Signs and symptoms of mdd
Depression (major depressive disorder) - Diagnosis and treatment
Diagnosis
Your doctor may determine a diagnosis of depression based on:
- Physical exam. Your doctor may do a physical exam and ask questions about your health. In some cases, depression may be linked to an underlying physical health problem.
- Lab tests. For example, your doctor may do a blood test called a complete blood count or test your thyroid to make sure it's functioning properly.
- Psychiatric evaluation. Your mental health professional asks about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
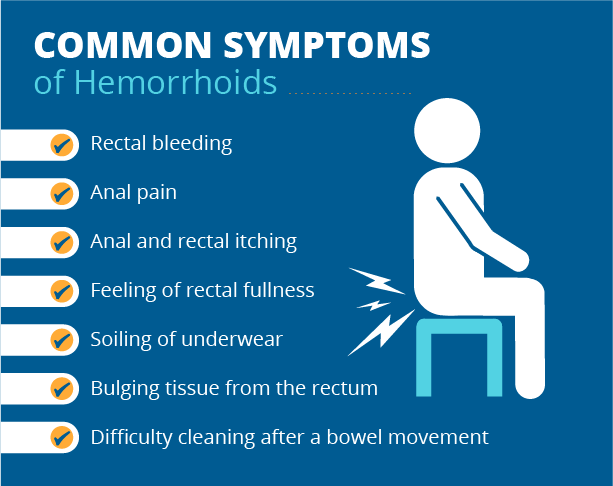
- DSM-5. Your mental health professional may use the criteria for depression listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Types of depression
Symptoms caused by major depression can vary from person to person. To clarify the type of depression you have, your doctor may add one or more specifiers. A specifier means that you have depression with specific features, such as:
- Anxious distress — depression with unusual restlessness or worry about possible events or loss of control
- Mixed features — simultaneous depression and mania, which includes elevated self-esteem, talking too much and increased energy
- Melancholic features — severe depression with lack of response to something that used to bring pleasure and associated with early morning awakening, worsened mood in the morning, major changes in appetite, and feelings of guilt, agitation or sluggishness
- Atypical features — depression that includes the ability to temporarily be cheered by happy events, increased appetite, excessive need for sleep, sensitivity to rejection, and a heavy feeling in the arms or legs
- Psychotic features — depression accompanied by delusions or hallucinations, which may involve personal inadequacy or other negative themes
- Catatonia — depression that includes motor activity that involves either uncontrollable and purposeless movement or fixed and inflexible posture
- Peripartum onset — depression that occurs during pregnancy or in the weeks or months after delivery (postpartum)
- Seasonal pattern — depression related to changes in seasons and reduced exposure to sunlight
Other disorders that cause depression symptoms
Several other disorders, such as those below, include depression as a symptom.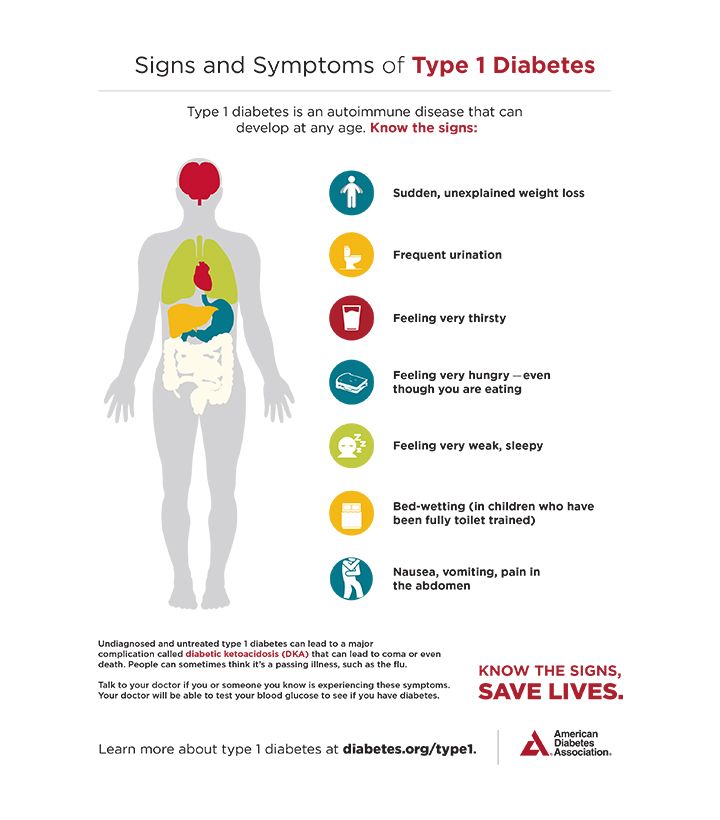 It's important to get an accurate diagnosis, so you can get appropriate treatment.
It's important to get an accurate diagnosis, so you can get appropriate treatment.
- Bipolar I and II disorders. These mood disorders include mood swings that range from highs (mania) to lows (depression). It's sometimes difficult to distinguish between bipolar disorder and depression.
- Cyclothymic disorder. Cyclothymic (sy-kloe-THIE-mik) disorder involves highs and lows that are milder than those of bipolar disorder.
- Disruptive mood dysregulation disorder. This mood disorder in children includes chronic and severe irritability and anger with frequent extreme temper outbursts. This disorder typically develops into depressive disorder or anxiety disorder during the teen years or adulthood.
- Persistent depressive disorder. Sometimes called dysthymia (dis-THIE-me-uh), this is a less severe but more chronic form of depression. While it's usually not disabling, persistent depressive disorder can prevent you from functioning normally in your daily routine and from living life to its fullest.
- Premenstrual dysphoric disorder. This involves depression symptoms associated with hormone changes that begin a week before and improve within a few days after the onset of your period, and are minimal or gone after completion of your period.
