Are all antidepressants ssris
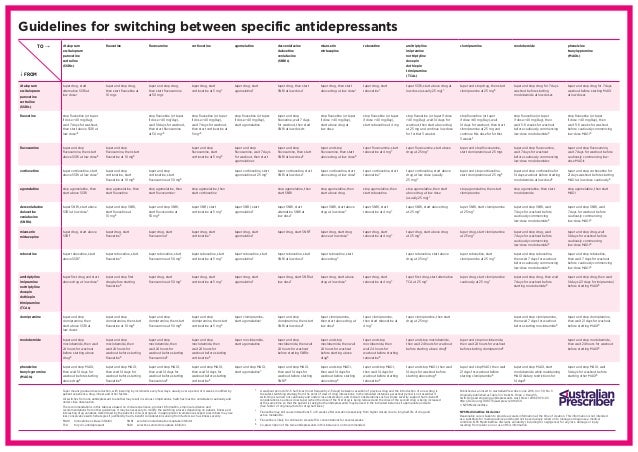
SSRI Alternatives: Other Options for Treating Depression
Medically reviewed by Kristin Hall, FNP
Written by Our Editorial Team
Last updated 11/10/2020
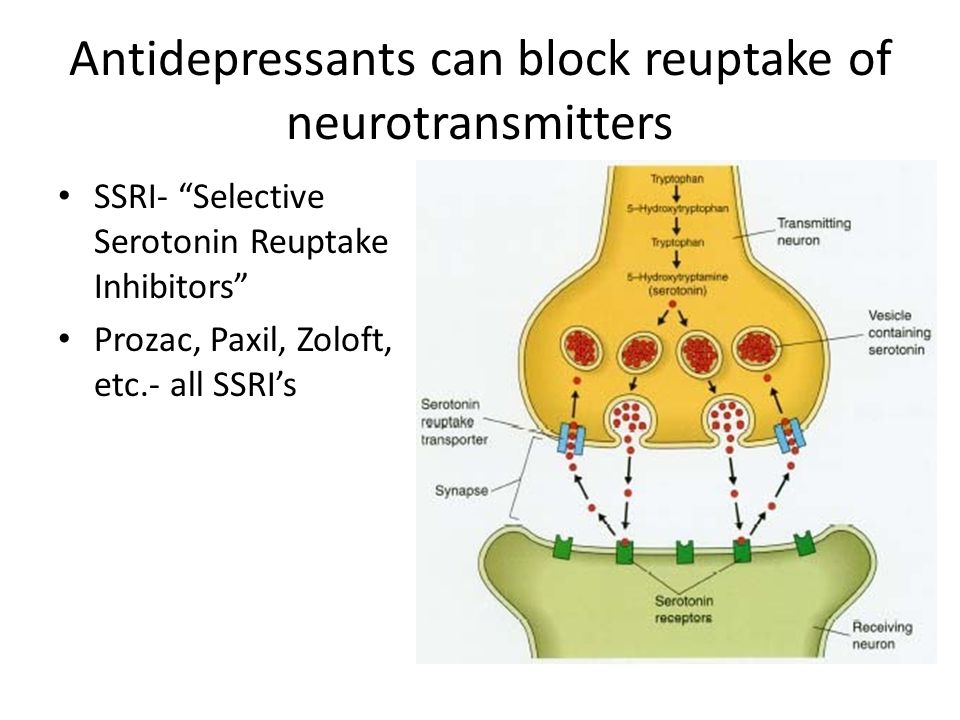
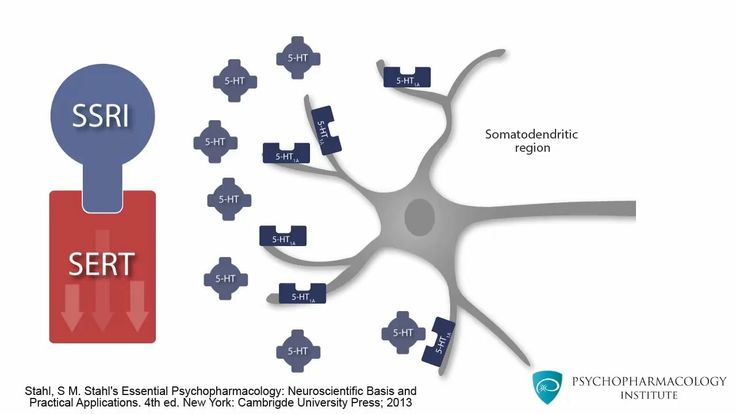
Selective serotonin reuptake inhibitors, commonly referred to as SSRIs, are some of the most widely prescribed medications in the United States.
SSRIs are primarily to treat depression. They work by increasing the level of serotonin in your brain and body. Serotonin plays an essential role in regulating your mood, and people with low levels of serotonin are often affected by depression.
For most people with depression or anxiety, SSRIs are a safe, effective form of treatment that produce real, noticeable results. However, not everyone with depression or anxiety gets good results from SSRIs.
For some people, SSRIs can cause side effects. For others, using an SSRI might not produce any significant improvement in their depression or anxiety symptoms.
Luckily, alternatives to SSRIs are available. From other antidepressants to psychotherapy and lifestyle changes, there are numerous SSRI alternatives that can allow you to treat depression or anxiety without using medications of this type.
Below, we’ve provided a complete list of SSRI alternatives for people affected by depression or anxiety disorders. We’ve also explained how each option works, its advantages, disadvantages, potential side effects and more.
When Shouldn’t You Use an SSRI?
Before getting into SSRI alternatives, it’s important to explain why you may not want to use an SSRI if you’ve been diagnosed with a form of depression or anxiety.
SSRIs are antidepressants. Although most people associate SSRIs with depression, they can actually be used to treat several other conditions, including several common anxiety and mood disorders.
Although most SSRIs are generally safe and effective, they’re not always the best option if you have depression, anxiety or a mood disorder. Common downsides of SSRIs include:
Side effects.
 Although SSRIs are generally less likely to cause side effects than older antidepressants, side effects are still quite a common experience for some people who use SSRIs to treat depression or anxiety.
Although SSRIs are generally less likely to cause side effects than older antidepressants, side effects are still quite a common experience for some people who use SSRIs to treat depression or anxiety.
As we’ve covered in our full guide to SSRIs, common SSRI side effects include nausea, agitation, anxiety and dizziness. Although these are often temporary, it’s possible for some SSRI side effects to persist or become overly severe.
The risk of side effects can vary significantly from one SSRI to another. However, if you are prone to side effects from SSRIs, it’s completely understandable that you may want to use a different type of medication.Drug interactions. SSRIs can interact with other medications. While some interactions aren’t serious, others can be life-threatening. For example, SSRIs can cause serotonin syndrome — a dangerous reaction — when used with other serotonin-affecting drugs.
Medications that can interact with SSRIs include other antidepressants, blood thinning medications, nonsteroidal anti-inflammatory drugs (NSAIDs) and others.
Withdrawal symptoms. Like many other medications, SSRIs and other antidepressants may cause withdrawal symptoms if they’re stopped abruptly. These are often referred to as antidepressant discontinuation syndrome.
Suicide risk. Although the potential suicide risk of antidepressants subject is subject to some scientific controversy, SSRIs and other antidepressants come with a warning from the FDA noting of their risk of causing suicidal thoughts or behavior in young people.
This risk is present in people aged 24 and under. It’s worth noting that this warning can be found on the packaging for all antidepressants, not only SSRIs, meaning that using one antidepressant over another may not affect the risk of suicidal actions.
If you’re at risk of any of the issues listed above, using an SSRI may not be the most effective option for you. However, if you’re currently prescribed an SSRI, you should always check with your healthcare provider before making any changes to your current medication usage.
Finally, some people simply don’t find SSRIs effective. Approximately one third of people who use antidepressants notice something known as “breakthrough depression” — a return of their depression symptoms after a period of their medication working normally.
Others simply don’t notice an improvement at all. In fact, according to data from Northwestern University, about half of all people who use antidepressants don’t experience noticeable relief from depression.
online mental health assessment
your mental health journey starts here
Alternatives to SSRIs
SSRIs aren’t the only option for treating depression and anxiety disorders. Other options may include psychotherapy, medications other than SSRIs and changes to your lifestyle and habits that help to minimize or manage your symptoms.
Other Antidepressants
If you have depression, other, non-SSRI antidepressants may be able to provide similar relief from your depression symptoms and help you work towards a long-term recovery. Non-SSRI antidepressants include:
Non-SSRI antidepressants include:
Serotonin–norepinephrine reuptake inhibitors (SNRIs). These medications function similarly to SSRIs, but also increase the level of the neurotransmitter norepinephrine in your brain. Norepinephrine is believed to affect your body’s response to stress.
Common SNRIs include venlafaxine (sold as Effexor®), duloxetine (Cymbalta®) and desvenlafaxine (Pristiq®).Bupropion. Sold under the brand name Wellbutrin®, this is an atypical antidepressant that works by affecting the neurotransmitters norepinephrine and dopamine.
Research has shown that bupropion is less likely to cause sexual side effects than other medications used to treat depression. As such, it’s often used as an SSRI alternative, or as a secondary medication in combination with an SSRI or SNRI.Tricyclic antidepressants (TCAs). These are an older class of antidepressants that aren’t used as frequently today. As with other antidepressants, they work by affecting the neurotransmitters that contribute to depression.
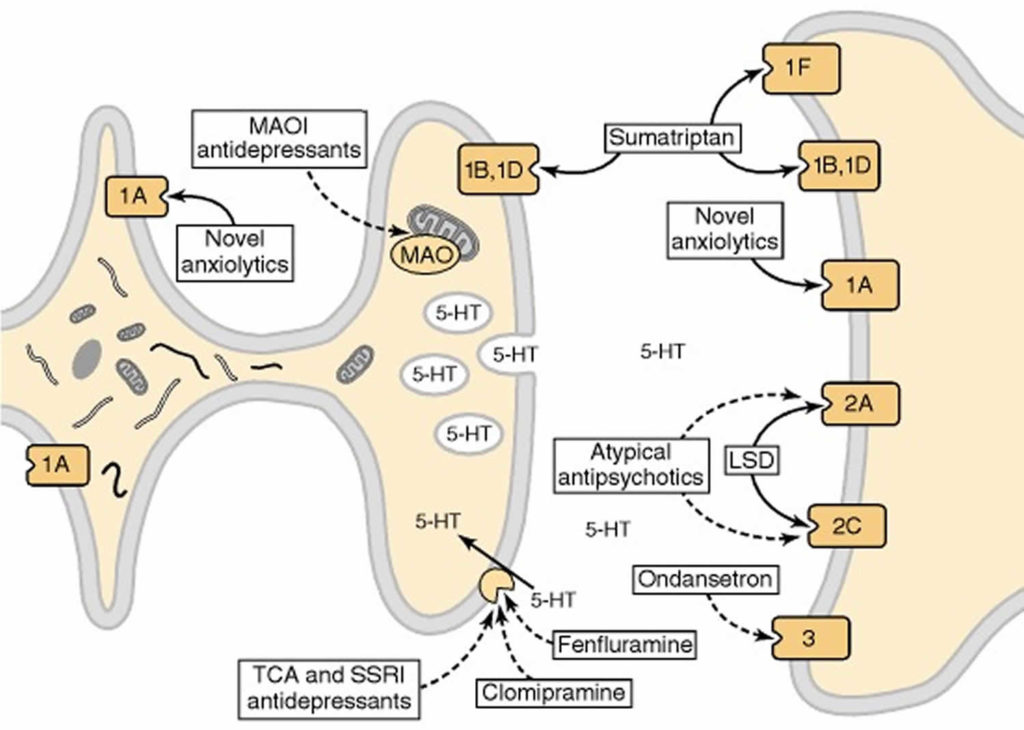
TCAs are designed to treat depression, but can cause more side effects and interactions than newer medications. Despite their side effect risk, TCAs are still prescribed to treat depression when other, newer medications haven’t worked effectively.Monoamine oxidase inhibitors (MAOIs). Another older class of antidepressants, these work by targeting the enzyme monoamine oxidase, which is responsible for controlling a variety of neurotransmitters in the brain.
