Is narcolepsy an autoimmune disease
Narcolepsy confirmed as autoimmune disease
Results also partly explain why the 2009 swine flu virus, and a vaccine against it, led to spikes in the sleep disorder.
Nerve cells (red) that act as receptors for hypocretins, hormones that regulate the sleep cycle, are attacked by the immune system in narcolepsy patients. Credit: C.J.Guerin, MRC Toxicology Unit/ Science Photo Library
As the h2N1 swine flu pandemic swept the world in 2009, China saw a spike in cases of narcolepsy — a mysterious disorder that involves sudden, uncontrollable sleepiness. Meanwhile, in Europe, around 1 in 15,000 children who were given Pandemrix — a now-defunct flu vaccine that contained fragments of the pandemic virus — also developed narcolepsy, a chronic disease.
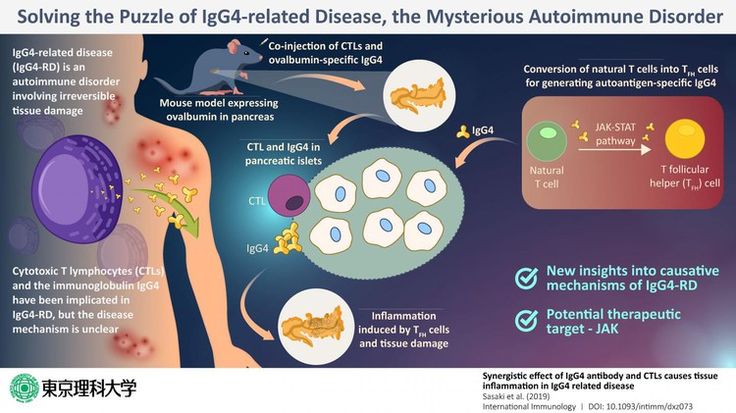
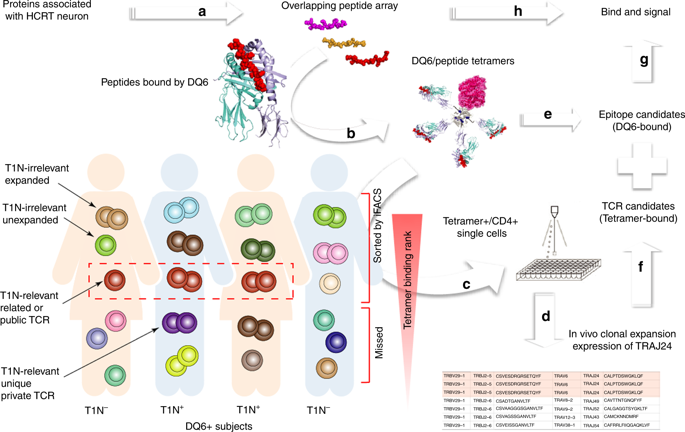
Immunologist Elizabeth Mellins and narcolepsy researcher Emmanuel Mignot at Stanford University School of Medicine in California and their collaborators have now partly solved the mystery behind these events, while also confirming a longstanding hypothesis that narcolepsy is an autoimmune disease, in which the immune system attacks healthy cells.
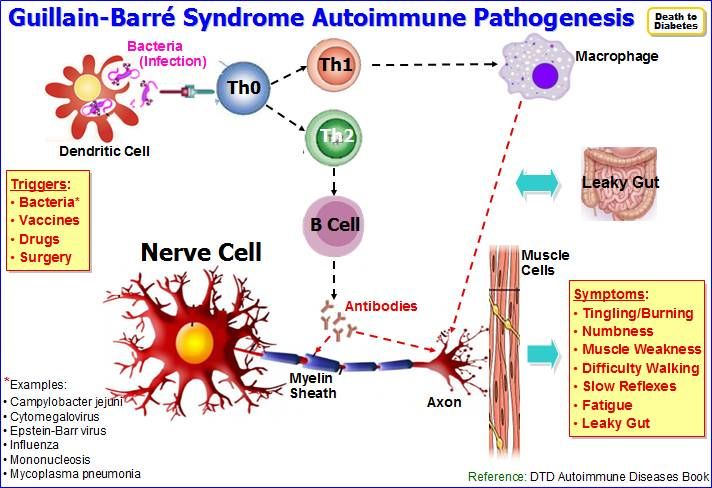
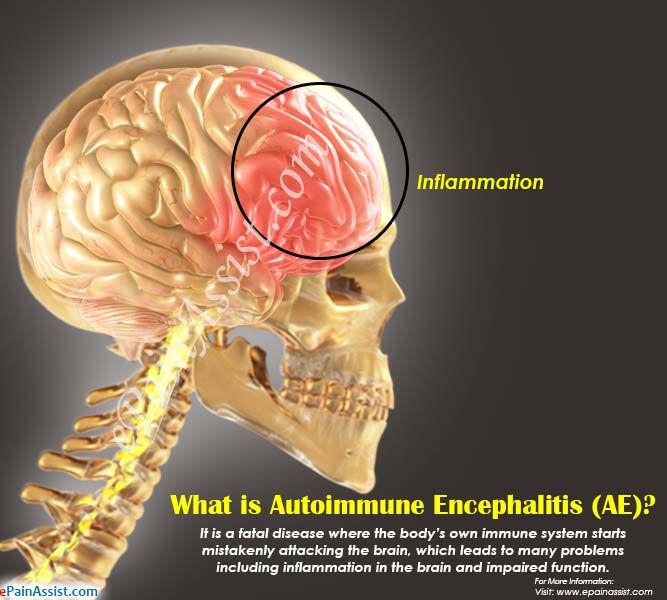
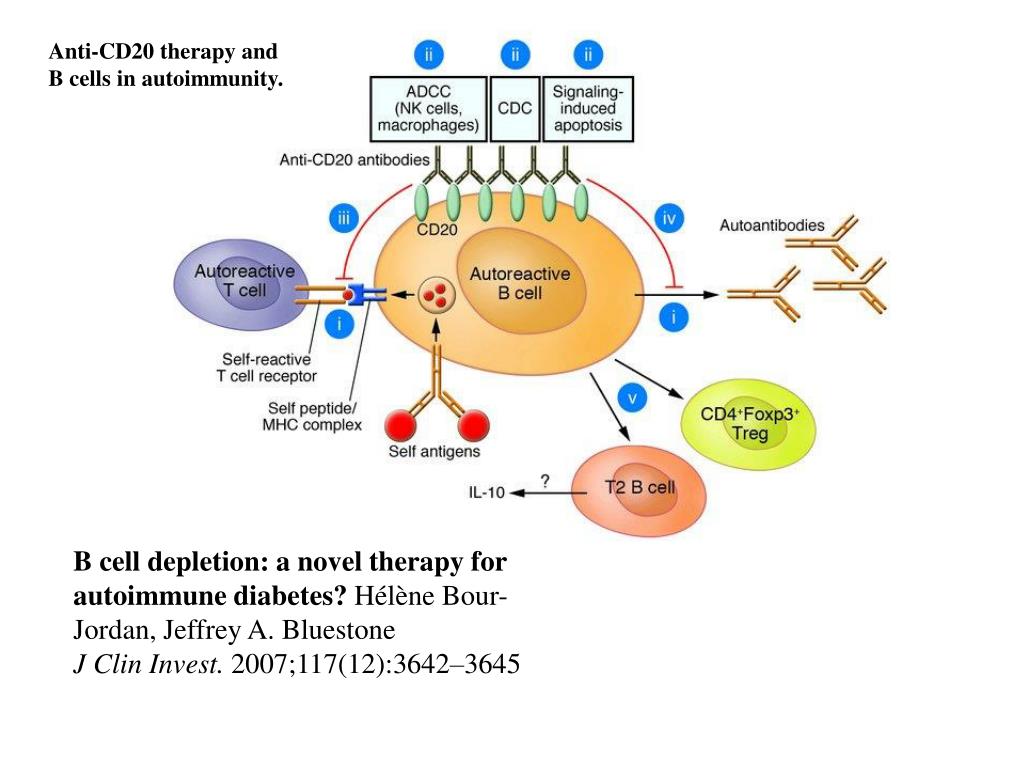
Narcolepsy is mostly caused by the gradual loss of neurons that produce hypocretin, a hormone that keeps us awake. Many scientists had suspected that the immune system was responsible, but the Stanford team has found the first direct evidence: a special group of CD4+ T cells (a type of immune cell) that targets hypocretin and is found only in people with narcolepsy.
“Up till now, the idea that narcolepsy was an autoimmune disorder was a very compelling hypothesis, but this is the first direct evidence of autoimmunity,” says Mellins. “I think these cells are a smoking gun.” The study is published today in Science Translational Medicine1.
Thomas Scammell, a neurologist at Harvard Medical School in Boston, Massachusetts, says that the results are welcome after “years of modest disappointment”, marked by many failures to find antibodies made by a person's body against their own hypocretin. “It’s one of the biggest things to happen in the narcolepsy field for some time.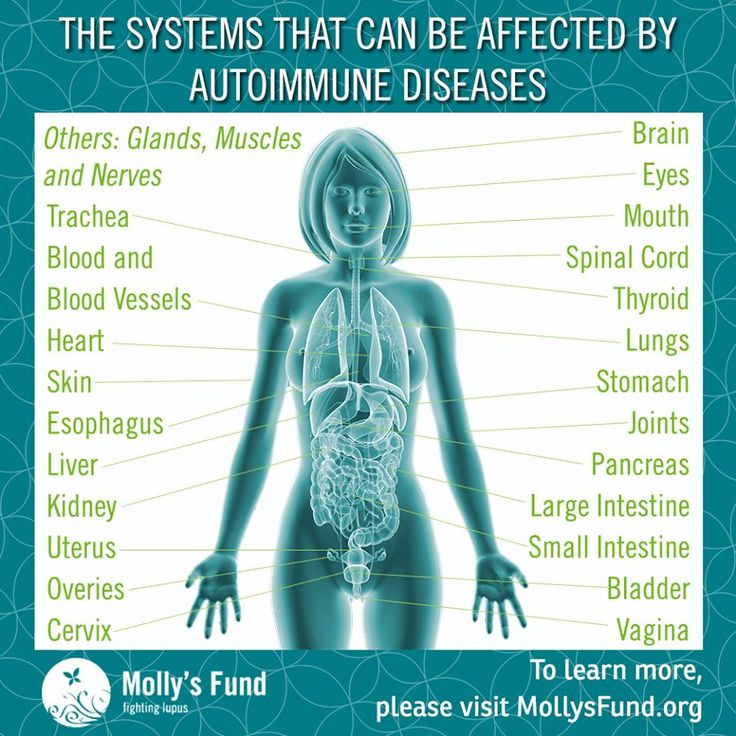 ”
”
Loose ends
It is not clear why some people make these T cells and others do not, but genetics may play a part. In earlier work2, Mignot showed that 98% of people with narcolepsy have a variant of the gene HLA that is found in only 25% of the general population.
Environmental factors, such as infections, probably matter too. Mellins’ working model is that narcolepsy happens when people with a genetic predisposition, which involves having several narcolepsy-related gene variants, encounter an environmental factor that mimics hypocretin, triggering a response from the immune system. The 2009 h2N1 virus was one such trigger: the team found that these same special CD4+ T cells also recognize a protein from the pandemic h2N1 virus.
Narcolepsy of course was around long before the 2009 pandemic. And since new cases of the disease tend to arise right after winter — following the seasonal peak in flu — it's possible that other strains or even other viruses are involved, too.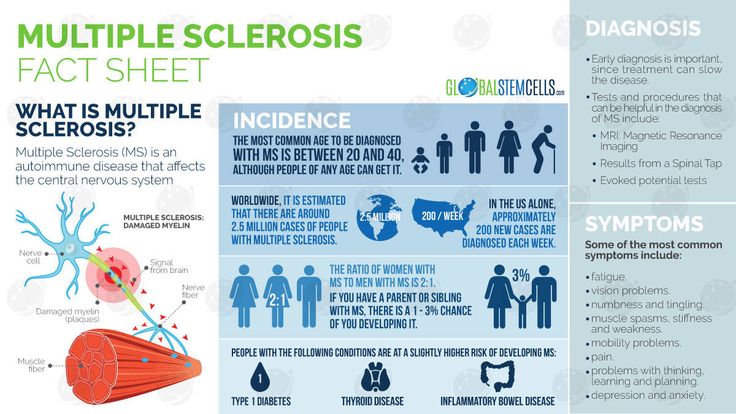
But the results do not fully explain the Pandemrix mystery, because other flu vaccines contained the same proteins but did not lead to a spike in narcolepsy cases. Regardless, Mellins says that it should be possible to avoid repeating the same mistake by ensuring that future flu vaccines do not contain components that resemble hypocretin.
Another loose end is that “they don’t show how these T cells are actually killing the hypocretin neurons”, adds Scammell. “It’s like a murder mystery and we don’t know who the real killer is.” He thinks that it is unlikely that the T cells are the true culprits; instead, they could be acting through an intermediary, or might merely be a symptom of some other destructive event.
“The results are very important, but they need to do a replication study in a large group of patients and controls,” says Gert Lammers, a neurologist at Leiden University Medical Center in the Netherlands and president of the European Narcolepsy Network. “If the findings are confirmed, the first important spin-off might be the development of a new diagnostic test. ”
”
Autoimmunity in narcolepsy - PMC
1. Nishino S, et al. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355(9197):39–40. [PubMed] [Google Scholar]
2. Gautvik KM, et al. Overview of the most prevalent hypothalamus-specific mRNAs, as identified by directional tag PCR subtraction. Proc Natl Acad Sci U S A. 1996;93(16):8733–8. [PMC free article] [PubMed] [Google Scholar]
3. de Lecea L, et al. The hypocretins: hypothalamus-specific peptides with neuroexcitatory activity. Proc Natl Acad Sci U S A. 1998;95(1):322–7. [PMC free article] [PubMed] [Google Scholar]
4. Thannickal TC, et al. Reduced number of hypocretin neurons in human narcolepsy. Neuron. 2000;27(3):469–74. [PMC free article] [PubMed] [Google Scholar]
5. Thannickal TC, Nienhuis R, Siegel JM. Localized loss of hypocretin (orexin) cells in narcolepsy without cataplexy. Sleep. 2009;32(8):993–8. [PMC free article] [PubMed] [Google Scholar]
6. Peyron C, et al. A mutation in a case of early onset narcolepsy and a generalized absence of hypocretin peptides in human narcoleptic brains. Nat Med. 2000;6(9):991–7. [PubMed] [Google Scholar]
Nat Med. 2000;6(9):991–7. [PubMed] [Google Scholar]
7. Juji T, et al. HLA antigens in Japanese patients with narcolepsy. All the patients were DR2 positive. Tissue Antigens. 1984;24(5):316–9. [PubMed] [Google Scholar]
8. Mignot E, et al. Complex HLA-DR and -DQ interactions confer risk of narcolepsy-cataplexy in three ethnic groups. Am J Hum Genet. 2001;68(3):686–99. [PMC free article] [PubMed] [Google Scholar]
9. Han F, et al. Genome wide analysis of narcolepsy in China implicates novel immune loci and reveals changes in association prior to versus after the 2009 h2N1 influenza pandemic. PLoS Genet. 2013;9(10):e1003880. [PMC free article] [PubMed] [Google Scholar]
10. Hor H, et al. Genome-wide association study identifies new HLA class II haplotypes strongly protective against narcolepsy. Nat Genet. 2010;42(9):786–9. [PubMed] [Google Scholar]
11. Faraco J, et al. ImmunoChip study implicates antigen presentation to T cells in narcolepsy. PLoS Genet. 2013;9(2):e1003270.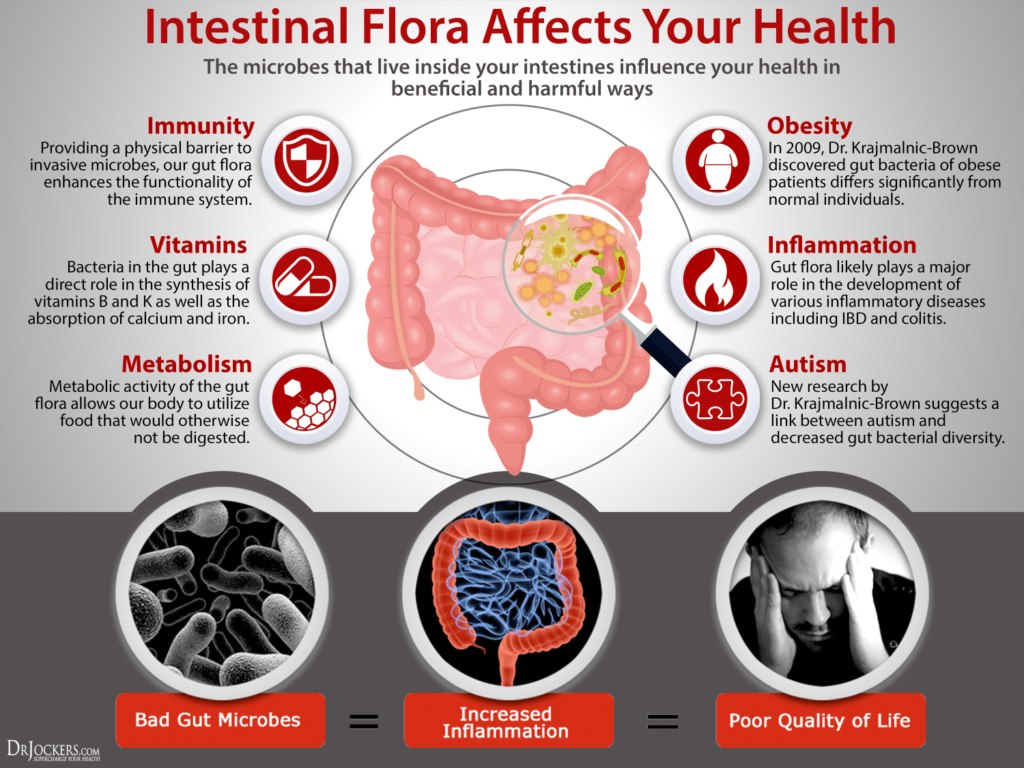 [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
12. Nohynek H, et al. AS03 adjuvanted Ah2N1 vaccine associated with an abrupt increase in the incidence of childhood narcolepsy in Finland. PLoS One. 2012;7(3):e33536. [PMC free article] [PubMed] [Google Scholar]
13. Han F, et al. Narcolepsy onset is seasonal and increased following the 2009 h2N1 pandemic in China. Ann Neurol. 2011;70(3):410–7. [PubMed] [Google Scholar]
14. Silber MH, et al. The epidemiology of narcolepsy in Olmsted County, Minnesota: a population-based study. Sleep. 2002;25(2):197–202. [PubMed] [Google Scholar]
15. Heier MS, et al. Prevalence of narcolepsy with cataplexy in Norway. Acta Neurol Scand. 2009;120(4):276–80. [PubMed] [Google Scholar]
16. Hublin C, et al. Epidemiology of narcolepsy. Sleep. 1994;17(8 Suppl):S7–12. [PubMed] [Google Scholar]
17. Hublin C, et al. The prevalence of narcolepsy: an epidemiological study of the Finnish Twin Cohort. Ann Neurol. 1994;35(6):709–16. [PubMed] [Google Scholar]
18. Ohayon MM, et al. Prevalence of narcolepsy symptomatology and diagnosis in the European general population. Neurology. 2002;58(12):1826–33. [PubMed] [Google Scholar]
Ohayon MM, et al. Prevalence of narcolepsy symptomatology and diagnosis in the European general population. Neurology. 2002;58(12):1826–33. [PubMed] [Google Scholar]
19. Wing YK, et al. The prevalence of narcolepsy among Chinese in Hong Kong. Ann Neurol. 2002;51(5):578–84. [PubMed] [Google Scholar]
20. Shin YK, et al. Prevalence of narcolepsy-cataplexy in Korean adolescents. Acta Neurol Scand. 2008;117(4):273–8. [PubMed] [Google Scholar]
21. Miyagawa T, et al. New susceptibility variants to narcolepsy identified in HLA class II region. Hum Mol Genet. 2015;24(3):891–8. [PubMed] [Google Scholar]
22. Wilner A, et al. Narcolepsy-cataplexy in Israeli Jews is associated exclusively with the HLA DR2 haplotype. A study at the serological and genomic level. Hum Immunol. 1988;21(1):15–22. [PubMed] [Google Scholar]
23. al Rajeh S, et al. A community survey of neurological disorders in Saudi Arabia: the Thugbah study. Neuroepidemiology. 1993;12(3):164–78. [PubMed] [Google Scholar]
24. Tafti M, et al. DQB1 locus alone explains most of the risk and protection in narcolepsy with cataplexy in Europe. Sleep. 2014;37(1):19–25. [PMC free article] [PubMed] [Google Scholar]
Tafti M, et al. DQB1 locus alone explains most of the risk and protection in narcolepsy with cataplexy in Europe. Sleep. 2014;37(1):19–25. [PMC free article] [PubMed] [Google Scholar]
25. Gragert L, et al. Six-locus high resolution HLA haplotype frequencies derived from mixed-resolution DNA typing for the entire US donor registry. Hum Immunol. 2013;74(10):1313–20. [PubMed] [Google Scholar]
26. Maiers M, Gragert L, Klitz W. High-resolution HLA alleles and haplotypes in the United States population. Hum Immunol. 2007;68(9):779–88. [PubMed] [Google Scholar]
27. Mignot E, et al. HLA DQB1*0602 is associated with cataplexy in 509 narcoleptic patients. Sleep. 1997;20(11):1012–20. [PubMed] [Google Scholar]
28. Juji T, et al. Narcolepsy and HLA in the Japanese. Ann N Y Acad Sci. 1988;540:106–14. [PubMed] [Google Scholar]
29. Smith GJ, et al. Origins and evolutionary genomics of the 2009 swine-origin h2N1 influenza A epidemic. Nature. 2009;459(7250):1122–5. [PubMed] [Google Scholar]
30. O’Flanagan D, et al. Investigation of an association between onset of narcolepsy and vaccination with pandemic influenza vaccine, Ireland April 2009–December 2010. Euro Surveill. 2014;19(17):15–25. [PubMed] [Google Scholar]
O’Flanagan D, et al. Investigation of an association between onset of narcolepsy and vaccination with pandemic influenza vaccine, Ireland April 2009–December 2010. Euro Surveill. 2014;19(17):15–25. [PubMed] [Google Scholar]
31. Dauvilliers Y, et al. Increased risk of narcolepsy in children and adults after pandemic h2N1 vaccination in France. Brain. 2013;136(Pt 8):2486–96. [PubMed] [Google Scholar]
32. Heier MS, et al. Incidence of narcolepsy in Norwegian children and adolescents after vaccination against h2N1 influenza A. Sleep Med. 2013;14(9):867–71. [PubMed] [Google Scholar]
33. Miller E, et al. Risk of narcolepsy in children and young people receiving AS03 adjuvanted pandemic A/h2N1 2009 influenza vaccine: retrospective analysis. BMJ. 2013;346:f794. [PubMed] [Google Scholar]
34. Bardage C, et al. Neurological and autoimmune disorders after vaccination against pandemic influenza A (h2N1) with a monovalent adjuvanted vaccine: population based cohort study in Stockholm, Sweden. BMJ. 2011;343:d5956. [PMC free article] [PubMed] [Google Scholar]
BMJ. 2011;343:d5956. [PMC free article] [PubMed] [Google Scholar]
35. Wijnans L, et al. The incidence of narcolepsy in Europe: before, during, and after the influenza A(h2N1)pdm09 pandemic and vaccination campaigns. Vaccine. 2013;31(8):1246–54. [PubMed] [Google Scholar]
36. Tsai TF, et al. Explorations of clinical trials and pharmacovigilance databases of MF59(R)-adjuvanted influenza vaccines for associated cases of narcolepsy. Scand J Infect Dis. 2011;43(9):702–6. [PubMed] [Google Scholar]
37. Kim WJ, et al. Incidence of narcolepsy before and after MF59-adjuvanted influenza A(h2N1)pdm09 vaccination in South Korean soldiers. Vaccine. 2015 [PubMed] [Google Scholar]
38. Duffy J, et al. Narcolepsy and influenza A(h2N1) pandemic 2009 vaccination in the United States. Neurology. 2014;83(20):1823–30. [PMC free article] [PubMed] [Google Scholar]
39. Montplaisir J, et al. Risk of narcolepsy associated with inactivated adjuvanted (AS03) A/h2N1 (2009) pandemic influenza vaccine in Quebec. PLoS One. 2014;9(9):e108489. [PMC free article] [PubMed] [Google Scholar]
PLoS One. 2014;9(9):e108489. [PMC free article] [PubMed] [Google Scholar]
40. Picchioni D, Hope CR, Harsh JR. A case-control study of the environmental risk factors for narcolepsy. Neuroepidemiology. 2007;29(3–4):185–92. [PubMed] [Google Scholar]
41. Aran A, et al. Clinical and therapeutic aspects of childhood narcolepsy-cataplexy: a retrospective study of 51 children. Sleep. 2010;33(11):1457–64. [PMC free article] [PubMed] [Google Scholar]
42** Jacob L, et al. Comparison of Pandemrix and Arepanrix, two ph2N1 AS03-adjuvanted vaccines differentially associated with narcolepsy development. Brain Behav Immun. 2015;47:44–57. This study did a detailed mass spectrometric characterization of influenza vaccines used in 2009 pandemic influenza season. [PubMed] [Google Scholar]
43. Canelle Q, et al. Evaluation of potential immunogenicity differences between Pandemrix and Arepanrix. Hum Vaccin Immunother. 2016;12(9):2289–98. [PMC free article] [PubMed] [Google Scholar]
44. Simmons KM, Michels AW. Type 1 diabetes: A predictable disease. World J Diabetes. 2015;6(3):380–90. [PMC free article] [PubMed] [Google Scholar]
Simmons KM, Michels AW. Type 1 diabetes: A predictable disease. World J Diabetes. 2015;6(3):380–90. [PMC free article] [PubMed] [Google Scholar]
45. du Pre MF, Sollid LM. T-cell and B-cell immunity in celiac disease. Best Pract Res Clin Gastroenterol. 2015;29(3):413–23. [PubMed] [Google Scholar]
46. van der Heide A, et al. Immunohistochemical screening for antibodies in recent onset type 1 narcolepsy and after h2N1 vaccination. J Neuroimmunol. 2015;283:58–62. [PubMed] [Google Scholar]
47. Toyoda H, et al. Anti-Tribbles homolog 2 autoantibodies in Japanese patients with narcolepsy. Sleep. 2010;33(7):875–8. [PMC free article] [PubMed] [Google Scholar]
48. Thebault S, et al. Neuronal Antibodies in Children with or without Narcolepsy following h2N1-AS03 Vaccination. PLoS One. 2015;10(6):e0129555. [PMC free article] [PubMed] [Google Scholar]
49. Tanaka S, et al. Detection of autoantibodies against hypocretin, hcrtrl, and hcrtr2 in narcolepsy: anti-Hcrt system antibody in narcolepsy. Sleep. 2006;29(5):633–8. [PubMed] [Google Scholar]
Sleep. 2006;29(5):633–8. [PubMed] [Google Scholar]
50. Saariaho AH, et al. Autoantibodies against ganglioside GM3 are associated with narcolepsy-cataplexy developing after Pandemrix vaccination against 2009 pandemic h2N1 type influenza virus. J Autoimmun. 2015 [PubMed] [Google Scholar]
51. Melen K, et al. No serological evidence of influenza A h2N1pdm09 virus infection as a contributing factor in childhood narcolepsy after Pandemrix vaccination campaign in Finland. PLoS One. 2013;8(8):e68402. [PMC free article] [PubMed] [Google Scholar]
52. Kornum BR, et al. Cerebrospinal fluid cytokine levels in type 1 narcolepsy patients very close to onset. Brain Behav Immun. 2015 [PMC free article] [PubMed] [Google Scholar]
53. Kawashima M, et al. Anti-Tribbles homolog 2 (TRIB2) autoantibodies in narcolepsy are associated with recent onset of cataplexy. Sleep. 2010;33(7):869–74. [PMC free article] [PubMed] [Google Scholar]
54. Cvetkovic-Lopes V, et al. Elevated Tribbles homolog 2-specific antibody levels in narcolepsy patients. J Clin Invest. 2010;120(3):713–9. [PMC free article] [PubMed] [Google Scholar]
J Clin Invest. 2010;120(3):713–9. [PMC free article] [PubMed] [Google Scholar]
55. Ahmed SS, et al. Antibodies to influenza nucleoprotein cross-react with human hypocretin receptor 2. Sci Transl Med. 2015;7(294):294ra105. [PubMed] [Google Scholar]
56. Lind A, et al. A/h2N1 antibodies and TRIB2 autoantibodies in narcolepsy patients diagnosed in conjunction with the Pandemrix vaccination campaign in Sweden 2009–2010. J Autoimmun. 2014;50:99–106. [PubMed] [Google Scholar]
57. Haggmark-Manberg A, et al. Autoantibody targets in vaccine-associated narcolepsy. Autoimmunity. 2016;49(6):421–433. [PubMed] [Google Scholar]
58. Saariaho AH, et al. Autoantibodies against ganglioside GM3 are associated with narcolepsy-cataplexy developing after Pandemrix vaccination against 2009 pandemic h2N1 type influenza virus. J Autoimmun. 2015;63:68–75. [PubMed] [Google Scholar]
59. Bergman P, et al. Narcolepsy patients have antibodies that stain distinct cell populations in rat brain and influence sleep patterns. Proc Natl Acad Sci U S A. 2014;111(35):E3735–44. [PMC free article] [PubMed] [Google Scholar]
Proc Natl Acad Sci U S A. 2014;111(35):E3735–44. [PMC free article] [PubMed] [Google Scholar]
60. Katzav A, et al. Passive transfer of narcolepsy: anti-TRIB2 autoantibody positive patient IgG causes hypothalamic orexin neuron loss and sleep attacks in mice. J Autoimmun. 2013;45:24–30. [PubMed] [Google Scholar]
61. Dauvilliers Y, et al. Post-h2N1 narcolepsy-cataplexy. Sleep. 2010;33(11):1428–30. [PMC free article] [PubMed] [Google Scholar]
62. Vaarala O, et al. Antigenic differences between AS03 adjuvanted influenza A (h2N1) pandemic vaccines: implications for pandemrix-associated narcolepsy risk. PLoS One. 2014;9(12):e114361. [PMC free article] [PubMed] [Google Scholar]
63. Giannoccaro MP, et al. Antibodies against hypocretin receptor 2 are rare in narcolepsy. Sleep. 2016 [PubMed] [Google Scholar]
64* Ambati A, et al. h2N1 viral proteome peptide microarray predicts individuals at risk for h2N1 infection and segregates infection versus Pandemrix((R)) vaccination.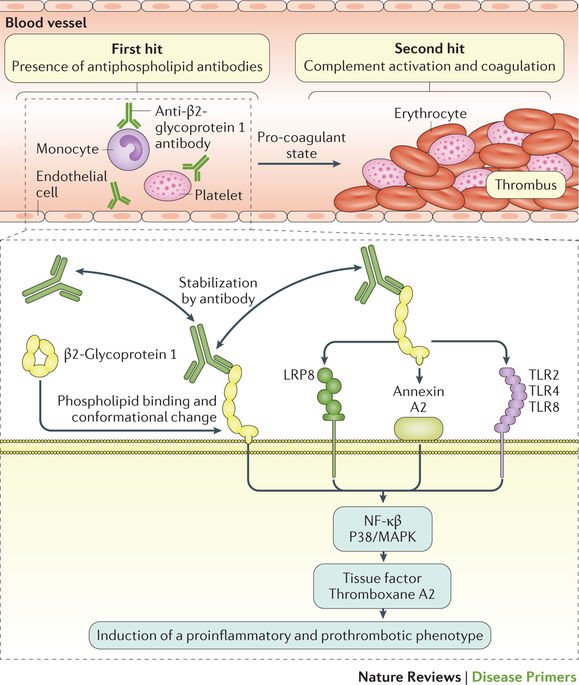 Immunology. 2015;145(3):357–66. first study to report an increased streptococcus specific T-cells in narcolepsy cases. [PMC free article] [PubMed] [Google Scholar]
Immunology. 2015;145(3):357–66. first study to report an increased streptococcus specific T-cells in narcolepsy cases. [PMC free article] [PubMed] [Google Scholar]
65. Zandian A, et al. Whole-Proteome Peptide Microarrays for Profiling Autoantibody Repertoires within Multiple Sclerosis and Narcolepsy. Journal of Proteome Research. 2017;16(3):1300–1314. [PubMed] [Google Scholar]
66. Lecendreux M, et al. Impact of cytokine in type 1 narcolepsy: Role of pandemic h2N1 vaccination ? J Autoimmun. 2015;60:20–31. [PubMed] [Google Scholar]
67. Hallmayer J, et al. Narcolepsy is strongly associated with the T-cell receptor alpha locus. Nat Genet. 2009;41(6):708–11. [PMC free article] [PubMed] [Google Scholar]
68. Roep BO, Kallan AA, De Vries RR. Beta-cell antigen-specific lysis of macrophages by CD4 T-cell clones from newly diagnosed IDDM patient. A putative mechanism of T-cell-mediated autoimmune islet cell destruction. Diabetes. 1992;41(11):1380–4. [PubMed] [Google Scholar]
69. Pelfrey CM, et al. Identification of a novel T cell epitope of human proteolipid protein (residues 40–60) recognized by proliferative and cytolytic CD4+ T cells from multiple sclerosis patients. J Neuroimmunol. 1993;46(1–2):33–42. [PubMed] [Google Scholar]
Pelfrey CM, et al. Identification of a novel T cell epitope of human proteolipid protein (residues 40–60) recognized by proliferative and cytolytic CD4+ T cells from multiple sclerosis patients. J Neuroimmunol. 1993;46(1–2):33–42. [PubMed] [Google Scholar]
70. Williams WV, et al. Restricted heterogeneity of T cell receptor transcripts in rheumatoid synovium. The Journal of Clinical Investigation. 90(2):326–333. [PMC free article] [PubMed] [Google Scholar]
71** Bernard-Valnet R, et al. CD8 T cell-mediated killing of orexinergic neurons induces a narcolepsy-like phenotype in mice. Proceedings of the National Academy of Sciences. 2016;113(39):10956–10961. first report to show increased hypcretin neuron cytotoxicity in a mouse model. [PMC free article] [PubMed] [Google Scholar]
72. Hartmann FJ, et al. High-dimensional single-cell analysis reveals the immune signature of narcolepsy. J Exp Med. 2016;213(12):2621–2633. [PMC free article] [PubMed] [Google Scholar]
73* Ollila HM, et al.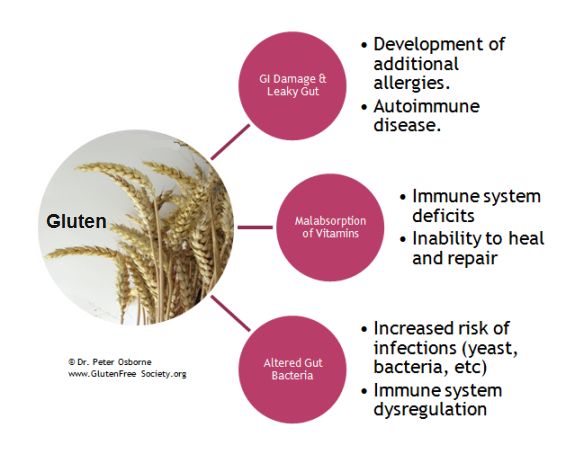 HLA-DPB1 and HLA class I confer risk of and protection from narcolepsy. Am J Hum Genet. 2015;96(1):136–46. one of the first reports to find HLA class 1 associations in narcolepsy cases. [PMC free article] [PubMed] [Google Scholar]
HLA-DPB1 and HLA class I confer risk of and protection from narcolepsy. Am J Hum Genet. 2015;96(1):136–46. one of the first reports to find HLA class 1 associations in narcolepsy cases. [PMC free article] [PubMed] [Google Scholar]
74* Tafti M, et al. Narcolepsy-Associated HLA Class I Alleles Implicate Cell-Mediated Cytotoxicity. Sleep. 2016;39(3):581–7. one of the first reports to find HLA class 1 associations in narcolepsy cases. [PMC free article] [PubMed] [Google Scholar]
75. Han F, et al. TCRA, P2RY11, and CPT1B/CHKB associations in Chinese narcolepsy. Sleep Med. 2012;13(3):269–72. [PMC free article] [PubMed] [Google Scholar]
76* Toyoda H, et al. A polymorphism in CCR1/CCR3 is associated with narcolepsy. Brain Behav Immun. 2015;49:148–55. Finding a novel association with immunogenetic risk factor in narcolepsy. [PubMed] [Google Scholar]
what is it, symptoms, treatment, causes of daytime sleepiness
Font size Color scheme Images
x
Make an appointment
Name* Phone* Adult Child (under 18)x
Sign up for analysis
Name* Telephone* ☆ st.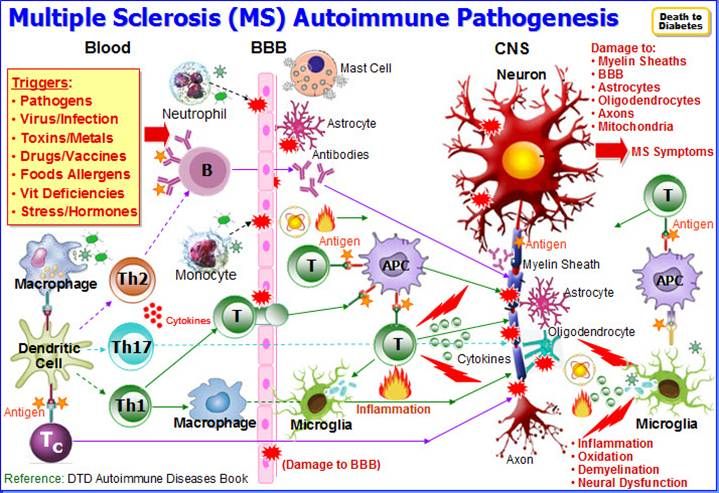 Malaya Balkanskaya, 23 (m. Kupchino)
Malaya Balkanskaya, 23 (m. Kupchino)
Dunaisky ave., 47 (m. Dunayskaya)
Udarnikov ave., 19 (m. Ladozhskaya)
st. Marshala Zakharova, 20 (metro station Leninskiy pr-t)
Vyborgskoe shosse, 17 (metro Prospect of Enlightenment)
- Call
435 55 55 -
Make an appointment
This disease is treated by Somnologist
The information provided on this page should not be used for self-treatment or self-diagnosis. If you suspect a disease, you should seek help from a qualified specialist. Only your doctor can diagnose and prescribe treatment.
Article content:
- Causes
- Symptoms of narcolepsy
- Diagnostics
- Narcolepsy treatment
- Prognosis and prevention
What is narcolepsy?
Narcolepsy is a pathological condition characterized by an inability to control sleep and wakefulness.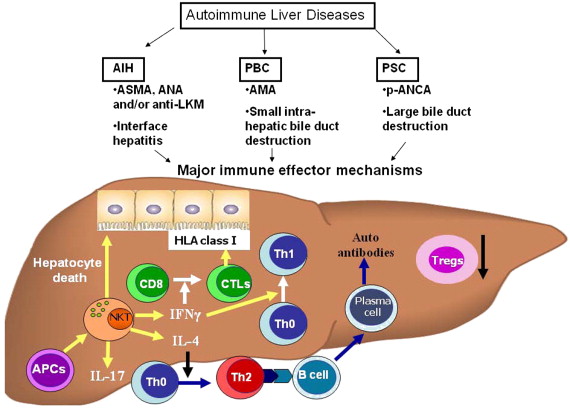 Sudden onset of excessive daytime sleepiness and other symptoms of narcolepsy can occur at any time, even in situations that require extreme concentration, such as driving. The risk group for the development of narcolepsy is men, the frequency of cases is 1 in 2 thousand people. But there is an opinion that the prevalence is higher due to the fact that not all patients do not seek medical help and treatment. Narcolepsy Source:
Sudden onset of excessive daytime sleepiness and other symptoms of narcolepsy can occur at any time, even in situations that require extreme concentration, such as driving. The risk group for the development of narcolepsy is men, the frequency of cases is 1 in 2 thousand people. But there is an opinion that the prevalence is higher due to the fact that not all patients do not seek medical help and treatment. Narcolepsy Source:
description of the clinical observation. Remizevich R.S., Kurasov E.S. Bulletin of the National Medical and Surgical Center. N. I. Pirogova, Volume 8, No. 4, 2013. pp. 141-145 - not a fatal pathology, but accidents still happen during attacks.
Causes
The exact causes of narcolepsy are unknown, although it has been established that heredity plays a role, as well as a lack of the neurotransmitter orexin, which is responsible for wakefulness.
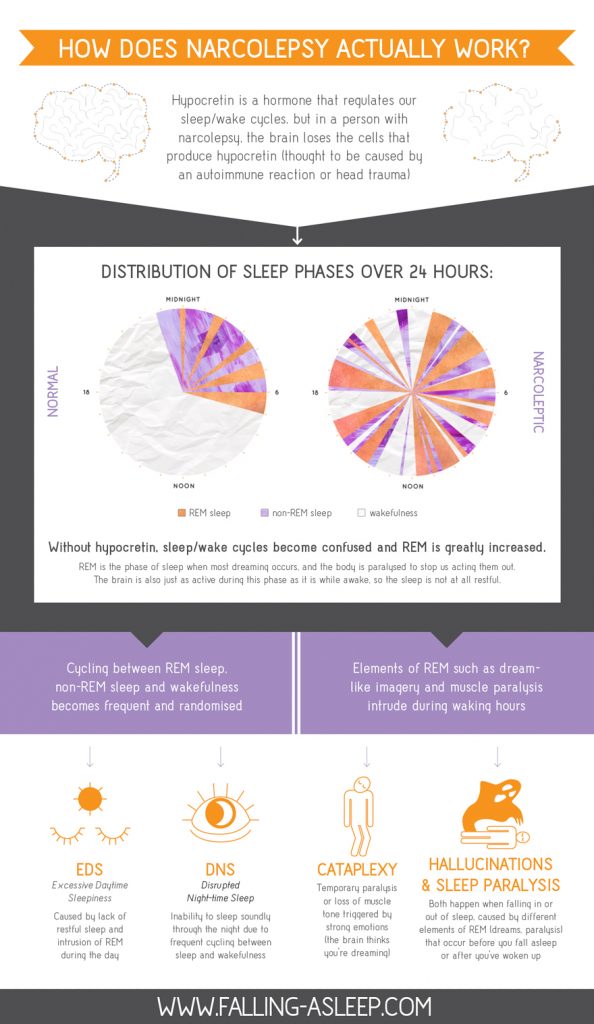
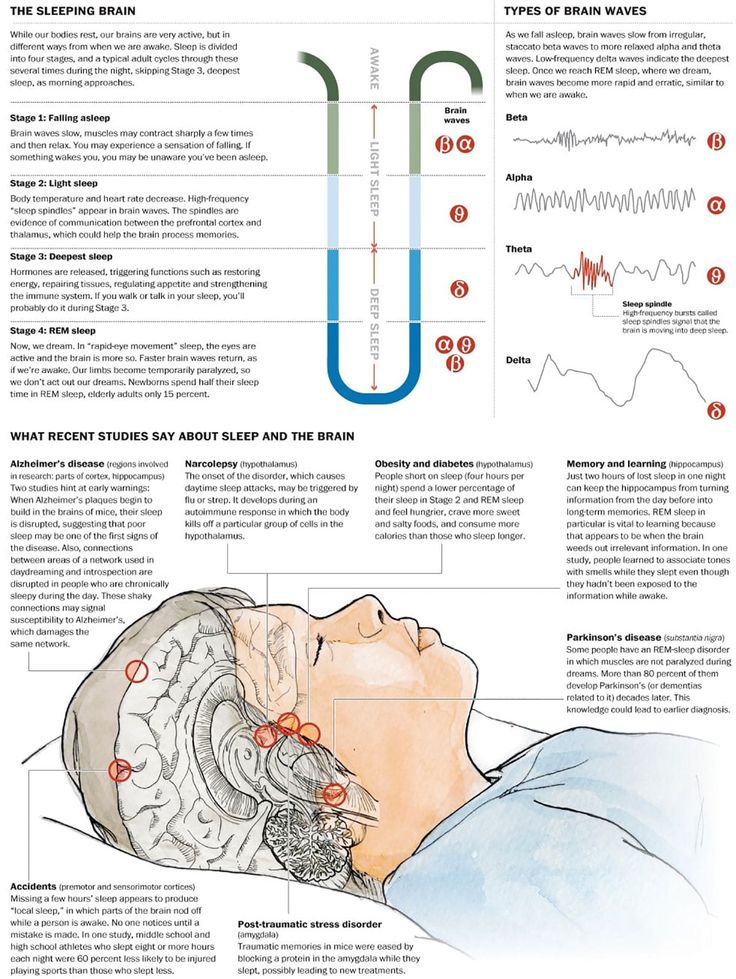
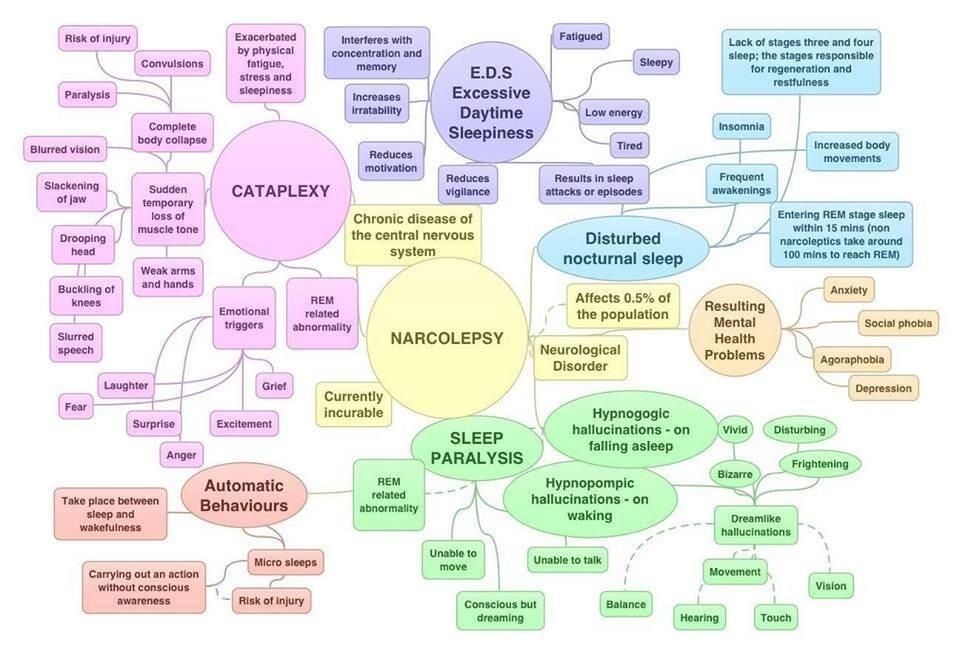
REM sleep literally invades the periods of wakefulness and the transition to sleep. Symptoms of narcolepsy are associated with a sharp loss of muscle tone, the appearance of vivid visions, which are just characteristic of the phase of REM sleep.
Symptoms of narcolepsy are associated with a sharp loss of muscle tone, the appearance of vivid visions, which are just characteristic of the phase of REM sleep.
It was not possible to establish the exact reasons for the decrease in the production of the neurotransmitter, but the predisposing factors for the development of the pathology were identified:
- serious craniocerebral injuries and their consequences;
- infectious diseases affecting the nervous system Source:
Autonomic disorders in narcolepsy (review of foreign literature). Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. pp. 165-168; - pronounced hormonal changes;
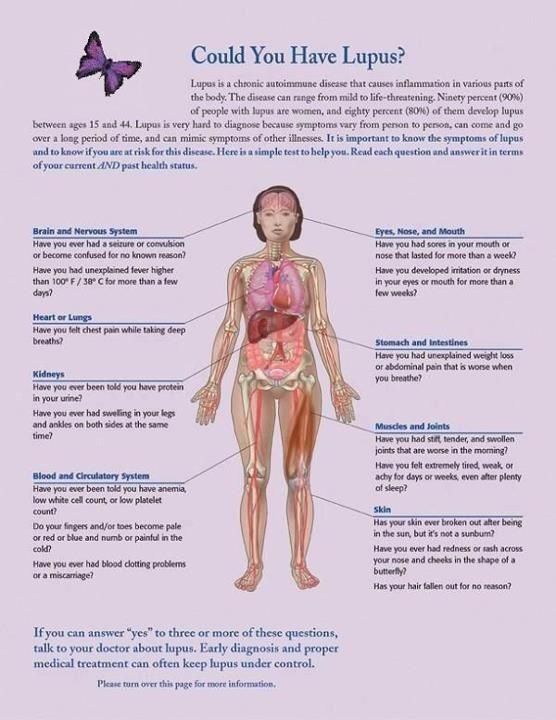
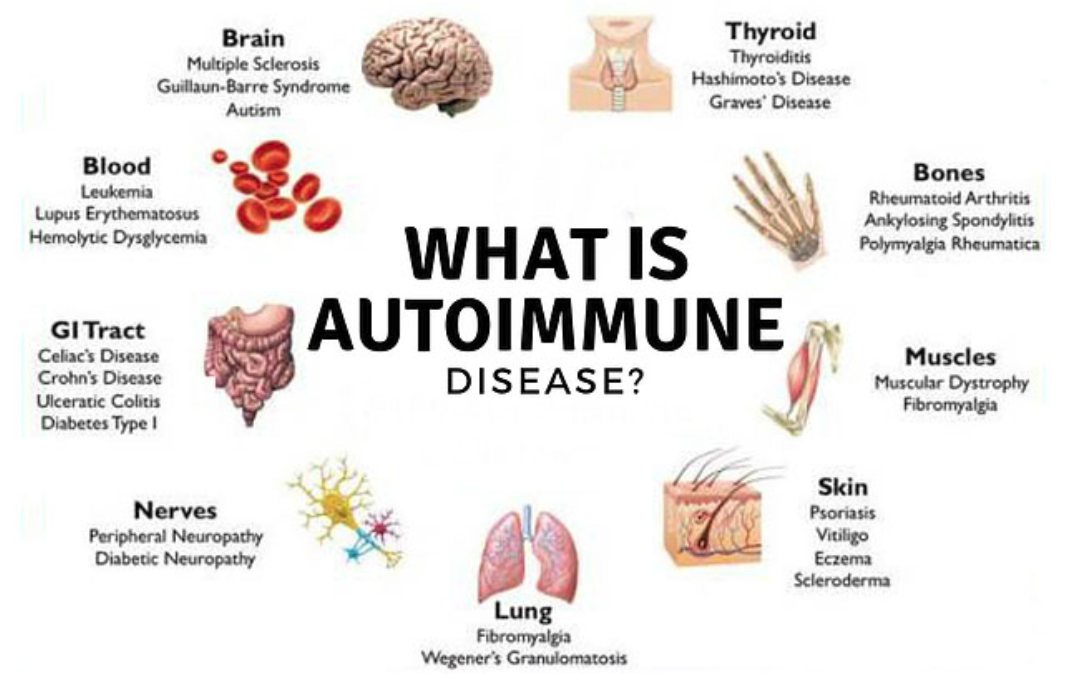
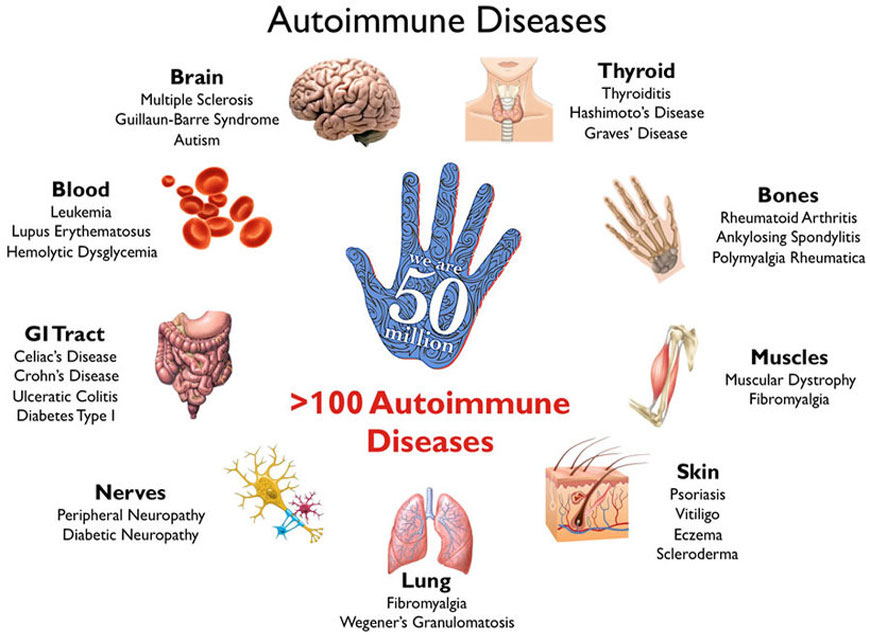
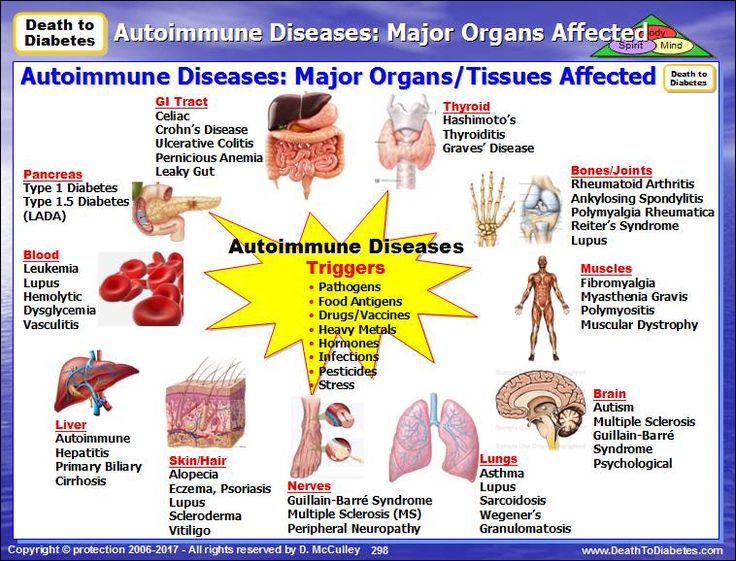
- autoimmune diseases;
- chronic stress and severe emotional upheaval;
- nervous and physical exhaustion.
As a rule, the development of a disease requires the combined action of several factors at once. Great importance in the mechanism of the development of the state is given to the work of immunity.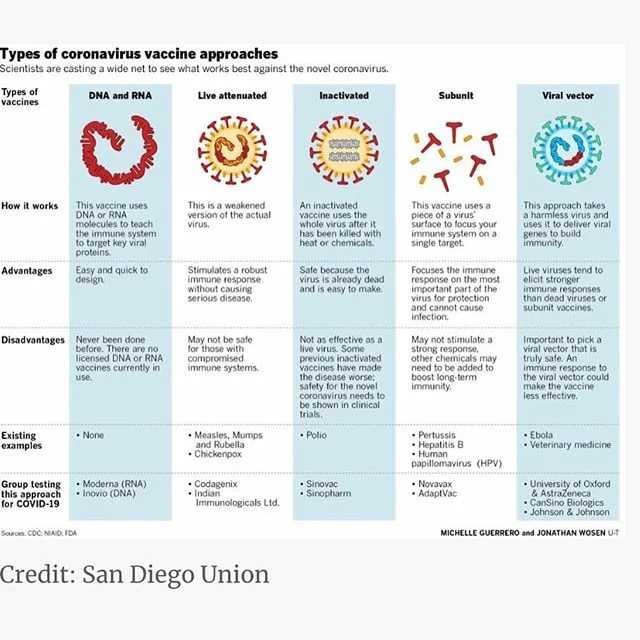 An immune response is triggered, as a result of which its own cells are mistakenly destroyed, which leads to the onset of symptoms.
An immune response is triggered, as a result of which its own cells are mistakenly destroyed, which leads to the onset of symptoms.
Symptoms of narcolepsy
The most common symptom is excessive daytime sleepiness, as well as persistent sleep disturbances at night. This creates inconvenience, spoils the quality of life, affects success in work and social relations.
Over time, the clinical picture changes, other signs join:
- The first and most common symptom is sudden falling asleep during the day. Drowsiness is severe, patients fall asleep against their will, even in unsuitable surroundings. But after waking up, they feel a surge of strength, there is no drowsiness. This state can be deceptive - after a short time they fall asleep again. At the same time, waking up the patient is no more difficult than during normal sleep.
- Cataplexy Source:
Narcolepsy with prepubertal onset cataplexy. Gromova D.O., Zinovieva O.E., Rogovina E.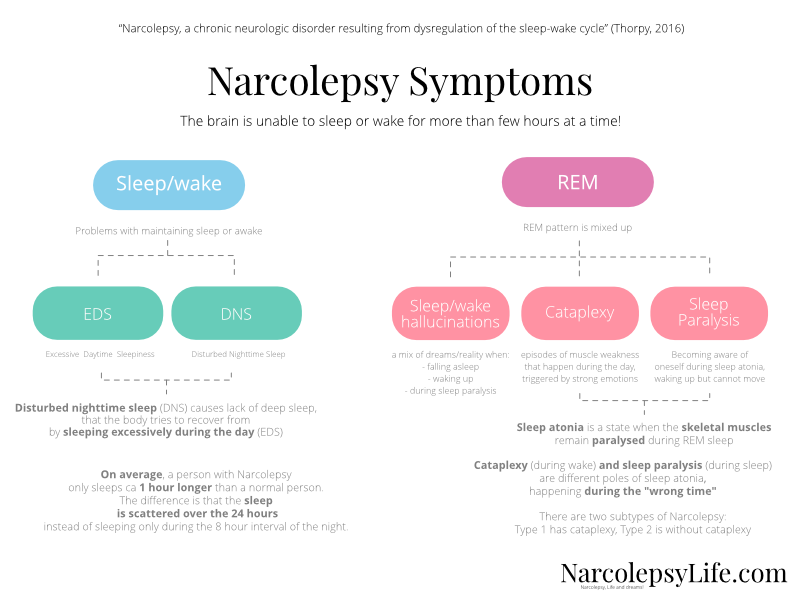 G., Poluektov M.G. Neurological journal No. 4, 2012. pp. 22-27 - sudden muscle weakness after strong emotional outbursts. The resulting weakness can be explained by a sharp loss of muscle tone, which often ends in injuries associated with a fall. The duration of the attack varies and lasts up to several minutes, followed by falling asleep.
G., Poluektov M.G. Neurological journal No. 4, 2012. pp. 22-27 - sudden muscle weakness after strong emotional outbursts. The resulting weakness can be explained by a sharp loss of muscle tone, which often ends in injuries associated with a fall. The duration of the attack varies and lasts up to several minutes, followed by falling asleep. - Hallucinations on falling asleep and waking up. They are characterized as vivid acoustic or visual visions that correspond to REM sleep. This state is sometimes called "waking sleep", and the patient himself does not realize that he is sleeping and dreaming. This is a dangerous condition that creates confusion between reality and dream.
- Sleep paralysis is a condition characterized by the inability to move after waking up, but the ability to breathe and blink remains. The patient is conscious, understands where he is. Most often, sleep paralysis is formed in the morning, less often in the evening and at night. Sleep paralysis is aggravated by hallucinations without the ability to move.
 The condition goes away after a few minutes.
The condition goes away after a few minutes.
Only 10% of patients present with all symptoms at once. Usually first appear in young people, with no previous diseases. Although they can be associated with strong emotional upheavals or chronic stress. After the first onset of symptoms, narcolepsy is permanent, but does not affect life expectancy.
In clinical practice, it is customary to distinguish 2 types of narcolepsy:
- the first occurs due to orexin deficiency, the appearance of cataplexy is characteristic Source:
Narcolepsy-cataplexy. Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. pp. 53-55; - the second is characterized by a normal level of the neurotransmitter and cataplexy does not occur.
Diagnostics
The main thing is to detect the pathology in time to prevent risks to the patient's physical health and harm to others. The patient cannot control narcolepsy, attacks occur even at the time of hard work and maximum concentration of attention, as well as performing tasks that involve risks to health and even life.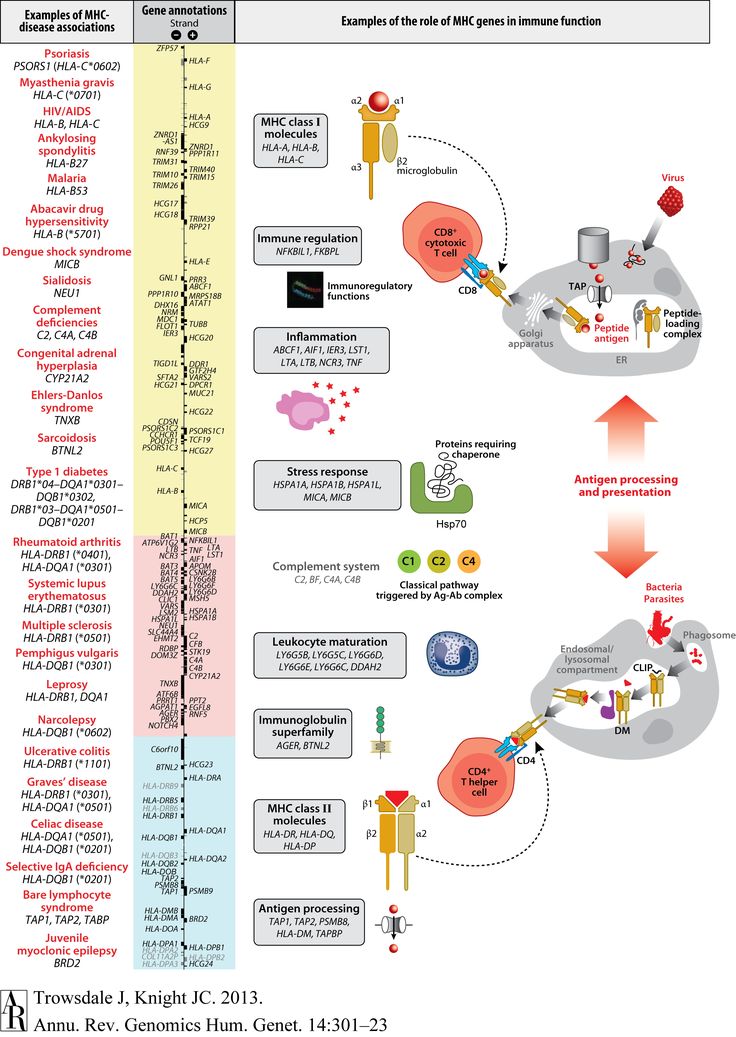
When visiting a doctor, the symptoms that characterize the diagnosis are studied in detail. The doctor is interested in:
- the patient's complaints, when the attack first occurred and how long it lasted, what symptoms are present;
- neurological examination data, some tests;
- results of additional examination methods to confirm the diagnosis.
These include polysomnography. Source:
Problems in the differential diagnosis of epileptic seizures and narcolepsy (clinical observation). Dmitrenko D.V., Alekseeva O.V., Sapronova M.R., Usoltseva A.A., Areshkina I.G. Bulletin of the North-Eastern Federal University. M. K. Ammosova. Series: Medical Sciences No. 4(13), 2018. pp. 44-51 with EEG data. This method of examination allows you to objectively assess the activity of the brain and sleep phases. The survey continues throughout the night. Electrodes are placed on the patient's head, which fix the indicators and give them out in the form of curves - the doctor analyzes the data.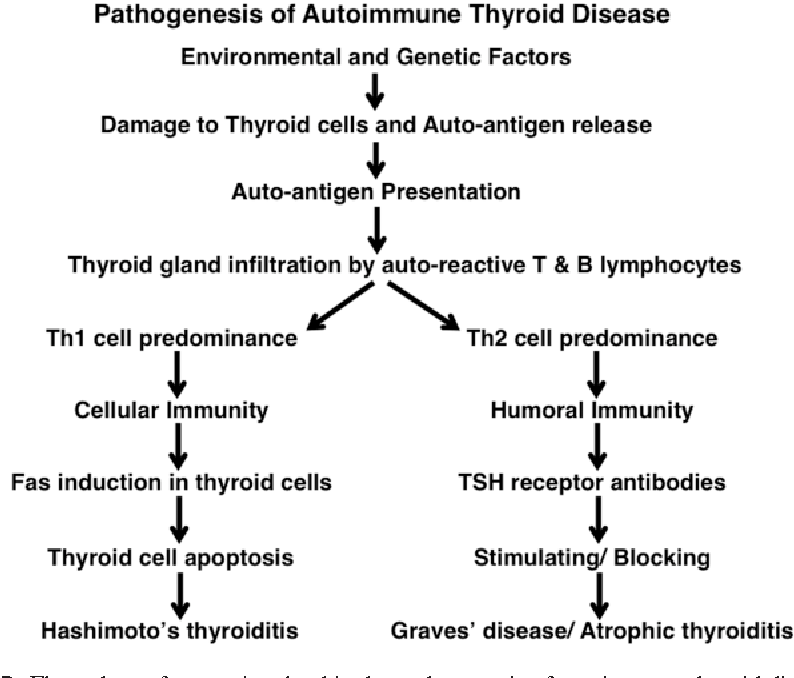
Additionally, CT and MRI are recommended to assess brain function and condition. In some cases, it may be necessary to analyze the cerebrospinal fluid, which is aimed at determining the concentration of orexin.
Treatment tactics are determined by the data obtained during the examination. This takes into account the severity of concomitant pathology, acquired diseases.
Treatment of narcolepsy
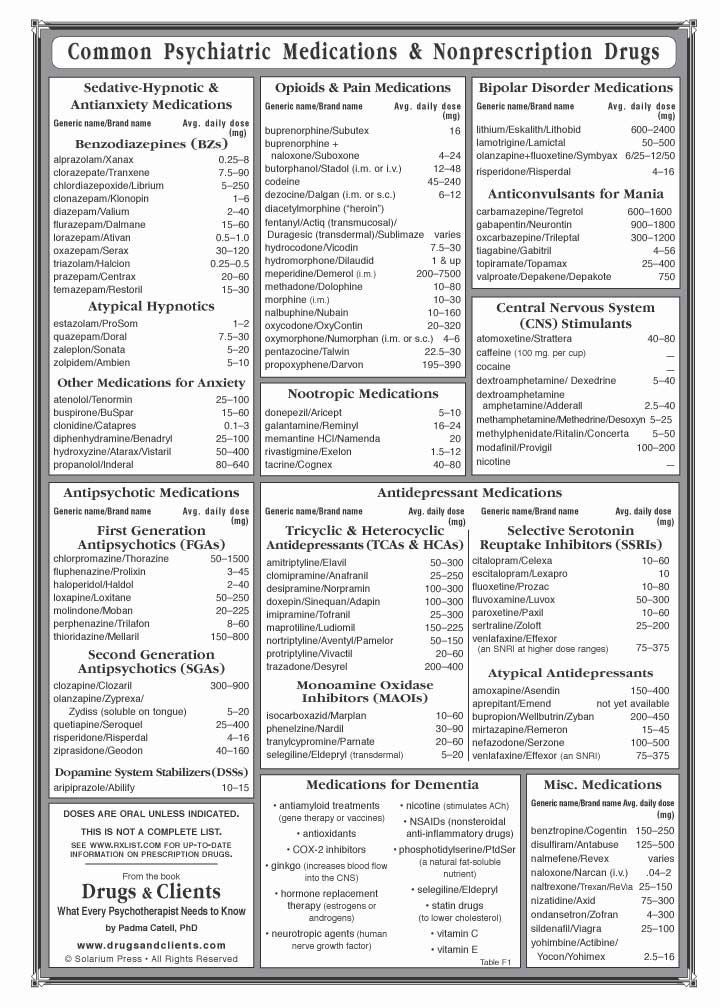
Drug treatment prescribed by specialists is constant, but the number of drugs depends on the clinical picture and the characteristics of the manifestation of the disease. Doctors usually prescribe:
- stimulants;
- sleeping pills to help normalize night sleep;
- antidepressants;
- means to combat daytime sleepiness.
Other recommendations are added to medications - lifestyle changes that help control symptoms. Patients with narcolepsy are recommended to:
- strictly follow the daily routine: go to bed and get up at the same time, regardless of holidays and weekends;
- give up alcohol completely and stop smoking;
- Minimize your intake of coffee, sugary sodas, energy drinks, and junk food;
- introduce a short daytime nap into your schedule;
- lead an active lifestyle, play sports, for example, exercise therapy, yoga.

Prognosis and prevention
Unfortunately, there is no cure for narcolepsy. All treatment is aimed at controlling and maximizing symptom relief. After the course of treatment, the patient returns to his usual way of life, although there are still some restrictions.
There are some prohibitions for all narcolepsy patients. They are forbidden to drive a car, as well as to occupy positions related to hazardous industries, for example, to work with machine tools, in large factories, etc. After all, an attack can happen at any moment, regardless of what a person is doing.
- Narcolepsy-cataplexy. Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. p.53-55
- Narcolepsy with cataplexy with onset in prepubertal age. Gromova D.O., Zinovieva O.E., Rogovina E.G., Poluektov M.G. Neurological journal №4, 2012. pp.22-27
- Modern concepts of narcolepsy with a description of clinical observation.
 Remizevich R.S., Kurasov E.S. Bulletin of the National Medical and Surgical Center. N. I. Pirogova, Volume 8, No. 4, 2013. p.141-145
Remizevich R.S., Kurasov E.S. Bulletin of the National Medical and Surgical Center. N. I. Pirogova, Volume 8, No. 4, 2013. p.141-145 - Autonomic disorders in narcolepsy (review of foreign literature). Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. p.165-168
- Problems of differential diagnosis of epileptic seizures and narcolepsy (clinical observation). Dmitrenko D.V., Alekseeva O.V., Sapronova M.R., Usoltseva A.A., Areshkina I.G. Bulletin of the North-Eastern Federal University. M. K. Ammosova. Series: Medical Sciences No. 4(13), 2018. p.44-51
Article published : 31/05/2017
Last updated : 30/11/2022
See also
Nightmares
Sleep disorders
Snoring treatment
Licenses
Medicom LLC
(Udarnikov Avenue)
Medicom LLC
(Vyborgskoye Highway)
Medi Len LLC
(Marshal Zakharov St. )
)
Medi Prof LLC
(Dunaisky Avenue)
Medi Prof LLC
(Malaya Balkanskaya St.)
Go to the license sectionGo to the legal information section
record from website DISCOUNT 10%
You are enrolling:
Clinic: {{department}}
Specialty: {{specialty}}
Doctor: {{doctor}}
Date and time: {{form.date | setTime(form.time) | dateTimeFormatted}}
Date of birth: {{age | dateFormatted}}
{{appointmentReply}}
By clicking "Sign up", I accept the terms of the user agreement, the provisions on the protection of personal data and give my consent to the processing of personal data.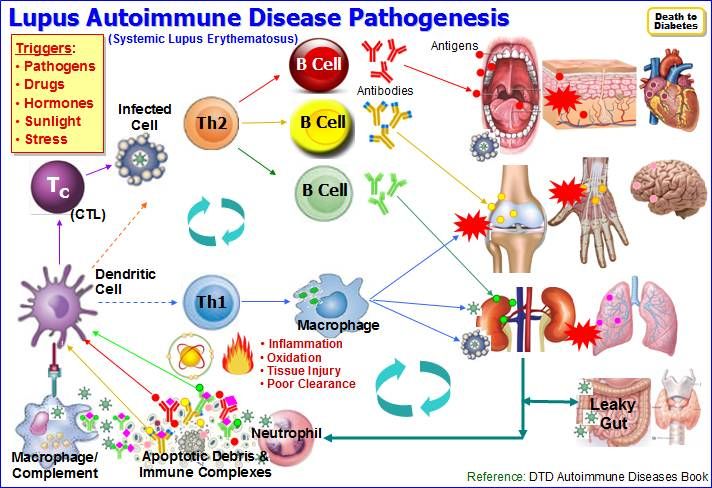
In order to pass the mandatory registration, you must come to the registration desk 10 minutes before your appointment with your passport.
If the patient is a minor (children under 18), it is mandatory to be accompanied by one of the parents with the presentation of his passport and birth certificate of the child.
Relatives and third parties accompanying a minor must have a notarized consent of the parents or legal representatives.
If you have made an appointment with a coloproctologist, please read the information about preparing for an appointment
The price of the consultation includes:
History taking, preliminary diagnosis and examination. All additional doctor's manipulations at the appointment are paid according to the price list.
If you change your mind, please unsubscribe from the appointment by phone +7 (812) 435-55-55
The price of the consultation includes:
History taking, preliminary diagnosis and examination appointment.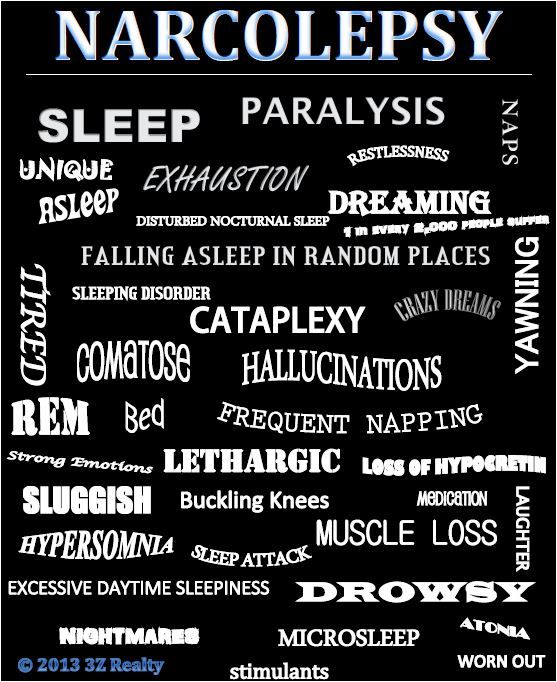 All additional doctor's manipulations at the appointment are paid according to the price list.
All additional doctor's manipulations at the appointment are paid according to the price list.
If you change your mind, please unsubscribe from the appointment using your Personal Account or by phone +7 (812) 435-55-55.
Are you sure you want to stop recording?
If you have any questions, call us at +7 (812) 435-55-55
Are you sure you want to change the current entry?
If you have any questions, call us at +7 (812) 435-55-55
You are subject to some restrictions on online booking.
Appointment possible via contact center.
You can sign up by phone +7 (812) 435-55-55
The specialist does not see patients of the specified age. To register please fill out the form below and you will be contacted.
Make an appointment
Would you like us to call you
?
Name Telephone
By clicking on the button, you consent to the processing of your personal data by
You will be contacted to confirm your application.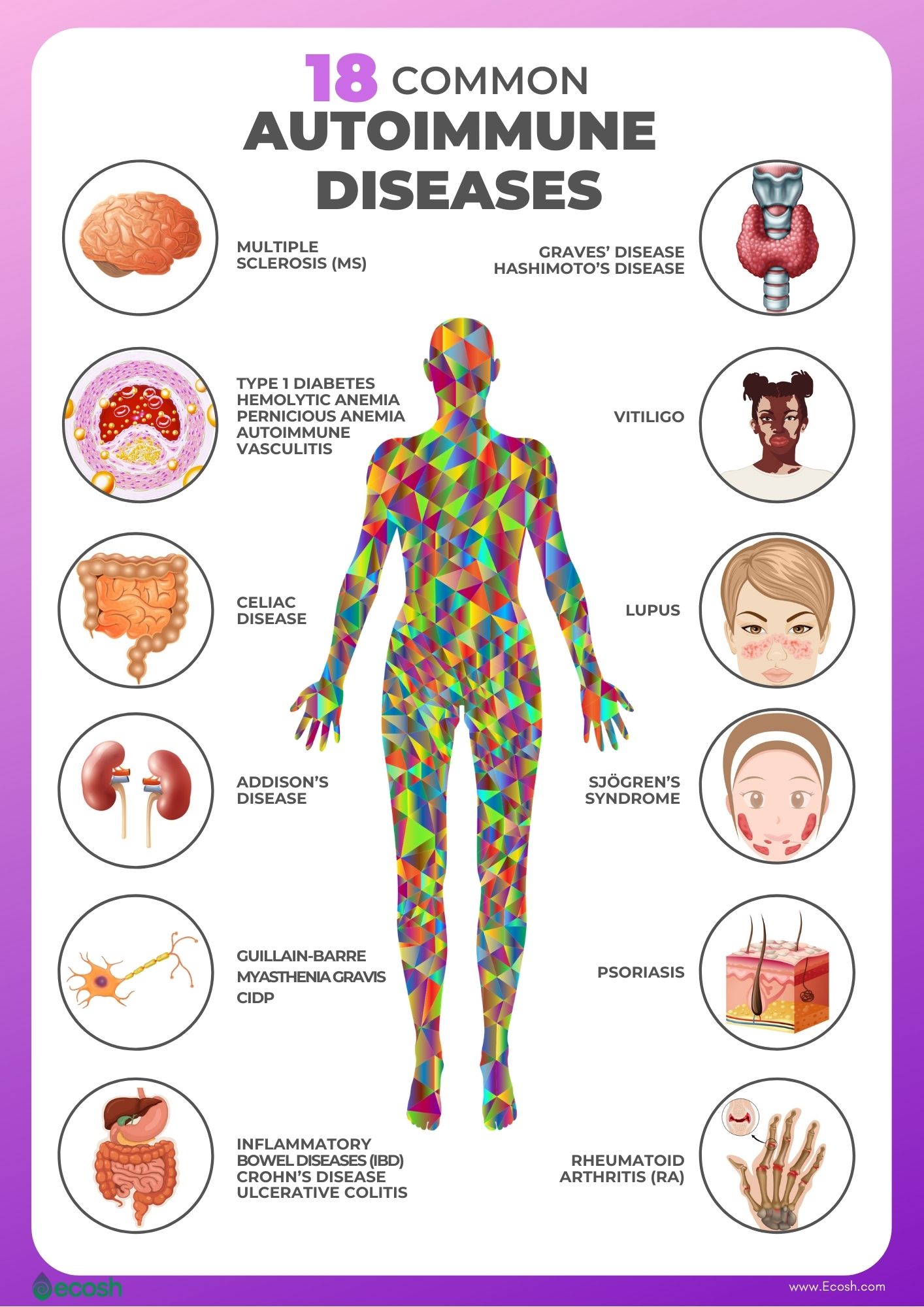
Making an appointment
Pre-registration through the site
Our employee will contact you to confirm the appointment with a specialist
By clicking on the button, you consent to the processing of your personal data by
Learn more about the quality assurance of medical services
Would you like us to call you
?
By clicking on the button, you consent to the processing of your personal data by
Leave a request and our specialist
will select a convenient time for a communication session with a doctor
By clicking on the button, you consent to the processing of your personal data by
Get a coupon for a return visit
Screenshot of a review from Yandex.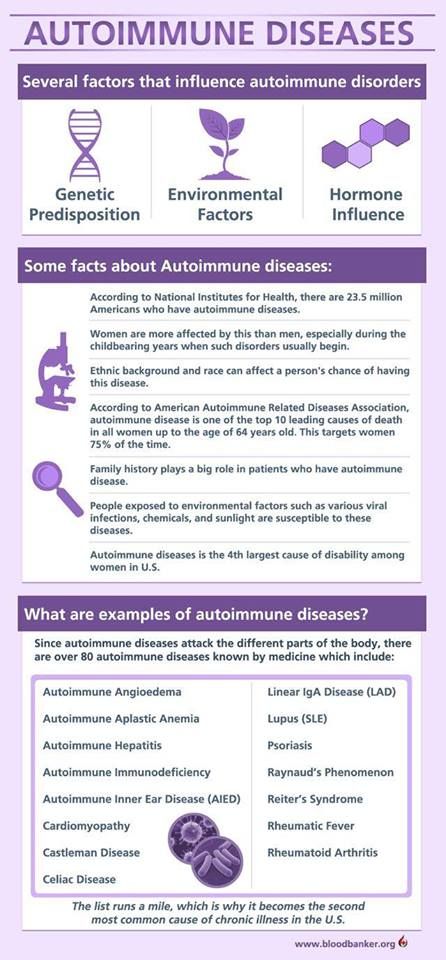 Maps*
Maps*
By clicking on the button, you consent to the processing of your personal data by
Sign up
for a consultation
Choose a clinic 1st. Marshal Zakharov, house 20Vyborg highway, house 17, bldg. 1
By clicking on the button, you consent to the processing of your personal data by
Learn more about the quality assurance of medical services
Appointment for tests
Preliminary appointment through the site
Our employee will contact you to confirm the appointment with a specialist
By clicking on the button, you consent
to process their personal data
Write to the head of customer support service
SM-Clinic
By clicking on the button, you consent to the processing of your personal data by
We use cookies. This allows us to analyze the interaction of visitors with the site and make it better. By continuing to use the site, you agree to the use of cookies.
This allows us to analyze the interaction of visitors with the site and make it better. By continuing to use the site, you agree to the use of cookies.
To accept
what are symptoms, treatment, causes
Narcolepsy - what is it?
Narcolepsy is a rare chronic brain disorder in which a person suddenly falls asleep at the wrong time.
The brain cannot properly regulate sleep and wake patterns, which can lead to the following symptoms:
- excessive daytime sleepiness (hypersomnia) Feeling very sleepy during the day, difficulty concentrating and staying awake
- Sleep attacks Falling asleep suddenly and without warning
- Cataplexy Temporary loss of muscle control leading to weakness and eventual collapse, often in response to such emotions like laughter and anger
- sleep paralysis - temporary inability to move or speak when waking up or falling asleep
- frequent dreams and wakefulness at night - dreams often come when you fall asleep (hypnogogic hallucinations) or just before or during awakening (hypnopompic hallucinations) and difficult to deal with emotionally.
Symptoms of narcolepsy
Excessive daytime sleepiness
Excessive daytime sleepiness is usually the first sign of narcolepsy. This can significantly affect daily life.
Feeling sleepy during the day and trying to stay awake makes it difficult to concentrate on work or school.
People with narcolepsy can be mistaken for being lazy or rude.
Sleep attacks
Sleep attacks, where you fall asleep suddenly and without warning, are also common in people with narcolepsy. They can happen at any moment.
The duration of a sleep attack depends on the individual. For some people, the "microsleep" lasts only a few seconds, while others may fall asleep for several minutes.
If narcolepsy is poorly controlled, sleep attacks may occur several times a day.
Cataplexy
Most people with narcolepsy also experience cataplexy, which is a sudden temporary weakness or loss of muscle control.
Typical symptoms of cataplexy:
- drooping jaw
- head drops down
- legs clench uncontrollably
- slurred speech
- double vision or difficulty focusing
Cataplexy attacks are usually triggered by an emotion such as excitement, laughter, anger or surprise.

Seizures may last from a few seconds to several minutes.
Some people with narcolepsy have cataplexy attacks once or twice a year, others several times a day.
In trying to avoid seizures, some people may become emotionally withdrawn and socially isolated.
Sleep paralysis
Some people with narcolepsy have episodes of sleep paralysis. This is a temporary inability to move or speak that occurs when waking up or falling asleep.
Episodes can last from a few seconds to several minutes. While sleep paralysis does no harm, being unable to move can be frightening.
Other symptoms
Narcolepsy can also cause a number of other symptoms, including:
- hallucinations - seeing or hearing unreal things, especially when going to bed or waking up; presence in the bedroom - most common hallucination
- memory problems
- headaches
- restless sleep - such as hot flashes, frequent awakenings, vivid nightmares, or physical manifestation of dreams
- automatic behavior - continuation of an activity without any recollection of it afterwards
- depression
Talk to a therapist if you have narcolepsy and feel depressed.
Your doctor can advise you on how to minimize the impact of narcolepsy on your daily life.
He can also put you in touch with narcolepsy organizations or support groups.
What Causes Narcolepsy: Causes
Narcolepsy is often caused by a deficiency in the brain chemical hypocretin (also known as orexin), which regulates wakefulness.
Hypocretin deficiency is thought to be caused by the immune system mistakenly attacking the cells that make it or the receptors that allow it to work.
But this does not explain all cases of narcolepsy, and the exact cause of the problem is often unclear.
Possible causes of narcolepsy include:
- hormonal changes that may occur during puberty or menopause
- severe psychological stress
- an infection, such as swine flu, or a medicine used to vaccinate against it (Pandemrix)
Immune system problem
Antibodies are normally produced by the body to destroy pathogens and toxins.
When antibodies mistakenly attack healthy cells and tissues, this is called an autoimmune response.
In 2010, scientists in Switzerland discovered that some people with narcolepsy develop antibodies against a protein called trib 2.
Trib 2 is produced by an area of the brain that also produces hypocretin. This results in a lack of hypocretin, which means the brain is less able to regulate sleep cycles.
These study results may help explain the cause of narcolepsy in many cases, but they do not explain why some people with the condition still produce near-normal levels of hypocretin.
Possible causes
A number of factors can increase the risk of narcolepsy or cause an autoimmune problem.
List of causes of narcolepsy:
- hereditary genetic error
- hormonal changes, including those that occur during puberty or menopause
- severe psychological stress
- sudden change in sleep pattern
- or infection such as swine flu streptococcal infection
- Pandemrix influenza vaccine
Studies have not yet confirmed whether all of these can lead to narcolepsy.
Pandemrix vaccine
A 2013 study found an association between the Pandemrix flu vaccine used during the 2009-10 swine flu epidemic and narcolepsy in children.
The risk is very low: the chance of developing narcolepsy after a dose of vaccine is estimated at about 1 in 52,000 shots.
But Pandemrix is no longer used in the UK for influenza vaccination.
Effects of narcolepsy on sleep
The total amount of time a person with narcolepsy sleeps is not necessarily different from the time spent by people who do not have the condition.
But narcolepsy can significantly affect sleep cycles and reduce sleep quality.
Sleep consists of cycles of different brain activity known as non-rapid eye movement (NREM) and rapid eye movement (REM).
During REM sleep, your brain activity increases and you may dream. Normal sleep begins with three stages of non-REM sleep, followed by a short period of REM sleep.

Then REM and REM sleep alternate during the night. In the second half of the night, REM sleep is more noticeable.
If you have narcolepsy, this picture is much more fragmented and you may wake up several times a night.
You may also experience REM sleep much earlier than usual after falling asleep, as well as the effects of REM sleep such as dreaming and paralysis while you are still conscious.
Secondary narcolepsy
Narcolepsy can sometimes be the result of an underlying disorder that damages areas of the brain that produce hypocretin.
For example, narcolepsy can develop after such diseases:
- Head injury
- The brain tumor
- Dispersed sclerosis (MS)
- Encephalitis
Narzlepsy, which occurred as a result of the identified underlying disease, is called secondary narcolence.
Who gets narcolepsy?
Narcolepsy is a fairly rare disease. It is difficult to determine exactly how many people have narcolepsy because many cases go unnoticed.
But it is estimated to affect around 30,000 people in the UK.
Narcolepsy is thought to affect men and women equally, although some studies have shown that the condition is more common in men.
Symptoms of narcolepsy often begin during adolescence, although it is usually diagnosed between the ages of 20 and 40.
Diagnosis of narcolepsy
See your doctor if you suspect you have narcolepsy. He may ask about your sleep habits and any other symptoms.
He may also do tests to rule out other conditions that may be causing your excessive daytime sleepiness, such as sleep apnea, restless leg syndrome in bed and jerky movements during sleep, or an underactive thyroid gland (hypothyroidism).
If necessary, you will be referred to a sleep specialist, a sleep doctor, who will analyze your sleep pattern.
This usually involves an overnight stay at a specialized sleep centre, a sleep laboratory, so that various aspects of your sleep can be monitored.
The exclusion of other factors
Narcolepsy can be difficult to diagnose, because the symptoms can be similar to symptoms of other conditions, such as:
- APNOE
- Epilepsy
- Depression of thyroid gland (Hypotiresis)
- previous head injury
Excessive daytime sleepiness can also sometimes be caused by the side effects of certain medications.
Your GP may do some tests to rule out other conditions that may be causing your symptoms.
For example, you may have a physical exam, blood pressure tests, and blood tests.
Sleep study
If your therapist thinks you may have narcolepsy, they will refer you to a sleep disorder specialist, a somnologist, who will evaluate your sleep patterns.
There are many different ways to analyze your sleep.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale is a questionnaire used to assess the likelihood that you will fall asleep while performing various activities.
Your therapist will use the results to decide if you should be referred to a sleep specialist.
When completing the questionnaire, you will be asked to rate your likelihood of falling asleep in situations such as sitting and reading, watching TV, and traveling as a passenger in a car.
A score of 10 or less means you have the same level of daytime sleepiness as the general population. If you score 11 or higher, you have an increased level of daytime sleepiness.
In this case, your therapist will likely refer you to a sleep specialist for further investigation.
Polysomnography
Polysomnography is a study of your sleep that is done at a specialist sleep centre.
This usually involves spending the night at a sleep center so your sleep patterns can be analyzed.
During the night, several different parts of your body will be monitored with electrodes and bandages placed over your body while you sleep.
The sensors will also be placed on your feet and the oxygen sensor will be attached to your finger.

A number of different tests will be performed during the polysomnography, including:
- electroencephalography (EEG), which tracks brain waves
- electrooculography, which tracks eye movements
- Electromyography (EMG), which monitors muscle tone
- Recordings of movements in the chest and abdomen (belly)
- Recordings of airflow through the mouth and nose
- Pulse oximetry, which measures heart rate and blood oxygen levels
- Electrocardiography (ECG) ) that controls your heart
Audio and video equipment can also be used to record sound and images.
After you get enough sleep, a specialist will review your test results to determine if you have normal brain activity, breathing patterns, muscle and eye movements.
Multiple Sleep Latency Test
The Multiple Sleep Latency Test measures how long it takes you to fall asleep during the day. You can have this test after a polysomnogram.
You will be asked to take several naps during the day and the specialist will analyze how quickly and easily you fall asleep.
If you have narcolepsy, you usually fall asleep easily and enter REM sleep very quickly.
You can also get a blood test to see if you have a genetic marker known as HLA DQB*0602 associated with narcolepsy.
A positive result confirms the diagnosis, but does not make it 100% - 30% of people without narcolepsy also have the genetic marker.
Measuring hypocretin (orexin)
Narcolepsy is often associated with a deficiency in the sleep-regulating brain chemical hypocretin, also known as orexin.
Research has shown that measuring hypocretin levels in the cerebrospinal fluid surrounding the brain and spinal cord can be helpful in diagnosing narcolepsy.
To measure hypocretin levels, a sample of cerebrospinal fluid is taken with a needle during a procedure called a lumbar puncture.
Sleep specialists are increasingly using this test to make a diagnosis.
Treatment for narcolepsy
There is currently no cure for narcolepsy, but making changes to improve sleep and taking medication can help minimize the impact of this condition on your daily life.
Frequent and short naps evenly distributed throughout the day are one of the best ways to deal with excessive daytime sleepiness.
This can be difficult when you're at work or school, but a therapist or specialist can create a sleep schedule to help you get used to daytime naps.
Keeping a strict sleep schedule can also help, so you should go to bed at the same time whenever possible.
If your symptoms are particularly bothersome, you may be given medication to help reduce daytime sleepiness, prevent cataplexy attacks, and improve your sleep at night.
These medicines are usually taken as tablets, capsules or drinking solutions.
Good Sleep Habits
Here's what you can do to reduce excessive daytime sleepiness and make it easier to sleep at night:
- frequent, short naps—spread sleep periods evenly throughout the day; a therapist or sleep specialist can help you plan a schedule that fits in with your other activities.

- stick to a strict sleep schedule - try to go to bed and wake up at the same time each day whenever possible.
- relax before bed - for example, take a warm bath
- provide a good sleeping environment - for example, keeping the bedroom temperature comfortable, quiet and free of distractions
- avoid caffeine (found in coffee, tea, and some carbonated drinks), alcohol, smoking before bed
- do not exercise before bed - leave at least 2 hours between the end of exercise and going to bed
- do not eat a lot, do not eat heavy meals before bed
Some medicines you buy at the pharmacy, such as cold and allergy medicines, can cause drowsiness as a side effect.
You should avoid taking these medicines during the day if you have narcolepsy as they can make your daytime sleepiness worse.
Talk to your doctor or pharmacist if you don't know which medicines make you sleepy. They may recommend alternatives that do not cause drowsiness.
Connect with others
Narcolepsy is not just a condition that is difficult to live with, it can be difficult for others to understand.
Some of the symptoms, such as sudden loss of muscle control (cataplexy), can be frightening for people who are unaware of the condition.
You may find it helpful to talk to friends and family about your condition.
Tell your child's teachers if your child has been diagnosed with narcolepsy. It is important that teachers are aware of your child's condition so that they do not mistake his behavior for laziness or for staying up too late.
If you have narcolepsy, there is no reason why you should not be able to work if your employer is aware of your condition and agrees to accommodate it, such as letting you work flexible hours or scheduling naps. But some jobs are not for you.
Your general practitioner or sleep specialist/sleep specialist can arrange for you to speak with a social worker if they think it might help.
A social worker can offer counseling and support, including advice about a career, any changes that may be made at school or work, and any financial or relationship problems you may have.
You may also find it helpful to contact your local or national narcolepsy support group.
They can give you advice on how to live with narcolepsy and connect you with others who are in a similar situation.
Drugs for narcolepsy
A number of different drugs are used to treat the symptoms of narcolepsy, but not all are licensed to treat narcolepsy, and the evidence for their effectiveness in treating this condition is not always conclusive.
The availability of some of these drugs may vary depending on the policy of your local drug regulator.
Stimulants
If necessary, a medicine known as a stimulant, such as modafinil, dexamphetamine, methylphenidate, or pitolisant, may be prescribed by a physician or specialist.
These medicines stimulate your central nervous system, which helps you stay awake during the day. They are usually taken in tablets every morning.
The total side effects of stimulants are as follows:
- Headaches
- Nausea
- Nervousness
- Problems of sleep at night (insomnia)
- Implicability
- Loss
Modafinil
Modafinil has been linked to irregular heartbeats (arrhythmias) and high blood pressure, so you will need to be monitored regularly for these problems during treatment.
Modafinil should not be taken during pregnancy as it may harm the unborn baby.
For this reason, it is not safe to get pregnant while taking modafinil. You must use effective birth control while taking it and for at least 2 months after you stop taking it.
If you are taking birth control pills, modafinil may make them less effective. So consider switching to a different type of contraception or using a different contraceptive along with the pill. A therapist or specialist can help you.
So consider switching to a different type of contraception or using a different contraceptive along with the pill. A therapist or specialist can help you.
Sodium oxybate
Sodium oxybate is a medicine that can improve sudden loss of muscle control and help you sleep at night and reduce daytime sleepiness.
Sodium oxybate is a liquid medicine you take at night in 2 doses: the first dose when you go to bed and the second dose 2.5 to 4 hours later.
You may need an alarm clock so that you can take your medicine at the right time.
You will need to take sodium oxybate 2 to 3 hours after eating, as food can affect how much of the medicine is absorbed into your body.
Do not drink alcohol while taking sodium oxybate. You should also avoid mentally demanding activities, such as driving or operating heavy machinery, for at least 6 hours after ingestion.
Although there is some uncertainty about how effective antidepressants are in treating narcolepsy, they are sometimes used to treat symptoms such as sudden loss of muscle control, hallucinations, and sleep paralysis.
Many different types of antidepressants have been used to treat people with narcolepsy, including:
- selective serotonin reuptake inhibitors (SSRIs), such as femoxetine, fluoxetine, and citalopram
- serotonin-norepinephrine reuptake inhibitors (SNRIs), such as venlafaxine
- tricyclic antidepressants (TCAs) such as imipramine and clomipramine
These medicines are thought to work by changing the levels of certain chemicals in your brain and reducing the number of dreams (REM) that are responsible for many of the symptoms of narcolepsy.
The side effects you may experience will depend on the specific medication you are taking, but common antidepressant side effects may include:
- Feelings of excitement, shakiness or anxiety
- Poor well -being
- Dry mouth
- Small clouding of vision
- SUBSTANCE
- DOISTRICTION
- Difficulty problems or Summary
- Sexy dysfunction, such with orgasm
Most side effects go away within a few weeks.