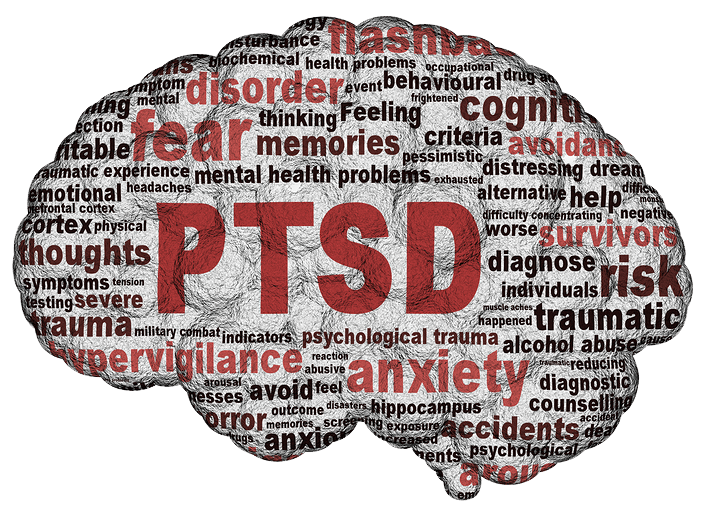
Ptsd repressed memory
Signs, Symptoms, and What to Do
The experience and aftermath of traumatic events can affect your memory. But can the memory of a trauma be truly repressed?
The theory of repressed memories focuses on a traumatic event that a person may not remember at all, or may not remember until after the event.
Repressed memories are memories that aren’t easily accessed consciously, says Saba Harouni Lurie, licensed marriage and family therapist, licensed art therapist, and founder of Los Angeles’ Take Root Therapy.
Remembering a repressed memory “could begin with dream-like memories,” says psychologist Pauline Peck, PhD. It’s “something that doesn’t feel like a coherent narrative. You might have bits and pieces of a memory or have a strong felt ‘sense.’”
“Trauma is stored as fragments, not as a linear story,” Peck says. “Sometimes it just takes being curious and, most importantly, being supported so you feel like you can uncover whatever might be there.”
The concept of repressed memory originated with Sigmund Freud, whose understanding of human psychology focused heavily on the unconscious and subconscious mind.
Freud developed the idea of repression during his work with psychoanalysis. Freud believed that repression was a defense mechanism in the face of traumatic experiences.
Freud’s theory of repression originally thought of repression as a response to traumatic stress, then termed “hysteria.” According to Freud, this could occur with excessive stress, even if not considered physically threatening or traumatic.
However, Freud’s theory of repression is highly controversial and remains unproven.
The concepts of repression and suppression are often mixed up.
Repression is related to large-scale and deeply impactful experiences. Suppression, on the other hand, is typically related to more temporary thoughts and emotions, such as anxiety or anger. Someone may intentionally suppress certain memories, but it can also occur automatically in people who suppress things often.
Since the 1970s, the concept of repressed memories has been debated. Peck points to a 2019 literature review that discusses this long-standing controversy, known as “memory wars.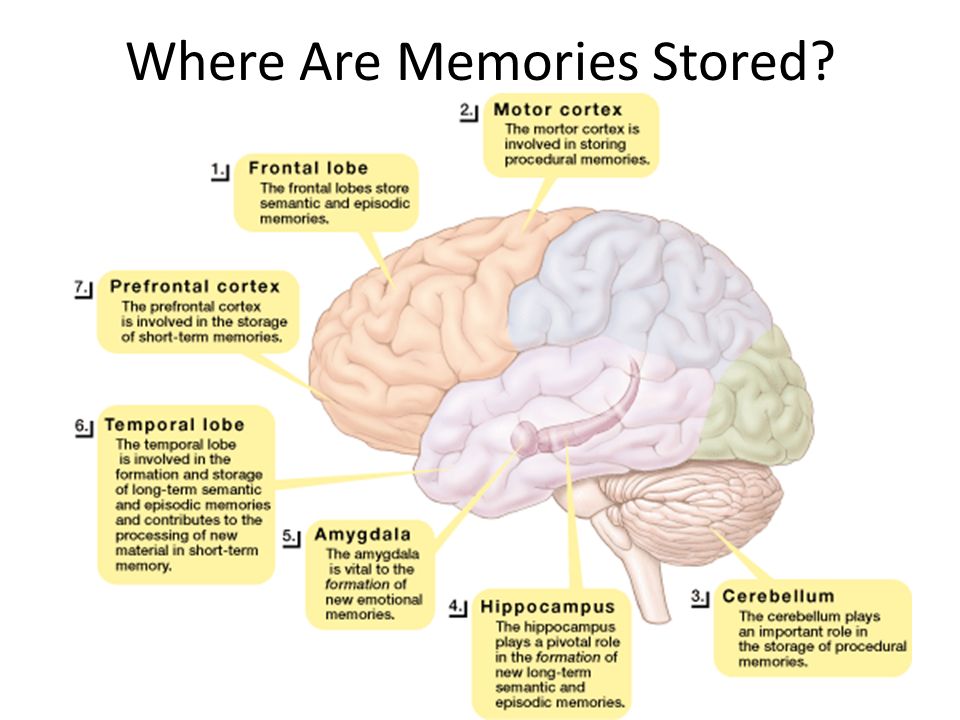 ”
”
The difference in opinion is driven by a few different narratives, including the idea of “planted memories,” in which a therapist — or in some cases, a legal prosecutor — may suggest forgotten memories.
Experts are split about repressed memories and trauma versus other explanations. But many agree that the brain has varied pathways to protection, including storing memories in ways that may not be completely remembered at all times.
The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) includes the idea of dissociative amnesia, which is defined as the inability to recall autobiographical information.
According to the DSM-5, this information is:
- traumatic or stressful
- inconsistent with ordinary forgetting
- successfully stored
- involves a period of time when the patient is unable to recall the experience
- is not caused by a substance or neurological condition, and
- always has the potential of being reversed
Because this definition is essentially the same as that of repressed memories, there’s continued skepticism about the phenomenon’s presence, despite the change in name and inclusion in the manual.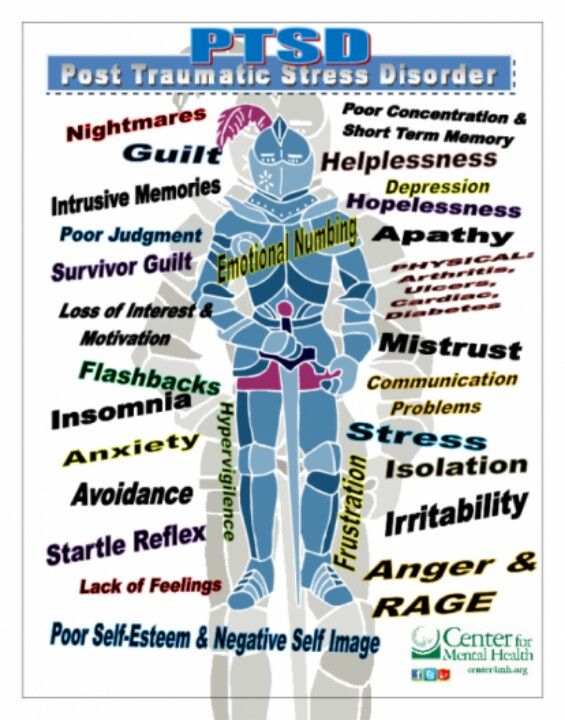
Arguments in favor of the validity of the concept of repressed memories include other memory-related phenomena to support the experience, such as:
Retrieval inhibition
The concept of retrieval inhibition states that remembering some information can lead to forgetting other information.
A connection between the two suggests that you can choose to not think about an event. This decision, in addition to remembering separate, less traumatic memories, makes the traumatic ones less accessible.
This is an idea that’s been discussed, but it hasn’t been studied enough in controlled settings to determine if it’s a valid explanation. There’s currently no evidence that says retrieval inhibition is more likely to occur in traumatic settings.