Like TCAs, MAOIS generally aren’t widely used today due to their side effects. Not only can they interact with other medications, but they can also cause dangerous interactions if they’re used with certain foods, such as cheeses and cured meats.
Despite this, MAOIs may be prescribed as an alternative antidepressant in some cases if newer medications aren’t effective.
Other Medications for Anxiety
If you’re prescribed an SSRI for an anxiety disorder rather than depression, you may be able to switch to a different type of anti-anxiety medication.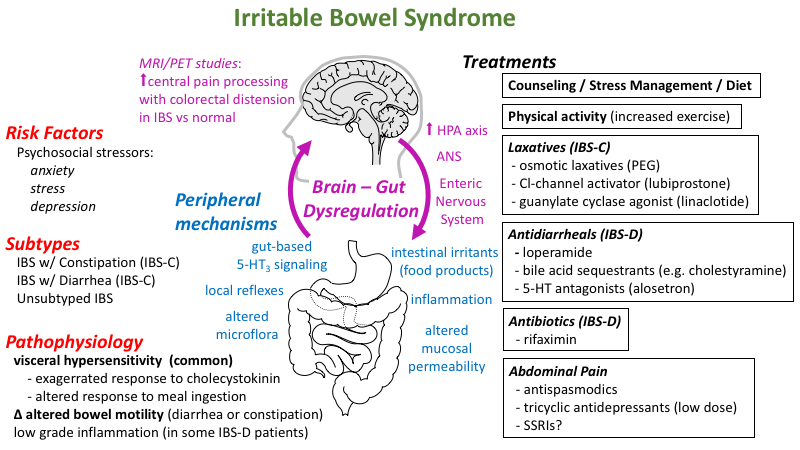 Options include:
Options include:
Benzodiazepines. These medications are often used to treat anxiety in the short term, as they work quickly and provide relief from anxiety symptoms in as little as 30 minutes to one hour.
However, they’re not recommended for long-term use, as they can cause dependence, become less effective over time and lead to withdrawal symptoms.
Buspirone. This is a modern anti-anxiety medication. It’s less likely to cause side effects than other medications and has no associated risk of causing dependence or withdrawal symptoms if treatment is stopped abruptly.
Buspirone is often prescribed as a second-line medication for people who don’t respond to SSRIs or experience side effects when using SSRIs to treat anxiety.
Psychotherapy
Depression, anxiety and other conditions for which SSRIs are commonly prescribed are often treated using psychotherapy.
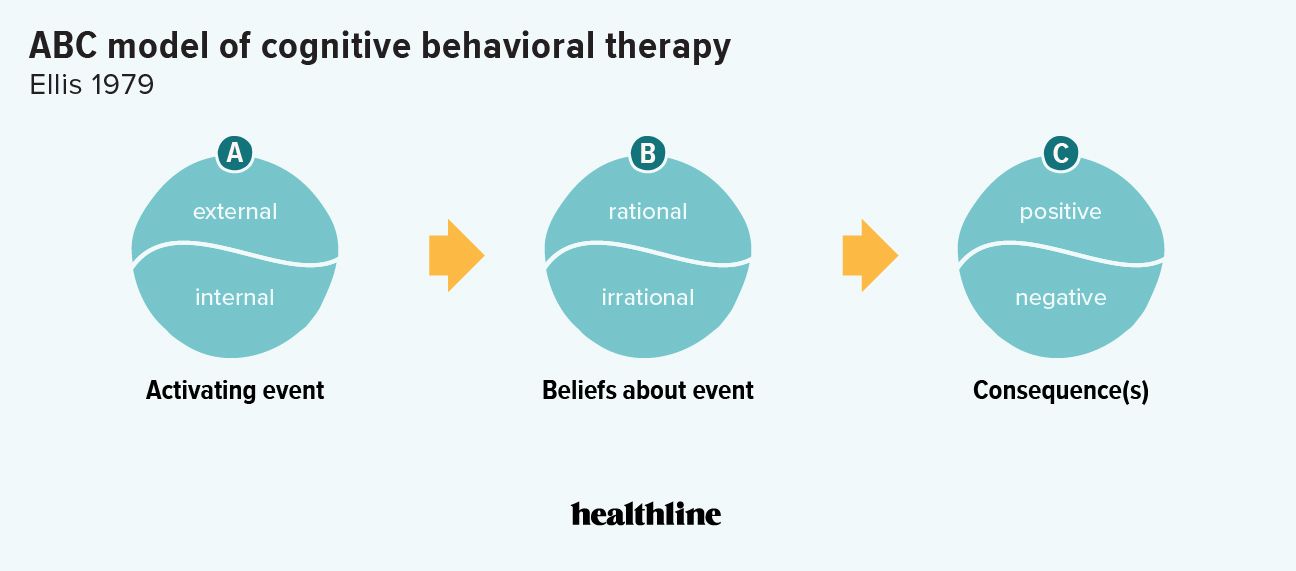
One of the most effective, well-estimated forms of therapy for treating depression is cognitive behavioral therapy, or CBT. It involves identifying and understanding the thought processes and behavior that can contribute to depression and anxiety symptoms.
It involves identifying and understanding the thought processes and behavior that can contribute to depression and anxiety symptoms.
One advantage of cognitive behavioral therapy is that it gives you control over your progress towards recovery. It usually takes 12 week to 16 weeks of therapy to see significant improvements from this type of therapy.
Depending on your disorder, you may benefit from other forms of therapy. Common forms of therapy used to treat depression, anxiety and other conditions often treated using SSRIs can include interpersonal therapy (IPT) and dialectical behavior therapy (DBT).
If you believe that therapy or online therapy might be an effective solution for you, try utilizing online mental health services.
Sometimes, therapy alone may be enough to provide relief from depression and/or anxiety. In some cases, you may need to take one of the medications listed above in combination with a form of therapy to treat your symptoms and work towards recovery.
Learn about an alternative type of therapy here: EFT Tapping: What Is It and Does It Work for Anxiety?
Natural Treatments
Some natural treatments, including herbal products and supplements, may offer some benefits for people with depression, anxiety and other mood disorders that are commonly treated using SSRIs.
However, these products should not be relied on as proven treatments for depression, anxiety or other mood disorders. If you’re currently prescribed an SSRI or other medication, don’t stop using it without first talking to your healthcare provider.
Common “natural antidepressants” include St. John’s wort — a herbal supplement found in teas, tablets and other products. While there’s some evidence that it may provide benefits for treating mild to moderate depression, research has found that it isn’t consistently effective.
If you use St. John’s wort to treat mild to moderate depression, make sure not to use it with any other antidepressants.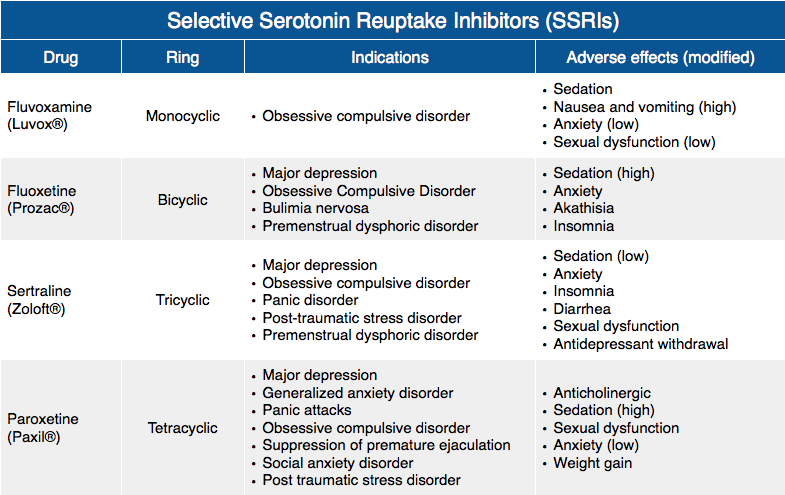 Combining St John’s wort with some antidepressants can potentially lead to serotonin syndrome — a dangerous, life-threatening reaction.
Combining St John’s wort with some antidepressants can potentially lead to serotonin syndrome — a dangerous, life-threatening reaction.
Other natural treatments often promoted as alternatives to SSRIs include S-Adenosylmethionine (SAM-e), saffron and folate.
In general, there’s little evidence that these treatments are effective, with few or no large-scale, high quality studies into their effects.
Lifestyle Changes
While most people associate treating depression with therapy and medication, making positive changes to your lifestyle and habits can have a surprisingly large impact.
Like natural treatments, lifestyle changes shouldn’t be viewed as perfect alternatives to antidepressants. However, they can complement other treatments for depression and anxiety, helping you to control your symptoms and make better progress towards recovery.
If you’re currently prescribed an SSRI, don’t stop taking it just to make changes to your habits and lifestyle.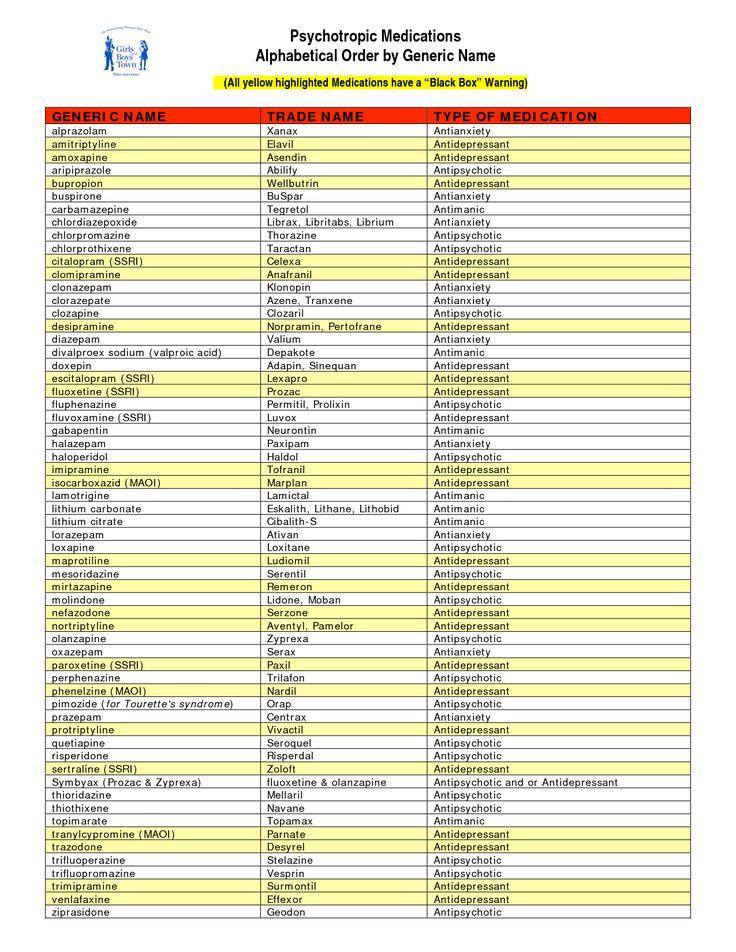 Instead, talk to your healthcare provider about how certain lifestyle changes and new habits may fit into your treatment.
Instead, talk to your healthcare provider about how certain lifestyle changes and new habits may fit into your treatment.
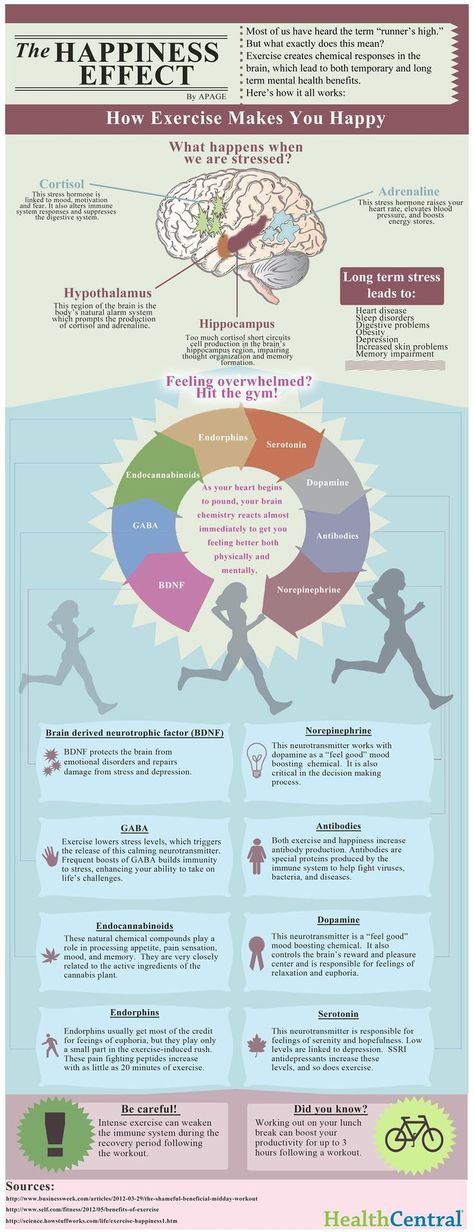
Lifestyle changes to consider include exercising regularly, eating a balanced diet, making sure you get enough sleep, taking steps to reduce stress in your life and spending time with friends, family and other loved ones.
