Psychotherapy anxiety disorder
Therapy for Anxiety Disorders - HelpGuide.org
Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dialogues in Clinical Neuroscience, 13(4), 413–421. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3263389/
Tolin, D. F. (2010). Is cognitive–behavioral therapy more effective than other therapies?: A meta-analytic review. Clinical Psychology Review, 30(6), 710–720. https://doi.org/10.1016/j.cpr.2010.05.003
Borza, L. (2017). Cognitive-behavioral therapy for generalized anxiety. Dialogues in Clinical Neuroscience, 19(2), 203–208. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5573564/
Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. – PsycNET. (n.d.). APA PsycNET. https://doi.org/10.1037/0022-006X.61.4.611
Heimberg, R. G. (2002). Cognitive-behavioral therapy for social anxiety disorder: Current status and future directions. Biological Psychiatry, 51(1), 101–108. https://doi.org/10.1016/S0006-3223(01)01183-0
Powers, M. B., Sigmarsson, S. R., & Emmelkamp, P. M. G. (2009, August 4). A Meta–Analytic Review of Psychological Treatments for Social Anxiety Disorder (world) [Research-article]. Http://Dx.Doi.Org/10.1521/Ijct.2008.1.2.94; Guilford Publications. https://doi.org/10.1521/ijct.2008.1.2.94
Schneider, S., Blatter-Meunier, J., Herren, C., Adornetto, C., In-Albon, T., & Lavallee, K. (2011). Disorder-Specific Cognitive-Behavioral Therapy for Separation Anxiety Disorder in Young Children: A Randomized Waiting-List-Controlled Trial. Psychotherapy and Psychosomatics, 80(4), 206–215. https://doi.org/10.1159/000323444
Reinecke, A., Thilo, K. V., Croft, A., & Harmer, C. J. (2018). Early effects of exposure-based cognitive behaviour therapy on the neural correlates of anxiety. Translational Psychiatry, 8(1), 1–9. https://doi.org/10.1038/s41398-018-0277-5
Ougrin, D. (2011). Efficacy of exposure versus cognitive therapy in anxiety disorders: Systematic review and meta-analysis. BMC Psychiatry, 11(1), 200. https://doi.org/10.1186/1471-244X-11-200
BMC Psychiatry, 11(1), 200. https://doi.org/10.1186/1471-244X-11-200
Roberge, P., Marchand, A., Reinharz, D., & Savard, P. (2008). Cognitive-Behavioral Treatment for Panic Disorder With Agoraphobia: A Randomized, Controlled Trial and Cost-Effectiveness Analysis. Behavior Modification, 32(3), 333–351. https://doi.org/10.1177/0145445507309025
Amick, H. R., Gartlehner, G., Gaynes, B. N., Forneris, C., Asher, G. N., Morgan, L. C., Coker-Schwimmer, E., Boland, E., Lux, L. J., Gaylord, S., Bann, C., Pierl, C. B., & Lohr, K. N. (2015). Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: Systematic review and meta-analysis. BMJ, 351, h6019. https://doi.org/10.1136/bmj.h6019
Hilty, D. M., Ferrer, D. C., Parish, M. B., Johnston, B., Callahan, E. J., & Yellowlees, P. M. (2013). The Effectiveness of Telemental Health: A 2013 Review. Telemedicine Journal and E-Health, 19(6), 444–454. https://doi.org/10.1089/tmj.2013.0075
https://doi.org/10.1089/tmj.2013.0075
Koonin, L. M. (2020). Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic—United States, January–March 2020. MMWR. Morbidity and Mortality Weekly Report, 69. https://doi.org/10.15585/mmwr.mm6943a3
