Post traumatic stress disorder infidelity
How Infidelity Causes Post Traumatic Stress Disorder
Of all of the threats to a committed relationship I have treated in four decades of working with couples, the most difficult to heal is infidelity. When a trusted partner in a committed relationship betrays the sacred trust of the other, the relationship will undergo severe instability.
The partner who has been betrayed is emotionally tortured and humiliated when knowledge of the infidelity emerges. They are clearly in trauma and experience the same array of symptoms that professionals now describe as post-traumatic stress disorder. Similar to any others who have suffered threats to their physical or emotional well-being and security, they are disoriented and confused by what has happened.
Similar to the classical symptoms of PTSD, relationship partners of both genders may experience:
- Repeated intrusive thoughts.
- Unstable emotional regulation.
- Out-of-body experiences.
- Alternating between feeling numb and striking out in retaliation.
- Inability to stop scanning for any new data that might cause more distress.
- Feeling overwhelmingly powerless and broken.
- A need to regain self-worth by assigning blame.
- Confusion and disorientation.
“Ever since I found out about the affair, I can’t stop thinking about what happened. I have repeated nightmares. My faith in trust and love is demolished. The person I believed in most in the world betrayed me without seeming to care. If I’d known something was wrong, maybe I could have stopped it before it got going. I spin between being devastated and being enraged. I can’t seem to find any peace, knowing that there is probably more than I will ever be told. I feel like a goddamn fool, humiliated and broken. How could my partner do this to me?”
The trauma of betrayal can also trigger memories of buried or unresolved emotional and spiritual damage from the past. When those prior traumatic experiences are triggered and re-emerge, they significantly complicate the healing process.
For there to be any chance that the couple undergoing this situation can ever transcend the distress of broken trust, they must deal with two simultaneous challenges: The first is to understand and work through the combination of both current and re-emerging trauma responses of the betrayed partner. The second is for both partners to commit to specific roles in the healing of their mutual distress.
The 5 Most Common Re-Emerging Issues
1. History of Prior Trauma
When people experience a life-threatening event earlier in life, they create defenses that allow them to survive those traumas. Those defenses can be either barricades to future pain or unconscious seduction to recreate what is familiar.
If a relationship partner has been harmed by threats of loss or harm in the past, he or she will have a stronger and more persistent trauma response to a partner’s current betrayal. Dependent on how much they appear similar to what is happening in the present, they will mesh with the current pain and make recovery that much harder.
2. Emotional and Physical Resilience
Whether born into a person or learned throughout life, resilience is the conqueror of prolonged sorrow. Though grief must not be denied, those who are lucky enough to be more resilient can endure it without falling prey to extended emotional heartbreak.
Resilience after a betrayal is also buoyed up by the kind of social support a person has access to. When infidelity is discovered, it is easy for traumatized partners to lose sight of their own worth. Authentic, caring, and responsive others are able to remind them of who they were before the trauma and help them to regain emotional stability.
Sadly, the most common excuse many unfaithful partners give when they stray is that they were unable to get their needs met in the relationship. Those accusations increase the anguish of the betrayed partner.
3. The Strength of the Primary Relationship
When people have a strong bond, both partners openly talk about their needs and disappointments as they occur in their relationship. They know that outside temptations are always possible, but they are committed to making their relationship stronger if they arise.
They know that outside temptations are always possible, but they are committed to making their relationship stronger if they arise.
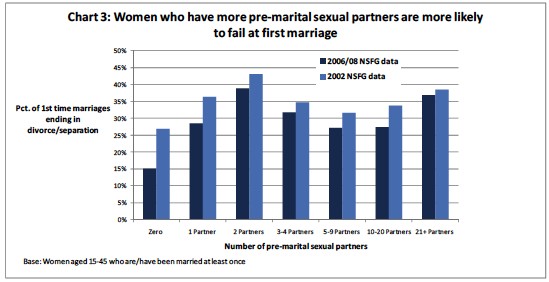
If a relationship is wavering and the people within it are no longer as bonded as they once were, one or both of the partners may be searching for meaning outside the relationship. If those yearnings are not shared and the relationship goes unresolved, they are more likely to transform into actions.
Some relationships feel more okay to one partner than they do to the other. If those feelings are not shared and an affair happens, the unknowing partner has had no opportunity to intervene. They feel they are doing everything right, that their love is intact, and that trust will never be broken. That partner is understandably more demolished when an affair emerges.