While these may seem simple, they can make a big difference, especially when combined with therapy and medication.
In Conclusion
SSRIs are commonly prescribed to treat depression and anxiety disorders. They generally work well, but they’re not always effective for everyone. For some people, they can cause side effects that make alternative methods of treatment worth considering.
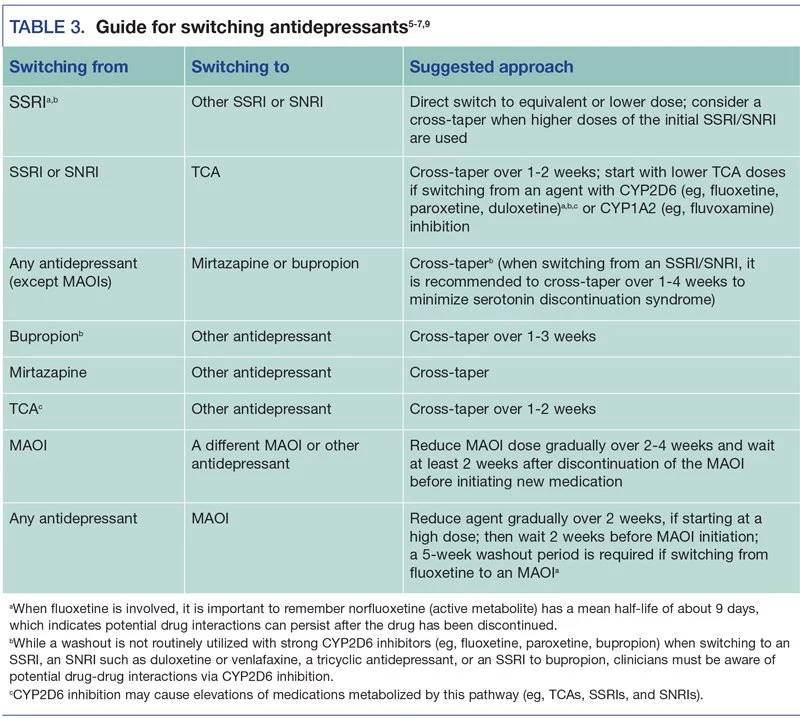
If you have depression and don’t want to use an SSRI, you may benefit from a different type of antidepressant, such as an SNRI, TCA, MAOI or bupropion. For anxiety, you may benefit from an anti-anxiety medication, such as buspirone.
Stopping SSRIs suddenly can cause withdrawal symptoms.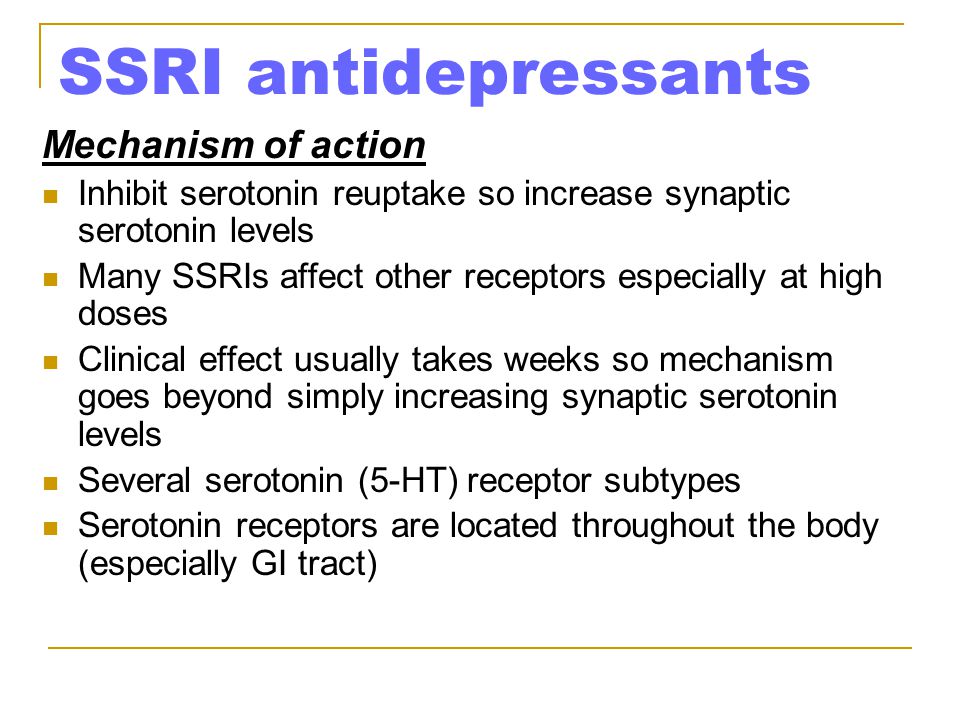 To keep yourself safe and prevent your symptoms from worsening, make sure to talk to your healthcare provider before you make any changes to the way you use your medication.
To keep yourself safe and prevent your symptoms from worsening, make sure to talk to your healthcare provider before you make any changes to the way you use your medication.
For expert help, you can receive an evaluation for depression treatment online to learn more about your treatment options.
psych meds online
psychiatrist-backed care, all from your couch
Learn More About SSRIs
In use since the late 1980s, SSRIs are some of the most common medications for depression and anxiety disorders. Our complete guide to SSRIs goes into greater detail about how SSRIs work, common SSRI medications, potential side effects and more.
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.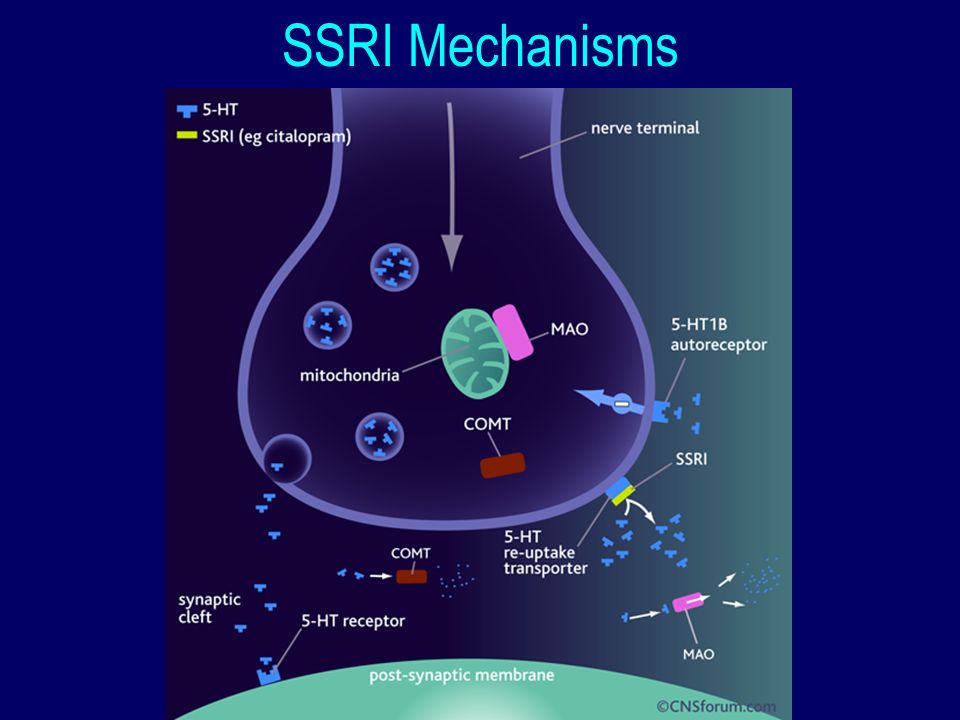
Types of Antidepressants: SSRIs, SNRIs, and More
Written by WebMD Editorial Contributors
In this Article
- Types of Antidepressants
- Atypical Antipsychotics
- What to Consider
- What Else to Keep in Mind
Everybody's different -- and everyone's depression is different, too. So if you and your doctor decide to try medicine to help treat it, you’ll work together to find one that helps.
Prescription drugs that lift your mood are called antidepressants. It may take some trial and error until you find one that's a good fit for your symptoms. It's important to keep in mind that these medications take a few weeks to start working. You might not notice results immediately.
Also keep in mind that depression treatment tends to have the best results when you also get counseling (“talk therapy”) and make lifestyle changes, like regular exercise. You and your doctor should talk about that. What you need may depend in part on how depressed you are.
If you don’t have a counselor, ask your doctor for a referral. Your friends and family may also have recommendations.
Types of Antidepressants
Antidepressants are drugs that treat depression. They help lift your mood and ease the sadness and hopelessness you might feel. They are also sometimes prescribed for physical pain, to treat symptoms of ADHD, to help with quitting smoking, or insomnia.
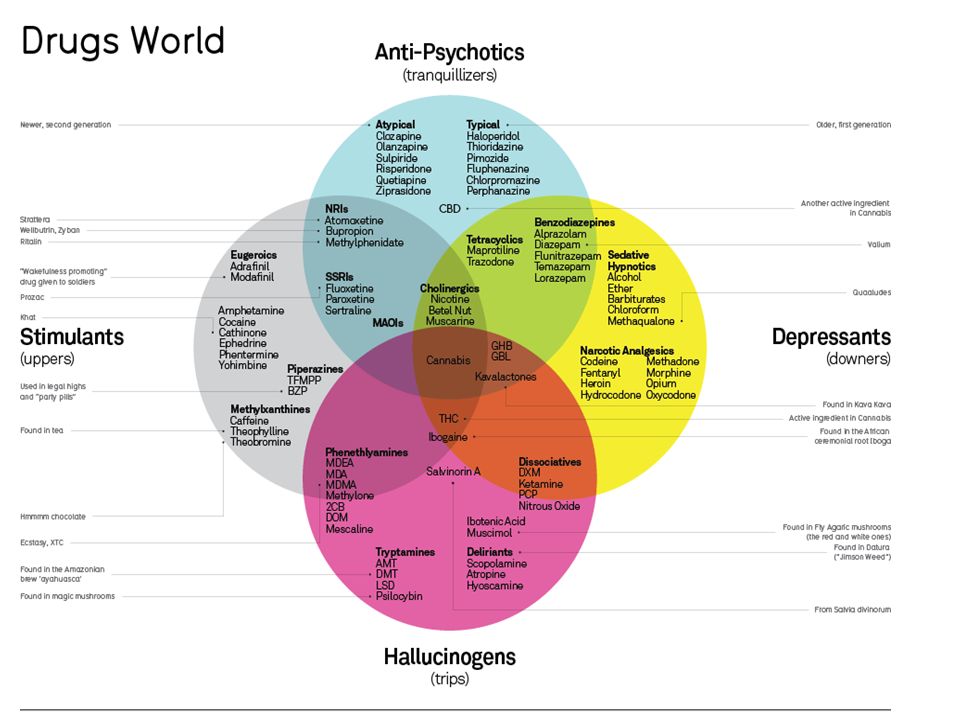
The major types of antidepressants are:
Atypical Antipsychotics
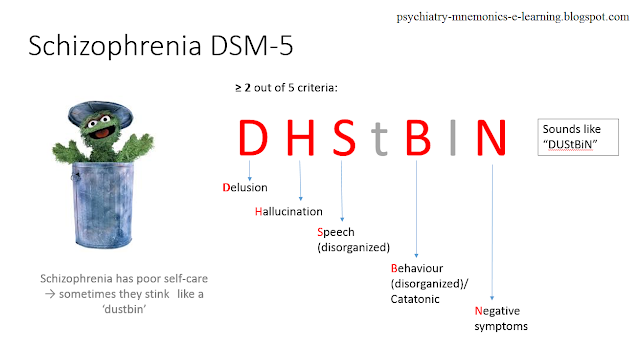
Some drugs that were first used to treat schizophrenia, called atypical antipsychotics, may also help certain kinds of depression, either alone or in combination with more traditional antidepressants.
