Safety of zoloft in pregnancy
Antidepressants and Pregnancy: Tips from an Expert
Most pregnant women want to do everything right for their baby, including eating right, exercising regularly and getting good prenatal care. But if you’re one of the many women who have a mood disorder, you might also be trying to manage your psychiatric symptoms as you prepare to welcome your new baby.
It’s common for doctors to tell women with mood disorders to stop taking drugs like antidepressants during pregnancy, leaving many moms-to-be conflicted about giving up the medications that help keep them healthy.
Lauren Osborne, M.D., assistant director of the Johns Hopkins Women’s Mood Disorders Center, talks about why stopping your medication may not be the right approach. She explains how women can — and should — balance their mental health needs with a healthy pregnancy.
Antidepressants and Pregnancy
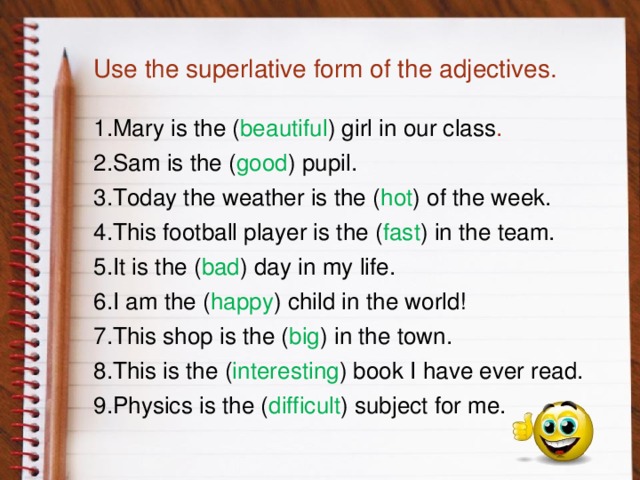
Women who take antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), during pregnancy may worry about whether the medications can cause birth defects.
There is good news on this front. Osborne says that there is generally no need to taper off medications during pregnancy. “We can say with strong confidence that antidepressants don’t cause birth defects,” says Osborne. She adds that most studies finding a physical effect on babies from antidepressants taken during pregnancy fail to account for the effects of the mother’s psychiatric illness.
In fact, untreated mental illness itself poses risks to a developing fetus. A woman who is depressed is less likely to get good prenatal care and more likely to engage in unhealthy or dangerous behaviors, like smoking and substance abuse. Osborne also says mental illness has direct effects on newborn babies.
“Untreated depression may increase preterm birth or cause low birth weight,” she says. “Babies of depressed moms have higher levels of a hormone called cortisol. This raises a baby’s risk of developing depression, anxiety and behavioral disorders later in life.”
Weighing the Risks
While doctors don’t believe antidepressants cause birth defects, it’s still possible for them to affect the baby. It’s important for a mother and her doctor to know the risks.
It’s important for a mother and her doctor to know the risks.
About 30 percent of babies whose mothers take SSRIs will experience neonatal adaptation syndrome, which can cause increased jitteriness, irritability and respiratory distress (difficulty breathing), among other symptoms. Doctors aren’t sure whether this effect is due to the baby’s withdrawal from the SSRI after birth or exposure to the drug itself before birth.
“It may be distressing and cause pediatricians to run tests, but it will go away,” says Osborne, pointing out that these symptoms also sometimes occur in babies whose mothers don’t take SSRIs.
Common medications women frequently ask about include:
- SSRIs: Some studies link SSRI use with a very rare defect called persistent pulmonary hypertension, which is a condition where babies’ lungs don’t inflate well. “The most recent study looked at 3.8 million women and showed there was no increase in risk to their babies,” says Osborne.

- Paroxetine: Early studies on a small number of patients connected the SSRI paroxetine with cardiac defects in babies. However, these studies didn’t account for smoking, obesity and other risk factors that are more common in women who have depression. Osborne says larger, more recent studies show no such link with cardiac defects. She doesn’t recommend switching medications if paroxetine is the only one that works for you.
- Benzodiazepines: Women should avoid using tranquilizers, such as diazepam, alprazolam and clonazepam, in high doses during pregnancy because they can lead to sedation and respiratory distress in the newborn. You can still use them in small doses for short periods of time. However, Osborne will typically try to get mothers on intermediate-acting options like lorazepam. These medications don’t linger in the baby’s bloodstream like longer-acting forms and aren’t associated with high rates of abuse like shorter-acting forms.

- Valproic acid: This medication treats seizures and bipolar disorder, and does carry significant risk to a developing fetus. Taking valproic acid during pregnancy carries a 10 percent risk of neural tube defects — birth defects that affect the brain or spinal cord, such as spina bifida — as well as risks to the baby’s cognitive development, such as lower IQ. “Valproic acid is the only one I’d never prescribe for pregnant women unless all other treatment had failed,” says Osborne .
Seeing a Reproductive Psychiatrist
If you have a mood disorder, you may benefit from speaking with a reproductive psychiatrist when you are pregnant or thinking about becoming pregnant. Ideally, this should happen when you are planning for pregnancy, although this isn’t always possible. Meeting with a doctor after you become pregnant is not too late.
Osborne says her approach with patients is to limit the number of potentially harmful exposures to the baby.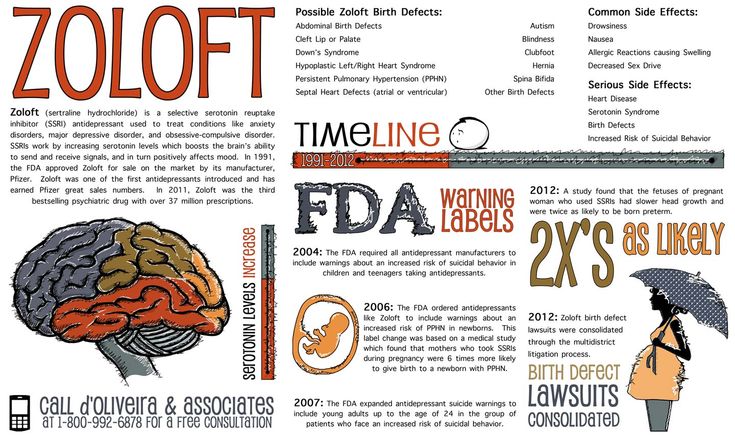 This means considering the number of medications a mother is on, as well as her psychiatric illness.
This means considering the number of medications a mother is on, as well as her psychiatric illness.
“If a woman takes a low dose of many medications and we have time to plan, we’ll try to get that down to a higher dose of fewer medications,” she says. “If a woman is on a low dose and it’s not controlling her illness, then her baby is exposed to both the medication and the illness. In that case, I would increase the medication dosage so her baby isn’t exposed to the illness.”
If your illness is mild, your doctor might recommend getting off medication and replacing it with treatments such as psychotherapy, prenatal yoga or acupuncture to improve your mood.
Ultimately, Osborne says women should weigh the risks of medication against the risk of untreated illness.
“If a particular side effect is extremely rare, it’s still a very rare event even if you double the risk,” she says. Medication risks are typically not greater than those of untreated mental illness. “Switching a woman’s medication is something I do very carefully and reluctantly. ”
”
Everything You Need To Know- K Health
Zoloft, the brand name of the generic medication sertraline, is a commonly prescribed antidepressant medication.
While many medications used for treating major depressive disorder are not safe for pregnancy, Zoloft is one of the few that may be continued under certain circumstances.
It is also one of the safest options to take when breastfeeding.
Zoloft is a selective serotonin reuptake inhibitor (SSRI) that works by preventing the brain from clearing serotonin, which helps to stabilize levels and alleviate symptoms of depression.
In this article we’ll explore Zoloft use during pregnancy and how to know what to expect.
While not every doctor will recommend Zoloft use during pregnancy, in some cases the benefits outweigh the potential risks.
This article will explain common dosages, potential side effects, drug interactions, and how to know when you should see a doctor.
Is It Safe To Take Zoloft During Pregnancy?
Taking an antidepressant like Zoloft during pregnancy is not fully risk-free.
However, the American College of Obstetricians and Gynecologists (ACOG) considers untreated depression during pregnancy to be risky for both the pregnant person and the baby.
Untreated depression during pregnancy can cause complications such as:
- Fetal growth problems
- Premature birth
- Low birth weight
- Postpartum complications in the parent
- Post-birth complications such as developmental delays in the baby
Among antidepressant options, Zoloft (sertraline) is considered to be one of the safest for pregnancy.
But there are still potential risks, and a patient should make the decision to continue Zoloft during pregnancy after considering risks versus benefits with their healthcare team.
Zoloft use in the first trimester was associated with an increased risk for cardiovascular malformations in the infant.
Other congenital anomalies were not significantly associated with Zoloft.
A Centers for Disease Control and Prevention (CDC) study did not find any link between birth defects and taking sertraline during pregnancy.
A slightly increased risk was observed with other types of selective serotonin reuptake inhibitors, such as paroxetine and fluoxetine.
There are other risks when it comes to taking Zoloft or any other SSRI during pregnancy.
Third trimester use may include a higher level of post-birth symptoms such as:
- Low blood sugar
- Jittering and irritability
- Delayed feeding ability
- Hyperactive reflexes
- Vomiting
- Seizures
- Respiratory distress
Only your healthcare provider and you can determine whether Zoloft is safe to continue for your pregnancy.
Do not suddenly stop taking Zoloft without first discussing this with your healthcare provider.
Should you stop taking Zoloft if you find out you’re pregnant?
If you find out that you are pregnant and you are currently taking Zoloft or any other antidepressant medication, let your healthcare provider know immediately.
Zoloft should not be suddenly discontinued due to fear of miscarriage.
A study that compared people taking SSRIs during early pregnancy to those who stopped taking SSRIs before pregnancy found that both groups had a similar miscarriage risk.
Discontinuing Zoloft if you find out you are pregnant will not impact miscarriage risk.
If you take Zoloft and want to discontinue use during pregnancy, work with your healthcare provider to taper your dose.
Antidepressants should not be suddenly stopped.
This can lead to serious adverse effects or withdrawal symptoms.
A medical provider can help you understand the risks versus benefits of discontinuing or taking Zoloft during pregnancy.
Pregnancy can increase the risk of anxiety or depression, and a pregnant person’s mental health can play a major role in pregnancy outcomes.
Common Dosage
Zoloft is available in 25, 50, and 100 mg tablets.
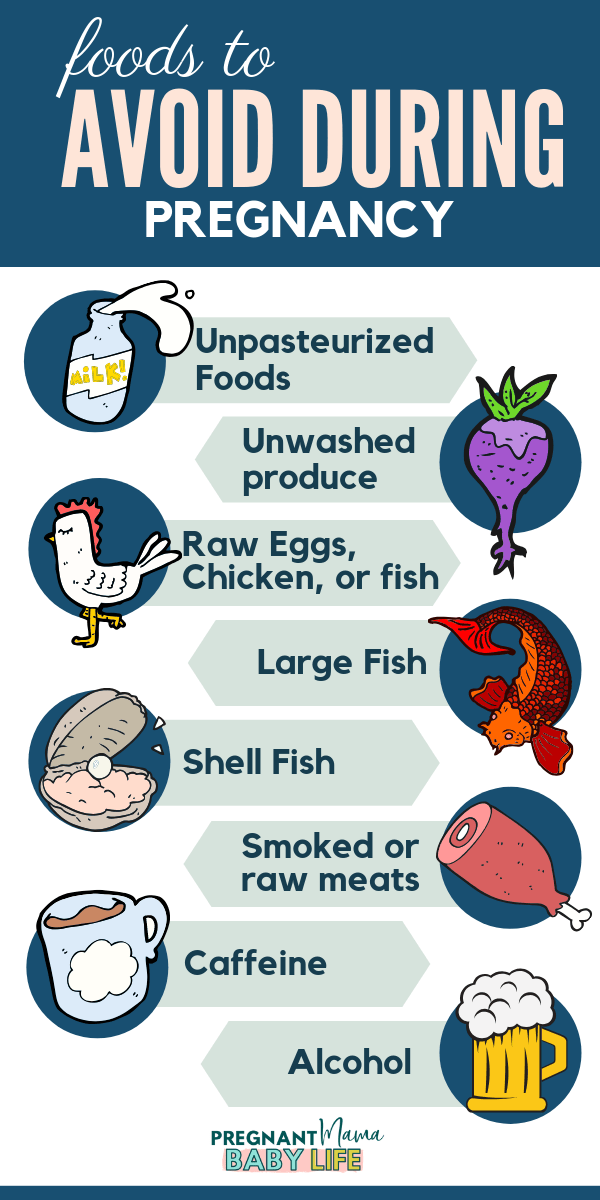
It is also available as an oral solution, though this form of the medication contains 12% alcohol and should not be used during pregnancy.
For pregnancy, the lowest effective dose of Zoloft should be used.
Dosages may start at 25-50 mg per day.
Is It Safe to Take Zoloft While Breastfeeding?
It is generally considered to be safe to take or continue taking Zoloft while breastfeeding.
A small amount of Zoloft may be able to pass into breast milk, but the risk for this SSRI is minimal compared to other antidepressants.
Because of this low risk, Zoloft is often a first choice for medical providers who are treating depression in postpartum people.
Side Effects
Zoloft may cause some common side effects.
Any symptoms associated with taking Zoloft should be reported to a medical provider.
Common Side Effects
Common side effects associated with Zoloft can include:
- Lightheadedness, dizziness, or fainting
- Nausea
- Diarrhea
- Sweating
- Dry mouth
- Fatigue
- Female sexual dysfunction
More Serious Side Effects
Less commonly, Zoloft may cause more serious side effects.
These can include confusion, hallucinations, and tremors.
Also, Zoloft carries a “black box warning” due to the increased suicide risk it may cause in children, adolescents, and young adults with major depression or other psychiatric disorders who take this medication.
If you notice any of the following symptoms, let a healthcare provider know immediately:
- Increased or worsening anxiety or agitation
- Aggression or hostility
- Panic attacks
- Insomnia
- Unusual changes in behavior or impulse control
- Restlessness or manic behavior
- Thoughts of suicide or self-harm
Drug Interactions
Zoloft can interact with many medications.
These interactions may increase the risk of serious side effects while taking Zoloft.
It’s important that you let your healthcare provider know if you take any other prescription medications, OTC medications, vitamins, herbal supplements, or anything else before starting Zoloft.
What to Avoid
You should not take Zoloft if you also take, or have recently taken:
- Monoamine oxidase inhibitors (MAOIs)
- St. John’s wort
- Eliglustat
- Flibanserin
- Isocarboxazid
- Lomitapide
- Phenelzine
- Pimozide
- Procarbazine
- Selegiline
- Thioridazine
- Tranylcypromine
Other Antidepressants That Are Safe for Pregnancy
Sertraline (Zoloft) is considered to be one of the safest options for use during pregnancy.
Certain other antidepressants may be prescribed during or after pregnancy, including:
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
There are risks associated with many medications during pregnancy.
However, your healthcare provider will discuss risks, benefits, and the effects of different medications.
You and your provider will work together to make the safest choice for you and your baby.
When to See a Doctor
IIf you take Zoloft or other antidepressant medications, see your doctor if you are thinking of becoming pregnant or find out that you are pregnant.
Some antidepressants carry a much higher risk during pregnancy than others.
Your healthcare provider may recommend switching medications or decreasing dosage.
You should never decrease your dose or stop taking any antidepressants suddenly without talking to your provider, since this could lead to serious side effects or withdrawal.
If you are pregnant and experiencing symptoms of depression, speak to a healthcare provider.
Treating depression during pregnancy can help to avoid certain complications before and after birth.
How K Health Can Help
Did you know you can get affordable primary care with the K Health app?
Download K to check your symptoms, explore conditions and treatments, and if needed text with a doctor in minutes. K Health’s AI-powered app is HIPAA compliant and based on 20 years of clinical data.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
K Health has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
-
Depression. (n.d.).
https://www.acog.org/en/Womens%20Health/FAQs/Depression -
Depression during pregnancy.
 (2015).
(2015).
https://pubmed.ncbi.nlm.nih.gov/25976080/ -
Sertraline. (2022).
https://medlineplus.gov/druginfo/meds/a697048.html -
Sertraline use in the first trimester and risk of congenital anomalies: a systemic review and meta-analysis of cohort studies.
 (2017).
(2017).
https://pubmed.ncbi.nlm.nih.gov/27770542/ -
Specific SSRIs and birth defects: bayesian analysis to interpret new data in the context of previous reports. (2015).
https://www.bmj.com/content/351/bmj.h4190 -
Prenatal Antidepressant Use and Risk of Adverse Neonatal Outcomes.
 (2020).
(2020).
https://publications.aap.org/pediatrics/article/146/1/e20192493/77032/Prenatal-Antidepressant-Use-and-Risk-of-Adverse -
Treatment with selective serotonin reuptake inhibitors in the third trimester of pregnancy: effects on the infant. (2005).
https://pubmed.ncbi.nlm.nih.gov/15963005/ -
Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage.
 (2014).
(2014).
https://pubmed.ncbi.nlm.nih.gov/25198261/ -
Zoloft (sertraline hydrochloride). (2016).
https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/019839S74S86S87_20990S35S44S45lbl.pdf -
Sertraline and Breastfeeding: Review and Meta-Analysis.
 (2016).
(2016).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4366287/ -
Sertraline. (2022).
https://www.ncbi.nlm.nih.gov/books/NBK547689/
FGBNU NTsPZ. ‹‹Depression in General Medicine: A Guide for Physicians››
The choice between the need for pharmacotherapy, on the one hand, and the prevention of risks to the health of the fetus or newborn (the risk of congenital malformations, pre- and neonatal complications, etc.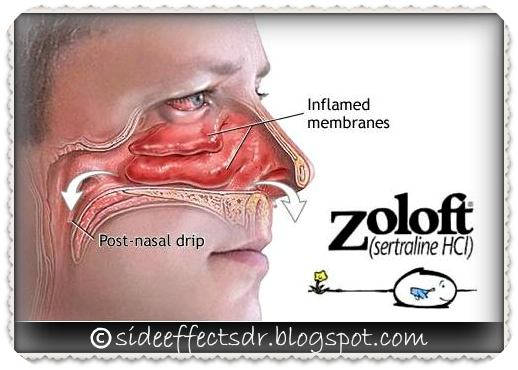 ) on the other, is required from the doctor in case of depression that manifests or worsens during the period pregnancy.
) on the other, is required from the doctor in case of depression that manifests or worsens during the period pregnancy.
When deciding on such an alternative (the proportion of benefit to the mother and the potential risk to the child), a number of circumstances are taken into account, including the possibility of a negative impact on the development of the fetus by the mother's severe mental state during pregnancy.
Psychotropic drugs for pregnant women are prescribed if absolutely necessary according to strict clinical indications:
- with pronounced affective manifestations with anxiety, agitation, sleep and appetite disorders, aggravating the somatic condition of pregnant women and women in childbirth;
- with suicidal thoughts and tendencies.
However, in some cases, such as unplanned pregnancy, antidepressants are taken out of ignorance - a depressed woman, not yet aware of the pregnancy, may continue to take psychotropic drugs and be exposed to them.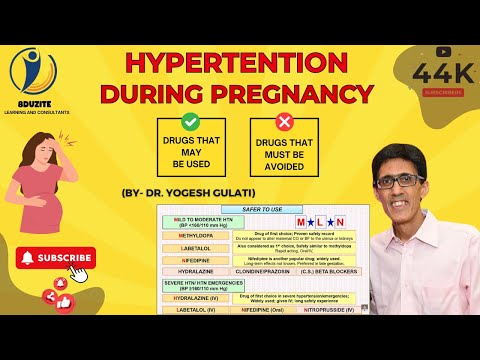
Penetrating through the placenta or with mother's milk, psychotropic drugs can have an adverse effect on the fetus or newborn. Microsomal enzymes of the fetal liver are less active and are in a lower concentration compared to the liver of adults, which prolongs and enhances the effect of drugs. In the prenatal period, the blood-brain barrier is not yet fully formed and the immature CNS is generally more sensitive to the action of drugs. At the stage of embryogenesis, as well as in the early postnatal (neonatal) period of ontogenesis, the development of these vital structures is not completed, which can enhance the toxic effect of psychotropic drugs on both the fetus and the newborn. Such effects include potentially reversible, dose-dependent effects that may be exacerbated by the fact that metabolic systems have not yet fully formed. The constant use of drugs by a pregnant woman can lead to drug dependence of the fetus and, ultimately, to a withdrawal syndrome in the newborn [Vybornykh D. E., 1996].
E., 1996].
During lactation, taking antidepressants due to the possibility of the neonatal complications listed above is also highly undesirable. The mother should be convinced that in this situation it is more appropriate to feed with donor milk or artificial mixtures.
Differentiation of antidepressants in accordance with the degree of risk of developing toxic effects for infants fed by a mother taking psychotropic drugs of this class is shown in Table. 16.
Table 16. Risk of developing toxic effects in children breastfed by mothers taking antidepressants
| Level of risk | ||
| short | average | high |
| Mianserin | SSRI | Doxepin |
| TCAs (majority) | ||
When deciding on the use of antidepressants during pregnancy, it is necessary to take into account data on the risk of teratogenic effects of antidepressants.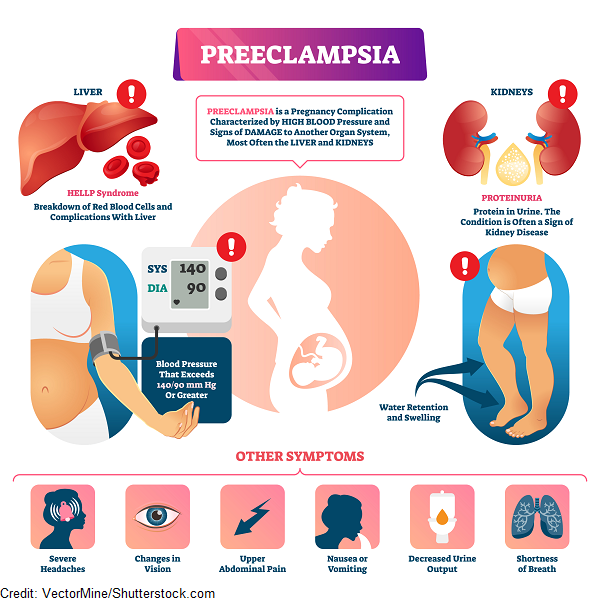 The teratogenic effects of antidepressants cannot be completely ruled out from laboratory animal data and some very limited clinical observations.
The teratogenic effects of antidepressants cannot be completely ruled out from laboratory animal data and some very limited clinical observations.
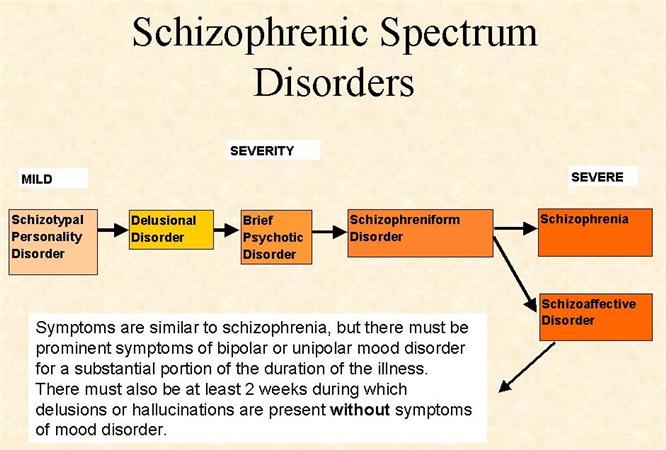
There are 3 classes of teratogenicity of psychotropic drugs: class A - no teratogenicity in animals, no studies of the risk of teratogenicity in humans, or teratogenicity in animals has been established, but not in humans;
class B - known to be teratogenic in animals, no risk of teratogenicity in humans, or no risk of teratogenicity in animals or humans;
class B - teratogenicity has been proven, but the benefits associated with prescribing drugs sometimes outweigh the risks (eg, in a life-threatening situation).
The distribution of drugs by teratogenicity classes is presented in Table. 17. Data are given for the first trimester of pregnancy.
Table 17. Distribution of psychotropic drugs by teratogenicity class Psychotropic Drug Directory, 1997]
| Teratogenic class | ||
| BUT | B | AT |
| SSRIs: fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft) | TCAs: imipramine (melipramine), clomipramine (anafranil), desipramine (petylyl), doxepin (sinequan) | TCAs: amitriptyline, nortriptyline |
| Tranquilizers: chlordiazepoxide (Elenium), alprazolam (Xanax), diazepam (Relanium), lorazepam (Ativan), oxazepam (Nozepam) | ||
| Antipsychotics: butyrophenone and phenothiazine derivatives, risperidone | ||
| SSOZS: tianeptine (coaxil)* | Normotimics: lithium preparations | |
| Tranquilizers: clonazepam (antelepsin) | ||
| Antipsychotics: clozapine (azaleptin) | ||
* Due to lack of human teratogenicity data, not recommended for use during pregnancy .
In this aspect, in the treatment of pregnant and lactating mothers, drugs of the group of irreversible MAOIs should be abandoned first of all.
These data show that the risk of a teratogenic effect is minimal with the use of class A drugs. Not found. The results of a meta-analysis, combining a large amount of information, indicate the safety of fluoxetine for intrauterine development of the fetus. Accordingly, the fact of exposure to fluoxetine does not require the termination of psychopharmacological therapy or termination of pregnancy [Addis A., Koren G., 2000]. Some reports, however, indicate that women treated with fluoxetine and TCAs were more likely than in the control group (6.8%) to have spontaneous abortions (13.5 and 12.2%, respectively) [Stokes P. S. , Holtz A., 1997].
According to preliminary data from a 12-month follow-up observation of children whose mothers took SSRIs (fluoxetine, fluvoxamine, sertraline) during pregnancy or lactation, no adverse effects on the development of the child were registered [Stowe Z. N., 1995; Winn, 1995; Stowe Z. N., Nemeroff S. V., 1996; Yoshida K. et al., 1997; Piontek C. M., 2001].
N., 1995; Winn, 1995; Stowe Z. N., Nemeroff S. V., 1996; Yoshida K. et al., 1997; Piontek C. M., 2001].
The introduction of class B drugs: melipramine-imipramine, anafranil-clomipramine, doxepin-sinequan in animal experiments at doses many times higher than those used in clinical practice may be accompanied by a teratogenic effect. At the same time, at the clinical level, there are currently no convincing data on an increased risk of defects in the embryonic development of the fetus due to the use of these drugs during pregnancy [Puzynski S., 1988]. At the same time, the use of TCAs classified as class B, , i.e., drugs with proven teratogenicity (amitriptyline, nortriptyline), requires special care (justified only in extreme, life-threatening situations for the patient) due to the threat of fetal developmental disorders .
Of great importance for successful therapy is the early detection of depression that manifests during pregnancy. Thanks to this, it is possible to carry out sparing psychopharmacotherapy - the relief of affective disorders at a still undeveloped stage with the help of low doses of medications in short courses. The use of psychotropic drugs in such cases is also the prevention of postpartum depression.
The use of psychotropic drugs in such cases is also the prevention of postpartum depression.
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Voltaren, KagocelHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year.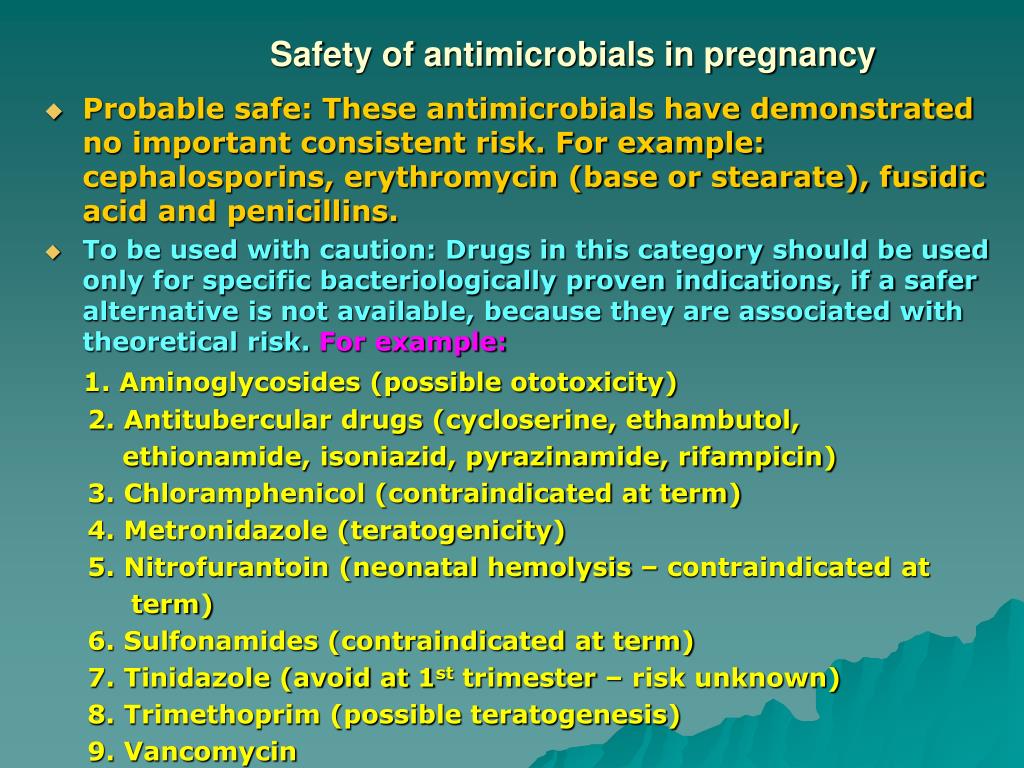 It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to yourself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to yourself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by depression
Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases. Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that the functions of neurotransmitters located in the brain are impaired. These substances transmit signals from neuron to neuron and are responsible for a person's mood. Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is depression treated
Depression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included taking drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive. These are drugs, the action of which is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are drugs, the action of which is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome a dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
You can only take these drugs with a doctor's prescription, as many of them are strong stimulants. Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, should be taken without any gaps or breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors. The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No correlation with blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies for people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Drugs with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
— Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.
Pluses
+ A lasting effect occurs after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
— Anxiety may increase in the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).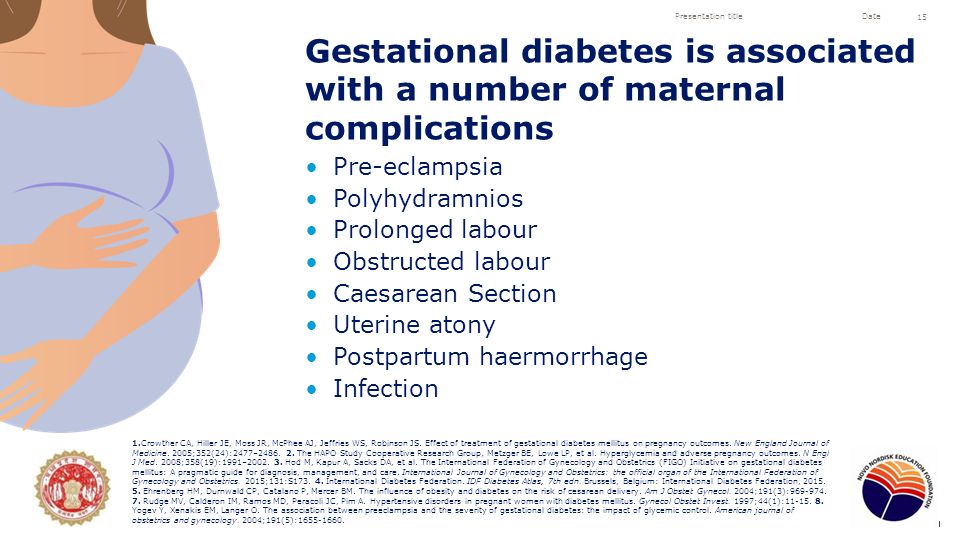
+ Combines well with most drugs in the general group.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the reception period, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
- Gastrointestinal disorders, insomnia, agitation are possible.