Physical effects of trauma
How Trauma Affects the Body
Source: Source: Pexels / Cottonbro
Trauma is a serious issue that requires trauma therapy.
- An estimated 90 percent of adults in the United States have experienced a traumatic event at least once in their lives.
- Eight million people have post-traumatic stress disorder (PTSD) at any given time.
- Approximately 7-8 percent of all adults—1 in 13 people in this country—will develop PTSD during their lifetime.
- About 10 percent of women develop PTSD sometime in their lives compared to 4 percent of men.
What Is Trauma?
When it comes to trauma, no two situations are ever the same, but trauma therapy can help.
Trauma can result from major life events like being in a combat zone, sexual assault, or a natural disaster, or more pervasive experiences like an abuse-filled childhood.
Initial Reactions to Trauma
These can include exhaustion, confusion, sadness, anxiety, agitation, numbness, dissociation, and physiological arousal. You might experience a few or all of these symptoms. Increased exhaustion is often the result as the more worried and stressed people are, the more tense and constricted muscles are. Over time the muscles become exhausted and ineffectual. After a traumatic event or repeated trauma, people respond differently, experiencing a wide range of physical and emotional reactions. There is no right or wrong way to think, feel, or respond to trauma. It’s traumatic! Everyone will react differently, so don’t judge your reactions or those of other people.
The Physiological Effects of Trauma
Trauma sensitizes the hypothalamic-pituitary-adrenal (HPA) axis, which is the body’s central stress response system. You can think of this as the juncture of our central nervous system and endocrine system, which makes us more reactive to stress and more likely to increase the stress hormone cortisol. In certain situations, hormones like cortisol are crucial. (Cortisol, the primary stress hormone, increases sugars in the bloodstream, enhances your brain’s use of glucose, and increases the availability of substances that repair tissues.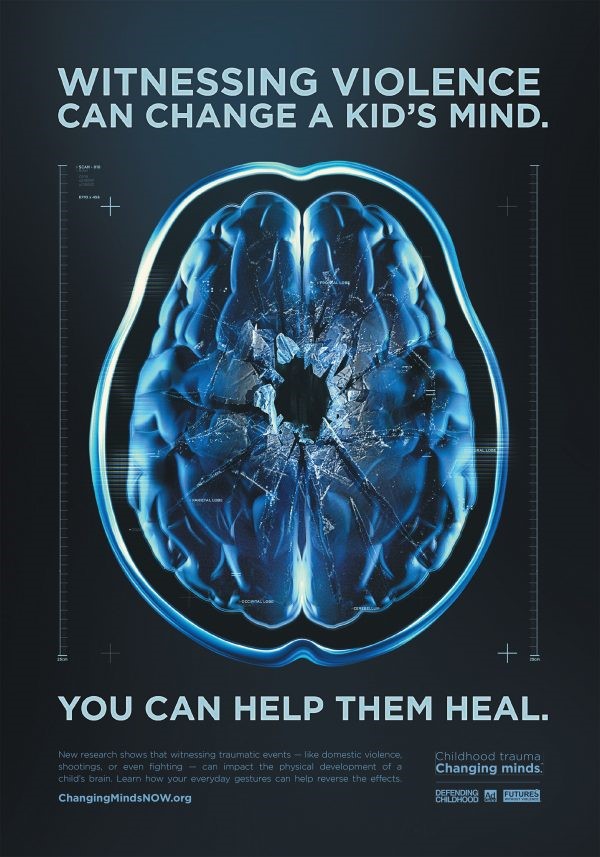 )
)
Unfortunately, Cortisol can be toxic when it is chronically high—ultimately leading to increased risks of health conditions such as depression or heart disease.
Remove the stressor, and the body’s hormones should respond in kind. The problem: Someone who is exposed to trauma may continue to produce these hormones, leading to adverse effects on the body over time. But trauma therapy can help to rebalance this natural reaction to stress.
Additionally, the indirect effects of trauma on the body can be subtle yet dangerous. Often, trauma’s physical and emotional pain can make it hard to cope, leading to unhealthy tendencies like smoking or drinking. Although these can be seemingly effective strategies in the short term, they only numb the emotions and prolong the trauma’s impact on our body and mind. We never learn how to deal with the underlying emotions effectively.
Psychological Effects
Frequently, trauma’s psychological effects are noticed first and can disrupt the individual’s day-to-day life with depression, anxiety, anger, intense fear, flashbacks, and paranoia. The traumatic experience could also affect and alter perceptions. This can lead to the belief that the world around them is unsafe and other people are dangerous, or in extreme cases, create altered personalities to help them cope with the trauma. This leads us to post-traumatic stress disorder (PTSD), which is often triggered by witnessing or experiencing a shocking, dangerous or terrifying event, such as in a combat zone. “However, symptoms may not appear until several months or even years later,” according to the Anxiety and Depression Association of America. There are several leading indicators:
The traumatic experience could also affect and alter perceptions. This can lead to the belief that the world around them is unsafe and other people are dangerous, or in extreme cases, create altered personalities to help them cope with the trauma. This leads us to post-traumatic stress disorder (PTSD), which is often triggered by witnessing or experiencing a shocking, dangerous or terrifying event, such as in a combat zone. “However, symptoms may not appear until several months or even years later,” according to the Anxiety and Depression Association of America. There are several leading indicators:
- Re-experiencing the trauma through distressing memories of the event, flashbacks, and nightmares
- Emotional detachment and avoidance of places, people, and activities that are reminders of the trauma
- Increased arousal, such as difficulty sleeping and concentrating, feeling jumpy, and being easily irritated and angered
- Adverse changes in thinking and mood
What Are the Best Treatments?
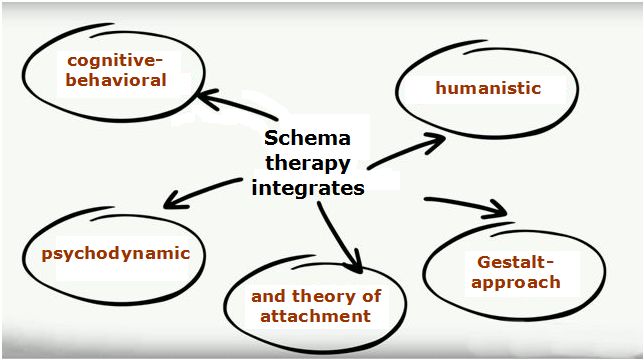
Trauma therapy is the first-line treatment in dealing with PTSD and trauma. Specifically, Cognitive Processing Therapy and Prolonged Exposure Therapy are evidence-based treatments to help individuals reduce PTSD symptoms. Research has shown that both treatments can significantly reduce PTSD symptoms after approximately 12 weeks (Lipov & Ritchie, 2015; Navaie, et al, 2014).
Specifically, Cognitive Processing Therapy and Prolonged Exposure Therapy are evidence-based treatments to help individuals reduce PTSD symptoms. Research has shown that both treatments can significantly reduce PTSD symptoms after approximately 12 weeks (Lipov & Ritchie, 2015; Navaie, et al, 2014).
Although not everyone who experiences trauma will develop PTSD, everyone who experiences trauma will have had their lives impacted significantly by the events. Yes, there are evidence-based treatments that can help, but sometimes more than the specific treatment, it is the relationship with a trusted provider that can make a big difference. Especially in a world where your trauma told you to think that the world and people are untrustworthy, having a stable, safe therapist can slowly shift you towards changing that schema.
Along with the specific treatments discussed above, it is essential to consider daily ways to reduce stress. One way of doing so is through mindfulness techniques. One easy way to employ mindfulness meditations into your day is by downloading an app such as Calm, Insight Timer, Headspace, or Breeth, which will guide you through mindfulness meditations. Doing these exercises every day and sometimes three times a day helps lower your overall physiological arousal and slowly shift to a calmer baseline.
One easy way to employ mindfulness meditations into your day is by downloading an app such as Calm, Insight Timer, Headspace, or Breeth, which will guide you through mindfulness meditations. Doing these exercises every day and sometimes three times a day helps lower your overall physiological arousal and slowly shift to a calmer baseline.
To find a mental health professional, visit Psychology Today's therapy directory.
Trauma Symptoms, Causes and Effects
Trauma is defined by the American Psychological Association (APA) as the emotional response someone has to an extremely negative event. While trauma is a normal reaction to a horrible event, the effects can be so severe that they interfere with an individual’s ability to live a normal life. In a case such as this, help may be needed to treat the stress and dysfunction caused by the traumatic event and to restore the individual to a state of emotional well-being.