Nordgren, L. B., Hedman, E., Etienne, J., Bodin, J., Kadowaki, Å., Eriksson, S., Lindkvist, E., Andersson, G., & Carlbring, P. (2014). Effectiveness and cost-effectiveness of individually tailored Internet-delivered cognitive behavior therapy for anxiety disorders in a primary care population: A randomized controlled trial. Behaviour Research and Therapy, 59, 1–11. https://doi.org/10.1016/j.brat.2014.05.007
Recognition of Psychotherapy Effectiveness. (n.d.). American Psychological Association (APA). Retrieved June 23, 2021, from https://www.apa.org/about/policy/resolution-psychotherapy
Geller, D. A., & March, J. (2012). Practice Parameter for the Assessment and Treatment of Children and Adolescents With Obsessive-Compulsive Disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98–113. https://doi.org/10.1016/j.jaac.2011.09.019
Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98–113. https://doi.org/10.1016/j.jaac.2011.09.019
Fineberg, N. A., Hollander, E., Pallanti, S., Walitza, S., Grünblatt, E., Dell’Osso, B. M., Albert, U., Geller, D. A., Brakoulias, V., Janardhan Reddy, Y. C., Arumugham, S. S., Shavitt, R. G., Drummond, L., Grancini, B., De Carlo, V., Cinosi, E., Chamberlain, S. R., Ioannidis, K., Rodriguez, C. I., … Menchon, J. M. (2020). Clinical advances in obsessive-compulsive disorder: A position statement by the International College of Obsessive-Compulsive Spectrum Disorders. International Clinical Psychopharmacology, 35(4), 173–193. https://doi.org/10.1097/YIC.0000000000000314
Hadley, S. J., Greenberg, J., & Hollander, E. (2002). Diagnosis and treatment of body dysmorphic disorder in adolescents. Current Psychiatry Reports, 4(2), 108–113. https://doi.org/10.1007/s11920-002-0043-4
Locke, A. B., Kirst, N., & Shultz, C. G. (2015). Diagnosis and Management of Generalized Anxiety Disorder and Panic Disorder in Adults. American Family Physician, 91(9), 617–624. https://www.aafp.org/afp/2015/0501/p617.html
American Family Physician, 91(9), 617–624. https://www.aafp.org/afp/2015/0501/p617.html
Walter, H. J., Bukstein, O. G., Abright, A. R., Keable, H., Ramtekkar, U., Ripperger-Suhler, J., & Rockhill, C. (2020). Clinical Practice Guideline for the Assessment and Treatment of Children and Adolescents With Anxiety Disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 59(10), 1107–1124. https://doi.org/10.1016/j.jaac.2020.05.005
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. https://doi.org/10.1037/0022-006X.61.4.611
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. https://doi. org/10.1016/j.cpr.2017.10.011
org/10.1016/j.cpr.2017.10.011
Shapero, B. G., Greenberg, J., Pedrelli, P., de Jong, M., & Desbordes, G. (2018). Mindfulness-Based Interventions in Psychiatry. Focus: Journal of Life Long Learning in Psychiatry, 16(1), 32–39. https://doi.org/10.1176/appi.focus.20170039
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M.-A., Paquin, K., & Hofmann, S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771. https://doi.org/10.1016/j.cpr.2013.05.005
Miller, J. J., Fletcher, K., & Kabat-Zinn, J. (1995). Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. General Hospital Psychiatry, 17(3), 192–200. https://doi.org/10.1016/0163-8343(95)00025-M
Schanche, E., Vøllestad, J., Binder, P.-E., Hjeltnes, A., Dundas, I., & Nielsen, G. H. (2020). Participant experiences of change in mindfulness-based stress reduction for anxiety disorders. International Journal of Qualitative Studies on Health and Well-Being, 15(1), 1776094. https://doi.org/10.1080/17482631.2020.1776094