Some examples are:
- Aripiprazole (Abilify)
- Brexpiprazole (Rexulti)
- Lurasidone (Latuda)
- Olanzapine-fluoxetine combination (Symbyax)
- Quetiapine (Seroquel)
What to Consider
If you and your doctor decide that it’s time to try a medicine, you’ll want to talk about things like:
What are the side effects? All medications have them.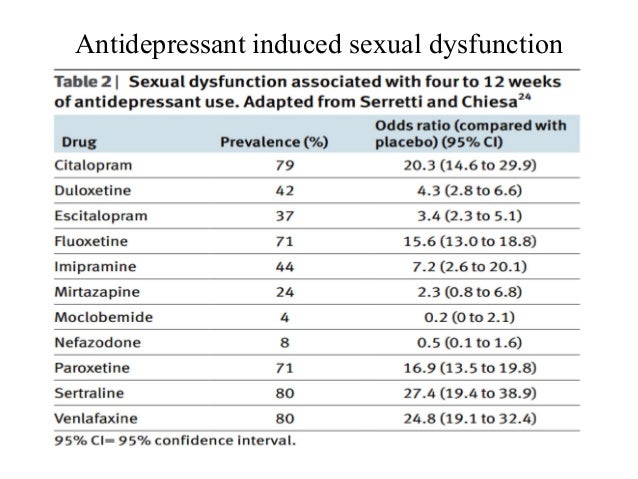 But which ones are more serious and which are you more likely to be OK with?
But which ones are more serious and which are you more likely to be OK with?
SSRIs, for example, can cause dry mouth, nausea, nervousness, insomnia, low sexual desire, and headache. Some atypical antidepressants, on the other hand, can raise or lower your appetite and cause insomnia or drowsiness but are less likely to cause sexual problems.
What are your other symptoms? If you have depression with anxiety or insomnia, for example, your doctor might prescribe a drug with a sedating effect. If you have pain or fatigue, a different medication might be best.
What are your other health conditions? Some antidepressants aren't safe for people with certain illnesses. The drugs could cause a bad interaction with your other prescriptions or directly worsen your medical problem.
How much does it cost? The cheapest prescriptions are generics, but not all medications come in this form.
Your insurance company may have a few "preferred" brands that cost more than generics but less than other name brands.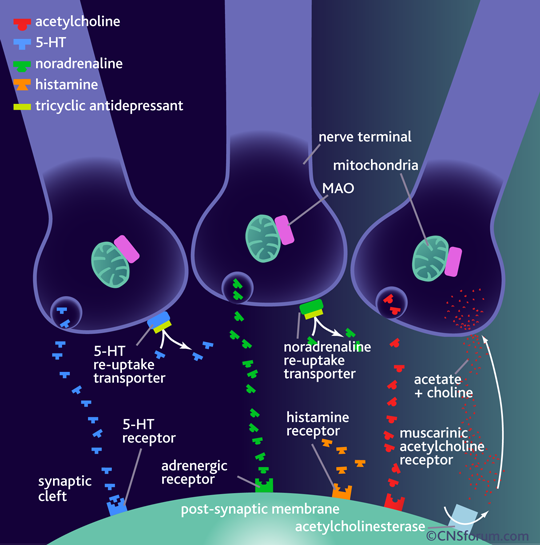
The most expensive drugs are those on your insurance plan's “non-preferred” list. If you can't afford them, you might want to try less costly antidepressants first. If they’re not effective or if they have side effects that bother you, your plan may then cover these more expensive drugs.
What Else to Keep in Mind
Antidepressants might also ease other symptoms, like anxiety, that can come with depression. But your doctor might think it's best to make a separate plan for these other problems.
The first antidepressant that you try might not work. But stick with it long enough to find out. It could take at least 4 weeks to feel the effects. If the prescription doesn't help, talk with your doctor about trying something new.
Selecting an antidepressant based on efficacy and tolerability
partners Keywords / keywords: Antidepressants, Velaxin, Venlafaxine, Categories of tolerability, Classification, Neuronal, Side effects, Neuropsychiatry, Toxic
Summary
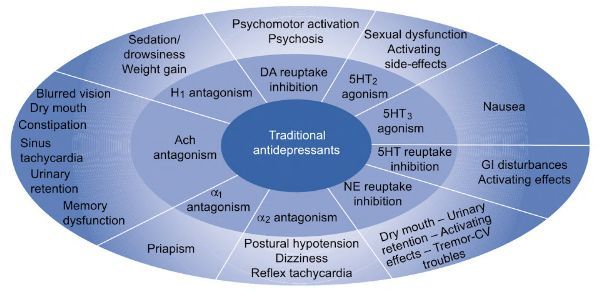
The classification of side effects of antidepressants is presented. Side effects can be toxic or neuronal. Neuronal side effects are divided into "extra-therapeutic" (persistent or reversible), as well as "paratherapeutic". Seven categories of antidepressant tolerance have been identified. The lowest category VII included clomipramine, imipramine, maprotiline, agomelatine. Category VI includes amitriptyline, V - pipofezin, trazodone, mianserin and mirtazapine, IV - vortioxetine, III - venlafaxine and duloxetine, II - sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran, and I - pirlindol and moclobemide. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine turned out to be the best tolerability category. This drug is the most effective and well tolerated antidepressant. Other options for the practical use of classifications are discussed.
Side effects can be toxic or neuronal. Neuronal side effects are divided into "extra-therapeutic" (persistent or reversible), as well as "paratherapeutic". Seven categories of antidepressant tolerance have been identified. The lowest category VII included clomipramine, imipramine, maprotiline, agomelatine. Category VI includes amitriptyline, V - pipofezin, trazodone, mianserin and mirtazapine, IV - vortioxetine, III - venlafaxine and duloxetine, II - sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran, and I - pirlindol and moclobemide. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine turned out to be the best tolerability category. This drug is the most effective and well tolerated antidepressant. Other options for the practical use of classifications are discussed.
Summary
A classification of the side effects of antidepressants is presented.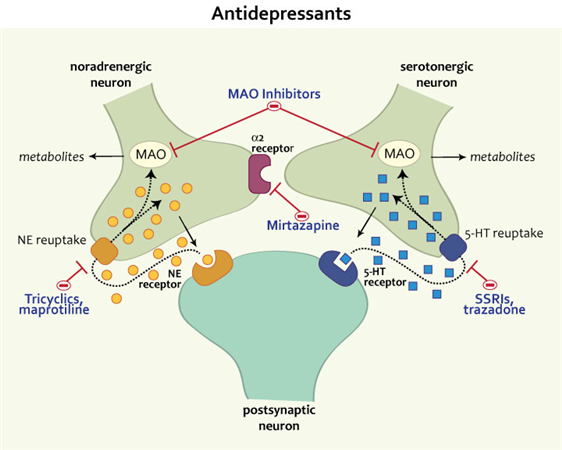 Side effects can be toxic or neuronal. Neuronal side effects are divided into "extratherapeutic" (persistent or reversible), as well as "paratherapeutic". Seven antidepressant tolerance categories have been identified. The lowest VII category included clomipramine, imipramine, maprotiline, agomelatine. Amitriptyline belongs to the VI category, pipofezin, trazodone, mianserin and mirtazapine to the V category, vortioxetine belongs to the IV category, venlafaxine and duloxetine to the III category, sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran to the II category, and pirlindole and moclobemide to the I category. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine was in the best category of tolerability. This drug is the most effective and tolerable antidepressant. Other options for the practical use of classifications are discussed.
Side effects can be toxic or neuronal. Neuronal side effects are divided into "extratherapeutic" (persistent or reversible), as well as "paratherapeutic". Seven antidepressant tolerance categories have been identified. The lowest VII category included clomipramine, imipramine, maprotiline, agomelatine. Amitriptyline belongs to the VI category, pipofezin, trazodone, mianserin and mirtazapine to the V category, vortioxetine belongs to the IV category, venlafaxine and duloxetine to the III category, sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran to the II category, and pirlindole and moclobemide to the I category. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine was in the best category of tolerability. This drug is the most effective and tolerable antidepressant. Other options for the practical use of classifications are discussed.
In the previous article, a description of the mechanism of action of various antidepressants (tricyclic - TcA, serotonin-modulating - CMA, four-cyclic - HcA, reversible monoamine oxidase type A inhibitors - RMAO-A, selective serotonin reuptake inhibitors - SSRIs, selective serotonin and norepinephrine reuptake inhibitors) was presented. - SNRIs, norepinephrine and selective serotonin - NaSSA, melatonergic - MeA, multimodal - MmA) (Table 1).
- SNRIs, norepinephrine and selective serotonin - NaSSA, melatonergic - MeA, multimodal - MmA) (Table 1).
Table 1. Known antidepressants in Russia, their effect on neurons and the "formula" of the mechanism of action (1-4).
* - white color - the drug does not affect neurons, dark gray - a pronounced increase in activity, light gray - a moderate increase in activity, ** - in high doses, IOD - neurotransmitter reuptake inhibitors, NERR - agents that affect regulatory receptors, RMAO-A - reversible inhibitors of monoamine oxidase type "A".
All these drugs, to varying degrees, contribute to the activation of serotonin (↑C or ↑s), noradrenaline (↑H or ↑n), dopamine (↑D or ↑d) or melatonin (↑M or ↑m) neurons, the “tone” of which decreases with depression. But the most pronounced effect on the vital activity of neurons is ↑SNd-antidepressants: amitriptyline and imipramine (TcA), as well as venlafaxine (SNRI) in high daily doses.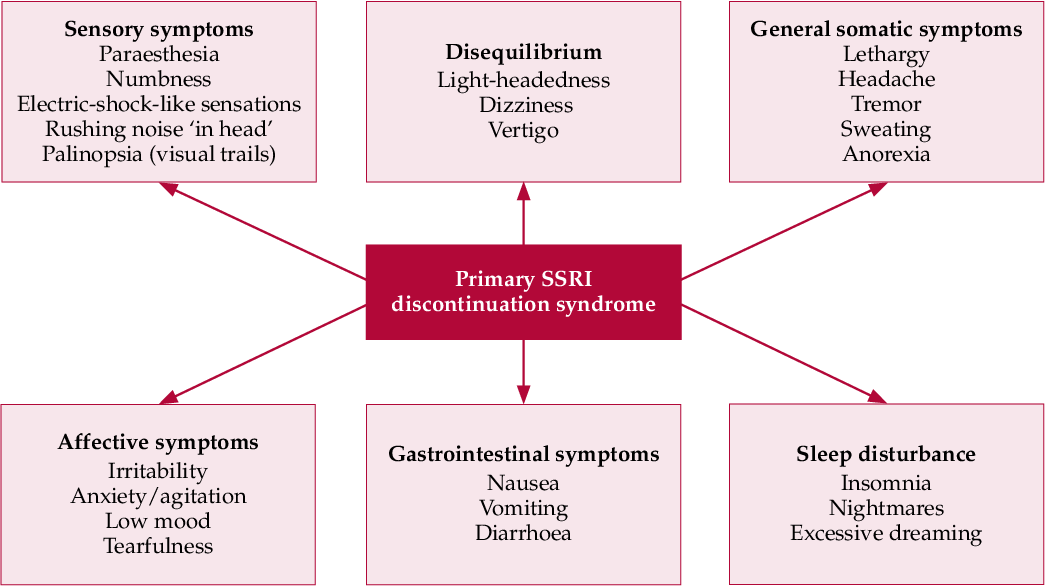 It is no coincidence that many experts refer to their most effective drugs for the treatment of depression (5).