What Are the Main Sources of Trauma?
Trauma can be caused by an overwhelmingly negative event that causes a lasting impact on the victim’s mental and emotional stability. While many sources of trauma are physically violent in nature, others are psychological. Some common sources of trauma include:
While many sources of trauma are physically violent in nature, others are psychological. Some common sources of trauma include:
- Rape
- Domestic violence
- Natural disasters
- Severe illness or injury
- The death of a loved one
- Witnessing an act of violence
Trauma is often but not always associated with being present at the site of a trauma-inducing event. It is also possible to sustain trauma after witnessing something from a distance. Young children are especially vulnerable to trauma and should be psychologically examined after a traumatic event has occurred to ensure their emotional well-being.
What Are the Signs of a Person Suffering from Trauma?
While the causes and symptoms of trauma are various, there are some basic signs of trauma that you can look out for. People who have endured traumatic events will often appear shaken and disoriented. They may not respond to conversation as they normally would and will often appear withdrawn or not present even when speaking.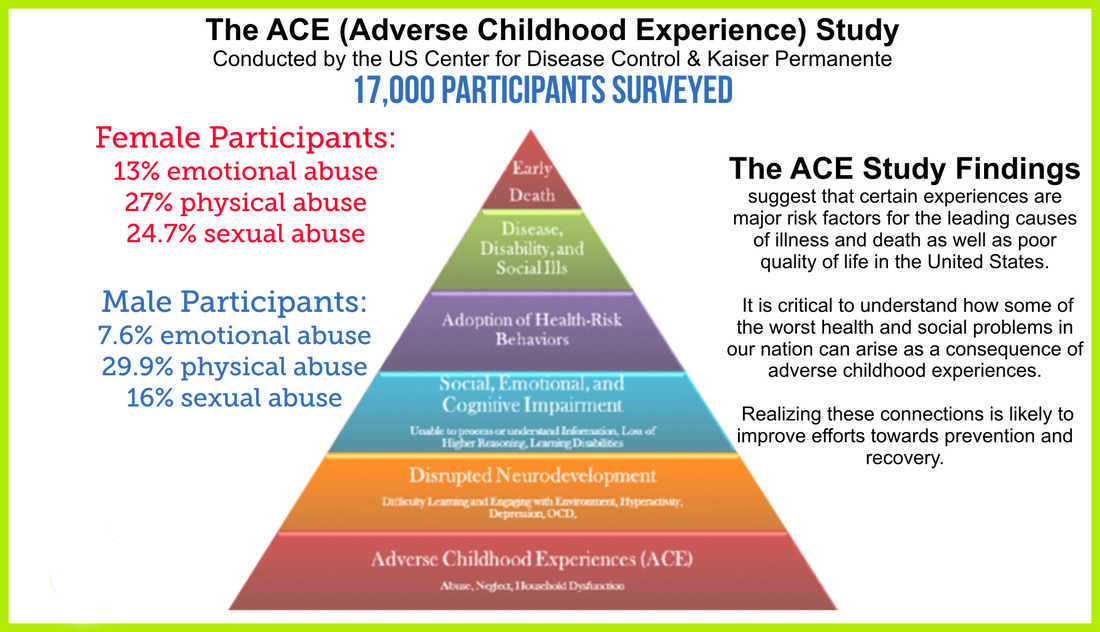
Don’t Face This Alone. Private, Professional Online Therapy Can Help You.
Find The Right Therapist For You Today
Another telltale sign of a trauma victim is anxiety. Anxiety due to trauma can manifest in problems such as night terrors, edginess, irritability, poor concentration and mood swings. While these symptoms of trauma are common, they are not exhaustive. Individuals respond to trauma in different ways. Sometimes trauma is virtually unnoticeable even to the victim’s closest friends and family. These cases illustrate the importance of talking to someone after a traumatic event has occurred, even if they show no initial signs of disturbance. Trauma can manifest days, months or even years after the actual event.
Emotional Symptoms of Trauma
Emotion is one of the most common ways in which trauma manifests. Some common emotional symptoms of trauma include denial, anger, sadness and emotional outbursts. Victim of trauma may redirect the overwhelming emotions they experience toward other sources, such as friends or family members. This is one of the reasons why trauma is difficult for loved ones as well. It is hard to help someone who pushes you away, but understanding the emotional symptoms that come after a traumatic event can help ease the process.
This is one of the reasons why trauma is difficult for loved ones as well. It is hard to help someone who pushes you away, but understanding the emotional symptoms that come after a traumatic event can help ease the process.
Physical Symptoms of Trauma
Trauma often manifests physically as well as emotionally. Some common physical signs of trauma include paleness, lethargy, fatigue, poor concentration and a racing heartbeat. The victim may have anxiety or panic attacks and be unable to cope in certain circumstances. The physical symptoms of trauma can be as real and alarming as those of physical injury or illness, and care should be taken to manage stress levels after a traumatic event.
Short-Term and Long-Term Effects of Trauma
All effects of trauma can take place either over a short period of time or over the course of weeks or even years. Any effects of trauma should be addressed immediately to prevent permanence. The sooner the trauma is addressed, the better chance a victim has of recovering successfully and fully.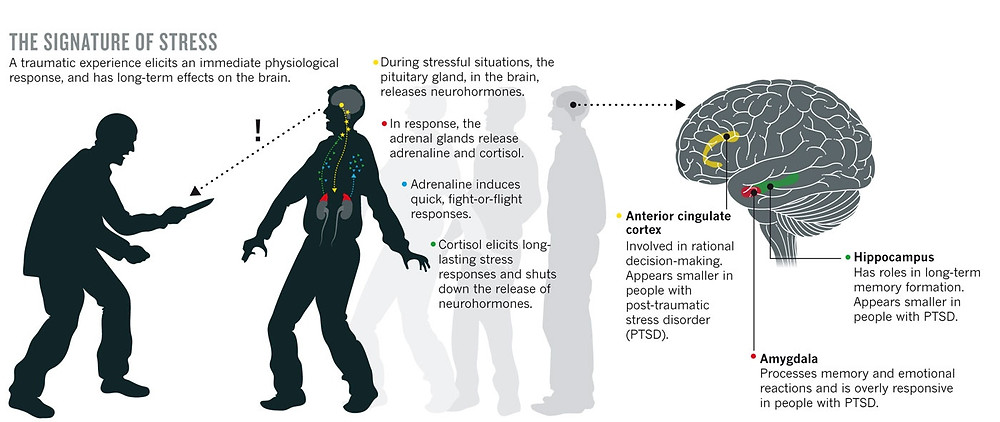
Short-term and long-term effects of trauma can be similar, but long-term effects are generally more severe. Short-term mood changes are fairly normal after trauma, but if the shifts in mood last for longer than a few weeks, a long-term effect can occur.
Is There a Test or Self-Assessment I Can Do?
While there are online assessments available for trauma, professional assessment is recommended over self-assessment. The victim or loved one will be biased and predisposed to see certain things, while a professional is objective and trained to compensate for bias.
If you would like more information on getting a professional assessment for yourself or a loved one who has experienced trauma, call our hotline at . Our friendly experts are available 24/7 to take your call and provide you with all the information you need to start your recovery.
Trauma Medication: Drug Options
While trauma, unlike some other mental disorders, is induced by an event or experience, it can be treated through the use of certain medications. Not all trauma requires medication, but it can be a useful tool in treating the symptoms of trauma, such as anxiety and depression. It is important to work with a healthcare professional to determine whether medication is necessary.
Not all trauma requires medication, but it can be a useful tool in treating the symptoms of trauma, such as anxiety and depression. It is important to work with a healthcare professional to determine whether medication is necessary.
Trauma Drugs: Possible Options
Drug options will depend on the individual’s psychological and medical history as well as the severity of the symptoms. If depression is severe and felt over an extended period of time, it may be treated with common antidepressant drugs. Clinical depression is defined as any depressive episode lasting longer than three months. Many trauma victims fall under the category of anxiety sufferers who are eligible for anti-anxiety medication.
Medication Side Effects
One of the considerations in whether or not to medicate for the symptoms of trauma is the presence of medication side effects. All medications have side effects, and the severity varies widely depending on drug class and individual body chemistry. Some side effects are more manageable than others, and potential negative side effects should always be compared to the potential benefit to the patient.