International Journal of Qualitative Studies on Health and Well-Being, 15(1), 1776094. https://doi.org/10.1080/17482631.2020.1776094
Schoenberg, P. L. A., & David, A. S. (2014). Biofeedback for Psychiatric Disorders: A Systematic Review. Applied Psychophysiology and Biofeedback, 39(2), 109–135. https://doi.org/10.1007/s10484-014-9246-9
Goessl, V. C., Curtiss, J. E., & Hofmann, S. G. (2017). The effect of heart rate variability biofeedback training on stress and anxiety: A meta-analysis. Psychological Medicine, 47(15), 2578–2586. https://doi.org/10.1017/S0033291717001003
Hammond, D. C. (2010). Hypnosis in the treatment of anxiety- and stress-related disorders. Expert Review of Neurotherapeutics, 10(2), 263–273. https://doi.org/10.1586/ern.09.140
Anbar, R. D. (2006). Hypnosis: An important multifaceted therapy. The Journal of Pediatrics, 149(4), 438–439. https://doi.org/10.1016/j.jpeds.2006.07.019
Mayo-Wilson, E., Dias, S., Mavranezouli, I., Kew, K., Clark, D. M., Ades, A. E., & Pilling, S. (2014). Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 1(5), 368–376. https://doi.org/10.1016/S2215-0366(14)70329-3
M., Ades, A. E., & Pilling, S. (2014). Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 1(5), 368–376. https://doi.org/10.1016/S2215-0366(14)70329-3
Craske, M. G., & Stein, M. B. (2016). Anxiety. Lancet (London, England), 388(10063), 3048–3059. https://doi.org/10.1016/S0140-6736(16)30381-6
Recognition of Psychotherapy Effectiveness. (n.d.). American Psychological Association (APA). Retrieved June 23, 2021, from https://www.apa.org/about/policy/resolution-psychotherapy
Aylett, E., Small, N., & Bower, P. (2018). Exercise in the treatment of clinical anxiety in general practice – a systematic review and meta-analysis. BMC Health Services Research, 18(1), 559. https://doi.org/10.1186/s12913-018-3313-5
Kandola, A., Vancampfort, D., Herring, M., Rebar, A., Hallgren, M., Firth, J., & Stubbs, B. (2018). Moving to Beat Anxiety: Epidemiology and Therapeutic Issues with Physical Activity for Anxiety. Current Psychiatry Reports, 20(8), 63. https://doi.org/10.1007/s11920-018-0923-x
Current Psychiatry Reports, 20(8), 63. https://doi.org/10.1007/s11920-018-0923-x
Anxiety Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x05_Anxiety_Disorders
Anxiety disorders - Diagnosis and treatment
Diagnosis
You may start by seeing your primary care provider to find out if your anxiety could be related to your physical health. He or she can check for signs of an underlying medical condition that may need treatment.
However, you may need to see a mental health specialist if you have severe anxiety. A psychiatrist is a medical doctor who specializes in diagnosing and treating mental health conditions. A psychologist and certain other mental health professionals can diagnose anxiety and provide counseling (psychotherapy).
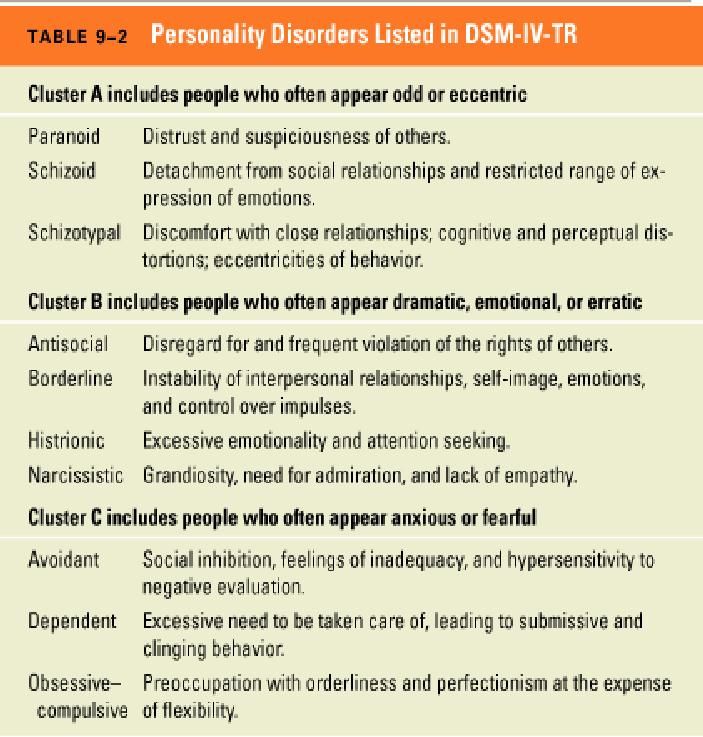
To help diagnose an anxiety disorder, your mental health provider may:
- Give you a psychological evaluation.
 This involves discussing your thoughts, feelings and behavior to help pinpoint a diagnosis and check for related complications. Anxiety disorders often occur along with other mental health problems — such as depression or substance misuse — which can make diagnosis more challenging.
This involves discussing your thoughts, feelings and behavior to help pinpoint a diagnosis and check for related complications. Anxiety disorders often occur along with other mental health problems — such as depression or substance misuse — which can make diagnosis more challenging. - Compare your symptoms to the criteria in the DSM-5. Many doctors use the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association, to diagnose an anxiety disorder.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your anxiety disorders-related health concerns Start Here
Treatment
The two main treatments for anxiety disorders are psychotherapy and medications. You may benefit most from a combination of the two. It may take some trial and error to discover which treatments work best for you.
Psychotherapy
Also known as talk therapy or psychological counseling, psychotherapy involves working with a therapist to reduce your anxiety symptoms. It can be an effective treatment for anxiety.
Cognitive behavioral therapy (CBT) is the most effective form of psychotherapy for anxiety disorders. Generally a short-term treatment, CBT focuses on teaching you specific skills to improve your symptoms and gradually return to the activities you've avoided because of anxiety.
CBT includes exposure therapy, in which you gradually encounter the object or situation that triggers your anxiety so you build confidence that you can manage the situation and anxiety symptoms.
Medications
Several types of medications are used to help relieve symptoms, depending on the type of anxiety disorder you have and whether you also have other mental or physical health issues. For example:
- Certain antidepressants are also used to treat anxiety disorders.
- An anti-anxiety medication called buspirone may be prescribed.

- In limited circumstances, your doctor may prescribe other types of medications, such as sedatives, also called benzodiazepines, or beta blockers. These medications are for short-term relief of anxiety symptoms and are not intended to be used long term.
Talk with your doctor about benefits, risks and possible side effects of medications.
More Information
- Anxiety disorders care at Mayo Clinic
- Psychotherapy
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
While most people with anxiety disorders need psychotherapy or medications to get anxiety under control, lifestyle changes also can make a difference. Here's what you can do:
Here's what you can do:
- Keep physically active. Develop a routine so that you're physically active most days of the week. Exercise is a powerful stress reducer. It may improve your mood and help you stay healthy. Start out slowly and gradually increase the amount and intensity of your activities.
- Avoid alcohol and recreational drugs. These substances can cause or worsen anxiety. If you can't quit on your own, see your doctor or find a support group to help you.
- Quit smoking and cut back or quit drinking caffeinated beverages. Both nicotine and caffeine can worsen anxiety.
- Use stress management and relaxation techniques. Visualization techniques, meditation and yoga are examples of relaxation techniques that can ease anxiety.
- Make sleep a priority. Do what you can to make sure you're getting enough sleep to feel rested. If you aren't sleeping well, see your doctor.

- Eat healthy. Healthy eating — such as focusing on vegetables, fruits, whole grains and fish — may be linked to reduced anxiety, but more research is needed.
Alternative medicine
Several herbal remedies have been studied as a treatment for anxiety, but more research is needed to understand the risks and benefits. Herbal and dietary supplements aren't monitored by the Food and Drug Administration (FDA) the same way medications are. You can't always be certain of what you're getting and whether it's safe. Some of these supplements can interfere with prescription medications or cause dangerous interactions.
Before taking herbal remedies or dietary supplements, talk to your doctor to make sure they're safe for you and won't interact with any medications you take.
Coping and support
To cope with an anxiety disorder, here's what you can do:
- Learn about your disorder. Talk to your doctor or mental health provider.
Find out what might be causing your specific condition and what treatments might be best for you. Involve your family and friends and ask for their support.
- Stick to your treatment plan. Take medications as directed. Keep therapy appointments and complete any assignments your therapist may give you. Consistency can make a big difference, especially when it comes to taking your medication.
- Take action. Learn what triggers your anxiety or causes you stress. Practice the strategies you developed with your mental health provider so you're ready to deal with anxious feelings in these situations.
- Keep a journal. Keeping track of your personal life can help you and your mental health provider identify what's causing you stress and what seems to help you feel better.
- Join an anxiety support group. Remember that you aren't alone. Support groups offer compassion, understanding and shared experiences.
 The National Alliance on Mental Illness and the Anxiety and Depression Association of America provide information on finding support.
The National Alliance on Mental Illness and the Anxiety and Depression Association of America provide information on finding support. - Learn time management techniques. You can reduce anxiety by learning how to carefully manage your time and energy.
- Socialize. Don't let worries isolate you from loved ones or activities.
- Break the cycle. When you feel anxious, take a brisk walk or delve into a hobby to refocus your mind away from your worries.
Preparing for your appointment
You may start by seeing your primary care provider. He or she may refer you to a mental health professional.
What you can do
Before your appointment, make a list of:
- Your anxiety symptoms. Note when they occur, whether anything seems to make them better or worse, and how much they affect your day-to-day activities and interactions.
- What causes you stress.
 Include any major life changes or stressful events you've dealt with recently. Also note any traumatic experiences you've had in the past or as a child.
Include any major life changes or stressful events you've dealt with recently. Also note any traumatic experiences you've had in the past or as a child. - Any family history of mental health problems. Note if your parents, grandparents, siblings or children have struggled with any mental health problems.
- Any other health problems you have. Include both physical conditions and mental health issues.
- All medications you're taking. Include any medications, vitamins, herbs or other supplements, and the doses.
- Questions to ask your doctor to make the most of your appointment.
Some basic questions to ask your doctor include:
- What's the most likely cause of my anxiety?
- Are there other possible situations, psychological issues or physical health problems that could be causing or worsening my anxiety?
- Do I need any tests?
- Should I see a psychiatrist, psychologist or other mental health provider?
- What type of therapy might help me?
- Would medication help? If so, is there a generic alternative to the medicine you're prescribing?
- In addition to treatment, are there any steps I can take at home that might help?
- Do you have any educational materials that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you several questions, such as:
- What are your symptoms, and how severe are they? How do they impact your ability to function?
- Have you ever had a panic attack?
- Do you avoid certain things or situations because they make you anxious?
- Have your feelings of anxiety been occasional or continuous?
- When did you first begin noticing your feelings of anxiety?
- Does anything in particular seem to trigger your anxiety or make it worse?
- What, if anything, seems to improve your feelings of anxiety?
- What traumatic experiences have you had recently or in the past?
- What, if any, physical or mental health conditions do you have?
- Do you take any prescription drugs?
- Do you regularly drink alcohol or use recreational drugs?
- Do you have any blood relatives who have anxiety or other mental health conditions, such as depression?
Preparing and anticipating questions will help you make the most of your time.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Treatment of Anxiety and Panic Disorders at the EMC Clinic of Psychiatry and Psychotherapy in Moscow
Anxiety disorders is a group of disorders in which irrational uncontrollable fear and a persistent feeling of anxiety become the predominant symptoms, which can occur in situations that do not really pose a current danger .
Anxiety is a normal adaptive response of the body to changing conditions or threatening events. However, fears can be a serious problem for a person if the level of anxiety reaches pathological proportions. This imposes restrictions on the normal functioning of the patient, which significantly reduces his quality of life. Also, the long-term existence of an anxiety disorder dramatically increases the risk of other mental disorders, such as depressive disorder (by about 15 times) and pathological addictions (by about 20 times).
Major anxiety disorders include the following disorders:
Panic disorder - the main symptoms of the disease include recurring attacks of irrational anxiety (panic), not limited to a specific situation or any specific circumstances.
Dominant symptoms : sudden onset tachycardia (rapid heartbeat), sweating, tremors, dry mouth, chest pain, difficulty breathing, feeling of suffocation and nausea, as well as dizziness and a feeling of unreality of what is happening.
Agoraphobia is a group of anxiety disorders that includes a number of phobias, which include a painful fear of open spaces and public places. Patients experience uncontrollable anxiety when they are in a crowd, refuse to visit shops and other crowded places, limit their exits from the house unaccompanied, and have difficulty using public transport on their own. Agoraphobia is one of the most maladaptive types of phobic disorders.
Dominant symptoms : when immersed in a frightening situation, patients experience a sharp increase in anxiety, increased heart rate and breathing, sweating and dizziness appear, in some cases a panic attack develops. As a rule, such patients try in every possible way to avoid those situations that cause them a panic attack, which contributes to the consolidation of an anxiety disorder, changes their usual lifestyle and interferes with normal life.
As a rule, such patients try in every possible way to avoid those situations that cause them a panic attack, which contributes to the consolidation of an anxiety disorder, changes their usual lifestyle and interferes with normal life.
Generalized anxiety disorder - manifested by a constant feeling of anxiety, tension and persistent anxiety about a variety of life events, the likelihood of which is extremely small. In this case, anxiety is not limited to any specific external circumstances, so it is often difficult for the patient to outline the circle of situations that trigger panic.
