What is a manic disorder
Bipolar disorder - Symptoms and causes
Overview
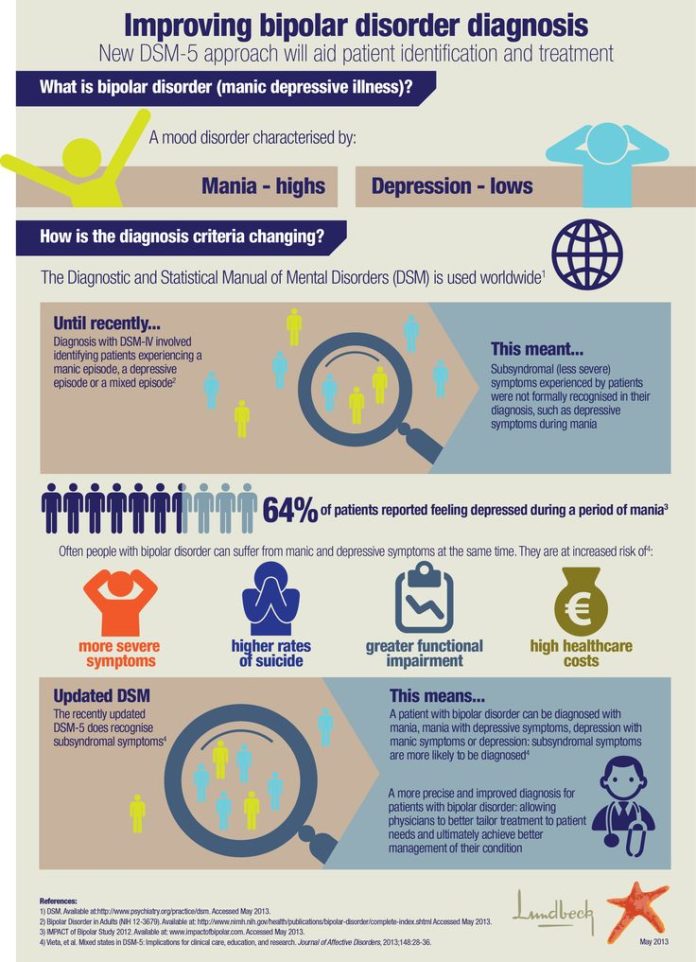
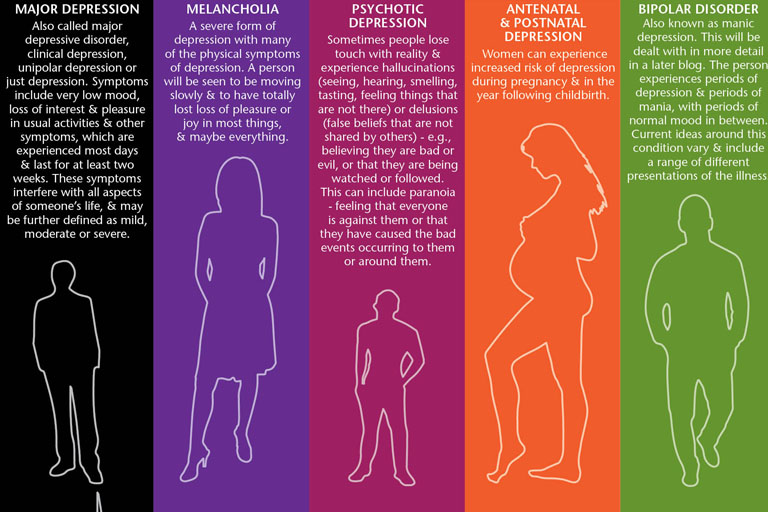
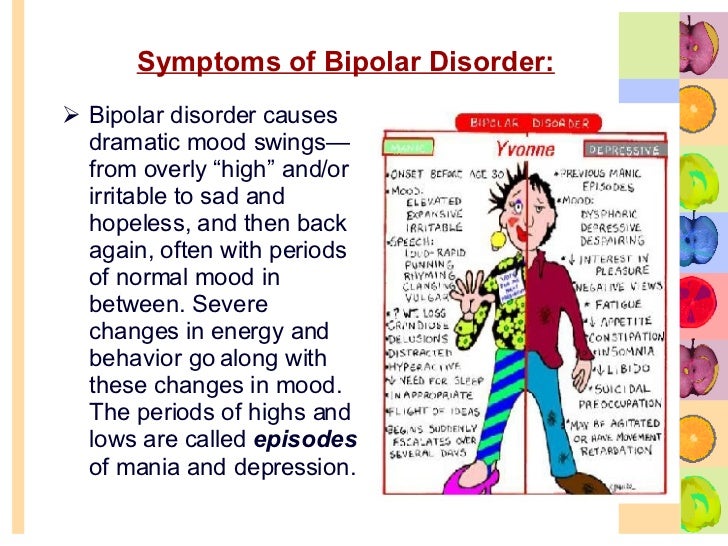
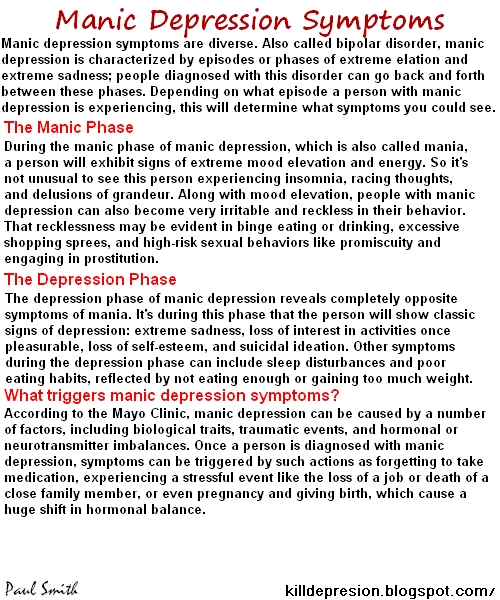
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, activity, judgment, behavior and the ability to think clearly.
Episodes of mood swings may occur rarely or multiple times a year. While most people will experience some emotional symptoms between episodes, some may not experience any.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).
Bipolar disorder care at Mayo Clinic
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
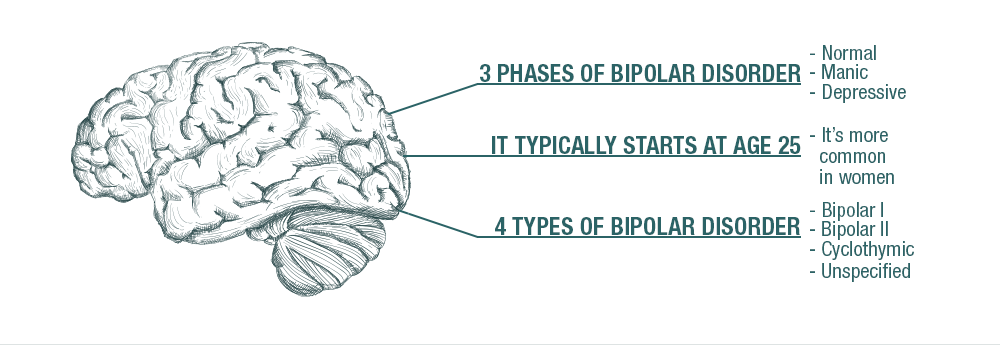
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life.
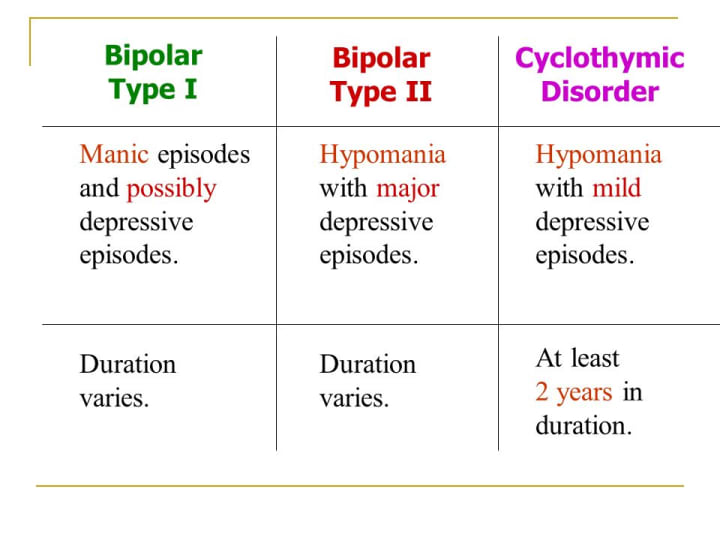
- Bipolar I disorder. You've had at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis).
- Bipolar II disorder. You've had at least one major depressive episode and at least one hypomanic episode, but you've never had a manic episode.
- Cyclothymic disorder. You've had at least two years — or one year in children and teenagers — of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment.
Although bipolar disorder can occur at any age, typically it's diagnosed in the teenage years or early 20s. Symptoms can vary from person to person, and symptoms may vary over time.
Mania and hypomania
Mania and hypomania are two distinct types of episodes, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.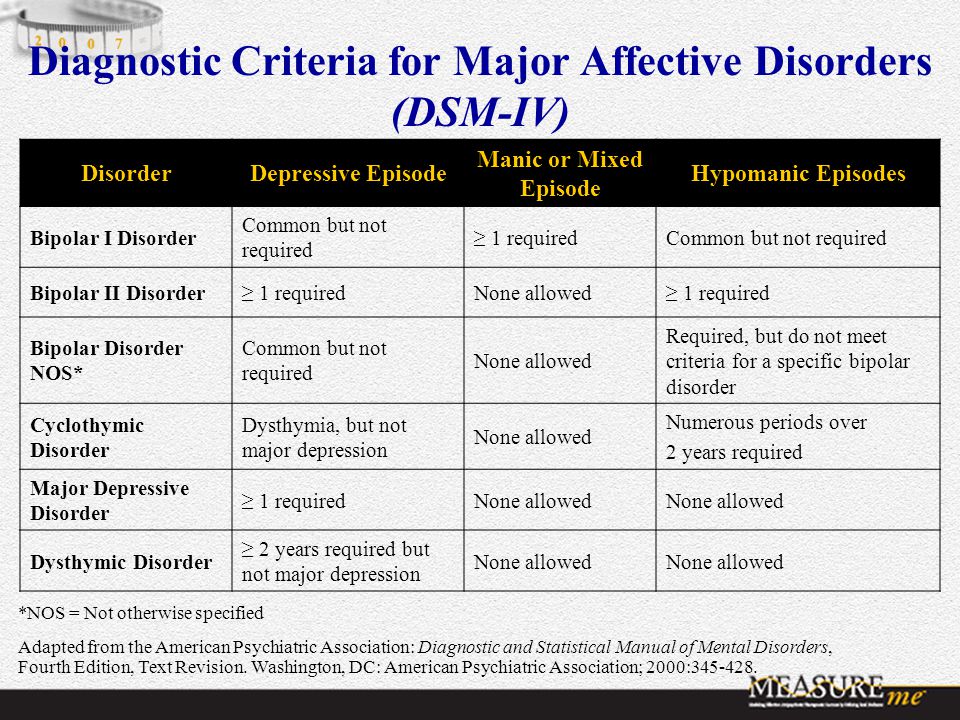
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making — for example, going on buying sprees, taking sexual risks or making foolish investments
Major depressive episode
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities or relationships. An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless or tearful (in children and teens, depressed mood can appear as irritability)
- Marked loss of interest or feeling no pleasure in all — or almost all — activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight as expected can be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning or attempting suicide
Other features of bipolar disorder
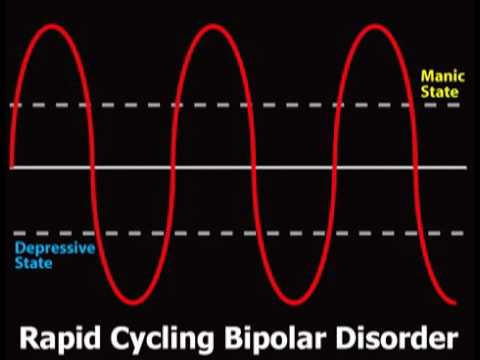
Signs and symptoms of bipolar I and bipolar II disorders may include other features, such as anxious distress, melancholy, psychosis or others.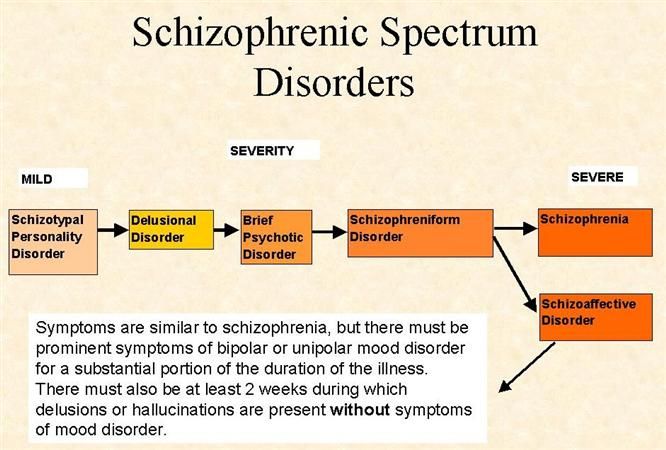 The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
Symptoms in children and teens
Symptoms of bipolar disorder can be difficult to identify in children and teens. It's often hard to tell whether these are normal ups and downs, the results of stress or trauma, or signs of a mental health problem other than bipolar disorder.
Children and teens may have distinct major depressive or manic or hypomanic episodes, but the pattern can vary from that of adults with bipolar disorder. And moods can rapidly shift during episodes. Some children may have periods without mood symptoms between episodes.
The most prominent signs of bipolar disorder in children and teenagers may include severe mood swings that are different from their usual mood swings.
When to see a doctor
Despite the mood extremes, people with bipolar disorder often don't recognize how much their emotional instability disrupts their lives and the lives of their loved ones and don't get the treatment they need.
And if you're like some people with bipolar disorder, you may enjoy the feelings of euphoria and cycles of being more productive. However, this euphoria is always followed by an emotional crash that can leave you depressed, worn out — and perhaps in financial, legal or relationship trouble.
If you have any symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder doesn't get better on its own. Getting treatment from a mental health professional with experience in bipolar disorder can help you get your symptoms under control.
When to get emergency help
Suicidal thoughts and behavior are common among people with bipolar disorder. If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week.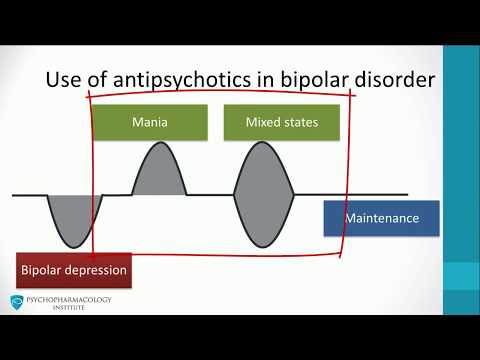 Or use the Lifeline Chat. Services are free and confidential.
Or use the Lifeline Chat. Services are free and confidential.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information.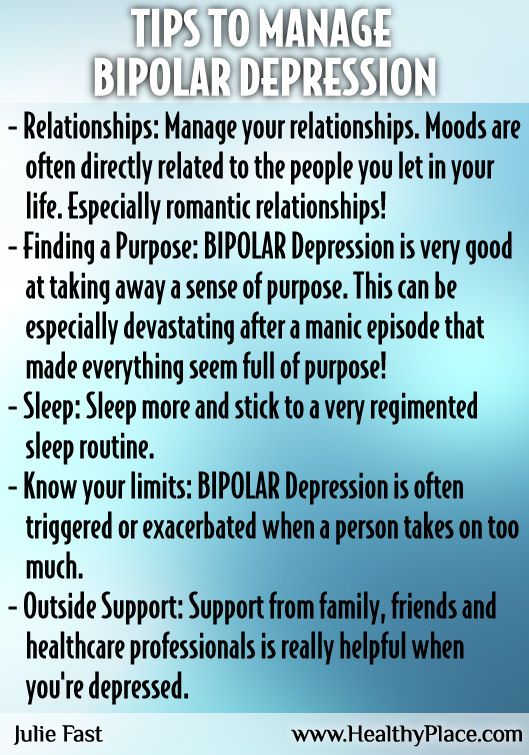 If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
The exact cause of bipolar disorder is unknown, but several factors may be involved, such as:
- Biological differences. People with bipolar disorder appear to have physical changes in their brains. The significance of these changes is still uncertain but may eventually help pinpoint causes.
- Genetics. Bipolar disorder is more common in people who have a first-degree relative, such as a sibling or parent, with the condition.
 Researchers are trying to find genes that may be involved in causing bipolar disorder.
Researchers are trying to find genes that may be involved in causing bipolar disorder.
Risk factors
Factors that may increase the risk of developing bipolar disorder or act as a trigger for the first episode include:
- Having a first-degree relative, such as a parent or sibling, with bipolar disorder
- Periods of high stress, such as the death of a loved one or other traumatic event
- Drug or alcohol abuse
Complications
Left untreated, bipolar disorder can result in serious problems that affect every area of your life, such as:
- Problems related to drug and alcohol use
- Suicide or suicide attempts
- Legal or financial problems
- Damaged relationships
- Poor work or school performance
Co-occurring conditions
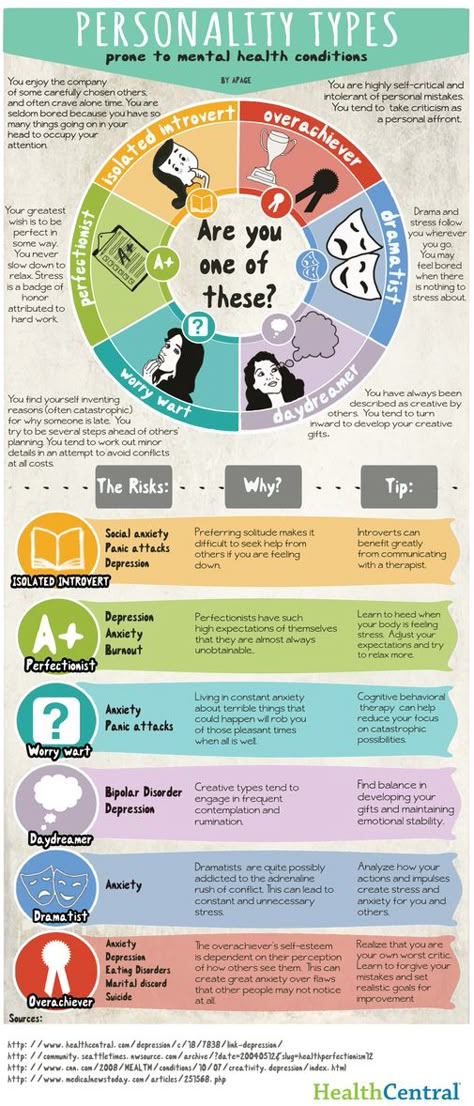
If you have bipolar disorder, you may also have another health condition that needs to be treated along with bipolar disorder. Some conditions can worsen bipolar disorder symptoms or make treatment less successful.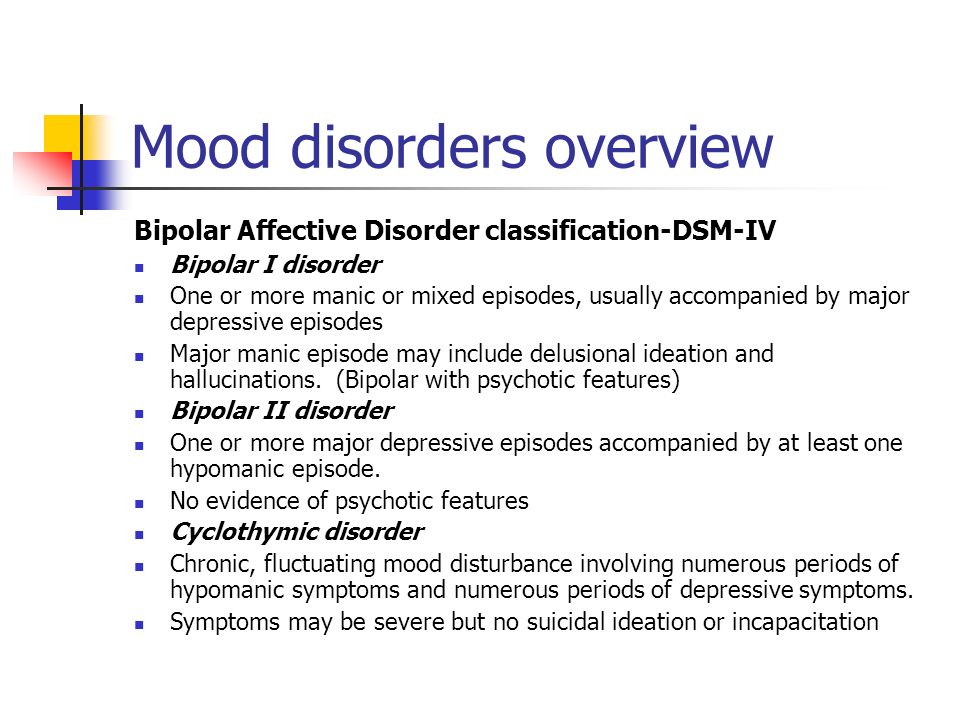 Examples include:
Examples include:
- Anxiety disorders
- Eating disorders
- Attention-deficit/hyperactivity disorder (ADHD)
- Alcohol or drug problems
- Physical health problems, such as heart disease, thyroid problems, headaches or obesity
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar disorder and alcoholism: Are they related?
Prevention
There's no sure way to prevent bipolar disorder. However, getting treatment at the earliest sign of a mental health disorder can help prevent bipolar disorder or other mental health conditions from worsening.
If you've been diagnosed with bipolar disorder, some strategies can help prevent minor symptoms from becoming full-blown episodes of mania or depression:
- Pay attention to warning signs. Addressing symptoms early on can prevent episodes from getting worse. You may have identified a pattern to your bipolar episodes and what triggers them.
 Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs.
Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs. - Avoid drugs and alcohol. Using alcohol or recreational drugs can worsen your symptoms and make them more likely to come back.
- Take your medications exactly as directed. You may be tempted to stop treatment — but don't. Stopping your medication or reducing your dose on your own may cause withdrawal effects or your symptoms may worsen or return.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Bipolar disorder - Diagnosis and treatment
Diagnosis
To determine if you have bipolar disorder, your evaluation may include:
- Physical exam. Your doctor may do a physical exam and lab tests to identify any medical problems that could be causing your symptoms.
- Psychiatric assessment.
 Your doctor may refer you to a psychiatrist, who will talk to you about your thoughts, feelings and behavior patterns. You may also fill out a psychological self-assessment or questionnaire. With your permission, family members or close friends may be asked to provide information about your symptoms.
Your doctor may refer you to a psychiatrist, who will talk to you about your thoughts, feelings and behavior patterns. You may also fill out a psychological self-assessment or questionnaire. With your permission, family members or close friends may be asked to provide information about your symptoms. - Mood charting. You may be asked to keep a daily record of your moods, sleep patterns or other factors that could help with diagnosis and finding the right treatment.
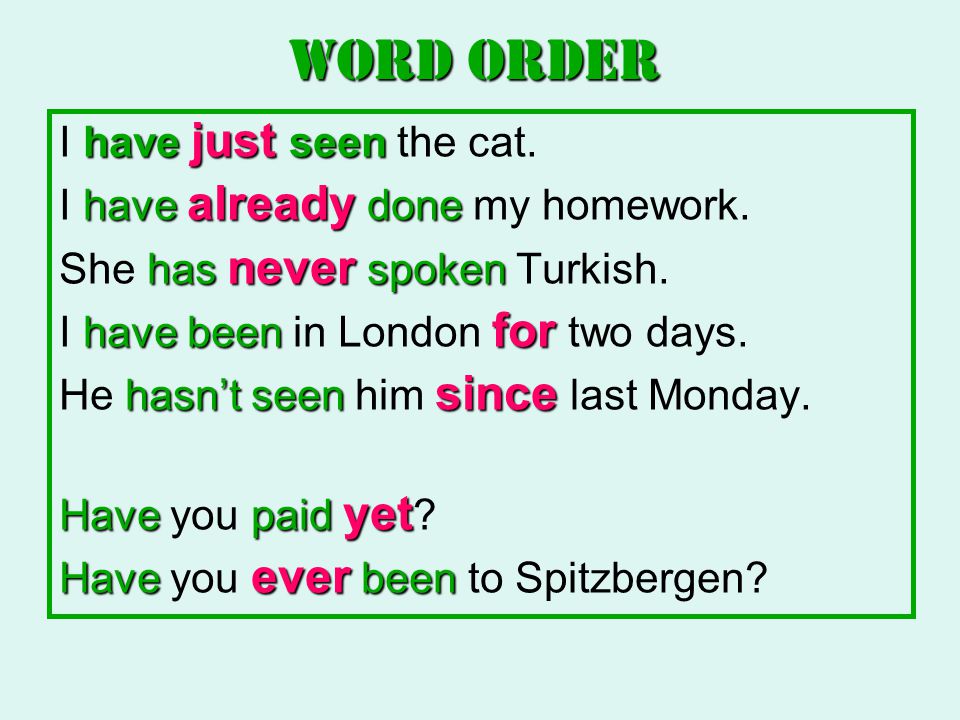
- Criteria for bipolar disorder. Your psychiatrist may compare your symptoms with the criteria for bipolar and related disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Diagnosis in children
Although diagnosis of children and teenagers with bipolar disorder includes the same criteria that are used for adults, symptoms in children and teens often have different patterns and may not fit neatly into the diagnostic categories.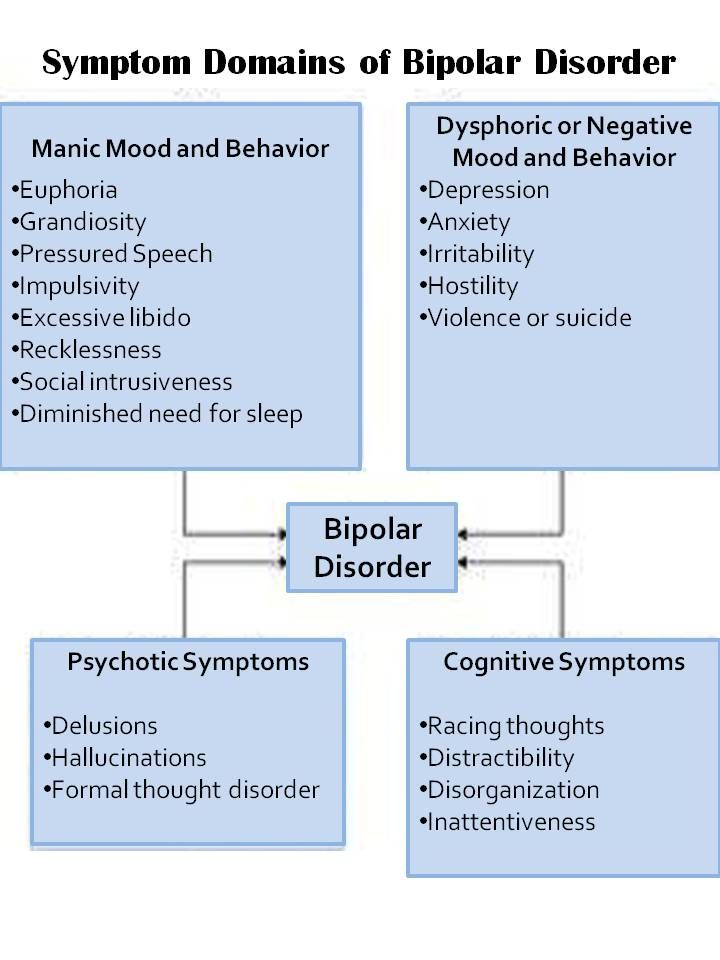
Also, children who have bipolar disorder are frequently also diagnosed with other mental health conditions such as attention-deficit/hyperactivity disorder (ADHD) or behavior problems, which can make diagnosis more complicated. Referral to a child psychiatrist with experience in bipolar disorder is recommended.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your bipolar disorder-related health concerns Start Here
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar in children
- Urinalysis
Treatment
Treatment is best guided by a medical doctor who specializes in diagnosing and treating mental health conditions (psychiatrist) who is skilled in treating bipolar and related disorders. You may have a treatment team that also includes a psychologist, social worker and psychiatric nurse.
Bipolar disorder is a lifelong condition.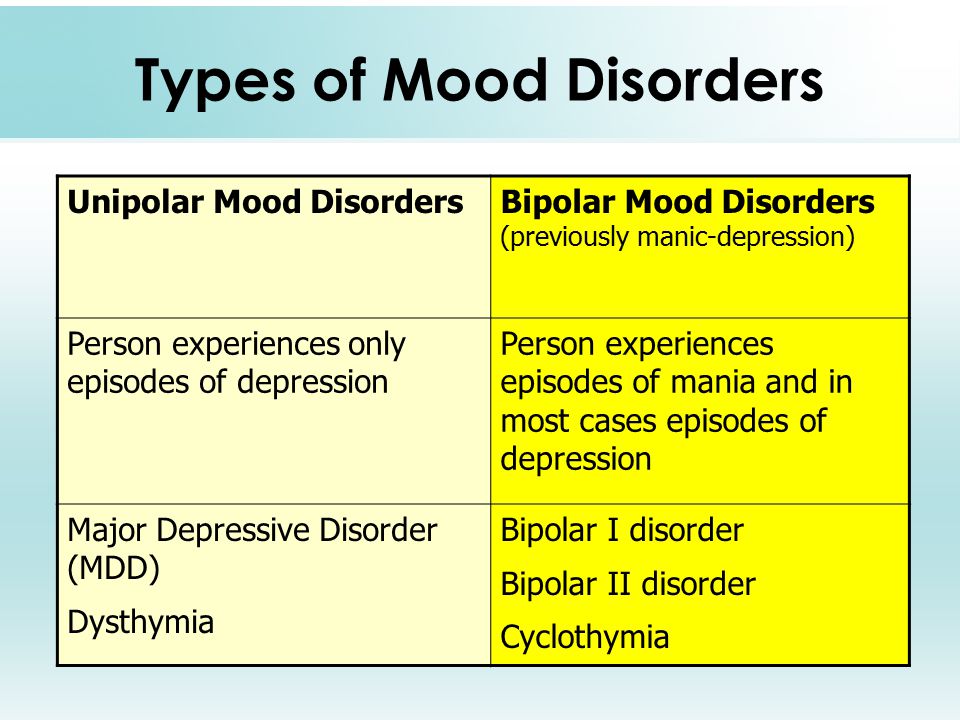 Treatment is directed at managing symptoms. Depending on your needs, treatment may include:
Treatment is directed at managing symptoms. Depending on your needs, treatment may include:
- Medications. Often, you'll need to start taking medications to balance your moods right away.
- Continued treatment. Bipolar disorder requires lifelong treatment with medications, even during periods when you feel better. People who skip maintenance treatment are at high risk of a relapse of symptoms or having minor mood changes turn into full-blown mania or depression.
- Day treatment programs. Your doctor may recommend a day treatment program. These programs provide the support and counseling you need while you get symptoms under control.
- Substance abuse treatment. If you have problems with alcohol or drugs, you'll also need substance abuse treatment. Otherwise, it can be very difficult to manage bipolar disorder.
- Hospitalization. Your doctor may recommend hospitalization if you're behaving dangerously, you feel suicidal or you become detached from reality (psychotic).
 Getting psychiatric treatment at a hospital can help keep you calm and safe and stabilize your mood, whether you're having a manic or major depressive episode.
Getting psychiatric treatment at a hospital can help keep you calm and safe and stabilize your mood, whether you're having a manic or major depressive episode.
The primary treatments for bipolar disorder include medications and psychological counseling (psychotherapy) to control symptoms, and also may include education and support groups.
Medications
A number of medications are used to treat bipolar disorder. The types and doses of medications prescribed are based on your particular symptoms.
Medications may include:
- Mood stabilizers. You'll typically need mood-stabilizing medication to control manic or hypomanic episodes. Examples of mood stabilizers include lithium (Lithobid), valproic acid (Depakene), divalproex sodium (Depakote), carbamazepine (Tegretol, Equetro, others) and lamotrigine (Lamictal).
- Antipsychotics. If symptoms of depression or mania persist in spite of treatment with other medications, adding an antipsychotic drug such as olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), aripiprazole (Abilify), ziprasidone (Geodon), lurasidone (Latuda) or asenapine (Saphris) may help.
 Your doctor may prescribe some of these medications alone or along with a mood stabilizer.
Your doctor may prescribe some of these medications alone or along with a mood stabilizer. - Antidepressants. Your doctor may add an antidepressant to help manage depression. Because an antidepressant can sometimes trigger a manic episode, it's usually prescribed along with a mood stabilizer or antipsychotic.
- Antidepressant-antipsychotic. The medication Symbyax combines the antidepressant fluoxetine and the antipsychotic olanzapine. It works as a depression treatment and a mood stabilizer.
- Anti-anxiety medications. Benzodiazepines may help with anxiety and improve sleep, but are usually used on a short-term basis.
Finding the right medication
Finding the right medication or medications for you will likely take some trial and error. If one doesn't work well for you, there are several others to try.
This process requires patience, as some medications need weeks to months to take full effect.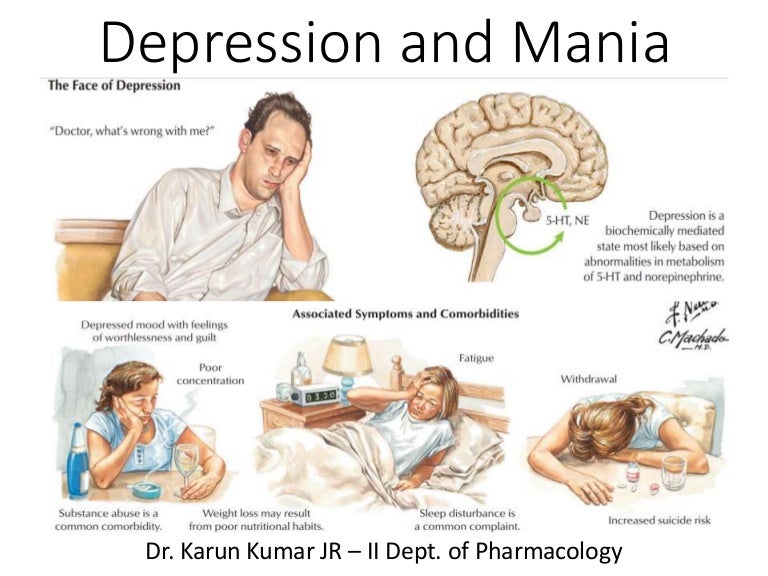 Generally only one medication is changed at a time so that your doctor can identify which medications work to relieve your symptoms with the least bothersome side effects. Medications also may need to be adjusted as your symptoms change.
Generally only one medication is changed at a time so that your doctor can identify which medications work to relieve your symptoms with the least bothersome side effects. Medications also may need to be adjusted as your symptoms change.
Side effects
Mild side effects often improve as you find the right medications and doses that work for you, and your body adjusts to the medications. Talk to your doctor or mental health professional if you have bothersome side effects.
Don't make changes or stop taking your medications. If you stop your medication, you may experience withdrawal effects or your symptoms may worsen or return. You may become very depressed, feel suicidal, or go into a manic or hypomanic episode. If you think you need to make a change, call your doctor.
Medications and pregnancy
A number of medications for bipolar disorder can be associated with birth defects and can pass through breast milk to your baby. Certain medications, such as valproic acid and divalproex sodium, should not be used during pregnancy. Also, birth control medications may lose effectiveness when taken along with certain bipolar disorder medications.
Also, birth control medications may lose effectiveness when taken along with certain bipolar disorder medications.
Discuss treatment options with your doctor before you become pregnant, if possible. If you're taking medication to treat your bipolar disorder and think you may be pregnant, talk to your doctor right away.
Psychotherapy
Psychotherapy is a vital part of bipolar disorder treatment and can be provided in individual, family or group settings. Several types of therapy may be helpful. These include:
- Interpersonal and social rhythm therapy (IPSRT). IPSRT focuses on the stabilization of daily rhythms, such as sleeping, waking and mealtimes. A consistent routine allows for better mood management. People with bipolar disorder may benefit from establishing a daily routine for sleep, diet and exercise.
- Cognitive behavioral therapy (CBT). The focus is identifying unhealthy, negative beliefs and behaviors and replacing them with healthy, positive ones.
 CBT can help identify what triggers your bipolar episodes. You also learn effective strategies to manage stress and to cope with upsetting situations.
CBT can help identify what triggers your bipolar episodes. You also learn effective strategies to manage stress and to cope with upsetting situations. - Psychoeducation. Learning about bipolar disorder (psychoeducation) can help you and your loved ones understand the condition. Knowing what's going on can help you get the best support, identify issues, make a plan to prevent relapse and stick with treatment.
- Family-focused therapy. Family support and communication can help you stick with your treatment plan and help you and your loved ones recognize and manage warning signs of mood swings.
Other treatment options
Depending on your needs, other treatments may be added to your depression therapy.
During electroconvulsive therapy (ECT), electrical currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry that can reverse symptoms of certain mental illnesses. ECT may be an option for bipolar treatment if you don't get better with medications, can't take antidepressants for health reasons such as pregnancy or are at high risk of suicide.
ECT may be an option for bipolar treatment if you don't get better with medications, can't take antidepressants for health reasons such as pregnancy or are at high risk of suicide.
Transcranial magnetic stimulation (TMS) is being investigated as an option for those who haven't responded to antidepressants.
Treatment in children and teenagers
Treatments for children and teenagers are generally decided on a case-by-case basis, depending on symptoms, medication side effects and other factors. Generally, treatment includes:
- Medications. Children and teens with bipolar disorder are often prescribed the same types of medications as those used in adults. There's less research on the safety and effectiveness of bipolar medications in children than in adults, so treatment decisions are often based on adult research.
- Psychotherapy. Initial and long-term therapy can help keep symptoms from returning. Psychotherapy can help children and teens manage their routines, develop coping skills, address learning difficulties, resolve social problems, and help strengthen family bonds and communication.
 And, if needed, it can help treat substance abuse problems common in older children and teens with bipolar disorder.
And, if needed, it can help treat substance abuse problems common in older children and teens with bipolar disorder. - Psychoeducation. Psychoeducation can include learning the symptoms of bipolar disorder and how they differ from behavior related to your child's developmental age, the situation and appropriate cultural behavior. Understanding about bipolar disorder can also help you support your child.
- Support. Working with teachers and school counselors and encouraging support from family and friends can help identify services and encourage success.
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar medications and weight gain
- Bipolar treatment: I vs. II
- Cognitive behavioral therapy
- Electroconvulsive therapy (ECT)
- Family therapy
- Psychotherapy
- Transcranial magnetic stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.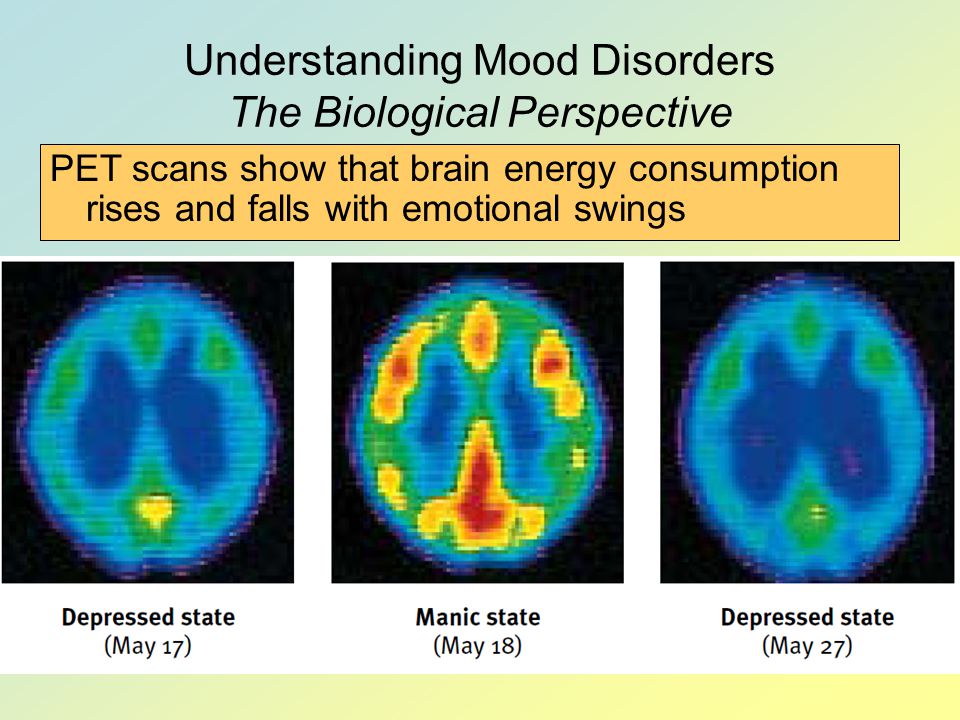
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.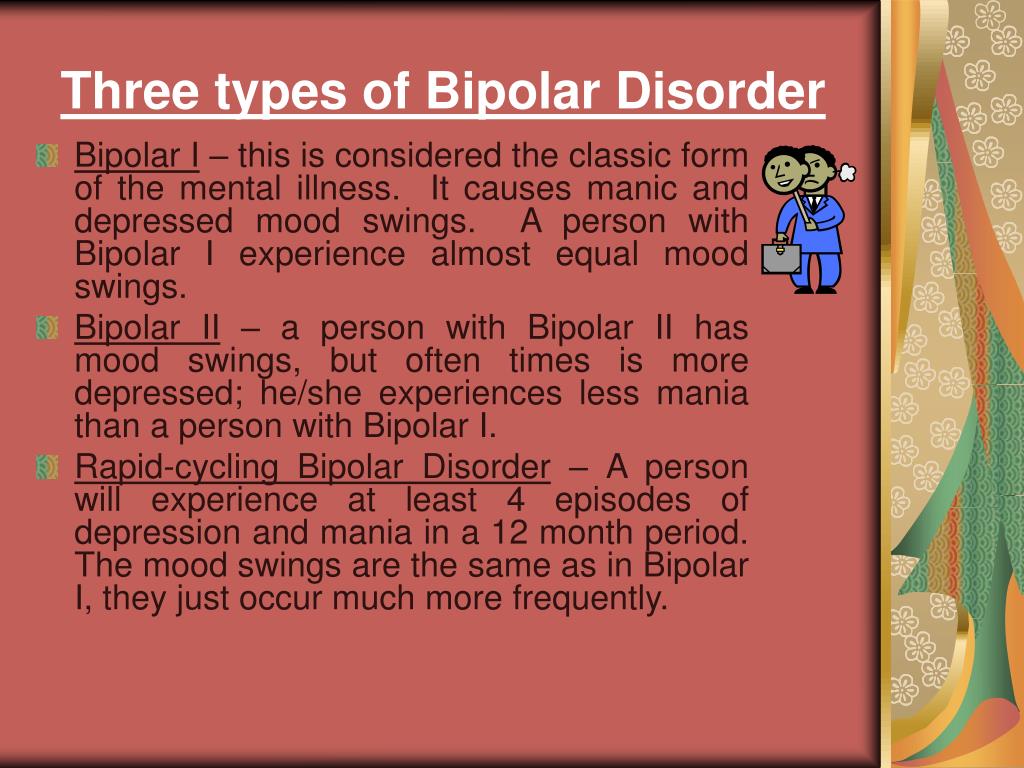
Lifestyle and home remedies
You'll probably need to make lifestyle changes to stop cycles of behavior that worsen your bipolar disorder. Here are some steps to take:
- Quit drinking or using recreational drugs. One of the biggest concerns with bipolar disorder is the negative consequences of risk-taking behavior and drug or alcohol abuse. Get help if you have trouble quitting on your own.
- Form healthy relationships. Surround yourself with people who are a positive influence. Friends and family members can provide support and help you watch for warning signs of mood shifts.
- Create a healthy routine. Having a regular routine for sleeping, eating and physical activity can help balance your moods. Check with your doctor before starting any exercise program. Eat a healthy diet. If you take lithium, talk with your doctor about appropriate fluid and salt intake. If you have trouble sleeping, talk to your doctor or mental health professional about what you can do.
- Check first before taking other medications. Call the doctor who's treating you for bipolar disorder before you take medications prescribed by another doctor or any over-the-counter supplements or medications. Sometimes other medications trigger episodes of depression or mania or may interfere with medications you're taking for bipolar disorder.
- Consider keeping a mood chart. Keeping a record of your daily moods, treatments, sleep, activities and feelings may help identify triggers, effective treatment options and when treatment needs to be adjusted.
Alternative medicine
There isn't much research on alternative or complementary medicine — sometimes called integrative medicine — and bipolar disorder. Most of the studies are on major depression, so it isn't clear how these nontraditional approaches work for bipolar disorder.
If you choose to use alternative or complementary medicine in addition to your physician-recommended treatment, take some precautions first:
- Don't stop taking your prescribed medications or skip therapy sessions.
 Alternative or complementary medicine is not a substitute for regular medical care when it comes to treating bipolar disorder.
Alternative or complementary medicine is not a substitute for regular medical care when it comes to treating bipolar disorder. - Be honest with your doctors and mental health professionals. Tell them exactly which alternative or complementary treatments you use or would like to try.
- Be aware of potential dangers. Alternative and complementary products aren't regulated the way prescription drugs are. Just because it's natural doesn't mean it's safe. Before using alternative or complementary medicine, talk to your doctor about the risks, including possible serious interactions with medications.
Coping and support
Coping with bipolar disorder can be challenging. Here are some strategies that can help:
- Learn about bipolar disorder. Education about your condition can empower you and motivate you to stick to your treatment plan and recognize mood changes. Help educate your family and friends about what you're going through.
- Stay focused on your goals. Learning to manage bipolar disorder can take time. Stay motivated by keeping your goals in mind and reminding yourself that you can work to repair damaged relationships and other problems caused by your mood swings.
- Join a support group. Support groups for people with bipolar disorder can help you connect to others facing similar challenges and share experiences.
- Find healthy outlets. Explore healthy ways to channel your energy, such as hobbies, exercise and recreational activities.
- Learn ways to relax and manage stress. Yoga, tai chi, massage, meditation or other relaxation techniques can be helpful.
Preparing for your appointment
You may start by seeing your primary care doctor or a psychiatrist. You may want to take a family member or friend along to your appointment, if possible, for support and to help remember information.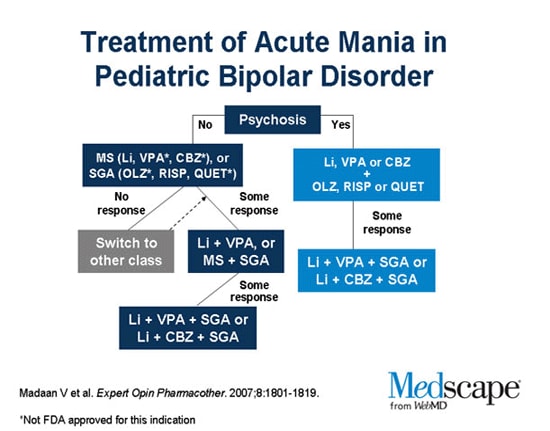
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for the appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins, herbs or other supplements you're taking, and the dosages
- Questions to ask your doctor
Some questions to ask your doctor may include:
- Do I have bipolar disorder?
- Are there any other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatments are available? Which do you recommend for me?
- What side effects are possible with that treatment?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions. How can I best manage these conditions together?
- Should I see a psychiatrist or other mental health professional?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask other questions during your appointment.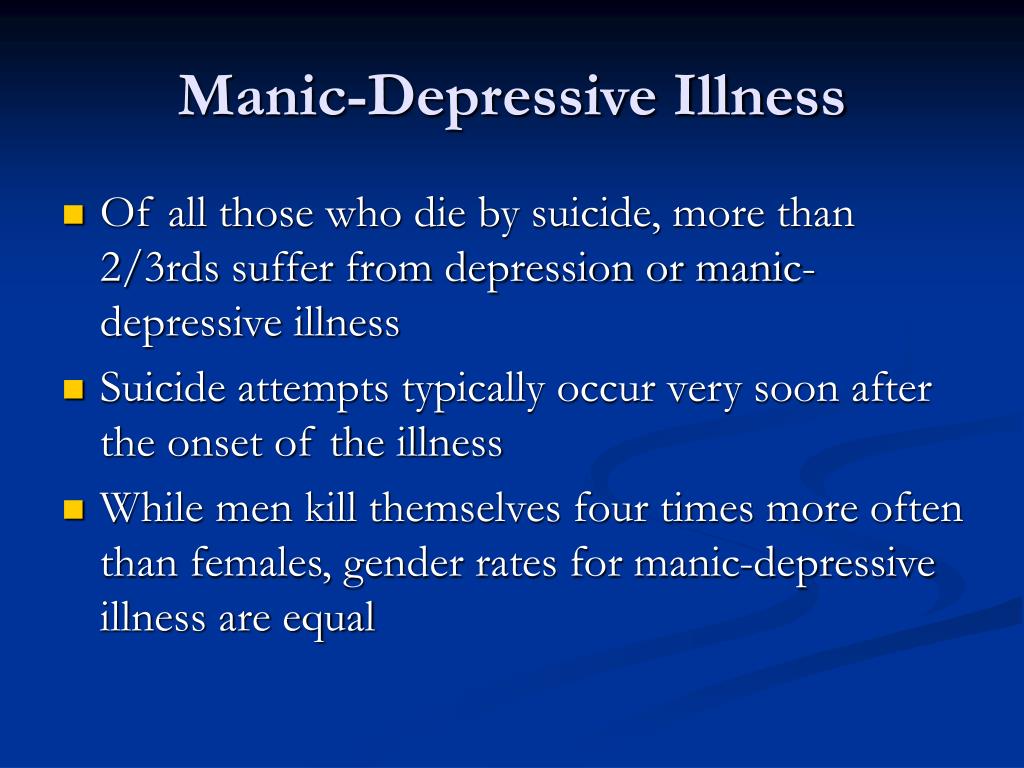
What to expect from your doctor
Your doctor will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first begin noticing your symptoms?
- How frequently do your moods change?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with bipolar disorder or depression?
- What other mental or physical health conditions do you have?
- Do you drink alcohol, smoke cigarettes or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- Do you go through periods when you take risks that you wouldn't normally take, such as unsafe sex or unwise, spontaneous financial decisions?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Manic disorders
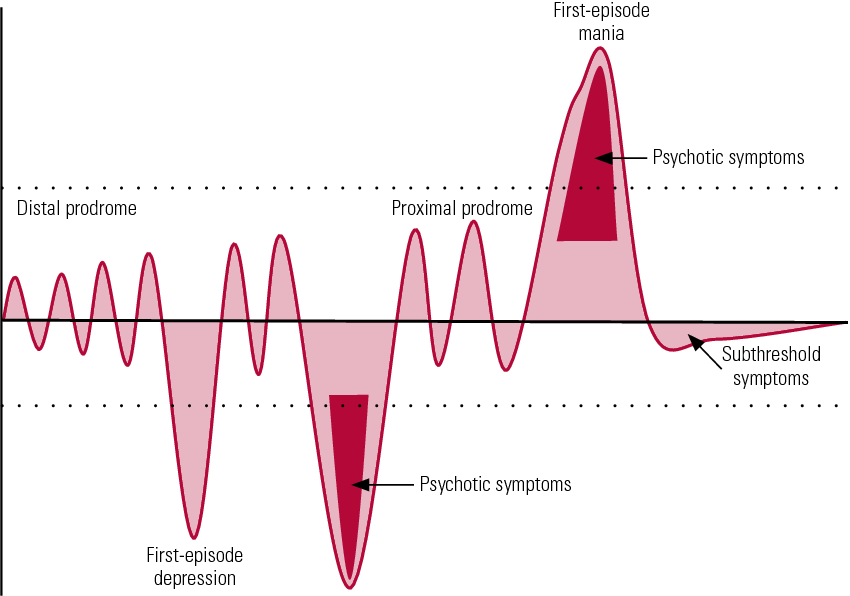
Classification of manic episodes by severity includes hypomania, mania without psychotic episodes, and mania with psychotic episodes.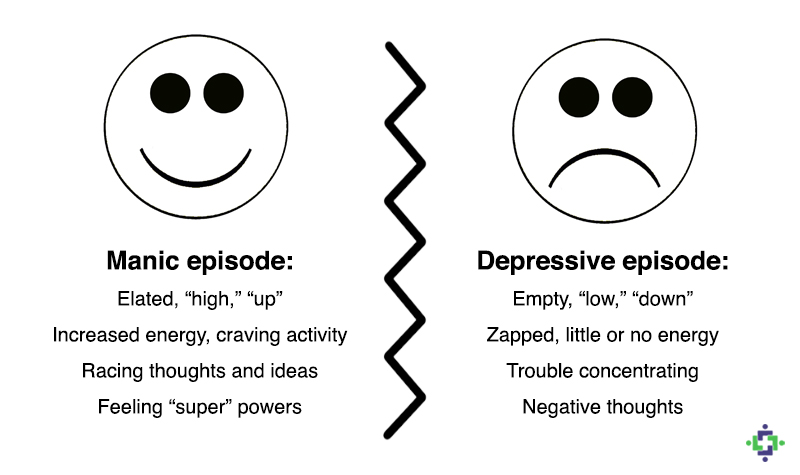
Under hypomania understand a mild degree of mania, in which changes in mood and behavior are long-term and pronounced, not accompanied by delusions and hallucinations. An elated mood manifests itself in the sphere of emotions as a joyful cloudlessness, irritability, in the sphere of speech - as increased talkativeness with ease and superficial judgments, increased contact. In the field of behavior, there is an increase in appetite, sexuality, distractibility, a decrease in the need for sleep, and individual actions that go beyond morality. Ease of associations, increase in working capacity and creative productivity are subjectively felt. Objectively, the number of social contacts and success increase. At the same time, there are episodes of reckless or irresponsible behavior, increased sociability or familiarity. nine0003
The main criterion for diagnosis is an elevated or irritable mood that is abnormal for the individual, persists for at least several days, and is accompanied by the above symptoms.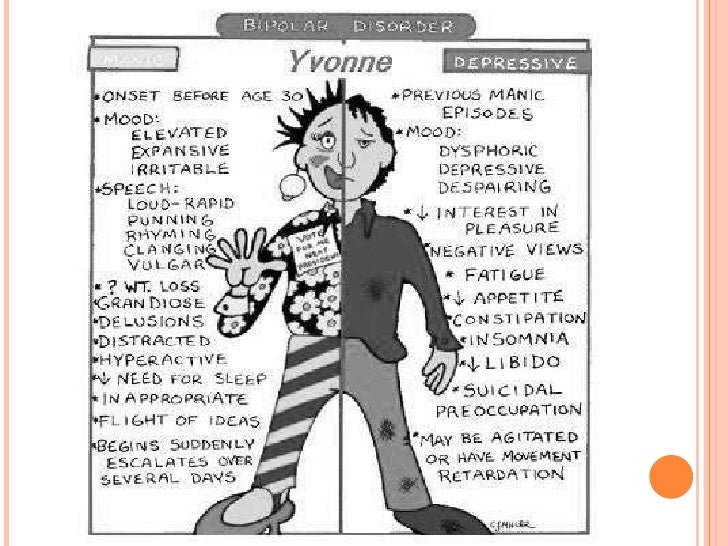
It should be noted that hypomanic episodes are possible in some somatic and psychiatric disorders. For example, with hyperthyroidism, anorexia or therapeutic starvation in the phase of food arousal; with intoxication with certain psychoactive substances - PAS (amphetamines, alcohol, marijuana, cocaine), however, there are other manifestations of somatic and mental pathology and PAS intoxication. nine0003
In its typical form , an extended manic state is manifested by the so-called manic triad: a painfully elevated mood, an accelerated flow of thoughts, and motor excitation. The leading sign of a manic state is a manic affect, manifested in an elevated mood, a feeling of happiness, contentment, well-being, an influx of pleasant memories and associations. It is characterized by an aggravation of sensations and perceptions, an increase in mechanical and some weakening of logical memory, superficial thinking, lightness and unproductiveness of judgments and conclusions, ideas of reassessment of one's own personality , up to delusional ideas of greatness, disinhibition of drives and weakening of higher feelings, instability, ease of switching attention.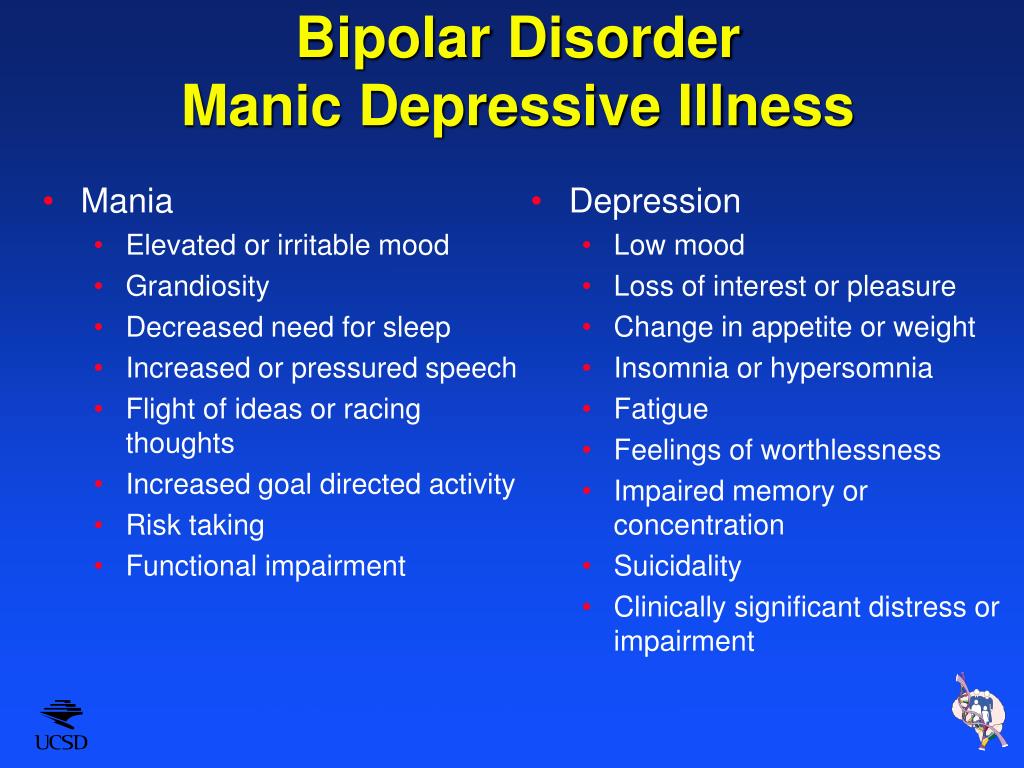
Mania without psychotic symptoms. The main difference from hypomania is that elevated mood affects the change in the norms of social functioning, manifests itself in inadequate actions that are not controlled by the patient. The pace of the passage of time accelerates and the need for sleep is significantly reduced. Tolerance and need for alcohol increase, sexual energy and appetite increase, there is a craving for travel and adventure. Thanks to the leap of ideas, many plans arise, the implementation of which is not carried out. The patient strives for bright and flashy clothes, speaks in a loud voice, incurs a lot of debt and gives money to people he hardly knows. He easily falls in love and is sure of the love of the whole world for himself. Gathering a lot of random people, he arranges holidays on credit. There is reckless driving, a marked increase in sexual energy, or sexual promiscuity. There are no hallucinations or delusions, although there may be perceptual disturbances (eg, subjective hyperacusis, vivid color perception).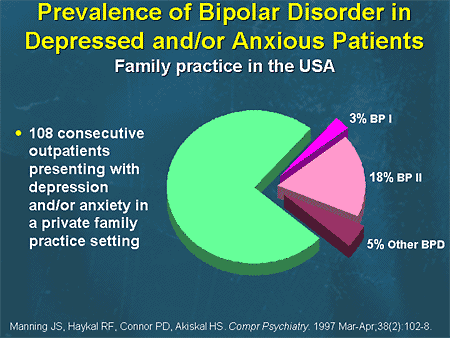 nine0003
nine0003
The main symptom is an elevated, expansive, irritable (angry) or suspicious mood, which is not characteristic of this individual. The change in mood should be distinct and persist throughout the week.
Mania with psychotic symptoms. It is a pronounced mania with a bright jump of ideas and manic excitement, to which secondary crazy ideas of greatness, high origin, hypereroticity, value join. There may be hallucinatory hails confirming the significance of the person, or "voices" telling the patient about emotionally neutral things, or delusions of meaning and persecution. The greatest difficulty lies in the differential diagnosis with schizoaffective disorders, however, with these disorders, there should be symptoms characteristic of schizophrenia, and delusions with them are less consistent with mood. However, the diagnosis can be considered as the starting point for the assessment of schizoaffective disorder (first episode). nine0003
Mental disorder formerly referred to as manic-depressive psychosis (MDP).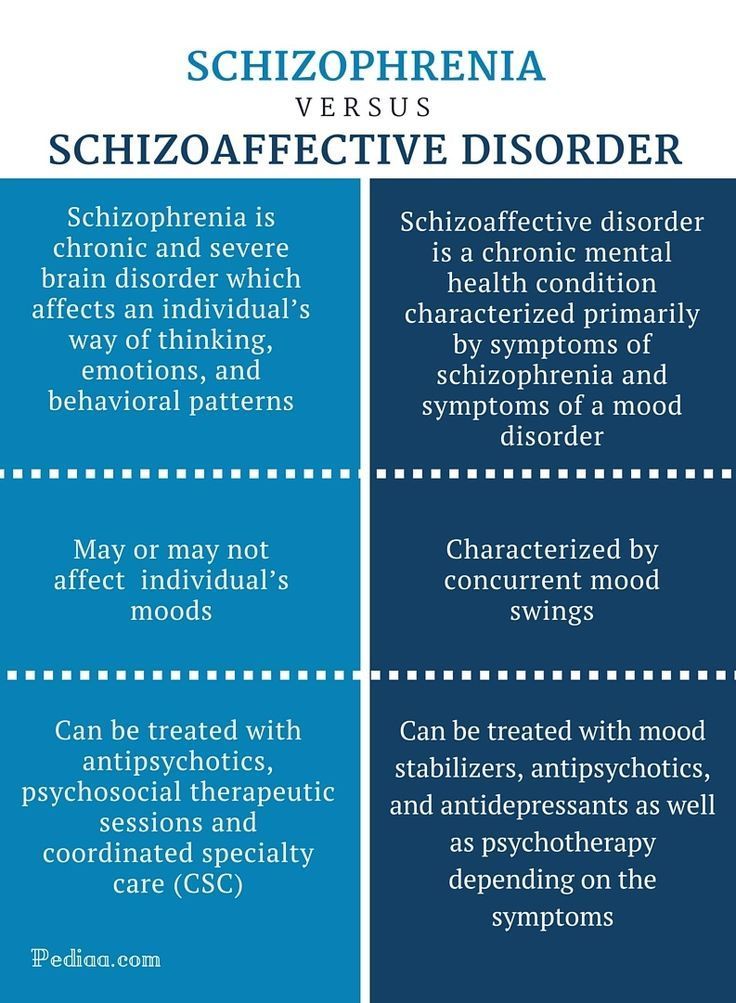 It is characterized by repeated (at least two) manic, depressive and mixed episodes that alternate without a definite sequence. A feature of this psychosis is the presence of light interphase gaps (intermissions), in which all signs of the disease disappear, a complete restoration of a critical attitude to the transferred painful condition is observed, premorbid characterological and personal properties, professional knowledge and skills are preserved. Its non-psychotic form (cyclothymia) in clinical terms is a reduced (weakened, outpatient) variant of the disease. nine0003
It is characterized by repeated (at least two) manic, depressive and mixed episodes that alternate without a definite sequence. A feature of this psychosis is the presence of light interphase gaps (intermissions), in which all signs of the disease disappear, a complete restoration of a critical attitude to the transferred painful condition is observed, premorbid characterological and personal properties, professional knowledge and skills are preserved. Its non-psychotic form (cyclothymia) in clinical terms is a reduced (weakened, outpatient) variant of the disease. nine0003
Manic episodes usually start suddenly and last from two weeks to 4-5 months (mean episode duration about 4 months). Depression tends to last longer (average duration about 6 months), although rarely more than a year (excluding elderly patients). Both episodes often follow stressful situations or trauma, although their presence is not required for a diagnosis. The first episode can occur at any age. The frequency of episodes and the pattern of remissions and exacerbations are highly variable, but remissions tend to shorten with age, and depressions become more frequent and prolonged after middle age. nine0003
nine0003
Although the earlier concept of manic-depressive disorder included patients who suffered only from depression, the term MDP is now used mainly as a synonym for bipolar disorder.
ATTENTION!!! Self-treatment is not allowed in any cases, a psychotherapist is needed
Manic personality disorder: symptoms, treatment
A condition accompanied by an increased level of affect, excitability. It is often referred to by psychiatrists as "the mirror image of depression." All signs of a depressive state are manifested completely opposite. The patient is characterized by an increased desire for life, reaching hyper-manifestations. nine0003
Manifested by a constant increase in symptoms, reaching severe manifestations of aggression. There is a tendency to aggression, anxiety grows.
Most commonly associated with manic-depressive disorder, but often indicative of other psychiatric diagnoses. For example, schizoaffective disorder, multiple sclerosis.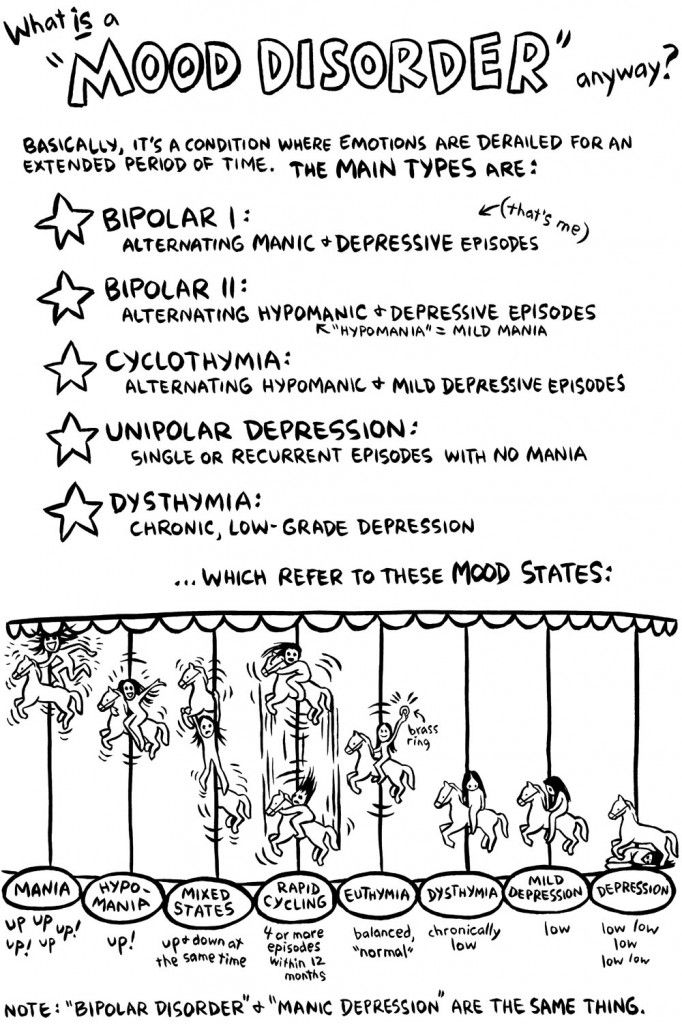 Often occurs on the background of taking medications. Like Prednisolone. The intake of anabolic drugs, drugs becomes a provocateur. First of all, cocaine. nine0003
Often occurs on the background of taking medications. Like Prednisolone. The intake of anabolic drugs, drugs becomes a provocateur. First of all, cocaine. nine0003
Manic disorder, symptoms
Symptoms differ between the mild stage, so-called hypomania, and insane mania. In the latter case, it is noted:
- disorientation;
- incoherent speech;
- pronounced psychosis;
- catatonia.
When diagnosing, the Altman self-assessment scale is used. The Young rating scale is applied. It often accompanies artistic and creative talent, without reaching a pathological level in such situations. nine0003
Bipolar manic disorder
Is a manifestation of MDP. It is observed in patients alternately with depressive states. In MDP, bipolar disorder is characterized by increased activity. Patients become hyperexcitable, lose control of behavior, actively entering into a dialogue. In manic-depressive psychosis, mania is always imputed as a period of depression.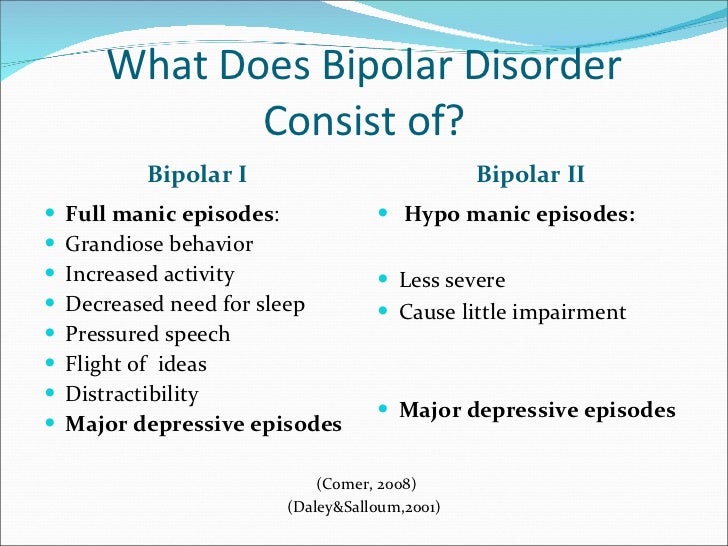
Manic phase of bipolar disorder
Passing into this stage, the patient with MDP strikes with a high degree of activity. The patient is prone to agitated actions. There is an increased level of self-confidence, confidence in their abilities. The period of continuous increase in activity lasts from several days to several weeks. Perhaps a state of hysteria, cases of increased aggression are detected. The patient in this state is capable of harming himself and others. nine0003
Manic personality disorder
The patient is unable to control his behavior. In medical practice, there are several variants of pathology. Each of them requires a clear definition for the appointment of an adequate course of therapy.
Bipolar disorder, manic-depressive psychosis
It is a complex somatic psychiatric disease requiring constant treatment and observation.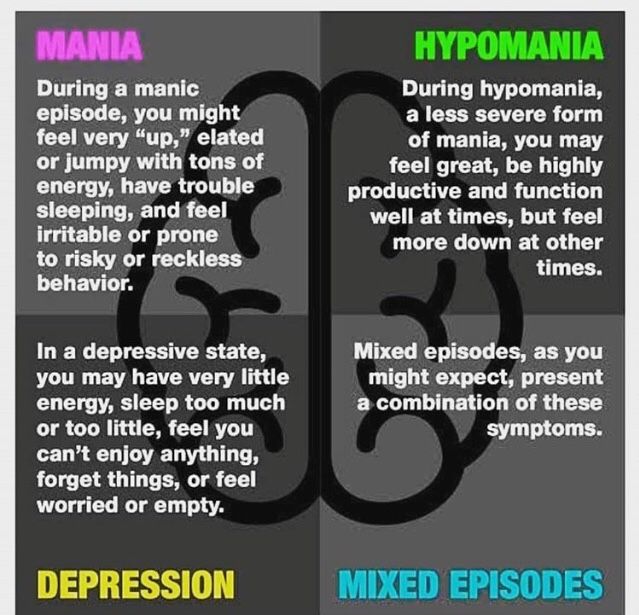 It is accompanied by periods of remission, a change from a manic, agitated state to a depressive one. nine0003
It is accompanied by periods of remission, a change from a manic, agitated state to a depressive one. nine0003
Manic depressive disorder
Accompanied by the patient being depressed most of the time. Often there are reflections on the meaninglessness of life. The patient loses interest in any form of activity.
Manic mental disorder
Recognized as the most affective of all bipolar disorders. It affects one in a hundred inhabitants of the planet. It usually starts before the age of 35. Euphoria easily turns into a depressed mood. During a period of unreasonable optimism, patients often lose their judgment, they may begin to consider themselves other personalities, for example, world leaders and heroes. Often occurs as a concomitant diagnosis of schizophrenia. It leads to serious personal lesions that contribute to the emergence of disability and disruption of ties in society and the family. nine0003
Manic affective disorder
Refers to manifestations of manic-depressive psychosis.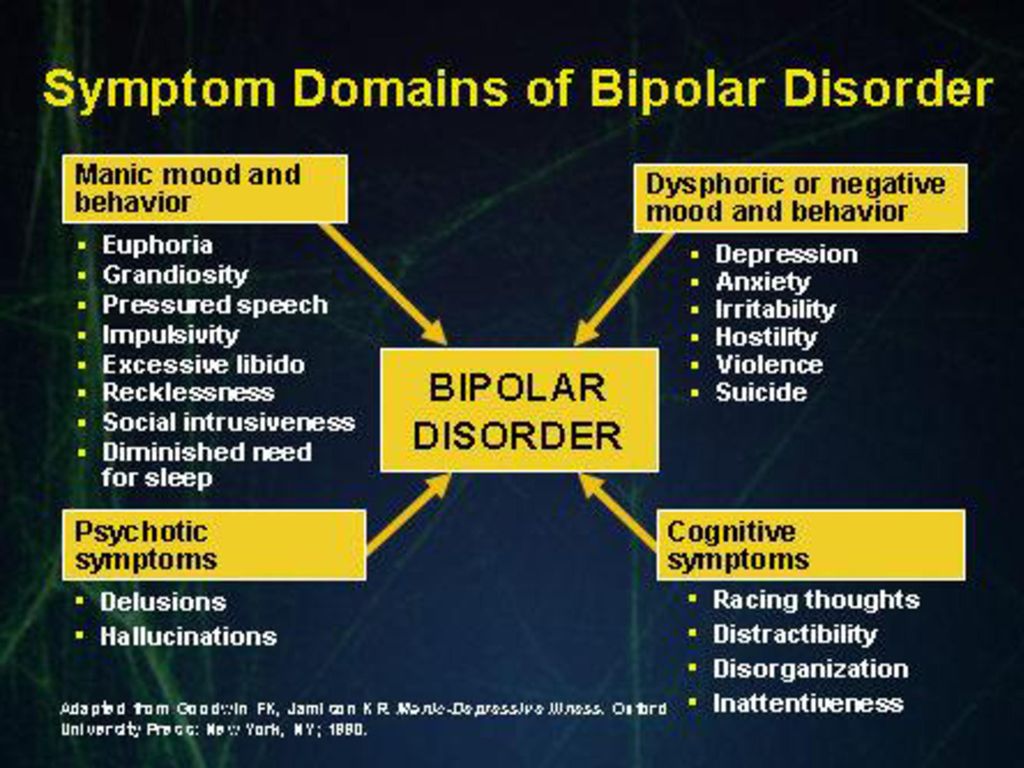 The patient loses control of mood swings. Often mood swings are observed several times during the day. It can become violent or vice versa fall into a state close to catatonia. The condition requires a mandatory referral to a specialist for advice. Many patients need to stay in the stage of active development in the hospital.