Motivated forgetting
Motivated forgetting means you can choose to intentionally forget something.
However, there are arguments against this phenomenon’s connection to memory repression. There’s no evidence that the memory is unavailable and then later remembered or retrieved.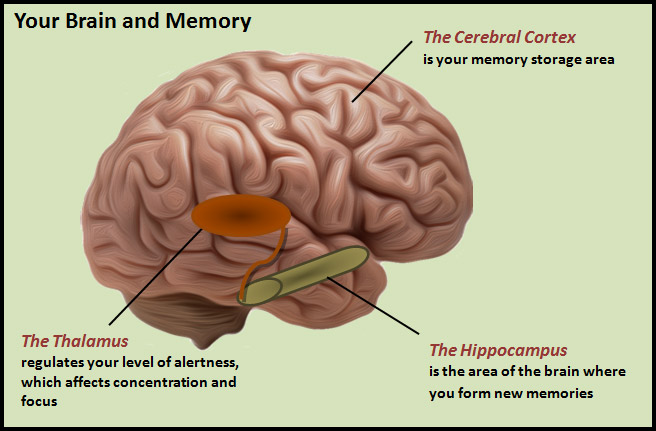
State-dependent remembering
This theory states that memories are best unlocked when the person is in a similar state of consciousness as when the event happened.
This concept was studied in rats, and the researchers tested the idea that traumatic events are held in separate neural networks than nontraumatic ones.
No definitive conclusion
Experts agree that more research is needed to come to a definitive conclusion. They also agree that there’s no plausible way to do so in an ethical manner.
Lurie says that while memories aren’t always the most reliable, this doesn’t take away from the need to honor people’s lived experiences.
“As humans, yes, our memories are not always reliable,” Lurie says. “But the experience that we had is what’s really going to be important, meaning the way that we experienced it [the trauma] in our body.”
Peck says that dissociating or keeping memories and experiences at arm’s length is the brain’s way of keeping us safe. “It’s a safety and survival mechanism. We repress all sorts of things until we are safe enough to be able to deal with them,” she says.
“It’s a safety and survival mechanism. We repress all sorts of things until we are safe enough to be able to deal with them,” she says.
Lurie says she had a memory from middle school where both the halls and lockers looked and felt huge. But when she returned as an adult, she realized that they were average-sized the entire time.
“Our body experiences things as it did at the time,” she says. “Maybe the way that it’s saved in memory is not 100% accurate, but the way that we experienced it matters and the impact that it’s had.”
Peck says that those who disclose their experiences and are met with negative responses are more likely to develop post-traumatic stress disorder (PTSD). This may increase the chances of repressed memory.
“I think it is hard for people to think about sexual abuse in general, as it elicits a lot of trauma symptoms,” Peck says. “Being in a safe therapeutic environment and learning good coping skills can help the person process the experience and cope with it more effectively.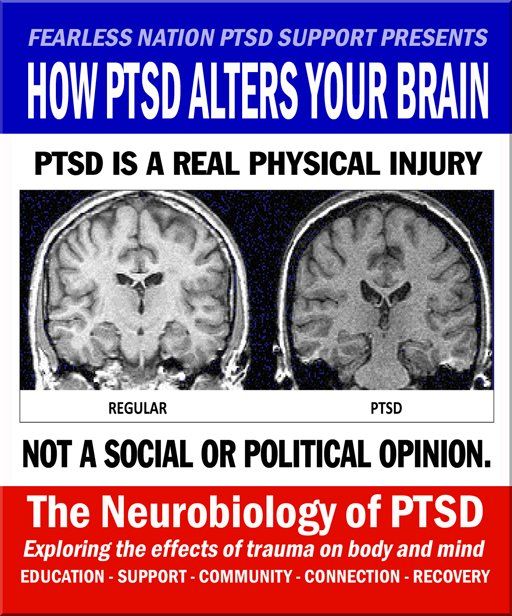 ”
”
Lurie, who believes there’s some validity to the concept of repressed memories, says that our bodies are hardwired to survive and that survival can lead to altered relationships.
“The body has different ways of responding to intense trauma,” Lurie says. “And one of the ways that we may manage and just try to survive [is that] we can repress memories of things that were really shocking to our system.”
Lurie says our body may respond to trauma as if it’s remembering things that we may not necessarily remember clearly.
When someone encounters a trigger for remembering a traumatic event, that may trigger a physiological “fight, flight, or freeze” response. This might be felt in the body as:
- the urge to escape (flight)
- increased heart rate
- muscle tension
- increased breathing
“There are things that maybe make us a bit uncomfortable or we disengage from, but we don’t know necessarily why,” she says. “And that’s where the repressed memories may be coming to the surface.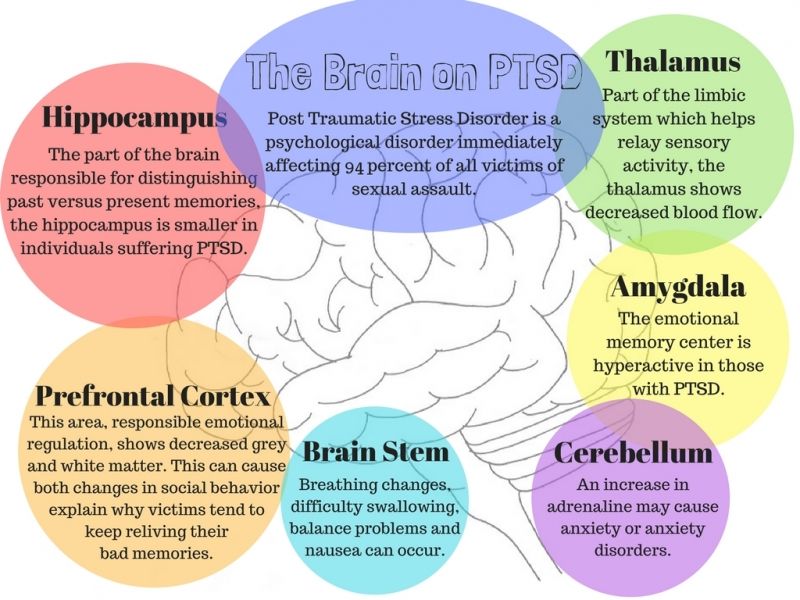 ”
”
“Even if our mind doesn’t have access to said memory, our body does, and it’s trying to keep us safe in whatever way it can,” Lurie says. “That might mean both repressing the memory and also having us withdraw from certain activities or situations.”
If you’re navigating memories of trauma, especially if they’ve recently reemerged, Lurie suggests tapping into journaling as a way to calm yourself.
“The type of journaling that I’m referring to is more like stream of consciousness journaling,“ Lurie says. “So you’re not worried about spelling, you’re not worried about ‘If I were to read this to someone, what if it didn’t make sense to them?’”
When it comes to clinical support, Peck suggests connecting with a professional who has substantial experience working with trauma and the ways it can show up.
“Being a trauma-informed clinician requires a lot of training. I would not suggest that someone who has not worked with these types of traumas begin treating them without the proper training, supervision, and/or consultation,” Peck says.
“Somatic modalities that incorporate the body at some level are most useful, as they address the holistic impact of the trauma,” she says.
Other suggestions for navigating and processing traumatic and repressed memories include:
- individual therapy modalities, such as Eye Movement Desensitization and Reprocessing (EMDR) therapy or cognitive processing therapy (CPT)
- group therapy
- yoga
- meditation
- art as therapy or expression
These “won’t help you resolve the trauma,” Lurie says, “but they can help your body feel safe, even if you’re not necessarily feeling safe in the moment due to a past experience or a past trauma.”
Repressed memories may occur after a traumatic event. Some people have experiences of remembering at a later date.
There’s controversy over the validity of the theory. Some experts argue that having less memory of a traumatic event doesn’t line up with what we know of the memory.
Despite the lack of consensus among experts and clinicians, honoring your experience is important, alongside getting the support you need to move through this process.
If you’re looking for a therapist but aren’t sure where to start, Psych Central’s How to Find Mental Health Support resource can help.
Signs, Symptoms, and What to Do
The experience and aftermath of traumatic events can affect your memory. But can the memory of a trauma be truly repressed?
The theory of repressed memories focuses on a traumatic event that a person may not remember at all, or may not remember until after the event.
Repressed memories are memories that aren’t easily accessed consciously, says Saba Harouni Lurie, licensed marriage and family therapist, licensed art therapist, and founder of Los Angeles’ Take Root Therapy.
Remembering a repressed memory “could begin with dream-like memories,” says psychologist Pauline Peck, PhD. It’s “something that doesn’t feel like a coherent narrative. You might have bits and pieces of a memory or have a strong felt ‘sense.’”
“Trauma is stored as fragments, not as a linear story,” Peck says. “Sometimes it just takes being curious and, most importantly, being supported so you feel like you can uncover whatever might be there.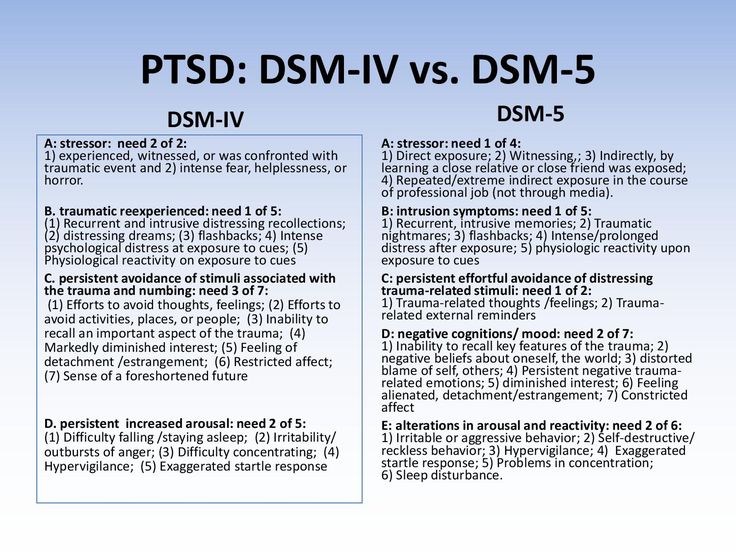 ”
”
The concept of repressed memory originated with Sigmund Freud, whose understanding of human psychology focused heavily on the unconscious and subconscious mind.
Freud developed the idea of repression during his work with psychoanalysis. Freud believed that repression was a defense mechanism in the face of traumatic experiences.
Freud’s theory of repression originally thought of repression as a response to traumatic stress, then termed “hysteria.” According to Freud, this could occur with excessive stress, even if not considered physically threatening or traumatic.
However, Freud’s theory of repression is highly controversial and remains unproven.
The concepts of repression and suppression are often mixed up.
Repression is related to large-scale and deeply impactful experiences. Suppression, on the other hand, is typically related to more temporary thoughts and emotions, such as anxiety or anger. Someone may intentionally suppress certain memories, but it can also occur automatically in people who suppress things often.
Since the 1970s, the concept of repressed memories has been debated. Peck points to a 2019 literature review that discusses this long-standing controversy, known as “memory wars.”
The difference in opinion is driven by a few different narratives, including the idea of “planted memories,” in which a therapist — or in some cases, a legal prosecutor — may suggest forgotten memories.
Experts are split about repressed memories and trauma versus other explanations. But many agree that the brain has varied pathways to protection, including storing memories in ways that may not be completely remembered at all times.
The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) includes the idea of dissociative amnesia, which is defined as the inability to recall autobiographical information.
According to the DSM-5, this information is:
- traumatic or stressful
- inconsistent with ordinary forgetting
- successfully stored
- involves a period of time when the patient is unable to recall the experience
- is not caused by a substance or neurological condition, and
- always has the potential of being reversed
Because this definition is essentially the same as that of repressed memories, there’s continued skepticism about the phenomenon’s presence, despite the change in name and inclusion in the manual.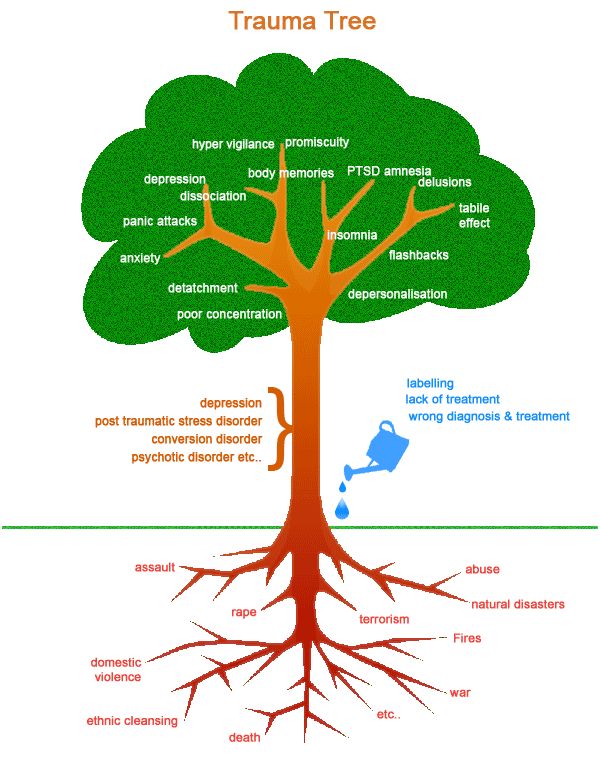
Arguments in favor of the validity of the concept of repressed memories include other memory-related phenomena to support the experience, such as:
Retrieval inhibition
The concept of retrieval inhibition states that remembering some information can lead to forgetting other information.
A connection between the two suggests that you can choose to not think about an event. This decision, in addition to remembering separate, less traumatic memories, makes the traumatic ones less accessible.
This is an idea that’s been discussed, but it hasn’t been studied enough in controlled settings to determine if it’s a valid explanation. There’s currently no evidence that says retrieval inhibition is more likely to occur in traumatic settings.
Motivated forgetting
Motivated forgetting means you can choose to intentionally forget something.
However, there are arguments against this phenomenon’s connection to memory repression. There’s no evidence that the memory is unavailable and then later remembered or retrieved.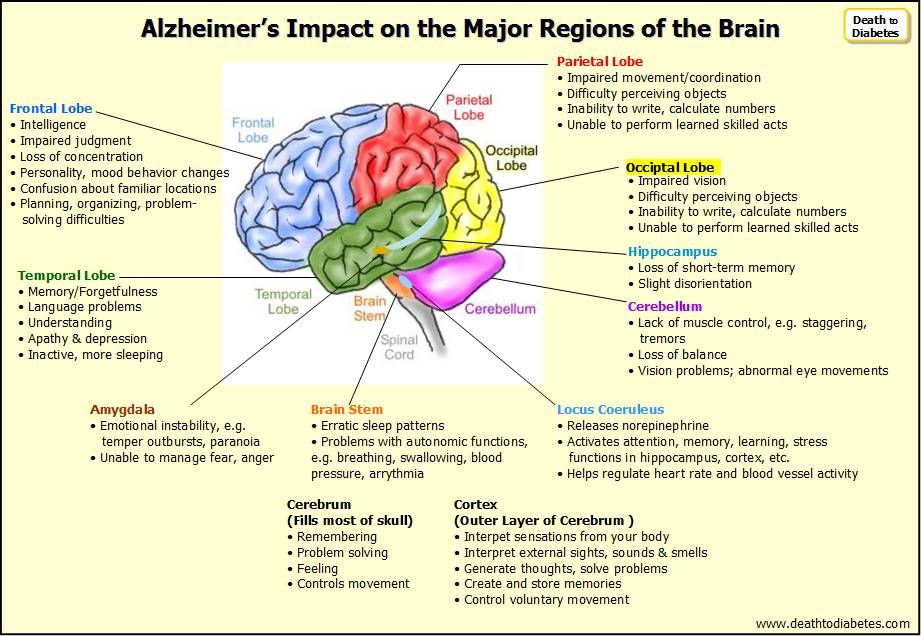
State-dependent remembering
This theory states that memories are best unlocked when the person is in a similar state of consciousness as when the event happened.
This concept was studied in rats, and the researchers tested the idea that traumatic events are held in separate neural networks than nontraumatic ones.
No definitive conclusion
Experts agree that more research is needed to come to a definitive conclusion. They also agree that there’s no plausible way to do so in an ethical manner.
Lurie says that while memories aren’t always the most reliable, this doesn’t take away from the need to honor people’s lived experiences.
“As humans, yes, our memories are not always reliable,” Lurie says. “But the experience that we had is what’s really going to be important, meaning the way that we experienced it [the trauma] in our body.”
Peck says that dissociating or keeping memories and experiences at arm’s length is the brain’s way of keeping us safe. “It’s a safety and survival mechanism. We repress all sorts of things until we are safe enough to be able to deal with them,” she says.
“It’s a safety and survival mechanism. We repress all sorts of things until we are safe enough to be able to deal with them,” she says.
Lurie says she had a memory from middle school where both the halls and lockers looked and felt huge. But when she returned as an adult, she realized that they were average-sized the entire time.
“Our body experiences things as it did at the time,” she says. “Maybe the way that it’s saved in memory is not 100% accurate, but the way that we experienced it matters and the impact that it’s had.”
Peck says that those who disclose their experiences and are met with negative responses are more likely to develop post-traumatic stress disorder (PTSD). This may increase the chances of repressed memory.
“I think it is hard for people to think about sexual abuse in general, as it elicits a lot of trauma symptoms,” Peck says. “Being in a safe therapeutic environment and learning good coping skills can help the person process the experience and cope with it more effectively. ”
Lurie, who believes there’s some validity to the concept of repressed memories, says that our bodies are hardwired to survive and that survival can lead to altered relationships.
“The body has different ways of responding to intense trauma,” Lurie says. “And one of the ways that we may manage and just try to survive [is that] we can repress memories of things that were really shocking to our system.”
Lurie says our body may respond to trauma as if it’s remembering things that we may not necessarily remember clearly.
When someone encounters a trigger for remembering a traumatic event, that may trigger a physiological “fight, flight, or freeze” response. This might be felt in the body as:
- the urge to escape (flight)
- increased heart rate
- muscle tension
- increased breathing
“There are things that maybe make us a bit uncomfortable or we disengage from, but we don’t know necessarily why,” she says. “And that’s where the repressed memories may be coming to the surface.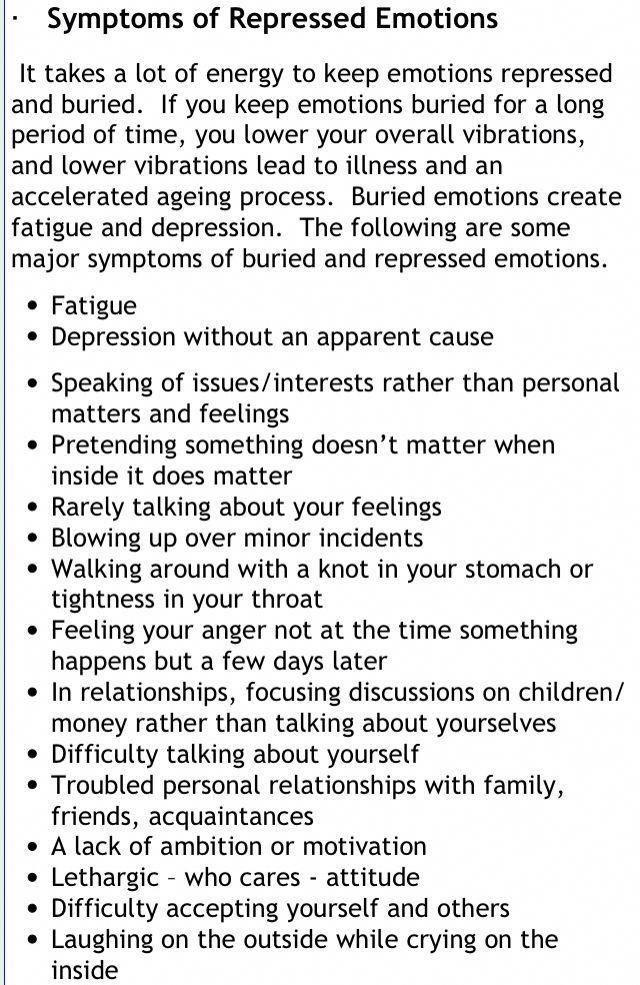 ”
”
“Even if our mind doesn’t have access to said memory, our body does, and it’s trying to keep us safe in whatever way it can,” Lurie says. “That might mean both repressing the memory and also having us withdraw from certain activities or situations.”
If you’re navigating memories of trauma, especially if they’ve recently reemerged, Lurie suggests tapping into journaling as a way to calm yourself.
“The type of journaling that I’m referring to is more like stream of consciousness journaling,“ Lurie says. “So you’re not worried about spelling, you’re not worried about ‘If I were to read this to someone, what if it didn’t make sense to them?’”
When it comes to clinical support, Peck suggests connecting with a professional who has substantial experience working with trauma and the ways it can show up.
“Being a trauma-informed clinician requires a lot of training. I would not suggest that someone who has not worked with these types of traumas begin treating them without the proper training, supervision, and/or consultation,” Peck says.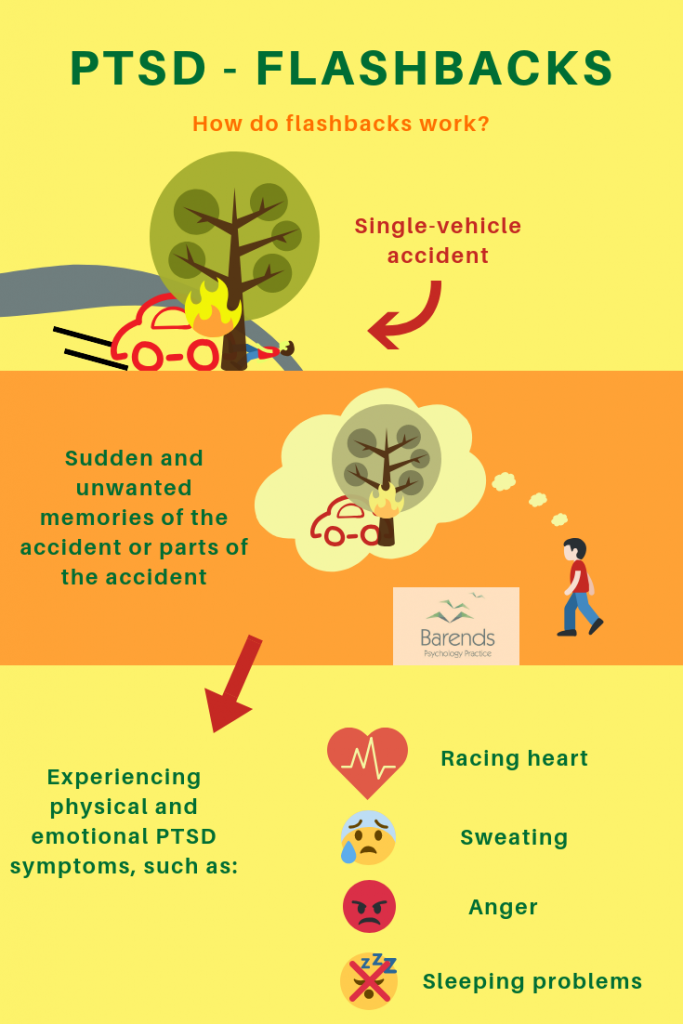
“Somatic modalities that incorporate the body at some level are most useful, as they address the holistic impact of the trauma,” she says.
Other suggestions for navigating and processing traumatic and repressed memories include:
- individual therapy modalities, such as Eye Movement Desensitization and Reprocessing (EMDR) therapy or cognitive processing therapy (CPT)
- group therapy
- yoga
- meditation
- art as therapy or expression
These “won’t help you resolve the trauma,” Lurie says, “but they can help your body feel safe, even if you’re not necessarily feeling safe in the moment due to a past experience or a past trauma.”
Repressed memories may occur after a traumatic event. Some people have experiences of remembering at a later date.
There’s controversy over the validity of the theory. Some experts argue that having less memory of a traumatic event doesn’t line up with what we know of the memory.
Despite the lack of consensus among experts and clinicians, honoring your experience is important, alongside getting the support you need to move through this process.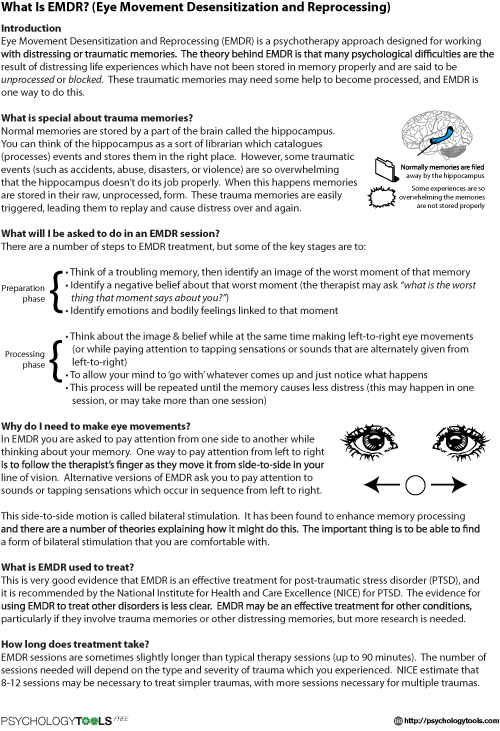
If you’re looking for a therapist but aren’t sure where to start, Psych Central’s How to Find Mental Health Support resource can help.
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.
This booklet deals with signs,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident.
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension.
PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment.
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event. you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last?
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this condition?
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men. The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.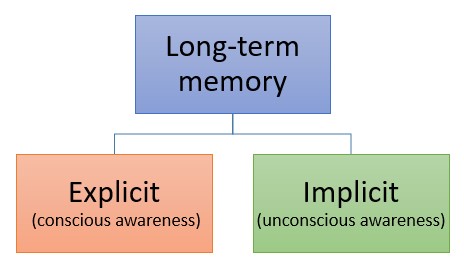
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD.
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What should I do to help myself in this situation?
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
Your doctor may prescribe medicine to help reduce your fear or tension. However, it should be borne in mind that usually several weeks before the medicine starts to work.
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite.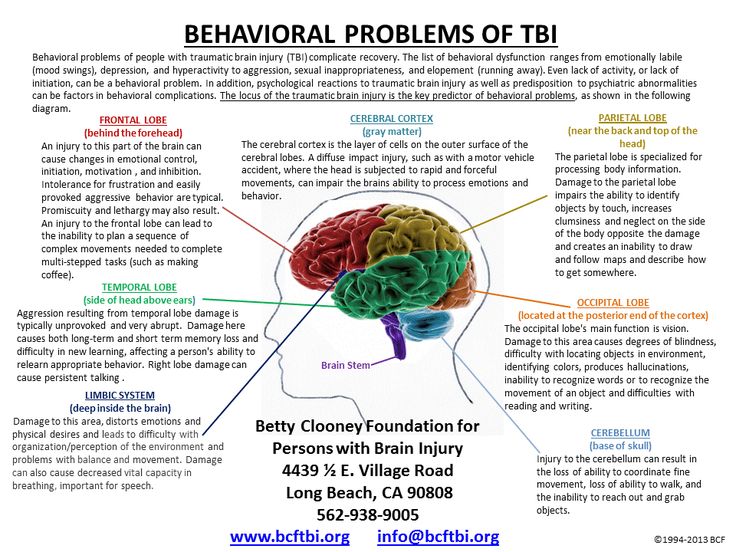 Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military. MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel.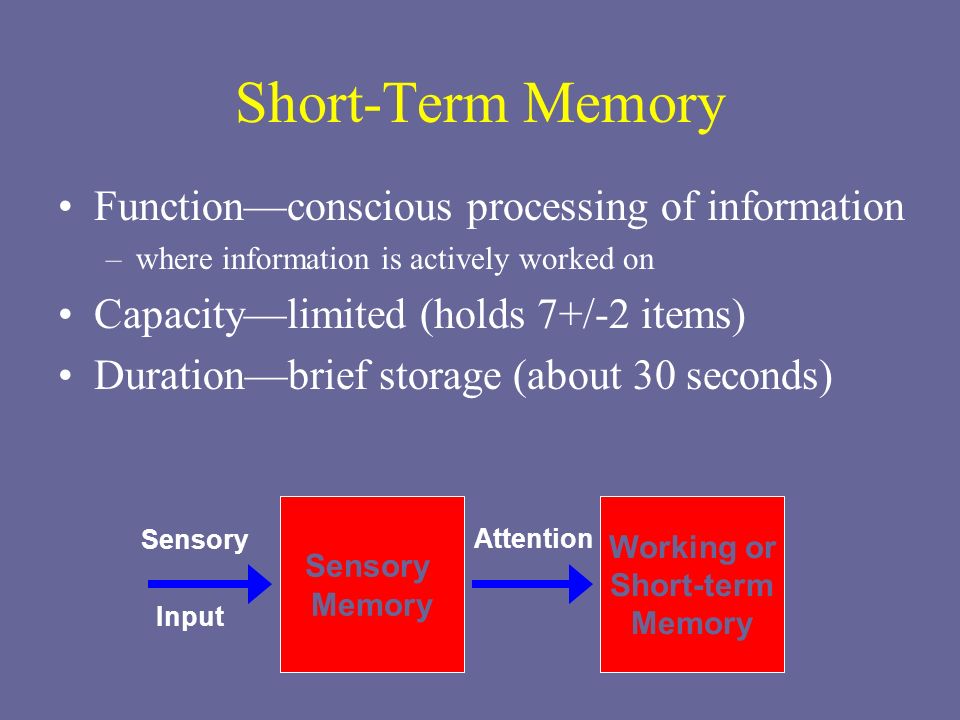 If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear. The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories.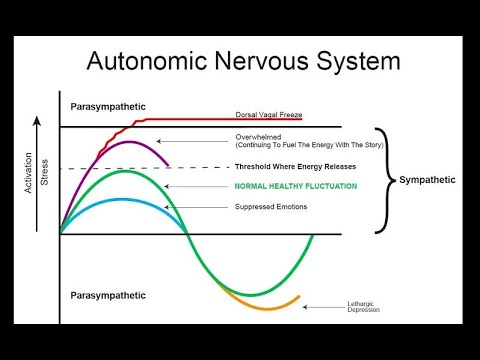 During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). 4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress. 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate.
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced. NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced. 9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation. First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal.
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease. During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: [email protected]
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www.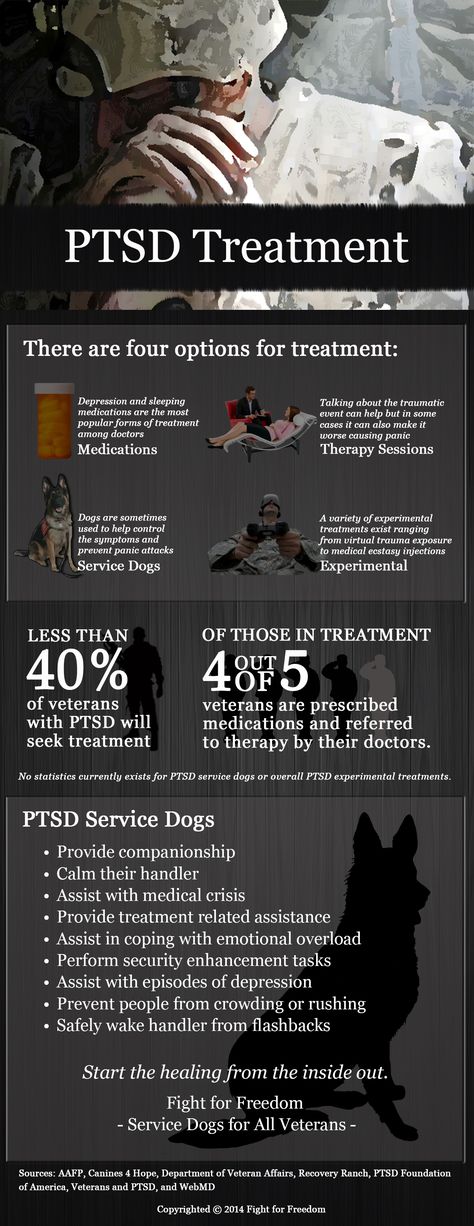 ncptsd.va.gov
ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction. Nature. Nov 7 2002;420(6911):70-74.
- 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus.
 Nat Neurosci. Mar 2005;8(3):365-371.
Nat Neurosci. Mar 2005;8(3):365-371. - Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711.
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder. Biol Psychiatry. Feb 3 2006.
- Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear.
 Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
Arch Gen Psychiatry. Nov 2004;61(11):1136-1144. - Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634.
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F. Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Division of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www.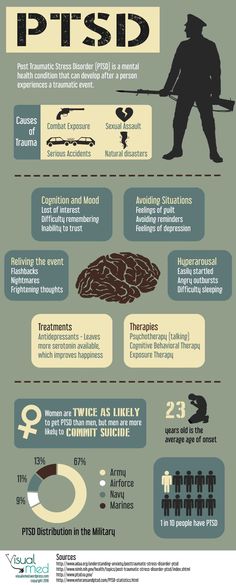 omh.ny.gov
omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Division of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
What is PTSD, symptoms and treatment of post-traumatic stress disorder in the article by psychotherapist Seregin D.
 A.
A. Above the article by the doctor Seryogin Dmitry Alekseevich worked literary editor Elena Berezhnaya, science editor Sergey Fedosov
Publication date 14 March 2018Updated 26 April 2021
Definition of disease. Causes of illness
Post-traumatic stress disorder (PTSD) is a mental disorder that can develop after a person is subjected to a traumatic experience (such as sexual assault, war, car accidents, or other threats to a person's life). [1]
Causes of PTSD
Most people who have experienced a traumatic event do not have PTSD. [2] People who experience personal trauma (eg, rape or child abuse) are more likely to develop PTSD than people who experience non-attack trauma, such as accidents and natural disasters. [7] About half of people experience PTSD after being raped. [2] Children are less likely than adults to develop PTSD after a traumatic event, especially if they are under ten years of age. [8]
[2] Children are less likely than adults to develop PTSD after a traumatic event, especially if they are under ten years of age. [8]
PTSD is associated with a wide range of traumatic events. The risk of developing PTSD after a traumatic event varies depending on the type of trauma and is highest after exposure to sexual violence (11.4%), especially rape (19.0%). [3] A person who has experienced domestic violence is predisposed to developing PTSD. There is a strong association between the development of PTSD in mothers who have experienced domestic violence during pregnancy. [4]
Military service is a risk factor for the development of PTSD. [8] 78% of combatants do not develop PTSD; in about 25% of military personnel who develop PTSD, its onset is delayed. [4] In addition, one study showed that soldiers whose white blood cells had more glucocorticoid receptors were more likely to develop PTSD after injury. Refugees are also at increased risk of PTSD due to traumatic events experienced during the war.
Refugees are also at increased risk of PTSD due to traumatic events experienced during the war.
Sudden, unexpected death of a loved one is the most common type of traumatic event reported in foreign studies. [3]
Medical conditions associated with an increased risk of PTSD include cancer, heart attack [5] and stroke. [6] Critical care (ICU) is also a risk factor for PTSD. [7] Some women experience PTSD as a result of finding breast cancer and having a mastectomy.
Women who have had a miscarriage are also at risk for PTSD. Those who have repeated miscarriages have an increased risk of PTSD compared to those who have had only one. [6] PTSD can also occur after childbirth, and the risk is increased if the woman experienced trauma prior to pregnancy. [3] [4]
There is evidence that susceptibility to PTSD is hereditary. Approximately 30% of the variance in PTSD is caused by genetics alone. [3] There is evidence that individuals with a smaller hippocampus are more likely to develop PTSD after a traumatic event. [7]
[3] There is evidence that individuals with a smaller hippocampus are more likely to develop PTSD after a traumatic event. [7]
Consult your doctor if you experience similar symptoms. Do not self-medicate - it is dangerous for your health!
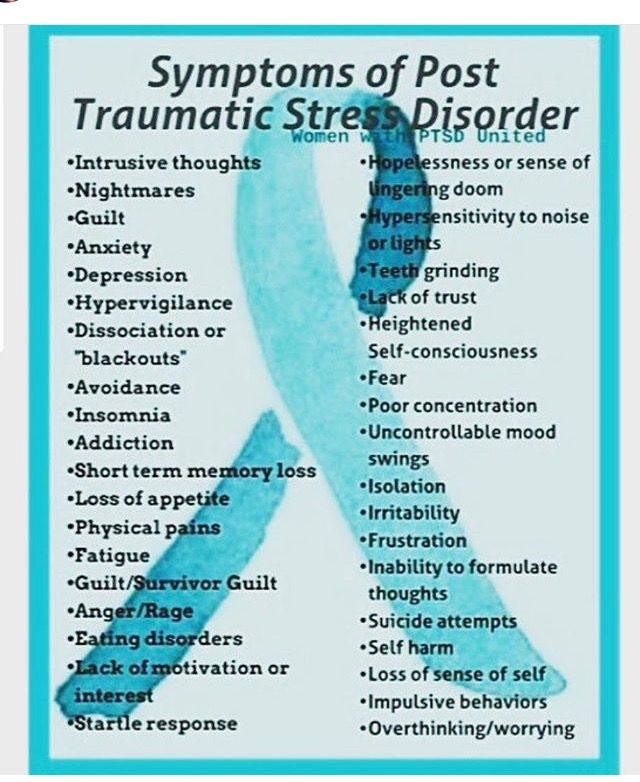
Symptoms of post-traumatic stress disorder
Symptoms of PTSD usually begin within the first 3 months after the onset of a traumatic event, but not later than a year. [1] [3] Typically, an individual with PTSD will persistently avoid trauma-related thoughts and emotions and discuss the traumatic event and may even show signs of amnesia regarding the event. However, the event is usually revived through intrusive, recurring flashbacks and nightmares. [17]
Symptoms of trauma-related mental disorders have been documented since at least the time of the ancient Greeks. [13] During the study of the world wars, the manifestations of the disease increased, and it was known by various terms, including "traumatic neurosis", "combat neurosis", "projectile shock", "Afghan syndrome", "combat psychic trauma". [14] The term "post-traumatic stress disorder" came into use in the 1970s in large part due to the diagnosis of Vietnam War veterans - "Vietnam Syndrome". [15] It was officially recognized by the American Psychiatric Association in 1980 in the third edition of the Diagnostic and Statistical Manual of Mental Disorders. [16]
[14] The term "post-traumatic stress disorder" came into use in the 1970s in large part due to the diagnosis of Vietnam War veterans - "Vietnam Syndrome". [15] It was officially recognized by the American Psychiatric Association in 1980 in the third edition of the Diagnostic and Statistical Manual of Mental Disorders. [16]
Pathogenesis of PTSD
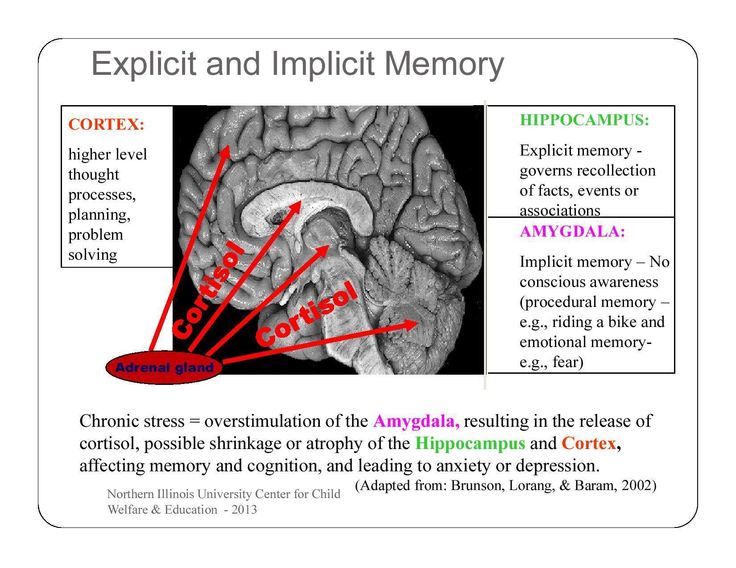
Symptoms of PTSD result from an over-reactive adrenaline response to a traumatic event, leaving a deep neurological trace in the brain. These patterns may persist long after the event that triggered the stress response, making the person more sensitive to future similar situations. [3] [18] During traumatic experiences, high levels of stress hormones suppress hypothalamic activity, which may be a major factor in the development of PTSD. [7]
PTSD causes biochemical changes in the brain and body that are different from other mental disorders such as depression. Individuals diagnosed with PTSD respond more strongly to a dexamethasone suppression test than individuals diagnosed with clinical depression. Most people with PTSD show low secretion of cortisol and high secretion of catecholamines in the urine [7] High brain catecholamine levels [8] and corticotropin releasing factor (CRF) concentrations are high. [1] [2] These findings suggest an abnormality in the hypothalamic-pituitary-adrenal (HPA) axis.
Individuals diagnosed with PTSD respond more strongly to a dexamethasone suppression test than individuals diagnosed with clinical depression. Most people with PTSD show low secretion of cortisol and high secretion of catecholamines in the urine [7] High brain catecholamine levels [8] and corticotropin releasing factor (CRF) concentrations are high. [1] [2] These findings suggest an abnormality in the hypothalamic-pituitary-adrenal (HPA) axis.
Fear maintenance has been shown to involve the HPA axis and connections between the limbic system and the frontal cortex. The HPA axis, which coordinates the hormonal response to stress, [3] which activates the LC-noradrenergic system, is associated with excessive consolidation of memories that occur after trauma. [4] This excessive consolidation increases the likelihood of developing PTSD. The amygdala is responsible for detecting threats and the conditioned and unconditioned fear responses that occur in response to a threat.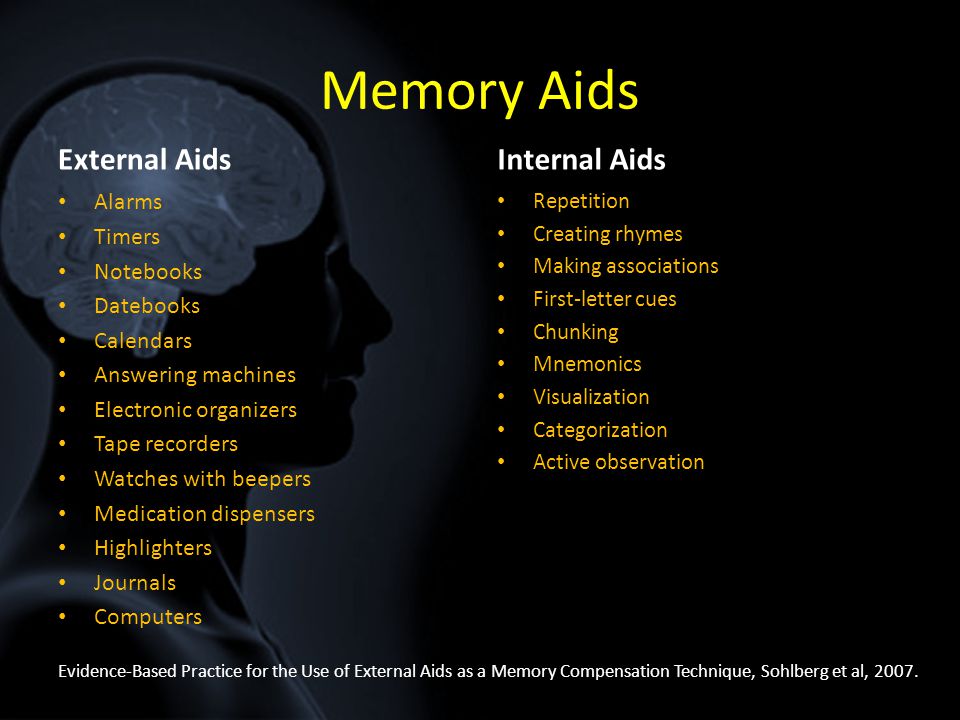 [7]
[7]
Research shows that people with PTSD have chronically low levels of serotonin, which contributes to commonly associated behavioral symptoms such as anxiety, irritability, aggression, suicidality, and impulsivity. Serotonin also helps stabilize the production of glucocorticoids.
Dopamine levels in a person with PTSD may contribute to the development of symptoms. Low levels of dopamine can contribute to anhedonia, apathy, impaired attention, and motor deficits. Elevated dopamine levels can cause psychosis, agitation, and restlessness. [9]
Elevated concentrations of the thyroid hormone triiodothyronine in PTSD have been described in several studies. [9] This may increase sensitivity to catecholamines and other stress mediators.
There is considerable controversy in the medical community regarding the neurobiology of PTSD. In a 2012 review, there was no clear link between cortisol levels and PTSD. Most reports show that people with PTSD have elevated levels of corticotropin-releasing hormone, lower levels of basal cortisol, and increased negative feedback on the HPA axis by dexamethasone. [7] [9]
Most reports show that people with PTSD have elevated levels of corticotropin-releasing hormone, lower levels of basal cortisol, and increased negative feedback on the HPA axis by dexamethasone. [7] [9]
Areas of the brain associated with stress and PTSD - prefrontal cortex, amygdala and hippocampus. Patients with PTSD have reduced brain activity in the dorsal and rostral anterior cortex and ventromedial prefrontal cortex, areas associated with experience and emotion regulation. [5]
The amygdala is actively involved in the formation of emotional memories, especially those associated with fear. During times of high stress, the activity of the hippocampus, which is associated with placing memories in the correct context of space and time, is suppressed. One theory is that this suppression may be the cause of the memories that can affect people with PTSD. When someone with PTSD is exposed to stimuli similar to a traumatic event, the body perceives the event as happening again because the memory was never recorded properly.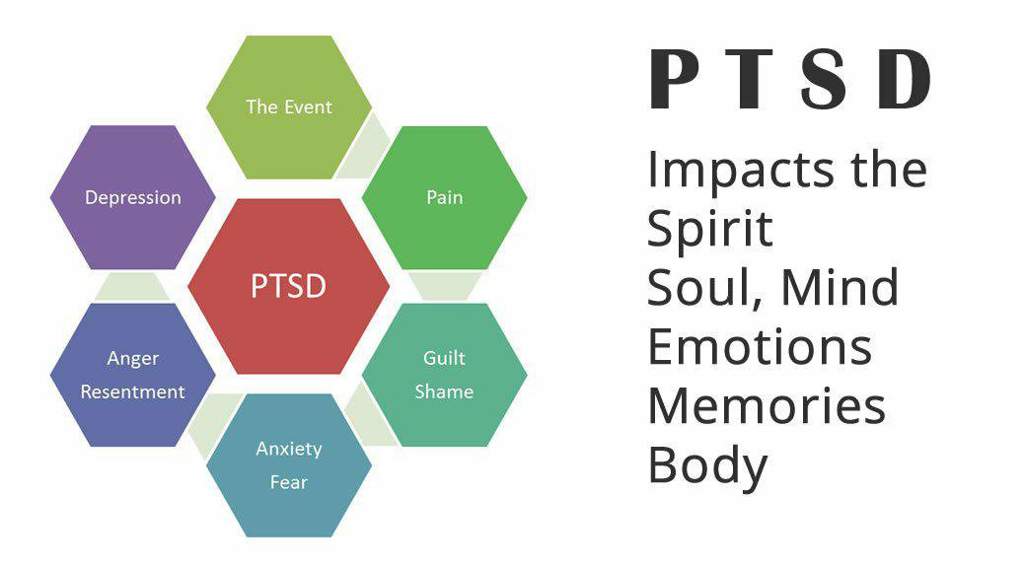 [6] [7]
[6] [7]
Classification and stages of development of post-traumatic stress disorder a few months after). Its functions persist for more than 30 days, which distinguishes it from the shorter acute stress disorder and disrupts all aspects of life.
It has three subforms :
- acute;
- chronic;
- delayed.
The diagnostic criteria for PTSD according to the Diagnostic and Statistical Manual of Mental Disorders can be summarized as:
A. Exposure to a traumatic event;
B. Constant rethinking;
C. Persistent avoidance of trauma-related stimuli;
D. Persistent symptoms of increased arousal;
E. Duration of symptoms more than 1 month;
F. Significant impairment in social, occupational, or other important areas of functioning.
Notably, criterion A (“stress”) has two parts, both of which must be used to diagnose PTSD. The first (A1) requires that "the person has experienced, witnessed or experienced an event or events that involve actual or threatened death or serious injury, or a threat to the physical integrity of oneself or others. " The second (A2) requires that "the person's response be accompanied by intense fear, helplessness, or horror."
" The second (A2) requires that "the person's response be accompanied by intense fear, helplessness, or horror."
Complications of post-traumatic stress disorder
The presence of PTSD may increase the risk of other mental health problems such as:
- depression and anxiety;
- drug or alcohol use;
- eating disorders;
- suicidal thoughts and actions.
Diagnosis of post-traumatic stress disorder
When to see a doctor
A psychotherapist should be consulted after traumatic experiences and stressful situations such as violence, catastrophes and other life threats.
For adult screening, a range of screening tools are used, such as the clinician-established PTSD score. [12] There are also several screening and assessment tools for use with children and adolescents. These include the Childhood PTSD Symptom Scale (CPSS). [17] [18]
The International Classification of Diseases and Related Health Problems 10 (ICD-10) classifies PTSD under 'Response to severe stress and adjustment disorders'. [14] The ICD-10 criteria for PTSD include re-experiencing, avoidance, and either increased reactivity or inability to recall some of the details associated with the event. [14]
[14] The ICD-10 criteria for PTSD include re-experiencing, avoidance, and either increased reactivity or inability to recall some of the details associated with the event. [14]
The diagnosis of PTSD requires that the person be exposed to excessive stress, such as life threatening. Any stressor can lead to a diagnosis of adjustment disorder, and it is an appropriate diagnosis for stress and a symptom that does not meet the criteria for PTSD. The differential diagnoses are schizophrenia or other disorders with psychotic features, such as psychotic disorders due to a general health condition. Narcotic psychotic disorders can be considered when it comes to substance abuse. [17]
Treatment of post-traumatic stress disorder
Cognitive behavioral therapy
This type of therapy aims to change the patterns of thought and behavior that are responsible for negative emotions. CBT has been proven to be an effective treatment for PTSD.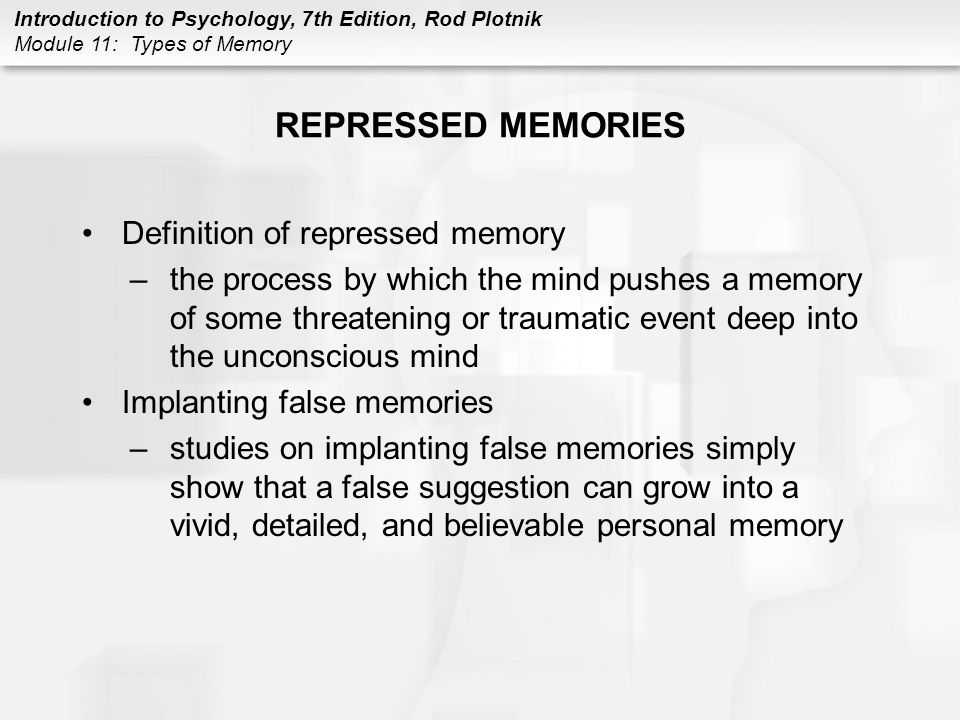 [15] Through this type of therapy, people learn to identify the thoughts that make them feel fearful or upset and to replace them with less anxious thoughts. The goal is to understand how certain thoughts about events cause PTSD-related stress. [13] [16]
[15] Through this type of therapy, people learn to identify the thoughts that make them feel fearful or upset and to replace them with less anxious thoughts. The goal is to understand how certain thoughts about events cause PTSD-related stress. [13] [16]
Drug treatment
Although many drugs do not have sufficient evidence to support their use, three (fluoxetine, paroxetine and venlafaxine) have been shown to have a slight advantage over placebo. [12] With many medications, residual PTSD symptoms after treatment are the rule, not the exception. [16]
- Antidepressants
Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) may be of some benefit in PTSD symptoms. [12] [16] Tricyclic antidepressants are equally effective. Evidence suggests slight to moderate improvement with sertraline, fluoxetine, paroxetine, and venlafaxine. [12] Thus, these four drugs are considered first-line drugs for PTSD.
[12] Thus, these four drugs are considered first-line drugs for PTSD.
- Benzodiazepines
Benzodiazepines are not recommended for the treatment of PTSD due to lack of evidence of benefit and risk of worsening PTSD symptoms. Some authors believe that the use of benzodiazepines is contraindicated for acute stress, as this group of drugs promotes dissociation. However, some use benzodiazepines with caution for short-term restlessness and insomnia. Although benzodiazepines may relieve acute anxiety, there is no strong evidence that they can stop the development of PTSD and may actually increase the risk of developing PTSD by 2-5 times. [11] Disadvantages include risk of benzodiazepine dependence and withdrawal. In addition, people with PTSD (even those without a history of alcohol or drug abuse) are at increased risk of benzodiazepine abuse. Benzodiazepines should be considered relatively contraindicated until all other treatment options have been exhausted.