- Other depression disorders. This includes depression that's caused by the use of recreational drugs, some prescribed medications or another medical condition.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your depression (major depressive disorder)-related health concerns Start Here
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Complete blood count (CBC)
Treatment
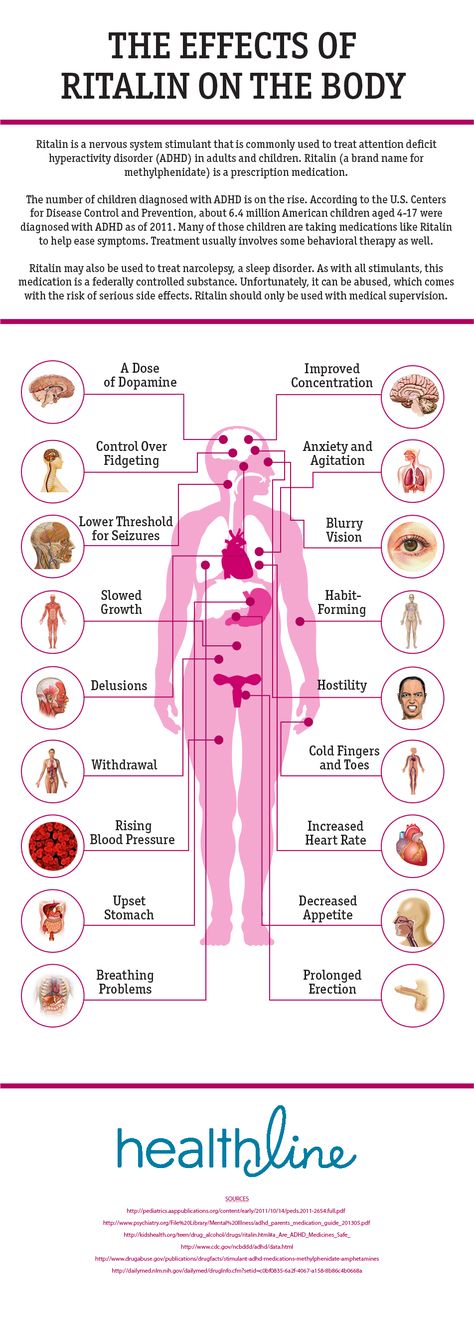
Medications and psychotherapy are effective for most people with depression. Your primary care doctor or psychiatrist can prescribe medications to relieve symptoms.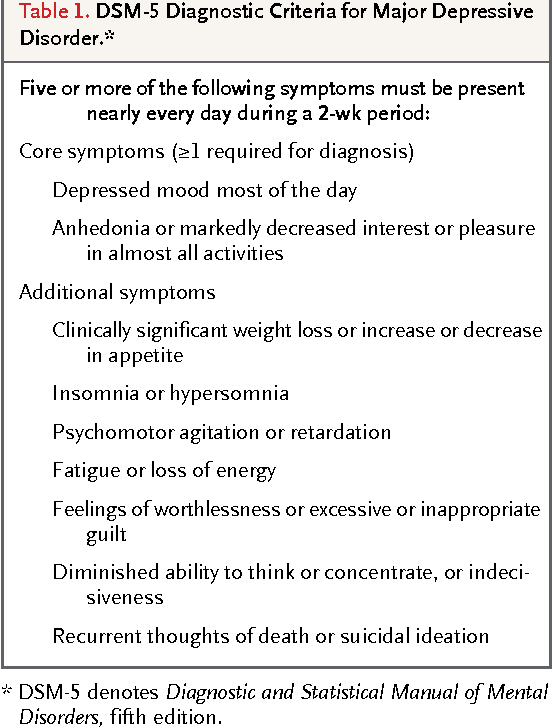 However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
If you have severe depression, you may need a hospital stay, or you may need to participate in an outpatient treatment program until your symptoms improve.
Here's a closer look at depression treatment options.
Medications
Many types of antidepressants are available, including those below. Be sure to discuss possible major side effects with your doctor or pharmacist.
- Selective serotonin reuptake inhibitors (SSRIs). Doctors often start by prescribing an SSRI. These drugs are considered safer and generally cause fewer bothersome side effects than other types of antidepressants. SSRIs include citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft) and vilazodone (Viibryd).
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Examples of SNRIs include duloxetine (Cymbalta), venlafaxine (Effexor XR), desvenlafaxine (Pristiq, Khedezla) and levomilnacipran (Fetzima).
- Atypical antidepressants. These medications don't fit neatly into any of the other antidepressant categories. They include bupropion (Wellbutrin XL, Wellbutrin SR, Aplenzin, Forfivo XL), mirtazapine (Remeron), nefazodone, trazodone and vortioxetine (Trintellix).
- Tricyclic antidepressants. These drugs — such as imipramine (Tofranil), nortriptyline (Pamelor), amitriptyline, doxepin, trimipramine (Surmontil), desipramine (Norpramin) and protriptyline (Vivactil) — can be very effective, but tend to cause more-severe side effects than newer antidepressants. So tricyclics generally aren't prescribed unless you've tried an SSRI first without improvement.
- Monoamine oxidase inhibitors (MAOIs). MAOIs — such as tranylcypromine (Parnate), phenelzine (Nardil) and isocarboxazid (Marplan) — may be prescribed, typically when other drugs haven't worked, because they can have serious side effects. Using MAOIs requires a strict diet because of dangerous (or even deadly) interactions with foods ― such as certain cheeses, pickles and wines ― and some medications and herbal supplements.
 Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs.
Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs. - Other medications. Other medications may be added to an antidepressant to enhance antidepressant effects. Your doctor may recommend combining two antidepressants or adding medications such as mood stabilizers or antipsychotics. Anti-anxiety and stimulant medications also may be added for short-term use.
Finding the right medication
If a family member has responded well to an antidepressant, it may be one that could help you. Or you may need to try several medications or a combination of medications before you find one that works. This requires patience, as some medications need several weeks or longer to take full effect and for side effects to ease as your body adjusts.
Inherited traits play a role in how antidepressants affect you. In some cases, where available, results of genetic tests (done by a blood test or cheek swab) may offer clues about how your body may respond to a particular antidepressant. However, other variables besides genetics can affect your response to medication.
However, other variables besides genetics can affect your response to medication.
Risks of abruptly stopping medication
Don't stop taking an antidepressant without talking to your doctor first. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur.
Stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, and quitting suddenly may cause a sudden worsening of depression. Work with your doctor to gradually and safely decrease your dose.
Antidepressants and pregnancy
If you're pregnant or breast-feeding, some antidepressants may pose an increased health risk to your unborn child or nursing child. Talk with your doctor if you become pregnant or you're planning to become pregnant.