4. Double Betrayal: When the Infidelity Is With a Known Party
Besides the experiences of humiliation and anguish, an even more destructive heartbreak occurs when the third member of the triangle is a close and trusted friend or a family member.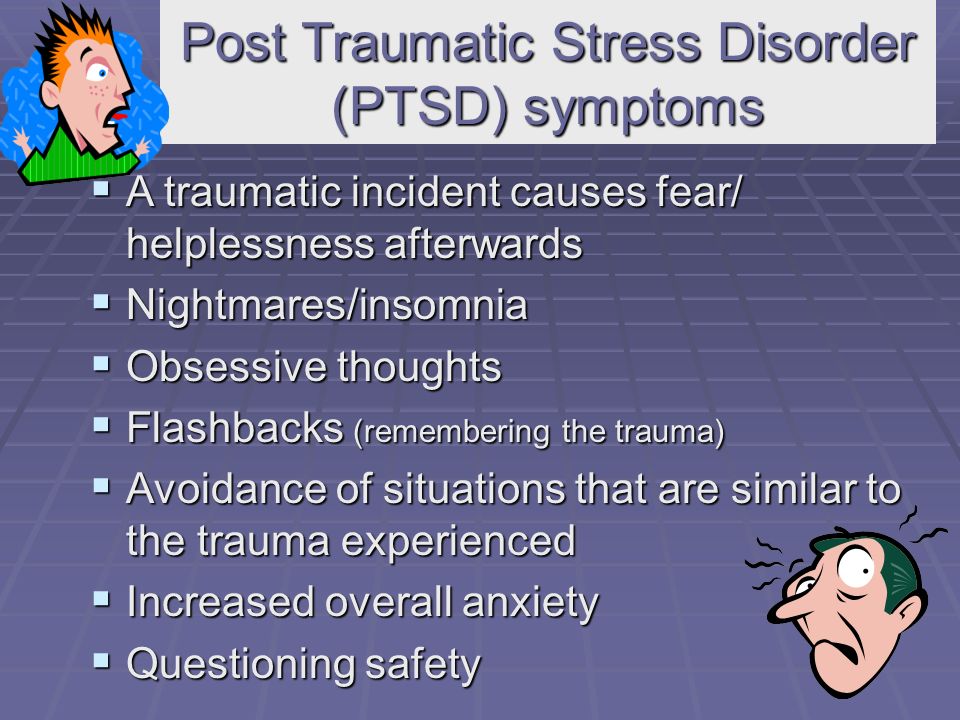
When the betrayed partner discovers that two deeply trusted people could collectively collude behind his or her back is almost unfathomable. In these cases, there are often others who know what is going on causing even more potential loss of relationships when the affair emerges. Those who have remained silent may then pull away for fear of being seen as accomplices.
5. How Long the Infidelity Has Been Going On
An affair that is quickly confessed along with true remorse and the desire to do whatever is necessary to help the betrayed partner heal, has the best chance of success if it never happens again.
On the other hand, a partner who finds out that the betrayal has been going on for weeks or months, or even that it is still active, is fundamentally more damaged and finds it much harder to heal. For most women, it is not just a passing affair anymore. It is a fully developed relationship of secrecy, passion, and emotional connection, stealing love and commitment from the existing partnership. For most men, it is the sabotage of being cuckolded by another male who has taken his woman from under his eyes and sold him out as a “brother.”
For most men, it is the sabotage of being cuckolded by another male who has taken his woman from under his eyes and sold him out as a “brother.”
The person outside of the primary relationship, who has been willing to be a co-betrayer, often feels that he or she has claimed possession of the infidel. That individual may not be willing to be dismissed and can become a deterrent to a relationship’s potential healing.
Given the seriousness of these potential emerging issues and the ways they may combine, it is understandable how much influence they may have on whether or not the relationship can heal and over what period of time.
How do two people who do not want to lose their relationship navigate the process of broken trust to a possibility of reconciliation?
How does a betrayed partner ever learn to believe the other again?
How does the partner who chose to act this way get past his or her guilt and remorse?
What must happen for recovery and recommitment to even be possible?
Once both partners understand how likely it is that a betrayed partner will evidence the symptoms of PTSD, they realize that the healing process is the same for all traumas. The betraying partner must simultaneously play the dual roles of an ally to his or her partner’s healing and a seeker of absolution from the very person they have carelessly wounded. The other must survive the trauma and learn to love again.
The betraying partner must simultaneously play the dual roles of an ally to his or her partner’s healing and a seeker of absolution from the very person they have carelessly wounded. The other must survive the trauma and learn to love again.
The Role of the Betraying Partner as an Ally in Healing the Trauma
Most betraying partners truly want to heal their relationship but have difficulty not blaming their other partner in some why they chose to stray. Gender responses are often different. For instance, more men than women justify that decision by stating that their sexual needs weren’t being met, that their partners didn’t pay enough attention to them in general, or that they felt exploited in the relationship. More women than men traditionally cite their reasons for an affair as lacking an emotional connection with their primary partner, a lack of availability in general, or inadequate romantic support.
In order to expedite healing, the betraying partner has to recognize that they must put aside anything they felt that drove them to give in to an affair until they recognize and feel remorse for the act of betrayal, itself. They are legitimately on trial for invalidating the worth of their primary relationship, succumbing to a self-serving motivation, and the willingness to risk severely wounding the other partner.
They are legitimately on trial for invalidating the worth of their primary relationship, succumbing to a self-serving motivation, and the willingness to risk severely wounding the other partner.
As now allies in healing the relationship, they must be prepared to encourage and weather whatever frustration, anguish, or retaliation their betrayed partner needs to express. They must be willing to stay in the game for however reasonable time it may take, to put their own needs and underlying grievances aside, and to fully commit to the healing of their partner’s rage and grief. The more committed the betrayer is to the process, the sooner his or her partner will be able to heal.
The Role of the Traumatized Partner
Feeling devastated, humiliated, and broken are hard experiences to survive. Though the traumatized partner has every reason to be upset, he or she must work through those responses in a sincere and committed way, alongside the other partner’s commitment to do whatever is mutually needed for healing.
The partner experiencing PTSD will most likely have wildly swinging mood changes, emerging experiences of underlying, unresolved issues, and agonizing waves of grief. While simultaneously feeling the need to strike back, run away, or feel immobilized, they must learn to self-soothe, create resilience, seek outside support, and commit to a renewed faith in a better future.
If, additionally, they’ve been the object of previous trauma, they must also sort out what is happening in the present from what they may have endured in the past, so as not to blame their partner’s current betrayal for something they did not cause.
