcohol and drugs, which only complicates the clinical picture and leads to further social maladaptation.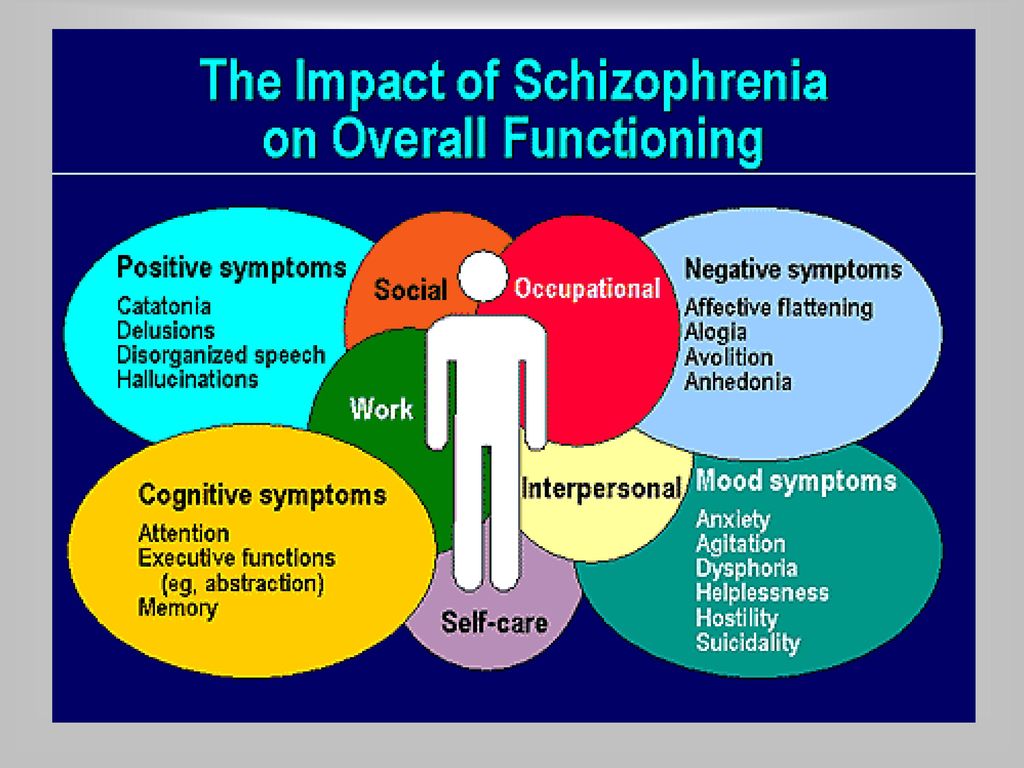
Under the influence of orders "voices" and against the background of delusional experiences, the risk of socially dangerous actions of patients increases. For example, cases of attacks on imaginary "persecutors" are known. But much more often, patients with endogenous mental pathology commit OOD through other mechanisms, including when their behavior is influenced by alcohol or drug intoxication, which is superimposed on negative symptoms.
Schizophrenia is the most common disease among patients in the Clinical Hospital No. 5 in Moscow.
Common diagnosis: Paranoid schizophrenia, episodic course with progressive defect, incomplete remission. The clinical picture with this diagnosis includes delusions and hallucinations (usually delusions of persecution and verbal hallucinations - "voices").