It is no coincidence that many experts refer to their most effective drugs for the treatment of depression (5).
Of course, the choice of any antidepressant should be associated not only with its medicinal properties (effectiveness), but also with side effects (tolerability). The vast majority of authors agree that tolerability is best with SSRIs and worse with TcA (6-9), with other drugs in between (1). This assessment of the tolerability of antidepressants is correct, but is generalized. To clarify it, one should refer to the data on the mechanisms of the formation of side effects.
A smaller part of them is due to the toxic effect of antidepressants on the organs and tissues of patients. These “toxic” side effects are very dangerous (10). For example, while taking some TcA (clomipramine, imipramine), as well as MeA (agomelaptin), drug-induced hepatitis is observed, which leads to the death of patients (10, 11). Serious toxic side effects are also found in maprotiline, which causes agranulocytosis and leukopenia (12). Fortunately, toxic side effects are very rare and can be detected in a timely manner by test results.
Fortunately, toxic side effects are very rare and can be detected in a timely manner by test results.
For example, when agomelatine was found to cause severe and drug-induced hepatitis, detailed precautionary instructions were added to its package leaflet (11). They include a biochemical blood test, which is prescribed to all patients (without exception) before prescribing the drug, as well as while taking it. A similar analysis is required for patients receiving clomipramine and imipramine (13,14). However, when prescribing these antidepressants, biochemical analysis is required only for patients with pre-existing liver disease. Finally, regular CBCs to detect agranulocytosis and leukopenia are also required during treatment with maprotiline (12).
Obviously, the need for additional tests can significantly complicate the use of antidepressants. Fortunately, this is only required when using the listed drugs. When prescribing other antidepressants, you do not need to resort to additional examinations.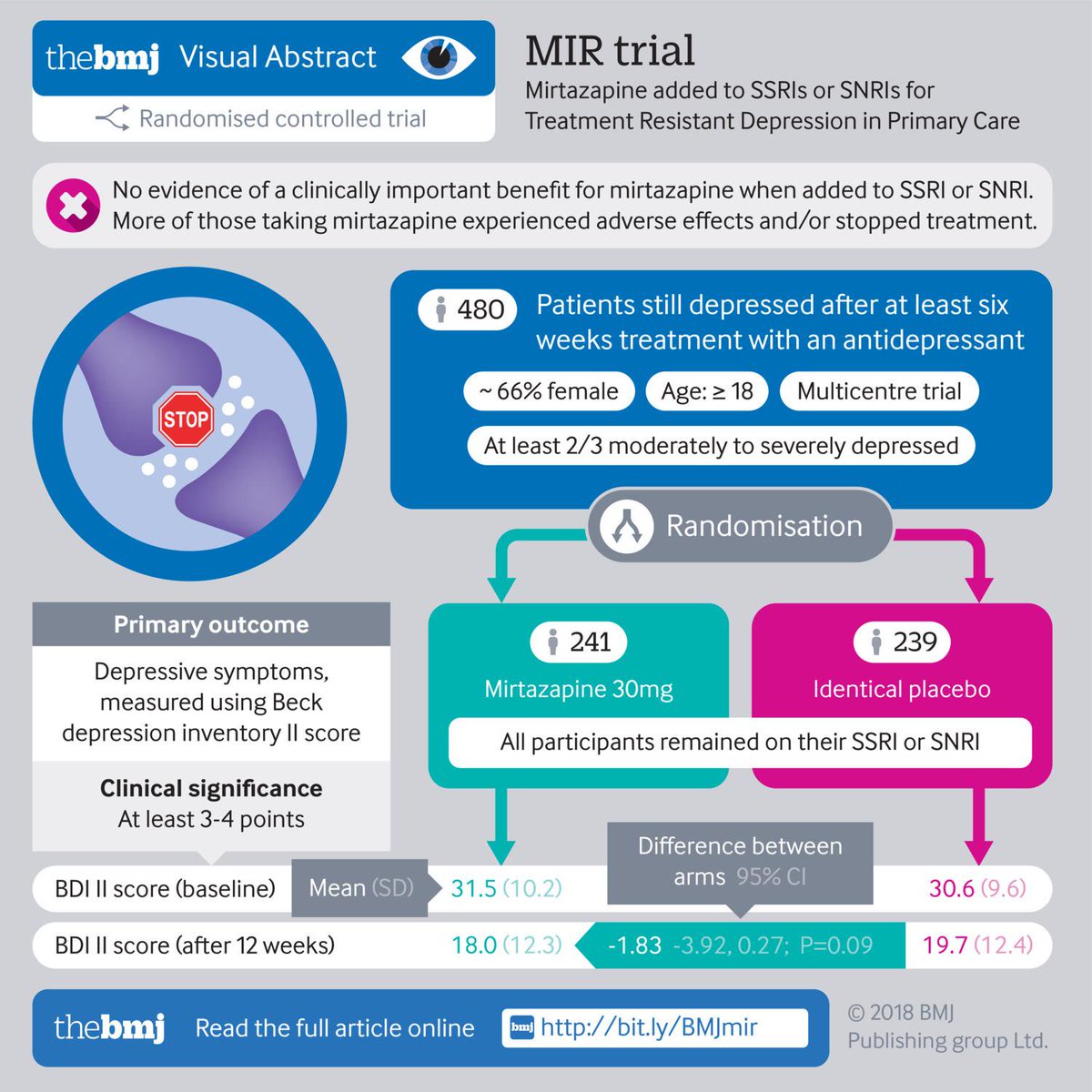 However, their tolerability may worsen due to the adverse effects of drugs on neurons. As a result, "neuronal" side effects are formed, which, however, do not directly threaten the lives of patients and are easily diagnosed by their complaints.
However, their tolerability may worsen due to the adverse effects of drugs on neurons. As a result, "neuronal" side effects are formed, which, however, do not directly threaten the lives of patients and are easily diagnosed by their complaints.
Some of the neuronal side effects are due to the effect of the antidepressant on histamine and acetylcholine neurons, which do not decrease their activity in the formation of mental disorders that are indications for antidepressant prescription (2,15). Accordingly, such pharmacological properties can be designated as "extra-therapeutic" (unnecessary, not related to the treatment process) side effects. They only increase the number of neuronal systems that suffer in the patient. Most often, "extra-curative" side effects are persistent. They may occur throughout the course of treatment, particularly when the antidepressant blocks excitatory receptors on histamine and acetylcholine neurons (15).
This mechanism of action, which is more characteristic of antipsychotics than antidepressants, leads to a sharp drop in the activity (inhibition) of these nerve cells (↓G and ↓A) (1,2).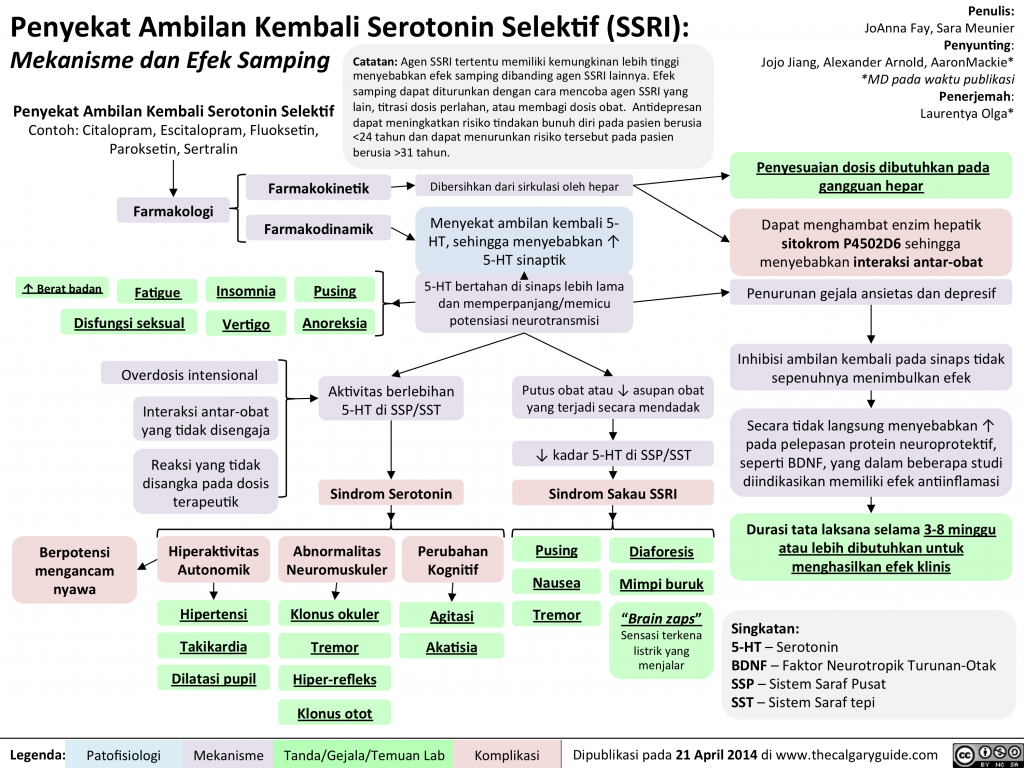 Moreover, normal histamine and acetylcholine neurons cannot restore their functions, since there are no effective compensatory mechanisms for this. Accordingly, patients develop persistent mental and somatic symptoms that seriously complicate treatment (Table 2).
Moreover, normal histamine and acetylcholine neurons cannot restore their functions, since there are no effective compensatory mechanisms for this. Accordingly, patients develop persistent mental and somatic symptoms that seriously complicate treatment (Table 2).
Table 2. The main "extra-therapeutic" side effects of antidepressants associated with the blockade of excitatory receptors on histamine and acetylcholine neurons (1,2)
Drowsiness, fatigue, deterioration of memory and attention are characteristic. There are complaints of dry mouth, disturbances of accommodation and urination, constipation, pain in the eyes due to an increase in intraocular pressure, heart rhythm disturbances, increased appetite and weight gain.
There is, however, an antidepressant that does not have permanent "off-the-shelf" side effects. This drug is vortioxetine. It does not inhibit histamine and acetylcholine neurons (due to the blockade of excitatory receptors), but increases their "tone" by influencing regulatory receptors (16). On the one hand, this provides vortioxetine with a unique nature of “non-therapeutic” side effects. In particular, when taking this antidepressant, excitement, anger, "unusual" dreams, and insomnia can be observed (Table 3).
On the one hand, this provides vortioxetine with a unique nature of “non-therapeutic” side effects. In particular, when taking this antidepressant, excitement, anger, "unusual" dreams, and insomnia can be observed (Table 3).
Table 3. "Extra-curative" side effects of vortioxetine (16,17).
Characterized by ketoacidosis, somatic complaints of dizziness, itching (including generalized), sweating, hot flashes, nausea, diarrhea, vomiting. On the other hand, these side effects are fundamentally reversible, since neurons have special mechanisms that are aimed at combating excessive activation. To do this, they can, for example, desensitize their regulatory receptors (a mechanism known as self-regulation). Therefore, the “non-therapeutic” side effects of vortioxetine often resolve spontaneously within the first two weeks of treatment (16).
Turning now to the rest of the antidepressants, we point out that the vast majority of them do not have "extra-curative" side effects at all, which increase the number of affected neuronal systems (2). Many drugs do not affect histamine and acetylcholine neurons. Moreover, they increase the activity of only those neurons (serotonin, norepinephrine and dopamine), whose "tone" is reduced in mental disorders, which are indications for the appointment of antidepressants. However, even this feature cannot save antidepressants from "neuronal" side effects. The latter will arise due to the fact that within any affected system of neurons, the activity of only part of the nerve cells decreases, while the functions of the other part are not disturbed. Antidepressants both activate the "affected" neurons and create therapeutic effects, and increase the "tone" of normally functioning nerve cells and cause side effects.
Many drugs do not affect histamine and acetylcholine neurons. Moreover, they increase the activity of only those neurons (serotonin, norepinephrine and dopamine), whose "tone" is reduced in mental disorders, which are indications for the appointment of antidepressants. However, even this feature cannot save antidepressants from "neuronal" side effects. The latter will arise due to the fact that within any affected system of neurons, the activity of only part of the nerve cells decreases, while the functions of the other part are not disturbed. Antidepressants both activate the "affected" neurons and create therapeutic effects, and increase the "tone" of normally functioning nerve cells and cause side effects.
