How to deal with ibs anxiety
Stress, Anxiety, and IBS: Coping Techniques
Here to keep you healthy. And informed.
Get 24/7 care over video chat from the comfort of home or wherever you go. Join today and experience primary care designed for real life, in-office and in-app.
Join Today
Home/ Blog/ Get Well/
Nov 1, 2013
By Christine Celio
Ever had an upset stomach or other gastrointestinal issues before a test, a first date, or a job interview? You’re not alone–for some, this is such a regular occurrence that they anticipate these events and pack extra Pepto-Bismol or locate the nearest restroom in advance.
Medical experts have long thought that excess stress may worsen underlying gastrointestinal issues. The good news: There are a number of effective strategies for dealing with these troublesome symptoms.
About IBS
Irritable bowel syndrome (IBS) is a disorder of the colon that can cause cramping, abdominal pain, bloating, gas, diarrhea, and constipation. Unlike more severe intestinal diseases such as ulcerative colitis and Crohn’s disease, IBS doesn’t cause inflammation or changes in bowel tissue or increase your risk of colorectal cancer.
Not all IBS cases are stress-related, but in many cases, it’s possible to control irritable bowel syndrome by managing your diet, lifestyle, and stress. However, it’s important to discuss your concerns with your health care provider to confirm you don’t have another underlying medical disorder causing these symptoms.
The Stress-IBS Link
The directional relationship between stress, anxiety, and IBS hasn’t been clearly established, but research indicates that they often co-exist. There are two primary theories about how the relationship functions.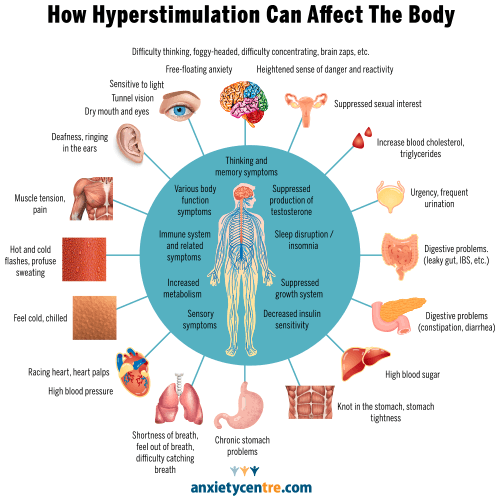 One is that stress and anxiety may make you hyperaware of spasms in the colon, potentially worsening your experience with these symptoms. Another theory is that IBS may be triggered by the immune system, which is affected by stress.
One is that stress and anxiety may make you hyperaware of spasms in the colon, potentially worsening your experience with these symptoms. Another theory is that IBS may be triggered by the immune system, which is affected by stress.
The human gut and brain are in constant communication. In prehistoric times, this relationship served us well: During times of imminent threat, the fight-or-flight response would kick in, and the stomach would react by either emptying immediately or holding on to its contents until the threat was over.
Today, despite the fact that our day-to-day stressors aren’t the momentary, potentially lethal threats our ancestors faced, we’re still wired the same way. Our “predators” aren’t the occasional large carnivores; they’re ever-present things like deadlines, performance reviews, and busy schedules. This constant stress and anxiety can result in chronic gastrointestinal issues.
Where to Turn for Help
A nutritionist or naturopathic doctor may be able to help resolve or reduce IBS symptoms, and can discuss the potential benefits of nutrition and supplementation. These health care providers may also help you identify possible dietary triggers to be aware of. In addition, there are some other steps you can take to positively impact how your brain and gut communicate, including cognitive behavioral therapy (CBT) for irritable bowel syndrome, and learning how to manage symptoms on your own.
These health care providers may also help you identify possible dietary triggers to be aware of. In addition, there are some other steps you can take to positively impact how your brain and gut communicate, including cognitive behavioral therapy (CBT) for irritable bowel syndrome, and learning how to manage symptoms on your own.
Cognitive Behavioral Therapy for IBS
Although experts don’t know what causes anxiety to trigger stomach pain, discomfort, diarrhea, and constipation, effectively managing emotional reactions seems to ease symptoms. CBT helps users identify thoughts and behaviors that affect the gastrointestinal system, and understand how, in turn, the gastrointestinal system affects mood. In addition, CBT equips users with coping techniques to manage these unhelpful thoughts and behaviors with the goal of reducing IBS symptoms.
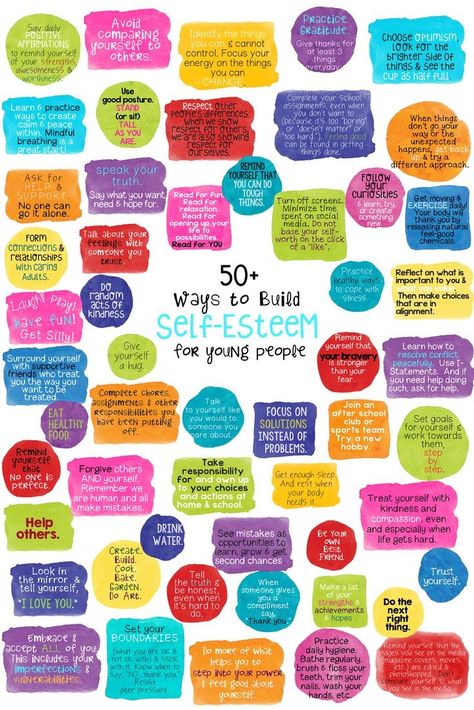
Relaxation exercises and calming self-talk are two CBT coping techniques that may help.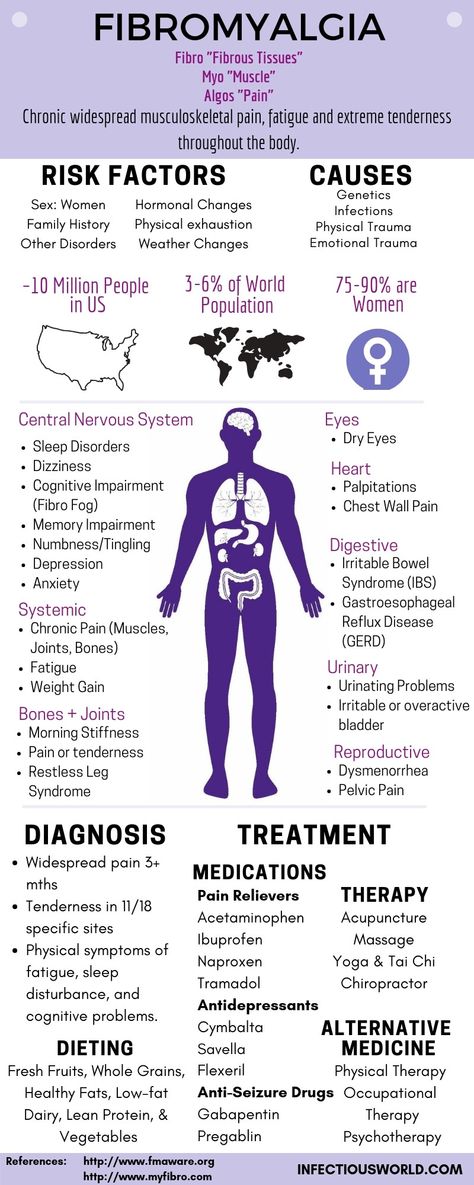 These exercises enable users to actively lessen the stress response, thereby reducing the gut changes that occur in response to thoughts and feelings. For example, when you breathe deeply or use calming self-talk to quell anxiety, you send a message to your body that there is no crisis. This reduces the effects of the body’s natural stress response on your digestive system, helping to ease symptoms. Breathing deeply also can lessen anxiety and may help reduce pain.
These exercises enable users to actively lessen the stress response, thereby reducing the gut changes that occur in response to thoughts and feelings. For example, when you breathe deeply or use calming self-talk to quell anxiety, you send a message to your body that there is no crisis. This reduces the effects of the body’s natural stress response on your digestive system, helping to ease symptoms. Breathing deeply also can lessen anxiety and may help reduce pain.
How to Be Prepared for Future IBS Attacks
Once you’ve had a bad IBS attack, it’s very common to be worried about having another one. You may find that you go on alert, scanning your body for signs and symptoms. Unfortunately, anxiety about future attacks may actually increase your chances of having one. To deal with this:
- Remain calm in the face of early symptoms. Try different coping techniques until you find what is most effective for you.

- Keep a symptom diary. This can help you identify possible patterns related to your attacks. For example, if you know you’re more likely to experience attacks in the morning, you can plan your day accordingly (e.g., ensuring you know where the nearest restroom is).
- Practice regular stress management activities.
- Be wise about what you eat. It’s important to be aware of dietary sensitivities that may trigger an attack. Common trigger foods include dairy, gluten, and caffeine. Know your triggers, and avoid or reduce your intake accordingly.
While the relationship between stress and gastrointestinal issues is still unclear, understanding how stress affects you can help you be prepared by developing a variety of coping strategies.
Here to keep you healthy. And informed.
Get 24/7 care over video chat from the comfort of home or wherever you go. Join today and experience primary care designed for real life, in-office and in-app.
Join Today
Tags
anxiety ibs irritable bowel syndrome stomach stress stressChristine Celio
As a licensed clinical psychologist, Christine approaches patient care with empathy and a listening ear. She has a broad base of experience in clinical psychology and research, having taught in various academic settings and published articles in several academic journals. After earning her master's in sociology from Stanford, Christine coordinated clinical research studies at the Stanford School of Medicine. She went on to complete an additional master's in clinical psychology and received her PhD in clinical psychology from Loyola University Chicago. She completed residency and fellowship at the West Los Angeles VA Medical Center and the San Francisco VA Medical Center/UCSF Center for Excellence in Primary Care. Christine is a board-certified psychologist.
Christine is a board-certified psychologist.
The One Medical blog is published by One Medical, a national, modern primary care practice pairing 24/7 virtual care services with inviting and convenient in-person care at over 100 locations across the U.S. One Medical is on a mission to transform health care for all through a human-centered, technology-powered approach to caring for people at every stage of life.
Any general advice posted on our blog, website, or app is for informational purposes only and is not intended to replace or substitute for any medical or other advice. 1Life Healthcare, Inc. and the One Medical entities make no representations or warranties and expressly disclaim any and all liability concerning any treatment, action by, or effect on any person following the general information offered or provided within or through the blog, website, or app. If you have specific concerns or a situation arises in which you require medical advice, you should consult with an appropriately trained and qualified medical services provider.
Overcoming Irritable Bowel Syndrome (IBS)
10.24.2018
Melissa G. Hunt, PhD
Melissa G. Hunt is a licensed clinical psychologist and serves as the Associate Director of Clinical Training in the Department of Psychology at the University of Pennsylvania. She is a Fellow and Diplomate of the Academy of Cognitive Therapy and a member of the Rome Foundation Psychogastroenterology working group.
Dr. Hunt conducts research on the best approaches for stress management, and into the causes and treatment of depression, anxiety disorders and chronic GI disorders. As a clinical scientist, her emphasis is on translating basic psychological science into treatments that are effective, acceptable, and accessible to patient populations. In particular, Dr. Hunt focuses on identifying and correcting the underlying patient factors (e.g. unhelpful beliefs and maladaptive avoidance) that lead to reduced quality of life, impairment and distress, particularly factors that exacerbate chronic health problems and make them harder to cope with. In addition to her research, she maintains an active private practice in clinical psychology in which she specializes in cognitive-behavioral treatment of mood, anxiety, obsessive-compulsive, and trauma disorders and on working with patients with chronic GI disorders and other health problems. Dr. Hunt is the author of the highly-regarded self-help book “Reclaim Your Life from IBS: A Scientifically Proven Plan for Relief without Restrictive Diets”
In addition to her research, she maintains an active private practice in clinical psychology in which she specializes in cognitive-behavioral treatment of mood, anxiety, obsessive-compulsive, and trauma disorders and on working with patients with chronic GI disorders and other health problems. Dr. Hunt is the author of the highly-regarded self-help book “Reclaim Your Life from IBS: A Scientifically Proven Plan for Relief without Restrictive Diets”
Boost Search Results
On
October 24, 2018
Overcoming Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS), an unpleasant and often debilitating condition, is characterized by frequent, recurrent abdominal pain, as well as problems with constipation and/or diarrhea. People with IBS often experience a strong urge to use the bathroom, and may avoid going to places without easy access to one. This means that many everyday locations (malls, parks, places of worship, movie theaters, classrooms, offices) feel risky, and people might start to limit their activities as a result. People with IBS also start to fear and avoid many foods believed to trigger IBS attacks, often leading to loss of pleasure in eating as well as reduced opportunities to socialize. This fuels a vicious cycle of discomfort, anxiety, vigilance, avoidance and visceral hypersensitivity, in which GI sensations get horribly amplified. For people with IBS, indigestion can feel like a terrifying event which could lead to excruciating pain, incontinence and humiliation.
People with IBS also start to fear and avoid many foods believed to trigger IBS attacks, often leading to loss of pleasure in eating as well as reduced opportunities to socialize. This fuels a vicious cycle of discomfort, anxiety, vigilance, avoidance and visceral hypersensitivity, in which GI sensations get horribly amplified. For people with IBS, indigestion can feel like a terrifying event which could lead to excruciating pain, incontinence and humiliation.
Luckily for sufferers of IBS, cognitive behavioral therapy (CBT) has been found to be an effective treatment for the condition. First, it is important for the practitioner to consult the patient’s other medical providers and ensure that several alternative diagnoses have been ruled out. The most important rule outs are inflammatory bowel diseases (Crohn’s and Colitis) and celiac disease (which leads to complete gluten intolerance). Fortunately, simple blood and stool tests are usually enough to rule these conditions out. The next step is educating the patient about the link between stress and arousal of the sympathetic nervous system, which can directly impact GI discomfort. IBS is not “all in your head” – the pain and GI dysfunction are very real. But stress makes GI problems worse through direct biological mechanisms. The practitioner should then train the patient in relaxation techniques like deep belly breathing.
IBS is not “all in your head” – the pain and GI dysfunction are very real. But stress makes GI problems worse through direct biological mechanisms. The practitioner should then train the patient in relaxation techniques like deep belly breathing.
Once the patient is able to use these relaxation techniques effectively, it is time to introduce the CBT model, which teaches that beliefs (not situations) affect our emotions and that beliefs can be inaccurate. Inaccurate beliefs, in this case catastrophic beliefs and predictions about GI symptoms, can be altered with the help of behavioral experiments. For example, it can be helpful to send the patient to a movie theater or house of worship and have them sit in the back and count the number of people who get up and leave and then return. Often, the patient will be surprised at how often this happens and how little other people react; it can help the patient understand that having to get up and use the bathroom is not a big deal.
The final step in CBT is exposure therapy in which the patient starts doing things they’ve been avoiding. For example, if they are afraid of long car trips, have them start by sitting in the car in their driveway for thirty minutes. Once that gets boring and easy, have them drive around the block 20 times. Then have them drive a mile away from home and back, and so on. If the patient fears incontinence, then in the safety of their own home have them experiment with “holding it” when they feel the urge, first for 30 seconds, then a minute, then 5 minutes. This will prove to them that they are able to “hold it” and catastrophizing is unnecessary.
For example, if they are afraid of long car trips, have them start by sitting in the car in their driveway for thirty minutes. Once that gets boring and easy, have them drive around the block 20 times. Then have them drive a mile away from home and back, and so on. If the patient fears incontinence, then in the safety of their own home have them experiment with “holding it” when they feel the urge, first for 30 seconds, then a minute, then 5 minutes. This will prove to them that they are able to “hold it” and catastrophizing is unnecessary.
This CBT treatment is presented at a much more detailed level in the book Reclaim Your Life from IBS: A Scientifically Proven Plan for Relief Without Restrictive Diets. The book was actually tested in a randomized controlled trial and was shown to be quite effective (Hunt, M., Ertel, E., Coello, J. & Rodriguez, L. (2014). Empirical Support for a Self-Help Treatment for IBS. Cognitive Therapy and Research, 39(2), 215-227).
You can also hear Dr. Hunt discuss this treatment strategy on an ADAA webinar, Overcoming Irritable Bowel Syndrome (IBS): Reclaim Your Life from Anxiety and Distress about IBS Symptoms.
Hunt discuss this treatment strategy on an ADAA webinar, Overcoming Irritable Bowel Syndrome (IBS): Reclaim Your Life from Anxiety and Distress about IBS Symptoms.
Melissa G. Hunt, PhD
Melissa G. Hunt is a licensed clinical psychologist and serves as the Associate Director of Clinical Training in the Department of Psychology at the University of Pennsylvania. She is a Fellow and Diplomate of the Academy of Cognitive Therapy and a member of the Rome Foundation Psychogastroenterology working group.
Dr. Hunt conducts research on the best approaches for stress management, and into the causes and treatment of depression, anxiety disorders and chronic GI disorders. As a clinical scientist, her emphasis is on translating basic psychological science into treatments that are effective, acceptable, and accessible to patient populations. In particular, Dr. Hunt focuses on identifying and correcting the underlying patient factors (e.g. unhelpful beliefs and maladaptive avoidance) that lead to reduced quality of life, impairment and distress, particularly factors that exacerbate chronic health problems and make them harder to cope with. In addition to her research, she maintains an active private practice in clinical psychology in which she specializes in cognitive-behavioral treatment of mood, anxiety, obsessive-compulsive, and trauma disorders and on working with patients with chronic GI disorders and other health problems. Dr. Hunt is the author of the highly-regarded self-help book “Reclaim Your Life from IBS: A Scientifically Proven Plan for Relief without Restrictive Diets”
In addition to her research, she maintains an active private practice in clinical psychology in which she specializes in cognitive-behavioral treatment of mood, anxiety, obsessive-compulsive, and trauma disorders and on working with patients with chronic GI disorders and other health problems. Dr. Hunt is the author of the highly-regarded self-help book “Reclaim Your Life from IBS: A Scientifically Proven Plan for Relief without Restrictive Diets”
Irritable Bowel Syndrome (IBS)
ADAA Blog Content and Blog Comments Policy
ADAA Blog Content and Blog Comments Policy
ADAA provides this Website blogs for the benefit of its members and the public. The content, view and opinions published in Blogs written by our personnel or contributors – or from links or posts on the Website from other sources - belong solely to their respective authors and do not necessarily reflect the views of ADAA, its members, management or employees. Any comments or opinions expressed are those of their respective contributors only. Please remember that the open and real-time nature of the comments posted to these venues makes it is impossible for ADAA to confirm the validity of any content posted, and though we reserve the right to review and edit or delete any such comment, we do not guarantee that we will monitor or review it. As such, we are not responsible for any messages posted or the consequences of following any advice offered within such posts. If you find any posts in these posts/comments to be offensive, inaccurate or objectionable, please contact us via email at [email protected] and reference the relevant content. If we determine that removal of a post or posts is necessary, we will make reasonable efforts to do so in a timely manner.
Please remember that the open and real-time nature of the comments posted to these venues makes it is impossible for ADAA to confirm the validity of any content posted, and though we reserve the right to review and edit or delete any such comment, we do not guarantee that we will monitor or review it. As such, we are not responsible for any messages posted or the consequences of following any advice offered within such posts. If you find any posts in these posts/comments to be offensive, inaccurate or objectionable, please contact us via email at [email protected] and reference the relevant content. If we determine that removal of a post or posts is necessary, we will make reasonable efforts to do so in a timely manner.
ADAA expressly disclaims responsibility for and liabilities resulting from, any information or communications from and between users of ADAA’s blog post commenting features. Users acknowledge and agree that they may be individually liable for anything they communicate using ADAA’s blogs, including but not limited to defamatory, discriminatory, false or unauthorized information. Users are cautioned that they are responsible for complying with the requirements of applicable copyright and trademark laws and regulations. By submitting a response, comment or content, you agree that such submission is non-confidential for all purposes. Any submission to this Website will be deemed and remain the property of ADAA.
Users are cautioned that they are responsible for complying with the requirements of applicable copyright and trademark laws and regulations. By submitting a response, comment or content, you agree that such submission is non-confidential for all purposes. Any submission to this Website will be deemed and remain the property of ADAA.
The ADAA blogs are forums for individuals to share their opinions, experiences and thoughts related to mental illness. ADAA wants to ensure the integrity of this service and therefore, use of this service is limited to participants who agree to adhere to the following guidelines:
1. Refrain from transmitting any message, information, data, or text that is unlawful, threatening, abusive, harassing, defamatory, vulgar, obscene, that may be invasive of another 's privacy, hateful, or bashing communications - especially those aimed at gender, race, color, sexual orientation, national origin, religious views or disability.
Please note that there is a review process whereby all comments posted to blog posts and webinars are reviewed by ADAA staff to determine appropriateness before comments are posted. ADAA reserves the right to remove or edit a post containing offensive material as defined by ADAA.
ADAA reserves the right to remove or edit a post containing offensive material as defined by ADAA.
ADAA reserves the right to remove or edit posts that contain explicit, obscene, offensive, or vulgar language. Similarly, posts that contain any graphic files will be removed immediately upon notice.
2. Refrain from posting or transmitting any unsolicited, promotional materials, "junk mail," "spam," "chain mail," "pyramid schemes" or any other form of solicitation. ADAA reserves the right to delete these posts immediately upon notice.
3. ADAA invites and encourages a healthy exchange of opinions. If you disagree with a participant 's post or opinion and wish to challenge it, do so with respect. The real objective of the ADAA blog post commenting function is to promote discussion and understanding, not to convince others that your opinion is "right." Name calling, insults, and personal attacks are not appropriate and will not be tolerated. ADAA will remove these posts immediately upon notice.
4. ADAA promotes privacy and encourages participants to keep personal information such as address and telephone number from being posted. Similarly, do not ask for personal information from other participants. Any comments that ask for telephone, address, e-mail, surveys and research studies will not be approved for posting.
5. Participants should be aware that the opinions, beliefs and statements on blog posts do not necessarily represent the opinions and beliefs of ADAA. Participants also agree that ADAA is not to be held liable for any loss or injury caused, in whole or in part, by sponsorship of blog post commenting. Participants also agree that ADAA reserves the right to report any suspicions of harm to self or others as evidenced by participant posts.
RESOURCES AND NEWS
Evidence-based Tips & Strategies from our Member Experts
RELATED ARTICLES
Block reference
TAKING ACTION
Searching for Sullivan
My struggle with depression and anxiety is one I still deal with every day. The hardest part is…
The hardest part is…
Read More
Load More
Coronary heart disease: doctor's advice
“Recently I was diagnosed with coronary heart disease (CHD). From that moment on, I constantly experience anxiety, the fear of "being a burden", the mood to live has disappeared. I don’t understand why I need all this and how to live my usual life?..”
Alexandra S., Seversk.
The question is answered by a psychotherapist, candidate of medical sciences, Elena Vladimirovna Lebedeva.
IHD usually occurs in a person of working age, when there is already a family, work, when there are still many plans for the future.
Your life may never be the same. You will have to change a lot: attitude, plans, lifestyle, rhythm... And one more thing: you will have to learn a lot to live in a new state. Your life also changed when you finished school, had a baby, gained/lost a family, changed your place of residence or job. It won't be easy. It is possible to build new plans and a new future, and this will be confirmed by many who have been in your place, and their relatives, and the doctors who accompanied them on this journey.
It won't be easy. It is possible to build new plans and a new future, and this will be confirmed by many who have been in your place, and their relatives, and the doctors who accompanied them on this journey.
To regain a sense of control over your life, the first thing to do is to understand what is happening. You can get information about IHD on the Internet, at Schools of Health, from medical acquaintances, friends with heart disease. It is important to understand what information is reliable. The stewardess is often in the cockpit and sees how they control the plane, maybe even "knows some buttons." But will you trust her to fly the plane?
General information about IHD
IHD (angina pectoris, unstable angina pectoris, myocardial infarction) - a consequence of narrowing and closing of the arteries of the heart by atherosclerotic plaques with difficulty in blood flow and lack of blood supply, usually manifested by angina pectoris (pain, compression, heaviness behind the sternum or shortness of breath, arising from physical exertion, stress , when inhaling cold air, less often at rest). Attacks of angina pectoris can increase with an increase in blood pressure (BP), smoking, untimely intake or withdrawal of drugs, a few hours after drinking alcohol. Some factors (the so-called risk factors) increase the likelihood of the disease: male gender, age, early development of coronary artery disease in close relatives (in men under 55 years old, in women under 65 years old), high blood pressure, smoking, high blood cholesterol, high blood glucose (diabetes), excessive alcohol consumption, sedentary lifestyle, overweight, stress, depression.
Attacks of angina pectoris can increase with an increase in blood pressure (BP), smoking, untimely intake or withdrawal of drugs, a few hours after drinking alcohol. Some factors (the so-called risk factors) increase the likelihood of the disease: male gender, age, early development of coronary artery disease in close relatives (in men under 55 years old, in women under 65 years old), high blood pressure, smoking, high blood cholesterol, high blood glucose (diabetes), excessive alcohol consumption, sedentary lifestyle, overweight, stress, depression.
Which of these factors did you identify in yourself?
Relationship between anxiety-depressive disorders and IHD.
Normally, at rest, we do not feel the work of the heart. Our body is arranged in such a way that when we are worried (remember, you have a speech in front of an audience or an exam ...), there is a heartbeat and other signs of the hard work of the cardiovascular system. Everyone in the course of life faces different stressors (traumatic events) that can lead to an imbalance in the functioning of the nervous system and a breakdown in adaptation (stress).
People usually use one of four strategies to cope with a problem situation: get out of the situation, change it, accept or adapt to the situation. What problem management strategies do you typically use?
The fact of a sudden appearance of a heart disease is perceived as a stressor, as a loss (loss of health). And it is experienced as a loss, through stages (denial, anger, guilt, depression, acceptance), which can pass sequentially or overlap each other (like the blooming of a bruise). In addition, it is necessary to come to terms with the need and validity of a new diagnostic or therapeutic intervention, which can cause a strong emotional reaction.
Patients with coronary artery disease and depressive disorders are characterized by low stress tolerance. One of the triggers for the development of both depression and coronary artery disease is usually a stressful event, individually significant, strong enough to stress the nervous regulation of the cardiovascular system. Then there are pathological changes in the hippocampus (the part of the brain responsible for emotions, memory), an increase in the activity of the coagulation system, an increase in cholesterol, and heart rhythm disturbance.
Then there are pathological changes in the hippocampus (the part of the brain responsible for emotions, memory), an increase in the activity of the coagulation system, an increase in cholesterol, and heart rhythm disturbance.
It is believed that these diseases are related at the biological level (genes that are common for the development of coronary artery disease and depression have been identified, there are also studies of twins confirming the relationship of their origin). Depression is often combined with anxiety and can be detected in half of patients with chronic coronary heart disease, and severe depressive disorders that require antidepressant therapy are found in every fourth patient with coronary artery disease. Then consultation of the psychotherapist or the psychiatrist is necessary.
You must know that the sensations you are currently experiencing will end. They are a manifestation of an anxious or depressive state, and not a heart disease. You can learn to listen to body signals, control your well-being and symptoms. It takes some time and some effort to feel the improvement.
It takes some time and some effort to feel the improvement.
Be healthy and happy!
The role of anxiety disorders in hypertension and the possibility of their correction | #03/07
In recent years, more and more evidence has been accumulating that anxiety and some other psychopathological conditions are independent risk factors for the development of arterial hypertension (AH) and should be considered in conjunction with recognized risk factors [7]. These pathologies increase morbidity and mortality from hypertension and coronary heart disease (CHD) [2]. Anxiety disorder should be detected and treated in a timely manner, as it worsens the prognosis of somatic pathology [1]. The importance of anxiety disorder in cardiology is confirmed by the results of a prospective 32-year study conducted in the United States by the Centers for Disease Control and Prevention [7], which showed that with increased anxiety, the probability of fatal myocardial infarction increases by 1. 9times, sudden death - 4.5 times. At the same time, social epidemiological studies using objective methods conducted at the State Research Center for Preventive Medicine showed that the population experienced an increase in the level of psychological stress. It was found that about 70% of the country's population lives in conditions of chronic high- and medium-level psychosocial stress [3].
9times, sudden death - 4.5 times. At the same time, social epidemiological studies using objective methods conducted at the State Research Center for Preventive Medicine showed that the population experienced an increase in the level of psychological stress. It was found that about 70% of the country's population lives in conditions of chronic high- and medium-level psychosocial stress [3].
In this regard, special attention is paid to the study of the role of anxiety in the development of hypertension, one of the main risk factors for coronary artery disease. It is known that hypertension is one of the most common cardiovascular diseases affecting, in particular, 25–35% of the Russian population. Assumptions that affective disorders, most often anxiety and depression, occupy an important place in the development and course of hypertension, were expressed at the beginning of the last century. Currently, work on the study of the relationship between hypertension and affective disorders is carried out in two directions.
On the one hand, the results of large studies have been published demonstrating the relationship between symptoms of anxiety or depression and the development of hypertension, on the other hand, hypertension is considered as a psychosomatic disease, in the treatment of which psychotropic drugs play a very important role [4].
According to the literature, the prevalence of neurotic and somatoform disorders with anxiety symptoms in patients with hypertension can reach 51.3% [2, 5]. However, the number of studies is limited, and there are no clear recommendations for the management of such patients. It is known that comorbid anxiety-depressive disorders, like hypertension, in themselves lead to a significant decrease in working capacity, while they aggravate the course of a somatic disease, contribute to the formation of a hypochondriacal type of internal disease [7]. In this regard, it seems very interesting and important to determine the possibility of the effect of complex therapy with antihypertensive drugs and a “daytime” anxiolytic on the course of hypertension in patients with anxiety.
Anxiolytic therapy significantly improves the quality of life of patients with cardiovascular diseases, contributes to their better compensation in the process of somatotropic therapy, and further adaptation to the disease. Tranquilizers are the most adequate, effective and safe drugs for the relief of adaptation disorders in cardiac patients [2, 3]. However, patients often avoid taking benzodiazepines, fearing the development of addiction symptoms, unpleasant side effects in the form of lethargy, muscle weakness, and impaired attention. Elderly patients often fear the development of coordination disorders in them due to the fear of falling, the appearance of instability.
Taking into account the noted problems, in recent years there has been an increasing need for drugs with a tranquilizing effect of the non-benzodiazepine series. These drugs include Tenoten.
The drug Tenoten is an ultra-low dose (ULD) to the brain-specific protein S100. The mechanisms of action of anti-S100 SMD in anxiety states are probably associated with a modification of the functional activity of the endogenous S100 protein and its ligands. As a result, its GABA-mimetic effect is realized, restoration of GABAergic neurotransmission. The clinical effect in this case is manifested by facilitating falling asleep, reducing behavioral manifestations of anxiety, improving memory, and reducing asthenia.
As a result, its GABA-mimetic effect is realized, restoration of GABAergic neurotransmission. The clinical effect in this case is manifested by facilitating falling asleep, reducing behavioral manifestations of anxiety, improving memory, and reducing asthenia.
The aim of the study was to evaluate the efficacy and tolerability of combined treatment with antihypertensive drugs and the anti-anxiety drug Tenoten in patients with hypertension. The duration of the study is 4 weeks.
The study involved 60 patients with hypertension aged 61.41 ± 6.91 years (from 38 to 77 years). Patients were divided randomly into two groups (main and control) of 30 people. There were 18 men and 12 women in the main group, 19 in the comparison group.men and 11 women.
AH in the main group with a moderate course (II degree) was observed in 60% of patients, with a severe course (III degree) - in 40%; in the comparison group, there were 66.6% of patients with a moderate course, and 33. 4% with a severe course. The average duration of AH disease was 10.61 ± 4.1 years (from 3 to 20 years).
4% with a severe course. The average duration of AH disease was 10.61 ± 4.1 years (from 3 to 20 years).
Of great importance in the course of hypertension is a family history, lifestyle, risk factors and comorbidities.
Persons with symptomatic hypertension and complicated forms of hypertension were excluded from the study.
In the comparison group, patients received only antihypertensive therapy - ACE inhibitors, β-blockers, diuretics (Enap, Hypothiazid, Acridilol, Arifon). Patients of the main group received combined treatment with antihypertensive drugs in combination with Tenoten, which was prescribed according to the scheme: 6 tablets per day for the first 2 weeks, and then 1 tablet 3 times a day.
Treatment was prescribed for a month. Monitoring in dynamics was carried out at the beginning of the study, after 2 and 4 weeks of therapy.
The personal anxiety scale (J. Teylor) was used to assess the mental status, which is designed to measure the level of anxiety (adapted by T. A. Nemchininov).
A. Nemchininov).
The questionnaire consists of 50 statements. Evaluation of the results of the study is carried out by counting the number of responses of the subject, indicating anxiety; the total score is:
40-50 points - an indicator of a very high level of anxiety;
20-40 points - high level of anxiety;
15-20 points - average level of anxiety with a tendency to high;
5-15 points - average level of anxiety with a tendency to low;
0-5 points - low level of anxiety.
A study of the mental status of patients in both groups revealed anxiety symptoms of varying severity in a significant proportion of patients. The number of patients with an initial high level of anxiety was 40% in the main group and 43% in the comparison group. The number of patients with an initial average level of anxiety with a tendency to high was 60% in the main group and 56.6% in the comparison group.
Research results
By the end of the study, the high level of anxiety decreased in the main group by 39. 39% and reached the average level of anxiety with a tendency to low, and in the comparison group, the level of anxiety decreased only by 3.6%.
39% and reached the average level of anxiety with a tendency to low, and in the comparison group, the level of anxiety decreased only by 3.6%.
In patients of the main group who took Tenoten, a clear decrease in the level of anxiety was noted already after 2 weeks and by the end of the month it reached significance in comparison with the group of patients who received standard antihypertensive therapy. The relief of affective disorders was accompanied by a decrease in complaints of anxiety, feelings of helplessness, self-doubt, a sense of threatening danger, poor sleep ( tab. 1 ).
The demonstrated differences in the dynamics of anxiety indicators in the studied groups of patients confirmed the possibility of effective correction of these disorders in patients with AH with Tenoten. However, it was extremely interesting to assess whether this therapy and the severity of associated anxiety disorders affect the effectiveness of antihypertensive therapy in general.
A decrease in the values of maximum systolic and diastolic pressure occurred in both studied groups. By the end of the month of treatment, the decrease in blood pressure (BP) reached a statistically significant significance. In the main group of patients who additionally took Tenoten, systolic blood pressure (BP) decreased by 24.28% - almost to the age norm, in the comparison group there was a decrease by 16.48%, i.e. there was some excess of normal values. The decrease in diastolic pressure by the end of the 4th week in the main group (by 17.7%) and in the comparison group (by 5.9%) was also significant ( tab. 2 , 3 ).
The addition of Tenoten to the complex therapy in patients with high and moderate levels of anxiety made it possible to achieve a much more pronounced improvement in blood pressure. Against the background of therapy with Tenoten, a more rapid effect of antihypertensive drugs is observed - after 2 weeks of combined administration of the drug in patients of the main group, blood pressure decreased to the target level, in contrast to the comparison group, where it remained above the target.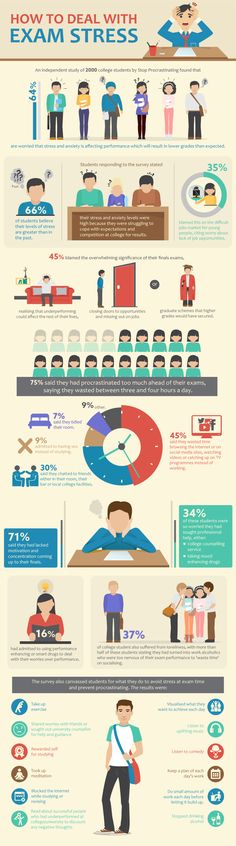
Conclusion
The results of our study show that all patients with hypertension have anxiety symptoms of varying severity, which aggravate the course of the disease, contributing to higher levels of both systolic and diastolic blood pressure. The inclusion of the modern "daytime" anxiolytic Tenoten in the complex therapy of patients with hypertension increases the effectiveness of the treatment, reduces the level of anxiety, which contributes to a more rapid onset of the hypotensive effect. Tenoten is well tolerated by patients, does not cause orthostatic hypotension and any other undesirable side effects.
Literature
- Avedisova AS Anxiety disorders // Yu. A. Aleksandrovsky. Mental disorders in general medical practice and their treatment. M.: GEOTAR-MED, 2004. S. 66–73.
- Kopina O. S., Suslova S. F., Zaikin E. R. Population studies of psychosocial stress as a risk factor for cardiovascular diseases// Cardiology.
 1996. No. 36 (3). pp. 53–56.
1996. No. 36 (3). pp. 53–56. - Sudakov KV Emotional stress and arterial hypertension. M.: VNIIMI, 1976.
- Chazov EI Ischemic heart disease and the possibility of improving the effectiveness of its treatment// Clinical trials of drugs in Russia. 2001. No. 1. S. 2–4.
- Kawachi I., Sparrow D., Vokonas P. S., Wess S. T. Symptoms of anxiety and risk of coronary heart disease. The Normative Aging Study. circulation. 1994; 90, 5: 2225–2229.
- Lavie C., Milani R. Prevalence of anxiety in coronary patients with improvement following cardiac rehabilitation and exercise training. Am J Cardiol. 2004; 93:336–339.
- Sonas B. S., Franks P., Ingram D. D. Are symptoms of anxiety and depression risk factor for hyprtension? Longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Arch. fam. Vtd. 1997; 6:43–9.
I. N. Nikolskaya , Doctor of Medical Sciences, Professor
I.