Antidepressants and increased suicide risk
Most antidepressants are generally safe, but the Food and Drug Administration (FDA) requires all antidepressants to carry a black box warning, the strictest warning for prescriptions. In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
Anyone taking an antidepressant should be watched closely for worsening depression or unusual behavior, especially when starting a new medication or with a change in dosage. If you or someone you know has suicidal thoughts when taking an antidepressant, immediately contact a doctor or get emergency help.
Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
Psychotherapy
Psychotherapy is a general term for treating depression by talking about your condition and related issues with a mental health professional. Psychotherapy is also known as talk therapy or psychological therapy.
Different types of psychotherapy can be effective for depression, such as cognitive behavioral therapy or interpersonal therapy.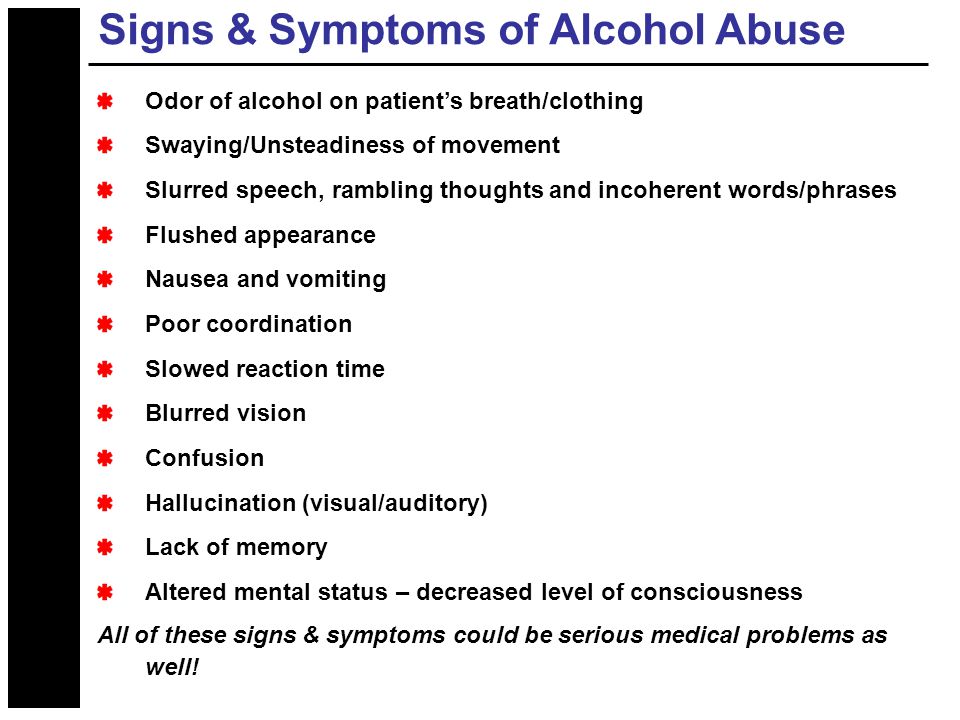 Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
- Adjust to a crisis or other current difficulty
- Identify negative beliefs and behaviors and replace them with healthy, positive ones
- Explore relationships and experiences, and develop positive interactions with others
- Find better ways to cope and solve problems
- Identify issues that contribute to your depression and change behaviors that make it worse
- Regain a sense of satisfaction and control in your life and help ease depression symptoms, such as hopelessness and anger
- Learn to set realistic goals for your life
- Develop the ability to tolerate and accept distress using healthier behaviors
Alternate formats for therapy
Formats for depression therapy as an alternative to face-to-face office sessions are available and may be an effective option for some people. Therapy can be provided, for example, as a computer program, by online sessions, or using videos or workbooks. Programs can be guided by a therapist or be partially or totally independent.
Programs can be guided by a therapist or be partially or totally independent.
Before you choose one of these options, discuss these formats with your therapist to determine if they may be helpful for you. Also, ask your therapist if he or she can recommend a trusted source or program. Some may not be covered by your insurance and not all developers and online therapists have the proper credentials or training.
Smartphones and tablets that offer mobile health apps, such as support and general education about depression, are not a substitute for seeing your doctor or therapist.
Hospital and residential treatment
In some people, depression is so severe that a hospital stay is needed. This may be necessary if you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else. Psychiatric treatment at a hospital can help keep you calm and safe until your mood improves.
Partial hospitalization or day treatment programs also may help some people. These programs provide the outpatient support and counseling needed to get symptoms under control.
These programs provide the outpatient support and counseling needed to get symptoms under control.
Other treatment options
For some people, other procedures, sometimes called brain stimulation therapies, may be suggested:
- Electroconvulsive therapy (ECT). In ECT, electrical currents are passed through the brain to impact the function and effect of neurotransmitters in your brain to relieve depression. ECT is usually used for people who don't get better with medications, can't take antidepressants for health reasons or are at high risk of suicide.
- Transcranial magnetic stimulation (TMS). TMS may be an option for those who haven't responded to antidepressants. During TMS, a treatment coil placed against your scalp sends brief magnetic pulses to stimulate nerve cells in your brain that are involved in mood regulation and depression.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Atypical antidepressants
- Monoamine oxidase inhibitors (MAOIs)
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- MAOIs and diet: Is it necessary to restrict tyramine?
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Depression generally isn't a disorder that you can treat on your own. But in addition to professional treatment, these self-care steps can help:
- Stick to your treatment plan. Don't skip psychotherapy sessions or appointments. Even if you're feeling well, don't skip your medications. If you stop, depression symptoms may come back, and you could also experience withdrawal-like symptoms. Recognize that it will take time to feel better.
- Learn about depression. Education about your condition can empower you and motivate you to stick to your treatment plan. Encourage your family to learn about depression to help them understand and support you.
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your depression symptoms. Make a plan so that you know what to do if your symptoms get worse. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
 Ask relatives or friends to help watch for warning signs.
Ask relatives or friends to help watch for warning signs. - Avoid alcohol and recreational drugs. It may seem like alcohol or drugs lessen depression symptoms, but in the long run they generally worsen symptoms and make depression harder to treat. Talk with your doctor or therapist if you need help with alcohol or substance use.
- Take care of yourself. Eat healthy, be physically active and get plenty of sleep. Consider walking, jogging, swimming, gardening or another activity that you enjoy. Sleeping well is important for both your physical and mental well-being. If you're having trouble sleeping, talk to your doctor about what you can do.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Depression, anxiety and exercise
Alternative medicine
Alternative medicine is the use of a nonconventional approach instead of conventional medicine. Complementary medicine is a nonconventional approach used along with conventional medicine — sometimes called integrative medicine.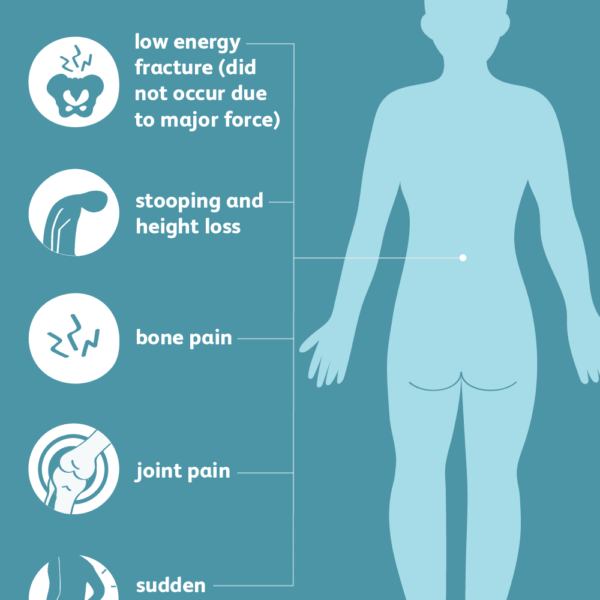
Make sure you understand the risks as well as possible benefits if you pursue alternative or complementary therapy. Don't replace conventional medical treatment or psychotherapy with alternative medicine. When it comes to depression, alternative treatments aren't a substitute for medical care.
Supplements
Examples of supplements that are sometimes used for depression include:
- St. John's wort. Although this herbal supplement isn't approved by the Food and Drug Administration (FDA) to treat depression in the U.S., it may be helpful for mild or moderate depression. But if you choose to use it, be careful — St. John's wort can interfere with a number of medications, such as heart drugs, blood-thinning drugs, birth control pills, chemotherapy, HIV/AIDS medications and drugs to prevent organ rejection after a transplant. Also, avoid taking St. John's wort while taking antidepressants because the combination can cause serious side effects.
- SAMe.
 Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder.
Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder. - Omega-3 fatty acids. These healthy fats are found in cold-water fish, flaxseed, flax oil, walnuts and some other foods. Omega-3 supplements are being studied as a possible treatment for depression. While considered generally safe, in high doses, omega-3 supplements may interact with other medications. More research is needed to determine if eating foods with omega-3 fatty acids can help relieve depression.
Nutritional and dietary products aren't monitored by the FDA the same way medications are. You can't always be certain of what you're getting and whether it's safe. Also, because some herbal and dietary supplements can interfere with prescription medications or cause dangerous interactions, talk to your doctor or pharmacist before taking any supplements.
Mind-body connections
Integrative medicine practitioners believe the mind and body must be in harmony for you to stay healthy. Examples of mind-body techniques that may be helpful for depression include:
- Acupuncture
- Relaxation techniques such as yoga or tai chi
- Meditation
- Guided imagery
- Massage therapy
- Music or art therapy
- Spirituality
- Aerobic exercise
Relying solely on these therapies is generally not enough to treat depression. They may be helpful when used in addition to medication and psychotherapy.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Natural remedies for depression: Are they effective?
Coping and support
Talk with your doctor or therapist about improving your coping skills, and try these tips:
- Simplify your life. Cut back on obligations when possible, and set reasonable goals for yourself.
 Give yourself permission to do less when you feel down.
Give yourself permission to do less when you feel down. - Write in a journal. Journaling, as part of your treatment, may improve mood by allowing you to express pain, anger, fear or other emotions.
- Read reputable self-help books and websites. Your doctor or therapist may be able to recommend books or websites to read.
- Locate helpful groups. Many organizations, such as the National Alliance on Mental Illness (NAMI) and the Depression and Bipolar Support Alliance, offer education, support groups, counseling and other resources to help with depression. Employee assistance programs and religious groups also may offer help for mental health concerns.
- Don't become isolated. Try to participate in social activities, and get together with family or friends regularly. Support groups for people with depression can help you connect to others facing similar challenges and share experiences.
- Learn ways to relax and manage your stress. Examples include meditation, progressive muscle relaxation, yoga and tai chi.
- Structure your time. Plan your day. You may find it helps to make a list of daily tasks, use sticky notes as reminders or use a planner to stay organized.
- Don't make important decisions when you're down. Avoid decision-making when you're feeling depressed, since you may not be thinking clearly.
Preparing for your appointment
You may see your primary care doctor, or your doctor may refer you to a mental health professional. Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for your appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins or other supplements that you're taking, including dosages
- Questions to ask your doctor or mental health professional
Take a family member or friend along, if possible, to help you remember all of the information provided during the appointment.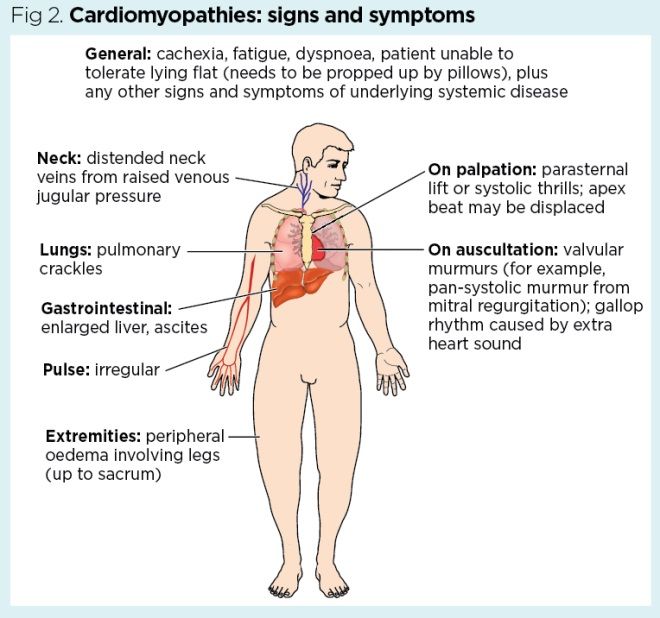
Some basic questions to ask your doctor include:
- Is depression the most likely cause of my symptoms?