Some side effects are more manageable than others, and potential negative side effects should always be compared to the potential benefit to the patient.
Drug Addiction, Dependence and Withdrawal
Unfortunately, it is not uncommon for victims of trauma to turn to drugs as a means of self-medicating and coping with the effects of trauma. Government studies estimate that 25 percent of people experience trauma before the age of 16, and those individuals are much more likely to become addicted to drugs or alcohol.
Medication Overdose
Medication overdose occurs when someone ingests a significant enough amount of medication to cause physical harm. Overdose often occurs in conjunction with substance abuse, but it may be accidental and occur under regular circumstances. Any instance of overdose should be taken seriously, and professional help should be sought to ensure that an overdose does not reoccur and to determine if the cause is substance abuse.
Depression and Trauma
Depression and trauma have high comorbidity rates, and feelings of despair, malaise and sadness can last longer than a few days or even weeks.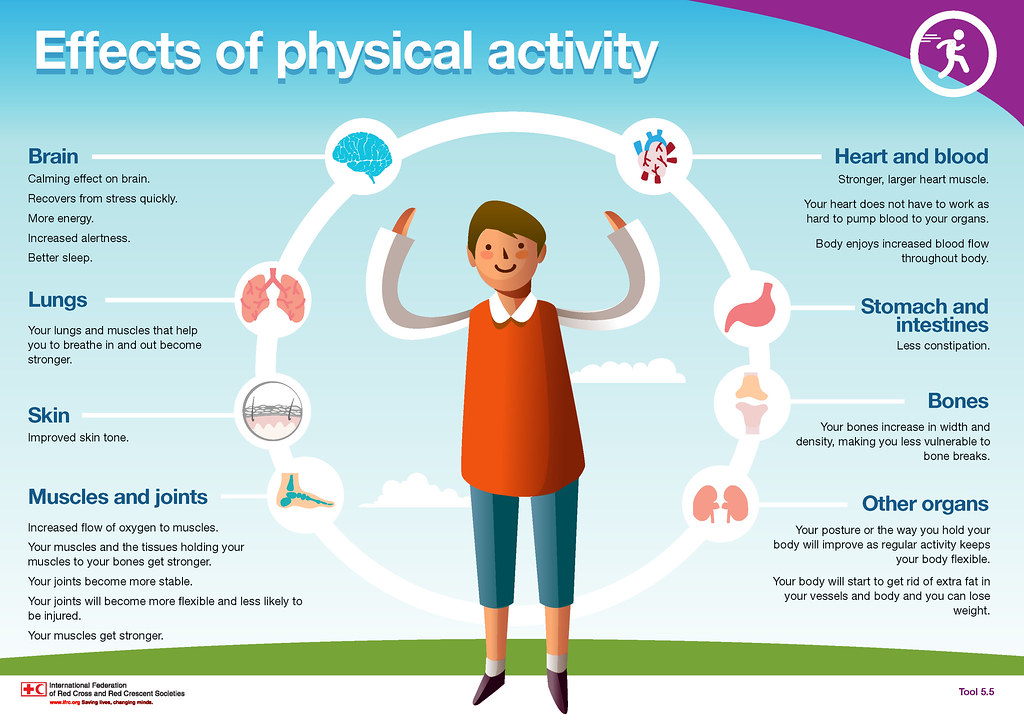 When a trauma occurs, post-traumatic stress disorder often occurs. The Department of Veteran Affairs estimates that depression is between three to five times more likely to occur in trauma victims who develop PTSD than in the general population.
When a trauma occurs, post-traumatic stress disorder often occurs. The Department of Veteran Affairs estimates that depression is between three to five times more likely to occur in trauma victims who develop PTSD than in the general population.
Dual Diagnosis: Addiction and Trauma
When the symptoms of PTSD, depression and anxiety become too much to cope with through normal means, many victims of trauma turn to substance abuse. As mentioned, victims are much more likely to develop addictions than other members of the general population. It is essential for the loved ones of a trauma victim to look out for the symptoms of addiction after trauma, even if the addiction is the only outward sign of PTSD.
Getting Help for Trauma-Related Issues
If you or a loved one is suffering from trauma, there is help available. With a variety of Trauma treatment options and caring professionals willing to help, the outlook for recovery is good. Often, people just need a little help with taking the first step.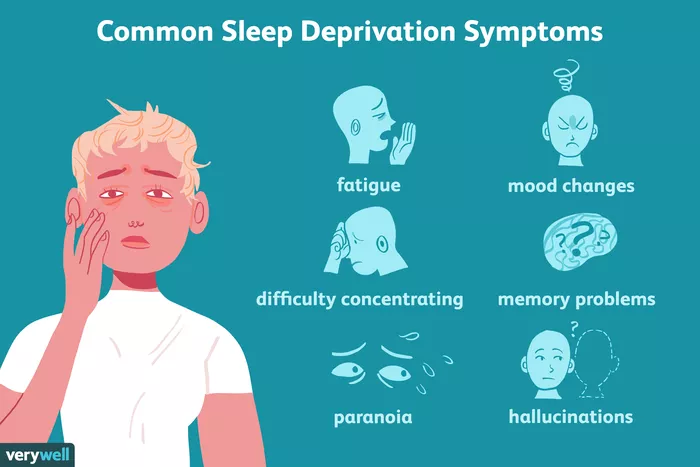 Our friendly representatives are available 24/7 to take your call and speak with you about getting help for trauma-related issues. Call our hotline at to start the journey toward recovery today.
Our friendly representatives are available 24/7 to take your call and speak with you about getting help for trauma-related issues. Call our hotline at to start the journey toward recovery today.
Rehabilitation after injuries (post-traumatic rehabilitation)
In the life of every person there are unexpected and unpleasant moments that lead to bruises, dislocations, bone fractures and damage to the musculoskeletal system.
Most of the injuries of the musculoskeletal system require surgical or conservative treatment. Successfully performed operation, correct reposition and cast is only the beginning of treatment. In most cases, patients who have suffered an injury require a complex of restorative measures. This is due to the fact that prolonged immobilization, lack of exercise, vascular and other changes lead to muscle atrophy, limited joint mobility, and trophic changes in the limb. The success of the treatment of an injury by more than half depends not only on the quality of the operation or reposition, but also on a well-performed post-traumatic rehabilitation .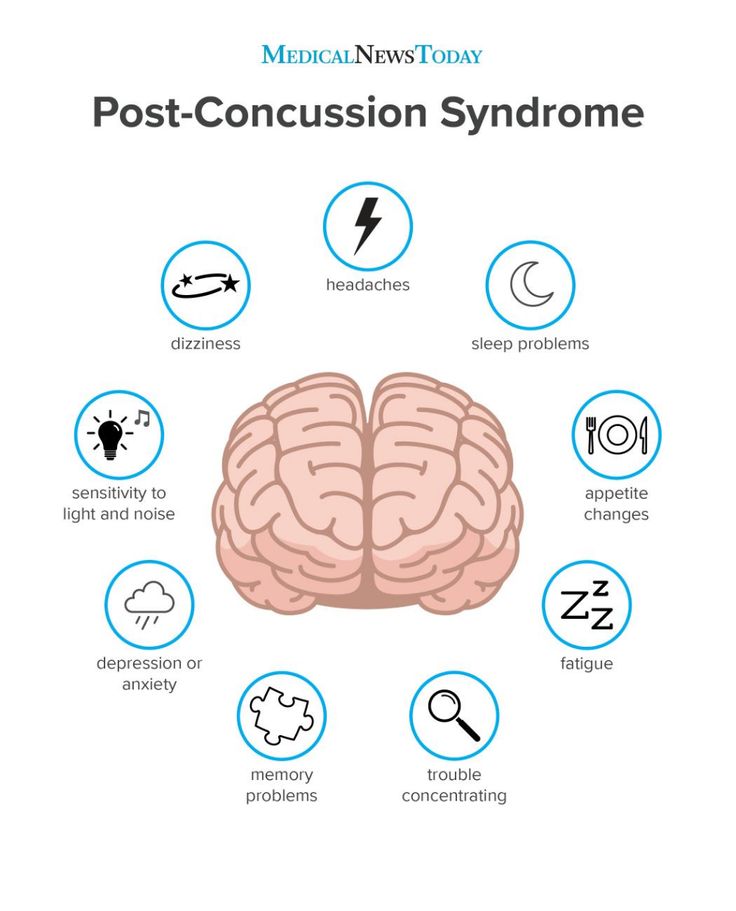 A fused fracture, reduced dislocation, does not always mean recovery. It often happens that the consolidation of the fracture has occurred, and the function of the limb is absent.