At the same time, the tolerability of antidepressants paradoxically turns out to be a “hostage” of their therapeutic properties. The more effectively the drug activates the affected neurons, the more it affects similar nerve cells that are still functioning at the proper level.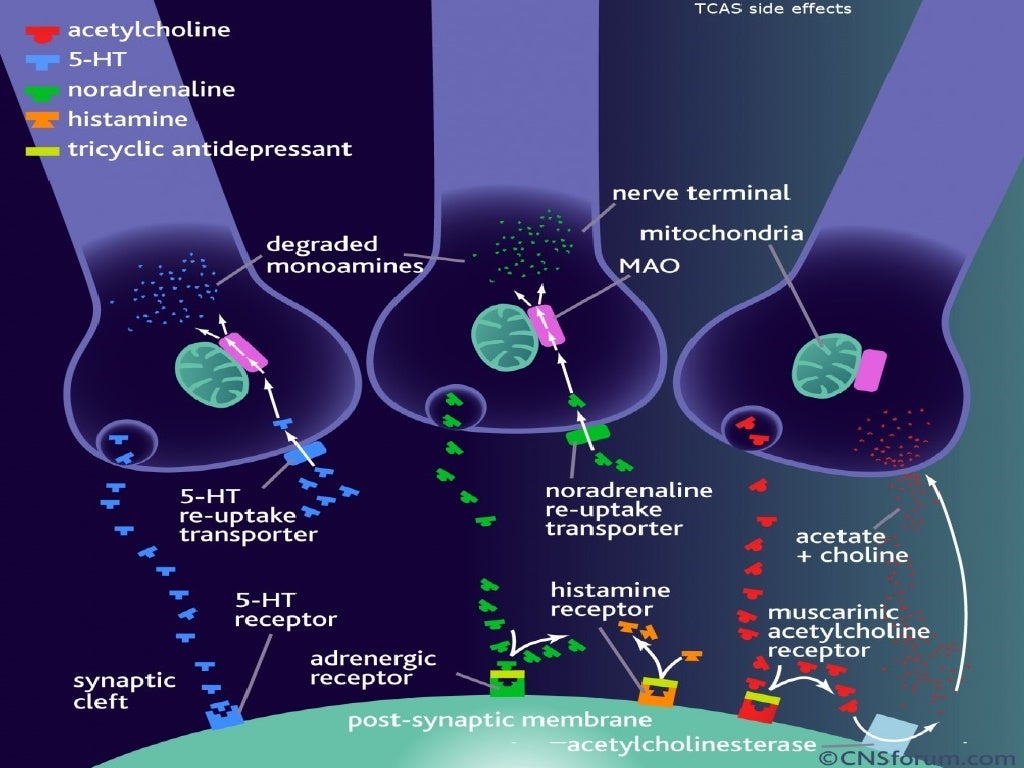 Therefore, it is advisable to designate the side effects under consideration as “paratherapeutic”. They are manifested by anxiety, restlessness, insomnia and anxiety (Table 4).
Therefore, it is advisable to designate the side effects under consideration as “paratherapeutic”. They are manifested by anxiety, restlessness, insomnia and anxiety (Table 4).
Table 4. Main "paratherapeutic" side effects of antidepressants (15)
Somatic complaints are represented by sexual dysfunction, disruption of the digestive organs and heart rhythm, fluctuations in blood pressure. As a rule, "paratherapeutic" side effects are reversible. They may resolve on their own in the second or third week of treatment (18). This is due to the above-mentioned ability of "normal" neurons to quickly adapt to excessive activation, reducing their sensitivity to neurotransmitters (2) 2 .
The presented data on toxic and neuronal side effects can be used to classify antidepressants into seven tolerability categories, where the last, seventh, is the worst, and the first is the best (Table 5).
Table 5.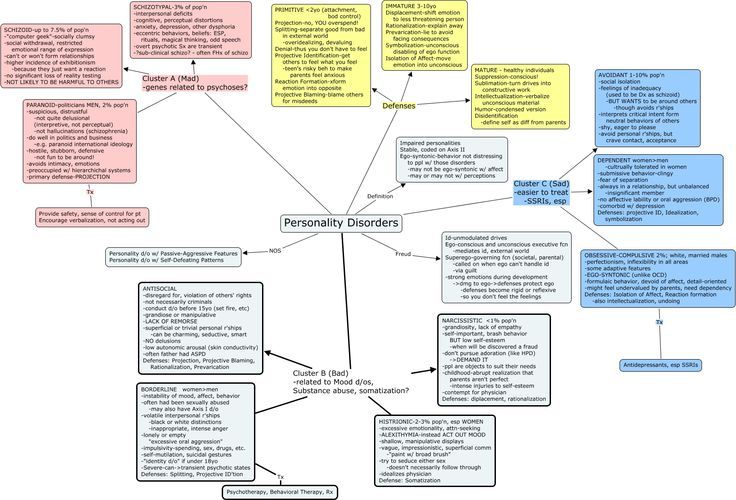 Antidepressant tolerance categories based on toxic and neuronal side effects.
Antidepressant tolerance categories based on toxic and neuronal side effects.
Thus, antidepressants from the lowest category VII (clomipramine, imipramine, maprotiline, agomelatine) have toxic side effects that directly threaten the lives of patients. Moreover, their appointment requires additional examination of patients. Problems with tolerability of other antidepressants are already due to neuronal side effects. All of them are not fatal, and additional examination is usually not required to identify them.
Neuronal side effects are divided into "extra-therapeutic" and "para-therapeutic". The first, as already mentioned above, are associated with an "additional" dysfunction of histamine and acetylcholine neurons, which do not reduce their activity in mental disorders, which are indications for prescribing antidepressants. Accordingly, "non-therapeutic" side effects, expanding the range of affected neuronal systems, determine the belonging of drugs to lower tolerance categories (VI, V and IV). In particular, amitriptyline contributes to a persistent decrease in the activity of histamine and acetylcholine neurons and is therefore classified as tolerability category VI. “Extra-curative” side effects for Category V antidepressants are more limited. After all, pipofezin, trazodone, mianserin and mirtazapine contribute to a persistent decrease in the activity of only histamine neurons. Vortioxetine is assigned to the next higher tolerance category IV. This antidepressant has the ability to increase the activity of histamine and acetylcholine neurons. However, the associated side effects are often reversible.
In particular, amitriptyline contributes to a persistent decrease in the activity of histamine and acetylcholine neurons and is therefore classified as tolerability category VI. “Extra-curative” side effects for Category V antidepressants are more limited. After all, pipofezin, trazodone, mianserin and mirtazapine contribute to a persistent decrease in the activity of only histamine neurons. Vortioxetine is assigned to the next higher tolerance category IV. This antidepressant has the ability to increase the activity of histamine and acetylcholine neurons. However, the associated side effects are often reversible.
The highest tolerance categories I-III include antidepressants that affect only serotonin, norepinephrine and dopamine neurons, which suffer from mental disorders that are indications for prescribing drugs. These drugs are characterized by "paratherapeutic" side effects that do not increase the number of affected neuronal systems (Table 5). They arise due to the activation of a part of serotonin, norepinephrine and dopamine neurons, which still retain their normal "tone" (2).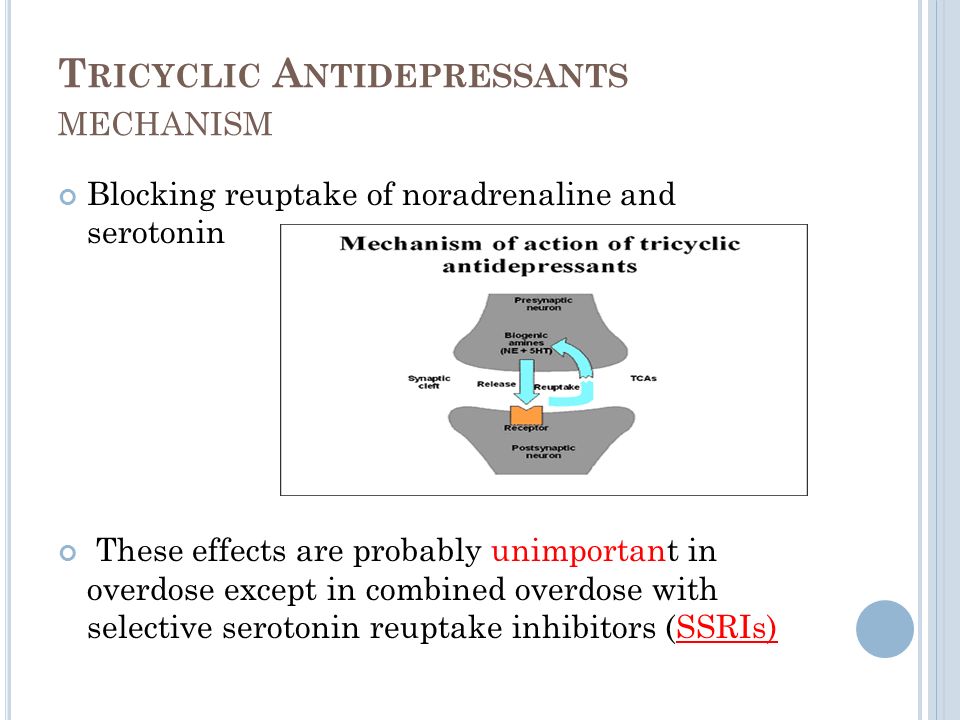 At the same time, the severity of "paratherapeutic" side effects depends, first of all, on the ability of the antidepressant to act on serotonin and norepinephrine nerve cells, since they all have little effect on dopamine (Table 1).
At the same time, the severity of "paratherapeutic" side effects depends, first of all, on the ability of the antidepressant to act on serotonin and norepinephrine nerve cells, since they all have little effect on dopamine (Table 1).
Accordingly, antidepressants, which simultaneously effectively activate serotonin and norepinephrine neurons, are assigned to category III of tolerance. These drugs are venlafaxine and duloxetine (Tables 1 and 5). The first of them, depending on the dose, is ↑CH- or ↑CHd-antidepressant. As for duloxetine, it has the properties of a ↑CH drug. Category II includes antidepressants that contribute to a pronounced activation of only serotonin or only norepinephrine neurons (Tables 1 and 5). These include all ↑C-antidepressants (sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine), as well as ↑cHd antidepressant - milnacipran. Finally, drugs that are not capable of strong activation of serotonin and norepinephrine neurons have the highest tolerance category I (Tables 1 and 5).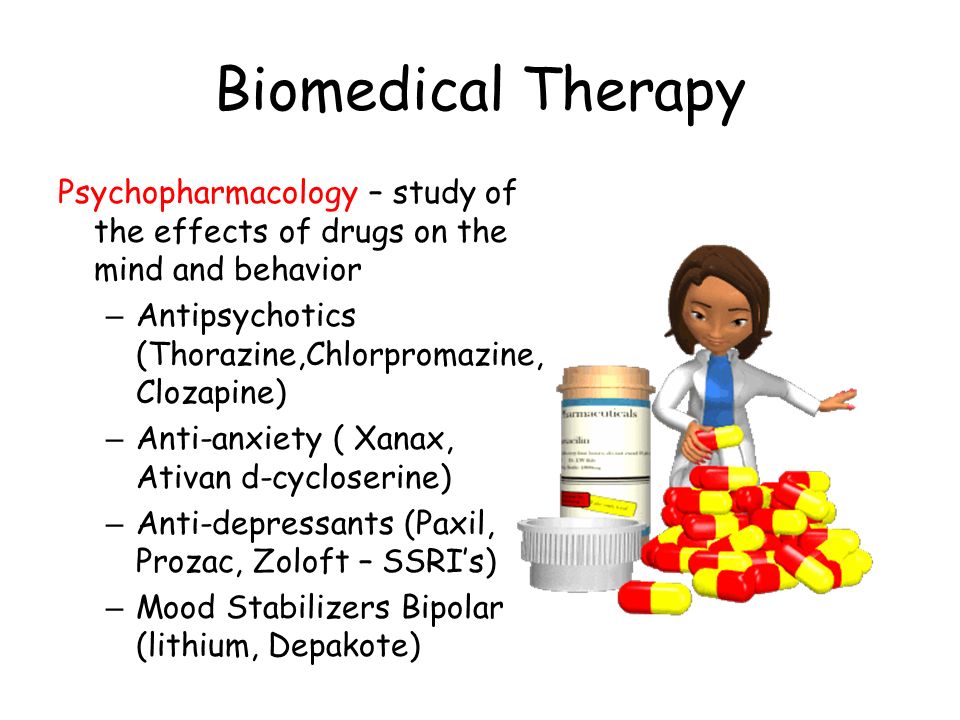 These are two ↑snd antidepressants - pirlindol and moclobemide.