Building a Future Relationship
Both partners must realize that their past relationship is over and that their goal is to build a new one that will withstand challenges in the future. When the partner who is the ally in healing merges with the partner who is ready to move on, they can create a new kind of sacred trust that can be significantly stronger by virtue of what they’ve been through together.
This process is not for those who want a quick fix, nor for those who hold fast to the past. Superficializing a true betrayal can create unresolvable pain. Similarly, carrying mistrust, anger, and pain forever will eventually destroy any hope of true healing. The betraying partner must take seriously what he or she has done. The partner who has been betrayed must truly want to rebuild the relationship and ultimately learn to trust that person again.
Yes, I have seen partners do this kind of healing, and do it beautifully. They take the lessons from the past, learn to communicate courageously and honestly, and build something neither has known before. Their relationship Phoenix can emerge from the ashes of their mutual sorrow.
Facebook image: Cat Box/Shutterstock
To Save Your Marriage, It’s Crucial to Address Post Infidelity Trauma Disorder
Skip to contentDespite extramarital affairs being commonplace today, these unfortunate happenings often feel like the dropping of a huge bomb.
Especially when you’re the one who was betrayed.
It’s not uncommon to feel trapped inside the traumatic experience, bubbling up rage and anger every time something reminds you of the incident.
Feeling unable to move into a place of healing, you may assume that you can’t salvage your relationship.
Sadly, because of this negative effect of trauma, many marriages like yours don’t ever recover from an affair.
Yet, rebuilding your marriage is possible. And healing is possible.
It’s important to understand that an affair is not only a heartbreaking but traumatic experience as well. For healing to occur, you must address the trauma the affair has caused you.
Actually, addressing the trauma is the very first step to recovery.
Your Response to the Affair Is Hardwired
As human beings, we’re biologically hardwired to bond with one another by developing deep nurturing attachments. This is how we’ve survived as a species, defending and caring for each other.
When that bond breaks—as in the case of an affair—it’s traumatizing.
The traumatized person experiences a biological reaction that resonates in their physical and emotional being. Often feeling devastated, you may not recognize this reaction in yourself. But it’s trauma nonetheless.
Understand Your Innate Response to Emotional Trauma
When a human being experiences emotional trauma, it activates a part of the autonomic nervous system, or otherwise known as the fight-or-flight response.
The funny thing about your nervous system is that it’s limited. Simply sensing a threat, it can’t tell the difference between a grizzly bear and a betraying partner. Your nervous system accepts them both as a “threat.”
For this reason, you likely had a difficult time expressing your emotions after you learned of your partner’s affair. Or you felt that your feelings were scattered all over the place.
This state of not knowing what you were feeling is undoubtedly the work of trauma. Ultimately, it can cloud your emotional discernment, resulting in you being unable to pinpoint or express your true feelings.
Ultimately, it can cloud your emotional discernment, resulting in you being unable to pinpoint or express your true feelings.
Instead, you may have only felt anger or rage. Wanting to blame and attack your partner, you may have adopted a new and vengeful type of controlling behavior aimed directly at your partner.
For example, it’s not uncommon for the betrayed partner to demand passwords, obsessively check social media for “clues,” or frequently drill their partner for information.
Acknowledge Normal Vs Optimal Responses to Infidelity
Keep in mind that although these reactions to infidelity are not optimal for your health and well-being, they are normal. However, in our society, they are only appropriate for a short while.
To recover from an affair, it’s essential to find healthier ways to cope with the situation long-term.
More often than not, trauma’s effect does not get resolved but deeply buried. Random and everyday events can trigger traumatic reactions.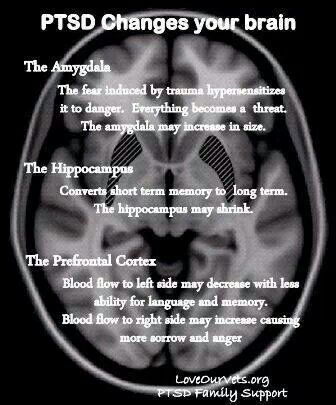
Remember, the human nervous system can’t distinguish one danger from another. Threats are lumped into one big life-threatening category, triggering an extreme emotional response. That’s because your body attempts to protect itself with a physical response, fighting off a perceived perpetrator. You experience these triggers at any time causing a preoccupation of the problem.
Soon, you may become stuck in a negative and reactive cycle of insecurity, rage, and suspicion, which will take a toll on your physical and emotional health. Not to mention the impact it will have on your loved ones and your productivity.
You may have felt like your response to your partner’s actions weren’t normal or your feelings are over the line. Some partners have even reported feeling like they were “going crazy” while trying to recover from an affair.
Earlier Trauma Can Make Symptoms of Post Infidelity Trauma Disorder Even Worse
Unfortunately, the notion that time heals all wounds isn’t true.
Furthermore, the way you respond to post infidelity trauma disorder may hurt you even deeper if it is somehow similar to another earlier traumatic or troubling experiences. In other words, trauma memories, feelings, and meanings may bubble up from something you experienced from your own earlier events.
Many people don’t want to acknowledge this fact because they feel so hurt and betrayed and just wish to have the perfect relationship. Grieving the loss of a perfectly secure relationship can be devastating.
We are not always aware of past traumatic memories and how they trigger strong emotions. To name a few, your memories may be about your parents preoccupied with their own marital issues and how that experience left you feeling unworthy, alone, or insecure.