Dominant symptoms : the most typical complaints are a feeling of constant nervousness, trembling, muscle tension, sweating, tachycardia, dizziness, discomfort in the epigastric region. Often the patient experiences fear for his loved ones, suffers from gloomy forebodings. For a diagnosis of generalized anxiety disorder, the symptoms described must have been present for at least 6 months.
Social phobia - this anxiety disorder is based on the fear of being seen by others, as well as being in an awkward position, being ridiculed or humiliated, which leads to the formation of a reaction to avoid such situations. Often this disorder is combined with low self-esteem and fear of criticism. Fears can manifest themselves when eating in a public place, the need to maintain a conversation during a casual meeting with friends in the presence of strangers, visiting public places and group activities.
Dominant symptoms : hand tremor, nausea (fear of vomiting may be present), urge to urinate or defecate (or fear of such an urge), flushing of the face. Sometimes the patient takes one of these side manifestations of anxiety for the underlying disease. Avoidance of frightening situations causes significant psycho-emotional stress, since the person himself realizes that his reaction is excessive and has no reasonable grounds.
Specific phobias are fears limited to narrowly specific situations, such as, for example, being in close proximity to animals of a certain biological species, being in the dark, at height, in a confined space. Specific phobias also include fear of air travel, fears of eating certain foods, visiting a doctor, medical procedures, and the sight of blood. When confronted with fearful stimuli or when thoughts about them arise, the person "triggers" anxiety and the symptoms described above are observed.
Specific phobias also include fear of air travel, fears of eating certain foods, visiting a doctor, medical procedures, and the sight of blood. When confronted with fearful stimuli or when thoughts about them arise, the person "triggers" anxiety and the symptoms described above are observed.
Benefits of treatment at EMC
- Thorough diagnosis of the patient's mental state, identification of risk factors.
- Designing an individual treatment program, including pharmacotherapy, cognitive behavioral therapy, if necessary, TMS.
- The Clinic for Psychiatry and Psychotherapy constantly organizes trainings that teach relaxation skills and coping with anxiety symptoms.
Principles and algorithms for psychotherapy of neurotic anxiety disorders (anxiety-phobic, panic and generalized anxiety disorders) | Karavaeva
1. Zalutskaya N.M. Generalized anxiety disorder: current theoretical models and approaches to diagnosis and therapy. Part 2. / Review of psychiatry and medical psychology. - 2014. - No. 4. - P. 129-134
Part 2. / Review of psychiatry and medical psychology. - 2014. - No. 4. - P. 129-134
2. Karvasarsky B.D. Psychotherapy: a textbook for universities. - Publishing house Peter - 2012 - 672 p.
3. Karavaeva T.A. The main trends in the change of psychotherapeutic and rehabilitation strategies in the treatment of neurotic disorders / Review of Psychiatry and Medical Psychology. V.M. Bekhterev. - 2010. - No. 3. - S. 71-74.
4. Karavaeva T.A., Kolotilshchikova E.A. Mizinova E.B. Changing psychotherapeutic and rehabilitation strategies in the treatment of neurotic disorders in the context of socio-economic changes. Part II. Changes in psychological characteristics in patients with neurotic disorders in the last three decades / Review of Psychiatry and Medical Psychology. V.M. Bekhterev. - 2010. - No. 3. - S. 63-65.