A fused fracture, reduced dislocation, does not always mean recovery. It often happens that the consolidation of the fracture has occurred, and the function of the limb is absent.
In domestic clinical medicine, one of the fundamental principles is anthropotherapy - the treatment of a sick person, proposed and developed by the luminaries of domestic science and practice M. Ya. Mudrov, G. A. Zakharyin, S. P. Botkin and others. , it is necessary to treat not only a fracture of a particular bone, but also a patient with a fracture, bearing in mind the various0005 injury and consequences of physical inactivity. At the heart of the development of many disorders of the body's activity and hypodynamia is a decrease in the intensity and even a perversion of kinesthetic stimuli, which leads to a violation of the dynamic stereotype of physiological functions, the basis of which are motor-visceral reflexes. This also includes the depressed state of the psyche, due to the severity of the injury, fear of consequences, pain syndrome.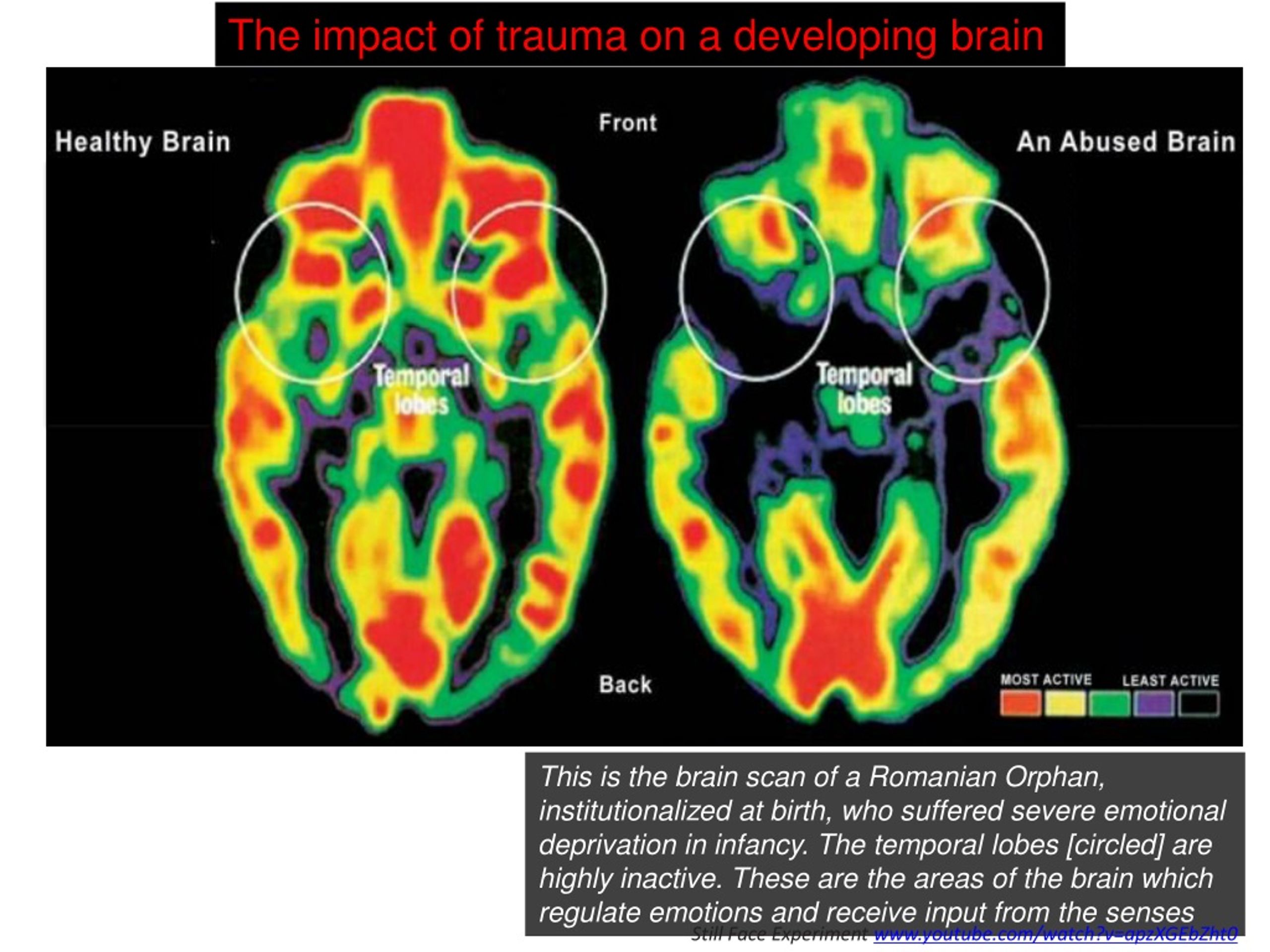
Significant changes occur in the activity of the circulatory organs. The blood circulation in the injury zone worsens due to the existing reflex muscle tension in this area, the stroke volume of the heart and the minute volume of blood circulation, the blood flow rate (especially in venules and small veins), the mass of circulating blood decrease, while its viscosity and coagulability increase. Ventilation deteriorates, the vital capacity of the lungs decreases, which affects primarily the central nervous system, which is most sensitive to ventilation disorders.
Hypodynamia slows down the resorption of the hematoma formed during trauma, adversely affects the state of the muscular system with the development of hypotension and malnutrition.
The degree of functional disorders depends on the location and severity of the damage, the method of fixation of bone fragments or the technique of surgical intervention, and the age of the patient.
The goal of restorative treatment is to achieve stable normalization of impaired human functions, as well as social functions and ability to work, in the appropriate time frame. Main methods rehabilitation after injuries are physiotherapy exercises (exercise therapy), manual therapy, massage, physiotherapy, mechanotherapy, labor therapy, psychotherapy.
Main methods rehabilitation after injuries are physiotherapy exercises (exercise therapy), manual therapy, massage, physiotherapy, mechanotherapy, labor therapy, psychotherapy.
An important role in the prevention and elimination of post-traumatic changes is played by physical exercises - specially organized for a specific purpose and strictly dosed movements. They are one of the important factors that support the vital activity of a healthy person and stimulate regenerative and compensatory mechanisms in the body of a sick person, since all adaptive processes are involved through the system of central regulations to ensure homeostasis.
IP Pavlov noted that movement is a natural function necessary for the existence of a person, affecting the entire body and relating to "the main reactive activity of the body."
Regular exercise creates dominant foci of excitation in the cerebral cortex, which, by the mechanism of negative induction, leads to suppression of foci of congestive excitation, i. e. eliminates "pain points".
e. eliminates "pain points".
The systematic use of physical exercises in the complex treatment of a patient eliminates the negative effect of physical inactivity on the body, has a versatile beneficial effect.
Rhythmic contraction and relaxation of skeletal muscles, tension and relaxation of tendons help to improve venous outflow, prevent venous stasis, and normalize microcirculation in tissues.
Physical exercise prevents the development of atrophy and degenerative changes in tissues and organs.
When choosing an exercise therapy technique, a number of factors must be taken into account. The nature and severity of injury , the stage of the pathological process, the physical and mental state of the patient, his physical fitness. A set of exercises should be compiled strictly individually, taking into account the phase of the process.
In the treatment of injuries of the musculoskeletal system, methods of physiotherapy are widely used. In the early stages after injuries, UHF, ultrasound, and magnetotherapy are used. This allows you to reduce swelling, improve microcirculation in the injured limb, and reduce pain. After the termination of immobilization, electrophoresis, phonophoresis with various drugs, laser therapy, electrical muscle stimulation are prescribed.
In the early stages after injuries, UHF, ultrasound, and magnetotherapy are used. This allows you to reduce swelling, improve microcirculation in the injured limb, and reduce pain. After the termination of immobilization, electrophoresis, phonophoresis with various drugs, laser therapy, electrical muscle stimulation are prescribed.
Massage and manual therapy allow you to strengthen muscles, make them more elastic, restore or increase the range of motion in the joints, correct muscle imbalance that occurs after a long forced position of the spine and limbs.
Rehabilitation treatment should begin as early as possible, rather than waiting for fracture consolidation, immobilization, or removal of sutures. In the best case, on the second or third day after injury or surgery. The earlier rehabilitation measures are started, the better the result.
MRC "Belyayevo" has a well-equipped gym, a physiotherapy department equipped with modern equipment, a diagnostic base, and qualified personnel.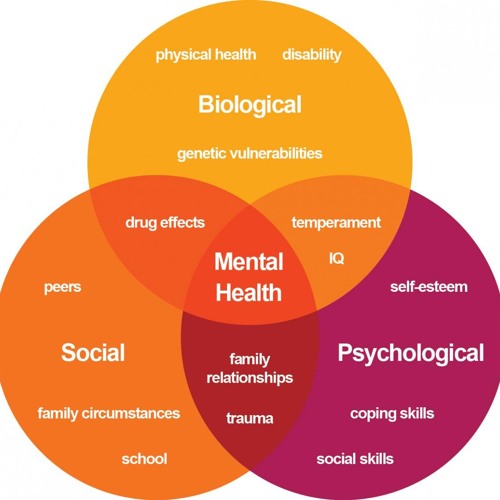 Treatment is carried out under the supervision of orthopedic traumatologists.
Treatment is carried out under the supervision of orthopedic traumatologists.
In the treatment of injuries and diseases of the musculoskeletal system, a modern method of immobilization "3M" using polymeric materials - "plastic gypsum" is used.
Injuries of the Central Nervous System -
Injuries of the Central Nervous System
In the majority of cases frequently occurring in our country, road traffic accidents cause serious injuries and damage to the central nervous system. In many countries of the world, injuries of the central nervous system occur in children, adolescents and young people and in most cases lead to death or disability. Accidents, a large proportion of which are traffic accidents, as well as falls, physical blows or other types of injuries, can lead to serious injuries to the brain, spinal cord, as well as their supporting systems and other body structures.
Head trauma
Scalp trauma:
If left untreated for a head injury, it can cause bleeding and later lead to shock.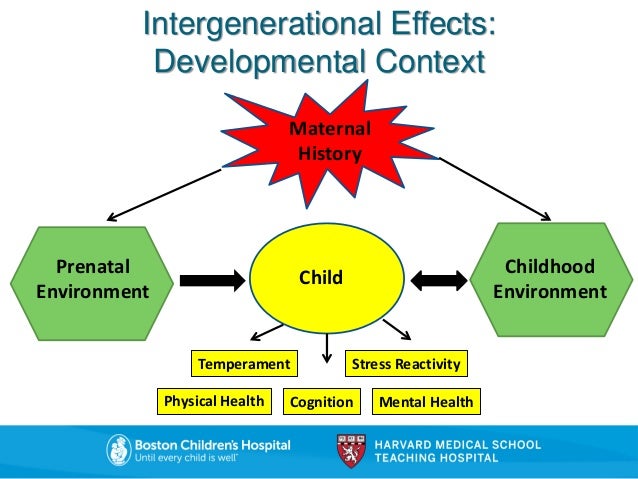 Bleeding can usually be controlled by applying a dressing or special clips attached to the scalp. Formed on the head, cuts or stab injuries should be closed as soon as possible. In the case of a penetrating skull fracture, the scalp tissue ruptures must be cleaned and treated in the operating room. Simple cuts to the scalp should be carefully cleaned and treated. If the wound has a small diameter, then its edges are closed or connected. In case of extensive injuries, the preferred method is the use of microsurgical techniques, thanks to which it is possible to suture the damaged area.
Bleeding can usually be controlled by applying a dressing or special clips attached to the scalp. Formed on the head, cuts or stab injuries should be closed as soon as possible. In the case of a penetrating skull fracture, the scalp tissue ruptures must be cleaned and treated in the operating room. Simple cuts to the scalp should be carefully cleaned and treated. If the wound has a small diameter, then its edges are closed or connected. In case of extensive injuries, the preferred method is the use of microsurgical techniques, thanks to which it is possible to suture the damaged area.
Injured scalp, if it loses its functionality, grafts can be used to close the damaged intact layer of the periosteum of patients. In such cases, the periosteum should be kept moist before surgery. In the absence of blood supply to the outer layer of the bone, its processing will be largely difficult. Any cuts or scalping injuries should be evaluated or managed by a neurosurgeon.
Fractures of the skull
Fractures of the skull are classified into the following types: fracture without damage to the skin (closed fracture), or in the event of tissue damage (open or compound fracture), fracture in only one line (linear fracture), fracture with multiple branches or lines of fractures (stellate fracture), or fragmentary (comminuted fracture) and / or a fracture in which the edges of the damaged segment are below the level of healthy bones (depressed) or the usual level (not depressed).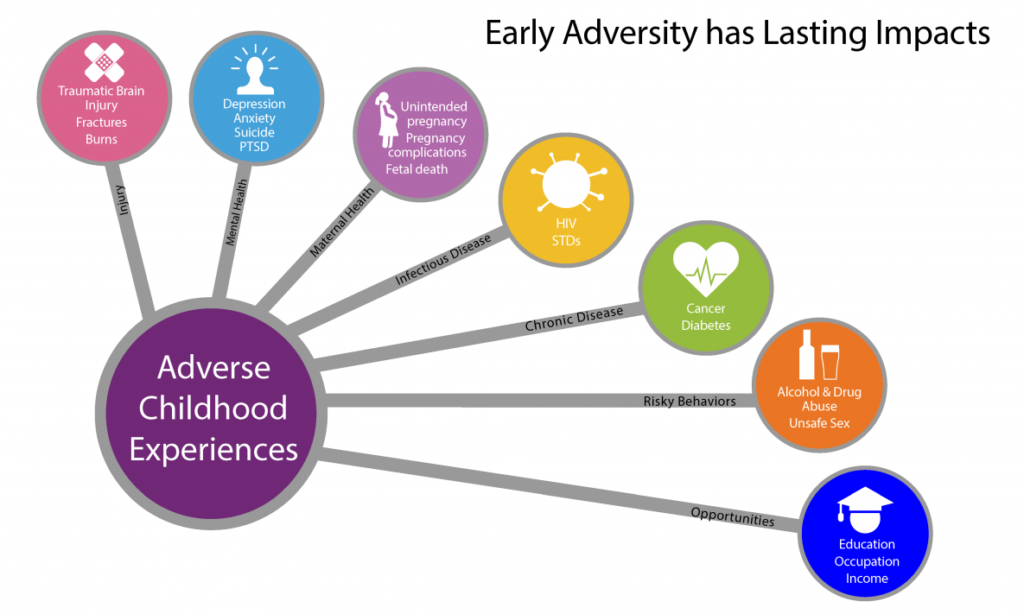
Simple skull fractures (linear, stellate or locally depressed) do not require special treatment. However, these injuries to the vascular channels or intracranial sinuses of the dura mater are potentially dangerous. In case of rupture of such channels, an epidural or subdural hematoma may occur. Simple skull fractures in which the sinuses or mastoid processes, being in contact with air, reach the mastoid air cells, such fractures are defined as "open".
Compression or depression fractures may require surgery, primarily to remove bone fragments. In the absence of any neurological signs during the operation, the dura mater should be examined and a planned operation to restore it should be performed.
Open skull fractures require surgery. For linear or stellate, (non-depressed) non-depressor-open fractures, the injured area should be debrided and covered after thorough cleaning. In case of severe damage to the lower bones with open fractures, a major operation with appropriate treatment is necessary.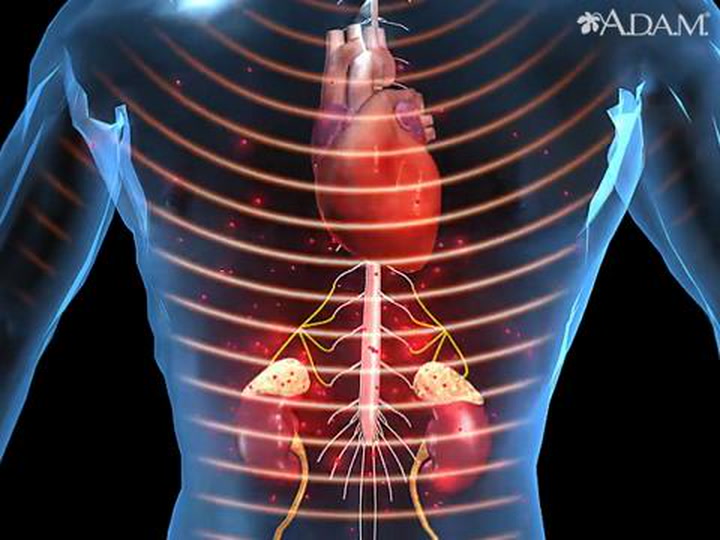 The dura mater of the brain must be examined in the most thorough manner. To prevent the risk of infection or leakage of cerebrospinal fluid (CSF), a fascial graft should be applied to the damaged area. After examining the dura mater and/or brain tissue, it is necessary to prepare and perform a craniotomy, during which appropriate procedures for an open fracture will be performed.