Remember that it’s not just about the here and now. When you are dealing with post infidelity trauma disorder, past trauma will easily get triggered—consciously and unconsciously—with strong and negative thoughts and emotions.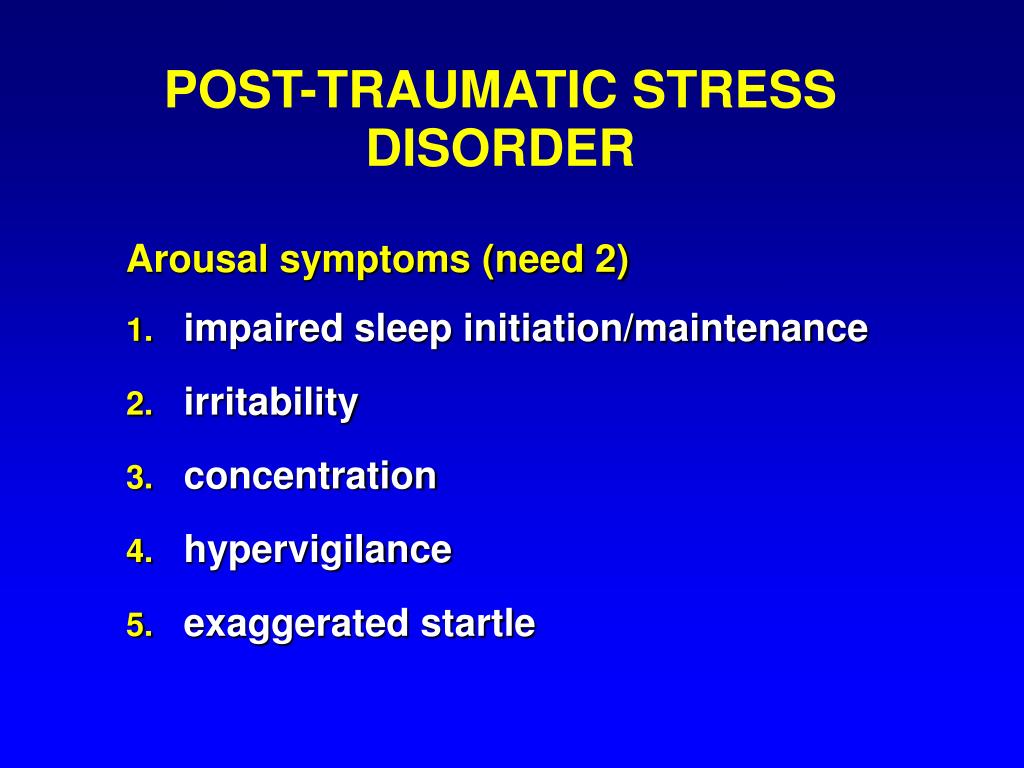
This type of reaction to trauma makes it evident that professional help is required.
Change the Message in Your Mind
To recover from an affair, you must move through the initial response to post infidelity trauma disorder.
As mentioned before, a therapist can help you understand how your brain works to cope with post infidelity trauma disorder and teach you ways to reclaim your calm.
The result of trauma treatment is to enable you to retreat back into a calm and relaxed mode, opposed to feeling overly aroused, hyper-vigilant, and on edge.
Trauma Therapy Decreases Negative Reactions of Post Infidelity Stress Disorder
Firstly, it’s important to make a decision whether or not you want to commit to staying in the marriage. And once you make the decision, you need to realize that all the strong, negative emotions are happening automatically as a result of the trauma response.
Also, ask yourself if you’re ready to be on the other side of your anger and rage. Or, do you want to continue to seek revenge on your spouse?
Or, do you want to continue to seek revenge on your spouse?
Once you are free of the emotional trauma trigger—becoming present and strategic—you’ll be able to communicate your feelings and needs. And you’ll be able to explore what went wrong in the relationship.
Resolving the trauma will enable you to become present for yourself first.
Ultimately, the decision is always yours.
You have the power to evaluate and assess your relationship now and always, in the future.
Steps to Recover from an Affair
Addressing the trauma caused by an affair is your first step towards recovery. From that calm place, you can then begin to evaluate your marriage and heal from the pain. (You may also want to read my post, “Why NOT to Rush to Couples Counseling After Infidelity.”)
I am here to help you reclaim your calm after an affair and help you find your path to healing.
For more information regarding trauma recovery and Rapid Resolution Therapy, please visit my RRT specialty page or contact me 713-4090370 for a consultation soon.
Reaching out for support is a sign of strength.
A new beginning is possible! I am here to help.
Now offering online or telephone visits, as well as face-to-face sessions.
Call now to schedule your first appointment:
(281) 693-1455
Recent Blog Posts
- Everything We Know About Overcoming Grief is Wrong
- Summertime Is Time to Take Care of You
- Hope Blooms in Springtime
- Keys to Manage Stress and Reduce Anxiety During the Coronavirus Epidemic
- Being Down During the Holidays Is Hard
Blog Categories
- Anxiety (7)
- Depression (4)
- Family (9)
- Rapid Resolution Therapy (9)
- Trauma (8)
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.
This booklet deals with signs,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident.
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension.
PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment.
