Depression with atypical features
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.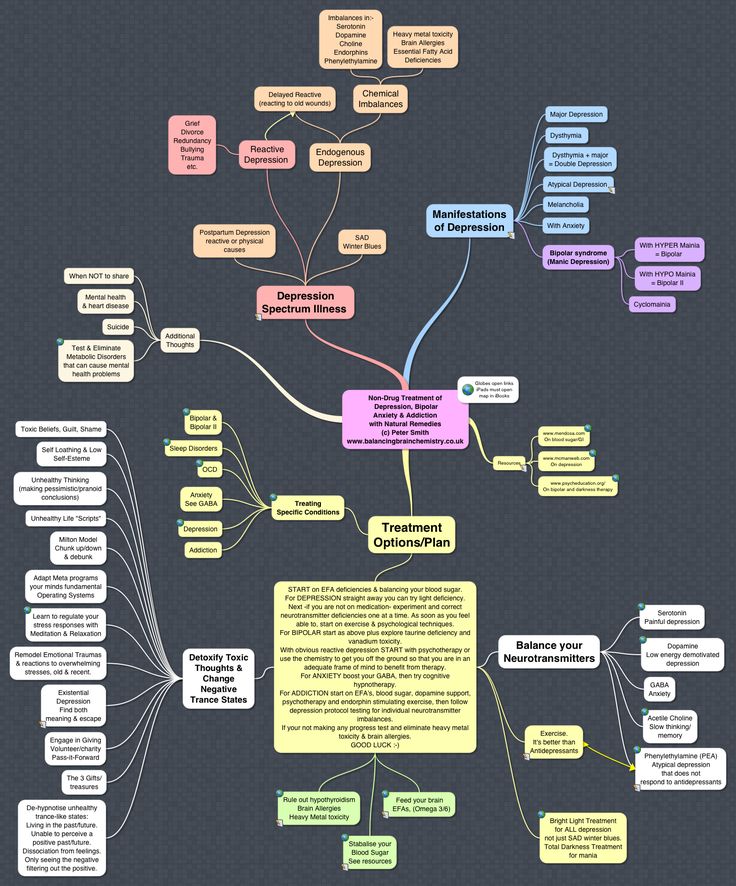 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Childhood depression
As strange as it sounds, children, including infants, also experience depression. True, it manifests itself in children a little differently than in an adult. Therefore, many parents, educators and teachers often do not even know what condition the child is in. Oddities in his behavior are attributed to the difficulties of character, improper upbringing and capriciousness. There can be several causative factors for the occurrence of depressive dynamics in a child. Let's consider the most basic of them. A significant loss for a child at the age of approximately one to two years actually guarantees some depressive dynamics. A child whose parent suddenly disappears will, by virtue of his understanding of the world, always develop the assumption that he himself is bad. The cause of childhood depression may be a family atmosphere where there is a negative attitude towards crying or mourning. Many parents model grief denial and insist that the child join the family myth that it will be better without the lost object, forcing the child to confirm that he does not feel pain. As a result, the child's experience of grief becomes hidden. It goes deeper and gradually takes the form of a conviction that something is wrong in one's own Self. In our subculture, it is not customary to take children to funerals, to tell the truth about death. Children experience intense, unspeakable pressure that comes from an emotionally burdened parent. In many families, it is not customary to openly experience grief, and taking care of yourself is considered selfish. Many parents throughout childhood admonish the child to "don't whine and pull himself together", despite the fact that the child's natural regressive reactions (returning to his earlier forms of behavior) in response to family problems should not be subject to parental control.
A child whose parent suddenly disappears will, by virtue of his understanding of the world, always develop the assumption that he himself is bad. The cause of childhood depression may be a family atmosphere where there is a negative attitude towards crying or mourning. Many parents model grief denial and insist that the child join the family myth that it will be better without the lost object, forcing the child to confirm that he does not feel pain. As a result, the child's experience of grief becomes hidden. It goes deeper and gradually takes the form of a conviction that something is wrong in one's own Self. In our subculture, it is not customary to take children to funerals, to tell the truth about death. Children experience intense, unspeakable pressure that comes from an emotionally burdened parent. In many families, it is not customary to openly experience grief, and taking care of yourself is considered selfish. Many parents throughout childhood admonish the child to "don't whine and pull himself together", despite the fact that the child's natural regressive reactions (returning to his earlier forms of behavior) in response to family problems should not be subject to parental control. Subsequently, in adulthood, such a child experiences an urgent need to hide from others any traumatic aspects of his life. The strongest causal factor in the occurrence of depression in a child is characterological depression in parents, especially in his early years of development. Children always experience deep anxiety in connection with the depression of their parents. They feel guilty about the natural demands of their age and come to believe that their needs are draining others. A depressed mother can only provide supervising care to the child, but she is emotionally unavailable to the child. A clean, well-groomed, beautifully dressed child is always perceived positively by others. But at the same time, he may be deprived of the emotional warmth of his own parents. Any child develops normally only in those relationships where he is satisfied. It is always necessary to satisfy not a direct, but a hidden request of a child. If a child asks his mother to play with him, this does not mean that he lacks a partner to play with, children always have an imaginary interlocutor.
Subsequently, in adulthood, such a child experiences an urgent need to hide from others any traumatic aspects of his life. The strongest causal factor in the occurrence of depression in a child is characterological depression in parents, especially in his early years of development. Children always experience deep anxiety in connection with the depression of their parents. They feel guilty about the natural demands of their age and come to believe that their needs are draining others. A depressed mother can only provide supervising care to the child, but she is emotionally unavailable to the child. A clean, well-groomed, beautifully dressed child is always perceived positively by others. But at the same time, he may be deprived of the emotional warmth of his own parents. Any child develops normally only in those relationships where he is satisfied. It is always necessary to satisfy not a direct, but a hidden request of a child. If a child asks his mother to play with him, this does not mean that he lacks a partner to play with, children always have an imaginary interlocutor. This means that the child needs at the moment in his mother's presence.
This means that the child needs at the moment in his mother's presence.
Childhood emotional disorders
Children's emotional disorders are affective disorders. Although it was previously believed that children are not prone to such disorders. Recognizing childhood depression is not difficult. When children are depressed, their mood is lowered or elevated, there is a noticeable decrease in activity in the speech or motor sphere. In depression, sleep and appetite are usually disturbed. Children with depression are characterized by pain of different localization. The child often has a headache and stomachache - these are the main points of somatic vulnerability in children. Recognizing such pain in a child is simple - the pain is not stopped by analgesics. Symptoms of depression include enuresis, constipation, tics, obsessions, and any atypical behavior in a child. After three years, depressed children may have hallucinatory phenomena. After 3-4 years, depressive states become more pronounced. Somatovegetative disorders predominate. Parents examine their children for violations of the systems and organs that they suffer, but doctors do not find any pathology there. In some cases, a depressed child has regression: thumb sucking, scratching sores, elective mutism (selective non-speaking). Monosymptoms in children always indicate an affective disorder, thus depression is expressed. Up to 10 years of age, affective disorders are usually masked by somatovegetative and behavioral disorders. Depressed schoolchildren usually experience a decline in academic performance.
Somatovegetative disorders predominate. Parents examine their children for violations of the systems and organs that they suffer, but doctors do not find any pathology there. In some cases, a depressed child has regression: thumb sucking, scratching sores, elective mutism (selective non-speaking). Monosymptoms in children always indicate an affective disorder, thus depression is expressed. Up to 10 years of age, affective disorders are usually masked by somatovegetative and behavioral disorders. Depressed schoolchildren usually experience a decline in academic performance.
Behavior and appearance of a depressed child
The behavior of children with depression is always stereotyped. A depressed child has absolutely no interest in life. For an ordinary healthy child, this condition is unnatural and abnormal. Childhood depression is not difficult to recognize. It is expressed in increasing motor lethargy, the child's emotional manifestations decrease, causeless prolonged whining, unmotivated crying appears. At the same time, the satisfaction of his desire does not lead to an end to whining. The face of a depressed child is usually motionless, it has a frozen mask, as it were, and there is practically no expression on the face. He has the lifeless face of a mannequin. Older children, latent (from 6 to 11 years old) and pre-pubertal (12-13 years old) ages, have a glued smile on their faces. A kind of half-smile, behind which pain, fear and shame are hidden. Such a smile may be an attempt to win the favor of an adult. If depression intensifies, then the child has a change in posture and gait. He begins to stoop and drag his feet. Parents usually swear at the same time, and the child simply has sluggish motor skills. When depressed, children refuse to go for a walk, they are not interested in walking. Depressed children have no desire to go out, either alone or with their parents. At night, a child with depression has insomnia, he just lies awake with his eyes open, but usually does not call either of the parents.
At the same time, the satisfaction of his desire does not lead to an end to whining. The face of a depressed child is usually motionless, it has a frozen mask, as it were, and there is practically no expression on the face. He has the lifeless face of a mannequin. Older children, latent (from 6 to 11 years old) and pre-pubertal (12-13 years old) ages, have a glued smile on their faces. A kind of half-smile, behind which pain, fear and shame are hidden. Such a smile may be an attempt to win the favor of an adult. If depression intensifies, then the child has a change in posture and gait. He begins to stoop and drag his feet. Parents usually swear at the same time, and the child simply has sluggish motor skills. When depressed, children refuse to go for a walk, they are not interested in walking. Depressed children have no desire to go out, either alone or with their parents. At night, a child with depression has insomnia, he just lies awake with his eyes open, but usually does not call either of the parents. A depressed child often complains of boredom, expressing it with the words: “I don’t want anything, I’m bored, I have nothing to do.” Older children say: "No one plays with me." Preteens (12-13 years old) usually start talking about their own inadequacy and guilt. A teenager with increasing depression, on the contrary, shows motor activity, anxiety, twirls something in his hands, constantly moves or shakes his legs. Motor inhibition is usually observed in the morning, in the evening there is some revival. Sometimes for a long time with depression, the child simply demonstrates indifference and indifference in behavior.
A depressed child often complains of boredom, expressing it with the words: “I don’t want anything, I’m bored, I have nothing to do.” Older children say: "No one plays with me." Preteens (12-13 years old) usually start talking about their own inadequacy and guilt. A teenager with increasing depression, on the contrary, shows motor activity, anxiety, twirls something in his hands, constantly moves or shakes his legs. Motor inhibition is usually observed in the morning, in the evening there is some revival. Sometimes for a long time with depression, the child simply demonstrates indifference and indifference in behavior.
Other manifestations of depression
In depressed children, as a rule, chilliness, sweating, pressure fluctuations, weight loss, dyskinesia, indigestion, and dysbacteriosis are observed. Parents intensively treat children with doctors, but in fact the child should be sent to a psychotherapeutic course with a child psychotherapist. As a rule, no one notices a decrease in a child's interest in the environment: a depressed child is usually quiet, calm, does not run, does not scream, and this is perceived by parents as the norm. A child with depression has hyperesthesia - increased sensitivity to stimuli or increased tactile sensitivity. The child cannot stand loud noises and sharp sounds; the collar, sweater or hat constantly interferes with him. In severe cases, the child loses previously acquired knowledge, skills, and his intellectual functioning decreases. Often such children are given a false diagnosis of mental retardation (MPD), under which a depressive syndrome is hidden. A child in depression is characterized by increased exhaustion, fatigue, capriciousness. When doing lessons, sitting at the table for many hours does not bring results. The ability to independently prepare lessons most often disappears. The ability to experience failure is impaired, the child refuses achievements so as not to feel helpless. Complains of boredom, he "has nothing to do." Preschool children are very touchy and vulnerable, they do not play with their peers, they have sad dreams, their fantasies are also very sad.
A child with depression has hyperesthesia - increased sensitivity to stimuli or increased tactile sensitivity. The child cannot stand loud noises and sharp sounds; the collar, sweater or hat constantly interferes with him. In severe cases, the child loses previously acquired knowledge, skills, and his intellectual functioning decreases. Often such children are given a false diagnosis of mental retardation (MPD), under which a depressive syndrome is hidden. A child in depression is characterized by increased exhaustion, fatigue, capriciousness. When doing lessons, sitting at the table for many hours does not bring results. The ability to independently prepare lessons most often disappears. The ability to experience failure is impaired, the child refuses achievements so as not to feel helpless. Complains of boredom, he "has nothing to do." Preschool children are very touchy and vulnerable, they do not play with their peers, they have sad dreams, their fantasies are also very sad.
Background of depressive disorder
After 5-6 years, against the background of a depressive disorder, a child often appears self-deprecating statements, unmotivated aggression. During latent (6-11 years) and prepubertal age (12-13 years), if there is a starting traumatic situation (death, divorce, parental illness), the child has guilt and a thirst for self-punishment (he constantly beats against something, gets injured , inflicts allegedly accidental damage to himself). Although the child does not have a reaction to a significant event, it should not be so. Veiled, the reaction manifests itself in the appearance of traumatic behavior, tics, obsessions, phobias, or some other symptoms. Depression in children disrupts the perception of body parts ("it's my hand to blame"). Awareness of activity is impaired (frequent questions like "mom, have I already eaten?", "dad, did we walk today?"), as well as awareness of gender and age (children cannot answer elementary questions about their gender and age). Depressed children tend to constantly and for no reason, insatiably ask their parents for forgiveness: "Daddy, please forgive me," and look for verbal confirmation of love: "Mom, do you really love me?" At the same time, the child's speech is usually slurred, more like a whisper, his dreams are gloomy.
During latent (6-11 years) and prepubertal age (12-13 years), if there is a starting traumatic situation (death, divorce, parental illness), the child has guilt and a thirst for self-punishment (he constantly beats against something, gets injured , inflicts allegedly accidental damage to himself). Although the child does not have a reaction to a significant event, it should not be so. Veiled, the reaction manifests itself in the appearance of traumatic behavior, tics, obsessions, phobias, or some other symptoms. Depression in children disrupts the perception of body parts ("it's my hand to blame"). Awareness of activity is impaired (frequent questions like "mom, have I already eaten?", "dad, did we walk today?"), as well as awareness of gender and age (children cannot answer elementary questions about their gender and age). Depressed children tend to constantly and for no reason, insatiably ask their parents for forgiveness: "Daddy, please forgive me," and look for verbal confirmation of love: "Mom, do you really love me?" At the same time, the child's speech is usually slurred, more like a whisper, his dreams are gloomy.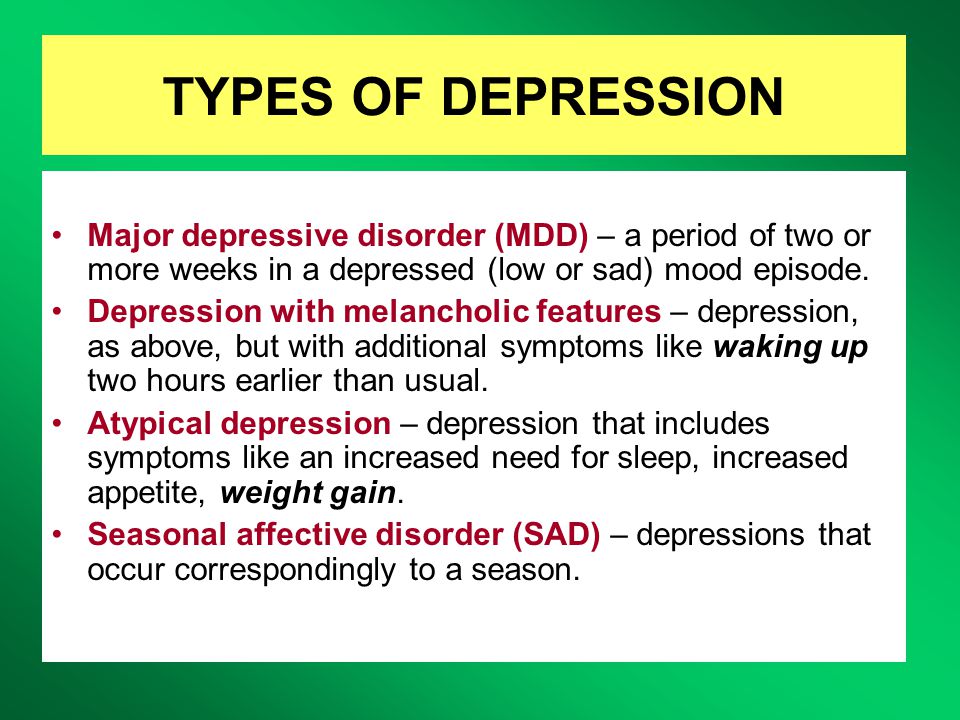 A child with depression may experience motor obsessions (he constantly jerks his arms, moves his legs), various phobias ("I'm afraid of a wolf", "I have a monster in my room"), verbal tics. In depression, the child's sense of identity is disturbed. He requires his parents to call him by a different name. Or asks to call him, for example, a kitten, a chicken. That is, the child replaces his identity with requests to call himself some kind of animal. In severe cases, the child may walk on all fours, meow, bark, and refuse normal human behavior. Often the parents themselves unconsciously provoke the child to such behavior, giving him home nicknames and nicknames ("kitten", "chicken", etc.).
A child with depression may experience motor obsessions (he constantly jerks his arms, moves his legs), various phobias ("I'm afraid of a wolf", "I have a monster in my room"), verbal tics. In depression, the child's sense of identity is disturbed. He requires his parents to call him by a different name. Or asks to call him, for example, a kitten, a chicken. That is, the child replaces his identity with requests to call himself some kind of animal. In severe cases, the child may walk on all fours, meow, bark, and refuse normal human behavior. Often the parents themselves unconsciously provoke the child to such behavior, giving him home nicknames and nicknames ("kitten", "chicken", etc.).
A child and his symptom is always evidence of an abnormal situation in the family.
Manic symptoms and syndromes in children
Children with similar symptoms can be called hyperactive children with motor disinhibition syndrome. They are characterized by motor restlessness with features of cheerfulness. Such a child grimaces, makes faces, grimace. His speech is usually sped up, he constantly changes topics of conversation. The sense of shame has been lost. Communication with peers with manic symptoms is impaired. Children simply do not want to communicate with such a child. The behavior of such children is usually qualified by educators as "bad behavior". Children are unceremonious, foolish, uncritical, they have no boundaries between themselves and adults. They are incapable of long-term activity. In severe cases, they demonstrate psychopathic behavior: slovenliness, throwing things around, can be aggressive with a danger to others. Psychopathic behavior is characterized by inappropriate responses to events. For example, when showing a story about a plane crash, such a child can gloatingly comment on the news with the words: "That's how they should be!".
Such a child grimaces, makes faces, grimace. His speech is usually sped up, he constantly changes topics of conversation. The sense of shame has been lost. Communication with peers with manic symptoms is impaired. Children simply do not want to communicate with such a child. The behavior of such children is usually qualified by educators as "bad behavior". Children are unceremonious, foolish, uncritical, they have no boundaries between themselves and adults. They are incapable of long-term activity. In severe cases, they demonstrate psychopathic behavior: slovenliness, throwing things around, can be aggressive with a danger to others. Psychopathic behavior is characterized by inappropriate responses to events. For example, when showing a story about a plane crash, such a child can gloatingly comment on the news with the words: "That's how they should be!".
Factors causing depression in children
What factors lead to depression in children? There may be several.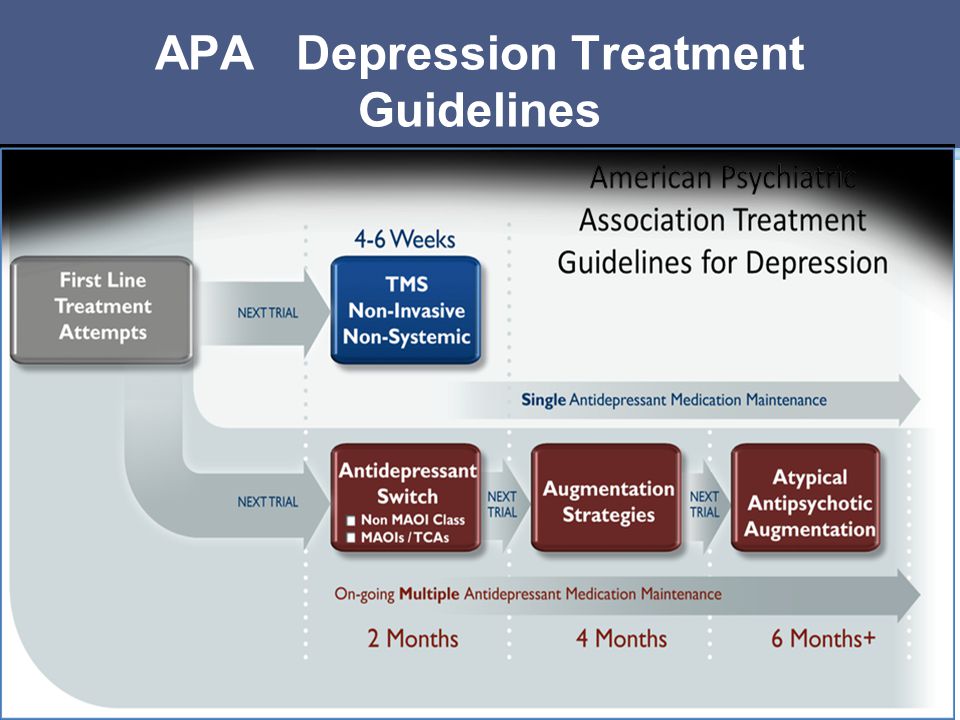 Here are the main ones:
Here are the main ones:
- Maternal deprivation, or prolonged absence of the mother.
- Serious social deprivation plus pedagogical affectivity (injustice, inadequate punishments).
- Acute psychosomatic diseases.
- Death of a person or pet significant to the child.
- Under the influence of depression of one of the parents who infects the child with his depression.
Take a close look at your child. It is possible that what you take for strange behavior may be precisely manifestations of depression. You can help your child get rid of depression with the help of specialists. In child psychoanalysis, when working with children, children's play therapy is used, during which the child gets rid of his symptoms.
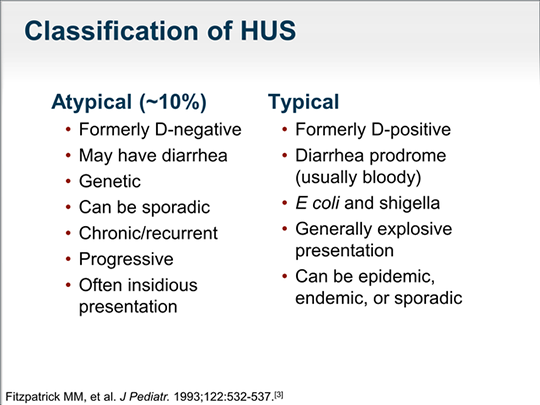
Atypical depression - asia-pharm.ru
Overview
Atypical depression used to be considered a form of depression. The American Psychiatric Association no longer recognizes atypical depression as a separate disorder. Instead, the condition is now referred to as major depression with atypical features.
Instead, the condition is now referred to as major depression with atypical features.
Major depressive disorder (MDD) is a mental disorder that can affect how people think, feel and behave. People with MDD often lose interest in activities they normally enjoy and have trouble completing everyday tasks. Sometimes they may also feel that life is not worth living. These symptoms can interfere with daily life and affect physical and emotional health.
Symptoms of MDD with atypical features are similar to those of classic MDD. However, there is a key difference. In people with MDD with atypical features, mood may improve in response to positive circumstances and events. A positive change is unlikely to improve mood in people with classic MDD.
Atypical symptoms of depression
Symptoms of MDD with atypical features can vary from person to person. However, in general, people with the condition often experience symptoms of MDD. These symptoms include:
- constant feeling of sadness or hopelessness
- anxiety or irritability
- sleeping too much or too little
- loss of interest in activities that were once enjoyable
- difficulty concentrating, making decisions, and remembering things 9004 low energy or fatigue
- thoughts or talk of suicide
They may also experience atypical MDD features such as:
- mood that temporarily lifts or improves in response to positive events or good news
- significant weight gain
- increased appetite
- feeling of heaviness in the arms or legs
- body aches or headaches
- sleeping for a long period of time during the day or night
- extremely negative reaction to perceived criticism or rejection
AD
Online therapy can help with depression
Improve your quality of life with the support of licensed BetterHelp therapists.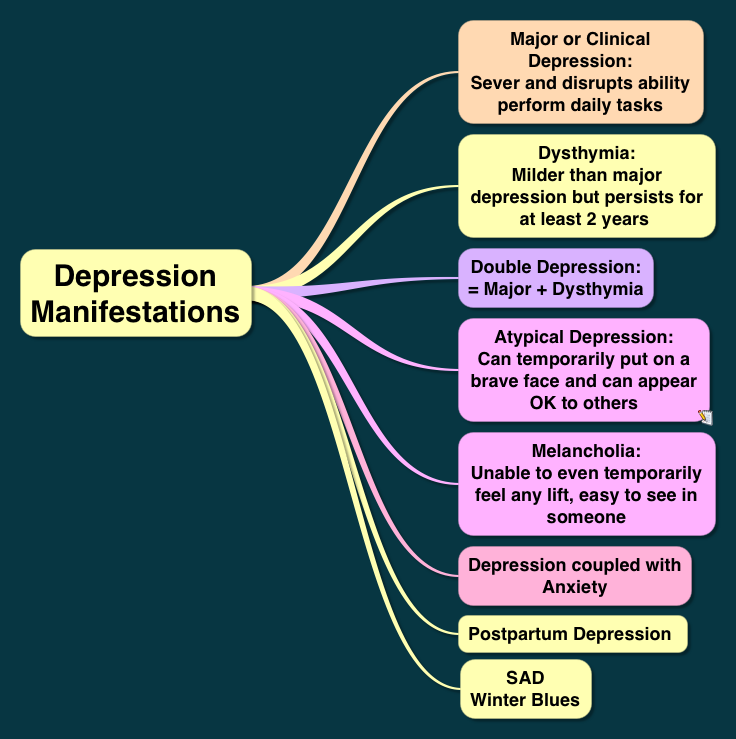 Get therapy when you need it, by phone, video or chat.
Get therapy when you need it, by phone, video or chat.
TAKE THE QUIZ
Causes of atypical depression
The exact cause of MDD with atypical features is not known. However, there are factors that can increase the risk of developing this condition. Common risk factors include:
- traumatic experiences such as physical abuse, death of a loved one or divorce
- history of alcohol and drug abuse
- diagnosed with a serious illness
Genetics may also play a role in the development of MDD. People who have a family history of MDD are more likely to develop the condition.
MDD can also be caused by an imbalance of mood-regulating brain chemicals such as serotonin, norepinephrine, and dopamine.
Diagnosis of atypical depression
Make an appointment with your doctor if you think you have MDD with atypical features. Your doctor may do a physical exam and order laboratory tests, such as a complete blood count and a thyroid function test. These tests can identify potential health issues that may be causing your symptoms. Treating the underlying condition can improve your mood and ease other symptoms associated with MDD.
These tests can identify potential health issues that may be causing your symptoms. Treating the underlying condition can improve your mood and ease other symptoms associated with MDD.
Your doctor may also have a psychological evaluation to look for signs of MDD with atypical features. They may ask you questions about your:
- symptoms
- personal life
- past experience
- current medications
- personal or family history
Your doctor may diagnose MDD with atypical features 9003 9003 that is causing your symptoms
Treatment of atypical depression
Treatment of MDD with atypical features may vary. However, in most cases, treatment involves a combination of medication, talking therapy, and lifestyle changes.
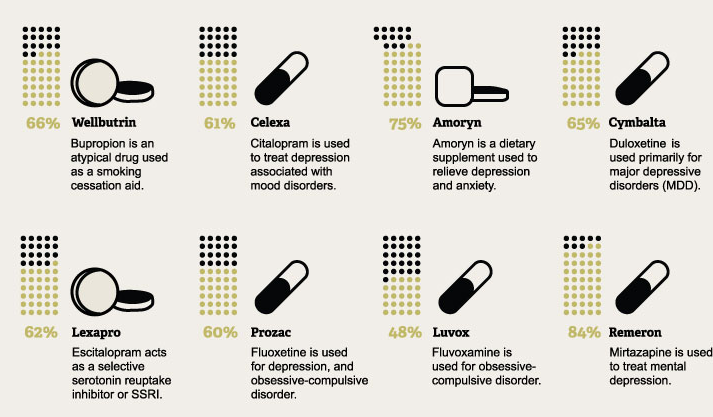
Medications
Your doctor may prescribe antidepressants such as monoamine oxidase inhibitors (MAOIs) or selective serotonin reuptake inhibitors (SSRIs). Some people with MDD with atypical features do not respond well to tricyclic antidepressants. However, numerous MAOIs and SSRIs have proven effective in treating the symptoms of the disorder. Your doctor may prescribe one medicine or a combination of medicines to control your symptoms.
Some people with MDD with atypical features do not respond well to tricyclic antidepressants. However, numerous MAOIs and SSRIs have proven effective in treating the symptoms of the disorder. Your doctor may prescribe one medicine or a combination of medicines to control your symptoms.
It is important to note that MAOIs may require a change in diet. These antidepressants may interact with certain foods and medications, including birth control pills and decongestants. Be sure to ask your doctor about side effects and food or drug interactions before starting a new medication.
Talk therapy
Talk therapy involves regular meetings with a psychotherapist or counselor. This type of treatment allows:
- express your feelings
- identify unhealthy thoughts
- learn to solve problems
This can help you cope with your condition and improve your outlook. Your therapist can also show you how to set realistic life goals so you can regain a sense of fulfillment and control over your life.
Lifestyle and home remedies
In addition to medications and therapies, lifestyle changes and home remedies can also help relieve symptoms of atypical MDD. This includes:
- avoid recreational drugs and alcohol
- exercise at least three times a week
- sleep a lot
- use relaxation techniques such as deep breathing and meditation
- take certain supplements such as fish oil and St. John's wort
Living with atypical depression
Talk therapy, medication, and lifestyle changes are effective treatments for atypical MDD. But there are other ways to deal with symptoms:
- Write in a diary every day.
- Plan ahead and manage your time well.
- Participate in activities that help manage stress, such as yoga, tai chi, or meditation.
- Surround yourself with family and friends instead of isolating yourself.