The dura mater of the brain must be examined in the most thorough manner. To prevent the risk of infection or leakage of cerebrospinal fluid (CSF), a fascial graft should be applied to the damaged area. After examining the dura mater and/or brain tissue, it is necessary to prepare and perform a craniotomy, during which appropriate procedures for an open fracture will be performed.
There may be bruising at the base of the fracture (traumatic goggles) or effect (bat ears). These clinical signs are observed more often in fractures of the anterior cranial and middle cranial fossa. In this type of fracture, isolated cranial nerve lesions located at the cranial nerve outlets may be seen. Depending on the tear or edema, the facial nerve is most often affected in craniocerebral fractures. Most lesions of the facial nerve resolve spontaneously and do not require any treatment. On the other hand, with complete damage to the facial nerve, serious surgical intervention is required.
In cases of rhinorrhea or nasal discharge of watery mucous secretion, treatment is necessary.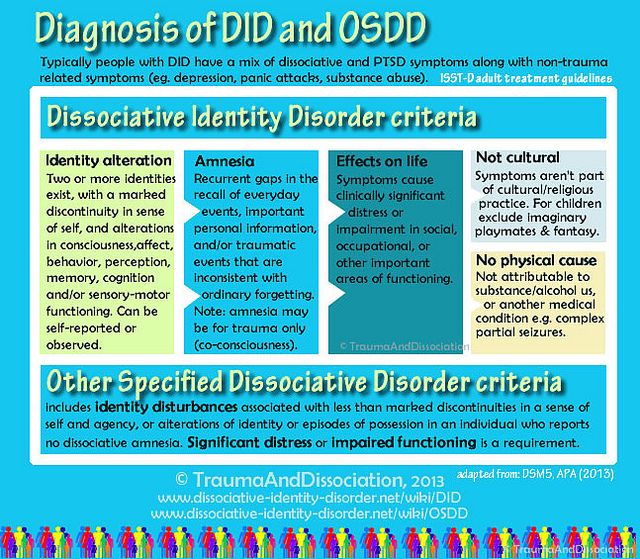 Traumatic discharge of CMF usually stops within the first 7 to 10 days. Such treatment must be carried out in a neurosurgical clinic.
Traumatic discharge of CMF usually stops within the first 7 to 10 days. Such treatment must be carried out in a neurosurgical clinic.
Penetrating Brain Injuries (Crush):
Penetrating Brain Injuries are caused by slowing, accelerating, rotating, or all of these simultaneously in connection with a blow. During the first stroke, neuronal and axonal breaks can form, which represent the primary injury. Complications that develop later, such as intracranial hematoma, cerebral edema, hypoxia, hypotension, hydrocephalus, or endocrine disorders, represent secondary injury.
Primary brain injury usually does not accompany mild head injury, and the neurological deficit is limited mainly to temporary loss of consciousness (concussion). On the other hand, in moderate to severe injuries, typical reversible or irreversible neurological deficits may be observed. In addition, injuries of this degree are usually accompanied by secondary brain damage.
Impacts that cause primary injury may be so severe that they can rupture capillaries, superficial subdural veins, or epidural arteries and veins, resulting in hematoma in the form of internal bleeding.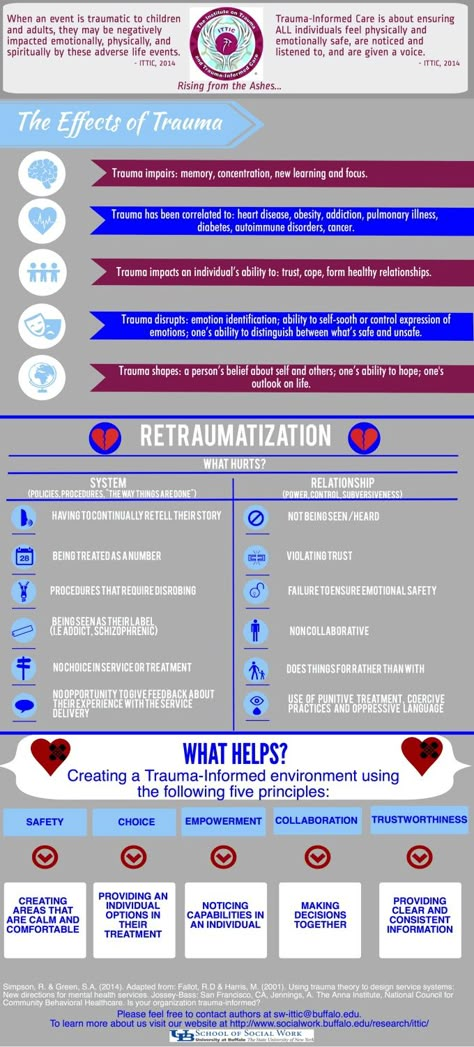 As a result of vasodilation and disruption of the blood-brain barrier, cerebral edema may occur. Ischemia associated with low blood pressure or anoxia can lead to cell death and cytotoxic edema. Mixing BOS with blood can lead to BOS malabsorption and hydrocephalus. The release of antidiuretic hormone or diabetes insipidius disturbs the fluid and electrolyte balance, and cerebral edema may increase even more. These changes, individually or combined, may result in an increase in ICP.
As a result of vasodilation and disruption of the blood-brain barrier, cerebral edema may occur. Ischemia associated with low blood pressure or anoxia can lead to cell death and cytotoxic edema. Mixing BOS with blood can lead to BOS malabsorption and hydrocephalus. The release of antidiuretic hormone or diabetes insipidius disturbs the fluid and electrolyte balance, and cerebral edema may increase even more. These changes, individually or combined, may result in an increase in ICP.
After a high ICP cerebral perfusion pressure (CPP) falls, secondary brain damage can occur. Elevated intercranial pressure is one of the most important factors affecting prognosis in head injuries. Therefore, aggressive treatment must be performed to prevent secondary brain damage when cerebral perfusion pressure falls. If possible, early intervention should be performed at the scene of the accident, with airway control and use of hyperventilation.
Emergency medical assistance is the basis for assessing the condition of the victim.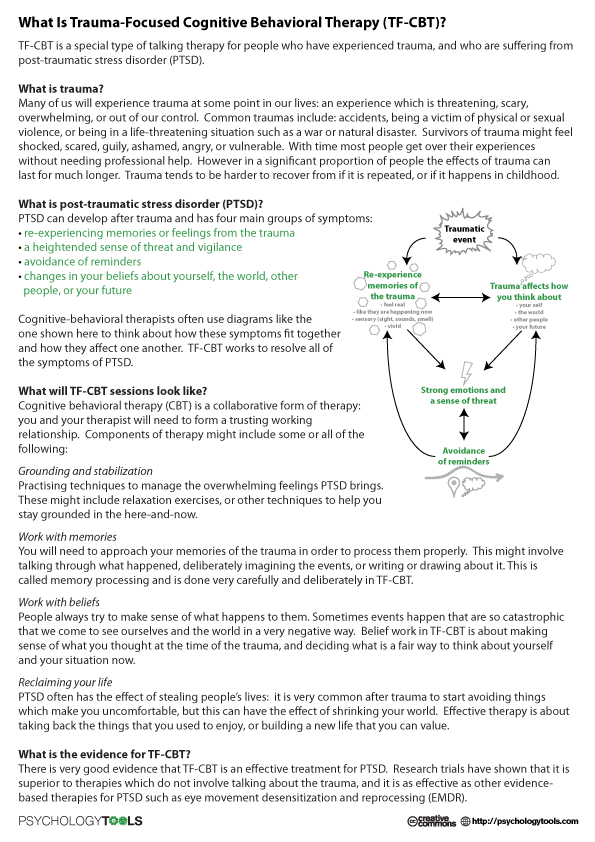 Despite the complexity of the overall neurological evaluation of patients who are unresponsive and non-cooperative, certain patient characteristics are critical.
Despite the complexity of the overall neurological evaluation of patients who are unresponsive and non-cooperative, certain patient characteristics are critical.
Patients who do not have headache, lethargy, or focal neurologic deficits are unlikely to develop a secondary complication as a result of head trauma. Imaging screening methods for asymptomatic patients are generally not performed. However, patients with or without focal neurologic deficits who also have severe symptoms should undergo computed tomography (CT).
Injuries of the spinal cord
Traumatic injuries of the spinal cord, fractures of the spine, dislocations with fractures, hyperextension in channels that were previously narrowed, can be observed with intervertebral herniation of disc material inside the channel, with gunshot wounds or stab wounds. Neurological deficits can be mild and temporary, or they can be severe and permanent. With or without the development of coma, in any head injury and multitrauma, a fracture or injury to the spine or spinal cord should always be suspected.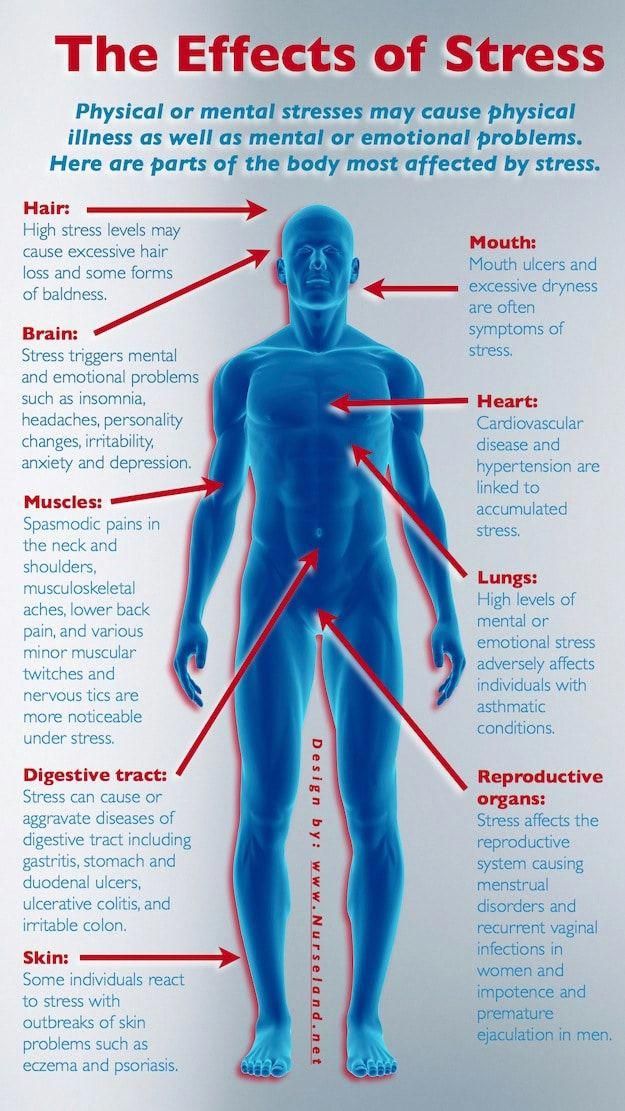 Assuming at first that the spine is unstable, the patient should be placed on a flat surface until a detailed examination and diagnosis can be made, in which case a stiff stretcher with neck support is best.
Assuming at first that the spine is unstable, the patient should be placed on a flat surface until a detailed examination and diagnosis can be made, in which case a stiff stretcher with neck support is best.
Clinical findings in injuries of the spine or spinal cord: spinal tenderness, loss of strength in the limbs, convulsions or paresthesia, respiratory failure and low blood pressure. If we are talking about clamping the nerve spinal endings, then in the corresponding myotome and dermatome, the loss of movement and sensitivity manifests itself in the form of a characteristic radiculopathy. When it comes to compression of the spinal cord, then various symptoms associated with developing myelopathy may appear
Complete tissue damage is expressed as a complete loss of movement and sensation below the level of functional damage, this is the manifestation of a complete anatomical or physiological incision. Under the level of damage to sharp incisions, areflexia, fluxidity, loss of sensation and autonomic paralysis appear.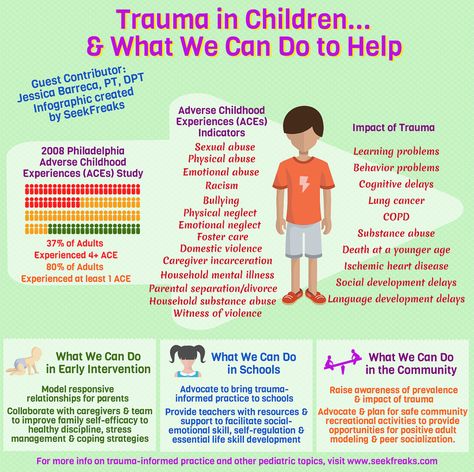 With all cuts above T5, there is a constant decrease in blood pressure, which develops in connection with the loss of sympathetic vascular tone.
With all cuts above T5, there is a constant decrease in blood pressure, which develops in connection with the loss of sympathetic vascular tone.
Incomplete spinal cord injury below the level of injury, along with loss of ipsilateral motor function and coordination/vibration sensation, as well as loss of pain sensation and temperature sensation, Brown Séquard syndrome may occur. Anatomically, this is due to a complete transverse lesion of the spinal cord. Central spinal syndrome is characterized mainly by paresis of the arms, weakness in the legs is less pronounced, there are varying degrees of sensitivity disturbance below the level of the lesion, urinary retention. In some cases, mainly with an injury accompanied by a sharp flexion of the spine, a syndrome of damage to the posterior cords of the spinal cord may develop - a loss of deep types of sensitivity.
Damage to the spinal cord (especially when its diameter is completely affected) is characterized by dysregulation of the functions of various internal organs: respiratory disorders in cervical lesions, intestinal paresis, dysfunction of the pelvic organs, trophic disorders with rapid development of bedsores.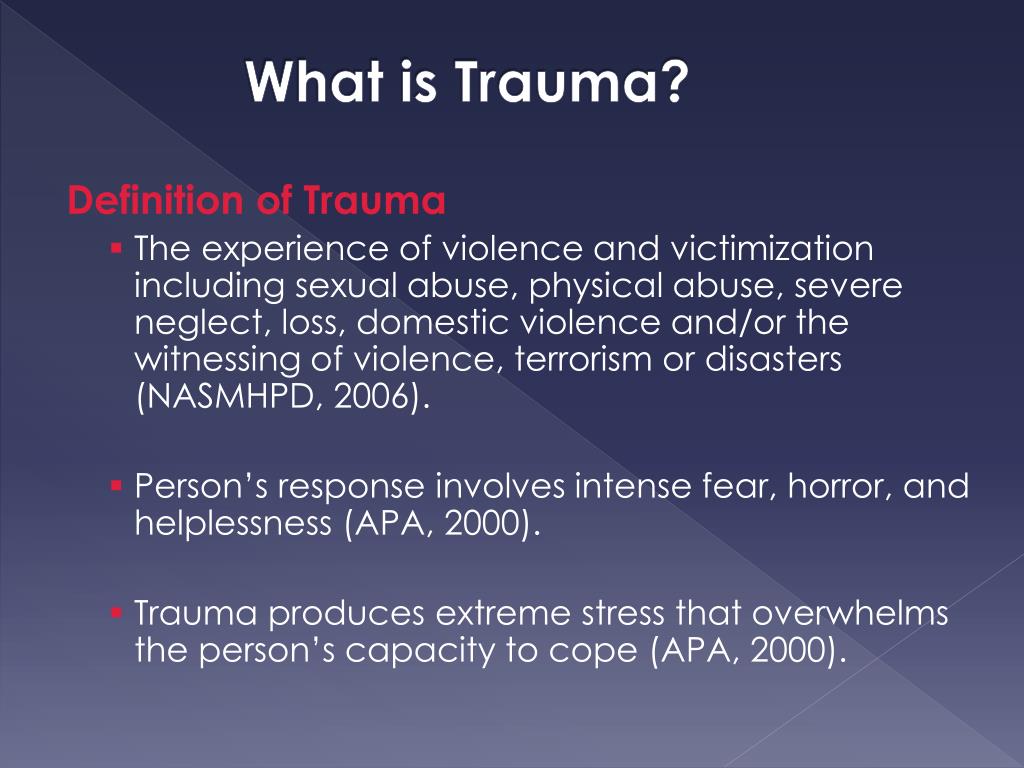
In the acute stage of injury, there are often violations of cardiovascular activity, a drop in blood pressure. With a fracture of the vertebrae, an external examination of the patient and the identification of such changes as concomitant damage to soft tissues, reflex muscle tension, sharp pain when pressing on the vertebrae, and finally, external deformation of the spine can have a certain value in its recognition.