The patient loses control of mood swings. Often mood swings are observed several times during the day. It can become violent or vice versa fall into a state close to catatonia. The condition requires a mandatory referral to a specialist for advice. Many patients need to stay in the stage of active development in the hospital.
Manic depressive bipolar disorder
It is the most striking manifestation of MDP with frequent changes in the patient's mood from deep euphoria to severe depression. The patient is unable to independently control abrupt changes. Pathology leads to a sharp decrease in the quality of life. Patients in the stage of depression go into a state of sharp rejection of the surrounding life. They become completely isolated from the outside world, catatonia may develop. During the period of the predominance of the manic state, patients are also difficult in everyday communication. They become overly friendly to strangers and often show aggression towards loved ones.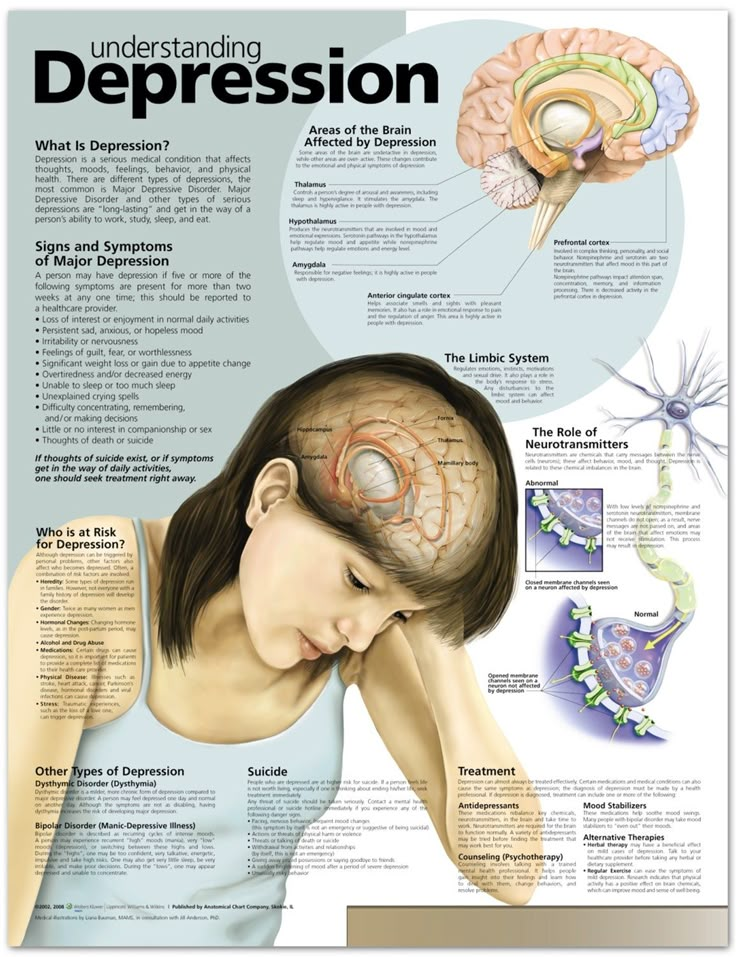 nine0003
nine0003
Any manic disorder requires immediate medical attention. Light stages are treated on an outpatient basis. In difficult situations, mandatory hospitalization is required to prescribe a course of adequate therapy. The disease requires life-long monitoring of the condition in any variant. Preventive medical examinations are recommended. Relatives and relatives of the patient are recommended to immediately contact a doctor for an invitation to examine the patient. In the depressive stage, there is a lack of desire to go to the doctors on their own due to the lack of desire and interest in life. The manic stage is accompanied by a denial of the presence of a complex diagnosis that can lead to attacks of strong and dangerous aggression. nine0003
When prescribing a course of therapy, a family history study is carried out. Often this disease is caused by family predisposition and heredity. The cause of the start of the pathology is also alcohol or drug addiction, which needs separate treatment.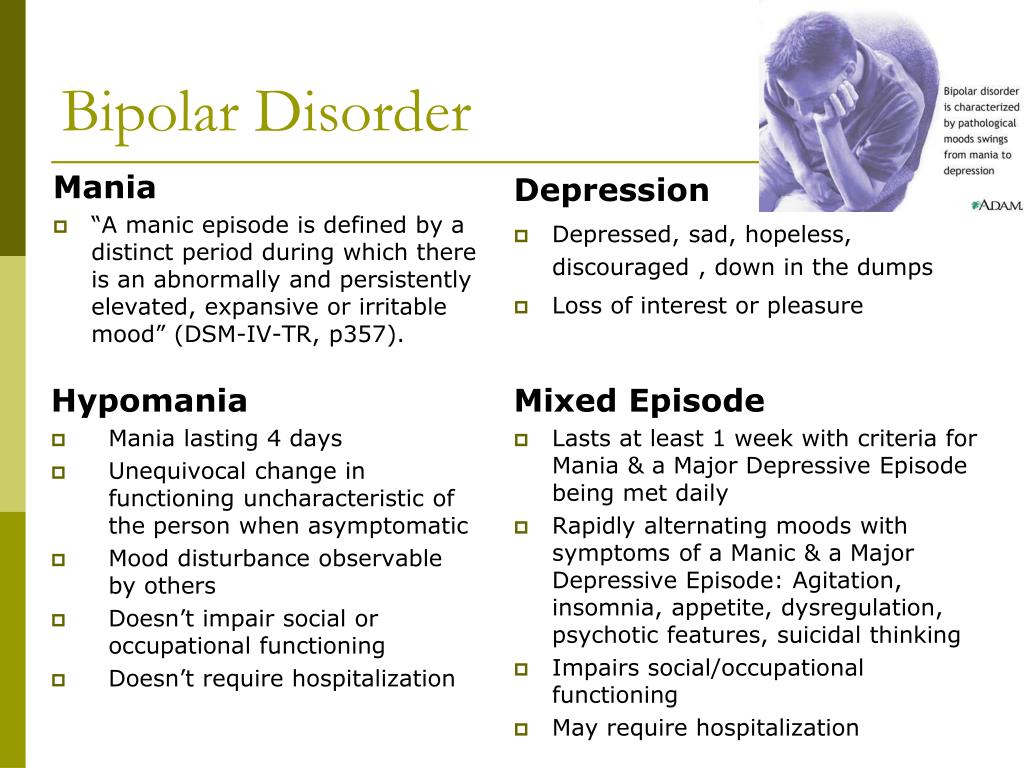 There may be additional psychiatric diagnoses. It also occurs against the background of taking part of the medication or as a manifestation of undiagnosed injuries, accompanied by damage to the cerebral cortex. nine0003
There may be additional psychiatric diagnoses. It also occurs against the background of taking part of the medication or as a manifestation of undiagnosed injuries, accompanied by damage to the cerebral cortex. nine0003
24-hour free consultations
8 (495) 664-40-40
We will be happy to answer all your questions!
The Salvation Private Clinic has been providing effective treatment for various psychiatric diseases and disorders for 19 years. Psychiatry is a complex area of medicine that requires doctors to have maximum knowledge and skills. Therefore, all employees of our clinic are highly professional, qualified and experienced specialists.
When to ask for help? nine0079
Have you noticed that your relative (grandmother, grandfather, mother or father) does not remember elementary things, forgets dates, names of objects or even does not recognize people? This clearly indicates some kind of mental disorder or mental illness. Self-medication in this case is not effective and even dangerous. Pills and medications taken on their own, without a doctor's prescription, at best, temporarily alleviate the patient's condition and relieve symptoms. At worst, they will cause irreparable harm to human health and lead to irreversible consequences. Alternative treatment at home is also not able to bring the desired results, not a single folk remedy will help with mental illness. By resorting to them, you will only lose precious time, which is so important when a person has a mental disorder. nine0003
Pills and medications taken on their own, without a doctor's prescription, at best, temporarily alleviate the patient's condition and relieve symptoms. At worst, they will cause irreparable harm to human health and lead to irreversible consequences. Alternative treatment at home is also not able to bring the desired results, not a single folk remedy will help with mental illness. By resorting to them, you will only lose precious time, which is so important when a person has a mental disorder. nine0003
If your relative has a bad memory, complete loss of memory, other signs that clearly indicate a mental disorder or a serious illness, do not hesitate, contact the Salvation Private Psychiatric Clinic.
Why choose us?
The clinic "Salvation" successfully treats fears, phobias, stress, memory disorders, psychopathy. We provide oncology care, stroke care, inpatient care for the elderly, elderly patients, and cancer treatment. We do not refuse the patient, even if he has the last stage of the disease. nine0003
nine0003
Many government agencies are reluctant to take on patients over the age of 50-60. We help everyone who applies and willingly provide treatment after 50-60-70 years. For this we have everything you need:
- boarding house;
- nursing home;
- bed hospice;
- professional nurses;
- sanatorium.
Old age is no reason to let the disease take its course! Complex therapy and rehabilitation gives every chance for the restoration of basic physical and mental functions in the vast majority of patients and significantly increases life expectancy. nine0003
Our specialists use modern methods of diagnostics and treatment, the most effective and safe medicines, hypnosis. If necessary, visits to the house are carried out, where doctors:
- conduct an initial examination;
- causes of mental disorder are investigated;
- a preliminary diagnosis is made;
- relieves acute attack or hangover;
- in severe cases, it is possible to force the patient to be placed in a hospital - a closed-type rehabilitation center.