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event.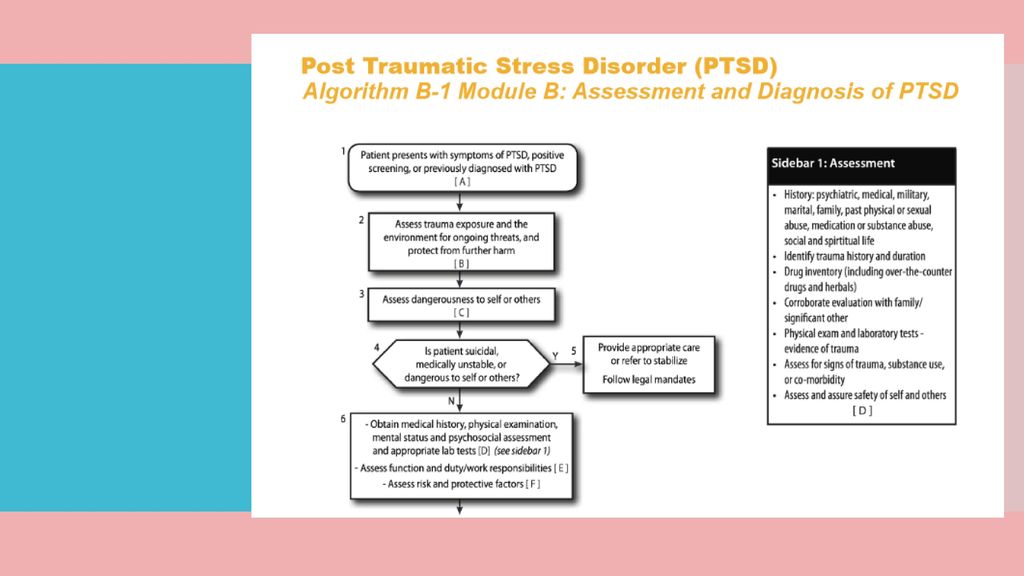 you try to hold on away from anything that might remind you of the experience.
you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last?
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this disease?
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men.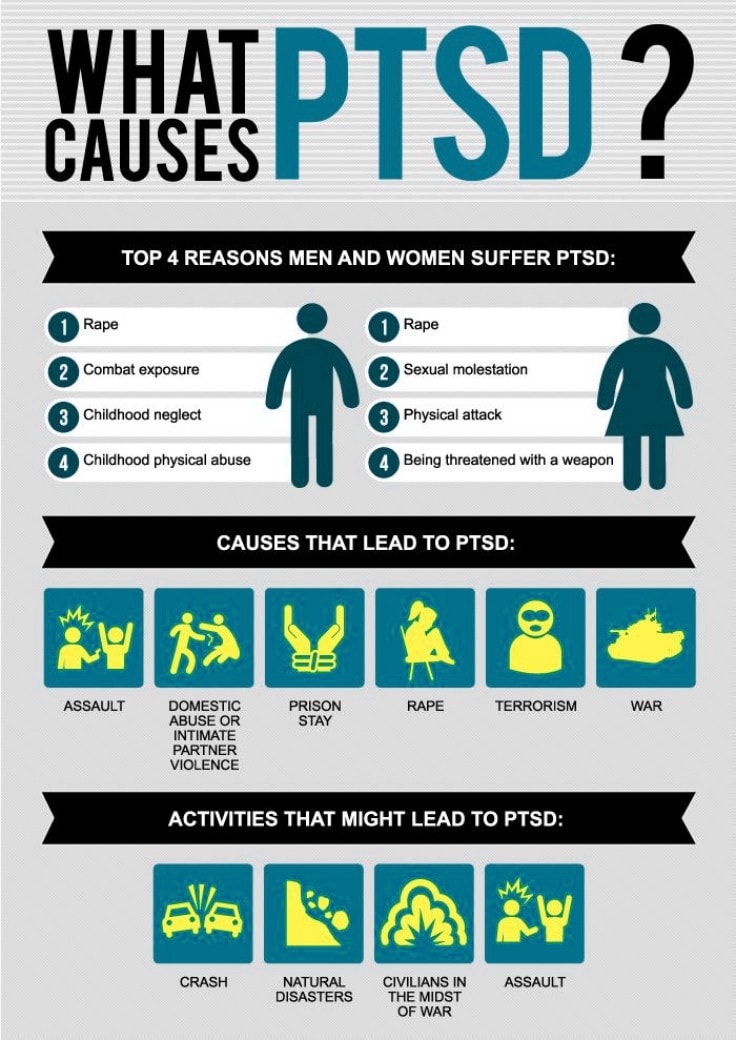 The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
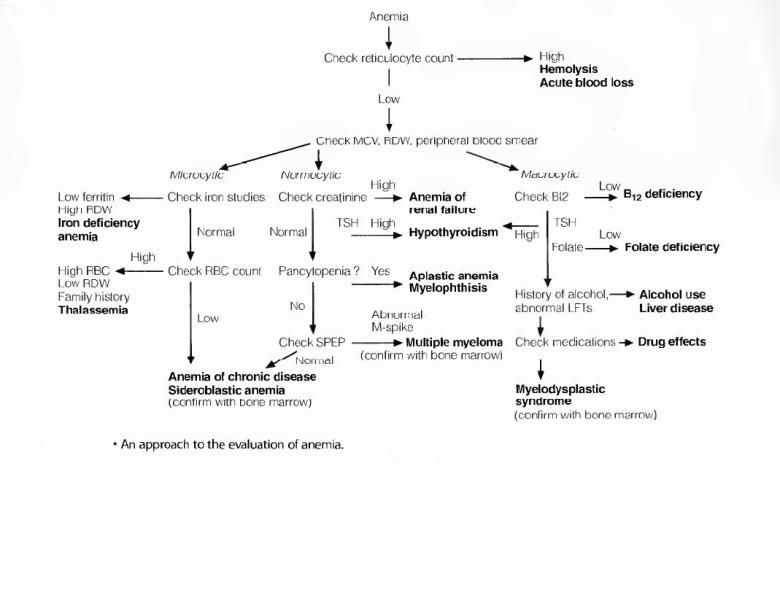
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD.