Treatment of schizophrenia includes antipsychotics, antidepressants, nootropics. The leading role belongs to antipsychotics, the action of which is aimed primarily at combating delusions and hallucinations.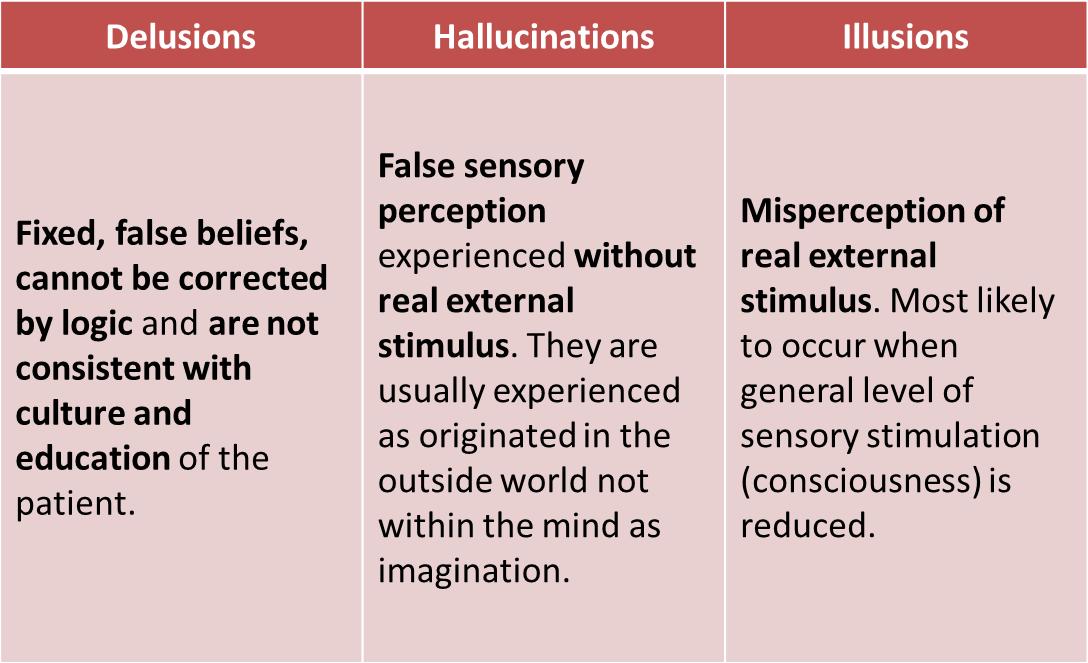 Against the background of treatment, at first, as a rule, the patient's affective reaction to his own experiences is dulled - he becomes calmer, psychomotor agitation passes. Then the hallucinations decrease in intensity or completely disappear. All these positive changes become noticeable already in the first days of the use of neuroleptics. But the plot (that is, the plot) of delirium can linger for a long time, although in the picture of internal experiences it fades significantly in relevance. After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization.
Against the background of treatment, at first, as a rule, the patient's affective reaction to his own experiences is dulled - he becomes calmer, psychomotor agitation passes. Then the hallucinations decrease in intensity or completely disappear. All these positive changes become noticeable already in the first days of the use of neuroleptics. But the plot (that is, the plot) of delirium can linger for a long time, although in the picture of internal experiences it fades significantly in relevance. After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization.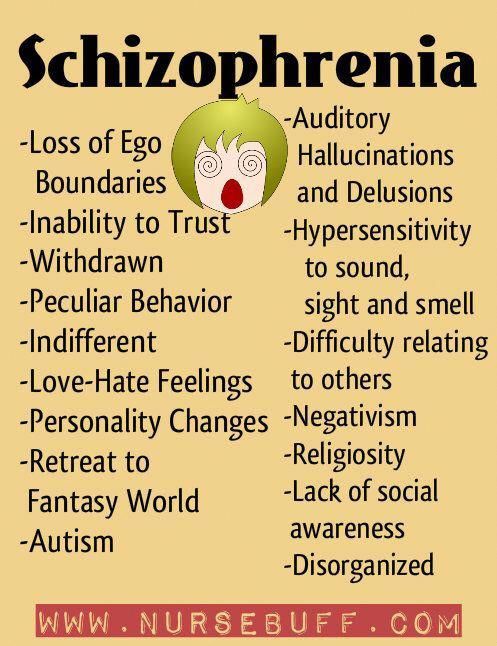 A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect.
A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect.
Although schizophrenia is a very formidable disease, it is not a death sentence. Due to the partial preservation of certain abilities (especially intellectual ones) and non-standard thinking, many of these patients have significant creative potential, which can be seen, among other things, from the works presented at the Ariadne's Thread festival of arts.
- Back
- Forward
- Are you here:
- Main page GBUZ "PKB No. 5 DZM" /
- For visitors /
- About mental disorders /
- Schizophrenia
Schizophrenia in children and adolescents
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
Fantasy has the best team of doctors!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate safety of treatment
We have made children's medicine safe! All our staff work according to the strictest international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception.