Schizophrenia vs did
Dissociative Identity Disorder vs. Schizophrenia
Schizophrenia and DID are complex mental health conditions that people often confuse for one another. While they have some overlapping symptoms, they are different conditions.
A major difference is that someone with DID has two or more distinct identity states, sometimes known as alternate identities, or alters. This is not present in schizophrenia. DID was formerly known as multiple personality disorder or split personality disorder, but clinicians no longer use these terms.
The term “schizophrenia” is derived from the Greek words for “splitting” (schizo) and “mind” (phren), so some people have taken this to mean “split personality.” People with schizophrenia experience symptoms that affect their thoughts, behaviors, and feelings, but they don’t have multiple distinct personalities.
While there’s some overlap between the two conditions, DID and schizophrenia are different in many ways.
There are a lot of misconceptions surrounding both DID and schizophrenia. Many people inaccurately believe that people with schizophrenia have “split personalities.” This isn’t the case.
This isn’t even technically true of DID. The Sidran Institute says that, although these personalities may feel or appear different, “They’re all manifestations of a single, whole person.”
While some symptoms do overlap between DID and schizophrenia, they are different in important ways, including their causes, treatments, and age of onset.
Causes
Neither condition has one definitive cause, but DID is associated with trauma while schizophrenia is more often associated with having certain genes.
Most people with DID have a history of severe childhood trauma. An estimated 90% of people with DID have a history of neglect or abuse. The condition can arise when a child dissociates as a defense mechanism to escape an intolerable reality.
Experts believe several factors play a role in the development of schizophrenia. A main one is your genes. Your environment, brain development and chemicals, and pregnancy complications may also be involved.
Which treatments work better
The first-line treatment for schizophrenia is a second-generation antipsychotic medication. Healthcare professionals may recommend a few other types of medications as well.
Along with medication, treatments for schizophrenia often include:
- different types of psychotherapy (talk therapy)
- family support
- community-based treatment programs
On the other hand, DID doesn’t have an approved medication for treatment. People with DID may take meds to treat coexisting conditions — like antidepressants to improve symptoms of depression — but antipsychotics are unlikely to improve symptoms.
Talk therapy is the primary treatment for DID. Talk therapy helps the person to understand their symptoms and their causes, and to learn ways to manage dissociative episodes. Types include:
- cognitive behavioral therapy (CBT)
- dialectical behavioral therapy (DBT)
Age of onset
One of the major differences between DID and schizophrenia is the age when symptoms typically first begin showing up.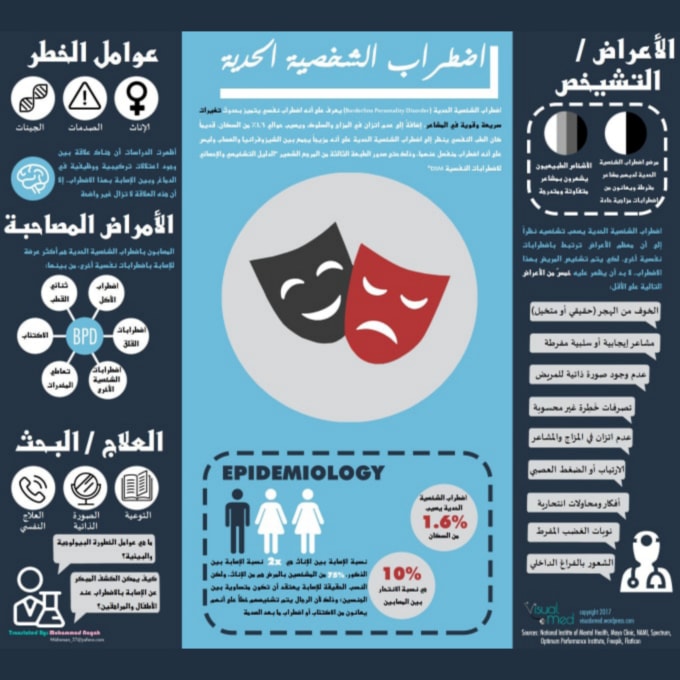 Schizophrenia usually has a later onset — in someone’s late teens to 30s. DID symptoms, on the other hand, typically start showing up in childhood.
Schizophrenia usually has a later onset — in someone’s late teens to 30s. DID symptoms, on the other hand, typically start showing up in childhood.
According to research from 2009, dissociative symptoms usually start between ages 5 to 10 for people with DID. Someone’s first alter may appear around age 6.
Hearing voices
While people with either DID or schizophrenia may hear voices, people with DID who do are reportedly more likely to start hearing them before age 18.
People with schizophrenia don’t usually start having hallucinations until their late teens to early 20s.
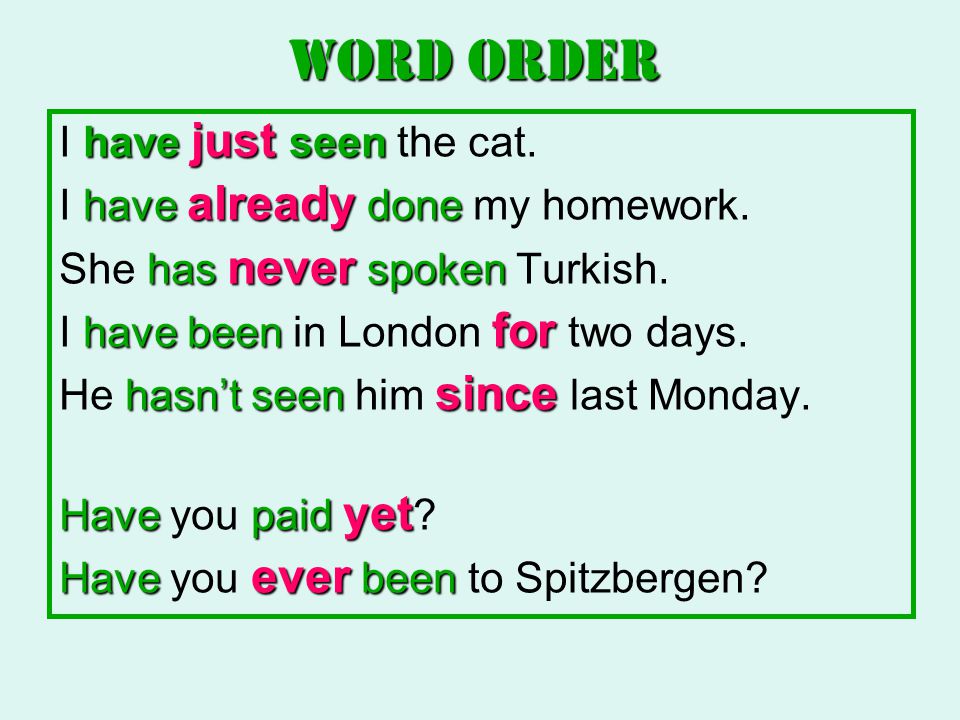
Differences in “hearing voices”People with schizophrenia may experience auditory hallucinations, such as hearing voices. People with DID may hear voices too, with some differences. People with DID typically:
- begin hearing voices earlier in life
- hear more voices
- experience voices that “talk” to one another
- hear a combination of adult and child voices, whereas people with schizophrenia most often only hear adult voices
- report they would miss the voices
Prevalence
About 1% of adults around the world live with schizophrenia.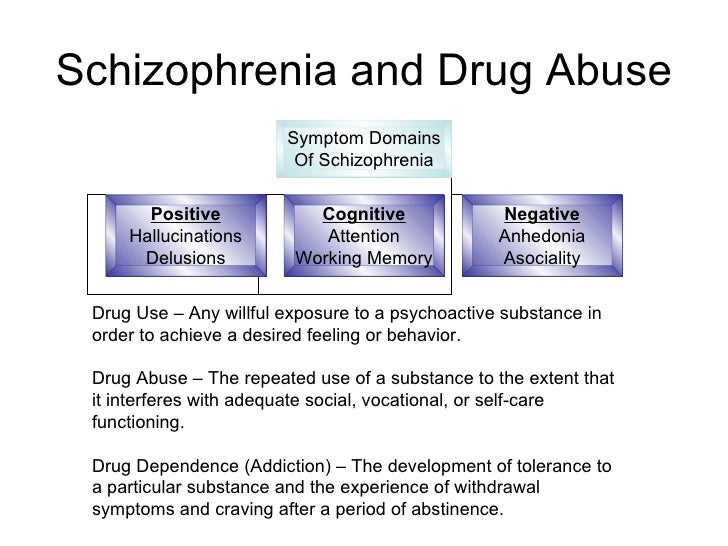 One study estimated that healthcare professionals diagnose schizophrenia in 5.1 per 1,000 people per year in the United States.
One study estimated that healthcare professionals diagnose schizophrenia in 5.1 per 1,000 people per year in the United States.
Worldwide, DID is diagnosed in about 1.5% of people. However, it’s often misdiagnosed, and some people may spend as much as 12 and a half years in treatment before they receive an accurate diagnosis.
Other notable differences
Memory loss, or amnesia, can occur in both schizophrenia and DID, but it’s more common in DID.
People with DID also have higher rates of derealization and depersonalization, according to research. For instance, if someone has “switched” to a different personality, they may look in the mirror and not recognize themselves.
People with schizophrenia may experience depersonalization and derealization, but this is less likely or happens less often.
Cognitive functioning issues and symptoms are often more common in schizophrenia than dissociative disorders.
There are a number of reasons why you might get DID and schizophrenia mixed up.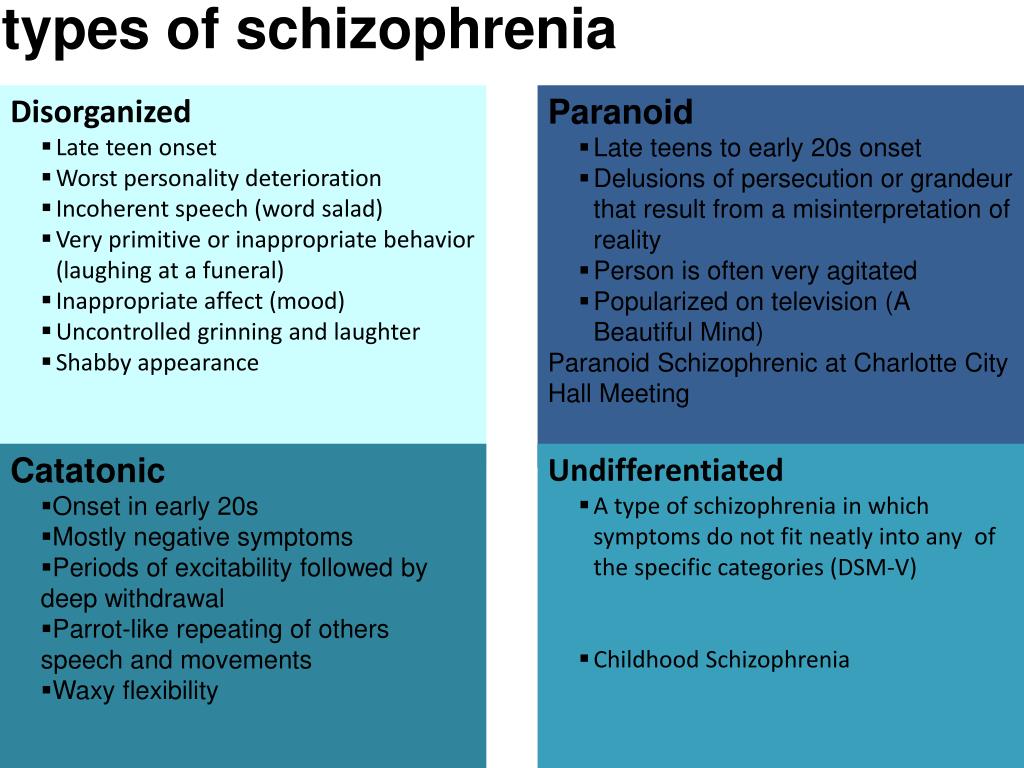
For starters, research has shown a high co-occurrence between dissociative disorders and schizophrenia spectrum disorders: Between 9% and 50% of people with schizophrenia also meet the criteria for a dissociative disorder.
They share some symptoms
One of the biggest reasons why people confuse the two conditions is their overlapping symptoms.
Popular culture portrayals may lead you to believe that hallucinations are unique to schizophrenia. However, people with DID, narcolepsy, and bipolar disorder, along with those who take certain substances, may also experience hallucinations.
Symptoms that DID and schizophrenia may have in common include:
- visual and auditory hallucinations
- issues with memory
- suicidal ideation
- difficulties sleeping
- delusions
- dissociation
Some of these symptoms are similar, so they may also be confused.
People with DID are typically more likely to have symptoms that overlap with positive symptoms of schizophrenia — the ones that involve altered perceptions, reality, and thinking.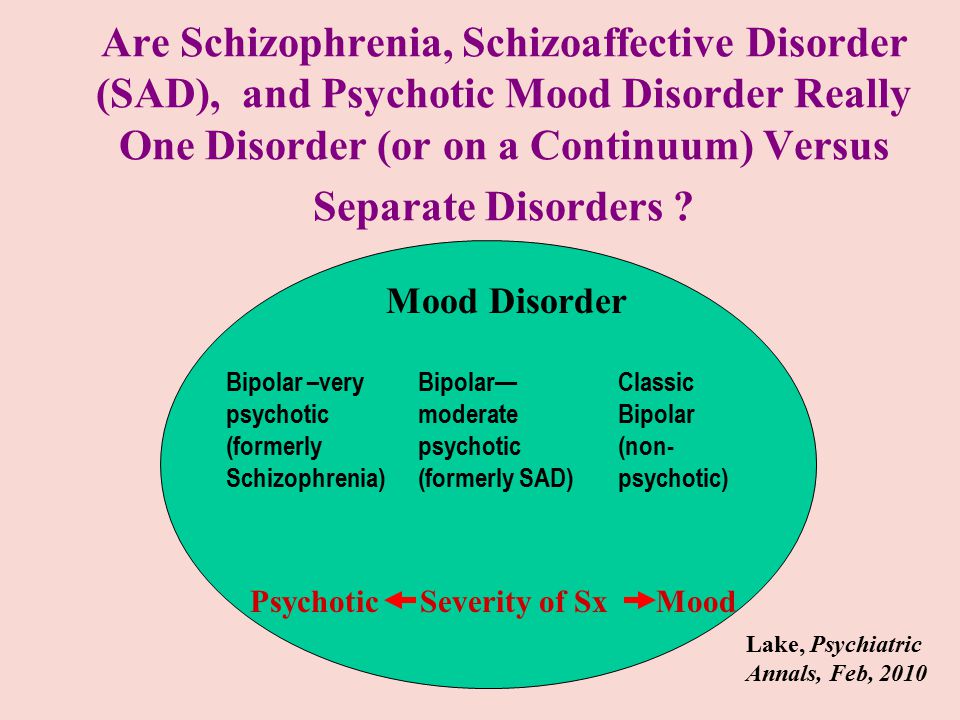 People with DID don’t often show many negative symptoms.
People with DID don’t often show many negative symptoms.
People with schizophrenia are less likely to experience dissociative symptoms. Those that do have them usually experienced some type of trauma.
DID is sometimes misdiagnosed
Healthcare professionals sometimes misdiagnose DID as schizophrenia.
It can be incredibly difficult to get a correct diagnosis of DID. According to research from 2016, only 60% of U.S. clinicians were able to accurately diagnose DID in an individual.
The clinicians misdiagnosed the condition as:
- post-traumatic stress disorder (PTSD)
- schizophrenia
- major depression
One reason for this confusion? Some clinicians might confuse someone’s belief that they have multiple identities with them experiencing delusions. The fact that both conditions can involve hearing voices and other overlapping symptoms can make diagnosis even more complex.
Other misdiagnosesThere are several conditions that can be confused with DID and schizophrenia, and possibly lead to misdiagnosis:
- borderline personality disorder
- bipolar disorder
- PTSD
- major depressive disorder
- schizoaffective disorder
- schizoid personality disorder
Multiple identities ≠ delusions or hallucinations
Some people confuse the multiple identities of DID for the delusions or hallucinations of schizophrenia, but they aren’t the same.
To break down the difference between these symptoms, let’s define them:
- Delusions. False beliefs that are not based in reality. If you have delusions, you believe them despite evidence to the contrary, even if everyone else believes otherwise. There are many types of delusions, including grandiose, bizarre, persecutory, and somatic (involving touch or sensation).
- Hallucinations. False perceptions — when someone sees, hears, or feels something that’s not actually happening. These sensory experiences feel real, but they’re not.
- Multiple identities. Also called alternate identities or “alters,” these occur when someone has more than one personality state. This alternate personality may appear to function separately from another. Alternate identities may have distinct behaviors, memories, expressions, languages, ages, and more. For instance, an alter of a 30-year-old female could be a 12-year-old male.
Coexisting conditions can complicate diagnosis
Other conditions that may simultaneously occur in people with DID and schizophrenia can complicate your symptoms and diagnosis.
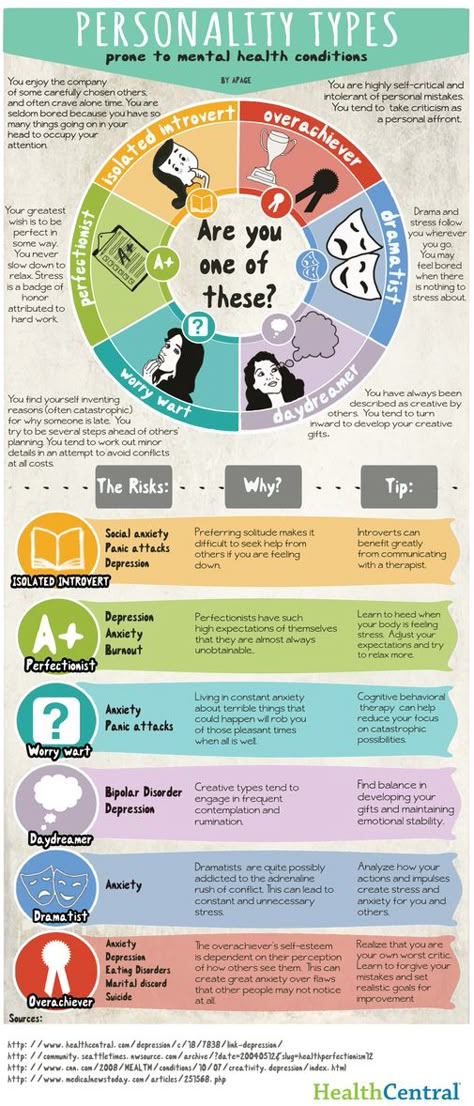
People with DID, particularly, have comorbid conditions or symptoms, such as:
- PTSD
- depression
- anxiety disorders
- substance use disorder
- nonepileptic seizures
- self-harm
- a personality disorder
- eating disorders
- sleep disorders
Someone with schizophrenia may also experience:
- substance use disorder
- anxiety disorders, such as panic disorder
- obsessive-compulsive disorder (OCD)
- a personality disorder
Outdated diagnostic criteria
A lot of the confusion may also come from older diagnostic criteria. As we’ve learned more about mental health, the criteria have become more specific and clear.
Not that long ago, depersonalization was a big part of a schizophrenia diagnosis. Depersonalization is when you feel detached from yourself and your thoughts and feelings. It may feel like an “out of body” experience.
Neither condition has depersonalization listed as a necessity for diagnosis, but it’s now more commonly considered part of dissociative disorders.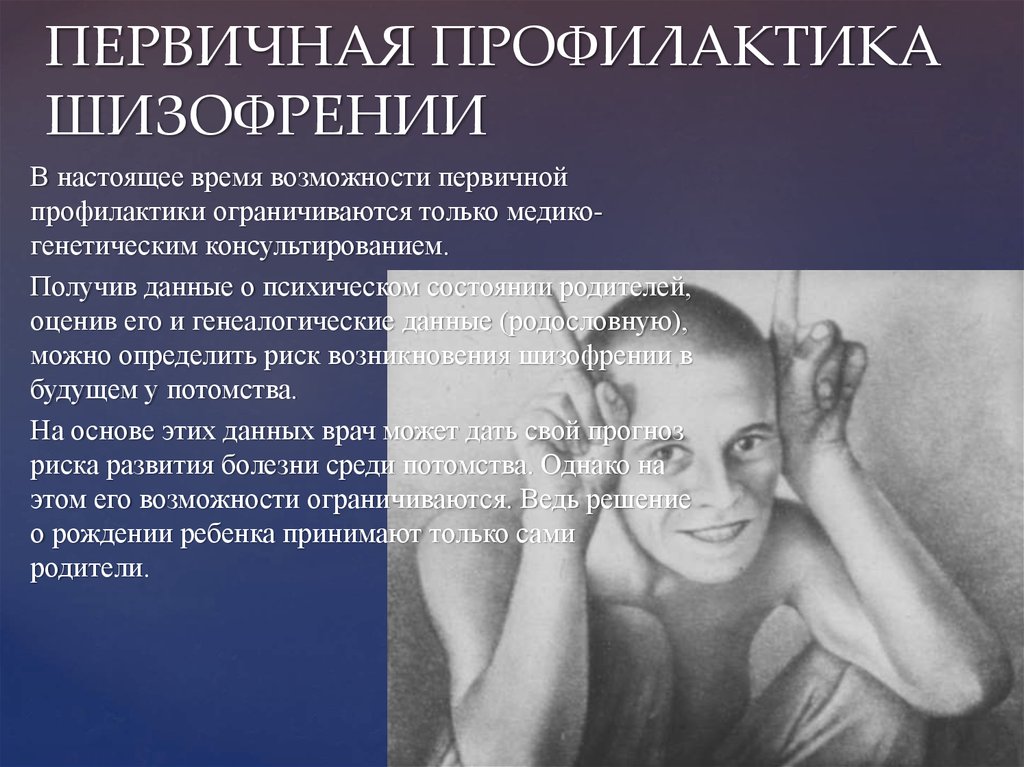 That said, some people with schizophrenia may still have it.
That said, some people with schizophrenia may still have it.
DID is a rare type of dissociative disorder. The main characteristic of DID is having two or more distinct personality states, also called alters or identities. People with DID may say they have more than one self in their mind or body.
The multiple identities are often distinct, with different names, mannerisms, and voices. They might have distinct histories and memories, ages, genders, sexualities, or interests. If you have DID, you might be aware of these identities or completely unaware.
Symptoms
Signs and symptoms of DID may include:
- two or more distinct personality states that affect behaviors, consciousness, memory, and more
- looking like you’re in a trance, blinking or rolling your eyes, or changing your posture when switching alters
- dissociative amnesia — big gaps in memory that are more than just forgetfulness
- dissociative fugue — losing your sense of awareness and engaging in some sort of travel away from home for a short or long period of time
- depersonalization and derealization — feeling detached or disconnected from yourself or the world
- behaviors of self-harm or suicide
- hallucinations, such as hearing voices
- sleep issues, such as insomnia or distressing dreams
For you to receive a DID diagnosis, these symptoms will affect your daily functioning and can’t be due to other causes, such as substance use or other medical conditions. However, someone with DID may use substances or have coexisting conditions.
However, someone with DID may use substances or have coexisting conditions.
In some cultures and religions, dissociation and possession or possession-like identities are an accepted norm, so dissociating in these ways wouldn’t be considered a disorder.
If you’re having thoughts of suicide or self-harm
Help is available right now.
- Call the National Suicide Prevention Lifeline anytime at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.
- Not in the U.S.? Find a helpline in your country with Befrienders Worldwide or the Suicide Stop International Help Center.
Causes and diagnosis
You may have a higher chance of developing DID if you experienced trauma or abuse as a child. Certain parenting styles, neglect, a lack of support or stability, and the ability to dissociate easily are also factors.
While it can be challenging to get accurately diagnosed with DID, reaching out to a mental health professional can be a positive first step.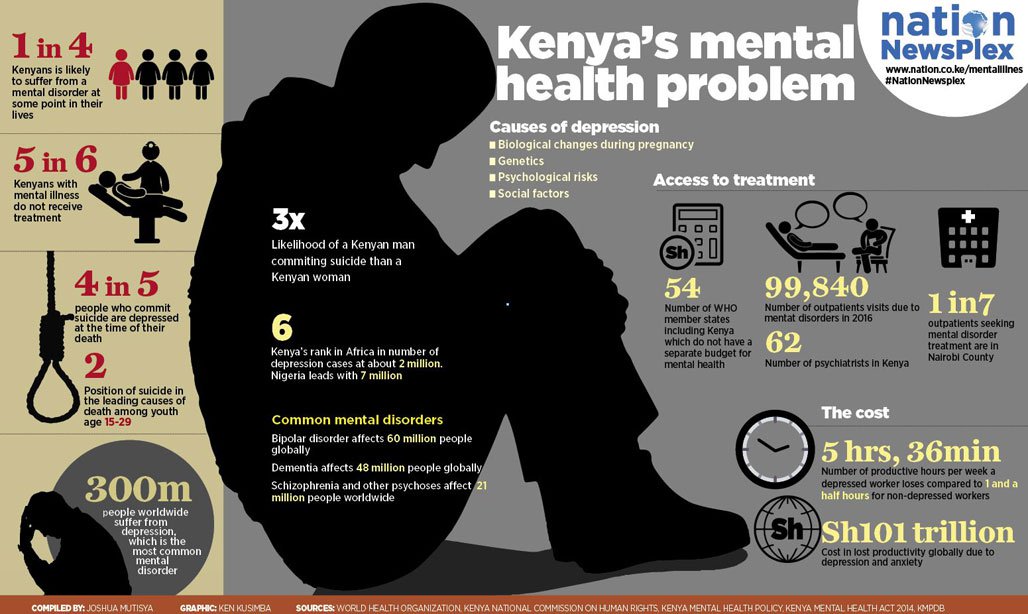 They’ll likely ask you questions about your symptoms, health history, and how you’re functioning in your day to day.
They’ll likely ask you questions about your symptoms, health history, and how you’re functioning in your day to day.
They might also use one of these evaluation tools:
- Dissociative Experiences Scale
- Dissociation Questionnaire
- Difficulties in Emotion Regulation Scale (DERS)
Treatments
While it can be a long road, treatments like talk therapy make managing and living well with DID possible. Everyone’s treatment plan will be personalized, but DID treatments typically involve:
- psychotherapy
- hypnosis
- eye movement desensitization and reprocessing (EMDR)
- coping tools to help regulate emotions, manage stress, and improve daily functioning
While no medications exist that treat DID specifically, healthcare professionals may prescribe meds to treat related symptoms or coexisting conditions.
Schizophrenia is a mental health condition that affects your thoughts, behaviors, and feelings. People often feel as if they’ve lost touch with reality, usually due to hallucinations and delusions.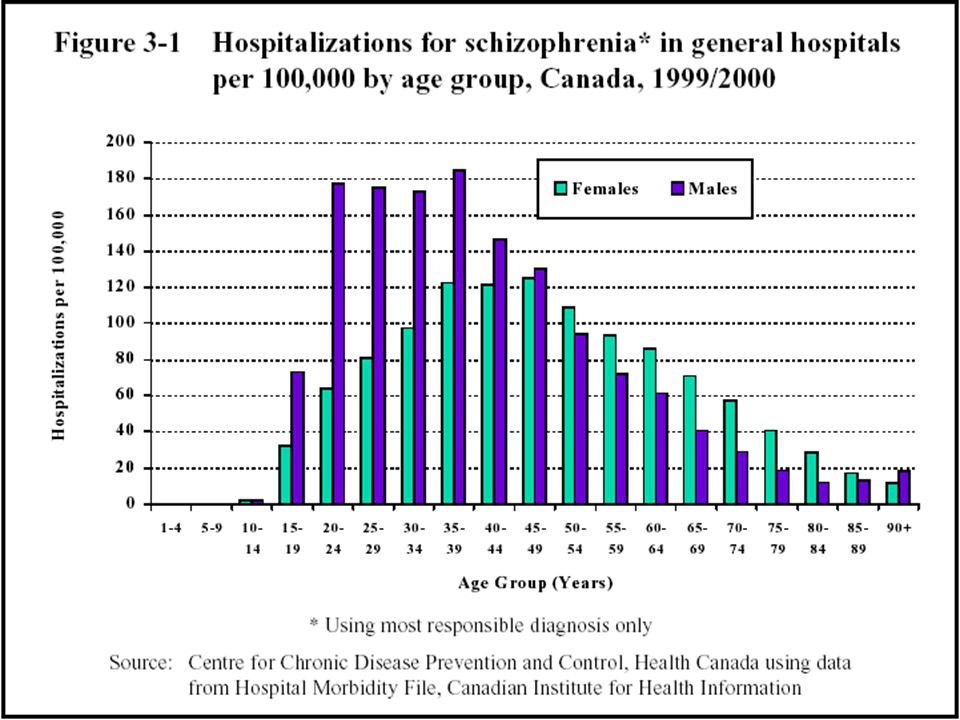 These are some of the most well-known symptoms of schizophrenia.
These are some of the most well-known symptoms of schizophrenia.
Schizophrenia onset usually happens in your teens to 30s. This is when someone has their first episode or starts showing prominent signs. Onset tends to occur earlier in males than females.
Symptoms
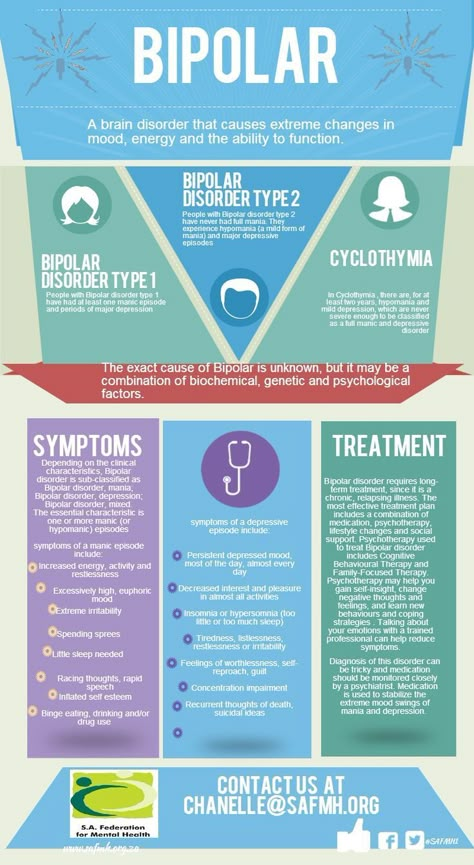
Healthcare professionals often break down the symptoms of schizophrenia into three categories: positive, negative, and cognitive symptoms.
Positive symptoms involve altered perceptions or thinking. You might experience:
- delusions
- hallucinations
- disorganized thinking
- unusual body movements, such as in catatonia
- suicidal thoughts or behaviors
Negative symptoms can be considered the absence of something, such as motivation or emotional expressions. These might look like:
- low motivation
- difficulty planning or following through with activities
- flat affect — a lack of emotional expression
- speaking less
- taking less pleasure in daily life
- social withdrawal
Cognitive symptoms are those that affect your memory or attention. These symptoms can be subtle or noticeable, depending on the person. Some examples include:
These symptoms can be subtle or noticeable, depending on the person. Some examples include:
- trouble making decisions
- having a hard time paying attention or focusing
- difficulty using information that you’ve just learned
Causes and diagnosis
A number of factors may contribute to developing schizophrenia. They include:
- genetics
- environment
- brain structure and function
- changes or differences in neurotransmitters
- social stressors
If you have schizophrenia, you might have received your first evaluation for the condition after experiencing your first episode of schizophrenia or psychosis. In many people, this first episode is severe enough to warrant seeking medical help or hospitalization.
According to the DSM-5, someone must meet the below criteria to receive a diagnosis of schizophrenia:
- two or more positive or negative symptoms most of the time during a 1-month period
- daily ability to function is extremely affected
- continuous signs of issues must occur for at least 6 months
- other mental health conditions or substance use aren’t causing the symptoms
A mental health professional will often talk with you about your health history and symptoms. They may try to rule out other conditions that may be causing your symptoms. To do this, they might give you mental health assessments and physical tests.
They may try to rule out other conditions that may be causing your symptoms. To do this, they might give you mental health assessments and physical tests.
Treatments
There are many tools and treatments available to help you if you’re living with schizophrenia.
Treatment plans often involve a combo of:
- medications, specifically antipsychotics
- psychotherapy
- family education, support, and therapy
- coordinated specialty care (CSC), a treatment program aimed at recovery from your first episode of psychosis
- assertive community treatment, a multidisciplinary team aimed to decrease hospitalizations and homelessness
- coping tools
DID and schizophrenia are two mental health conditions that may be confused for each other, but they aren’t the same. It’s also possible to have both conditions at once or other overlapping conditions that make diagnosis difficult.
If you think you’re experiencing symptoms of these or another condition, consider reaching out to a mental health professional for an evaluation. If you’ve already received a diagnosis of DID or schizophrenia but don’t think it’s the right one, consider getting a second opinion.
If you’ve already received a diagnosis of DID or schizophrenia but don’t think it’s the right one, consider getting a second opinion.
Whether you have schizophrenia, DID, or another condition altogether, you can thrive with the right coping tools, treatments, and support.
If you’re looking for peer support, you can try the Connection Group or Family Support Group from the National Alliance on Mental Illness (NAMI).
Here are additional resources for DID:
- International Society for the Study of Trauma and Dissociation: Find a Therapist
- Sidran Institute: Help Desk
Here are additional resources for schizophrenia:
- Schizophrenia & Psychosis Action Alliance: Peer Support Groups
- National Institute of Mental Health (NIMH): RAISE Resources (Recovery After an Initial Schizophrenia Episode)
- Read more about the best online schizophrenia support groups.
Probing Question: How do schizophrenia and DID differ?
"What will I have for dinner?"
"Is it going to rain later?"
"I wonder what she meant by that.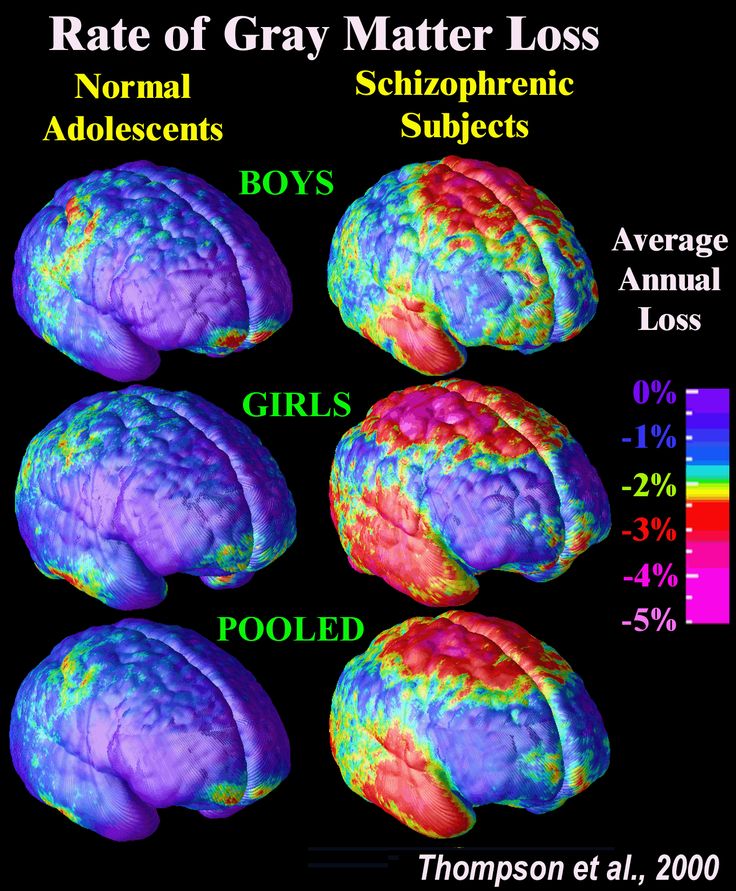 "
"
Questions or comments like these silently passing through our minds reflect how most of us think; they're normal. When the comments heard internally are the voices of other people, however, then psychiatrists suspect schizophrenia.
Among the myths surrounding schizophrenia, one of the most persistent is that it involves a "split personality," two separate and conflicting identities sharing one brain. A National Alliance on Mental Illness survey found that 64 percent of the public shares this misconception.
"It's an extremely common misunderstanding," says Randon Welton, assistant professor of psychiatry at Penn State Milton S. Hershey Medical Center. "It's based on the name. If you go to the Greek roots of the word—schizein, meaning splitting and phren, meaning mind—you have "split brain" or "split mind." However, the intended reference is to a split between rationality and emotions, not a split within a personality, explains Welton.
Split personality, more properly, is an old name for multiple personality disorder, which is itself an outdated name for dissociative identity disorder (DID), an officially recognized but still controversial diagnosis. Welton notes that DID came to the public's attention following the release of books and films such as The Three Faces of Eve and Sybil, accounts of women who developed multiple, distinct personalities following severe abuse as children.
Welton notes that DID came to the public's attention following the release of books and films such as The Three Faces of Eve and Sybil, accounts of women who developed multiple, distinct personalities following severe abuse as children.
"I would describe DID as a trauma-based illness," Welton says. Those affected by it have "at least two and often more distinct identity states which each have fairly consistent patterns of relating to the environment." The American Psychiatric Association definition specifies that "at least two of these identities or personality states recurrently take control of the person's behavior."
By contrast, Welton describes schizophrenia as "a largely genetic illness, one that seems to be clustered within families. It seems to be more neurodevelopmental, influenced by how the brain develops. It usually presents in late teens to young adulthood and is more common than DID, with 2.2 million Americans living with the disease. Explains Welton, "You see a gradual, overall decrease in functioning with acute exacerbation, lasting weeks or months, of overtly psychotic symptoms--unless they are caught and treated. "
"
While trauma is associated with both disorders, Welton explains that "the traditional difference is that with schizophrenia, the trauma tends to follow the disease. It is a consequence of the illness; it is not causative. Trauma doesn't make someone have schizophrenia, whereas for almost everyone with DID I've ever heard about, it is a reaction to the trauma." Schizophrenia is classified as a psychotic disorder and managed primarily through drugs, whereas DID is considered a developmental disorder that is more responsive to psychotherapy and behavioral modifications.
On the surface, the difference between the two disorders seems clear cut. But some psychiatrists, such as Brad Foote of the Albert Einstein College of Medicine, are warning their peers that it may be possible to confuse the two conditions early in the course of treatment. This may happen if voices of alternate personalities in a case of DID "leak through" and comment on events, or talk directly to the core, central personality, without completely taking it over.
"Traditionally, any time a patient reports hearing voices like this, it was a strong indication of schizophrenia," Welton says. "Psychosis is not a diagnostic key for DID but it is a common finding in that they will hear one personality talking to another or a personality commenting on them."
If these observations are accurate, Welton says "it would be very easy to put that person into a psychotic disorder category because you did not ask the right questions or you didn't ask in the right way."
Hearing voices may be more complicated than doctors or patients knew.
Randon Welton, MD, is assistant professor of psychiatry at the Pennsylvania Psychiatric Institute, Penn State Hershey Medical Center. He can be reached at [email protected].
Last Updated October 26, 2010
10 questions about schizophrenia - Gazeta.Ru
Are people with schizophrenia dangerous? Are they boisterous? Hear voices? Are they isolated from society? "Gazeta.Ru" answers questions that are formed by common myths about schizophrenia.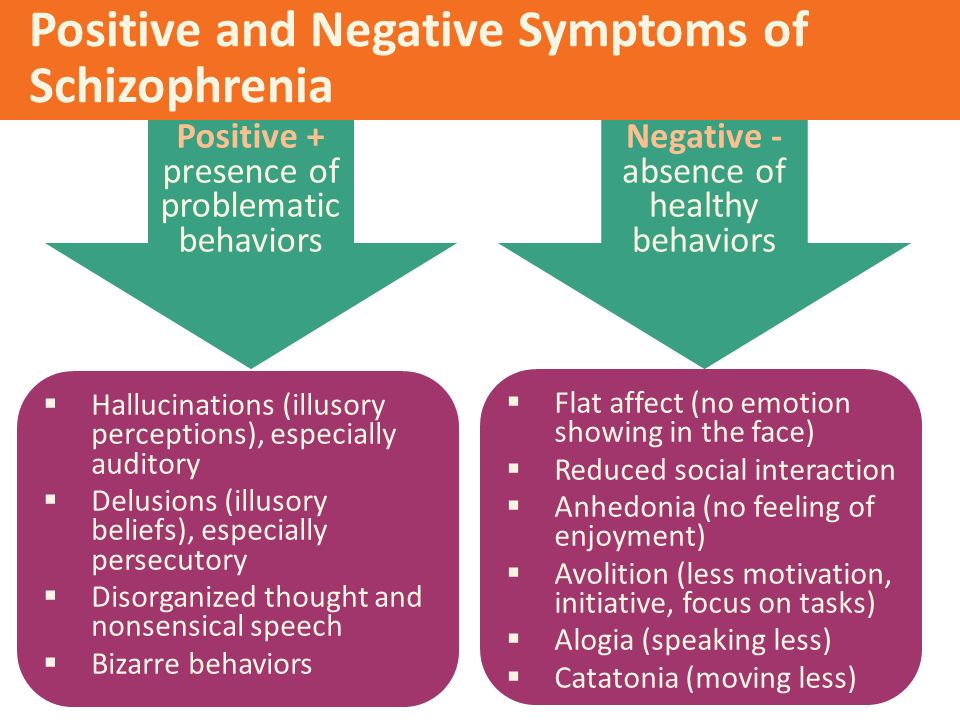 This material is conceived as an educational program with the aim of destigmatizing the diagnosis of schizophrenia. With its help, we would like to convey the thesis that the diagnosis of schizophrenia is not a final verdict, and ordinary life is possible with it.
This material is conceived as an educational program with the aim of destigmatizing the diagnosis of schizophrenia. With its help, we would like to convey the thesis that the diagnosis of schizophrenia is not a final verdict, and ordinary life is possible with it.
1. Who is to blame if a person develops schizophrenia?
Medicine does not yet know what causes the disorder. It is assumed that this is a coincidence of genetic factors, violations of chemical processes in the brain and environmental influences.
Scientists cannot examine and evaluate the processes that take place in the brain of people diagnosed with schizophrenia. But the studies that are already available have shown that in this disease there are problems in the work of neurotransmitters, mainly dopamine. These are substances through which impulses are transmitted from one nerve cell to another. The brain and central nervous system are also somewhat altered in this disorder. But how these changes affect and when they develop is still unknown.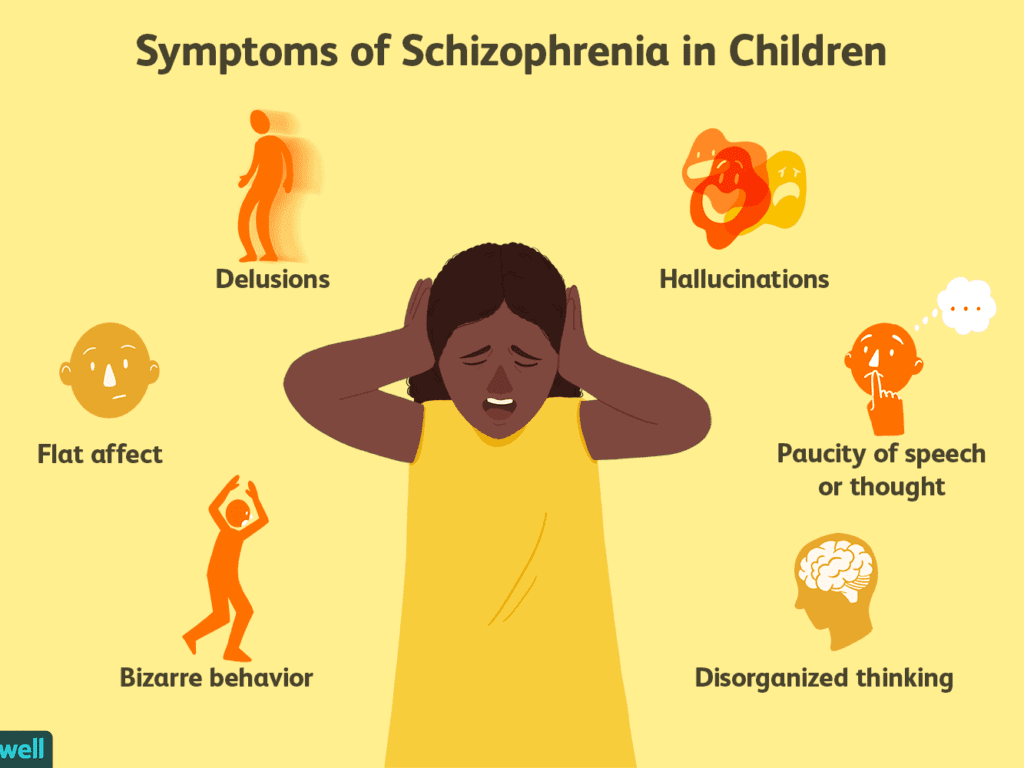 nine0003
nine0003
2. Is there any way I can tell if I or a loved one has schizophrenia?
Diagnosing schizophrenia in oneself is quite difficult: people with a mental disorder most often do not realize that something is wrong with them. Relatives and friends of the sick person who notice changes in behavior, thinking, habits, and reactions often turn to specialists.
The first signs of the disease can not always be recognized precisely as pathological. A person can joke strangely, move away from people and the professional community. He can talk about unusual feelings and experiences, share unusual ideas and try to implement them. In general terms, his behavior can be described as follows: a closed eccentric, convinced of his inventions. Perhaps this is just a temporary state caused by some kind of experience or stress. But sometimes schizophrenia begins with such non-obvious symptoms. nine0003
3. How do people behave when they definitely have schizophrenia?
The disease manifests itself differently in everyone, in different combinations of symptoms and complaints.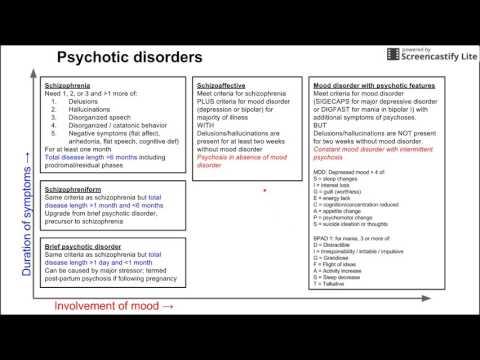 If relatives or the person himself notice that his (her) condition has signs of a mental disorder, then you need to contact a specialist - only he can diagnose and distinguish one disease from another with similar symptoms.
If relatives or the person himself notice that his (her) condition has signs of a mental disorder, then you need to contact a specialist - only he can diagnose and distinguish one disease from another with similar symptoms.
In general, symptoms of schizophrenia may include:
- Delirium. A person begins to think that something is happening that is related to him or to the world around him: as if someone is watching him, persecuting him, trying to harm him, slander, offend him. It may seem to a patient with schizophrenia that someone has written down thoughts, conversations, texts, tasks in his head and made him think about it, pronounce it, decide it. He is sure that others also hear what is going on in his head, and tries to communicate on this topic. For some, information “appears” that something tragic, dangerous is about to happen in the country, in the world, on Earth. The most important thing is that a person sincerely believes in the reality of all this.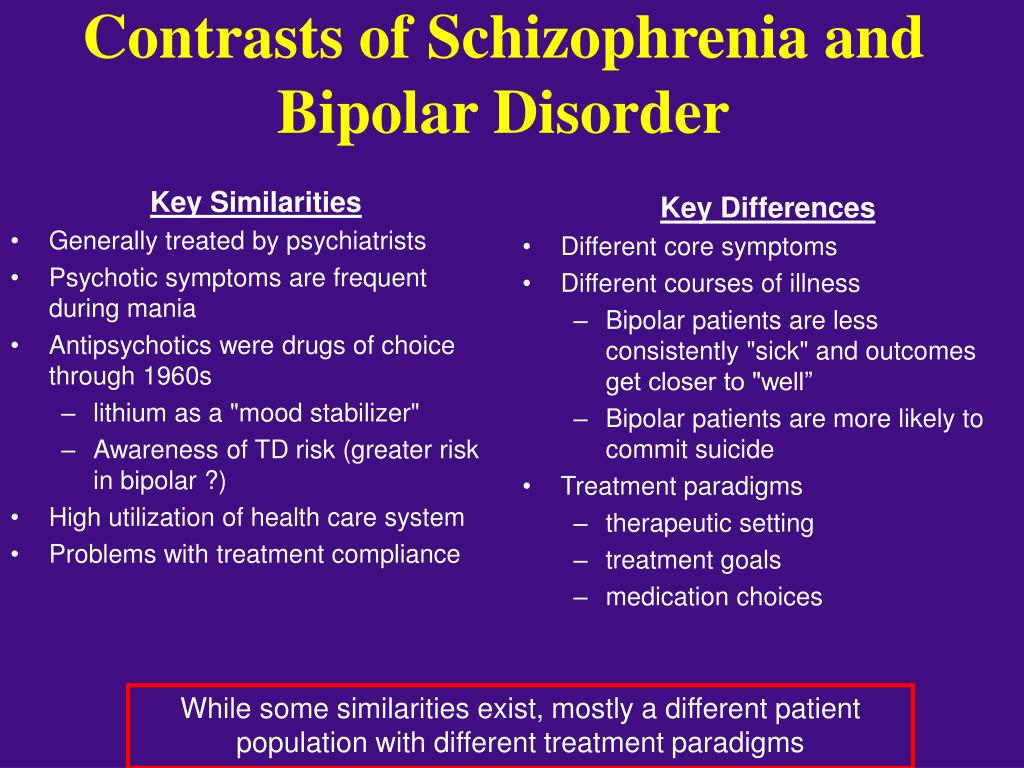 nine0003
nine0003
- Hallucinations. These are false auditory, tactile, visual sensations. A person with schizophrenia lives them, for him they are real.
- Negative symptoms. What is listed above is called productive symptoms - they were brought by the disease, this is its product. Negative symptoms are those that the disease takes away, minus from the life of the sick person. The liveliness of movements, energy, will, desire to do something, to communicate disappear. A patient with schizophrenia may not want anything, he (she) is not interested in anything, he (she) ceases to take care of himself and observe the simplest hygiene. nine0003
- Disorders of thought and speech. For others, they look like a "salad of thoughts and words." The sick person may ask questions to himself or receive them from others, begin to answer and get confused in words.
- Unusual behavior. A person becomes characterized by childishness, antics, frozen postures or, conversely, fussy and meaningless movements, which often do not fit either with the situation, or with the environment, or with the tasks.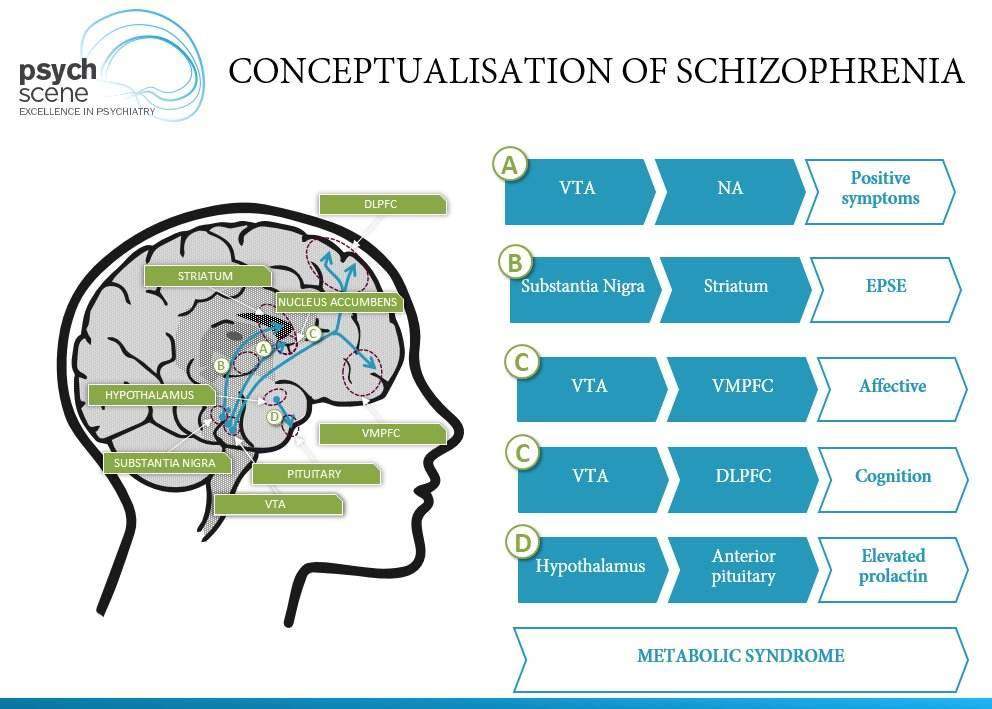
4. So, if my friend has these symptoms, then he (she)…? nine0005
Not always. Yes, and one symptom from this description, and a combination of several, may indicate schizophrenia, but in the same way they can be disguised as manifestations of a completely different disorder.
close
100%
A non-specialist should not suspect schizophrenia in a person. Even experienced professionals conduct many examinations and tests before making a diagnosis. Therefore, the best tactic in this case is to convince to visit a specialist.
5. It seems that this happened to my relative. Will he be sent to a psychiatric hospital now? nine0005
Optional. Schizophrenia can proceed in different ways, many are successfully treated only at home, on an outpatient basis. If the behavior of your loved one has changed and has become a concern, then do not invent diagnoses, and even more so do not voice the assumption to outsiders. Talk to the person himself, find out what he feels and what worries him.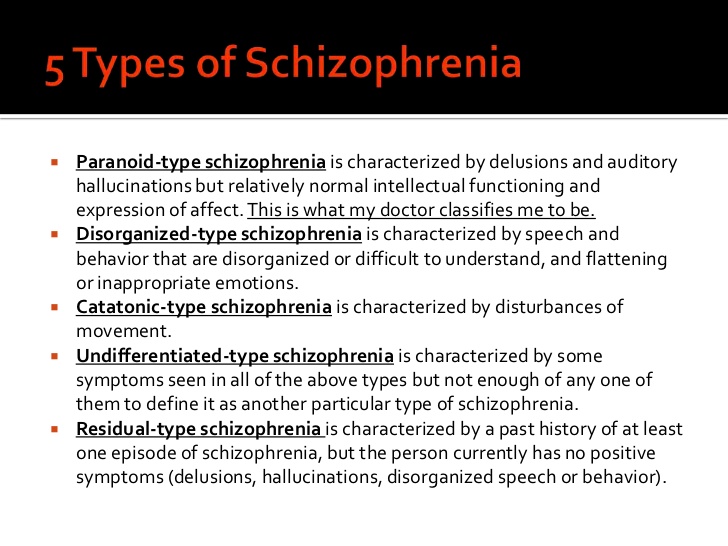 And together with him sign up for a specialist if you understand that he:
And together with him sign up for a specialist if you understand that he:
- has become suspicious, listens to something, checks something;
- suddenly loses the thought or thread of the conversation, cuts off speech in mid-sentence or does not complete the matter; nine0059 - has problems with social adaptation (cannot perform the simplest actions - for example, buy groceries in a store).
Unfortunately, the circumstances of the disease develop in such a way that from the very beginning the sick person needs help and support from relatives and friends. And it starts with the need to convince him to go to a specialist.
You may have seen the movie A Beautiful Mind. It was created based on the life story of a real-life American mathematician, scientist and Princeton University professor John Nash. He had schizophrenia, which caused his strange behavior, but did not lead to the loss of the ability to think scientifically. The film shows well how the support of loved ones helped John Nash.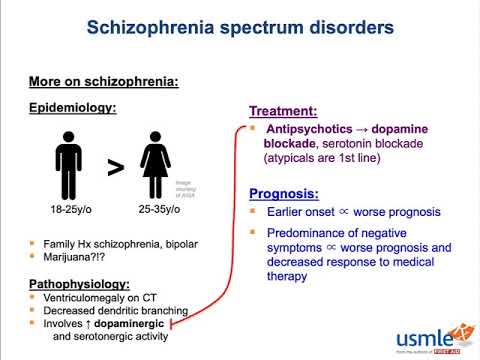 nine0003
nine0003
This is, of course, an isolated example, but it shows that it is wrong to equate schizophrenia with complete loss of reason. The disease can proceed in different ways, the treatment can be so effective that a person will live almost the same as before.
6. Registration
It's not a shame. This is right and necessary: everyone should receive treatment for their disease. Help for schizophrenia is provided by a specialist, and accounting is a diary of monitoring the course of the disease. It has long been understood abroad that only treatment and control help many people with schizophrenia avoid difficult life situations (vagrancy, alcohol or drug abuse), notice a relapse (return of symptoms) in time, and return to remission. nine0003
7. So now you are on pills all your life?
That would be perfect! If loved ones can convince a person with schizophrenia to take prescribed medications and come to check-ups on time, then symptoms can be controlled and a relapse can be prevented.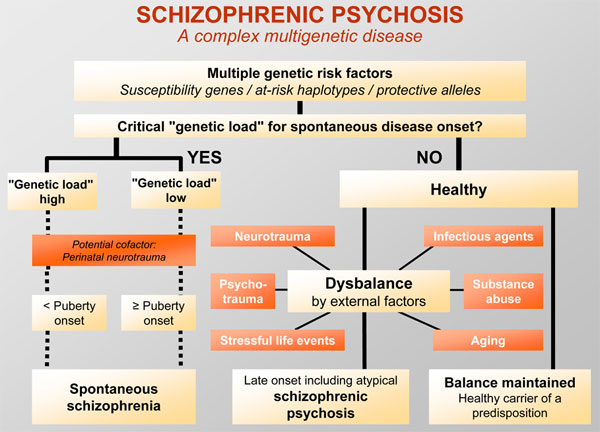
8. What does “under control” mean? Don't pills cure?
To control means to use drugs and additional methods (psychotherapy, for example) to make the symptoms of the disease affect life as little as possible. This is called remission. With a favorable course of the disease, remission on medications can be such that a person will remain in society, will live almost the same as before the diagnosis. nine0003
close
100%
Some people with this condition manage to take control of their medication and treatment. But still, most need support from loved ones, compassion without obsession and excessive anxiety. In practice, this can be a donated pill box, in which the desired drug is pre-filled. Or creating a calm environment in the house and a joint visit to a psychotherapist. Or daily walks and organizing participation in household chores so that a person does not feel excluded from family life and does not concentrate on experiences. nine0003
9. When can a person be considered healthy?
There is no cure for schizophrenia yet.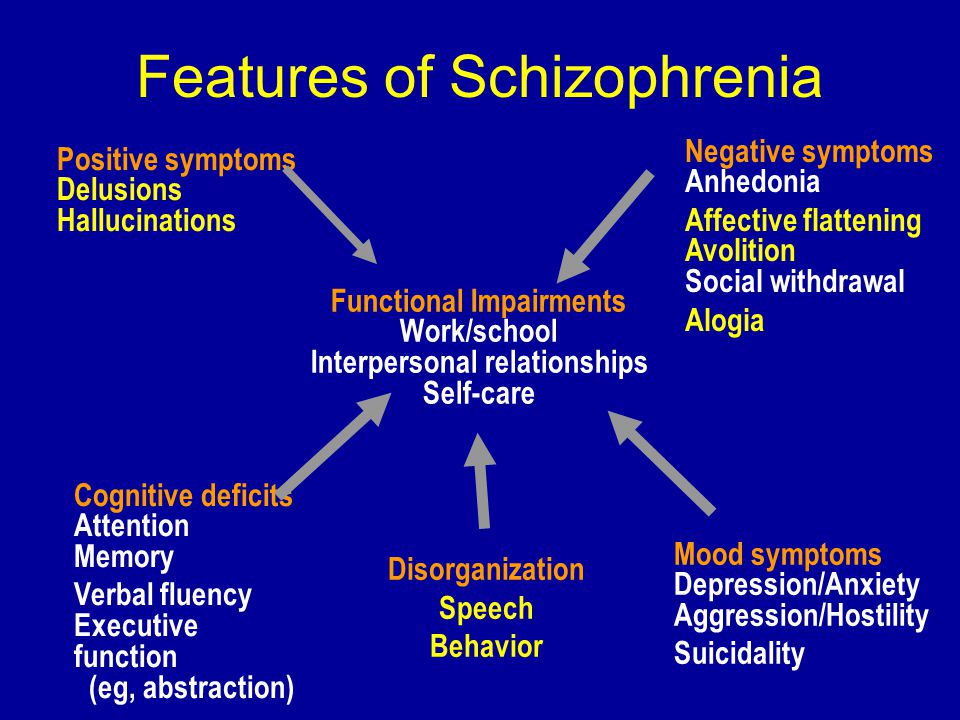 And there are quite a few diseases that can only be brought into remission with the help of drugs: for example, diabetes mellitus or hypertension - people have to take drugs all their lives, but no one considers them defective.
And there are quite a few diseases that can only be brought into remission with the help of drugs: for example, diabetes mellitus or hypertension - people have to take drugs all their lives, but no one considers them defective.
And, of course, the scientific world is looking for, developing, testing drugs that can work as efficiently as possible. For example, in Russia there is a drug from the pharmaceutical company Gideon Richter, which can help fight productive and negative symptoms and make it possible to live more harmoniously in society. nine0003
10. They say that people with this diagnosis can suddenly attack, try to kill, do they become strong like animals?
There are factors that can lead to an outbreak of aggression. But this does not mean that the sick are just waiting for someone to attack. If you had to deal with this, then protect the patient (close the windows, turn off the gas, take away knives and matches, etc.), yourself, family members, animals and call an ambulance, telling what is happening.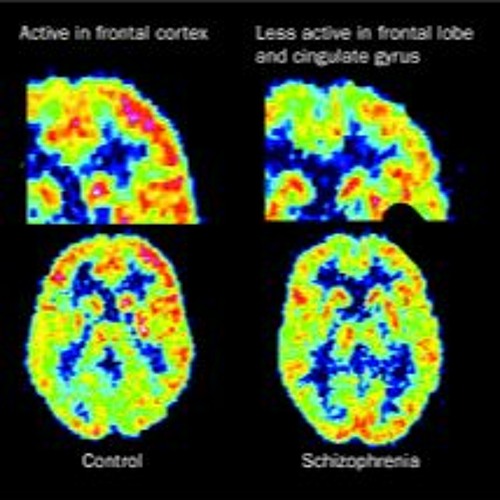 There is no need to enter into disputes with the patient, mock, demand to calm down or remember the techniques of martial arts. Stay calm, speak in a calm voice. nine0003
There is no need to enter into disputes with the patient, mock, demand to calm down or remember the techniques of martial arts. Stay calm, speak in a calm voice. nine0003
According to various data obtained by foreign researchers, people with schizophrenia commit 5 to 10% of crimes related to aggression or violence. The rest of these crimes are committed by people without this diagnosis.
The material was prepared with the support of Gideon Richter.
-
Sources:
1. Schizophrenia. https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms-causes/syc-20354443
2. What Is Schizophrenia? https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia
3. Expert Q & A: Schizophrenia https://www.psychiatry.org/patients-families/schizophrenia/expert-q-and-a
4. Violence and schizophrenia: Examining the evidence https://www.cambridge. org/core/journals/the-british-journal-of-psychiatry/article/violence-and-schizophrenia-examining-the-evidence/BEC530F212F98C0400D3D32CB2710BA9
5. Violence and mental illness: an overview https://pubmed.ncbi.nlm .nih.gov/16946914/
Violence and mental illness: an overview https://pubmed.ncbi.nlm .nih.gov/16946914/
Largest study on schizophrenia identifies more than 100 genes that cause the disease
The most extensive study of schizophrenia has been carried out: Vera Golimbet, Doctor of Biology, told Gazeta.Ru about its results and the contribution of Russian geneticists to this work.
Schizophrenia is one of those mental illnesses that everyone has heard of. But why this disease happens and what links of brain mechanics break down in this case is still unclear even to doctors. The ambiguity of the biological nature entails the uncertainty of the diagnosis, therefore, anything can be squeezed into it, from dissent, which was used with might and main by the punitive Soviet psychiatry with a wonderful diagnosis " sluggish schizophrenia ", to autism, which until recently, when a person reached the age of 18, suddenly turned into schizophrenia .
Schizophrenia is more complicated than it was said
Scientists managed to obtain molecular clues to the occurrence of schizophrenia by sequencing the genomes of patients .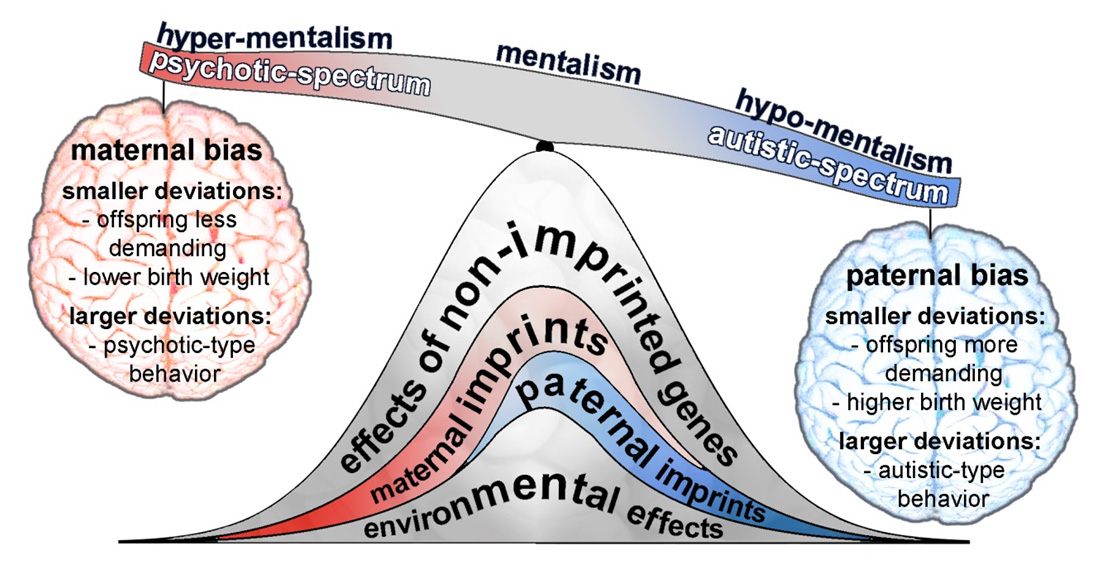 ..
..
January 23 13:38
If the biological nature of the disease is unclear, then how to treat it is also unclear.
Therefore, until now, schizophrenia is treated by the same methods as 60 years ago, namely, antipsychotic drugs, or antipsychotics. nine0003
They suppress, inhibit the processes of excitation in the central nervous system, extinguish psychoses, including hallucinations, paranoia. But this is only part of the symptoms of schizophrenia. At the same time, neuroleptics not only do not improve intellectual activity, social behavior, but, on the contrary, inhibit it. And as was recently shown, in high doses leads to a decrease in brain volume . No fundamentally new treatment has been invented during this time.
Schizophrenia affects on average every hundredth inhabitant of the planet. It often occurs in adolescence and young age, up to 20 years. nine0003
The economic burden of schizophrenia, for example, in the United States is $60 million, but for Russia it simply has not been calculated.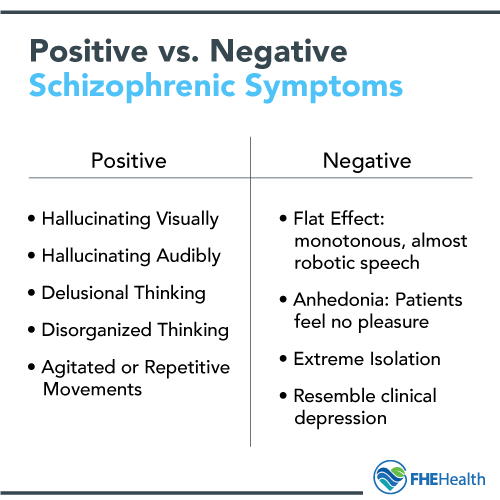
Since schizophrenia is largely dependent on heredity, its genetic nature, scientists have taken care not yesterday. So, in a study published in Nature six months ago, about which Gazeta.Ru wrote, methods of complete sequencing (reading DNA) of the genomes of sick and healthy volunteers managed to identify about 30 mutations associated with schizophrenia. Latest study, , the results of which are published in the latest issue of Nature , is much larger. Russian researchers from the Institute of Molecular Genetics of the Russian Academy of Sciences and the Scientific Center for Mental Health of the Russian Academy of Medical Sciences also took part in it.
Scientists analyzed nearly 37,000 DNA samples from schizophrenic patients compared to 113,000 DNA from healthy people, both European and Asian.
Antipsychotics dry out the brain
Taking antipsychotics, the main drug prescribed for patients with schizophrenia...
September 18 14:07
This is the result of several years of research by the Schizophrenia Working Group of the Psychiatric Genomics Consortium , an international, multidisciplinary collaboration founded in 2007. It includes about 500 researchers from more than 80 organizations in 25 countries. The work is coordinated by specialists from the Broad Institute of the Massachusetts General Hospital.
It includes about 500 researchers from more than 80 organizations in 25 countries. The work is coordinated by specialists from the Broad Institute of the Massachusetts General Hospital.
Scientists applied the so-called Genome-Wide Association Search (GWAS) . Two words about what it is. Throughout the genome (that is, DNA) there are regions in which one nucleotide can be replaced by another - these are the so-called polymorphic regions. They may differ for different people. This is single nucleotide polymorphism (SNP) - the same as point mutations. So, the variations of these parts of the genome are compared in a population of healthy people and in a population of patients with a disease. And they find which variations (SNPs) are associated with a given disease. nine0003
After reviewing nearly 10 million of these variations, geneticists have identified 108 of them, which are more common in the group of patients and, therefore, are associated with schizophrenia.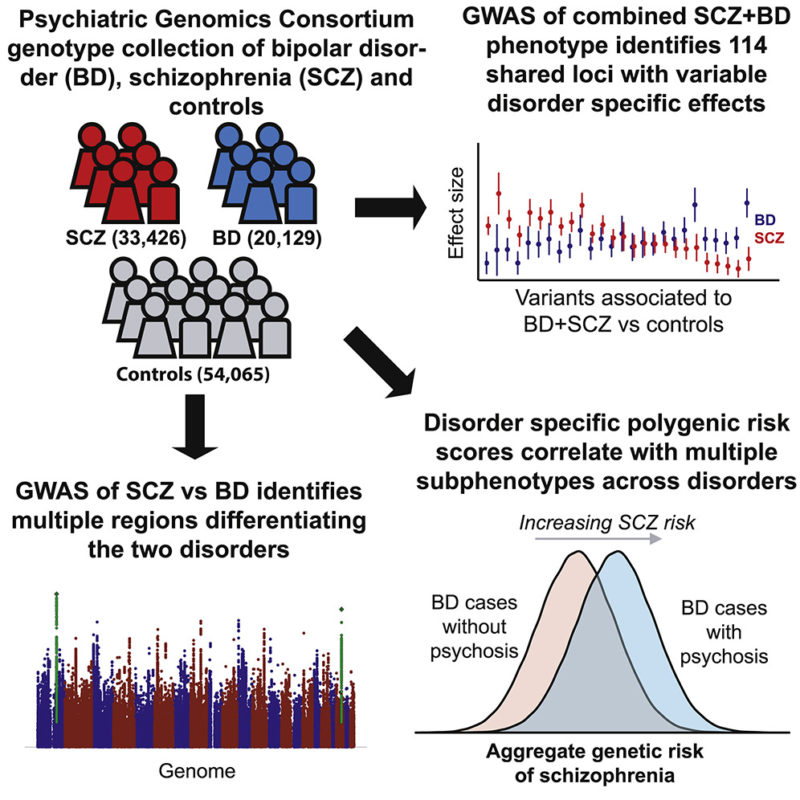 Moreover, 83 of them have not yet been known.
Moreover, 83 of them have not yet been known.
Most of the genes in which these variations are found work in the brain, they are associated with the functions of neurons and synapses. In particular, these genes provide synaptic plasticity necessary for learning and memory, and are responsible for the functioning of calcium ion channels involved in the transmission of nerve signals. A mutation in any one gene causes a cascade of changes in the so-called signaling pathways, chains of biochemical reactions.
“We are bad at treating”
Despite the difficult political situation, a major international conference on autism is taking place in Moscow. At...
June 03 14:08
Finding out these pathways will help find drug targets to correct these changes.
Among others, scientists have found a link between schizophrenia and the neurotransmitter 9 receptor gene0021 dopamine (DRD2), as well as genes involved in the metabolism of neurotransmitter glutamate .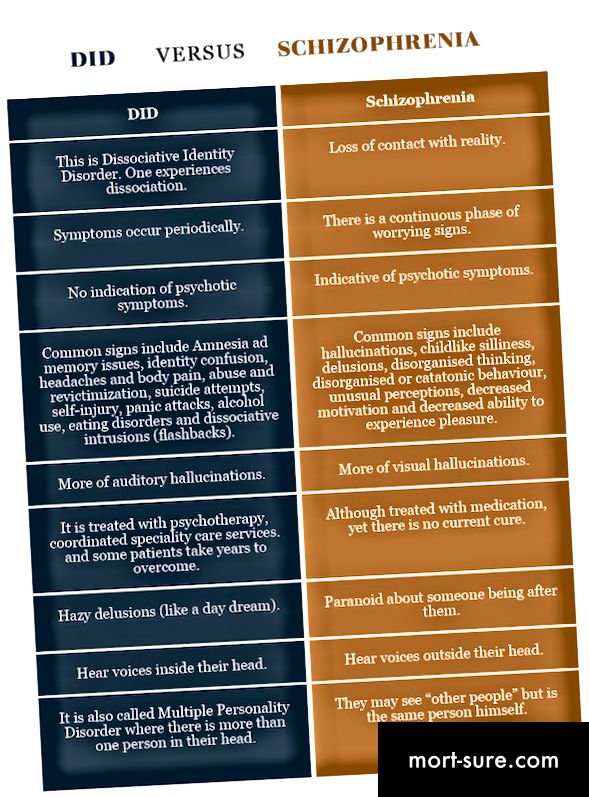 Both substances are the most important transmitters of the nerve signal in synapses - contacts between neurons.
Both substances are the most important transmitters of the nerve signal in synapses - contacts between neurons.
Thus, the biological picture of schizophrenia has become much more complete.
In particular, the connection of this disease with immune disorders was confirmed, because among the genes associated with schizophrenia there were many genes of the immune system.
Vera Golimbet, Doctor of Biology, Head of the Laboratory of Clinical Genetics of the Scientific Center for Mental Health of the Russian Academy of Medical Sciences, told Gazeta.Ru about the participation of Russian scientists in the work.
— What part of the work did you and your colleagues do?
- Our part was that we formed a sample of patients with schizophrenia and a sample of healthy people without mental illness, took DNA samples and prepared them for genotyping.
— How many Russian patients were there? nine0022
- About 500 people in each group - sick and healthy.
— What are the main features of this work?
- This is a meta-analysis of a large number of studies of patients from different ethnic groups.
Different psychos have common genes
For the first time in a genome-wide study on a large population, scientists have clarified the contribution of different gene variations...
August 12 17:30
The scientists conducting them have formed a large international consortium for schizophrenia research. nine0003
And managed to collect the largest amount of data, on the largest sample, than ever.
— What was the basis for genotyping?
— Genotyping, including our samples, was carried out on biochips; this method can immediately determine a large number of genetic polymorphisms. This was done by the Icelandic company deCode.
— Do you also perform genotyping in the laboratory of clinical genetics?
— Yes, but not at that level. Today, large international studies are a common practice because they are becoming more and more expensive, and this is the only way to study a disease with such a complex and unclear etiology as schizophrenia.