5. Kolotilshchikova, E.A., Mizinova E.B., Chekhlatii E.I. Coping behavior in patients with neurosis and its dynamics in the process of short-term interpersonal group psychotherapy // Bulletin of psychotherapy.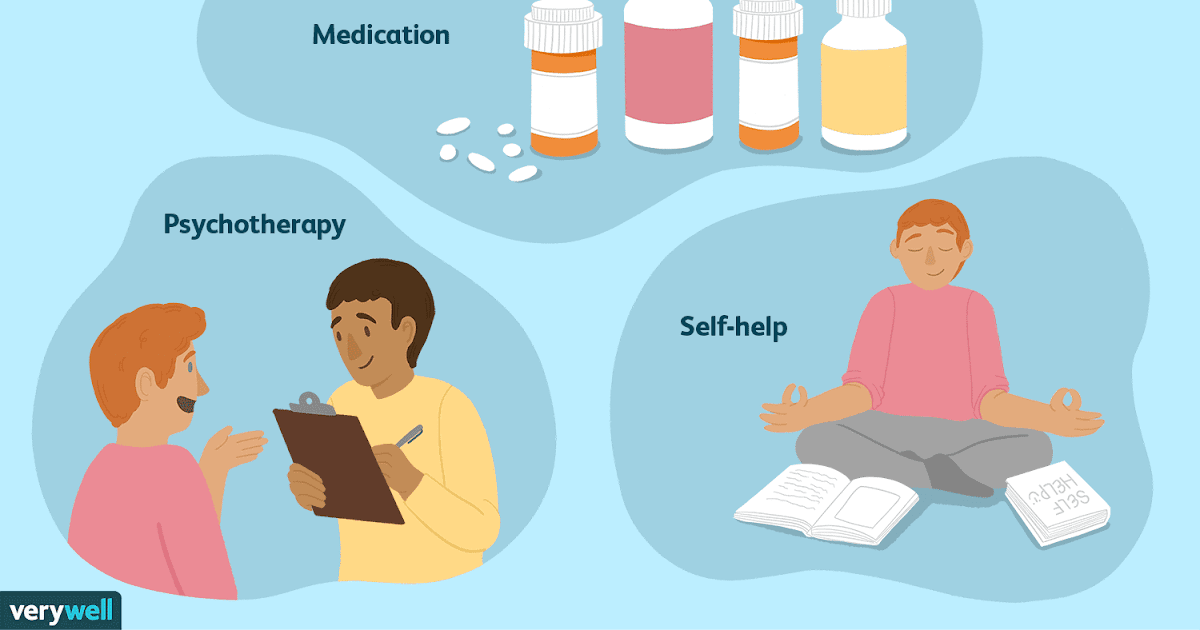 - 2004. - No. 12 (17). - p. 9-23.
- 2004. - No. 12 (17). - p. 9-23.
6. Kotsyubinsky A.P., Sheinina N.S., Butoma B.G., Erichev A.N., Melnikova Yu.V., Savrasov R.G. Holistic diagnostic approach in psychiatry. Message 1. // Social and clinical psychiatry. - 2013 - T. 23. - No. 4 - S.45-50.
7. Poltorak S.V., Karavaeva T.A., Vasilyeva A.V. Changes in the ratio of psychotherapy and pharmacotherapy for neurotic disorders in the second half of the 20th and early 21st centuries. // Bulletin of psychotherapy. - 2013. - No. 47(52). - P.29-37.
8. Pribytkov A.A., Erichev A.N., Kotsyubinsky A.P., Yurkova I.O. Questions of therapy of somatoform disorders: drug and psychotherapeutic approaches // Social and Clinical Psychiatry. - 2014. - T. 24. - No. 4 - S. 73-80.
9. Beck A. T. [et al.]. Cognitive Therapy of Depression. - N.Y.: Guilford Press. - 1980. - 425 p.
10. Behar, E., Borkovec, T.D. The nature and treatment of generalized anxiety disorder. In: B.O. Rothbaum (Ed.), The nature and treatment of pathological anxiety: essays in honor of Edna B. Foa. - New York: Guilford. - 2005. - R.181-196.
Foa. - New York: Guilford. - 2005. - R.181-196.
11. Chambless D. L. Spacing of exposure sessions in treatment of phobia. Paper presented at the 22nd Annaul Session for Advancement of Behavior Therapy. -N.Y.-1989.
12. Daniels CY. panic disorder. 2010. http://emedicine. medscape.com/article/287913-overview
13. Diefenbach, G. J., Stanley, M. A. Beck, J. G. Worry content reported by older adults with and without generalized anxiety disorder. - Aging and Mental Health. - 2001. - Vol.5. - P. 269-274.
14. Ellis A. Rational-Emotive Therapie./ Corsini R.J. Current psychotherapies (4 ed.). - Itasca, Ill.: Peacock. -1989. - P. 197-238.
15. Ellis A. Rational-Emotive Therapy // Current psychotherapies (ed. Corsini R. J.) -Itasca, III: Peacock. -1989. - P. 197-238.
16. Garfield S.L. Research on client variables in psychotherapy. In A.E. Bergin and S.L. Garfield (Eds>). - Handbook of Psychothera-py and Behavior Change, 4th ed. - New York: Wiley. - 1994.