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What should I do to help myself in this situation?
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
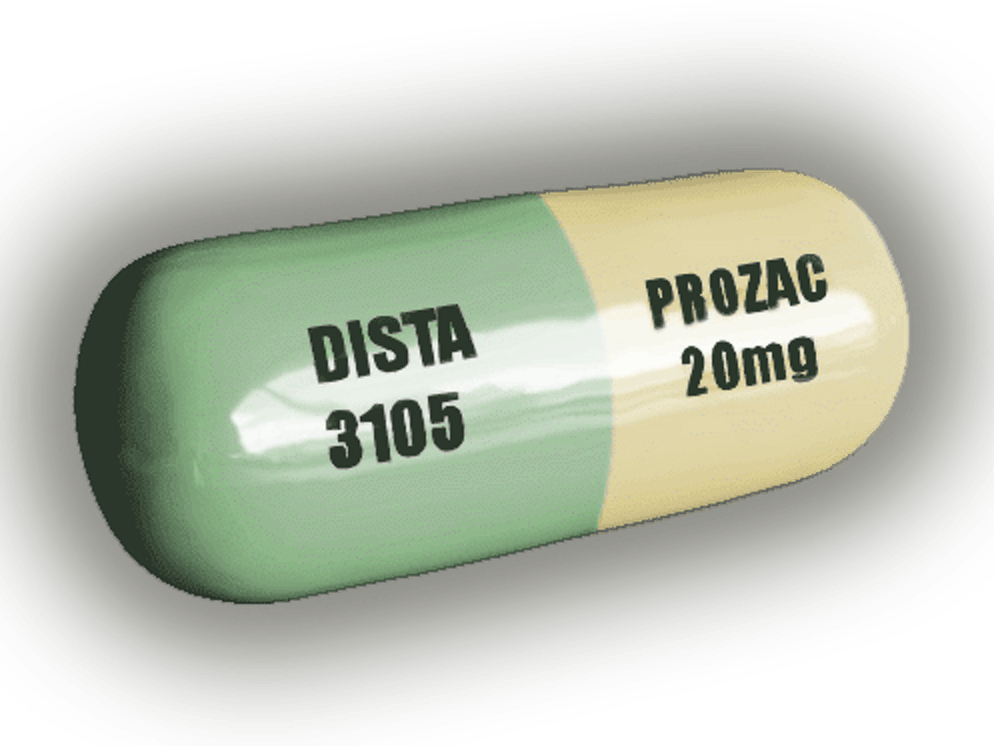
Your doctor may prescribe medicine to help reduce your fear or tension. However, it should be borne in mind that usually several weeks before the medicine starts to work.
However, it should be borne in mind that usually several weeks before the medicine starts to work.
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
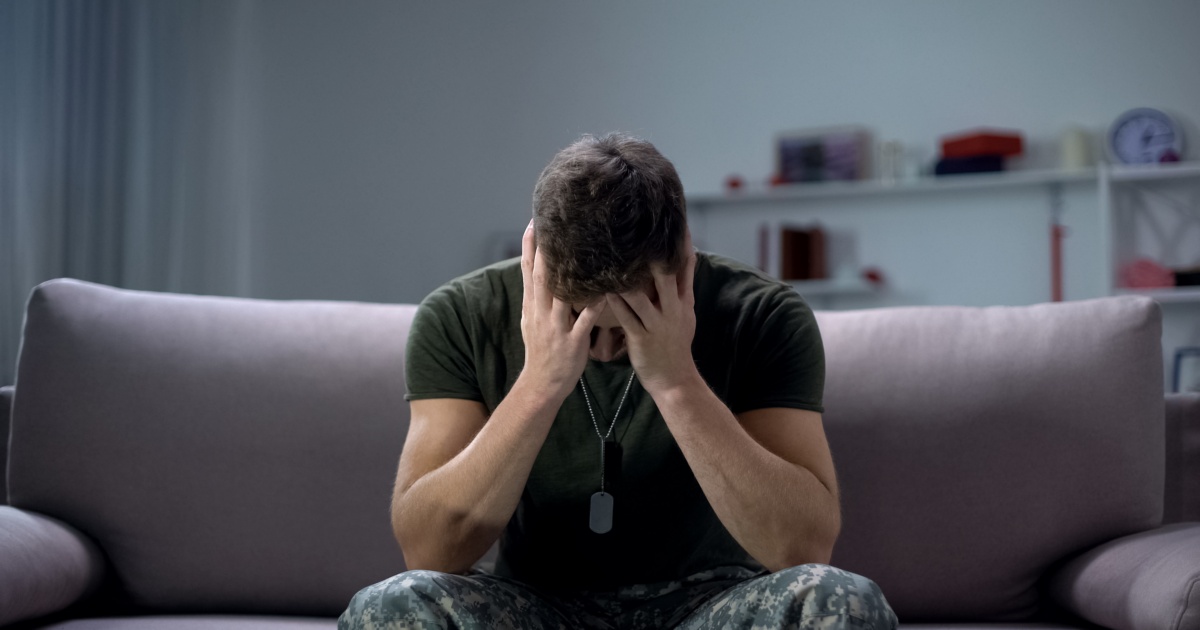
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military. MST can happen with men and women, and can occur in peacetime, during war training or during the war.
MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear.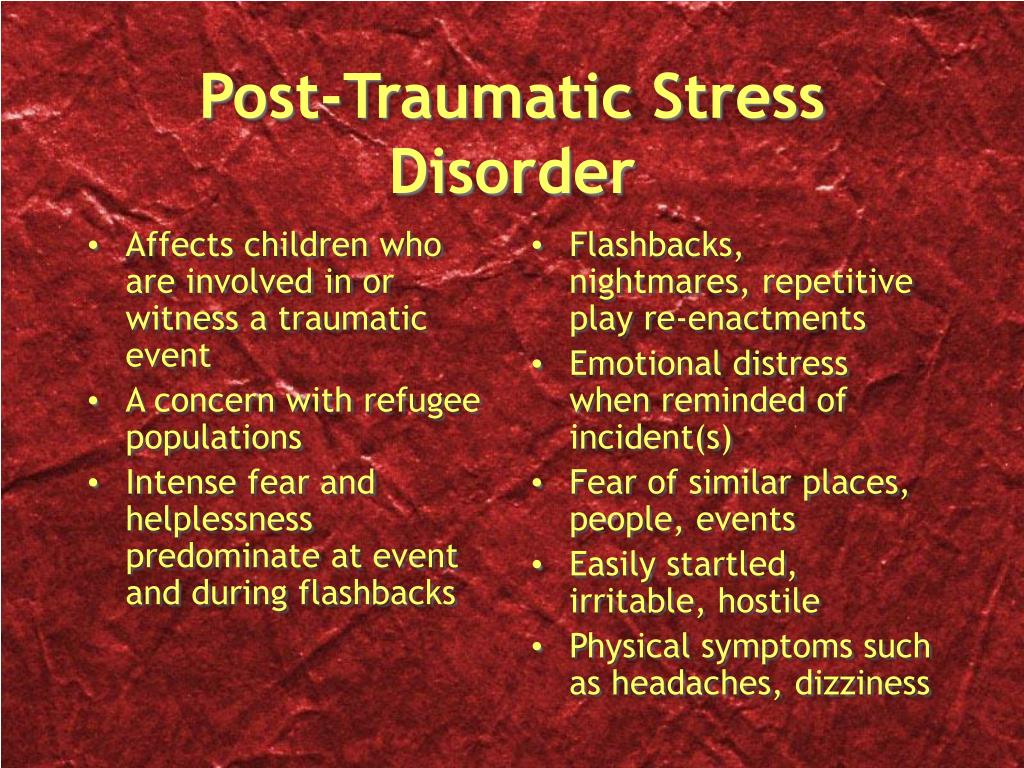 The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space.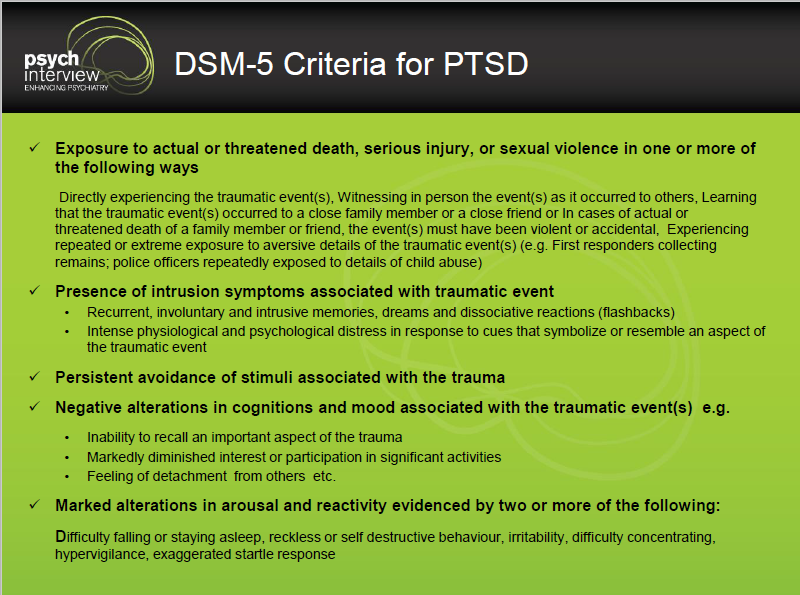 1
1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). 4
4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress. 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.
7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.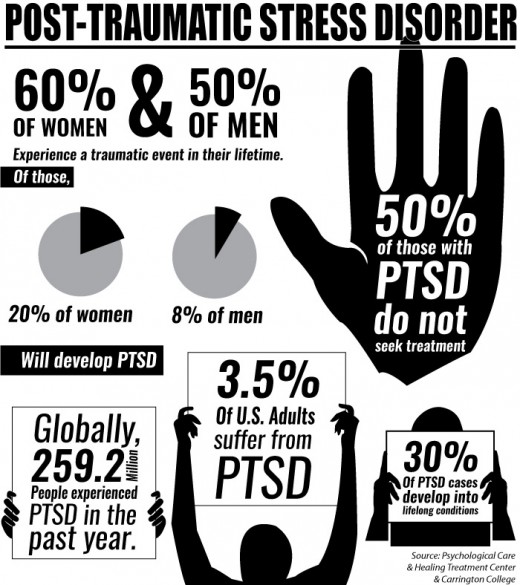
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate.
