Recovering from mental illness
Recovery and mental illness.
This section looks at what it means to recover from a mental illness. Recovery means different things to different people. We focus on personal recovery and suggest different ways that you can help your own recovery. Also, we know that often people need support to recover. We hope that this information will help you to work out what recovery means to you, and help you find ways in which you can focus on your recovery. If your loved one has a mental illness, you may find this section helpful too.
If you would like more advice or information you can contact our Advice and Information Service by clicking here.
Download Recovery factsheet
- Overview
- What is recovery?
- What can help me recover?
- Further reading
- Useful contacts
Overview
- You can recover from mental illness.
Recovery means different things to different people. People often talk about clinical and personal recovery. In this section we focus on ‘personal recovery’. Personal recovery is about working towards something that is important to you.
- You may still have mental health symptoms when you are recovered.
- Treatment can often help towards recovery. But there are other options that you can try at the same time to help your recovery.
- Recovery is a personal journey. This is something you might be able to do yourself, and also with the support of others.
Need more advice?
If you need more advice or information you can contact our Advice and Information Service.
Contact us Contact us
What is recovery?
What is recovery?
There is no widely accepted definition of recovery. Recovery means different things to different people.
Recovery means different things to different people.
For some people recovery means aiming to be symptom free. For others it might mean managing your mental illness well to be able to live a meaningful life. Recovery can be a short-term or long-term thing.
In recovery, there are usually things that people can do to help themselves. People need help from others too, such as mental health and social care professionals or loved ones.
Recovery within the NHS mental health system is often referred to as the “recovery model”. This model highlights the importance of building the resilience of people with mental health problems. As well as the importance of family and professionals supporting people’s identity and self-esteem.
People often see recovery in terms of:
- clinical recovery, and
- personal recovery.
There is often an overlap between them.
What does clinical recovery mean?
Your doctor might have talked to you about ‘recovery’. Some doctors and health professionals think of recovery as no longer having mental health symptoms. Or a reduction of symptoms, which means you’re able to live a meaningful life. Sometimes this is called ‘clinical recovery’.
Some doctors and health professionals think of recovery as no longer having mental health symptoms. Or a reduction of symptoms, which means you’re able to live a meaningful life. Sometimes this is called ‘clinical recovery’.
You may be under the care of a mental health team or have people such as doctors, key workers, social workers or other professionals involved in your care. They should support you in achieving your recovery goals, and what you think is important for your wellbeing.
Dealing with symptoms is important to a lot of people. But we think recovery is wider than this, we call it ‘personal recovery.’
What can personal recovery mean?
Personal recovery can mean that you are able to live a meaningful life.
The meaning of personal recovery and how you start on the road to it is individual to you. You can think about what is important to you and what it means to you to live a ‘meaningful’ life. Remember, personal recovery is can mean different things to people. What is important for your recovery is individual to you.
What is important for your recovery is individual to you.
Think about what you would like to do and work towards that goal.
Below are some ways you can think about recovery.
- Taking steps to get closer to where you would like to be.
- Feeling part of the local community. Working with others to achieve a goal.
- Achieving something that you found difficult to do. Such as getting out of the house.
- Thinking more positively.
- Feeling settled with your treatment plan.
- Feeling in more control of your emotions.
- Having a better social life.
- Being able to have a healthy friendships and relationships.
- Having hope for the future.
Recovery is an ongoing process. It’s normal to have difficulties or setbacks along the way. You could describe yourself as ‘recovered’ at any stage in your recovery if you feel comfortable in doing so. You don’t need to wait for the ‘end’ or when you reach a certain goal.
What other things do I need to consider in my personal recovery journey?
We think people who are affected severely by mental illness need to access high quality treatment in a timely manner. But this is only one vital part of the picture.
We also need to think about all the other factors that shape our mental health: our housing, our jobs, our financial situation, trauma, economic inequality, poverty and our support networks.
We understand that lack of support can make mental health problems worse. This can leave people not knowing where to turn.
We think it’s time that communities come together to play their part in helping people who live with mental illness. You can have a read more about this in our ‘Communities that care’ report by clicking the following link: www.rethink.org/get-involved/campaign-with-us/influencing-the-nhs/communities-that-care/
It is important to remember, that recovery is possible when you have the correct tools. This includes receiving support from others. And without support from others it can be difficult.
This includes receiving support from others. And without support from others it can be difficult.
If you have support from others, it may be helpful to utilise these tools. Whether that’s your friends or family or your care team or keyworker.
Remember, it’s not always possible to do everything on your own. It’s important to accept help from others and if you haven’t got support, to reach out to get it. It’s important to remember that help is available to you.
What can help me recover?
What can help me recover?
There are different things that may help you recover. You should recover in a way that works for you. There is no right or wrong way to do so, it is a personal journey. Some people call this process a ‘recovery journey’.
The following areas may be helpful for you to explore as part of your recovery journey.
- NHS support
- Social care support
- Hope
- Acceptance
- Control
- Setting achievable goals
- Stability
- Relationships
- Support groups
- Lifestyle
- Rewarding yourself
There is more information about each of the above on this page.
What support do the NHS provide?
There are different types of support that you can get from the NHS.
What treatment should I be offered?
The right treatment is important to many people. It is often the first step towards recovery.
Often there are different treatments that are used to treat the same symptoms. You may start your recovery journey by finding a treatment that helps your symptoms and has the least amount of side effects for you.
Medication is helpful for a lot of people but not everyone needs it to recover. It’s important to remember that medication may not work straight away.
Other treatment options may be important to you such as:
- talking therapy,
- mindfulness,
- art therapy, or
- complementary therapies.
Complementary therapies aren’t generally available on the NHS.
What is social prescribing?
Social prescribing is non-medical option to help improve your wellbeing.
You can talk to your GP about a link worker. Link workers aren’t yet available in all areas of the country. The NHS have committed to having 1,000 link workers in place by April 2021. There will be more link workers in place by 2024.
A link worker will work with you to find out what is important to you. They can connect you with local support such as:
- activity groups,
- support groups,
- services, such as charities, and
- social services.
What are recovery colleges?
Recovery colleges are part of the NHS. They offer free courses about mental health to help you manage your symptoms. They can help you to take control of your wellbeing and recovery. You can usually self-refer to a recovery college.
Recovery colleges are available in most areas. To see if there is a recovery college in your area you can use a search on the internet or call NHS 111.
You can find more information about:
- Talking treatments by clicking here.
- Medication. Choice and managing problems by clicking here.
- Complementary and alternative treatments by clicking here.
What if I’m not happy with my treatment?
If you aren’t happy with your treatment you can:
- talk to your doctor about your treatment options,
- ask for a second opinion,
- get an advocate to help you speak to professionals,
- contact Patient Advice and Liaison Service (PALS) and see whether they can help, or
- make a complaint.
There is more information about these options below.
How can I talk to my doctor about my treatment?
You can speak to your doctor about your treatment. You can explain why you aren’t happy with it. You could ask what other treatments you can try.
Tell your doctor if there is a type of treatment that you would like to try. Doctors should listen to your preference. If you aren’t given this treatment, ask your doctor to explain why it isn’t suitable for you.
What is a second opinion?
A second opinion means that you would like a different doctor to give their opinion about what treatment you should have. You can also ask for a second opinion if you disagree with your diagnosis.
You don’t have a right to a second opinion. But your doctor should listen to your reason for wanting a second opinion and may offer you one.
What is advocacy?
An advocate is independent from the NHS. They are free to use. They can be useful if you find it difficult to get your views heard.
There are different types of advocates available. Community advocates can support you to get a health professional to listen to your concerns. And help you to get the treatment that you would like. They aren’t available in all areas.
You can ask an advocate to help you make a complaint. Advocates that do this are called NHS complaints advocates. They are free to use and don’t work for the NHS. They’re available in all areas.
You can search online to search for a local advocacy service. If you can’t find a service you can call our advice service 0808 801 0525 (Monday to Friday, 9.30am-4pm, excluding bank holidays). You can email us too at [email protected]. We will look for you.
How can I complain?
If you can’t sort your problem, you can make a complaint. This is where your concerns are investigated in further detail.
You can ask a member of your health team to explain how to make a complaint and for their complaints policy.
You can find out more about:
- Medication - Choice and managing problems by clicking here.
- Second opinions by clicking here.
- Advocacy by clicking here.
- Complaining about the NHS or social services by clicking here.
What is social care support?
You may be entitled to get help from social services. Social care support can include support to help you to do things like:
- get out of the house,
- keep in touch with friends and family,
- get a job or take part in education,
- prepare meals or go shopping, and
- manage money.
Your entitled to a social care assessment, to see if you qualify for social care support and what your needs are. With more support you may feel more able to take control of your recovery.
You can find more information about:
- Medication. Choice and managing problems by clicking here.
- Advocacy by clicking here.
- Social care assessment under the Care Act 2014 by clicking here.
- Social care - care and support planning by clicking here.
How is hope important to recovery?
Hope is an important part of recovery. You might find it helpful to read stories from people about their recovery. You can take a look at the following websites as a first step.
- www.time-to-change.org.uk/personal-stories
- www.mind.org.uk/information-support/your-stories/
You could join a support group. A support group is where people come together to share information, experiences and give each other support.
See support groups further down this page for more information about how to find a group.
You could also contact an emotional support line for support. Sometimes speaking to someone else can help you feel more hopeful when you’re not feeling your best. You can find a list of emotional support lines at the bottom of this page.
How can acceptance help?
We understand that for some people it can be difficult to be diagnosed with a mental illness. Some people have found that their recovery journey may be easier after they learn to accept their illness and the difficulties it causes. Others prefer to concentrate on their symptoms and how they can be helped.
It can sometimes be useful to recognise that your illness might make some things difficult or impossible for you to do. You can think about how this affects your life, what you can do to overcome challenges and what help you need.
It may be helpful for you to also focus on what you can do. You are more likely to reach your goal if it is something you can achieve.
Acceptance may help you to make positive changes and help you to reach new goals.
It might help you to:
- read about your illness or symptoms, and
- talk to other people with similar issues, or who have the same diagnosis as you.
See support groups further down this page for more information about how to find a group.
Spiritual or religious beliefs and practices may also help you to make sense of your experiences and find meaning.
You can find more about ‘Spirituality, religion and mental illness’ by clicking here.
Why is control important?
Whilst it’s difficult to take control of everything, you may find it is helpful to focus on the things you can control
It may be helpful to think about these questions.
- What makes me happy?
- How can I be happier?
- What do I want to have changed in my life by this time next year?
- How can I do it?
- Do I need support to do it?
- Who can support me?
Control may mean that you are more involved with your medication and treatment options. Speak to your family, doctor or other health professionals if you want more support.
Speak to your family, doctor or other health professionals if you want more support.
You can find more information about:
- Medication - choice and managing problems by clicking here.
- NHS – your rights by clicking here.
What is a mood diary?
Keeping a diary or log of your mental health for a few weeks may be helpful. You could use this diary to reflect on things that happen that may have had a toll on your mental health. This may help you to take control of your symptoms.
You could write down when you feel mentally unwell or stressed. You can include things like:
- When do you feel mentally unwell or stressed?
- What happened just before you felt this way?
- Were you on your own or with someone?
- How did you cope with your feelings?
The mood diary could also help you to identify things which can make you unwell. These things are known as ‘triggers.’ Identifying your triggers can help you to have more control over your stress levels.
There is a template for a mental health diary at the end of the attached factsheet; available to download using the link at the top of this page.
What can I do to achieve goals?
Setting achievable goals can help you to recover.
To help you to set yourself a goal, think about what is important to you.
For example, a goal you might have is to give yourself a routine and stick to it. Or having a goal to make new friends or change your job.
Some goals will need more work than other goals and will take longer to achieve. Make sure that you are realistic with your goals. You don’t want to give yourself a goal which you are unlikely to be able to achieve. This is likely to have a negative impact on your mental wellbeing.
You can think about making SMART goals. SMART stands for:
- Simple – is your goal simple to follow?
- Meaningful – does your goal mean something to you?
- Achievable – is your goal achievable.
 Is it something you can do?
Is it something you can do? - Realistic – is your goal appropriate for you? If so, how will you do it?
- Time limited – make sure you set a date of when you want to achieve this goal. This can help keep you accountable.
Below is an example of a SMART plan.
Peter's Plan
What is your specific goal?
- To cook at least 2 healthy meals per week for the next 6 months.
Why is this goal meaningful to you?
- Cooking 2 healthy meals per week is good for my physical health and cooking can be good for mental wellbeing too.
Is this goal achievable?
- My goal is achievable as it’s only 2 meals a week and realistic to the time I’ve got available and it doesn’t seem too stressful.
How are you going to prepare for this activity?
- I’m going to plan how long the meal will take to cook. I’ll make sure I leave myself enough time to prepare, cook and eat the meal.
 It will be good for me to plan what meal I want to cook.
It will be good for me to plan what meal I want to cook.
What is your deadline?
- I am going to cook 2 healthy meals per week for the next 6 months. This is realistic and gives me time to get used to cooking. If it goes well I might do more.
How will you do this activity?
- I am going to find healthy and affordable recipes to cook. I will search on BBC Good Food for this.
- I am going to buy the ingredients for this meal when I go shopping with my support worker.
What will you do when you have finished your task?
- I will acknowledge that I have achieved something which I found difficult. I will reward myself by doing something that I enjoy. I will think about if I can cook more meals a week.
What will you do if you haven’t stuck to your deadline?
- I won’t be as hard on myself and I will make a new deadline and start again.
What advice can I get about money and housing issues?
Money and housing worries can cause a lot of stress and make mental health problems worse. Secure finances and a suitable place to live are an important part of recovery.
Secure finances and a suitable place to live are an important part of recovery.
Get help early if you start to have money or housing problems. If you ignore issues, they are unlikely to go away and may get worse.
If you find it difficult to manage your money due to your mental health take a look at the following website:
www.mentalhealthandmoneyadvice.org/en/managing-money/how-do-i-manage-my-money-if-i-have-mental-health-problems/
You can find more information about:
- Housing options by clicking here.
You can find more information about ‘Debt and Money Management’ and ‘Debt – Options when you are in debt’ at www.rethink.org/advice-and-information/living-with-mental-illness/money-benefits-and-mental-health/
These factsheets include organisations you can contact for free housing and money advice.
How can I stay in contact with people?
Stay in contact with people who can help you stay well. You can stay in contact with people by the following.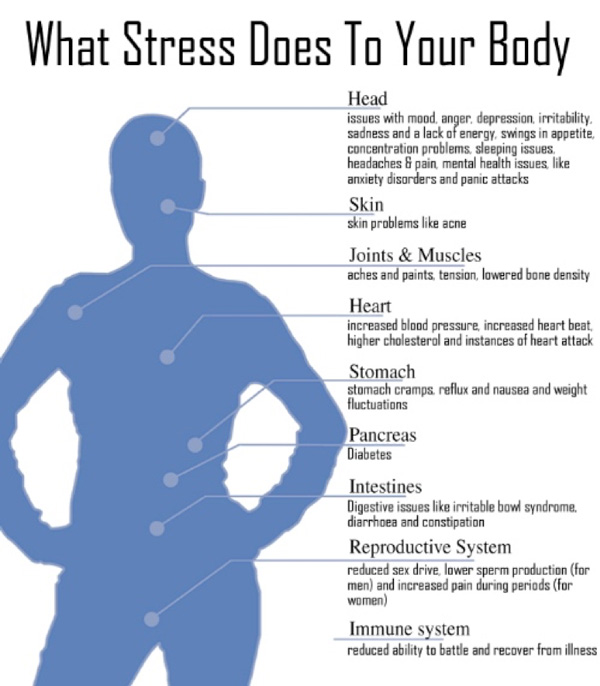
- Face to face. You could visit a friend or loved one.
- Online. You can use a free online programme such as ‘Zoom’ or ‘WhatsApp’ to speak to family or friends.
- Online forums. This is where people talk about a particular subject. For example, if you’re interested in cars you can join a forum where people discuss cars.
- Telephone.
- Text message.
- E-mail.
- Letter.
You don’t have to talk about your mental illness unless you want to.
Below are some things you can do if you want to make more contact with
other people.
- Get back in touch with people you already know.
- Join support groups.
- Join online forums.
- Join social groups such as through ‘Meet up.’ Their website is www.meetup.com
- Join a recovery college.
- Volunteer with a charity you care about.
- Contact a befriending service.
- Look for local classes or clubs that interest you.
- Get help from the NHS or local authority.
- Get into work or training.
How can friends and family support me?
Friends and family members can offer support to you and help to build hope for your future.
You could tell them about any care plans that you have and tell them about any goals you have.
They may be able to offer you better support if they understand your illness. You could suggest that they read information about your illness.
We have information on different mental health conditions at www.rethink.org.
You and your family may also find family intervention useful.
What is family intervention?
Family intervention is offered through the NHS for people who experience psychosis. It is a therapy where you and your family work with mental health professionals to help to manage relationships.
This should be offered to people who you live with or who you are in close contact with. The support that you and your family are given will depend on what problems there are and what preferences you all have.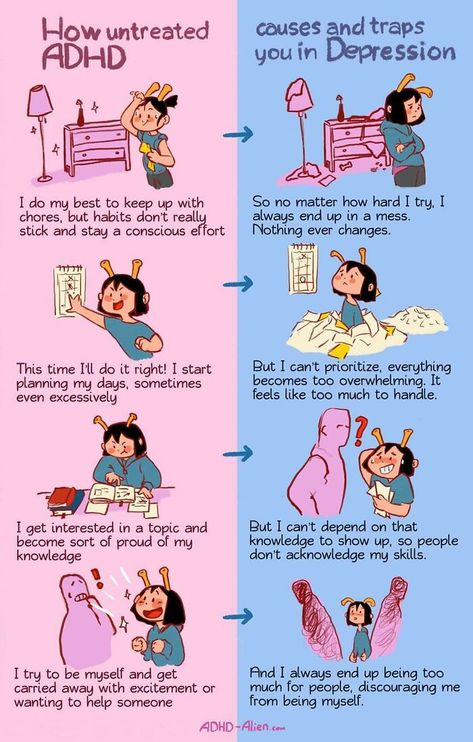 This could be group family sessions or individual sessions. Your family should get support for 3 months to 1 year and should have at least 10 planned sessions.
This could be group family sessions or individual sessions. Your family should get support for 3 months to 1 year and should have at least 10 planned sessions.
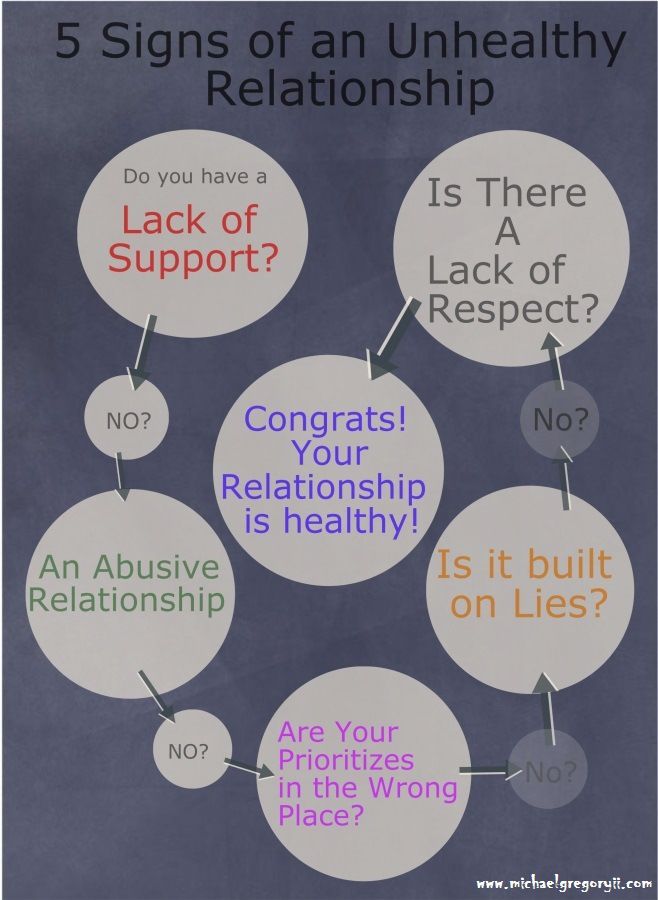
How can I think about how relationships affect me?
Unfortunately, not all relationships are positive. It is important to recognise when your relationships with others is having a negative effect on you.
Keeping a mood diary may help you to identify people who are making you feel unwell or stressed. See the mood diary section of this page for more information.
The following links contain some helpful advice about relationships. You may find them helpful:
Guide to investing in relationships:
www.mentalhealth.org.uk/sites/default/files/guide-investing-relationships-may-2016.pdf
Tips for building a healthy relationship:
www.helpguide.org/articles/relationships-communication/relationship-help.htm
What are support groups?
Joining a support group can be a good way to help yourself. Support groups may give you hope for the future or help you to take control of your life. They are a place where you can share experiences with others and get mutual support. You can search for local support groups below:
Support groups may give you hope for the future or help you to take control of your life. They are a place where you can share experiences with others and get mutual support. You can search for local support groups below:
- Rethink Mental Illness: www.rethink.org/about-us/our-support-groups
- Local Minds: www.mind.org.uk/about-us/local-minds/
- Bipolar UK: www.bipolaruk.org/find-a-support-group
- Carers Trust (for support groups and services for carers): www.carers.org/search/network-partners;
There are also online support services:
- Elefriends (Mind): www.elefriends.org.uk/
- 7 Cups: www.7cups.com
- Sane: www.sane.org.uk/what_we_do/support/supportforum
- Big White Wall: www.bigwhitewall.com
What are emotional support lines?
You can contact an emotional support lines for support. Emotional support lines are also known as listening services. They are a place that you can off load how you are feeling to someone who is trained to listen. Emotional support lines aren’t the same as counselling. Counselling is a type of talking treatment.
Emotional support lines are also known as listening services. They are a place that you can off load how you are feeling to someone who is trained to listen. Emotional support lines aren’t the same as counselling. Counselling is a type of talking treatment.
You can find a list of emotional support lines at the end of this page.
How can lifestyle changes help?
Making small lifestyle changes can improve your wellbeing and can help your recovery.
Routine
Routine may help to improve your mental wellbeing. It will help to give a structure to your day and may give you a sense of purpose.
This could be a simple routine. Such as eating and going to bed at the same time each day.
John's Story
Learn something new
You may want the learn something new. New activities can help you to learn new skills and meet new people.
You can also include time for your new activity into your daily or weekly routine.
To learn new skills, you could try the following.
- Volunteer
- Study
- Get a job
- Talk to your employer about new things that you can learn as part of your job
- Do housework or gardening
- Learn a new hobby
- Go to a class
- Get a pet
- Exercise
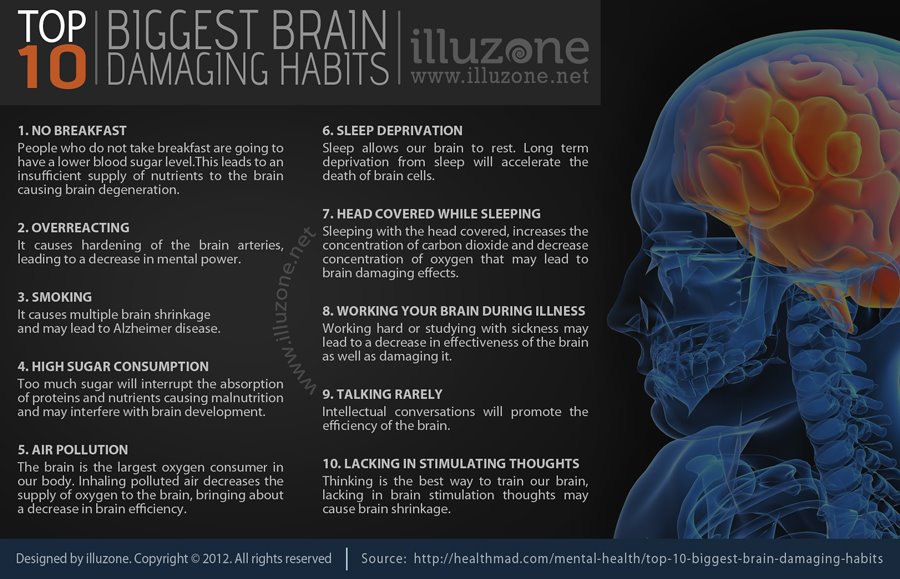
Sleep
Sleep is very important. If you’re dealing with mental health issues such as stress, you may struggle to sleep well. Your mental health symptoms may feel worse if you are tired.
Not getting enough sleep can cause problems such as poor concentration and low mood. Long term sleep issues can lead to mental health problems such as anxiety and depression.
If you struggle with sleep, you can try to:
- talk to your doctor,
- refer yourself for NHS talking therapy, or
- practice sleep hygiene.
Sleep hygiene means things like:
- having a regular bedtime routine,
- only using your bed for sleep,
- exercising regularly but avoiding lots of exercise too close to bedtime,
- cutting down on caffeine, especially in the evening,
- making the place you sleep is a comfortable temperature,
- making sure the place you sleep is dark,
- not using your phone or computer immediately before bedtime, and
- making sure that the place you sleep is tidy.

You can find out more about how to improve your sleep at:
www.rethink.org/advice-and-information/living-with-mental-illness/wellbeing-physical-health/how-can-i-improve-my-sleep/
Eat well
You can feel emotionally well if you eat well. Eating well will mean something different to different people. Generally, it means:
- Your weight stays normal. Not too low or too high for your height.
- Your weight stays stable. Not going up and down all the time.
- You eat the necessary food groups regularly, such as fruit and vegetables.
- Eating is enjoyable.
You can find out more about eating well here: www.nhs.uk/live-well/eat-well
Exercise
Exercise can improve your mental health. It can help with depression and anxiety and symptoms such as:
- negative mood,
- low self-esteem,
- social withdrawal, and
- thinking clearly.
Exercise can help improve mild depression, just as good as antidepressants or talking treatments.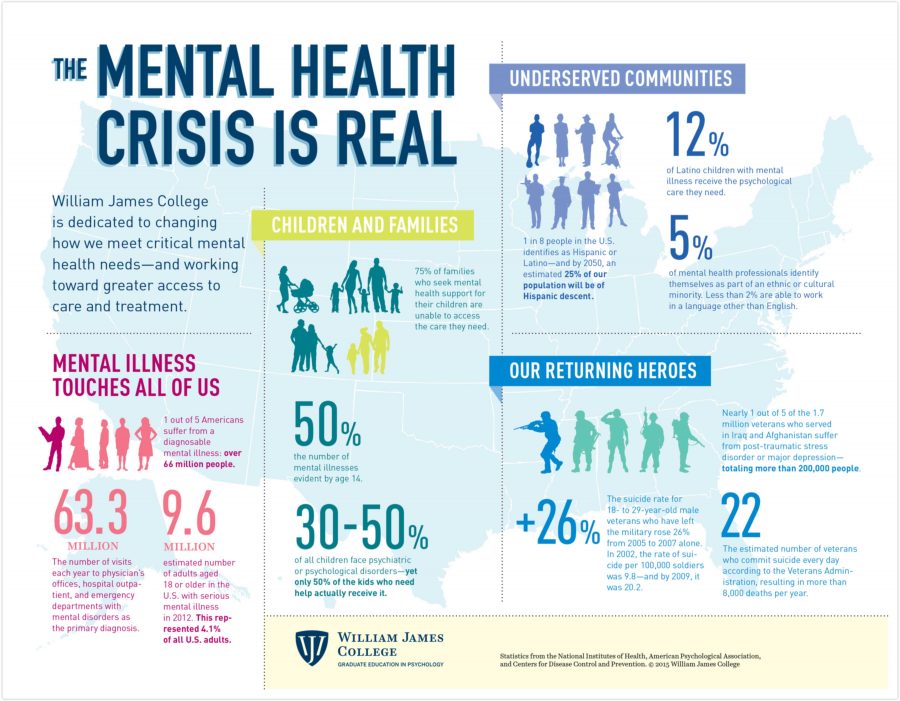
GP’s can prescribe exercise in some areas in the UK. They do this by helping you get a free or reduced rate gym membership. This is part of social prescribing. See social prescribing in this factsheet for more information.
If you need some support to start exercising you could look at the information on the ‘We are undefeatable’ website. We are undefeatable is an exercise campaign that Rethink Mental Illness are involved with.
Click the following link for more information:
www.weareundefeatable.co.uk/
You can read more about physical health and lifestyle changes below
here: www.rethink.org/advice-and-information/living-with-mental-illness/wellbeing-physical-health/
Reward yourself
Make sure you reward yourself for any positive changes you make.
It is all too easy to be hard on yourself. Often, we are our own worst critic.
Remember to congratulate yourself for any achievement. And be kind to yourself when you haven’t achieved a goal.
Wellness Recovery Action Plan (WRAP) Plus. Formerly living without Depression and Manic Depression - Mary Ellen Copeland, PhD.
The Wellness Recovery Action Plan® or WRAP® is a self-designed wellness process. You can use a WRAP to get well, stay well and make your life your own. It was developed in 1997 by a group of people who were searching for ways to overcome their own mental health issues and move on to fulfilling their life dreams and goals.
Website: www.mentalhealthrecovery.com
Staying Well with bi-polar Guide. Rethink Mental Illness.
Staying well with bipolar is a guide based on the research conducted by Rethink Mental Illness. It is based on the personal experiences and learning of 32 people
Website: www.rethink.org/advice-and-information/living-with-mental-illness/treatment-and-support/staying-well-with-bipolar/
Live your best working life.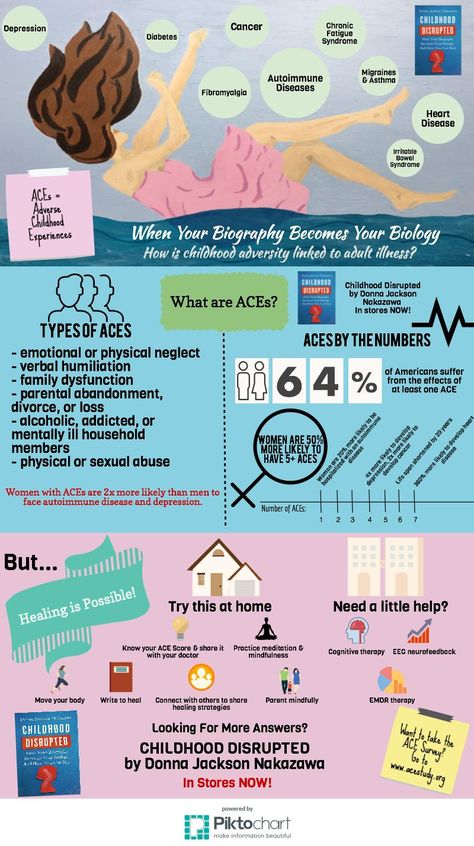 Mental Health UK
Mental Health UK
Mental Health UK is made up of 4 mental health charities working across the UK, including Rethink Mental Illness. They provide videos and information on issues relating to mental health. This page has tips and ideas to help you manage your mental health and wellbeing, so you can be your best at work.
Website: www.mentalhealth.org.uk/a-to-z/w/work-life-balance
Recovery Star
Developed by the Mental Health Providers Forum, the recovery star measures outcomes to allow people to measure their recovery progress.
Website: www.mentalhealthpartnerships.com/resource/recovery-star
Useful contacts
Emotional Support lines
Samaritans
Can be contacted by telephone, letter, e-mail and mini-com. There's also a face-to-face service, available at their local branches. They are open 24 hours a day, every day of the year.
Telephone: 116 123
Email: jo@samaritans.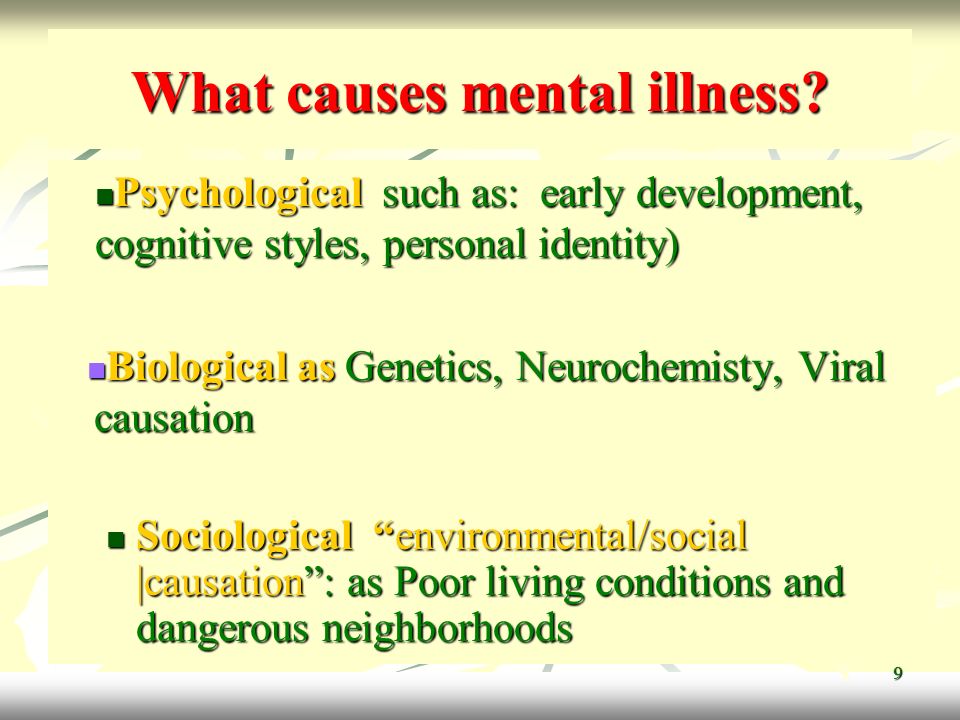 org
org
Website: www.samaritans.org
Sane Line
Work with anyone affected by mental illness, including families, friends and carers. Their helpline is open between 4:30pm and 10.30pm every day of the year. They also provide a free text-based support service called Textcare and an online supportive forum community where anyone can share their experiences of mental health.
Telephone: 0300 304 7000 (4:30pm – 10:30pm every evening)
Textcare: www.sane.org.uk/what_we_do/support/textcare
Support Forum: www.sane.org.uk/what_we_do/support/supportforum
Website: www.sane.org.uk
Support Line
They offer confidential emotional support to children, young adults and adults by telephone, email and post. They work with callers to develop healthy, positive coping strategies, an inner feeling of strength and increased self-esteem to encourage healing, recovery and moving forward with life.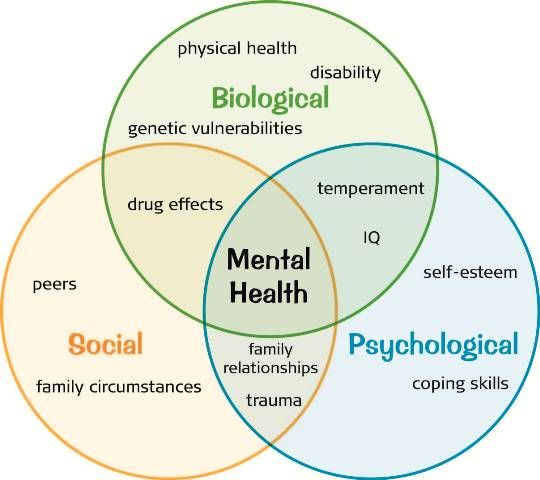 Their opening hours vary so you need to ring them for details.
Their opening hours vary so you need to ring them for details.
Telephone: 01708 765200
E-mail: [email protected]
Website: www.supportline.org.uk
Papyrus UK
Work with people under 35 who are having suicidal feelings. And with people who are worried about someone under 35. Their helpline is open 9am – 10pm in the week. And between 2pm and 10pm at weekends and bank holidays.
Telephone: 0800 068 41 41
Email: [email protected]
Text: 07786 209697
Website: www.papyrus-uk.org
C.A.L.M. (Campaign Against Living Miserably)
Aimed specifically at men. Their helpline is open between 5pm and midnight every day of the year.
Telephone (outside London): 0800 58 58 58
Telephone (London): 0808 802 58 58
Webchat: through the website
Website: www.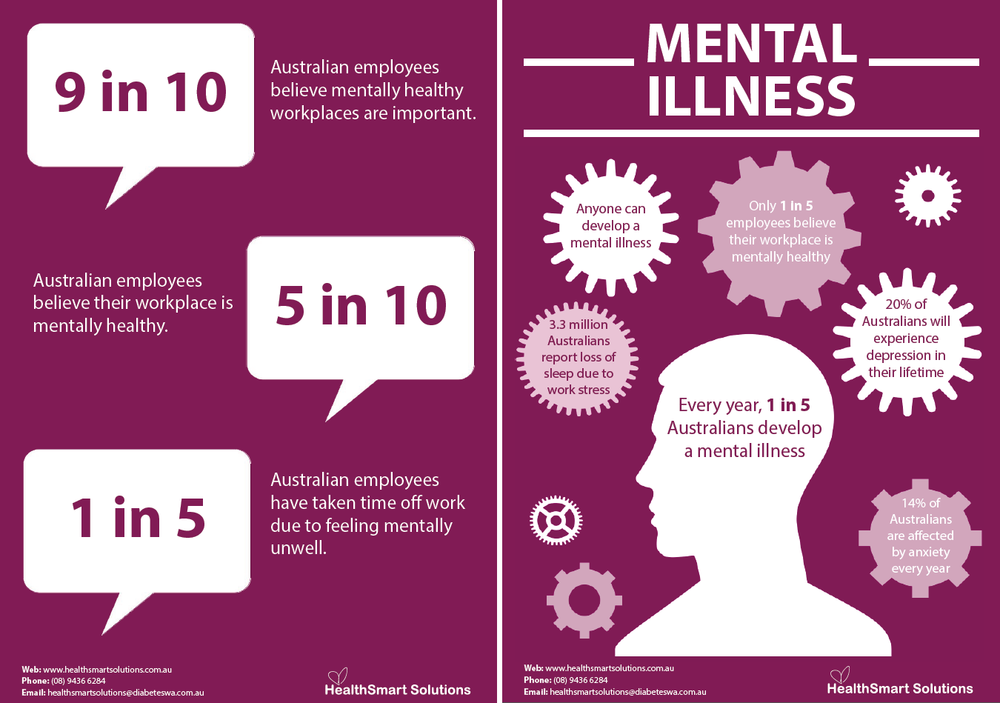 thecalmzone.net
thecalmzone.net
Silverline
Aimed at people over 55. The Silver Line operates the only confidential, free helpline for older people across the UK that’s open 24 hours a day, seven days a week, 365 days of the year. They also offer telephone friendship where we match volunteers with older people based on their interests, facilitated group calls, and help to connect people with local services in their area.
Telephone: 0800 4 70 80 90
Website: www.thesilverline.org.uk
The Mix
Aimed at people under 25. Their helpline is open between 4pm and 11pm, 7 days a week. They also run a crisis text service which is open 24 hours a day, 7 days a week.
Telephone: 0808 808 4994
E-mail: through the website.
Crisis text message service: Text THEMIX to 85258
Webchat: through the website. (4pm - 11pm, 7 days a week - chats may not be connected after 10:15pm)
Website: www. themix.org.uk
themix.org.uk
Mood Swings
Aimed at anyone affected by a mood disorder, including friends, families and carers.
Telephone: 0161 832 37 36
E-mail: [email protected]
Website: www.moodswings.org.uk
If you are in crisis you can contact the following text support service for help and support:
Shout
If you’re experiencing a personal crisis, are unable to cope and need support, text Shout to 85258. Shout can help with urgent issues such as suicidal thoughts, abuse or assault, self-harm, bullying and relationship challenges.
Text: Text Shout to 85258
Website: www.giveusashout.org/
Need more advice?
If you need more advice or information you can contact our Advice and Information Service.
Contact us Contact us
Serious Mental Illness Recovery: The Basics
AUG.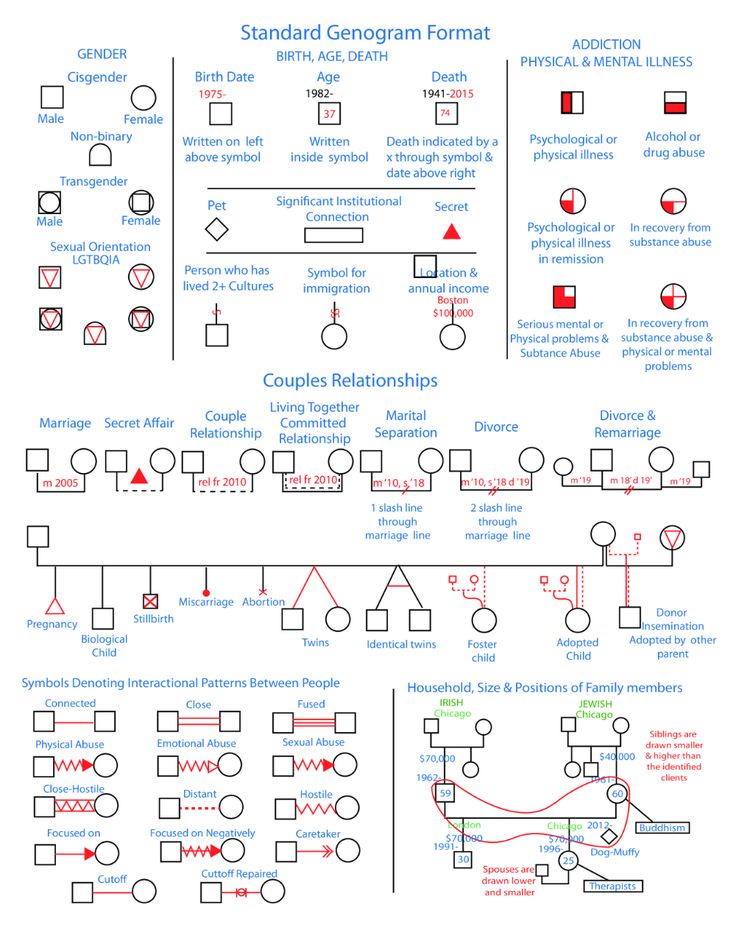 11, 2021
11, 2021
By Larry Davidson, Ph.D., and Katherine Ponte, B.A., J.D., MBA, CPRP
When managing serious mental illness (SMI), the recovery journey can be long and challenging. It often requires creative and prolonged efforts to build and maintain a full life, but many people do reach recovery. In fact, up to 65% of people living with SMI experience partial to full recovery over time.
The term “recovery” refers to the process of learning how to minimize the symptoms associated with SMI. Note that recovery does not mean symptoms stop entirely or that deficits disappear. Ultimately, recovery is not synonymous with “cured.” Rather, it means reaching a place where you are able to pursue a safe, dignified and meaningful life.
The cornerstones of recovery are self-determination, treatment, engagement with family and friends, work and hope. Loved ones play a critical role in a person’s recovery, especially when well-intentioned caregivers listen to and respect their loved one’s goals. Additionally, the guidance of competent, experienced and compassionate mental health practitioners can also be invaluable.
Additionally, the guidance of competent, experienced and compassionate mental health practitioners can also be invaluable.
While recovery may look different for different people, there are several basic strategies that can serve anyone looking to manage their illness. These basics may help you reach recovery more quickly and easily.
Maintaining Hope
Recovery is rarely achieved in the absence of hope. Its power cannot be overestimated. You must always try to maintain hope despite the challenges (including loss, stigma, discrimination) you face. Hope doesn’t have to come solely from internal strength; it can come from caregivers, friends, peers, people outside of a mental health context, and even animals or faith. Feeling supported, accepted and loved as a person of value and worth can foster and nurture hope.
Practicing Self-Determination
Recovery has to be pursued; it does not simply occur in response to medication or other treatments. That is why it is so important to make your own decisions and actively use treatment, services, supports or other resources. For example, preparing a Psychiatric Advance Directive, which states your treatment preferences in the event of a mental health crisis, can allow you to retain control over care even if you become impaired. As with any illness, you may have to self-advocate to ensure everyone in your care team respects your right to have a say in your care.
That is why it is so important to make your own decisions and actively use treatment, services, supports or other resources. For example, preparing a Psychiatric Advance Directive, which states your treatment preferences in the event of a mental health crisis, can allow you to retain control over care even if you become impaired. As with any illness, you may have to self-advocate to ensure everyone in your care team respects your right to have a say in your care.
Do not give up on your dreams. Identifying your life pursuits, such as living, working, learning and participating fully in the community, is an important recovery goal. After establishing these objectives, you can work with your providers and caregivers to make those goals a part of your care plan.
Starting Now
You should not delay the pursuit of recovery in the hopes that your symptoms will go away on their own. Progress typically occurs through a series of small steps, which may involve considerable effort, patience and persistence over time. These accomplishments become possible and noticeable if you set and achieve realistic and short-term, if not immediate, personal goals. Small, incremental steps can build on each other, positioning you to address more ambitious goals further down the line. Celebrating achievements, no matter how seemingly mundane, is an important part of the recovery process.
These accomplishments become possible and noticeable if you set and achieve realistic and short-term, if not immediate, personal goals. Small, incremental steps can build on each other, positioning you to address more ambitious goals further down the line. Celebrating achievements, no matter how seemingly mundane, is an important part of the recovery process.
Finding the Right Care
Finding caring, trusting, supportive relationships with a practitioner is critical for recovery. Practitioners should encourage and support your hopes, interests, assets, talents, energies, efforts and goals. To achieve these, you should discuss calculated risk-taking with your practitioner. A calculated risk is a carefully considered decision that could be beneficial but includes some degree of risk. For example, making the decision to change your treatment plan or medication regimen.
Care should be person-centered and you should hold an active role in your care. Accordingly, practitioners should engage your participation using a strengths-based approach.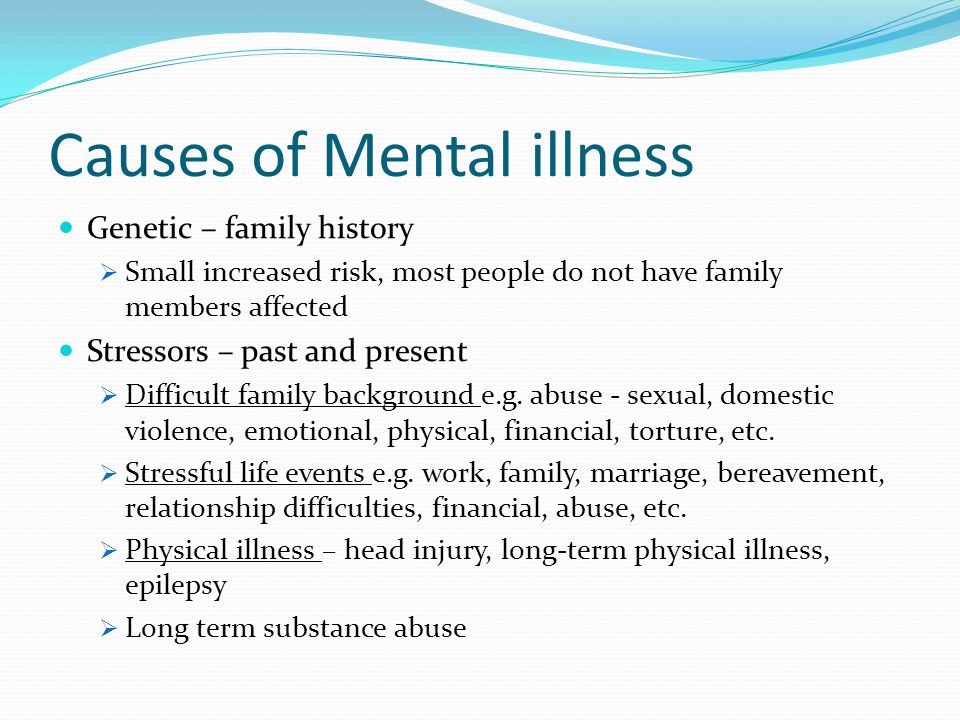 This approach, known as shared decision-making, is evidence-based and has been shown to improve outcomes.
This approach, known as shared decision-making, is evidence-based and has been shown to improve outcomes.
Care should also be grounded in your “life-context,” which acknowledges, builds on and appreciates your unique history, experiences, situations, developmental trajectory and aspirations. Care plans should be based on individualized, culturally sensitive, holistic and multidisciplinary considerations and developed in collaboration with you and your supporters each step of the way. Your care should focus on helping you live the life you want and choose.
Gathering Information on Community Factors
Practitioners should have adequate knowledge of community factors that may impact care, including opportunities, resources and potential barriers. These may relate to access to employment opportunities as well as employment disincentives that are built into programs for access to affordable housing and medical care. If practitioners cannot offer you guidance on these subjects, they should at least be able to share resources and provide referrals to people who can.
Coping with Stigma
Stigma is widespread, even among friends and family and within the mental health care system, including from practitioners themselves. The detrimental impact of stigma can be greater than that of the illness itself. Thus, you may need to develop coping strategies to manage stigma, particularly if you are experiencing self-stigma.
You might consider discussing how you are impacted by insensitive statements with those who use them. You could also consider limiting interaction, if possible, with people who may continue to stigmatize you. Talking to peers can also be helpful to process the way stigma affects you.
Engaging with Peer Support
Peer support can be invaluable. People living with a similar condition can help you normalize SMI, address loneliness and isolation, and offer acceptance and support. They also can provide insights based on their own struggles and achievements, and they can help take away some of the uncertainty of living with SMI by helping you understand what to expect.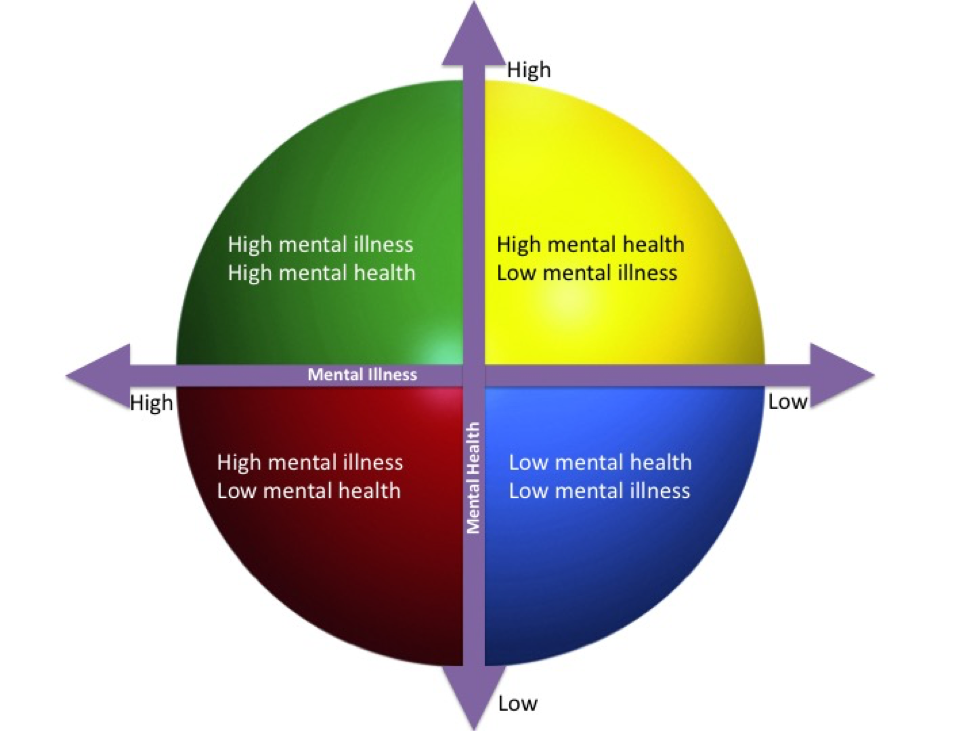 They can offer hope as a mentor who is a living example of the reality of recovery.
They can offer hope as a mentor who is a living example of the reality of recovery.
The recovery journey is never easy, but it is always worth it. When a person with SMI reaches recovery, they often regain their self-love, self-worth and self-esteem. Recovery can then free a person from stigma, shame and embarrassment. Perhaps most importantly, it can stop them from defining themselves merely by their illness.
Some people with SMI have to recognize that the greatest barrier to reaching recovery may be their own mindset. People who refuse to take back control of their lives (including their care) and refuse to take responsibility for their illness will find it more difficult to reach recovery. It is a great tragedy that so many never reach recovery because it is possible for so many more.
Ultimately, we all need more visible and promoted examples of everyday people living in recovery. The promise of eliminating stigma does offer hope, but recovery offers so much more.
Note: An extremely helpful recovery resource is: A Practical Guide to Recovery-Oriented Practice: Tools for Transforming Mental Health Care.
Larry Davidson, Ph.D., is a Professor of Psychiatry and Director of the Program for Recovery and Community Health at Yale University’s School of Medicine. He is the author and co-author of more than 450 publications on the processes of recovery and the development of innovative policies and programs to promote the recovery and community inclusion of individuals with serious mental illnesses and addictions.
Katherine Ponte is happily living in recovery from severe bipolar I disorder. She’s the Founder of ForLikeMinds’ mental illness peer support community, BipolarThriving: Recovery Coaching and Psych Ward Greeting Cards. Katherine is also a faculty member of the Yale University Program for Recovery and Community Health and has authored ForLikeMinds: Mental Illness Recovery Insights.
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness.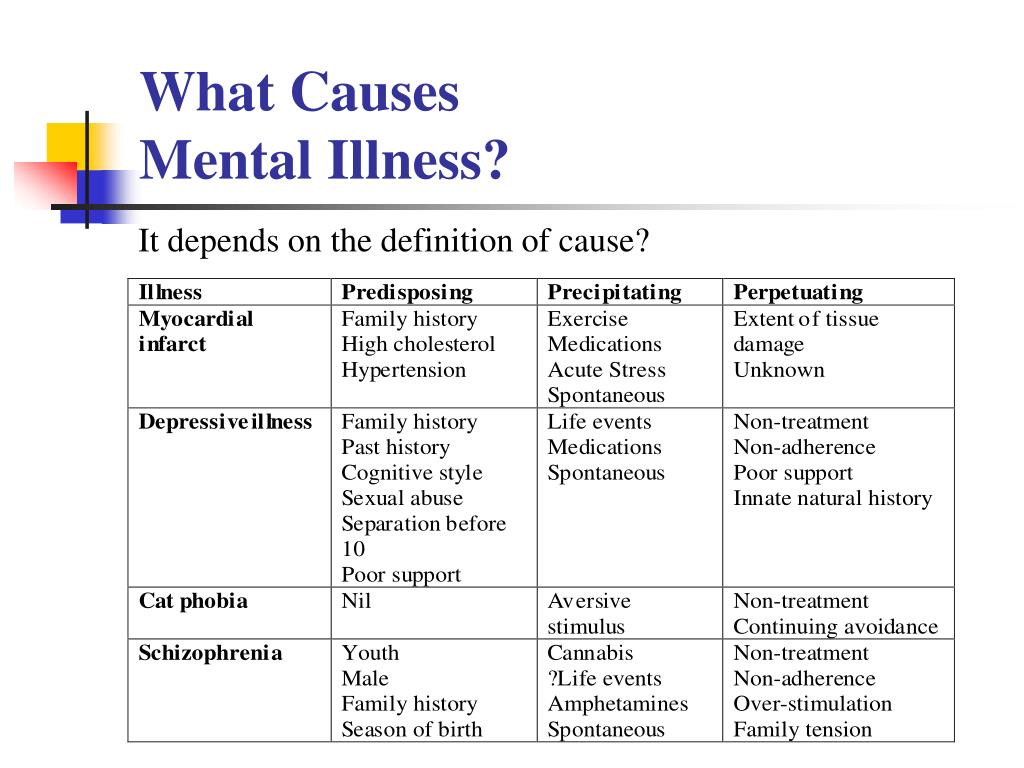 Most importantly: We feature your voices.
Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
LEARN MORE
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.
This booklet deals with signs,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident. nine0024
- I jump on the spot and feel uneasy at any sudden movement or surprise.
 I feel alert all the time.
I feel alert all the time. - It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension. nine0024
PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment. nine0003
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event. you try to hold on away from anything that might remind you of the experience.
you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last? nine0011
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this condition? nine0011
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men.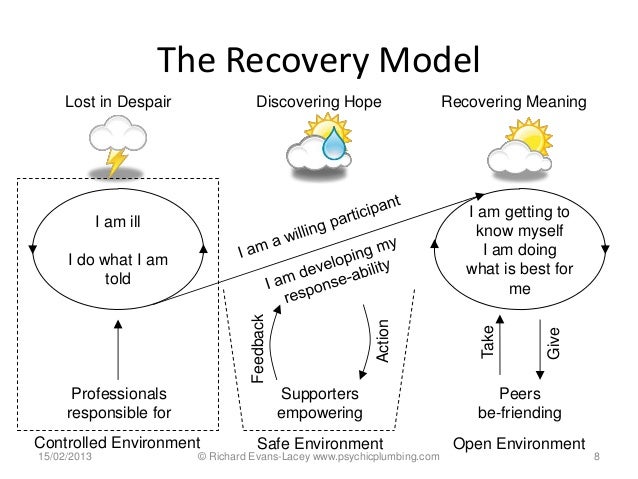 The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse. nine0003
The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse. nine0003
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.
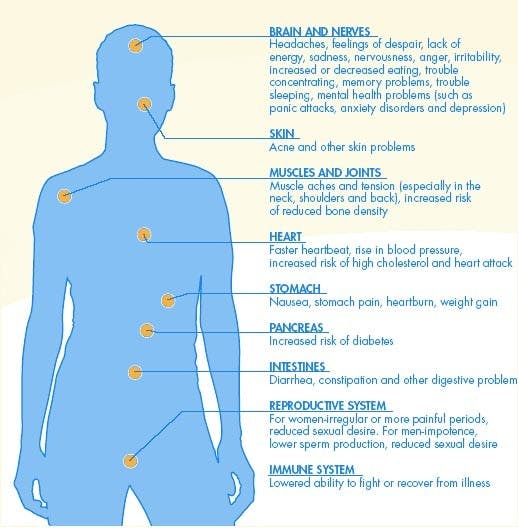
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD. nine0003
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What should I do to help myself in this situation? nine0011
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses. nine0003
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
Your doctor may prescribe medicine to help reduce your fear or tension.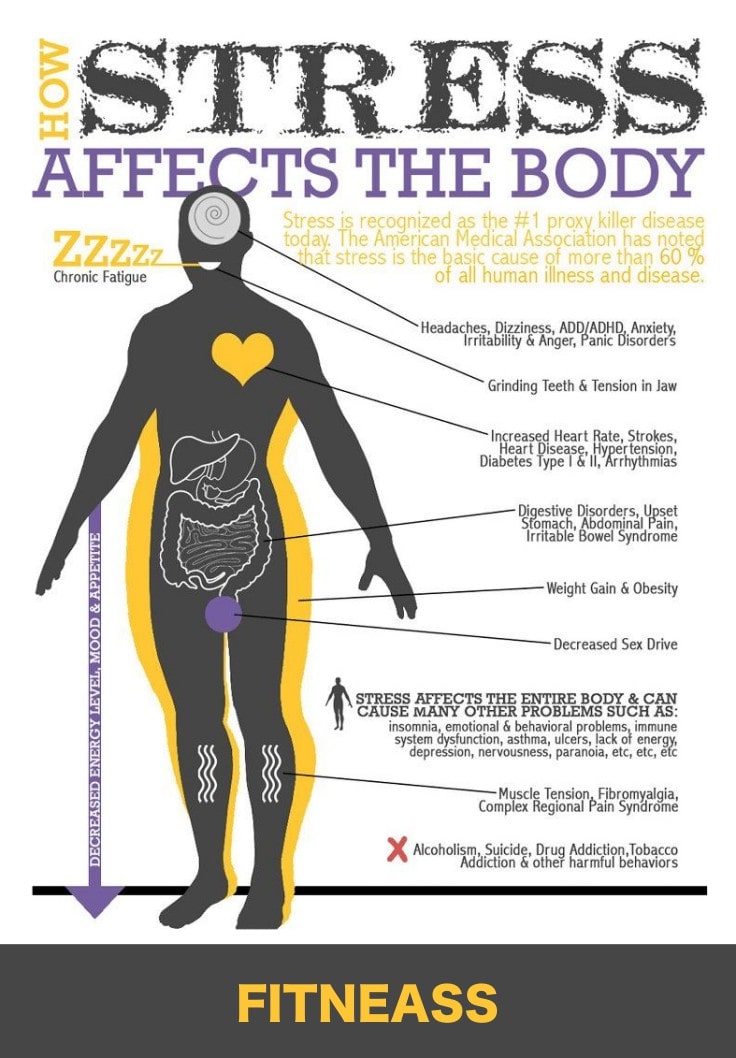 However, it should be borne in mind that usually several weeks before the medicine starts to work. nine0003
However, it should be borne in mind that usually several weeks before the medicine starts to work. nine0003
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories. nine0003
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD. nine0003
You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD. nine0003
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is. nine0003
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military.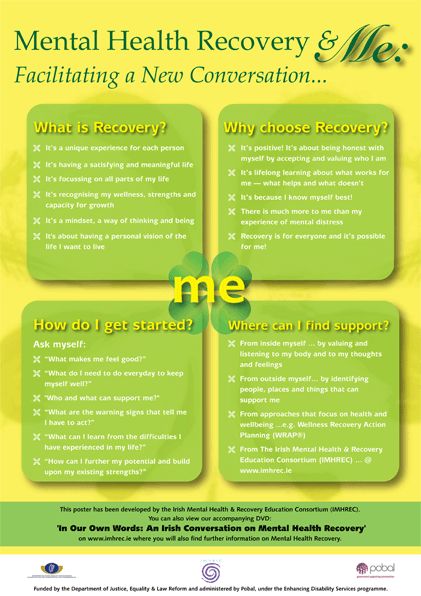 MST can happen with men and women, and can occur in peacetime, during war training or during the war.
MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear. The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease. nine0003
The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease. nine0003
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. nine0184 1
nine0184 1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. nine0184 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). nine0184 4
nine0184 4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress. nine0184 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. nine0184 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't. nine0003
nine0184 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't. nine0003
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate. nine0003
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced. NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced. 9
9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. nine0184 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. nine0184 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation. First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. nine0184 12
First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. nine0184 12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal. nine0003
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease.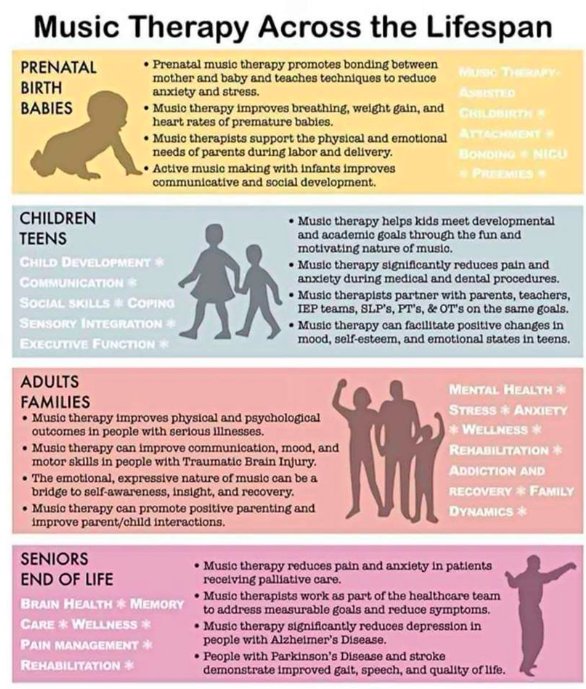 During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment. nine0003
During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment. nine0003
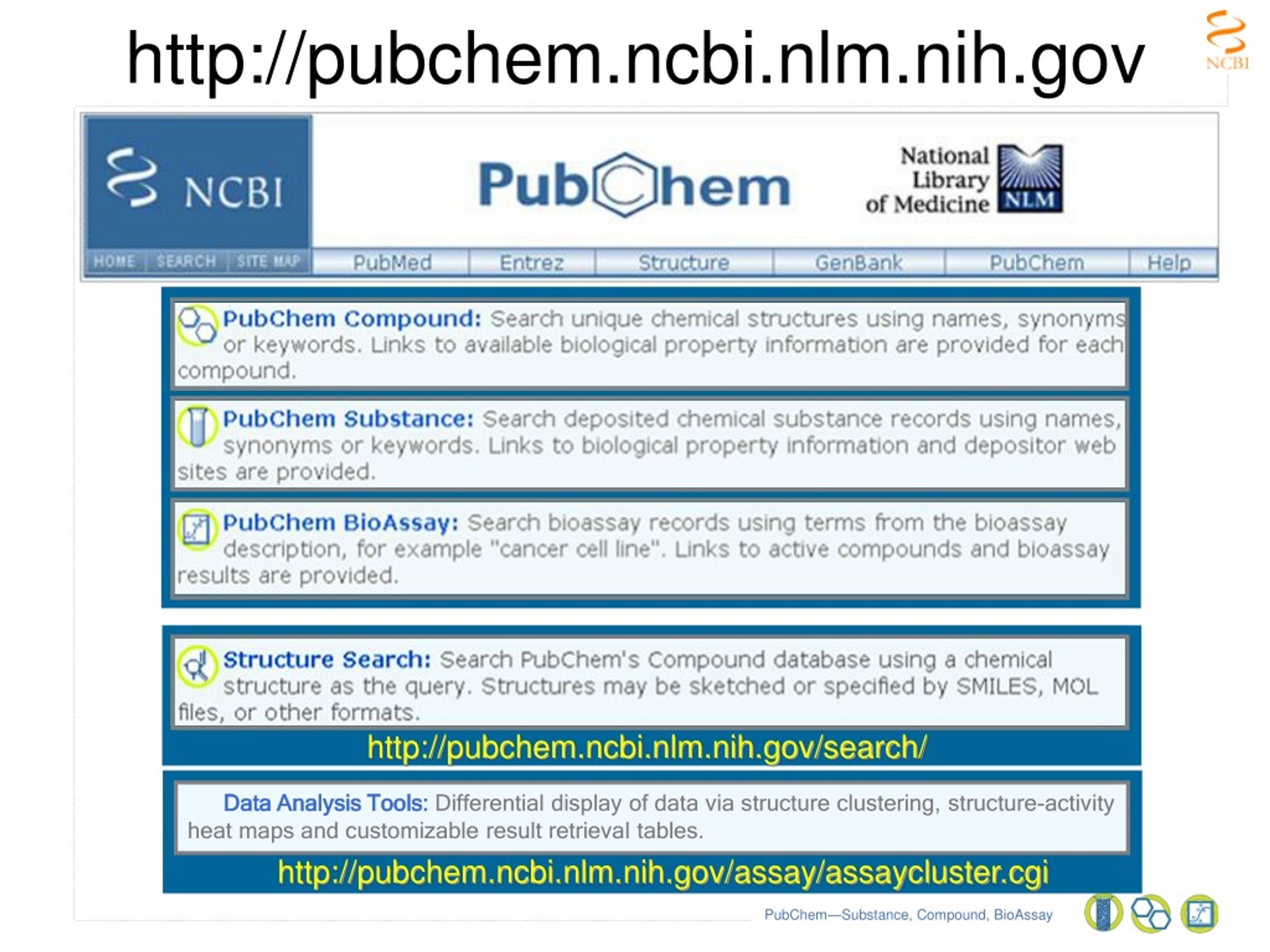
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: nimhinfo@nih. gov
gov
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www.ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction.
 Nature. Nov 7 2002;420(6911):70-74.
Nature. Nov 7 2002;420(6911):70-74. - 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus. Nat Neurosci. Mar 2005;8(3):365-371.
- Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711. nine0024
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder.
 Biol Psychiatry. Feb 3 2006.
Biol Psychiatry. Feb 3 2006. - Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
- Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634. nine0024
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F. Hogan, PhD
Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Department of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www.omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Department of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
What mental illnesses are inherited - Atlant Medical Center
Are mental illnesses hereditary? This question worries many parents. After all, it is very scary to “reward” your child with a mental disorder. nine0003
After all, it is very scary to “reward” your child with a mental disorder. nine0003
How mental illnesses are transmitted
The fact that mental illness can be inherited has been noticed for a long time. Today, geneticists confirm: indeed, mental disorders are more likely to appear in a child in a family where a relative suffered from a similar illness. And the reason for this are violations in the structure of genes.
There is such a thing as the coefficient of hereditary risk. The higher this coefficient, the higher the likelihood that the child will inherit the disease of relatives. nine0003
Only some mental illnesses are directly related to breakdowns in the genes, for example, Huntington's chorea, the hereditary risk coefficient of which is 5000. For comparison, for such a mental illness as schizophrenia, it is 9.
How does the degree of relationship affect hereditary diseases?
The risk of developing a mental illness depends on the degree of relationship with a sick family member and on the number of sick relatives.
The highest probability of transmission of the disease in identical twins, followed by 1st degree relationship (parents, children, brothers, sisters). In 2nd degree relatives, the risk is significantly reduced
So, with schizophrenia, which is present in the mother and father, the probability of its occurrence in children is 46%, if one parent is sick - about 13%, if the grandfather or grandmother is sick - 5%.
What mental illnesses are most often inherited
1. Disorders of the mental development of children
- Attention deficit hyperactivity disorder (ADHD) is manifested by impulsivity, difficulty concentrating, increased physical activity. Often this disorder is combined with depression, behavioral disorders.
- Dyslexia - the inability to read, compare what is written with speech in some cases is hereditary.
- Autism is a severe mental disorder, which is expressed in violation of social adaptation. An autistic child is closed, he does not want to communicate with the outside world, he exists in his personal space.
 He does not tolerate any change, he has his own rituals, which he strictly observes. He constantly repeats stereotypical movements (rocking, bouncing) or the same phrases. nine0024
He does not tolerate any change, he has his own rituals, which he strictly observes. He constantly repeats stereotypical movements (rocking, bouncing) or the same phrases. nine0024
Autism is usually diagnosed in the first three years of a child's life.
It is believed that the role of heredity in the occurrence of this disease is great.
2. Schizophrenia
This is a mental illness, which is characterized by disturbances in thinking, perception of the world, inappropriate behavior and an abnormal reaction to stimuli. The disease may be accompanied by agitation, delusions, hallucinations. Patients are prone to depression and suicidal. nine0003
As a rule, the onset of the disease falls on the age of 20-22 to 30 years.
Heredity plays a significant role in the occurrence of this disease, but other factors are no less important: complications during gestation, difficult childbirth in the mother, infections, difficult psycho-emotional situations, and even birth in winter.
3. Affective bipolar disorder
Otherwise, this mental illness is called manic-depressive psychosis. It proceeds with an alternation of phases: depression and excitement, sometimes with aggression. There may be gaps between these phases. nine0003
4. Alzheimer's disease
This disease develops after the age of 65 and is expressed first in forgetfulness, difficulty concentrating. Then there is confusion, loss of orientation in space. Irritability, unmotivated aggression appear, speech is disturbed. Dementia develops.
Rarely enough, the disease begins earlier, and here the hereditary factor, the pathological gene, plays a significant role. nine0003
Other hereditary mental illnesses:
- epilepsy;
- psychopathy;
- alcohol dependence;
- dementia;
- Down syndrome;
- Huntington's chorea;
- "cat cry" syndrome;
- Klinefelter's syndrome.
All of these mental illnesses can be inherited.