- What are other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatment is likely to work best for me?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a psychiatrist or other mental health professional?
- What are the main side effects of the medications you're recommending?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first notice your symptoms of depression?
- How long have you felt depressed? Do you generally always feel down, or does your mood fluctuate?
- Does your mood ever swing from feeling down to feeling intensely happy (euphoric) and full of energy?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with depression or another mood disorder?
- What other mental or physical health conditions do you have?
- Do you drink alcohol or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.
Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Duchenne myodystrophy (muscular dystrophy) - ALL about the disease
Duchenne dystrophy is a hereditary neuromuscular disease that manifests itself in boys and is characterized by progressive muscle weakness and fatigue, symmetrical pseudohypertrophies of the legs and symmetrical atrophies of other muscles in combination with osteoarticular deformities, cardiovascular and respiratory disorders. Duchenne muscular dystrophy has an X-linked recessive type of inheritance, the English abbreviation DMD is denoted as the name of the gene dystrophin , and the name of the disease is Duchenne muscular dystrophy.
Duchenne muscular dystrophy has an X-linked recessive type of inheritance, the English abbreviation DMD is denoted as the name of the gene dystrophin , and the name of the disease is Duchenne muscular dystrophy.
If you are a relative, doctor, or just know someone with Duchenne or Becker muscular dystrophy, please tell them about the MyMyo National Registry. In the Register, we combine data on all patients with DMD/BMD in Russia. The data will make it possible to collect statistics to argue the problems of a rare patient, which in turn will increase the level of argumentation in protecting the rights of people with Duchenne/Becker muscular dystrophy, will help build a model of medical care, which means helping such patients more and more efficiently. nine0007
Together we are stronger, join us!
Basic information about the disease
- This condition (previously often referred to as Duchenne myopathy) progresses rapidly.
 On average, at the age of 8-12 years, the ability to move independently occurs. Cardiomyopathy develops and cardiac and respiratory failure progresses. nine0017 Corticosteroid therapy allows the patient to prolong the time of ability to move independently
On average, at the age of 8-12 years, the ability to move independently occurs. Cardiomyopathy develops and cardiac and respiratory failure progresses. nine0017 Corticosteroid therapy allows the patient to prolong the time of ability to move independently - Proactive administration of ACE inhibitors and beta-blockers will help protect the heart
- Proper rehabilitation measures (use of technical rehabilitation aids (RTD) and physical management) can prevent early spinal curvature, chest deformity, and multiple large joint contractures. nine0018
Causes of Duchenne muscular dystrophy
Etiology and pathogenesis The DMD dystrophin gene is localized on the short arm of the X chromosome (Xp21.2–p21.1 locus). This is one of the largest human genes, which is why sporadic mutations occur so often in it (up to 40%). The disease in 60% of cases is inherited by boys from female carriers, as a typical X-linked recessive inheritance.
The absence of dystrophin (as occurs in Duchenne muscular dystrophy) entails a violation of the integrity of the sarcolemma, the destruction of myocytes and their replacement with adipose and connective tissue. Clinically, this process is expressed by a progressive decrease in the ability of muscles to contract, loss of muscle strength and tone, and muscle atrophy. nine0007
The pathogenesis of Duchenne myodystrophy includes immunopathological processes. The process of regeneration is disturbed in the body, and almost immediately after birth, a cascade of inflammatory reactions is launched. Due to the resulting defect in the lipid layer of the sarcolemma, its permeability increases, which provokes rhabdomyolysis. Through the missing protective cell barrier, intracellular CPK enters the blood, and extracellular calcium enters myocytes.
Duchenne myopathy symptoms
Clinical disease cardThere are 5 stages of the disease.
| Stage | Description, features | |
|---|---|---|
| 1 | Presymptomatic | Increased levels of CPK, LDH, AST and ALT in a biochemical blood test. nine0062 |
| 2 | Early (outpatient) The ability to move independently is preserved | Use of Gowers' techniques when standing up, myopathic "duck" gait, walking on toes. The child climbs the steps with a side step and / or with support. |
| 3 | nine0061 Late (outpatient) The ability to move independently is preservedIncreasing difficulty walking, loss of ability to climb stairs and get up from the floor. | |
| 4 | Early (non-ambulatory) Lost the ability to move independently | nine0061 The patient is able to move independently for some time, is able to maintain the position of the body. High risks of developing skeletal deformities, cardiomyopathy and respiratory disorders.|
| 5 | Late (non-ambulatory) Lost the ability to move independently | Increasing limitation of upper limb function, skeletal deformities, cardiomyopathy and respiratory disorders. Difficulty maintaining body position. nine0062 Difficulty maintaining body position. nine0062 |
Newborns with Duchenne muscular dystrophy may not have significant or noticeable abnormalities. Then, for the first months and even a year, the motor development of the child occurs within the normal range or with a slight delay. Up to 30% of patients in the first year of life have a lag in psychoverbal development. Also, these children, more often than the average in the population, are diagnosed with autism spectrum disorders.
nine0002 Up to 10% of patients with Duchenne PMD may have clinical manifestations in the 1st year of life in the form of a “sluggish child” symptom complex. The main symptoms are weakness of the muscles of the pelvic girdle, pathological muscle fatigue during exercise. Change in gait according to the "duck" type - by the age of 4-5, a gait defect is formed: the patient spreads his legs wide, when walking he rolls from side to side, moves on his toes, patients help themselves with their hands, waving them strongly when walking. On average, patients with Duchenne myopathy lose the ability to move independently from 8 to 12 years of age. However, there are patients who have lost the ability to move independently at the age of 6, and patients who move independently at the age of 16-17. Apparently, this depends on the individual characteristics of the course of the disease. nine0007
On average, patients with Duchenne myopathy lose the ability to move independently from 8 to 12 years of age. However, there are patients who have lost the ability to move independently at the age of 6, and patients who move independently at the age of 16-17. Apparently, this depends on the individual characteristics of the course of the disease. nine0007 Cardiovascular disorders - pulse lability, blood pressure, muffled tones, expansion of the boundaries of the heart, heart failure. Approximately 73% of the population have manifestations of cardiac pathology. The cardiovascular system is involved in the pathological process quite early. There are changes in the myocardium (blockade of the legs of the bundle of His, etc.).
Diagnosis of Duchenne muscular dystrophy
The first step in the diagnosis of suspected Duchenne Study of the activity of CPK in blood serum.
In Duchenne myopathy, myocytes break down (rhabdomyolysis) and release CPK and other cytolysis products into the blood.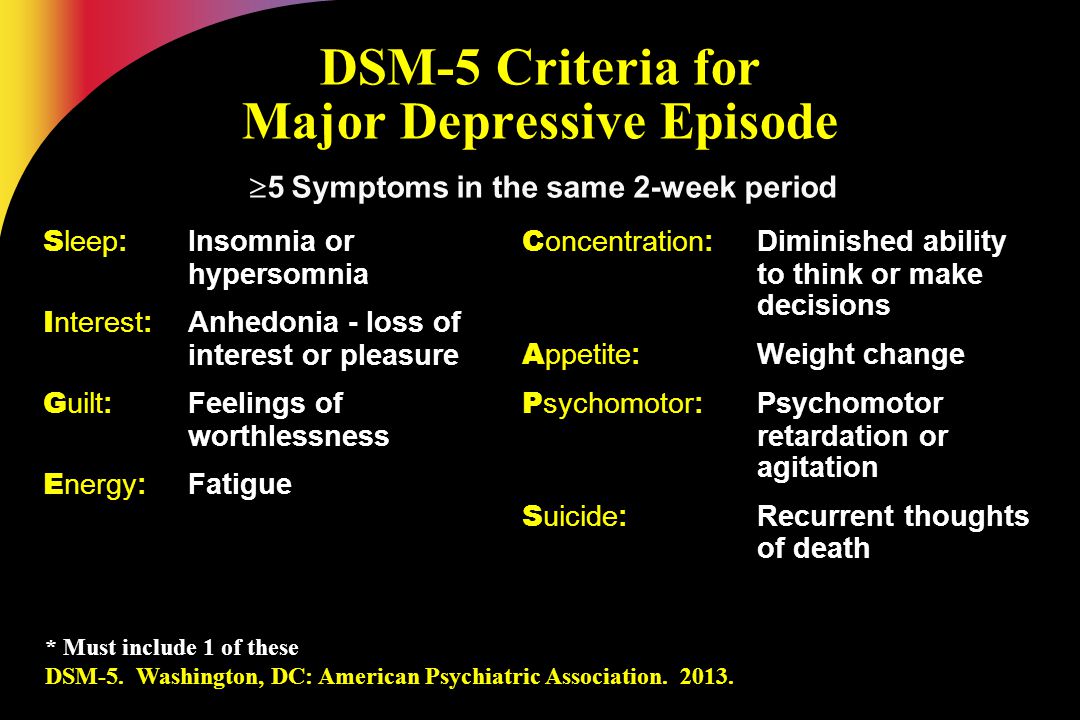 Therefore, the level of CPK in the blood is significantly increased. Deviations in the level of CPK activity by 100 or more times. Thus, the study of the activity of CPK in the blood serum can be the first step in the diagnosis of the disease.
Therefore, the level of CPK in the blood is significantly increased. Deviations in the level of CPK activity by 100 or more times. Thus, the study of the activity of CPK in the blood serum can be the first step in the diagnosis of the disease.
To verify the diagnosis Progressive Duchenne muscular dystrophy genetic diagnostics.
DNA testing Genetic testing usually begins with a simple MLPA (Multiplex ligation-dependent probe amplification) method, which allows you to check the presence of all 79 exons in the DMD gene - this way a deletion of exons / s can be detected .
Identification duplications of are handled by modified MLPA. If the mutation has not been identified, sequencing of the DMD gene is used to detect point mutations. Various types of genetic studies provide more detailed information about changes in the structure (mutations) of DNA in Duchenne PMD. For the study, 2 ml of venous blood is needed. Confirmation of the diagnosis by the results of a genetic study allows the child to be included in clinical trials, and for his parents to develop recommendations for prenatal diagnosis in future pregnancies. After determining the mutation (changes in the dystrophin gene), the mother of the child is invited to undergo a genetic test to identify the carriage of the mutation in the DMD gene. Such information is important for other female relatives on the mother's side (her sisters, daughters, aunts, cousins), as they may also be carriers of this mutation. nine0007
It is possible to carry out prenatal diagnosis of Duchenne PMD by methods of molecular genetic research (material for research from the mother must be taken before the 12th week of pregnancy), as well as preimplantation gene diagnosis in the case of in vitro fertilization.
Treatment of Duchenne muscular dystrophy
Glucocorticoids (or glucocorticosteroids) nine0002 The current anti-inflammatory treatment with corticosteroids is the gold standard described in the international guidelines for the management of patients with Duchenne. Data from randomized controlled trials have shown the benefit of corticosteroids in restoring muscle strength. In addition to the main anti-inflammatory effect (relieves swelling and inflammation, stabilizes the muscle membrane), corticosteroid therapy allows the patient to extend the time of the ability to move independently (walk). Currently, corticosteroids are maintained even after the patient has lost the ability to walk. Continued therapy will help curb the development of scoliosis, maintain muscle strength in the upper limbs, and support respiratory and cardiac function. Because corticosteroids have been used in patients with Duchenne for a long time, it is important to monitor adverse events and complications of such therapy (eg, weight gain, behavioral changes, growth and/or puberty retardation, etc. ). nine0007 Cardioprotective therapy
). nine0007 Cardioprotective therapy
Cardiomyopathy and heart failure are major causes of death in patients with DMD.
The goal of cardioprotective therapy is to reduce the load on the myocardium. The effectiveness of the appointment of ACE inhibitors for the prevention of dilated cardiomyopathy has been proven. For example, one of the first was a study by the Institute of Myology in Paris, which showed that with the early appointment of ACE inhibitors by the age of 15, cardiomyopathy formed in only 20-30 percent of patients instead of 70 percent, as it was before. Also prescribed drugs that reduce heart rate - beta-blockers. This refers to the stage of compensation. nine0007 Cardiometabolic therapy (L-carnitine, coenzyme Q10)
At the stage of decompensation, the specialist may recommend additional drugs (eg, cardiotonic).
Metabolic therapy For the prevention of osteoporosis, the appointment of drugs containing vitamin D3 and calcium is indicated.
The goal of etiotropic treatment is to eliminate the cause of the disease - a mutation in the DMD gene, thereby restoring the synthesis of dystrophin. Currently, several drugs that restore protein synthesis are approved in the world. nine0007 Nonsense mutation. Stop codon
Approximately 10-15% of DMD is caused by point mutations leading to the formation of a premature stop codon, that is, a premature stop in the synthesis of the dystrophin protein. Ataluren (Translarna, PTC Therapeutics, USA) is designed to skip premature stop codons. Ataluren binds to ribosomal RNA and impairs premature stop codon recognition, which allows restoration of translation and synthesis of modified dystrophin. nine0007 Skipping exon/s
The violation of the reading frame (the process of synthesis of the protein dystrophin) in most cases is associated with deletions and duplications, so the main strategy of gene therapy being developed was the method of skipping an exon or exons. This method leads to the restoration of the reading frame, in other words, the resumption of expression of the truncated dystrophin. Restoration of expression of partially functional dystrophin should convert the malignant form of DMD with severe phenotypic presentation to BMD, Becker muscular dystrophy. This treatment can help most patients with Duchenne muscular dystrophy. Exceptions are deletions that destroy actin-binding domains in the N-terminal region or affect the first or last exons and large chromosomal rearrangements. Such mutations are quite rare and together make up less than 10% of all described mutations in the DMD gene. Currently, three drugs have been approved using exon skipping with AOH antisense oligonucleotides. nine0007 Other gene therapy drug developments underway
This method leads to the restoration of the reading frame, in other words, the resumption of expression of the truncated dystrophin. Restoration of expression of partially functional dystrophin should convert the malignant form of DMD with severe phenotypic presentation to BMD, Becker muscular dystrophy. This treatment can help most patients with Duchenne muscular dystrophy. Exceptions are deletions that destroy actin-binding domains in the N-terminal region or affect the first or last exons and large chromosomal rearrangements. Such mutations are quite rare and together make up less than 10% of all described mutations in the DMD gene. Currently, three drugs have been approved using exon skipping with AOH antisense oligonucleotides. nine0007 Other gene therapy drug developments underway
The most anticipated is a universal drug or method that can be used for any kind of mutation in the dystrophin gene.
Mini and microdystrophin or method CRISPR/Cas9 can be called such preparation.
Disease prognosis
The introduction of a multidisciplinary approach and adherence to standards of care has increased the life expectancy of patients with Duchenne muscular dystrophy in the world according to a retrospective analysis to an average of 27.9years (from 23 to 38.6 years).
Links to used articles:Saito T, Kawai M, Kimura E et al. Study of Duchenne muscular dystrophy long-term survivors aged 40 years and older living in specialized institutions in Japan. Neuromuscul Discord. 2017 Feb;27(2):107-114. doi: 10.1016/j.nmd.2016.11.012.
Passamano L., Taglia A., Palladino A. Improvement of survival in Duchenne Muscular Dystrophy: a retrospective analysis of 835 patients. Acta Myol. 2012 Oct; 31(2): 121–125. nine0007
Skuk D, Goulet M, Roy B, Chapdelaine P, Bouchard JP, Roy R, et al. Dystrophin expression in muscles of Duchenne muscular dystrophy patients after high-density injections of normal myogenic cells. J Neuropathol Exp Neurol. 2006;65(4):371–86. https://doi.org/10.1097/01. jnen.0000218443.45782
J Neuropathol Exp Neurol. 2006;65(4):371–86. https://doi.org/10.1097/01. jnen.0000218443.45782
The article is for informational and fact-finding purposes. Diagnosis of the disease and treatment is possible only under the supervision of specialists
description, features of infection, diagnosis and treatment
- Causes of Duchenne myopathy
- Symptoms and clinical picture of the disease
- Diagnostics
- Treatment of myopathy
- Forecast
Image by Freepik
Duchenne muscular dystrophy or Duchenne myopathy is a rare hereditary disease that is passed from mother to son. Women themselves do not suffer from this pathology. The disease is diagnosed in one in 3500-4000 boys and manifests itself at an early age. nine0007
Causes of Duchenne myopathy
The root cause of muscular dystrophy is a mutation (duplication or deletion) in the dystrophin gene, which is located on the X chromosome. Because boys only have one X chromosome, they are more susceptible to this condition. In girls, pathology occurs, but it is extremely rare, and it is expressed with mild symptoms: myocardial damage, slight muscle weakness.
Because boys only have one X chromosome, they are more susceptible to this condition. In girls, pathology occurs, but it is extremely rare, and it is expressed with mild symptoms: myocardial damage, slight muscle weakness.
Among women, an analysis is carried out to identify a genetic mutation that leads to the development of the disease in a child. The study is effective in 80% of cases. nine0007
However, a normal test result does not always exclude the risk of developing a fetus with this disease:
- some cases of Duchenne myopathy are caused by other mutations, such as a point mutation;
- up to 30% of cases of diseases that are diagnosed as muscular dystrophy develop not as a result of inheritance of maternal genes, but due to a new mutation in the fetus.
In Russia, this analysis is done free of charge. nine0004
The sons of a woman who carries the disease gene have a 50% chance of developing myopathy. Daughters will become carriers of the same gene.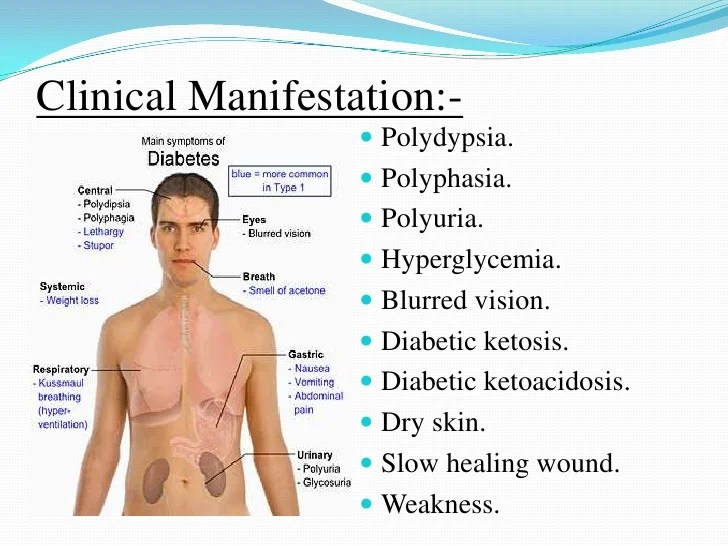
Symptoms and clinical picture of the disease
Dystrophin, a protein found in muscle tissue, is essential for normal muscle function. In patients with Duchenne myopathy, this substance is not enough. Over time, muscle fibers become damaged and weaken.
The first manifestations of the disease are observed in children aged 2-3 years. It all starts with the defeat of the lower extremities, which affects the gait: the child waddles, begins to move on his fingers. It is difficult for children with this disease to perform active actions: run, jump, get up from the floor and climb stairs. They are more prone to fractures because they fall more often than others. Then the pathology affects the pelvic and spinal muscles, chest and upper limbs. Almost all patients have scoliosis and contracture of the limbs. nine0007
With Duchenne myopathy, there is a replacement of individual muscle groups with fibrous or adipose tissue, in particular at the ankles.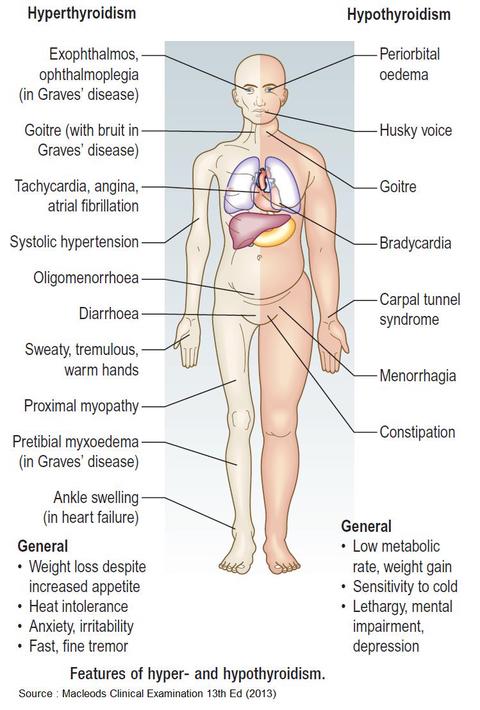 By the age of 12, a wheelchair is required for movement.
By the age of 12, a wheelchair is required for movement.
By the age of 14, 30% of patients and all patients with muscular dystrophy older than 18 years have complications on the heart muscle: arrhythmia, cardiomyopathy, conduction disturbance. However, these pathologies are asymptomatic, since patients are not capable of physical activity. About a third of patients suffer from dementia, which affects verbal ability more than productivity. nine0232 The danger of the disease lies in the late diagnosis. Most parents notice Duchenne at a later age because they are not able to immediately identify movement difficulties.
Overweight affects mainly children who are prescribed corticosteroids. In other adolescent and adult patients, on the contrary, there is a lack of muscle mass. Therefore, in addition to the main treatment, patients need to consult a nutritionist. Fiber is important to prevent constipation. nine0232 In the later stages, many patients have trouble chewing and swallowing food, and in severe cases, a gastrostomy, the surgical insertion of a tube into the stomach for nutrition, may be required.
Diagnostics
To diagnose the disease, an analysis is required for the presence of a mutated gene, in some cases muscle biopsy, electromyography are also prescribed. The prerequisites for examination for Duchenne myopia are a family history, the presence of clinical signs. nine0007
In the presence of disease, a biopsy shows a change in the size and necrosis of muscle fibers that are not separated from the motor units. Also, the patient has an increased level of creatine kinase (100 times higher than the normal level).
The main clinical test confirming the disease is the study of DNA mutations in peripheral blood leukocytes. About 70% of patients with muscular dystrophy have dystrophin deletions, and about 10% have duplications.
Urine analysis, general and biochemical blood tests are also used for diagnosis. A consultation with a geneticist is recommended. nine0007
Treatment of myopathy
There is no specific treatment for Duchenne myopathy. The patient is prescribed supportive measures, in some cases taking deflazacort or prednisone, beta-blockers, ACE inhibitors. A radical method of treatment can be chosen - corrective surgery (in particular for scoliosis).
The patient is prescribed supportive measures, in some cases taking deflazacort or prednisone, beta-blockers, ACE inhibitors. A radical method of treatment can be chosen - corrective surgery (in particular for scoliosis).
Patients are shown light and passive exercises that allow them to maintain their ability to move longer and prevent the development of dysfunctional atrophy. Orthopedic interventions are indicated to prevent contractures. For example, wearing an ankle brace during sleep helps prevent flexion contractures. nine0007
It is important for patients with Duchenne myopathy to maintain a harmonious diet in order to avoid obesity: due to the decrease in motor functions, people with this disease have a lower calorie requirement.
Nasal masks and other types of non-invasive respiratory support are sometimes used to treat respiratory failure. Elective tracheotomy (surgical incision in the trachea to create an alternative breathing path) is becoming more common. This procedure allows patients with Duchenne myopathy to prolong life. nine0007
This procedure allows patients with Duchenne myopathy to prolong life. nine0007
Patients older than 5 years whose motor skills have stopped developing or regressing are prescribed deflazacort or prednisone daily. 10 days after the start of the course, the drugs begin to act. The peak of effectiveness occurs at 3 months from the start of therapy and persists for the next 6 months.
With long-term use, the patient's endurance increases, he loses his motor abilities 1.4–2.5 years later. Also, the treatment has a positive effect on lung function, reduces the need for surgical correction of scoliosis and other orthopedic complications, stabilizes the work of the heart muscle, and increases survival. nine0007
Among the side effects of taking prednisone is weight gain (manifested in the interval of 6–18 months from the moment the drug was started). It also increases the risk of fractures of long bones, the spine.
Forecast
Duchenne myopathy is an incurable disease with a poor prognosis.