These are two ↑snd antidepressants - pirlindol and moclobemide.
In conclusion, it should be noted that the presented classification of antidepressants according to tolerability does not claim to be comprehensive. However, it provides clear criteria for assessing the main side effects, which allow you to compare different drugs with each other. It seems that this is especially important in a situation where there are no clear recommendations for taking into account side effects when prescribing antidepressants. For example, a generalized formula is currently used in various publications and instructions. An antidepressant is suggested to be used "only after careful assessment of the expected benefit/risk ratio in patients" (11). But the results of such a "thorough assessment" tend to be in favor of prescribing the drug.
In particular, they write about agomelatine that if all the requirements of the instructions for prescribing an antidepressant are met, then the risk of developing drug-induced hepatitis becomes minimal (19).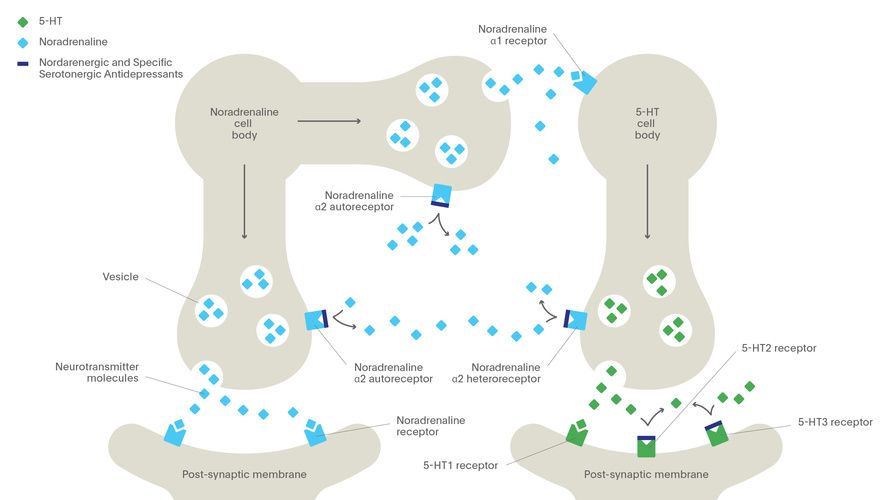 However, the unique mechanism of action attributed to agomelatine suggests that the benefits of prescribing an antidepressant are far greater than the disadvantages associated with its hepatotoxicity (19). Meanwhile, all the uniqueness of the mechanism of action of agomelatine is reduced to the possibility of influencing the neurons of the suprachiasmatic nucleus, the neurotransmitter of which is melatonin. And this effect is not required at all for the treatment of depression, since any antidepressant that activates serotonin and norepinephrine neurons can compensate for the deficiency of melatonin activity (20).
However, the unique mechanism of action attributed to agomelatine suggests that the benefits of prescribing an antidepressant are far greater than the disadvantages associated with its hepatotoxicity (19). Meanwhile, all the uniqueness of the mechanism of action of agomelatine is reduced to the possibility of influencing the neurons of the suprachiasmatic nucleus, the neurotransmitter of which is melatonin. And this effect is not required at all for the treatment of depression, since any antidepressant that activates serotonin and norepinephrine neurons can compensate for the deficiency of melatonin activity (20).
The recommendations for "thorough evaluation" presented here are not the only examples of flippant judgments about the tolerability of antidepressants. Some authors believe that side effects are weakly related to the mechanism of action of drugs. Side effects are said to be non-specific, probabilistic and therefore almost unpredictable (18). Other authors are at least looking for the reasons for the formation of side effects in order to take them into account when prescribing antidepressants.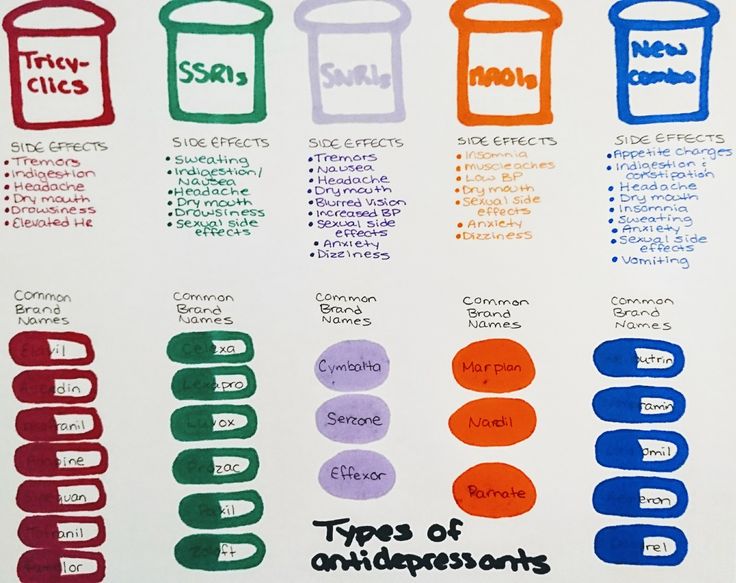 Unfortunately, they find these reasons not in the mechanisms of action of drugs, but in the characteristics of depression, public opinion or the psychology of the patient.
Unfortunately, they find these reasons not in the mechanisms of action of drugs, but in the characteristics of depression, public opinion or the psychology of the patient.
Thus, it is reported that even with the use of any of the “most easily tolerated drugs in 80% of patients with mild to moderate depression” (21), heterogeneous adverse events are noted. They are most common in dysthymia, first depressive states, with anxiety and somatic symptoms (21, 22), in persons over 45 years of age, with a high body weight deficit (22), and a history of negative placebo reactions in anamnesis (23). Poor tolerability of antidepressants has been reported to be associated with patients' high demands for quality of life (24) and their anxiety about social exclusion (25). The initially negative attitude towards psychiatry on the part of public opinion, the patient's low awareness of his own illness and the therapy recommended by the doctor, the unsatisfactory experience of previous treatment, etc. , also contribute to the problem. (22, 26).
, also contribute to the problem. (22, 26).
The speculation of such constructions is obvious. To refute them, it suffices to say that the side effects of drugs, as defined by the WHO, are caused by their pharmacological properties (37). It is hard to imagine that the inhibition of histamine and acetylcholine neurons arose due to the patient's high demands on the quality of life, the excessive activation of serotonin, norepinephrine and dopamine neurons due to the negative attitude towards psychiatry on the part of public opinion, and drug-induced hepatitis due to anxiety about social maladaptation.
Thus, the presented classification of antidepressants according to tolerability categories allows us to return the study of side effects to the mainstream of biological psychiatry. In addition, this classification is easy to use in practical medicine. In particular, the lower the tolerability category of an antidepressant, the greater the need for a special justification for prescribing it (effectiveness, positive experience of treatment in the past, the patient's desire, etc.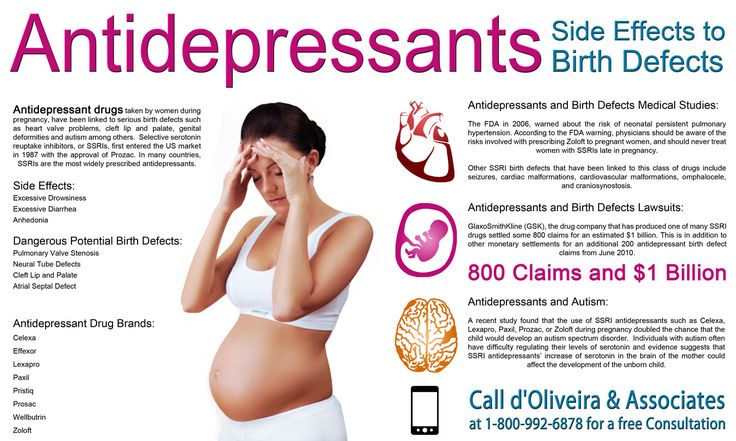 ). In turn, the appearance of such a detailed justification in the history of the disease will help to avoid many problems (psychological, social and others) that arise in the process of treatment between the doctor and his patient.
). In turn, the appearance of such a detailed justification in the history of the disease will help to avoid many problems (psychological, social and others) that arise in the process of treatment between the doctor and his patient.
With the help of the presented classification, it is easy to decide on the choice of the most effective and tolerable antidepressant. To do this, it is only necessary to compare the tolerability categories of the most effective drugs: amitriptyline (TcA), imipramine (TcA) and venlafaxine (SNRI) (5). The first of them (amitriptyline) belongs to the VI category of tolerance (Table 5). The side effects of the second antidepressant (imipramine) are even worse. This drug belongs to the VII category of tolerance. As for venlafaxine, the side effects of this antidepressant are much weaker, and this drug belongs to category III tolerance. Thus, venlafaxine, when used at high doses, is the most effective and tolerated drug in the treatment of depression.
Venlafaksin is well-known in our country under the trade name Velaksin (Egis). This drug has been studied in leading scientific organizations that carry out cutting-edge research in the field of psychiatry. Among them are the Federal State Budgetary Institutions “State Scientific Center for Social and Forensic Psychiatry named after V.P. Serbsky" and "Moscow Research Institute of Psychiatry" of the Ministry of Health of Russia, St. Petersburg Research Institute. V.M. Bekhterev (28.29). Prolonged-release capsules (Velaxin retard) (30) are also well-known, with the use of which there is a significant reduction in the frequency of such a side effect of the drug as nausea (31). In addition, the study of Velaksin was successfully carried out not only in psychiatry, but also in neurology (32).
This drug has been studied in leading scientific organizations that carry out cutting-edge research in the field of psychiatry. Among them are the Federal State Budgetary Institutions “State Scientific Center for Social and Forensic Psychiatry named after V.P. Serbsky" and "Moscow Research Institute of Psychiatry" of the Ministry of Health of Russia, St. Petersburg Research Institute. V.M. Bekhterev (28.29). Prolonged-release capsules (Velaxin retard) (30) are also well-known, with the use of which there is a significant reduction in the frequency of such a side effect of the drug as nausea (31). In addition, the study of Velaksin was successfully carried out not only in psychiatry, but also in neurology (32).
M.Yu Drobizhev's video on the same topic can be viewed at the link: https://www.youtube.com/watch?v=SwtO_bC_838&t=11s
References
- Antidepressant therapy and other treatments for depressive disorders.
 Report of the CINP Working Group based on a review of the evidence. Ed. V.N. Krasnov. M., 2008. - 215 S.
Report of the CINP Working Group based on a review of the evidence. Ed. V.N. Krasnov. M., 2008. - 215 S. - Stahl S.M. Stahl's essential psychopharmacology: neuroscientific basis and practical application. — 3nd ed. Cambridge University Press, 2008. - 1117P.
- Drobizhev M. Yu., Fedotova A. V., Kikta S. V., Antokhin E. Yu. Between depression and fibromyalgia: the fate of an antidepressant. Journal of Neurology and Psychiatry. S.S. Korsakov. 2016;116(4): 114-120. DOI:10.17116/jnevro201611641114-120.,
- Shagiakhmetov F.Sh., Anokhin P.K., Shamakina I.Yu. Vortioxetine: mechanisms of multimodality and clinical efficacy. Social and Clinical Psychiatry 2016;26(4): 84-96
- Bauer M., Pfennig A., Severus E., Weibrau P.S., J. Angst, Müller H.-J. Clinical guidelines of the World Federation of Societies of Biological Psychiatry for the biological therapy of unipolar depressive disorders. Part 1: Acute and ongoing treatment of unipolar depressive disorders as of 2013.