There may be obstruction of gastric distention, which usually requires nasogastric drainage. Similarly, bladder distention occurs, which occurs due to contraction of the muscles of the bladder and pelvic floor. Bladder emptying adversely affects venous circulation and may lead to increased systemic hypotension of the inferior vena cava or by putting severe pressure on the pelvic veins, preventing excessive distention.
If the spinal cord injury is above T5, blood pressure is usually low. In this case, a denervation of the sympathetic nervous system is formed, which causes an increase in vein blockage and a weakening of venous circulation.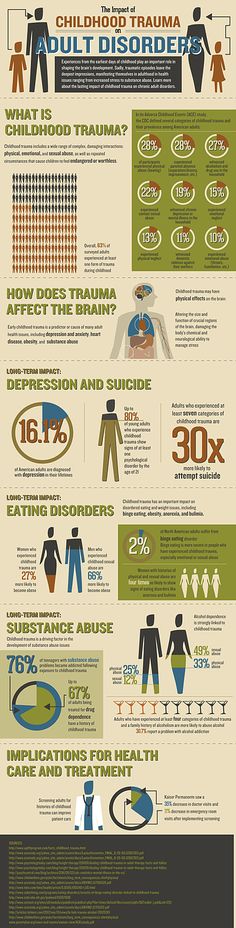
Tachycardia is a compensatory response to hypotension and is common in cervical spinal cord injury and bradycardia. If patients do not have symptoms of myocardial infarction or are at risk of stroke or paralysis due to other serious illnesses, this type of bradycardia does not need treatment.
After hemodynamic fixation is achieved, it is necessary to perform an X-ray of the patient's spine, who must stand motionless on a special spine fixation board with a rigid cervical collar attached. Ensure that the fixation is firm enough to ensure the accuracy of the resulting images. If the patient has multiple traumas and/or is in a coma, it is necessary to obtain clear images of his spine, which will fully display all segments of the spine. For a more detailed examination of fracture sites, CT scans can be performed, as well as axial and sagittal images. If no anomalies are detected on radiographs and at the same time, if there is a neurological deficit against the background of the spinal cord, then to detect damage to the intervertebral discs or spinal epidural hematoma after CT, the patient can be examined using MRI or myelography.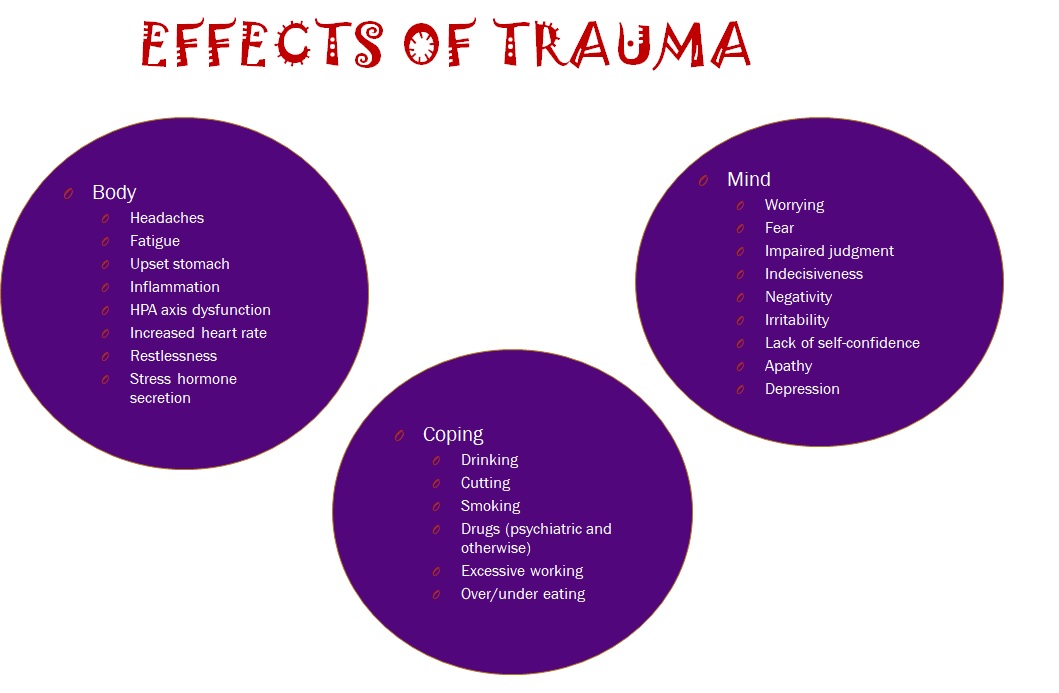
Treatment is aimed at correcting the structure of the spine, protecting the intact nervous tissue, restoring the nervous tissue and ensuring long-term stabilization of the spine. In this case, priority is given to the correction and fixation of displaced vertebrae or the elimination of any fractures or injuries of the spinal segments.
Vertebral misalignment can almost always be corrected in the neutral position with skeletal traction. In order to make sure that the vertebrae are built correctly, X-rays are often taken.
In patients with fractures of the lumbar spine, treatment begins primarily with fixation. At the same time, the fixation is not so tight compared to cervical fractures. Avoiding bending, stretching, rotation, the patient should lie motionless on a flat bed. There are generally far fewer systemic complications associated with neurological disorders, and yet vigilance must be exercised to ensure neurological recovery.
Indications for the need for early surgery in patients with spinal cord injury are: fractures/displacement that cannot be cured by closed surgical methods, neurological disorders in patients with local lesions; penetrating injuries that cause or do not cause CMF to leak or cause severe pressure on the spinal cord, or cause damage to channels imaged by MRI or myelography.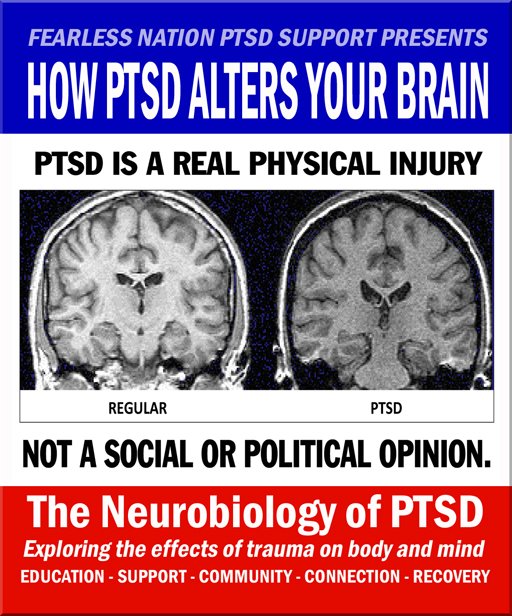 For open wounds, such as stab wounds and gunshot wounds, despite the fact that the spine is completely damaged, it is necessary to wash and treat and cover the injury very carefully. them or bruises. nye place even. whether or not wounds are cleaned and sealed. Reasons for early spinal stabilization surgery are justified. Because it provides the possibility of early mobilization and rehabilitation of the patient. Depending on the nature and extent of spinal injury, arthroscopic or a posterion methods may be used.
For open wounds, such as stab wounds and gunshot wounds, despite the fact that the spine is completely damaged, it is necessary to wash and treat and cover the injury very carefully. them or bruises. nye place even. whether or not wounds are cleaned and sealed. Reasons for early spinal stabilization surgery are justified. Because it provides the possibility of early mobilization and rehabilitation of the patient. Depending on the nature and extent of spinal injury, arthroscopic or a posterion methods may be used.
If repair with closed techniques has been successful and the fracture site has been secured, full recovery may require at least 3 months of stable external immobilization.
Stable external immobilization is also required for recovery surgery and/or when it is urgently needed. After the application of arthroscopic or a posterion plates, the use of a cervical collar will suffice. When fixing the lumbar spine, again, it is necessary, at least for 3 months, to ensure the immobility of the spine with a plastic jacket or a plastic-gypsum fixator.