Schizophrenia behavioral symptoms
Schizophrenia - Symptoms and causes
Overview
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
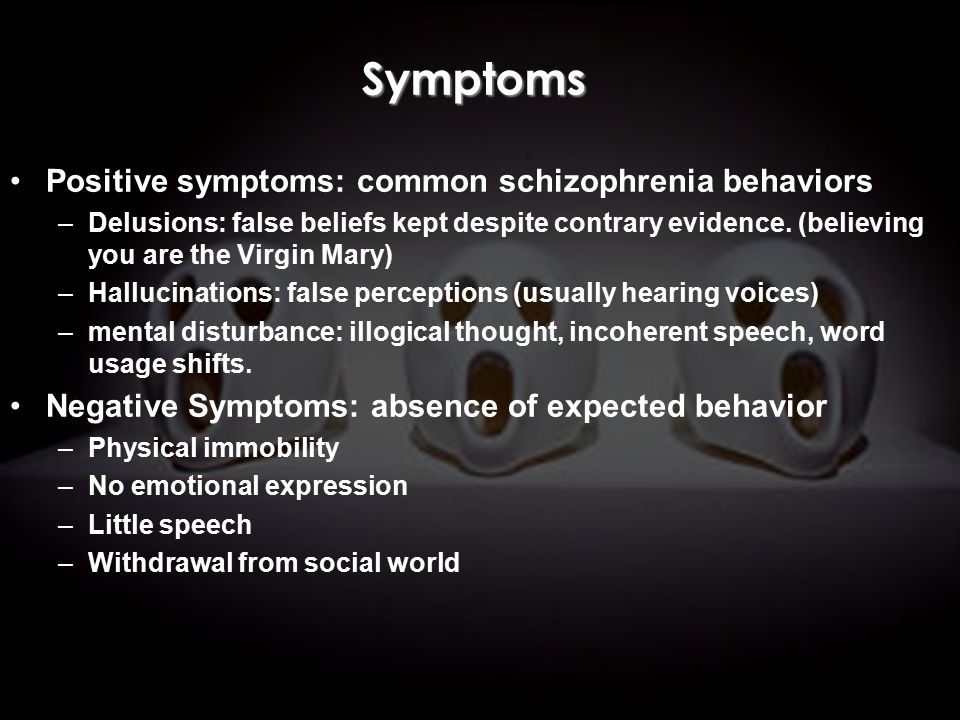
Symptoms
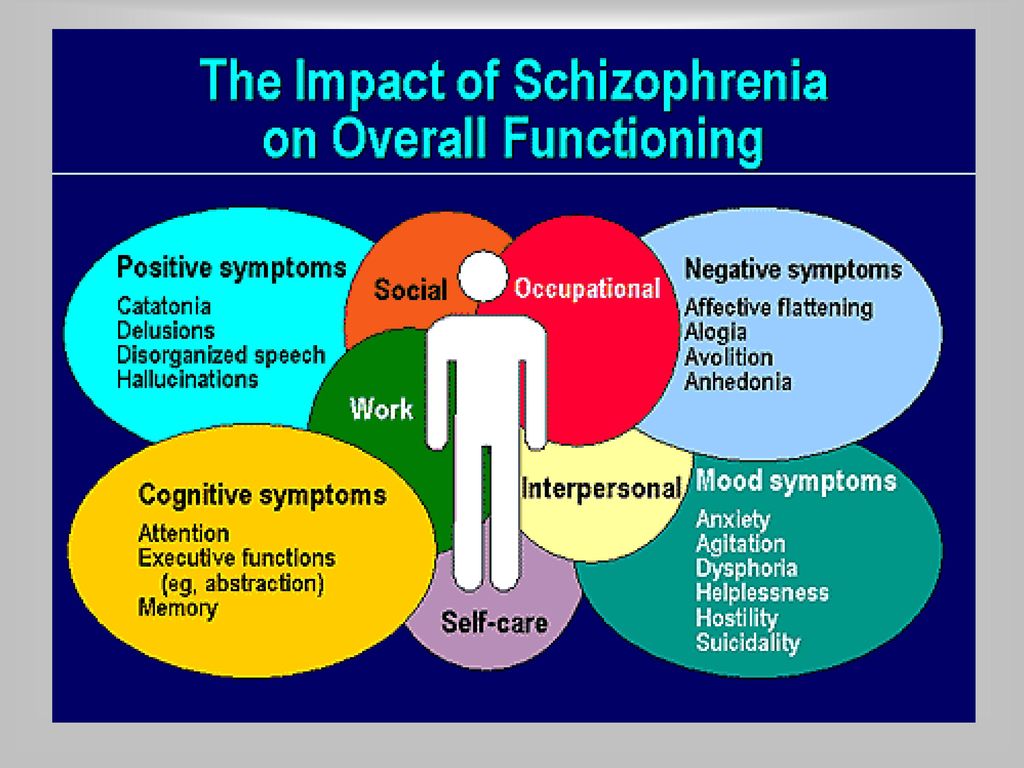
Schizophrenia involves a range of problems with thinking (cognition), behavior and emotions. Signs and symptoms may vary, but usually involve delusions, hallucinations or disorganized speech, and reflect an impaired ability to function. Symptoms may include:
- Delusions. These are false beliefs that are not based in reality.
For example, you think that you're being harmed or harassed; certain gestures or comments are directed at you; you have exceptional ability or fame; another person is in love with you; or a major catastrophe is about to occur. Delusions occur in most people with schizophrenia.
- Hallucinations. These usually involve seeing or hearing things that don't exist. Yet for the person with schizophrenia, they have the full force and impact of a normal experience. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganized thinking (speech). Disorganized thinking is inferred from disorganized speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated. Rarely, speech may include putting together meaningless words that can't be understood, sometimes known as word salad.
- Extremely disorganized or abnormal motor behavior.
 This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement.
This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement. - Negative symptoms. This refers to reduced or lack of ability to function normally. For example, the person may neglect personal hygiene or appear to lack emotion (doesn't make eye contact, doesn't change facial expressions or speaks in a monotone). Also, the person may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Symptoms can vary in type and severity over time, with periods of worsening and remission of symptoms. Some symptoms may always be present.
In men, schizophrenia symptoms typically start in the early to mid-20s. In women, symptoms typically begin in the late 20s. It's uncommon for children to be diagnosed with schizophrenia and rare for those older than age 45.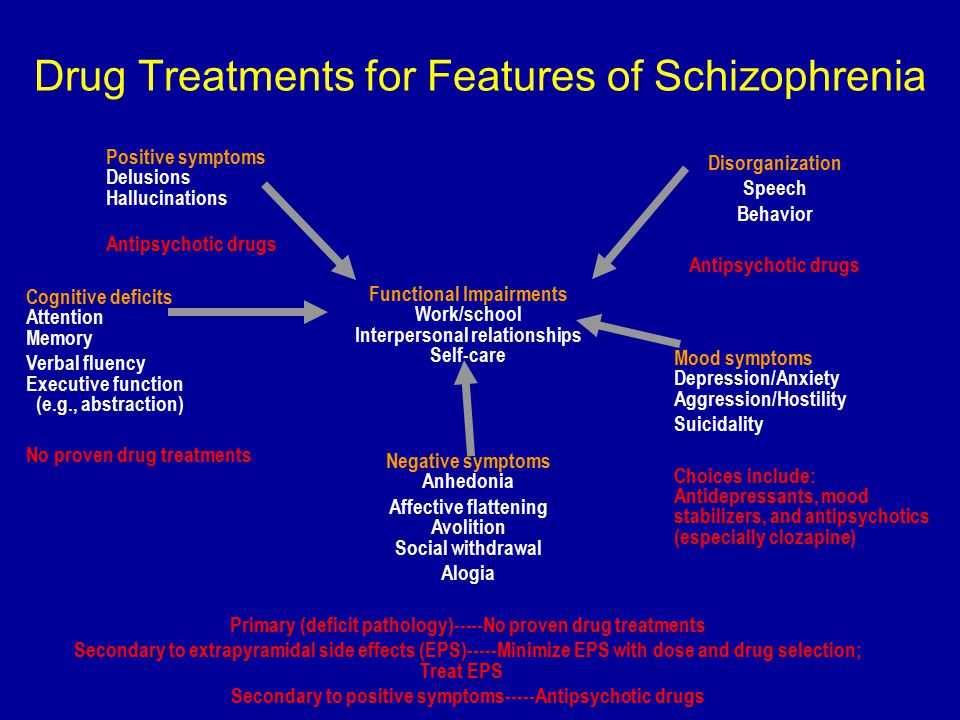
Symptoms in teenagers
Schizophrenia symptoms in teenagers are similar to those in adults, but the condition may be more difficult to recognize. This may be in part because some of the early symptoms of schizophrenia in teenagers are common for typical development during teen years, such as:
- Withdrawal from friends and family
- A drop in performance at school
- Trouble sleeping
- Irritability or depressed mood
- Lack of motivation
Also, recreational substance use, such as marijuana, methamphetamines or LSD, can sometimes cause similar signs and symptoms.
Compared with schizophrenia symptoms in adults, teens may be:
- Less likely to have delusions
- More likely to have visual hallucinations
When to see a doctor
People with schizophrenia often lack awareness that their difficulties stem from a mental disorder that requires medical attention. So it often falls to family or friends to get them help.
Helping someone who may have schizophrenia
If you think someone you know may have symptoms of schizophrenia, talk to him or her about your concerns. Although you can't force someone to seek professional help, you can offer encouragement and support and help your loved one find a qualified doctor or mental health professional.
If your loved one poses a danger to self or others or can't provide his or her own food, clothing, or shelter, you may need to call 911 or other emergency responders for help so that your loved one can be evaluated by a mental health professional.
In some cases, emergency hospitalization may be needed. Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and behavior are common among people with schizophrenia. If you have a loved one who is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person.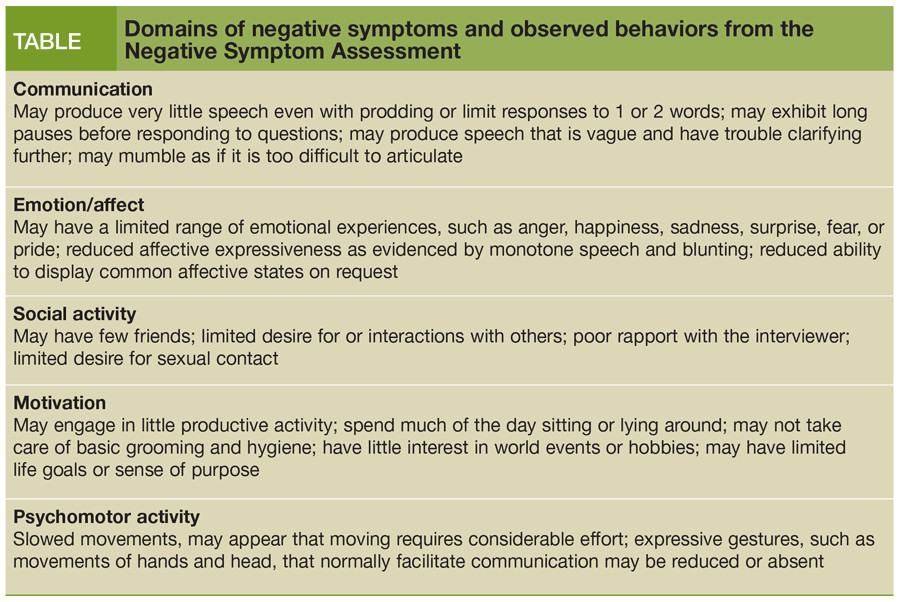 Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.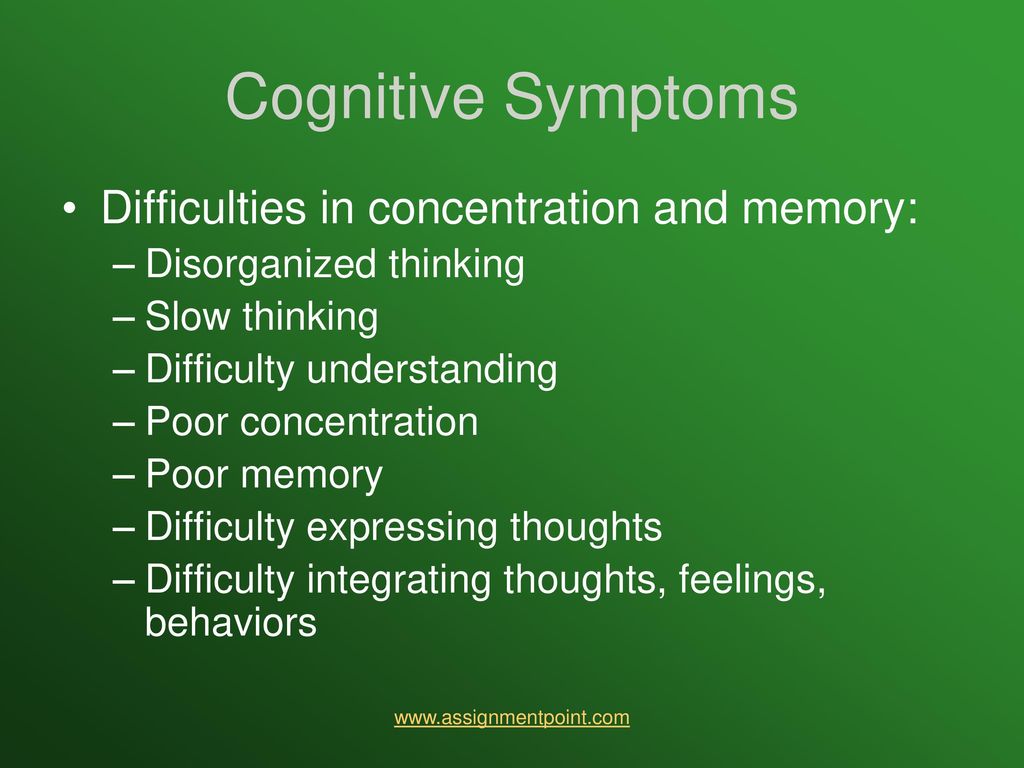 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
It's not known what causes schizophrenia, but researchers believe that a combination of genetics, brain chemistry and environment contributes to development of the disorder.
Problems with certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neuroimaging studies show differences in the brain structure and central nervous system of people with schizophrenia. While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
Risk factors
Although the precise cause of schizophrenia isn't known, certain factors seem to increase the risk of developing or triggering schizophrenia, including:
- Having a family history of schizophrenia
- Some pregnancy and birth complications, such as malnutrition or exposure to toxins or viruses that may impact brain development
- Taking mind-altering (psychoactive or psychotropic) drugs during teen years and young adulthood
Complications
Left untreated, schizophrenia can result in severe problems that affect every area of life.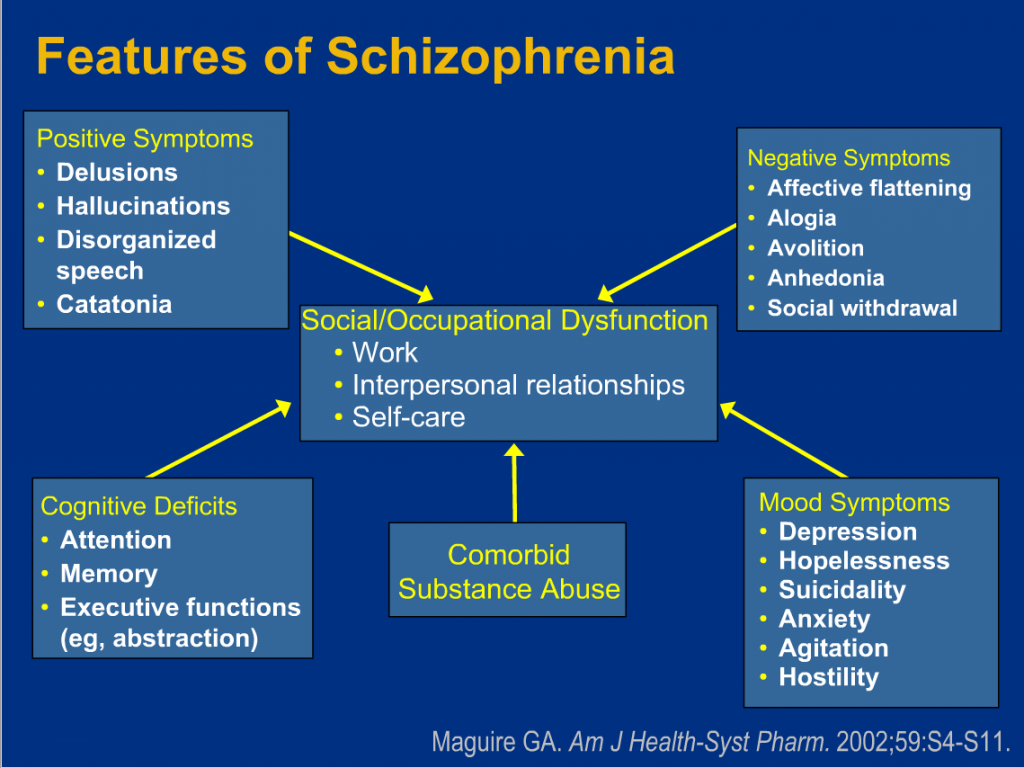 Complications that schizophrenia may cause or be associated with include:
Complications that schizophrenia may cause or be associated with include:
- Suicide, suicide attempts and thoughts of suicide
- Anxiety disorders and obsessive-compulsive disorder (OCD)
- Depression
- Abuse of alcohol or other drugs, including nicotine
- Inability to work or attend school
- Financial problems and homelessness
- Social isolation
- Health and medical problems
- Being victimized
- Aggressive behavior, although it's uncommon
Prevention
There's no sure way to prevent schizophrenia, but sticking with the treatment plan can help prevent relapses or worsening of symptoms. In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Schizophrenia Symptoms: Behavior, Delusions, and Coping
Schizophrenia is a type of mental health condition that can change how you think and act, as well as how you feel.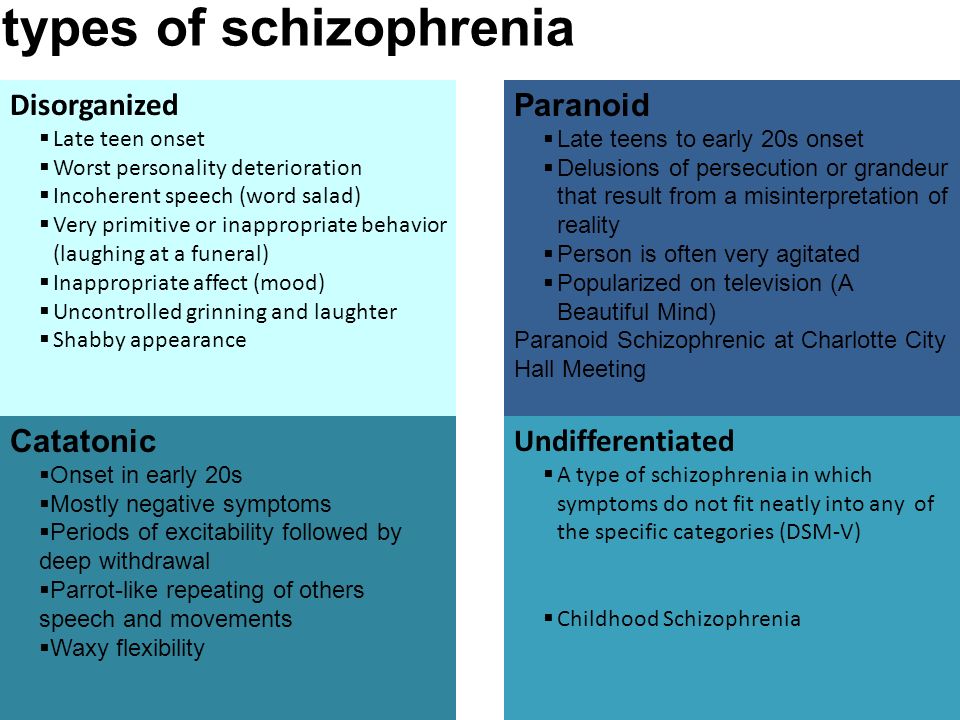
The symptoms can be severe enough to disrupt daily life, performance in school and work, and relationships. It’s estimated that one-third of people treated for schizophrenia still struggle with their symptoms.
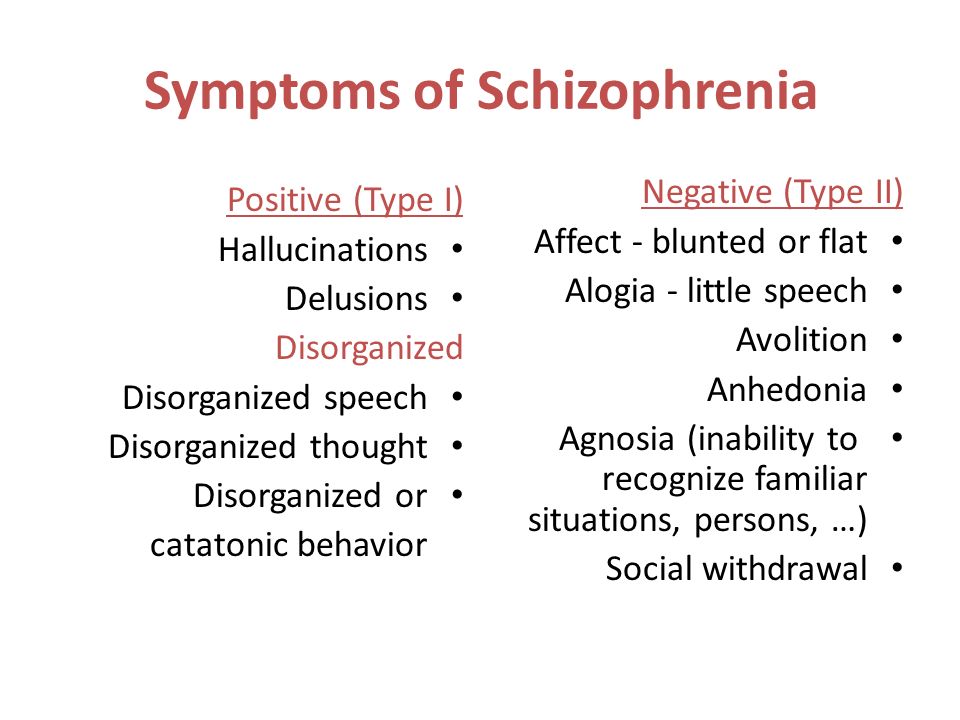
Schizophrenia symptoms may be further broken down into three types:
- negative
- positive
- cognitive
Negative symptoms result in the absence of what might be considered “normal” functions, like motivation, speech, and thinking skills. Positive ones are attributed to symptoms that are present but shouldn’t be, like delusions and hallucinations.
Cognitive symptoms affect brain functions like concentration, memory, and attention. These symptoms may impact your ability to navigate and complete your daily routine.
To diagnose schizophrenia, a mental health professional, like a psychiatrist, will conduct an exam along with tests to rule out other possible neurological or mental health conditions.
The examining psychiatrist may also need to speak with friends, family members, or other physicians for corroborative information that can help to assess the quality and duration of symptoms.
Typically, your symptoms will occur for 6 months or longer to be considered schizophrenia.
Negative symptoms of schizophrenia are typically seen through decreased motivation and social withdrawal. These symptoms may also be sometimes misdiagnosed as those related to clinical depression.
Below, you’ll find some of the most common negative symptoms of schizophrenia.
Lack of pleasure (anhedonia)
Often associated with clinical depression, a lack of pleasure in things you once enjoyed can also be a symptom of schizophrenia. This may include socializing, favorite hobbies, activities, and more.
It’s also important to note the possibility of having both depression and schizophrenia at the same time. According to a 2017 review, it’s estimated that about 40 percent of people with schizophrenia may experience depression.
If depression exists in patients with schizophrenia, a more careful evaluation of symptom duration may help to clarify whether it could be schizoaffective disorder, bipolar disorder, or a psychotic depression.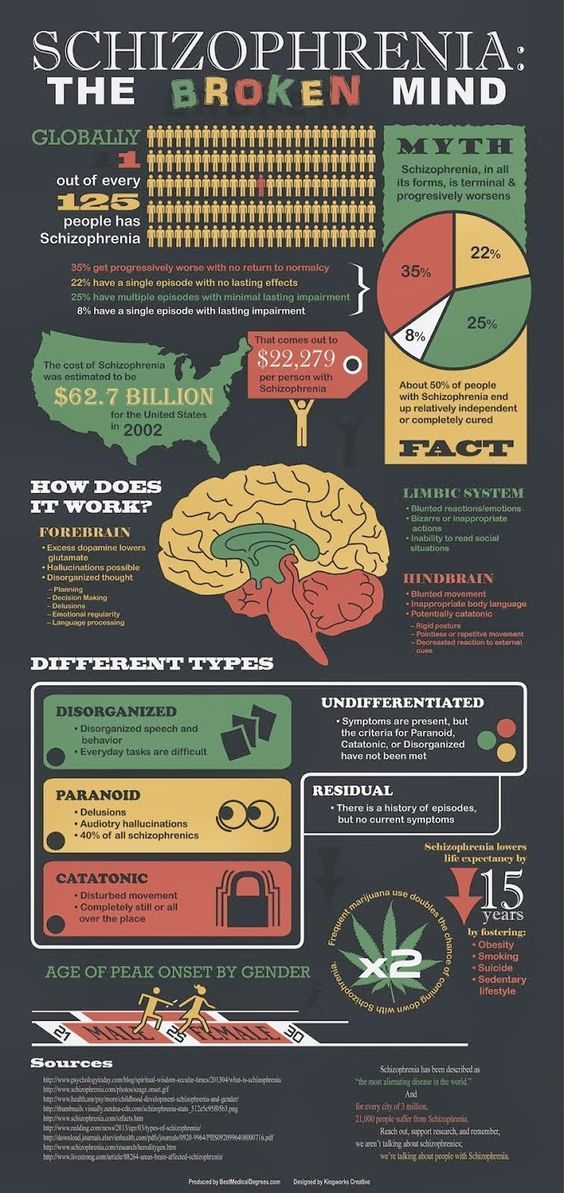
Trouble with speech (alogia)
Schizophrenia may cause a type of speech difficulty called alogia. It’s thought that trouble with speech in schizophrenia is attributed to difficulties with putting thoughts together.
You might notice a loved one not making much logical sense with their words. This can be confusing if you’ve known them for a long time and it’s not in line with their usual behavior.
Affective flatteningA person with affective flattening, may appear stoic or expressionless in their facial appearance. Their voice may sound “flat” or “blunted”. This symptom is sometimes mischaracterized as apathy.
Trouble with daily tasks (avolition)
While you might experience a lack of motivation from time to time, schizophrenia may cause a more extreme form called avolition. It can make everyday tasks, like getting dressed and brushing your teeth, very difficult to accomplish.
Decreased desire to socialize
Another possible symptom seen in clinical depression, a desire to withdraw from others is another symptom that can occur in schizophrenia.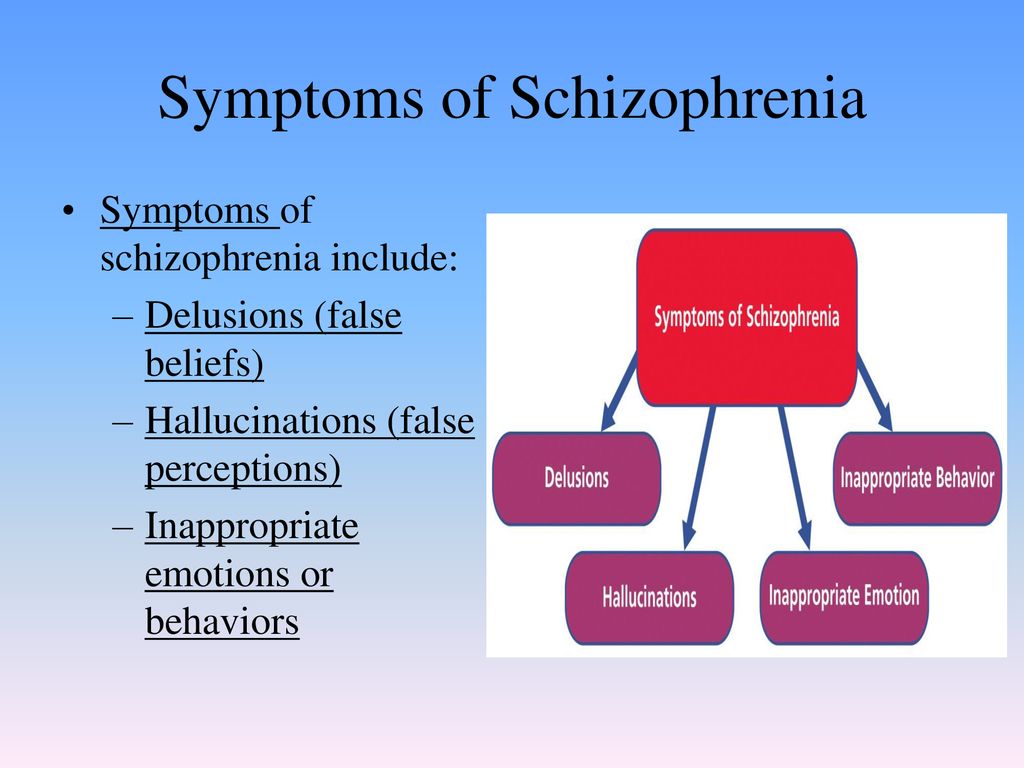 You may also lack a desire to have a conversation with your friends and loved ones.
You may also lack a desire to have a conversation with your friends and loved ones.
Positive symptoms of schizophrenia are ones that are atypically present, as they can disrupt a person’s grasp of reality. Some mental health professionals also collectively refer to these symptoms as psychosis. Positive symptoms are experienced on a more “active” basis.
Consider the most common positive symptoms of schizophrenia:
Hallucinations
Hallucinations refers to sensory experiences that may seem like they’re really happening, but they don’t actually occur in real life.
In schizophrenia, hallucinations may be further broken down into the following types:
- auditory (the most common), in which you hear voices
- visual, which can cause you to vividly see people or items
- tastes or smells, including good or bad ones
- physical or tactile sensations
Delusions
Delusions refer to thinking or fixation around false beliefs. These may seem unreasonable — and easy to prove wrong — to others.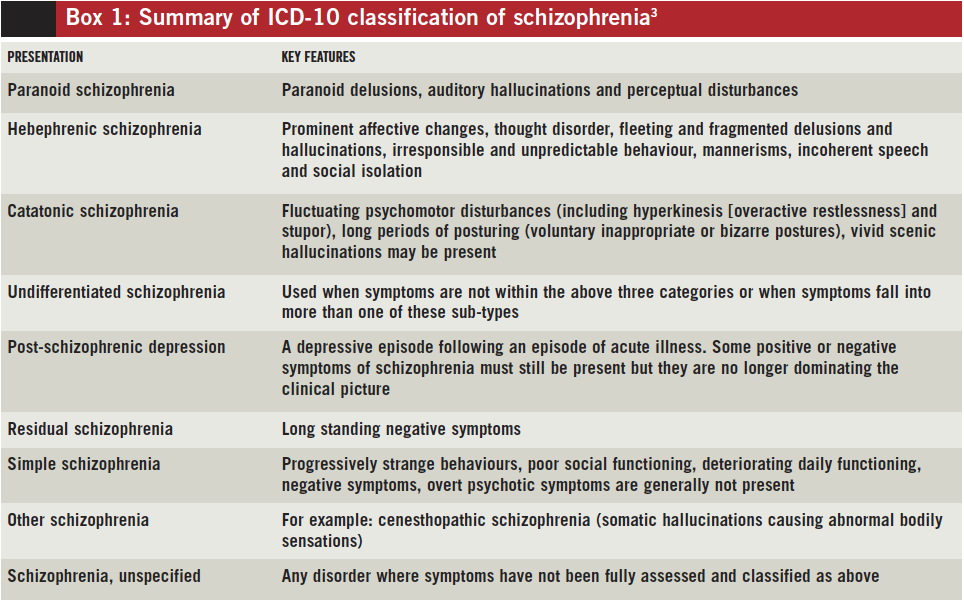 But, like hallucinations, they are very real to the person experiencing them.
But, like hallucinations, they are very real to the person experiencing them.
Types of delusions may include:
- paranoid/persecutory, which can cause you to believe others want to harm you or follow you
- grandiose, where you might believe you are rich, famous, or extremely talented
- referential, in which there’s a belief that public art or communications are directed towards you
- delusional jealousy/erotomanic, which can cause you to think a famous person is in love with you, or are convinced that your current partner is cheating on you
- religious, in which you might believe you have connections with a deity or a demon
- somatic, where you have delusions about your own body pertaining to an unlikely illness, or missing part
Movement disorders
Schizophrenia may cause a state of catatonia, in which you lie unusually still for long periods of time. On the flipside, you might also feel unusually jumpy, and perhaps engage in different movements repeatedly.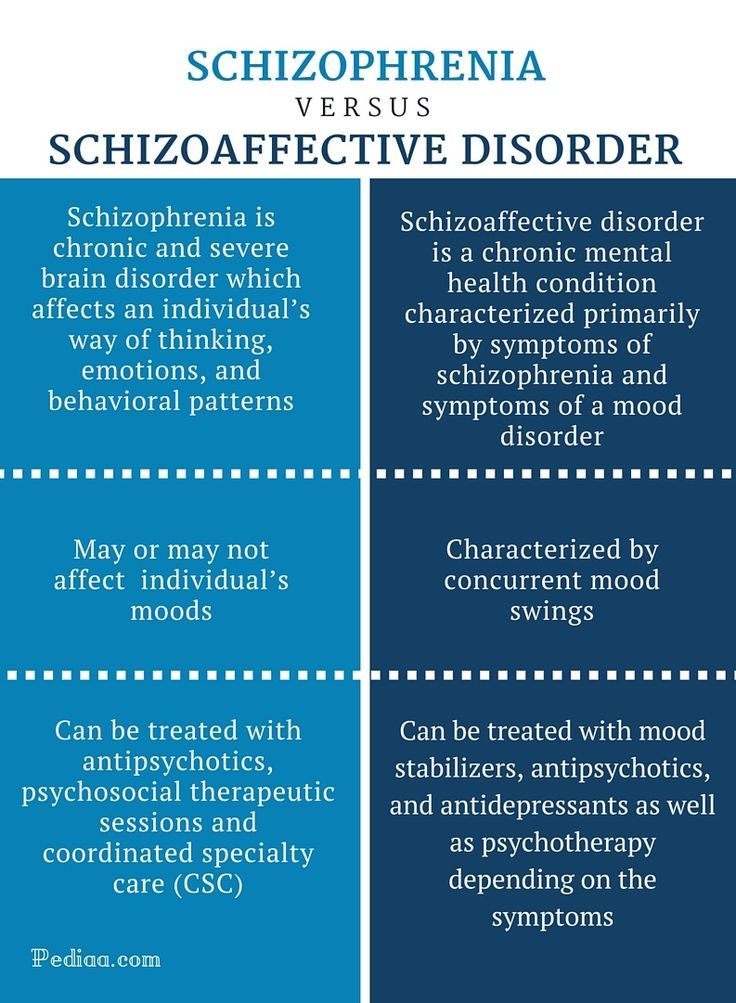
Schizophrenia may also affect daily cognition skills, possibly leading to difficulties with memory, attention, and concentration. People with schizophrenia may also have a harder time completing everyday tasks.
Concentration difficulties combined with struggles to put thoughts together can also lead to disorganized speech. Cognitive changes can make it difficult to make decisions, and can affect short-term memory.
Another potential cognitive issue seen in schizophrenia is a lack of insight (anosognosia), which can make a person unaware that they have this condition.
Like other types of mental health conditions, schizophrenia doesn’t cause many physical symptoms. But you might notice that your loved one appears more still, jumpy, or expressionless than usual.
Also, if your loved one is struggling with everyday tasks, they might appear more disheveled or unkempt than what’s considered normal for them.
It’s a misconception that people with schizophrenia are violent. In fact, research shows that individuals with this condition are more likely to be victims of violence. At the same time, the chances of violence or self-harm are greater if the condition isn’t treated.
In fact, research shows that individuals with this condition are more likely to be victims of violence. At the same time, the chances of violence or self-harm are greater if the condition isn’t treated.
Symptoms of schizophrenia tend to appear during your 20s or 30s, but they may occur as early as your teens or early adulthood — especially in males. Teenagers may exhibit earlier symptoms as a precursor to schizophrenia, like:
- struggles with school
- problems with motivation
- difficulty with relationships
- issues with making decisions/poor judgment
Keep in mind that such symptoms aren’t exclusive to schizophrenia, and these may be common adolescent behaviors. For teens with schizophrenia, the above issues become apparent over the course of a year or two. A person who has always had the struggles listed above may have other issues.
At the same time, it’s important to be aware that subtle changes in mood, social function, and thought processes may occur in schizophrenia before more obvious positive symptoms develop.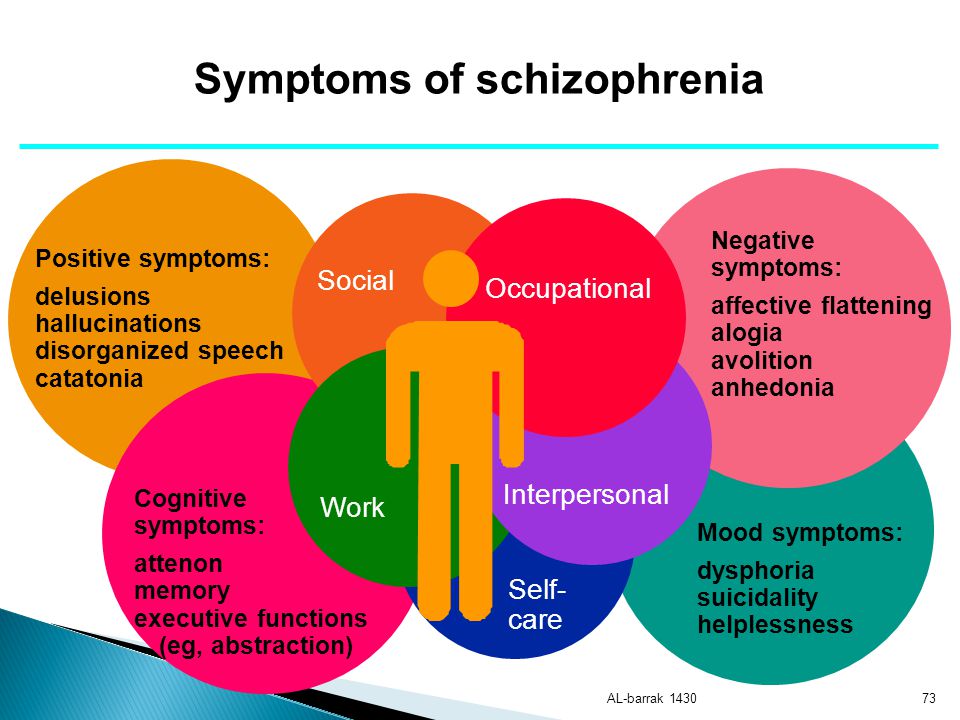
If you have concerns about your teen’s mental health, it’s important to talk with them and to reach out to their doctor or therapist.
Managing schizophrenia is a lifelong process that requires a combination of medications and therapies to help minimize the effects that some symptoms may have on your everyday life. Social skills and life-management skills classes can also help you develop more independence and confidence.
It’s also important to have a support system. This may include family or loved ones, friends, or people you might meet in group therapy. You can also talk with your doctor if you’re concerned about any new or worsening symptoms.
Finally, it’s important to take care of yourself. A balanced diet, regular exercise, and relaxation techniques can all promote well-being and decrease stress.
Schizophrenia has no cure, so long-term treatment is important to help improve quality of life and to prevent complications. Symptoms may be classified as positive or negative, though this mental health disorder can lead to cognitive effects that impact your daily life.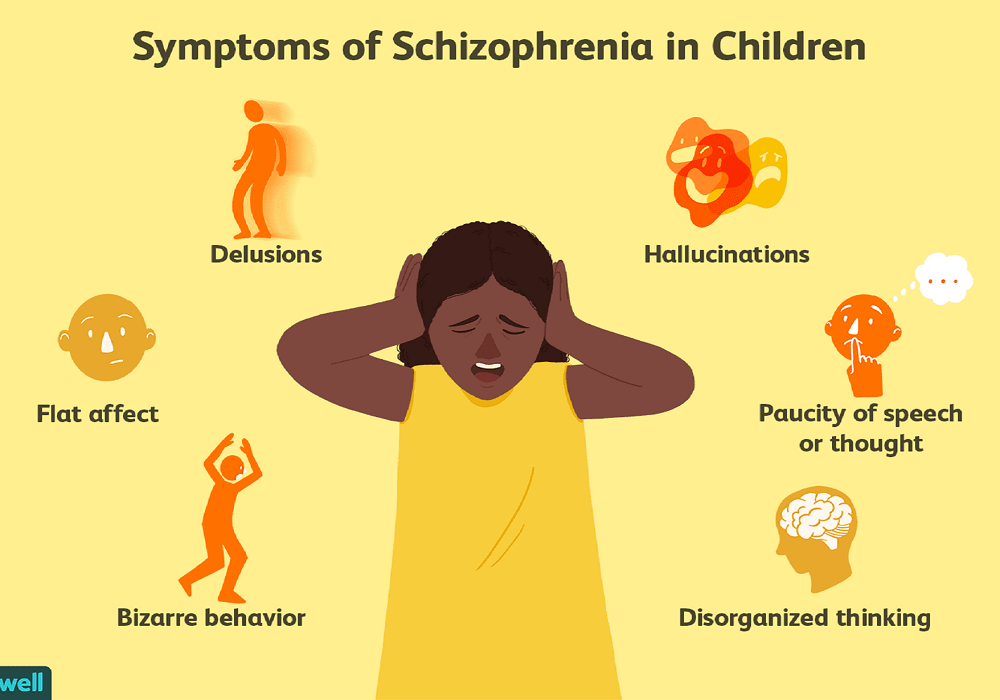
Regardless of what types of symptoms you’re currently experiencing, it’s helpful to keep track of them for yourself or a loved one so you can share them with your doctor.
Also, while it’s important to know the symptoms of schizophrenia, you should never diagnose yourself or others — only a mental health professional can provide an accurate diagnosis so you or your loved one can obtain appropriate treatment.
The structure of aggressiveness and compensatory behavioral tendencies in patients with paranoid schizophrenia
There is a fairly large amount of data in the literature indicating a significant proportion of schizophrenia among patients who have committed socially dangerous acts (SOD) [1-3], and the psychopathological mechanisms of SOD are described in this case disease [3].
Many researchers [3-9] distinguish the following signs of aggressiveness and aggressive behavior at various stages of the course of paranoid schizophrenia: suspicion, distrust, increased hostility to others, guilt, tension, weakening of self-control, impulsiveness in behavior with irritability, negativism, decreased contact of patients , ideas of persecution and self-blame.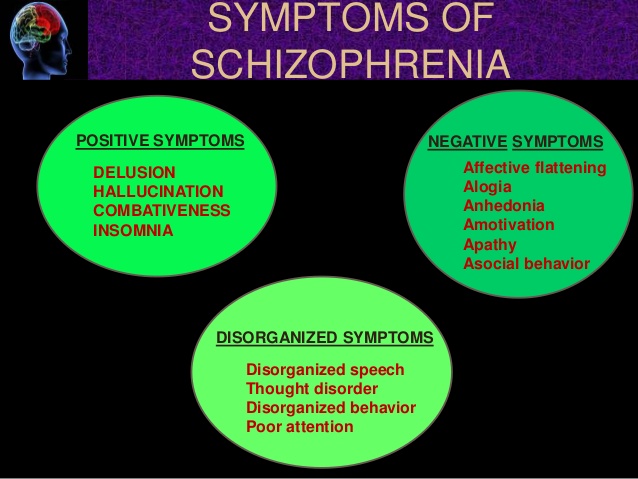 Aggressive behavior of patients with schizophrenia, along with other clinical signs, is considered [3] as a marker of exacerbation of the disease.
Aggressive behavior of patients with schizophrenia, along with other clinical signs, is considered [3] as a marker of exacerbation of the disease.
In our opinion, the study of the characteristics of aggression, aggressiveness and features of aggressive behavior can expand the understanding of the mechanisms of social maladaptation in patients with paranoid schizophrenia.
In world and Russian psychology and psychiatry today there is no unity in relation to the concepts of "aggression", "aggressiveness" and "aggressive behavior". Relevant research is carried out from the standpoint of a variety of approaches: within the frustration theory of aggression [10], social learning theory [11], from the standpoint of ethological [12], psychodynamic [13], activity [14] and clinical [15] approaches, which led to to significant contradictions both in relation to the results obtained and research methodology [14, 16, 17].
Aggressiveness is a systemic socio-psychological property that is formed in the process of socialization of the individual and acquires, depending on the biological, psychological and social factors, a constructive (socialized) or, in case of violation of socialization, a destructive character [18].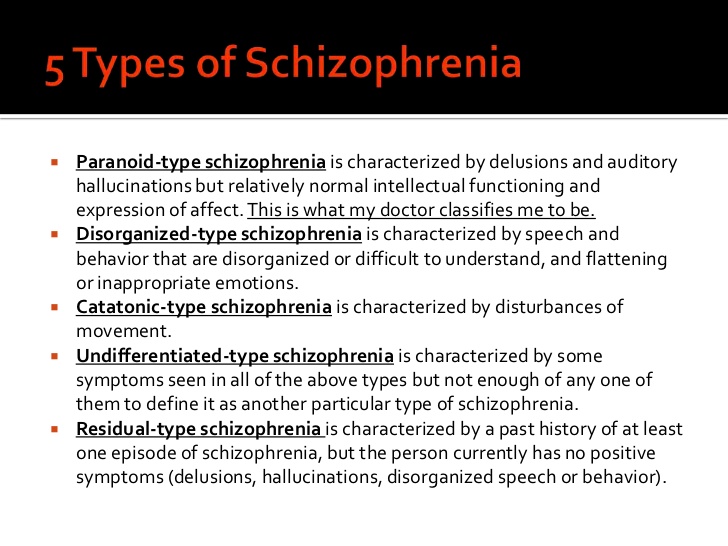 The internal structure of aggressiveness includes cognitive (a certain way of perceiving and interpreting the external situation), emotional (emotions of irritation, anger or anxiety and feelings of guilt) and volitional processes [18].
The internal structure of aggressiveness includes cognitive (a certain way of perceiving and interpreting the external situation), emotional (emotions of irritation, anger or anxiety and feelings of guilt) and volitional processes [18].
By aggression we mean mental activity aimed at discharging internal tension, the source of which can be both internal and external factors; Aggressive behavior is defined as behavior that violates the norms and rules for the coexistence of people in society, determined by socio-historical conditions.
The purpose of this study is to study the structure of aggressiveness and features of compensatory tendencies in patients with paranoid schizophrenia at the behavioral level.
Material and methods
The study was conducted at the Republican Clinical Psychiatric Hospital (Izhevsk).
Examined 203 people aged 18 to 64 years. The main group included 102 patients with paranoid schizophrenia in remission (medication).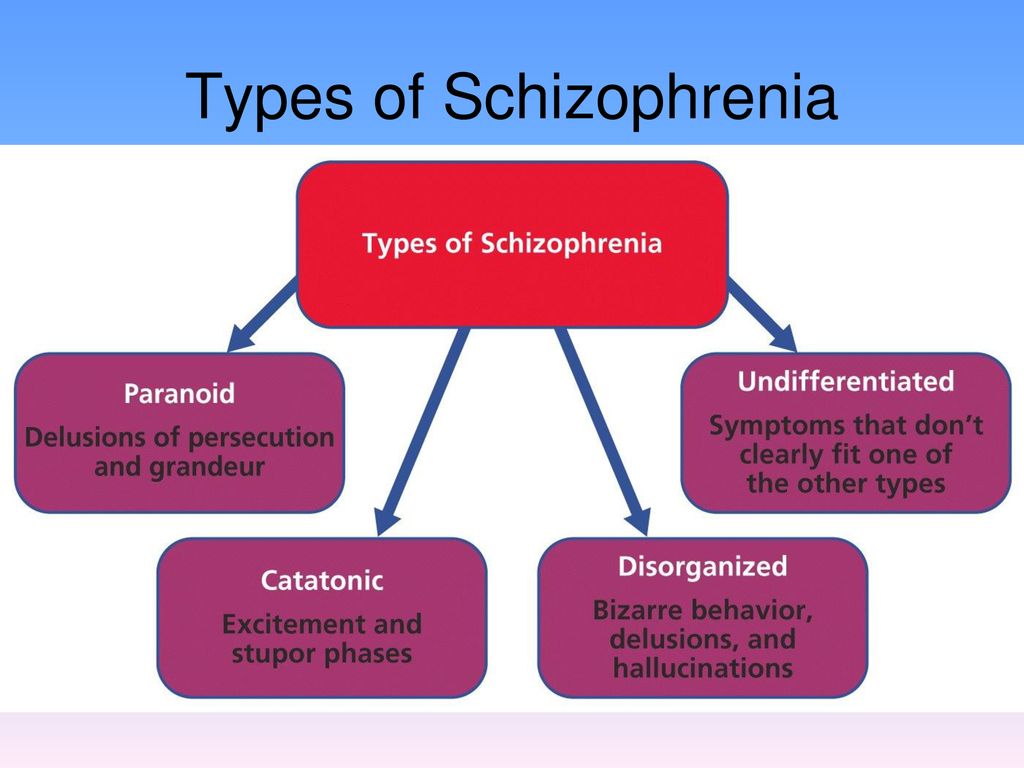 In the control group - 101 healthy. The examined in these groups were divided into subgroups according to gender and duration of the disease. The characteristics of these groups are presented in Table. 1
In the control group - 101 healthy. The examined in these groups were divided into subgroups according to gender and duration of the disease. The characteristics of these groups are presented in Table. 1
Table 1 Characteristics of study groups
To study the structure of aggressiveness, the standardized Bass-Perry questionnaire [19] was used, to assess the indicators of aggressive behavioral tendencies and propensity to aggressive behavior, a projective Hand test [20].
Statistical analysis of psychometric data was performed using non-parametric Mann-Whitney tests (for the analysis of differences in mean values), Spearman's correlation coefficient.
Results and discussion
The structure of aggressiveness of healthy people and patients with paranoid schizophrenia with different duration of the disease was studied. According to the data presented in table. 2, CGJ was characterized by a lack of connection between the behavioral and emotional components of aggression, which suggests a possible discrepancy between the woman's behavior and her experiences in a situation of increased subjective tension. In CGM, a high interdependence of the manifestations of all three components (behavioral, cognitive and emotional) was revealed, which ensured the adequacy of aggressive manifestations.
In CGM, a high interdependence of the manifestations of all three components (behavioral, cognitive and emotional) was revealed, which ensured the adequacy of aggressive manifestations.
Table 2. Correlations between the components of aggressiveness - behavioral, cognitive and emotional Note. * — p<0.05, ** — p<0.01.
In the main group (both women and men), there were no significant relationships between the components, which indicates a dissociated structure of aggressiveness. Significant links between behavioral and emotional components were found in AHJ2, which also confirms the dissociated nature of the aggressiveness structure. Emotional stress manifested itself directly in behavior and was not mediated by cognitive processing. In OGM2, the structure of aggressiveness was also dissociated, while the non-differentiation of the manifestation of aggression in thinking, behavior and emotions was determined.
The qualitative specificity of the aggressiveness structure was investigated.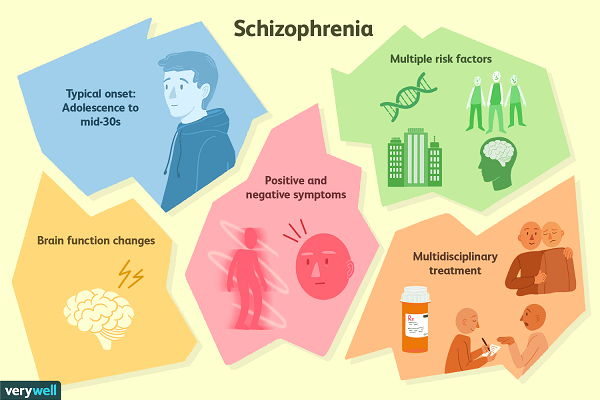 Homogeneity of cognitive, emotional and behavioral components was noted in CGJ, as indicated by the data given in Table. 3. In KGM, the behavioral component prevailed with the minimization of the emotional. Men and women of the control group were inclined to deny manifestations of aggression in their opinions, emotional experiences, behavior. Patients with paranoid schizophrenia with different duration of the disease (both women and men) were distinguished by hostility (high cognitive component of aggressiveness).
Homogeneity of cognitive, emotional and behavioral components was noted in CGJ, as indicated by the data given in Table. 3. In KGM, the behavioral component prevailed with the minimization of the emotional. Men and women of the control group were inclined to deny manifestations of aggression in their opinions, emotional experiences, behavior. Patients with paranoid schizophrenia with different duration of the disease (both women and men) were distinguished by hostility (high cognitive component of aggressiveness).
Table 3. Qualitative specificity of the aggressiveness structure of
Behavioral aggressive tendencies and tendency to aggressive behavior were studied. There were no significant differences in the level of behavioral aggressive tendencies in the groups of men and women. Given in table. 4 data allow us to talk about an increase in the propensity for open aggressive behavior in AGM2. An analysis of the correlation of the category suggests that the main reason for the increase in aggression is associated with a change in the indicators of social cooperation (for sick women, these are the categories "communication" and "dependence"). The absence of differences between the control and both experimental groups in the "affection" category, combined with a significant decrease in communicative indicators, indicates the inability of sick women to subject-business communication with a predominance of an emotional-evaluative context in relations with other people. Patients with AH1 are characterized by features of dependence.
Table 4. Aggressive behavioral tendencies and indicators of social cooperation
OGM1 was characterized by an increase in indicators in the "communication" category. The absence of differences between the control and both experimental groups of men in the category of "affection" in combination with an increase in communicative indicators indicates the predominance of formal communication with other people. In addition, men with paranoid schizophrenia are more likely to perceive neutral situations as personally significant.
Along with a decrease in the ability to communicate in schizophrenia, compensatory tendencies were identified at the behavioral level. In CGZH, with increased aggression, there was a refusal to act ( p <0.05), in OGZH1, passivity in relation to the physical environment ( p <0.05) and auto-aggressive reactions ( p <0.05) increased. In OGJ2, aggression decreased with an increase in the formality of activity ( p <0.05). In OGM2, with increased aggression, activity in relation to the physical environment decreased ( p <0.05).
Thus, in patients with paranoid schizophrenia, a dissociated structure of aggressiveness is determined, which is manifested by a mismatch of cognitive, emotional and behavioral components. There is a qualitative specificity in the structure of aggressiveness in sick men and women with paranoid schizophrenia in the form of a predominance of the cognitive component. Compensatory tendencies at the behavioral level were revealed.
No conflict of interest.
Treatment of schizophrenia - its signs and symptoms, causes
Schizophrenia is a severe polymorphic mental disorder accompanied by a bifurcation of intellectual and emotional-volitional functions. People can no longer adequately perceive reality and have pathological behavioral characteristics that do not allow them to live a normal life.
People can no longer adequately perceive reality and have pathological behavioral characteristics that do not allow them to live a normal life.
The mechanism of the development of the disease is not associated with environmental factors, but is due to an internal dysfunction of the body. In the vast majority of cases, self-treatment is ineffective, therefore, if symptoms are detected, it is necessary to immediately contact doctors who will conduct a comprehensive diagnosis of the body, determine the presence and level of the problem, and prescribe adequate treatment.
Schizophrenia: symptoms and signs
Most often, the disease in women manifests itself in the form of seizures, which are accompanied by a symptom complex: paranoia, delusions, hallucinations, frequent reflections, as well as the formation of conflict situations with other people against the background of social interests.
It develops at the age of 27 to 37 years, during the critical days, the symptoms can quickly worsen - this is due to the rapid change in hormonal levels.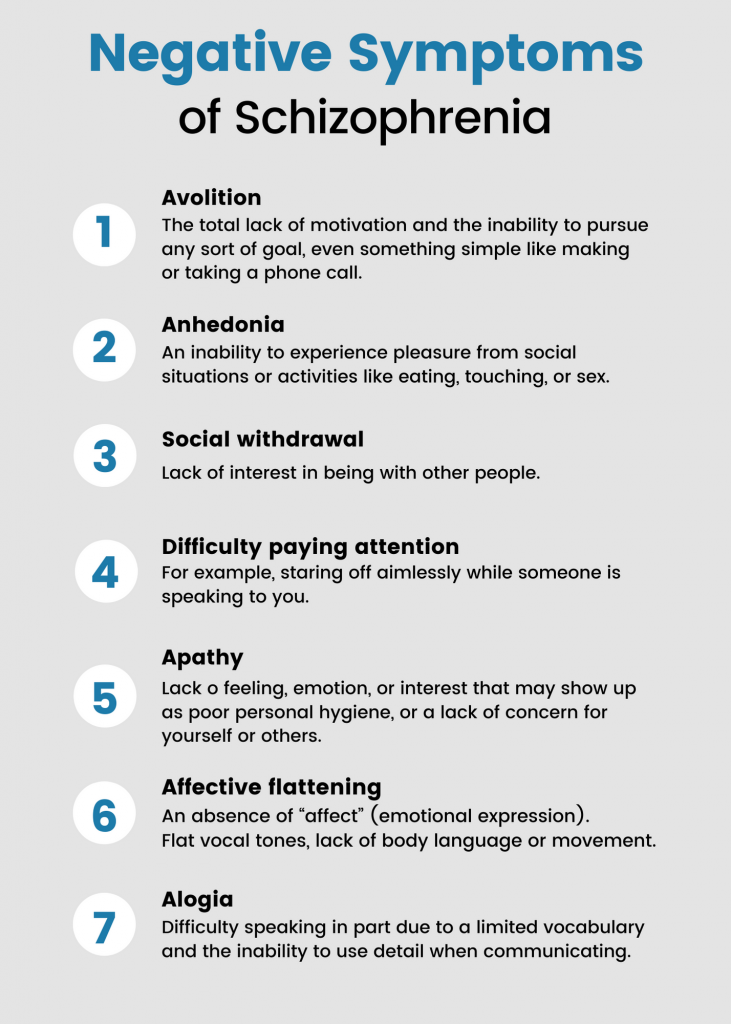 With a single manifestation of an attack, doctors do not always diagnose a persistent disease.
With a single manifestation of an attack, doctors do not always diagnose a persistent disease.
Motivation for treatment
24/7 emergency care
Top specialists
Quality assurance
Symptoms and signs of schizophrenia in men 35 years. An interesting fact is that in bachelor men the problem occurs 4 times more often than in married men.
In most cases, it has a constant course and is accompanied by a characteristic symptom complex: self-isolation from society and close people, aggression without objective reasons, the appearance of extraneous voices in the head and persecution mania.
Causes of schizophrenia
The exact cause of the development of pathology has not been established today, however, there is a clear relationship at the genetic level, when people whose ancestors have already encountered this problem are exposed to the disease, as well as some other mental illnesses, including: suicidal tendencies, depression , psychoses.
In scientific circles, the theory of the development of schizophrenia in women who have given birth to a child is quite widespread - there is no evidence for it, but we can talk about the presence of a stressful situation that can serve as a catalyst for the manifestation of the disease. Among other reasons, experts note: social factors, drug addiction and alcoholism.
Free consultation
+38 (067) 126 04 04
Forms and stages of schizophrenia
The disease has several main forms and stages. In accordance with the nature of the manifestation, as well as the intensity of symptomatic manifestations, there are four main forms:
- Catatonic - accompanied by a stupor in actions and thinking. Perhaps the appearance of short-term stages of excitation;
- Paranoid - severe form, accompanied by obsessions, hallucinations and delusions;
- Residual - characterized by a chronic course, accompanied by a blunted emotional state;
- Hebephrenic - often observed in young people, is considered the most difficult type, accompanied by a loss of the ability to adapt in the social environment.
It has three main stages of flow: mastery (the familiar world is distorted by hallucinations, its perception changes), adaptation (there is getting used to the new realities of the disease - the state becomes ordinary), degradation (emotional devastation occurs, time and space lose their significance for the patient) .
Methods and treatment of schizophrenia at the Profi-Detox Clinic
Profi-Detox Psychiatric Clinic provides services for the treatment of patients suffering from schizophrenia at all stages of development. The clinic employs experienced highly qualified specialists, providing an individual approach to each patient.
For the treatment of patients, an integrated approach is used, including two main methods: biological (involves the use of medical procedures and medications) and psychosocial (involves the psychological work of specialized doctors). The choice of the optimal scheme is made only by the doctor, based on the data of the initial examination and the results of the tests.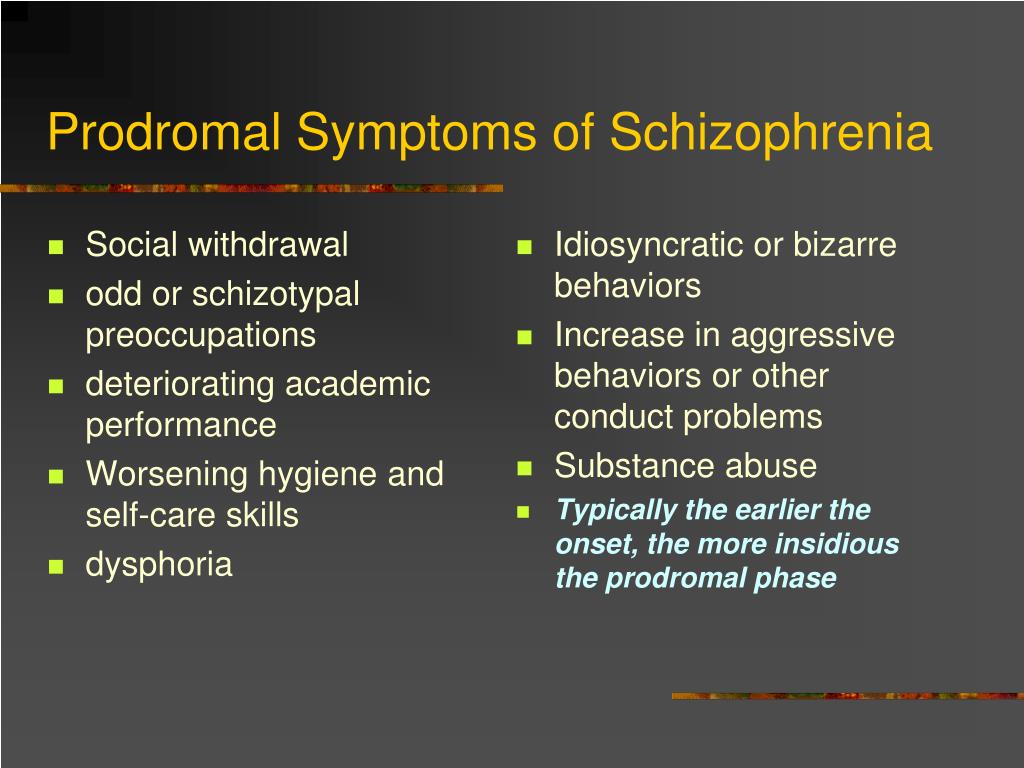
Patient transfer
We arrive at the address within 45 - 60 minutes.
Free consultation
Call and ask any question.
Guaranteed anonymity
No one will know that you are on treatment.
Treatment of schizophrenia in men
Schizophrenia in men is treated in an integrated approach that involves the use of medications and a range of therapies. The stage is lengthy and may take several years.
Treatments are prescribed taking into account the nature of the course of the disease in men, and therefore may differ significantly from the treatment of female schizophrenia. For men, the support of loved ones and those around them is very important.
Treatment of schizophrenia in women
Women are treated based on two main methods: biological and social therapy. Biological therapy may include shock and drug treatments. Particular attention is paid to the relief of exacerbations, leading to a general deterioration of the situation.