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced. NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced.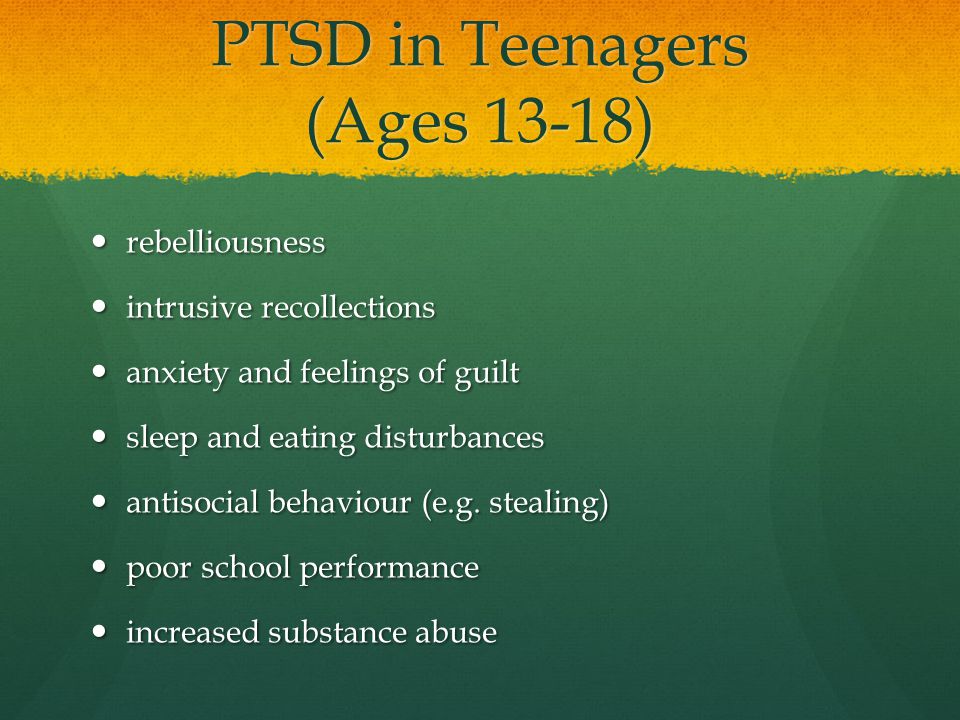 9
9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation. First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal.
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease. During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: nimhinfo@nih. gov
gov
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www.ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction.
 Nature. Nov 7 2002;420(6911):70-74.
Nature. Nov 7 2002;420(6911):70-74. - 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus. Nat Neurosci. Mar 2005;8(3):365-371.
- Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711.
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder.
 Biol Psychiatry. Feb 3 2006.
Biol Psychiatry. Feb 3 2006. - Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
- Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634.
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F. Hogan, PhD
Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Department of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www.omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Department of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
How to recognize PTSD in everyday life
49,045
Knowing yourself A man among peopleAntistress
Most of us are familiar with the term "post-traumatic stress disorder". But not everyone understands that we get traumatic experiences in everyday life. Sometimes it happens completely unnoticed. Psychological trauma can cause anxiety and other problems that differ both in strength and in the way they are expressed.
But not everyone understands that we get traumatic experiences in everyday life. Sometimes it happens completely unnoticed. Psychological trauma can cause anxiety and other problems that differ both in strength and in the way they are expressed.
How does PTSD occur?
The nature of PTSD is quite difficult to comprehend. At a fundamental level, trauma causes shock and fear. The reaction of our mind and body differs depending on the intensity and suddenness of the most traumatic event. When something discouraging or unnerving happens, it throws us off balance.
Usually it only takes time to recover, but sometimes the effects of trauma continue to affect us again and again. Our emotions become out of balance, especially when the arousal and response systems are at work.
Trauma also affects thinking and mood. We try to avoid uncomfortable situations, especially if they somehow resemble a traumatic event.
When all these symptoms are exacerbated to such an extent that a person cannot cope with them independently and normally exist in society, the syndrome becomes a disorder.
Who gets the disorder?
"Classic" cases of PTSD occur in combat veterans who have seen death and destruction, survivors of natural disasters, victims of physical and sexual abuse. But if the injury occurred in less extreme circumstances, it is more difficult to determine that a person is showing symptoms of post-traumatic stress.
It is often possible to get hurt in a relationship with someone. For example, if there was a betrayal, although the marriage seemed strong and happy. This causes shock, a person loses a sense of the reality of what is happening. At first, he may fall into a stupor.
When the shock wears off, a cascade of emotions descends upon him—horror, anger, bitterness, sadness, and even despair. They are exhausting in themselves, but the expectation of the next “trip” from the universe gives rise to constant anxiety.
Case Study
One of my patients came to therapy after learning that her husband (with whom she had been living together for 30 years) was in a long-term relationship with another woman.
They communicated through social networks and never met in person, but for the wife it was still a terrible betrayal and shock.
Despite the emotional coldness that appeared in her relationship with her husband, it seemed to her that everything was fine
The discovery turned her life upside down. She had little idea of what was real and what was not. She could not eat or sleep, did not control her emotions - swings from anger to tears happened all the time. But the most unpleasant moment was the obsessive thoughts and scenes that stood before her eyes: their romantic communication, his face on the day she found out everything. It couldn't be stopped.
Of course the woman received professional help. But her story is one example of trauma that shows up in everyday life. For most of us, the likelihood of getting PTSD under dramatic circumstances, in war or in a disaster, is relatively small. But other types of traumatic events occur at every turn.