 Modern therapy of mental disorders 2015;4:33-39.).
Modern therapy of mental disorders 2015;4:33-39.). - Anderson IM. SSRIS versus tricyclic antidepressants in depressed inpatients: a meta-analysis of efficacy and tolerability. depression. Anxiety. 1998;7(Suppl 1):11-17.
- Anderson IM, Nutt DJ, Deakin JF. Evidence based guidelines for treating depressive disorders with antidepressants: a revision of the 1993 British Association for Psychopharmacology guidelines. J Psychopharmacol. 2000;14:3-20.
- Peretti S, Judge R, Hindmarch I. Safety and tolerability considerations: tricyclic antidepressants vs. selective serotonin reuptake inhibitors. Acta Psychiatr. Scand. 2000; Suppl. 403:17-25.
- Wilson K, Mottram P, Sivanranthan A, Nightingale A. Antidepressant versus placebo for depressed elderly. 2001 Cochrane. database. Syst. Rev. CD000561.) and worse for TcA
- Liver Tox. https://livertox.nlm.nih.gov
- Valdoxan - instructions for the medical use of the drug.
 https://medi.ru/instrukciya/valdoksan_5084/
https://medi.ru/instrukciya/valdoksan_5084/ - Lyudiomil - official instructions for use. https://medi.ru/instrukciya/lyudiomil_9448/
- Anafranil tablets - instructions (information for specialists) on the use of the drug. https://medi.ru/instrukciya/anafranil-tabletki_8616/
- Melipramine tablets - official instructions for use. https://medi.ru/instrukciya/melipramin-tabletki_4780/
- Drobizhev M.Yu., Ovchinnikov A.A., Kikta S.V. Why do antidepressants have side effects? Pharmateka. 2015. No. 20 (313). pp. 72-77.
- Brintellix (Brintellix). https://www.rlsnet.ru/tn_index_id_87791.htm
- Subeesh V, Singh H, Maheswari E, Beulah E. Novel adverse events of vortioxetine: A disproportionality analysis in USFDA adverse event reporting system database. Asian J Psychiatr. 2017 Dec;30:152-156. doi: 10.1016/j.ajp.2017.09.005.
- Borodin V.I. Tolerability of treatment in patients with depressive disorders (complex analysis).
 Abstract for the competition … doc. honey. Sciences. Moscow. 2009.
Abstract for the competition … doc. honey. Sciences. Moscow. 2009. - Freiesleben SD, Furczyk K.J A systematic review of agomelatine-induced liver injury. Mol Psychiatry. 2015 Apr 21;3(1):4. doi: 10.1186/s40303-015-0011-7. eCollection 2015.
- Drobizhev M.Yu. Timing of meta-analyses and efficacy of antidepressants in depression. Social and clinical psychiatry. 2017;4:81-88.
- Aldushin A.A. Antidepressant therapy tolerance and withdrawal forecast based on the analysis of nocebo effects. Russian psychiatric journal. 2009; 3:55-61.
- Avedisova A.S., Borodin V.I., Aldushin A.A. Comparison of the efficacy and tolerability of antidepressants of different groups in mild and moderate depression. Journal of Neurology and Psychiatry. S.S. Korsakov. 2006;11:15-19.
- Lapin I.P. Personality and medicine. Introduction to the psychology of pharmacotherapy. - St. Petersburg: Dean, 2001.-416C.
- Roberis H. Neurotic patients who terminate their own treatment.
 Br. J. Psychiatry. 1985; 146(4):443-445.
Br. J. Psychiatry. 1985; 146(4):443-445. - Mosolov S.N., red. Reference guide to psychopharmacology. Psychopharmacological and antiepileptic drugs approved for use in Russia: 2nd ed. BINOM, Moscow, 2004. - 304C.
- Avedisova A.S., Borodin V.I. Non-compliance or refusal of psychopharmacotherapy? Russian psychiatric journal. 2006; 1:61-65.
- http://vmede.org/sait/?id=Farmakologija_klin_farm_y4ebnik_kykes_2009&menu=Farmakologija_klin_farm_y4ebnik_kykes_2009&page=7
- Krasnov V.N., Kryukov V.V. Velaxin® (venlafaxine) in modern therapy of depression: results of the first Russian multicenter efficacy and safety study. Psychiatry and psychopharmacotherapy. 2007;9 (4), http://www.consilium-medicum.com/magazines/special/psychiatry/article/15426
- Mosolov S.N., Kostyukova E.G., Gorodnichev A.V., Timofeev I.V., Ladyzhensky M.Ya., Serditov O.V. Clinical efficacy and tolerability of venlafaxine (Velaxin) in the treatment of moderate and severe depression.
 Modern therapy of mental disorders. 2007;3:58-63.
Modern therapy of mental disorders. 2007;3:58-63. - Avedisova A.S., Zakharova K.V., Kanaeva L.S., Vazagaeva T.I., Aldushin A.A. Psychiatry and psychopharmacotherapy. 2009;11(1):36-40.
- Avedisova A.S. Venlafaxine (velaxin): results of international trials of a third-generation antidepressant. Psychiatrist. and a psychopharmacologist. 2006; 11(2):2-7.
- Mosolov S.N. Clinical use of modern antidepressants. SPb., 1995.-565C.).
M.Yu. Drobizhev , Doctor of Medical Sciences, Head of the Educational Department of the Training Center of the Association of Medical and Pharmaceutical Universities of Russia. Contact information – [email protected]
E.Yu. Antokhin , Candidate of Medical Sciences, Associate Professor, Head of the Department of Clinical Psychology and Psychotherapy, Orenburg State Medical University, Ministry of Health of Russia.
R.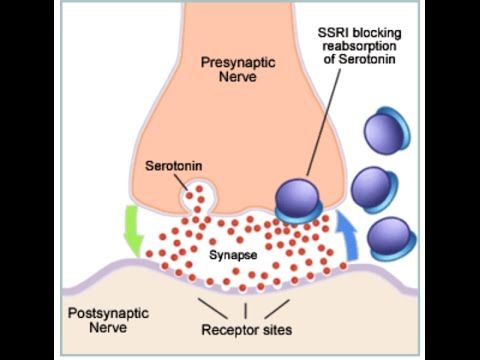 I. Palaeva – Assistant of the Department of Clinical Psychology and Psychotherapy of FSBEI HE “Orenburg State Medical University” of the Ministry of Health of Russia.
I. Palaeva – Assistant of the Department of Clinical Psychology and Psychotherapy of FSBEI HE “Orenburg State Medical University” of the Ministry of Health of Russia.
S. V. Kikta , candidate of medical sciences, head. Department of the Federal State Budgetary Institution "Polyclinic No. 3" of the Administration of the President of the Russian Federation, Moscow
1 There are probably side effects due to excessive activation of melatonin nerve cells. However, they are not yet described even in the instructions for agomelatine, a melatonergic drug that has a direct effect on them (11).
2 Theoretically, “paratherapeutic” side effects can be observed even against the background of “extra-therapeutic” ones. After all, any antidepressants to varying degrees activate serotonin, norepinephrine or dopamine neurons. However, drugs are dominated by "extra-curative" side effects, if only because they are most often persistent.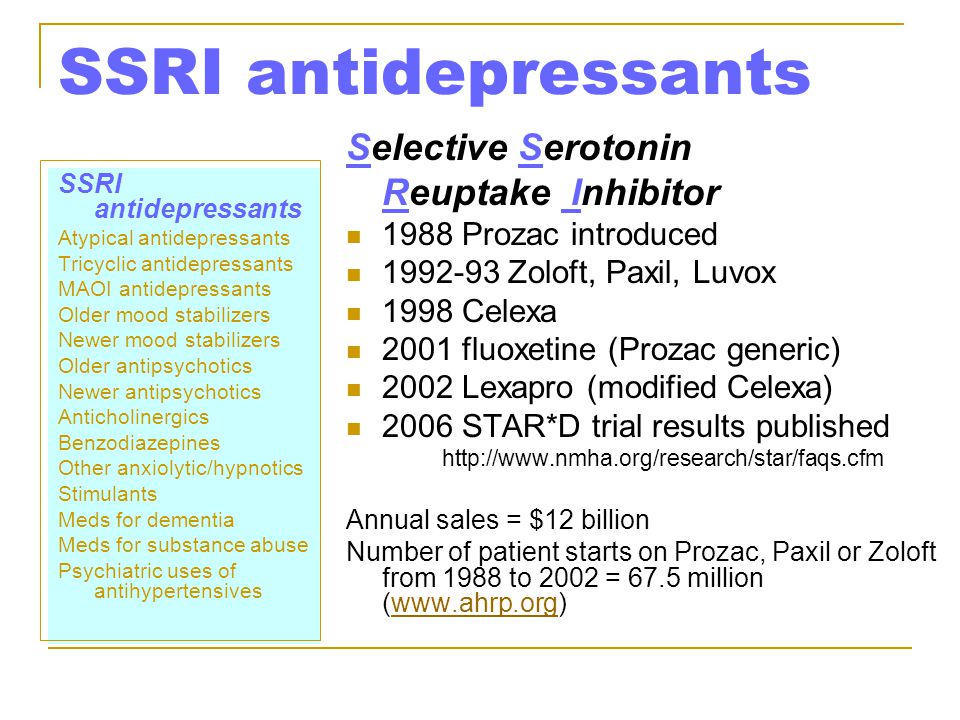 At the same time, "paratherapeutic" side effects are always reversible. In addition, not all antidepressants that have “non-therapeutic” side effects are capable of seriously activating serotonin, norepinephrine and dopamine neurons.
At the same time, "paratherapeutic" side effects are always reversible. In addition, not all antidepressants that have “non-therapeutic” side effects are capable of seriously activating serotonin, norepinephrine and dopamine neurons.
| Share It is emphasized that the study is preliminary and its results require confirmation in the future. Although a relationship has been found between antidepressant use and a reduction in the frequency of epileptic seizures, a causal relationship still needs to be proven.
← Previous news Next news → Read more You may be interested in
|
 " j="The study, to be presented Monday at the American Epilepsy Society's annual meeting in San Diego, includes patients who were prescribed one of two types of antidepressants - selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors (SNRIs). " g="The study, to be presented Monday at the annual meeting of the American Epilepsy Society in San Diego, included patients who were prescribed one of two types of antidepressants -- selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors ( SNRIs).">
" j="The study, to be presented Monday at the American Epilepsy Society's annual meeting in San Diego, includes patients who were prescribed one of two types of antidepressants - selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors (SNRIs). " g="The study, to be presented Monday at the annual meeting of the American Epilepsy Society in San Diego, included patients who were prescribed one of two types of antidepressants -- selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors ( SNRIs)."> 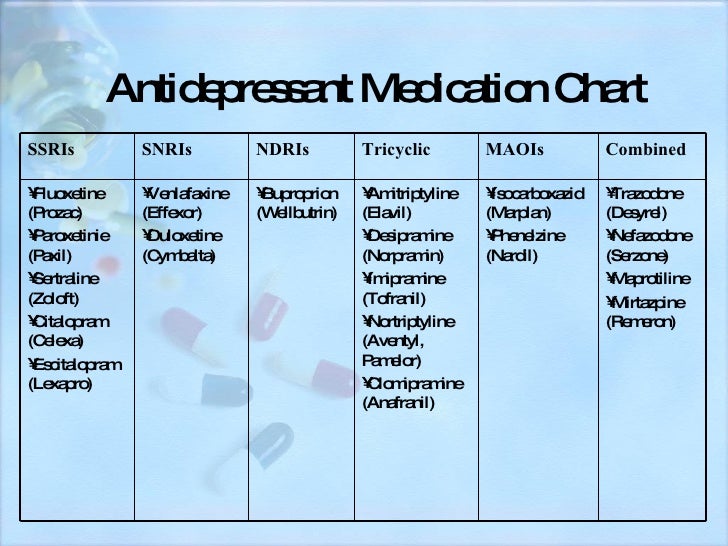 Along with this, it was found that the use of antidepressants even reduced the frequency of epileptic seizures in those volunteers who experienced them frequently.
Along with this, it was found that the use of antidepressants even reduced the frequency of epileptic seizures in those volunteers who experienced them frequently.